*NURSING > NCLEX-RN > C H A P T E R 1 0 Vital Signs and Laboratory Reference Intervals: From Saunders Comprehensive Review (All)
C H A P T E R 1 0 Vital Signs and Laboratory Reference Intervals: From Saunders Comprehensive Review for the NCLEX-RN Examination 8th Edition. (Available: https://bit.ly/2HeJuMt ). Contains Practice questions and Answers with the Rationale, Test-Taking Strategy, Level of Cognitive Ability, Client Needs, Integrated Process, Content Area, Health Problem, Priority Concepts and Reference
Document Content and Description Below
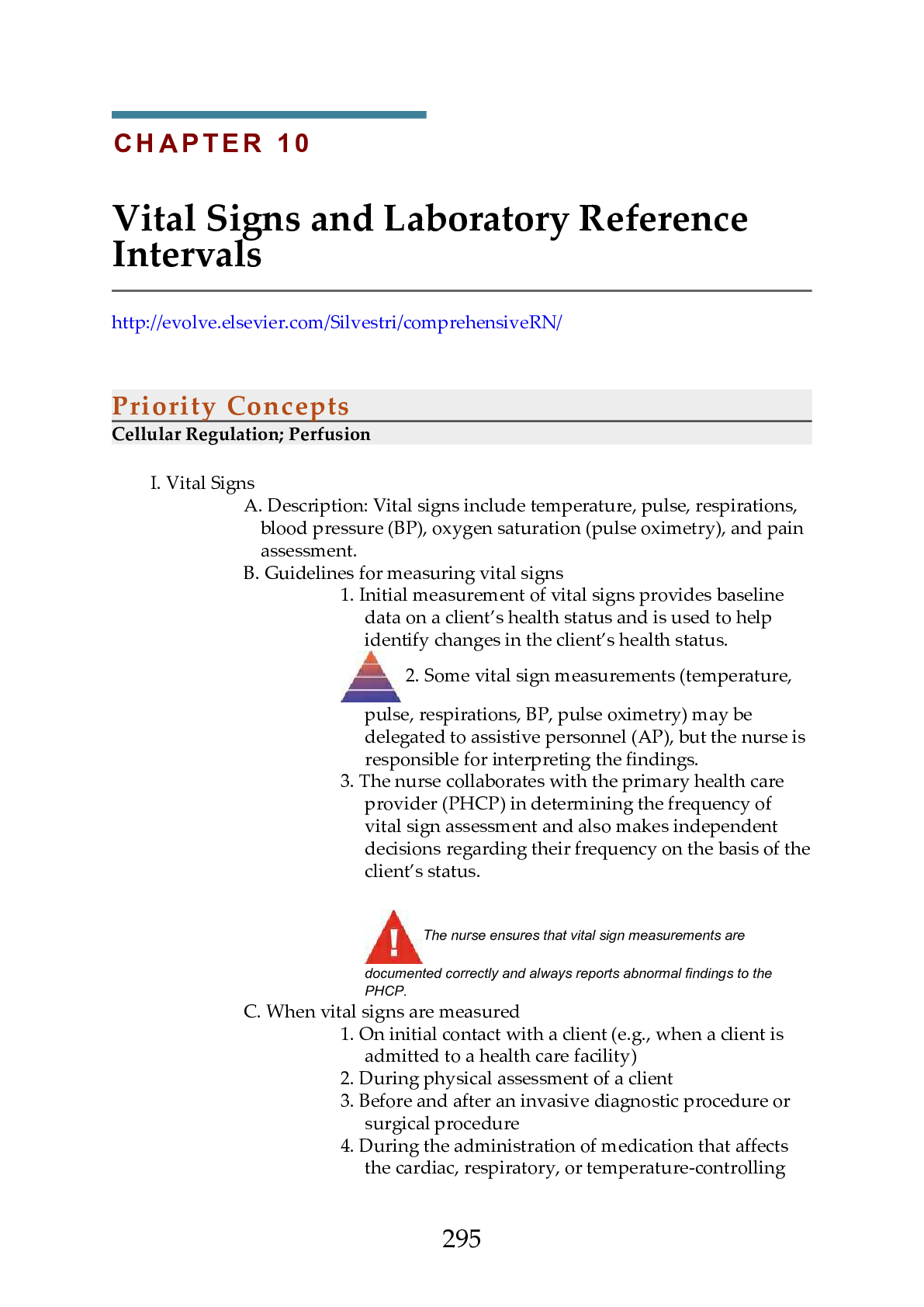
Priority Concepts Cellular Regulation; Perfusion I. Vital Signs A. Description: Vital signs include temperature, pulse, respirations, blood pressure (BP), oxygen saturation (pulse oximetry), and p... ain assessment. B. Guidelines for measuring vital signs 1. Initial measurement of vital signs provides baseline data on a client’s health status and is used to help identify changes in the client’s health status. 2. Some vital sign measurements (temperature, pulse, respirations, BP, pulse oximetry) may be delegated to assistive personnel (AP), but the nurse is responsible for interpreting the findings. 3. The nurse collaborates with the primary health care provider (PHCP) in determining the frequency of vital sign assessment and also makes independent decisions regarding their frequency on the basis of the client’s status. The nurse ensures that vital sign measurements are documented correctly and always reports abnormal findings to the PHCP. C. When vital signs are measured 1. On initial contact with a client (e.g., when a client is admitted to a health care facility) 2. During physical assessment of a client 3. Before and after an invasive diagnostic procedure or surgical procedure 4. During the administration of medication that affects the cardiac, respiratory, or temperature-controlling 295functions (e.g., in a client who has a fever); may be required before, during, and after administration of the medication 5. Before, during, and after a blood transfusion 6. Whenever a client’s condition changes or the client verbalizes unusual feelings such as nonspecific symptoms of physical distress (i.e., feeling funny or different) 7. Whenever an intervention (e.g., ambulation) may affect a client’s condition 8. When a fever or known infection is present (check vital signs every 2 to 4 hours) II. Temperature A. Description 1. Normal body temperature ranges from 36.4° to 37.5° Celsius (C) (97.5° to 99.5° Fahrenheit [F]); the average in a healthy young adult is 37.0° C (98.6° F). 2. Common measurement sites are the mouth, rectum (unless contraindicated), axilla, ear, and across the forehead (temporal artery site); various types of electronic measuring devices are commonly used to measure temperature. 3. Rectal temperatures are usually 1° F (0.5° C) higher and tympanic and axillary temperatures about 1° F (0.5° C) lower than the normal oral temperature. 4. Know how to convert a temperature to a Fahrenheit or Celsius value (Box 10-1). B. Nursing considerations 1. Time of day a. Temperature is generally in the lownormal range at the time of awakening as a result of muscle inactivity. b. Afternoon body temperature may be high-normal as a result of the metabolic process, activity, and environmental temperature. 2. Environmental temperature: Body temperature is lower in cold weather and higher in warm weather. 3. Age: Temperature may fluctuate during the first year of life because the infant’s heat-regulating mechanism is not fully developed. 4. Physical exercise: Use of the large muscles creates heat, causing an increase in body temperature. 5. Menstrual cycle: Temperature decreases slightly just before ovulation but may increase to 1° F above normal during ovulation. 6. Pregnancy: Body temperature may consistently stay at high-normal because of an increase in the woman’s 296metabolic rate. 7. Stress: Emotions increase hormonal secretion, leading to increased heat production and a higher temperature. 8. Illness: Infective agents and the inflammatory response may cause an increase in temperature. 9. The inability to obtain a temperature should not be ignored, because it could represent a condition of hypothermia, a life-threatening condition in very young and older clients. C. Methods of measurement 1. Oral a. If the client has recently consumed hot or cold foods or liquids or has smoked or chewed gum, the nurse must wait 15 to 30 minutes before taking the temperature orally. b. The thermometer is placed under the tongue in one of the posterior sublingual pockets; ask the client to keep the tongue down and the lips closed and to not bite down on the thermometer. 2. Rectal a. Place the client in the Sims’ position. b. The temperature is taken rectally when an accurate temperature cannot be obtained orally or via other methods including by an electronic method, or when the client has nasal congestion, has undergone nasal or oral surgery or had the jaws wired, has a nasogastric tube in place, is unable to keep the mouth closed, or is at risk for seizures. c. The thermometer is lubricated and inserted into the rectum, toward the umbilicus, about 1.5 inches (3.8 cm) (no more than 0.5 inch [1.25 cm] in an infant). The temperature is not taken rectally in cardiac clients; the client who has undergone rectal surgery; or the client with diarrhea, fecal impaction, or rectal bleeding or who is at risk for bleeding. 3. Axillary a. This method of taking the temperature 297is used when the oral or other methods of temperature measurement are contraindicated. b. Axillary measurement is not as accurate as the oral, rectal, tympanic, or temporal artery method but is used when other methods of measurement are not possible. c. The thermometer is placed in the client’s dry axilla, and the client is asked to hold the arm tightly against the chest, resting the arm on the chest; follow the instructions accompanying the measurement device for the amount of time the thermometer should remain in the axillary area. 4. Tympanic a. The auditory canal is checked for the presence of redness, swelling, discharge, or a foreign body before the probe is inserted; the probe should not be inserted if the client has an inflammatory condition of the auditory canal or if there is discharge from the ear. b. The reading may be affected by an ear infection or excessive wax blocking the ear canal. 5. Temporal artery a. Ensure that the client’s forehead is dry. b. The thermometer probe is placed flush against the skin and slid across the forehead or placed in the area of the temporal artery and held in place. c. If the client is diaphoretic, the temporal artery thermometer probe may be placed on the neck, just behind the earlobe. III. Pulse A. Description 1. Pulse is a palpable bounding of blood flow in a peripheral artery; it is an indirect indicator of circulatory status. 2. The average adult pulse (heart) rate is 60 to 100 beats per minute. 3. Changes in pulse rate are used to evaluate the client’s tolerance of interventions such as ambulation, 298bathing, dressing, and exercise. 4. Pedal pulses are checked to determine whether the circulation is blocked in the artery up to that pulse point. 5. When the pedal pulse is difficult to locate, a Doppler ultrasound stethoscope (ultrasonic stethoscope) may be needed to amplify the sounds of pulse waves. B. Nursing considerations 1. The heart rate slows with age. 2. Exercise increases the heart rate. 3. Emotions stimulate the sympathetic nervous system, increasing the heart rate. 4. Pain increases the heart rate. 5. Increased body temperature causes the heart rate to increase. 6. Stimulant medications increase the heart rate; depressants and medications affecting the cardiac system slow it. 7. When the BP is low, the heart rate is usually increased. 8. Hemorrhage increases the heart rate. C. Assessing pulse qualities 1. When the pulse is being counted, note the rate, rhythm, strength (force or amplitude), and equality. 2. Once you have checked these parameters, use the grading scale for pulses to assess the information you have elicited (Box 10-2). D. Pulse points and locations 1. The temporal artery can be palpated anterior to or in the front of the ear. 2. The carotid artery is located in the groove between the trachea and the sternocleidomastoid muscle, medial to and alongside the muscle. 3. The apical pulse may be detected at the left midclavicular, fifth intercostal space. 4. The brachial pulse is located above the elbow at the antecubital fossa, between the biceps and triceps muscles. 5. The radial pulse is located in the groove along the radial or thumb side of the client’s inner wrist. 6. The ulnar pulse is located on the medial side of the wrist (little finger side of the forearm at the wrist). 7. The femoral pulse is located below the inguinal ligament, midway between the symphysis pubis and the anterosuperior iliac spine. 8. The popliteal pulse is located behind the knee. 9. The posterior tibial pulse is located on the inner side of the ankle, behind and below the medial malleolus 299(ankle bone). 10. The dorsalis pedis pulse is located on the top of the foot, in line with the groove between the extensor tendons of the great and first toes. The apical pulse is counted for 1 full minute and is assessed in clients with an irregular radial pulse or a heart condition, before the administration of cardiac medications such as digoxin and beta blockers, and in children younger than 2 years. E. Pulse deficit 1. In this condition, the peripheral pulse rate (radial pulse) is less than the ventricular contraction rate (apical pulse). 2. A pulse deficit indicates a lack of peripheral perfusion; it can be an indication of cardiac dysrhythmias. 3. One-examiner technique: Auscultate and count the apical pulse first and then immediately count the radial pulse. 4. Two-examiner technique: One person counts the apical pulse and the other counts the radial pulse simultaneously. 5. A pulse deficit indicates that cardiac contractions are ineffective, failing to send pulse waves to the periphery. 6. If a difference in pulse rate is noted, the PHCP is notified. IV. Respirations A. Description 1. Respiration is a mechanism the body uses to exchange gases between the atmosphere and the blood and between the blood and the cells. 2. Respiratory rates vary with age. 3. The normal adult respiratory rate is 12 to 20 breaths per minute. B. Nursing considerations 1. Many of the factors that affect the pulse rate also affect the respiratory rate. 2. An increased level of carbon dioxide or a lower level of oxygen in the blood results in an increase in respiratory rate. 3. Head injury or increased intracranial pressure will depress the respiratory center in the brain, resulting in shallow respirations or slowed breathing. 4. Medications such as opioid analgesics depress respirations. 5. Additional factors that can affect the respiratory rate 300include exercise, pain, anxiety, smoking, and body position. C. Assessing respiratory rate 1. Count the client’s respirations after measuring the radial pulse. (Continue holding the client’s wrist while counting the respirations or position the hand on the client's chest.) 2. One respiration includes both inspiration and expiration. 3. The rate, depth, pattern, and sounds are assessed. The respiratory rate may be counted for 30 seconds and multiplied by 2, except in a client who is known to be very ill or is exhibiting irregular respirations, in which case respirations are counted for 1 full minute. V. Blood Pressure A. Description 1. Blood pressure (BP) is the force on the walls of an artery exerted by the pulsating blood under pressure from the heart. 2. The heart’s contraction forces blood under high pressure into the aorta; the peak of maximum pressure when ejection occurs is the systolic pressure; the blood remaining in the arteries when the ventricles relax exerts a force known as the diastolic pressure. 3. The difference between the systolic and diastolic pressures is called the pulse pressure. 4. For an adult (age 18 years and older), a normal BP is a systolic pressure below 120 mm Hg and a diastolic pressure below 80 mm Hg. 5. Categories of hypertension (Box 10-3). 6. In postural (orthostatic) hypotension, a normotensive client exhibits symptoms and low BP on rising to an upright position. 7. To obtain orthostatic vital sign measurements, check the BP and pulse with the client supine, sitting, and standing; readings are obtained 1 to 3 minutes after the client changes position. B. Nursing considerations 1. Factors affecting BP a. BP tends to increase as the aging process progresses. b. Stress results in sympathetic 301 Practice Questions 64. A client with atrial fibrillation who is receiving maintenance therapy of warfarin sodium has a prothrombin time (PT) of 35 seconds. On the basis of these laboratory values, the nurse anticipates which prescription? 1. Adding a dose of heparin sodium 2. Holding the next dose of warfarin 3. Increasing the next dose of warfarin 4. Administering the next dose of warfarin 65. A staff nurse is precepting a new graduate nurse and the new graduate is assigned to care for a client with chronic pain. Which statement, if made by 323the new graduate nurse, indicates the need for further teaching regarding pain management? 1. “I will be sure to ask my client what his pain level is on a scale of 0 to 10.” 2. “I know that I should follow up after giving medication to make sure it is effective.” 3. “I will be sure to cue in to any indicators that the client may be exaggerating their pain.” 4. “I know that pain in the older client might manifest as sleep disturbances or depression.” 66. A client has been admitted to the hospital for gastroenteritis and dehydration. The nurse determines that the client has received adequate volume replacement if the blood urea nitrogen (BUN) level drops to which value? 1. 3 mg/dL (1.08 mmol/L) 2. 15 mg/dL (5.4 mmol/L) 3. 29 mg/dL (10.44 mmol/L) 4. 35 mg/dL (12.6 mmol/L) 67. The nurse is explaining the appropriate methods for measuring an accurate temperature to an assistive personnel (AP). Which method, if noted by the UAP as being an appropriate method, indicates the need for further teaching? 1. Taking a rectal temperature for a client who has undergone nasal surgery 2. Taking an oral temperature for a client with a cough and nasal congestion 3. Taking an axillary temperature for a client who has just consumed hot coffee 4. Taking a temperature on the neck behind the ear using an electronic device for a client who is diaphoretic 68. A client is receiving a continuous intravenous infusion of heparin sodium to treat deep vein thrombosis. The client’s activated partial thromboplastin time (aPTT) is 65 seconds. The nurse anticipates that which action is needed? 1. Discontinuing the heparin infusion 2. Increasing the rate of the heparin infusion 3. Decreasing the rate of the heparin infusion 4. Leaving the rate of the heparin infusion as is 69. 69. A client with a history of heart failure is due for a morning dose of furosemide. Which serum potassium level, if noted in the client’s laboratory report, should be reported before administering the dose of furosemide? 1. 3.2 mEq/L (3.2 mmol/L) 2. 3.8 mEq/L (3.8 mmol/L) 3. 2 mEq/L (4.2 mmol/L) 4. 8 mEq/L (4.8 mmol/L) 70. Several laboratory tests are prescribed for a client, and the nurse reviews the results of the tests. Which laboratory test results should the nurse report? Select all that apply. 3241. Platelets 35,000 mm3 (35 × 109/L) 2. Sodium 150 mEq/L (150 mmol/L) 3. Potassium 5.0 mEq/L (5.0 mmol/L) 4. Segmented neutrophils 40% (0.40) 5. Serum creatinine, 1 mg/dL (88.3 mcmol/L) 6. White blood cells, 3000 mm3 (3.0 × 109/L) 71. The nurse is caring for a client who takes ibuprofen for pain. The nurse is gathering information on the client’s medication history and determines it is necessary to contact the primary health care provider (PHCP) if the client is also taking which medications? Select all that apply. 1. Warfarin 2. Glimepiride 3. Amlodipine 4. Simvastatin 5. Atorvastatin 72. A client with diabetes mellitus has a glycosylated hemoglobin A1c level of 8%. On the basis of this test result, the nurse plans to teach the client about the need for which measure? 1. Avoiding infection 2. Taking in adequate fluids 3. Preventing and recognizing hypoglycemia 4. Preventing and recognizing hyperglycemia 73. The nurse is caring for a client with a diagnosis of breast cancer who is immunosuppressed. The nurse would consider implementing neutropenic precautions if the client’s white blood cell count was which value? 1. 2000 mm3 (2.0 × 109/L) 2. 5800 mm3 (5.8 × 109/L) 3. 8400 mm3 (8.4 × 109/L) 4. 11,500 mm3 (11.5 × 109/L) 74. A client brought to the emergency department states that he has accidentally been taking 2 times his prescribed dose of warfarin for the past week. After noting that the client has no evidence of obvious bleeding, the nurse plans to take which action? 1. Prepare to administer an antidote. 2. Draw a sample for type and crossmatch and transfuse the client. 3. Draw a sample for an activated partial thromboplastin time (aPTT) level. 4. Draw a sample for prothrombin time (PT) and international normalized ratio (INR). 75. The nurse is caring for a postoperative client who is receiving demand-dose hydromorphone via a patient-controlled analgesia (PCA) pump for pain 325control. The nurse enters the client’s room and finds the client drowsy and records the following vital signs: temperature 97.2° F (36.2° C) orally, pulse 52 beats per minute, blood pressure 101/58 mm Hg, respiratory rate 11 breaths per minute, and SpO2 of 93% on 3 liters of oxygen via nasal cannula. Which action should the nurse take next? 1. Document the findings. 2. Attempt to arouse the client. 3. Contact the primary health care provider (PHCP) immediately. 4. Check the medication administration history on the PCA pump. 76. An adult female client has a hemoglobin level of 10.8 g/dL (108 mmol/L). The nurse interprets that this result is most likely caused by which condition noted in the client’s history? 1. Dehydration 2. Heart failure 3. Iron deficiency anemia 4. Chronic obstructive pulmonary disease 77. A client with a history of upper gastrointestinal bleeding has a platelet count of 300,000 mm3 (300 × 109/L). The nurse should take which action after seeing the laboratory results? 1. Report the abnormally low count. 2. Report the abnormally high count. 3. Place the client on bleeding precautions. 4. Place the normal report in the client’s medical record. [Show More]
Last updated: 1 year ago
Preview 1 out of 38 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Oct 22, 2020
Number of pages
38
Written in
Additional information
This document has been written for:
Uploaded
Oct 22, 2020
Downloads
0
Views
102