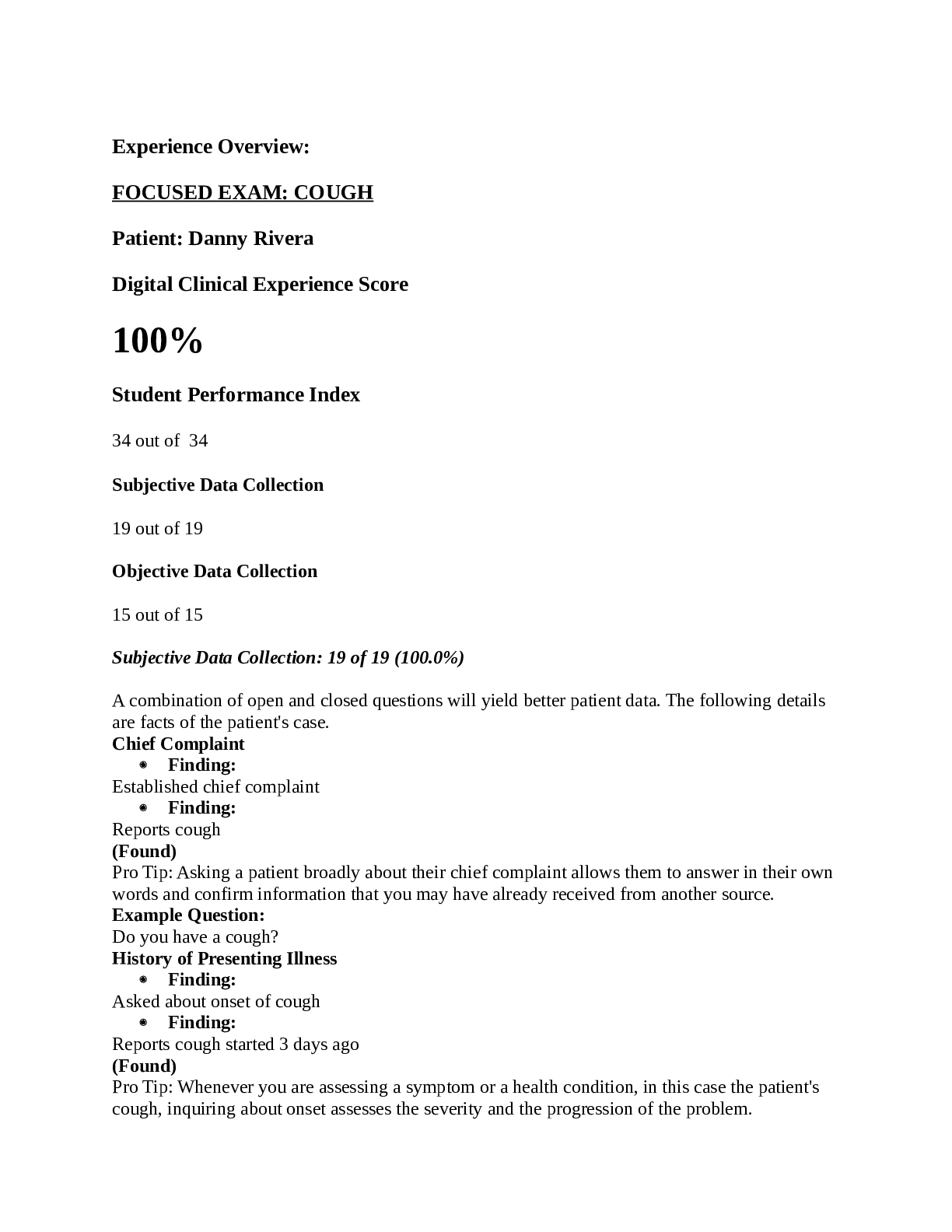
*NURSING > SHADOW HEALTH > FOCUSED EXAM: COUGH Patient: Danny Rivera Digital Clinical Experience Score 100% Student Performance (All)
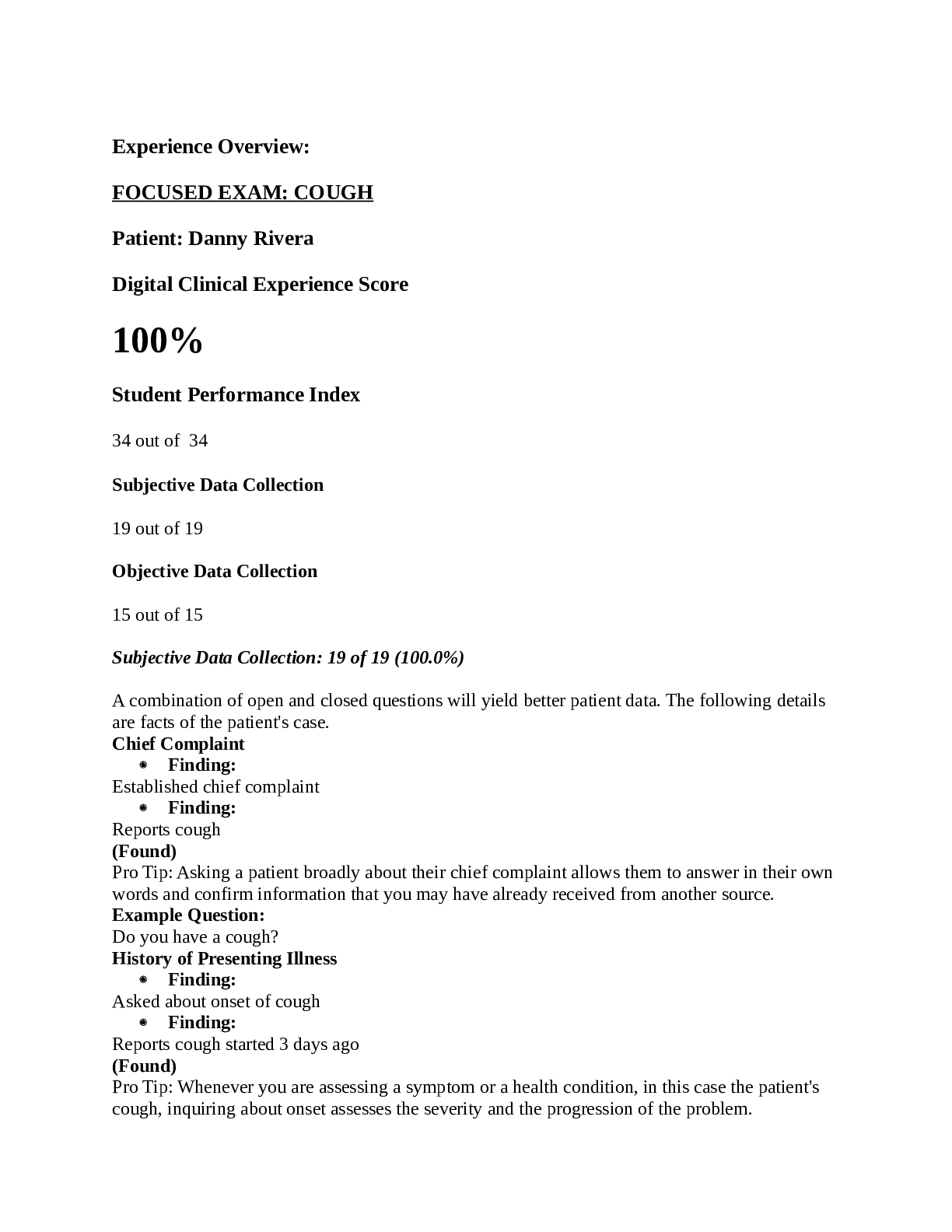
FOCUSED EXAM: COUGH Patient: Danny Rivera Digital Clinical Experience Score 100% Student Performance Index 34 out of 34
Document Content and Description Below
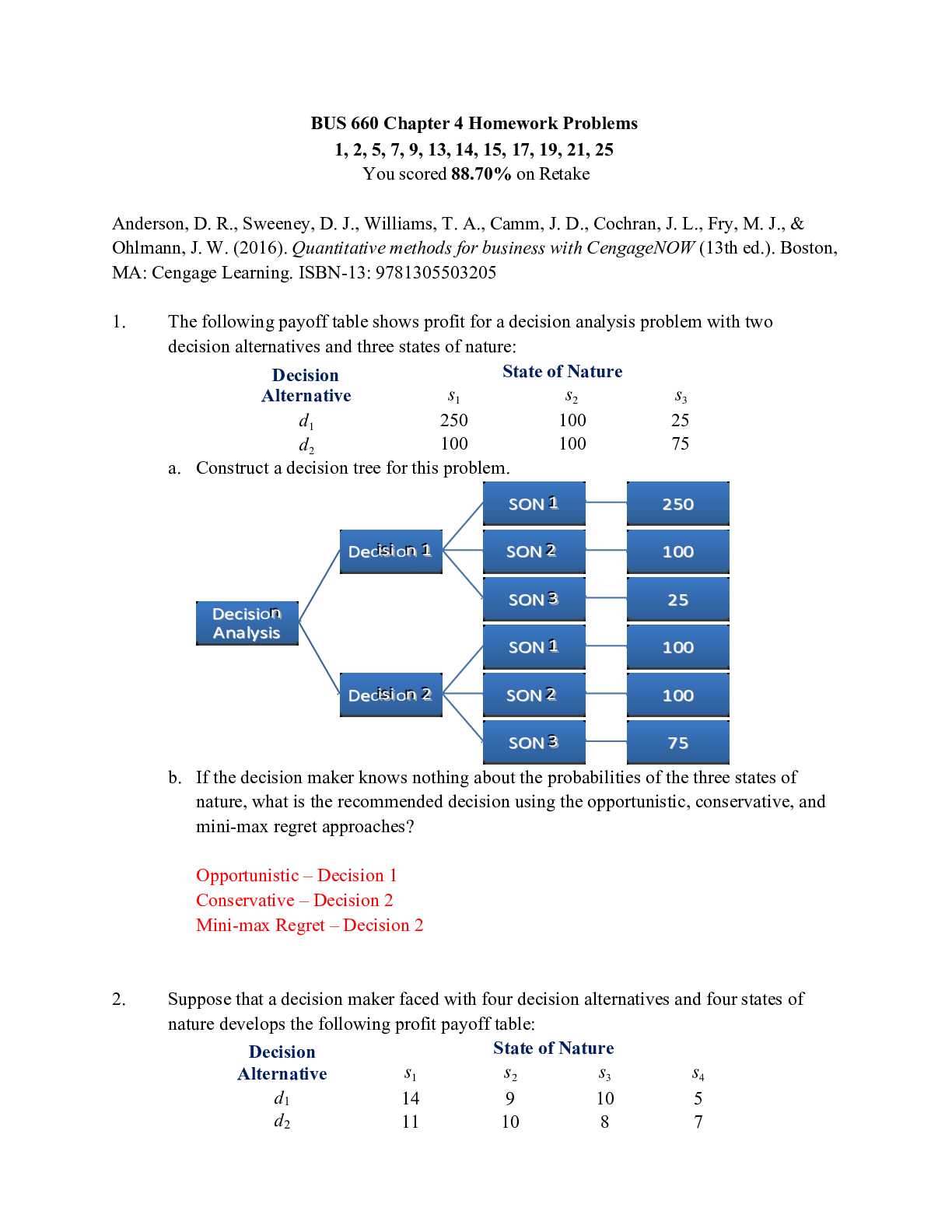
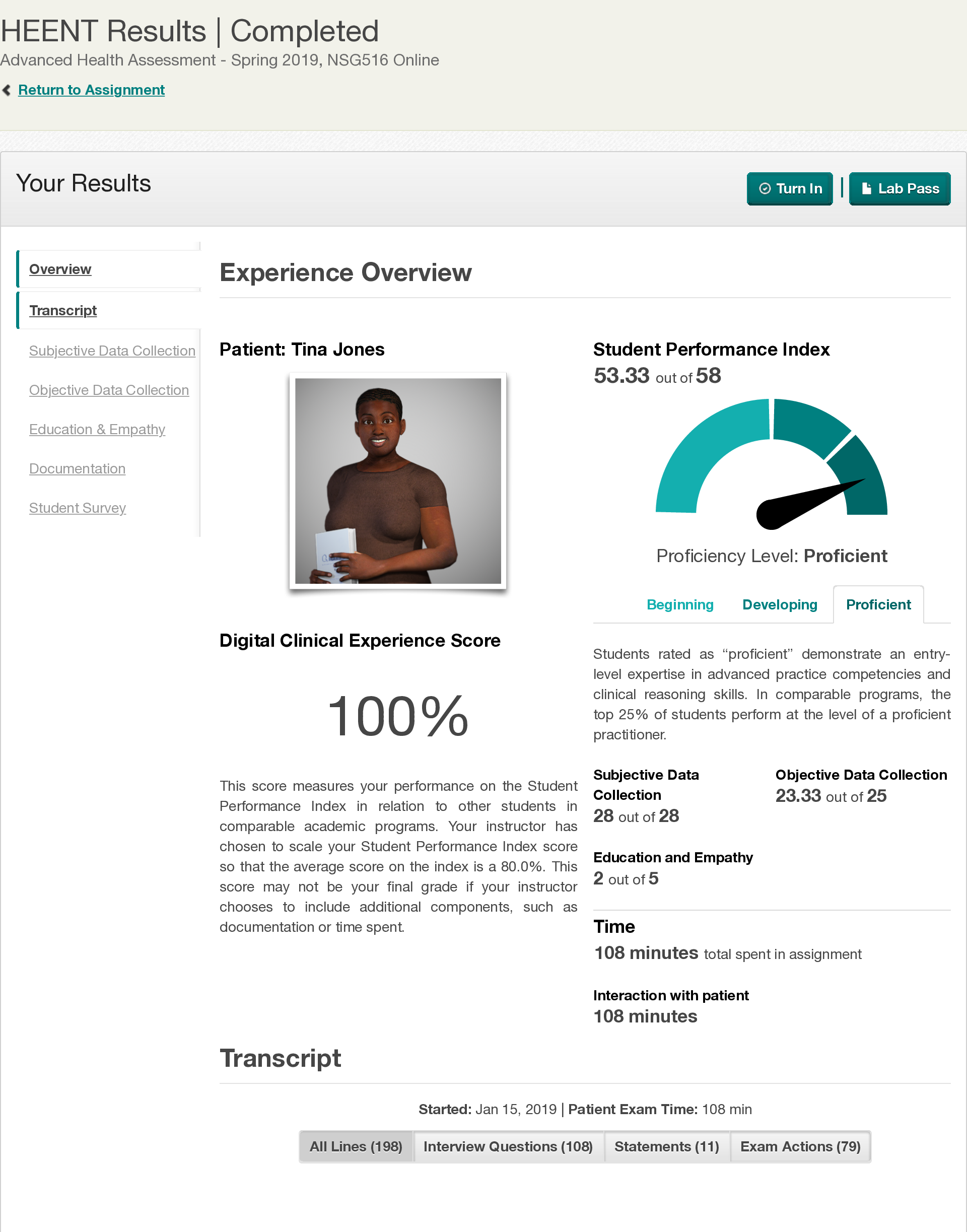
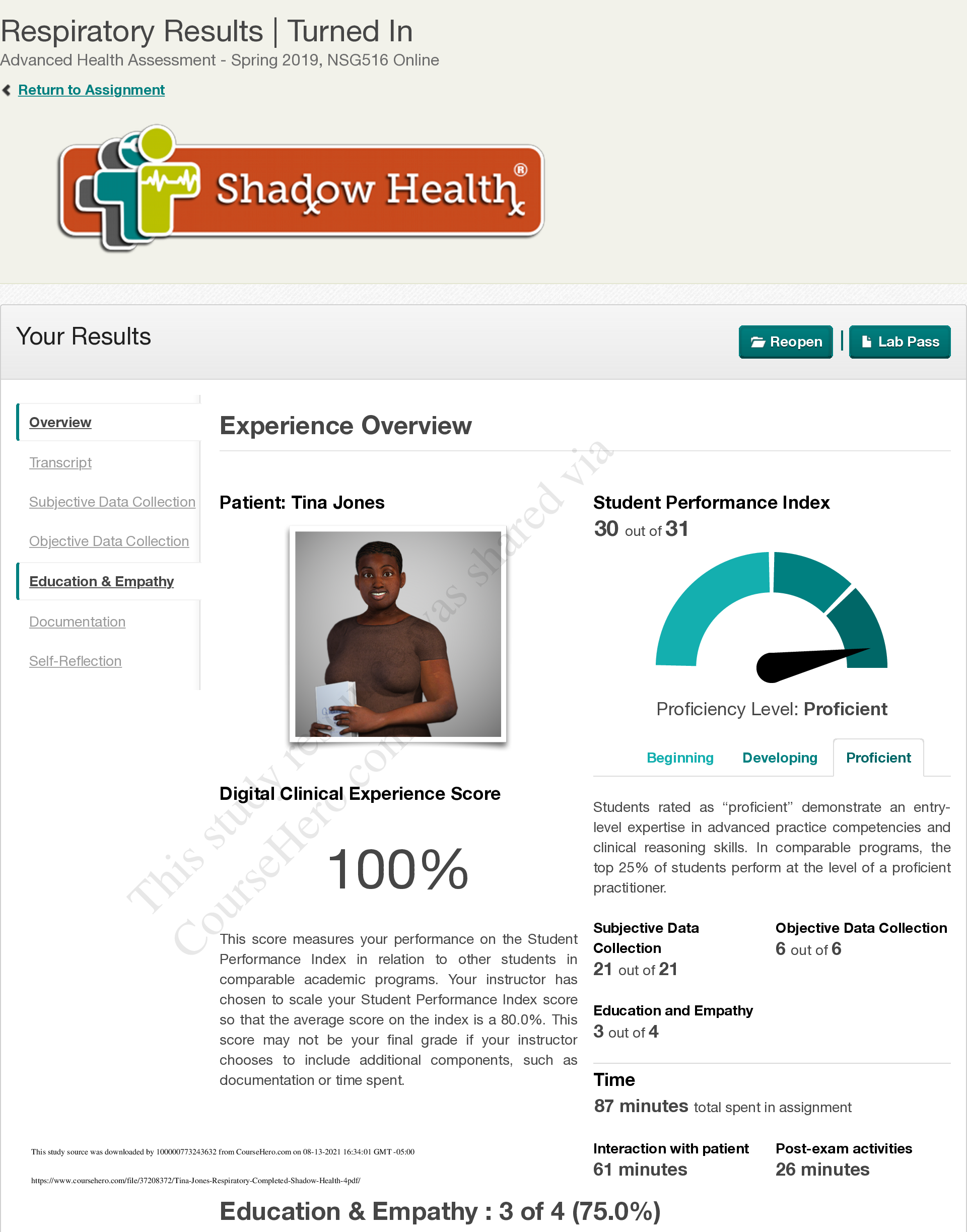
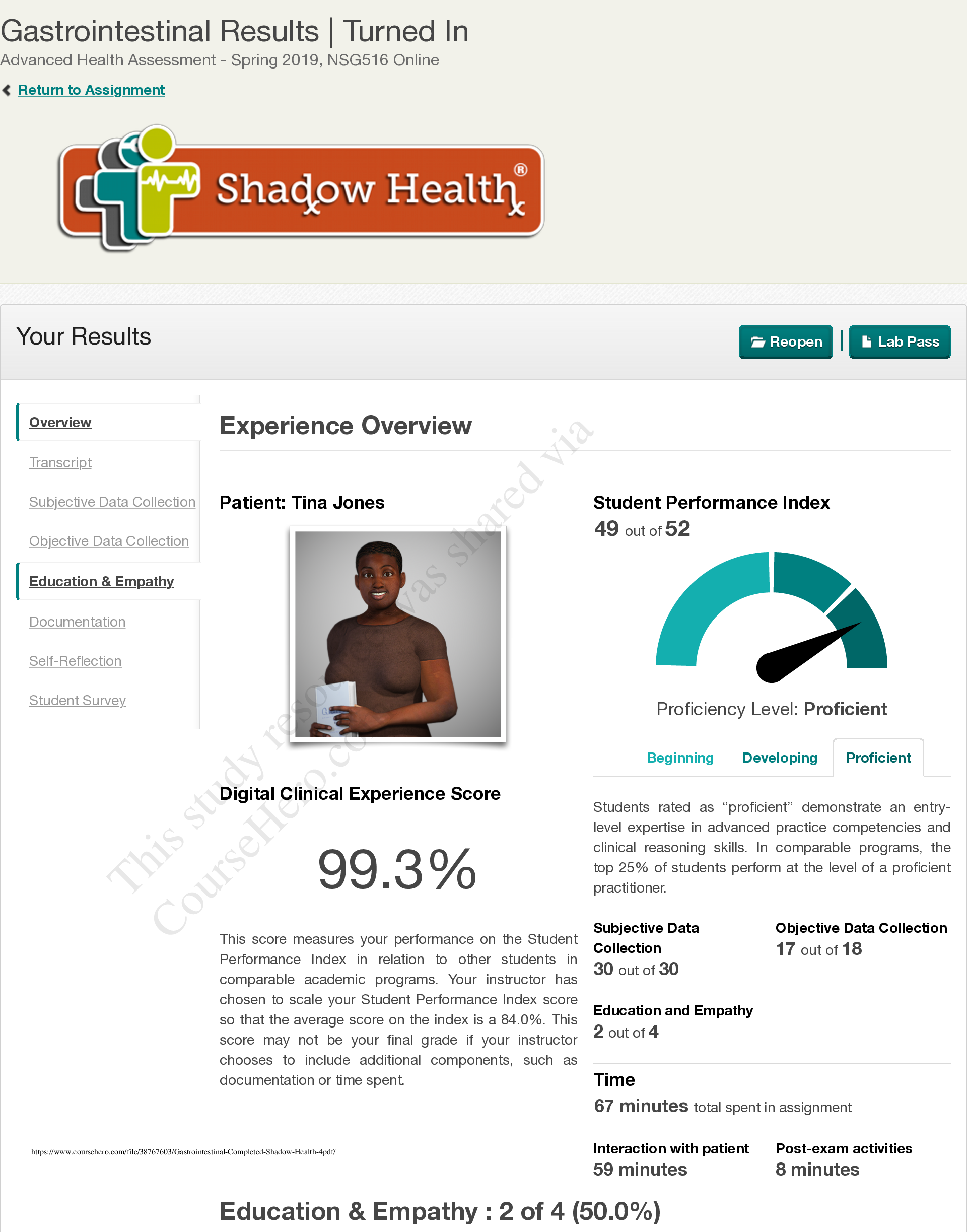
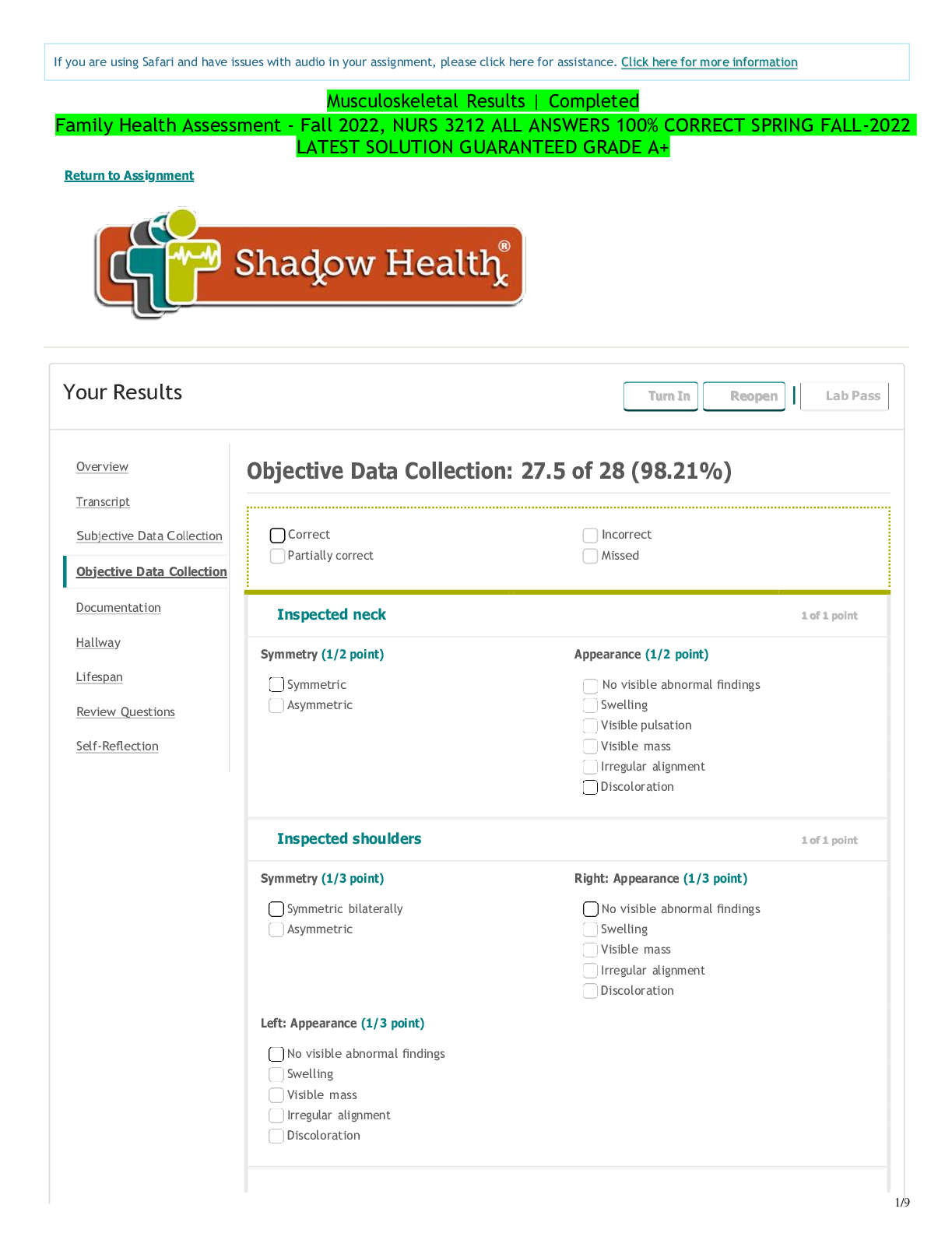
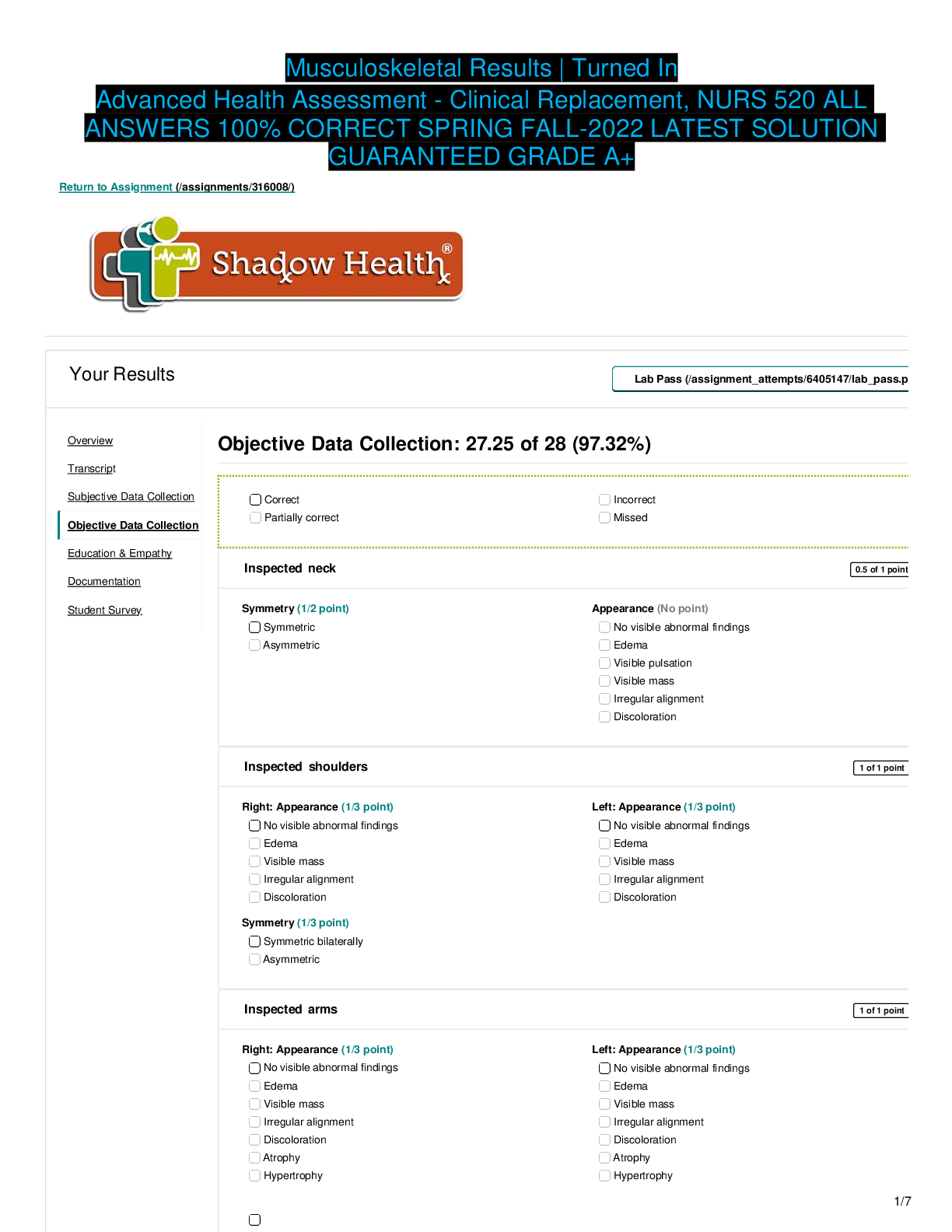
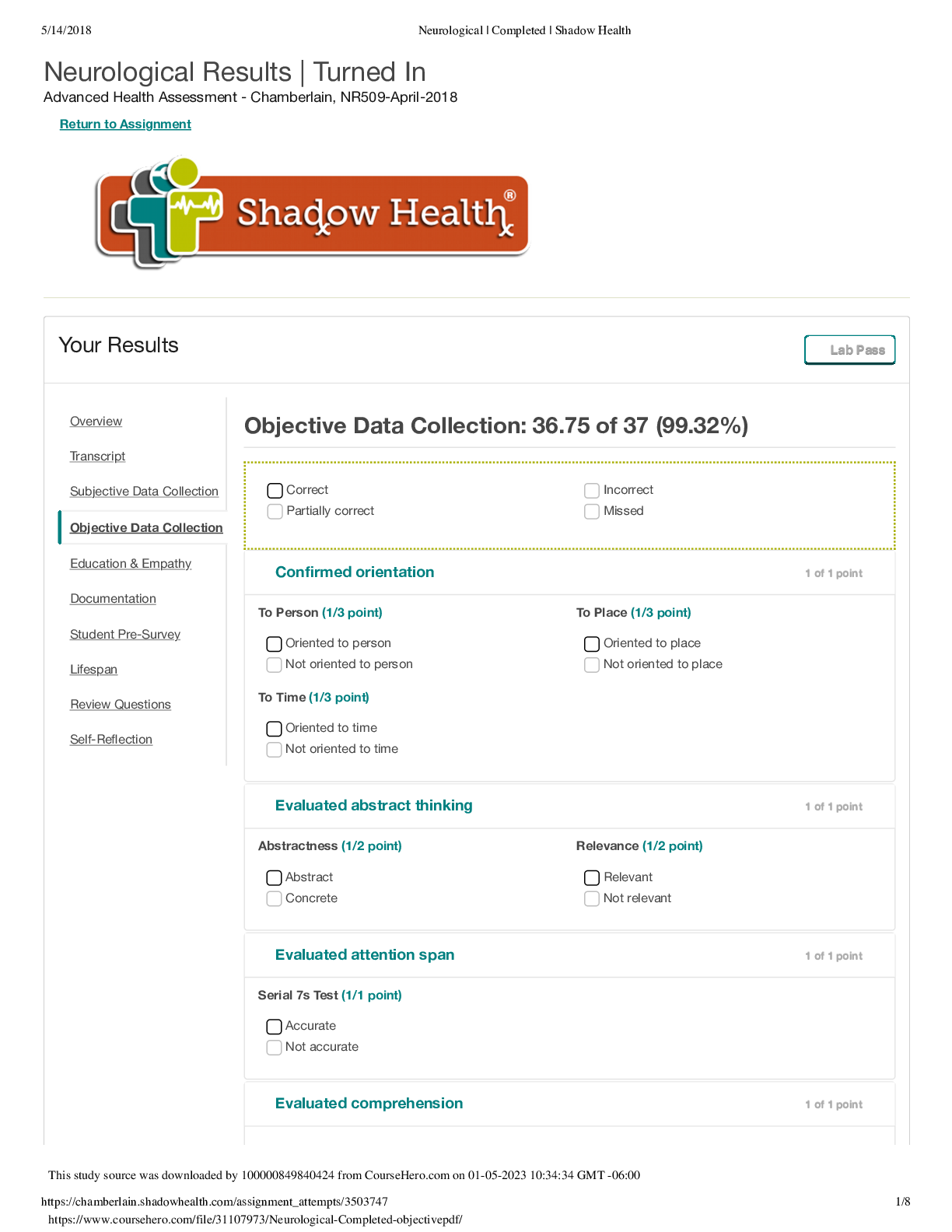
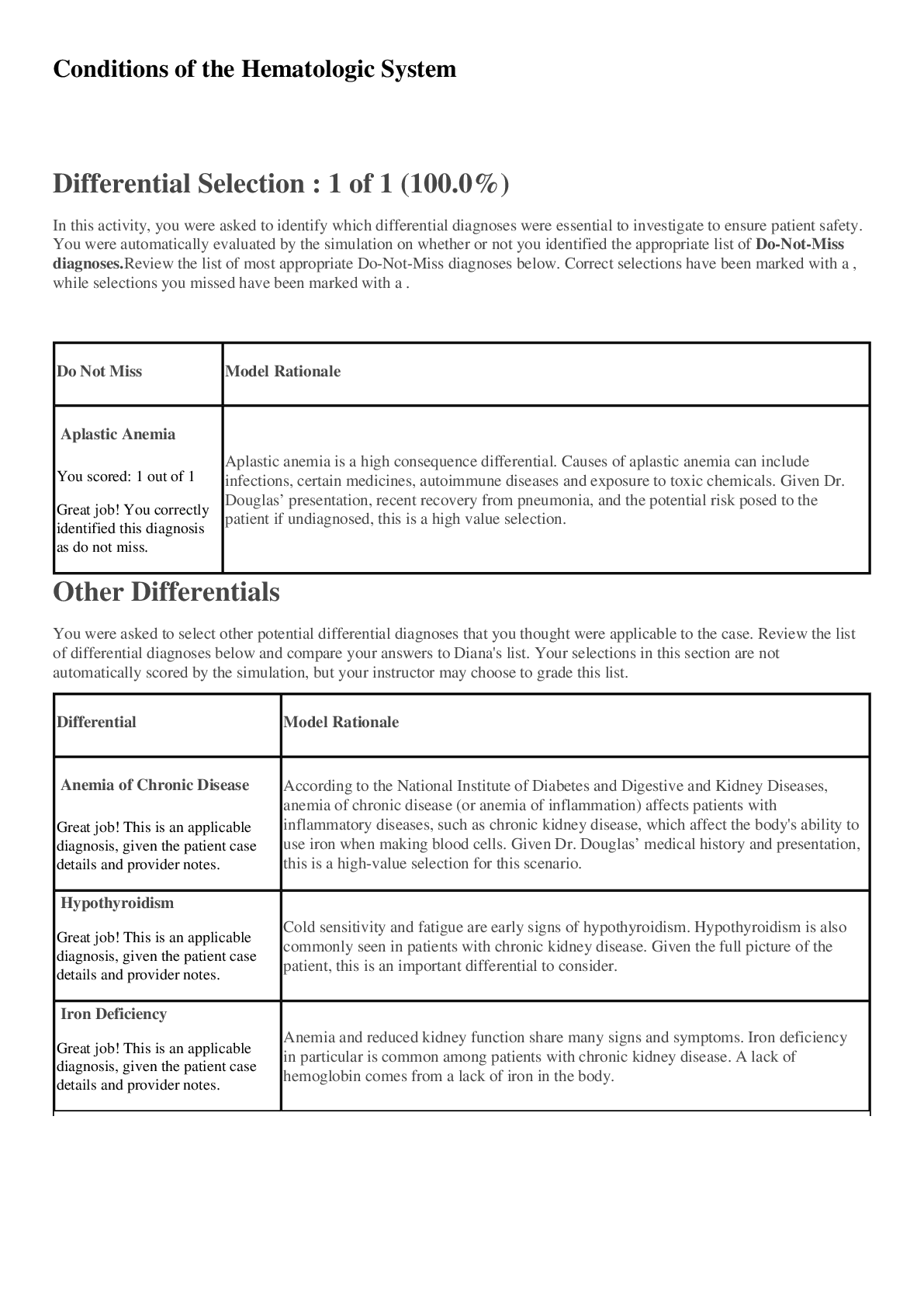
FOCUSED EXAM: COUGH Patient: Danny Rivera Digital Clinical Experience Score 100% Student Performance Index 34 out of 34 Experience Overview: FOCUSED EXAM: COUGH Patient: Danny Rivera Digital Clini... cal Experience Score 100% Student Performance Index 34 out of 34 Subjective Data Collection 19 out of 19 Objective Data Collection 15 out of 15 Subjective Data Collection: 19 of 19 (100.0%) A combination of open and closed questions will yield better patient data. The following details are facts of the patient's case. Chief Complaint Finding: Established chief complaint Finding: Reports cough (Found) Pro Tip: Asking a patient broadly about their chief complaint allows them to answer in their own words and confirm information that you may have already received from another source. Example Question: Do you have a cough? History of Presenting Illness Finding: Asked about onset of cough Finding: Reports cough started 3 days ago (Found) Pro Tip: Whenever you are assessing a symptom or a health condition, in this case the patient's cough, inquiring about onset assesses the severity and the progression of the problem.Example Question: How long have you had a cough? Finding: Asked about characteristics of cough Finding: Reports cough is wet (Available) Pro Tip: The characteristics of a cough, such as whether it is dry or wet, can indicate key information about the type of illness the patient has. Example Question: Is your cough a wet cough? Finding: Reports clear sputum with cough (Found) Pro Tip: The characteristics of a cough, such as whether it is productive, can indicate key information about the type of illness the patient has. Example Question: Do you produce any phlegm or sputum with your cough? Finding: Asked about frequency and duration of cough Finding: Reports coughing every few minutes (Found) Pro Tip: Establishing how frequently Danny coughs will illustrate how long he has been suffering these particular symptoms and might indicate possible triggers. Example Question: How frequently are you coughing? Finding: Reports coughs last a few seconds (Available) Pro Tip: Establishing how long Danny's coughs last will illustrate how long he has been suffering these particular symptoms and might indicate possible triggers. Example Question: How long do your coughs last? Finding: Asked about aggravating factors for cough Finding: Reports cough is worse at night (Found) Pro Tip: Establishing a timeline for Danny's coughing will illustrate how long he has been suffering these particular symptoms and might indicate possible triggers. Example Question: Is the cough worse at night? Finding: Denies smoking (Available)Pro Tip: Tobacco use puts the patient at risk for many medical conditions. Asking even young patients about whether they consume tobacco products helps you assess this risk factor. Example Question: Do you smoke? Finding: Reports being exposed to secondhand smoke through father (Available) Pro Tip: Tobacco use puts the patient at risk for many medical conditions. Asking about whether a patient is exposed to secondhand smoke allows you to assess this risk factor. Example Question: Are you ever around cigarette smoke? Finding: Reports he doesn't know what triggers the cough (Found) Pro Tip: Asking about aggravating factors of Danny's cough will allow you to determine potential causes and educate the patient on what to avoid. Example Question: What makes your cough worse? Finding: Asked about relieving factors for cough Finding: Reports cough is temporarily relieved by cough medicine (Found) Pro Tip: Asking about how the patient has been managing their pain assesses their current condition and their approach to self-care. The results of their previous treatment may be helpful in your diagnosis and the development of their new treatment plan, as well as a good opportunity to educate the patient on effective self-care practices. Example Question: Have you done anything to treat your cough? Finding: Followed up on cough medicine Finding: Reports cough medicine was purple (Available) Pro Tip: The type of cough medicine a patient takes, and how they take it, can impact its effectiveness. Following up on the cough medicine's color may help you identify the type of medication it is. Example Question: What color was the cough medicine? Finding: Reports taking one spoonful of cough medicine (Available) Pro Tip: The type of cough medicine a patient takes, and how they take it, can impact its effectiveness. Following up on the dose of cough medicine allows you to determine whether it is being taken correctly. Example Question:How much medicine did you take? Finding: Reports mother gave him the medicine (Found) Pro Tip: Children should only take medication under the supervision of an adult who can assure it is taken as directed. You should ask younger patients whether the medicine was given to them and by whom. Example Question: Who gave you the medicine for your cough? Finding: Reports only took the medicine this morning (Found) Pro Tip: The type of cough medicine a patient takes, and how they take it, can impact its effectiveness. Following up on the frequency Danny took cough medicine allows you to determine whether it is being taken correctly. Example Question: How many times have you taken the cough medicine? Finding: Denies home remedies (Available) Pro Tip: Patients sometimes try non-medicinal home remedies to treat coughs, such as breathing steam, or drinking tea with honey. Not all home remedies are effective or advisable, so it's important to find out what remedies the patient has tried. Example Question: Have you tried any home remedies for your cough? Finding: Asked about typical medication use Finding: Denies taking medication (Found) Pro Tip: Knowing a patient's current medication regimen helps you determine if any future treatments will be safe and effective. Example Question: Do you take any medications from a doctor? Finding: Reports taking daily vitamin (Found) Pro Tip: Some symptoms can occur as a result of a vitamin deficiency, and others as a result of vitamin excess. Vitamins can also interfere with some treatments, so it's important to know what your patient is taking. Example Question: Do you take vitamins? Finding: Asked about activity level Finding: Reports typical high activity level(Available) Pro Tip: Establishing a patient's typical activity level is an important baseline to help you determine how an illness is affecting his life. Example Question: Are you usually active? Finding: Reports activity level low since getting sick (Available) Pro Tip: Establishing a patient's activity level, and whether it has been impacted since becoming ill, is an important baseline to help you determine how an illness is affecting his life. Example Question: Have you been less active since getting sick? Finding: Reports still able to run or play (Found) Pro Tip: Ability to remain active indicates that the patient's breathing is not dangerously affected, and that the patient isn't seriously fatigued. Example Question: Are you able to keep up when you play with your classmates? Finding: Reports focusing in class is difficult (Available) Pro Tip: Mental lethargy and difficulty concentrating are common symptoms when a patient is sick. Example Question: Are you able to focus in class? Finding: Asked about nasal symptoms Finding: Reports current runny nose (Found) Pro Tip: Asking your patient if his nose is running will allow you to determine the symptoms he is experiencing and possible triggers. Example Question: Do you currently have a runny nose? Finding: Denies sneezing (Available) Pro Tip: Asking your patient if he has been sneezing will allow you to determine the symptoms he is experiencing and possible triggers. Example Question: Have you been sneezing? Finding: Followed up on nasal discharge Finding: Reports nasal discharge is clear(Available) Pro Tip: The color of a patient's nasal discharge can provide you key information as to the type of condition the patient has. Example Question: What color is your snot? Finding: Reports nasal discharge is thin (Available) Pro Tip: The consistency of a patient's nasal discharge can provide you key information as to the type of condition the patient has. Example Question: What is the consistency of your nasal discharge? Finding: Asked about ear symptoms Finding: Denies ear pain (Found) Pro Tip: Ear pain is often coincident with coughs and sinus problems. Asking about them allows you to ascertain if Danny needs follow-up care for his ears. Example Question: Do you have any ear pain? Finding: Reports history of frequent ear infections (Available) Pro Tip: Asking about Danny's history of ear infections allows you to ascertain his risk for current and future ear infections. Example Question: Have you ever had ear infections? Finding: Denies ear discharge (Available) Pro Tip: Asking Danny about ear discharge, which are often coincident with of ear infections, allows you to ascertain his risk for current and future ear infections. Example Question: Do you have any ear discharge? Finding: Denies hearing problems (Available) Pro Tip: Simply talking with the patient assesses his hearing; however, some types of hearing loss are only apparent in specific settings such as noisy environments. Asking the patient about hearing problems identifies conditions that may not be readily apparent. Example Question: Do you have any hearing problems? Finding: Asked about throat symptoms Finding:Reports sore throat (Found) Pro Tip: Sore throats are often coincident with coughs and sinus problems. Asking about them allows you to ascertain if Danny needs follow-up care for his throat. Example Question: Is your throat sore? Finding: Reports a little pain with swallowing (Available) Pro Tip: Pain when swallowing helps you understand how severe the patient's sore throat is. Example Question: Does it hurt when you swallow? Past Medical History Finding: Asked about relevant medical history Finding: Reports frequent runny noses (Found) Pro Tip: Asking how often Danny experiences runny noses like the one he has now may help you determine the source of the problem. Example Question: Do you get runny noses often? Finding: Reports past frequent coughs (Available) Pro Tip: A patient experiencing a cough should be asked about their history of coughs so you can determine whether their current condition fits into a recurring pattern. Example Question: Do you have coughs very often? Finding: Reports past pneumonia (Available) Pro Tip: Pneumonia is a serious medical condition that can be life-threatening if not managed appropriately. Regardless of the patient's presenting illness, it is critical to identify current medical conditions in order to treat the patient appropriately. Specific questions should be asked about previous medical problems, even if the patient doesn't notice current symptoms. Example Question: Have you had pneumonia? Finding: Denies asthma diagnosis (Available) Pro Tip: Asthma is a serious medical condition that can be life-threatening if not managed appropriately. Regardless of the patient's presenting illness, it is critical to identify current medical conditions in order to treat the patient appropriately. Specific questions should be asked about previous medical problems, even if the patient doesn't notice current symptoms. Example Question:Do you have asthma? Finding: Reports immunizations as current (Available) Pro Tip: A health assessment should include an evaluation of the patient's immunization status in order to identify diseases to which the patient is vulnerable. Example Question: Do you have current immunizations? Finding: Asked about allergies Finding: Denies seasonal allergies (Found) Pro Tip: Seasonal allergies can cause symptoms like runny nose, cough, and discomfort. Asking Danny if he has seasonal allergies can help you to ascertain possible triggers for symptoms. Example Question: Do you have seasonal allergies? Finding: Denies food allergies (Found) Pro Tip: Knowing if your patient has food allergies is important and relevant medical history. Asking your patient about food allergies will allow you to most effectively treat him. Example Question: Do you have food allergies? Finding: Denies medication allergies (Found) Pro Tip: Knowing if your patient has allergies to medicine is important and relevant medical history. Asking your patient about medicine allergies will allow you to most effectively treat him. Example Question: Are you allergic to any medication? Finding: Asked relevant family history Finding: Reports father has history of asthma (Available) Pro Tip: Medical problems such as asthma that are present in a patient's immediate family can represent increased risk factors to respiratory conditions such as the ones the patient currently has. Example Question: Do you have a family history of asthma? Finding: Denies family history of allergies (Found)Pro Tip: Medical problems such as allergies that are present in a patient's immediate family can represent increased risk factors to respiratory conditions such as the ones the patient currently has. Example Question: Do you have a family history of allergies? Review of Systems Finding: Asked about constitutional health Finding: Denies chills (Available) Pro Tip: Soliciting a shallow history of your patient's symptoms will help you to most effectively treat him. Asking Danny if he has chills will illustrate the way his symptoms manifest. Example Question: Do you have chills? Finding: Denies fever (Available) Pro Tip: Soliciting a shallow history of your patient's symptoms will help you to most effectively treat him. Asking Danny if he has a fever will illustrate the way his symptoms manifest. Example Question: Do you have a fever? Finding: Reports feeling somewhat fatigued (Found) Pro Tip: Soliciting a shallow history of your patient's symptoms will help you to most effectively treat him. Asking Danny if he has fatigue will illustrate the way his symptoms manifest. Example Question: Do you have fatigue? Finding: Denies night sweats (Available) Pro Tip: Soliciting a shallow history of your patient's symptoms will help you to most effectively treat him. Asking Danny if he has night sweats will illustrate the way his symptoms manifest. Example Question: Do you have night sweats? Finding: Reports cough makes it difficult to sleep (Available) Pro Tip: Soliciting a shallow history of your patient's symptoms will help you to most effectively treat him. Asking Danny if he has had difficulty sleeping will illustrate the way his symptoms manifest. Example Question: Have you been sleeping okay? Finding: Denies swelling(Available) Pro Tip: Soliciting a shallow history of your patient's symptoms will help you to most effectively treat him. Asking Danny if he has had swelling will illustrate the way his symptoms manifest. Example Question: Have you noticed any swelling? Finding: Asked about additional review of systems for HEENT Finding: Reports frequent colds (Available) Pro Tip: A patient such as Danny who is presenting with a cough and a runny nose may have a cold, so you should ask about his history of colds to determine whether this is part of a larger pattern. Example Question: Do you have unusually frequent colds? Finding: Denies headaches (Found) Pro Tip: Headaches are a common complaint that can be caused by a variety of benign conditions. However, headaches can be an indicator of serious underlying neurological conditions such as cerebral hemorrhage, meningitis, or brain tumors. They may also be a symptom of sinus infection. Example Question: Do you get headaches? Finding: Denies nosebleeds (Available) Pro Tip: When a patient presents with symptoms that are often seen with respiratory infections, you should ask about similar signs of respiratory infections such as nosebleeds. Example Question: Do you have nosebleeds? Finding: Denies vision difficulty (Available) Pro Tip: Eye or vision problems can lower one's ability to function and can be a major safety risk. Example Question: Do you have any problems with your vision? Finding: Denies dizziness (Available) Pro Tip: Asking about dizziness helps you assess the risk for inner ear, neurological, or cardiovascular problems. Example Question: Do you have any dizziness? Finding:Denies watery eyes (Available) Pro Tip: Whether a patient has watery eyes may help you indicate the type of sinus problem he is experiencing. Example Question: Do you have watery eyes? Finding: Denies eye redness (Available) Pro Tip: Whether a patient has eye redness may help you indicate the type of sinus problem he is experiencing. Example Question: Do you have eye redness? Finding: Denies eye pain (Available) Pro Tip: Eye pain can lower one's ability to function and can be a major safety risk. Example Question: Do you have any eye pain? Finding: Denies sinus pain (Found) Pro Tip: Patients with sinus problems such as a runny nose may be at greater risk for sinus pain. Example Question: Do you have any sinus pain? Finding: Asked about review of systems for respiratory Finding: Denies chest tightness (Available) Pro Tip: Chest pain may indicate cardiac conditions, muscular inflammation, gastric upset, or respiratory distress. If chest tightness is present, asking about its location, characteristics, and related factors helps to determine the cause of the discomfort. Example Question: Do you have chest tightness? Finding: Denies chest pain (Available) Pro Tip: Chest pain may indicate cardiac conditions, muscular inflammation, gastric upset, or respiratory distress. If chest pain is present, asking about its location, characteristics, and related factors helps to determine the cause of the discomfort. Example Question: Do you have any chest pain? Finding: Denies difficulty breathingOBJECTIVE DATA: Inspected eyes and orbital area 1 of 1 point Orbital Area (1/4 point) No visible abnormal findings Ptosis Eyelid Lesion Sclera (1/4 point) White Yellow tint Redness Conjunctiva (1/4 point) Moist and pink Dry appearance Redness Swelling Conjunctival Discharge (1/4 point) No discharge Clear, watery discharge Purulent discharge Inspected nasal cavities 1 of 1 point Color (1/4 point) Pink Red Bluish Discharge (1/4 point) No discharge Clear discharge Bloody discharge Purulent dischargeTurbinate Patency (1/4 point) Patent Decreased patency Not patent Observations (1/4 point) No additional visible abnormal findings Foreign body present Polyp Septum perforated Septum deviated Lesion Inspected ears 1 of 1 point Right: Auditory Canal Color (1/10 point) Pink Red Pallor Right: Tympanic Membrane Color (1/10 point) Pearly gray Red Opaque Yellow Not visible because of cerumen Right: Tympanic Membrane Appearance (1/10 point) No visible abnormal findings Fluid observed Visible scars Bulging Perforation Retraction Right: Cone Of Light (1/10 point) 5:00 Cone of light distortedRight: Discharge (1/10 point) No discharge Cerumen Clear discharge Bloody discharge Purulent discharge Left: Auditory Canal Color (1/10 point) Pink Red Pallor Left: Tympanic Membrane Color (1/10 point) Pearly gray Red Opaque Yellow Not visible because of cerumen Left: Tympanic Membrane Appearance (1/10 point) No visible abnormal findings Fluid observed Visible scars Bulging Perforation Retraction Left: Cone Of Light (1/10 point) 7:00 Cone of light distorted Left: Discharge (1/10 point) No discharge Cerumen Clear discharge Bloody discharge Purulent discharge Inspected mouth and throat1 of 1 point Oral Mucosa (1/5 point) Moist and pink Dry appearance Redness Tonsils (1/5 point) No visible abnormal findings Swelling Redness Throat Color (1/5 point) Pink Red Throat Texture (1/5 point) No abnormal findings Cobblestoning Exudate Post Nasal Drip (1/5 point) No discharge Clear discharge Purulent discharge Inspected neck 1 of 1 point Symmetry (1/2 point) Symmetric Asymmetric Appearance (1/2 point) No visible abnormal findings Swelling Visible pulsation Visible mass Discoloration Inspected chest 1 of 1 point Symmetry (1/2 point) Symmetric Asymmetric Appearance (1/2 point) No visible abnormal findings Rash Barrel chest Intercostal retraction while breathing Excessive use of accessory muscles while breathing Skin growths (freckles or moles) Auscultated breath sounds 1 of 1 point Breath Sounds (1/3 point) Present in all areas Diminished in some areas Absent in some areas Adventitious Sounds (1/3 point) No adventitious sounds Wheezing Fine crackles Stridor Rhonchi Rales Location (1/3 point) All areas clear Adventitious sounds in anterior right upper lobe Adventitious sounds in anterior right middle lobe Adventitious sounds in anterior right lower lobe Adventitious sounds in anterior left upper lobe Adventitious sounds in anterior left lower lobe Adventitious sounds in posterior right upper lobe Adventitious sounds in posterior right lower lobe Adventitious sounds in posterior left upper lobe Adventitious sounds in posterior left lower lobe Auscultated for bronchophony 1 of 1 point Bronchophony (1/1 point) Positive Negative Auscultated heart sounds 1 of 1 point Heart Sounds (1/2 point) S1 and S2 audible S1, S2, and S3 audible S1, S2, and S4 audible S1, S2, S3, and S4 audible Extra Heart Sounds (1/2 point) No extra sounds Gallops Murmur Friction rub Valve clicks Percussed chest wall 1 of 1 point Observations (1/2 point) All areas resonant Some areas dull, some resonant Some areas hyperresonant, some resonant Location (1/2 point) No areas of dullness Dullness, anterior right upper lobe Dullness, anterior right middle lobe Dullness, anterior right lower lobe Dullness, anterior left upper lobe Dullness, anterior left lower lobe Dullness, posterior right upper lobe Dullness, posterior right lower lobe Dullness, posterior left upper lobe Dullness, posterior left lower lobe Measured diaphragmatic excursion 1 of 1 point Range (1/1 point) 3-5 cm Greater than 3-5 cm Less than 3-5 cm Palpated sinuses 1 of 1 point Frontal (1/2 point) None reported Tenderness reported Maxillary (1/2 point) None reported Tenderness reported Palpated lymph nodes 1 of 1 point Head And Neck (1/3 point) No palpable nodes Palpable nodes on right side Palpable nodes on left side Supraclavicular (1/3 point) No palpable nodes Palpable nodes on right side Palpable nodes on left side Axillary (1/3 point) No palpable nodes Palpable nodes on right side Palpable nodes on left side Palpated fremitus 1 of 1 point Symmetry (1/2 point) Equal bilaterally Unequal bilaterally Vibration (1/2 point) Expected fremitus Decreased fremitus Palpated chest expansion 1 of 1 point Symmetry (1/1 point) Equal bilaterally Unequal bilaterally Vitals Blood Pressure 120/76 O2 Sat 96 Pulse 91 Resp. Rate 28 Temperature 37.2 C/ 99.0 F Spirometry FVC 3.91 FEV1 3.15SBAR 1. Situation Danny Rivera is an 8 year old boy presenting a wet cough. It began 3 days ago per his recount. Model Note Danny Rivera is an 8-year-old boy presenting with a wet cough. He reports that the cough has lasted three days. He describes the cough as wet and “gurgly.” 2. Background He presented with pneumonia last year. Mother has treated cough at home with dimetapp. Cough has lasted 3 days. Risk factors include second hand smoke from father. Model Note The cough is temporarily treated by the children’s cough medicine his mother gave him; he reports that the cough is not aggravated by activity. He says the cough gets worse at night, which keeps him up. He reports tenderness in his throat. He reports a history of frequent rhinorrhea and cough. Risk factors include second-hand smoke from father, history of pneumonia in the past year, and being overweight for his age. 3. Assessment No acute respiratory distress, lung sounds are clear, throat appera red with visible cobblestoning, some nasal clear drainage, has an increased respiratory rate, and presents mild tachycardia. Model Note He has no acute respiratory distress; his lungs are clear to auscultation and is afebrile. He has current rhinorrhea; examination of the nose reveals boggy turbinate. His throat appears red with visible cobblestoning in the back. His respiratory rate is increased, and he presents mild tachycardia. 4. Recommendation I recommend calling his grandmother to see if someone can pick him up from school. He should see his primary care pediatrician. He sould get plenty of rest and be given cough medicine PRN. Model Note I recommend calling his grandmother to arrange for someone to pick him up from school. He should see his primary care provider within the next few days for an evaluation and tests to rule out asthma or allergies. In the meantime, he should be allowed to rest and should be given cough medicine as needed.What are you here for today? Question 12/03/18 1:29 PM CST My music teacher Mr. Hillman sent me here because he said I look sick. I have been coughing a lot. . . and I feel kinda tired. When did your cough start? Question 12/03/18 1:31 PM CST I think the cough started two . . . No, it started three days ago. Does it hurt anywhere when you cough? Question 12/03/18 1:35 PM CST Nothing really hurts. I've just had this cough for about three days. . . and I feel kind of tired. Do you cough anything up? Question 12/03/18 1:55 PM CST Is that the gross, slimy stuff? Yeah, I've been coughing some of that up. It's clear. Do you cough stuff up more in the mornings? Question 12/03/18 1:56 PM CST I mostly cough during the nighttime. are you coughing up anything? Question 12/06/18 8:34 PM CST Is that the gross, slimy stuff? Yeah, I've been coughing some of that up. It's clear.how long have you had a cough? Question 12/06/18 8:34 PM CST I think the cough started two . . . No, it started three days ago. how often do you cough? Question 12/06/18 8:35 PM CST I just keep feeling like I have to cough every couple minutes or so. I think it gets worse at night. what makes your cough better? Question 12/06/18 8:35 PM CST My mom gave me some medicine this morning. . . that helped my cough a little. I don't remember what it was called though, sorry. do you take any medications? Question 12/06/18 8:35 PM CST Just when I'm sick and my mom or the doctor says I should take some medicine. My mom gave me some cough medicine this morning. Oh, I also have vitamins. I love those. They're yummy and healthy so I sneak a few more of them. does exercise make the cough worse? Question 12/06/18 8:36 PM CST No . . . I did feel a little bit tired during gym class, but I think it is because I couldn't sleep much. I didn't cough more though. do you have a runny nose? Question 12/06/18 8:37 PMCST My nose is always a little bit runny. . .but ever since I started coughing it's been worse, I think. what color is it ? (Clarified to What color is your sputum?.) Question 12/06/18 8:38 PM CST Is that the gross, slimy stuff? Yeah, I've been coughing some of that up. It's clear. (Clarified to what color my sputum is.) when did the nasal discharge get worse? (No matching questions found.) Question 12/06/18 8:38 PM CST when did your runny nose start? Question 12/06/18 8:39 PM CST My nose is always a little bit runny. . .but ever since I started coughing it's been worse, I think. do your ears hurt? Question 12/06/18 8:39 PM CST My ears are okay. They don't hurt or anything. does your throat hurt? Question 12/06/18 8:39 PM CST It feels a little bit sore, yeah. nasal discharge? (Clarified to Has your nose been running?.) Question 12/06/18 8:40 PMCST My nose is always a little bit runny. . .but ever since I started coughing it's been worse, I think. (Clarified to if my nose has been runny.) does anything make your runny nose worse? Question 12/06/18 8:40 PM CST I don't know what makes it run; it just does sometimes. are you allergic to anything? Question 12/06/18 8:40 PM CST I don't think I have any allergies. do you have a family history of allergies? Question 12/06/18 8:41 PM CST [Show More]
Last updated: 1 year ago
Preview 1 out of 24 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Mar 03, 2022
Number of pages
24
Written in
Additional information
This document has been written for:
Uploaded
Mar 03, 2022
Downloads
0
Views
110