*NURSING > SHADOW HEALTH > Antepartum Care UNFOLDING Reasoning Anne Jones, 17 years old (All)
Antepartum Care UNFOLDING Reasoning Anne Jones, 17 years old
Document Content and Description Below
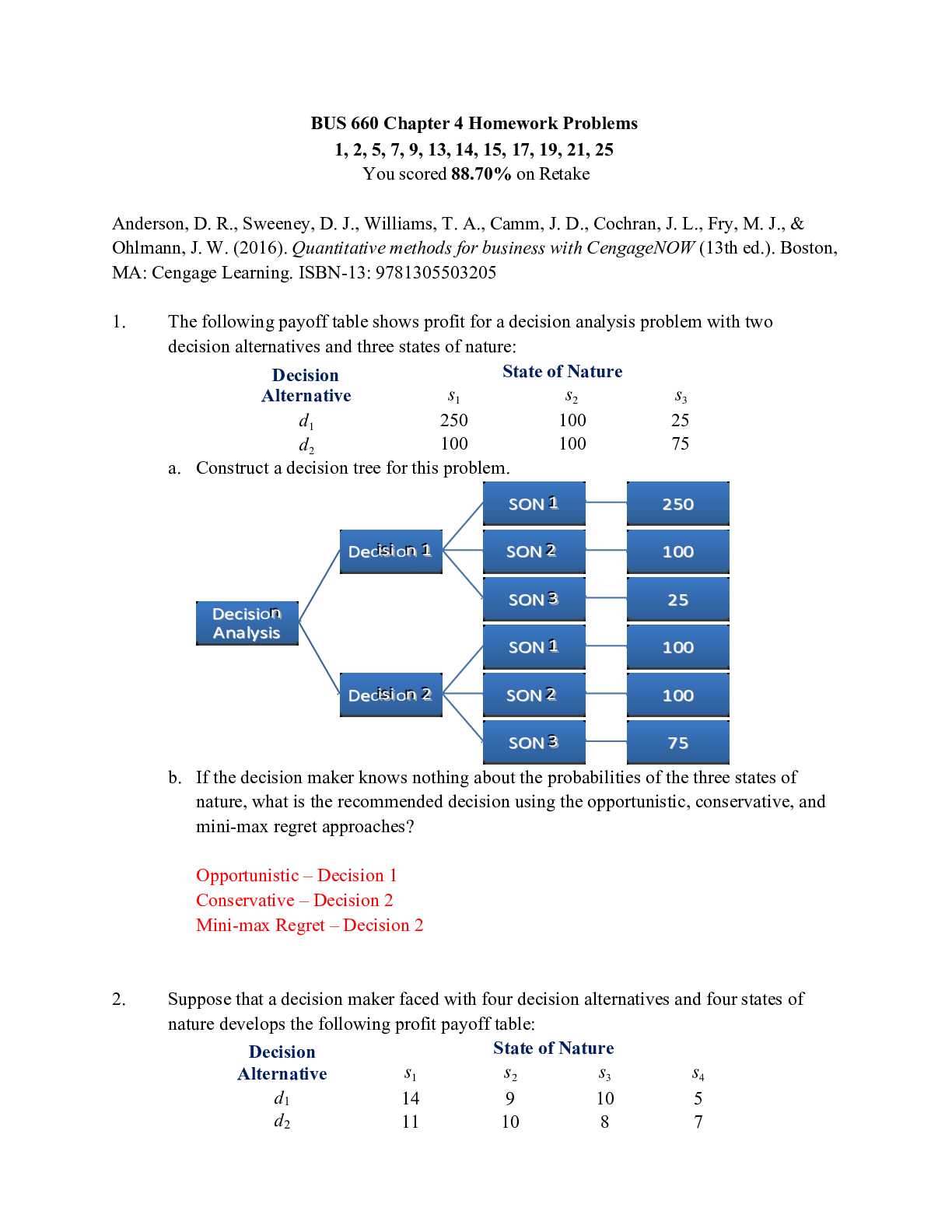
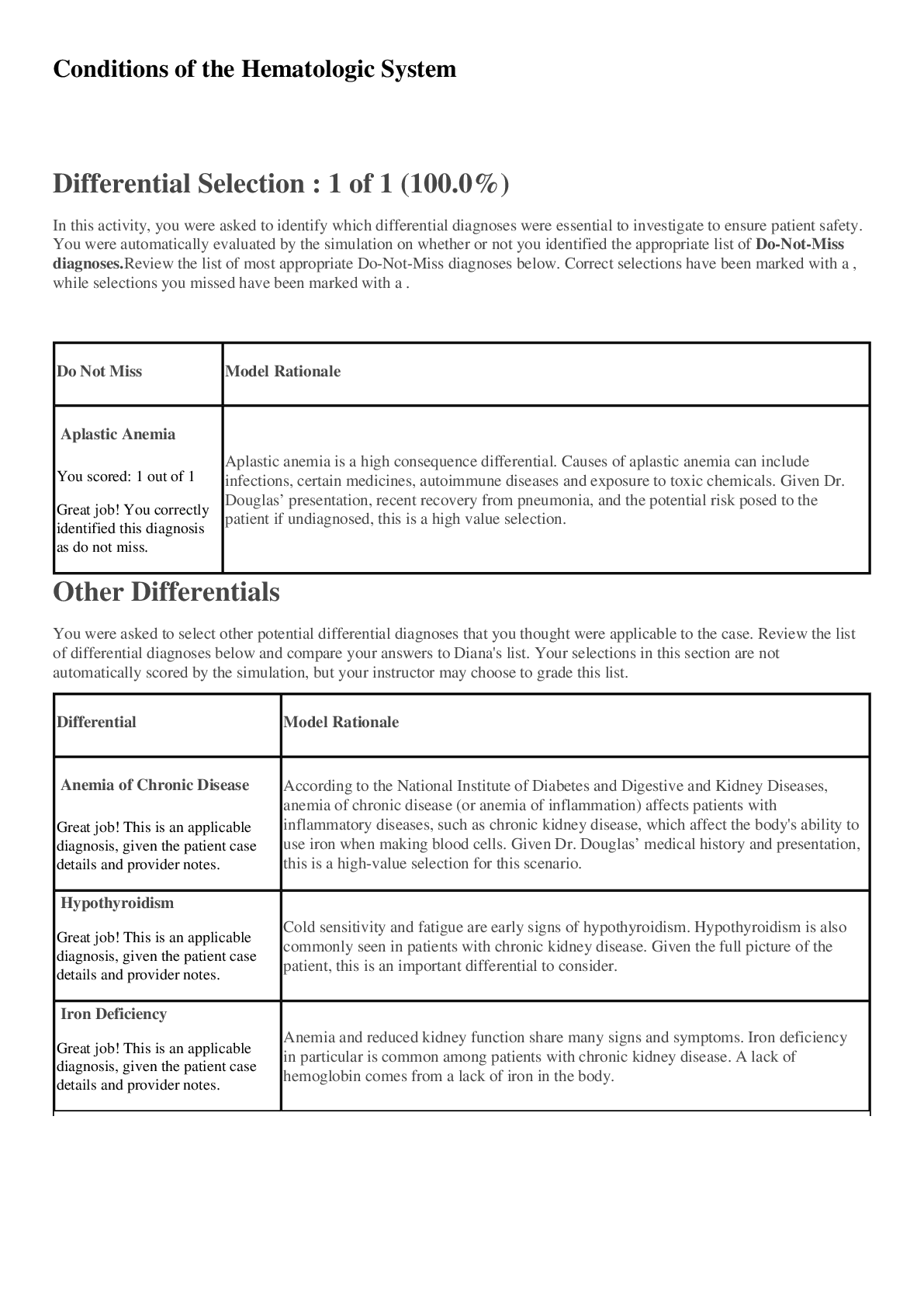
Antepartum Care UNFOLDING Reasoning Anne Jones, 17 years old Antepartum Care UNFOLDING Reasoning Primary Concept Reproduction Interrelated Concepts (In order of emphasis) 1. Nutrition 2. Patien... t Education 3. Stress 4. Coping 5. Clinical Judgment 6. Communication NCLEX Client Need Categories Percentage of Items from Each Category/Subcategory Covered in Case Study Safe and Effective Care Environment • Management of Care 17-23% ✓ • Safety and Infection Control 9-15% Health Promotion and Maintenance 6-12% ✓ Psychosocial Integrity 6-12% ✓ Physiological Integrity • Basic Care and Comfort 6-12% ✓ • Pharmacological and Parenteral Therapies 12-18% ✓ • Reduction of Risk Potential 9-15% ✓ • Physiological Adaptation 11-17% ✓ Anne Jones, 17 years oldHistory of Present Problem: Anne Jones is a 17-year-old Caucasian teenager who thinks she may be pregnant because she has missed two periods. Her last menstrual period, she thinks, was about one month ago. She states she had a little bit of spotting last week but didn’t have a “full period”. She complains of her breasts being tender, swollen, frequent urination, and nausea in the morning. This is her first office visit and she is not sure why she feels so crummy but suspects she might be pregnant. Her urine pregnancy test is positive. Her primary care provider orders a prenatal lab panel and a urinalysis. Personal/Social History: Anne is a senior in high school who stands on her feet while working at McDonalds after school. She drinks six colas daily, denies alcohol use, and does not smoke. She takes no medications except for occasional acetaminophen for headaches and ibuprofen for menstrual cramps. Anne is 5’4” (160 cm) and weighs about 105 lbs. (47.7 kg) according to Anne. A 24-hour recall nutrition history reveals a typical day’s diet: breakfast- pop tart and can of cola; Lunch- a slice of pizza, chocolate chip cookie, can of cola; Dinner- fried chicken, green beans, biscuit, can of cola; snacks, including cookies and can of cola. She broke up last week with her boyfriend, and he is not aware she might be pregnant. She wants to keep the baby but has not told her parents. What data from the histories are RELEVANT and must be interpreted as clinically significant by the nurse? (Reduction of Risk Potential) RELEVANT Data from Present Problem: Clinical Significance: 1. 17-year-old female reports two missed periods. 2. Reported some spotting last week 3. C/O breast tenderness, swelling, increased frequent in urination, and a.m. nausea 4. (+) pregnancy test 5. Provider has ordered urinalysis and pre-natal lab panel -These are all presumptive signs of pregnancy. RELEVANT Data from Social History: Clinical Significance: 1. Senior in H/S. 2. Works in a job that requires constant standing 3. Denies use of alcohol/nicotine & is not on any prescription medications 4. Reports a daily diet of poor nutritional value 5. Does not currently have a support system, as she has not informed anyone of her present situation -Patient is in stable health with no known major medical concerns at this point. We know that she will need her nutrition and dietary habits addressed to successfully accommodate a growing fetus. She will also need a support system and education on what to expect in the coming months. We’ll know more when her lab panel comes back. Patient Care Begins: Current VS: P-Q-R-S-T Pain Assessment: T: 98.6 F/37.0 C (oral) Provoking/Palliative: Breast tenderness P: 76 (regular) Quality: Tender to touch and movement R: 18 (regular) Region/Radiation: Both breasts BP: 125/80 Severity: 4/10 but better if wears a bra O2 sat: not assessed Timing: For the past couple of monthsWhat VS data are RELEVANT and must be interpreted as clinically significant by the nurse? (Reduction of Risk Potential/Health Promotion and Maintenance) RELEVANT VS Data: Clinical Significance: 1. Temp, HR, & RR are all within expected/acceptabl e ranges 2. BP is on the upper end of acceptable -There really is no significance to her first three VS, but her BP being on the higher end of acceptable is mildly concerning. Considering how young she is and that she isn’t overweight and doesn’t have any other diagnosed medical conditions, we’d like to see that number be a little lower; especially because as she progresses further into the pregnancy we know that BP will continue to rise. So with her current baseline, she’s at an increased risk of having a BP that’s excessively high later on down the line. Current Assessment: GENERAL APPEARANCE: Calm, body relaxed, no grimacing, appears to be slightly nervous, Height 5’4” (160 cm), weight 100 lbs. (45.5 kg), 5 lbs. (2.3 kg) weight loss from pre-pregnant weight, no appetite. BMI 18 RESP: Breath sounds clear with equal aeration bilaterally ant/post, nonlabored respiratory effort CARDIAC: Pink, warm & dry, no edema, heart sounds regular with no abnormal beats, pulses strong, equal with palpation at radial, brisk cap refill NEURO: Alert and oriented to person, place, time, and situation (x4) HEENT: Normal cephalic, slight bleeding at gum lines. Conjunctiva of eyelids; appears pale Chest: Breasts tender on palpation, areola darkened and occasional veins present Abdomen: Soft; no masses, uterus palpable below the level of the symphysis pubis, Extremities: Mild spider varicose veins on the medial aspect of the left leg, deep tendon reflexes 2+ Pelvic Exam: Vagina and cervix deep purple in color, uterus slightly enlarged, and Hagar’s sign present What assessment data are RELEVANT and must be interpreted as clinically significant by the nurse? (Reduction of Risk Potential/Health Promotion and Maintenance) RELEVANT Assessment Data: Clinical Significance: 1. She’s had a 5lb weight loss since pregnancy 2. She reports some bleeding at the gums 3. Her conjunctiva is pale a. Breasts tender b. Varicose veins—lower extremity c. Purple cervix/ + Hagar’s sign -Her weight lost is concerning, especially since she was so thin to begin with. We already know she has a poor diet that lacks many of the basic nutrients that she and her baby will need -Bleeding of the gums is a common issue during pregnancy, however, it’s one that needs to be addressed. She is more susceptible to plaque buildup with leads in inflammation and bleeding. We’ll need to make sure she focuses more on oral care as far as brushing and flossing her teeth are concerned -The paleness of her conjunctive makes me think we’re looking at some anemia here, especially with the pregnancy and her nutritional history -The other assessment findings are expected and of no concern at this pointLab Results: Prenatal Panel Hemoglobin RPR/VDRL HBsAG Blood type Rubella HCG ELISA Current: 11.0 mg/dL Negative Negative B- Nonimmune 20,700 mlU/ml Negative What lab results are RELEVANT and must be interpreted as clinically significant by the nurse? (Reduction of Risk Potential/Physiologic Adaptation) RELEVANT Lab(s): Clinical Significance: TREND: Improve/ Worsening/ Stable: 1. All these labs are relevant; however, there are some that will need to be addressed. a. Hemoglobi n b. – Rh status c. – neg immunity to Rubella -Her hemoglobin is slightly lower than the expected range in 1st trimester pregnancies. However, since she is pregnant we know that this is something that continue to be depleted with the increased 02 needs of the fetus. It’s important to make sure we can have those levels as high as possible to prepare for this. This can be accomplished by diet and by the use of vitamins as well. -Although, there really isn’t anything we’re going to do with her Rh- status, it needs to be noted -We also can so anything with her lack of immunity to Rubella except remind her to stay away from those that have the disease and urge her to get the vaccine right after she delivers while still in the hospital -This is her initial set of labs, so we have established a baseline for her going forward but not a trend at this point Urine Dipstick Color: Clarity: Sp. Gr. Protein Glucose Ketones Leukocytes/Nitrite Blood Chlamydia Gonorrhea Current: Yellow Clear 1.010 neg neg neg none none positive What lab results are RELEVANT and must be interpreted as clinically significant by the nurse? (Reduction of Risk Potential/Physiologic Adaptation) RELEVANT Lab(s): Clinical Significance: 1. Urine specific gravity 2. + C/G result -Her urine dipstick didn’t reveal to many concerning findings; although, her urine specific gravity is quite high meaning she may not be hydrating herself enough -And her chlamydia/gonorrhea screen came back positive, so we’re going to need to address that and also make sure this isn’t something that she exposes herself to again in the futureLab Planning: Creating a Plan of Care with a PRIORITY Lab (Reduction of Risk Potential/Physiologic Adaptation) Lab: Normal Value: Clinical Significance: Nursing Assessments/Interventions Required: HGB: 11.0 Critical Value: -This low hemoglobin value puts the patient at risk for anemia. Since Hg equals a decreased amount of RBCs, this means there is less 02 to circulate for both mom and baby -explain to the patient to role of hemoglobin for her and her baby and inform her of the results of her blood test -provide supplementation in the way of vitamins - possibly consider IV iron if needed -educate patient on dietary sources of iron so that she can increase her daily intake of those particular items Lab: Normal Value: Clinical Significance: Nursing Assessments/Interventions Required: Chlamydia Gonorrhea POSITIVE Critica l Value: -This is a significant finding. It’s important that we address this. Left intreated, this can lead to lower birth weights and pre-term labor. -We need to make sure we treat the infection successfully and also obtain follow up testing after treatment to ensure there is no evidence of infection -Education also needs to be provided on safe sex practices so as to not become re-infected prior to delivery Clinical Reasoning Begins… 1. Interpreting relevant clinical data, what is the primary concern? What primary health related concepts does this primary problem represent? (Management of Care/Physiologic Adaptation) Problem: Physiology of Changes in OWN Words: Primary Concept: -Our primary concern at this point is the patient’s poor diet and nutrition status -As the fetus grows, more and more energy and nutrients are needed to provide and environment that is suitable for this growth. -Things like protein, glucose, iron, and oxygen are necessary components to this successful growth, and most of this comes from our diet. -It’s important to consume foods that foster that growth and supplement what we can’t get from our diet in the form of vitamins -Healthy mom = healthy baby -You don’t have to eat for two, but you need to increase your caloric intake -Make food choices that encourage optimal growth and function Collaborative Care: Nursing 2. What nursing priority (ies) will guide your plan of care? (Management of Care) Nursing PRIORITY: Provide education to patient and their support persons about theimportance of proper diet and vitamin supplementation during pregnancy PRIORITY Nursing Interventions: Rationale: Expected Outcome: 1. Schedule some sessions with the patient and her support people and provide education on nutrition and diet 2. Provide the patient with prenatal vitamins and explain their purpose and give instructions on usage If the patient and her support system is aware of the benefits of proper diet and nutrition during pregnancy and the negative effects of poor nutrition on mom and baby, it stands to reason that this will increase compliance of the plan of care The outcome of these interventions should moderate the behavior of the patient to initiate a healthier diet that is more conducive to fetal health and growth 3. What body system(s) will you assess most thoroughly based on the primary/priority need? (Reduction of Risk Potential/Physiologic Adaptation) PRIORITY Body System: PRIORITY Nursing Assessments: The GI/Digestive system is the priority body system to that will most heavily be impacted and monitored to assess progress and current status -We will need to consistently monitor the patient’s weight as this is a good indicator of how she is doing with her eating. -We’re also going to want to keep an eye on her labs so that we can assess not only that she is eating, but that she is eating foods that are high in protein, iron, calcium, magnesium etc. 4. What is the worst possible/most likely complication(s) to anticipate based on the primary need for this patient? (Reduction of Risk Potential/Physiologic Adaptation) Worst Possible/Most Likely Complication to Anticipate: Continued lack of adherence to increased dietary needs Nursing Interventions to PREVENT this Complication: Assessments to Identify Problem EARLY: Nursing Interventions to Rescue: 1. Close follow up and monitoring of patient’s nutritional state by assessment of blood work and weight monitoring during the pregnancy 2. Positive reinforcement of compliance 3. Setting reasonable goals that allow the patient to have some input 4. Compromise on things things can be compromised on -Frequently monitor weight at prenatal office visits -Have the patient keep a food journal to be reviewed with the nurse so that planned interventions are properly targeted -As the patient is 17 and still lives at home, involve her parents (if possible) in helping to make sure that she stays on track with appropriate consumption of nutrient dense foods and selfadministration of supplements -As she is still an adolescent, there may be some body image issues going on here. In the event that compliance is difficult to obtain, a nutrition expert and a counselor should be brought in to consult on the matter as well5. What psychosocial/holistic care PRIORITIES need to be addressed for this patient? (Psychosocial Integrity/Basic Care and Comfort) Psychosocial PRIORITIES: Factor in patient’s age and stage in life when making treatment decisions and interventions PRIORITY Nursing Interventions: Rationale: Expected Outcome: CARE/COMFORT: Caring/compassion as a nurse -schedule follow up appointments in the later part of the afternoon so that the patient doesn’t need to leave school early and feel more divided from her peers Physical comfort measures -provide resources that can help the patient feel more comfortable as her pregnancy progresses and make sure she is adequately comfortable during school hours; help with accommodating this if needed -Pregnancy is already a difficult transition for any women; it’s that much more difficult for someone who hasn’t even fully transitioned themselves into adulthood -Using the same methods of care and treatment will not have the same effect because your patient has different priorities and different goals and needs - With a treatment plan and goals that take into account the lifestyle modifications of an adolescent, you increase the probability of their compliance -With goals that the patient has had input in and that factor their individuality into the mix, the patient will maintain adequate levels of caloric intake and nutrition EMOTIONAL (How to develop a therapeutic relationship): Discuss the following principles needed as conditions essential for a therapeutic relationship: • Rapport • Trust • Respect • Genuineness • Empathy Lack of support system -discuss the importance of having a support system in place during pregnancy and offer to set the patient up with a counselor or social worker to meet with her and her mom/dad Unplanned pregnancy -start to discuss what resources the patient has in place for the baby since this was not a planned pregnancy -Emotional support is just as important as physical and/or financial support. Lack of this will have just as much of a fall out if not properly addressed, especially during pregnancy when emotions tend to run rampant. -The patient will have a less stressful pregnancy and a solid support system that will aid her in preparing for the birth of her baby.SPIRITUAL: -Inquire if the patient has any spiritual beliefs; and if so, if any of these beliefs will need to be incorporated into the pregnancy or the birth experience -It’s important to be aware of people’s spiritual beliefs, especially because many times this is a factor in their healthcare as far as decisions and treatment compliance may be concerned. -The patient will express any spiritual beliefs and concerns at initial appointment so that care and treatment decisions can take those beliefs into consideration TWELVE-WEEKS LATER… Anne returns to the office for her fourth visit. She is now 20 weeks pregnant. She states her morning sickness has gotten better and she felt the baby move a few weeks ago. She has gained 10 lbs. (4.5 kg) since the first visit. She had her MFAP and triple marker blood screening labs drawn at 16 weeks which was negative. She has told her parents, and they are supportive. She also told her boyfriend, but he has no interest to be involved. RELEVANT Data: Clinical Significance: -20wks gestation -Resolution of morning sickness -10lb weight gain -16wk screening labs all – (neg) -Support system in place -The patient is halfway through the pregnancy -The resolution of her morning sickness has dissipated allowing patient to gain weight -Patient has an established support system Current VS: First visit: Current PQRST: T: 98.6 F/37.0 C (oral) 98.6 F/37.0 C (oral) Provoking/Palliative: Standing for long time P: 80 (regular) 76 (regular) Quality: Dull R: 18 (regular) 18 (regular) Region/Radiation: Lower back BP: 120/70 125/80 Severity: Mild, 3/10 O2 sat: not assessed not assessed Timing: occasional Current Assessment: GENERAL APPEARANCE: Calm, body relaxed, no grimacing, appears to be resting comfortably RESP: Breath sounds clear with equal aeration bilaterally ant/post, nonlabored respiratory effort CARDIAC: Pink, warm & dry, no edema, heart sounds regular with soft murmur heard at the left sternal border, pulses strong, equal with palpation at radial/pedal/post-tibial landmarks, brisk cap refill NEURO: Alert and oriented to person, place, time, and situation (x4) HEENT: Normal cephalic, slight bleeding at gum lines. Conjunctiva of eyelids appear pale Chest: Breasts tender on palpation, areola darkened and occasional veins present Abdomen: Soft; no masses, uterus palpable at midway between symphysis pubis and umbilicus, light linea nigra present Extremities: Mild spider varicose veins on the medial aspect of the left leg, deep tendon reflexes 2+ Fetal Heart Rate: 150 bpm, Lower Left Quadrant (LLQ)Lab Results: Prenatal Labs Hemoglobin RPR/VDRL HBsAG Blood type Rubella HCG MFAP Triple Marker Current: 10.1 mg/dL Normal Negative Most Recent: First visit 11.0 mg/dL Positive Negative B- Nonimmun e 20,700 mlU/ml 1. What data is RELEVANT and must be interpreted as clinically significant by the nurse? (Reduction of Risk Potential/Health Promotion and Maintenance) RELEVANT VS Data: Clinical Significance: -BP has decreased since last visit -Reports occasional mild lower back pain when standing for long periods of time -Her decrease in blood pressure is a good sign and therefore a trend in a positive direction -She complains of some back back, but that is not an unexpected finding at this point. She does have a job at McDonald’s where constant standing would be involved RELEVANT Assessment Data: Clinical Significance: -Bleeding at the gum line -Pale conjunctiva -Bleeding gums indicate that perhaps there has been no increase in dental hygiene -Pale conjunctiva indicates anemia RELEVANT Lab Data: Clinical Significance: -Hg has decreased even further -Indicates that either iron rich foods have not been getting consumes or perhaps pre-natal vitamins are not being taken regularly 2. Has the status improved or not as expected to this point? Does your nursing priority or plan of care need to be modified in any way after this evaluation assessment? (Management of Care, Physiological Adaptation) Evaluation of Current Status: Modifications to Current Plan of Care: -There has been improvement to the status, just not 100 percent of the goal has been reached -Schedule consultation with a nutrition to see if any alterations can be made to increase dietary intake to more nutrient dense foods 3. Based on your current evaluation, what are your CURRENT nursing priorities and plan of care? (Management of Care) CURRENT Nursing PRIORITY: Focus more heavily on diet and nutrition intake to increase hemoglobin levels PRIORITY Nursing Interventions: Rationale: Expected Outcome: -Have the patient consult with a nutritionist to provide more education and possible meal plan to include necessary items of nutrition during pregnancy -A specialist will more easily be able to pinpoint the source of the problem, whether it is dietary or not and how to better address the issue of correcting the problem -With the help of the specialist, a meal plan can be incorporated into the patient’s daily routing that incorporate the foods needed to obtain adequate nutrition for mom and babyEducation Priorities/Discharge Planning What educational/discharge priorities will be needed to develop a teaching plan for this patient and/or family? (Health Promotion and Maintenance) Education PRIORITY: Adequate day-day care of a newborn PRIORITY Topics to Teach: Rationale: -General care of the newborn: feeding, bathing, sleeping/eating habits, and when to call the provider -As a 17-year-old soon to be parent, it’s probably this patient doesn’t have much experience with babies. She will need education on how to care for the infant to keep them safe and healthy Caring and the “Art” of Nursing What is the patient likely experiencing/feeling right now in this situation? What can you do to engage yourself with this patient’s experience, and show that he/she matters to you as a person? (Psychosocial Integrity) What Patient is Experiencing: How to Engage: -The patient is probably feeling very nervous and scared. There’s no doubt some feeling of excitement, but fear of the unknown (labor, motherhood) is probably the strongest emotion at this point. -Ask the patient how she feels. Find out if she does indeed have any fears, and if so, what they are. Try to see if there are things you can do as the nurse, to address some of those fears. Use Reflection to THINK Like a Nurse Reflection-IN-action (Tanner, 2006) is the nurse’s ability to accurately interpret the patient’s response to an intervention at the moment as the events are unfolding to make a correct clinical judgment. What did you learn that you can apply to future patients you care for? Reflect on your current strengths and weaknesses this case study identified. What is your plan to make any weakness a future strength? What Did You Learn? What did you do well in this case study? I learned that you can lead the horse to water, but you can’t make them drink. Patients are individuals, with their own thoughts, perceptions, beliefs, fears and values. Just because you tell them to do something doesn’t mean that they are going to just automatically listen. You have to be in tune with each patient on an individual level if you want them to change a particular way of being. Without understanding their beliefs and who they are fundamentally, it will be impossible to provide any care that involves the patient making a change to their life as they know. It sounds crazy because you’re just trying to provide the best care to your patients, but without their “buy in” so to speak, you are dead in the water. I think it’s easy to look at a picture and determine what doesn’t “fit”. I’ve always been good at stepping out of the box and trying to assess a situation with a different lens than just the immediate one that’s right in front of one’s face. Critically thinking and determining the root cause of a problem is a strength of mine, some might say to a fault. I say it’s what I do best. What could have been done better? What is your plan to make any weakness a future strength? Determining a contingency plan is something I could have done better. In my personal life, I am the Queen Contingency! I have a backup plan for the backup plan… in the backup plan fails. There’s always a Plan A, Plan B, contingency to Plan B, and a Plan C—in case Plan B’s contingency is a wash. I practice that mindset in my day to day work in the clinical setting with patients in the real world. When I tell a patient The plan is to learn—learn from every mistake, everyone else’s mistakes, and not make that mistake again. We are all going to walk into clinical experiences with weaknesses, that’s a give in. Don’t let that weakness define you; and if you do, let it be the motivation behind making yourself stronger. When we’re dealingthat they can’t smoke anymore now that they have oxygen at home, I’m already thinking of what other resources we can get them set up with to facilitate that when they come back in a month and they still reek of cigarettes. By the time they’ve walked in through the door, I’ve already got brochures ready on quitting, and support group information, and literature on Chantix. I somehow assumed a pregnant woman would be different; that they would immediately follow any and all recommendations because…let’s face it—they’re single handedly responsible for keeping another human safe and [Show More]
Last updated: 1 year ago
Preview 1 out of 11 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Nov 08, 2022
Number of pages
11
Written in
Additional information
This document has been written for:
Uploaded
Nov 08, 2022
Downloads
0
Views
26





 Transcript.png)