*NURSING > EXAM REVIEW > NR511 / NR 511: Differential Diagnosis & Primary Care Practicum Week 5 (Davis Edge) Review Questions (All)
NR511 / NR 511: Differential Diagnosis & Primary Care Practicum Week 5 (Davis Edge) Review Questions Latest Update : Chamberlain College Of Nursing
Document Content and Description Below
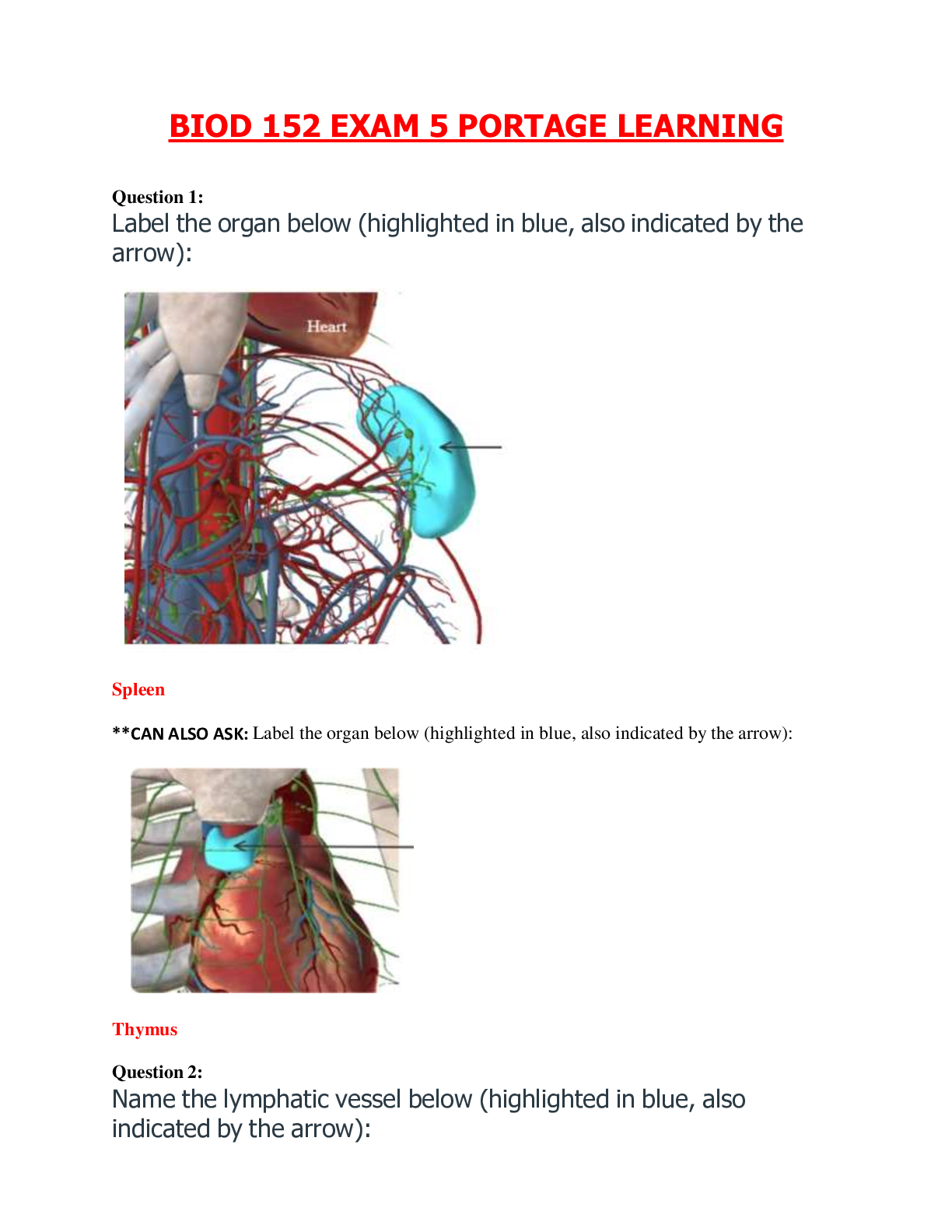
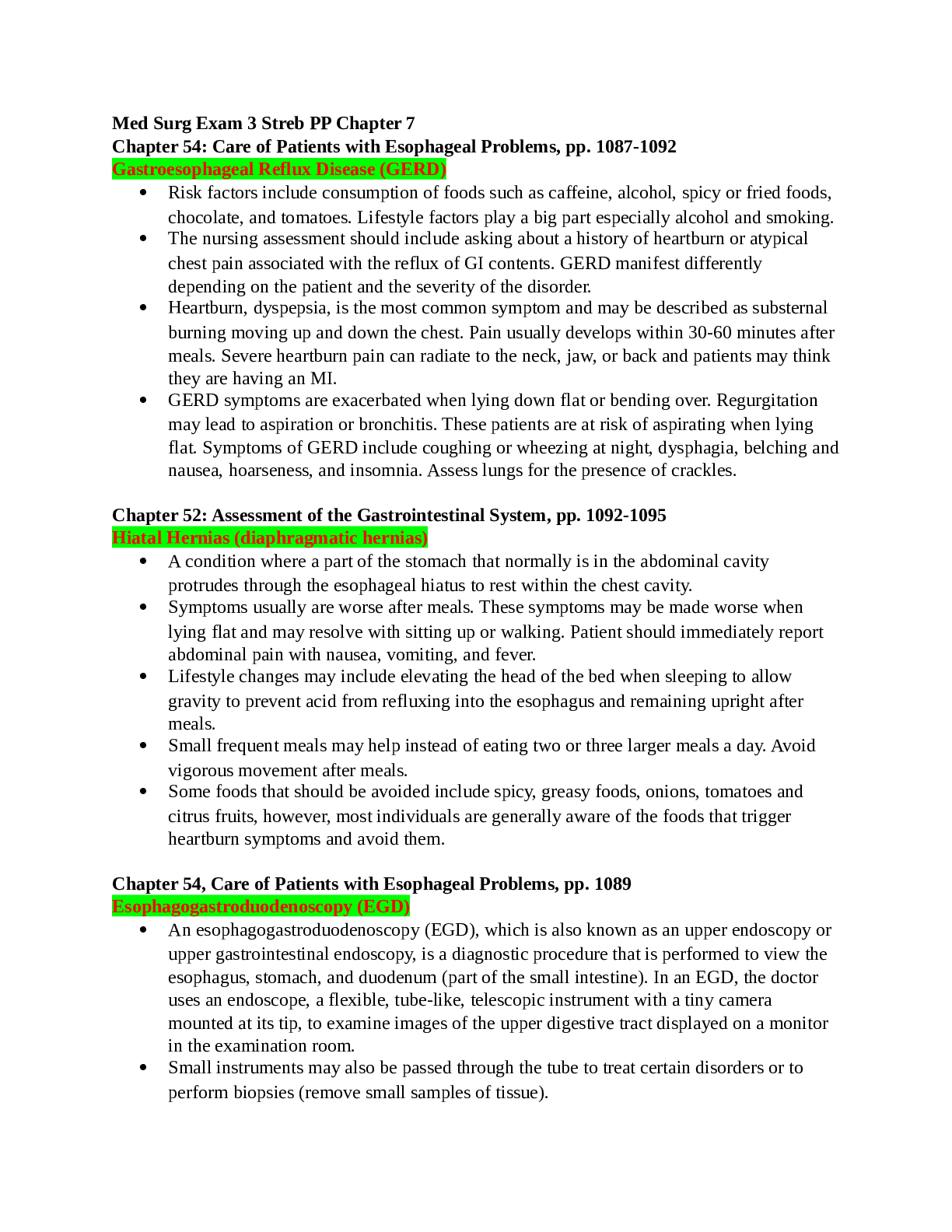
NR-511 Differential Diagnosis & Primary Care Practicum Week 5 (Davis Edge) Review Questions MUSCULOSKELETAL PROBLEMS Question 1. A 13-year-old obese (body mass index [BMI] above the 95t... h percentile) boy reports low-grade left knee pain for the past 2 months. He denies antecedent trauma but admits to frequent “horseplay” with his friends. The pain has progressively worsened, and he is now unable to bear weight at all on his left leg. His current complaints include left groin, thigh, and medial knee pain and tenderness. His examination demonstrates negative drawer, Lachman, and McMurray tests; left hip with decreased internal rotation and abduction; and external hip rotation with knee flexion. Based on the above scenario, the nurse practitioner should suspect: 1. A left meniscal tear. 2. A left anterior cruciate ligament (ACL) tear. 3. A slipped capital femoral epiphysis (SCFE). 4. Osgood-Schlatter disease. Rationales Option 1: There would be a positive McMurray sign in a meniscal tear. Option 2: There would be a positive Lachman and/or drawer test in an ACL tear. Option 3: SCFE is a displacement of the femoral head relative to the femoral neck that occurs through the physis (growth plate) of the femur. The vast majority of clients with this condition are obese, as the added weight increases shear stress across the physis. The mean age at diagnosis is 12 years for females and 13.5 years for males. Surgery is often required via in situ pin fixation (single screw) to stabilize the growth plate to prevent further slippage and avoid complications. Option 4: Osgood-Schlatter disease would result in swelling, pain, and tenderness at the tibial tubercle. Question 2. In assessing the skeletal muscles, the nurse practitioner turns the patient’s forearm so that the palm is up. This is called: 1. Supination. 2. Pronation. 3. Abduction. 4. Eversion. Rationales Option 1: Turning the forearm so that the palm is up is called supination. Option 2: Turning the forearm so that the palm is down is called pronation. Option 3: Moving a limb away from the midline of the body is called abduction. Option 4: Moving the sole of the foot outward at the ankle is called eversion. Question 3. Cass, age 67, tells the nurse practitioner (NP) that she has been diagnosed with a condition that causes sudden flares of pain, swelling, and redness of the joints in her toes. She cannot remember the name of the diagnosis, but she knows it is caused by urate crystals that “get stuck in the joint and cause pain.” She is on hydrochlorothiazide (HCTZ) for management of her hypertension. The NP should suspect a diagnosis of: 1. Septic arthritis. 2. Gout. 3. Rheumatoid arthritis. 4. Charcot neuro-osteoarthropathy. Rationales Option 1: Like gout, septic arthritis presents with an acute onset of swelling, pain, and heat in a joint. However, unlike gout, it occurs most frequently in the knee, followed by the hip, shoulder, wrist, and ankle. Option 2: Gout is a disorder that involves abnormal metabolism of uric acid and results in hyperuricemia. High concentrations of urate precipitate into crystals that collect in tissue and joint spaces and can cause pain and inflammation. The patient’s symptoms may be aggravated by the use of HCTZ. Option 3: Rheumatoid arthritis typically affects multiple joints simultaneously and is a slow and progressive disease. Option 4: Charcot neuro-osteoarthropathy occurs in diabetic patients and presents as hot, swollen, and red joints. These patients usually report a history of trauma, surgery, or prior infection. Question 4. Matthew, age 52, is a chef who just severed 2 of his fingers with a meat cutter. You would recommend that he: 1. Wrap the severed fingers tightly in a dry towel for transport to the emergency department with him. 2. Leave the severed fingers at the scene because fingers cannot be reattached. 3. Immediately freeze the severed fingers for reattachment in the near future. 4. Wrap the fingers in a clean, damp cloth; seal them in a plastic bag; and place the bag in an ice water bath. Rationales Option 1: Severed fingers should be wrapped in a clean, damp cloth; sealed in a plastic bag; and placed in an ice water bath. Option 2: Severed fingers can be reattached after 1 to 2 days—or more—if properly stored. Option 3: Severed fingers should be wrapped in a clean, damp cloth; sealed in a plastic bag; and placed in an ice water bath, not frozen or kept at body temperature. Option 4: If a client has severed his fingers, the fingers should be wrapped in a clean, damp cloth; sealed in a plastic bag; placed in an ice water bath; and transported to the emergency room along with the client. Question 5. Marsha, age 34, presents with symptoms resembling both fibromyalgia and chronic fatigue syndrome, which have many similarities. Which of the following is more characteristic of fibromyalgia than of chronic fatigue syndrome? 1. Musculoskeletal pain. 2. Difficulty sleeping. 3. Depression. 4. Fatigue. Rationales Option 1: Musculoskeletal pain is not characteristic of chronic fatigue syndrome; rather, it is characteristic of fibromyalgia. The musculoskeletal pain, usually an achy muscle pain that may be localized or involve the entire body, is usually gradual in onset, although the onset may occasionally be sudden, such as after a viral illness. Option 2: Difficulty sleeping occurs with both disorders. Option 3: Depression occurs with both disorders. Option 4: Fatigue is a more significant feature of chronic fatigue syndrome. Question 6. Mrs. Kelly, age 80, has a curvature of the spine. This is likely to indicate which age-related change? 1. Lordosis. 2. Dorsal kyphosis. 3. Scoliosis. 4. Kyphoscoliosis. Rationales Option 1: Lordosis occurs when the normal lumbar concavity is further accentuated, such as with pregnancy or obesity. Option 2: Dorsal kyphosis, an exaggerated convexity of the thoracic curvature, typically accompanies the aging process. Option 3: Scoliosis, which is more prevalent in adolescent girls, is a lateral S- or C-shaped curvature of the thoracic and/or lumbar spine that can also involve vertebral rotation. Option 4: Kyphoscoliosis is a combination of kyphosis and scoliosis that involves curvature in both the coronal and sagittal planes. Question 7. The valgus stress test, varus stress test, Lachman test, and thumb sign are all considered standard tests to check the integrity of the ligaments of the knee. Which test would the nurse practitioner choose to assess the anterior cruciate ligament (ACL), which is the most commonly involved structure in severe knee injury? 1. Valgus stress test. 2. Varus stress test. 3. Lachman test. 4. Thumb sign. Rationales Option 1: The valgus stress test assesses stability of the medial collateral ligament (MCL). Option 2: The varus stress test assesses stability of the lateral collateral ligament (LCL). Option 3: The Lachman test assesses the ACL. Option 4: The thumb sign assesses the posterior cruciate ligament (PCL). Question 8. Lillian, age 70, was told that she has osteoporosis. When she asks you what this is, you respond that osteoporosis: 1. Develops when loss of bone occurs more rapidly than new bone growth. 2. Is a degenerative joint disease characterized by loss of cartilage in certain joints. 3. Is a chronic inflammatory disorder that affects multiple joints. 4. Is a bone disorder that has to do with inadequate mineralization of the bones. Rationales Option 1:Osteoporosis develops when bone resorption occurs more rapidly than bone deposition. Option 2: Osteoarthritis is a degenerative joint disease characterized by degeneration and loss of articular cartilage in synovial joints. Option 3: Rheumatoid arthritis is a chronic, systemic inflammatory disorder characterized by persistent synovitis of multiple joints. Option 4: Osteomalacia is a metabolic bone disorder characterized by inadequate mineralization of the bone matrix, often caused by vitamin D deficiency. Question 9. Mike, age 42, a golf pro, has had chronic back pain for many years. His workup reveals that it is not the result of a degenerative disk problem. His back “goes out” about twice per year, and he is out of work for about a week each time. Which of the following should the nurse practitioner advise him to do? 1. Consider changing careers to something less physical. 2. Begin a planned exercise program to strengthen back muscles. 3. Make an appointment with a neurosurgeon for a surgical consultation. 4. Start on a daily low-dose narcotic to take away the pain. Rationales Option 1: Suggesting a career change should be considered only in cases of disability or inability to safely continue one’s current employment. Option 2: In this case, Mike may benefit from a regular planned exercise program to strengthen his back muscles and attempt to reduce the probability of future episodes of back pain. Option 3: Surgery is recommended only for clients with low back pain caused by degenerative disk disorders, and then only when severe neurologic involvement has occurred. Surgery benefits only approximately 1% of people with low back problems. Option 4: Narcotic pain medications are not considered first-line treatment for mechanical back pain. Question 10. Janine, age 69, has class III rheumatoid arthritis. According to the American Rheumatism Association, which of the following describes her ability to function? 1. Adequate for normal activities despite a handicap of discomfort or limited motion of one or more joints. 2. Largely or wholly incapacitated, bedridden, or confined to a wheelchair, permitting little or no self-care. 3. Completely able to carry out all usual duties without handicap. 4. Adequate to perform only a few or none of the duties of usual occupation or self-care. Rationales Option 1: Class II refers to the client whose function is adequate for normal activities despite a handicap of discomfort or limited motion of one or more joints. Option 2: Class IV refers to the client who is largely or wholly incapacitated, bedridden, or confined to a wheelchair, permitting little or no self-care. Option 3: Class I refers to the client who can carry out all usual duties without handicap. Option 4: The American Rheumatism Association has established functional classes I to IV to describe a client’s ability to accomplish activities of daily living. Because Janine is class III, her function would be adequate to perform only a few or none of the duties of usual occupation or self-care. Question 11. Mickey, age 18, is on a chemotherapeutic antibiotic for a musculoskeletal neoplasm. Which drug do you think he is taking? 1. Cyclophosphamide (Cytoxan). 2. Doxorubicin (Adriamycin). 3. Methotrexate (Rheumatrex). 4. Cisplatin (Platinol). Rationales Option 1: Cyclophosphamide (Cytoxan) is an alkylating agent. Option 2: The only antineoplastic antibiotic listed is doxorubicin (Adriamycin). All of the other medications are chemotherapeutic agents of other classifications that may be used for musculoskeletal neoplasms. Option 3: Methotrexate (Rheumatrex) is an antimetabolite. Option 4: Cisplatin (Platinol) is an inorganic platinum agent. Question 12. Upon assessment, the nurse practitioner notes unilateral back pain of acute onset that increases when standing and bending. A straight leg raise test is negative. The most likely diagnosis is: 1. Herniated nucleus pulposus. 2. Muscle strain. 3. Osteoarthritis. 4. Spondylolisthesis. Rationales Option 1: A herniated nucleus pulposus causes unilateral back pain that is acute and increases when sitting or bending but decreases when standing. The straight leg raise test is positive, and the plain x-ray is negative. Option 2: Muscle strain is usually located in the low back and is unilateral in location. The onset is acute, and pain increases with standing and bending and decreases with sitting. The straight leg raise test and plain x-ray are both negative. Option 3: Back pain related to osteoarthritis is usually bilateral in nature and has an insidious onset. Pain increases when standing and decreases when sitting. A straight leg raise test is negative, and a plain x-ray is positive. Option 4: Spondylolisthesis has an insidious onset, and low back pain increases when standing or bending and decreases when sitting. A straight leg raise test is negative, and a plain x-ray is positive. Question 13. A 55-year-old patient presents with complaints of paresthesias in the lower lateral arm, thumb, and middle finger. The nerve roots most commonly related to these symptoms are C6 and C7. The most likely diagnosis would be: 1. Brachial plexus neuritis. 2. Cervical radiculopathy. 3. Peripheral polyneuropathy. 4. Thoracic outlet syndrome. Rationales Option 1: Brachial plexus neuritis presents with dysfunction ranging from momentary paresthesias to completely flail extremities and is usually caused by injuries to the C5 and C6 nerve roots. Option 2: Cervical nerve root compression of C6 and C7 causes cervical radiculopathy. Option 3: Peripheral polyneuropathy is associated with distal sensorimotor paresthesia and diminished deep tendon reflexes. Option 4: Thoracic outlet syndrome is caused by compression of the brachial plexus and/or subclavian vessels as they exit the space between the superior shoulder girdle and the first rib. Symptoms are color changes in the hand and sensory changes and weakness in the fourth and fifth fingers. Question 14. For an adult patient with a knee injury, the nurse practitioner orders a nonsteroidal anti-inflammatory drug (NSAID) to be taken on a routine basis for the next 2 weeks. Patient teaching should include which of the following? 1. “You may take this medication on an empty stomach as long as you eat within two to three hours of taking it.” 2. “If one pill does not seem to help, you can double the dose for subsequent doses.” 3. “If you notice nausea, vomiting, or black or bloody stools, take the next dose with a glass of milk or a full meal.” 4. “If you have additional pain, an occasional acetaminophen (Tylenol) is permitted in between the usual doses of the NSAID.” Rationales Option 1: When teaching clients about NSAIDs, tell them not to take these drugs on an empty stomach but to take them with food or milk. Option 2: Clients should be taught to never take more than the prescribed dose of an NSAID due to the likelihood of increasing the chances of gastrointestinal (GI) and kidney damage. Option 3: When teaching clients about NSAIDs, tell them to stop the medication and call immediately if they notice any nausea, vomiting, coffee-grounds emesis, black stools, or blood in the stool. Option 4: If the client is having additional pain, acetaminophen (Tylenol) may be taken in conjunction with an NSAID because it is not an NSAID and will not potentiate gastric bleeding. Question 15. You are assessing Jamal, age 16, after a football injury to his right knee. You elicit a positive anterior/posterior drawer sign. This test indicates an injury to the: 1. Lateral meniscus. 2. Cruciate ligament. 3. Medial meniscus. 4. Collateral ligament. Rationales Option 1: Meniscal tears are common injuries and common causes of knee joint pain, with the medial meniscus being injured more frequently than the lateral meniscus. The most consistent physical finding of a meniscal tear is tenderness to palpation along the joint line. To examine for a meniscal tear, perform the McMurray test by fully flexing the knee with the leg externally rotated for the medial meniscus and internally rotated for the lateral meniscus. Then firmly extend the leg. A painful cartilage click is considered a positive McMurray test for meniscal injury. Option 2: Positive anterior and posterior drawer signs indicate injury to the anterior cruciate ligament and posterior cruciate ligament, respectively. The drawer and Lachman tests are utilized to assess for cruciate ligament injury. Option 3: Meniscal tears are common injuries and common causes of knee joint pain, with the medial meniscus being injured more frequently than the lateral meniscus. The most consistent physical finding of a meniscal tear is tenderness to palpation along the joint line. To examine for a meniscal tear, perform the McMurray test by fully flexing the knee with the leg externally rotated for the medial meniscus and internally rotated for the lateral meniscus. Then firmly extend the leg. A painful cartilage click is considered a positive McMurray test for meniscal injury. Option 4: The abduction, or valgus, stress test and the adduction, or varus, stress test are used to test the medial collateral ligament (MCL) and lateral collateral ligament (LCL), respectively. Question 16. Sean, a factory line worker, has osteoarthritis (OA) of the right hand. According to the American College of Rheumatology (ACR), the guidelines for pharmacologic treatment include: 1. Acetaminophen, tramadol, and intra-articular corticosteroid injections. 2. Oral nonsteroidal anti-inflammatory drugs (NSAIDs), tramadol, and articular corticosteroid injections. 3. Acetaminophen, topical capsaicin, and topical nonsteroidal anti-inflammatory drugs (NSAIDs). 4. Topical capsaicin, topical nonsteroidal anti-inflammatory drugs (NSAIDs), and oral NSAIDs. Rationales Option 1: Acetaminophen, oral nonsteroidal anti-inflammatory drugs (NSAIDs), tramadol, and intra-articular corticosteroid injections are recommended for initial management of hip OA. Option 2: Acetaminophen, oral NSAIDs, tramadol, and intra-articular corticosteroid injections are recommended for initial management of hip OA. Option 3: The ACR conditionally recommends acetaminophen, oral NSAIDs, topical NSAIDs, tramadol, and intra-articular corticosteroid injections for OA of the knee. Option 4: Topical capsaicin, topical NSAIDs, oral NSAIDs, and tramadol are recommended by the ACR for the treatment of OA of the hand. Question 17. Margaret, age 55, presents to you for evaluation of left hand and wrist pain and swelling after a slip and fall on the ice yesterday. On examination, you note tenderness at her “anatomical snuffbox.” You know this probably indicates a(n): 1. Ulnar styloid fracture. 2. Scaphoid fracture. 3. Hamate fracture. 4. Radial head fracture. Rationales Option 1: An ulnar styloid fracture would produce tenderness at the distal ulna. Option 2: There is tenderness over the “anatomical snuffbox” in a scaphoid (aka navicular) fracture, the most common injury of the carpal bones. Poor blood supply puts the scaphoid bone at risk of avascular necrosis; therefore, wrist pain and tenderness in the anatomical snuffbox, even without history of antecedent trauma, warrant a wrist x-ray. Option 3: A fracture of the hook of the hamate is an uncommon injury seen in golfers and players of racket sports that involves pain and tenderness on the ulnar side of the palm. Option 4: A radial head fracture would result in pain at the elbow joint where the radial head lies proximal to the distal humerus. Be sure not to confuse the radial head (proximal end of the radius) with the radial styloid (distal end of the radius at the wrist). Question 18. Christian, age 22, is a carpenter who is right hand dominant. He comes to the clinic for follow-up from the emergency department, where he was seen for right forearm pain. He states he was diagnosed with right forearm tendinitis and wants the provider to explain this diagnosis to him. Patient teaching should explain that he has inflammation of one or more tendons, which are: 1. The ropelike bundles of collagen fibrils that connect bone to bone. 2. The collagen fibers that connect muscle to bone. 3. The pouches of synovial fluid that cushion bone and other joint structures. 4. The fibrocartilaginous disks that separate bony surfaces. Rationales Option 1: Ligaments connect bone to bone at the joints. Option 2: Tendons are the collagen fibers that connect muscle to bone. Option 3: Bursae are the pouches of synovial fluid that reduce friction between bones, muscles, and tendons. Option 4: Fibrocartilaginous disks separate bony surfaces, such as those between the vertebrae. Question 19. Steve, age 32, fell off a roof while shingling it. He is complaining of pain in his left hip and leg area. Other than an x-ray, what would make you suspect a fractured pelvis? 1. A clicking sensation when moving the hips. 2. A positive pelvic tilt test. 3. Hematuria. 4. Absence of distal reflexes. Rationales Option 1: A clicking sensation when moving the hips is not diagnostic of a fractured pelvis. Option 2: A positive pelvic tilt test is not diagnostic of a fractured pelvis. Option 3: If a client has a fractured pelvis, a test for hematuria will usually prove positive. A fracture of the pelvis usually results in hypovolemia due to a generally significant associated blood loss. Surrounding blood vessels rupture, which results in a large retroperitoneal hematoma and shock. Pelvic fractures also commonly injure the urinary bladder or urethra. A client with a fracture in several locations of the pelvis may need a pneumatic antishock garment to control the blood loss and stabilize the pelvis. Only x-ray studies will confirm the diagnosis. Option 4: Absence of distal reflexes is not correlated with a fracture of the pelvis. Question 20. John, age 16, works as a stock boy at the local supermarket. He is in the office for a routine visit. You notice that he had an episode of low back pain 6 months ago after lifting heavy boxes improperly. In discussing with him proper body mechanics to prevent future injuries, you tell him: 1. “Bend your knees and face the object straight on.” 2. “Hold boxes away from your body at arm’s length.” 3. “Bend and twist simultaneously as you lift.” 4. “Keep your feet firmly together.” Rationales Option 1: In discussing with John proper body mechanics to prevent future injuries, you tell him to bend his knees and face the object straight on, to hold boxes close to his body and not at arm’s length, and to spread his feet about shoulder width apart. Using legs and arms, facing objects straight on, and keeping a wide stance will provide a broad base of support and allow for use of supporting muscles, relieving stress on the back muscles. Option 2: He should hold boxes close to his body. Option 3: He should never bend and twist simultaneously, but rather keep the spine straight to minimize injury. Option 4: He should spread his feet about shoulder width apart. Question 21. During assessment of a client’s foot, the nurse practitioner notes that the foot is in alignment with the long axis of the lower leg and that weight-bearing falls on the middle of the foot from the heel, along the midfoot, to between the second and third toes. These findings best describe: 1. A normal foot. 2. Hallux valgus. 3. Talipes equinovarus. 4. Hammertoes. Rationales Option 1: If you note during your assessment of your client’s foot that the foot is in alignment with the long axis of the lower leg and that weight-bearing falls on the middle of the foot from the heel, along the midfoot, to between the second and third toes, you would diagnose a normal foot. Option 2: Hallux valgus is a common deformity in which a lateral or outward deviation of the toe and medial prominence of the head of the first metatarsal are present. Option 3: Talipes equinovarus (clubfoot) is a congenital defect; it presents as a rigid and fixed malposition of the foot, including inversion, forefoot adduction, and downward foot pointing. Option 4: A hammertoe deformity is common in hallux valgus and is a deformity in the second, third, fourth, or fifth toe that includes hyperextension of the metatarsophalangeal joint and flexion of the proximal interphalangeal joint. Question 22. Jeffrey, age 16, was involved in a motor vehicle accident. He walks in to the office with an obvious facial fracture and then collapses. What should the first action of the nurse practitioner be? 1. Calling his parents for permission to treat. 2. Assessing for an adequate airway. 3. Obtaining a head and maxillofacial computed tomography (CT). 4. Assessing for a septal hematoma. Rationales Option 1: Once his airway is established as adequate and stable and he is stabilized, permission to treat Jeffrey can be obtained from his parents. Option 2: The primary concern in the management of facial fractures is ensuring an adequate and stable airway. Displaced soft tissues, blood, secretions, or other foreign material may obstruct the airway and cause asphyxia. Option 3: A head and maxillofacial CT would be obtained once Jeffrey’s airway was established. Option 4: Septal hematomas are more commonly seen in children than in adults, but the first priority is to maintain an adequate airway. Question 23. Beth, age 49, comes in with low back pain. An x-ray of the lumbosacral spine is within normal limits. Which of the following diagnoses do you explore further? 1. Scoliosis. 2. Osteoarthritis. 3. Spinal stenosis. 4. Herniated nucleus pulposus. Rationales Option 1: A plain x-ray will show scoliosis. Option 2: A plain x-ray will show osteoarthritis. Option 3: A plain x-ray will show spinal stenosis. Option 4: A plain x-ray will not show a herniated nucleus pulposus or a muscle strain. It will show spondylolisthesis, scoliosis, osteoarthritis, and spinal stenosis. Note that x-rays of the spine are not indicated in low back pain unless the cause of the pain is thought to be bony in origin or traumatic in nature or there is a need to rule out systemic disease. Question 24. The nurse practitioner suspects adolescent idiopathic scoliosis in Victoria, age 15, who is in her “growth spurt.” An Adams forward bend test is performed, and it is noted that the patient has a right-sided rib hump. What is this indicative of? 1. Right lumbar shifting. 2. Right thoracic curvature. 3. Right truncal shift. 4. Spondylolysis. Rationales Option 1: The shifting has occurred in the right thoracic curve, not the lumbar region. Option 2: When you have a client bend forward to assess the spine (ie, the Adams forward bend test) and you note a right-sided rib hump, this is indicative of a right thoracic curve. Adolescent idiopathic scoliosis is defined as a lateral spinal curvature of greater than 10 degrees with no determined pathologic cause. Management consists of the 3 Os: observation, orthosis, and operation. Option 3: Victoria’s right-sided rib hump is the result of a right thoracic curve, not a truncal shift. Option 4: Spondylolysis is a bony defect of the pars interarticularis. Question 25. Jim, age 22, a stock boy, has an acute episode of low back pain. The nurse practitioner orders a nonsteroidal anti-inflammatory drug (NSAID) and should educate him in which of the following? 1. Maintaining moderate bed rest for 3 to 4 days. 2. Calling the office for narcotic medication if there is no relief with the NSAID after 24 to 48 hours. 3. Beginning lower back strengthening exercises depending on pain tolerance. 4. Wearing a Boston brace at night. Rationales Option 1: Years ago, muscle relaxants and bed rest were the treatments of choice for low back pain. Studies have now shown that resuming normal activity within the limits imposed by the pain has an effect as good as, if not better than, 2 days of bed rest. Option 2: NSAIDs, not narcotics, are generally the first-line medication treatment of low back pain and have no risk of opioid dependency. Option 3: Years ago, muscle relaxants and bed rest were the treatments of choice for low back pain. Studies have now shown that resuming normal activity within the limits imposed by the pain has an effect as good as, if not better than, 2 days of bed rest. The key here is letting pain be your guide. Exercise should begin as soon as possible after the acute injury and be directed at building endurance and stamina, with consideration given to one’s pain tolerance. Option 4: A Boston brace may be used in the treatment of scoliosis. Question 26. Jessie, age 49, states she thinks she has rheumatoid arthritis. Before any diagnostic tests are ordered, the nurse practitioner completes a physical examination and makes a diagnosis of osteoarthritis rather than rheumatoid arthritis. Which clinical manifestation ruled out rheumatoid arthritis? 1. Fatigue. 2. Affected joints are swollen, cool, and bony hard on palpation. 3. Decreased range of motion. 4. Joint stiffness. Rationales Option 1: Fatigue is common to both diseases. Option 2: In osteoarthritis, the affected joints are swollen, cool, and bony hard on palpation. With rheumatoid arthritis, the affected joints are red, hot, and swollen and boggy and tender on palpation. Option 3: Decreased range of motion is common to both diseases. Option 4: Joint stiffness is common to both diseases. Question 27. Joyce, age 87, broke her wrist after falling off a curb. She just had a plaster cast applied to her wrist. In instructing Joyce and her family on allowing the cast to dry properly, tell them to: 1. Continuously elevate Joyce’s arm on a pillow. 2. Change the position of Joyce’s arm every hour. 3. Position a fan near Joyce during the night to ensure even drying of the cast. 4. Put a blanket over the cast to absorb the dampness. Rationales Option 1: Elevating her arm will prevent edema, but continuous elevation is not needed. Option 2: Instructions to the client and family on how to allow a cast to dry properly should include advising them to change the position of the casted extremity every hour. In this case, Joyce’s arm should be repositioned frequently to prevent indentations in the cast itself (caused by continuous placement on a pillow) and to ensure drying of all surfaces of the cast. Option 3: A fan will dry only the outside of the cast. Option 4: A blanket will prevent drying of the cast. Question 28. Sandy, age 49, presents with loss of anal sphincter tone, impaired micturition, incontinence, and progressive loss of strength in the legs. You suspect cauda equina syndrome. What is your next action? 1. Ordering physical therapy. 2. Ordering a lumbosacral x-ray. 3. Ordering extensive lab work. 4. Referring to a neurosurgeon. Rationales Option 1: A prompt referral to a neurosurgeon is required when a diagnosis of cauda equina syndrome is suspected. Option 2: An x-ray is not helpful in the diagnosis of cauda equina syndrome, and precious time should not be wasted with a client who has suspected cauda equina syndrome. Magnetic resonance imaging (MRI) can be a useful diagnostic tool, but prompt evaluation by a neurosurgeon is an essential first step in preventing permanent neurologic damage. Option 3: A prompt referral to a neurosurgeon is required when a diagnosis of cauda equina syndrome is suspected. Option 4: A prompt referral to a neurosurgeon is required when a diagnosis of cauda equina syndrome is suspected. Cauda equina syndrome is a widespread neurologic disorder in which there is loss of anal sphincter tone; impaired micturition; incontinence; saddle anesthesia (ie, loss of sensation in the anus, perineum, genitals, and inner thighs); and motor weakness or sensory loss in both legs. Question 29. When teaching Alice, age 77, to use a cane because of osteoarthritis of her left knee, an important point to stress is: 1. Carrying the cane in the ipsilateral hand. 2. Advancing the cane with the ipsilateral leg. 3. Making sure the cane length equals the height of the iliac crest. 4. Using the cane to aid in joint protection and safety. Rationales Option 1: The cane should be carried in the contralateral hand. Option 2: When teaching clients about using a cane, tell them to advance the cane with the ipsilateral (affected) leg. Option 3: The cane length should equal the height of the greater trochanter. Option 4: The use of assistive devices is an important strategy for protecting the joints and providing safety, but clients must be taught the proper use of all devices. Question 30. June, age 67, presents with back pain with no precipitating event. The pain is located over her lower back muscles and spine, without sciatica, and it is aggravated by sitting, standing, and certain movements. It is alleviated with rest. Palpation localizes the pain, and muscle spasms are felt. There was an insidious onset with progressive improvement. What is the most likely diagnosis? 1. Ankylosing spondylitis. 2. Musculoskeletal strain. 3. Spondylolisthesis. 4. Herniated disk. Rationales Option 1: Ankylosing spondylitis refers to back pain and stiffness occurring over several months due to a systemic inflammatory condition of the vertebral column and sacroiliac joints. Painful ankylosed sacroiliac joints, reduced chest wall expansion, and excessive thoracic kyphosis are also present. There is also reduced flexibility of the spine and relief with exercise. It most frequently affects males between the ages of 20 and 30 and causes chronic low back pain that is worse in the morning. Option 2: Pain over the lower back muscles and spine, without sciatica, is caused by musculoskeletal strain. Often there is no precipitating event, and there is an insidious onset. It is aggravated by sitting, standing, and certain movements. Palpation localizes the pain, and muscle spasms may be felt. It is alleviated by rest, and there is progressive improvement. Option 3: With spondylolisthesis, there is a defect or fracture of the pars interarticularis and forward shifting of one vertebra on top of another. This can cause nerve irritation and damage if the vertebrae are pressing on a spinal nerve root. Option 4: A herniated disk is often preceded by years of recurrent episodes of localized back pain, and there is usually leg pain that overshadows the back pain. Question 31. You are caring for a patient who has a history of psoriasis and is now showing signs of joint involvement. Seropositivity provides a definitive diagnosis of psoriatic arthritis (PsA). The initial treatment choice for management of the patient is: 1. Disease-modifying antirheumatic drugs (DMARDs). 2. Nonsteroidal anti-inflammatory drugs (NSAIDs). 3. Tumor necrosis factor-alpha (TNF-α) inhibitors. 4. Uricosuric medications. Rationales Option 1: DMARDs, such as methotrexate, are used for early-stage treatment of active disease with structural damage and inflammation. Option 2: NSAIDs are the first-line treatment for musculoskeletal signs and symptoms with joint involvement. Option 3: Biologic agents, or TNF-a inhibitors, are considered for patients with active disease and inadequate response to one or more systemic DMARDs or very active PsA. Option 4: A uricosuric such as probenecid, with the addition of the anti-inflammatory colchicine, is indicated for chronic gouty arthritis. Question 32. Anne, age 67, sustained a fall on an outstretched hand. She presents holding her arm against her chest with her elbow flexed. Based on the specific location of her pain, you suspect a radial head fracture. The best initial strategy to assess for a radial head fracture would be: 1. To palpate for tenderness, swelling, and crepitus just distal to the lateral epicondyle. 2. To palpate for tenderness, swelling, and crepitus along the radial wrist. 3. To palpate for tenderness in the “anatomical snuffbox.” 4. To order an x-ray of the wrist. Rationales Option 1: The radial head is the proximal aspect of the radius, located in the elbow joint. Falling on an outstretched hand transfers a significant amount of force to the radial head. Often a fracture line cannot be seen on an x-ray, but the presence of an anterior or posterior fat pad sign (or sail sign) indicates an occult radial head fracture. Option 2: Tenderness, swelling, and crepitus at the radial wrist could indicate a distal radius fracture or fracture of the carpal bones. Option 3: Tenderness in the “anatomical snuffbox” indicates a possible fracture of the scaphoid bone in the wrist. Option 4: A wrist x-ray will demonstrate abnormalities of only the distal radius, ulna, and carpal bones. An elbow x-ray would assist in the diagnosis of a radial head fracture. Question 33. Hilda, age 73, presents with a complaint of low back pain. Red flags in her history of a minor fall, osteopenia, and prolonged steroid use for systemic lupus erythematosus suggest the possibility of which of the following serious underlying conditions as the cause of her low back pain? 1. Cancer. 2. Cauda equina syndrome. 3. Neurologic compromise. 4. Spinal fracture. Rationales Option 1:Cancer may be suspected if the low back pain is accompanied by unexplained weight loss and immunosuppression in a person over age 50. Option 2: Low back pain accompanied by acute onset of urinary retention or overflow incontinence, loss of anal sphincter tone or fecal incontinence, loss of sensation in the buttocks and perineum, and motor weakness in the lower extremities is a red flag for cauda equina syndrome or severe neurologic compromise. Option 3: Low back pain accompanied by acute onset of urinary retention or overflow incontinence, loss of anal sphincter tone or fecal incontinence, loss of sensation in the buttocks and perineum, and motor weakness in the lower extremities is a red flag for cauda equina syndrome or severe neurologic compromise. Option 4: The red flags for spinal fracture include major trauma or direct blow to the back in an adult, a minor fall or heavy lifting in a potentially osteoporotic or elderly person, prolonged steroid use, and age greater than 70. Question 34. Anne Marie states she has a maternal history of rheumatoid disease, but she has never been affected. Today she presents with complaints of dryness of the eyes and mouth. What is the most likely diagnosis? 1. Rheumatoid arthritis (RA). 2. Systemic lupus erythematosus (SLE). 3. Sjögren syndrome. 4. Rosacea. Rationales Option 1:Because Anne Marie has no other symptoms of RA or systemic lupus erythematosus (SLE), Sjögren syndrome should be considered first. Option 2: Because Anne Marie has no other symptoms of rheumatoid arthritis (RA) or SLE, Sjögren syndrome should be considered first. Option 3: Sjögren syndrome, which affects the salivary and lacrimal glands, causes clients to have dry eyes and mouths. It is an inflammatory disease of the exocrine glands and may be an isolated entity or may be associated with other rheumatic diseases, such as rheumatoid arthritis (RA) or systemic lupus erythematosus (SLE). Option 4: Rosacea is a chronic facial skin disorder with a vascular component. Question 35. A nurse practitioner is driving home from work and stops at the scene of a motorcycle accident that must have just occurred, as there are no rescue vehicles present. The driver is lying unconscious at the side of the road with an obvious open fracture of his femur. Which of the following actions should take priority? 1. Stopping the bleeding from the wound. 2. Determining if there has been a cervical fracture. 3. Establishing an airway. 4. Palpating the peripheral pulses. Rationales Option 1: This is an important action, but establishing an airway is the first priority. Option 2: This is an important action, but establishing an airway is the first priority. Option 3: Follow the ABCs of first aid: airway, breathing, and circulation. Establishing an airway is the first priority, followed by breathing, and then circulation. Stopping the bleeding from the wound, assessing if there has been a cervical fracture, and palpating the peripheral pulses are all important actions, but if the client is not breathing, the other actions will not be necessary. Option 4: This is an important action, but establishing an airway is the first priority. Question 36. A nurse practitioner is trying to distinguish between an articular and a nonarticular musculoskeletal complaint in a 26-year-old patient complaining of pain in the elbow area. Which of the following would characterize nonarticular bursitis? 1. Deep or diffuse pain. 2. Limited range of motion (ROM) on active and passive movement. 3. Point or focal tenderness. 4. Swelling and instability. Rationales Option 1: Deep or diffuse pain is characteristic of articular disorders. Option 2: Limited ROM on active and passive movement is characteristic of articular disorders. Option 3: Articular disorders are characterized by deep or diffuse pain, limited range of motion (ROM) on both active and passive movement, swelling, crepitation, instability, and deformity. Nonarticular disorders are characterized by painful active but not passive movement and point or focal tenderness in regions far from articular surfaces. Option 4: Swelling and instability are characteristic of articular disorders. Question 37. Greg, age 26, runs marathons and frequently complains of painful contractions of his calf muscles after running. You attribute this to: 1. Hypercalcemia. 2. Hyponatremia. 3. Heat exhaustion. 4. Dehydration. Rationales Option 1: Hypercalcemia may affect gastrointestinal, renal, and neurologic function. Symptoms may include constipation and polyuria as well as nausea, vomiting, and anorexia at times. Option 2: Painful contractions of muscles after exertion, such as heat cramps, may be related to hyponatremia or other electrolyte imbalances. Usually the gastrocnemius and hamstring muscles are involved. Treatment of heat cramps includes passive muscle stretching, cessation of activities, transfer to a cooler environment, and drinking cool liquids. Sports drinks that contain electrolytes, such as Gatorade, may be beneficial. Option 3: Heat exhaustion is a more serious condition, with symptoms ranging from nausea, vomiting, headache, loss of appetite, and dizziness to irritability, tachycardia, and hyperventilation. Option 4: Greg’s painful muscle contractions are attributed to his hyponatremia, but this would be a good second choice. Question 38. Mr. McKinsey, age 69, was recently given a diagnosis of degenerative joint disease. Which assessment should the nurse practitioner use to check for effusion of the patient’s knee? 1. Thomas test. 2. Tinel test. 3. Bulge test. 4. Phalen test. Rationales Option 1: The Thomas test is used to assess for hip problems. Option 2: The Tinel test assesses for carpal tunnel syndrome. Option 3: The bulge test assesses for an effusion of the knee. If effusion is present, a bulge will appear at the sides of or below the patella when the practitioner compresses the area above the patella. Option 4: The Phalen test assesses for carpal tunnel syndrome. Question 39. The nurse practitioner is considering a diagnosis of calcium pyrophosphate deposition disease (CPPD), or pseudogout, in a 72-year-old man who presents with complaints of pain and stiffness in his wrists and knees. The most useful diagnostic tests to assist in confirming this diagnosis would be: 1. Synovial fluid analysis and x-ray. 2. Bacterial cultures. 3. Bone scan and magnetic resonance imaging (MRI). 4. Anticitrullinated protein antibodies (ACPA) and rheumatoid factor (RF). Rationales Option 1: CPPD (pseudogout) may appear clinically similar to gouty arthritis; however, in CPPD crystals form in the cartilage and lead to inflammation. The typical age of onset is later than that of gout, initially presenting in the sixth decade of life or later. Diagnosis is made through synovial fluid analysis and will reveal positive calcium pyrophosphate dihydrate crystals. An x-ray will show radiographic evidence of chondrocalcinosis or calcification in the hyaline cartilage and/or fibrocartilage of the affected joint. Option 2: Bacterial cultures would be warranted to aid in the diagnosis of cellulitis. Option 3: Bone scan and MRI are used to differentiate gouty arthritis from Charcot neuro-osteoarthropathy. Option 4: ACPA and RF assist in the diagnosis of rheumatoid arthritis. Question 40. Ethan, age 10, jumped off a 2-foot wall, twisting his foot and ankle upon landing. His ankle x-ray demonstrates a fracture of the distal tibia, over the articular surface, through the epiphysis and physis. Based on the Salter-Harris classification of growth plate injuries, you know this is a: 1. Salter-Harris II fracture. 2. Salter-Harris III fracture. 3. Salter-Harris IV fracture. 4. Salter-Harris V fracture. Rationales Option 1: A Salter-Harris II fracture travels through the metaphysis and physis. Option 2: The Salter-Harris classification system of growth plate injuries divides most growth plate injuries into 5 categories based on the damage: A Salter-Harris III fracture travels through the epiphysis and physis. A Salter-Harris I fracture travels through the physis. Option 3: A Salter-Harris IV fracture travels through the metaphysis, epiphysis, and physis. Option 4: A Salter-Harris V fracture involves a compression injury of the physis. Question 41. Sam, age 50, presents with Paget disease that has been stable for several years. Recently, his serum alkaline phosphatase level has been steadily rising. The nurse practitioner determines that it is time to start him on pharmacologic management. Which of the following should she initially prescribe? 1. Nonsteroidal anti-inflammatory drugs (NSAIDs). 2. Corticosteroids. 3. Bisphosphonates. 4. Calcitonin. Rationales Option 1: NSAIDs are helpful for clients with Paget disease who have mild symptoms and pain. Option 2: Corticosteroids do inhibit bone metabolism, but their use is limited by the side effects of long-term therapy with high doses. Option 3: When the serum alkaline phosphatase level rises—which indicates the disease has progressed—bisphosphonates, which decrease bone resorption by inhibiting osteoclast activity, are the treatment of choice. Option 4: Calcitonin (Calcimar) also inhibits osteoclastic bone resorption but is not as powerful as the bisphosphonates and does not suppress disease activity for as long after cessation. Question 42. James, age 17, has been complaining of a painful knob below his right knee that has prevented him from actively participating in sports. He has recently been given a diagnosis of Osgood-Schlatter disease and asks you about his treatment options. The nurse practitioner should tell him that the initial treatment is: 1. Relative rest; he could benefit from hamstring, heel cord, and quadriceps stretching exercises. 2. Immobilization; a long-leg knee immobilizer is recommended. 3. Surgical intervention; removal of the bony fragments is necessary. 4. Bed rest for 1 week. Rationales Option 1: Osgood-Schlatter disease is an overuse injury that results from the excessive tension and pull of the patellar tendon on the tibial tuberosity. Treating the client conservatively while an adolescent will prevent potential problems as an active adult. Initially, relative rest should be used with hamstring, heel cord, and quadriceps stretching exercises. Option 2: If the problem persists, a long-leg knee immobilizer may be used. Option 3: Surgical intervention is rarely required and then only in adults after bone growth is complete. Option 4: Rest should be combined with stretching and strengthening exercises. Question 43. In assessing a patient, you place the tips of your first 2 fingers in front of each ear and ask the patient to open and close his mouth. Then you drop your fingers into the depressed area over the joint and assess for smooth motion of the mandible. With this action, you are checking for: 1. Maxillomandibular integrity. 2. Well-positioned permanent teeth or well-fitting dentures. 3. Temporomandibular joint syndrome. 4. Mastoid inflammation. Rationales Option 1: Maxillomandibular integrity indicates a properly functioning temporomandibular joint (TMJ). Option 2: In most cases, well-positioned permanent teeth and well-fitting dentures prevent the development of temporomandibular joint (TMJ) syndrome. Option 3: In assessing your client, place the tips of your first 2 fingers in front of each ear and ask him to open and close his mouth. Then drop your fingers into the depressed area over the temporomandibular joint (TMJ) and check for smooth motion of the mandible. With this action, you are assessing for TMJ syndrome. Clicking or popping noises, decreased range of motion, pain, or swelling may indicate TMJ syndrome. However, an audible and palpable snap or click does occur in many normal people as they open their mouths. In rare cases, this may indicate osteoarthritis. Option 4: Mastoid inflammation is manifested behind, not in front of, the ear. Question 44. Sandra, a computer programmer, has just been given a new diagnosis of carpal tunnel syndrome. The nurse practitioner’s next step is to: 1. Refer her to a hand surgeon. 2. Take a more complete history. 3. Try neutral position wrist splinting and order an oral nonsteroidal anti-inflammatory drug (NSAID). 4. Order nerve conduction studies and electromyography (EMG). Rationales Option 1:For refractory cases, median nerve decompression may be accomplished with surgery, but complete recovery is not possible if atrophy is pronounced. Option 2: Taking a more complete history is not essential at this point because a diagnosis has already been made. Option 3: For the client who has just been given a diagnosis of carpal tunnel syndrome, your next step is to try neutral position wrist splinting and order an oral NSAID. For symptoms of less than 10 months’ duration, conservative treatment should be tried first. Option 4: Nerve conduction studies and EMG confirm focal median nerve conduction delay within the carpal canal and also provide information about disease severity. Question 45. A 55-year-old patient is able to complete range of motion (ROM) against gravity with some resistance. The nurse practitioner would assign which of the following numerical grades to this manual muscle testing description? 1. 5. 2. 4. 3. 3. 4. 2. Rationales Option 1: Normal muscle strength and function and complete ROM against gravity with full or normal resistance would be given a numerical grade of 5. Option 2: Complete ROM against gravity with some resistance is given a numerical grade of 4 and described as good muscle strength. Option 3: Complete ROM against gravity is indicative of fair muscle strength and function and is given a numerical grade of 3. Option 4: A grade of 2, denoting poor muscle strength, is given for complete ROM with gravity eliminated. Question 46. Alexander, age 12, sprained his ankle playing ice hockey. He is confused as to whether he should apply heat or cold. What should the nurse practitioner tell him? 1. “Use continuous heat for the first 12 hours and then use heat or cold to your own preference.” 2. “Use continuous cold for the first 12 hours and then use heat or cold to your own preference.” 3. “Apply cold for 20 minutes, then remove it for 30 to 45 minutes; repeat this for the first 24 to 48 hours while awake.” 4. “Alternate between cold and heat for 20 minutes each for the first 24 to 48 hours.” Rationales Option 1: Applying heat may increase swelling and subsequently slow recovery. Option 2: Ice has been proven to speed recovery in ankle sprains; however, ice should never be applied continuously because it could hinder proper circulation and cause frostbite. Therefore, always recommend protective padding between the ice and the skin. Option 3: Tell a client who has sprained his ankle to apply cold for 20 minutes, then remove it for 30 to 45 minutes, and repeat that procedure for the first 24 to 48 hours while awake. Cold will cause vasoconstriction and decrease edema, preventing any further bleeding into the tissues. After any sprain, use the principles of RICE: rest, ice, compression, and elevation. Option 4: Applying heat may increase swelling and subsequently slow recovery. Question 47. Daniel, age 45, is of Northern European ancestry and has a dysfunctional and disfiguring condition affecting the palmar tissue under the skin of the distal palm and fourth and fifth fingers. What do you suspect? 1. Hallux valgus. 2. De Quervain tenosynovitis. 3. Dupuytren contracture. 4. Hallux rigidus. Rationales Option 1:Hallux valgus, commonly referred to as a bunion, is an osseous deformity of the metatarsophalangeal (MTP) joint of the great toe that involves medial deviation of the toe. Option 2: De Quervain tenosynovitis is a painful inflammation of tendons around the thumb. Option 3: Dupuytren contracture affects the palmar tissue under the skin of the distal palm and fingers—most often the fourth and fifth fingers, but also the thumb-index finger web space. It is progressive and results in a flexion contracture, though it does not affect the flexor tendons. Occurring most frequently in males between the ages of 40 and 60, it is common among people of Northern European ancestry. It is dysfunctional and disfiguring. Although it is not actually painful, it may be tender. Surgery is recommended when the inability to straighten the fingers limits the client’s hand function. Option 4: Hallux rigidus is a common type of arthritis that affects the base of the great toe at the metatarsophalangeal (MTP) joint, causing stiffness and decreased movement of the great toe. Question 48. Paul has a malignant fibrosarcoma of the femur. He recently had surgery and is now on radiation therapy. You want to order a test to determine the extent of the tumor invasion of the surrounding tissues and the response of the bone tumor to the radiation. Which of the following tests should you order? 1. An x-ray. 2. A magnetic resonance imaging (MRI) scan. 3. A computed tomography (CT) scan. 4. A needle biopsy. Rationales Option 1: A conventional x-ray will show the location of the tumor and the extent of bone involvement. Metastatic bone destruction has a characteristic “moth-eaten” pattern in which the growth has a poorly defined margin that cannot be separated from normal bone. Option 2: For Paul, who has a malignant fibrosarcoma of the femur, an MRI scan will determine the extent of the tumor invasion of the surrounding tissues and the response of the bone tumor to the radiation. It will also determine response to chemotherapy and detect recurrent disease. Option 3: A CT scan will evaluate the extent of the tumor invasion of bone, soft tissues, and neurovascular structures. Option 4: A needle biopsy, usually performed at the time of surgery, will determine the type of tumor. Question 49. The nurse practitioner (NP) suspects a herniated disk in a 72-year-old patient. The NP elevates the patient’s affected leg when she is in the supine position, and it elicits back and sciatic nerve pain, which indicates a positive test. This is known as which test or sign? 1. Femoral stretch test. 2. Crossed straight leg raise test. 3. Doorbell sign. 4. Straight leg raise test. Rationales Option 1: The femoral stretch test is done with the client prone and the leg extended and knee flexed. Pain radiating to the anterior thigh indicates L4 radiculopathy. Option 2: In the crossed straight leg raise test, the uninvolved leg is elevated; sciatic pain down the contralateral leg indicates a herniated disk. Option 3: The doorbell sign indicates development of radiculopathy when the patient’s symptoms are reproduced by compressing the neurologic and muscular structures in the lateral aspect of the neck. Option 4: All of the tests listed are tests done to assess for a herniated disk. In the straight leg raise test, you elevate the affected leg when the client is in the supine position; back pain and sciatic nerve pain (ie, radiating leg pain) indicate a herniated disk. Question 50. Jill, age 49, has recently begun a rigorous weightlifting regimen. She presents to the primary care office with a shoulder dislocation. Which of the following clinical manifestations leads the nurse practitioner to suspect an anterior shoulder dislocation over a posterior dislocation? 1. Inability to shrug the shoulder. 2. Absence of pain. 3. Inability to rotate the shoulder externally. 4. Shortening of the arm. Rationales Option 1: Clinical manifestations of an anterior shoulder dislocation, which is far more common than a posterior dislocation, include the inability to shrug the shoulder, pain, and lengthening of the arm. Option 2: Pain is a clinical manifestation of anterior shoulder dislocation. Option 3: The inability to rotate the shoulder externally, along with the inability to elevate the arm, is a clinical manifestation of a posterior shoulder dislocation. Option 4: Lengthening of the arm is a clinical manifestation of anterior shoulder dislocation. Question 51. Karen, who is postmenopausal, is taking 1200 mg of calcium daily but does not understand why she also needs to take vitamin D. You tell her that: 1. A deficiency of vitamin D results in inadequate mineralization of bone matrix. 2. All vitamins need to be supplemented. 3. Vitamin D increases intestinal absorption of dietary calcium and mobilizes calcium from the bone. 4. Vitamin D binds with calcium to allow active transport into the cells. Rationales Option 1: Vitamin D deficiency does result in inadequate mineralization of bone matrix (ie, rickets)—which is more commonly seen in children—but that is not the reason why Karen should take vitamin D. Option 2: Not all vitamins need to be supplemented; indeed, harm can result if certain vitamins are taken in higher than recommended doses. Option 3: Advise clients taking calcium supplements that they also need to take vitamin D because vitamin D raises serum calcium levels by increasing the intestinal absorption of dietary calcium and mobilizing calcium from the bone. Option 4: Vitamin D does not bind with calcium to allow active transport into the cells. Question 52. Lois, age 52, who has just been given a diagnosis of sarcoidosis, has joint symptoms, including arthralgias and arthritis. Your next plan of action would be to: 1. Order a bone scan. 2. Obtain a tissue biopsy. 3. Begin a course of glucocorticoids. 4. Order daily doses of vitamin B. Rationales Option 1: There is no present need for a bone scan. Option 2: There is no present need for a tissue biopsy. Option 3: Sarcoidosis is the result of an exaggerated immune system response to a class of antigens or self-antigens. Fifty percent of clients experience joint symptoms, including myopathy and polyarthritis; glucocorticoids are prescribed to suppress the immune process, thus relieving symptoms. Option 4: Vitamin B is not routinely ordered, as it has not been shown to impact sarcoidosis. Question 53. The nurse practitioner (NP) is assessing Maya, a 69-year-old Asian woman, for the first time. When trying to differentiate between scoliosis and kyphosis, the NP recalls that kyphosis involves: 1. Asymmetry of the shoulders, scapulae, and waist creases. 2. A lateral curvature and vertebral rotation on posteroanterior x-rays. 3. One leg appearing shorter than the other. 4. A posterior rounding at the thoracic level. Rationales Option 1: Scoliosis involves asymmetry of the shoulders, scapulae, and waist creases. Option 2: Scoliosis involves a lateral curvature and vertebral rotation on posteroanterior x-rays. Option 3: In a client with scoliosis, the legs may appear uneven in length. Option 4: Kyphosis involves a posterior rounding at the thoracic level and a kyphotic curve of more than 45 degrees on an x-ray. There may be moderate pain with kyphosis. Question 54. Alan, age 46, presents with a tender, red, swollen knee. You rule out septic arthritis and diagnose gout by confirming: 1. An elevated white blood cell (WBC) count. 2. Hyperuricemia. 3. A significant response to a dose of ceftriaxone (Rocephin). 4. A positive antinuclear antibody test. Rationales Option 1: A septic joint would likely cause an elevated WBC and a positive bacterial joint culture. Option 2: To diagnose gout, there should be hyperuricemia and a negative joint culture. Option 3: Ceftriaxone (Rocephin) is an antibiotic used in the treatment of bacterial infections such as septic arthritis. Option 4: A positive antinuclear antibody test may indicate systemic lupus erythematosus or scleroderma. [Show More]
Last updated: 1 year ago
Preview 1 out of 23 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Nov 14, 2020
Number of pages
23
Written in
Additional information
This document has been written for:
Uploaded
Nov 14, 2020
Downloads
0
Views
47


x.png)

.png)

.png)