*NURSING > EXAM REVIEW > NR511 / NR 511: Differential Diagnosis & Primary Care Practicum Week 2 (Davis Edge) Review Questions (All)
NR511 / NR 511: Differential Diagnosis & Primary Care Practicum Week 2 (Davis Edge) Review Questions Latest Update : Chamberlain College Of Nursing
Document Content and Description Below
NR-511 Differential Diagnosis & Primary Care Practicum Week 2 (Davis Edge) Practice Questions 1. Jill, a 34-year-old bank teller, presents with symptoms of hay fever. She complains of nasa... l congestion, runny nose with clear mucus, and itchy nose and eyes. On physical assessment, you observe that she has pale nasal turbinates. What is your diagnosis? a) Allergic rhinitis (The symptoms of hay fever, also called allergic rhinitis, are similar to those of viral rhinitis but usually persist and are seasonal in nature. When assessing the nasal mucosa, you will observe that the turbinates are usually pale or violaceous because of venous engorgement) b) Viral rhinitis (with viral rhinitis, the turbinates are typically erythematous) c) Nasal polyps (With nasal polyps, there are usually yellowish, boggy masses of hypertrophic mucosa) d) Nasal vestibulitis from folliculitis (Nasal vestibulitis usually results from folliculitis of the hairs that line the nares) 2. A 75-year-old African American male presents to your family practice office complaining of visual impairment. He has worn corrective lenses for many years but has noticed that his vision has gotten progressively worse the past 6 months. He denies pain. He states his vision is worse in both eyes in the peripheral aspects of his visual field. He also notes trouble driving at night and halos around street lights at night. You test his intraocular pressure, and it is 23 mm Hg. What is his most likely diagnosis? a) Open-angle glaucoma (This is the typical presentation of chronic, or open-angle, glaucoma) b) Angle-closure glaucoma (This is an acute, painful form of glaucoma) c) Cataracts (This is a loss of central vision) d) Macular degeneration (This also affects central vision) 3. Which of the following is not a cause of conductive hearing loss? a) Presbycusis (This is a cause of sensorineural hearing loss) b) Cerumen impaction. c) Otitis media. d) Otosclerosis. 4. Which of the following is not a complication of untreated group A streptococcal pharyngitis? a) Glomerulonephritis. b) Rheumatic heart disease. c) Scarlet fever. d) Hemolytic anemia (This is a complication of mononucleosis) 5. Alexandra, age 34, was treated with oral antibiotics 2 weeks ago for a urinary tract infection. She is seen in the office today for a follow-up visit. On physical examination, the nurse practitioner notices that she has some painless, white, slightly raised patches in her mouth. This is probably caused by: a) Herpes simplex (Herpes simplex (a viral infection) sores are usually discrete and not spread over a large area) b) Aphthous ulcers (Aphthous ulcers (canker sores) are extremely painful) c) Candidiasis (Painless, white, slightly raised patches in a client’s mouth are probably caused by candidiasis (thrush) d) Oral cancer (Cancerous lesions are usually discrete and not spread over a large area) 6. Mattie, age 64, presents with blurred vision in 1 eye and states that it felt like “a curtain came down over my eye.” She doesn’t have any pain or redness. What do you suspect? a) Retinal detachment (The classic sign of retinal detachment is a client stating that “a curtain came down over my eye.” Typically, the person presents with blurred vision in 1 eye that becomes progressively worse, with no pain or redness) b) Acute angle-closure glaucoma (In older adults with acute angle-closure glaucoma, there is a rapid onset, with severe pain and profound visual loss. The eye is red, with a steamy cornea and a dilated pupil) c) Open-angle glaucoma (In older adults with open-angle glaucoma, there is an insidious onset, a gradual loss of peripheral vision over a period of years, and a perception of “halos” around lights) d) Cataract (With a cataract, there is blurred vision that is progressive over months or years and no pain or redness) 7. While doing a face, head, and neck examination on a 16-year-old patient, you note that the palpebral fissures are abnormally narrow. What are you examining? a) The nasolabial folds (The nasolabial folds are the skin creases that extend from the angle of the nose to the corners of the mouth) b) The openings between the margins of the upper and lower eyelids (The palpebral fissures are the openings between the margins of the upper and lower eyelids. Someone who appears to be squinting is said to have narrow palpebral fissures) c) The thyroid gland in relation to the trachea (The thyroid is a butterfly-shaped gland located in the front of the neck, just below the Adam’s apple; it is wrapped around the trachea) d) The distance between the trigeminal nerve branches (The trigeminal nerve is the fifth cranial nerve located within the brain. It is composed of 3 branches—ophthalmic, maxillary, and mandibular—and is primarily responsible for transmitting sensations from the face to the brain. It is also the nerve that controls the muscles used for chewing) 8. When the Weber test is performed with a tuning fork to assess hearing and there is no lateralization, the nurse practitioner should document this finding as: a) Conductive deafness (With conductive deafness, sound lateralizes to the defective ear because it is transmitted through bone rather than air) b) Perceptive deafness (With perceptive deafness, sound lateralizes to the better ear) c) A normal finding (A Weber test assesses hearing by bone conduction. With normal hearing, sound is heard equally well in both ears, meaning there is no lateralization) d) Nerve damage (Damage to cranial nerve VIII (CN VIII), the vestibulocochlear nerve, causes symptoms of hearing loss, vertigo, and loss of equilibrium) 9. What significant finding(s) in a 3-year-old child with otitis media with effusion would prompt more aggressive treatment and referral? a) There is a change in the child’s hearing threshold to greater than 25 dB (If a child with otitis media with effusion has a change in the hearing threshold greater than 25 dB and has notable speech and language delays, more aggressive treatment is indicated. When the child’s hearing examination reveals a change in the hearing threshold, it is extremely important that the provider evaluate the child’s achievement of developmental milestones in speech and language. Any abnormal findings warrant referral) b) The child has become a fussy eater. c) The child’s speech and language skills seem slightly delayed. d) Persistent rhinitis is present. 10. A 25-year-old client who plays in a band complains that he finds it difficult to understand his fellow musicians at the end of a night of performing, a problem that is compounded by the noisy environment of the club. These symptoms are most characteristic of which of the following? a) Sensorineural loss (Sensorineural loss comes from exposure to loud noises, inner ear infections, tumors, congenital and familial disorders, and aging. The results of the Weber and Rinne tests will assist in the diagnosis) b) Conductive loss (The etiology of conductive loss includes ear infection, presence of a foreign body, perforated drum, and otosclerosis of the ossicles) c) Tinnitus (Tinnitus is ringing in the ears. The client does not complain of this symptom) d) Vertigo (Vertigo is dizziness associated with inner ear dysfunction. The client does not complain of this symptom) 11. A 64-year-old obese woman comes in complaining of difficulty swallowing for the past 3 weeks. She states that “some foods get stuck” and she has been having “heartburn” at night when she lies down, especially if she has had a heavy meal. Occasionally, she awakes at night coughing. She denies weight gain and/or weight loss, vomiting, or change in bowel movements or color of stools. She denies alcohol and tobacco use. There is no pertinent family history or findings on review of systems (ROS). Physical examination is normal, with no abdominal tenderness, and the stool is occult blood (OB) negative. What is the most likely diagnosis? a) Esophageal varices. b) Esophageal cancer. c) Gastroesophageal reflux disease (GERD) (Though the historical data are incomplete, this client has no obvious risk factors for esophageal varices or esophageal cancer. She is a nondrinker and denies weight loss and changes in bowel function or color of stools, which could be a clue to a gastrointestinal bleed. The fact that her worst symptoms occur at night with regurgitation and heartburn is classic for GERD. Dysphagia is frequently a prominent symptom of GERD. She has no abdominal tenderness, and aside from the nighttime symptoms and dysphagia, she reports no symptoms with food or lack of food) d) Peptic ulcer disease (PUD). 12. Marcia, age 4, is brought in to the office by her mother. She has a sore throat, difficulty swallowing, copious oral secretions, respiratory difficulty, stridor, and a temperature of 102°F but no pharyngeal erythema or cough. What do you suspect? a) Epiglottitis (A symptom cluster of severe throat pain with difficulty swallowing, copious oral secretions, respiratory difficulty, stridor, and fever but without pharyngeal erythema or cough is indicative of epiglottitis) b) Group A beta-hemolytic streptococcal pharyngitis (Streptococcal pharyngitis presents with cervical adenitis, petechiae, a beefy-red uvula, and a tonsillar exudate) c) Tonsillitis (A mild case of tonsillitis may appear to be only a slight sore throat. A more severe case would involve inflamed, swollen tonsils; a very sore throat; and a high fever) d) Diphtheria (Diphtheria starts with a sore throat, fever, headache, and nausea, and then progresses to patches of grayish or dirty-yellowish membranes in the throat that eventually grow into 1 membrane) 13. An 80-year-old woman comes in to the office with complaints of a rash on the left side of her face that is blistered and painful and accompanied by left-sided eye pain. The rash broke out 2 days ago, and she remembers being very tired and feeling feverish for a week before the rash appeared. On examination, the rash follows the trigeminal nerve on the left, and she has some scleral injection and tearing. You suspect herpes zoster ophthalmicus. Based on what you know to be complications of this disease, you explain to her that she needs: a) Antibiotics. b) A biopsy of the rash. c) Immediate hospitalization. d) Ophthalmological consultation (In this case, because the herpes virus seems to be along the ophthalmic branch of cranial nerve V, there is considerable risk that this client could develop permanent damage in that eye; therefore, an ophthalmological consult needs to be arranged promptly to ascertain current damage and prevent any further damage) 14. You are assessing a first grader and find that the tonsils are touching the uvula. How would you grade this finding? a) Grade 1 (Grade 1 indicates the tonsils are visible) b) Grade 2 (Grade 2 indicates the tonsils are halfway between the tonsillar pillars and the uvula) c) Grade 3 (Grade 3 indicates the tonsils are touching the uvula. Tonsils are enlarged to 2, 3, or 4 with an acute infection) d) Grade 4 (Grade 4 indicates the tonsils are touching each other) 15. Nystatin (Mycostatin) is ordered for Michael, a 56-year-old banker who has an oral fungal infection. What instructions for taking the medication do you give Michael? a) “Dilute the oral medication with one tablespoon of water for easier digestion.” (The oral medication should not be diluted, as that may compromise the absorption) b) “Take the medication with meals so that it’s absorbed better.” (Taking the medication with meals may compromise the absorption) c) “Swish and swallow the medication.” (When ordering nystatin (Mycostatin) for an oral fungal infection, tell the client to swish the medication in the mouth to coat all the lesions and then to swallow it) d) “Apply the medication only to the lesions.” (It is almost impossible to apply this liquid medication to only the lesions; swishing it in the mouth coats all the lesions more effectively) 16. April, age 50, presents with soft, raised, yellow plaques on her eyelids at the inner canthi. She is concerned that they may be cancerous skin lesions. You tell her that they are probably: a) Xanthelasmas (Xanthelasmas are soft, raised, yellow plaques on the eyelids at the inner canthi. They appear frequently in women, in their 50s. Xanthelasmas occur with both high and normal lipid levels and have no pathological significance) b) Pingueculae (Pingueculae are yellowish, elevated nodules appearing on the sclera. They are caused by a thickening of the bulbar conjunctiva from prolonged exposure to the sun, wind, and dust) c) The result of arcus senilis (Arcus senilis appears as gray-white arcs or circles around the limbus and is a result of deposits of lipid material that make the cornea look cloudy) d) Actinic keratosis (Actinic keratoses are wartlike growths on the skin that occur in middle-aged or older adults and are caused by excessive exposure to the sun) 17. Cynthia, a 31-year-old woman with a history of depression, is seen in the office today for complaints of headaches. She was recently promoted at her job, and this has caused increased stress. She describes the headache as a tightening (viselike) feeling in the temporal and nuchal areas. The pain is bilateral and tends to wax and wane. It started approximately 2 days ago and is still present. What kind of headache is she describing? a) Classic migraine (Classic migraine headaches occur after an aura, which may include visual, auditory, or olfactory symptoms) b) Tension headache (Tension headache is the most common type of headache. These headaches are usually bilateral and tend to wax and wane but have a characteristic pressure/tightening (viselike grip) in the forehead, temporal, or nuchal areas and can last from minutes to weeks. Tension headache may be associated with stress, depression, or anxiety disorders) c) Sinus headache (Sinus headache would usually be precipitated by allergies or cold symptoms. These headaches are described as pain, pressure, or fullness in the cheeks, brow, or forehead, with worsening pain when leaning forward) d) Cluster headache (Cluster headaches come in clusters, with exquisite pain that awakens the client from sleep. They are more common in males than females) 18. In a young child, unilateral purulent rhinitis is most often caused by: a) A foreign body (In a young child, unilateral purulent rhinitis is most often caused by a foreign body. The key word here is unilateral) b) A viral infection (Viral infections usually affect both nares) c) A bacterial infection (Bacterial infections usually affect both nares) d) An allergic reaction (Allergic reactions usually affect both nares) 19. Kevin, age 26, has AIDS and presents to the clinic with complaints of a painful tongue covered with what look like creamy white, curdlike patches overlying erythematous mucosa. You are able to scrape off these “curds” with a tongue depressor, which assists you in making which of the following diagnoses? a) Leukoplakia (Leukoplakia cannot be removed by rubbing the mucosal surface; it appears as little white lesions on the tongue) b) Lichen planus (Oral lichen planus is a chronic inflammatory autoimmune disease; it also has white lesions that do not rub off) c) Oral candidiasis (Oral candidiasis (thrush) is distinctive because the white areas on the tongue can be rubbed off with a tongue depressor. Thrush may be seen in denture wearers, in debilitated clients, and in those who are immunocompromised or taking corticosteroids or broad-spectrum antibiotics) d) Oral cancer (Oral cancer must be ruled out in any lesion because early detection is the key to successful management and a good prognosis) 20. You diagnose 46-year-old Mabel with viral conjunctivitis. Your treatment should include: a) Gentamicin ophthalmic ointment (Antibiotics should not be used in clients with viral conjunctivitis) b) Ciprofloxacin ophthalmic drops (Antibiotics should not be used in clients with viral conjunctivitis) c) Supportive measures and lubricating drops (artificial tears) (Viral conjunctivitis is treated with supportive measures, including cold compresses and lubricating eye drops. Preventive measures, such as frequent handwashing, are important, as viral conjunctivitis is highly contagious) d) Oral erythromycin for 14 days (Antibiotics should not be used in clients with viral conjunctivitis) 21. The antibiotic of choice for recurrent acute otitis media (AOM) and/or treatment failure in children is: a) Amoxicillin (Amoxil) (Amoxicillin (Amoxil) is used as the first-line treatment of AOM. However, it is not used in patients with recurrent AOM or treatment failure) b) Amoxicillin and potassium clavulanate (Augmentin) (The antibiotic of choice for recurrent AOM or treatment failure is amoxicillin and potassium clavulanate (Augmentin) c) Azithromycin (Zithromax) (Azithromycin (Zithromax) for otitis media is usually reserved for patients with penicillin allergy) d) Prednisone (Deltasone) (Prednisone (Deltasone) is not an antibiotic) 22. Kevin, a 56-year-old lawyer, has throbbing pain in the left eye, an irregular pupil shape, marked photophobia, and redness around the iris. What is your initial diagnosis? a) Conjunctivitis (A client with conjunctivitis has redness more prominently at the periphery of the eye, along with tearing and itching. The client may also complain of a scratchy, burning, or gritty sensation but not pain, although photophobia may be present) b) Iritis (If a client has throbbing pain in the eye, an irregular pupil shape, marked photophobia, and redness (a deep, dull, red halo or ciliary flush) around the iris and/or cornea, suspect iritis. An immediate referral is warranted. The client may also have blurred vision) c) Subconjunctival hemorrhage (A client with subconjunctival hemorrhage presents with sudden onset of a painless, bright-red appearance on the bulbar conjunctiva that usually results from pressure exerted during coughing, sneezing, or Valsalva maneuver. Other conditions that may result in a subconjunctival hemorrhage include uncontrolled hypertension and the use of anticoagulant medication) d) Acute glaucoma (A client with acute glaucoma presents with circumcorneal redness, with the redness radiating around the iris, and a dilated pupil) 23. Mallory brings her 4-week-old infant to the office because she noticed small, yellow-white, glistening bumps on her infant’s gums. She says they look like teeth, but she is worried that they may be cancer. You diagnose these bumps as: a) Bednar aphthae (Bednar aphthae are traumatic areas or ulcers that appear on the posterior hard palate on either side of the midline. They result from abrasions while sucking) b) Epstein pearls (Bednar aphthae are traumatic areas or ulcers that appear on the posterior hard palate on either side of the midline. They result from abrasions while sucking) c) Buccal tumors (A buccal tumor is a tumor on the inside of the cheek) d) Exostosis (Exostosis (torus palatinus) is found in the midline of the posterior two-thirds of the hard palate and is benign. It is a smooth, symmetrical bony structure) 24. Mandy, 44, was given a diagnosis of flu 1 day ago and wants to start on the “new flu medicine” right away. What do you tell her? a) “The medication is effective only if started within the first 72 hours after symptoms begin.” (Oseltamivir (Tamiflu) and zanamivir (Relenza) are most effective if started early in the course of the disease (within 48 hours after symptoms begin) b) “If you treat a cold, it goes away in 7 days; if you don’t treat it, it goes away in 1 week.” (The flu is not a cold (rhinovirus)) c) “The medicine has not proven its effectiveness.” (Oseltamivir (Tamiflu) and zanamivir (Relenza) are particularly effective against the influenza viruses that cause the flu) d) “I’ll start you on oseltamivir (Tamiflu) today. It may shorten the course of the disease and perhaps lessen the severity of your symptoms.” (Two antiviral drugs, oseltamivir (Tamiflu), a pill taken by mouth, and zanamivir (Relenza), an inhaled medication, are particularly effective against the influenza viruses that cause the flu. If the virus causing the flu is type A influenza, the client may benefit from either one of these drugs) 25. Sally, age 19, presents with pain and pressure over her cheeks and discolored nasal discharge. You cannot transilluminate the sinuses. You suspect which sinus to be affected? a) Maxillary sinus (The maxillary sinus is the largest of the paranasal sinuses and is the most commonly affected sinus. There is usually pain and pressure over the cheek. Inability to transilluminate the cavity usually indicates a cavity filled with purulent material. Discolored nasal discharge, as well as a poor response to decongestants, may also indicate sinusitis.) b) Ethmoid sinus (The ethmoid sinuses are usually nonpalpable and may not be transilluminated) c) Sphenoid sinus (The sphenoid sinuses are usually nonpalpable and may not be transilluminated) d) Frontal sinus (The frontal sinuses are just below the eyebrows. Frontal sinusitis also includes pain and tenderness of the forehead) 26. A 10-year-old male in 5th grade presents to the pediatric office with his mother complaining of itchy and red eyes for 1 day. The patient complains of watery drainage in both eyes, associated with repetitive itching. On physical exam, he has no fever or constitutional symptoms. His vision is normal, with no decrease in extraocular movements. The patient has a sibling that just started day care recently. He also has bilateral preauricular lymph nodes that are inflamed. What is the patient’s diagnosis? a) Viral conjunctivitis (This is the classic presentation of viral conjunctivitis. The patient also has exposure to kids at school and a sibling with day care exposure) b) Bacterial conjunctivitis. c) Allergic conjunctivitis. d) Blepharitis (This would present with red eye and purulent discharge, especially at the eyelashes and around the eye) 27. A 75-year-old female presents to your office complaining of dizziness and hearing loss. The patient states she awoke yesterday with dizziness, which she described as feeling the room spinning. She also notes intermittent ringing in her ears. On physical exam, the patient has lateralization of her hearing loss to the unaffected ear. Rinne test shows air conduction lasts longer than bone conduction. What is the next step in helping this patient’s symptoms? a) Order a computed tomography (CT) scan to rule out acoustic neuroma. b) Start her on high-dose Augmentin. c) Start the patient on a low-salt, low-caffeine diet and give her meclizine for vertigo attacks (This is the treatment for symptoms of Meniere disease. You would also want to consider an ear, nose, and throat consult to rule out other etiologies of the patient’s symptoms. Meniere disease is diagnosed based on history and the exclusion of other conditions as well) d) Immediate referral to an ear, nose, and throat (ENT) specialist. 28. A 6-year-old female presents to your pediatric office with her mother complaining of right ear pain for 3 days. This pain resolved with Tylenol. The patient has also had noted fevers of 101.3°F over the last 2 nights. The patient had a nonproductive cough for 7 days prior to the ear pain. On physical exam, the patient has tenderness with tugging on the auricle of the ear. The tympanic membrane is not mobile with pneumatic otoscopy and is erythematous and full. The patient has no drainage from the ear and no mastoid tenderness. What is the next step? a) Symptom management and reassurance that symptoms will resolve with time. b) Computed tomography (CT) of the head. c) Amoxicillin 80 to 90 mg/kg/d (This is the treatment of choice for acute otitis media) d) Augmentin 45 mg/kg/d (This is the treatment of choice for chronic/treatment-resistant otitis media) 29. You prescribe Levaquin (levofloxacin) for a severe sinus infection. What is not a possible adverse reaction to this medication? a) Achilles tendon rupture. b) Peripheral neuropathy. c) Nephrotoxicity. d) Stevens-Johnson syndrome (Stevens-Johnson syndrome is usually caused by allopurinol and beta-lactam antibiotics) 30. A 20-year-old male presents to your primary care clinic. This patient is a college student. He complains of fatigue, sore throat, and low-grade fever for 3 days. On physical exam, he has a temperature of 100.7°F. His ear exam is normal. His nose and throat exam shows mild erythema of the nasal mucosa and edematous, enlarged tonsils bilaterally, with erythema of the pharyngeal wall and tonsillar exudates. He has inflamed posterior cervical lymph nodes. He has a mild nonproductive cough and clear lung exam. What is his most likely diagnosis? a) Viral pharyngitis. b) Mononucleosis (This presentation could be a viral pharyngitis; however, with posterior cervical lymphadenitis, you would suspect mononucleosis) c) Streptococcal pharyngitis. d) Upper respiratory infection. 31. Which of the following is not recommended for hoarseness? a) Vocal rest. b) Tobacco cessation. c) Decrease in caffeine use. d) Oral steroids (Oral steroids are not routinely used to treat hoarseness) 32. Marlene, a 57-year-old cashier, comes to the clinic because she is unable to differentiate between sharp and dull stimulation on both sides of her face. You suspect: a) Bell palsy (Bell palsy affects the facial nerve, resulting in weakness or paralysis of 1 side of the face) b) A lesion affecting the trigeminal nerve (A lesion affecting the sensory portion of the trigeminal nerve could be manifested by bilateral symptoms) c) A stroke—brain attack, cerebrovascular accident (CVA) (A stroke is unilateral in its presentation) d) Shingles (Shingles is unilateral in its presentation) 33. Sharon, a 47-year-old bank teller, is seen by the nurse practitioner in the office for a red eye. You are trying to decide between a diagnosis of conjunctivitis and iritis. One distinguishing characteristic between the two is: a) Eye discomfort (Clients with iritis and those with conjunctivitis both complain of eye discomfort, although in iritis the pain is moderately severe, with intermittent stabbing) b) Slow progression (Both conditions generally produce a slowly progressive redness.) c) A ciliary flush (When trying to decide between a diagnosis of conjunctivitis and iritis, one distinguishing characteristic is the ciliary flush present in iritis. Photophobia is not usually present in conjunctivitis, but it is always present with iritis. Photophobia occurs with corneal inflammation, iritis, and angle-closure glaucoma) d) No change in or slightly blurred vision (Vision is normal with conjunctivitis and blurred with iritis) 34. Susan is a 19-year-old college student and avid swimmer. She frequently gets swimmer’s ear and asks if there is anything she can do to help prevent it other than wearing earplugs, which do not really work for her. What do you suggest? a) Start using a cotton-tipped applicator to dry the ears after swimming. b) Use ear drops made of a solution of equal parts alcohol and vinegar in each ear after swimming (Using ear drops made of a solution of equal parts alcohol and vinegar in each ear after swimming is effective in drying the ear canal and maintaining an acidic environment, therefore preventing a favorable medium for the growth of bacteria, the cause of swimmer’s ear) c) Use a hair dryer on the highest setting to dry the ears. d) Stop swimming 35. Which of the following conditions produces sharp, piercing facial pain that lasts for seconds to minutes? a) Trigeminal neuralgia (Trigeminal neuralgia is described as a sharp, piercing, shooting facial pain that is severe but usually lasts only a short time. The origin is cranial nerve V (CN V), the trigeminal nerve) b) Temporomandibular joint (TMJ) syndrome (TMJ dysfunction is associated with pain on opening and closing the mouth and is also associated with crepitus of that joint) c) Goiter (A goiter is generally painless) d) Preauricular adenitis (Preauricular adenitis (enlarged and inflamed preauricular nodes) would be sustained until the etiological cause was identified and treated) 36. Mary, age 82, presents with several eye problems. She states that her eyes are always dry and look “sunken in.” What do you suspect? a) Hypothyroidism (With hyperthyroidism, the eyes appear to bulge out (exophthalmos), but in hypothyroidism, the eyes do not appear any different) b) Normal age-related changes (Dryness of the eyes and the appearance of “sunken” eyes are normal age-related changes) c) Cushing syndrome (A moon face is apparent with Cushing syndrome, and this might make the eyes appear to be sunken in, although on close examination, they are not) d) A detached retina (With a detached retina, the outward appearance is normal, but the client complains of seeing floaters or spots in the visual field and describes the sensation as like a curtain being drawn across the vision) 37. Marjorie, age 37, has asthma and has been told she has nasal polyps. What do you tell her about them? a) Nasal polyps are usually precancerous. b) Nasal polyps are benign growths (Nasal polyps are benign growths that occur frequently in clients with sinus problems, asthma, and allergic rhinitis. Polyps are neither neoplastic growths nor precancerous, but they do have the potential to affect the flow of air through the nasal passages. Clients who have asthma and have nasal polyps may have an associated allergy to aspirin, a syndrome that is referred to as Samter triad.) c) The majority of nasal polyps are neoplastic. d) They are probably inflamed turbinates, not polyps, because polyps are infrequent in clients with asthma. 38. Erica, age 39, has a sudden onset of shivering, sweating, headache, aching in the orbits, and general malaise and misery. Her temperature is 102°F. The nurse practitioner diagnosed her with influenza (flu). What is your next course of action? a) Order amoxicillin (Amoxil) 500 mg every 12 hours for 7 days. b) Prescribe rest, fluids, acetaminophen (Tylenol), and possibly a decongestant and an antitussive (Management of flu is generally symptomatic and includes rest, fluids, acetaminophen (Tylenol), and possibly a decongestant and an antitussive. The client should be advised to call or return to the clinic in 4 days if symptoms are not improving) c) Order a complete blood count (CBC). d) Consult with your collaborating physician. 39. Samantha, age 12, presents with ear pain. When you begin to assess her ear, you tug on her normal-appearing auricle, eliciting severe pain. This leads you to suspect: a) Otitis media (Otitis media, with or without effusion, cannot be diagnosed without examining the tympanic membrane) b) Otitis media with effusion (Otitis media, with or without effusion, cannot be diagnosed without examining the tympanic membrane) c) Otitis externa (When severe pain is elicited by tugging on a normal-appearing auricle, an acute infection of the external ear canal (otitis externa) is suspected) d) Primary otalgia (Otalgia is ear pain) 40. Which manifestation is noted with carbon monoxide poisoning? a) Circumoral pallor of the lips (In light-skinned clients, circumoral pallor of the lips occurs with shock and anemia) b) Cherry-red lips (Cherry-red lips are a manifestation of carbon monoxide poisoning. They also occur with ketoacidosis or acidosis from aspirin poisoning) c) Cyanosis of the lips (Cyanosis of the lips occurs with hypoxemia and chilling) d) Pale pink lips (Some lips are normally pale pink) 41. Kathleen, age 54, has persistent pruritus of the external auditory canal. External otitis and dermatological conditions, such as seborrheic dermatitis and psoriasis, have been ruled out. What can you advise her to do? a) Use a cotton-tipped applicator daily to remove all moisture and potential bacteria. b) Wash daily with soap and water. c) Apply mineral oil to counteract dryness (Pruritus of the external ear canal is a common problem. In most cases, the pruritus is self-induced from overenthusiastic cleaning or excoriation. The protective cerumen covering must be allowed to regenerate and may be helped to do so by application of a small amount of mineral oil, which helps counteract dryness and reject moisture. Often, the use of isopropyl alcohol may relieve ear canal pruritus as well) d) Avoid topical corticosteroids. 42. The most common cause of a white pupil (leukokoria or leukocoria) in a newborn is: a) A congenital cataract (The most common cause of a white pupil (leukokoria or leukocoria) in a newborn is a congenital cataract. The incidence may be as high as 1 in every 500 to 1000 live births, and there is usually a family history. Some infants require no treatment; however, in other cases surgery may be performed during the first few weeks of life) b) Retinoblastoma ( Retinoblastoma, a common intraocular malignancy, is detected within the first few weeks of life and is the second most common cause of a white pupil.) c) Persistent hyperplastic primary vitreous ( Persistent hyperplastic primary vitreous is the third most common cause of a white pupil and is a congenital developmental abnormality.) d) Retinal detachment (Retinal detachment may occur as a result of trauma or disease and only rarely occurs in infancy.) 43. Ellen, a 56-year-old social worker, is seen by the nurse practitioner for complaints of fever; left-sided facial pain; moderate amounts of purulent, malodorous nasal discharge; and pain and headache when bending forward. The symptoms have been occurring for approximately 6 days. On physical assessment, there is marked redness and swelling of the nasal passages and tenderness/pain on palpation over the cheekbones. The nurse practitioner should suspect: a) Dental abscess. b) Acute rhinosinusitis (The client is exhibiting classic characteristics of acute rhinosinusitis) c) Chronic rhinosinusitis. d) Nasal tumor 44. Which of the following statements about macular degeneration is not true? a) Macular degeneration is characterized by gradual loss of peripheral vision (This is how open-angle glaucoma is characterized. Macular degeneration is gradual loss of central vision) b) Macular degeneration is the leading cause of blindness in people younger than 60. c) Tobacco use is a risk factor for macular degeneration. d) There are 2 different types of macular degeneration: wet and dry. 45. What is the most common bacterial pathogen associated with acute otitis media? a) Streptococcus pneumonia (This causes 40% to 50% of cases) b) Haemophilus influenza (This causes 10% to 30% of cases) c) Streptococcus pyogenes (this is an uncommon cause) d) Moraxella (Branhamella) catarrhalis (This is an uncommon cause) 46. You are the nurse practitioner caring for Martha, a 47-year-old accountant. You have made a diagnosis of acute sinusitis based on Martha’s history and the fact that she complains of pain behind her eye. Which sinuses are affected? a) Maxillary (Maxillary sinus pain is felt over the cheek and into the upper teeth) b) Ethmoid (With ethmoid sinus problems, the pain is felt behind the eye and high on the nose) c) Frontal (Frontal sinus pain is felt over the lower forehead_ d) Sphenoid (Sphenoid sinus pain is felt in the occiput, vertex, or middle of the head) 47. Jonathan, age 19, has just been given a diagnosis of mononucleosis. Which of the following statements is true? a) The offending organism is a bacterium, and Jonathan should be treated with antibiotics (Antibiotic therapy is not indicated for Epstein-Barr virus (EBV) b) Convalescence is usually only a few days, and Jonathan should be back to normal in a week (The patient should be instructed to avoid stress and that convalescence may take several weeks) c) Mononucleosis is rarely contagious (The virus that causes mononucleosis is transmitted through saliva, hence the nickname the “kissing disease.” It is contagious and can be transmitted through kissing or sharing utensils. Bed rest is necessary only in severe cases) d) Jonathan should avoid contact sports and heavy lifting (When teaching clients about mononucleosis, or Epstein-Barr virus (EBV), tell them to avoid contact sports and heavy lifting because of splenomegaly and a threat of rupture) 48. A 65-year-old man presents complaining of a left-sided, deep, throbbing headache and mild fatigue. On examination, the client has a tender, tortuous temporal artery. You suspect giant cell arteritis (GCA), or temporal arteritis. What is the least invasive procedure to help with diagnosis? a) Magnetic resonance imaging (MRI) of the head (Magnetic resonance angiography (MRA), not MRI, can be done to evaluate the blood vessels in the brain, but the blood test is less invasive) b) Erythrocyte sedimentation rate (ESR) (An elevated ESR—anywhere from 30 to 100 mm/h—may be seen in giant cell arteritis (temporal arteritis); however, the ESR may also be normal. The temporal artery supplies the optic nerve; if temporal arteritis is suspected due to the age of the client (50 and older) and the location and character of the pain, it is essential that a referral to a surgeon be made for immediate biopsy of the artery before damage to the optic nerve occurs. A temporal artery biopsy (TAB), an invasive procedure, is the criterion standard for diagnosing temporal arteritis) c) Electroencephalogram (EEG) (EEG is not used in the diagnosis of GCA) d) Otoscopy (Otoscopy is not used in the diagnosis of GCA.) 49. When you are assessing the internal structure of the eye of your 59-year-old patient, the absence of a red reflex may indicate (When assessing the internal structure of the eye, absence of a red reflex may indicate the total opacity of the pupil because of a cataract or hemorrhage into the vitreous humor. It may also be a result of improper positioning of the ophthalmoscope) a) A cataract or hemorrhage into the vitreous humor (When assessing the internal structure of the eye, absence of a red reflex may indicate the total opacity of the pupil because of a cataract or hemorrhage into the vitreous humor. It may also be a result of improper positioning of the ophthalmoscope) b) Acute iritis (Acute iritis is noted by constriction of the pupil accompanied by pain and circumcorneal redness (ciliary flush) c) Nothing; this is a normal finding in older adults. d) Diabetes or long-standing hypertension (If areas of hemorrhage, exudate, and white patches are present when the internal structure of the eye is assessed, they are usually a result of diabetes or long-standing hypertension) 50. Mia, a 27-year-old school teacher, has a 2-day history of severe left ear pain that began after 1 week of upper respiratory infection (URI) symptoms. On physical examination, you find that she has acute otitis media (AOM). She has a severe allergy to penicillin. The most appropriate antimicrobial option for this patient is: a) Ciprofloxacin (Cipro) (Ciprofloxacin, a fluoroquinolone antibiotic, is not recommended for the treatment of acute otitis media) b) Azithromycin (Zithromax) (Azithromycin is not a perfect option for treating otitis media; however, it is preferred for patients with severe penicillin allergy) c) Amoxicillin (Amoxil) ( Amoxicillin is a penicillin-based antibiotic and should not be given to a patient with a penicillin allergy) d) Cephalexin (Keflex) (Cephalexin is a penicillin-based antibiotic and should not be given to a patient with a penicillin allergy) 51. Mr. Johnson, age 69, has had Meniere disease for several years. He has some hearing loss but now has persistent vertigo. What treatment might be instituted to relieve the vertigo? a) A labyrinthectomy (A labyrinthectomy is the surgery of last resort for a client with Meniere disease because the labyrinth is completely removed and cochlear function destroyed. This procedure is used only when hearing loss is nearly complete) b) Pharmacological therapy (Oral diuretics and a low-sodium diet may aid in maintaining a lower labyrinth pressure, which may help slightly) c) A vestibular neurectomy (For a client who has had Meniere disease for several years, with some hearing loss and now persistent vertigo, treatment by vestibular neurectomy might relieve the vertigo. In vestibular neurectomy, the portion of cranial nerve VIII that controls balance and the sensation of vertigo is severed. Vertigo is usually relieved in 90% of cases) d) Wearing an earplug in the ear that has the most hearing loss (Wearing an earplug will not help and may aggravate the condition) 52. Mr. Clark, age 78, is being treated with timolol maleate (Timoptic) drops for his chronic open-angle glaucoma. While performing a new client history and physical, you note that he is taking other medications. Which medication would you be most concerned about? a) Aspirin therapy as prophylaxis for heart attack. b) Ranitidine (Zantac) for gastroesophageal reflux disease. c) Alprazolam (Xanax), an anxiolytic. d) Atenolol (Tenormin), a beta blocker for high blood pressure (If a client is taking timolol maleate (Timoptic) drops for chronic open-angle glaucoma, you should be most concerned if the client is also taking atenolol (Tenormin), a beta blocker, for high blood pressure. Because timolol maleate drops are beta-adrenergic blockers, additional beta blockers can cause worsening of congestive heart failure or reactive airway disease, as well as acute delirium) 53. Mario, a 17-year-old high school student, came to the office for evaluation. He is complaining of persistent sore throat, fever, and malaise not relieved by the penicillin therapy prescribed recently at the urgent care center. As the nurse practitioner, what would you order next? a) A throat culture (A throat culture is performed to help diagnose group A beta-hemolytic streptococcal infection) b) A Monospot test (If a client has a persistent sore throat, fever, and malaise not relieved by penicillin therapy, a Monospot test should be performed to rule out mononucleosis (Epstein-Barr virus) c) A rapid antigen test (A rapid antigen test is performed to help diagnose group A beta-hemolytic streptococcal infection) d) A Thayer-Martin plate test (A Thayer-Martin plate test is performed to diagnose a gonococcal infection) 54. Regular ocular pressure testing is indicated for older adults taking: a) High-dose inhaled glucocorticoids (Although regular ocular pressure testing is indicated on a routine basis for all older adults, it is especially important for clients taking an extended regimen of high-dose inhaled glucocorticoids because prolonged continuous use increases the risk of ocular hypertension or open-angle glaucoma) b) Nonsteroidal anti-inflammatory drugs (NSAIDs). c) Angiotensin-converting enzyme (ACE) inhibitors. d) Insulin (Older adults taking insulin need to have regular eye examinations because they are diabetic and have a risk of diabetic retinopathy, not because they are taking insulin) 55. A 25-year-old male presents with “bleeding in my eye” for 1 day. He awoke this morning with a dark area of redness in his eye. He has no visual loss or changes. He denies constitutional symptoms, pruritus, drainage, or recent trauma. The redness presents on physical exam as a dark red area in the patient’s sclera of the right eye only and takes up less than 50% of the eye. The patient’s remaining sclera is clear and white. He also notes he was drinking alcohol last night and vomited afterward. What is the best treatment? a) Topical steroids and close follow-up with an ophthalmologist (his would be the treatment for an infectious process; however, topical steroids need to be used in the eye with care) b) Sending the patient to the emergency department for immediate ophthalmology consult (This would be the treatment for a globe rupture or acute angle-closure glaucoma) c) Reassurance that this lesion will resolve without any treatment in 2 to 4 weeks (This is the classic presentation of a subconjunctival hemorrhage. It will resolve without treatment in 2 to 4 weeks. Vomiting probably caused his hemorrhage) d) Cold compresses and frequent handwashing (This is the treatment for viral conjunctivitis) 56. What is the most common cause of epistaxis? a) Digital trauma (Picking the nose is the most common cause of nosebleeds) b) Warfarin. c) Vitamin C deficiency (This can cause nasal tissue friability and epistaxis) d) Hemophilia A (This would increase the risk of bleeding from the nose, but hemophilia itself is not a cause of epistaxis) 57. Aaron, age 4, is brought in to the clinic by his father. His tympanic membrane is perforated from otitis media. His father asks about repair of the eardrum. How do you respond? a) “The eardrum, in most cases, heals within several weeks.” (Most perforated tympanic membranes seen with acute otitis media heal within several weeks) b) “We need to schedule Aaron for a surgical repair.” (If the eardrum has not healed within 3 to 6 months, a surgical repair can be done, but not until age 7 to 9 years) c) “He must absolutely stay out of the water for 3 to 6 months.” (Aaron can swim on the surface with the use of an ear mold but must not dive, jump, or swim underwater) d) “If the eardrum is not healed in several months, it can be surgically repaired.” (If the eardrum has not healed within 3 to 6 months, a surgical repair can be done, but not until age 7 to 9 years) 58. Martin, age 24, presents to the office with an erythematous ear canal and pain on manipulation of the auricle. He is on vacation and has been swimming daily at the resort. What is your diagnosis? a) Acute otitis media (acute otitis media is painful, is usually a result of cotton swab use or physical trauma, and usually follows an upper respiratory infection) b) Chronic otitis media (Chronic otitis media is usually not painful, although the ear may be painful during an exacerbation) c) External otitis (With external otitis, there is pain, an erythematous ear canal, and usually a history of recent swimming) d) Temporomandibular joint (TMJ) syndrome (Ear pain may also be the result of TMJ dysfunction. It is usually made worse by chewing or grinding the teeth) 59. A 44-year-old banker comes to your office for evaluation of a pulsating headache over the left temporal region, and he rates the pain as an 8 on a scale of 1 to 10. The pain has been constant for the past several hours and is accompanied by nausea and sensitivity to light. He has had frequent, though less severe, headaches for many years, and they are usually relieved by over-the-counter medicines. He is unclear as to a precipitating event but notes that he has had visual disturbances before each headache and he has been under a lot of stress in his job. Based on this description, what is the most likely diagnosis of this type of headache? a) Tension (Tension headaches are not associated with photophobia and are usually bilateral and associated with limited neck range of motion (ROM). Tension headaches are not preceded by an aura) b) Migraine (Migraines are classically preceded by an aura and accompanied by nausea, vomiting (sometimes), and photophobia. They are usually unilateral) c) Cluster (Cluster headaches are unilateral, frequently occur at night, and bear some resemblance to migraines; however, cluster headaches are accompanied by tearing, nasal stuffiness, and sweating on the same side as the headache, and they come in clusters.) d) Temporal arteritis (The client is not in the age range (older than 50) for temporal arteritis) 60. Max, age 35, states that he thinks he has an ear infection because he just flew back from a business trip and feels unusual pressure in his ear. You diagnose barotrauma. What is your next action? a) Prescribe nasal steroids and oral decongestants (Barotrauma of the auditory canal, causing a sensation of abnormal middle ear pressure, may be relieved by the use of nasal steroids and oral decongestants) b) Prescribe antibiotic ear drops (With barotrauma, there is no infection, just swelling of the airways, which causes the sensation of abnormal pressure; therefore, antibiotics are not indicated) c) Prescribe systemic antibiotics (With barotrauma, there is no infection, just swelling of the airways, which causes the sensation of abnormal pressure; therefore, antibiotics are not indicated) d) Refer Max to an ear, nose, and throat specialist (This condition is certainly within the practitioner’s scope of practice, and a referral is not indicated) 61. Your client, a 72-year-old smoker of 50 years, is at the office today for a routine physical. During your inspection of the oral mucosa, you discover a white lesion on the lateral surface of the tongue that you suspect to be cancerous. You document your finding as: a) A superficial, translucent, subepithelial, vesicle-like lesion in the oral mucosa (A superficial mucocele presents as a small, clear vesicle on noninflamed mucosa) b) A white, painless, firm, ulcerated lesion with indurated borders (Approximately 90% of oral cancers are squamous cell carcinoma (SCC), which is seen typically on the lip or lateral part of the tongue, usually as a lesion that is white, red, or mixed white and red. SCCs are characterized by painless, firm lesions with indurated borders) c) An abnormal white coating of the dorsal surface of the tongue (The term “hairy tongue” is used to describe an abnormal coating on the top (dorsal) surface of the tongue. It is a relatively common, temporary, and harmless condition that occurs in as much as 13% of the population. Hairy tongue can occur at any age but is more frequent in older age) d) A round, smooth, firm lump on the lateral side of the tongue (A round, smooth, firm lump attached at its base or by a stalk to part of the oral cavity tissue is called a fibroma. It may occur anywhere in the oral cavity but most often develops on the inner lining of the cheeks and lips. A fibroma is a common benign oral cavity tumor) 62. At the clinic, you are assessing Kyle, a 4-month-old baby, for the first time and notice that both eyes are turning inward. What is this called? a) Pseudostrabismus (Pseudostrabismus has the appearance of strabismus because of the presence of epicanthic folds but is normal in young children) b) Strabismus (Strabismus, also called tropia, is the constant malalignment of the eye axes. It is likely to cause amblyopia) c) Esotropia (Esotropia is the inward turning of the eyes) d) Exotropia (Exotropia is the outward turning of the eyes) 63. You diagnose acute epiglottitis in Sally, age 5, and immediately send her to the local emergency room. Which of the following symptoms would indicate that an airway obstruction is imminent? a) Reddened face. b) Screaming. c) Grabbing her throat. d) Stridor (In a pediatric client with acute epiglottitis, a number of symptoms can indicate that airway obstruction is imminent: stridor, restlessness, nasal flaring, as well as the use of accessory muscles of respiration) 64. Mrs. Johnson, a 54-year-old accountant, presents to the office with a painful red eye without discharge. You should suspect a) Bacterial conjunctivitis (With bacterial conjunctivitis, there is purulent, thick discharge) b) Viral conjunctivitis (With viral conjunctivitis, there is usually a watery discharge) c) Allergic conjunctivitis (With allergic conjunctivitis, there is a stringy, mucoid discharge) d) Iritis (In a client with iritis, there is rarely a discharge) 65. Cataracts are a common occurrence in patients over 60 years of age. You counsel your patient that the best cure for cataracts is: a) Medications. b) Dietary supplements. c) Corrective lens surgery (To date, no pharmaceutical treatment proven to delay, prevent, or reverse the development of cataracts exists. The definitive management for a cataract is a surgical approach, one that removes the defective lens and replaces it with an artificial one) d) Optical devices. 66. A 62-year-old woman presents to your clinic with a sudden right-sided headache that is worse in her right eye. She states that her vision seems blurred, and her right pupil is dilated and slow to react. The right conjunctiva is markedly injected, and the eyeball is firm. You screen her vision and find that she is 20/30 OS and 20/30 OD. She most likely has: a) Open-angle glaucoma (With open-angle glaucoma, the onset is more insidious) b) Angle-closure glaucoma (In angle-closure glaucoma, the patient presents with a sudden onset of symptoms as described in this case. This client has a visual deficit and pain as well as fullness of the affected eye. This is a medical emergency, and she should be referred immediately because, without intervention, blindness can occur within days) c) Herpetic conjunctivitis (Herpetic conjunctivitis is generally associated with a herpetic rash, and the pain is dull in character) d) Diabetic retinopathy (Diabetic retinopathy is a complication of diabetes that affects both eyes. It is caused by damage to the blood vessels of the light-sensitive tissue at the back of the eye (ie, the retina) 67. How would you describe the cervical lymphadenopathy associated with asymptomatic human immunodeficiency virus (HIV) infection? a) Movable, discrete, soft, and nontender lymph nodes (In a healthy person, cervical nodes are often palpable and are movable, discrete, soft, and nontender) b) Enlarged, warm, tender, and firm but freely movable lymph nodes (In a client with an acute infection, the cervical nodes are bilaterally enlarged, warm, tender, and firm but freely movable) c) Hard, unilateral, nontender, and fixed lymph nodes (Cancerous nodes are hard, unilateral, nontender, and fixed) d) Nontender, mobile, and firm but not hard lymph nodes (The cervical lymphadenopathy associated with asymptomatic HIV infection may be described as lymph nodes that are nontender, mobile, and firm but not hard.) 68. Treatment for achalasia may include: a) Balloon dilation of the lower esophageal sphincter (Achalasia is an absence of peristalsis of the esophagus and a high gastroesophageal sphincter pressure. After initial noninvasive treatments, clients may require a balloon dilation of the lower esophageal sphincter) b) Beta blockers. c) A fundoplication. d) An esophagogastrectomy. 69. Zena just had a hemorrhoidectomy. You know she has not understood your teaching when she tells you she will: a) Take a sitz bath after each bowel movement for 1 to 2 weeks after surgery (Clients who have just had a hemorrhoidectomy should take a sitz bath after each bowel movement for 1 to 2 weeks after surgery to promote relaxation and aid with discomfort) b) Drink at least 2000 mL of fluids per day (Clients who have just had a hemorrhoidectomy should drink at least 2000 mL of fluids per day) c) Decrease her dietary fiber for 1 month (For clients who have just had a hemorrhoidectomy, teaching would include advising them to maintain an adequate intake of dietary fiber to maintain stool bulk) d) Take stool softeners as prescribed (Clients who have just had a hemorrhoidectomy should take stool softeners as prescribed (for short-term relief only) and exercise regularly to maintain stool bulk, softness, and regularity) 70. Stacy, a nursing student, is to begin her series of hepatitis B vaccinations. You test her for a serological marker, and the results show hepatitis B surface antibodies (HBsAb). You tell Stacy that she: a) Needs to begin the hepatitis B series as soon as possible. b) Needs to be tested again because one reading is not indicative of immunity. c) Is permanently immune to hepatitis B (The marker for permanent immunity, hepatitis B surface antibodies in the serum, will be present 4 to 10 months after exposure and immunity to hepatitis B) d) Has an acute hepatitis B infection (Hepatitis B surface antigen is the earliest indicator of the presence of an acute infection and is present 4 to 12 weeks after exposure. This marker is also indicative of a chronic infection) 71. Margie, age 52, has an extremely stressful job and was just given a diagnosis of gastric ulcer. She tells you she is sure it is going to be malignant. How do you respond? a) “Don’t worry. Gastric ulcers are not cancerous.” b) “About 95% of gastric ulcers are benign.” (About 95% of gastric ulcers are benign even though some of these seem to look malignant on x-ray) c) “You have about a 50% chance of having gastric cancer from your ulcer.” d) “Even if it is cancer, surgery is 100% successful.” 72. Susan, age 59, has no specific complaints when she comes in for her annual examination. She does, however, have type 2 diabetes mellitus (DM), slight hypertension, dyslipidemia, and central obesity. How would you diagnose her? a) As a healthy adult with several problems. b) As having a glycemic event (If Susan’s DM were out of control, she would have a “glycemic event.) c) As having metabolic syndrome (Susan has a constellation of symptoms known as metabolic syndrome. The World Health Organization (WHO), National Cholesterol Education Program Adult Treatment Panel III (NCEP ATP III), and International Diabetes Federation (IDF) have slightly different criteria for this diagnosis. They all, however, include hypertension, dyslipidemia, and central obesity.) d) As having multiple organ dysfunction (Eventually, Susan may end up with multiple organ dysfunction. You might consider that she is headed toward that result) 73. Tom has just been diagnosed with celiac disease. Which of the following might you tell him? a) There is a new pharmaceutical cure for celiac disease. b) A strict gluten-free diet is the only treatment for celiac disease (A strict gluten-free diet is the only treatment for celiac disease) c) Your children will not be at a higher risk for developing this disease (Patients with first- or second-degree relatives affected by celiac disease are at higher risk for developing it) d) The presence of celiac disease is decreasing dramatically in the United States (The prevalence of celiac disease in the United States has increased dramatically. Approximately 1% of today’s US residents are affected by it) 74. Matt, age 26, recently returned from a camping trip and has gastroenteritis. He says that he has been eating only canned food. Which of the following pathogens do you suspect? a) Campylobacter jejuni (C jejuni is found primarily in eggs and poultry but may be found in domestic animals) b) Clostridium botulinum (C botulinum is an anaerobic, gram-positive bacillus that produces toxins. It is widely distributed in the soil and vegetation. Improperly processed home-canned low-acid vegetables and contaminated meats are the usual cause of food-borne botulism) c) Clostridium perfringens (C perfringens is found in soil, feces, air, and water. Outbreaks are caused most often by contaminated meat) d) Staphylococcus (Staphylococcus is a common cause of food poisoning. It is caused by the ingestion of an enterotoxin found in improperly handled or stored foods) 75. Ruby has a colostomy and complains that her stools are too loose. What food(s) do you suggest to help thicken the stools? a) Cheese (Cheese, bread, pasta, rice, pretzels, and yogurt all help to thicken stools) b) Leafy green vegetables (This may loosen) c) Raw fruits and vegetables (This may loosen) d) Dried beans (This may loosen) 76. Anson tells you he thinks his antacids are causing his diarrhea. You respond: a) “Antacids contain fructose, which may not be totally absorbed, resulting in fluid being drawn into the bowel.” (Fructose is not usually contained in antacids. Fructose is present in apple juice, pear juice, grapes, honey, dates, nuts, figs, and fruit-flavored soft drinks) b) “Antacids contain sorbitol or mannitol, which are sugars that aren’t absorbed and can cause fluid to be drawn into the bowel.” (Sorbitol and mannitol are not usually contained in antacids. Sorbitol or mannitol is present in apple juice, pear juice, sugarless gums, and mints) c) “Antacids contain caffeine, which decreases bowel transit time.” (Caffeine is not usually contained in antacids. Caffeine is present in coffee, tea, cola drinks, and over-the-counter analgesics) d) “Antacids may contain magnesium, which decreases bowel transit time and may contain poorly absorbed salts that draw fluid into the bowel.” (Antacids may contain magnesium, which decreases bowel transit time and may contain poorly absorbed salts that result in an osmotic draw of fluid into the bowel resulting in diarrhea) 77. Cydney has been given a diagnosis of ascariasis. Which symptoms would you expect to see? a) Low-grade fever, productive cough with blood-tinged sputum, wheezing, and dyspnea (Ascariasis is the most common intestinal helminth (parasitic worm). It causes pulmonary manifestations, such as low-grade fever, productive cough with blood-tinged sputum, wheezing, and dyspnea, because the larvae are transmitted to the lungs from the vascular system. The larvae burrow through alveolar walls, migrating up the bronchial tree to the pharynx, and then down the esophagus, back to the intestine) b) Nocturnal perianal and perineal pruritus (Nocturnal perianal and perineal pruritus occur with enterobiasis (pinworm infection) c) Diarrhea, cramps, and malaise (Diarrhea, cramps, and malaise are common with trichinosis) d) Ascites and facial and extremity edema (Ascites and facial and extremity edema are common with trichuriasis) 78. Rose, a client with gastroesophageal reflux disease (GERD), has many other concurrent conditions. In teaching Rose about medications to avoid, what do you recommend she refrain from using? a) Antibiotics. b) Nonsteroidal anti-inflammatory drugs (NSAIDs) (Clients with GERD should avoid taking NSAIDs because they tend to aggravate the already irritated gastric mucosa) c) Oral contraceptives. d) Antifungals. 79. Lucy, age 49, has pain in both the left and right lower quadrants. What might you suspect? a) A gastric ulcer (Pain in the left upper quadrant may signify a gastric ulcer, gastritis, pancreatitis, splenic abscess, or pleurisy) b) Gastritis (Pain in the left upper quadrant may signify a gastric ulcer, gastritis, pancreatitis, splenic abscess, or pleurisy) c) Pelvic inflammatory disease (The pain associated with pelvic inflammatory disease can be palpated in both the right and left lower quadrants) d) Pancreatitis (Pain in the left upper quadrant may signify a gastric ulcer, gastritis, pancreatitis, splenic abscess, or pleurisy) 80. Shelby has recently been diagnosed with pancreatitis. Of the following objective findings that can result from the pancreatic inflammatory process, which is known as Grey Turner sign? a) Left-sided pleural effusion (Left-sided pleural effusion can result from the pancreatic inflammatory process) b) Bluish discoloration over the flanks (Grey Turner sign is a bluish discoloration over the flanks) c) Bluish discoloration around the umbilicus (Cullen sign is a bluish discoloration around the umbilicus) d) Jaundice (Jaundice caused by impingement on the common bile duct can result from the pancreatic inflammatory process) 81. A mother brings in her 4-year-old child, who she states has acute abdominal pain and a rash. Which of the following do you initially rule out? a) Rocky Mountain spotted fever. (Rocky Mountain spotted fever causes acute abdominal pain and a rash) b) Measles (Measles causes acute abdominal pain and a rash) c) Appendicitis (There are many systemic causes of acute abdominal pain that also result in a rash. Appendicitis does not present with a rash) d) A food allergy (A food allergy may also present as abdominal pain along with dermatitis) 82. Harvey just came back from Mexico. Which pathogen do you suspect is responsible for his diarrhea? a) Enterococci (Enterococci may result in diarrhea, but because Harvey just came back from Mexico, his traveler’s diarrhea is most likely caused by E coli) b) Escherichia coli (E coli is the pathogen most often responsible for traveler’s diarrhea (infectious diarrhea). Other causes may include viruses, other bacteria, protozoa, or parasites.) c) Klebsiella (Klebsiella may result in diarrhea, but because Harvey just came back from Mexico, his traveler’s diarrhea is most likely caused by E coli) d) Staphylococci (Staphylococci may result in diarrhea, but because Harvey just came back from Mexico, his traveler’s diarrhea is most likely caused by E coli) 83. Marian, age 52, is obese. She complains of a rapid onset of severe right upper quadrant abdominal cramping pain, nausea, and vomiting. Your differential diagnosis might be: a) Appendicitis (Pain associated with appendicitis would typically be near the navel, progressing to the right lower quadrant) b) Crohn’s disease (In Crohn’s disease, the pain and cramping in the abdomen are more diffuse and not usually accompanied by nausea and vomiting) c) Cholecystitis (A rapid onset of severe right upper quadrant (RUQ) abdominal cramping pain with nausea and vomiting is a classic presentation of acute cholecystitis; 90% to 95% of clients with acute cholecystitis also have gallstones. Other symptoms include low-grade fever, epigastric tenderness, guarding, and pain on inspiration during palpation of the RUQ (Murphy sign). The 7 F’s of cholecystitis are fair, fat, 40, female, fertile, fat intolerant, and flatulent.) d) Irritable bowel syndrome (In irritable bowel syndrome (IBS), the pain and cramping in the abdomen are more diffuse and not usually accompanied by nausea and vomiting. The pain with IBS originates over some area of the colon, with the left lower quadrant being most often affected) 84. Which of the following is not true regarding hepatitis C? a) The greatest rate of infection in the general population is seen in people born between 1945 and 1965. b) Many hepatitis C infections are asymptomatic. c) Hepatitis C is seen more frequently in men than women. d) If hepatitis is asymptomatic it doesn’t cause cirrhosis or liver cancer (This is untrue; the reason many people end up with cirrhosis or liver cancer is because the disease can often be asymptomatic) 85. A 75-year-old male presents for a routine physical. He is obese and has no abdominal pain or recent injuries or problems. He has no complaints. He lies supine for his abdominal exam. He is nontender to palpation and has a normal exam. When he sits up you see a large mass protrude from his abdomen. It is central to his abdomen and inferior to his rib cage. It disappears when he is sitting up fully. What is the patient’s diagnosis? a) Ventral (epigastric) hernia (This is the hernia described in the question; most of these hernias are asymptomatic) b) Inguinal hernia (This is in the groin and most commonly palpated via a testicular exam) c) Femoral hernia (This is in the groin and most common in women) d) Umbilical hernia (This is present at the umbilicus, not where it is described in the question) 86. What is the best diagnostic test to confirm the diagnosis of celiac disease? a) Anti-tTG IgA (This is the most sensitive and specific test for diagnosing celiac disease) b) Anti-dsDNA (This test is positive in a diagnosis of lupus) c) Colonoscopy (This would be the best diagnostic tool to use for irritable bowel disease) d) Anti-CCP protein (This is a test to diagnose rheumatoid arthritis) 87. A 50-year-old female presents to the urgent care clinic complaining of left lower quadrant pain. She has associated nausea and vomiting, and her vital signs are as follows: temperature 102.5°F, pulse 110, blood pressure 150/90, pulse oximetry 99% on room air. What is the best test to evaluate this patient? a) Sigmoidoscopy (This patient has symptoms of diverticulitis; a sigmoidoscopy would be painful but would help rule out cancer) b) Abdominal series (This could be done but is unlikely to diagnose diverticulitis) c) Computed tomography (CT) scan with oral contrast (This is the best diagnostic choice. While diverticulitis is likely the cause of the patient’s symptoms, a CT of the abdomen would show if the patient has any gynecologic etiology (such as ovarian cyst or tumor) of this pain) d) Abdominal ultrasound (This would show the patient’s ovaries and uterus but would not show the colon) 88. Which oral medication might be used to treat a client with chronic cholelithiasis who is a poor candidate for surgery? a) Ursodiol (Actigall) (Ursodiol (Actigall) is an oral bile acid that dissolves gallstones. For dissolution, 8 to 10 mg/kg per day is given in 2 to 3 divided doses; for prevention, 300 mg twice per day is given. The safety of its use after 24 months has not been established) b) Ibuprofen (Advil) (Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen (Advil), may be very irritating to the gastrointestinal mucosa) c) Prednisone (Deltasone) (Steroids, such as prednisone (Deltasone), may mask an infection as well as irritate the gastric mucosa) d) Surgery is the only answer (Surgery is not the only solution for chronic cholelithiasis) 89. You auscultate Julie’s abdomen and hear a peritoneal friction rub. Which condition do you rule out? a) Peritonitis (A peritoneal friction rub, which sounds like a rough, grating sound, occurs over organs with a large surface area in contact with the peritoneum when there is peritoneal inflammation (peritonitis) b) A liver or spleen abscess (When a peritoneal friction rub is heard over the lower right rib cage, it may be caused by an abscess or tumor of the liver. When heard over the lower left rib cage in the left anterior axillary line, it may indicate infection of the spleen or an abscess or tumor of the spleen) c) A liver or spleen metastatic tumor (When a peritoneal friction rub is heard over the lower right rib cage, it may be caused by an abscess or tumor of the liver. When heard over the lower left rib cage in the left anterior axillary line, it may indicate infection of the spleen or an abscess or tumor of the spleen) d) Irritable bowel syndrome (Irritable bowel syndrome does not produce a friction rub) 90. Nausea is difficult to discern in a young child. What question might you ask to determine if a child has nausea? a) “Are you sick to your tummy?” (Young children sometimes equate being “sick to my tummy” with vomiting and thus might answer no when questioned about nausea) b) “Are you hungry?” (To elicit information concerning nausea in a young child, ask the child about hunger because a young child cannot usually differentiate between hunger and mild nausea) c) “Are you eating the way you normally eat?” (A young child might not understand this question) d) “Are you nauseous?” (A young child might not understand this question) 91. You are counseling Lillian, who is lactose intolerant, about foods to avoid. You know she misunderstands the teaching when she tells you she can have: a) Yogurt (Fermented dairy products, such as aged or hard cheeses and cultured yogurt, are easier to digest and contain less lactose than other dairy products) b) Foods containing whey (Advise clients who are lactose intolerant to avoid foods containing whey. Whey is a lactose-rich ingredient found in some foods, so clients who are lactose intolerant need to read labels on all foods. To control symptoms, dietary lactose should be reduced or restricted by using lactose-reduced and lactose-free dairy products or by eating lactose-rich foods in small amounts or in combination with low-lactose or lactose-free foods) c) Prehydrolyzed milk (Most stores carry milk that has been pretreated with lactase, making it more than 70% lactose-free. This reduced-lactose milk is also known as prehydrolyzed milk) d) Oranges (Lillian can eat oranges) 92. Martina, age 34, has AIDS and currently suffers from diarrhea. You suspect she has which protozoal infection of the bowel? a) Giardiasis (Giardiasis is also a protozoal infection affecting the intestine, but because Martina has AIDS, the answer must be cryptosporidiosis) b) Amebiasis (Amebiasis is also a protozoal infection affecting the intestine, but because Martina has AIDS, the answer must be cryptosporidiosis) c) Cryptosporidiosis (Cryptosporidiosis, a protozoal infection of the bowel, is common in immunocompromised clients. It causes villous atrophy and mild inflammatory changes and may secrete an enterotoxin) d) Escherichia coli (E coli is a gram-negative bacterium) 93. Tina has a chronic hepatitis C infection. She asks you how to prevent its transmission. You respond: a) “Do not donate blood until one year after diagnosis.” (Clients with hepatitis C should not donate blood.) b) “Abstain from sex altogether.” (here is no need to abstain from sex altogether) c) “There is no possibility of transmission through razors or toothbrushes.” (There is a possibility of transmission through razors, toothbrushes, and tattoo instruments) d) “Abstain from sex during your period.” (Because the hepatitis C virus is transmitted in blood, including menstrual blood, clients should abstain from sex during menstruation. You might also test Tina to see which genotype her hepatitis C is to see if she is a candidate for Harvoni or Epclusa) 94. Sandy, age 52, presents with jaundice, dark urine, and light-colored stools, stating that she is slightly improved over last week’s symptoms. Which stage of viral hepatitis do you suspect? a) Incubation (During the incubation period of viral hepatitis, there are no subjective or objective complaints) b) Prodromal (During the prodromal stage, there is anorexia, nausea, vomiting, malaise, upper respiratory infection (nasal discharge and pharyngitis), myalgia, arthralgia, easy fatigability, fever (hepatitis A virus), and abdominal pain) c) Icteric (In the icteric stage of viral hepatitis, there is jaundice, dark urine, and light-colored stools. There are continued prodromal complaints, with gradual improvement) d) Convalescent (During the convalescent stage, there is an increased sense of well-being, the appetite returns, and the jaundice, abdominal pain, and fatigability abate) 95. You suspect appendicitis in Andrew, who is 18. With his right hip and knee flexed, you slowly rotate his right leg internally to stretch a muscle. He states that it is painful over his right lower quadrant. Which sign did you elicit? a) Rovsing sign (Rovsing sign is pain elicited with deep palpation over the left lower quadrant (LLQ), with sudden resultant pain in the right lower quadrant (RLQ). This causes tenderness over the RLQ and is considered a positive finding) b) Psoas sign (Psoas sign is pain elicited when the patient is instructed to try to lift the right leg against gentle pressure applied by the examiner or when the patient is placed in the left lateral decubitus position, extending the right leg at the hip. An increase in pain is considered positive and is an indication of the inflamed appendix irritating the psoas muscle) c) Obturator sign (Obturator sign is elicited when, with the patient’s right hip and knee flexed, the examiner slowly rotates the right leg internally, which stretches the obturator muscle. Pain over the right lower quadrant (RLQ) is considered a positive sign) d) McBurney sign (McBurney sign is pain elicited when pressure is applied to McBurney point, which is located halfway between the umbilicus and the anterior spine of the ilium) 96. In a 2-month-old infant with vomiting and diarrhea, the most effective way of determining a fluid deficit is to check for: a) Decreased peripheral perfusion (In a 2-month-old infant with vomiting and diarrhea, the most effective way of determining a fluid deficit is to check for decreased peripheral perfusion, dry oral mucous membranes, and sunken fontanels. The body compensates for loss of fluid by shifting the interstitial fluid into the intravascular space, thereby maintaining perfusion of vital organs. If the fluid loss continues, circulating volume is diminished and vasoconstriction occurs in the peripheral vessels, resulting in decreased perfusion) b) Hyperventilation (Hyperventilation may be related to a multitude of factors) c) Irritability (Irritability may be related to a multitude of factors) d) Hyperthermia (Hyperthermia may be related to a multitude of factors) 97. Olive has an acute exacerbation of Crohn’s disease. Which laboratory test value(s) would you expect to be decreased? a) Sedimentation rate (The sedimentation rate is increased) b) Liver enzyme levels (The liver enzyme levels are increased) c) Vitamin A, B complex, and C levels (Folic acid and serum levels of most vitamins, including A, B complex, C, and the fat-soluble vitamins, are decreased in Crohn’s disease as a result of malabsorption) d) Bilirubin level (The bilirubin levels are increased.) 98. Dottie brings in her infant, who has gastroesophageal reflux. What do you tell her about positioning her infant? a) “Always position infants on their back to prevent sudden infant death syndrome.” (Babies with gastroesophageal reflux should, from birth, be placed to sleep on their back on a firm, flat mattress that is not elevated. Elevating the sleeping surface for back-sleeping babies does not reduce reflux and is not recommended. In addition, these babies should be fed a formula thickened with rice cereal and held in an upright position for 1 hour after feeding, as gravity helps prevent reflux.) b) “Rotate your infant between lying on the back and on the stomach.” (In babies with gastroesophageal reflux, the risk of sudden death when the baby is in the tummy- or side-sleeping position outweighs any benefits of tummy or left side positioning of babies.) c) “Your infant should be placed on the left side.” (In babies with gastroesophageal reflux, the risk of sudden death when the baby is in the tummy- or side-sleeping position outweighs any benefits of tummy or left side positioning of babies) d) “Place your infant in whatever position she remains quiet.” (Babies with gastroesophageal reflux should, from birth, be placed to sleep on their back on a firm, flat mattress that is not elevated) 99. A 45-year-old homeless man presents to your urgent care clinic for evaluation. His chief complaint is diarrhea. The patient states he started to have diarrhea 2-3 days ago, and it is getting progressively worse. He also notes nausea without vomiting, dry mouth, and double vision. On exam you notice his pupillary reflex is absent. The patient states he lives on the street and eats mostly canned goods that he scavenges from a grocery store dumpster. What is the likely cause of the patient’s symptoms? a) Botulism (This patient has a gastrointestinal illness associated with descending neurological symptoms after eating canned food; this is the presentation of botulism) b) Salmonella (This is a bacterial illness not normally associated with neurological changes) c) Lyme disease (The patient has no skin eruptions or tick bites) d) Vitamin C deficiency (Vitamin C deficiency, or scurvy, is normally associated with bleeding gums and easy bruising) 100. What is the most common bacterial cause of traveler’s diarrhea? a) Escherichia coli (E coli is the most common pathogen responsible for traveler’s diarrhea) b) Campylobacter jejuni. c) Salmonella. d) Shigella. 101. A 54-year-old female presents to your primary care office for routine reevaluation for gastroesophageal reflux disease (GERD). She has been treated with diet modifications and 6 weeks of omeprazole without improvement of her symptoms. What is the next step in management of this patient’s GERD? a) Order an endoscopy (This is the next step in treatment in order to evaluate the etiology of the patient’s GERD and consider biopsy if necessary) b) Order a Helicobacter pylori blood test (The next step in care is an endoscopy. If warranted, a biopsy can be done and sent for H pylori at that time) c) Try adding ranitidine to the patient’s regimen (H2 antagonists are considered a less aggressive treatment for GERD and would likely not help the patient’s symptoms) d) Try adding bismuth to the patient’s regimen (Bismuth can be added to help treat Helicobacter pylori, but that diagnosis has not yet been made) 102. A 25-year-old male presents complaining of hematochezia. The patient states he has noticed this for 2 days. He states there is a streak of bright blood along his stool every time he has a bowel movement. The patient has no pain with his bowel movements. He admits to eating a poor diet. The patient has no abdominal pain, nausea, or vomiting. On physical exam the patient has a positive fecal occult blood test but has no noticeable rectal bleeding or lesions. What is the likely diagnosis? a) Internal hemorrhoid (This is the likely diagnosis, as the patient has painless hematochezia) b) External hemorrhoid (This would be painful, and on exam the patient would likely have a sign of an inflamed blood vessel at the rectum) c) Bleeding peptic ulcer (This would present with dark bloody stool) d) Rectal fissure (This would cause pain every time the patient had a bowel movement) 103. What would you expect to see on an abdominal series that would lead toward a diagnosis of small-bowel obstruction? a) Air-fluid levels (This finding on an abdominal x-ray is the hallmark of a small-bowel obstruction) b) A lead pipe colon (This finding on an abdominal x-ray would be seen in toxic megacolon, a sequela of inflammatory bowel disease) c) Free air under the diaphragm (This would be seen on a bowel perforation) d) Steeple sign (This is a narrowing of the esophagus seen in croup) 104. Which gastrointestinal disease below could theoretically be completely eradicated with a total colectomy? a) Crohn’s disease (This disease can be anywhere in the digestive system; therefore, a colectomy would not eradicate the disease) b) Irritable bowel syndrome (This is generally a psychological condition that presents with gastrointestinal symptoms. Diet modification, cognitive therapy, and antidepressant medications work well) c) Ulcerative colitis (Ulcerative colitis is a disease only of the colon. While it is not the first treatment choice, total colectomy is a treatment option that can completely resolve this problem) d) Celiac disease (This is a problem with digestion of gluten-containing foods. Treatment includes avoidance of gluten-containing foods) 105. The screening guidelines for colon cancer recommend which of the following for the general population? a) Colonoscopy starting at age 50 (This is the recommended age to start colonoscopic examination in someone with a low risk for colon cancer) b) Colonoscopy starting at age 45. c) Fecal occult blood test (FOBT) and rectal exam starting at age 50 (Rectal exam and FOBT are recommended annually starting at age 40) d) Fecal occult blood test (FOBT) and rectal exam starting at age 45 (Rectal exam and FOBT are recommended annually starting at age 40) 106. All of the following medications are used for the control of nausea and vomiting. Which medication works by affecting the chemoreceptor trigger zone, thereby stimulating upper gastrointestinal motility and increasing lower esophageal sphincter pressure? a) Anticholinergics, such as scopolamine (Donnatal) (These anticholinergic (antispasmodic) drugs block the action of a neurotransmitter called acetylcholine which inhibits nerve impulses that are responsible for involuntary muscle movements) b) Antidopaminergic agents, such as prochlorperazine (Compazine) (These dopamine antagonists block dopamine receptors and as antiemetics aid in the treatment of nausea and vomiting) c) Antidopaminergic and cholinergic agents, such as metoclopramide (Reglan) (Metoclopramide (Reglan) is used for diabetic gastroparesis and postoperative nausea and vomiting. It works by affecting the chemoreceptor trigger zone, thereby stimulating upper gastrointestinal motility and increasing lower esophageal sphincter pressure) d) Tetrahydrocannabinols, such as dronabinol (Marinol) (The site and mechanism of tetrahydrocannabinols are unknown) 107. Which is the most common presenting symptom of gastric cancer? a) Weight loss (Weight loss is usually the presenting symptom of gastric cancer) b) Dysphagia (Dysphagia is another symptom of gastric cancer, but not as common as weight loss) c) Hematemesis (Hematemesis occurs in 10% to 15% of all clients with gastric cancer) d) Gastrointestinal bleeding (Gastrointestinal bleeding is uncommon with gastric cancer, although it is common with colorectal cancer) 108. The metabolism of which drug is not affected in Marsha, age 74? a) Alcohol (Although drug metabolism by the liver is usually impaired in older adults, the metabolism of alcohol is unchanged) b) Anticonvulsants (Drug metabolism by the liver is usually impaired in older adults) c) Psychotropics (Drug metabolism by the liver is usually impaired in older adults) d) Oral anticoagulants (Drug metabolism by the liver is usually impaired in older adults) 109. Marcie just returned from Central America with traveler’s diarrhea. Which is the best treatment? a) Metronidazole (Flagyl) (Metronidazole may be used for Clostridium difficile and for Entamoeba histolytica (amebiasis)) b) Supportive care (Enterotoxigenic Escherichia coli (ETEC) is the most common cause of traveler’s diarrhea, which occurs after ingesting contaminated food or water. It is usually self-limiting, requiring no treatment other than supportive care. It is common in developing countries. Traveler’s diarrhea caused by E coli used to be frequently treated with a 3- to 5-day course of a quinolone antibiotic, such as ciprofloxacin (Cipro)) c) Quinolone antibiotics (Quinolone antibiotics may be used for Salmonella if associated with a fever or systemic disease) d) Gastric lavage (Gastric lavage may be used for Clostridium botulinum) 110. Your client’s 2-month-old daughter is admitted with gastroenteritis and dehydration after 2 days of vomiting and diarrhea. When the father asks you what is causing the child’s diarrhea, how do you respond? a) “She must be lactose intolerant from the formula, and this is altering the fluid balance.” (The clinician cannot assume she is lactose intolerant. If she were, this probably would have happened before 2 months) b) “Her body’s telling you that it’s time to introduce some solids into her system.” (Infants should not be given solid food until 4 to 6 months) c) “The virus is causing irritation of the gastrointestinal lining, which causes diarrhea.” (Irritation of the gastrointestinal (GI) lining in itself will probably not cause diarrhea) d) “The infectious agent invaded the stomach lining and is affecting the balance of water and nutrients.” (In 80% of cases, gastroenteritis is viral in nature. This viral infection causes diarrhea by stimulating the secretion of electrolytes into the intestine. This is rapidly followed by water along the osmotic gradient, resulting in watery stools) 111. When Sammy asks you what he can do to help his wife, who has dumping syndrome, what do you suggest he encourage her to do? a) Eat foods higher in carbohydrates (To help clients with dumping syndrome, suggest that they reduce the amount of carbohydrates consumed) b) Eat 3 large meals plus 3 snacks per day (To help clients with dumping syndrome, suggest that they eat 6 small meals per day) c) Eat foods with a moderate fat and protein content (To help clients with dumping syndrome, suggest that they eat foods with a moderate fat and protein content. These foods tend to leave the stomach more slowly and do not draw fluid into the intestine) d) Drink fluids with each meal (To help clients with dumping syndrome, suggest that they take fluids between meals and not at mealtime) 112. You elicit costovertebral angle tenderness in Gordon, age 29. Which condition do you suspect? a) Cirrhosis (Percussion of the abdomen may elicit pain due to cirrhosis) b) Inflammation of the kidney (Costovertebral angle tenderness is tenderness or sharp pain that is elicited when one hand is “thumped” with the ulnar edge of the other fist over the 12th rib at the costovertebral angle on the back. It indicates inflammation of the kidney (and possible associated renal calculi, renal artery or vein occlusion, and perirenal abscess) c) Inflammation of the spleen (Percussion of the abdomen may elicit pain due to inflammation of the spleen) d) Peritonitis (Percussion of the abdomen may elicit pain due to peritonitis) 113. You are trying to differentiate between functional (acquired) constipation and Hirschsprung disease in a neonate. Distinguishing features of Hirschsprung disease include which of the following? a) Small ribbonlike stools (Hirschsprung disease is common in male infants, results in small ribbonlike stools, usually has no accompanying abdominal pain unless there is obstruction, and may be accompanied by failure to thrive. Other symptoms may include swollen belly; vomiting, including vomiting a green or brown substance; constipation; gas, which might make a newborn fussy; and diarrhea) b) Obvious abdominal pain (The infant with functional (acquired) constipation is usually male and has very large stools and abdominal pain) c) Female gender (Hirschsprung disease is more common in male infants) d) Small weight gain (Hirschsprung disease may be accompanied by failure to thrive. This is uncommon in infants with functional constipation) 114. You are doing routine teaching with a patient who has a family history of colorectal cancer. You know she misunderstands the teaching when she tells you she will: a) Decrease her fat intake (Decreased fat intake is recommended) b) Increase her fiber intake (Increased fiber intake is recommended) c) Continue her daily use of aspirin (The daily use of aspirin has been shown to decrease the incidence of colorectal cancer as well as dramatically decrease the incidence of metastasis) d) Increase her fluid intake (Increasing fluid intake has not been shown to decrease the risk of colorectal cancer. Current recommendations to aid in preventing colorectal cancer include decreased fat consumption, increased fiber consumption, and the daily use of aspirin) 115. Bobby, age 6, has constant periumbilical pain shifting to the right lower quadrant, vomiting, a small volume of diarrhea, absence of headache, a mild elevation of the white blood cell count with an early left shift, and white blood cells in the urine. You suspect: a) Appendicitis (Constant periumbilical pain shifting to the right lower quadrant; vomiting following the pain; a small volume of diarrhea; no systemic symptoms, such as a headache, malaise, or myalgia; a mild elevation of the white blood cell count with an early left shift; and white blood cells (WBCs) or red blood cells (RBCs) in the urine are indications of appendicitis. The WBC count becomes high only with gangrene or perforation of the appendix. The urine may have WBCs or RBCs if the bladder is irritated and ketonuria if there is prolonged vomiting) b) Gastroenteritis (Gastroenteritis would result in a large volume of diarrhea) c) Acute pancreatitis (Acute pancreatitis would result in vomiting and a fever in a child) d) Rocky Mountain spotted fever (Rocky Mountain spotted fever would present with nausea, vomiting, and fever) 116. Melva, age 63, presents with an acute exacerbation of pancreatitis, and you are going to admit her to the hospital. Which is the most important factor in determining a negative long-term outcome for her? a) Age (The older the patient, the greater the possibility of a negative outcome) b) Infection (The most important factor in determining long-term negative outcomes for pancreatitis is the presence of infection. Despite best practices, mortality associated with severe acute pancreatitis remains approximately 20% to 25% because of systemic complications) c) Pain (Pain should not factor into this outcome) d) Length of time between exacerbations (If a patient has many frequent exacerbations without much time between them, he or she also has a possibility of a negative outcome) 117. To differentiate among the different diagnoses of inflammatory bowel diseases, you look at the client’s histological, culture, and radiological features. Mary has transmural inflammation, granulomas, focal involvement of the colon with some skipped areas, and sparing of the rectal mucosa. What do you suspect? a) Crohn disease (Crohn disease would show transmural inflammation, granulomas, focal involvement of the colon with some skipped areas, and sparing of the rectal mucosa. The key words are “skipped areas of mucosal involvement.) b) Ulcerative colitis (Ulcerative colitis would show acute inflammatory infiltrates, depleted goblet cells, negative cultures, and continuous involvement of the mucosa) c) Infectious colitis (Infectious colitis, because of the toxic products released, may induce periportal inflammation, mild hepatomegaly, and low-grade liver enzyme abnormalities, but usually without trophozoites in the liver) d) Ischemic colitis (Ischemic colitis seen on colonoscopy reveals segmental inflammatory changes most often in the rectosigmoid and the splenic flexure, where there is more collateral circulation) 118. You suspect that Nikki has a gastroduodenal ulcer caused by Helicobacter pylori and plan to treat her empirically. What medications should you order? a) A proton pump inhibitor (omeprazole), tetracycline or amoxicillin, and metronidazole (Flagyl) (All of the drugs listed are used in the eradication of H pylori. Traditional 14-day “triple therapy” with a proton pump inhibitor (omeprazole), tetracycline or amoxicillin, and metronidazole (Flagyl) has consistently produced eradication rates of approximately 95% and is the least expensive therapy) b) Bismuth subsalicylate (Pepto-Bismol) and omeprazole (Prilosec) (Both drugs listed are used in the eradication of H pylori, but do not complete the regimen) c) Amoxicillin (Amoxil) and omeprazole (Prilosec) (Both drugs listed are used in the eradication of H pylori, but do not complete the regimen) d) Clarithromycin (Biaxin) and metronidazole (Flagyl) (Both drugs listed are used in the eradication of H pylori, but do not complete the regimen) 119. Which of the following medications/drugs are not known to cause heartburn or dyspepsia? a) Alcohol. b) Motrin. c) Prednisone. d) Tylenol. 120. A 7-year-old male presents with his mother to the urgent care clinic complaining of abdominal pain. He started to complain of pain prior to going to bed; however, it has gotten progressively worse and is now preventing him from sleeping. He is nauseous but hasn’t vomited and didn’t eat dinner due to the pain. The patient appears pale and is complaining of right-sided abdominal pain. His vitals are as follows: blood pressure 130/85, pulse 120, temperature 100.5°F, pulse oximetry 98% on room air. On physical exam he is tender in the right lower quadrant. His complete blood count (CBC) shows a white blood cell count (WBC) of 17.0. What is the patient’s likely diagnosis? a) Appendicitis (This is the clinical scenario typical for appendicitis) b) Cholecystitis (The patient’s pain is in the right lower quadrant (RLQ), not the right upper quadrant (RUQ); also, cholecystitis is rare in children) c) Constipation (Constipation doesn’t cause leukocytosis or vital sign changes) d) Gastroenteritis (The patient has no diarrhea or vomiting) 121. Hepatitis D is an RNA virus that requires a coinfection with which of the following strains of hepatitis in order to replicate? a) Hepatitis A (Hepatitis A is not associated with coinfection of hepatitis D) b) Hepatitis B (Hepatitis D requires hepatitis B surface antigen to replicate) c) Hepatitis C (Hepatitis C is not associated with coinfection of hepatitis D) d) Hepatitis E (Hepatitis E is not associated with coinfection of hepatitis D) 122. Which of the following is the most common cause of acute pancreatitis? a) Gallstone obstruction of the pancreatic duct (Both gallstones and alcoholism are the most common causes of acute pancreatitis) b) Alcoholism (Both gallstones and alcoholism are the most common causes of acute pancreatitis) c) Hypertriglyceridemia (his is a cause of pancreatitis but is less common) d) Gallstone obstruction of the pancreatic duct and alcoholism (Both gallstones and alcoholism are the most common causes of acute pancreatitis) 123. A patient asks how to avoid contracting pharyngitis and tonsillitis. Which piece of advice is not appropriate for this patient? a) “Replace your toothbrush as soon as you develop a sore throat.” (Toothbrushes may harbor causative microorganisms) b) “Use condoms or dental dams when performing oral sex.” (Latex barrier protection can help avoid orogenital transmission of infectious organisms) c) “Take antibiotics when well to avoid future infections.” (Patients should only be prescribed antibiotics if a throat culture confirms disease of bacterial origin) d) ”Avoid low-humidity environments.” (Avoiding environmental irritants such as tobacco and marijuana smoke, pollution, dust, and low-humidity environments can help prevent noninfectious forms of pharyngitis) 124. Simon, age 72, states that he is worried because he has a bowel movement only every third day. You respond a) “You should have two to three stools per day.” (Patterns of defecation vary widely; there is no “normal” pattern) b) “You should defecate once a day.” (Patterns of defecation vary widely; there is no “normal” pattern) c) “You should have at least three stools per week.” (Patterns of defecation vary widely; there is no “normal” pattern) d) “There is no such thing as a ‘normal’ pattern of defecation.” (There is no such thing as a “normal” pattern of defecation. Patterns of defecation vary widely and may in part be affected by dietary habits, fluid intake, bacteria in the stool, psychological stress, or voluntary postponement of defecation. Defecating every third day could be the routine pattern for Simon. He should be questioned if this is routine for him) 125. Timothy, age 68, complains of an abrupt change in his defecation pattern. You evaluate him for: a) Constipation (Constipation may be part of the pattern between constipation and diarrhea in many conditions; for example, Irritable bowel syndrome may result in either) b) Colorectal cancer (A middle-aged or older client with an abrupt change in defecation pattern must be evaluated for colorectal cancer) c) Irritable bowel syndrome (Irritable bowel syndrome may result in constipation or diarrhea) d) Acute appendicitis (Fecal stasis may be a factor in acute appendicitis, BUT an abrupt change in defecation patterns must be evaluated for possible colorectal cancer) 126. Ellie, age 42, has a seizure disorder and has been taking phenytoin (Dilantin) for years. Which supplement should she also be taking if no other problems exist? a) Vitamin B12. (Vitamin B12 is not affected by phenytoin.) b) Iron (Iron is not affected by phenytoin) c) Folic acid (Clients taking phenytoin (Dilantin) should also be taking 0.4 to 1 mg/d of folic acid because Dilantin promotes a folate deficiency) d) Calcium (Phenytoin may also contribute to demineralization of the bone, so serum calcium levels should be checked as well. If demineralization is detected, then vitamin D should be added) 127. Marvin, a known alcoholic with cirrhosis, is frequently admitted for coagulopathies and occasionally receives blood transfusions. His wife asks you why he has bleeding problems. How do you respond? a) “Occasionally he accumulates blood in the gut.” (An accumulation of blood in the gut would not affect coagulation) b) “There is an interruption of the normal clotting mechanism” (Because of Marvin’s alcoholism and his resulting dietary insufficiencies, there is an inadequate amount of vitamin K in the liver for thrombin to convert fibrinogen to fibrin; thus, the sequence of coagulation is disrupted) c) “Long-term alcohol abuse has made his vessels very friable.” (Large numbers of spider angiomas are associated with liver cirrhosis. Excessive drinking also widens blood vessels and increases blood flow to the skin; hence, it can lead to thread veins, a reddened “drinker’s nose,” and rosacea) d) “His bone marrow has been affected.” (While vitamin K plays an important role in bone metabolism and the optimization of bone health, the reverse is not true; bone marrow does not affect the amount of vitamin K) 128. Icterus due to hyperbilirubinemia is seen when the serum level of bilirubin is greater than? a) 2.5 mg/dL (A bilirubin level greater than 2.5-3 mg/dL is associated with yellowing of the eyes) b) mg/dL. c) 2.0 mg/dL. d) 0.5 mg/dL. 129. Samantha, age 28, is 100 lb overweight and wants to have a gastroplasty performed. In discussing this with her, you explain that by having this procedure she may: a) Develop diarrhea (Diarrhea is a common problem after a gastroplasty because of the induced malabsorption) b) Lose too much weight (Clients usually do not end up losing too much weight because sometimes the only foods they can tolerate are high-calorie foods (simple sugars), such as ice cream) c) Develop hemorrhoids (Losing weight will probably help a hemorrhoid problem) d) Vomit after she eats (While Samantha may vomit after she eats, the problem of diarrhea is much more common) 130. You suspect that Harry has a peptic ulcer and tell him that it has been found to be strongly associated with: a) Anxiety and panic attacks (Stress-related conditions, such as anxiety and panic attacks, may contribute to and aggravate peptic ulcer disease) b) Long-term use of nonsteroidal anti-inflammatory drugs (NSAIDs) (Long-term use of NSAIDs may contribute to and aggravate peptic ulcer disease) c) Infection by Helicobacter pylori (About 90% of cases of peptic ulcers have been found to be caused by infection with the bacteria H pylori) d) A family history of peptic ulcers (Research studies have been inconclusive regarding the hereditary factor for gastric and duodenal ulcers.) 131. What is the recommended treatment to eradicate a Helicobacter pylori infection? a) Ranitidine, amoxicillin, and clarithromycin for 2 weeks (This treatment is missing a proton pump inhibitor (PPI), instead using an H2 antagonist) b) Amoxicillin, clarithromycin, and omeprazole for 2 weeks (This is the recommended treatment to eradicate H pylori) c) Bismuth, amoxicillin, and clarithromycin for 2 weeks (This regimen is missing a proton pump inhibitor (PPI), instead using bismuth) d) Bismuth, doxycycline, metronidazole, and ranitidine (This 4-medication regimen can be used; however, a proton pump inhibitor (PPI) needs to be exchanged for the H2 antagonist) 132. Which of the following is not a risk factor for cholecystitis? a) Female gender. b) Obesity. c) Sickle cell anemia. d) Younger age. [Show More]
Last updated: 1 year ago
Preview 1 out of 33 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Nov 14, 2020
Number of pages
33
Written in
Additional information
This document has been written for:
Uploaded
Nov 14, 2020
Downloads
0
Views
35


x.png)

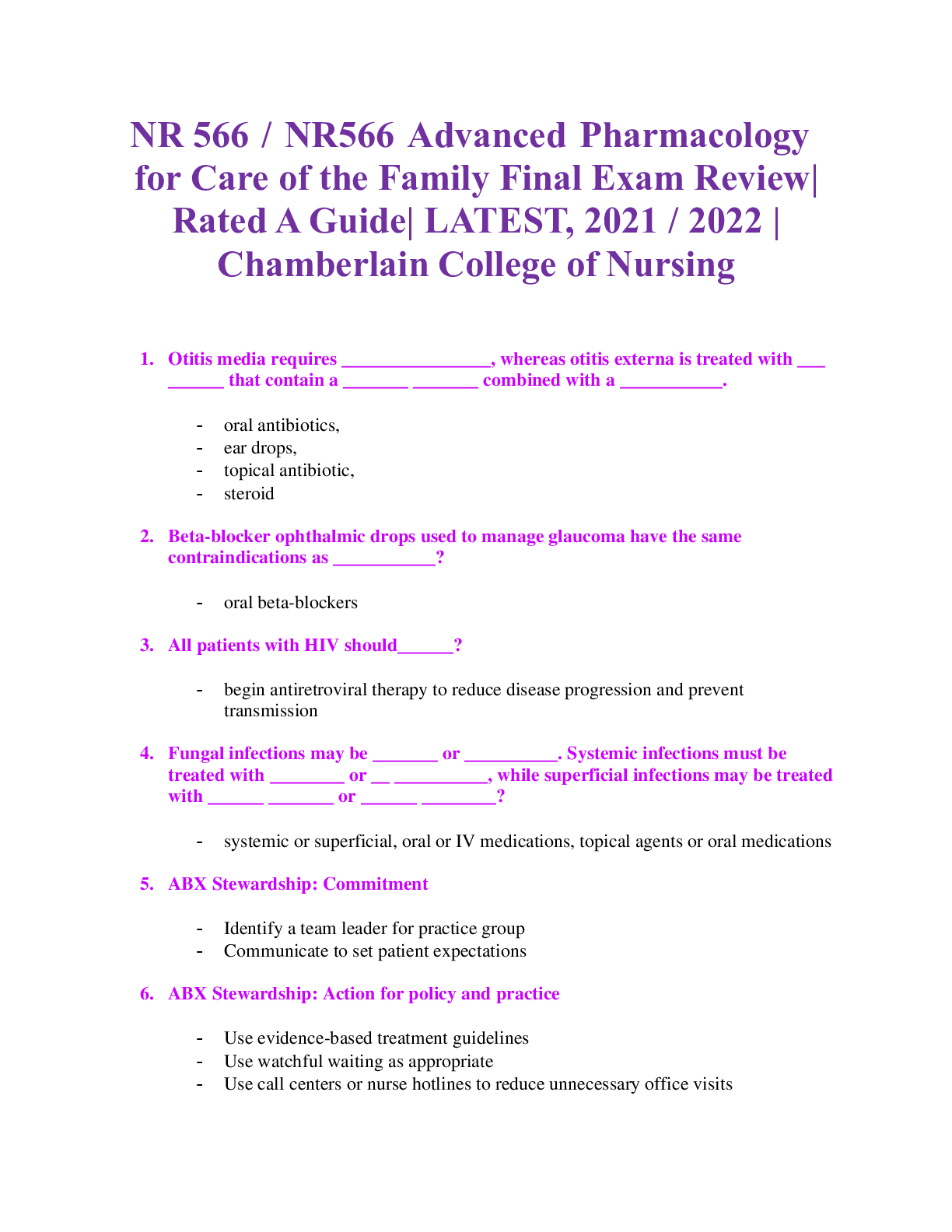
.png)
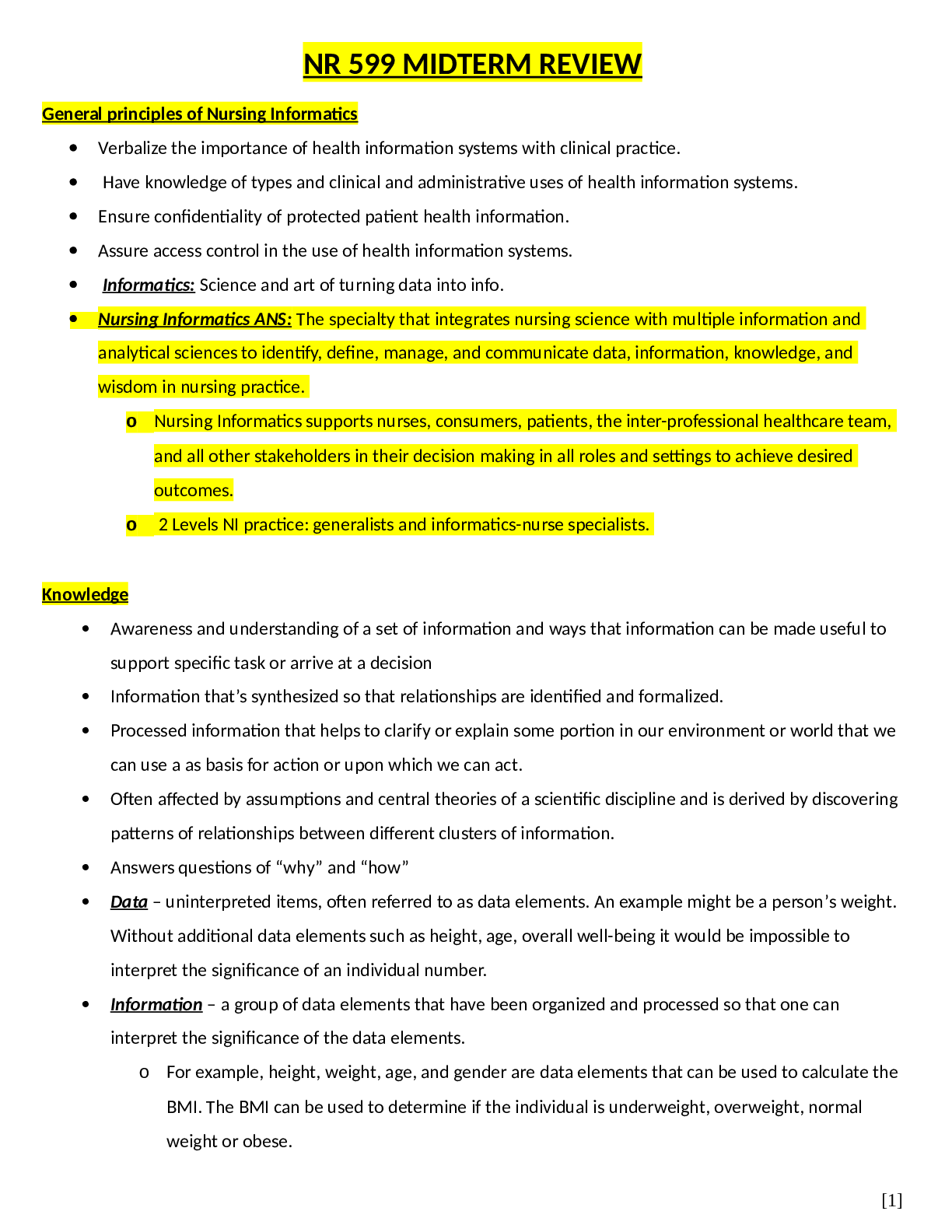

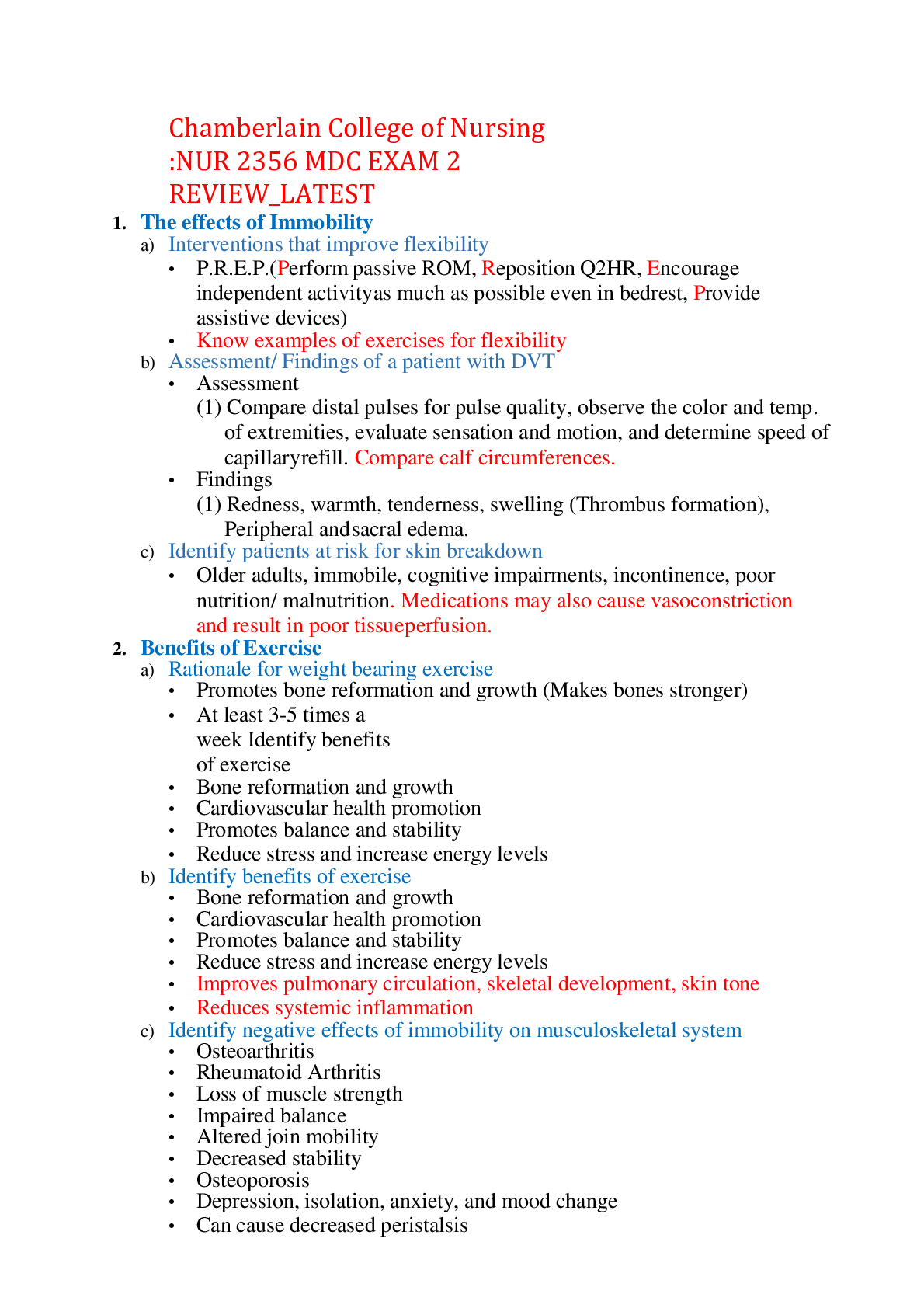
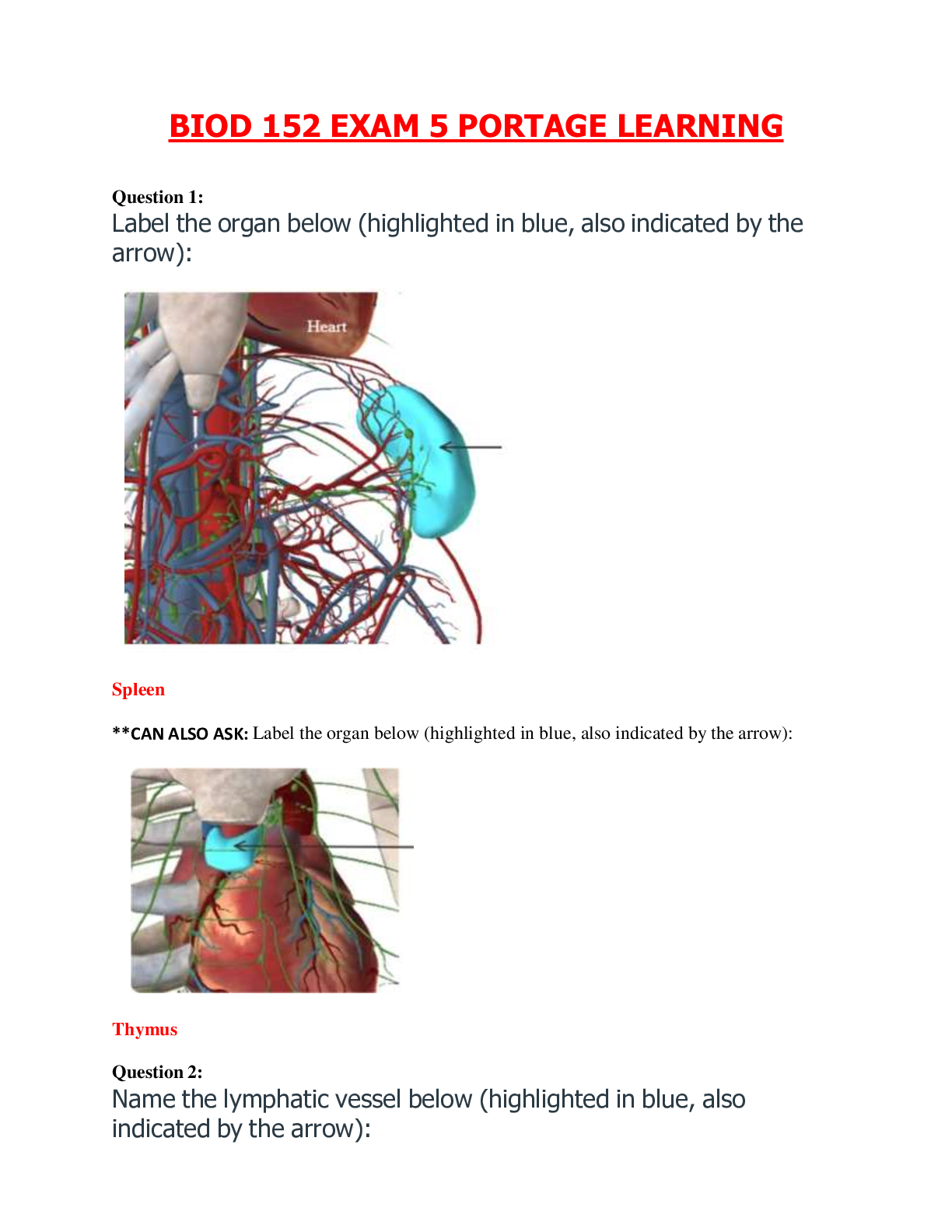
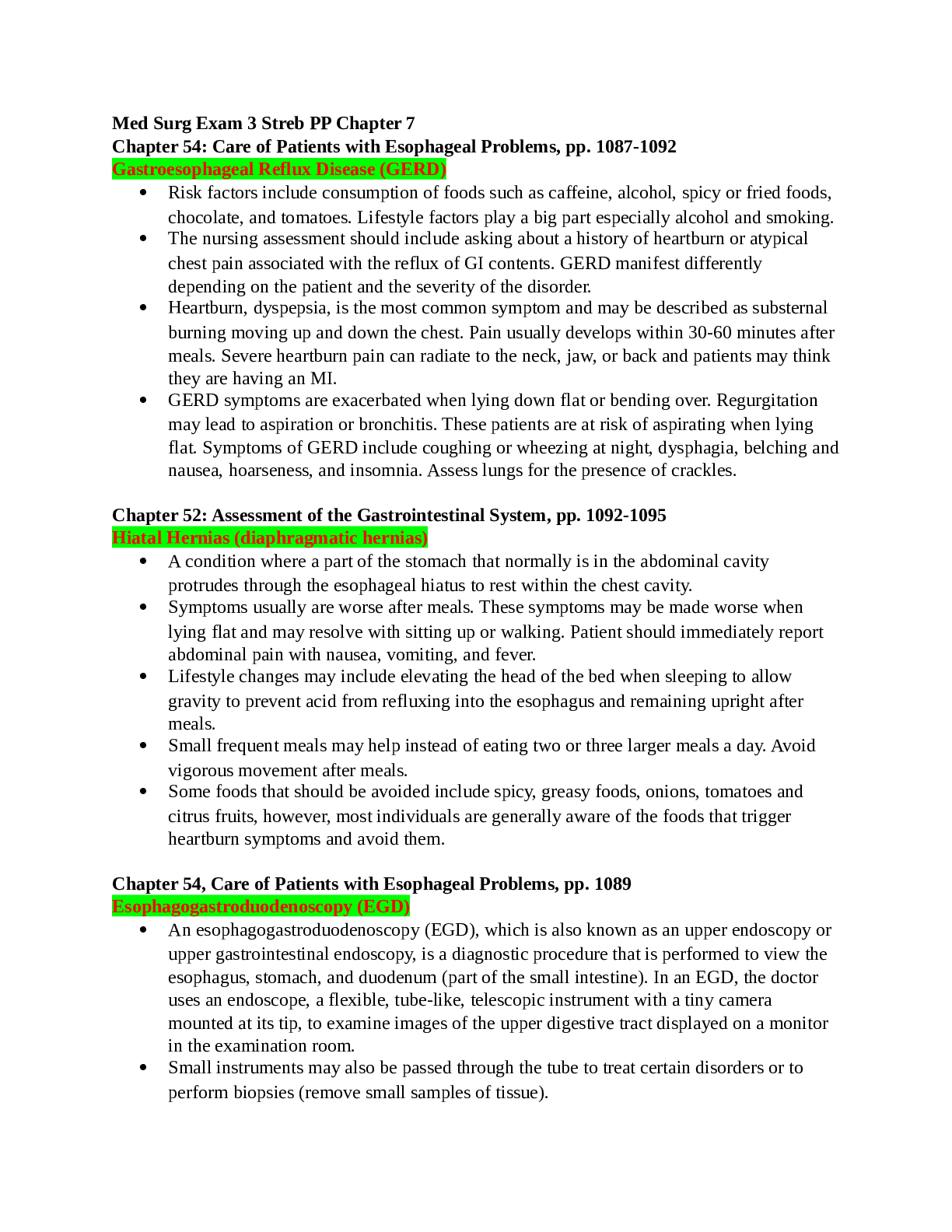
.png)