Health Care > EXAM > HIT 252 CCA Exam 1 Questions and Answers | 100% Guaranteed Distinction (All)
HIT 252 CCA Exam 1 Questions and Answers | 100% Guaranteed Distinction
Document Content and Description Below
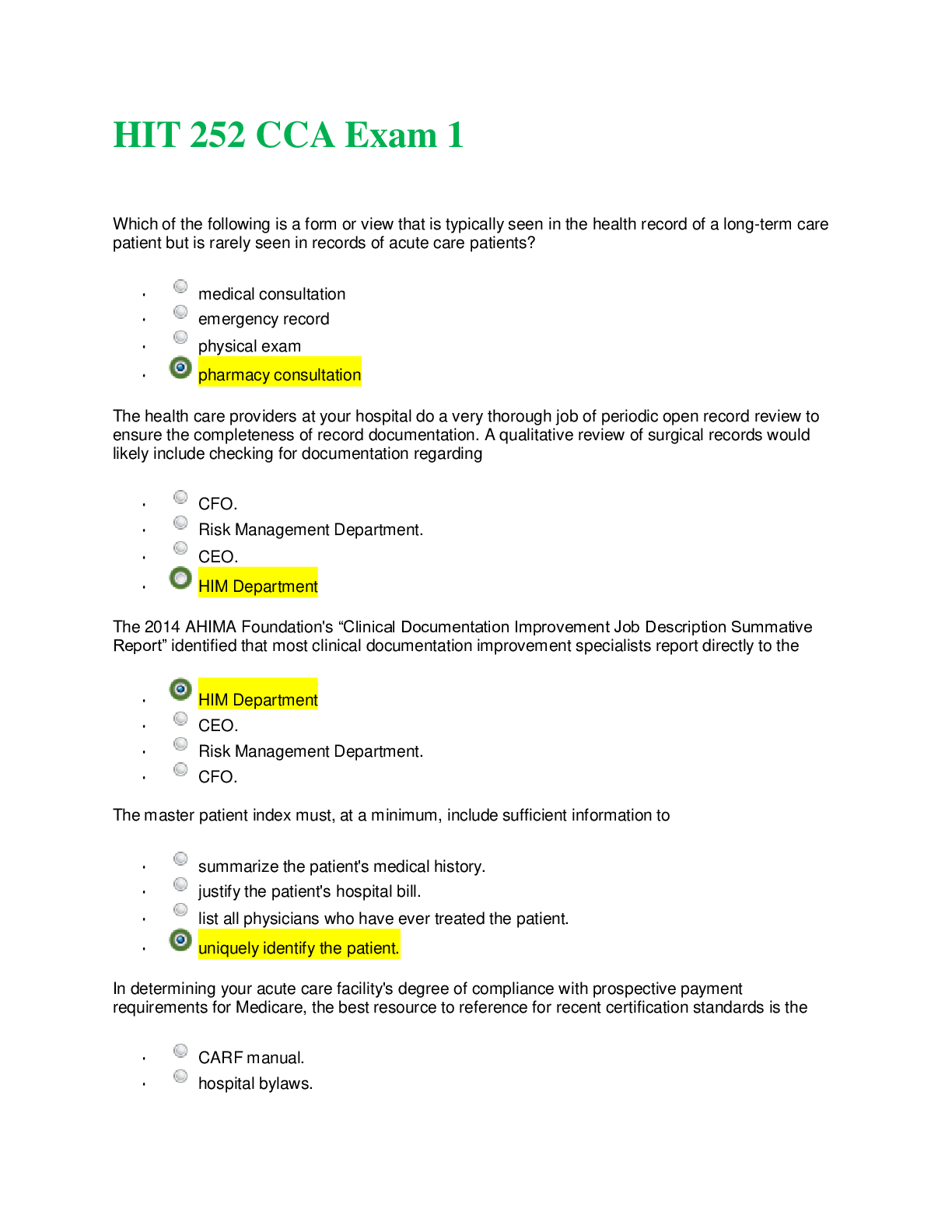
HIT 252 CCA Exam 1 Which of the following is a form or view that is typically seen in the health record of a long-term care patient but is rarely seen in records of acute care patients? • me... dical consultation • emergency record • physical exam • pharmacy consultation The health care providers at your hospital do a very thorough job of periodic open record review to ensure the completeness of record documentation. A qualitative review of surgical records would likely include checking for documentation regarding • CFO. • Risk Management Department. • CEO. • HIM Department The 2014 AHIMA Foundation's “Clinical Documentation Improvement Job Description Summative Report” identified that most clinical documentation improvement specialists report directly to the • HIM Department • CEO. • Risk Management Department. • CFO. The master patient index must, at a minimum, include sufficient information to • summarize the patient's medical history. • justify the patient's hospital bill. • list all physicians who have ever treated the patient. • uniquely identify the patient. In determining your acute care facility's degree of compliance with prospective payment requirements for Medicare, the best resource to reference for recent certification standards is the • CARF manual. • hospital bylaws. • Federal Register. • Joint Commission accreditation manual. The health record states that the patient is a female, but the registration record has the patient listed as male. Which of the following characteristics of data quality has been compromised in this case? • data comprehensiveness • data accuracy • data precision • data granularity Protected health information includes • individually identifiable health information in any format stored by a health care provider or business associate. • only electronic individually identifiable health information. • individually identifiable health information in any format stored by a health care provider. • only paper individually identifiable health information. A retrospective review as part of quality improvement activities is conducted after the patient has been • discharged. • admitted. • released from the surgical recovery room. • cleared for surgery. As the chair of a Forms Review Committee, you need to track the field name of a particular data field and the security levels applicable to that field. Your best source for this information would be the • UHDDS. • MDS. • facility's data dictionary. • glossary of health care terms. The first patient with cancer seen in your facility on January 1, 2018 was diagnosed with colon cancer with no known history of previous malignancies. The accession number assigned to this patient is • 18-0001/00. • 18-0000/01. • 18-0000/00. • 18-0001/01. According to the following table, the most serious record delinquency problem occurred in which of the following months? Record Delinquency for Second Quarter April May June Percentage incomplete records 70% 88% 79% Percentage delinquent records 51% 43% 61% Percentage delinquent due to missing H&P 3% 1.4% 0.5% • June • May • cannot determine from these data • April In quality review activities, departments are directed to focus on clinical processes that are • most commonplace. • low volume. • high risk. • expensive. Identify an appropriate use of the emergency access procedure. • The coder who usually codes the emergency room charts is out sick and the charts are left on a desk in the ER admitting area. • Data is collected for administrative purposes. • An audit is being conducted by the OIG. • A patient is crashing. The attending physician is not in the hospital, so a physician who is available helps the patient. Using the SOAP style of documenting progress notes, choose the "subjective" statement from the following. • patient states low back pain is as severe as it was on admission • patient moving about very cautiously, appears to be in pain • adjust pain medication; begin physical therapy tomorrow • sciatica unimproved with hot pack therapy The old practices of flagging records for deficiencies and requiring retrospective documentation add little or no value to patient care. You try to convince the entire health care team to consistently enter data into the patient's record at the time and location of service instead of waiting for retrospective analysis to alert them to complete the record. You are proposing • quantitative record review. • concurrent record analysis. • clinical pertinence review. • point-of-care documentation. During a retrospective review of Rose Hunter's inpatient health record, the health information clerk notes that on day 4 of hospitalization, there was one missed dose of insulin. What type of review is this clerk performing? • qualitative review • utilization review • quantitative review • legal review Which method of identification of authorship or authentication of entries would be inappropriate to use in a patient's health record? • delegated use of computer key by radiology secretary • written signature of the provider of care • a unique identification code entered by the person making the report • identifiable initials of a nurse writing a nursing note A key data item you would expect to find recorded on an ER record but would probably NOT see in an acute care record is the • lab and diagnostic test results. • time and means of arrival. • physical findings. • instructions for follow-up care. Which of the four distinct components of the problem-oriented record serves to help index documentation throughout the record? • problem list • database • initial plan A data item to include on a qualitative review checklist of newborn inpatient health records that need NOT be included on adult records would be • chief complaint. • time and means of arrival. • APGAR score. • condition on discharge. progress notes You are developing a complete data dictionary for your facility. Which of the following resources will be most helpful in providing standard definitions for data commonly collected in acute care hospitals? • Federal Register • Conditions of Participation • Uniform Hospital Discharge Data Set • Minimum Data Set As a new HIM manager of an acute care facility, you have been asked to update the facility's policy for a physician's verbal orders in accordance with Joint Commission standards and state law. Your first area of concern is the qualifications of those individuals in your facility who have been authorized to record verbal orders. For this information, you will consult the • consolidated manual for hospitals. • Federal Register. • hospital bylaws, rules, and regulations. • policy and procedure manual. A health care facility has made a decision to destroy computerized data. AHIMA recommends which one of the following as the preferred method of destruction for computerized data? • disk reformatting • overwriting the backup tapes • overwriting data with a series of characters • magnetic degaussing In the computerization of forms, good screen-view design, along with the options of alerts and alarms, makes it easier to ensure that all essential data items have been captured. One essential item to be captured on the physical exam is the • subjective review of systems. • family history as related by the patient. • chief complaint. • general appearance as assessed by the physician. Which of the following should NOT be included in the documentation of record destruction? • method of destruction • signature of the individuals supervising and witnessing the destruction • statement that records were destroyed in the normal course of business • dates not covered in destruction You are the office manager at a large group practice. One of the physicians at your practice has asked you to research and supply her with information about the legislation signed into law in 2015 which required the removal of social security numbers from all Medicare cards. You will provide this inquisitive physician with a fact sheet concerning this legislation: • Healthcare Quality Improvement Act • Health Information Technology for Economic and Clinical Health Act (HITECH) • Medicare Access and CHIP Reauthorization Act (MACRA) • Tax Equity and Fiscal Responsibility Act (TEFRA) In your acute care facility it has become critical that up-to-date information regarding patients who are transferred to the oncology patient care unit be immediately sent to an outpatient scheduling system to facilitate outpatient appointments. This transfer of service can be obtained most readily from • the indicator monitoring program. • the disease index. • the R-ADT system. • generic screens used by record abstractors. Joint Commission standards require that a complete history and physical be documented on the health records of operative patients. Does this report carry a time requirement? • yes, within 8 hours postsurgery • yes, within 24 hours postsurgery • no, as long as it is done ASAP • yes, prior to surgery Many of the principles of forms design apply to both paper-based and computer-based systems. For example, the physical layout of the form and/or screen should be organized to match the way the information is requested. Facilities that are scanning and imaging paper records as part of a computer-based system must give careful consideration to • signature line for authentication. • bar code placement. • placement of hospital logo. • use of box design. n 1987, OBRA helped shift the focus in long-term care to patient outcomes. As a result, core assessment data elements are collected on each SNF resident as defined in the • MDS. • UHDDS. • Uniform Clinical Data Set. • Uniform Ambulatory Core Data. Reviewing a medical record to ensure that all diagnoses are justified by documentation throughout the chart is an example of • legal analysis. • quantitative review. • qualitative review. • peer review. Patient mortality, infection and complication rates, adherence to living will requirements, adequate pain control, and other documentation that describe end results of care or a measurable change in the patient's health are examples of • incident reports. • outcome measures. • sentinel events. • threshold level. Improving the specificity of clinical reports through the use of a physician query is a documentation goal that may be shared by the coding staff and this specialist: • CHPS • CDIP • Certified Health Data Analyst • CTR Setting up a drop-down menu to make sure that the registration clerk collects "gender" as "male, female, or unknown" is an example of ensuring data • timeliness. • reliability. • precision. • validity. You notice on the admission H&P that Mr. McKahan, a Medicare patient, was admitted for disc surgery, but the progress notes indicate that due to some heart irregularities, he may not be a good surgical risk. Because of your knowledge of COP regulations, you expect that a(n) will be added to his health record. • interval summary • interdisciplinary care plan • advance directive • consultation report Gerda Smith has presented to the ER in a coma with injuries sustained in a motor vehicle accident. According to her sister, Gerda has had a recent medical history taken at the public health department. The physician on call is grateful that she can access this patient information using the area's • EDMS system. • RHIO. • expert system. • CPOE. As a trauma registrar working in an emergency department, you want to begin comparing your trauma care services to other hospital-based emergency departments. To ensure that your facility is collecting the same data as other facilities, you review elements from which data set? • MDS • UHDDS • ORYX • DEEDS Under which of the following conditions can an original paper-based patient health record be physically removed from the hospital? • when the record is taken to a physician's private office for a follow-up patient visit post discharge • when the director of health records is acting in response to a subpoena duces tecum and takes the health record to court • when the patient is discharged by the physician and at the time of discharge is transported to a long-term care facility with his health record • when the patient is brought to the hospital emergency department following a motor vehicle accident and, after assessment, is transferred with his health record to a trauma- designated emergency department at another hospital In creating a new form or computer view, the designer should be most driven by • medical staff bylaws. • QIO standards. • needs of the users. • flow of data on the page or screen. Based on the following documentation in an acute care record, where would you expect this excerpt to appear? • discharge summary • admission note • physical exam • clinical laboratory report You have been appointed as chair of the Health Record Committee at a new hospital. Your committee has been asked to recommend time-limited documentation standards for inclusion in the medical staff bylaws, rules, and regulations. The committee documentation standards must meet the standards of both the Joint Commission and the Medicare Conditions of Participation. The standards for the history and physical exam documentation are discussed first. You advise them that the time period for completion of this report should be set at • 24 hours after admission or prior to surgery. • 12 hours after admission. • 12 hours after admission or prior to surgery. • 24 hours after admission. The Joint Commission has a standard stating that a hospital must plan and design information management processes to meet information needs. • internal • external • patient record • both internal and external A clinical documentation specialist performs many duties. These include reviewing the data and looking for trends or patterns over time, as well as noting any variances that require further investigation. In this role, the CDS professional is acting as a(n) • analyst. • educator. • reviewer. • ambassador. Which of the following reports would normally be considered a consultation? • tissue examination done by the pathologist • technical interpretation of electrocardiogram • interpretation of a radiologic study • impressions of a cardiologist asked to determine whether patient is a good surgical risk As the compliance officer for a large physician practice group, you are interested in researching the original requirements for meaningful use of certified EHRs for use in an upcoming presentation. You begin by googling • Health Care Quality Improvement Act. • HIPAA. • EMTALA. • HITECH Act. In an acute care hospital, a complete history and physical may not be required for a new admission when • a legible copy of a current H&P performed in the attending physician's office is available. • the patient's stay is less than 24 hours. • the patient is readmitted for a similar problem within 1 year. • the patient has an uneventful course in the hospital. Currently, the enforcement of HIPAA Privacy and Security Rules is the responsibility of the • FBI. • Office for Civil Rights. • Department of Recovery Audit Coordinators. • Office of Inspector General. Though you work in an integrated delivery network, not all systems in your network communicate with one another. As you meet with your partner organizations, you begin to sell them on the concept of an important development intended to support the exchange of health information across the continuum within a geographical community. You are promoting that your organization join a • continuum of care. • regional health information organization. • data warehouse. • data retrieval portal group. Which of the following is least likely to be identified by a retrospective quantitative analysis of a health record? • need for physician authentication of two verbal orders • X-ray report charted on the wrong record • missing discharge summary • discrepancy between postoperative diagnosis by the surgeon and pathology diagnosis by the pathologist An example of a primary data source for health care statistics is the • MPI. • disease index. • accession register. • health record. [Show More]
Last updated: 1 year ago
Preview 1 out of 12 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Aug 03, 2022
Number of pages
12
Written in
Additional information
This document has been written for:
Uploaded
Aug 03, 2022
Downloads
0
Views
37

.png)


.png)