Health Care > iHuman > Ihuman WEEK 12: Sarah O'Neil, 25y/o FEMALE CC. DEPRESSION (All)
Ihuman WEEK 12: Sarah O'Neil, 25y/o FEMALE CC. DEPRESSION
Document Content and Description Below
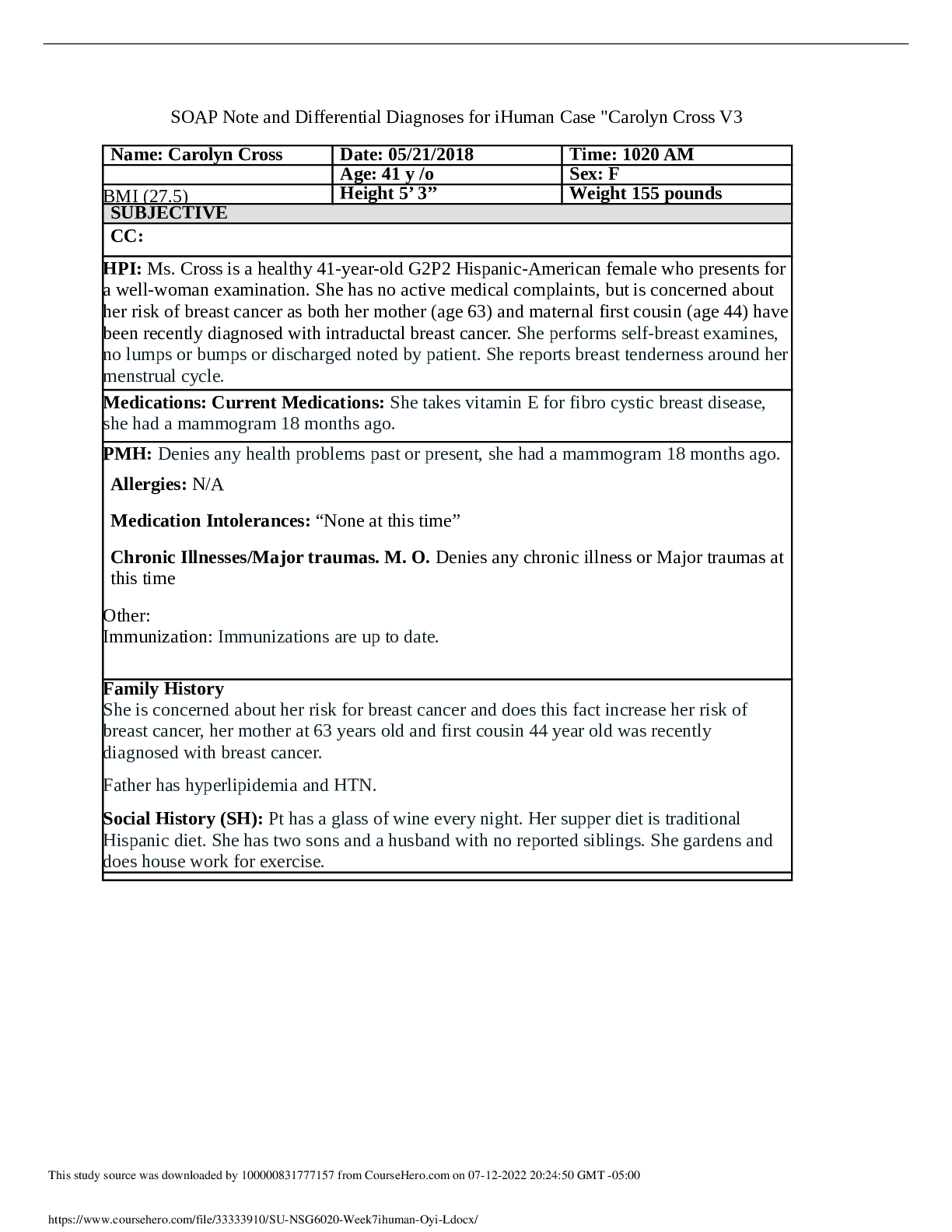
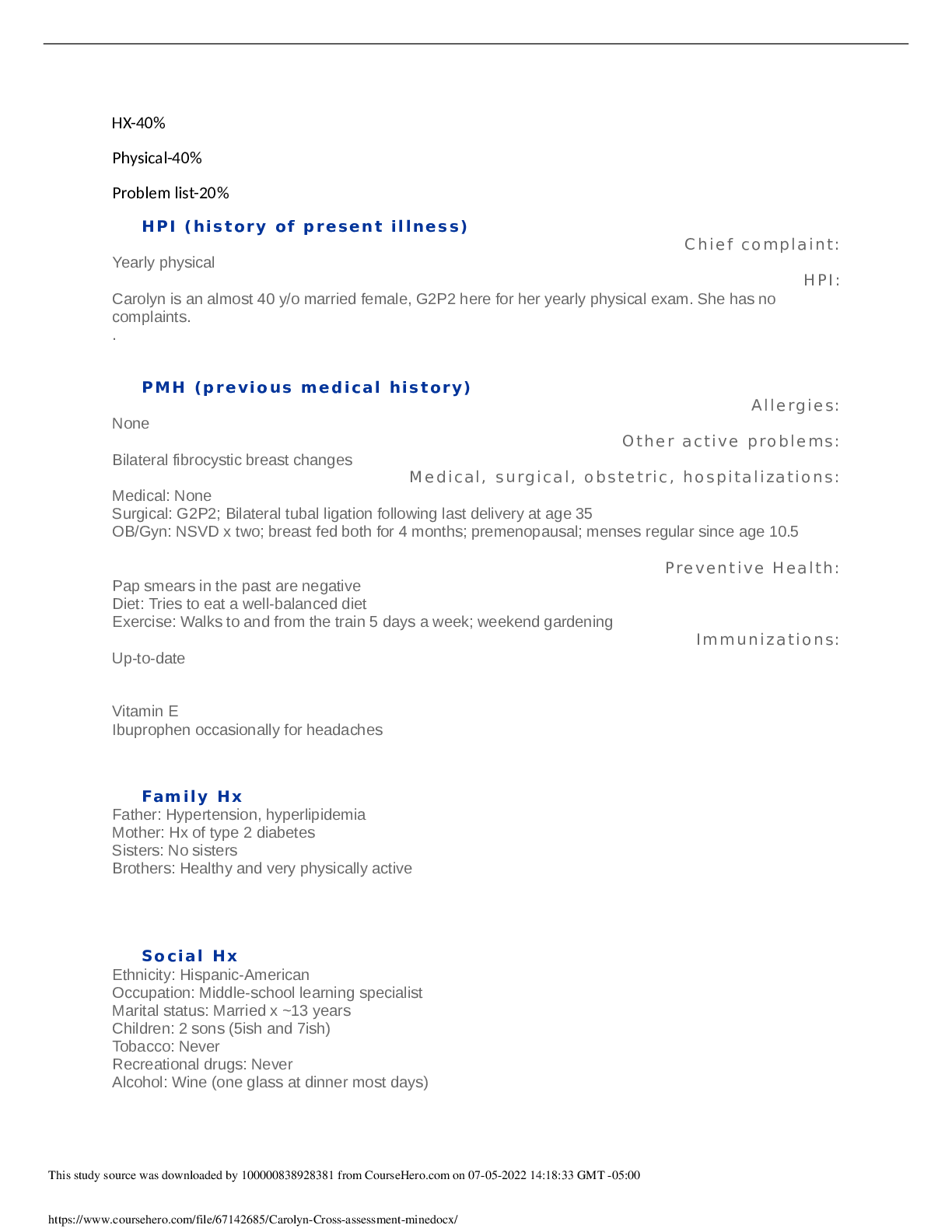
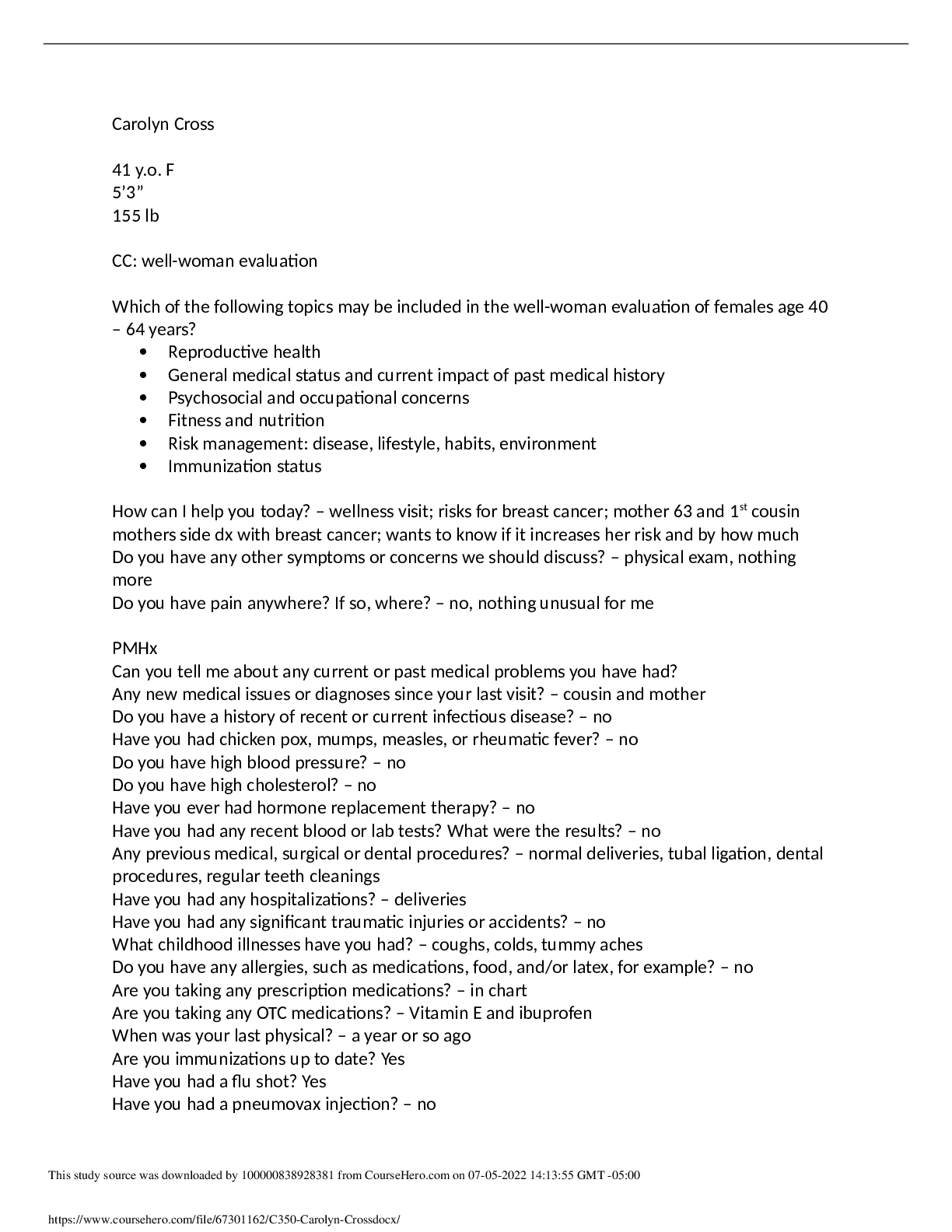
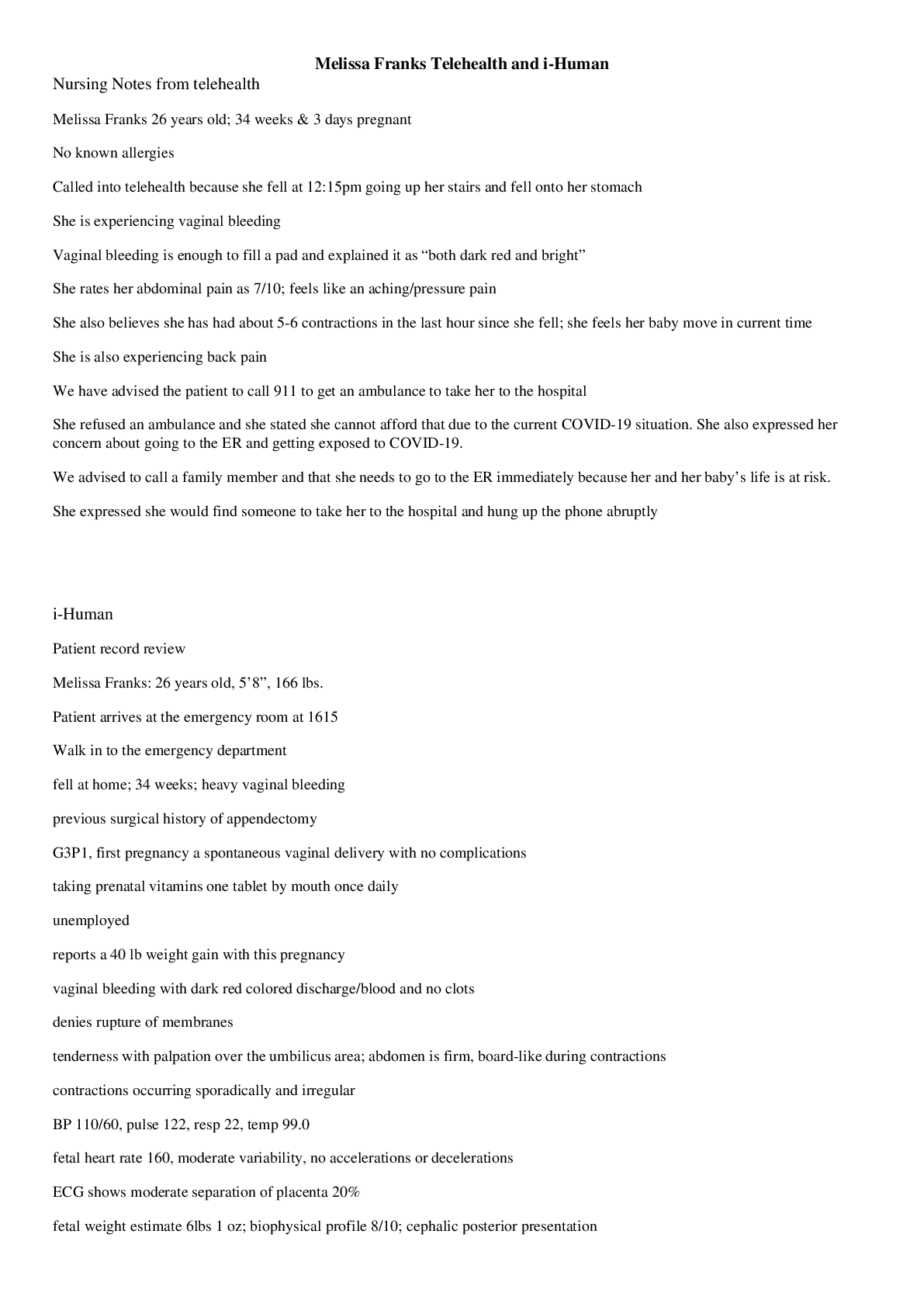
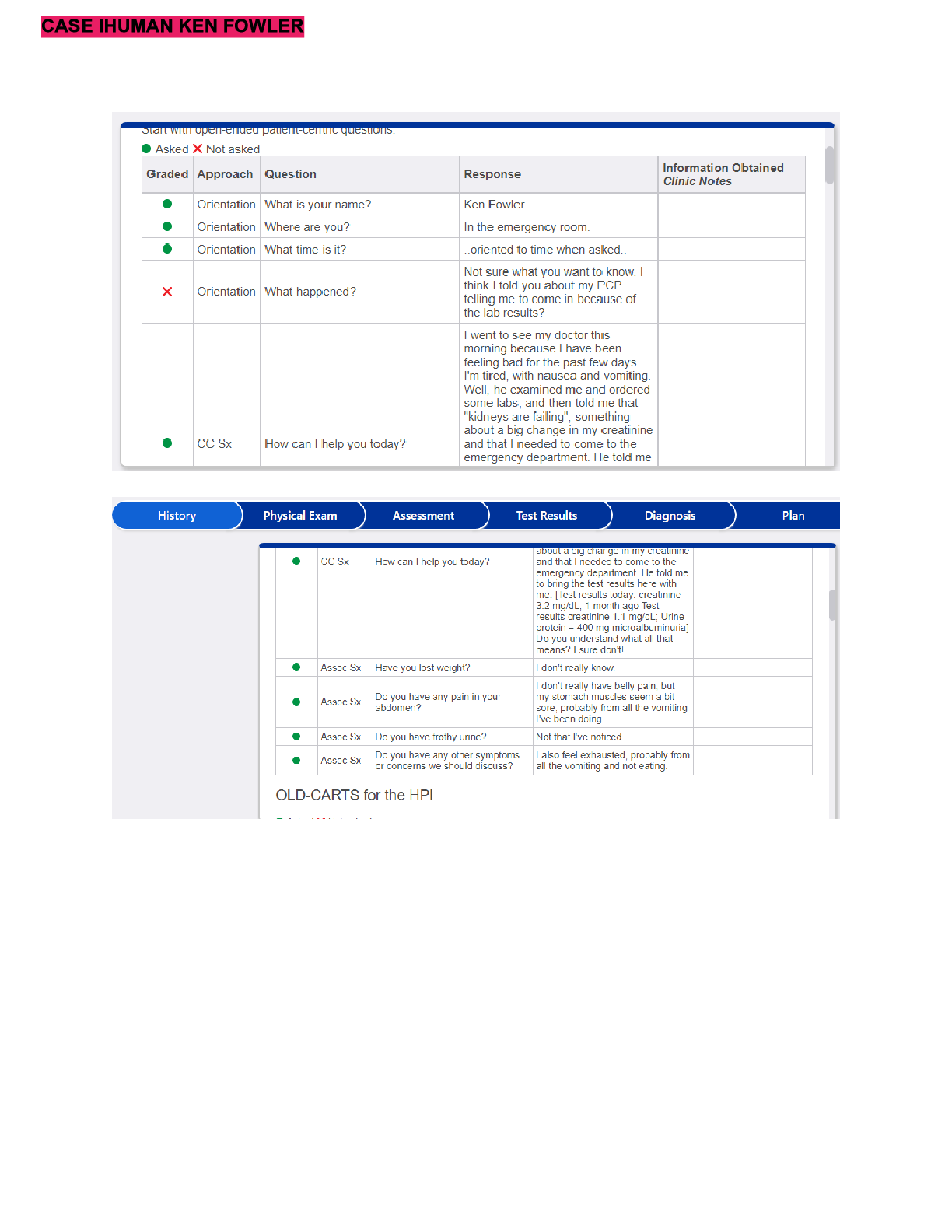
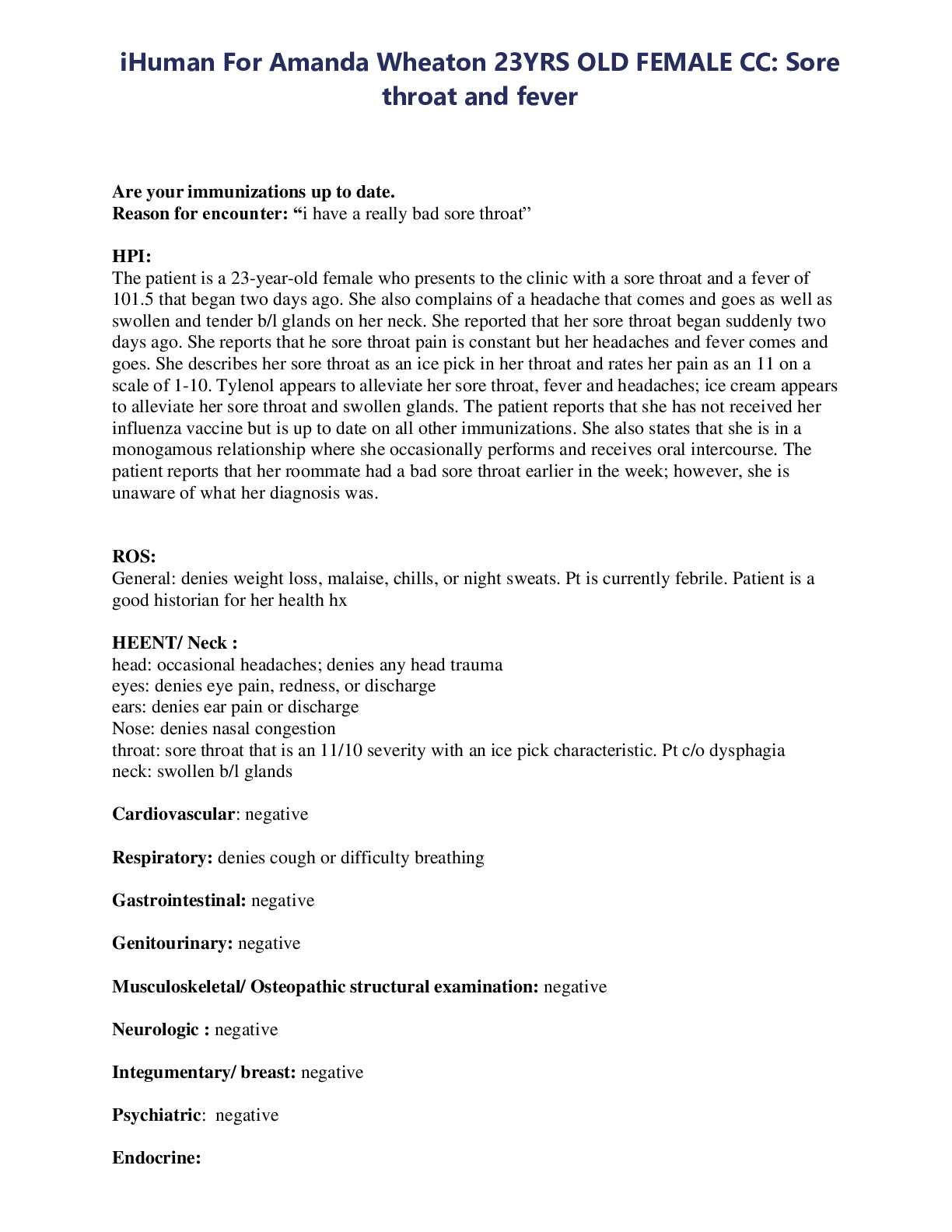
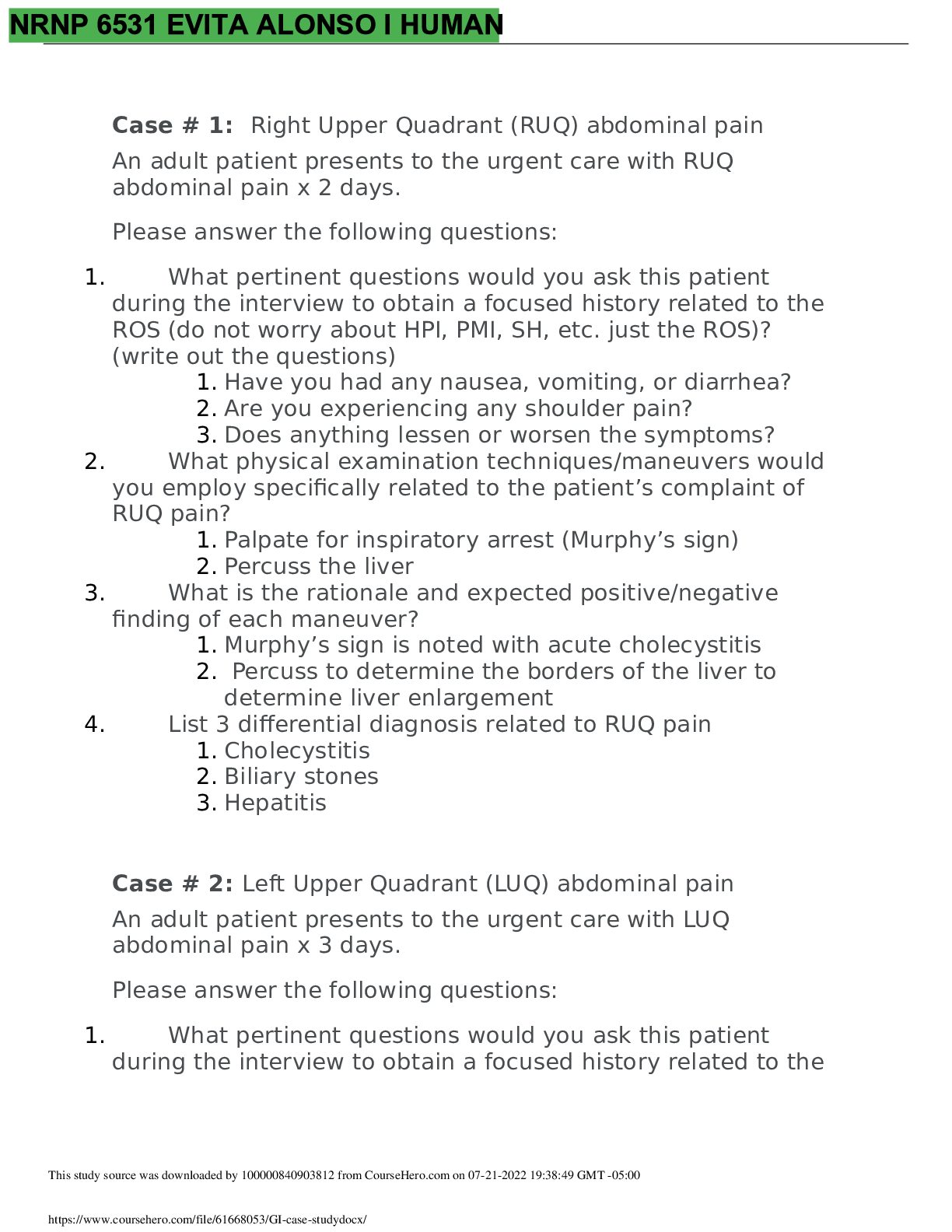
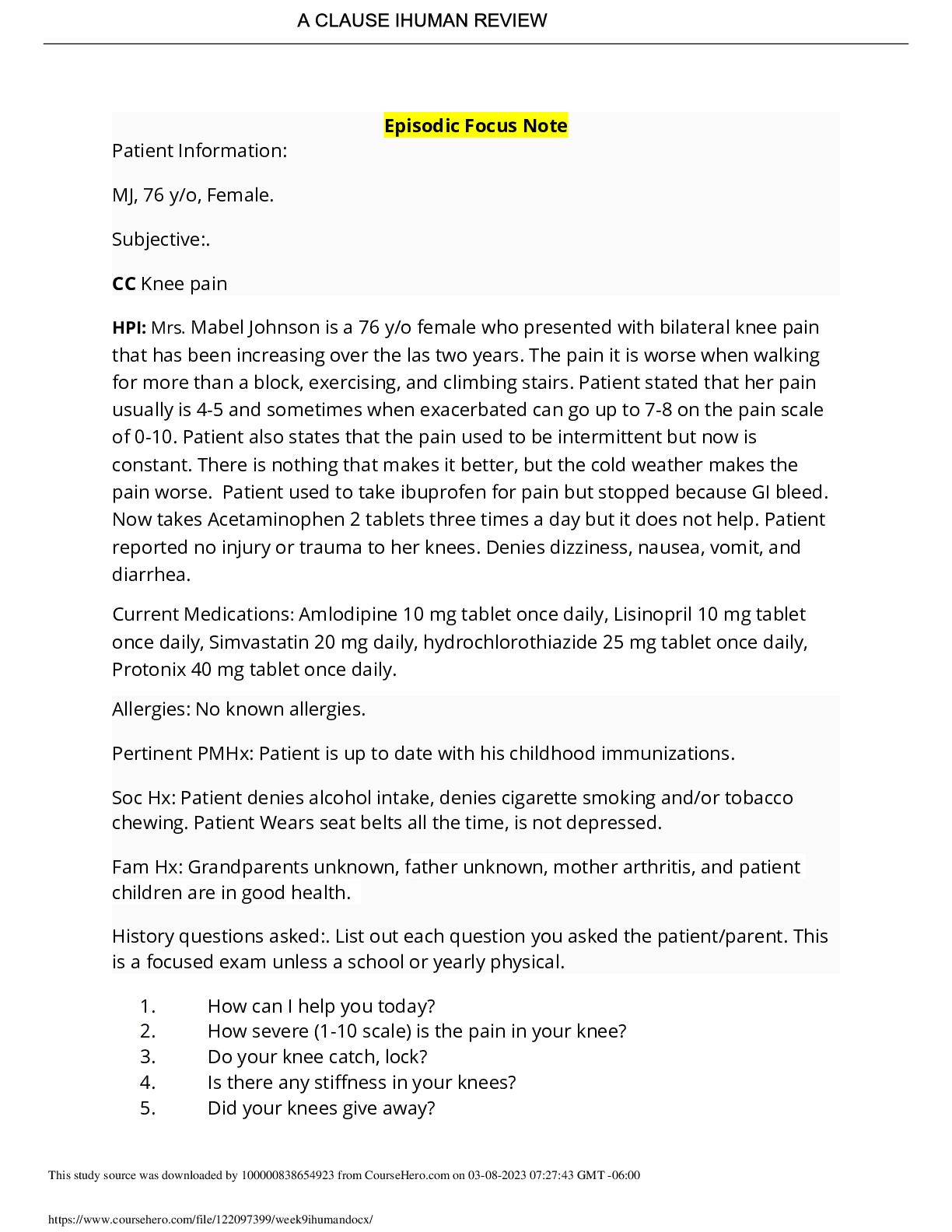
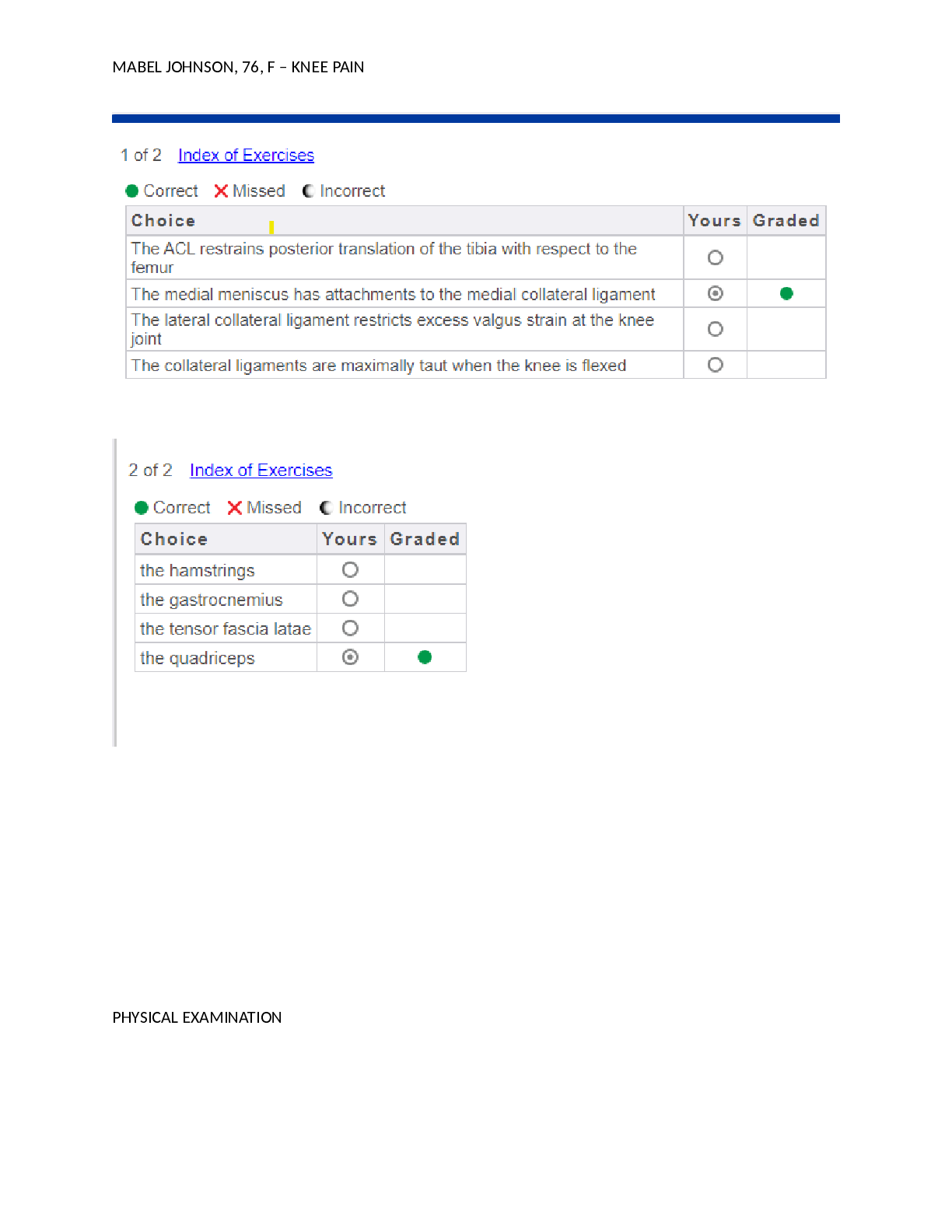
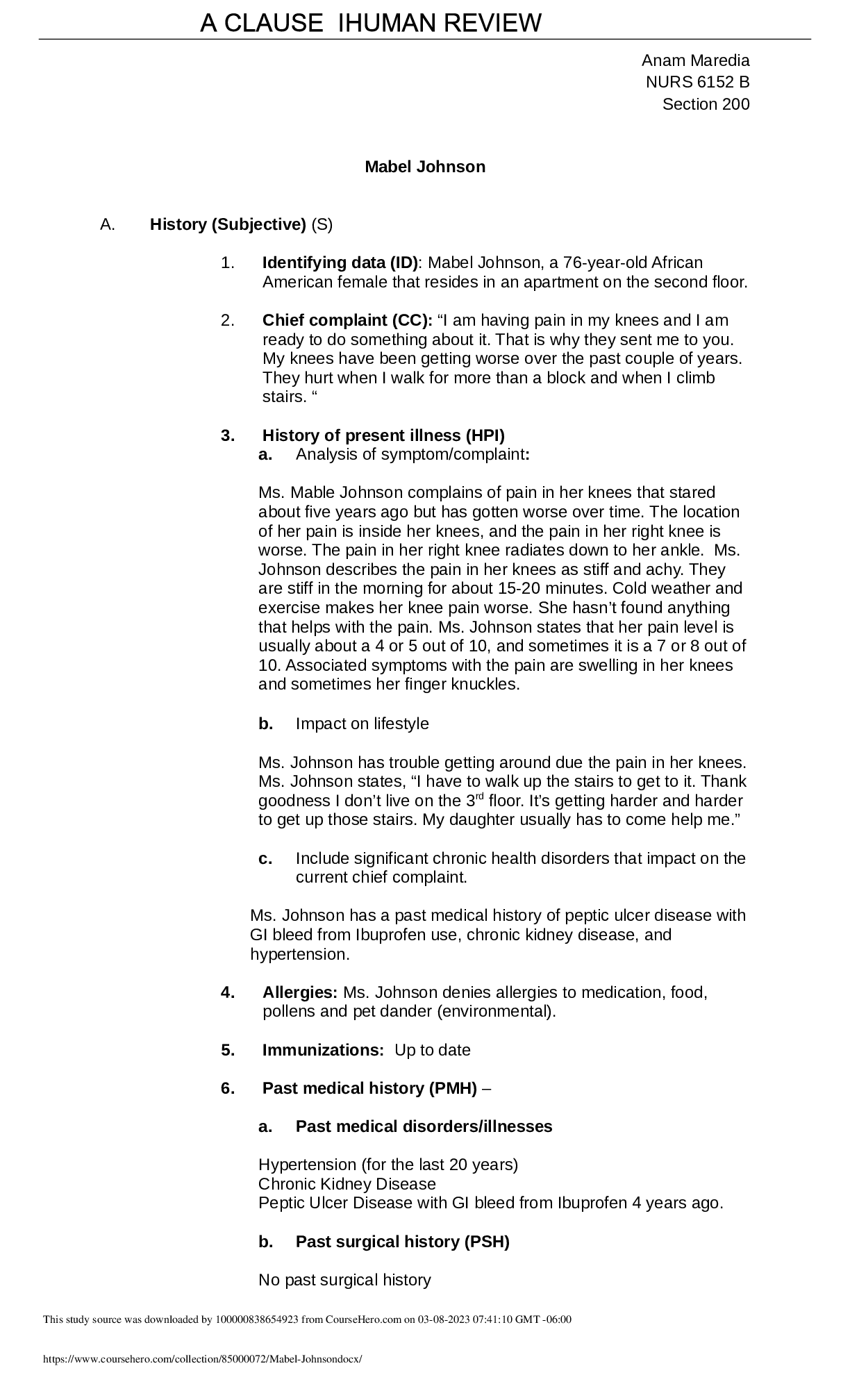
Informed Consent The patient was presented with informed consent about the psychiatric interview process and treatment. She verbally agreed and signed the informed consent to be treated. Identifyin... g Data Name: Sarah O'Neil Age: 25 years old Gender: Female Sarah, a 25-year-old female, Depression Subjective: Chief Complaint: Depression. "I've been so sad almost every day for the past month." HPI Sarah is aged 25 years and married. Her primary physician referred her to the emergency department care for a depression diagnosis after a physical examination revealed no organic explanations. Sarah came to PCP for an evaluation after her manager encouraged her to do so due to sobbing bouts at work and impaired work performance. Sarah has been sad every day for the past month and "every minute of the day" for the previous two weeks, according to her. She supports suicidal thoughts but says she would not act on them because of her family and faith. She's having paranoid thoughts and feels her coworkers are conspiring to get her fired. Sarah also claims that about six weeks ago, she went days without sleeping, attempted to write a novel, and acted in a way that was out of character for her. She went to a pub by herself, considered having an extramarital affair, almost left with a male stranger, and passed out. Sarah also claims to have gained weight recently and is dissatisfied with her appearance. Her sadness affects her employment and relationships, and her marriage is suffering. Sarah recalls a previous depressive period in high school, during which she engaged in self-harming behavior. Family history is crucial because of the mother's illness and suicide seven years ago, the father's alcoholism, and the sister's sadness. 3 Psychiatric History: None Medical History: Up-to-date immunizations. Childhood asthma. Fatigue. Obesity Social History: Married. Her spouse is kind, but her depression is straining their relationship. There have been no reports of domestic violence. There are no firearms in the house. Working in a pediatrician's office Education – Currently has an Associate's Degree and taking a Bachelor's Degree at a night school Has encountered blackouts with drinking in the past (high school) and 5 weeks ago. Drinks 1-2 alcoholic beverages per week, rarely heavy usage of alcohol. There are no tobacco use. There is no use of illegal drugs. Surgical History: Appendectomy Medications: Multivitamin and Orthotricyclen for birth control Allergies: None Family History: Father abuses alcohol but is in recovery at the moment Mother had schizophrenia and committed suicide Review of Systems Constitutional: Patient is positive for fatigue, weight changes, difficulty sleeping but denies fever and sweating at night. HEENT: Denies headache, blurred vision, difficulty swallowing, nasal congestion, sinus pain, problem hearing, and sore throat. 4 Cardiovascular: Denies chest pain, decreased exercise tolerance, palpitations, edema, cold fingers, syncope, and cold toes. Gastrointestinal: Denies vomiting, bloating, constipation, nausea, early satiety, and diarrhea Genitourinary: Denies pain, continency, changes in urination frequency, odor, dribbles, and dysuria Musculoskeletal: Denies cramps, walking limitations, discomfort when sitting, redness, joint deformities, hip and neck pain. Neurological: Denies unconsciousness, speech dysfunction, disorientation, sensory disturbances, dizziness, seizures, hallucinations, attention difficulties, tingling, numbness, concentration, and motor disturbances. Psychiatric: Positive for nervousness, anxiety, lack of interest, depression, mood changes, memory loss, difficulty, and hearing or seeing things that do not exist. Endocrine: Denies appetite change, unusual thirst, cold intolerance, frequent urination, and heat intolerance Hematologic/Lymphatic: Denies glands that are swollen, unusual bleeding, and bruising easily. Allergic/Immunologic: Denies any kind of allergies. Objective Vitals Temperature: 98.9 F (oral) Blood Pressure: 110/76 left arm while sitting Pulse: 68 bpm 5 Respiration: 14 bpm SP02: 97% Physical Exam Height: 5'3" Weight: 175 lbs. BMI: 31 General: The 25 y/o female is interactive and answers appropriately but appears to be obese. HEENT: Normal hair distribution and thickness, normocephalic, supple neck eyes PERRL with equal pupils that react to light. Neck: No lymphadenopathy and Carotids 2+ Respiratory: No wheezing or coughing. Lungs sound is clear Cardiovascular: Heart with regular S1 and S2 and rythm Abdomen: Normal, soft, and non-distended with no masses Neurologic: Intact CN I-XII grossly Musculoskeletal: Normal range of movement and symmetrical. Genitourinary: No enlarged prostate and tenderness, no testicular lump, no change in size, ulcer, and warts. Gastrointestinal: Bowel sounds are present in all [Show More]
Last updated: 6 months ago
Preview 1 out of 10 pages

Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Aug 31, 2022
Number of pages
10
Written in
Additional information
This document has been written for:
Uploaded
Aug 31, 2022
Downloads
1
Views
134



 2021.png)