*NURSING > STUDY GUIDE > NR503 FINAL EXAM STUDY GUIDE 2022 GRADED A (All)
NR503 FINAL EXAM STUDY GUIDE 2022 GRADED A
Document Content and Description Below
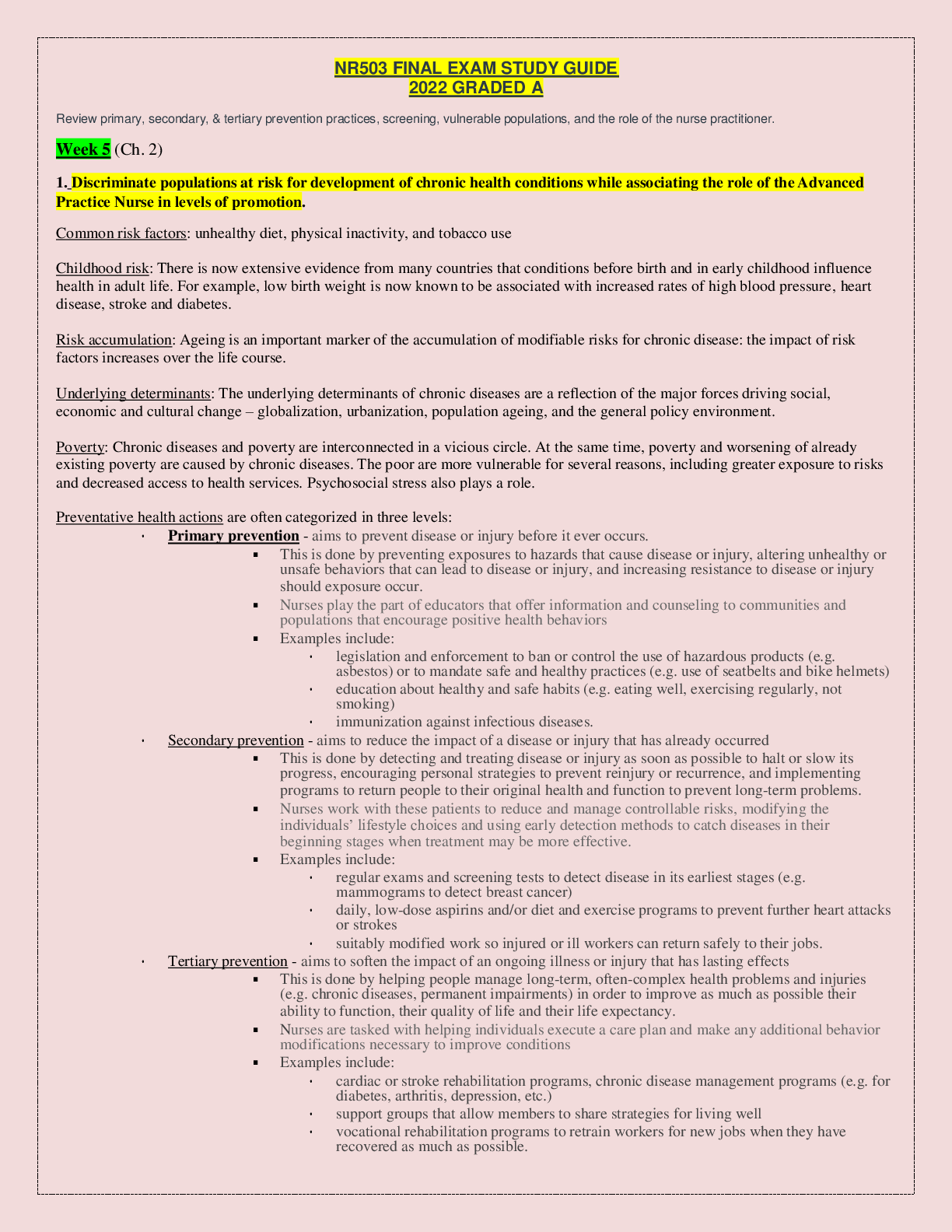
NR503 FINAL EXAM STUDY GUIDE 2022 GRADED A Review primary, secondary, & tertiary prevention practices, screening, vulnerable populations, and the role of the nurse practitioner. Week 5 (Ch. 2) 1.... Discriminate populations at risk for development of chronic health conditions while associating the role of the Advanced Practice Nurse in levels of promotion. Common risk factors: unhealthy diet, physical inactivity, and tobacco use Childhood risk: There is now extensive evidence from many countries that conditions before birth and in early childhood influence health in adult life. For example, low birth weight is now known to be associated with increased rates of high blood pressure, heart disease, stroke and diabetes. Risk accumulation: Ageing is an important marker of the accumulation of modifiable risks for chronic disease: the impact of risk factors increases over the life course. Underlying determinants: The underlying determinants of chronic diseases are a reflection of the major forces driving social, economic and cultural change – globalization, urbanization, population ageing, and the general policy environment. Poverty: Chronic diseases and poverty are interconnected in a vicious circle. At the same time, poverty and worsening of already existing poverty are caused by chronic diseases. The poor are more vulnerable for several reasons, including greater exposure to risks and decreased access to health services. Psychosocial stress also plays a role. Preventative health actions are often categorized in three levels: • Primary prevention - aims to prevent disease or injury before it ever occurs. ▪ This is done by preventing exposures to hazards that cause disease or injury, altering unhealthy or unsafe behaviors that can lead to disease or injury, and increasing resistance to disease or injury should exposure occur. ▪ Nurses play the part of educators that offer information and counseling to communities and populations that encourage positive health behaviors ▪ Examples include: • legislation and enforcement to ban or control the use of hazardous products (e.g. asbestos) or to mandate safe and healthy practices (e.g. use of seatbelts and bike helmets) • education about healthy and safe habits (e.g. eating well, exercising regularly, not smoking) • immunization against infectious diseases. • Secondary prevention - aims to reduce the impact of a disease or injury that has already occurred ▪ This is done by detecting and treating disease or injury as soon as possible to halt or slow its progress, encouraging personal strategies to prevent reinjury or recurrence, and implementing programs to return people to their original health and function to prevent long-term problems. ▪ Nurses work with these patients to reduce and manage controllable risks, modifying the individuals’ lifestyle choices and using early detection methods to catch diseases in their beginning stages when treatment may be more effective. ▪ Examples include: • regular exams and screening tests to detect disease in its earliest stages (e.g. mammograms to detect breast cancer) • daily, low-dose aspirins and/or diet and exercise programs to prevent further heart attacks or strokes • suitably modified work so injured or ill workers can return safely to their jobs. • Tertiary prevention - aims to soften the impact of an ongoing illness or injury that has lasting effects ▪ This is done by helping people manage long-term, often-complex health problems and injuries (e.g. chronic diseases, permanent impairments) in order to improve as much as possible their ability to function, their quality of life and their life expectancy. ▪ Nurses are tasked with helping individuals execute a care plan and make any additional behavior modifications necessary to improve conditions ▪ Examples include: • cardiac or stroke rehabilitation programs, chronic disease management programs (e.g. for diabetes, arthritis, depression, etc.) • support groups that allow members to share strategies for living well • vocational rehabilitation programs to retrain workers for new jobs when they have recovered as much as possible. • Members of minorities are overrepresented on the low tiers of the socioeconomic ladder. Poor economic achievement is also a common characteristic among populations at risk, such as the homeless, migrant workers, and refugees. However, the APN should be able to distinguish between cultural and socioeconomic class issues and not interpret behavior as having a cultural origin when the fact is based on socioeconomic class. A good resource for APNs is the Cross-Cultural Health Care Program (CCHCP), which has a plethora of materials to improve cultural competency among healthcare providers, including a training program for healthcare providers. In order to provide appropriate healthcare interventions, culture and all its variants must be addressed. (p28)APRNs may be able to access health information needed by working together with other sectors outside of health, such as housing, labor, education, and community-based or faith-based organizations that offer services to immigrant communities. This involves the collection, documentation, and use of data that can be used to monitor health inequalities in exposures, opportunities, and outcomes. Examples of social determinants that are related to health inequalities include poverty, educational level, racism, income, and poor housing. These inequalities can lead to poor quality of life, poor self-rated health, multiple morbidities, limited access to resources, premature death, and unnecessary risks and vulnerabilities. (p25) APRNs can best determine the effectiveness of an intervention and long-term impact by focusing on an accurate assessment and interpretation of data that are generated or collected using individual, population, and community health indicators. (p27)APRNs can work in partnership with community members to identify what community members see as relevant and important, build social capital, use outcome data to advocate for changes in policy, and then continue to work in partnership to identify strategies to intervene, monitor,and improve those outcomes (p40-41)APRNs have numerous resources they can access to improve quality and timely access to quality healthcare and decrease health disparities. The National Partnership for Action (NPA) to End Health Disparities ( minorityhealth.hhs.gov/npa) was started by the Office of Minority Health [Show More]
Last updated: 1 year ago
Preview 1 out of 26 pages
Instant download
Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Sep 06, 2022
Number of pages
26
Written in
Additional information
This document has been written for:
Uploaded
Sep 06, 2022
Downloads
0
Views
44