*NURSING > STUDY GUIDE > NURSE-UN 240 A&E I– FINAL EXAM STUDY GUIDE WEEK 7 – OXYGENATION, CIRCULATION & TISSUE PERFUSION; (All)
NURSE-UN 240 A&E I– FINAL EXAM STUDY GUIDE WEEK 7 – OXYGENATION, CIRCULATION & TISSUE PERFUSION; COPD,100% CORRECT
Document Content and Description Below
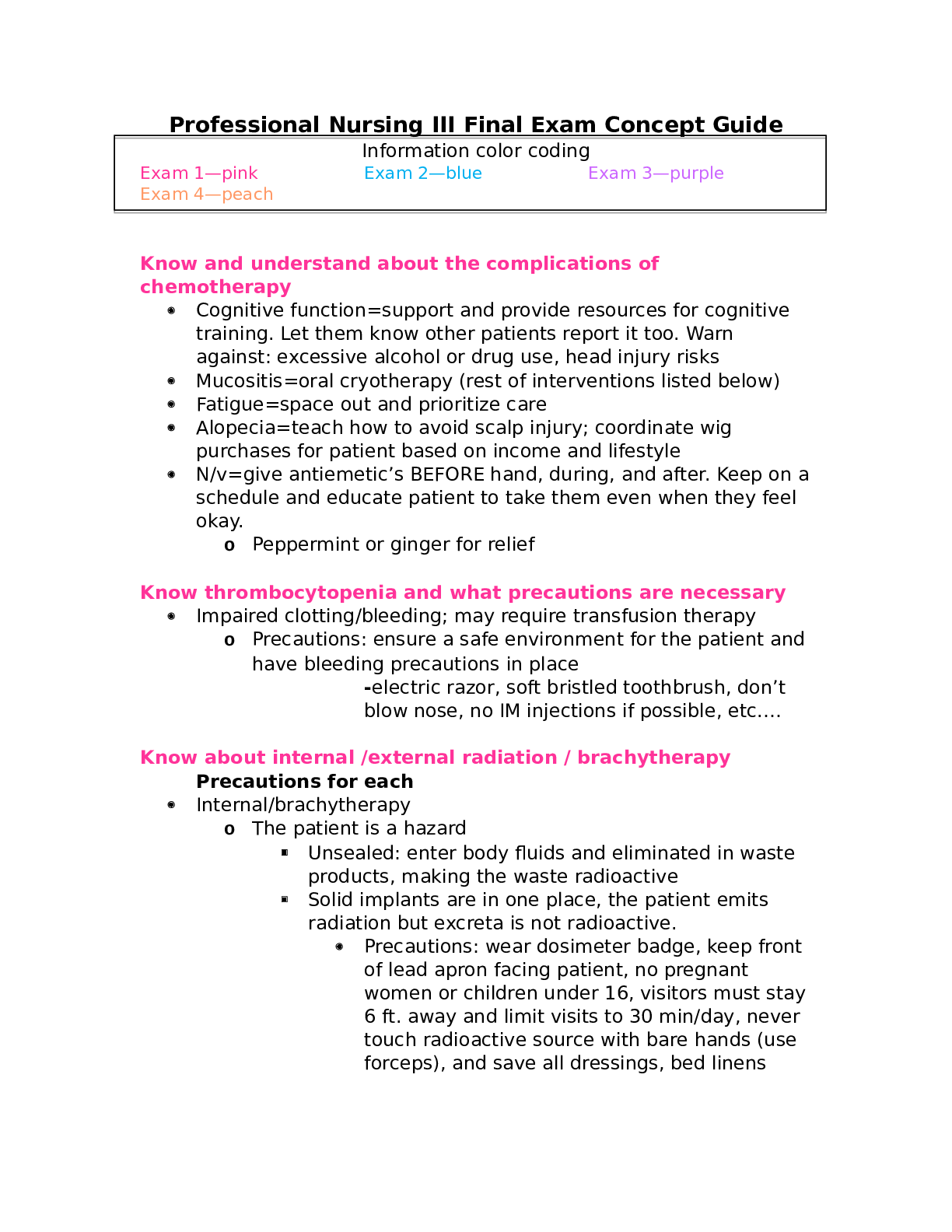
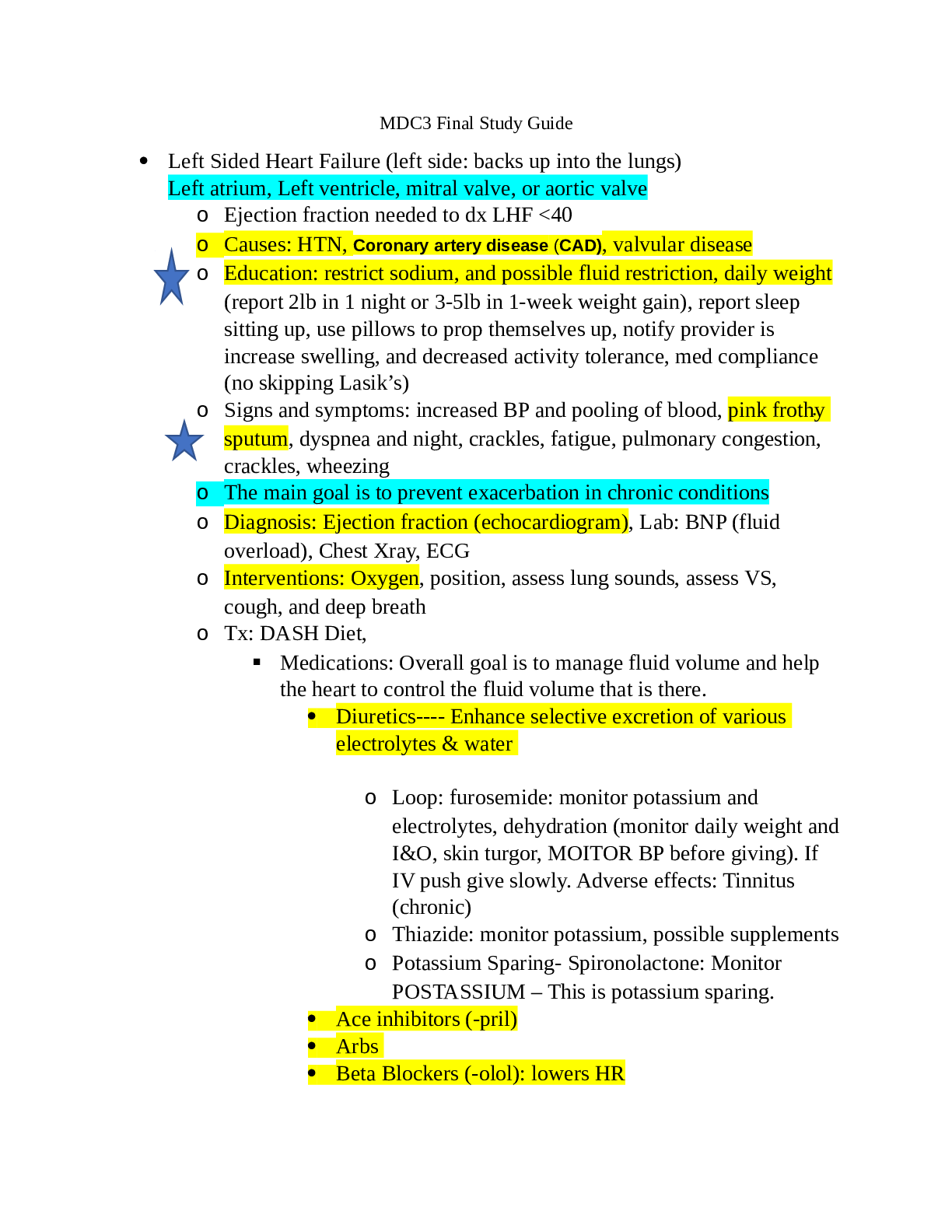
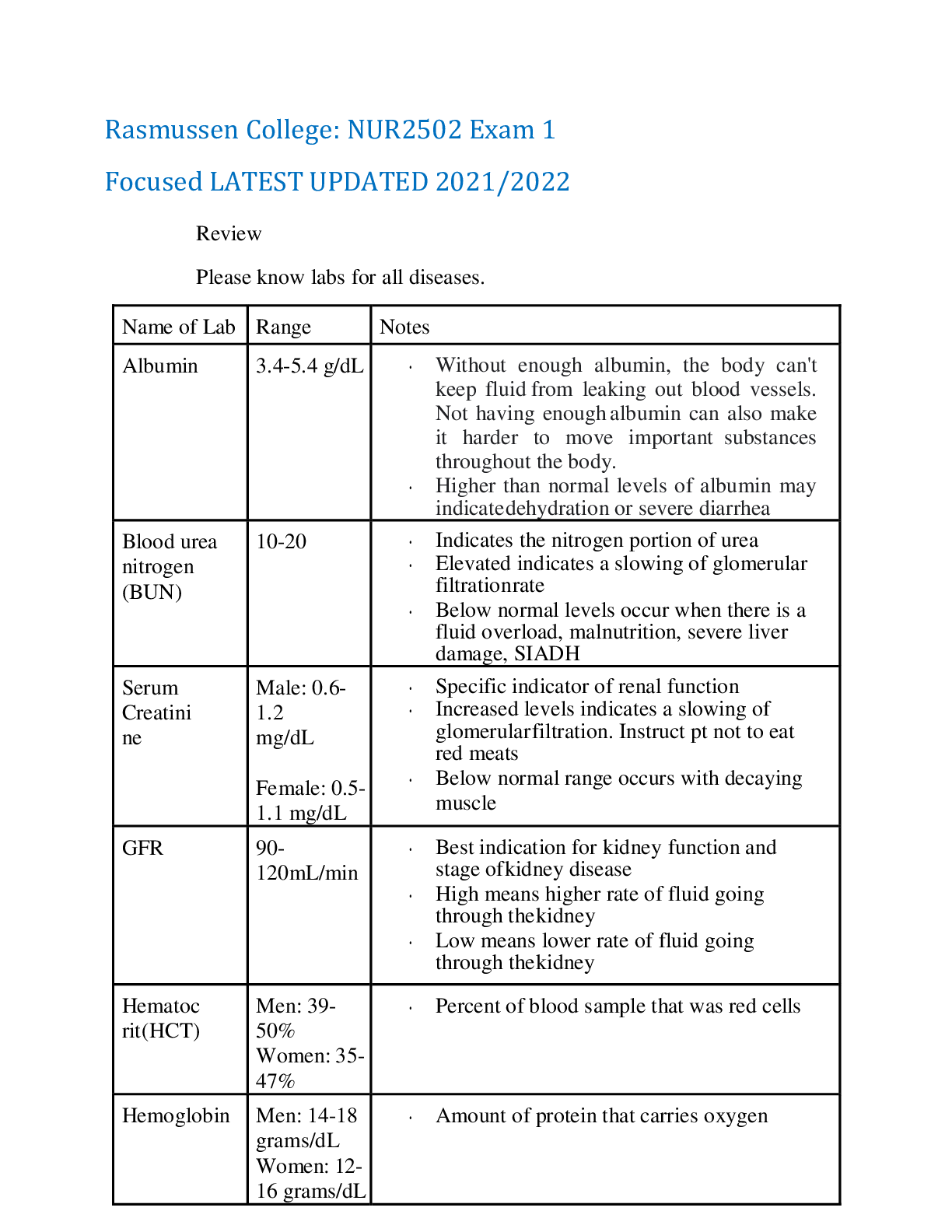
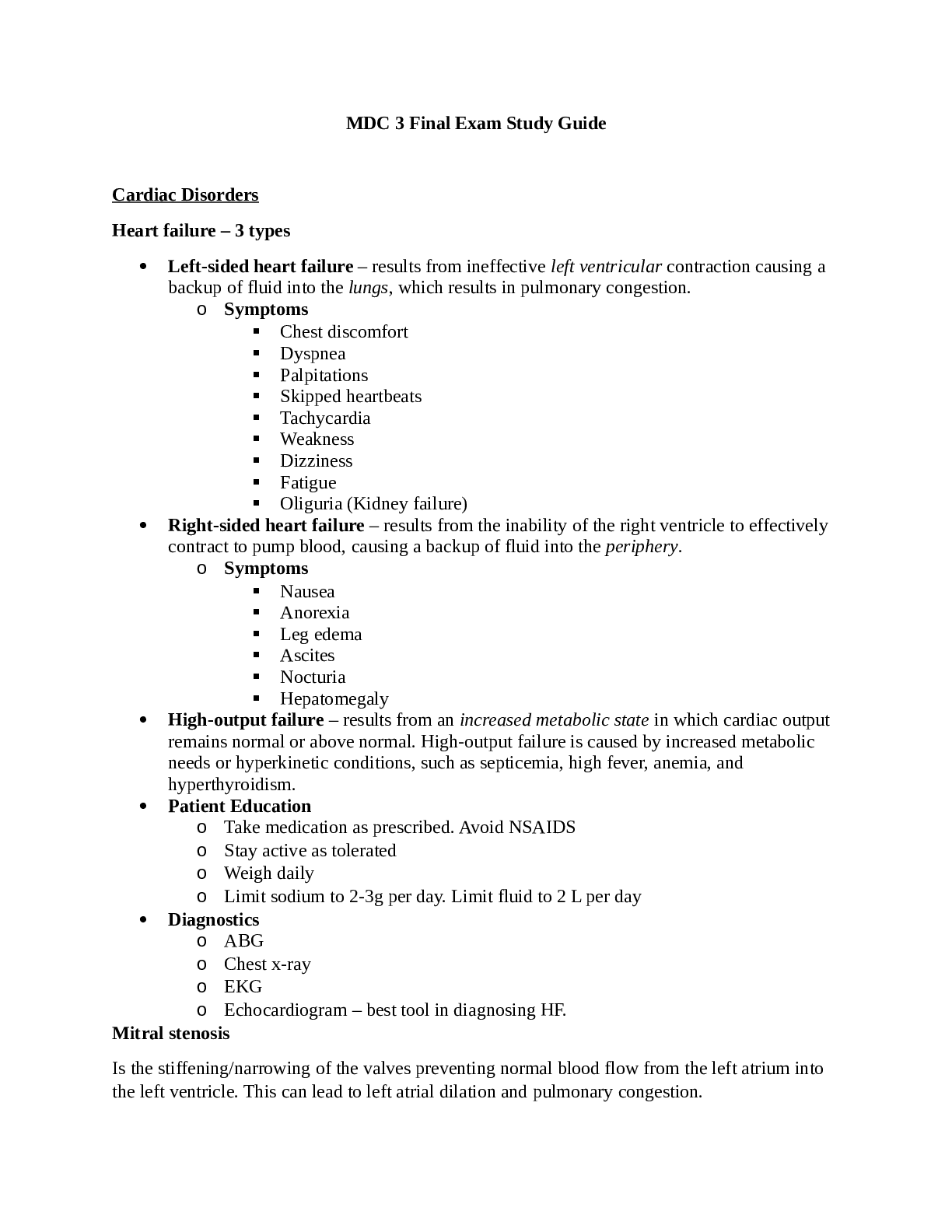
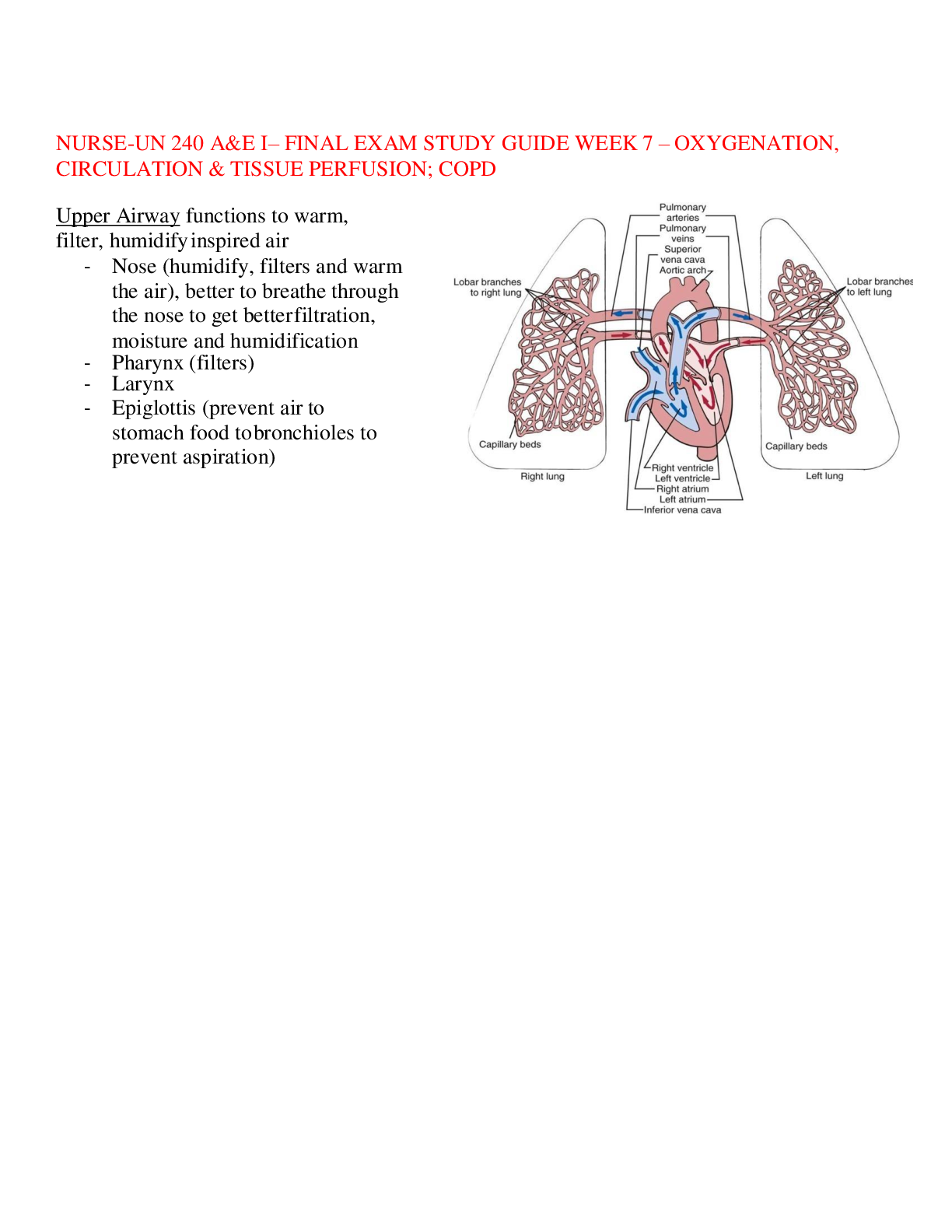
NURSE-UN 240 A&E I– FINAL EXAM STUDY GUIDE WEEK 7 – OXYGENATION, CIRCULATION & TISSUE PERFUSION; COPD Upper Airway functions to warm, filter, humidify inspired air - Nose (humidify, filters an... d warm the air), better to breathe through the nose to get better filtration, moisture and humidification - Pharynx (filters) - Larynx - Epiglottis (prevent air to stomach food to bronchioles to prevent aspiration) Lower Airway/Tracheobronchial tree functions to conduct air, mucociliary clearance and production of pulmonary surfactant - Provides air to all our 5 lobes of the lungs alveoli fill it up gas exchange - Components: trachea right and left mainstem bronchi segmental bronchi terminal bronchioles alveoli - Complication: blockages from a tumor, food and fluid or inflammation Oxygenation - Ventilation – process of moving gases into and out of the lungs o Respiratory muscles o Lung compliance & elasticity; do not expand or contract easily o Lung volume o Pulmonary circulation; no good gas exchange o Oxygen and carbon dioxide transport (not enough HGB/RBC) - Perfusion – ability of CV system to pump oxygenated blood to tissues and return deoxygenated blood to the lungs o Cardiac chambers/myocardial blood flow; arteries do not expand or contract easily atherosclerosis o Conduction system o Coronary blood flow; if none, MI o Systemic circulation; pt with DM, HTN may not get adequate flow - Diffusion – exchange of respiratory gases in the alveoli and capillaries CO = SV x HR - Cardiac output: vol of blood pumped each minute (normal ~5L/min) - Stroke vol: how much blood pumped out each beat/contraction - Heartrate: the number of beats per minute - Preload: end-diastolic pressure; the volume before you pump out - Afterload: resistance to left ventricular ejection; what you are pumping against; if HTN, you are pushing against a lot of pressure in their BV that are stretched or can be clogged Frank-Starling principle (“contractility) – illustrates relationship b/w cardiac output and L ventricular end diastolic volume (relationship b/w stroke volume and R atrial pressure) - Greater stretch = greater contraction - Pumping out the blood: the heart stretches, the more it stretches, the harder it actually pump so better to push the blood around the body (but it can only stretch so much) - Need a good preload (stretch) to get a good contractility to pump out Respiration physiology - Disorders = hyperventilation, hypoventilation, & hypoxia - Ventilation: moves gases in and out of lungs o Respiratory muscles (diaphragm**, intercostals, sternocleidomastoid) o Lung compliance and elasticity o Lung volume o Pulmonary circulation (blood exchange) o O2 and CO2 transport Cardiovascular physiology - Disorders = disturbed conduction, impaired valves, myocardial hypoxia, cardiomyopathy, peripheral tissue hypoxia - Perfusion: ability of cardiovascular system to pump oxygenated blood to tissues and return deoxygenated blood to lungs (systemic circulation) o Cardiac chambers/myocardial blood flow – blood fueling heart because it’s a muscle too o Conduction system – electrical impulses o Coronary blood flow – circulation of blood vessels of heart itself o Systemic circulation - Left sided heart failure: left ventricle supplies most of heart’s pumping power, L is oxygenated o Can lose it’s ability to contract – not enough force to send blood through body o Can lose it’s ability to relax (stiffening) – heart can’t fill between beats o Pulmonary problems (think L is from the lungs) - Right sided heart failure: right ventricle pumps out blood to go to lungs for O2, R is not oxygenated o Occurs as result of L sided heart failure o Blood backs up in veins, causes peripheral edema Balance between ventilation and perfusion - If you have just a cardio issue or just a respiratory issue, eventually one will affect another - Untreated resp issues can cause cardiac issues and vice versa Cardiac conduction system - Altered cardiac functioning o Disturbances in condition (cardiac dysrhythmias) o Altered CO (heart failure, L/R sides or both = biventricular) o Impaired valvar fxn (ex: stenosis, emptying/filling uses) o Myocardial ischemia (no O2 blood supply) ▪ Angina ▪ MI or acute coronary syndrome (ACS) ▪ MI = death of cardiac tissue, total blockage ▪ Ischemia = decrease in blood flow Conduction system via EKG - Normal sinus rhythm (NSR) o Originates at the SA node, follows normal sequence through conduction system o P wave: atrial contracting (atrium depolarization) o PR interval: conduction from atrium to ventricular o QRS complex: ventricular depolarization o QT interval: ventricular repolarization Major factors effecting oxygenation - Physiological factor o Pregnancy, PVD, cardiac disorders, COPD, CHF, HTN, DM, chronic dx o Decrease O2 carrying capacity – decreased HgB, increased in RBC destruction, blood loss, inhaling CO ▪ Ex: anemia o Decrease inspires O2 intake, narrowed airways ▪ Ex: high altitude where O2 % is lower o Hypovolemia – not enough O2 in blood due to hemorrhage, shock, dehydration o Increase metabolic rate – put body in hypermetabolic state which requires more O2 ▪ Ex: fever or hyperthyroidism - Developmental: size of lung, amount of O2 needed palsy, MS, congenital, less vital capacity, arteries get stiffer - Lifestyle: smoking, general CV health - Environmental: asbestos, occupational health, ppl in the city more exposure to pollution - Conditions affecting chest wall movement o Pregnancy and obesity – abdominal girth pushes on diaphragm o Musculoskeletal abnormalities – decreases space in thoracic cage ▪ Ex: kyphosis, scoliosis, lordosis (sway in) o Trauma (gunshot wound causes change in pressure) o CNS/neuromuscular disease – can cause hypercapnia and hypoxemia ▪ Guillain Barre – causes ascending muscle weakness (diaphragm = muscle) - Altered respiratory function o Hyperventilation – fast and deep, increased removal of CO2 threatens acid base balance o Hypoventilation – not taking in O2, slow and shallow ▪ Pneumonia, changes in mental status, etc. o Hypoxia – decreased oxygen in tissues ▪ 1st sign is change in mental status and associated cyanosis ▪ Early sign: shows fast breathing to get more O2 in (tachypnea) ▪ Late sign: breathing slows due to fatigue (bradypnea) ▪ Central: buccal mucosa change ▪ Peripheral: extremities change o Hypoxemia – decreased oxygen in arterial blood Assessment of oxygenation - Hx focus: explore factors or conditions associated with impaired oxygenation (smoking, any CV dx) - Physical assessment: level of consciousness, general appearance, breathing pattern (tachypnea, bradypnea), etc. o Auscultate for lung and heart sounds; PNA – crackles, COPD – ronchi, asthma – wheezing o Assesses capillary refill, edema (aka fluid in interstitial tissues no fluid back into the heart no preload heart doesn’t stretch no good contractility no good CO), JVD - In-depth history of a patient’s normal and present cardiopulmonary fxns - Past impairments in circulatory or respiratory functioning - Methods that pt uses to optimize oxygenation (masks, tubing, tank, where they got it and how they use it) - Review of drug, food and other allergies (hypersensitivity issues) - Physical examination - Labs and diagnostic test Ventilation and oxygenation diagnostic studies - X-rays – one dimensional view, can show cardiomegaly HF, consolidation, pulmonary edema - Blood tests: CBC/hemogram, cardiac enzymes (diagnose acute MI), serum electrolytes (especially for diuretic), cholesterol (increase risk cardiac disease) - Bronchoscopy: visual exam of airways - Lung CT scan (gold standard): can ID abnormal masses - O2 saturation - Thoracentesis: use needle to chest wall to aspirate fluid - TB tests (PPD and QuantiFERON) - Sputum tests: used for culture and sensitivity, can ID lung cancer, for active infection - Cardiac tests: EKG, echo and stress test Complete blood count - Normal values vary with age and gender - Determines # and type of red and white cells per mm3 - Measures RBC count, volume of red and white cells - Concentration of hemoglobin (reflects patient capacity to carry o2) Normal values - HgB o Male – 13.5 – 16.5 g/dL o Female – 12-15 g/dL - Hct: % of RBC in the blood o Male – 41-50% o Female – 36-44% - RBC (4.5 – 5.5 x 10^6 cells/mL) - WBC o 4,500-11,000/mm3 Cardiac enzymes: cells break down and release enzymes - Cardiac troponins o Plasma cardiac troponin 1 <0.03ng/mL **results faster ▪ Evaluate 3 hours after myocardial injury ▪ Values remain elevated 7-10 days o Plasma cardiac troponin T <0.1ng/mL ▪ Values remain elevated for 10-14 days - Creatine Kinase (CK): CK with 50% increase between 2 samples 3-6 hours apart, peaking 12-24 hours after chest pain, or a single CK elevation (twofold) diagnosis acute MI - Myoglobin: not specific because it’s related to ALL muscles, not just heart o <90 mcg/L o Early sign of damage to myocardium (no O2, wasn’t perfused cell death) in MI or reinfarction o Values increase within 3 hours Serum electrolytes: - Potassium: 3.5-5 mEq/L o Patients on diuretics = at risk for hypokalemia (and hyponatremia) because diuretics excrete K and Na unless potassium sparing o Patients on ACE inhibitors (opposite of aldosterone) and anti-HTN meds = at risk for hyperkalemia Cholesterol: normal levels - Fasting < 200 mg/dL - LDLs (bad) < 100 mg/dL - VLDLs 7-32 mg/dL - HDL (good) o Male >40 mg/dL o Female >50 mg/dL - Triglycerides < 160 mg/dL Possible nursing diagnoses: activity intolerance, impaired gas exchange, risk for aspiration, decreased cardiac output, impaired verbal communication, ineffective breathing pattern, fatigue, ineffective airway clearance, ineffective health maintenance Nursing interventions/implementation - Ambulation (good for everything!) - Suction - Chest PT - Artificial airway - Oxygenation - Positioning for lung expansion to reduce pulmonary stasis, reduce pressure on diaphragm, and maintain ventilation & oxygenation - Incentive spirometry to encourage voluntary deep breathing Maintenance of Promotion of Oxygenation - O2 therapy to prevent or relieve hypoxia - Safety precautions - Supply of oxygen (tanks or wall-piped system) - Methods of O2 delivery (nasal cannula, O2 mask) Home Oxygen Systems: needs to be properly taught (general education and safety) - Indications – PaO2 of 55 mmHg or less OR SaO2 of 88% or less on RA at rest, on exertion, or w/ exercise - Administered via nasal cannula or face mask - T tube or tracheostomy collar used it pt has permeant tracheostomy - Beneficial effects for pt w/ chronic cardiopulmonary dz Administering Inhaled Medications - Bronchodilators: open narrowed airways - Nebulizers: disperse fine particles of liquid medication into deeper passages of the respiratory tract thru a mask - Meter-dose inhalers: deliver a controlled dose of medication with each compression of the canister - Dry powder inhalers: breath-activated delivery of medications Types of artificial airways due to hypoxia - Oropharyngeal and nasopharyngeal airway (temporary to stick thru nasopharyngeal airway) - Endotracheal tube (short term, mechanically ventilated, during surgery) - Tracheostomy tube (long term) Bronchoscopy - Common diagnostic procedure, can see growth and tumors - Patient prep: nurse’s responsibility to explain procedure, verify informed consent has been obtained by MD and make sure signature is from pt, check NPO status 4-8 hrs before procedure, give sedatives/anti-anxiety PRN, check blood work results - During procedure: monitor vitals, maintain IV access - Follow-up care: monitor vitals for complications, bleeding, hypoxemia, injuries, punctures, check for damaged teeth and vocal cords Thoracentesis: access interpleural space to get specimen - Use for analysis/receive pleural effusion - Make sure patient has proper position for procedure (tripod!) - Make sure MD got consent - Monitor vials during and after and for potential complications (possible pneumothorax from sticking needle into the lungs) - Chest x ray after procedure – important to see lung puncture - Auscultate breath sounds - Check puncture site for bleeding and leakage - Document procedure Interpreting PPD: look for induration, not redness - Considered POSITIVE if… o It’s 15mm o It’s 10mm AND you’re an immigrant, injection drug users, residents and employees of high-risk settings, children less than 4 years of age, infants, and adolescents, exposure to high-risk results o It’s 5mm or more AND you have HIV/AIDS, have had organ transplants or have depressed immune system - BCG vaccine (protects from TB, given in other countries) will show a positive reaction Vaccinations - Flu and pneumococcal - Influenza vaccine administered annually (to prevent further complication like COPD) based on CDC surveillance data - Live, attenuated nasal spray flu vax not for older adults - Pneumococcal advised q5 yr for those >65 if advised by HCP esp for those living in long term care institutions Evaluation - Ask about: o Degree of breathlessness o If distance ambulated w/o fatigue has increased o Rating breathlessness from 0 to 10 o Which interventions reduce dyspnea o Frequency of cough and sputum production - Perform o Observe RR before, during and after any activity o Assess any sputum produced o Auscultate lung sounds for improvement in adventitious sounds COPD - Chronic obstructive pulmonary disease (COPD – refers to chronic lung disorders that result in blocked airflow in the lungs, and thus retention of CO2. The two main COPD disorders are emphysema and chronic bronchitis. Although these are separate disorders with different pathologic processes, many patients with emphysema also have chronic bronchitis at the same time. - Usually damage is permanent and irreversible o Emphysema – ALVEOLAR PROBLEM – Loss of lung elasticity and abnormal permanent enlargement of the air space distal to the terminal bronchioles result in dyspnea and the need for an increased respiratory rate. ▪ Loss of recoil in alveolar walls results in hyperinflation of the lungs, which flattens the diaphragm. As a result, the patient needs to use accessory muscles in the neck, chest wall, and abdomen to inhale and exhale. This increased effort increases the need for oxygen. ▪ Gas exchange is affected by the increased work of breathing and the loss of alveolar tissue. Although some alveoli enlarge, the curve of alveolar walls decrease and less surface area is available for gas exchange. ▪ Carbon dioxide is produced faster than it can be eliminated, resulting in carbon dioxide retention and chronic respiratory acidosis. ▪ The patient with late-stage emphysema also has a low arterial oxygen level because it is difficult for oxygen to move from diseased alveoli into the blood. o Chronic bronchitis – AIRWAY PROBLEM – Chronic inflammation of the bronchi and the bronchioles caused by exposure to irritants, causing vasodilation, congestion, mucosal edema, congestion, and bronchospasm. ▪ Chronic inflammation increases the number and size of mucus glands, which produce large amounts of thick mucus. The bronchial walls thicken and impair airflow. This thickening, along with excessive mucus, blocks some of the smaller airways and narrows larger ones. ▪ Mucus provides a breeding ground for organisms and leads to chronic infection. ▪ Narrowed airways result in decreased oxygen levels, increased arterial carbon dioxide levels, and respiratory acidosis. - Cigarette smoking is the greatest risk factor for COPD o Consequences due to increase in proteases (protective enzymes in the lungs): ▪ Decreased ciliary activity (for airflow and dust removal) ▪ Possible loss of ciliated cells (metaplasia) ▪ Cellular hyperplasia (decreased width of bronchiole) ▪ Production of mucus ▪ Reduction in airway diameter ▪ Increased difficulty in clearing secretions o Nicotine – acts as a stimulate to the sympathetic nervous system increased HR, peripheral vasoconstriction, increased BP and cardiac workload - Alpha1-antitrypsin deficiency is a less common but important risk factor for COPD. o AAT is normally present in the lungs and inhibits excessive protease activity so that the proteases only break down inhaled pollutants and do not damage lung structures. o The production of normal amounts of AAT depends on the inheritance of a pair of normal gene alleles for this protein. The AAT gene is recessive. - The prevalence of chronic bronchitis and emphysema in the United States has been estimated at about 15.8 million. COPD is the fourth leading cause of morbidity and mortality in the United States. Assessment - History – risk factors include age, gender, occupational history, family history - Physical assessment – abnormal breath sounds (wheezes, crackles or ronchi), barrel chest, clubbing, cyanosis – late sign, dyspnea, use of accessory muscles, tripod position, unplanned wt loss - Diagnostic tests o CXR – not useful in early or moderate dz, used to r/o other pulmonary conditions o Patient presentation – productive cough lasting for at least 3 months in a year for at least 2 consecutive years chronic bronchitis - Emphysema – pink puffers - Chronic bronchitis – blue bloaters - Labs including: o ABG: respiratory acidosis (pH < 7.35, HCO - >26 mEq/L), hypoxia (PaO < 80 mmHg), hypercapnia (PaCo2 > 45 mmHg) ▪ Normal ranges: pH 7.35-7.45, CO2 35-45 mmHg, HCO3 22-26 mEq/L ▪ COPD pt usually have chronic respiratory acidosis r/t hypercarbia or hypercapnia o CBC: polycythemia, elevated WBC o Alpha-1 antitrypsin deficiency (genetic cause of emphysema) – deficiency indicates inability to inhibit excess proteases o Sputum analysis – for hospitalized pt w/ acute respiratory infection o Decreased oxygen saturation – know pt’s baseline, usually lower than 90% o Pulmonary function tests are also used to diagnose COPD, particularly FEV1. ▪ Spirometry is a method of assessing lung function by measuring the total vol of air the patient can hold and expel from the lungs after a max inhalation ▪ Spirometry readings in patients with COPD show: • Reduced FEV1/FVC (ratio of <0.7-0.8, suggestive of obstructive lung dz): the fraction of air exhaled in the first second relative to the total volume exhaled • Increased RV (residual vol) • As the disease progresses, the ratio of FEV1 to FVC becomes smaller as FEV1 decreases and FVC increases. COPD Complications - Hypoxemia & acidosis - Respiratory infections – can be life threatening - Cor pulmonale (right sided heart failure) is a late-stage complication of COPD. o Pathophysiology: Air trapping, airway collapse, and stiff alveolar walls increase the lung tissue pressure and narrow lung blood vessels, making blood flow more difficult increased pressure creates a heavy workload on the right side of the heart, which pumps blood into the lungs in response to heavy pressures, right ventricular hypertrophy occurs and leads to fatigue, increasing dyspnea, distended jugular veins, peripheral edema, and an enlarged and tender liver. o Clinical manifestations: increased dyspnea, fatigue, distended neck veins, dependent edema, enlarged and tender liver - Cardiac dysrhythmias COPD: Priority Nursing Diagnosis - Hypoxemia with hypercapnia r/t alveolar-capillary membrane changes, reduced airway size, ventilatory muscle fatigue, excessive mucus production, airway obstruction, diaphragm flattening, fatigue and decreased energy - Wt loss r/t dyspnea, excessive secretions, anorexia and fatigue - Anxiety r/t dyspnea, a change in health status and situational crisis - Activity intolerance r/t fatigue, dyspnea and an imbalance between oxygen supply and demand - Risk for infection MANAGEMENT Drug Therapy - Drugs used to manage COPD include bronchodilators (e.g albuterol), anti-inflammatories/steroids (e.g. Pulicort), and combination inhalers (e.g. Combivent which is albuterol & Atrovent; Advair diskus which is albuterol & steroids) o Bronchodilators decrease airway resistance and hyperinflation, reduces dyspnea Oxygen Therapy - Low flow O2 therapy (2-4 L/min via nasal cannula or up to 40% via Venturi mask) is used to treat hypoxemia o Important to restrict oxygen delivery because COPD patients have a hypoxic drive (due to chronic hypercapnia desensitizing chemoreceptors) o Goal: to bring SpO2 levels up between 88-92% (and PaO2 to 60-65%). o Humidification also commonly used - Chronic O2 therapy at home – improves prognosis, neuropsychologic fxn, exercise tolerance; reduces pulmonary HTN Collaborative Care - Placing the patient in an upright position with the head of the bed elevated can help alleviate dyspnea by increasing chest expansion and keeping the diaphragm in the proper position to contract. This position conserves energy by supporting the patient’s arms and upper body. - Breathing techniques such as diaphragmatic breathing (to achieve maximum inhalation and slow RR) and pursed-lip breathing (prolongs exhalation). - Controlled coughing is helpful in removing excessive mucus. - Exercise for conditioning and pulmonary rehabilitation can improve function and endurance in patients with COPD, especially swimming; encourage pt to remain as active as possible even if O2 is needed - Maintaining hydration (fluid intake of at least 2 L/day) may thin the thick, tenacious (sticky) secretions, making them easier to remove by coughing. - Patient should eat 5-6 small meals to avoid feeling bloated. Avoid a high carbohydrate diet to prevent an increased CO2 load. - Prevent respiratory infections – teach pt to avoid large crowds & importance of immunizations (flu & pna) - Smoking cessation o Accelerated decline in pulmonary function slows and function usually improves o Most significant factor in slowing progression of dz!! - Lung reduction surgery in patients with emphysema removes hyperinflated lung tissues that are filled with stagnant air containing little, if any, oxygen. Successful lung reduction results in increased FEV and decreased total lung capacity and RV. [Show More]
Last updated: 1 year ago
Preview 1 out of 19 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
We Accept:

Reviews( 0 )
$14.00
Document information
Connected school, study & course
About the document
Uploaded On
Nov 12, 2022
Number of pages
19
Written in
Additional information
This document has been written for:
Uploaded
Nov 12, 2022
Downloads
0
Views
48