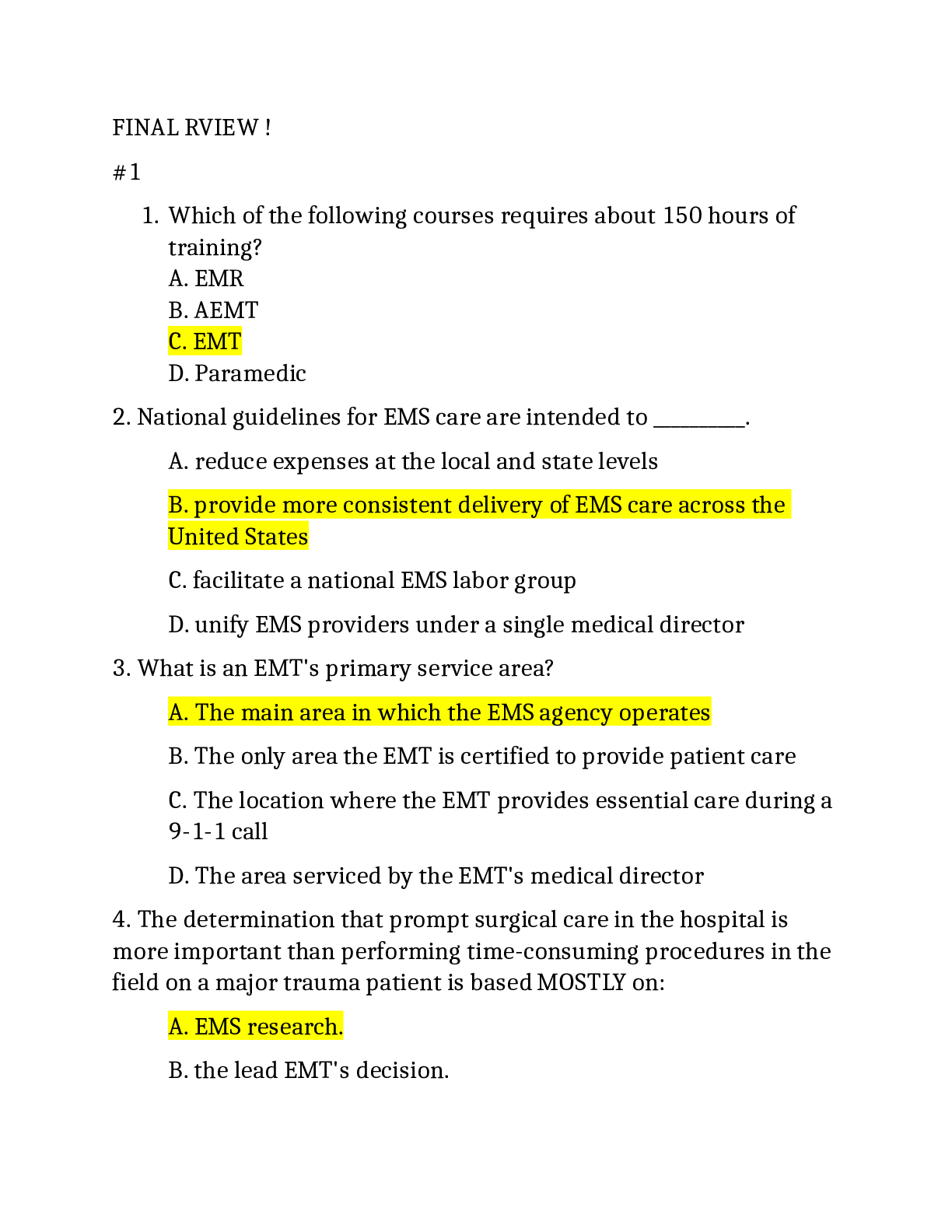
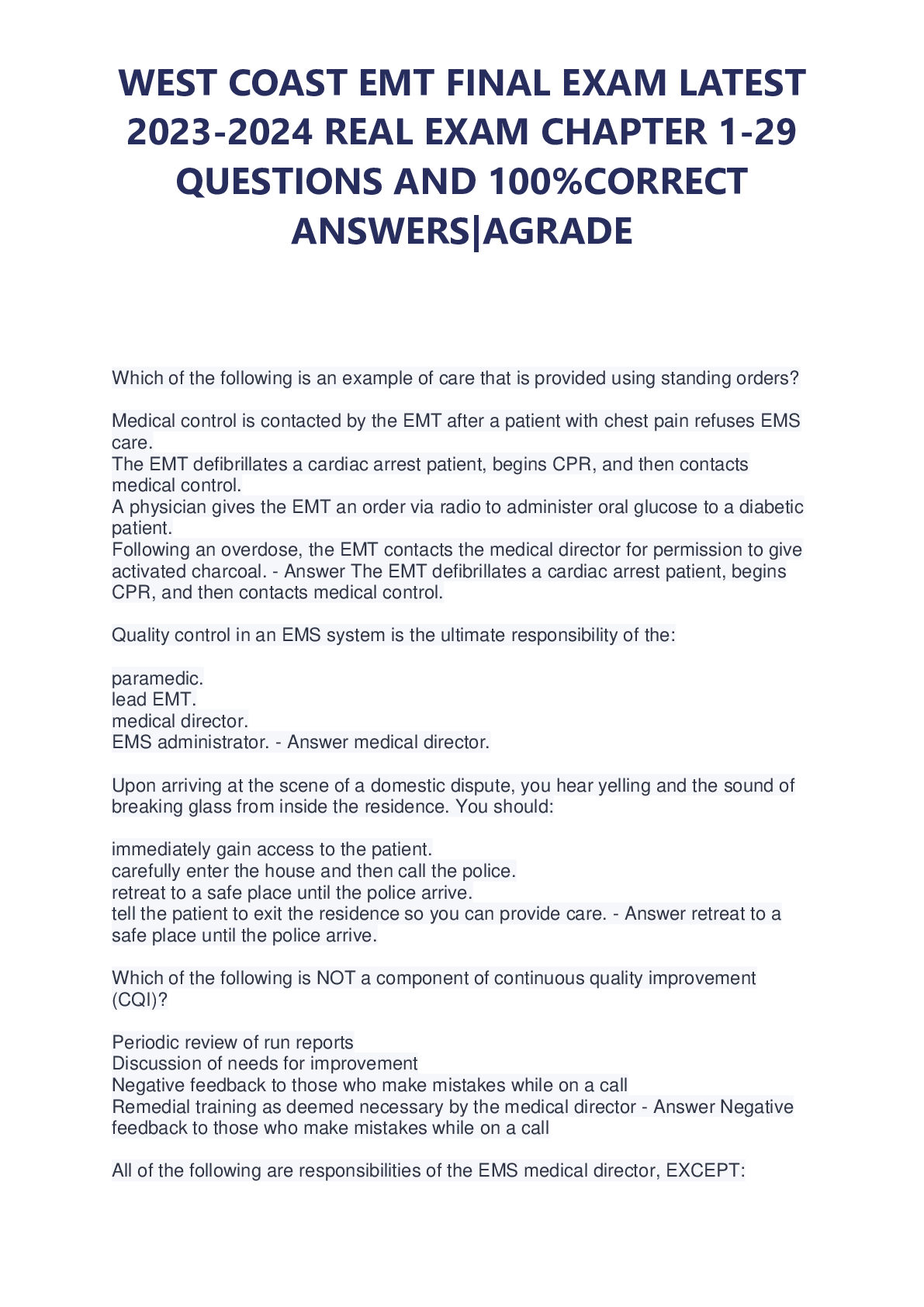
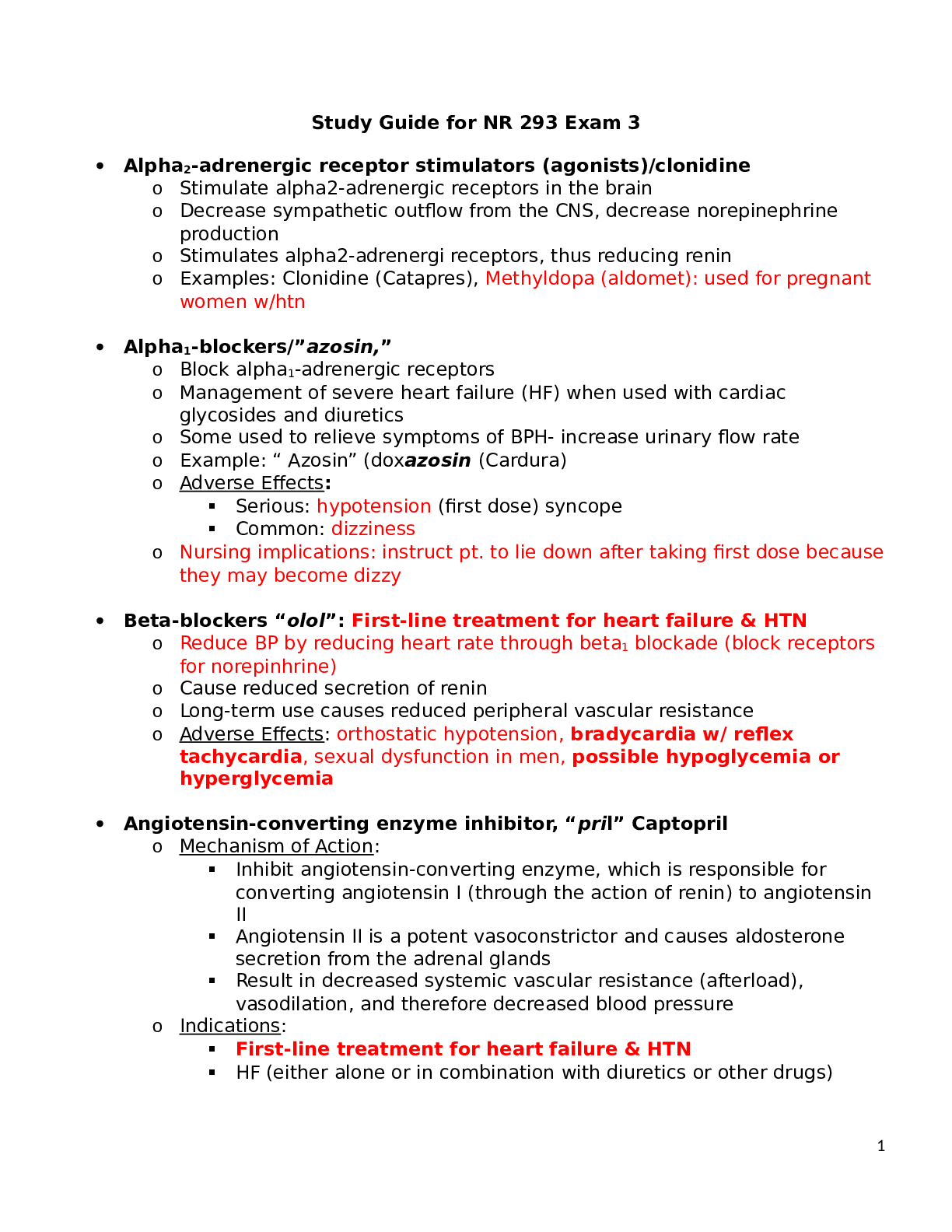
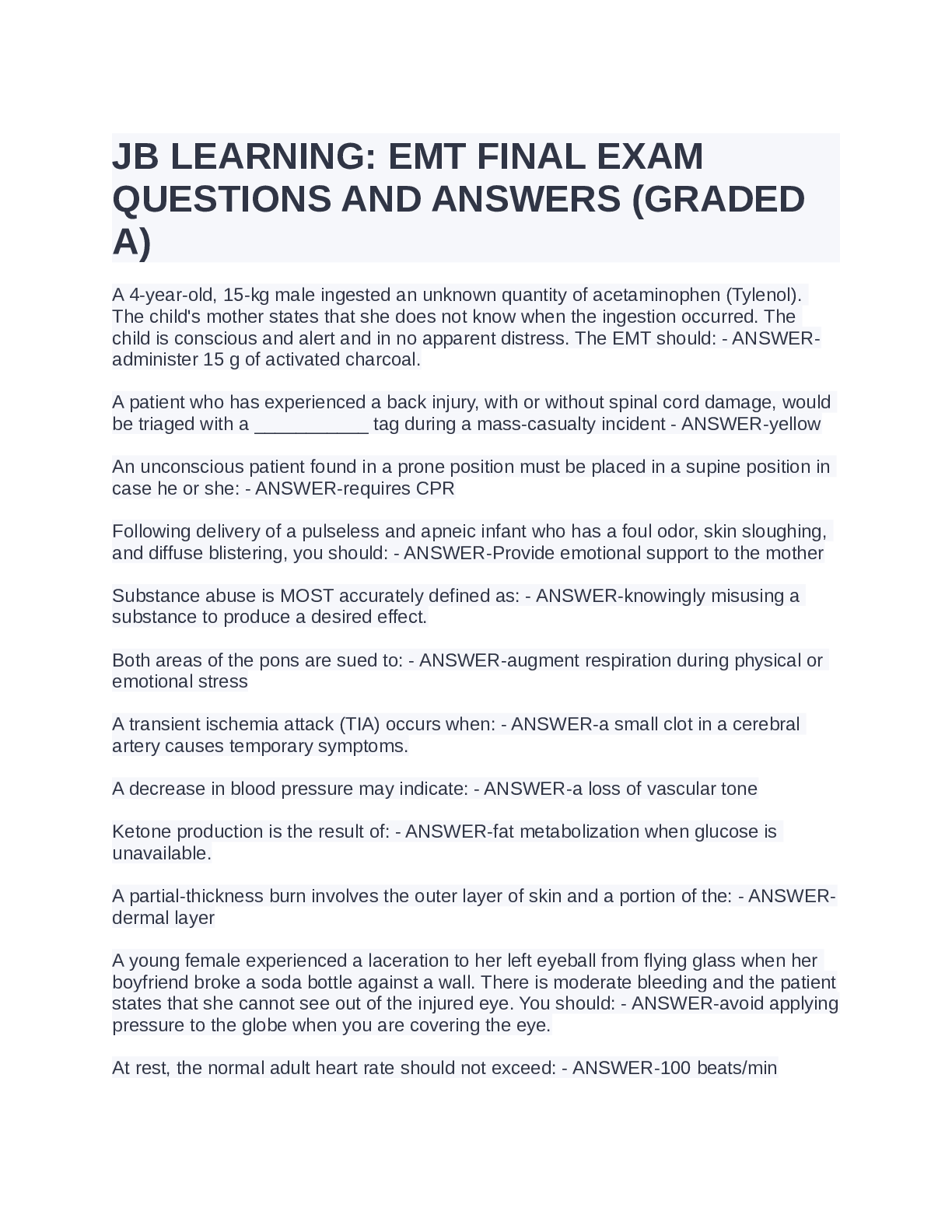
*NURSING > EXAM REVIEW > NURSE-UN 001 STUDY GUIDE FOR EMT Final Exam Review_Melissa Perkowski,100% CORRECT (All)
NURSE-UN 001 STUDY GUIDE FOR EMT Final Exam Review_Melissa Perkowski,100% CORRECT
Document Content and Description Below
NURSE-UN 001 STUDY GUIDE FOR EMT Final Exam Review_Melissa Perkowski 1. Review types of consent (implied, expressed, etc) o Consent ➔ is generally required from every conscious adult before ca... re can be started. The foundation of consent is decision-making capacity. o Implied consent ➔ legal assumption that treatment was desired. ▪ Applies to patients who are unconscious or are otherwise incapable of making a rational, informed decision about care. It applies only when a serious medical condition exists and should never be used unless there is a threat to life or limb. ▪ The principle of implied consent is known as the emergency doctrine. ▪ Sometimes what represents a “serious threat” is unclear, and it may become a legal question. o Expressed consent ➔ patient gives express authorization for provision of care or transport. The patient acknowledges he or she wants you to provide care or transport. ▪ To be valid, the patient must provide informed consent, which means you have explained the treatment being offered, along with the potential risks, benefits, and alternatives, as well as the potential consequences of refusing treatment. Informed consent is valid if given orally. Always document when a patient provides informed consent, or have someone witness the patient’s consent. o Involuntary consent ➔ Applies to patients who are mentally ill, in a behavioral (psychological) crisis, are developmentally delayed. ▪ You should obtain consent from the guardian or conservator; however, it is not always possible to obtain such consent, so understand your local provisions (sometimes need a law enforcement authority to be present to take person to medical facility) 2. Review what your actions should be if you come across an MVC as an EMT on duty and off duty o If you are off duty and come upon a crash, you are not legally obligated to stop and assist patients. 3. Recall the functions of the National Registry, AHA, DOT, Trauma centers, Local EMS offices, State EMS offices o National Registry of Emergency Medical Technicians (NREMT) ➔ is a nongovernmental agency that provides national standardized EMS testing and certification in much of the United States. May states use the National Registry standards in certifying their EMTs and grant licensing reciprocity to NREMT-certified EMTs ▪ EMS is regulated ENTIRELY by the state in which you are licensed o American Heart Association (AHA) ➔Every 3 to 5 years, the AHA unveils a revised set of guidelines based on large amounts of evidence and serves as a standard for basic life support (BLS) and cardiopulmonary resuscitation (CPR). o Department of Transportation (DOT) ➔ DOT published the first EMT training curriculum in the early 1970s. In the late 1970s, the DOT developed a recommended National Standard Curriculum. o Trauma Centers ➔ Trauma centers are categorized as either adult trauma centers or pediatric trauma centers, but not necessarily both. The goal of a trauma system is to get the right patient to the right facility in the right amount of time. ▪ Trauma patients with shock, or a suspicious MOI, generally should go to a trauma center. ▪ Trauma centers are classified from levels I III, with level I being able to handle every trauma. o Local EMS offices ➔At the local level, each EMS service operates in a designated PSA in which it’s responsible for the provision of prehospital emergency care and the transportation of the sick and injured to the hospital. The medical director decides day-to-day limits of EMS personnel. Examples include the medications that will be carried on an ambulance or where patients are transported. o State office of EMS➔ is the standards for prehospital emergency care and the individuals who provide it are typically regulated by the state office of EMS ▪ EMT training in nearly every state meets or exceeds the guidelines recommended by the National Highway Traffic Safety Administration (NHTSA) 4. Review types of medical direction, and know situations that would dictate the use of each type o Medical direction ➔ a physician medical director authorizes EMTs to provide medical care in the field. Appropriate care is described in standing orders and protocols. ▪ Medical control can be off-line or online. ➢ Off-line (indirect) - Standing orders, training, supervision ➢ Online (direct) - Physician directions given over the phone or radio 5. Review the components of an EMS system o There are 14 components of the EMS system o The EMS Agenda for the Future outlines 14 components of an EMS system ▪ Public access ➔ easy access to help in an emergency is essential. The 9-1-1 system is the public safety access point. At the communication center, trained dispatchers obtain information and dispatch the ambulance crew and other equipment and responders. An emergency medical dispatch (EMD) system has been developed to assist dispatchers in providing callers with vital medical instructions until EMS arrival. ▪ Communication systems ➔ From caller information, the dispatcher selects the appropriate parts of the emergency system to activate. EMS may be: part of the fire department, part of the police department, Independent (either public or private). New technology helps responders locate their patients for example cellular telephones linked to global positioning system (GPS) units. ▪ Clinical care ➔ Describes the pieces of equipment, scope of practice for using that equipment and familiarizes EMTs with their primary service area (PSA), or main area in which an agency operates. Overall, it familiarizes EMTs with ambulance controls. ▪ Human resources ➔ Focuses on the people who deliver the care such as their compensation, interaction with other members of medical community and well-being. Efforts are underway to allow EMS providers to move from state to state more seamlessly. The EMS Agenda for the Future encourages the creation of systems to help protect the well-being of EMS providers, including building career ladders. ▪ Medical direction ➔ Physician medical director authorizes EMTs to provide medical care in the field. Appropriate care is described in standing orders and protocols. ▪ Legislation and regulation ➔ Although each EMS system, medical direction, and training program has latitude, its training, protocols, and practice must follow state legislation, rules, regulations, and guidelines. A senior EMS official is usually in charge of necessary administrative tasks such as scheduling, personnel, budgets, purchasing, and vehicle maintenance, and the daily operations of ambulances and crews. ▪ Integration of health services ➔ Prehospital care by the EMT is coordinated with care administered by the receiving hospital. Care simply continues in the hospital emergency department. This ensures that the patient receives comprehensive continuity of care. ▪ Evaluation ➔ The medical director maintains quality control. CQI reviews and performs audits of the EMS system to identify areas of improvement and/or assign remedial training. Information and skills in emergency medical care change constantly. Refresher training and continuing education are important. Minimizing errors is the goal. ▪ Information systems ➔ Systems are used to document the care provided. Once stored electronically, the information can be used to improve care. For example, stored information can help determine: Average on-scene time for trauma patients, Need for educational sessions, National trends ▪ System finance ➔ Finance systems vary depending on which organization is involved. Personnel may be paid, volunteer, or a mix. EMTs may be involved in gathering insurance information, attending fund- raisers, or other activities that will help the department secure its finances. ▪ Education systems ➔ EMS instructors are licensed in most states. ALS training is usually provided in college, adult career center, or hospital settings. Continuing education is needed to update knowledge and refresh skills. ▪ Prevention and public education ➔ Prevention and public education are aspects of EMS where the focus is on public health. Public health examines the health needs of entire populations with the goal of preventing health problems. 6. Recall the following terms and know the importance in the prehospital setting Negligence, Abandonment, CQI, PCR, EMS administrator, Medical Director, DNR, living will. o Negligence ➔ Failure to provide standard of care ▪ It’s based on the following four factors: duty, breach of duty, damages, and causation. All four elements must be present for the legal doctrine of negligence to apply and for a plaintiff to prevail in a lawsuit against an EMS service or provider. o Abandonment ➔ Unilateral termination of care. It’s termination of care without the patient’s consent and without making provisions for the transfer of care to a medical professional with skills at the same level or at a higher level than your own skills. Abandonment is legally and ethically a very serious act. o Continuous Quality Improvement (CQI) ➔ A system of internal reviews and audits of the EMS system to identify areas of improvement and/or assign remedial training. Positive feedback is also discussed. If a problem appears to be repeated by a single EMT or crew, the medical director will discuss the details with the individual involved. o Patient care report aka Prehospital Care Report (PCR) ➔ is a legal document It records all care from dispatch to hospital arrival. It serves six functions: continuity of care, legal documentation, education, administrative information, essential research record, evaluation and continuous quality improvement o EMS Administrator ➔ sees to the daily operations and overall direction of the service or company. o Medical Director ➔ sees to the daily operations and overall direction of the service or company. The medical director maintains quality control at the LOCAL level. o Do-not-resuscitate (DNR)➔ an order not to administer CPR in the event of cardiac or respiratory arrest. “Do not resuscitate” does not mean “do not treat.” Even in the presence of a DNR order, you are still obligated to provide supportive measures (oxygen, pain relief, and comfort) to a patient who is not in cardiac arrest, whenever possible. o Living will aka Health care directive aka advance directive - a legal document stating a person's wishes regarding life- prolonging medical treatments. It take effect only when a patient is no longer able to make or communicate healthcare decisions for him- or her- self. ▪ As long as a patient is still able to make and express decisions, the existence (or lack) of an advance directive is irrelevant. Regardless of the contents of any existing advance directive, healthcare providers must honor the direct instructions of a competent patient. 7. “I am a communicable disease.” “How can I get to you today.” o communicable disease is any disease that can be spread from one person or species to another. o Infection risk can be minimized by: immunizations, protective techniques, hand washing ▪ When these protective measures are used, the risk of the health care provider contracting a serious disease is negligible. o Transmission is the way an infections disease is spread. It may be through: ▪ Direct contact (eg, blood) ▪ Indirect contact (eg, needlesticks) ▪ Airborne transmission (eg, sneezing) ▪ Foodborne transmission (eg, contaminated food) ▪ Vector-borne transmission (eg, fleas) 8. Review base stations, repeaters, multiplex, mobile radios, simplex, duplex o Base Station - A base station is any radio hardware containing a transmitter and receiver that is located in a fixed place. It is a two-way radio consists of transmitter and receiver. o Repeater –is a special base station radio. Receives messages and signals on one frequency. Automatically retransmits them on a second frequency. Provides outstanding EMS communications o Multiplex- A system that has the capability of transmitting two signals, usually voice and ECG, on the same frequency. This allows a paramedic to transmit ECG telemetry to a hospital while continuing to talk with the on-line medical control physician. o Mobile Radio – is installed in a vehicle. They are used in the ambulance to communicate with: the dispatcher and medical control ▪ An ambulance often has more than one mobile radio. Portable radios are hand-held devices. ▪ Portable radios are essential at the scene of an MCI. ▪ When away from the ambulance, a portable radio is helpful to communicate with: Dispatch, Another unit and Medical control o Simplex – is a Two-way radio hardware may operate in simplex mode. Simplex is push to talk, release to listen. A communication system that uses radios that transmits and receives on the same frequency. This means that only one radio in the system can transmit at a time. o Duplex – is a Two-way radio hardware may operate in duplex mode. Duplex is simultaneous talk-listen. A communication system that uses radios that transmits and receives on different frequencies. The paired receive and transmit frequencies in a system that is referred to as a channel. Radios can transmit and receive simultaneously, allowing communications to take place as if they were going over a telephone line. 9. Know the functions of the following glands: Thyroid, parathyroid, adrenal, pituitary o Thyroid ➔ Regulates metabolism. Person who has their thyroid removed will have decreased tolerance of hot and cold. ▪ Located in neck (over the larynx). ▪ Hormones Produced: Thyroxine and others. o Parathyroid ➔ Regulates serum calcium. ▪ Located on the neck (behind and besides the thyroid). Has a total of 3-5 glands. ▪ Hormones Produced: Parathyroid Hormones. o Adrenal Gland ➔ Regulates stress response, fight-or-flight response. ▪ Located above the kidneys. ▪ Hormones Produced: Epinephrine, norepinephrine, and others o Pituitary Gland ➔ Regulates all other endocrine glands. ▪ located at the base of skull. ▪ Hormones Produced: a few hormones that control other endocrine glands. 10. Review the abdominal quadrants and know the organs that are situated in each. o The abdomen is divided into quadrants for communication purposes. o Organs commonly found ▪ Right Upper Qudrant (RUQ): Liver, Gallbladder, duodenum of intestines, smaller portion of pancreas ▪ Left Upper Quadrant (LUQ): Stomach, Spleen ▪ Right Lower Quadrant (RLQ): Large and small intestines, ascending colon and the right half of the transverse colon, appendix ▪ Left Lower Quadrant (LLQ): descending colon, left half of the transverse colon 11. “Hello my name is skin” “do you know my layers”? o The skin has two principal layers: ▪ Epidermis ➔ tough, external layer that forms a watertight covering for the body. It’s composed of several layers ▪ Dermis ➔ the inner layer of the skin. It contains the hair follicles, sweat glands, and sebaceous glands. Blood vessels in the dermis provide the skin with nutrients and oxygen 12. Know the proper positioning of patients and know the situations that would dictate the use of each. Eg. Fowlers, semi-fowlers, trendelenburg, shock, supine, prone, recovery o Fowler’s ➔ sitting up with the knees bent greater than 45 degrees, helps them breathe better and control the airway. o Semi-Fowler’s ➔ sitting up = less than 45 degrees. The position of a patient who is lying in bed in a supine position with the head of the bed at approximately 45 degrees. o Trendelenburg ➔ patients are in a supine position on an incline with their feet higher than their head to keep blood in the core of their body. Their FEET are 6 to 12 inches higher than their HEAD. o Shock position (modified Trendelenburg position)- the patients head and torso are supine, and the lower extremities are elevated 6 to 12 inches higher than the head to help increase blood flow to the brain o Supine ➔ body is facing up o Prone ➔ body is facing down o Recovery Position ➔ on left side. A patient should be placed in the recovery position when he or she is unconscious, uninjured, and breathing adequately. 13. Review following terms Cerebrum, cerebellum, brain stem, diencephalon, frontal, parietal, temporal, occipital lobes o The cerebrum is the largest part. ▪ Located above the cerebellum, is divided into right and left hemispheres. ▪ Each controls activities on the opposite side of the body. o The cerebellum controls muscle and body coordination. ▪ Walking, writing, picking up a coin, playing the piano ▪ Sometimes called the "little brain" o The brain stem controls the most basic functions. ▪ Breathing, blood pressure, swallowing, pupil constriction o Diencephalon➔ controls pain and temperature. ▪ consists almost all of gray matter ▪ located between the midbrain and the cerebrum ▪ consists of the thalamus (sensation and emotion), hypothalamus, optic chiasm, and pineal body ▪ Sometimes called the “interbrain” o Frontal Lobe ➔ front of the cerebrum, controls emotion and thought. o Parietal Lobe➔ middle part of the cerebrum, controls touch and movement. o Occipital Lobe➔back part of the cerebrum, processes sight. 14. Do you know the differences and parts of the central and peripheral nervous systems? o The nervous system is divided into two parts ▪ Central Nervous System (CNS) ➔ consists of the brain and the spinal cord ➢ is covered and protected by 3 layers of tissue called meninges: dura mater, arachnoid, pia mater ▪ Peripheral Nervous System (PNS) ➔ Long nerve cells that link these cells to the body's various organs through openings in the spinal column ➢ The peripheral nervous system has two anatomic parts: o 31 pairs of Spinal Nerves: Conduct impulses from the skin and other organs to the spinal cord. Conduct motor impulses from the spinal cord to the muscles. The spinal nerves serving the extremities are arranged in complex networks. o 12 pairs of Cranial Nerves: Transmit information directly to or from the brain. Perform special functions in the head and face, including sight, smell, taste, hearing, and facial expressions ➢ There are two major types of peripheral nerves. o Sensory nerves: Carry only one type of information from the body to the brain via the spinal cord. o Motor nerves: One for each muscle. Carry information from the CNS to the muscles. ➢ The connecting nerves are found only in the brain and spinal cord. Connect the sensory and motor nerves with short fibers Allow the exchange of simple messages 15. How do check Perfusion, Motor and Sensory in a patients with suspected extremity fractures o Examination of the injured limb should include the 6 P’s of musculoskeletal assessment: ▪ PAIN, PARALYSIS, PARESTHESIA (numbness or tingling), PULSELESSNESS, PALLOR (pale or delayed capillary refill in children), PRESSURE 16. Recall the following terms and know their function Erythrocytes, leukocytes, thrombocytes, monocytes o Erythrocytes ➔ Red blood cells that contain hemoglobin which gives blood its color. Hemoglobin carries oxygen. o Leukocytes ➔ White blood cells that play a role in the body’s immune defense to fight infection. o Thrombocytes ➔ platelets those are essential in the initial formation of a blood clot. o Monocytes ➔ a type of white blood cell that attack bacteria or viruses. 17. Know the following terms and what they represent physiologically Systole, diastole, stroke volume, cardiac output Systolic ➔ high point of wave as heart is contracting, the left ventricle of heart contracts, it pumps blood from ventricle into aorta. Indicates heart pumping effectiveness, and blood available to the heart o Diastolic ➔ low point of wave as ventricle relaxes; therefore the ventricle fills with blood. Indicates adequacy of the amount of blood vessel contraction (arterial), and amount of blood within blood vessels. o Stroke volume (SV) ➔ is the amount of blood moved by one beat. o Cardiac output (CO) ➔ is the amount of blood moved in 1 minute. ▪ CO can be expressed by Cardiac output (CO) = heart rate (HR) × stroke volume (SV) 18. Review and know the difference between pulmonary and systemic circulation. o Two circuits in the body: systemic circulation and pulmonary circulation ▪ Systemic circulation—body ➢ Carries oxygen-rich blood from the left ventricle through the body and back to the right atrium. ➢ The portion of the circulatory system outside of the heart and lungs. ▪ Pulmonary circulation—lungs ➢ Carries oxygen-poor blood from the right ventricle through the lungs and back to the left atrium. ➢ The flow of blood from the right ventricle through the pulmonary arteries and all of their branches and capillaries in the lungs and back to the left atrium through the venules and pulmonary veins; also called the lesser circulation. 19. Know the major arterial and venous vessels o Arteries ➔Arteries carry blood from the heart to all body tissues ▪ Major Arteries: ➢ Aorta➔ Principal artery leaving the left side of the heart and carrying freshly oxygenated blood to the body. Divides at the level of the umbilicus into the iliac arteries ➢ Pulmonary ➔ Artery originating at the right ventricle. Carries oxygen-poor blood to the lungs ➢ Carotid ➔ Major artery of the neck. Supplies the head and brain with blood. Palpation site for pulse on either side of the neck ➢ Femoral ➔ The major artery of the thigh. Supplies the lower extremities with blood. Palpation site for pulse in the groin area (the crease between the abdomen and thigh) ➢ Posterior tibial ➔Palpation site for pulse on the posterior surface of the medial lleolus ➢ Dorsalis pedis ➔ Palpation site for pulse on the anterior surface of the foot ➢ Brachial ➔Major artery of the upper extremity. Supplies blood to the arm. Palpation site for pulse on the inside of the arm between the elbow and the shoulder. Used when determining blood pressure (BP) with a ➢ BP cuff and a stethoscope ➢ Radial ➔ Major artery of the lower arm. Palpation site for pulse at the thumb side of the wrist. o Veins➔ Return oxygen-depleted blood to the heart ▪ Major Vein: Vena cava ➢ Superior vena cava carries blood returning from the head, neck, shoulders, and upper extremities. ➢ Inferior vena cava carries blood from the abdomen, pelvis, and lower extremities. ➢ **These two veins join at the right atrium. 20. Know what is considered significant blood loss in an adult and child patient. Know percentages as well as liters. o The body will not tolerate an acute blood loss of greater than 20% of blood volume. The typical adult had approximately 70 mL of blood per kilogram of body weight, or 6L (10 to 12 pints) in a body weighing 80 kg (175 lbs). o IN ADULT ▪ If the typical adult loses more than 1 L of blood (about 2 pints), significant changes in vital signs will occur, including increasing heart & respiratory rates and decreasing blood pressure. Because infants & children have less blood volume to begin with, the same effect is seen with smaller amounts of blood loss. o IN A CHILD ▪ For example, a 1 year old has a total blood volume of about 800 mL. Significant symptoms of blood loss will occur after only 100 to 200 mL of blood loss. To put this in perspective, a soft drink can holds roughly 355 mL of liquid. o A healthy adult can comfortably donate 1 unit (500 mL) of blood during a period of 15 to 20 minutes and adapts well to this decrease in blood volume. 21. Know examples and locations of central versus peripheral pulses o Central Pulse ➔examples are femoral and carotid pulses o Peripheral Pulse ➔ examples are Radial, Brachial, posterior tibial, and dorsalis pedis pulses 22. Review the following terms Heart Rate, Stroke volume, Cardiac Output, Minute Volume o Heart Rate ➔number of heart beats per minute ▪ Normal Pulse rates include ➢ Adult and adolescent: 60 to 100 beats/min ➢ Child: 70 to 140 beats/min ➢ Toddler: 90 to 150 beats/min ➢ Infant: 100 to 160 beats/min o Stroke volume (SV) ➔ is the amount of blood moved by one beat. o Cardiac output (CO)➔ is the amount of blood moved in 1 minute. ▪ CO can be expressed by CO = HR × SV o Minute Volume aka minute ventilation ➔ is the amount of air that moves in and out of the lungs in 1 minute minus the dead space. ▪ Minute Volume =Respiratory Rate (RR) x Tidal Volume (TV) 23. Review the following terms and know what they are associated with. SA node, AV node, Bundle of His, Purkinje fibers. o SA Node ➔ is the heart’s main pacemaker, which is located in the wall of the right atrium, where it meets the superior vena cava. ▪ There are three intermodal pathways that transmit the pacing impulse form the SA node to the AV node o AV node ➔ transmits the impulse from the atria to the ventricles o Bundle of His➔ starts at the AV node and then splits into the right and left bundle branches ▪ the right and left bundle branches, which travel through the interventricular septum and lead to the purkinje fibers in the ventricular walls Purkinje Fibers ➔ electrical conduction travels to the ventricles, causing the cardiac muscle of the ventricles to contract at a paced interval. 24. Know the phases of General adaptation syndrome o General Adaption Syndrome - Body's three-stage response to stress. ▪ Alarm response to stress ▪ Reaction/Resistance to stress ▪ Recovery—or if the stress is prolonged then exhaustion. 25. Review the following terms Acute stress, Cumulative stress, CISD, CISM, PTSD. o Acute Stress Reaction – occur during a stressful situation. The EMT feels nervous, excited, and his or her ability to focus increases. This can be very helpful in managing a crisis situation. But if the stress of the situation becomes too great, the EMT is at risk of being caught up in emotional and physical reactions to stress. o Cumulative stress – exposure to prolonged or excessive stress o Critical incident stress management (CISM) ➔ a theoretical process that confronts the responses to critical incidents and defuses them, directing the emergency services personnel toward physical and emotional equilibrium. ▪ was developed to address acute stress situations and potentially decrease the likelihood that PTSD will develop after such an incident. o Critical Incident Stress Debriefing (CISD) ➔ the CISM can be held formally as debriefing sessions are held within 24 to 72 hours of a major incident. o Post Traumatic Stress (PTSD) ➔ Characterized by reexperiencing the event and over responding to the stimuli that recall the event . Some of the symptoms include depression, startle reactions, flashback phenomena, and dissociative episodes (e.g. is amnesia of the event). 26. Hey, do you know Kubler Ross? He developed something really cool. Please know its components o In 1969, DR. Elizabeth Kubler-Ross published research revealing people go through several stages of grieving. They are as follows: ▪ Denial ➔ refusal to accept diagnosis or care, unrealistic demands for miracles, or persistent failure to understand hwy there is no improvement. ▪ Anger, hostility ➔ projection of bad news onto the environment and commonly in all directions, at times almost at random. The person lashes out, someone must be blamed, and those who are responsible must be punished. This is usually the ugly phase, and may even be inappropriately directed toward the EMT. ▪ Bargaining ➔ an attempt to secure a prize for good behavior or promise to change lifestyle. “I promise to be a “perfect patient” only if I can live under “x event. ▪ Depression ➔ internalized anger, hopelessness, and the desire to die. It rarely involves suicidal threats, complete withdrawal, or giving up long before the illness seems terminal. The patient is usually silent. ▪ Acceptance ➔ Acceptance of impending death by the patient, or the acceptance of the death of a loved one. o The stages may follow one another, occur simultaneously or a person may jump back and forth between stages. 27. Review the hypoxic drive Hypoxic drive ➔ is the backup system that controls breathing. It is less sensitive and less powerful than the carbon dioxide sensors in the brain stem. It senses drops in the oxygen level in the blood and then the body uses this drive. 28. Know the difference between respiration and ventilation o Respiration – is the process of breathing, it is the actual exchange of oxygen and carbon dioxide in the alveoli and in tissues of the body. ▪ The medulla keeps us breathing so we do not have to think about it. It initiates the ventilation cycles, stimulated by high carbon dioxide levels. Medulla has two main portions: ➢ Dorsal respiratory group (DRG) which initiates inspiration and sets pattern for respirations ➢ Ventral respiratory group (VRG) which provides for forced inspiration or expiration as needed. o Ventilation – is simple movement of air into and out of the lungs. You provide ventilation when you administer oxygen. It is the process of inhalation and exhalation, it is a physical act. 29. Know the MAJOR differences between child and adult anatomy o Pediatric airway is smaller in diameter and shorter in length. i. Breath sounds are more easily heard because of their thinner chest walls. o Occiput is larger and rounder, which requires more careful positioning of the airway. o Tongue is larger relative to the size of the mouth and in a more anterior location in the mouth. Child’s tongue can easily block the airway. o Open growth plates allow bones to grow during childhood. As a result of open growth plates, children’s bones are softer and more flexible, making them prone to stress fracture o The thoracic cage in children is highly elastic and pliable because it is primarily composed of cartilaginous connective tissue. The ribs and vital organs are less protected by muscle and fat. 30. Review the difference between Osmosis and Diffusion o Osmosis ➔is the diffusion of water across a semi-permeable membrane from an area of high concentration to an area of low concentration o Diffusion ➔is a passive process in which molecules move from an area with a higher concentration of molecules to an area of lower concentration. ▪ *no semi-permeable membrane is involved o Diffusion is the dilution of solutes and osmosis is the movement of fluids. 31. Be able to describe the process of Inhalation and Exhalation. Think active vs passive process, position of diaphragm, status of intercostals muscles and pressure differences. o Inhalation is an active process in which the diaphragm and intercostal muscles contract and moving the ribs up and out enlarging the chest cavity, decreasing the pressure in the lungs. This causes air to flow into the lungs. o Exhalation is a passive process, in which the diaphragm and intercostal muscles relax, (no muscular effort) decreasing the chest cavity, increasing the pressure in the lungs. The air flows out of the lungs. 32. Review solid versus hollow organs o Hollow Organs ureters, bladder, stomach, intestines, fallopian tubes, small intestines, large intestines, gallbladder ▪ Injury: spill contents into the abdomen, blunt and penetrating trauma can cause hollow organ injuries o Solid Organ liver, spleen, pancreas, ovary, adrenal gland, kidneys, great vessels, abdominal aorta, IVC ▪ Injury: can bleed significantly and cause rapid blood loss, liver is very vascular and the largest organ in the abdomen and often injured first by a fractured lower right rib or penetrating trauma, look out for Kehr sign to suspect liver damage 33. Know the respiratory structures in ascending and descending order o Upper Airway: nose, mouth, tongue, jaw, oral cavity, pharynx, (nasopharynx, pharynx, oropharynx), epiglottis o Lower Airway: Larynx, trachea, bronchi, brochioles, alveoli 34. Know the following terms Thyroid cartilage, Cricoid cartilage, uvula, pharynx o Thyroid Cartilage➔ A firm prominence of cartilage that forms the upper part of the larynx; the Adam's apple. Easily seen in the middle of the front of the neck; the anterior part of the larynx. o Cricoid Cartilage ➔ A firm ridge of cartilage that forms the lower part of the larynx; immediately below the thyroid cartilage. The location for using the Sellick maneuver to help in maintaining a proper airway. o Uvula ➔ Small flesh mass that hangs from the center of the soft plate, conical in shape. o Pharynx ➔ Composed of the nasopharynx, oropharynx, and the laryngopharynx. Food and liquids enter the pharynx & pass into the esophagus, which carries them to the stomach. Air and other gases enter the trachea and go to the lungs. ▪ Two passages are located at the bottom of the pharynx: ➢ Esophagus behind ➢ Trachea (windpipe) in front 35. Know the types of muscles and examples of where each can be found o 3 types of muscles ▪ Skeletal a muscle that is connected at either or both ends to a bone and so move parts of the skeleton, form the major muscle mass of the body. It is voluntary. Also called a striated muscle. ▪ Cardiac muscle tissue of the heart ▪ Smooth a muscle that contracts without conscious control and found in walls of internal organs such as stomach and intestine and bladder and blood vessels (excluding the heart). It constitutes the bulk of the GI tract and is present in nearly every organ to regulate autonomic activity. 36. What is the difference between voluntary and involuntary muscles? o Voluntary Muscles ➔it is under direct voluntary control of the brain. It connects to the bones of the skeletal system o Involuntary Muscles➔ The muscle over which a person has no conscious control. It is found in many automatic regulating systems of the body. ▪ Includes smooth muscles ad cardiac muscles 37. Hey remember that leaf-shaped respiratory airway structure? I hope you do. o Epiglottis ➔ protects the opening of the trachea. It is a hin, lead-shaped valve that allows air to pass into the trachea but prevents food and liquid from entering the trachea 38. I am a spinal column do you know my section? ➔ Spinal cord has 33 bones called vertebrae o Cervical: 7 *Most prominent vertebrae is C7* o Thoracic: 12 o Lumbar: 5 o Sacral: 5 o Coccyx: 4 (fused) 39. How do you assess and treat patients with joint injuries o Focus on determining whether the patient has a pulse, has adequate perfusion, or is bleeding. Hypoperfusion and bleeding problems will most likely be your primary concern. o Steps ▪ gently support the limb at the site of injury (to prevent excessive movement) ▪ place the rigid splint under or alongside the limb ▪ place padding between the limb and the splint to make sure there is even pressure and even contact, ▪ apply bindings to hold the splint securely to the limb ▪ check and record the distal nervous and circulatory (neurovascular) function 40. Know all about Nitroglycerin also know the important questions to ask you patient and what action you should take after administering this drug. important question o Nitroglycerin ➔medication that helps relieve the pain of angina (chest pain). Administered sublingually/ The purpose is to increase blood flow to relieve the spasms or causing the arteries to dilate. It does this by replacing the muscular walls of the coronary arteries and veins. Nitroglycerin also relaxes veins throughout the body, so less blood is returned to the heart and the heart does not have to work as hard each time it contacts. In short, BP is decreased. ▪ ALWAYS take persons BP before administering medication, patient MUST HAVE BP higher than 120 mm Hg ➢ If systolic BP is less than 120 mm Hg, nitroglycerin may have harmful effects of lowering blood flow to the heart’s low blood vessel. ▪ Trade name: Nitrostat ▪ Action: Dilates blood vessels ▪ Indications; chest pain due to myocardial infarction or angina ▪ Contraindications: hypotention, erectile dysfunction meds within past 36 hours, head injury ▪ Routes: SL/Spray or Tablet form (use gloves if using tablets) ▪ Side effects: headache, burning under tongue, hypotention, nausea ▪ Interactions: increasing dilating effects of other blood vessel-dilating medications ▪ Adult Dose: 0.3-0.4 mg SL, 0.4 mg spray ▪ Administration concerns: ensure ALS is en route 41. Know trade names and generic name of commonly used drugs o Brand Name- a brand name that a manufacturer gives to a medication, ▪ Begins with a capital letter ▪ One drug may have more than one trade name o Generic Name - usually the original chemical name of a medication. (It is a simple, clear, nonproprietary name) ▪ Not capitalized o Examples Trade Generic Tylenol Acetaminophen Advil, Nuprin, Motrin Ibuprofen Albuterol Proventil, Ventolin Alupent Metaproterenol Nitroglycerin Nitrostat, Isordil Bayer Aspirin Actidose with Sorbitol Activated Charcoal Benadryl Diphenhydramine EpiPen Epinephrine Glucose Oral Glucose Oxygen (has no trade name) Oxygen 42. Know the side effects of commonly used drugs Drug Side Effect Tylenol Allergic Rxn Advil, Nuprin, Motrin, Ibuprofen Nausea, vomiting, stomach pain, bleeding, allergic rxn Albuterol, Proventil, Ventolin Hypertention, tachycardia, anxiety, restlessness Alupent, Metaproterenol Increased pulse rate (tachycardia), anxiety, nausea, cough, wheezing, tremors, and/or dizziness. Nitroglycerin, Nitrostat, Isordil Headache, burning under tongue, hypotension, nausea Bayer, Aspirin Nausea, vomiting, stomach pain, bleeding, allergic rxn Actidose with Sorbitol, Activated Charcoal Nausea, vomiting, constipation, black stool Benadryl, Diphenyhydramine Sleepiness, dry mouth + throat EpiPen, Epinephrine Hypertention, tachycardia, anxiety, restlessness Glucose, Oral Glucose Nausea, vomiting Oxygen (has no trade name) Decreased respiratory effort in rare cases in patients w/COPD 43. Review the following terms therapeutic effects, side effects, indications, contraindications, dose, route, form of drug o Therapeutic effects➔ consequence of a medical treatment of any kind, the results of which are judged to be desirable/ beneficial and even unintended consequence of the treatment. ▪ Quizlet; When administering albuterol to patient with shortness of breath, the EMT realizes that the therapeutic effect of this medication is achieved by: dilating the small airways. o Side Effects ➔ Any actions of a medication other than the desired ones. ▪ Unintended effects: Effects that are undesirable but pose little risk to the patient. ▪ Untoward effects: Effects that can be harmful to the patient. o Indications ➔ Reasons or conditions for which a particular medication is given. o Contraindications ➔ When a medication would either harm the patient or have no positive effect. o Dose ➔ The amount of the medication that is given; depends on: patient’s weight, patient’s age, desired action of the medication o Route ➔ the way in which a medication is intended to be taken o Form of a Drug ➔ form of a medication usually dictates the route of administration. ▪ Basic Medication forms include: ➢ Tablets and capsules are swallowed ➢ Solutions and suspensions Solutions can be given by almost any route (orally, IV, IM, or SC injection) while suspensions are usually given by mouth, also rectally, applied directly to skin, IM or SC injections) ➢ Metered-dose inhalers (MDIs) ➢ Topical medications Applied to the skin surface and only affect that area ➢ Transcutaneous medications are absorbed through skin ➢ Gels orally (have consistency of paste, example oral glucose) ➢ Gases for inhalation delivered through nonrebreathing mask or nasal cannula 44. Review the routes of medicine administration. Know the fastest & slowest route & conditions that may affect each 45. What is the name of the structures found on the head of an infant and at what age does it close o The bones of an infant’s head are flexible and soft. The soft spots are located at the front and back of the head and are called fontanelles. ▪ These allow the infant’s head to pass through the birth canal. ▪ The three or four bones of the skull eventually bind together and form suture joints. ➢ The posterior fontanelle fuses by 3 months. ➢ The anterior fontanelle fuses between 9 and 18 months of age. 46. Know the indications for the use of epi-pen( refer to state protocol) o Indication for Epi-Pen: ▪ Difficulty breathing, hives, itching, tongue swelling, patient is unable to swallow ▪ ALL 3 MUST BE PRESENT: ➢ Pt. has physician prescribed auto-injector ➢ Pt has a medical historu of allergic rxns and is conscious/unconscious with anaphylaxis ➢ Pt complains of respiratory distress or displays signs/symptoms of shock o State Protocol (NY): The EMT-B is trained to recognize the signs and symptoms of anaphylaxis and the contraindications for epinephrine. In cases of an allergic reaction, where the patient is conscious and alert, the patient should be able to participate in the decision and the delivery of the epinephrine autoinjector. 47. Know the side effects, dose and route of administration of epi-pen o Side Effects: increased heart rate, pallow, dizziness, chest pain, nausea, vomiting, excitability, anxious, headache o Dose: 0.3 mg for adults (Epi-Pen) 0.15 mg for child (Epi-Junior) o Route of Administration: intramuscularly 48. Know the signs and symptoms and how to treat a patient with hypoglycemia o Hypoglycemia is a state in which the blood glucose is below normal. ▪ Untreated, it results in unresponsiveness and eventually hypoglycemic crisis. ▪ Signs and symptoms include: ➢ History: Insufficient food intake; excessive insulin dosage; rapid onset (minutes); pale, cool, moist skin ➢ Gastrointestinal tract: Absence of thirst and intense hunger ➢ Respiratory system: Normal to shallow or rapid respirations ➢ Cardiovascular system: Normal to low blood pressure; rapid, weak pulse ➢ Nervous system: Altered mental status (aggressive, confused, lethargic, or unusual behavior); seizure, fainting, or coma; unsteady gait (weakness on one side of the body, may mimic stroke) ➢ Response to treatment: Immediate ▪ Treatment: Oral Glucose (give sublingually, whole tube) 49. What is the action of Aspirin and what type of patient would receive Aspirin o Purposes(Action) ▪ Antipyretic (reduces fever) ▪ Analgesic (reduces pain) ▪ Anti-inflammatory (reduces inflammation) ▪ Inhibits platelet aggregation (clumping), which is useful during a potential heart attack o Contraindications ▪ Hypersensitivity to aspirin ▪ Preexisting liver damage, bleeding disorders, and asthma ▪ Children during episodes of fever-causing illnesses o Type of Patient who would receive Aspirin ▪ Patients at risk for coronary artery disease, or potential heart attack patients o Depending on protocol: Administer low-dose aspirin. ▪ Effects: Prevents blood clots from forming or getting bigger , 81-mg chewable tablets, Recommended dose: 162 mg (two tablets) to 324 mg (four tablets) 50. Know the liter flow per minute and the percentage of the different oxygen delivery devices. Also know the indication for the use of each. o Nonrebreathing mask at 10 to 15 L/min provides up to 90% oxygen concentration ▪ Preferred method of giving oxygen, used on conscious patient. o Nasal cannula at 1 to 6 L/min provides 24% to 44% oxygen concentration. ▪ Used on conscious patient when non-rebreather mask cannot be tolerated o Bag-mask device at 10 to 15 L/min provides 90% oxygen concentration. ▪ Used on unconscious patient o Mouth-to-mask device at 15 L/min provides nearly 100% oxygen concentration ▪ Used on unconscious patient. o Blow-by technique at 6 L/min provides more than 21% oxygen concentration. ▪ Give to child with shortness of breath because many will not tolerate (or refuse to wear) a face mask. Rather than fighting with the child, provide blow-by-oxygen by holding the oxygen mask in front of the child’s face or ask the parent to hold the mask. 51. Know the common medications used to treat Asthma, hypertension, allergic reactions, heart disease o Common Medications used to treat: ▪ Asthma ➔ In asthma patients, they seem to have problems with EXHALATION, not inhalation. Patients with asthma do not have great difficulty with oxygenation their problem is more related to severe contraction of the muscles surrounding the lower airways. ➢ An MDI (metered-dose inhaler) is often used by a patient with respiratory illnesses (including asthma and emphysema) ➢ Trade names of some asthma inhalers (Beta 2 agonist ➔ cause bronchodilation) o Primatene Mist, Bronitin Mist, Bronkaid Mist, Medihaler-Epi o Albuterol (generic is Proventil or Ventolin) is a medication commonly used during asthma attacks. It’s available in an inhaler and in a small volume nebulizer (SVN). Albuterol acts on the (beta2) receptors of the sympathetic nervous system, which results in dilation of the airways. ▪ Hypertension ➔ Blood pressure that is higher than the normal range. ➢ Treated with diuretics, beta blockers (decreases HR and decreases heart contraction), alpha blockers (dilate blood vessels in heart), and vasodilators. o Drugs: Diovan HCT/valsartanand hydrocholorothiazide treat hypertention ▪ Allergic Reactions ➔ body's exaggerated immune response to an internal or surface agent ➢ Treated with auto injectable epinephrine, and some meter dosed inhalers. ▪ Heart Disease ➔ ex. Congestive heart failure (CHF), acute myocardial infarction (classic heart attack), ➢ Treated with nitroglycerin (dilates blood vessels), and aspirin (acts as anti-platelet, treats chest pain or suspected ischemic origin) ➢ More Drugs: o Lipidor/atorvastatin lowers cholesterol o Toprol/metoprolol lowers blood pressure o Vytorin/ezetimibe and simvastatin lowers cholesterol o Diovan/valsartan lowers high blood pressure o Zetia/ezetimibe lowers cholesterol o Crestor/rosuvastatin lowers cholesterol 52. Know the differences between signs and symptoms o Symptom ➔ is a subjective condition the patient feels and tells you about. o Sign ➔ is an objective condition you can observe about the patient. 53. Review and know the components steps of patient assessment. Also know the goal of each component. o The assessment process begins with the scene size-up ➔ which identifies real or potential hazards. The patient should not be approached until these hazards have been dealt with in a way that eliminates or minimizes risk to the EMTs and the patient(s). Can be done at a distance, ask yourself: ▪ BSI Body Substance Isolation (example, wearing medical gloves) ▪ Scene Safety (Hazards, threats) ▪ How many patients? ▪ MOI (mechanism of injury for trauma)/ NOI (nature of illness) ▪ Call for backup if necessary o The primary assessment ➔is performed on all patients. It includes forming an initial general impression of the patient, including the level of consciousness, and identifies any life-threatening conditions to the ABCs. A rapid scan is performed to assist in prioritizing time and mode of transport. ▪ Any life threats identified must be treated before moving on to the next step of the assessment. ▪ Airway, breathing, and circulation are assessed to evaluate the patient’s general condition. o History taking ➔ includes an investigation of the patient’s chief complaint or history of present illness. A SAMPLE history is generally taken during this step of the assessment process. This information may be obtained from the patient, family, friends, or bystanders. ▪ By asking several important questions, you will be able to determine the patient’s signs and symptoms, allergies, medications, pertinent past history, last oral intake, and events leading up to the incident. ▪ SAMPLE History (Make sure you have Broad and Open ended questions!) ➢ S – Symptoms “So what’s going on today? Or “Can you tell me what’s been bothering you today?” ➢ A – Allergies “Have you ever had an allergic reaction?” or “Are you allergic to any foods or medication?” o Person has “no known allergies” you can write “NKA” ➢ M – Medications “Are you currently taking any medications that are prescribed, over the counter, or herbal?” ➢ P – Past/Pertinent Medical History “Have you ever been hospitalized for this or any other reason before?” ➢ L – Last Oral Intake “What was the last time you ate or drank anything?” ➢ E – Events Leading Up To Present Illness / Injury “What were you doing before you felt ill/this happened to you?” or “What was going on today before this happened?” ▪ Assessment of Pain ➢ O—Onset “When did the problem begin?” and “What caused it?” ➢ P—Provocation/Palliation “Does anything make it feel better or worse?” ➢ Q—Quality “How is the pain like—sharp, dull, crushing, tearing?” ➢ R—Region/Radiation “Where does it hurt?” and “Does the pain move anywhere?” ➢ S—Severity “On a scale of 1 to 0, how would you rate your pain?” ➢ T—Timing “When did the pain start?” o The secondary assessment ➔ is a systematic physical examination of the patient. The physical examination may be a systematic head-to-toe, full-body scan or a systematic assessment that focuses on a certain area or region of the body, often determined through the chief complaint. Circumstances will dictate which aspects of the physical examination will be used. ▪ Is performed on scene or in the back of the ambulance en route to the hospital; there are times when you may not have time to perform a secondary assessment at all if the patient has serious life threats. o The reassessment ➔is performed on all patients. It gives you an opportunity to reevaluate the chief complaint and to reassess interventions to ensure that they are still being delivered correctly. ▪ Information from the reassessment may be used to identify and treat changes in the patient’s condition. ▪ A patient in stable condition should be reassessed every 15 minutes, whereas a patient in unstable condition should be reassessed every 5 minutes. 54. Know the term MOI and be able to recognize examples of significant MOI and non Significant MOI o MOI (mechanism of injury for trauma) ➔ how the traumatic injury occurred. o You must evaluate three factors: ▪ the amount of force applied to the body ▪ the length of time the force was applied ▪ and the areas of the body that are involved 55. Know the term surfactant and what it is associated with o Surfactant ➔ is a liquid protein substance that coats the alveoli in the lungs, decreases alveoli surface tension, and keeps the alveoli expanded making it easier for gas exchanged; a low level in a premature infant contributes to respiratory distress syndrome. ▪ Quizlet: Pulmonary surfactant serves which of the following functions? It facilitates the transport of oxygen-poor blood from the right ventricle to the lungs. 56. Know the normal heart and respiration rates of adults, children and infants o Heart Rate ➔number of heart beats per minute ▪ Normal Pulse rates include ➢ Adult and adolescent: 60 to 100 beats/min ➢ Child: 70 to 140 beats/min ➢ Toddler: 90 to 150 beats/min ➢ Infant: 100 to 160 beats/min o Respiratory Rates ➔number of breathes per minute ▪ Normal Respiratory Rate ➢ Adults and adolescent: 12 to 20 breaths/min ➢ Children (1-12 years old): 15 to 30 breaths/min ➢ Infants: 25-50 breaths/min 57. Know when to use capillary refill and know what is considered abnormal and what could the abnormal findings suggest o Capillary Refill ➔ is evaluated to assess the ability of the circulatory system to restore blood to the capillary system. It provides the patients level of perfusion. ▪ Normally Capillary Refill time is a return of color to your nail beds after 2 seconds. A time of more than 2 seconds is considered abnormal, and suggests there is poor perfusion. ▪ Capillary refill is unreliable in elderly people because of compromised circulation. ▪ To test a patient's capillary refill, the EMT will: firmly compress and then release pressure on the nail bed. Normal color to the tested area should return within 2 seconds. 58. Know the differences between compensated, decompensated and irreversible shock. o Compensated shock – In early stages of shock, the body can still compensate for blood loss. ▪ Signs and symptoms: Agitation, Anxiety, Restlessness, Feeling of impending doom, Altered mental status, Weak, rapid (thready), or absent pulse, Clammy (pale, cool, moist) skin, Pallor, with cyanosis about the lips, Shallow, rapid breathing, Air hunger (shortness of breath), especially if there is a chest injury, Nausea or vomiting , Capillary refill of longer than 2 seconds in infants and children, Marked thirst o Decompensated shock - The late stage, when blood pressure is fallin ▪ Signs and symptoms: falling blood pressure (systolic blood pressure of 90 mm Hg or lower in an adult), Labored or irregular breathing, ashen, mottled, or cyanotic skin, thready or absent peripheral pulses, dull eyes, dilated pupils, poor urinary output o Irreversible shock- Terminal stage of shock. A transfusion of any type will not be enough to save a patient’s life. 59. Know the components of blood o Plasma ➔ the liquid portion of blood) contains: ▪ Water ( a primary component),proteins (a primary component), oxygen, carbon dioxide, nitrogen, nutrients, cellular wastes o Red blood cells (erythrocytes) ➔ contain hemoglobin which gives blood its color ▪ Hemoglobin carries oxygen. o White blood cells (leukocytes) ➔ which play a role in the body’s immune defense to fight infection o Platelets ➔ are essential in the initial formation of a blood clot 60. Know the different types of shock & be able to recognize the signs & symptoms that are consistent with each type o Types of Shock: Distributive, Obstructive, Cardiogenic, Hypovolemic, Septic, Anaphylatic o Shock (hypoperfusion) means a state of collapse and failure of the cardiovascular system. ▪ In the early stages of shock, the body attempts to maintain homeostasis (a balance of all systems in the body). ▪ As shock progresses, however, blood circulation slows and eventually ceases. o Shock can result from many conditions, including bleeding, respiratory failure, acute allergic reactions, and overwhelming infection. o Cardiogenic shock ▪ Cardiogenic shock is caused by inadequate function of the heart, or pump failure. ▪ A major effect is the backup of blood into the lungs. The resulting buildup of pulmonary fluid is called pulmonary edema. Edema is the presence of abnormally large amounts of fluid between cells in body tissues, causing swelling of the affected area. Pulmonary edema leads to impaired ventilation. ▪ Cardiogenic shock develops when the heart cannot maintain sufficient output to meet the demands of the body. Cardiac output is the volume of blood that the heart can pump per minute, and it is dependent upon several factors. The heart must have adequate strength, which is largely determined by the ability of the heart muscle to contract (myocardial contractility). ▪ The heart must receive adequate blood to pump. The resistance to flow in the peripheral circulation must be appropriate. o Obstructive shock ▪ Occurs when conditions that cause mechanical obstruction of the cardiac muscle also affect the pump function. Common examples: ➢ Cardiac tamponade - It is a collection of fluid between the pericardial sac and the myocardium. It is caused by blunt or penetrating trauma and can progress rapidly. Blood leaks into the tough fibrous membrane known as the pericardium, causing an accumulation of blood within the pericardial sac. This accumulation leads to compression of the heart. Signs and symptoms of cardiac tamponade are referred to as Beck’s triad, the presence of jugular vein distention, muffled heart sounds, and systolic and diastolic blood pressure starting to merge. ➢ Tension pneumothorax - It is caused by damage to lung tissue. The damage allows air normally held within the lung to escape into the chest cavity. This air applies pressure to the organs, including the heart. o Distributive Shock (“SNAP” septic, neurogenic, anaphylaxis, psychogenic) ▪ Results when there is widespread dilation of small arterioles,venules, or both. The circulating blood volume pools in the expanded vascular beds and tissue perfusion decreases. ▪ Septic shock ➢ occurs as result of severe infections, usually bacterial, in which toxins are generated by the bacteria or by infected body tissues. The toxins damage the vessel walls, causing increased cellular permeability. The vessel walls leak and are unable to contract well. Widespread dilation of vessels, in combination with plasma loss through the injured vessel walls, results in shock. ➢ Septic shock is a complex problem. There is an insufficient volume of fluid in the container, because much of the plasma has leaked out of the vascular system (hypovolemia). The fluid that has leaked out often collects in the respiratory system, interfering with ventilation. The vasodilation leads to a larger-than-normal vascular bed to contain the smaller-than-normal volume of intravascular fluid. ➢ Septic shock is almost always a complication of a very serious illness, injury, or surgery. ▪ Neurogenic Shock ➢ Is usually a result of injury to the part of the nervous system that controls the size and muscle tone of the blood vessels. Causes include: o Damage to the spinal cord o Brain conditions o Tumors o Pressure on the spinal cord o Spina bifida ➢ In neurogenic shock, the muscles in the walls of the blood vessels are cut off from the sympathetic nervous system and nerve impulses that cause them to contract. All vessels below the level of the spinal injury dilate widely, increasing the size and capacity of the vascular system and causing blood to pool. The available 6 L of blood in the body can no longer fill the enlarged vascular system. ➢ Even though no blood or fluid has been lost, perfusion of organs and tissues becomes inadequate, and shock occurs. ▪ Anaphylactic shock ➢ Occurs when a person reacts violently to a substance to which he or she has been sensitized. ➢ Sensitization means becoming sensitive to a substance that did not initially cause a reaction. Each subsequent exposure after sensitization tends to produce a more severe reaction. Common causes include: o Injections (tetanus antitoxin, penicillin) o Stings (honeybee, wasp, yellow jacket, hornet) o Ingestion (shellfish, fruit, medication) o Inhalation (dust, pollen) o Anaphylactic shock can develop within minutes or even seconds of contact with the substance ➢ Note that cyanosis (bluish color of the skin) is a late sign of anaphylactic shock. ▪ Psychogenic shock ➢ A patient in psychogenic shock has had a sudden reaction of the nervous system that produces a temporary, generalized vascular dilation, resulting in fainting, or syncope. ➢ Blood pools in the dilated vessels, reducing the blood supply to the brain. As a result, the brain ceases to function normally, and the patient faints. o Life-threatening causes include irregular heartbeat and brain aneurysm. o Non–life-threatening causes include receiving bad news, experiencing fear, or seeing unpleasant sights (like the sight of blood). o Hypovolemic shock ▪ Hypovolemic shock is the result of an inadequate amount of fluid or volume in the system. ▪ There are hemorrhagic causes and nonhemorrhagic causes. Hypovolemic shock also occurs with severe thermal burns. Intravascular plasma is lost. Plasma leaks from the circulatory system into the burned tissues that lie adjacent to the injury. ▪ Dehydration, the loss of water or fluid from body tissues, can cause or aggravate shock. Fluid loss may be a result of severe vomiting and/or diarrhea. 61. Review indications for the use of the AED and the indication for CPR. Remember the ratios for the different age groups. Compression to ventilations, depth of compressions, hand position, number of cycles with one and two rescuers. o CPR ➔ used to establish artificial ventilation and circulation in a patient who is not breathing and has no pulse. ▪ Adult CPR is performed by performing 30 high quality compressions at least 2” deep at the rate of 100 per minute followed by 2 breaths that ensure adequate chest rise (for both 1 rescue or 2 rescuers). With a second rescuer, make one ventilate). CPR should be performed for 2 minute intervals. ➢ For adults, hands should be placed in the lower 2/3 of the sternum. ▪ For a child perform 30 compressions (approx 2” depth) to 2 ventilations for one rescuer and 15:2 for 2 rescuers. For an infant perform 30:2 (approx. 1 ½”) for 1 rescuer and 15:2 for 2 rescuers. ➢ For children and infants, two finger method should be placed in the middle of the sternum with one finger touching the nipple line. ▪ Give CPR when a person has no pulse. ➢ One Rescuer ADULT/CHILD: 30 compressions: 2 ventilations ➢ Two Rescuers ADULT give 30 compressions: 2 ventilations and CHILD/INFANT give 15 compressions: 2 ventilations o With a child/infant, do 10 cycles o With an adult, do 5 cycles o AED➔ a device that detects treatable life-threatening cardiac arrhythmias (ventricular fibrillation and ventricular tachycardia) and delivers the appropriate electrical shock to the patients). It should be applied to any cardiac arrest patient as soon as possible. ▪ AEDs can be used in children using the pediatric-sized pads and a dose-attenuating system. However, if these are unavailable, you should use an adult AED. 62. Pay particular attention to the ratios for intubated patients and the neonate o Rescue Breathing for ▪ Intubated Patients ➔ deliver one rescue breath every 6 to 8 seconds. ▪ Neonate ➔ A compression to ventilation ratio of 3:1 should be used, which yields 120 actions per minute (90 compressions & 30 vents) ▪ Infant ➔ covering both the nose and the mouth of the infant with the mask, deliver breaths at a rate of 40 to 60 breaths/min. 63. Review the primary differences between the causes of cardiac or respiratory in adults and children o Recognize Respiratory arrest vs. cardiac arrest ▪ Cardiac arrests in children frequently result from respiratory failure. That is why it is important to give rescue breaths to a child who is not breathing but has a pulse! ▪ While in adults, they often go straight to cardiac arrest (have no pulse and stop breathing) 64. Review kinetic energy, potential energy, force, and work o Three concepts of energy are typically associated with injury: potential energy, kinetic energy, and work ▪ Potential energy ➔is the product of mass (weight), force of gravity, and height; it is mostly associated with the energy of falling objects. ▪ Kinetic Energy ➔ is the work of a moving object. Kinetic energy reflects the relationship between the mass (weight) of the object and the velocity (speech) at which it is traveling. According to the equation for kinetic energy, the energy that is available to cause injury doubles when an object’s weight doubles but quadruples when its speed doubles. ▪ Force ➔ any interaction which tends to change the motion of an object. ▪ Work ➔is defined as force acting over a distance. Forces that bend, pull, or compress tissues beyond their inherent limits result in the work that causes injury. o Example: if the worker falls, potential energy is converted to kinetic energy. As the worker hits the ground, kinetic energy is converted into work that is the work of bringing the body to a stop and thereby fracturing bones and damaging tissues. 65. Review the following terms hypoperfusion, hypoxemia, cyanosis, fibrin, fibrinogen, plasminogen,dysrhythmia, hypoxia, perfusion and hyphema o Shock (hypoperfusion) ➔means a state of collapse and failure of the cardiovascular system. It is a condition that occurs when the level of tissue perfusion decreases below that needed to maintain normal cellular functions. o Hypoxemia ➔ a deficiency if oxygen in the blood. o Cyanosis ➔ Cyanosis reflects a decreased level of oxygen in the blood where a person starts to have a bluish gray skin color that is caused by a reduced level of oxygen in the blood ▪ Is a late sign of respiratory failure or shock. o Fibrin ➔an insoluble protein formed from fibrinogen during the clotting of blood. It forms a fibrous mesh that impedes the flow of blood. o Fibrinogen ➔a soluble protein present in blood plasma, from which fibrin is produced by the action of the enzyme thrombin. It helps in the formation of clots. o Plasma ➔is a sticky, yellow fluid that carries the blood cells and nutrients. This is the liquid portion of the blood. The primary components are water and proteins. All of the other components together make up 1% of the plasma. Water is 92% of plasma, proteins is 7% of plasma (major protein is albumin which functions to regulate oncotic pressure), oxygen, carbon dioxide, and nitrogen. o As red blood cells begin to clump together to form a clot, fibrinogen ➔reinforces the clumped red blood cells. o Plasminogen ➔ the inactive precursor of the enzyme plasmin, present in blood. It is released from the liver and is a zymogen, but active when it gets converted to plasmin. o Dysrhythmia ➔ an abnormality in an otherwise normal rhythmic pattern. o Hypoxia ➔ a dangerous condition in which the body tissues and cells do not have enough oxygen. o Perfusion➔ circulation of blood within an organ or tissue in adequate amounts to meet current needs of the cells o Hyphema➔ bleeding into the anterior chamber of the eye, obscuring all parts of the iris. Common in blunt trauma and may cause seriously impaired vision. 66. “I am a nose bleed. Please treat me” o Epistaxis ➔ or nosebleed, is a common emergency. Occasionally, it can cause enough of a blood loss to send a person into shock. Much of the blood may pass down the throat into the stomach as the patient swallows and they may become nauseated and start vomiting the blood, which is sometimes confused with internal bleeding. o Treatment: ▪ How to treat epistaxis: Help the patient to lean forwadr with the head tilted forward. This position stops the blood from trickling down the throat or being aspirated into the lungs. Apply direct pressure (for 15 min) by pinching the fleshy part of the nostrils together. An alternative method is to use pressure with a rolled gauze bandage between the upper lip and gum. Apply ice over the nose. Maintain pressure until bleeding is controlled. 67. How are internal and external bleeds treated o Internal Bleeding ▪ Determine if there is internal bleeding, some signs include: hematemesis (vomiting blood), hemoptysis (coughing up blood), melena (black, foul-smelling, tarry stool that contains digested blood) and then transport the patient immediately. They require surgery for proper treatment. o External Bleeding ▪ Always attempt to determine the amount of external blood loss. ▪ Recognize type of bleed ➢ Bright red, spurting blood = arterial bleed. ➢ Dark red, flowing blood = venous bleed. ➢ Slow, oozing blood = capillary bleed. ▪ Several methods are available to control external bleeding. ➢ Direct, even pressure and elevation ➢ Pressure dressings and/or splints ➢ Tourniquets ➢ It will often be useful to combine these methods. 68. Review the following terms hematoma, laceration, incision, avulsion, evisceration, contusion, amputations o Hematoma - a mass of blood in the soft tissues beneath the skin, sign of internal bleeding. Closed skin injury. It is the collection of blood within the tissue from damaged blood vessels. ▪ Names are bases on location in brain : ➢ Subdural Hematoma - below the dura mater bleeding due to tearing of blood vessels on the surface of brain. Due to bleeding from bridging veins. ➢ Epidural Hematoma- above the dura mater usually rapid bleeding * bleeding between skull and protective covering of brain. Du to bleeding of middle meningeal artery. ➢ Intracerebral Hematoma- Bleeding within the brain parenchyma (tissue) o Laceration – is a jagged cut caused by a sharp object or a blunt force that tears the tissue. Open skin injury. They vary in depth. o Incision – is a sharp, smooth cut. Open skin injury. o Avulsion – loose flap of skin. Separates various layers of soft tissue (usually between the subcutaneous layer and fascia) so that they become either completely detached or hang as a flap. Often there is significant bleeding. Never remove an avulsion skin flap, regardless of its size. Open skin injury o Evisceration – organs protrude from the skin o Contusion – bruising or ecchymosis (most common in head, extremity, pelvic, and abdominal injuries). Closed skin injury. o Amputation - an injury in which part of the body is completely severed. You can easily control the bleeding from some amputations, such as the fingers, with direct pressure and pressure dressings. If there is massive bleeding, you will need to treat the patient for hypovolemic shock. 69. Hello I am a mucous membrane. Do you know where I can be found? o Mucous Membrane ➔ the lining of body cavities and passages that are in direct contact with the outside environment. They are similar to skin but provide a protective barrier against bacterial invasion and secrete mucus. ▪ Includes: eyes, mouth, whole GI tract, anus, vagina 70. Know the appropriate treatment for avulsions, amputations, lacerations, eviscerations, hematomas, burns o Treating Avulsions ▪ clean the wound surface ▪ fold skin back to normal position ▪ control bleeding ▪ apply bulky pressure dressing o Treating Amputation ▪ Wrap amputated parts in dry (or moist, depending on medical direction), sterile gauze dressing. ▪ Apply a tourniquet approximately 2” proximal to the site of amputation, and transport rapidly. ▪ Put in a plastic bag. Keep the amputated part cool by placing over ice or in a cooler, but do not freeze it. Take the amputated part with the patient o Treating Lacerations ▪ Depending on where it is, apply pressure bandage roller gauze and transport. o Treating Eviscerations ▪ Need to be covered with a moist, sterile dressing or gauze, and then cover that with an occlusive dressing sealed on all sides. Maintain temperature by insulating the wound with layers of thicker dressing because exposed organs lose body heat and moisture rapidly. ▪ If there is no spinal injury, position the patient in a supine position with knees bent, which helps to relax abdominal muscles. o Treating Hematomas ▪ Death will follow very rapidly without surgery so transport promptly and give oxygen to patient o Treating Burns (There are many types of burn) ▪ If it’s a chemical burn that went into the eye and was caused by an alkali or a strong acid, you should irrigate the eyes for at least 20 minutes. ▪ For burns on skin, after determining that breathing, and circulation are intact, you should cool the burn with water ▪ Provide high flow oxygen and keep the patient warm. 71. Know all about the meninges and CSF o Meninges ➔ the three membranes covering the brain and spinal cord: dura mater, arachnoid, and pia mater ▪ Dura mater ➔ the outermost, toughest of the three meninges (membranes) of the brain and spinal cord) ▪ Arachnoid ➔ the delicate membrane interposed between the dura mater and the pia mater ▪ Pia mater ➔ the innermost of the three meninges covering the brain and spinal cord o Cerebral Spinal Fluid (CSF) ➔ fluid within the ventricles of the brain, the subarachnoid space, and the central canal. Acts as shock absorber; there is 125 to 150 ml of CSF in brain at any given time. CSF is a plasma like clear fluid circulation in and around the brain and spinal cord. 72. Review these terms peritonitis, hematuria, hemoptysis, hematochezia, hematemasis, guarding o Peritonitis ➔inflammation of peritoneum (membrane lining the abdominal cavity and surrounding the organs within it) o Hematuria➔ blood in the urine ▪ *common finding of an injured kidney o Hemoptysis ➔ coughing up blood ▪ *could be a sign of pulmonary emboli ▪ Sign of internal bleeding o Hematochezia ➔ passage of bloody feces o Hematemesis ➔ vomiting blood (can be red or dark red) ▪ Sign of internal bleeding o Guarding ➔ there are 2 types of guarding ▪ Involuntary Guarding abdominal wall muscle contraction caused by inflammation of the peritoneum (peritonitis) that the patient cannot control. Also called rigidity ▪ Voluntary Guarding Conscious contraction of the abdominal muscles in an attempt to prevent painful palpation 73. Know these terms. Bursa, fascia, tendons, ligaments, cartilage o Bursa ➔ a fluid-filled sac or sac-like cavity, especially one countering friction at a joint. o Fascia ➔The fiber-like connective tissue that covers arteries, veins, tendons, and ligaments o Tendon ➔ connects muscle to bone o Ligament ➔connects bone to bone o Cartilage ➔ cushion between the bones 74. Review the indications and contraindications for PASG/MAST (remember the hand out I gave you?) o MAST pants, officially known as military anti-shock trousers (also known as pneumatic anti-shock garmets, PSAG) contraindications (Do not use the PASG if any of the following conditions exist) ▪ Pregnancy, Pulmonary edema, Acute heart failure, Penetrating chest injuries, Groin injuries, Major head injuries, A transport time of less than 30 minutes 75. How are dislocations treated? o Dislocation is a disruption of a joint in which the bone ends are no longer in contact. o Signs of Dislocation: Marked deformity, swelling, pain aggravated by motion, tenderness on palpation, near complete loss of motion, numbness, impaired circulation. o For treatment, you should always split all fractures, dislocations, sprains. ▪ Remove clothing from area; note neurovascular condition; cover wounds with dry, sterile; do not move before splinting extremity, unless in danger; pad all rigid splints; maintain manual stabilization; if you encounter resistance, splint in position; stabilize all suspected spinal in neutral, in-line; when in doubt splint. o For shoulder dislocations: ▪ Humeral head is usually anteriorly. It is hard to stabilize due to pain. Bringing arms to the chest hurts therefore stabilize where it is most comfortable for the patient. 76. Review the terms ecchymosis, crepitus, involuntary and voluntary guarding o Ecchymosis➔ blood or black discoloration under skin from bruising or bleeding . Alsoknown as aka contusion or bruising. o Crepitus ➔ A grating or grinding sensation can be felt and sometimes even heard when fractured bone ends rub together. o Involuntary Guarding ➔ abdominal wall muscle contraction caused by inflammation of the peritoneum (peritonitis) that the patient cannot control. Also called rigidity o Voluntary Guarding ➔ Conscious contraction of the abdominal muscles in an attempt to prevent painful palpation 77. Know the types of traumatic injuries that may result in Hypovolemic shock ▪ Hypovolemic shock is the result of an inadequate amount of fluid or volume in the system. ▪ There are hemorrhagic causes and nonhemorrhagic causes. Hypovolemic shock also occurs with ➢ Severe lacerations and severe thermal burns. o Intravascular plasma is lost. Plasma leaks from the circulatory system into the burned tissues that lie adjacent to the injury or significant blood volume lost. ➢ Dehydration, the loss of water or fluid from body tissues, can cause or aggravate shock. Fluid loss may be a result of severe vomiting and/or diarrhea. 78. I am very very very cold. What could my temperature be? o Hypothermia is a core temperature of the body falls below 95°F (35°C) the internal body temperature becomes abnormally low. Normal body temperature is 98.6°F (37°C). ▪ It is considered a serious condition and often fatal ▪ At 86°F (30°C) the brain can survive without perfusion for about 10 minutes. ▪ Mild hypothermia occurs when the core temperature is between 90°F and 95°F (32°C and 35°C). ➢ The patient is usually alert and shivering. Pulse rate and respirations are usually rapid. Skin may appear red, pale, or cyanotic. ▪ More severe hypothermia occurs when the core temperature is less than 90°F (32°C). ➢ Shivering stops. Muscular activity decreases. o The key to treating hypothermic patients is to stabilize vital functions and prevent further heat loss. Do not attempt to rewarm patients who have moderate to severe hypothermia because they are prone to developing arrhythmias. 79. Review the way heat can be lost from the body ( convection, evaporation etc) o There are five ways the body can lose heat: ▪ Conduction ➔ Direct transfer of heat from a part of the body to a colder object by direct contact. Heat can also be gained if the substance being touched is warm. ▪ Convection ➔ Transfer of heat to circulating air, as when cool air moves across the body ▪ Evaporation ➔Conversion of any liquid to a gas. Evaporation is the natural mechanism by which sweating cools the body. Measures should be taken to keep a person dry if he or she is too cold. ▪ Radiation ➔Transfer of heat by radiant energy Radiant energy is a type of invisible light that transfers heat. ▪ Respiration ➔ Loss of body heat during normal breathing. Warm air in the lungs is exhaled into the atmosphere and cooler air is inhaled. 80. How does the body protect against heat loss? o To protect against heat loss, the ▪ Blood vessels in the skin constrict and blood is shunted from the extremities to more important vital organs. ▪ Body will shiver to increase metabolism and generate more heat through muscular activity o In response to being cold, the body shivers 81. Hello I am the diving reflex. Please know all about me o The diving reflex (slowing of the heart rate caused by submersion in cold water) may cause immediate bradycardia (slow heart rhythm). The diver may be able to survive for an extended period of time under water, thanks to a lowering of the metabolic rate associated with hypothermia. Continue full resuscitation efforts no matter how long the patient has been submerged. ▪ Question from Quizlet: The EMT shows she understands the concept of the mammalian diving reflex by stating: "It may provide benefit to the patient by diverting oxygen-rich blood to the brain and heart." 82. Review the brown recluse and black widow o Only two spiders native to the United States—the female black widow spider and the brown recluse spider—deliver serious, even life-threatening bites. o Brown Recluse ➔ The venom is not neurotoxic but cytotoxic; it causes severe local tissue damage. ▪ Appearance: Dull brown in color and 1″ long. The short- haired body has a violin-shaped mark, brown to yellow in color, on its back. ▪ Bite Mark: Typically, the bite is not painful at first but becomes so within hours. The area becomes swollen and tender, developing a pale, mottled, cyanotic center and possibly a small blister. A scab of dead skin, fat, and debris will form and dig down into the skin, producing a large ulcer that may not heal unless treated promptly. o Black Widow ➔ its venom is poisonous to nerve tissues (neurotoxic) ▪ Appearance: The female black widow spider is fairly large, measuring approximately 2″ across with its legs extended. It is usually black with a distinctive, bright red-orange marking in the shape of an hourglass on its abdomen. The female is larger and more toxic than the male. ▪ Bite Mark: The bite is sometimes overlooked. If the site becomes numb right away, the patient may not even recall being bit; however, most black widow spider bites cause localized pain and symptoms, including agonizing muscle spasms. 83. Neonate resuscitation (remember it is different from infants) o When performing CRP on a newborn, a compression to ventilation ratio of 3:1 should be used; this will yield a total of 120 “actions” per minute o If chest compressions are required, use either the hand-encircling technique or the two-finger technique. ▪ Coordinate chest compressions with ventilations at a ratio of 3:1. ▪ This will yield a total of 120 “actions” per minute (90 compressions and 30 ventilations). o If the newborn’s cardiac arrest is believed to be of cardiac origin, consider a higher ratio (ie, 15:2). Adequate ventilation is absolutely critical to successful resuscitation of the neonate. 84. Review the stages of labor o There are three stages of labor: ▪ Dilation of the cervix, ▪ Delivery of the infant ▪ Delivery of the placenta. o The first stage begins with the onset of contractions as the fetus enters the birth canal and ends when the cervix is fully dilated. o The second stage of labor begins when the fetus begins to encounter the birth canal and ends when the infant is born (spontaneous birth). o The third stage of labor begins with the birth of the infant and ends with the delivery of the placenta. 85. What are the differences between pre-eclampsia & eclampsia & what stage of pregnancy they most commonly occur o Pre-eclampsia➔ One complication that occurs most commonly in patients who are pregnant for the first time is preeclampsia, or pregnancy-induced hypertension. Signs and Symptoms include headache, visual changes, and swelling of the hands and feet. ▪ This condition can develop between the 20th and 30th week of gestation. o Eclampsia ➔ a condition characterized by seizures that occur as a result of hypertension ▪ Not treating pre-eclampsia can lead to eclampsia so therefore it occurs in the 30th+ week of pregnancy (late stage). Often times, the infant will be prone to having seizures during its lifetime. 86. Review the following terms imminent birth, nuchal cord, mucus plug, crowning, amniotic sac o Imminent Delivery/Birth ➔during the 2nd stage of labor, when the fetus is progressing through the bitch canal, the head presses against the woman’s rectum; this gives her the urge to move her bowels and is a sign of imminent delivery. Delivery will occur any moment! ▪ One of the most reliable indicators of imminent delivery is when the patient states, I’m having this baby now!” This is especially true in women who have given birth in the past. ▪ This statement, coupled with the patient’s urge to push or move her bowels, should promt you to prepare for imminent delivery. o Nuchal Cord ➔ umbilical cord that’s wrapped around the infant’s neck and can cause the infant to strangle ▪ Usually, you can slip the cord gently over the infant’s delivered head. If not, you must cut it. o Mucus Plug ➔ During pregnancy, the cervix contains a mucous plug that seals the uterine opening, preventing contamination. o Crowning ➔ appearance of the infant’s head at the vaginal opening during labor o Amniotic Sac➔ also called the bag of waters, it is a fluid filled or baglike membrane where the fetus develops ▪ Contains about 500 to 1,000 mL of amniotic fluid, which helps insulate and protect the floating fetus. ▪ The amniotic fluid is released in a gush when the sac ruptures, usually at the beginning of labor. 87. Know the appropriate treatment for a mother who is bleeding after delivery. Also know what is considered normal blood loss after delivery o After delivery of the placenta and before transport, place a sterile pad or sanitary napkin over the vagina and straighten the mother’s legs. You can help to slow bleeding by gently massaging the mother’s abdomen with a firm, circular, “kneading” motion. You should be able to feel a firm, grapefruit-sized mass in the lower abdomen, called the fundus (dome-shaped top of the uterus) o Normal Blood Loss before the delivery of the placenta is about 500 mL. Anything more than that or if the placenta does not deliver, you must transport the mother and infant to the hospital promptly. 88. What is the Pediatric Assessment Triangle and what are the components? Also know what it is used for. (Remember to other handout I gave?) o Pediatric Assessment Triangle ➔ is used to form a general impression of pediatrics o It is a 15- to 30-second structured assessment tool that allows you to rapidly form a general impression without touching the patient. o PAT consists of three elements and requires no equipment: ▪ Appearance (muscle tone and mental status) ➢ Note the level of consciousness or interactiveness and muscle tone. ➢ An infant or child with a normal level of consciousness will act appropriately his or her age, exhibiting good muscle tone and maintaining good eye contact. ➢ Poor muscle tone or poor eye contact can mean an abnormal level of consciousness. ➢ TICLS mnemonic can help determine if the patient is sick: o Tone, Interactiveness, Consolability, Look or gaze, Speech or cry ▪ Work of breathing ➢ Increases as the body attempts to compensate for abnormalities in oxygenation and ventilation Increased work of breathing often manifests as: Tachypnea, Abnormal airway noise, Retractions of the intercostal muscles or sternum ▪ Circulation to the skin ➢ When cardiac output fails, the body shunts blood from areas of lesser need (such as skin) to areas of greater need (such as organs). ➢ Pallor of the skin and mucous membranes may be seen in compensated shock. May also be a sign of anemia or hypoxia ➢ Mottling is another sign of poor perfusion. ➢ Cyanosis reflects a decreased level of oxygen in the blood. o Is a late sign of respiratory failure or shock. 89. How do you treat a bradycardic infant o Bradycardia is almost always an ominous sign in pediatric patients. o If the heart rate is slow (less than 60 bpm) or absent, especially in an unconscious infant or child, you must begin CPR immediately. o Without aggressive airway management, bradycardia may quickly progress to cardiopulmonary arrest. 90. What are the primary differences between croup and epiglottitis o Croup ➔Inflammation and swelling of the pharynx, larynx, and trachea. ▪ Typically seen in children between 6 months and 3 years of age. This disease is often secondary to an acute viral infection of the upper respiratory tract ▪ Easily passed between children ▪ Croup often responds well to the administration of humidified oxygen. o Epiglottitis ➔ Inflammation of the epiglottis as the result of a bacterial infection. ▪ More predominant in children but can also occur in elderly patients. ▪ Treat children gently and try not to make them cry. Do not attempt to suction the airway or place an oropharyngeal airway in the patient with suspected epiglottis. Do not put anything in their mouths. ▪ To force a patient with epiglottitis to lie supine may cause upper airway obstruction that could result in death. ▪ Position comfortably and provide high-flow oxygen. 91. Review terms cataracts, glaucoma, conjunctivitis, retinitis o Cataracts ➔ Clouding of the lens of the eye or its surrounding transparent membranes. o Glaucoma ➔intraocular pressure damages the optic nerve and inhibits the ability of the eye to transmit visual information properly. o Conjunctivitis ➔inflamed conjunctiva where the eye becomes red and inflamed. ▪ Quizlet: For a patient suffering from conjunctivitis, the EMT would expect to observe a/an: reddened membrane over the sclera. o Retinitis ➔inflammation of the retina in the eye, which may lead to blindness. 92. Review the following terms. Kyphosis, scoliosis, miosis, lordosis o Kyphosis - Curvature of the spine that causes the neck and shoulders to curve forward. It’s an exaggerated posterior curvature of the thoracic spine that causes significant back pain and limited mobility ▪ They require padding to keep the patient supine when immobilizing them. o Scoliosis - lateral curvature of the spine o Miosis ➔ excessive constriction of the pupil in the eye. Often occurs when a person is exposed to nerve gas or have taken opiates. o Lordosis ➔ is the inward curvature of a portion of the lumbar and cervical vertebrae column. 93. What is a AAA o Abdominal aortic aneurysm (AAA) ➔A condition in which the walls of the aorta in the abdomen weaken and blood leaks into the layers of the vessel, causing it to bulge. 94. Review the proper techniques for lifting and moving o For safely, lift and carry a patient, you and your partner must anticipate and understand every move, and each move must be executed in a coordinated matter. To avoid confusion, one person should call out all of the lifting commands. o General guidelines should be followed when lifting a patient: ▪ Keep your legs should width apart (15” apart) ▪ Keep your back in a straight, locked-in position ▪ Keep the weight as close to your body as possible ▪ Bend at the knees, not the waist, when lifting ▪ Avoid lifting and reaching at the same time ▪ Avoid twisting your body as you are lifting ▪ Lift with your palms facing up (power grip) ▪ Communicate with your partner (or team) at all times. o You may injure your back: If you lift with your back curved. If you lift with your back straight but bent significantly forward at the hips o Power lift ➔ Legs should be spread about 15″ apart (shoulder width). Place feet so that your center of gravity is properly balanced. With your back held upright, bring your upper body down by bending the legs. Grasp the patient or stretcher. Keep your arms the same distance apart as when hanging your arms at each side of your body. Lift the patient by raising your upper body and arms and straightening your legs until you are standing. Keep the weight you are lifting as close to your body as possible. Lifting by extending the properly placed flexed legs is the most powerful way to lift. 95. Know the different types of lifting & moving techniques & know the situations that would dictate the use of each o Power grip gets maximum force from hands. Palms up, Hands about 10″ apart, All fingers at same angle, Fully support the handle on your curved palm. o Draw sheet Method ➔ To lift a patient by a sheet or blanket: Center the patient. Tightly roll up excess fabric on the sides. Use that cylindrical handle to grasp the fabric and lift the patient. o Diamond carry ➔ uses one EMT at the head and one at the foot of the backboard, and one on each side of the torso o One-handed carry ➔ includes four or more rescuers each using one hand to support the backboard so that they are able to face forward as they are walking backboard should be used instead for a patient in cardiac arrest, who must be moved in supine position, and who must be immobilized. o Direct Carry: Face the patient while standing between the bed and the stretcher. Slide one arm under the patient’s neck and cup the patient’s shoulder. Your partner should slide his or her hand under the patient’s hip and lift slightly. You should then slide your other arm under the patient’s back, and your partner should place both arms underneath the patient’s hips and calves. Lift the patient in a smooth, coordinated fashion. Slowly walk the patient around, and position him or her over the stretcher. Slowly and gently lower the patient onto the stretcher. 96. Know the difference between shunts, G-tube, CS tube o Shunts ➔tubes that extend from the brain to the abdomen to drain excess cerebrospinal fluid that may accumulate near the brain. Helps to lower pressure in the brain. o Gastric Tube (G-tube) ➔an advanced airway adjunct that provides a channel directly into a patient's stomach, allowing for removal of gas, blood, and toxins and for instilling medications and nutrition. o Central venous catheter (CS tube) ➔ a venous access device with the tip of the catheter in the vena cava – is used for many types of home care patients, including those receiving chemotherapy, long-term antibiotic or pain management, high concentration glucose solutions, and hemodialysis. 97. Review the important elements of ambulance operations. Think parking, hazmat, wind direction etc o When parking an accident scene, park the ambulance 100 feet past the scene on the same side of the road. o At a hazmat incident, you should stop at a safe distance and park upwind or uphill from the incident. 98. Review the differences between entrapment, disentanglement, extrication, rescue o Entrapment➔ person is caught within a closed area with no way out or has a limb or other body part trapped. o extrication/disentanglement ➔ Removal of a patient from entrapment or a dangerous situation or position, such as removal from a wrecked vehicle, industrial accident, or building collapse. o Rescue ➔ the moment after the patient has been extricated when the patient is being removed and treated. 99. Recall operations of the use of the portable and mounted suction units o 100. Review the term START triage and all the tags that are assign to patients during a MCI o START triage Stands for Simple Triage And Rapid Treatment ▪ Uses a limited assessment of the patient’s ability to walk, respiratory status, hemodynamic status (pulse), and neurologic status ▪ START Triage colors: Red tag (immediate), Yellow tag (delayed), Green tag (minimal). ➢ The first step is performed on arrival at the scene by calling out to patients at the disaster site and then directing them to an easily identifiable landmark. The injured persons in this group are the walking wounded and are considered minimal (green) priority, or third-priority patients. ➢ The second step is directed toward nonwalking patients. You move to the first nonambulatory patient and assess the respiratory status. o If the patient is not breathing, you should open the airway by using a simple manual maneuver. A patient who still does not begin to breathe is triaged as expectant (black). If the patient begins to breathe, tag him or her as immediate (red), place the patient in the recovery position, and move on to the next patient. If the patient is breathing, a quick estimation of the respiratory rate should be made. ➢ The next step is to assess the hemodynamic status of the patient by checking for bilateral radial pulses. ➢ The final assessment is to assess the patient’s neurologic status by assessing the patient’s ability to follow simple commands. 101. Review the terms Cystitis, Cholecystitis, appendicitis, pancreatitis. Also know the signs and systems and the body system or organ they affect. o Cystitis ➔ is a bladder inflammation and is common, especially in women. Also called urinary tract infection (UTI). It is caused by bacterial infection. Patients usually have lower quadrant abdominal pain. They may report an urgency and frequency in urination . This can become a serious problem if infection spreads to the urethra or kidneys o Cholecystitis ➔ it is a gallbladder inflammation, patient has right upper quadrant pain and referred pain to the right shoulder. They will have a substantial elevation in temperature. o Appendicitis ➔ inflammation or infection in the appendix. This can cause tissues to die, causing an abscess, peritonitis, or shock. Pain is initially more generalized and dull. Pain later localizes to the right lower quadrant. ▪ Patient may complain of: nausea and vomiting, anorexia, fever, chills, rebound tenderness o Pancreatitis➔inflammation of the pancreas, caused by obstructing gallstone, alcohol abuse, or other diseases ▪ Signs and symptoms: severe pain in upper left and right quadrants, often radiating to the back, nausea, vomiting, abdominal distention , tenderness, sepsis or hemorrhage may occur. Look for fever or tachycardia. 102. Know the signs and symptoms of patients with Hypoglcemia and Hyperglycemia o Hyperglycemia is a state in which the blood glucose is above normal. ▪ The result of a lack of insulin, which causes excessive amounts of glucose to remain in the blood ▪ Untreated, it results in DKA. ▪ Signs and symptoms include: ➢ History: Excessive food intake, insufficient insulin dosage, gradual onset (hours to days), warm and dry skin, infection is common ➢ Gastrointestinal tract: Dehydration; lack of appetite; weakness, nausea, and vomiting ➢ Respiratory system: Rapid, deep (Kussmaul) respirations; sweet, fruity breath odor ➢ Cardiovascular system: Normal to low blood pressure; rapid, weak, and thread pulse ➢ Nervous system: Restless; possible progression to coma; abnormal or slurred speech; unsteady gait ➢ Response to treatment: Gradual, 6–12 hours following medical treatment o Hypoglycemia is a state in which the blood glucose is below normal. ▪ Untreated, it results in unresponsiveness and eventually hypoglycemic crisis. ▪ Signs and symptoms include: ➢ History: Insufficient food intake; excessive insulin dosage; rapid onset (minutes); pale, cool, moist skin ➢ Gastrointestinal tract: Absence of thirst and intense hunger ➢ Respiratory system: Normal to shallow or rapid respirations ➢ Cardiovascular system: Normal to low blood pressure; rapid, weak pulse ➢ Nervous system: Altered mental status (aggressive, confused, lethargic, or unusual behavior); seizure, fainting, or coma; unsteady gait (weakness on one side of the body, may mimic stroke) ➢ Response to treatment: Immediate 103. Review Kussmaul, chyene-stokes respirations and know what they are associated with o Kussmaul Respirations ➔ Deep, gasping respirations commonly seen in patients with metabolic acidosis o Cheyne-Stokes Respirations ➔ When a patient breathes with an increasing rate and depth of respirations that is followed by a period of apnea 104. Know the differences between type 1 and type 2 diabetes o There are two types of diabetes. Both can affect many tissues and functions other than the body’s glucose regulating mechanism, & both require life-long medical management. ▪ Type 1 diabetes ➔ type of diabetic disease that typically develops in childhood and requires synthetic insulin for proper treatment and control. ➢ Patients do not produce insulin. ➢ Common Medications: Patients need daily injections of supplemental, synthetic insulin. ➢ In the past, referred to as insulin-dependent diabetes mellitus (IDDM) ➢ Age of Onset: Typically develops during childhood (“juvenile-onset diabetes”), though it can also develop later in life (child onset) ➢ Patients more likely to have metabolic problems and organ damage (eg, blindness, heart disease, kidney failure, and nerve disorders) ➢ S/S: Considered an autoimmune problem o The body is allergic to and destroys insulin-producing cells of pancreas’ endocrine glands ▪ Type 2 diabetes patients ➔ type of diabetic disease that typically develops in later life and often can be controlled through diet and oral medications. ➢ They produce inadequate amounts of insulin, or a normal amount that does not function effectively. ➢ Age of onset: Usually appears later in life (Adult-onset) ➢ Common Medication/Treatment: Treatment may be diet, exercise, oral medications (hypoglycemic agents), or supplemental insulin. o Non–insulin-type oral medications stimulate pancreas to produce more insulin. o Hypoglycemic agent administration may cause hypoglycemia in some patient (eg, those who are very active or who exercise a lot). ➢ In the past, referred to as non–insulin-dependent diabetes mellitus (NIDDM) or adult (maturity)-onset diabetes. Some patients, however, may require insulin. Easier to regulate and much more common ➢ The severity of diabetic complications depends on how high a patient’s average blood glucose level is and how early in life the diabetes began. Obesity increases the risk of diabetes. 105. Do you know these guys Histamines, Leukotrienes, allergens, antibody, & urticaria? If not, get to know them. o Histamines ➔ Substances released by the immune system in allergic reactions that are responsible for many of the symptoms of anaphylaxis, such as vasodilation. It is released into the bloodstream in response to the release of antibodies to a particular antigen. o Leukotrienes ➔ Chemical substances that contribute to anaphylaxis; released by the immune system in allergic reactions. o Allergen ➔ a substance that causes an allergic reaction. Some examples of antigens include microorganisms (such as bacteria, fungi, parasites, and viruses) and chemicals. o Antibody ➔ a protein produced by the body's immune system when it detects harmful substances, called antigens o Urticaria ➔ Small spots of generalized itching and/or burning that appear as multiple raised areas on the skin; hives. 106. Review the routes of poisoning and review the fastest and slowest routes o Fastest Route of poisoning ➔ intravenuous (injection) o Slowest Route of poisoning ➔ Inhalation, absorption, ingestion 107. Know examples of opioids, hypnotics, cholinergics, sympathomimetics o Opioids ➔ medicines with actions similar to morphine ▪ Include codeine, oxycodone (Percocet), heroin o Hynotics ➔substance that enhances sleep ▪ Includes flunitrazepam (Rohypnol) which is a common daterape drug, Alaprazolam (xanax) etc. o Cholinergics ➔ includes pilocarpine & nerve gas, organophosphate insecticides, Pilocarpine. These agents overstimulate normal body function controlled by the parasympathetic system resulting in salivation, mucous secretion, urination, crying and abnormal heart rate o Synpathomimetics ➔ includes epinephrine, speed, ecstasy, albuterol, cocaine, & methamphetamine. Drugs that mimic the effects of the sympathetic nervous system; hypertension, tachycardia, and dilated pupils 108. Know the common antidotes for the most common poisoning situations you may meet in the field. o Antidote for OPIOID OVERDOSE: only effective one are narcotic antagonists such as Naloxone (Narcan) o Antidote for SEDATIVE-HYPNOTIC DRUGS (Benzodiazepine overdose): Flumazenil that’s given intravenously o Antidote for CHOLINERGIC DRUGS (organophosphate, nerve gas agents): 2-PAM/atropine o Antidote for INGESTION OF POISON: activated charcoal 109. Know how and what organs are affected by the most common overdose you learned in lecture 110.Recall the factors that contribute to suicide 111. Know the appropriate action to take when caring for patients with behavioral emergencies 112.Review everything about PID 113.Know the signs & symptoms of patients with COPD, cardiogenic Shock, right sided heart failure and left sided heart failure 114.Review the terms index of suspicion, unresponsive, unconscious, base line vital signs, rapid body scan 115. Know how to recognize low vs high priority patients 116. Review the terms hepatitis, meningitis, tuberculosis, Hantavirus, Anthrax. Also know the signs and symptoms 117. Hey what do you know about Alpha, beta, gamma, and X-rays o The energy that is emitted from a strong radiologic source is alpha, beta, gamma (x-ray), or neutron radiation. ▪ Alpha ➔ is the least harmful penetrating type and cannot move through most objects. ▪ Beta ➔radiation is slightly more penetrating than alpha and requires a layer of clothing to stop it. ▪ Gamma (x-ray)➔ rays are far faster and stronger than alpha and beta rays. These rays easily penetrate through the human body and require lead or several inches of concrete to prevent penetration. 118. Hmmm!!! What do I know about WMD 119. Know the signs and symptoms and treatment of patient with the following: acute pulmonary edema, pulmonary embolism, pneumothorax tension pneumothorax sucking chest wound, exacerbation of COPD, 120. Recall all the adventitious lung sounds and what they may indicate 121. Review the following terms: angina pectoris, unstable angina, arteriosclerosis, atherosclerosis 122.Review the terms visceral and parietal 123.Know the different layers of the heart and where does the blood supply originate 124.How does a patient present after a seizure 125. Know the signs and symptoms of patients with head injuries and know what part of the brain can be affected based on the S/S presenting 126. Review the where blood supply for different parts of the heart originate 127. Review the terms status epilepticus and status asthmaticus. Also know the signs and symptoms and treatment 128. Review the terms referred pain, radiating pain, visceral pain, somatic pain Remember this review is not intended to replace a comprehensive period of study for your final exam. However, try to get the answers for each of these bullets as it would supplement the studies you have already done. Please read all question carefully. Also, it would be wise to ready the question and quickly establish what the question is asking and what topic is it addressing before you read the answer choices. It is natural to think that some of the answers are the same. They are actually not (unless it is a typo). If you are able to narrow it down to two choices one of the two is a “Distracter”. When you reach to this point read the question again. This may help you to identify the distracter and subsequently choose the correct answer. Once again look out for questions that include words like LEAST, MOST, EXCEPT. If an answer contains words or sentences that absolutely don’t make sense then that’s probably not the answer. Use this review wisely. It’s a bit long but it is worth going through in its entirety. If you have any questions please do hesitate to contact me. GOOD LUCK!!! [Show More]
Last updated: 1 year ago
Preview 1 out of 61 pages
Instant download

Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Nov 21, 2022
Number of pages
61
Written in
Additional information
This document has been written for:
Uploaded
Nov 21, 2022
Downloads
0
Views
49