*NURSING > EXAM REVIEW > Rasmussen College: NUR2392 MDC 2 Exam 3 Focused Review Modules 8, 9, & 10_LATEST,100% CORRECT (All)
Rasmussen College: NUR2392 MDC 2 Exam 3 Focused Review Modules 8, 9, & 10_LATEST,100% CORRECT
Document Content and Description Below
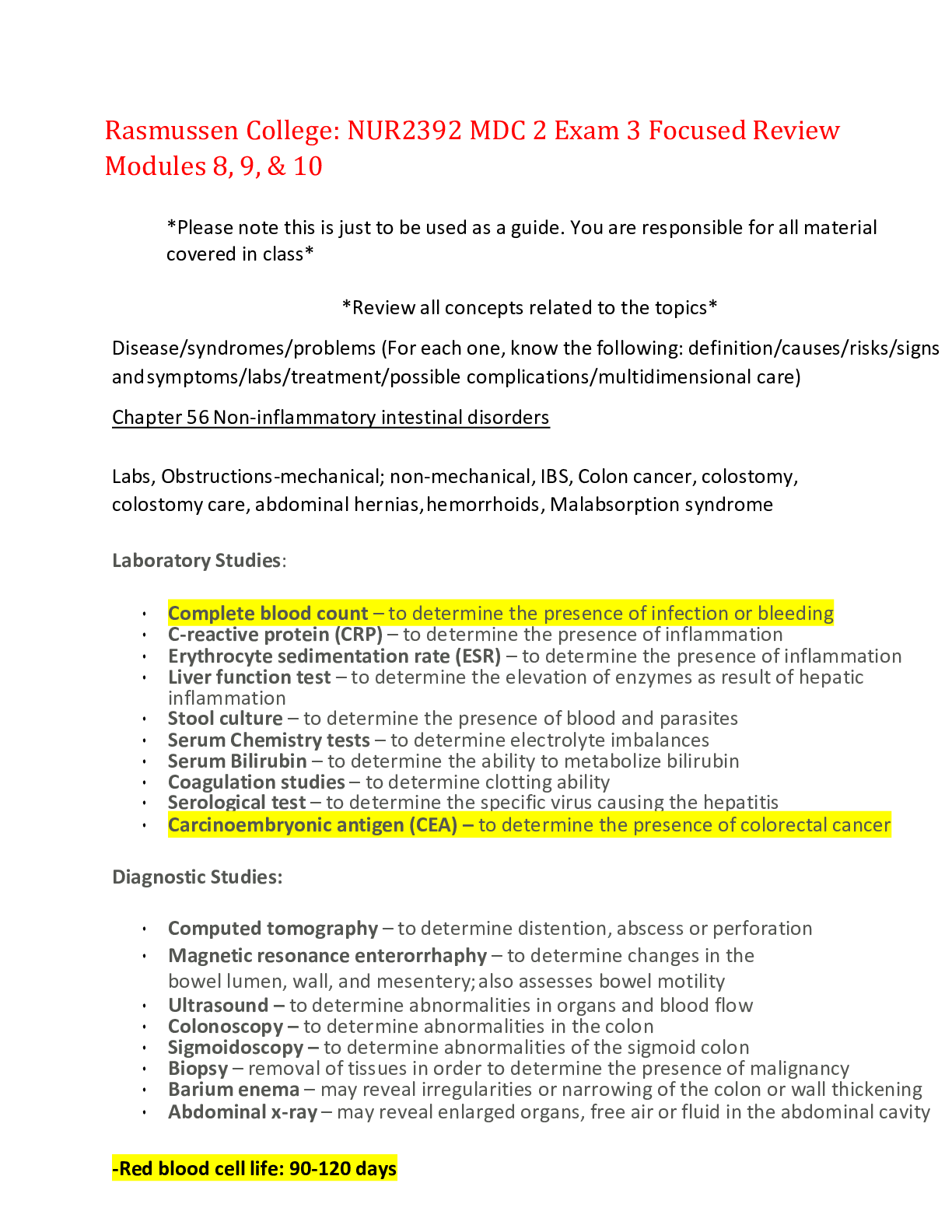
Rasmussen College: NUR2392 MDC 2 Exam 3 Focused Review Modules 8, 9, & 10 *Please note this is just to be used as a guide. You are responsible for all material covered in class* *Review all con... cepts related to the topics* Disease/syndromes/problems (For each one, know the following: definition/causes/risks/signs and symptoms/labs/treatment/possible complications/multidimensional care) Chapter 56 Non-inflammatory intestinal disorders Labs, Obstructions-mechanical; non-mechanical, IBS, Colon cancer, colostomy, colostomy care, abdominal hernias, hemorrhoids, Malabsorption syndrome Laboratory Studies: • Complete blood count – to determine the presence of infection or bleeding • C-reactive protein (CRP) – to determine the presence of inflammation • Erythrocyte sedimentation rate (ESR) – to determine the presence of inflammation • Liver function test – to determine the elevation of enzymes as result of hepatic inflammation • Stool culture – to determine the presence of blood and parasites • Serum Chemistry tests – to determine electrolyte imbalances • Serum Bilirubin – to determine the ability to metabolize bilirubin • Coagulation studies – to determine clotting ability • Serological test – to determine the specific virus causing the hepatitis • Carcinoembryonic antigen (CEA) – to determine the presence of colorectal cancer Diagnostic Studies: • Computed tomography – to determine distention, abscess or perforation • Magnetic resonance enterorrhaphy – to determine changes in the bowel lumen, wall, and mesentery; also assesses bowel motility • Ultrasound – to determine abnormalities in organs and blood flow • Colonoscopy – to determine abnormalities in the colon • Sigmoidoscopy – to determine abnormalities of the sigmoid colon • Biopsy – removal of tissues in order to determine the presence of malignancy • Barium enema – may reveal irregularities or narrowing of the colon or wall thickening • Abdominal x-ray – may reveal enlarged organs, free air or fluid in the abdominal cavity -Red blood cell life: 90-120 days -WBC life: 13-17 days Obstructions -Intestinal contents continue to accumulate above the obstruction which results in the distention of the abdomen. Results in decreased absorption of fluid and electrolytes. Mechanical Obstruction: The bowel is physically blocked by problems outside of the intestine (adhesions), in the bowel wall (Crohn’s disease), or in the intestinal lumen (tumors). • Complications of appendicitis • Hernias • Fecal impactions • Intussusception: telescoping of a segment of the intestine within itself • Volvulus (twisting of intestine) Nonmechanical: (paralytic ileus or a dynamic ileus) peristalsis is decreased or absent as a result of neuromuscular disturbance, resulting in a slowing of the movement or a backup of intestinal contents. • Complication of surgery: day 3/4, no bowel sounds • Hypokalemia Signs and Symptoms • Obstipation: severe constipation • Abdominal distention • Peristaltic waves • Borborygmic: gurgling or rumbling noise • High-pitched bowel sounds/none at all • Tachycardia • Hypokalemia Complications • Metabolic alkalosis/acidosis • Hypovolemia • Peritonitis (more so from strangulated obstruction) • Septic Shock • Increased intrabdominal pressure or ACS Interventions Non-surgical management o NG tube: at least every 4 hours, assess the patient with an NGT for proper placement, tube patency, and output (quality and quantity). Also assess for peristalsis. ▪ Confirmation by x-ray, aspirate contents and irrigate tube with 30 mL of normal saline every 4 hours. ▪ Decompresses the bowel by draining fluid and air. o IV fluid replacement ▪ 2-4L of isotonic (normal saline or lactated ringers) solution with added potassium o Give alvimopan (entereg) as prescribed for patients with postoperative ileus. Surgical Management o Exploratory laparotomy Colorectal Cancer: refers to colon and rectum, which together make up the large intestine • Most are adenocarcinomas • Etiology o Age>50 years o Genetic predisposition o Personal/family history o Familial adenomatous polyps • Assessment o Bleeding, anemia and change in stool (most common signs) o Fecal Occult Blood test (FOBT) yearly o Carcinoembryonic antigen (CEA) normal value is less than 5 ng/mL o Sigmoidoscopy every 5 years o Colonoscopy every 10 years • Potential for metastasis due to colorectal caner o Most common site is the liver • Potential for grieving • Planning and Implementation o Radiation o Chemo o Surgical management Colostomies o Healthy stoma should be reddish, pink, moist and about ¾ (2cm) from the abdominal wall Irritable Bowel Syndrome: functional GI disorder that causes chronic or recurrent diarrhea, constipation, and/or abdominal pain and bloating. o Sometimes referred to as spastic colon, mucous colon, nervous colon o Most common digestive disorder o Pain in the left lower quadrant, intermittent diarrhea o Diagnosed when there are symptoms in the absence of another diagnosis o Positive hydrogen breath test: indicating small-intestinal overgrowth or malabsorption of nutrients o Patients with IBS exhale an increased amount of hydrogen. Health Teaching o 30-40g of fiber daily o Promote normal bowel function o Stress reduction o Probiotics Drug therapy o Symptom specific Abdominal Hernias o Can happen from congenital muscle weakness and increase intra-abdominal pressure. o Surgical Interventions: herniorrhaphy Hemorrhoid o Swollen or distended veins in the anorectal area; can be internal or external. o Internal: lie above anal sphincter o External: lie below anal sphincter and can be seen o Results from… pregnancy, constipation with straining, obesity, heart failure, prolonged standing and/or sitting, and strenuous exercise and weight lifting. o Treatment o Increase dietary fiber o Stool softeners o Surgical management: Hemorrhoidectomy Malabsorption Syndrome o Associated with a variety of disorders in which the small intestine is unable to absorb nutrients o Causes Include…. o Trauma to intestine from surgery or infections o Lactose Intolerance o Congenital disorders o Radiation therapy o Medication o Crohns disease o Heart failure o Symptoms o Chronic diarrhea is classic symptom o Steatorrhea o Edema o Bone pain o Decreased libido o Interventions o Avoidance of substances that aggravate malabsorption o Supplementation of nutrients o Surgical management to correct disorder Chapter 57 Inflammatory intestinal disorders Labs, Appendicitis, peritonitis, gastroenteritis, ulcerative colitis, crohn’s disease, diverticulosis, diverticulitis, anorectal abscess, anal fissure, anal fistula, food poisoning, Inflammatory Bowel Disorder- potentially life threatening. Prompt treatment required. *Appendicitis: inflammation of the appendix. If left untreated, appendix may rupture and result in infection. o Mcburney’s point, abdominal pain that increase with cough or movement and is relieved by bending the right hip or the knees suggests perforation and peritonitis. -Surgical removal *Peritonitis: inflammation of the peritoneum, which can occur from a variety of causes. Dominant cause of death from surgical infections. Symptoms o Rigid, board like abdomen, abdominal pain, tenderness and distention o Lab assessment: WBC counts are elevated to 20,000/mm3 o Left untreated can lead to risk of infection, sepsis, and respiratory problems. o NG tube o Antibiotics o Surgical management o Exploratory laparotomy o Wound exploration Gastroenteritis- very common health problem that causes diarrhea and/or vomiting as a result of inflammation of the mucous membranes of the stomach and intestinal tract. It mainly affects the small bowel and can be causes by either viral or bacterial infection. o Norovirus is the leading foodborne disease that causes gastroenteritis. Chronic Inflammatory Bowel Disease: Ulcerative colitis and Crohn’s Disease Ulcerative Colitis- classified as an inflammatory bowel disorder that can occur anywhere in the GI tract. Inflammation and ulceration of the mucosa of the colon. Intestinal mucosa becomes hyperemic, edematous, and reddened and in more severe, the lining can bleed, and small erosions, or ulcers can occur. Abscesses can form and result in tissue necrosis. Continued edema and mucosal thickening can lead to a narrowed colon and possible a partial bowel obstruction. o Symptoms o Stool is bloody and mucous o Tenesmus (unpleasant urge to defecate) o Lower abdominal colicky pain o Malaise, anorexia, anemia, dehydration, fever, and weight loss o Complication o Hemorrhage o Nutritional deficiencies o Treatment o Nutritional therapy o Antidiarrheal o Salicylates o Steroids o Modify diet o Surgical management ▪ Restorative proctocolectomy with ileo pouch-anal anastomosis ▪ Total Proctocolectomy with a permanent ileostomy Crohn’s Disease- classified as an inflammatory bowel disease in which part of the GI tract becomes inflamed and can result in development of abscesses, fistulas, and fissures. Be especially on the lookout for S&S of peritonitis, small bowel obstruction, and nutritional/fluid imbalances. o Same symptoms as above o Steatorrhea (fatty diarrheal stools) o Complications o Fistulas o Nutritional deficiencies o Treatment o Anti-inflammatory medications o Immune system suppressors o Antibiotics o Antidiarrheal o Nutrition therapy o Surgical Management ▪ Laparotomy to remove damaged bowel ▪ Repair of fistulas o Fistulas: abnormal tracts between two or more body areas. They can be between the bowel and the bladder, between 2 segments of bowel, between the skin and bowel, or between the bowel and vagina. ▪ Pt requires at least 3,000 calories a day to promote healing of the fistula ▪ Increased risk for intrabdominal abscesses and sepsis Diverticular Disease- herniation or outpouching of the mucous membrane of the bowel caused by an increase in pressure within the colon. Diverticulosis: presence of many abnormal pouchlike herniations (diverticula) Diverticulitis: Inflammation or infection of diverticula o Symptoms o Left lower abdominal pain o Fever o Bleeding o Nausea o Nutritional therapy o While diverticulitis is active, provide a low-fiber diet and when inflammation resolves provide a high-fiber diet o Antibiotics o Colon resection with or without colostomy Anorectal abscess- localized area of induration and pus caused by inflammation of the soft tissue near the rectum or anus. Most often the result of the ducts of glands in the anorectal region. o Symptoms o Rectal pain o Inflammation signs and symptoms o Antibiotics o Incision and drainage o Encourage use of warm sitz baths, analgesics, bulk-producing agents, and stool softeners after the surgery to promote healing. Anal Fissure- develops from cracks or ulcers in the lining of the anal canal. Occur with straining to have a stool. Larger deeper fissures can be a result of another disorder or from trauma. Anal Fistula- abnormal tract leading from the anal canal to the perianal skin resulting from anorectal abscesses, which are caused by the obstruction of anal glands, tuberculosis, crohns disease, or cancer. Chapter 58 Liver problems Labs, Cirrhosis, hepatitis (viral-A, B, C, D), esophageal varices, fatty liver disease, NAFLD, NASH, liver trauma, liver cancer, liver transplant Cirrhosis- extensive, irreversible scarring of the liver, usually caused by chronic reaction to hepatic inflammation and necrosis. In compensated cirrhosis the liver is scarred and cellular regulation is impaired, but the organ can still perform essential functions without causing major symptoms. In decompensated, liver function is impaired with obvious signs and symptoms of liver failure. o Complications o Portal hypertension o Ascites (collection of free fluid within the peritoneal cavity caused by increased hydrostatic pressure from portal hypertension) and esophageal varices (occur when fragile, thin-walled esophageal veins become distended and tortuous from increased pressure) o Coagulation defects o Jaundice o PSE with hepatic coma o Hepatorenal syndrome o Spontaneous bacterial peritonitis o Encephalopathy o Symptoms o Fatigue, significant weight change, anorexia, vomiting, abdominal pain, jaundice, dry skin, edema, rashes --Hepatitis- inflammation of the liver resulting from a viral or bacterial infection, drug use, alcohol or exposure to chemicals. Hep. C is leading cause of cirrhosis in U.S. Hep B & D leading worldwide. NAFLD (nonalcoholic fatty liver disease): Most common cause of liver disease in the world o Assessments o AST, ALT, LDH o Alkaline phosphatase o GGT o Serum protein, albumin o ABD xrays, CT, MRI, MR elastography o Liver US, arteriography, EGD, ERCP Cancer of the Liver- usually results from metastasis from a primary site. Risk factors for cancer development include chronic hepatitis B or C infection, nutritional deficiencies, alcoholism, and smoking. Chapter 59 Biliary system and pancreas Cholecystitis- acute or chronic inflammation of the gallbladder. When the gallbladder is inflamed, trapped bile is reabsorbed and acts as a chemical irritant to the gallbladder wall. Caused by too much fat intake. o Acute Types: o Calculous (most common)- chemical irritation and inflammation result from gallstones (cholelithiasis) that obstruct the cystic duct, gallbladder neck, or common bile duct. o Alcalculous- typically associated with biliary stasis caused by any condition that affects the regular filling or emptying of the gallbladder. o Symptoms o Upper abdominal pain- radiates to the right shoulder o Pain triggered by eating o Chronic Cholecystitis: results when repeated episodes of cystic duct obstruction cause inflammation. Calculi are always present, the gallbladder becomes fibrotic and contracted, which results in decreased motility and deficient absorption. o Treatment o Extracorporeal shock wave lithotripsy o Cholecystectomy o Laparoscopic benefits: less recovery time, lower risk for infection o Promoting nutrition ▪ High-fiber, low fat diet ▪ Small frequent meals o Manage Pain ▪ Drug therapy ▪ Lithotripsy: breaks up gallstones o Diagnostics o Ultrasound o HIDA scan o ERCP o MRCP Pancreatitis- inflammation of the pancreas that can be classified as acute or chronic Acute- results from autodigestion of the pancreas o Complications o Hypovolemia o Hemorrhage o Acute kidney failure o Paralytic ileus o Shock o Diabetes o Symptoms o Abdominal pain o Jaundice o Gray-blue discoloration of the abdomen and periumbilical are and flank o Absent or decreased bowel sounds o Abdominal rigidity o Treatment o NPO and IV fluids o Opioids- 1st line of treatment o Histamine receptor antagonists o PPI’s o NG tube o Surgical: exploratory laparotomy and/or sphincterotomy Chapter 61 Assessment of Endocrine Negative feedback concept- control of hormone synthesis Hypothalamus: corticotropic hormone (CRH), thyroid releasing hormone (TRH), growth hormone releasing hormone, gonadotropic releasing hormone Pituitary: MASTER GLAND: thyroid stimulating hormone (TSH), prolactin, follicle stimulating hormone (FSH), Luteinizing hormone (LH), adrenocorticotropic hormone (ACTH), growth hormone (GH) o Posterior: Antidiuretic hormone (ADH), oxytocin o Communicates with thyroid Hypopituitarism: under secretion or failure of the pituitary gland to produce required hormones. o Most life-threatening- ACTH & TSH o Growth hormone stimulates liver to produce somatomedins that enhance growth activity o Deficiency of gonadotropins o Causes: o Trauma o Malnutrition o Weight loss o Adenoma tumor o Infection o Partial or total hypophysectomy o Congenital defects o Deficiency of hypothalamus releasing hormone • Treatments o Lifelong replacement of deficient hormones o Androgen therapy- gynecomastia can occur o Estrogen and progesterone o Growth hormone Hyperpituitarism: over secretion of the growth hormone which results in acromegaly or gigantism o Gigantism: extra growth hormone before puberty o Acromegaly: extra growth hormone after puberty -Post-op: assess neurologic status ADH- DI & SIADH disorders: released by posterior pituitary gland Diabetes Insipidus: disorder in which water loss is caused by antidiuretic hormone (ADH) deficiency or the inability of the kidneys to produce ADH creating a fluid and electrolyte imbalance. o Key concepts o Electrolytes- serum sodium-decreased o Serum osmolality- decreased o Dehydration o Increase in frequency of urination and excessive thirst (polydipsia) o Large amount of dilute urine with low specific gravity (under 1.005) o Hypernatremia o Treatment: vasopressin or desmopressin SIADH: excessive release of the ADH hormone which results in hyponatremia and excess body water o Key Concepts o Vasopressin secretes even when plasma osmolarity is low or normal o Causes kidneys to absorb more water o Concentrated urine o Fluid volume excess ▪ Tachycardia, hypertension, weight gain, crackles, muscle cramping, hyponatremia o Drug Therapy: Diuretics, hypertonic saline, demeclocycline Thyroid: T3, T4, Calcitonin o Control of metabolism o Calcium and phosphorus (always opposite) o Always look at T3 and T4 first, TSH will always be the opposite o Thyroid cancer: elevated thyroglobulin 1 Graves’ Disease (hyperthyroidism) o Causes o Iodine excess o Levothyroxine excess o Assessment: increased T3 and T4, hypertension, hyperthermia, grape eyes, exophthalmos, goiter, pretibial myxedema, tachycardia, palpitations, weight loss, AFIB, diaphoresis, diarrhea o Thyrotoxicosis: thyroid storm, early signs are agitation and confusion are early signs o Treatment o High protein, carbs, and calories with frequent meals and snacks, low fiber, no spicy foods, no caffeine o Methimazole, Propylthiouracil, SSKI (potassium iodide), beta blockers Hypothyroidism o Causes o Hoshimotos o Decreased iodine o Pituitary tumor o Assessment: Myxedema coma, CNS depression, hypotension, bradycardia, hypothermia, constipation, weight gain, alopecia o Myxedema coma risk factors: thyroidectomy, abrupt stop of levothyroxine o Treatment: levothyroxine for life, takes 4 weeks to work, noticeable changes in about 2 weeks Priority after thyroidectomy o Airway (laryngeal stridor, noisy breathing, hoarseness/weak voice) o Breathing (noisy) o Circulation (want: neutral head and neck alignment, HOB 30-45 degrees, no flexing) o Calcium that is low: HYPOcalcemia- less than 8.0 o Positive trousseaus and Chvostek’s signs Parathyroid: parathyroid hormone (PTH) o Regulates calcium and phosphorus metabolism by acting on bones, kidneys, GI tract o Increases bone resorption o Serum calcium levels determine PTH secretion Hyperparathyroidism: hypercalcemia o Assessment: kidney stones, osteoporosis, constipation, lethargic, fatigue o Causes o Non-cancerous growth o Enlargement of gland o Cancerous tumor o Calcium & vitamin d deficiency o Renal failure Hypoparathyroidism: hypocalcemia o Assessment: positive trousseaus, Chvostek’s signs, diarrhea, tingling of mouth o Causes o Autoimmune disease o Malabsorption syndrome o Chronic kidney disease o Malnutrition o Treatment- replacing calcium, vitamin D, and magnesium Adrenal: cortex: (mineralocorticoids)Aldosterone, (glucocorticoids) cortisol, androgens Medulla: (catecholamines) epinephrine, norepinephrine o Steroids control sugar, sex, sex and hair o Pheochromocytoma: benign tumor in adrenal gland from excessive epi and norepi Addison’s Disease: insufficient secretion of ACTH hormone (hyporcortisolism) (not enough steroids) o Assessment o Hyponatremia, hypokalemia, severe hypotension occurs from the blood volume depletion that occurs with the loss of aldosterone, hypoglycemia, weakness, hyperpigmentation o Causes o Autoimmune disorders o Cancer o AIDS o TBI o Sepsis & hemorrhage o Adrenalectomy o Drugs (sudden cessation of long-term high-dose glucocorticoid therapy) o Addisonian crisis: life-threatening event in which the need for cortisol and aldosterone is greater than the body’s supply; usually occurs in response to a stressful event, abrupt stop of steroids, hypotensive crisis o Treatment: add some steroids- especially when stressed, strenuous exercise, and sepsis o Add high protein, carbs, and sodium o Life-long hormone therapy Cushing’s Disease: (hypercortisolism) ACTH) disorder in which excess secretion of cortisol from the adrenal cortex occurs. May be a result of dysfunction in the adrenal cortex or anterior pituitary gland. o Assessment o Hypertension, hyperglycemia, hypernatremia, truncal obesity, moon face, buffalo hump, hirsutism, purple strieae, slow wound healing, risk for fractures from brittle bones/osteoporosis o Causes o Long-term therapy of steroids o Tumors o Small cell lung cancer o Treatment: control causes (cut out tumor or steroids-slowly decreased) Pheochromocytoma o Catecholamine-producing tumors arising in the adrenal medulla o Tumors produce, store, and release epi and norepi. Pancreas: insulin & glucagon o Islet cells o Exocrine and endocrine function o Somatostatin- inhibits release of glucagon and insulin from pancreas DIABETES MELLITUS (TYPE 1 & 2) Metabolic Syndrome o Hemoglobin A1C: levels of glucose over a 3-month period o Normal <6 o Hypoglycemia: capillary blood glucose Type 1: NO INSULIN is being made o Genetics Type 2: FEW INSULIN (insulin resistance) o Hemoglobin A1C: levels of glucose over a 3-month period o Normal <6 o Diet & genetics o B- BP meds or high BP o B-Blood sugar meds or high blood sugar (fasting over 100) o O-Obese waist size: 35+ female, 45+male o L-Lipids: high cholesterol panel o Treatment o Diet ▪ AVOID: Simple sugars (soda, candy, white bread/rice, juices) Bad carbs (low fiber, simple carbs) (white bread, pasta, fries, low-fat milk) ▪ GOOD: High fiber (complex carbs) BROWN (beans, rice, bread, peanut butter, whole grains o Exercise o Oral meds o Insulin (last line) Hyperglycemia o Assessment: polyuria (too much urine), polydipsia (too much drink), polyphagia (hunger) o Causes: o Acute: sugar of 115 or more o 4 S’s ▪ Sepsis ▪ Stress ▪ Skin insulin ▪ Steroids o Chronic: HgBA1c 6.5+ ▪ Diet simple sugar (white bread, soda, candy NO fiber) o 7 insulin rules o Peaks + Plates= give FOOD during peaks o Deadly hypoglycemia (70 or less) o NO peak NO mix= long acting o IVP/IV only = regular insulin ▪ R-REGULAR INSULIN ▪ R-RIGHT INTO THE VEIN o Draw up clear to cloudy ▪ Draw up regular insulin first and then NPH o Rotate locations, never aspirate o DKA- Type 1- sick days o Insulin Types o Long Acting- no peak, no mix, not food dependent ▪ Duration: 24 hours o NPH- Intermediate, NEVER IV, mix clear to cloudy, given 2x a day ▪ Duration 14+ hours ▪ Peak 4-12 hours o Regular- IV, ONLY IV insulin ▪ Duration 5-8 hours ▪ Peak 2-4 hours o Rapid- aspart, lispro, gluisine, most deadly w/ 15-minute onset, hyperglycemia accident ▪ Duration 3-5 hours ▪ Peak 30-90 minutes Hypoglycemia o Assessment: cool, pallor, diaphoresis, trembling & shaking, confusion, lethargic o Treatment: o Awake and NOT NPO: ask to eat: orange juice, soda, crackers, low fat milk o Sleep: Stab with IV D50 (Dextrose IV) o Reassess sugar in 15 minutes o Causes o Exercise o Alcohol o Insulin peak times [Show More]
Last updated: 1 year ago
Preview 1 out of 27 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Feb 11, 2022
Number of pages
27
Written in
Additional information
This document has been written for:
Uploaded
Feb 11, 2022
Downloads
0
Views
37


.png)