Pharmacology > STUDY GUIDE > Charles R. Drew University of Medicine and Science - PHARMA 620 Pharmacology Exam 2 Study Guide (All)
Charles R. Drew University of Medicine and Science - PHARMA 620 Pharmacology Exam 2 Study Guide
Document Content and Description Below
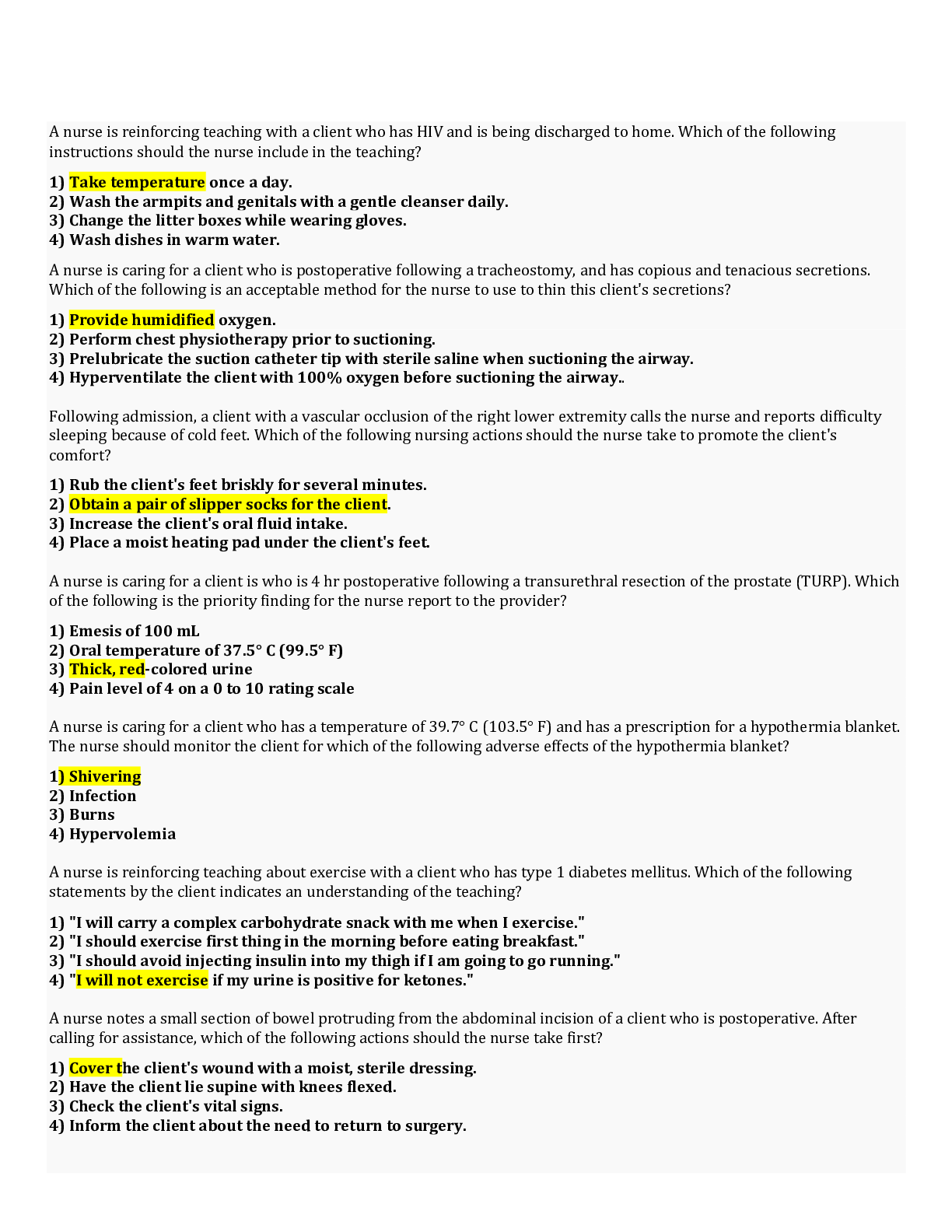
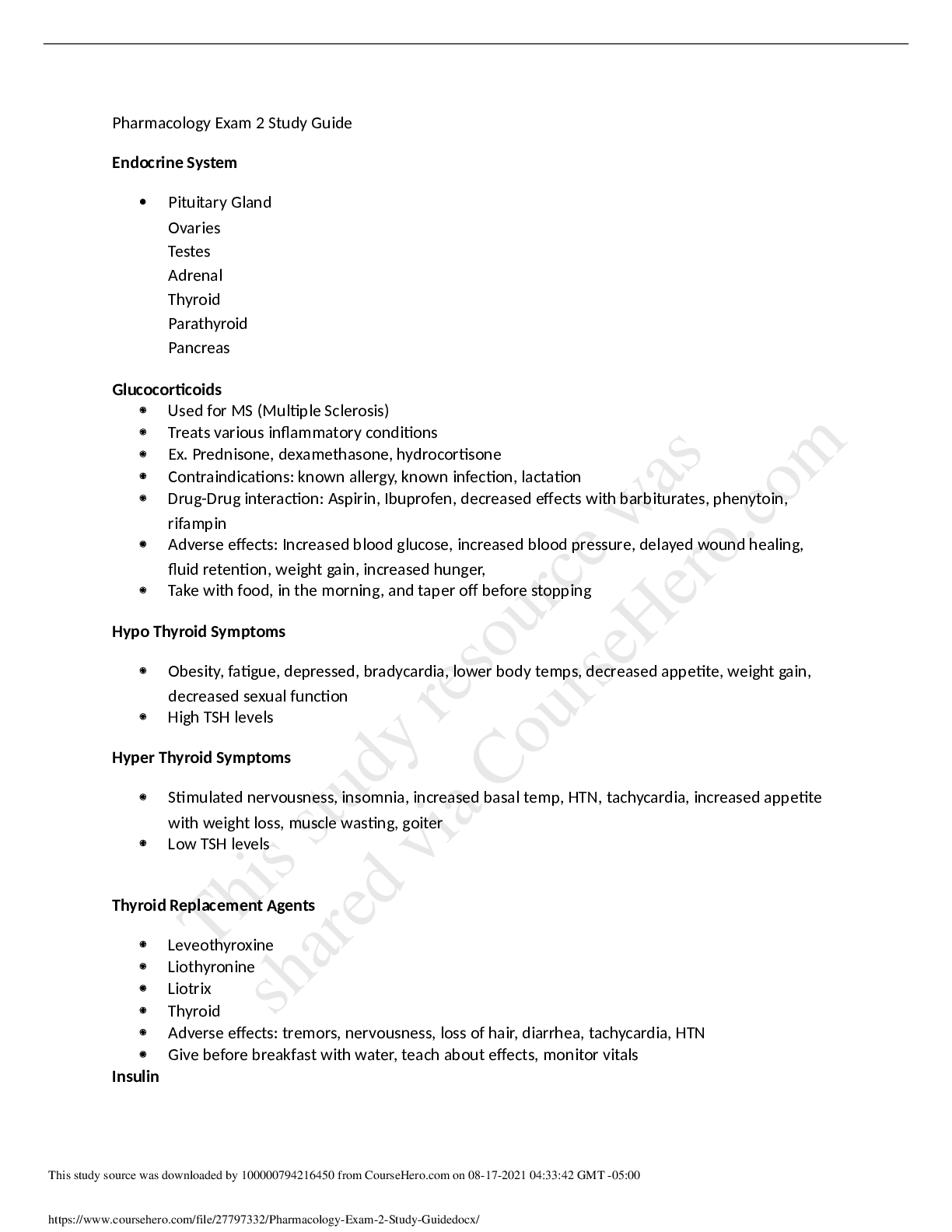
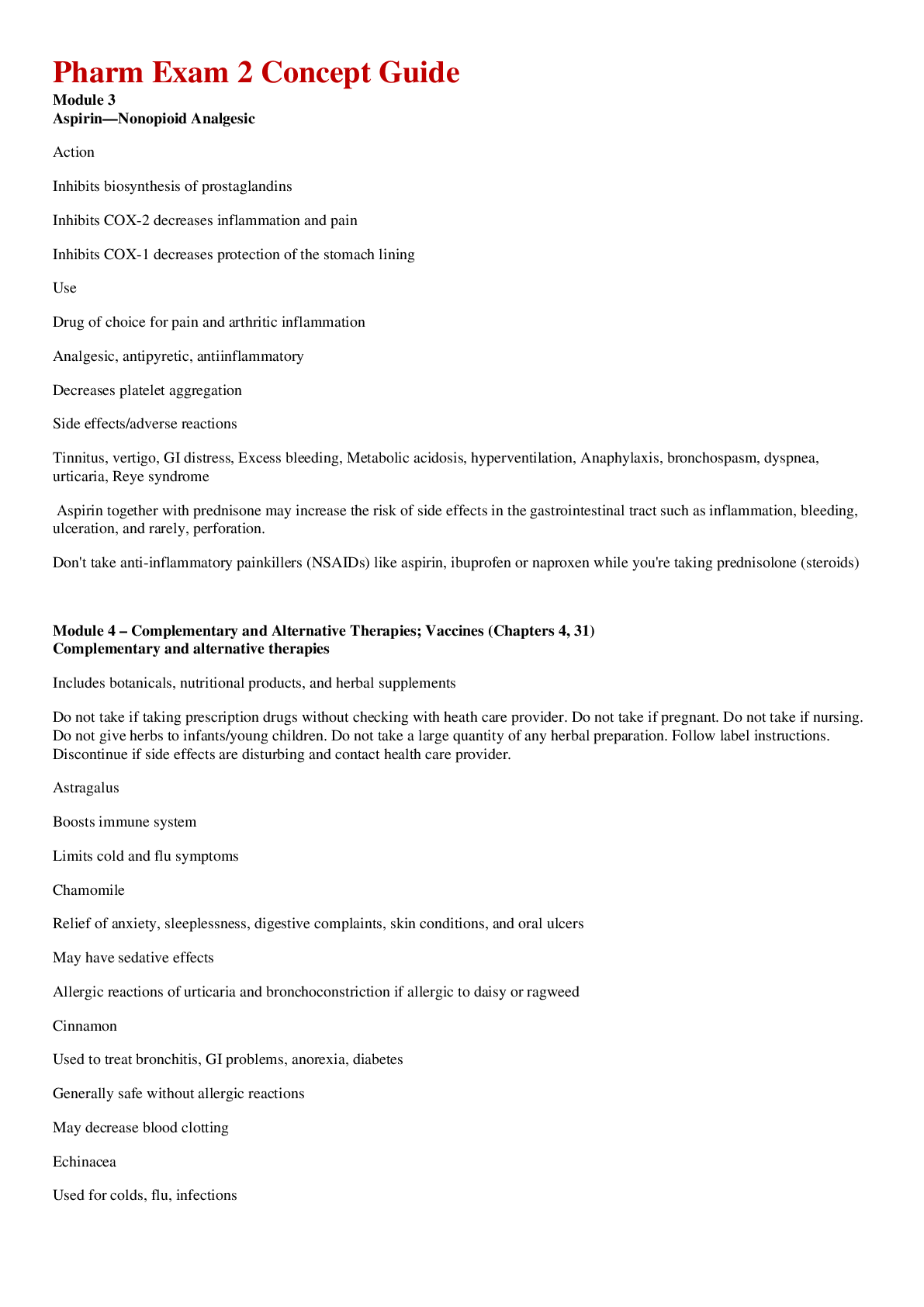
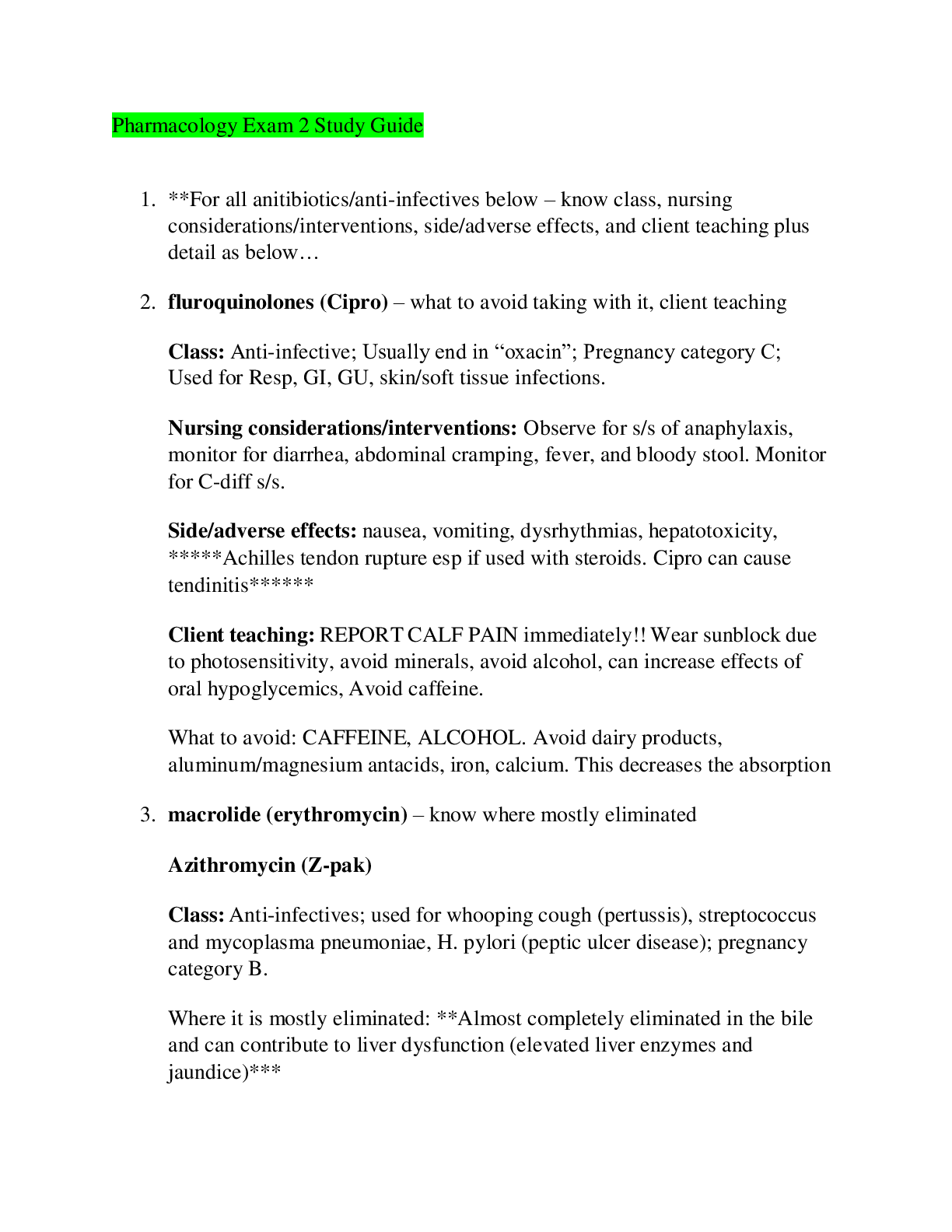
Pharmacology Exam 2 Study Guide Respiratory Drugs (Bronchodilators and Anti-inflammatory) • Know the appropriate methods of administering dry powder inhaler (DPI) and metered-dose inhaler (MDI). ... (hint: is Advair a DPI or an MDI?) o Advair is a DPI o For an MDI, instruct the client to: » ▪ Remove cap from inhaler. » ▪ Shake inhaler five to six times. » ▪ Hold inhaler with mouthpiece at the bottom. » ▪ Hold inhaler with thumb near mouthpiece and index and middle fingers at top. » ▪ Hold inhaler approximately 2 to 4 cm (1 to 2 in) away from front of mouth. » ▪ Take a deep breath, and then exhale. » ▪ Tilt head back slightly, and press inhaler. While pressing inhaler, begin a slow, deep breath that should last for 3 to 5 seconds to facilitate delivery to the air passages. » ▪ Hold breath for 10 seconds to allow medication to deposit in airways. » ▪ Take inhaler out of mouth, and slowly exhale through pursed lips. » ▪ Resume normal breathing. o For a DPI, instruct client to: » ▪ Avoid shaking device. » ▪ Take the cover off the mouthpiece. » ▪ Follow directions of manufacturer for preparing medication, such as turning wheel of inhaler. » Exhale completely. » ▪ Place mouthpiece between lips, and take a deep breath through mouth. » ▪ Hold breath for 5 to 10 seconds. » ▪ Take inhaler out of mouth, and slowly exhale through pursed lips. » ▪ Resume normal breathing. » ▪ If more than one puff is ordered, wait length of time directed before administering second puff. » ▪ Remove canister, and rinse inhaler, cap, and spacer once a day with warm running water, and dry completely before using again. ▪ Never exhale into inhaler, wash inhaler, or shake • Know the adverse effects of beta agonists and important nursing implications. ▪ Beta Andrenergic Agonist • SABA o “terol” albuterol o Route ▪ PO= lomg term, not PRN ▪ INH= PRN = “rescue inhaler” • LABA o “terol” samiterol o Route= INH o Indications ▪ First line drugs for COPD o Contraindications’ ▪ Using LABA alone in asthma= Asthma induced death o Action ▪ Beta2-adrenergic agonists act by selectively activating the beta2-receptors in the bronchial smooth muscle, resulting in bronchodilation. As a result of this: ■ Bronchospasm is relieved. ■ Histamine release is inhibited. ■ Ciliary motility is increased o A/E ▪ Oral agents can cause tachycardia and angina because of activation of alpha1 receptors in the heart • Advise clients to observe for chest, jaw, or arm pain or palpitations and to notify the provider if they occur. › • Instruct clients to check pulse and to report an increase of greater than 20 to 30 beats/min. › • Advise clients to avoid caffeine. › • Dosage may need to be reduced. ▪ Tremors caused by activation of beta2 receptors in skeletal muscle. • Tremors usually resolve with continued medication use. › Dosage may need to be reduced. o Interaction ▪ › Use of beta-adrenergic blockers (propranolol) can negate effects of both medications. • Beta-adrenergic blockers should not be used concurrently. ▪ MAOIs and tricyclic antidepressants can increase the risk of tachycardia and angina. • Instruct clients to report changes in heart rate and chest pain. o N/A ▪ Instruct clients to follow manufacturer’s instructions for use of metered-dose inhaler (MDI), dry-powder inhaler (DPI), and nebulizer. ▪ When a client is prescribed an inhaled beta2-agonist and an inhaled glucocorticoid, advise the client to inhale the beta2-agonist before inhaling the glucocorticoid. The beta2-agonist promotes bronchodilation and enhances absorption of the glucocorticoid. ▪ Advise clients not to exceed prescribed dosages. ▪ Ensure that clients know the appropriate dosage schedule (if the medication is to be taken on a fixed or a as-needed schedule). ▪ Formoterol and salmeterol are both long-acting beta2-agonist inhalers. These inhalers are used every 12 hr for long-term control and are not used to abort an asthma attack, or exacerbation. These long-acting agents are not used alone but are prescribed in combination with an inhaled corticosteroid. ▪ A short-acting beta2-agonist is used to treat an acute episode. ▪ Advise clients to observe for indications of an impending asthma episode and to keep a log of the frequency and intensity of exacerbations. ● ▪ Instruct clients to notify the provider if there is an increase in the frequency and intensity of asthma exacerbations. • Know the important nursing implications for patients who are taking theophylline. o Action ▪ Theophylline causes relaxation of bronchial smooth muscle, resulting in bronchodilation. ▪ Oral theophylline is used for long-term control of chronic asthma or COPD. (Not PRN) o A/E ▪ Mild toxicity reaction may include GI distress and restlessness. › • Monitor theophylline serum levels to keep within therapeutic range (5 to 15 mcg/ mL). Adverse effects are unlikely to occur at levels less than 20 mcg/mL ▪ More severe reactions can occur with higher therapeutic levels and can include dysrhythmias and seizures. • › If manifestations occur, stop the medication. Activated charcoal is used to decrease absorption, lidocaine is used to treat dysrhythmias, and diazepam is used to control seizures. › • Instruct client that periodic blood levels are needed. Advise client to report nausea, diarrhea, or restlessness, which are indicative of toxicity. o Interactions ▪ Caffeine increases CNS and cardiac adverse effects of theophylline. ▪ Caffeine can increase theophylline levels. ▪ Think “Caffiene” (increased CNS (tremors, nervousness, insomnia), increased HR • Advise clients to avoid consuming caffeinated beverages (coffee, caffeinated colas). ▪ › Phenobarbital and phenytoin decrease theophylline levels. • When theophylline is used concurrently with these medications, increase the dosage of theophylline. ▪ Cimetidine (Tagamet), ciprofloxacin (Cipro), and other fluoroquinolone antibiotics increase theophylline levels. • When theophylline is used concurrently with these medications, decrease the dosage of theophylline o Contraindication ▪ Use cautiously in clients who have heart disease, hypertension, liver and kidney dysfunction, and diabetes. ▪ Use cautiously in children and older adults [Show More]
Last updated: 1 year ago
Preview 1 out of 20 pages
Instant download
.png)
Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Jan 24, 2021
Number of pages
20
Written in
Additional information
This document has been written for:
Uploaded
Jan 24, 2021
Downloads
0
Views
32