*NURSING > Class Notes > West Coast University: NURS MISC Week 6 Pharmacology Lecture Notes 1 (All)
West Coast University: NURS MISC Week 6 Pharmacology Lecture Notes 1
Document Content and Description Below
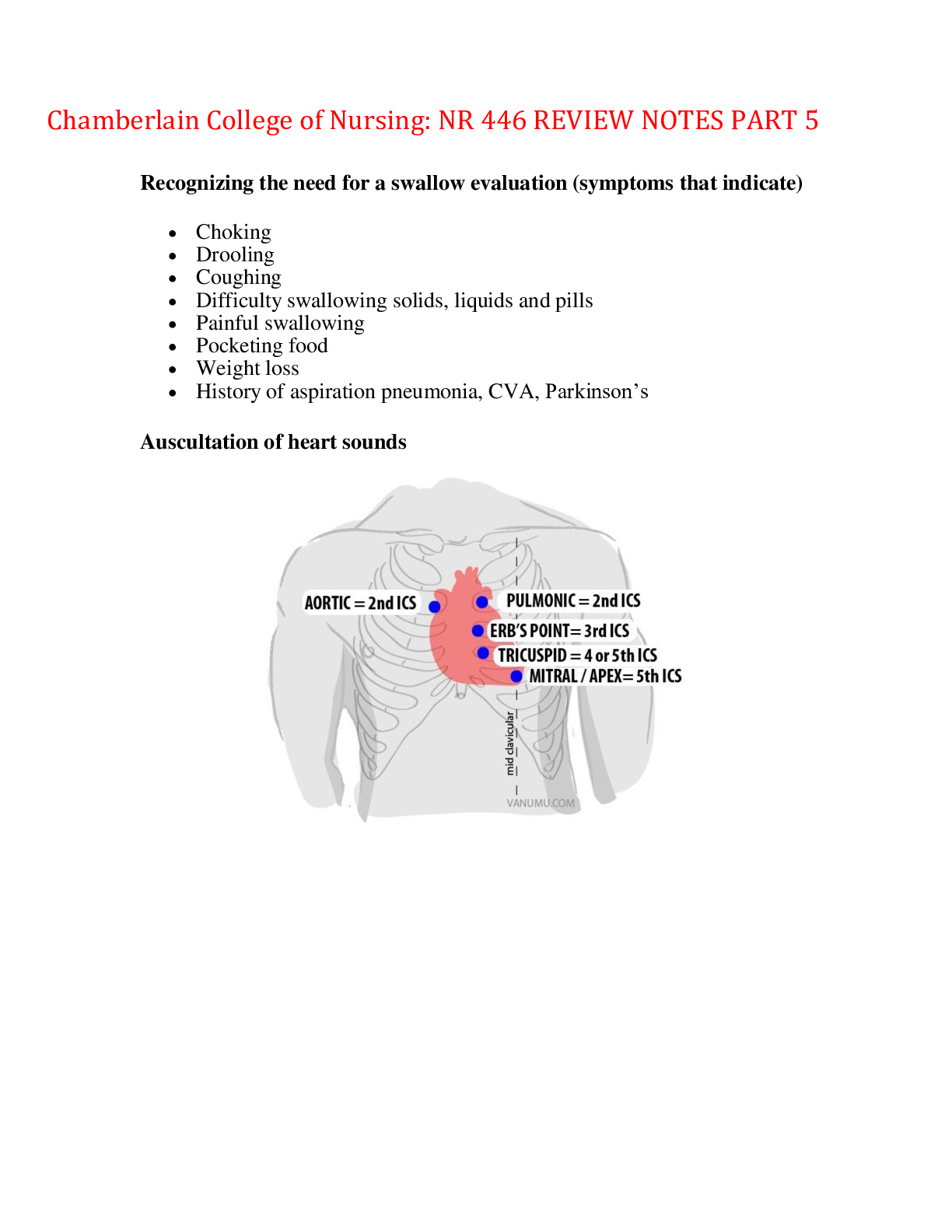
West Coast University: NURS MISC Week 6 Pharmacology Lecture Notes 1 CARDIAC GLYCOSIDES AND HEART FAILURE (Chapter 21, Page 163) Cardiac glycosides= Prototype medication: Digoxin Purpose • Positi... ve inotropic effect= Increases contraction • Negative chronotropic effect= Decreases heart rate: Apical pulse has to be at least 60 before you give the medication ▪ Have to count for the full minute ▪ Fifth intercostal space, midclavicular line • Negative dromotropic effect= Slows down rhythm Therapeutic uses • Treatment of heart failure • Dysrhythmias (atrial fibrillation) = Because of the negative dromotropic effect Complications: Digoxin toxicity= Therapeutic level of digoxin: 0.8-2.0. Antidote: Digibind. Know the signs and symptoms of digoxin toxicity: ▪ First sign is anorexia (loss of appetite) ▪ Nausea/vomiting ▪ Diarrhea ▪ Bradycardia ▪ Hypotension ▪ Hypokalemia ➢ CHF patients are usually on loop diuretics which can result in hypokalemia as well ➢ If a patient is hypokalemic, they are at risk for digoxin toxicity ➢ If the patient is hyperkalemic, digoxin is less effective ➢ Potassium levels need to be within the normal range ▪ Blurring of vision ▪ Diplopia (double vision) ▪ Xeropthalmia (yellowish-green halos around objects) ▪ Dysrhythmias Interactions • Cimetidine (Histamine2-receptor antagonist) increases digoxin levels • Quinidine increases the risk of digoxin toxicity • Verapamil increases plasma levels of digoxin Nursing Administration • IV digoxin has to be over at least five minutes • Monitor lab values, vital signs, potassium levels, therapeutic levels Adrenergic agonists= Prototype medication: epinephrine, dopamine, dobutamine. Know which of these drugs act on which receptors • Epinephrine: alpha1, beta1, beta2 • Dopamine: beta1, beta2 Purpose: • Increase blood pressure • Bronchodilation • They make the heart pump • Dobutamine: beta1 • Please someone double-check this • All these drugs will increase the heart rate, but that’s not their purpose Epinephrine= Given for anaphylactic shock and cardiac arrest • It causes vasoconstriction and bronchodilation • When given for cardiac arrest, give it as fast as possible • And you have to do CPR when you give the epinephrine, otherwise, it won’t go anywhere. Because the heart’s not working= Note that when your heart’s not working, your blood pressure is zero. • Don’t give IV epinephrine to a patient who’s healthy and walking and talking – the vasoconstriction will cause a hypertensive crisis Dopamine= When given as a low dose, its purpose is to increase renal perfusion. It dilates the renal blood vessels. • Usually the dose is 5mcg/min. • We don’t titrate this dose • These patients can stay in the telemetry unit When given as a high dose, it’s given for shock (super low blood pressure). It causes systemic vasoconstriction. • Titration o Based on the patient’s blood pressure, you increase or decrease the dose ▪ Dosage changes are up to the RN. ▪ Order might look something like “Dopamine IV drip to keep patient’s systolic BP between and .” o Always start with the lowest dosage, then go up o Every time you make a dosage change, you have to document it= Ex. “changed dosage from 10mcg to 12mcg because BP was .” o These patients have to be in the ICU. Complications. Antidote: phentolamine. Dopamine can cause necrosis if the IV becomes infiltrated. • Stop the drug • Inject the antidote through the same IV Always make sure the IV site is working before you give dopamine. • Pull IV out Dobutamine • Given for heart failure • Helps with pumping ANGINA (Chapter 22, Page 169) Angina: chest pain due to lack of oxygenation to the heart. We want drugs for angina to increase oxygen to the heart Organic nitrates= Prototype medication: Nitroglycerin (NTG) Complications: • Headache o Instruct clients to use aspirin or acetaminophen to relieve pain. Do not use opioids o Educate the patient to expect headaches • Orthostatic hypotension • Reflex tachycardia= Because of the decrease in blood pressure • Tolerance • Photosensitivity Interactions= Do not use PDE5 inhibitors with nitroglycerin → life-threatening hypotension Nursing administration: • Before every dose, document the blood pressure • Sublingual tablet o Medication is photosensitive, so keep the tablets in the original bottles and store in a cool, dark place: The patients who take these medications every day are also photosensitive, so you’ll want to cover as much of the body as possible when they go outside o When they’re taking a sublingual tablet for an angina attack ▪ Stop the activity. Sit or lie down. ▪ Take one sublingual tablet. ▪ Wait for 5 minutes. ▪ If pain isn’t relieved by the first tablet, call 911, then take a second tablet. ▪ After another 5 minutes, take a third tablet if pain is still not relieved. ▪ Do not take more than 3 sublingual tablets. • Translingual spray o Spray under the tongue o 0.4 mg NTG in every pump/spray o The particles are really small – you might not see anything being sprayed. Do not spray twice just because you don’t see anything come out. • Transdermal o Patches can only be kept on for 12 hours o “12 hours on, 12 hours off” o If you leave it on for longer, patient will develop tolerance to the medication • Topical ointment o Wear gloves o Do not massage the ointment into the skin ▪ We use creams because they provide slow absorption, if you massage the ointment into the skin, it will absorb faster o The orders come in lengths ▪ Ex. “NTG, ½ inch over the chest wall” ▪ The medicine comes with a ruler • Intravenous o The medicine comes in a white bottle, and it’s photosensitive, so we have to cover it with a brown bag o The patient cannot ambulate when they’re on this medication o Patient should be on a cardiac monitor Antianginal agent: Prototype medication: Ranolazine (Ranexa) o Complications ▪ QT prolongation • If left untreated, can become ventricular fibrillation, which can lead to asystole • Monitor the EKGs ▪ Elevated blood pressure MEDICATIONS AFFECTING CARDIAC RHYTHMS (Chapter 23, Page 175) Antidysrhythmic medications: Prototype medications: Class I Medications (Sodium channel blockers) = Procainamide, Lidocaine Class II Medications (Beta-adrenergic blockers) = Propranolol Class III Medications (Potassium channel blockers) = Amiodarone Class IV Medications (Calcium channel blockers) = Verapamil Lidocaine • Also given as an anesthetic • Lidocaine loading dose: 1 mg/kg • Lidocaine maintenance dose: 1-4 mg/min • Complications o CNS effects= Drowsiness, altered mental status, paresthesia, seizures • Contraindications • Lidocaine with epinephrine is used to prevent bleeding= This is a topical medication. Never give this medication as an IV, it can lead to hypertensive crisis o Respiratory arrest= When you give too much lidocaine o Stokes-Adams Syndrome: Sudden collapse into unconsciousness due to a disorder of heart rhythm in which there is a slow or absent pulse resulting in syncope (fainting) with or without convulsions o Wolff-Parkinson-White syndrome: An extra electrical pathway between your heart’s upper and lower chambers causes a rapid heartbeat Procainamide: Complications: • Widening of QRS complex → untreated, can lead to ventricular tachycardia • Bradycardia • CNS effects: drowsiness • Systemic lupus syndrome/Systemic lupus erythematosus (SLE) o Fever o Painful/swollen joints o Butterfly-shaped rash on face • Neutropenia and thrombocytopenia • Hypotension Propranolol (Taken from Week 5 Notes) Purpose • Decrease heart rate (negative chronotropic action) • Decrease myocardial contractility (negative inotropic action) Complications: 5 B’s • Bradycardia • Bronchoconstriction • Blood pressure drop • Blocks AV node/slows down the heart too much Nursing Considerations • Decrease rate of conduction through the AV node (negative dromotropic action) • Blood sugar drop= Not common, but happens with patients on insulin because gluconeogenesis doesn’t happen • Check heart rate before giving the med. It has to be at least 60 bpm. • Contraindicated with COPD and asthma • Always check blood pressure with antihypertensive • Beta-blockers will mask the tachycardia in hypoglycemic patients (Week 2 Notes) • Patients with MI will be on beta blockers because we want the heart to get some rest o Beta blockers decrease the mortality rate of MI’s by 80% • Toxicity: GLUCAGON Amiodarone • ACLS medication • Given for ventricular dysrhythmias • Initial dose is 150 mg for a code, followed by 300 mg • Complications o Pulmonary toxicity → respiratory depression o Visual disturbances= Photophobia (sensitivity to light), blurred vision, can lead to blindness o GI disturbances Adenosine Given for patients with SVT (Supraventricular tachycardia) • Anything can cause SVT (ex. Caffeine, energy drinks, etc.) • Heart rate is about 150 bpm • Sudden onset of chest pain, shortness of breath • To treat SVT, we tell the patient to bear down (Valsalva’s maneuver) = This slows down the heart by stimulating baroreceptors Complications= Sinus bradycardia Nursing Administration • Initial dose is 6 mg. If that doesn’t work, then a second dose of 12 mg is given. If that doesn’t work, then we give calcium channel blockers • The half-life of this medication is less than 10 seconds, so the drug has to reach the heart in 10 seconds= Push the medication quickly, and follow it with 20 cc of NS IV push • Always have an IV NS bag hanging with this medication o Core measures: certain standards set by Joint Commission for certain diagnoses= Hospitals make sure that patients with MI’s are on beta blockers o Blue-gray discoloration to the skin o Hypotension Bradycardia • For children with SVT, we fill a tray with ice then throw it on their face so that they stop breathing and bear down. If this doesn’t work, then administer medication • The patient should be on oxygen and on a tele monitor • Always have a crash cart at the bedside • This medication will stop the heart. It flatlines then goes back to normal sinus rhythm. • Quick fix: after administering amiodarone and the heart goes back to normal sinus rhythm, the patient can go home ANTILIPEMIC AGENTS (Chapter 24, Page 183) Antilipemic = anticholesterol Good cholesterol: HDL= Increase HDL by exercising at least 30 minutes every day Bad cholesterol: LDL. If you have high levels of LDLs, you are at increased risk for an MI Two common side effects of antilipemic drugs • Hepatotoxicity • Myopathy/myositis o Inflammation inside of the muscles o Breakdown of protein (myoglobin) gets stuck in the kidneys o This leads to renal failure o Urine will be dark-tea-colored or red o Rhabdomyolysis HMG-CoA reductase inhibitors (“statin”): Prototype medication: Rosuvastatin (Crestor) • Crestor is not recommended for Asians because it causes a lot of myositis in Asians Complications • Hepatotoxicity • Myopathy Contraindications= No grapefruit juice – increases statin levels in the blood Nursing administration: Statins should be given with a CoQ10 supplement: • Statins decrease the levels of this enzyme • Patient will feel very fatigued • Skin starts to wrinkle → patient will look 10 years older Cholesterol absorption inhibitor: Prototype medication: Ezetimibe Complications • Hepatitis • Myopathy Bile-acid sequestrants: Prototype medication: Colesevelam. Bile breaks down fat Other medication: Colestipol • Constipation o Doesn’t have the usual side effects o Constipation • Nursing administration= Give 30 minutes before a meal Nicotinic acid, niacin (Vitamin B). Purpose: Decrease in LDL cholesterol and triglyceride levels • Complications o Facial flushing ▪ Face becomes red ▪ This is a reaction to the drug o Hyperglycemia o Hyperuricemia o Hepatotoxicity ▪ Temporary – usually goes away after taking it, but if it persists, drug should be stopped Fibrates: Prototype medication: Gemfibrozil (Lopid) Purpose • Prevents cholesterol absorption • Decreases LDL levels Complications • Gallstones: S/S of gallstones: right upper quadrant pain, fat intolerance, bloating, positive Murphy’s sign. Murphy’s sign: Test for gallbladder disease where the patient is asked to inhale while the examiner’s fingers are hooked under the liver border at the bottom of the rib cage. The inhalation causes the gallbladder to descend onto the fingers, producing pain if the gallbladder is inflamed • Myopathy • Hepatotoxicity Nursing Administration= Take the medication 30 minutes prior to breakfast and dinner Antisense oligonucleotide= Prototype medication: Mipomersen Complications: • Liver toxicity • Musculoskeletal pain • Flu-like medications, nausea, headache • Hypertension MEDICATIONS AFFECTING COAGULATION (Chapter 25, Page 191) There are three kinds 1. Antiplatelet: prevents platelet aggregation 2. Anticoagulants: prevent the clot: There are two types of anticoagulants i. Traditional anticoagulants • Most of these medications have antidotes ii. New generation anticoagulants • Most of these medications don’t have antidotes 3. Thrombolytics: breaks down clots • You can monitor the anticoagulant effects with lab tests • There are no lab tests that you can monitor Parenteral anticoagulants: Prototype medication: Heparin MOA: Activates antithrombin → inactivates both thrombin and factor Xa . (It acts on the clotting factors) Purpose: Given to patients with MI, DVT, stroke • Not all kinds of stroke. Heparin is given for ischemic/embolic stroke (when there is a clot in the brain). How do you know it’s this kind of stroke? CT scan. • When given for MI, you give a loading dose, followed by a maintenance dose. Complications • Hemorrhage: Monitor activated partial thromboplastin time (aPTT) o The normal value of aPTT is 30-40 seconds. o When on heparin, the aPTT is 1.5-2 times the normal value ▪ This is called “therapeutic aPTT”. It’s called therapeutic because the patient is on a medication ▪ If it’s more than twice the normal value, that’s abnormal • Thrombocytopenia • Toxicity o Antidote: protamine sulfate o Protamine should be administered slowly IV, no faster than 20 mg/min or 50 mg in 10 minutes o Do not exceed 100 mg in a 2-hour period Nursing Administration • Before giving heparin, check for signs of bleeding= Look at the gums, rectal, urine, guiac tests, check for petechiae • For low molecular weight heparins, there’s usually a bubble of air in the bottle to seal the injection site • Rotate sites so that patient doesn’t bleed • When flushing, use HEPAFLUSH • When using heparin to prevent DVTs, you don’t have to check the dosage with another nurse. But for all other purposes, you have to double check the dosage with another nurse. Oral anticoagulant= Prototype medication: Warfarin (Coumadin) MOA: Acts on clotting factors VII, IX, X, and prothrombin Complications • Antidote: Vitamin K o Patient needs to be on a Vitamin K- controlled diet. • Hemorrhage o You can’t have Vitamin K fluctuations, it will affect the drug in your body. o Monitor PT and INR= It will be a therapeutic PT and INR (1.5 to 2 times normal) o We change the dose of warfarin depending on PT and INR= There places called Coumadin clinics specifically for this reason. • Hepatitis (hepatotoxicity) Nursing Administration • The full therapeutic effect of warfarin takes 3 to 5 days. If they’re going from an IV heparin drip to oral warfarin, there will probably be some overlap Direct thrombin inhibitors: Prototype medication: Dabigatran (Pradaxa) • Antidote: Idarucizumab (Praxbind) Complications • Bleeding • GI effects • Hepatotoxic This is a new generation drug, so there are no labs to check • We don’t know if the patient is being properly medicated, overmedicated, etc. Direct inhibitor of factor Xa: Prototype medication: Rivaroxaba (Xavelto) Complications • Bleeding • Hepatotoxicit No antidotes, no labs Antiplatelets Prototype medications: • Antiplatelet/salicylic: Aspirin • Antiplatelet/ADP inhibitors: Clopidogrel (Plavix)=Usually given as 75 mg daily • Antiplatelet/arterial vasodilator: Pentoxifylline o Good for diabetic patients o Arteries in limbs go into spasms = Raynaud’s syndrome: a medical condition in which spasm of arteries cause episodes or reduced blood flow o Complications: ▪ GI effects ▪ Metabolic alkalosis ▪ Respiratory acidosis ▪ Tinnitus, hearing loss Thrombolytic medications (“plase”): Prototype medication: Alteplase Purpose • Breaks down clots • Use for DVTs, stroke, MI, pulmonary edema • Also used for flushing central lines (Cathflo). If central line isn’t working o Flush with Cathflo, wait 30 minutes o If it’s still not working, flush with Cathflo, wait 2 hours • Complications o Bleeding ▪ Compared to anticoagulants, bleeding is a lot more severe o If it’s still not working, take the central line out ▪ Check for signs of bleeding o Reperfusion ventricular fibrillation ▪ If the clot was in the heart, and you gave a thrombolytic, the part of the heart that didn’t have oxygen gets shocked by the sudden influx of oxygen. ▪ This can lead to ventricular fibrillation • Nursing administration= Give within 3 hours of symptoms ▪ Whenever you give this medication, always be ready to defibrillate ▪ This is the reason doctors usually start with heparin instead • Notes on MI: From the time the patient complains of chest pain, you have a maximum of 10 minutes to do an EKG. (“door-to-EKG”): o “Door-to-cathlab” time is 60 minutes ▪ You have one hour to do the EKG, start a line, draw blood, and give all the meds ▪ If a hospital doesn’t have a cathlab, they will need a contract with an ambulance company. If not, then they’ll need to call 911. o “Door-to-needle” time is 90 minutes= Needle = angiogram or angioplasty o These are nationally recognized times set by Joint Commission. If you miss a time, everyone knows about it. Reports are sent out. GROWTH FACTORS (Chapter 26, Page 201) Erythropoietic growth factors • Prototype medication: Epoetin alfa (Epogen) (Procrit) • Increased RBC → thicker blood • Complications o Hypertension o Risk for a thrombotic event o Deep-vein thrombosis o Headache and body aches • Nursing administration o Don’t shake the vial too much → causes frothiness o Stop medication when hemoglobin is about 11 Leukopoietic growth factors Prototype medication: Filgrastim (Neupogen) • Other medication: Pegfilgrastim (Neulesta) o Given after every chemotherapy cycle o There’s usually 14 days between every chemo cycle Purpose • For low white blood cell count, especially after chemotherapy • Also given to stem cell donors o Stem cell donation ▪ Donor has to inject themselves with Neupogen weeks before donating ▪ WBC has to be about 60,000. But no more than 100K ▪ Donor lies on bed during the 6 hour procedure with a large IV on each arm Complications • Bone pain/body aches because of increased WBC count • Leukocytosis o Increase in WBC count o Splenomegaly (spleen enlargement) and risk of splenic rupture Granulocyte-macrophage colony-stimulating factor • Prototype medication: Sargramostim (Leukine) • Complications o Diarrhea o Bone pain o Leukocytosis o First IV dose effect (infusion reactions) = Tachycardia + hypotension Thrombopoietic growth factors • Prototype medication: Oprelvekin (Neumega) • Complications o Fluid retention o Cardiac dysrhythmias= Tachycardia, atrial fibrillation, atrial flutter o Eye effects ▪ Infections in the eye ▪ Visual problems ▪ Papilledema (inflammation of the eye and eyelid) ▪ Use an opthalmoscope to look at the back of the retina → check for inflamed, engorged blood vessels [Show More]
Last updated: 1 year ago
Preview 1 out of 15 pages
Instant download
Instant download
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Apr 04, 2023
Number of pages
15
Written in
Additional information
This document has been written for:
Uploaded
Apr 04, 2023
Downloads
0
Views
71