Med Surg 1, 2 & Comprehensive Rationales ,100% CORRECT
Document Content and Description Below
Med Surg 1, 2 & Comprehensive Rationales Med Surg 1A Topics 1. Cushing’s Syndrome (2 questions) → hypersecretion of ACTH (hormone that allows body to react to stress) ○ https://www.youtube... .com/watch?v=ea1sXgd5ui8 ● Signs & Symptoms → fatigue, muscle weakness, weight gain, thinning extremities, thin & fragile skin, moon face & ruddy complexion, hirsutism, truncal obesity, broad purple striae, bruising, impaired wound healing, increased blood pressure & sodium, hypokalemia, hyperglycemia, buffalo hump, DM ● Treatment → restore hormone balance by radiation, drug therapy or adrenalectomy (removal of one or both adrenal glands) ● Nursing Considerations → Frequently monitor VS (especially BP), monitor labs for electrolyte changes, monitor daily weight, check for signs of infection, perform passive range of motion for those that have osteoporosis or are bedridden ○ Post-surgery nursing considerations → encourage coughing & deep breathing, monitor for shock & HTN, administer cortisone as ordered ○ Diet → High in protein & potassium, but low in carbs & sodium, high calcium + vit. D 2. Hepatitis (3 questions) → inflammation of the liver that causes liver cell damage ○ https://www.youtube.com/watch?v=eocRM7MhF68 ○ Chronic hepatitis (> 6 months) can lead to cirrhosis of the liver ● Causes → bacteria, toxins or viruses , 6 viral types → A, B, C, D, E, G ● Hepatitis A & E → fecal to oral (shellfish from contaminated waters is a major source) ● Hep. A stages ○ Pre-icteric: malaise, N/V, anorexia ○ Icteric: jaundice, clay colored stool, tea colored urine ○ Convalescent: SX resolves ● Hepatitis B,C, D & G → parenteral drug abuse, sex, blood & body fluids, ● Signs & Symptoms → jaundice, anorexia, RUQ pain (due to hepatomegaly), clay-colored stools, tea-colored urine (due to bilirubin leakage), apendicitispruritus, elevated LFT’s (AST & ALT) & prolonged PT ● Treatment → symptomatic → vitamin K, anti-histamines, corticosteroids, anti-emetics & apply calamine lotion ● Nursing Interventions → improve sanitation, vaccination, no ETOH, instruct pt to balance rest and activity, patient cannot donate blood! HAND WASHING #1! ● Diet: low in fat, high in carbs and protein 3. Cytoscopy → direct visualization of the urethra, bladder, ureteral orifices, and prostatic urethra ○ https://www.youtube.com/watch?v=eiw8YM4YLFE - for males ○ https://www.youtube.com/watch?v=P0-HXugWdDw - for females ○ Helps assess ureters and the pelvis of each kidney ○ Can obtain a urine specimen from each kidney to evaluate its function ○ Assist in performing a biopsy ○ Assist in removing calculi from the urethra, bladder and ureter ○ Performed in both lower and upper tract ● Lower tract cystoscopy ○ Pt. is usually awake; discomfort is equal to that of catheterization ○ Viscous lidocaine can be injected prior to the study to minimize post-test discomfort ○ General anesthesia is usually administered ● Upper Tract cystoscopy ○ Pt. usually kept NPO for several hours before test ○ A sedative may be administered ○ Pt. can expect some burning on voiding, blood in urine, urinary frequency ○ Heat applications are helpful in relieving pain and relaxing muscles ● Nursing Care → monitor pt. with prostatic hyperplasia (enlarged prostate that can cause urine difficulty) for urine retention, suggest warm sitz baths and antispasmodic meds, monitor for s/s of UTI 4. Diabetes Mellitus (4 questions) → know setting priorities → Condition is characterized by a high level of glucose in the body ○ Signs & Symptoms → THE POLY’s (polyuria,polydipsia, polyphagia), weakness, dizziness, fatigue i. In Children → those above + enuresis (bed-wetting), unusual fatigue & irritability ○ Type 1 → beta cells in pancreas are destroyed and produce no insulin i. Treatment → insulin injections, continuous infusion via pump & diet control ○ Type 2 → beta cells in pancreas secrete insulin, but the body is resistant to its effects i. Treatment → insulin, oral hypoglycemic injections & diet control ○ Diet Management → monitor total calories, carbs & timing of food ○ Diet Intake → meals with complex carbs, ↓ fat, ↑ fiber, some protein i. Time meals with peak effect of insulin ii. Provide extra snacks for unplanned physical activity iii. Substitute soft foods 6-8 times per day if you cannot stick with the usual meal plan iv. If vomiting, diarrhea or fever persist take in some liquids like ½ cup coke, juice, broth or 1 cup of gatorade to maintain caloric intake every ½ hour or hour v. Report nausea, vomiting & diarrhea to HCp → extreme fluid loss = dangerous vi. Unable to retain fluids = hospitalization to prevent DKA ○ Patient Teachings → lose weight if obese, oral hypoglycemic agents, maintain healthy weight, s/s of hypoglycemia & hyperglycemia, self-monitoring of glucose, skin/foot care, importance of exercise ○ “Sick Day” Rules → guidelines for managing diabetes when ill → aimed at preventing DKA i. Take insulin or hypoglycemic agents as usual ii. Test blood glucose & urine ketones every 3-4 hrs → report elevated levels to MD iii. If you take insulin, you may need supplemental doses every 3-4 hours ○ Dawn Phenomena → early morning glucose levels are elevated caused by nocturnal release of growth hormone ○ Somogyi Effect → fall in blood glucose during the night with ↑ morning glucose levels → caused by 5. Thermal Injury (4 questions) ● First degree (Superficial partial-thickness)→ epidermis affected (destroyed or injured); painful, red, dry, min. or no edema ● Second degree (Deep partial-thickness) → epidermis and part of dermis affected; painful, red, exudes fluid, edema, blistered ● Third degree → Total destruction of epidermis, entire dermis, and in some cases subcutaneous tissue, muscle or bone; painless, varied color (white, red, black, brown or charred), dry, leathery, edema, symptoms of shock, probable hematuria (RBC in urine) and hemolysis (break down of RBC’s) ● First responder interventions: ensure safety of yourself, extinguish flames, cool burn by briefly applying cool water to burn and clothing covering burn, remove other clothing, cover wound to prevent contamination, irrigate chemical burns, asses ABC’s ● Treatment: grafts → use of skin or other materials to cover burned areas ● Nursing Care: IV Lactated Ringers, plasma; F/C to monitor I/O (should be 30ml/hr), check for s/s of fluid overload vs. dehydration, monitor BP, v/s, weight, electrolytes, wound care at least once a day (administer pain meds 30min before wound care), sterile technique, tetanus prophylaxis; high caloric, high-carb, high-protein diet, may require parenteral nutrition; estimate TBSA (total body surface area) with the Rule off 6. Herpes Zoster (Shingles) → Acute infectious viral disease that is reactive of chickenpox virus, presents as unilateral, painful rash, group of vesicles on an erythematous base along a dermatome ○ Treatment → calamine lotion to soothe itching & pain, Acyclovir, corticosteroids to reduce inflammation, vaccination to prevent or modify the disease course ● Nursing considerations: minimize pain & prevent complications, analgesics, apply compresses (wet dressings to skin lesions & cold compresses to ruptured vesicles), administer systemic corticosteroids to diminish severity, prevent spread- contagious to anyone who has not had chickenpox or is immunocompromised 7. Hernia (2 questions → know Umbilical Hernia) → protrusion of intestines through a weakness in the umbilical ring, muscle & fascia Types of Hernias ● https://www.youtube.com/watch?v=3wUrJGDgGO4 ● Umbilical → Hernia occurring at the naval ; more common in women who are obese or multiparous ○ S/S → bulging protrusion at the umbilicus → pain, discomfort at site ○ Treatment → Size of fascial ring less than 2 cm = none; larger = surgery → laparascope ○ Nursing Care → do not use a belly band or tape a silver dollar to the area, keep pressure dressing in place until sutures are healed, sponge-bath child until the dressing is removed & keep diapers folded below the dressing ● Hiatal → opening in diaphragm through which esophagus passes ○ S/S: heartburn, full after meals, GI bleed and N/V (severe) ● Inguinal → Protrusion of the hernia sac containing the intestine of the inguinal opening 8. Incentive Spirometer → Breathing device used to maximize lung expansion by opening closed alveoli and mobilize secretions → facilitates tissue oxygenation!, prevents atelectasis ● Nursing considerations: instruct client to breath in and exhale normally, seal lips around mouthpiece, inhale slowly and deeply, holding breath for at least 3 seconds while keeping ball or cylinder elevate, exhale, take several normal breaths and repeat 4-5 to,es; client should cough after procedure to facilitate secretion removal 9. NG Tube Insertion → Tube from nose into stomach inserted to instill medication ,food, fluids, to remove stomach contents, to obtain specimen for laboratory analysis ● Insertion: ○ Measure distance from tip of nose to earlobe plus the distance from the earlobe to the bottom of the xiphoid process, mark the distance on the tube with tape ○ Lube end of tube with water-soluble lubricant, insert tube through the nose to the stomach; offer sips of water and advance gently; bend head forward to close epiglottis, closing trachea ○ Observe for respiratory distress→ an indication of misplacement in the lungs ○ If in correctly, secure tube w/ hypoallergenic tape and verify placement by evaluating gastric aspirate; aspirate should have pH of =4 ■ If in lungs = resp. distress ○ Different types of tubes: ■ Lebin tube: used for decompression and tube feeding ■ Salem tube: decompression and suction ■ Seng-staken Blakemore tube: bleeding and esophageal varices 10. Diabetic Ketoacidosis → Life-threatening condition in type 1 DM; caused by lack of insulin; body drawing on fat & protein stores for energy; ketone of Na+, Cl-, K+, water, increased RR & urine output, & leads to dehydration & hypoxia ● When acidosis is severe, Pt can lose consciousness (diabetic coma) ○ Indications of impending coma include HA, drowsiness, weakness, confusion, hypotension, tachycardia, warm dry flushed skin, dry mucous membranes, N/V, elevated temperature, polyuria, polydipsia, rapid & deep respirations (Kussmaul’s respirations), fruity odor to breath (from ketone bodies) ● Nursing intervention: administer insulin; IV fluids; electrolytes as ordered; monitor electrolytes status, I&O’s, blood glucose levels; insert & maintain NG tube & urinary catheter as needed ● Teach measures to prevent recurrence such as daily monitoring of blood glucose & monitoring ketones if blood glucose is over 250-300mg/dL, adherence to diabetes management program (including insulin administration), exercise, keeping appointments, recognizing symptoms of infection (a major cause of DKA), & phoning for assistance if symptoms noted 11. Thyroid Disorders (5 questions → know Grave’s disease & Hypothyroid) → ○ Hyperthyroidism → hypersecretion of thyroid gland (Graves Disease) i. S/S → hyperthermia, HTN, tachycardia, heat intolerance, diaphoresis, increased appetite, irritability, muscle fatigue, hyperactivity, sleep deprivation, hyperreflexia ii. Treatment → radioactive ablation, complete or partial removal, anti-thyroid meds 1. Radioactive precautions: flush toilet twice, use gloves, put clothes in radioactive sealed bag, don’t hand wash clothes (machine wash only x 2 on hot) iii. Nursing Care → monitor for thyroid storm, heart failure, cardiac dysrhythmias, quiet environment with little stimulus iv. Patient Education → high protein, carb, vitamin & mineral diet, cool clothes, balance rest & activity, may need hormone replacement therapy ○ Thyroid Storm → hyperpyrexia (fever), cardiac dysrhythmias & altered mental status → hypothermic blanket, O2 & meds to suppress thyroid ○ Hypothyroidism → low secretion or cellular resistance to thyroid hormone i. S/S → weakness, fatigue, unexplained weight gain, constipation, edema, slow pulse rate, decreased libido, infertility ii. Treatment → gradual thyroid replacement with levothyroxine iii. Nursing Care → high-bulk(protein), low-calorie diet & encourage activity ○ Myxedema → patients w/ hypothyroidism i. non-pitting edema in periorbital area & hands/feet caused by severe or long standing hypothyroidism → patient must continue meds for hypothyroidism to prevent this! 12. Immobility Hazards → know hazardous things if patient is immobile ● Includes pressure ulcers, osteoporosis, hypercalcemia, negative nitrogen balance, increased cardiac workload, orthostatic hypotension, stasis of respiratory secretions, boredom, depression ● Nursing considerations: turn frequently, provide good skin care, give high-protein diet with small-frequent feedings, rise from bed slowly, turn, cough,and deep breathe. ROM exercises at least 3x each or as much as pt. can tolerate, high protein diet, vitamin A and C ● Tx: enoxaparin → prevents DVT 13. Diabetes Insipidus → results from a deficiency in circulating ADH (vasopressin) → results from dysfunction of the pituitary gland ○ Signs & Symptoms → extreme polyuria, polydipsia (especially cold, iced drinks), nocturia, ↑ plasma osmolality, urine specific gravity 1.001-1.005, fatigue, dehydration → weight loss, poor skin turgor, dry mucous membranes, constipation, muscle weakness, tachycardia & hypotension ○ Medical Causes → brain tumor, head injury, brain surgery & lithium therapy ○ Treatment → identify cause of diabetes insipidus & treat it! Until cause is identified, give vasopressin or vasopressin stimulate to control fluid balance & prevent dehydration. You may also give thiazide diuretics to ↓ fluid volume by creating mild salt depletion ○ Nursing Considerations → monitor I&O, urine specific gravity, skin condition, check weight daily weight, s/s of hypovolemic shock (BP, HR & respirations) & monitor labs for hypernatremia ○ Complications → hypernatremia, severe dehydration & vasoconstriction 14. Hyperglycemia → elevated blood glucose level, usually associated with diabetes ○ Signs & Symptoms → THE POLY’s (polyuria, polydipsia, polyphagia), vision changes, fatigue/weakness, dry skin, slow healing wounds, recurrent infections, numbness/tingling in hands or feet ○ Treatment → varies depending on which type of diabetes i. Type 1 → insulin injections ii. Type 2 → Diet, exercise, oral hypoglycemic agents ○ Nursing Care → work with patients on management of the disorder & how to prevent acute & long-term complications 15. Hypoglycemia → abnormally low level of glucose in the blood, usually occurs suddenly as a complication of diabetes ○ Signs & Symptoms → sweating, tremors, tachycardia/palpitations, nervousness, hunger, confusion, headache ○ Treatment → give either 15 grams of carbs in the form of candy, juice or sugar, 1 mg subq or IM glucagon, 25-50 mL IV 50% dextrose in water to unconscious patients i. After symptoms resolve, give a snack of protein or starch 16. Liver: Cirrhosis (2 questions) → chronic, progressive liver disease caused usually by alcoholism, but can also be caused by viral infections, toxins, bile stasis or obstruction ○ Signs & Symptoms → indigestion, gas, constipation, N/V, esophageal varices, hematemesis, hemorrhage, ascites, anemia, edema in extremities, JAUNDICE, pruritus, DARK URINE, CLAY-COLORED STOOLS, palma erythemia ○ Treatment → must treat what is causing the cirrhosis! i. Lactalose → for ammonia ii. If ascites → paracentesis iii. Shunts to relieve portal hypertension iv. Liver transplant v. Diet: high carb, high protein ○ Nursing Care → HIGH PROTEIN DIET (high carb in early stages, but in late stages restrict fiber, protein, fat & sodium) & give supplemental vitamins i. Check skin, gums, stool & emesis regularly for bleeding ii. Apply pressure to injection sites iii. Assess fluid retention → daily weight iv. Avoid using soap when bathing patient to prevent skin breakdown v. LABS: low H & H 17. Allergy → hypersensitivity caused by exposure to an allergen, a true allergy will cause production of IgE antibodies ○ Allergic reaction is caused by large amounts of histamine being dispersed throughout the circulatory system → causes vasodilation & edema of the tissues ○ Signs & Symptoms → SOB, wheezing, inflamed airways, itching, congestion, erythema ○ Common allergens → PCN, radiopaque dyes, aspirin, blood components, Toxins (snake, bee, wasp, hornet), food (berries, milk, chocolate, eggs, shellfish, seafood, wheat, nuts) & latex i. High risk populations for latex allergy → spina bifida kids, urogenital abnormalities, spinal cord injuries, multiple surgeries, health-care workers ii. Why spina bifida kids? https://www.ifglobal.org/en/37-temp-news/9-latex-allergies ○ Nursing Care → obtain detailed history, establish airway, administer epinephrine or diphenhydramine in the event of a reaction i. Latex allergy → avoid condoms, balloons, gloves, catheters, brown ace bandages, elastic pressure stockings ii. Do not give d5 LR → causes a reaction ○ Client Education → use of inhaler & epi pen, paint walls, toys should be wood, plastic or metal, remove rugs, move bed away from forced air vent ○ Allergic Rhinitis → allergic rxn that results in watery rhinorrhea, nasal obstruction, sneezing, nasal pruritus i. Nursing Care → Anti-histamines & topical anti-inflammatory drugs ○ Allergen Desensitization → used to treat the allergy when the patient is unable to avoid the allergy. Patient is exposed to larger and larger amounts of allergen in an attempt to change the immune system's response. i. Useful for environmental allergies, mostly ii. Serial injections given → start with small doses and gradually increased iii. Safety → Observe for anaphylaxis, have epi on hand, always keep client in office for 30 minutes ○ Eczema → itchy, red skin rash commonly seen in young children, may ooze and form a crust → can also form as a result of an allergen i. Common causes: milk, wheat, eggs ii. Treatment → avoid allergen, apply astringent solution, corticosteroid cream & antihistamines, keep patient from scratching 18. Dialysis (know AV fistula) → 2 types = Peritoneal & Hemodialysis ○ https://www.youtube.com/watch?v=mi34xCfmLhw → forward to 3:50 ○ Peritoneal → removal of excessive fluids & wastes through the peritoneal cavity by surgically inserted catheter i. Before procedure → obtain baseline vitals, breath sounds, weight, glucose & electrolyte levels ii. During procedure → infuse 1-2 L of fluid into cavity by gravity using sterile technique, leave fluid in for 20 minutes & then remove it by gravity iii. After procedure → take vital signs, check for respiratory distress, pain or discomfort, assess dressing around catheter for wetness iv. Complications → peritonitis (fever, abd pain & cloudy dialysis drainage, swelling, tenderness, redness or purulent secretions at site), abdominal pain, insufficient return of fluid v. Nursing Care → instruct patient to consume high protein & fiber diet ○ Hemodialysis → removal of excess fluids & wastes by circulating patient’s blood through a semi-permeable membrane that acts as an artificial kidney i. Done through a mature AV shunt, fistula or graft (4-6 weeks old) → created by surgical anastomosis of an artery & a vein (usually radial artery & cephalic vein) 1. Complications→ air embolism, blood leaks, blockage/clotting, contamination & exsanguination ii. Nursing Considerations → check thrill & bruit every 8 hours, do not use that site for BP or blood specimens, assess site for infection, instruct patient to not lift anything heavy on that side or sleep on top of it, monitor closely for hypotension, N/V, malaise, HA, dizziness & muscle cramps 19. Cholecystectomy (2 questions) → surgical removal of the gallbladder to restore biliary flow, can be done either laparoscopic or traditional (T-tube) ○ Before surgery → keep on clear liquids/NPO 24 hours before, assess respiratory status ○ After laparoscopic surgery → monitor wounds & dressings, anesthesia related nausea/vomiting, keep in Semi-Fowlers position, encourage early ambulation, apply heat to right shoulder to alleviate any pain caused by phrenic irritation ○ https://www.youtube.com/watch?v=ffoKThdqo4I ○ After traditional surgery → Low Fowler’s position, splint the affected side, assess drainage from T tube & position (make sure it is level with abdomen) watch for signs of post cholecystectomy syndrome (fever, abd pain, jaundice) ○ https://www.youtube.com/watch?v=sFtRwDUTavo ○ Patient Education → Encourage client to walk, instruct them that they will need assistance for the first 24-48 hrs after surgery, report any elevated temperatures, apply heat pad, sit-up in bed & that they should return to normal activities within one week ○ Diet: avoids spicey foods and fatty foods 20. Kidney Transplant → Transplantation of a donor kidney from a live donor or a cadaver, attractive alternative to dialysis or ESRD ○ Symptoms of Rejection → oliguria (little urine), edema, fever, hypertension, weight gain, tenderness over kidney ○ Nursing Interventions → monitor I & O’s, monitor K+ labs, and observe for signs of bleeding, report output of less than 100 mL/hr to MD ○ Patient Teaching → Record I&O’s to monitor kidney function, weigh yourself twice a week and report any rapid gain, avoid crowds or contact with people with known/suspected infections for 3 months after surgery, continue immunosuppressant therapy throughout the entire time to prevent rejection 21. Fracture → break in continuity of the bone ○ Open vs. closed fracture i. Open/compound fracture: fractured bone that breaks through the skin ii. Closed/simple fracture: does not penetrate through the skin (skin is intact) ○ Complications of fracture: fat emboli, hemorrhage, sepsis, compartment syndrome ○ Emergency Care → immobilize joint above & below fracture, cover any wound with sterile dressings, check temperature, color, sensation & cap refill, elevate above heart level to reduce swelling i. Extreme caution with spinal fractures → C-spine & log-roll patient ○ Hip Fracture (common in the elderly) → one leg may be shortened, externally rotated or adducted, be very painful, possess a hematoma, muscle spasms i. Treatment → immobilize using Buck’s traction, open or closed reduction with internal fixation, hemiarthroplasty (femoral head prosthesis) ii. Bucks traction: https://www.youtube.com/watch?v=2ZEWz_Ps7vo iii. Nursing Care → apply hip protector pads in patients at risk for falls, monitor for hypovolemic shock post surgery, use compression stockings/ICD’s or anti-coagulants to prevent DVT’s, encourage patient to keep moving by using trapeze, administer pain meds, monitor hydration/nutrition/urine output, access the 6 P’s (pain, paresthesia, pallor, paralysis, pulse, poikilothermia (unable to regulate temp.) ○ Skull Fracture → results from direct impact, signs & symptoms may not be evident immediately i. Signs & Symptoms → ecchymosis behind ears, over mastoid process (Battle’s sign) or around eyes (raccoon eyes), CSF leakage from nose or ears, cranial nerve injury manifestations 1. Complications → brain abscess, meningitis, increased ICP 22. Lyme Disease → Inflammatory disorder caused by a spirochete (Borrelia burgdorferi) → spread to humans by deer tick bites ○ Symptoms → flat, flu-like sx, slightly raised red lesions (bulls-eye pattern); fever; fatigue, chills; muscle pain; progresses to joint pain, persistent fatigue, headache, and stiff neck ○ Diagnostic Tests → blood tests to identify the bacteria → anti-body titers, ELISA, Western Blot i. Lumbar puncture to test CSF for the bacteria ii. RBC → anemia, WBC, ↑ sedimentation rate ○ Treatment → antibiotic therapy(3-4 weeks) → Doxycycline, Ceftriaxone, Azithromyocin, Amoxicillin; Analgesics & Anti-pyretics → reduce inflammation & fever, NSAIDs → treat arthritic symptoms ○ Patient Teaching → medication may be required up to 1 month → stress importance of maintaining consistent schedule of NSAIDs; provide education on transmission and prevention (wear long sleeves & pants outside in summer & early fall), use insect repellent, 23. Osteomyelitis → Infection of the bone from a soft tissue infection, bone surgery, trauma or blood-borne infection caused by Staphylococcus aureus ○ Carried by blood from primary site of infection (upper respiratory infections (URIs), otitis media, and tonsillitis). ○ Often a chronic problem → can get sepsis ○ Symptoms → fever, chills, malaise, septicemia, throbbing and deep pain & swelling over the infected area ○ Diagnostic Tests → X-rays, bone scans, blood studies (↑ WBC), wound & blood cultures to identify bacteria ○ Treatment → IV antibiotics around the clock for 3-6 weeks followed by 3 months oral antibiotic therapy i. Immobilization of the affected limb ii. Warm soaks to increase circulation iii. Surgery to expose & remove the abscess (debridement), irrigate with saline solution & apply antibiotic beads to the wound iv. Amputation to relieve pain & avoid therapy resistant osteomyelitis ○ Patient Teaching/Nursing Considerations → support affected extremity with pillows & splints to maintain proper body alignment i. Sterile technique when changing wounds ii. IV fluids, prevent dehydration, diet high in protein and vitamin C 24. Urinary Tract Infection → infection that begins in the urethra, bladder, ureters or bladder usually caused by Gram negative bacteria, more common in females than males ○ Cystitis → bladder inflammation ○ Pyelonephritis → inflammation of the kidney ○ Signs & Symptoms → frequent urination, urges, pain/burning when urinating, nocturia, pain/tenderness over bladder, cloudy or foul smelling urine, fever, retroperitoneal pain & N/V, confusion in the elderly ○ Diagnostic Tests → Clean-catch mid-stream UA, culture & sensitivity ○ Treatment → antibiotics, pyridium, vaginal estrogen therapy, ↑ fluid intake to 3000 mL/day, vitamin C & cranberry juice ○ Nursing Care → preventative education, empty bladder after sex, avoid douche/powders, wipe from front to back 25. Therapeutic Communication (2 questions) → listening to & understanding the client while promoting clarification & insight → occurs in stages during nurse interaction ○ Purpose → develops trust & promotes open communication ○ Goal → understand the client’s message, facilitate client’s verbalization of feelings, communicate nurses understanding & acceptance ○ Techniques → silence, general leads or broad openings, clarification & reflection Nurse-Patient Relationship Stages ● Pre-Interaction → review patient data ● Orientation → introduction to patient - use verbal & non-verbal skills ● Working → team building phase between you, patient & health care team ● Termination → discharge planning, nurse is no longer needed 26. Ileostomy (2 questions → know how to care for one) → surgical passage through abdominal wall (R lower quadrant) into the ileum → drains GI contents when rest of GI system cannot function properly ○ Drainage → liquid stool containing proteolytic enzymes & bile salts ○ Nursing Care → empty the bag when ⅓-½ full, change the bag every 3-7 days during inactive time (before meals or at bedtime), check skin for irritation ○ Patient Education → be cautious of high fiber & high cellulose foods (popcorn, peanuts, coconut, chinese veggies, shrimp, rice, bran, corn, peas) → may cause diarrhea i. No enteric coated meds, laxatives or enemas ii. Always report an increase or decrease in drainage to HCP 27. Anaphylaxis (2 questions) → serious, immediate multiple system response (vasogenic shock) to an antigen-antibody reaction upon exposure (rarely the first time) ○ Signs & Symptoms → feelings of impending doom/fright, weakness, sweating, sneezing, pruritus, urticaria (hives), angioedema, cardiovascular changes, respiratory discomforts & dyspnea ○ Treatment → immediate injection of epinephrine ( you may repeat every 5-20 minutes) ○ Nursing Care → maintain a patent airway is the most important thing i. Start CPR if patient goes into arrest ii. Monitor for hypotension & shock (maintain volume with volume expanders) iii. Monitor I&O, O2 & suction 28. Addison Disease (3 questions - know Addisonian Crisis) → deficiency in adrenocortical hormones ○ Addisonian Crisis → acute adrenocortical insufficiency caused by stress, surgery, trauma or infections i. Signs & Symptoms → classic shock symptoms (hypotension & cyanosis), profound weakness & fatigue, severe N/V, dehydration, H/A, confusion, abdominal pain ○ Signs & Symptoms → weakness/fatigue, anorexia/weight loss, N/V, constipation/diarrhea, BRONZE skin discoloration, increased pigmentation of the mucous membranes, poor coordination, fasting hypoglycemia, craving salty food, amenorrhea ○ Treatment → corticosteroid replacement therapy → cortisone or hydrocortisone i. Fludrocortisone to prevent dehydration & hypotension ii. In crisis → give dexamethasone, hydrocortisone or both ○ Nursing Care → monitor vitals & for s/s of shock, hyperkalemia before treatment & hypokalemia after therapy i. Glucose levels checked if patient also has diabetes ii. Diet → sodium & potassium balance iii. Record weight & monitor fluid/electrolyte intake 29. Impaired: Integument → disruption of skin surface or skin layers ○ Great indicator of overall health status & can provide info that could indicate underlying disease ○ Nursing Assessment → nails (shape, angle, texture, color), skin (vascularity, bleeding, bruising)), hair & scalp (lesions, infestations) Types of Wounds ❏ Abrasion → denuded skin ❏ Avulsion → tissue torn away from supporting structures ❏ Cut → longer than deeper, edges well defined ❏ Ecchymosis/Contusion → blood trapped under the skin ❏ Hematoma → tumorlike mass of blood trapped under the skin ❏ Laceration → irregular edges & vein bridging at site of skin tear ❏ Patterned → wound caused by object which leaves imprint ❏ Stab → deeper thain longer, well-defined edges Assess wounds for S/S of infection → purulent drainage, pain, redness, swelling, ↑ temperature & WBC ● Signs of Infection? → wound culture to determine bacteria type Types of lesions…. Pressure Ulcers → assess for redness, warmth, induration or hardness, swelling & signs of infection ● Stage 1 → area of skin with observable pressure related changes ● Stage 2 → superficial partial thickness wound that involves the epidermis & dermis ● Stage 3 → full-thickness wound with tissue damage or necrosis of subcutaneous tissue ● Stage 4 → full-thickness skin loss with extensive damage, destruction or necrosis to muscle, bone or supporting structures ○ Treatment → debridement of necrotic tissue, provide a moist wound-healing environment & good nutrition (protein, vitamin C & vitamin A) ● Pruritus → severe, intense itching, tingling & burning ○ Causes → rubbing, scratching, allergies, hyperbilirubinemia ○ Treatment → remove causative agent, corticosteroid, anti-histamines ○ Nursing Care → soothing tepid baths, short nails & mittens ● Psoriasis → chronic, noninfectious inflammatory disease of the skin ○ Signs & Symptoms → thick, itchy, silvery-white scales with symmetrical distribution → common areas are scalp, knees, sacrum, elbows & behind ears ○ Nursing Considerations → oil or coal tar bath, topical steroids, soft brush, anti-metabolites, UV light 30. SIADH → Syndrome of Inappropriate Antidiuretic Hormone → excessive amounts of antidiuretic hormone that results in water imbalance causing water intoxication caused by fluid retention ○ Signs & Symptoms → decreased LOC (cerebral edema, ↑ ICP, HA, irritability, delirium), seizures, coma, sodium less than 120 ○ Treatment → treat the underlying cause! i. Fluid restriction (500-600 mL/24 hours) ii. Sodium replacement iii. Diuretics ○ Nursing Care → daily weight, neuro checks, I&O, check electrolytes,BUN & creatinine, position flat in bed 31. Osteoarthritis (degenerative bone disease) (2 questions) → chronic degenerative disorder that causes deterioration of the joint cartilage; most common form of arthritis ○ S/S → joint pain/atrophy in the hips, knees, hands & cervical/lumbar spine & stiffness in the morning or after exercise (relieved by rest), decreased ROM, crepitus, Heberden’s & Bouchard’s nodes (bony, cartilaginous enlargements in the joints of the hands) ○ Treatment → PALLIATIVE to reduce pain, NOT CURATIVE i. Aspirin, phenylbutazone, indomethacin, ketolorac ii. Intra-articular injections of corticosteroids iii. Glucosamine & Chondroitin → improve tissue function & retard breakdown of cartilage iv. Massage, Acupuncture, moist heat, rest v. Gentle exercise, weight reduction vi. Surgical → arthroplasty, osteotomy, osteoplasty ○ Nursing Care → moderate activities, get plenty of rest, stress importance of maintaining muscle tone, recommend palliative measures (massage, acupuncture, hot soaks) 32. Rheumatoid Arthritis (3 questions) → chronic, systemic inflammatory disease that primarily attacks peripheral joints and surrounding muscles, tendons, ligaments & blood vessels ○ S/S → joints that are painful, red, warm, stiff (especially in the morning), fatigue, weight loss, anorexia ○ Treatment → immunosuppressives (methotrexate), salicylates, NSAID’s, analgesics, corticosteroids, antidepressants (sleep,depression, pain mgmt) & reconstructive surgery ○ Nursing Care → assess all joints carefully - check for deformities, contractures, immobility & inability to perform ADL’s i. Monitor vitals & note weight changes ii. Meticulous skin care & monitor duration of morning sickness iii. Tell pt to take hot showers before bedtime & eat a balanced diet iv. Apply splints carefully & observe for pressure ulcers v. Make sure pt understands the chronic nature of RA & that it will require lifestyle changes 33. Amputation (2 questions) → Surgical removal of a part of the body ○ Complications: phantom limb pain, infection, & hip contracture ○ Nursing Considerations: ROM to prevent contracture of hip, place Pt prone for 20-30 min q3-4hrs; do not elevate residual limb on a pillow after the immediate postoperative period; after the pressure dressing & drains are removed, inspect the wound for inflammation; dressing changed daily until sutures are removed; residual limb wrapped with an elastic bandage to shape the residual limb and keep the dressing in place; observe for symptoms of inadequate tissue perfusion. 34. Kidney: Nephrectomy → Removal of kidney because of tumor, infection, anomalies, advanced kidney cancer that is refractory to chemo. ○ Nursing Considerations → position client in lateral recumbent position, patient will have drains and indwelling catheter, check urine output closely (color, consistency, output → blood in urine is not normal, report to doctor), administer analgesics as prescribed, encouraged to cough and deep breathe, use incentive spirometer, splint incision to help with coughing and encourage early ambulation. i. Four Types of nephrectomy that are performed: 1. Partial Nephrectomy: portion of kidney is removed 2. Simple Nephrectomy: entire kidney is removed 3. Radical Nephrectomy: entire kidney, adrenal gland, and surrounding fat tissue are removed. Patients are placed in a side-lying position during surgery. A 7-inch flank incision just below the diaphragm is needed to perform an open radical nephrectomy. This involves removal of the 12th rib. 4. Nephroureterectomy: entire kidney, surrounding fat tissue, and entire ureter are removed. 35. Colonoscopy: direct visualization of the colon with a fiberoptic colonoscope ○ Purpose: Aids the diagnosis of inflammatory and ulcerative bowel disease, pinpoints lower GI bleeding, detects lower GI abnormalities including, polyps, hemorrhoids, and abscesses. ○ Pre-test: clear liquid diet 24 to72 hours before exam (nothing with red dye), cathartic in evening for 1-2 days before exam, enema the morning of the exam, take enema morning of exam ○ Post-test: allowing client to rest, observing for passage of blood, abdominal pain, signs of perforated bowel (fever, chills, N/V, severe abdominal pain), hemorrhage, and respiratory distress, monitor for resp. distress 36. Irritable Bowel Syndrome: Functional disorder of bowel motility ○ Cause: certain foods, food allergies ○ S/S: Constipation, diarrhea, combination of constipation and diarrhea, pain, bloating, abdominal distension. ○ Nursing considerations: diet goal of providing adequate nutrition tailored to specific GI pattern of IBS, food allergies and intolerance common. ○ Client Education: eat at regular times and slowly, chew food slowly, do not drink fluids with meals, drink fluids between meals, increase fiber along with fluids to normalize GI function while monitoring GI function closely for adverse effects, decrease anxiety and stress, avoid alcohol, large meals, simple sugars, caffeine, excess fats, and cigarettes 37. Laminectomy: Surgical removal of a section of the lamina, a portion of the vertebral body between the spinous process and facet pedicle. Excision allows health care provider the chance to inspect the spinal canal, locate and remove herniated nucleus pulposus that is impinging on spinal cord and nerves relieving and pain. ○ Cervical → lamina located in the cervical spine i. Nursing consideration: sore throat-responds to throat lozenges, humidification, and not talking. Dysphagia-pureed or soft diet easier to swallow than regular. Assess neurovascular function of upper and lower extremities and neurological function using the Glasgow coma scale. Monitor respiratory function. Hematoma formation and edema can occlude the airway. Have tracheostomy tray by room door and suction in room ready to use. Assess dressing for serosanguineous drainage indicating spinal fluid leak, also noted with the client reporting headache. Hoarseness and inability to cough effectively might represent damage to the recurrent laryngeal nerve, inability to cough could lead to atelectasis and pneumonia ii. Client Education: wear collar as directed, avoid twisting or bending or flexing or extending or rotating neck, avoid sitting or standing for over 30 minutes. ○ Lumbar → removal of one or more vertebral laminae plus osteocytes and herniated nucleus pulposus through an incision. i. Postoperative nursing care: checking for fever and hypotension, checking dressing, performing neurovascular (circulation, movement, and sensation) assessment, client should wear antiembolic stockings, log roll every 2 hours by two people, when out of bed, back should be kept straight 38. Cast Care: ○ Immediate cast care: avoid covering cast until dry, handle with palms, not fingertips (plaster cast). Avoid resting cast on hard surfaces or sharp edges. Keep affected limb elevated above heart on soft surface until dry. Observe for blueness or paleness, pain, numbness on affected area. ○ Intermediate care: encourage client to perform prescribed exercises, report any break in cast or foul odor, inform client to not scratch skin underneath cast and avoid putting anything underneath cast. ○ Types of Casts: i. Non-plaster or fiberglass cast: 1. Consist of open-weave, nonabsorbent fabric impregnated with cool water-activated hardeners. Used for nondisplaced fracture and long-term wear. ii. Plaster cast: 1. Rolls of plaster are wet with cool water and smoothed onto body; a crystallizing reaction occurs and heat is given off. ○ Complications: Pressure ulcers, Disuse syndrome, Compartment syndrome and delayed union or nonunion of fractures 39. Urinary Calculi→ (urolithiasis [kidney stone disease]) calcifications in urinary system, commonly called stones; formed in any part of the urinary tract, usually kidney (nephrolithiasis), and can migrate within tract; may be composed of one type of crystal or a combination, calcium being most common; others oxalate, struvite, uric acid, cystine, xanthine. Important to collect stones to determine composition and appropriate treatment. ○ Indications S/S: sharp, severe, sudden pain depending on location of stone, diaphoresis, N/V, fever, chills, hematuria, pallor, anxiety, increased BP and pulse. ○ Interventions: surgery, extracorporeal shock wave lithotripsy ○ Nursing Interventions: administer analgesics as prescribed, monitor I/O, force fluids (urine output should be 3-4 L/day and urine should appear colorless), strain urine and save any stone material, monitor temp., daily weights, teach diet for prevention of stones (dependent upon composition of stones). ○ Patient Teaching: teach recognition of urinary tract infections and need to contact health care provider promptly 40. Urinary Tract Disorders→ Infection of one or more structures in urinary tract (cystitis, pyelonephritis, urethritis.) Usually caused by gram-negative bacteria. ○ More common in females than males. i. Indications S/S: urinary frequency, urgency, burning, pain with voiding, nocturia, pain or tenderness over bladder, cloudy or foul smelling urine, fever with or without chills, retroperitoneal pain, nausea vomiting, possibly visible blood or pus in urine. ii. Nursing Interventions: obtain clean catch midstream urine specimen for urinalysis, culture sensitivity and possibly gram stain. Force fluids to 3000 mL/day, encourage cranberry juice or other urinary acidifiers iii. Treatment: Antibiotic therapy, Pyridium, Vaginal estrogen therapy, increased fluids, and increased vitamin C and cranberry juice intake. iv. Pt. teaching: females void following intercourse, avoidance of douche or powders, bladder cath care, clean properly after defecation (wipe front to back). ○ Children: i. Indications S/S: Hematuria, enuresis, fever, foul-smelling urine, poor appetite, painful urination ii. Parent instructions: administration of prescribed antibiotics, encourage child to drink clear liquids, instruct parents of good perineal hygiene, avoid tight clothing or diapers, encourage child to void frequently. ○ Cystitis → Bladder inflammation i. S/S: burning or pain on urination, urinary frequency, urinary urgency, bladder spasms. ii. Treatment: Symptomatic, organism-specific antibiotic iii. Nursing considerations: Monitor urination for frequency and amount, assess urine for cloudiness and hematuria, obtain specimen for analysis and culture and sensitivity, iv. Client Education: increase fluid intake to dilute urine, use heating pad on lower abdomen for bladder spasms, take meds as directed. ○ Pyelonephritis: Inflammation of the kidney caused by bacterial infection, UTI, pregnancy, tumors, or urinary obstruction. i. S/S: chills, fever, malaise, flank pain, costovertebral angle tenderness ii. Nursing care: bed rest during acute phase, administer and teach about antibiotics, encourage fluids. 41. HIV/AIDS (3 questions) ○ HIV (Human Immunodeficiency Virus) i. Virus that causes immunodeficiency that can lead to AIDS 1. Transmitted: via blood and body fluids 2. S/S: early stage: asymptomatic, later as immune system deteriorates...opportunistic infections. 3. Medical Treatment: antiretroviral medications, organism-specific medications, chemotherapy, antidepressants, nutritional support, symptomatic. 4. Nursing Considerations: user personal protective equipment to prevent infection, supportive care depending on presence of opportunistic infections. 5. Client and Public Education: Practice safe sex. ○ AIDS: i. Syndrome distinguished by serious deficits in cellular immune function; causes opportunistic such as Pneumocystis jiroveci pneumonia, Candida albicans stomatitis and esophagitis, cytomegalovirus, Kaposi sarcoma. 1. Pneumocystis jiroveci Pneumonia is the most common opportunistic infection of AIDS a. Indications: Gradually worsening chest tightness, SOB, persistent, dry, nonproductive cough, dyspnea, tachypnea, fever, progressive hypoxemia, cyanosis. b. Nursing Care: offering high-protein, high-caloric diet, monitoring vitals signs, chest sounds, suction and maintaining oxygen as ordered, monitoring for indications of secondary infection, provide restful environment, assisting with personal care, implementing infection control precautions, handwashing when entering and leaving room, monitoring for oral infections, assessing breath sounds, monitoring weight, encouraging nutritional supplements, assessing hydration, encouraging client to express feelings. ○ AIDS Dementia Complex: Dementia resulting from effects of HIV ○ Children with AIDS: 91% of children with AIDS were infected through perinatal transmission. i. Indications: lymphadenopathy, hepatosplenomegaly, Candida albicans stomatitis, chronic or recurrent diarrhea, failure to thrive, developmental delays; Pneumocystis jiroverci pneumonia most common opportunistic infection in children. ii. Treatment → antiretroviral drugs iii. Nursing considerations: scrupulous handwashing, instructing child and family about importance of handwashing, children from being around persons who are infectious, restricting infected children who bite or do not have control of bodily functions, providing high-calorie, high-protein meals and snacks, monitoring child’s weight and height, encouraging child to participate in activities with other children, providing anticipatory guidance to the family because child has potentially fatal disease. 42. Chronic Kidney Disease (2 questions) → know a lot of nursing judgment and concepts ○ Irreversible, progressive reduction of functional kidney tissue resulting in inability of kidneys to excrete wastes, concentrate urine, and conserve electrolytes. i. Indications S/S: anemia, acidosis, azotemia, fluid retention, hypertension, hypocalcemia, anorexia, N/V, constipation, impaired insulin action. ii. Interventions: to slow progression, control blood pressure and make fluid and dietary adjustments. Dialysis or transplantation may be done when these measures are no longer effective. iii. Nursing interventions: Monitor fluid status, encourage nutrition by decreasing nausea, vomiting and stomatitis, and other GI symptoms, teach appropriate diet (low protein, low potassium, low sodium), manage constipation, teach to balance rest and activity, encourage good skin care with emphasis on moisturizing, teach coping skills to client and fam, teach dialysis-related procedures, explain transplantation process and subsequent potential issues and care. Important to increase non-protein calories, such as fruit ice. iv. Diagnostic tests: 1. Urine specimen (reveals low specific gravity, hematuria, proteinuria) 2. Blood studies (reveal elevated BUN, creatinine, potassium) 3. Creatinine clearance test (measures glomerular filtration rate) 4. Ultrasonography of kidneys, renal scan, CT scan 43. Peptic Ulcer Disease (3 questions) ○ Excavation formed in mucosal wall of stomach, pylorus, duodenum. Caused by infections with Helicobacter pylori (H. Pylori), a gram-negative bacterium. i. Indication: normal-hypersecretion of HCl, weight loss may occur, pain occurs 0.5-1 hour after a meal, vomiting, hemorrhage more likely occurs with duodenal ulcer. ii. Predisposing factors: ages 40-60, familial tendencies, chronic use of NSAIDs, alcohol ingestion, excessive smoking. iii. Diagnostic tests: noninvasive; include immunological tests of antibodies to H. pylori and urea breath tests. Invasive; endoscopy, gastric biopsy, and biopsy with bacterial culture for H. pylori. iv. Nursing considerations: small, frequent feedings if not taking antacids or histamine blocker, avoid coffee, alcohol, seasonings if use causes discomfort, reduce stress. Instruct patient to take medication 1 hour before meals. v. Treatment therapy: 1. Antacids a. Proton pump inhibitors or H2 receptor antagonists 2. Anticholinergics a. Inhibit the vagus nerve effect on parietal cells and reduce gastrin production. 3. Physical rest to promote healing 4. Gastroscopy to facilitate coagulation of bleeding site 5. Surgery if patient: a. Does not respond to treatment, has perforation, or suspected cancer or other complications 44. Gastrointestinal Tests: Upper GI→allows practitioner to visualize the upper GI organs and sphincters for diagnosis of anatomic or functional abnormalities. Used to diagnose ulcers, varices, tumors, regional enteritis, malabsorption syndromes, gastritis, cancer, hiatal hernia, diverticula, and strictures. ○ Upper GI is ingestion of barium sulfate to determine patency and size of esophagus, size and condition of gastric walls, patency of pyloric valve, and rate of passage to small bowel. i. Preparation: Maintaining NPO after midnight, informing client that stool will be light-colored after procedure. ii. Post-test: encouraging fluids, administering laxatives to prevent constipation, and informing client that stool will be white from barium 45. Esophagogastroduodenoscopy ○ Visualization of esophagus, stomach, and duodenal mucosa through light, flexible fiberoptic tube. Identifies ulcerations, tumors, and obtains tissue biopsy (detect presence of Helicobacter pylori or to rule out gastric carcinoma) or fluid samples. i. Preparation: verify informed consent has been obtained, maintain NPO at least 8 hours before procedure, teach client about numbness of throat due to local anesthetic applied to posterior pharynx. ii. Post Procedure: maintain NPO until gag reflex returns, observe for vomiting of blood, respiratory distress, inform client to expect sore throat for 3-4 days after procedure. ○ Description of Procedure: i. Patient is sedated ii. Lubricated endoscope is passed through the mouth and into the esophagus for visualization of the gastric wall and sphincters. iii. Endoscope is advanced to duodenum iv. Still and video images are taken, or images are shown on a monitor for continuous viewing during the procedure. v. Biopsy forceps are passed through the scope to obtain any necessary tissue samples 46. Inflammatory Bowel Disease: Includes Crohn’s disease and ulcerative colitis ○ Indications: abdominal pain, diarrhea, fluid imbalance, weight loss. Diarrhea in Crohn’s disease is less severe than in ulcerative colitis. ○ Nursing Considerations: include high-protein, high-calorie, low-fat, low-fiber diet, may require TPN to rest the bowel, administer analgesics, anticholinergics, sulfonamides (gentamicin), corticosteroids, antidiarrheals, and anti peristaltics, maintain fluid/electrolyte balance, monitor electrolytes, promote rest, relieve anxiety. i. Crohn’s Disease: Subacute and chronic inflammatory bowel disease involving segments of the terminal ileum and proximal colon; extends through all layers of the bowel wall; restricts absorption of nutrients. 1. Symptoms: colicky lower right quadrant pain not relieved by defecation, diarrhea, weight loss, low-grade fever, nutritional deficit, anemia, dehydrations; fistulas, anorectal fissure or fistula. 2. Treatment: medications→antidiarrheals, antispasmodics, anticholinergics, sulfonamides, steroids. 3. Diet: High calorie, high protein, parenteral nutrition used for bowel rest. NO cocoa, chocolate, citrus juices, cold or carbonated drinks, nuts seeds, popcorn or alcohol. 4. Nursing considerations: High-Protein, high-calorie, low-fat, low-fiber diet, administer medications, maintain fluid and electrolyte balance. ii. Ulcerative colitis: Inflammatory condition of colon characterized by eroded areas of mucous membrane and tissue beneath it. 1. Indications: rectal bleeding, blood, pus, mucus in stool, abdominal pain occurs pre defecation, may have 20 to 30 diarrhea stools daily, nutrition deficit, weight loss, anemia, dehydration. 2. Diet: High-protein, high-calorie, low-fat, low-fiber diet, TPN used for bowel rest, analgesics, anticholinergics, antibiotics, corticosteroids to reduce inflammation, ileostomy. 3. Nursing Considerations: Instruct client about medications and diet, maintain fluid/electrolyte balance, monitor electrolytes, promote rest, relieve anxiety. 47. Lithotripsy: Extracorporeal Shock-wave → noninvasive technique that uses high-energy shock waves to break up obstructive renal calculi & allow their normal passage ○ Preparation → tell the patient that he may receive general or epidural anesthetic, will have an IV line & foley in place after the procedure ○ Morning & Aftercare → encourage ambulation as early as possible after treatment, increase fluid intake to aid passage of calculi, strain urine - educate patient that slight hematuria usually occurs for several days after procedure but tell the doctor if there is frank or persistent bleeding ○ Patient Education → drink 3-4 L of water up to 1 month after treatment, strain all urine for one week, report severe hematuria or inability to void 48. Safety: Older Adult → know safety & intervention 49. Continuous Passive Motion → known devices? ○ Device to supply slow continuous range of motion to joint by an electronically controlled vise. i. Uses: promotes healing after a total joint arthroplasty, increases circulation to the area, prevents joint contracture, encourages early motion of joint; degrees of flexion and extension and amount to be increased over specified time frame determined by healthcare provider and physical therapist. ii. Nursing Considerations: Neurovascular assessment of affected extremity, administer pain meds as ordered, ensure proper alignment of extremity in devise, document degrees of flexion and contraction and time in device, allow client control over time in and out of device as possible. iii. Client Education: rationale for use of machine, expected time in device, degrees of flexion and extension. 50. Pancreatitis→Inflammation of pancreas that can be acute or chronic. ○ Acute: mild inflammation with minimal discomfort to severe disease that is unresponsive to any medication, ending in death. This is caused by the premature activation of enzymes, particularly trypsin, which then self-digest the pancreas. The process of self-digestion is often triggered by the obstruction of the common bile duct by gallstones, causing bile to reflux back into the pancreatic duct, which stimulates the premature activation of the pancreatic enzyme (normally, activation begins later in the duodenum.) i. S/S: Severe, acute abdominal pain, back pain, abd distension, N/V, decreased intestinal motility, fever, jaundice, ALOC, Hypotension, ARF, Tachycardia, Respiratory distress, Hyperglycemia, Hypocalcemia. ii. Treatment: Parenteral nutrition, withhold oral intake so pancreatic enzymes are not stimulated. Nasogastric suction, Biliary drains and stents, surgery, and intravenous fluids after the initial crisis is over to restore electrolytes. 1. Meds: a. Histamine-2 (H2) antagonists. (cimetidine {Tagamet}, ranitidine {Zantac}), to decrease gastric acid production b. Analgesics for pain c. Antiemetics to prevent vomiting. iii. Nursing Care: 1. Record I & O hourly, and monitor electrolyte levels. 2. Patients with NG, good mouth and nose care and assess respiratory patterns regularly. 3. Administer pain meds 4. Watch for complications from parenteral nutrition (hypokalemia, overhydration, metabolic acidosis) and watch for signs of a calcium deficiency (cramps, tetany, seizures). 5. Instruct patient on the need for lifestyle modifications to prevent recurrences and to avoid factors that aggravate the dx. (alcohol). ○ Chronic: Characterized by the progressive destruction of the pancreas after repeated attacks of pancreatitis. Protein plugs and calculi in the pancreas form as a result of the hypersecretion of protein as a result of excessive alcohol consumption over long period of time. Alcohol is also toxic to pancreatic cells. Cells are eventually replaced by fibrous tissue, which obstructs the pancreatic and common bile ducts, blocking drainage to the duodenum. i. S/S: Attacks of severe abd and back pain, N/V, Anorexia, and weight loss, Malabsorption and foul-smelling stools with high-fat content (steatorrhea), and calcification of the pancreas. ii. Treatment: 1. Endoscopy, to remove duct stones and dilate strictures 2. Pain meds and avoidance of pain triggers (alcohol) 3. Diet, insulin, or oral antidiabetic agents, to treat diabetes if present 4. Pancreatic enzyme replacement, to treat malabsorption and steatorrhea 5. Surgery (pancreaticojejunostomy, pancreaticoduodenectomy or the Whipple procedure, to relieve pain, restore proper drainage of pancreas and to reduce the frequency of attacks. 51. Intestinal Obstruction: Partial or complete blockage of lumen of large or small intestines; compression of the bowel lumen leading to blockage of passage through intestines. ○ Causes: May be mechanical (tumor, hernia, adhesions, intussusception, volvulus) or nonmechanical (paralytic ileus, abdominal infections, intestinal ischemia.) Manifestations depend on location of obstruction. ○ S/S: absence of bowel sounds, intermittent and severe abdominal pain and distension, vomiting, tympanitic and tender abdomen, obstipation (absence of stool or gas), obstruction of ileum causes fecal vomiting, nausea, abdominal tenderness, decreased bowel movements. ○ Treatment: NPO, insertion of NG or Intestinal tube for decompression, IV fluid and electrolyte replacement, laxatives or enemas for fecal impaction, disimpaction, pain management, possible surgical intervention of colectomy possibly including temporary or permanent colostomy or ileostomy. ○ Complications: fluid volume deficit, bowel strangulation, necrosis, perforation, infection, nutritional deficiencies. ○ Nursing Considerations: maintenance of nasogastric tube (record amount and color of drainage) , monitoring for complications (metabolic acidosis/alkalosis), IV fluid replacement, postoperative care, monitor fluid and electrolyte levels, assist with ADLs, good oral and skin car, monitor vital signs (observe closely for signs of shock), Fowler's position to facilitate breathing, measure abdominal girth, administer antibiotics, pain and N/V management, auscultate for bowel sounds and watch for signs of returning peristalsis, ○ Client Education: Encourage high Fiber diet and plenty of fluids. ○ Diagnostic tests: i. Laboratory studies (electrolyte studies, complete blood count), which reveal dehydration, loss of plasma volume, and sometimes infection ii. Abdominal x-ray, which show abnormal amounts of gas and/or fluid in the bowel. In large bowel obstruction, they show a distended colon. iii. Barium studies are contraindicated. 52. Hyperglycemic, Hyperosmolar, Nonketotic syndrome → know Hyperosmolar Nephrotic Syndrome is a complication of hyperglycemia, which also involves hyperosmolarity, minimal to absent ketosis, and altered sense of awareness. Occurs in type 2 diabetics over 50 years of age ○ Pathophysiology: i. Uncontrolled hyperglycemia causes the kidneys to excrete the excess glucose with water and electrolytes (osmotic diuresis). ii. Water then shifts from intracellular fluid space to extracellular fluid space, causing hypernatremia and increased osmolarity. 1. Indications: glucose levels greater than 800 mg/dL, hypotension, dry mucous membranes, poor skin turgor, tachycardia, altered awareness, seizures, hemiparesis; ketosis and acidosis do not occur. 2. Nursing Care: Administer normal saline and regular insulin, assess vital signs, blood glucose, central venous pressure, LOC, urine output, and temperature. 53. Acute Kidney Disease/injury → Abrupt acute disruption in kidney function that impairs ability of body to maintain balance of fluid, electrolytes, and acid-base status. ○ Phases of ARF: i. Initiation: Begins with initial insult and ends when oliguria develop ii. Oliguria: Output less than 400 mL/day; increase in BUN, creatinine, uric acid, potassium, magnesium; uremic symptoms occur 1. Indications: N/V, irritability, drowsiness, confusion, coma, restlessness, twitching, seizures, hypertension, pulmonary edema, increased serum potassium, BUN, creatinine, calcium, sodium, and pH. iii. Diuresis: gradual increased urinary output; may still have uremic symptoms. 1. Indications: increased urinary output, decreased serum sodium, potassium, BUN, creatinine, correction of metabolic acidosis, increased mental and physical activity. iv. Recovery period : 1. Indications: returned to normal functioning while healing takes place. ○ Interventions: treat underlying cause, treat fluid and electrolyte imbalance, prevent infection, administer high caloric and low protein diet, possible dialysis ○ Nursing Interventions: maintain strict intake and output and compliance with fluid restriction/intake as ordered, daily weights, monitor vital signs closely, assist client with managing anorexia and eating appropriate foods, provide good skin care, monitor for infection, encourage rest, support dialysis if indicated. ○ Nephrotic syndrome: Minimal-change nephrotic syndrome (MCNS) most common in type of nephrotic syndrome in children; i. Indications: periorbital or ankle edema, larger than expected weight gain, decreased urinary output, pallor, fatigue, hyperalbuminuria, hypoalbuminemia, ascites, hypovolemia. ii. Treatment: restrict salt, corticosteroid therapy, immunosuppressive therapy iii. Nursing considerations: monitor I/O, daily weights, test urine for albumin, measure abdominal girth, protect from upper respiratory infection, instruct parents about S/S to observe for at home, how to administer steroid therapy, and adverse effects. ○ Diagnostic tests: Urine specimen (reveals low specific gravity, hematuria, proteinuria), Blood studies (reveals elevated BUN, creatinine, potassium), Creatinine Clearance test (measures glomerular filtration rate), and Ultrasonography of kidneys, renal scan and CT scan. 54. Thyroidectomy → complete or partial excision of the thyroid gland ○ Purpose → corrects hyperthyroidism, removes breathing obstruction caused by goiter, treats thyroid cancer, treats hyperparathyroidism ○ After surgery → monitor respiratory status, ensure that incision drains properly, monitor pulse & temperature for indications of thyrotoxicosis or thyroid storm ( fever, tachycardia > 130, delirium, coma) i. Monitor for tetany → could indicate that parathyroid glands were damaged during surgery which would cause hypocalcemia (Chovsteks & Trousseau’s sign) ii. Keep patient in Semi-Fowlers position, apply ice to reduce the swelling iii. Make sure to have suction, O2, trach set, IV calcium & suture removal kit at bedside iv. Ask patient to speak every 2 hours to check tone & hoarseness v. Emphasize importance of adhering to thyroid replacement therapy after discharge vi. Keep incisions clean & dry 55. Cholecystitis→Inflammation of gallbladder, that may be calculous (obstructed by calculi or gallstones) or acalculous (not obstructed by gallstones.) ○ Indications & S/S: intolerance to fatty foods, indigestion, N/V, severe pain in upper right quadrant of abdomen, elevated temp, Belching that leaves a sour taste in the mouth, Flatulence and possible jaundice and clay-colored stools with common duct obstruction. ○ Risk factors: obesity, sedentary lifestyle, female, ages 50-60 ○ Nursing Considerations: administer antibiotics, analgesics, antispasmodics, NPO until acute symptoms subside, reduce weight if needed, instruct to avoid fatty, fried foods. ○ Treatment: Surgery (usually elective), Vit K for itching, jaundice, and bleeding tendencies caused by Vit K deficiency. Nonsurgical treatment=insertion of flexible catheter, formed around T tube, through the sinus tract into the common bile duct. Guided by fluoroscopy, the doctor directs the catheter toward the stone, A Dormia basket in threaded through the catheter to entrap the calculi. i. Preparing for surgery: 1. Monitor and stabilize nutritional status and fluid balance 2. Clear liquid 24 hour before surgery 3. Give pre op meds, and insert NG tube ii. Aftercare: 1. Monitor site for infection 2. Monitor N/V from anesthesia 3. Apply heat to pt. Shoulder to alleviate right shoulder pain caused by phrenic irritation from carbon dioxide under the diaphragm. 4. Semi-Fowler’s to decrease discomfort 5. Early ambulation ○ Diagnostic tests: Abdominal X-Ray, Ultrasonography, Radionuclide imaging or cholescintigraphy, and ERCP. 56. Paracentesis → removal of fluid from the peritoneal cavity (2-3 liters) ○ Preparation → Informed consent, encourage voiding, take vitals, measure abdominal girth & weigh client ○ During → take vitals Q15min ○ After → document amount, color & characteristics of drainage obtained, assess pressure dressing for drainage, keep patient in bed until vitals are stable Other topics from Vangie... 1. Lumbar puncture → tests CSF, normal should be clear, cloudy = infection, 2. Hypertensive crisis can’t find Kaplan rationale- Med Surg book pg.873 ❖ Emergency- BP are > 180/120 and BP must be lowered immediately to halt or prevent damage to target organs. Conditions that could cause hypertensive crisis are: pregnancy, acute MI, intracranial hemorrhage, and dissecting aortic aneurysm. ➢ TX: ICU- reduce mean blood pressure 20-25% 1st hour, a further reduction to a goal pressure of 160-100 over a period of 6 hours and a more gradual reduction over the next few days. Titrate hydrochloride (Cardene), nitroprusside, (Nitropress) and fluids ➢ *Exceptions to this TX are: ischemic stroke, aortic dissection (lower BP sys 100, if pt. can tolerate) Urgency- no evidence of organ damage TX: anti-htn meds 3. Pneumonia ❖ Inflammatory process that results into edema of the lung tissues and extravasation of fluid into alveoli causing hypoxia. ➢ S/SX: fever, leukocytosis, cough productive of rusted color, green, or whitish yellow sputum, dyspnea, pleuritic pain, tachycardia ➢ Nursing Intv: administer antibiotics, Q4H vitals, cough/deep breath Q2H, assess breath sounds, use incentive spirometer, encourage fluids 3,000ml/24 hours, semi fowler's position, O2 therapy Med Surg 2B Topics → 90 Test Questions 1. Pancreatic Cancer → Cancer of the pancreas can affect the head (75-80 %), body, or tail of the pancreas. The location of the cancer and whether pancreatic islet cells are functional influence the clinical picture. ○ S/SX → weight loss, Vague upper or mid-abdominal discomfort, abnormal glucose tolerance test (hyperglycemia), jaundice, clay-colored stools, dark urine,pruritus, ascites, feeling full ○ Nursing Intv → include high-calorie, bland, low-fat diet, small frequent feedings, avoid alcohol, administer anticholinergics, pain; medication; treatment antineoplastic chemotherapy, surgery- Whipple procedure; postoperative care after Whipple procedure; survival rate for clients with unresectable pancreatic cancer is approximately 6 months. ○ Tx: whipple procedure, pancreatic enzymes 2. Radical Pancreaticoduodenectomy (Whipple Procedure) → know why patient needs whipple https://www.youtube.com/watch?v=68XsPhyMEZA ❖ Procedure is for pancreatic carcinoma in head of pancreas: ❖ Removal of the head of the pancreas, distal portion of common bile duct, the duodenum, and part of the stomach. Radical pancreaticoduodenectomy ( Whipple Procedure) is used for resectable pancreatic cancer that is confined to the head of the pancreas, the most common site of tumors. Purpose of procedure is to remove tumor and allow bile to flow into jejunum, Survival rate is 20% in 1st 5 years. Procedure can take 8 hours ❖ postoperative nursing care includes monitor for peritonitis and intestinal obstruction and hypotension and steatorrhea and diabetes mellitus, administer pancreatic enzymes. In this procedure the following organs are removed: ■ Gallbladder (cholecystectomy) ■ Distal Portion of the stomach ( antrectomy) ■ Distal Portion of the common bile duct ( Choledochectomy) ■ Duodenum ■ Proximal jejunum ■ Head of pancreas ■ Regional Lymph nodes ❖ After organs are removed, remaining pancreas and bile duct are attached to jejunum (pancreaticojejunostomy and choledochojejunostomy, respectively) 3. Infection Precautions: Neutropenic (2 questions) → know understanding concept, making nursing judgment = protecting them → Used for clients at increased risk for infection, such as immunosuppressed with neutrophil count under 500 ➢ Nursing Intv: private rooms scrupulously cleaned; meticulous hand washing and use of personal protective equipment by all; restriction of visitors; no fresh fruit or vegetables; avoid invasive procedures, such as catheterization-unless essential, Air in rooms should be under positive pressure, All rooms should have own wash basin and toilet, which should be sanitized after each use, Supply of single use gloves, gowns, aprons, and masks must be kept in the room, keep door closed, Wear HEPA filter mask if neutropenia is severe.Provide low microbial diet; eliminate fresh salads and unpeeled fresh fruits or veggies and any uncooked foods, avoid any invasive procedure. Good Assessment: Monitor for any signs of infection, skin, no IM injections, breath sounds, temp, no rectal temps, change IV site frequently, shower daily with Dial soap preferably (antimicrobial soap) and CBC 4. Bell’s Palsy a. https://www.youtube.com/watch?v=aDkofQthvt0 ❖ Unilateral facial paralysis involving seventh cranial nerve; usually temporary; indications include inability to close eye, decreased corneal reflex, increased lacrimation, drooping mouth, speech difficulty; eating difficulty; nursing interventions include protect head from cold and drafts, administer analgesics, assist with electrical stimulation, teach isometric exercises for facial muscles and also gentle massage and warm packs, prevent corneal abrasions ( artificial tears), sunglasses during the day, eye patch at night, reassure client that client has not had a stroke, provide emotional support for altered body image. ➢ TX: ■ Prednisone (to reduce edema), specific antiviral agents, electrotherapy may help prevent atrophy of facial muscles. ➢ Nursing Intv: ■ Apply moist heat to affected area (for pain), massage pt’s face with a gentle upward motion 2-3 times a day for 5-10min, apply fascial sling to improve lip alignment, provide frequent oral care, provide support. Provide thickened liquids due to difficulty swallowing 5. Dysphasia → Speech impairment, causes: brain trauma, brain tumor, neurological disorder. 6. Respiratory: Respirations (2 questions) ❖ To measure respirations place hand on abdomen, observe a complete respiratory cycle, then count respirations for 30 sec and multiply by 2, if respirations are slow or irregular count for 1 full min, normal rate is 12-20 per min. ➢ Normal Breath Sounds: Vesicular slow low pitched breezy sounds, heard over peripheral lung sounds. ➢ Diaphragmatic breathing: resp using diaphragm, normal rhythmic breathing, chest muscles not used, occurs with pleurisy, pericarditis, fractured ribs. ➢ Abnormal breath sounds: Adventitious sounds: crackles, non- musical cracking sound, wheezes( high pitched), rhonchi( low pitched) snoring, rattling, stridor (high pitched whistle). ■ https://www.easyauscultation.com/lung-sounds-reference-guide ➢ Breathing Pattern: apnea, biot’s bradypnea (varying and slow w/ periods of apnea), cheyne stokes (fast then slow w/ period of apnea), rapid breathing, regular, hyperventilation (resp. alkalosis), hypoventilation, tachypnea, diaphragmatic. ➢ Hyperventilation: rapid breathing over prolonged time that will cause 02/CO2 imbalance. ■ S/SX: tingling, numbness on tip of lips, fingers, toes, dizziness, spots before eyes, carpopedal spasm. ■ TX: breathing into a bag. Hypoxia: insufficient cellular oxygen ■ S/SX: apprehension, restlessness,dizziness, confusion, fatigue, tachycardia, hyperpnea, dyspnea. Interventions: multiple pillows when lying down, medications, oxygen, relaxation, physical reconditioning. Orthopnea: breathing made difficult when in supine or prone position, and made easier when in a sitting or standing position. Can be caused by left ventricular failure or other cardiac or resp disorders. Pt sleeps w/ 3-5 pillows for comfort. 7. Bladder: Neurogenic 8. Bladder dysfunction related to a lower motor lesion of the spinal cord. AKA : flaccid (inability to get rid of urine) or spastic/reflexive (continually contracted/spasms) neurogenic bladder. Manifested by incontinence; frequency; urgency; a reflexive neurogenic bladder manifested by no control of micturition causing an over distention of bladder and incontinence; sensory neurogenic bladder manifests with poor bladder sensation, infrequent voiding and large residual voiding; intermittent catheterization most common method of bladder management; important to determine bladder volume and amount of residual urine when deciding how often to catheterize client. a. TX: i. Focused on preventing complications such as infections, overdistention, kidney damage, & minimizing social and psychological effects of the disorder. ii. Medical management: anticholinergic drugs to decrease hyperactivity, Cholinergic to increase muscle tone. Muscle relaxants to decrease external sphincter tone, Desmopressin to treat nocturia, Botulinum to paralyze muscles of the external sphincter, Bladder retraining including voiding at certain times assuming body postures that make voiding possible, diet low in calcium, to avoid stone formation. iii. Surgical Management: TURP, Urinary catheterization, urethral dilation, external sphincterotomy, implant of artificial sphincter. b. Nursing Intv: Monitor for s&s of infection, encourage plenty of fluids, measure I&O, encourage mobility, refer to enterostomal for urinary diversion if needed, educate pt about condition c. S & S: Incontinence, frequency, urgency 9. Stroke (Cerebrovascular Accident) (6 questions) → know setting priorities, understanding concept, making nursing judgments, recognizing and recalling information ❖ Sudden disruption in blood supply to brain resulting in sudden loss of brain function that may be temporary or permanent; caused by thrombotic embolism, ischemia, or hemorrhage; indications include loss of movement, thought, memory, speech, or sensation; nursing responsibilities include encouraging the client to attain maximum independence, stimulating multiple senses, repeating directions and breaking down tasks into components, facing the client and speaking clearly slowly, giving the client time to respond, maintaining skin integrity and providing exercises (ROM and facial), self-care activities, and teaching Stating, antihypertensives, and platelet-inhibiting meds decrease incidence of CVA. Recombinant t-PA dissolve obstructive blood clots. t-PA therapy nursing interventions: withhold anticoagulants for next 24hrs, weigh patient to determine dose, and vital signs ( 15min first 2hrs, 30min for next 6hrs, every following hour until 24hrs after treatment). ➢ Transient Ischemic attacks (TIS): transient interruption of blood flow to the brain, it is a warning sign for stroke, repeated TIS can cause brain damage, cause includes clot in the brain, blood vessel injury, blood vessel stenosis. Risk factors: atrial fibrillation, high cholesterol,hypertension, diabetes mellitus, family history, age over 65. ➢ S/SX: they last minutes to hours, include unilateral vision loss, hemiparesis,numbness, loss of sensation, aphasia, dizziness, vertigo, tinnitus, vision changes, dysarthria, dysphagia, coordination problems. ■ Diagnostic tests: CT, MRI, 12 lead electrocardiogram, carotid ultrasound. ➢ TX: Modification of risk factors 10. Respiratory: Infections (2 Questions) ❖ Acute Bronchitis: inflammation of the bronchioles ➢ S&SX: repetitive coughing with sputum, caused by virus or bacteria. ➢ TX: rest, increase fluid intake, humidifiers, antibiotics, antipyretics, analgesics. Nursing responsibilities: listen to breath sound, encourage them to take antibiotics, push fluids. ❖ Upper respiratory infection: rhinitis, sinusitis ➢ S&SX: rhinorrhea,nasal congestion,nasal discharge, sneezing, tearing watery eyes, sore throat; indications of sinusitis include facial pressure, stuffy nose, purulent nasal discharge, headache, ear pain, dental pain, prevention includes frequent hand washing, cover mouth when coughing or sneezing, avoid people with infections; encourage client to increase fluid intake, elevate head of bed, throat lozenges for sore throat notify health care provider if stridor, drooling, difficulty swallowing or if there is moderate to severe shortness of breath. ❖ Legionnaires disease: pneumonia caused by legionella pneumophila which is a gram negative organism found in water. Risk factors include advanced age,severe immunosuppression, end- kidney stage kidney disease,diabetes, smoking, and pulmonary disease; ➢ S/SX: malaise, headache, dry nonproductive cough, dyspnea, chest pain, and elevated temperature; treatment includes oxygen therapy, possible mechanical ventilation, IV fluids, and possible temporary kidney, dialysis. ➢ Nursing Intv:: careful respiratory monitoring; assess for shock, provide oxygen. ➢ Inflammatory process that results in edema of lung tissues and extravasation of fluid into alveoli causing hypoxia; indications include fever, leukocytosis, cough productive of rust-colored, green, or whitish-yellow sputum, dyspnea, pleuritic pain, tachycardia, administer antibiotics, assess vital signs every 4hrs, cough and deep breathing q2 hour, assess breath sounds, incentive spirometer, encourage fluid to 3000 ml/24hrs, semi-Fowler’s position, administer oxygen therapy. ❖ Respiratory infections in children: caused by viruses, ages (6 months- 3 years) ➢ S/SX: fever, listlessness, irritability, anorexia, vomiting, diarrhea, nursing care: Warm or cool mist, rest, careful handwashing, antipyretic, offer fluids. Aspirate nose, ❖ Respiratory Syncytial Virus: most important pathogen in infancy and early childhood. ➢ S/SX: rhinorrhea,low-grade fever, cough, wheezing, tachypnea, treatment, increase humidity, encourage fluids, rest, ribavirin, ➢ Nursing Intv: From suspected RSV → droplet, contact and standard precautions. For definitive RSV → only contact and standard precautions are taken. Place in separate room or with other children that have the same diagnosis. Do not provide care if pregnant. 11. Arterial Blood Gases (2 questions) → know how to draw as skill Overview: Value Normal Acidosis Alkalosis pH 7.35-7.45 less than 7.35 greater than 7.45 PaO2 80-100 mm Hg SaO2 95%-98% PaCO2 45-35 mm Hg Resp. > than 45 mmHg Resp. < 35 m HCO3 22-26 mEq/L Met. < than 22 mEq/L Met. >26 mEq/L ❖ Distinguish between acidosis vs alkalosis, respiratory vs metabolic, and compensated vs uncompensated. Perform Allen’s test to determine the adequacy of peripheral blood flow to the extremity. To prepare for the test, perform Allen test to check collateral circulation, obtain arterial blood in heparinized syringe, ensure that blood does not clot or that air bubbles are not present; posttest, apply pressure to site for 5 minutes to prevent hematoma, place specimen on ice and occlude the needle to avoid air in syringe, note on lab slip if client is breathing room air or oxygen and how much oxygen, check arm for swelling, discoloration, pain, numbness, and tingling. ❖ Nursing Intervention: do not draw if just suctioned 15 minutes and changed position 12. Sickle Cell Disease ❖ Hereditary severe chronic anemia condition in which abnormal hemoglobin distorts erythrocytes, increases their fragility, and causes them to become sickled in shape and rigid; periods of exacerbation called crises occur; ➢ S/SX: are systemic and include chronic anemia (hemoglobin, 6 to 9 g/dL), possible growth retardation and delayed sexual maturity, pain (often especially focused on joints), swelling, jaundice, priapism, impaired renal function, cardiac murmurs, altered pulmonary function, increased susceptibility to infection ➢ Nursing Intv: include rest, oxygen, IV fluids and electrolytes, sedation, analgesia, possible transfusion; nursing interventions include promote rest, administer analgesia as prescribed and teach use of patient-controlled analgesia (PCA) pump as indicated, administer oxygen, maintain I and O and ensure adequate fluid intake, monitor for infection, encourage activity as tolerated when not in crisis. Follow normal immunizations + pneumococcal regardless of age ➢ TX: Although there is no cure for sickle cell anemia, treatment is preventative and palliative. Primary treatment modalities include: Bone marrow transplant (BMT), hydroxyurea, arginine, long-term red blood cell (RBC) transfusion. During painful vaso-occlusive crisis: Sedation, analgesia, blood transfusions, oxygen therapy, oral and intravenous fluids (large amounts of both), analgesics (to relieve pain) ➢ Sickle cell crisis/vaso-oclusive crises → sickle cell gets stuck . DO NOT USE COLD COMPRESS → vasoconstricts. Use warm compresses 13. Respiratory: Acute Disorders (2 questions) ❖ Atelectasis: collapsed or airless lung condition (alveoli collapsed); indications include dyspnea, cyanosis, cough tachycardia, pleuritic chest pain; nursing considerations include suctioning, postural drainage, antibiotics, turn, cough and deep breathe ❖ Pulmonary Embolism: an obstruction of the pulmonary artery, usually caused by embolism from lower extremity thrombosis; indications include pleuritic or anginal chest pain, acute dyspnea, restlessness and apprehension; nursing care includes administering IV heparin, elevating head of bed, administering prescribed oxygen ❖ Flail chest: abnormality of the chest wall occurring when two or more ribs fracture which creates a segment of rib that is not attached on either end;these fractures cause chest wall to become unstable and respond paradoxically; flail area moves in with inspiration and out with expiration; immediate respiratory failure may result and mechanical ventilation may be required with the use of high inspiratory pressures; nursing considerations: monitor for shock, administer humidified oxygen, pain management, monitor ABGs, encourage turning, deep breathing, coughing ❖ Pleurisy: inflammation of the pleura; nursing care: position semi-Fowler’s to high-Fowler’s to aid breathing, encourage respiratory toilet hourly, treat pain as ordered ❖ Pneumothorax: lung collapse caused by accumulation of air or fluid in the pleural cavity; indications include pleuritic pain, tachypnea, diminished breath sounds; treatment includes chest tubes. ➢ Nursing intervention: insert the chest tube ASAP to remove fluids 14. Liver Cancer → know nursing judgments ❖ Usually develops as metastasis from esophagus, stomach, colon, rectum, breasts, lungs; can also be the primary site. Only 7% of patients live for 5 years after the diagnosis ➢ S/SX: Most liver cancer is asymptomatic until it has advanced beyond the point at which it can be resected. Epigastric or right upper quadrant abdominal pain, fatigue, anorexia, weight loss: later indications include jaundice, ascites, bleeding. ➢ TX:While a very small number of primary liver tumors are resectable, most patients are so sick with liver disease that the risk of surgery is often too great. Radiation and chemotherapy have been used with mixed results but always to alleviate symptoms not to cure the cancer. ➢ Nursing Intv: Nursing care ■ For a patient undergoing surgery, monitor for cardiopulmonary complications and liver dysfunction. ■ Monitor intravenous blood and fluids, including 10% glucose, postoperatively. ■ Monitor the biliary drainage system and instruct patient on its use and care after she is discharged, including keeping it clean by irrigation with sterile saline. ■ Instruct the patient receiving chemotherapy and radiation to recognize complications and side effects and report these to the physician. ■ Instruct patient on how to care for the chemotherapy infusion site. ■ Help patient and her family to cope with the poor prognosis. ■ Be sure patient has adequate pain medications, good nutritional support, and adequate treatment of any complications. ■ Help family to make the decision to choose hospice care when needed 15. Meniere’s Disease ❖ Meniere’s disease is caused by dilation of the endolymphatic system. Meniere’s disease is a disease of the inner ear characterized by too much endolymph fluid in the membranous labyrinth. It can lead to severe hearing loss and debilitating episodes of vertigo. The disease occurs with equal frequency in men and women and may affect either ear or both ears. ➢ S/SX: include tinnitus (ringing in ears), unilateral sensorineural hearing loss, vertigo,Intense vertigo (dizziness), with associated pallor, nausea, vomiting, and sweating, lasting minutes to hours, Feelings of imbalance, Episodic, progressive hearing loss, Pressure in the ear ➢ TX: includes salt and fluid restriction to decrease amount of endolymphatic fluid, antihistamines, antiemetics, corticosteroids, low sodium diet and surgery. ➢ Dx: choloric stimulation test: cold water → eyeball will move and back. Hot water → moves towards and away = positive for meniere’s disease ■ Surgical Tx: ● Endolymphatic sac surgery in which a shunt is installed to drain excess endolymph and to relieve pressure ● Ototoxic medicine (e.g., gentamicin) infusion into the inner ear, to diminish vestibular function and reduce vertigo ● Vestibular nerve section, to relieve vertigo by severing the nerve communication pathway to the brain 16. Mantoux Test ❖ Tuberculin skin test, tubercle bacillus extract, purified protein derivative (PPD) given intradermally in the forearm; read in 48-72 hour ❖ induration (hard area under skin) of 5 or more millimeters is considered positive in HIV-infected persons, recent contact of a person with tuberculosis (TB) disease, persons with fibrotic changes on chest radiograph consistent with prior TB, clients with organ transplants, persons who are immunosuppressed for other reasons (e.g., taking the equivalent of greater than 15mg/day of prednisone for 1 month or longer or taking tumor necrosis factor-alpha ❖ induration of 10 or more millimeters is considered positive in recent immigrants (less than 5 years) from high-prevalence countries, injection drug users, residents and employees of high-risk congregate settings, mycobacteriology laboratory personnel, person with clinical conditions that place them at high risk, children less than 4 years of age, infants and children and adolescents exposed to adults in high-risk categories; induration of 15 or more millimeters is considered positive in any person, including persons with no known risk factors for TB; however, targeted skin testing programs should only be conducted among high-risk groups; induration indicates exposure to TB or presence of inactive (dormant) disease. ➢ Nursing Intv: ■ The mantoux test determines whether a person has been infected with TB bacillus. Tubercle bacillus extract (tuberculin), purified protein derivative (PPD), is injected into the forearm. ➢ Procedure: ■ Use intermediate-strength PPD in a tuberculin syringe with half-inch 26 or 27 gauge needle ■ Insert the needle (bevel facing up) into the intradermal layer of the inner aspect of the forearm, approximately four inches below the elbow. ■ Inject 0.1 mL of the PPD, creating a wheal or bleb ■ Record site, antigen name, strength, lot number, date and time of the test ■ Wait 48 to 72 hours to read test result : ● A reaction occurs when there is both induration and erythema present ● Inspect area and lightly palpate across injection site from normal area of skin to the margins of the induration ● Measure the induration (not erythema) in millimeters (mm) at its widest part 17. Parkinson’s Disease (3 questions) a. https://www.youtube.com/watch?v=VIEUEV9wlyI ❖ Parkinson’s disease is a chronic disease of the nervous system characterized by fine, slowly spreading tremor, muscular rigidity and altered gait; nursing care includes encouraging finger exercises (e.g., piano playing, range of motion (ROM) as appropriate, teaching client ambulation modification, referring to physical therapy, teaching goose-stepping walk, walking with wider base, concentrating on swinging arms while walking, turning around slowly using small steps; promoting family understanding of the disease, intellect not impaired, sight and hearing are intact, teaching that disease is progressive but slow, does not lead paralysis, referring for speech therapy, potential stereotactic surgery; administering medication. ➢ Nursing Intv: ■ Parkinson’s disease is slowly progressive, degenerative disorder that can appear at any age and affect both sexes but mostly commonly appears in men over age 60. ➢ S/SX: ■ Gradual onset, tremor (beginning with a pill-roll tremor), Muscle rigidity (uniform or jerky), Bradykinesia (abnormally slow movements), Gait disturbances (difficulty walking), High-pitched monotone voice, Mask-like facies (poor blink reflex, wide open eyes, Loss of postural control (body bends forwards when walking) , Dysphonia (slow, monotonous slurred speech), Micrographia (shrinking, slow handwriting), Depression, dementia, sleep disturbances, and hallucinations ➢ TX: ■ Treatment is mainly palliative and not curative. The object is to maintain as high a level of function as possible for as long as possible. Unfortunately, response to medications is often transient and symptoms inevitably become progressively medication resistant. ● Medical Therapy ◆ Levodopa is combined with carbidopa (Sinemet), to reduce side effects of levodopa (e.g., confusion, hallucinations, depression, sleep alterations) ◆ Dopamine agonists (e.g., pergolide), to postpone use of levodopa and carbidopa ◆ Anticholinergics (e.g., trihexyphenidyl) to control tremor and rigidity ◆ Monoamine oxidase inhibitors (e.g., selegiline ([symmetrel]), to reduce rigidity, tremor, and bradykinesia → no tyramine foods 18. Gastric Cancer ❖ Malignant neoplasm of the stomach; predisposing factors include with Helicobacter pylori, history of pernicious (B12 deficiency) anemia, ingestion of pickled foods, salted fish, salted meat, nitrates in smoked foods. Most gastric cancers, which are adenocarcinomas, occur in any part of the stomach. The tumor infiltrates the surrounding mucosa, penetrating the stomach wall and adjacent organs. At the time of diagnosis, the liver, esophagus and duodenum are often affected. Prognosis is poor. ➢ S/SX: Early stages: may be absent, Progressive disease: anorexia, dyspepsia (indigestion), weight loss, abdominal pain, constipation, anemia, indigestion, abdominal discomfort and/or pain, nausea, vomiting, obstructive symptoms, weight loss, feeling full after a small meal ➢ TX: is surgical resection combined with chemotherapy or radiation therapy- cure is possible if tumor is isolated and hasn’t spread. ■ Post-op: watch for S&S’s ➢ Nursing Intv: includes monitoring for postoperative complications (pneumonia, hemorrhage, bowel obstruction, dumping syndrome), administering enteral feeding, observing teaching about how to prevent dumping syndrome. 19. Cardiac: Heart Diseases (2 questions) ❖ Angina Pectoris: chest pain is quick or slow in onset, caused by myocardial ischemia, and often related to coronary artery disease ➢ S/SX: indications include retrosternal (or slightly to left of sternum) chest pain that radiates usually to left shoulder and upper arm proceeds down arm into fingers; may also radiate to right shoulder, neck, jaw, or epigastrium; usually lasts less than 5 minutes; may describe pain as usually mild or moderate in severity and as squeezing, burning, aching, or bursting pressure and may often say that pain is like gas, indigestion, or heartburn; dyspnea, pallor,palpitations, dizziness, and diaphoresis; pain that is aggravated by activity and relieved by rest and nitrates ➢ TX:relieved by rest and nitroglycerin; surgical interventions: percutaneous transluminal coronary angioplasty (PTCA) or coronary artery bypass graft surgery (CABG) ➢ Nursing Intv: teach about medications for prevention (antiplatelet agents vasodilators, beta blockers, and calcium channel blockers); pain relief (nitrates given sublingually); teach about nitroglycerin purpose and appropriate usage; encourage control of modifiable risk factors such as high cholesterol, smoking, hypertension, diabetes mellitus, obesity, lack of exercise, and stress ❖ Coronary Artery Disease (CAD): most prevalent form of cardiovascular disease in adults ➢ non modifiable risk factors: age, gender (men are prone), family history of heart disease, ethnicity (african americans are prone) ➢ modifiable risk factors: smoking, hypertension, elevated serum cholesterol levels, inactivity, obesity, diabetes mellitus; atherosclerosis causes ischemia which results in angina, myocardial infarction (MI), and sudden cardiac death; focus is to prevent disease by modifying modifiable risk factors; ❖ Infective Endocarditis: infection of heart lining and valves ➢ S/SX: fever, malaise, back and joint pain, splinter hemorrhages under fingernails and toenails, petechiae in conjunctiva and mucous membranes, heart murmur; ➢ TX: IV antibiotic for 4-6 weeks, may need surgery for heart valve replacement ❖ Cardiomyopathy: disease of the heart muscle which can lead to heart failure, dysrhythmias, and death; most common form is dilated cardiomyopathy (affects systolic) → significant dilation of the ventricles without hypertrophy of the muscle; other forms include restrictive cardiomyopathy (affects diastolic) → muscle size stays the same, but less ventricular volume and ejection fraction arrhythmogenic cardiomyopathy (affects diastolic) → right ventricular dysplasia (scar tissue replaces fibrous tissue in R ventricle) ➢ S/SX: signs and symptoms of heart failure ❖ Tamponade: excessive fluid accumulates in the pericardium causing decreased venous return to heart which decreases cardiac output causing compression to the heart. Caused by penetrating injuries, metastasis, cardiac surgery, advanced heart failure. ➢ S/SX: decreased systolic blood pressure, narrowing pulse pressure, increased venous pressure and muffled heart sounds ➢ TX: is removal of the fluid in the pericardial sac ➢ Nursing Intv: for pulsus paradoxus (systolic blood pressure is lower during inhalation than exhalation), hemodynamic status, assists with pericardiocentesis ❖ Cor Pulmonale: right ventricle fails as a result of a pulmonary condition (buildup of fluid) ➢ S/SX:: exertional dyspnea, productive cough, fatigue, weakness, jugular venous distention (JVD), and peripheral edema ➢ Nursing Intv: include rest, fluid restriction diuretic administration, monitoring vital signs, cardiac rhythm, arterial blood gases (ABG’s), intake and output and weight ❖ Pericarditis: inflammation of the pericardial sac; cause unknown or observed with myocardial infarction, end-stage kidney failure, bacterial infections, cardiac surgical procedures, or autoimmune disorders ➢ S/SX: chest pain is sharp, occurs suddenly, severity varies with position changes; pericardial friction rub auscultated; fever may be present ➢ TX: includes administration of NSAIDs and corticosteroids, and specific therapies for bacterial infection or autoimmune disorders ➢ Nursing Intv: administration of NSAIDS or corticosteroids, positioning, monitoring for complications, pericardial effusion and cardiac tamponade. 20. IV: Implanted Infusion Port ❖ Central venous catheter connected to an implanted subcutaneous port that is surgically implanted into a subcutaneous pocket on the chest wall. An implanted infusion port is one type of central venous access device (CVAD). A central venous catheter is connected to the implanted port and surgically connected to a subcutaneous pocket either on the anterior chest wall or on the forearm. Benefits: long-term IV therapy, little care required, allows patients freedom of movement, less thrombogenic and less prone to infection than external, short-term devices. ➢ Nursing Intv: includes dressing changes using strict aseptic technique, flush catheter on schedule with appropriate solution, use non-coring needle (Huber-point needle) to access. Risks: Pneumothorax, air embolism, clotted or displaced catheter, sepsis, hyperglycemia, rebound hypoglycemia, fluid overload 21. Respiratory: Oxygen Therapy (2 questions) ❖ NO: candles, cigarettes in area, sign posted on the door to the room, grounded electrical outlets, avoid use of electric razors, hair dryers, electric blankets, electric heaters that may cause spark, avoid flammable or oil based products, it tank is used, secure in upright position ❖ Oxygen toxicity: rare condition that can cause acute respiratory distress syndrome ❖ Low oxygen delivery systems include: ➢ nasal cannula (20%-40%FIO2) 1-5 L/min ■ assess the patency out nostril, apply water soluble jelly to nostrils every 3-4 hours, and perform a good mouth care ➢ simple face mask (40%-60%FIO2)- flow rate 5-10L/min ■ Remove mask every 1-2 hours, wash, dry, apply lotion to skin, provide emotional support to decrease feeling of claustrophobia ➢ partial rebreather mask (50%-75%FIO2)- flow rate 6-15L/min ■ adjust O2 flow to keep reservoir bag 2/3rds full during inspiration ➢ non-rebreather (80%-100%FIO2)- flow rate 10-15 L/min ■ bag should never collapse High-flow oxygen delivery systems include: ➢ venture mask (24%-55%FIO2)- flow rate 4-10L/min ■ gives most accurate amount of O2/ good for COPD patients ➢ Aerosol mask, face tent, tracheostomy collar (24%-100% FIO2)- flow rate 10L/min ➢ Face tents are rarely used except to provide children with mist, tent should only be opened when necessary, make sure tent is tucked in tightly, check temp inside tent and change child’s clothing as needed, no stuffed toys because they will become wet 22. Cough & Deep Breathe → After surgery or immobility for any period of time, client develops pulmonary disorders → for the prevention of atelectasis and DVT ➢ Nursing Intv: ■ coughing and deep breathing, will alleviate these problems ■ client may use incentive spirometer or may just take several deep breaths and cough ■ once mucous is disturbed the client will cough it up, ■ Independent nursing activity: ● Each cycle includes 3 deep breaths and 1 deep cough, 10Xs every 1-2 hours 23. Brachytherapy (2 questions) ❖ Implants (aka seeds, internal radium implants, internal radiation) that are radioactive that are used at tx site, usually a malignant lesion. Seeds are usually placed in body tumor and source is then sealed. If seed becomes dislodged, radiology should be called immediately. ➢ Nursing Intv: ■ save all dressings and bed linens until the source is removed and then discard the dressings and linen as usual.This is done to ensure that no radiation source is in linen or dressings: urine, feces, and linen are not radioactive ■ Nurse should not stand close or in line with radioactive source. ■ Organize care so limited time is spent in pt.s room (nurses should switch to prevent prolonged exposure per nurse → 30 minutes per shift) ■ Encourage pt. to do own care, pt must stay in bed while implant is in place, position source of radiation is verified by radiography 24. American Cancer Society Warning Signs (Caution) CAUTION C: Change in bowel or or bladder habits A: A sore that does not heal U: Unusual bleeding or discharge from any body orifice T: Thickening or a lump in the breast or elsewhere I: Indigestion or difficulty swallowing O: Obvious change in a wart or mole N: Nagging cough or hoarseness ❖ Risk Factors of Cancer: ➢ Smoking/chewing tobacco ➢ Excessive exposure to UV rays of sun ➢ Exposure to ionizing radiation ➢ Exposure to chemicals, aromatic amines and aniline dyes. Pesticides, formaldehydes, arsenic, soot, tars, asbestos, benzene, nickel, zinc ores, polyvinyl chloride ➢ Family HX cancer ➢ High consumption of alcohol, fat, salt cured meats, smoked meats, and nitrate containing food ➢ Overweight ➢ Prolonged estrogen replacement therapy ➢ Viruses with carcinogenic potential, e.g. Epstein-Barr virus, Herpes Simplex virus type 2 ❖ To reduce cancer risk: ➢ NO smoking ➢ increase fresh vegetables, fiber, vitamin C, ➢ weight control, reduce dietary fat ➢ limit alcohol, overexposure to sun, avoid carcinogens: sun, asbestos etc. 25. Epilepsy (2 questions) Chronic disorder characterized by recurrent seizure disorder, symptoms of brain or central nervous system (CNS) irritation. Classification generalized seizure: a. tonic-clonic seizure (begins with tonic phase and immediate loss of consciousness, followed by clonic phase, rhythmic jerking of all extremities) i. Signs and Symptoms: 1. Beginning with loud cry 2. Change in LOC 3. Body stiffening- alternating between stiffening and relaxation 4. Tongue biting, incontinence, labored breathing, apnea, cyanosis 5. On wakening: possible confusion, difficulty talking 6. Drowsiness, fatigue, H/A, muscle soreness, weakness b. absence seizures- brief periods of loss of consciousness like day-dreaming, more common in children i. Signs and Symptoms: 1. Blinking or rolling eyes, blank stare 2. Slight mouth movements c. myoclonic seizure- brief jerking of extremities i. Signs and Symptoms: 1. Brief involuntary muscular jerks of the body or extremities d. atonic seizures- sudden loss of muscle tone, client falls; complex partial seizure-client backs out for a few seconds, automatism may occur e. simple partial seizures- remains conscious, often reports aura i. Signs and Symptoms:: 1. sensory(flashing lights, smells, auditory hallucinations) 2. Autonomic (sweating, flushing, pupil dilation) 3. Psychic (dream states, anger, fear) f. idiopathic- occur for no known season; Nursing intv: g. Include observing and documenting type and progress of seizure activity and postictal behavior, O2 and suction at bedside; post-seizure, position on back with head turned to side or position on side to prevent aspiration and promote drainage of secretions; treatment includes medication. TX: h. Medications: phenytoin, carbamazepine, and ethosuximide i. Surgery if meds don’t work j. Emergency tx for status epilepticus consists of diazepam, lorazepam, lorazepam, fosphenytoin, phenobarbital, 50%dextrose I.V., thiamine IV * check blood levels regularly 26. Cardiac: Blood Pressure(2 questions) Pressure exerted by circulating volume of blood on walls of arteries, veins and chambers of the heart; cover 40% percent of limb from shoulder to olecranon with cuff (primary cause of falsely elevated BP when cuff it too narrow. Check both arms and compare results, knowing difference of 5 to 10 Hg is normal a. Hypertension: i. Persistent elevation of the systolic blood pressure above 140 mmHg and diastolic blood pressure above 90 mmHg 1. Prehypertension: 120-139/80-89 2. Hypertension Stage 1: 140-159/90-99 3. Hypertension Stage 2: 160+/100+ a. may or may not have symptoms: symptoms may include: b. headache, dizziness, angina pain 4. Hypertensive Urgency: 160/110 5. Hypertensive Emergency: 180/120 b. nursing care includes: i. administering antihypertensive medication ii. teaching about medication side effects, weight control, moderate alcohol intake, increase physical activity, smoking cessation, importance of health care follow up. c. Pulse Pressure: normal pulse pressure (diff between sys-dias) is 30-40 mmHg. d. Postural Hypotension(Orthostatic): drop in BP within 3 minutes after sitting or standing, drop of more than 20 mm Hg systolic or more than 10 mm Hg diastolic S/SX: 1. Dizziness, lightheadedness, syncope Causes: 2. Dehydration, hemorrhage, vasodilation, tachycardia, Nursing Intv: 3. Safety, obtain BP and pulse after lying for 10 minutes, assist to sitting position with legs dependent of each other and after 2 mins take BP and pulse, assist client to stand and immediately take BP and pulse every 2 mins for 10 minutes. If pt. Displays symptoms have client sit/ or lying position 4. Have pt. Change positions slowly, dangle legs at end of bed before sitting or standing 27. Glaucoma (2 questions) Abnormal increase in intraocular pressure (intraocular pressure IOP) leading to visual disability and blindness; causes obstruction of outflow of aqueous humor; indications include cloudy or blurry vision or loss of vision, artificial lights appear to have rainbows or halos around them, decreased peripheral vision, pain, headache, nausea, vomiting a. Nursing Intv: instruct about correct usage of prescribed medication (miotics), avoid tight collars, instruct about the danger signs of glaucoma – brow arching, halos around lights, blurry vision, diminished peripheral vision, headache, or eye pain. Chronic open angle glaucoma (symptoms don’t appear until late) include mild eye aching, seeing halos and night blindness not corrected with glasses. Acute narrow angle glaucoma (rapid onset) pressure over the eye, moderate pupil dilation not reactive to light, cloudy cornea and blurring, and photophobia. b. TX: includes beta-adrenergic blockers (timolol or betaxolol), epinephrine, or carbonic anhydrase inhibitor, mitotic eye drops. Interventions: watch for hyphema (hemorrhaging into the anterior chamber of the eye). 28. Increased Intracranial Pressure (2 questions) → know understanding flow of ICP Cranium is a closed cavity; increase in pressure causes shifting of brain; causes of increased intracranial pressure include bleeding, tumors, edema; indications include change in level of consciousness, restlessness, confusion, pupil changes, motor changes, cardiac rate changes, headache, nausea and vomiting, diplopia (double vision). Effects cranial nerves → 3, 4, 6 a. TX: i. osmotic diuretics, steroids, antihypertensives, anticonvulsants, hyperventilation, surgery for decompression or shunt b. Nursing Intv: i. includes maintaining airway by suctioning, elevating head of bed 30 degrees, keeping head in midline position, administering fluids as ordered ii. Check for cushing’s triad: irregular resp., bradycardia, systolic hypertension (widening pulse pressure) 29. Spinal Cord Injury (5 questions) → know early and late signs Indications include loss of motor and sensory function below level of injury ❖ spinal shocks symptoms (flaccid paralysis, complete loss of all sensation, decreased pulses, suppression of somatic and visceral reflexes), postural hypotension, edema, alteration in normal thermoregulation ❖ nursing consideration include skeletal tractions, administer steroid therapy, move client by log-rolling technique, provide good skin care provide emotional support, ensure adequate nutrition, bladder and bowel training, catheterization, client and family education to cope with detailed care at home, prevent complication of autonomic dysreflexia. ❖ Risk factors: under 32 of age in males, car accident, trauma, compression fractures osteoporosis ❖ Complication of of Spinal Cord Injury: DVT, skin breakdown, UTI’s ❖ Spinal cord injury/rehabilitation potential: ➢ https://www.youtube.com/watch?v=PseUxltIw_U ➢ C3 and above ■ are unable to care for self, life-sustaining ventilatory support essential ➢ C4 are unable to care for self, may self-feed with powered devices (depending on respiratory function) C5 can drive electric wheelchair, may be able to feed self with powered devices ➢ C6 may self-propel a lightweight wheelchair, may feed self with devices, can write and care for self, can transfer from chair in bed ➢ C7 can dress lower extremities, minimal assistance needed, independent in wheelchair, can drive car with hand controls ➢ C8 same as C7 in general activities easier ➢ T1-T4 have some independence from wheelchair, long leg braces for standing exercises ➢ T5-L2 still require wheelchair, limited ambulation with long-leg braces and crutches ➢ L3-L5 may use crutches or cane for ambulation ➢ L5-S3 ambulation. 30. Respiratory: Chronic Obstructive Disorders (4 questions) ❖ Illnesses or disorders occurring in respiratory tract. Starts in the nose and mouth and continues into the lungs, may involve part of all of the respiratory tract. It includes infectious processes as well as abnormalities. ➢ Asthma: ■ Chronic inflammatory disease of the airways caused by increased responsiveness of tracheobronchial tree to various stimuli. ■ S/SX: cough, dyspnea, wheezing, ■ TX: assess respiratory status, administer medications, use peak flow meter, MDI, avoid asthma triggers. ➢ Status Asthmaticus is a medical emergency: ■ Nursing Intv: correcting dehydration, and acidosis, improving ventilation, assessing color, respiratory effort, LOC, pulse oximetry, frequent blood gases, SaO2 90%, IV therapy, inhale short acting beta2 agonists. ➢ Bronchiectasis: ■ Chronic dilation of bronchi, frequently on the lower portion of the lung caused by long standing infection. May be acquired or congenital. Involves one or both lungs. ■ S/SX: cough, dyspnea, increased sputum production and wheezing ■ TX: antibiotics, postural drainage, possible resection of diseased areas of lung, ■ Nursing Intv: thorough assessment of respiratory system, O2 sat, elevation of ABGs, increase oral intake, patent airway, sterile suctioning with strict hyperoxygenation prior to suctioning, restrictions on patients activity levels. ➢ Bronchospasm: ■ Narrowing of lumen of bronchi due to muscle spasm. Is frequently associated with reactive airway diseases such as asthma and bronchitis ■ S/SX: coughing frequently and wheezing ■ TX: steroids, bronchodilator, maintain airway ➢ Occupational Lung Disease: pneumoconioses- Silicosis, asbestosis, coal miners,(black lung disease, coal workers lung disease) farmer’s lung, histoplasmosis related to inhaling mineral or inorganic dust, manufactured fibers, metal dusts, biological dusts, or toxic fumes in workplace. Causes lung fibrosis and changes within the lung that lead to dyspnea, respiratory distress, respiratory failure and death. ■ TX: similar to COPD and/or lung transplant 31. Trigeminal Neuralgia (Tic Douloureux) a. https://www.youtube.com/watch?v=wYpWgeC3K-s b. Risk factors: multiple sclerosis, compression of the blood vessels c. Background for RN Care: Condition of the trigeminal nerve causing involuntary contraction of facial muscles and episodes of extreme facial pain. Trigeminal nerve is fifth cranial nerve and controls facial sensation, corneal reflex, and mastication. i. Consists of three branches: 1. Ophthalmic 2. Mandibular 3. Maxillary. ii. Pain is most significant in maxillary and mandibular divisions. d. Overview: Type of neuralgia involving one or more branches of the fifth cranial nerve. i. Causes: infections of sinuses, teeth, mouth, or irritation of the nerve from pressure. ii. Indications: stabbing or burning facial pain that is excruciating, unpredictable, and paroxysmal; twitching grimacing of facial muscles. iii. Nursing Considerations: include identify and avoid stimuli that exacerbate the attacks, administer anticonvulsants and analgesics, avoid rubbing the eye, and chew on opposite side of the mouth. iv. Surgical interventions: microvascular decompression of the trigeminal nerve and percutaneous radiofrequency trigeminal gangliolysis. 32. Cardiopulmonary Resuscitation (CPR) a. Overview: process of externally supporting circulation and respiration; failure to institute ventilation within 4-6 minutes results in brain damage; sequence is CAB (compression-airway-breathing). If the rescuer witnesses the collapse start by activating EMS. If the rescuer doesn't witness the collapse start by establishing unresponsiveness, breathing, and pulse. If victim drowned or is a child, rescuer starts with 2 min of CPR before activating EMS. i. Step 1: establish unresponsiveness, breathing, and pulse. ii. Step 2: Activate EMS. iii. Step 3: Start Compressions, 100/min, depth (2in for adult) or (1/3 a-p diameter or 2in child) or (1/3 a-p or 1.5in in infant). iv. Step 4: establish airway using head/chin tilt; if trauma suspected then use jaw thrust. v. Step 5: breathing. 8-10 breaths/min ensure chest rise. b. Compression-ventilation rate: Adult: 30:2 1 or 2 rescuers. Infant/Child 30:2 for 2 rescuers. Neonates: 3:1 for 1 rescuer, 30:2 for 2 rescuers. 3:1 ratio facilitates provision of adequate minute ventilation, which is considered critical for the vast majority of newborns who have an asphyxial arrest. 15:2 ratio recognizes that newborns with a cardiac etiology of arrest may benefit from a higher compression to ventilation ratio. c. Infant CPR: CAB: i. Circulation: check the brachial artery for 10 sec for a pulse; if it is not found, compress the lower sternum with two to three fingers 1/3 of the ap diameter or 1.5 in; allow chest to recoil between compressions; minimize interruption of compression; if necessary, interruption should be less than 10 seconds; use the hand farthest from the infant's head; 1. ratio for 2 rescuers: 15 compressions to 2 breaths at rate of 100 compressions per min; 2. ratio for 1 rescuer: 30 compressions to 2 breaths at a rate of 100 compressions per minute. ii. Airway: Open airway with head tilt/chin lift maneuver. iii. Breathing: assess for breathing; if the infant is not breathing, place mouth over the infant's mouth and nose and ventilate the infant; observe chest rise. d. The Heimlich Maneuver: only be performed for a conscious, choking client, who is showing severe obstruction, demonstrated by the inability to speak. If the client is in bed, position a backboard or other rigid surface beneath client. Instead of abdominal thrusts, perform chest thrusts for a client who is pregnant or obese 33. Electroencephalogram (EEG) a. Electrodes detect brain activity b. Do not give any stimulants (coffee, tea) or meds in order to get accurate reading c. Overview: Records electrical activity of the brain; i. Nursing Care: in preparation for the test includes explain procedure; tranquilizer, cigarettes, and stimulants (coffee, cola, tea) withheld according to institution policy; client may be asked to hyperventilate 3-4 minutes and watch bright flashing light, eat regularly scheduled meals; posttest care includes help client remove paste from hair, administer prescribed medication withheld before EEG, observe for seizure activity in clients who are seizure-prone. d. Essential Nursing Care: i. Purpose: EEGs can help identify seizure disorders, head injuries, intracranial lesions (such as abscesses and tumors), TIAs, stroke, or brain death. ii. RN Care: Prep: not to sleep night before EEg, if recommended. No anti seizure meds, tranquilizers, stimulants, and depressants for 24-48 hrs before. Explain tech will apply paste and attach electrodes to areas of skin on the patient's head and neck after these areas have been lightly abraded to ensure good contact. Discuss any specific activity that the patient will be asked to perform, such as hyperventilating for 3 minutes or sleeping, depending on the purpose of the EEG. e. Aftercare: i. Use acetone to remove any remaining paste from the patient’s skin. ii. Encourage patient to resume normal activities, as ordered 34. Eye Trauma i. Leading cause of blindness -- occupational injuries, sports, assault, mva, explosions. ii. Medical treatment: removal of foreign object, antibiotic systemically or eye ointment, surgery as indicated (vitrectomy or enucleation or repair of detached retina or ocular surface grafting). iii. Nursing Considerations: 1. Chemical: if chemical in eye, flood immediately with saline or running tap water. 2. Foreign Object: do not remove or jar to prevent further injury and apply no tight covering. Use eye shild or stiff small inverted paper cup, administer tetanus immunization. iv. Client Education: activity restriction, take a medication as needed, keep eye patched, use eye lubricant as directed, return for follow-up appointments as directed. v. Community Education: prevent trauma by providing safe toys, use eye protectors when working with chemicals or tools and when playing sports, protect eyes from ultraviolet light vi. When chemicals in eyes → flush it out immediately, but only to inner to outer canthus vii. If there is foreign object → do not try and remove, cover it w/ eye patch and go to doctor immediately 1. Administer tetanus if there is a foreign object 35. Cardiac: Heart Failure (3 questions) a. Failure of the heart to pump enough blood to meet metabolic (oxygen and nutrient) demands of tissues, left and right ventricles can fail separately. b. Left-sided failure indications: dyspnea, orthopnea, cough, crackles, tachycardia, fatigue, anxiety, restlessness, confusion. c. Right-sided failure indicators: jugular vein distention (JVD), dependent edema (especially lower extremities and progressing up the body eventually up to the abdomen), hepatomegaly, right upper quadrant tenderness, increasing hepatic dysfunction, ascites, anorexia, nausea, weight gain, weakness, respiratory distress, abdominal pain, altered liver function and liver function tests, gastrointestinal distress. d. Treatment: oxygen, digoxin, diuretics, vasodilators, potassium supplements, low-sodium diet, bed rest. e. Nursing Responsibilities: promoting physical and emotional rest, high fowler’s position, assessing vital signs, lung sounds, intake and output, good skin care, and client education 36. Lung Cancer (2 questions) a. Malignancy in epithelium of respiratory tract; cigarette smoking is the primary risk factor; no effective screening test, limited treatment options, usually poor prognosis; b. Indications: change in respiratory patterns, persistent cough, bloody or purulent sputum, unexplained dyspnea, unexplained weight loss, recurrent pulmonary system problems, pain in arm or shoulder or chest or back. c. Interventions include surgery, chemotherapy, radiation. d. Nursing Interventions Related to Surgery: usual preoperative and postoperative teaching (especially related to respiration), maintenance of chest tube drainage system. e. Nursing Interventions Related to Chemotherapy and Radiation: gentle and careful skin care, administration of antiemetics and analgesics, provide mouth care, appealing small frequent meals high in calories and protein, hair care, including coping with alopecia, balance rest with activity 37. Myasthenia Gravis (2 questions)8 a. https://www.youtube.com/watch?v=bYGxGdu9MsQ b. Systemic disturbance (auto-immune disease) of nerve impulse transmission because of deficiency of acetylcholine at myoneural junction; exacerbations and remissions. c. Indications: muscular weakness after repeated or sustained movements; muscles regain strength after rest; diplopia, ptosis; weakness of facial muscles; impaired speech; dysphagia; respiratory distress that might become severe in myasthenic or cholinergic crisis; no muscular atrophy; no loss of sensation; no loss of intellect. d. Nursing Interventions: administering medications (anticholinesterases, corticosteroids) and stressing the importance of taking them on time, based on prescription, physiologic needs, living patterns; give good eye care; maintain optimal mobility; encourage deep breathing and coughing; have suction at bedside; may need oxygen; provide environment that is restful and free of stress; teach client to avoid factors that may precipitate myasthenic crisis (eg: infections, emotional upsets, use of streptomycin neomycin, which produce muscular weakness); teach to recognize symptoms of myasthenia crisis (sudden inability to swallow, speak, or maintain patent airway) 38. Cardiac: Valvular Disease (3 questions) → know Peripheral Arterial Disease vs. Peripheral vascular Disease a. Cardiac: Valvular Disease i. Mitral Stenosis: valve opening narrows preventing normal flow of blood from left atrium to left ventricle. ii. Mitral Regurgitation: the mitral valve does not close completely during systole, which allows backflow of blood into the left atrium. iii. Indications: dyspnea, fatigue, weakness, palpitations, or cough due to pulmonary congestion. iv. Treatment: same as for heart failure: 1. oxygen, digoxin, diuretics, vasodilators, potassium supplements, low-sodium diet, bed rest. v. Mitral Valve Prolapse: valvular leaflets enlarge and prolapse into left atrium; may progress to mitral regurgitation. vi. Aortic Stenosis: aortic valve narrows and obstructs left ventricular outflow during systole. vii. Aortic Regurgitation: regurgitation of blood from the aorta back to left ventricle during diastole. viii. Stenosed valves: do not open freely; scarring and retraction of valve leaflets result in incomplete closure. ix. Murmur: sound made by turbulent blood flow through normal or abnormal valves. Classified according to when murmur occurs during cardiac cycle. Graded according to intensity. 1. Grade I: barely audible and heard only in a quiet room, and then with difficulty. 2. Grade II: faint but recognizable. 3. Grade III: moderately loud and easy to hear with the stethoscope on the chest. 4. Grade IV: loud and accompanied by palpable thrill. 5. Grade V: very loud and can be heard with one corner of the stethoscope lifted off the chest wall. 6. Grade VI: extremely loud and can be heard with the entire stethoscope slightly above the chest wall. Work load increases until heart fails. x. Indications: dyspnea on exertion, orthopnea, paroxysmal nocturnal dyspnea, hepatomegaly, neck vein distention, pitting edema. xi. Treatment: diuretics, beta blockers, digoxin and oxygen, surgical reconstruction or replace of the valve. xii. Nursing Considerations: ensure the client understands the medication, the prophylactic use of antibiotics and help client balance rest and activity. b. Cardiac: Arterial Disorders i. Arterial Insufficiency: 1. Indications: rubor, cool shiny skin, cyanosis, ulcers, gangrene, impaired sensation, intermittent claudication. 2. Nursing Care: monitoring peripheral pulses, maintaining good foot care. 3. Treatment: sympathectomy, grafting, vasodilators. 4. Client Education: avoid crossing legs, regular exercises, place legs in dependent position to relieve pain at rest, smoking cessation. ii. Arteriosclerosis: condition that involves thickening of the walls of the arteries, reducing the ability of the heart to contract effectively. A chronic condition that develops over a number of years. The most common form of arteriosclerosis is atherosclerosis, which is characterized by the presence of cholesterol-lipid-calcium deposits in arterial walls. Risk factors are characterized as modifiable or non-modifiable. iii. Aortic Stenosis: narrowing of the aortic valve; causes decreased cardiac output and heart failure; usually hear murmur. 1. Treatment: aortic valvotomy (surgery to open the valve) via cardiac catheterization or open or closed heart surgery or aortic valvuloplasty or aortic valve replacement via cardiac catheterization or open heart surgery. iv. Atherosclerosis: due to accumulation of fat, neutrophils, macrophages, and platelets in the intima and media layers of arteries; damage to the vascular endothelium precipitates a chronic inflammatory process; damage caused by hypertension, diabetes mellitus, smoking, increased low density lipoprotein (LDL) levels decreased high density lipoprotein (HDL) levels and increased homocysteine levels; injured endothelial cells produce decreased amounts of protective cytokines and increased inflammatory cytokines are formed resulting in fatty streak and eventual atherosclerotic plaque formation. 1. Nursing care: identification of risk factors, education about lifestyle changes, and education about medications. v. Pulmonic Stenosis: narrowing of the entrance to the pulmonary artery. Resistance to blood flow exiting the right side of the heart causes right ventricular hypertrophy. Severity of defect = severity of symptoms. 1. Treatment: pulmonary valvotomy via cardiac catheterization or open or closed heart surgery or pulmonary valvuloplasty or pulmonary valve replacement via cardiac catheterization or open heart surgery. c. Peripheral Vascular Disease: caused by thrombus formation: may be arterial (arteriosclerosis, Raynaud’s disease, Buerger's disease) or venous (venous insufficiency, varicose veins, thrombophlebitis). i. Indications (Arterial): rubor, cool shiny skin, cyanosis, ulcers, gangrene, impaired sensation, intermittent claudication, decreased peripheral pulses. ii. Indications (Venous): cool, brown skin, edema, ulcers, pain, normal or decreased pulses, performing dorsiflexion of the foot, Homan’s sign, is contraindicated as it might dislodge the clot resulting in pulmonary embolism. iii. Predisposing Factors (Arterial): smoking, exposure to cold, emotional stress, diabetes mellitus, high-fat diet, hypertension, obesity. iv. Treatment (Arterial): sympathectomy, grafting, vasodilators, anticoagulants, endarterectomy. v. Predisposing Factors (Venous): immobility, pregnancy, heredity, obesity, surgery, heart failure, injury to vein wall, hypercoagulability. vi. Nursing Interventions (Arterial): monitor peripheral pulses, lower legs, do not cross legs, encourage regular exercise, stop smoking, administer vasodilators, anticoagulants. vii. Nursing Interventions (Venous): monitor peripheral pulses, elevate legs, carefully measure and apply elastic antithrombotic stockings, establish and monitor intermittent pneumatic compression device as ordered, administer anticoagulants are ordered, maintain bed rest until anticoagulants are started, apply warm moist packs. viii. Intermittent Claudication: cramping, pain, aching experienced in lower extremity muscles during exercise; amount of exercise should not cause pain unless there is arterial circulation impairment; pain usually relieved by stopping the activity causing the pain; usually indicates aorta, iliac, femoral, and/or popliteal disease; could also be an indicator of coronary, carotid, or cerebral artery disease. ix. S/S PAD: shiny smooth hairless skin, decreased or absent pulses, bruit or thrill over site of occlusion. x. Diagnosis: blood flow studies (ankle-brachial index, angiography, plethysmography) xi. Treatment: regular exercise program, stopping to rest when pain occurs, increasing time exercising without pain slowly and regularly, angiography with stent placement or removal of clot, arterial bypass surgery 39. Guillain Barre Syndrome a. Progressive inflammatory autoimmune response occurring in peripheral nervous system, results in compression of nerve roots and peripheral nerves. i. Indications: paresthesia, pain often occurring in glove-and-stocking distribution, hypotension, tachycardia, vasomotor flushing, paralytic ileus, profuse sweating; motor losses symmetrical, usually beginning in lower extremities, then extend upward to include trunk, upper extremities, cranial nerves, and vasomotor function. ii. Nursing Considerations: administer steroids in acute phase, aggressive respiratory care, prevent hazards of immobility maintain adequate nutrition, pain-reducing measures, eye care, psychological support to deal with fear, anxiety, and altered body image 40. Meningitis a. Infection or inflammation of membranes covering brain and spinal cord; bacterial, viral, or fungal in origin. i. Indications: h/a, fever, photophobia, signs of meningeal irritation (nuchal rigidity, Kernig’s sign, Brudzinski’s sign, opisthotonus position), changes in level of consciousness, seizures; in infants indications include refuse feedings, vomiting, diarrhea, bulging fontanelles, vacant stare, high pitched cry. ii. Diagnostic Tests: Lumbar Puncture to test CSF for increase pressure, increase protein, decrease glucose, + Kernig’s, + Brudzinski's iii. Nursing Interventions: administer antibiotics or antifungals as ordered, observe for increased intracranial pressure, maintain seizure precautions, maintain adequate fluids and electrolyte imbalances. iv. Treatment: 1. Immediate antibiotics to stop the multiplication of bacteria is necessary. IV for 2 wks and orally thereafter. a. Penicillins, Cephalosporins, Vancomycin with rifampin (for resistant strains) b. Dexamethasone as adjunct therapy for bacterial meningitis. c. Supportive care for viral meningitis. d. Digoxin to control arrhythmias. e. Mannitol to decrease cerebral edema. f. Phenytoin (Dilantin) for seizures or sedatives to reduce restlessness. g. Acetaminophen for h/a and fever h. Vaccination as prophylaxis for high risk population i. For contacts of meningitis patients: antimicrobials i. Rifampin ii. Cipro iii. Rocephin 41. Headache (3 questions, 2 tension, 1 migraine) a. Tension: most common headache. i. Indications: mild to moderate pressure or tightness, bilateral, discomfort worse with activity. ii. Nursing Considerations: careful assessment of onset of s/s and triggers, patterns, presence of lethargy, weakness, nausea, vomiting, instruct about analgesics, relaxation techniques, massage, moist hot packs to neck. b. Migraine: recurrent vascular headache, lasts 4-72 hrs. i. Indications: severe pain, throbbing in nature, unilateral, associated with nausea, vomiting, diarrhea. Sometimes prodromal aura present (lights, lines, tastes, odors, tingling, vertigo, tinnitus), blurred vision, photophobia, focal neurological symptoms (vertigo, dysarthria, ataxia, diplopia), scalp tenderness, mood alterations. ii. Interventions: prevention with various medications and modifying trigger factors, treatment of attacks with ergotamine, NSAIDs, antiemetics, sumatriptan, and a quiet dark room and lying down can be helpful. c. Indications for Immediate Follow Up in Children: increased frequency and severity of headache, headaches that awaken a child at night, early morning headaches, headaches that worsen when child gets out of bed in morning, any changes in behavior or personality 42. Coma (2 questions) a. Sustained unconsciousness. b. Indications: no response to verbal stimuli, no voluntary movement, possibly varying responses to painful stimuli, possible altered pupil response to light, no blinking, possible altered respiratory pattern; preventing complications is a priority. c. Nursing Interventions: frequent objective assessment, especially of neurological status (including alertness for potential seizures); enteral feeding (parenteral if paralytic ileus) to give nutrition and prevent muscle wasting; prevent fluid volume deficit; frequent turning or oscillating bed to prevent pneumonia and decubiti; side rails up and bed in lowest position to prevent injury; eye drops or artificial tears to keep cornea moist and prevent abrasions, possibly use protective shield over eyes or tape eyes closed; maintain airway, suction as needed; frequent oral care; passive range of motion for joint mobility and to decrease muscle wasting; extremity positioning in correct alignment to prevent contractures; sequential compression stockings to prevent venous thromboembolism (VTE) 43. Suctioning a. Explain procedure; elevate head of bed to semi-fowler, hyperoxygenate client, use sterile technique; lubricate the catheter with sterile saline, insert the catheter without applying suction, and advance the catheter as far as possible; withdraw the catheter and apply suction for 10 sec; rotate catheter when withdrawing. b. Wall Unit / Portable Unit: i. Adult: 100-150 mmHg / 10-15 ii. Children: 100-120 mmHg / 10-12 iii. Infants: 80-100 mmHg / 8-10 iv. Neonate: 60-80 mmHg / 6-8 44. Cardiac: Myocardial Infarction (2 questions) → know setting priorities, acute MI vs STEMI a. MI: partial blockage i. S3 heart sound indicates an MI b. STEMI: complete blockage of the Coronary artery dx’d on 12-lead EKG → elevated ST segment c. Formation of localized necrotic areas within the myocardium, usually following the sudden occlusion of a coronary artery and the abrupt decrease of blood and oxygen to the heart muscle. d. Indications: severe crushing chest pain, may radiate to arms and/or jaw and/or neck and/or back, dyspnea, nausea, vomiting, gastric discomfort, indigestion, apprehension, restlessness, fear of death. e. Enzymes: creatine kinase (CK), its isoenzyme CK-MB, myoglobin, troponin T and I. i. CK increases 3-6 hours post myocardial infarction (MI), peaks 24-36 hours, and returns to normal by day 3. ii. CK-MB (most rapid) increases in 4-8 hours, peaks in 12-24 hours, and returns to normal in 3-4 days. iii. Myoglobin increases in 1-3 hours, peaks in 4-12 hours, and returns to normal 12 hours after the MI. iv. Troponin T or I increases in 3-4 hours, peaks in 4-24 hours, and returns to normal in 1-3 weeks. f. Nursing Care: providing thrombolytic therapy, relieving family’s anxiety, ensuring bed rest, monitoring vital signs and intake and output, instructing about modification of lifestyle. i. Lifestyle Modifications: 1. Stop smoking 2. Reduce stress. 3. Regular physical activity. g. Essential Nursing Care: i. MOnitor and record ECG readings, blood pressure, temperature, and heart and breath sounds. Frequently monitor the ECG to detect heart rate changes or dysrhythmias. ii. Assess pain and administer analgesics, as ordered. Record the severity and duration of pain. Avoid giving IM injections because absorption from the muscle is unpredictable. iii. Check the client’s bp after giving nitroglycerin, especially the first dose. iv. Watch for signs and symptoms of fluid retention (crackles, cough, tachypnea, and edema), which may indicate impending heart failure. Carefully monitor daily weight, intake and output, respirations, and serum enzyme levels. v. Assist with range-of-motion exercises and ambulation, as allowed. vi. Promote comfort, rest, and emotional well-being. Involve client’s family to participate in care as much as possible. vii. Evaluate the client 45. Tuberculosis a. Infectious disease of insidious onset that primarily affects the lungs. b. S/S: fatigue, lethargy, anorexia, weight loss, low-grade fever, and productive cough with mucopurulent (bloody) sputum. c. Diagnostics: Mantoux test, sputum positive for acid-fast bacilli x 3 sputum test and chest X-ray. d. Treatment: 9 month regimen of isoniazid combined with streptomycin, ethambutol, rifampin, or pyrazinamide. e. Education: instruct client to cover mouth and nose with tissue when coughing, sneezing, laughing, burn tissues, to perform good hand washing, to practice good nutrition, to take full course of medications, to return to clinic for sputum smears f. 2 stages: i. Active TB: has S&S → Weight loss, lack of energy, and night sweats (late sign) ii. Dormant TB: no S&S, but TB is present 46. Ear Surgery a. Stapedectomy: surgical removal of stapes and replacement with a prosthesis to treat hearing loss caused by otosclerosis. i. Postop: reinforcing dressing. Avoid blowing nose, sneezing, and coughing. Position on unaffected side. Observe for facial nerve damage, infection, vertigo, tinnitus. Instruct client to avoid getting water in the ear, flying, drafts, and crowds of people with upper respiratory infections. b. Tympanoplasty: restore or improve hearing by repairing the ear drum or small bones. c. Tympanostomy: tubes placed after at least 6 months of bilateral otitis media with effusion. Tube place in tympanic membrane (eardrum) to equalize the pressure in and for ventilation of the middle ear. Done to allow drainage of effusion to promote healing and prevent scarring and loss of elasticity leading to hearing loss. i. Complications: plugged tubes, repeat replacement, persistent perforation, atrophy of eardrum, cholesteatoma. ii. Patient Education: use of earplugs to prevent water from entering the ear, notify HCP if tube (small plastic circle) falls out. d. Myringotomy: incision in tympanic membrane to insert tympanostomy tubes due to recurrent and chronic otitis media. i. Nursing considerations: include no diving, jumping, or submerging in water without earplugs, keep bath water and shampoo out of ear. Wear earplugs when swimming in lake water. Inform parents that tubes will eventually fall out, notify practitioner when this occurs. ii. Postop: keep mouth open when sneezing or coughing, avoid upper respiratory infections, and keep ear dry for 6 weeks 47. Respiratory: Treatments a. Chest tubes: placed in the pleural space to drain air and blood so that the lung can re-expand. Drainage system consists of one or more chest tubes. Collection container placed below the chest and a water seal is used to keep air from entering the chest. i. RN Responsibilities: observing for constant bubbling in the water-seal chamber (indicates a leak in the drainage system). If chest tube becomes dislodged, apply pressure over the insertion site with a dressing that is tented on one side to allow for the escape of air. If the tube becomes disconnected from the drainage system, cut the contaminated tip off of the tubing using sterile scissors and immerse the end of the chest tube in 2 cm sterile water until system can be reestablished. ii. Complications: pneumothorax, hemothorax, cardiopulmonary complications, respiratory distress, infection, pulmonary edema, formation of air leak, atelectasis (alveolar collapse), and tension pneumothorax. b. Continuous Positive Airway Pressure (CPAP): mode of ventilation for spontaneously breathing client in which slight pressure is administered throughout the respiratory cycle to prevent alveolar collapse during expiration. i. RN Considerations: securing tracheal tube, monitoring vital signs, airway patency, and neurological, cardiac, and respiratory status, and ensuring ventilator alarms are functioning. c. Pneumonectomy: surgical removal of lung. Do not turn client on operative side immediately following surgery because increases stress on suture line and increases risk of mediastinal shift. i. Indications of mediastinal shift: trachea is shifted toward operative side, shortness of breath, respiratory distress. ii. PostOp: client should lie on operative side to allow fluid left in the space to consolidate, move from back to operative side hourly, encourage client to cough and deep breathe, administer pain medication. Splint chest when coughing 48. Eye: Detached Retina a. Retina is a nervous tissue membrane of the eye that perceives light images of external objects and transmits impulses to the optic nerve. Detachment is separation of retina form choroid, resulting from trauma to the eye, aging process, diabetes or tumors. b. Indications: flashes of light, blurred or “sooty” vision, sensation of particles moving in line of vision, delineated areas of vision blank, feeling of a curtain coming up or down, loss of vision, confusion, apprehension. c. Treatment: surgery to reattach the retina by laser, scleral buckling, or other intraocular procedures. d. Interventions: maintain bed rest. Patch for affected eye or both eyes (as ordered by health care provider), positioning based on surgical procedure performed and location of detachment, and as prescribed by health care provider. e. Client Education: prevent bumping head, do not move eyes rapidly, avoid rapidly jerking head, delay hair washing for 1 week, do not perform strenuous activity for 3 months, use of stool softeners to avoid straining at stool, maintain head in position as ordered by health care provider 49. Thrombocytopenia a. Excessive destruction of platelets. Increased platelet count (100,000-400,000/mm3) indicates improvement. Immune Thrombocytopenic Purpura (ITP) is the autoimmune form. i. Causes: infections, medications, immune disorders, portal hypertension. ii. S/S: petechiae, prolonged bleeding with even minor trauma, spontaneous bleeding, easy bruising, heavy menses. iii. Treatment: removal or treatment of underlying cause, blood and or platelet transfusions. iv. Nursing Considerations: assess activities that increase risk for bleeding, avoid constipation, monitor for internal and external bleeding, use humidifier or nasal saline spray to prevent drying nasal passages. v. Client Education: bleeding precautions (use soft toothbrush, electric razor), avoid contact sports, dental floss, ASA, NSAIDs, feverfew, ginger, ginkgo, garlic, kava, and corticosteroids, and contact health care provider if there is a head or abd trauma, inform every HCP of bleeding potential, and wear closed heel and toe shoes and socks. vi. Child Pt. Instructions: no contact sports, bike riding, skateboarding, climbing, or running; encourage quiet activities 50. Blood Administration a. Nursing Care: identify client. Check for allergies and previous blood reactions, using 19-gauge needle and standard blood filter, starting infusion slowly during first 15 min and staying with client, taking vital signs before, after 15 minutes, and every hour or per agency protocol. Check for reactions, infusion over 2 to 4 hours, changing administration set with every unit. b. Transfusion Reaction: immunogenic or nonimmunogenic response to blood products. May cause reactions in all major body systems. S/S and specific treatments vary according to causes. General standard procedures include stop the blood, restart the saline, notify hcp, provide supportive care. i. Types of reactions: usually occur within the first 50 mL of transfusion, which is usually within first 15 minutes, so nurse should remain with client during that time. 1. Allergic: hypersensitivity to donor antibodies. Urticaria, pruritus, fever, anaphylactic shock. 2. Hemolytic: incompatibility. Nausea, vomiting, pain in lower back, hypotension, hematuria. 3. Febrile: antibodies to donor platelets or leukocytes. Fever, chills, nausea, headache, flushing, tachycardia. 4. Bacterial: contaminated blood products. Tachycardia, hypotension, fever, chills, shock. ii. Circulatory Overload: may also occur from infusion of blood at too rapid a rate for client size and condition. Cough, dyspnea, pulmonary congestion, tachycardia, headache, sudden anxiety, hypertension, distended neck veins. c. Fresh Frozen Plasma (FFP): plasma volume expander, uncoagulated plasma separated from red blood cells (RBCs), high in coagulation factors V, VIII, and IX. i. Action: increase plasma volume. ii. Use: treat post surgical hemorrhage and shock, replace a specific factor when that factor is not available individually for infusion. iii. Volume of one unit is 200-250 mL. iv. A/E: hypocalcemia may result from multiple transfusions of FFP. v. RN Considerations: infuse with a straight line IV set as fast as the client will tolerate. d. Platelet Transfusion: transfusion of only the platelet component of the blood. Used when blood clotting is problematic. Prepared from whole blood. i. 30-50 mL is one unit. e. Packed Red Blood Cells (PRBCs): red blood cells that have been separated from the plasma. Used for blood replacement when red blood cells are needed but not the fluid (plasma). Transfused like other products. 51. Hearing Impairment a. Hearing loss includes conductive, sensorineural, and mixed (both conductive and sensorineural). Conductive hearing loss caused by interruption of sound passing through the external auditory canal and middle ear. Related to cerumen in the ear , otitis media, or fixation of the auditory ossicles. b. Otosclerosis: fixation of the footplate of the stapes, one of the three small bones or ossicles in the middle ears. Stapes cannot vibrate and carry the sounds transmitted by the other two ossicles to the inner ear. i. S/S: conductive or mixed hearing loss, progressive in nature, with or without tinnitus. ii. Tx: surgical stapedectomy or stepedotomy. c. Sensorineural Hearing loss: caused by impairment of the functioning of the inner ear, auditory nerve, brainstem, or cortical auditory pathways. i. Causes: congenital, noise injury, aging, ototoxicity. d. Presbycusis: age-related hearing loss caused by inner ear changes. Decreased ability to hear pitched spuds. Important to enhance communication by positioning self directly in front of client, converse in a well-lit, quiet room, make sure client knows the nurse is speaking, speak clearly and slowly, do not shout, keep hands and other objects away from mouth when speaking, ask client to repeat statements, use appropriate hand motions, write message down if client is able to read. e. Hearing Aid Care: change batteries at least weekly, removing or disconnecting battery when not in use. Clean hearing aid with soft cloth do not use hairspray and perfume when wearing hearing aid, do not submerse in water 52. Glasgow Coma Scale a. Quick, practical, and standardized system for assessing level of consciousness. 1. 1-4 Eye Response 2. 1-5 Verbal Response 3. 1-6 Motor Response ii. Total 3-15 1. < 8 Coma 2. 3-8 Severe Head Injury 3. 8-12 Moderate Head Injury 4. 13-14 Minor Head Injury 5. 15 A/O b. Glasgow Coma Scale for Infants: Assess eye opening, verbal response, and motor response. Score of 15 indicates unaltered LOC. Score of 8 or below indicates comatose state. Verbal score in children under the age of 2 years assesses smiling crying, and interaction. A score of 2 on the verbal assessment is assigned to a child who is agitated and restless 53. Gag Reflex a. Involves gagging or vomiting if the throat and/or pharynx is irritated. In some cases, irritation can be as little as inspecting the throat with a tongue blade. Important to assess the gag reflex in a client who has a decreased level of consciousness before giving anything by mouth. To test the gag reflex the nurse looks for bilateral contraction of the palatial muscles initiated by stroking or touching either side of the posterior pharynx or soft palate with a tongue blade. If reflex weak or absent, client is in danger of aspirating 54. Positron Emission Tomography (PET) a. Used to assess metabolic and physiologic function of the brain to diagnose stroke, brain tumor, epilepsy, Parkinson’s disease, and head injury. Preparation includes withhold caffeine, alcohol, and tobacco for 4 hours before the test, according to agency policy. NPO status (nothing by mouth) for 6-12 hours before the procedure. Encourage fluids after the procedure 55. Inhalers: Metered Dose & Dry Powder a. MDI: aerosol, pressurized inhaler allows bronchodilators, mast cell stabilizers, and corticosteroids to be applied directly to site of action -- the lung and airways -- through the mouth. Enables smaller doses and rapid absorption and onset of action. “Maintenance” inhalers used daily to prevent acute respiratory distress. “Rescue” inhalers of short-acting medications used for immediate relief of acute respiratory distress. Give bronchodilators first. Remove the cap and shake the inhaler vigorously five or six times immediately before use. Breathe out all the way, then put the inhaler in the mouth or 1 to 2 inches in front of the mouth and depress the inhaler while inhaling deeply and slowly three to five seconds. If using a spacer, close mouth around mouthpiece, depress canister, and inhale deeply and slowly for three to five seconds. Hold the breath for several seconds after inhalation is complete. Exhale slowly through pursed lips. If repeating, wait two to five minutes. Rinse mouth with water after steroid inhalation to prevent oral candidiasis. b. DPI: use to deliver medications in the form of a dry, micronized powder directly into the lungs. Are easier to use than metered dose inhalers (MDIs). Do not require propellant. Deliver more medication than MDIs. Do not shake inhaler prior to administration, load medication as directed by manufacturer, exhale before inhalation of medication, position mouthpiece between lips, inhale deeply through mouth hold breath for 5 to 10 seconds, wait for prescribed time before next inhalation. Inform client that a gagging sensation may occur. Other topics Vangie mentioned…. 1. Asthma a. Asthma: i. Chronic inflammatory disease of the airways caused by increased responsiveness of tracheobronchial tree to various stimuli. ii. S/SX: cough, dyspnea, wheezing, iii. TX: assess respiratory status, administer medications, use peak flow meter, MDI, avoid asthma triggers. b. Status Asthmaticus is a medical emergency: i. Nursing Intv: correcting dehydration, and acidosis, improving ventilation, assessing color, respiratory effort, LOC, pulse oximetry, frequent blood gases, SaO2 90%, IV therapy, inhale short acting beta2 agonists. 2. Hypertension a. Persistent elevation of the systolic blood pressure. i. Normal < 120/80 ii. Prehypertension: 120-139/80-89 iii. Stage 1: 140-159/90-99 iv. Stage 2: 160+/100+ b. S/S: headache, dizziness, anginal pain, asymptomatic. c. Nursing Care: administering antihypertensive medication, teaching about medication a/e, weight control, moderate alcohol intake, physical activity, smoking cessation, importance of health care follow-up. 3. Murmurs a. Sound made by turbulent blood flow through normal or abnormal valves. Classified according to when murmur occurs during cardiac cycle. Graded according to intensity. i. Grade I: barely audible and heard only in a quiet room, and then with difficulty. ii. Grade II: faint but recognizable. iii. Grade III: moderately loud and easy to hear with the stethoscope on the chest. iv. Grade IV: loud and accompanied by palpable thrill. v. Grade V: very loud and can be heard with one corner of the stethoscope lifted off the chest wall. vi. Grade VI: extremely loud and can be heard with the entire stethoscope slightly above the chest wall. Work load increases until heart fails. 4. Chest tubes a. Placed in the pleural space to drain air and blood so that the lung can re-expand. Drainage system consists of one or more chest tubes. Collection container placed below the chest and a water seal is used to keep air from entering the chest. i. RN Responsibilities: observing for constant bubbling in the water-seal chamber (indicates a leak in the drainage system). If chest tube becomes dislodged, apply pressure over the insertion site with a dressing that is tented on one side to allow for the escape of air. If the tube becomes disconnected from the drainage system, cut the contaminated tip off of the tubing using sterile scissors and immerse the end of the chest tube in 2 cm sterile water until system can be reestablished. ii. Complications: pneumothorax, hemothorax, cardiopulmonary complications, respiratory distress, infection, pulmonary edema, formation of air leak, atelectasis (alveolar collapse), and tension pneumothorax. 5. Autonomic dysreflexia (I can’t find anything on Kaplan, found a Quizlet Kaplan for it) a. What is autonomic dysreflexia? i. Exaggerated autonomic responses to stimuli that are harmless in normal people, Acute emergency b. When does autonomic dysreflexia occur? i. Occurs only after spinal shock has resolved, mostly in T6 injuries and above c. Signs and symptoms of autonomic dysreflexia? i. Severe HA, HTN, blurred vision, Diaphoresis above level of injury, nasal congestion, apprehension, bradycardia, nausea d. Etiology of autonomic dysreflexia i. Bladder distention (most common), Skin irritation, Fecal impaction/constipation, ingrown toenails, thermal stimuli e. Nursing management for patient with autonomic dysreflexia i. GOAL: remove triggering stimulus ii. place in sitting position, check foley, disimpact fecal mass, remove skin irritation, prevent drafts of cold air Kaplan Med-Surg Comprehensive B Exam Topics 1. Alzheimer’s Disease → Chronic, progressive, disease resulting in cerebral atrophy, decline in cognitive function, motor and sensory function, and affect. ● Indications → changes in personality, motor restlessness, pacing, ● Stage 1 → memory loss, agitated or apathetic mood, attempts to cover up symptoms, depression, sleep disturbances ● Stage 2 → impaired language, motor ability, object recognition, bowel and bladder incontinence, inability to perform ADL, unable to recognize family members ● Stage 3 → loss of continence, ambulation, language skills, compulsive touching, decreased response to stimuli ● RN Responsibility → reorienting as needed, speaking slowly, providing clocks and calendars in client’s room, promoting sleep, hygiene, grooming, nutrition, safety, protecting from self-injury and injury to others, encourage social interaction, increasing self-esteem, assisting family to understand and cope. 2. ABG’s → Overview: Alkalosis greater than 7.45 Resp. < 35 m Met. >26 mEq/L ❖ Distinguish between acidosis vs alkalosis, respiratory vs metabolic, and compensated vs uncompensated. ❖ Perform Allen’s test to determine the adequacy of peripheral blood flow to the extremity. ❖ Obtain arterial blood in heparinized syringe, ensure that blood does not clot or that air bubbles are not present; posttest, apply pressure to site for 5 minutes to prevent hematoma, place specimen on ice and occlude the needle to avoid air in syringe, note on lab slip if client is breathing room air or oxygen and how much oxygen, check arm for swelling, discoloration, pain, numbness, and tingling. ❖ Nursing Intervention: do not draw if just suctioned or changed position → wait 15 minutes 3. Pancreatitis → Inflammation of pancreas that can be acute or chronic. Whipple - Increase lipase, decrease amylase. Clay colored stools. Glucose alteration. a. Acute: mild inflammation with minimal discomfort to severe disease that is unresponsive to any medication, ending in death. This is caused by the premature activation of enzymes, particularly trypsin, which then self-digest the pancreas. The process of self-digestion is often triggered by the obstruction of the common bile duct by gallstones, causing bile to reflux back into the pancreatic duct, which stimulates the premature activation of the pancreatic enzyme (normally, activation begins later in the duodenum.) i. S/S: Severe, acute abdominal pain, back pain, abd distension, N/V, decreased intestinal motility, fever, jaundice, ALOC, hypotension, ARF, tachycardia, respiratory distress, hyperglycemia, hypocalcemia. ii. Treatment: Parenteral nutrition, withhold oral intake so pancreatic enzymes are not stimulated. Nasogastric suction, Biliary drains and stents, surgery, and intravenous fluids after the initial crisis is over to restore electrolytes. 1. Meds: a. Histamine-2 (H2) antagonists. (cimetidine {Tagamet}, ranitidine {Zantac}), to decrease gastric acid production b. Analgesics for pain c. Antiemetics to prevent vomiting. iii. Nursing Care: 1. Record I & O hourly, and monitor electrolyte levels. 2. Patients with NG, good mouth and nose care and assess respiratory patterns regularly. 3. Administer pain meds 4. Watch for complications from parenteral nutrition (hypokalemia, overhydration, metabolic acidosis) and watch for signs of a calcium deficiency (cramps, tetany, seizures). 5. Monitor for glucose alterations, hyperglycemia/hypoglycemia. 6. Instruct patient on the need for lifestyle modifications to prevent recurrences and to avoid factors that aggravate the dx. (alcohol). b. Chronic: Characterized by the progressive destruction of the pancreas after repeated attacks of pancreatitis. Protein plugs and calculi in the pancreas form as a result of the hypersecretion of protein as a result of excessive alcohol consumption over long period of time. Alcohol is also toxic to pancreatic cells. Cells are eventually replaced by fibrous tissue, which obstructs the pancreatic and common bile ducts, blocking drainage to the duodenum. i. S/S: Attacks of severe abd and back pain, N/V, Anorexia, and weight loss, Malabsorption and foul-smelling stools with high-fat content (steatorrhea), and calcification of the pancreas. ii. Treatment: 1. Endoscopy, to remove duct stones and dilate strictures 2. Pain meds and avoidance of pain triggers (alcohol) 3. Diet, insulin, or oral antidiabetic agents, to treat diabetes if present 4. Pancreatic enzyme replacement, to treat malabsorption and steatorrhea 5. Surgery (pancreaticojejunostomy, pancreaticoduodenectomy or the Whipple procedure, to relieve pain, restore proper drainage of pancreas and to reduce the frequency of attacks. 4. Cast Care a. Immediate cast care: avoid covering cast until dry, handle with palms, not fingertips (plaster cast). Avoid resting cast on hard surfaces or sharp edges. Keep affected limb elevated above heart on soft surface until dry. Observe for blueness or paleness, pain, numbness on affected area. b. Intermediate care: encourage client to perform prescribed exercises, report any break in cast or foul odor, inform client to not scratch skin underneath cast and avoid putting anything underneath cast. Follow up with doctor if there is any numbness or tingling in the affected area c. Types of Casts: i. Non-plaster or fiberglass cast: 1. Consist of open-weave, nonabsorbent fabric impregnated with cool water-activated hardeners. Used for nondisplaced fracture and long-term wear. ii. Plaster cast: 1. Rolls of plaster are wet with cool water and smoothed onto body; a crystallizing reaction occurs and heat is given off. d. Complications: Pressure ulcers, Disuse syndrome, Compartment syndrome and delayed union or nonunion of fractures 5. Thermal Injury (2 questions) → ● First degree (Superficial partial-thickness)→ epidermis affected (destroyed or injured); painful, red, dry, min. or no edema ● Second degree (Deep partial-thickness) → epidermis and part of dermis affected; painful, red, exudes fluid, edema, blistered ● Third degree → Total destruction of epidermis, entire dermis, and in some cases subcutaneous tissue, muscle or bone; painless, varied color (white, red, black, brown or charred), dry, leathery, edema, presence of eschar, symptoms of shock, probable hematuria (RBC in urine) and hemolysis (breakdown of RBC’s) ● First responder interventions: ensure safety of yourself, extinguish flames, cool burn by briefly applying cool water to burn and clothing covering burn, remove other clothing, cover wound to prevent contamination, irrigate chemical burns, asses ABC’s ● Treatment: grafts → use of skin or other materials to cover burned areas ● Nursing Care: IV Lactated Ringers, plasma; F/C to monitor I/O (should be 30ml/hr), check for s/s of fluid overload vs. dehydration, monitor BP, v/s, weight, electrolytes, wound care at least once a day (administer pain meds 30min before wound care), sterile technique, tetanus prophylaxis; high caloric, high-carb, high-protein diet, may require parenteral nutrition; estimate TBSA (total body surface area) with the Rule of Nines 6. Head Injury (3 questions, 1 SATA) ● May be open or closed injury: trauma to scalp, skull, brain, loss of consciousness can occur with brain injury ● most common head injury is concussion, others are contusion, laceration, fractures ● Indications: changes in VS, confusion, disturbances of consciousness, sudden loss of neurologic deficits, pupillary abnormalities, sensory dysfunction, visual, hearing impairment, vertigo, headache, spasticity, movement disorders, seizures, hypovolemic shock ● Treatment: close observation, possible surgery, preservation of brain homeostasis and prevention of secondary brain damage, lower ICP, prevent seizures with anticonvulsants, maintain fluid and electrolyte balance, may intubate if needed, mechanical ventilation, and maintain NG ● RN responsibility: maintain airway, maintain fluid and electrolyte balance, NG feedings, prevent injury, improve cognitive function. Monitor adequate nutrition, O2, HOB elevated, pain, signs of ICP.. ● Dementia can occur secondary to head injury ○ Indications: displaying bx associated with mental disorders ○ RN considerations: monitor VS, especially HR, monitor attention, memory, and ability to perform simple tasks, LOC, reasoning 7. Dialysis (2 questions) → a. https://www.youtube.com/watch?v=mi34xCfmLhw → forward to 3:50 b. Peritoneal → removal of excessive fluids & wastes through the peritoneal cavity by surgically inserted catheter i. Before procedure → obtain baseline vitals, breath sounds, weight, glucose & electrolyte levels, warm fluid prior to procedure. ii. During procedure → infuse 1-2 L of fluid into cavity by gravity using sterile technique, leave fluid in for 20 minutes & then remove it by gravity iii. After procedure → take vital signs, check for respiratory distress, pain or discomfort, assess dressing around catheter for wetness iv. Complications → peritonitis (fever, abd pain & cloudy dialysis drainage, swelling, tenderness, redness or purulent secretions at site), abdominal pain, insufficient return of fluid v. Nursing Care → instruct patient to consume high protein & fiber diet c. Hemodialysis → removal of excess fluids & wastes by circulating patient’s blood through a semi-permeable membrane that acts as an artificial kidney i. Done through a mature AV shunt, fistula or graft (4-6 weeks old) → created by surgical anastomosis of an artery & a vein (usually radial artery & cephalic vein) 1. Complications→ air embolism, blood leaks, blockage/clotting, contamination & exsanguination ii. Nursing Considerations → check thrill & bruit every 8 hours, do not use that site for BP or blood specimens, assess site for infection, instruct patient to not lift anything heavy on that side or sleep on top of it, monitor closely for hypotension, N/V, malaise, HA, dizziness & muscle cramps 8. Medications: Sodium Channel Blockers ● https://www.youtube.com/watch?v=D8ft_3_oMYU ● antidysrhythmic, decrease conduction speed in the atria, ventricles, and His-Purkinje fibers ● may also cause current dysrhythmia to worsen or new ones to form ● 3 classes 1A slows repolarization, 1B speeds up repolarization, 1C may also create new dysrhythmias ○ Class A (Procainamide) → use for atrial and ventricular dysrhythmia, maintenance of normal sinus rhythm after conversion from Afib or flutter, ■ Adverse effects → seizure, dysrhythmias, diarrhea, hypotension, N/V, confusion, dizziness, agranulocytosis, chills, fever, systemic lupus syndrome, rash, blood dyscrasias, ■ RN consideration → monitor HR, rhythm, BP, CBC, liver enzymes, ■ Client Education → request assistance when getting out of bed and ambulation, carry medical identification regarding medication and disease process ○ Class A (Quinidine) → Use paroxysmal ventricular tachycardia, complete AV block, hepatotoxicity, acute asthma attack, angioedema, ■ A/E → vertigo, fever, HA, ventricular tachycardia, atrial fib or flutter, premature atrial and ventricular fib ■ RN consideration → check apical pulse and BP before administering med, monitor for atypical ventricular tachycardia and ECG EKG changes such as widening of the QRS complex ○ Class B (Lidocaine) → use premature ventricular contractions ■ A/E → hypotension, tremors, double vision, tinnitus, confusion, blurred vision, drowsiness, dizziness, ■ RN consideration → administer O2, keep resuscitation equipment available, use infusion pump for IV, cardiac monitoring, local anesthetic (prevents conduction of nerve impulses by inhibiting ion transport across membranes), assess for OD, ○ Class C (Flecainide) → use treat paroxysmal supraventricular contractions, ■ A/E → dizziness, HA, syncope, new or worsened dysrhythmias, cardiac arrest, edema, flushing, blurred vision, dyspnea, nausea, constipation, ■ RN consideration→ use med cautiously in client with heart failure, severe kidney or hepatic disease, sick sinus syndrome, ■ Contraindications → second or third degree heart block, recent MI, cardiogenic shock ● Class C (propafenone) → use life threatening ventricular dysrhythmias ■ A/E→ dizziness, ataxia, syncope, HF, bradycardia, ventricular tachycardia, premature ventricular contractions, v-fib, ■ RN considerations→ monitor K, BP, to avoid hypotension, do not crush extended release tablets 9. Parenteral Nutrition → intensive nutritional support, an excess of 2,500 kcal/ day. A hypotonic solution containing essential nutrients including protein, carbohydrates, electrolytes, vitamins, water, and trace elements. ● https://www.youtube.com/watch?v=jjs9F1QYUDA&t=301s ● Indications → unable to ingest, digest, absorb nutrients in oral foods ● Administered through catheter into subclavian or internal jugular vein ● contains high concentrations of glucose and proteins, hypertonic solutions (if given to fast client experiences glucose overload and excessive diuresis with the excretion of glucose), may develop dehydration and shock, HA, nausea, postural hypotension, seizures. ● Considerations → infection, fluid overload, phlebitis, metabolic complications ● During delivery, patient develops signs or air embolism (decreased LOC, anxiety, "feeling of impending doom" chest pain). Help patient lie on left side with head in trendelenburg position, it prevents air from flowing into the pulmonary veins, increases intrathoracic pressure which decreases amount of blood pulled into vena cava during inhalation. ● RN Responsibilities → check blood sugar often 10. Respiratory: Treatments → a. Chest tubes → https://www.youtube.com/watch?v=JB-CqwMyrTM i. placed in the pleural space to drain air and blood so that the lung can re-expand. Drainage system consists of one or more chest tubes. Collection container placed below the chest and a water seal is used to keep air from entering the chest. ii. Suction = 20 for adults and 15 for kids iii. RN Responsibilities→ observing for constant bubbling in the water-seal chamber (indicates a leak in the drainage system). If chest tube becomes dislodged, apply pressure over the insertion site with a dressing that is tented on one side to allow for the escape of air. If the tube becomes disconnected from the drainage system, cut the contaminated tip off of the tubing using sterile scissors and immerse the end of the chest tube in 2 cm sterile water until system can be reestablished. To remove → ask patient to do valsalva manuever. Dont “milk” line because it causes increase in pressure. iv. Complications→ pneumothorax, hemothorax, cardiopulmonary complications, respiratory distress, infection, pulmonary edema, formation of air leak, atelectasis (alveolar collapse), and tension pneumothorax. b. Continuous Positive Airway Pressure (CPAP): https://www.youtube.com/watch?v=iGD-erEWM4Q https://www.youtube.com/watch?v=OHQK5PUTQ_0 i. mode of ventilation for spontaneously breathing client in which slight pressure is administered throughout the respiratory cycle to prevent alveolar collapse during expiration. ii. RN Considerations→ securing tracheal tube, monitoring vital signs, airway patency, and neurological, cardiac, and respiratory status, and ensuring ventilator alarms are functioning. c. Pneumonectomy: surgical removal of lung. Do not turn client on operative side immediately following surgery because increases stress on suture line and increases risk of mediastinal shift. i. Indications of mediastinal shift: trachea is shifted toward operative side, shortness of breath, respiratory distress. ii. PostOp: client should lie on operative side to allow fluid left in the space to consolidate, move from back to operative side hourly, encourage client to cough and deep breathe, administer pain medication. Splint chest when coughing 11. Pain (2 questions) ● Subjective → it is whatever the patient says it is and it is wherever the patient says it is ● can be acute or chronic ● culture and past experiences with pain are a major factor ● Indications → increased BP, HR, rapid irregular respirations, pupil dilation, increased perspiration, increased muscle tension, apprehension and irritability, grimacing, guarding, verbalization of pain, crying in infants and children, ● RN interventions → establish therapeutic relationship, 24 hour pain profile, teach pt about pain and its relief, reduce anxiety and fears, provide comfort measures, administer pain meds, use preventative measures, ● Gate control theory: describes varied responses to pain stimuli, pain transmission to the CNS if the gate is open, pain transmission to CNS is absent if gate is closed. ● CNS modification of pain stimulus transmission due to distractions, relaxation, fatigue, anxiety, ● PSN modification of pain stimulus transmission due to rubbing, heat or cold application, or vibration Abdominal ● Visceral → poorly localized and dull, aching, burning, or cramping, ● Parietal → more localized or more severe and steady ● Referred → occurs at distant sites innervated at the same level as abdominal organ and highly localized at that distant site Back Pain ● risk factors → poor muscle tone, obesity, poor posture, poor body mechanics, smoking, stress Neuropathic ● poorly localized, may occur with minimal or no stimulation ● the peripheral or central nervous system does not process sensory describing as "shooting," sharp, burning, ● RN Care → administer analgesics, education about complementary and alternative therapies, emotional support, education about diabetes treatment measures 12. Cardiac: Dysrhythmias (2 questions) → rhythm disturbances of the heart caused by an interruption at any point in the normal conduction process SINUS→ SA node, tachycardia, bradycardia ATRIAL → premature atrial contractions (PACs), paroxysmal atrial tachycardia (PAT), atrial flutter, atrial fibrillation ● rapid irregular atrial contractions leading to ineffective atrial emptying of blood into the ventricles and irregular response of the ventricles ● blood pools in atria possible forming clots that can embolize to the body ● Causes → hypoxia hypercarbia, cardiac structural abnormalities ● Indications → irregular HR, ventricular response determines rapidity, dizziness, dyspnea, palpitations, syncope ● Diagnosis → electrocardiogram ● Treatment → TX other diseases causing the dysrhythmia, cardioversion, calcium channel blocker, beta blocker, digoxin, anticoagulation, radiofrequency catheter ablation ● Complications → stroke, kidney failure, death of the intestines ● RN considerations→ monitor cardiac rhythm, and oxygenation levels VENTRICULAR→ premature ventricular contractions (PVC)- AV node blocks all electrical impulses to ventricles resulting in atrioventricular dissociation, pacemaker in each chamber fires randomly ● Signs & Symptoms → dizziness, palpitations, dyspnea, disorientation, syncope, cyanosis, random P and QRS waves on ECG ● RN considerations→ O2, ECG monitoring, emergent temporary/permanent pacemaker. VENTRICULAR TACHYCARDIA → causes inefficient pumping due to short cardiac filling time, inadequate tissue perfusion, death if untreated. https://www.youtube.com/watch?v=xAfj5AHxC2I ● Treatment → dysrhythmic agents, precordial electric shock Supraventricular tachycardia (SVT) → rapid stimulation of atrial tissue impulse circulates repeatedly through the atrial tissue at a rapid rate; called paroxysmal supraventricular tachycardia (PSVT) if rhythmic intermittent ● Indications → chest pain, weakness, SOB, no intervention if stops on its own, ● Treatment → breaking the reentry pattern, break SVT by massaging the carotid (one side only), having the client gag, holding the breath, immersing face in ice water, increasing parasympathetic stimulation, valsalva maneuver, antidysrhythmic meds, cardioversion Ventricular-Fibrillation / Heart Block→ bundle branch block, first degree block, second degree block ● delay in the conduction of impulses within the atrioventricular system ● in second degree heart block, AV junction conducts only some impulses arising in the atria ● Indication→ syncope, lightheadedness, dizziness, palpitations, or asymptomatic ● Causes→ infection, digitalis toxicity, CAD ● Treatment→ medication, pacemaker if needed, ● RN considerations→ obtain apical and radial pulse for a full minute, monitor pulse deficit, promote stress reduction Complete Heart Block → AV node blocks all electrical impulses to ventricles resulting in atrioventricular dissociation, pacemaker in each chamber fires randomly. https://www.youtube.com/watch?v=2-I2TWE7D-E ● Signs & Symptoms→ dizziness, palpations, dyspnea, disorientation, syncope, cyanosis, random P and QRS waves ● Indications→ dizziness, syncope, chest pain, palpitations, abnormal heart sounds, N/V, dyspnea, abnormal pulse rate 13. Hepatitis → inflammation of the liver that causes liver cell damage a. https://www.youtube.com/watch?v=eocRM7MhF68 b. Chronic hepatitis (> 6 months) can lead to cirrhosis of the liver ● Causes → bacteria, toxins or viruses , 6 viral types → A, B, C, D, E, G ● Hepatitis A & E → fecal to oral (shellfish from contaminated waters is a major source) ● Hep. A stages ○ Pre-icteric: malaise, N/V, anorexia ○ Icteric: jaundice, clay colored stool, tea colored urine ○ Convalescent: SX resolves ● Hepatitis B,C, D & G → parenteral drug abuse, sex, blood & body fluids, ● Signs & Symptoms → jaundice, anorexia, RUQ pain (due to hepatomegaly), clay-colored stools, tea-colored urine (due to bilirubin leakage), appendicitis pruritus, elevated LFT’s (AST & ALT) & prolonged PT ● Treatment → symptomatic → vitamin K, anti-histamines, corticosteroids, anti-emetics & apply calamine lotion ● Nursing Interventions → improve sanitation, vaccination, no ETOH, instruct pt to balance rest and activity, patient cannot donate blood! ● Diet: low in fat, high in carbs and protein 14. Paralytic Ileus → decrease in or absence of intestinal peristalses following abdominal surgery or peritoneal injury or in connection with various diseases. overall cause of intestinal obstruction ● temporary, resolves in 2-3 days ● Signs & Symptoms → abdominal pain and distention, constipation, weakness, diaphoresis, restlessness and anxiety ● Indications → absent bowel sounds, no flatus or stool, abdominal tenderness and distention, N/V, fluid and electrolyte imbalance, ● Treatment → IV fluids, intubation with miller-abbot tube, NG tube, cholinergic agents, analgesics and sedatives ● RN Intervention → monitor intestinal and cardiovascular, side effects of cholinergic agents, monitor bowel sounds, bed rest, low Fowler's, NPO, monitor results of intestinal tube attached to suction for decompression and drainage, IV fluids, I&O, measure abdominal girth ● Complications → Bowel perforation and gang greene 15. Lyme Disease → Inflammatory disorder caused by a spirochete (Borrelia burgdorferi) → spread to humans by deer tick bites a. Symptoms → flat, flu-like sx, slightly raised red lesions or rash (bulls-eye pattern); fever; fatigue, chills; muscle pain; progresses to joint pain, persistent fatigue, headache, and stiff neck b. Diagnostic Tests → blood tests to identify the bacteria → anti-body titers, ELISA, Western Blot i. Lumbar puncture to test CSF for the bacteria ii. RBC → anemia, WBC, ↑ sedimentation rate c. Treatment → antibiotic therapy(3-4 weeks) → Doxycycline, Ceftriaxone, Azithromyocin, Amoxicillin; Analgesics & Anti-pyretics → reduce inflammation & fever, NSAIDs → treat arthritic symptoms d. Patient Teaching → medication may be required up to 1 month → stress importance of maintaining consistent schedule of NSAIDs; provide education on transmission and prevention (wear long sleeves & pants outside in summer & early fall), use insect repellent, 16. Sickle Cell Disease → Most common in African Americans; Negative- Limit water intake; ❖ Hereditary severe chronic anemia condition in which abnormal hemoglobin distorts erythrocytes, increases their fragility, and causes them to become sickled in shape and rigid; periods of exacerbation called crises occur; ➢ S/SX: are systemic and include chronic anemia (hemoglobin, 6 to 9 g/dL), possible growth retardation and delayed sexual maturity, pain (often especially focused on joints), swelling, jaundice, priapism (prolonged erection), impaired renal function, cardiac murmurs, altered pulmonary function, increased susceptibility to infection ➢ Nursing Intv: include rest, oxygen, IV fluids and electrolytes, sedation, analgesia, possible transfusion; nursing interventions include promote rest, administer analgesia as prescribed and teach use of patient-controlled analgesia (PCA) pump as indicated, administer oxygen, maintain I and O and ensure adequate fluid intake, monitor for infection, encourage activity as tolerated when not in crisis. Follow normal immunizations + pneumococcal regardless of age ➢ TX: Although there is no cure for sickle cell anemia, treatment is preventative and palliative. Primary treatment modalities include: Bone marrow transplant (BMT), hydroxyurea, arginine, long-term red blood cell (RBC) transfusion. During painful vaso-occlusive crisis: Sedation, analgesia, blood transfusions, oxygen therapy, oral and intravenous fluids (large amounts of both), analgesics (to relieve pain) ➢ Sickle cell crisis/vaso-occlusive crises → sickle cell gets stuck . DO NOT USE COLD COMPRESS → vasoconstricts. Use warm compresses! 17. Appendicitis → inflammation of the appendix due to infection or obstruction pg 251 ● Signs & Symptoms → abdominal pain (R lower Q) → first before N/V, anorexia, N/V, constipation, boardlike abdominal rigidity, retractive respirations, increasingly severe abdominal spasms and rebound spasms, increased temp, ● Treatment → appendectomy, if peritonitis develops treatment involves GI intubation, parenteral replacement of fluids and electrolytes and administer antibiotics ● RN Interventions → no heating pads, enemas, laxatives preop, maintain NPO until lab reports received, no analgesics until cause of pain is determined, ice bag to abdomen to alleviate pain, Fowler's position (not heat), observe for s/s peritonitis, recognize that loss of pain indicates perforation and is an emergency ● DX → CT or ultrasound ● Complications → obstruction and abscess 18. Glomerular Nephritis→ damage to glomeruli caused by an immunologic reaction that results in proliferative and inflammatory changes within the glomerular structure. Cause by beta hemolytic streptococcal infection. Occurs 10 days after skin or throat infection. ● Indications → fever, chills, hematuria red cell casts, proteinuria, weakness, pallor, dyspnea, weight gain, lung rales, fluid overload, generalized and/or facial and periorbital edema, htn, oliguria w/ fixed specific gravity ● Complications → htn encephalopathy, acute cardiac decompensation, AKI, ● RN care → administer abx, corticosteroids, antihypertensive, restrict Na+, restrict H2O if oliguria restrict high potassium foods during oliguria, assess VS, daily weight, I&O, assess cerebral complications, record characteristics of urine, bed rest 19. Medications: Adrenocortical Hormones: Glucocorticoids a. Non Rapid acting→ synthetic steroid; produced by adrenal cortex i. Action → suppress severe inflammation or immune response, decrease release of inflammatory mediators, decrease infiltration of inflammatory cells, decrease edema and hyperactivity of airways and mucous production. Converts carbs, fats, and protein → glucose. ii. Adverse Effects → hyperglycemia, peptic ulcers, muscle wasting, fluid retention, hypokalemia, moon face, depression, euphoria, osteoporosis, thromboembolism, weight gain, increased risk of infection, and fluid/electrolyte disturbances, buffalo hump, increased ICP, anorexia, nausea, acne, delayed wound healing, vomiting, psychoses, restlessness, joint avascular necrosis, hypokalemic alkalosis, increased intraocular pressure, cataracts, hypertension, ecchymosis, petechiae, thrombophlebitis, muscle pain, personality changes, hirsutism, fragility, agitation, diarrhea, Churg-Strauss Syndrome, dry mouth, oral/esophageal candidiasis, nasal congestion, dizziness, insomnia, hoarseness, bronchospasm,, cough, dyspepsia, allergic reaction, growth suppression, rash, urticaria, sneezing, epistaxis, eye tearing, pharyngitis, sinusitis, rhinorrhea, dysphonia, skin atrophy and burning and dryness and irritation, allergic contact dermatitis, hypopigmentation, miliaria, striae, folliculitis, irritation of the airways, hypertrichosis, maceration, hyperglycemia, osteoporosis, psychosis, weakness, purple skin striations, psychological depression, truncal obesity, masculinization in females, hypocalcemia. DAMN! iii. Nursing Considerations → Monitor bp and lab values, intake and output, and daily weights. Admin with food or milk. Do not crush. Nightmares often first indication of steroid psychosis, MONITOR GLUCOSE iv. Client Education → no grapefruit juice. Taper before discontinuation. Not for acute bronchospasms. v. Hydrocortisone (Cortef, Solu-Cortef), Methylprednisolone (Medrol), Prednisolone (Delta-Cortef, Flo-Pred, Prelone), Prednisone (Deltasone, Meticorten) vi. Question: (Focused Assessment A) A client calls the nurse 10 days after beginning to use beclomethasone nasal spray due to seasonal allergies. The client reports that even though the medication is being used correctly, the client has experienced only slight relief. Which action by the nurse is MOST important? 1. Remind the client that the peak effect can take up to three weeks of regular use. 20. Diabetes Mellitus (3 questions) → a. Signs & Symptoms → THE POLY’s (polyuria,polydipsia, polyphagia), weakness, dizziness, fatigue i. In Children → those above + enuresis (bed-wetting), unusual fatigue & irritability b. Type 1 → beta cells in pancreas are destroyed and produce no insulin i. Treatment → insulin injections, continuous infusion via pump & diet control c. Type 2 → beta cells in pancreas secrete insulin, but the body is resistant to its effects i. DX → Hemoglobin A1C (indication of glucose control over last 90 days) ii. Treatment → insulin, oral hypoglycemic injections & diet control d. Diet Management → monitor total calories, carbs & timing of food e. Diet Intake → meals with complex carbs, ↓ fat, ↑ fiber, some protein i. Time meals with peak effect of insulin ii. Provide extra snacks for unplanned physical activity iii. Substitute soft foods 6-8 times per day if you cannot stick with the usual meal plan iv. If vomiting, diarrhea or fever persist take in some liquids like ½ cup coke, juice, broth or 1 cup of gatorade to maintain caloric intake every ½ hour or hour v. Report nausea, vomiting & diarrhea to HCp → extreme fluid loss = dangerous vi. Unable to retain fluids = hospitalization to prevent DKA f. Patient Teachings → lose weight if obese, oral hypoglycemic agents, maintain healthy weight, s/s of hypoglycemia & hyperglycemia self-monitoring of glucose, skin/foot care, importance of exercise g. “Sick Day” Rules → guidelines for managing diabetes when ill → aimed at preventing DKA i. Take insulin or hypoglycemic agents as usual ii. Test blood glucose & urine ketones every 3-4 hrs → report elevated levels to MD iii. If you take insulin, you may need supplemental doses every 3-4 hours h. Dawn Phenomena → early morning glucose levels are elevated caused by nocturnal release of growth hormone i. Somogyi Effect → fall in blood glucose during the night with ↑ morning glucose levels → caused by 21. Kidney Disease: Chronic → know a lot of nursing judgment and concepts a. Irreversible, progressive reduction of functional kidney tissue resulting in inability of kidneys to excrete wastes, concentrate urine, and conserve electrolytes. i. Indications S/S: anemia, acidosis, azotemia, fluid retention, hypertension, hypocalcemia, anorexia, N/V, constipation, impaired insulin action. ii. Interventions: to slow progression, control blood pressure and make fluid and dietary adjustments. Dialysis or transplantation may be done when these measures are no longer effective. iii. Nursing interventions: Monitor fluid status, encourage nutrition by decreasing nausea, vomiting and stomatitis, and other GI symptoms, teach appropriate diet (low protein, low potassium, low sodium), manage constipation, teach to balance rest and activity, encourage good skin care with emphasis on moisturizing, teach coping skills to client and fam, teach dialysis-related procedures, explain transplantation process and subsequent potential issues and care. Important to increase non-protein calories, such as fruit ice. iv. Diagnostic tests: 1. Urine specimen (reveals low specific gravity, hematuria, proteinuria) 2. Blood studies (reveal elevated BUN, creatinine, potassium) 3. Creatinine clearance test (measures glomerular filtration rate) 4. Ultrasonography of kidneys, renal scan, CT scan 22. CPR → a. Overview: process of externally supporting circulation and respiration; failure to institute ventilation within 4-6 minutes results in brain damage; sequence is CAB (compression-airway-breathing). If the rescuer witnesses the collapse start by activating EMS. If the rescuer doesn't witness the collapse start by establishing unresponsiveness, breathing, and pulse. If victim drowned or is a child, rescuer starts with 2 min of CPR before activating EMS. i. Step 1: establish unresponsiveness, breathing, and pulse using the sternocleido mastoid in the neck. ii. Step 2: Activate EMS. iii. Step 3: Start Compressions, 100/min, depth (2in for adult) or (1/3 a-p diameter or 2in child) or (1/3 a-p or 1.5in in infant). iv. Step 4: establish airway using head/chin tilt; if trauma suspected then use jaw thrust. v. Step 5: breathing. 8-10 breaths/min ensure chest rise. b. Compression-ventilation rate: Adult: 30:2 1 or 2 rescuers. Infant/Child 30:2 for 2 rescuers. Neonates: 3:1 for 1 rescuer, 30:2 for 2 rescuers. 3:1 ratio facilitates provision of adequate minute ventilation, which is considered critical for the vast majority of newborns who have an asphyxial arrest. 15:2 ratio recognizes that newborns with a cardiac etiology of arrest may benefit from a higher compression to ventilation ratio. c. Infant CPR: CAB: i. Circulation: check the brachial artery for 10 sec for a pulse; if it is not found, compress the lower sternum with two to three fingers 1/3 of the ap diameter or 1.5 in; allow chest to recoil between compressions; minimize interruption of compression; if necessary, interruption should be less than 10 seconds; use the hand farthest from the infant's head; 1. ratio for 2 rescuers: 15 compressions to 2 breaths at rate of 100 compressions per min; 2. ratio for 1 rescuer: 30 compressions to 2 breaths at a rate of 100 compressions per minute. ii. Airway: Open airway with head tilt/chin lift maneuver. iii. Breathing: assess for breathing; if the infant is not breathing, place mouth over the infant's mouth and nose and ventilate the infant; observe chest rise. d. The Heimlich Maneuver: only be performed for a conscious, choking client, who is showing severe obstruction, demonstrated by the inability to speak. If the client is in bed, position a backboard or other rigid surface beneath client. Instead of abdominal thrusts, perform chest thrusts for a client who is pregnant or obese 23. Fracture (2 questions) → break in continuity of the bone a. Open vs. closed fracture i. Open/compound fracture: fractured bone that breaks through the skin ii. Closed/simple fracture: does not penetrate through the skin (skin is intact) b. Complications of fracture: fat emboli, hemorrhage, sepsis, compartment syndrome c. Emergency Care → immobilize joint above & below fracture, cover any wound with sterile dressings, check temperature, color, sensation & cap refill, elevate above heart level to reduce swelling i. Extreme caution with spinal fractures → C-spine & log-roll patient d. Hip Fracture (common in the elderly) → one leg may be shortened, externally rotated or adducted, be very painful, possess a hematoma, muscle spasms i. Treatment → immobilize using Buck’s traction, open or closed reduction with internal fixation, hemiarthroplasty (femoral head prosthesis) ii. Bucks traction: https://www.youtube.com/watch?v=2ZEWz_Ps7vo iii. Nursing Care → apply hip protector pads in patients at risk for falls, monitor for hypovolemic shock post surgery, use compression stockings/ICD’s or anti-coagulants to prevent DVT’s, encourage patient to keep moving by using trapeze, administer pain meds, monitor hydration/nutrition/urine output, access the 6 P’s (pain, paresthesia (burning/pricking feeling), pallor, paralysis, pulse, poikilothermia (unable to regulate temp.) e. Skull Fracture → results from direct impact, signs & symptoms may not be evident immediately i. Signs & Symptoms → ecchymosis behind ears, over mastoid process (Battle’s sign) or around eyes (raccoon eyes), CSF leakage from nose or ears, cranial nerve injury manifestations 1. Complications → brain abscess, meningitis, increased ICP 24. Parkinson’s Disease (2 questions) → a. https://www.youtube.com/watch?v=VIEUEV9wlyI ❖ Parkinson’s disease is a chronic disease of the nervous system characterized by fine, slowly spreading tremor, muscular rigidity and altered gait; nursing care includes encouraging finger exercises (e.g., piano playing, range of motion (ROM) as appropriate, teaching client ambulation modification, referring to physical therapy, teaching goose-stepping walk, walking with wider base, concentrating on swinging arms while walking, turning around slowly using small steps; promoting family understanding of the disease, intellect not impaired, sight and hearing are intact, teaching that disease is progressive but slow, does not lead paralysis, referring for speech therapy, potential stereotactic surgery; administering medication. ➢ Nursing Intv: ■ Parkinson’s disease is slowly progressive, degenerative disorder that can appear at any age and affect both sexes but mostly commonly appears in men over age 60. ➢ S/SX: ■ Gradual onset, tremor (beginning with a pill-roll tremor), Muscle rigidity (uniform or jerky), Bradykinesia (abnormally slow movements), Gait disturbances (difficulty walking), High-pitched monotone voice, Mask-like facies (poor blink reflex, wide open eyes, Loss of postural control (body bends forwards when walking) , Dysphonia (slow, monotonous slurred speech), Micrographia (shrinking, slow handwriting), Depression, dementia, sleep disturbances, and hallucinations ➢ TX: ■ Treatment is mainly palliative and not curative. The object is to maintain as high a level of function as possible for as long as possible. Unfortunately, response to medications is often transient and symptoms inevitably become progressively medication resistant. ● Medical Therapy ◆ Levodopa is combined with carbidopa (Sinemet), to reduce side effects of levodopa (e.g., confusion, hallucinations, depression, sleep alterations) ◆ Dopamine agonists (e.g., pergolide), to postpone use of levodopa and carbidopa ◆ Anticholinergics (e.g., trihexyphenidyl) to control tremor and rigidity ◆ Monoamine oxidase inhibitors (e.g., selegiline ([symmetrel]), to reduce rigidity, tremor, and bradykinesia → no tyramine foods 25. Biopsy→ removal of tissue for evaluation, usually microscopically. Allows for evaluation of overall blood composition, including blood elements, precursor cells, and abnormal malignant cells ● Bone marrow → aspiration is removal and examination of number, size, and shape of RBCs, WBCs, and platelet precursors in the bone marrow to assess and identify blood dyscrasias, informed consent required, specimen obtained from iliac crest and sternum. local anesthetic used, best position for patient is prone. ○ RN post test → cleanse site with alcohol to remove povidone iodine, apply pressure with sterile gauze pad for several minutes to control bleeding, apply sterile pressure dressing ● Breast → removal of suspicious tissue related to possible breast cancer ○ Post Biopsy period → ligation of an artery or vein is the great risk, RN should observe for frank bleeding and pallor, cold, clammy skin, increased pulse, decreased BP ● Kidney → tissue obtained through needle aspiration. Instruct client to hold breath during needle insertion ○ Post Test RN care → pressure applied to site for 20 min, pressure dressing applied, position supine for 24 hrs, observe for hematuria and site for bleeding ● Liver → needle biopsy under local anesthetic ○ Prep → administer vit k, NPO 6 hrs before exam, teach client to hold breath 5-10 seconds while tissue is removed ○ RN Care Post biopsy → VS every 15 min x4, every 30 min x2, then hourly x4, finally every 4 hrs for 24 hrs, position in the right lateral position for 1-2 hrs, bed rest several hrs, check clotting time, platelets, hematocrit, report severe pain immediately (may indicate perforation of bile ducts and peritonitis) ● Skin → removal of tissue for examination and testing. Usually done to determine underlying cause of abnormality of skin 26. Cardiac Tests (2 questions) ● Capillary Refill Time → noninvasive evaluation of adequate arterial blood flow, performed by gently squeezing finger/toenails to induce blanching, then releasing pressure and observing length of time before normal color returns, normal values are < 3 seconds, values > 3 indicate poor perfusion ● Catherization → radioplaque catheter inserted through peripheral blood vessels into chambers of heart, usually used with angiography. Purpose is diagnosing or can be used as intervention in some congenital heart defects ○ Preprocedural RN Considerations → measure height to help determine correct catheter selection, assess allergies, infection, mark pedal pulses, ○ Postprocedural RN Considerations → assess pulses, temp, color of affected extremities, assess HR every 15 min for a full minute, signs of hemorrhage, ensure adequate hydration ● Carotid Anteriogram → visualization of the carotid arteries by using the radiopaque contrast medium dye injected via the femoral and brachial artery ● Pulmonary Wedge Pressure (PAWP) → pressure measured in the pulmonary artery via catheter (Swan-Ganz), with the balloon inflated the pressure is tested in the pulmonary capillary bed and left atrium, if the mitral valve is competent the pressure is the left ventricular end-diastolic pressure ○ normal pulmonary artery pressure 20-30mm Hg and 8-12 mm Hg diastolic ○ normal pulmonary artery wedge pressure 4-12 mm Hg ○ elevated pressure indicates fluid overload ○ RN consideration → prepare and set up transducer set, monitor pressure as ordered, balance and calibrate per institution policy, know procedure to follow if balloon does not deflate ● Pulse Oximetry → estimates the degree of oxygen saturation in arterial blood, uses wavelengths of light ○ RN Interventions → select appropriate site for sensor every 2 hrs, adhesive sensors every 4 hrs, protect sensor from bright light with a towel or sheet ● Stress Test → assesses cardiovascular response to increased workload, stress induction by medication or physical exercise using treadmill or bicycle to target HR or development of a/e ○ RN Considerations → establish baseline ECG to compare intra-and-post-procedure, ensure emergency equipment is available ● Central Venous Pressure (CVP) → measurement of effective blood volume and ability of right side of heart to manage a fluid load. Used as guide for fluid replacement, involves a central line, transducer, and IV fluids. ○ Normal is 2-8 ○ over 8 indicates hypervolemia or poor cardiac contractility, ○ under 2 indicates hypovolemia ○ Complications → pneumothorax, air embolism, infection at insertion site ○ RN responsibility → accurate measurement, dry sterile dressing at insertion site, check and secure all connections, instruct valsalva maneuver for cath insertion, withdrawal and changing ● Echocardiogram → diagnostic test using ultra sound to visualize cardiac structures and abnormalities 27. Colonoscopy → direct visualization of the colon with a fiberoptic colonoscope a. Purpose: Aids the diagnosis of inflammatory and ulcerative bowel disease, pinpoints lower GI bleeding, detects lower GI abnormalities including, polyps, hemorrhoids, and abscesses. b. Pre-test: clear liquid diet 24 to72 hours before exam (nothing with red dye), cathartic in evening for 1-2 days before exam, enema the morning of the exam, take enema morning of exam c. Post-test: allowing client to rest, observing for passage of blood, abdominal pain, signs of perforated bowel (fever, chills, N/V, severe abdominal pain), hemorrhage, and respiratory distress, monitor for resp. distress 28. Thyroidectomy → complete or partial excision of the thyroid gland - Check laryngeal nerve- tingeling in fingers and toes after procedure ( Calcium depletion) a. Purpose → corrects hyperthyroidism, removes breathing obstruction caused by goiter, treats thyroid cancer, treats hyperparathyroidism b. After surgery → monitor respiratory status, ensure that incision drains properly, monitor pulse & temperature for indications of thyrotoxicosis or thyroid storm ( fever, tachycardia > 130, delirium, coma) i. Monitor for tetany → could indicate that parathyroid glands were damaged during surgery which would cause hypocalcemia (Chovsteks & Trousseau’s sign) ii. Keep patient in Semi-Fowlers position, apply ice to reduce the swelling iii. Make sure to have suction, O2, trach set, IV calcium & suture removal kit at bedside iv. Ask patient to speak every 2 hours to check tone & hoarseness v. Emphasize importance of adhering to thyroid replacement therapy after discharge vi. Keep incisions clean & dry 29. Ileal Conduit → Ureter is implanted into a portion of the ileum and brought through abdominal wall, provides an alternate route of urine excretion when a disorder, such as bladder cancer, impedes normal flow through the bladder. ● Ureter is implanted into a portion of the ileum and brought through abdominal wall ● RN responsibility→ skin barrier, transparent disposable urine bag, applied around the conduit and connected to drainage, appliance is changed as needed to prevent leakage of urine (usually every 3-5 days), ○ Post Op→ appliance should be no more than 1.6mm larger than stoma, check and record urine output, perform ostomy maintenance 30. Kidney Injury: Acute → Abrupt acute disruption in kidney function that impairs ability of body to maintain balance of fluid, electrolytes, and acid-base status. a. Phases of ARF: i. Initiation: Begins with initial insult and ends when oliguria develop ii. Oliguria: Output less than 400 mL/day; increase in BUN, creatinine, uric acid, potassium, magnesium; uremic symptoms occur 1. Indications: N/V, irritability, drowsiness, confusion, coma, restlessness, twitching, seizures, hypertension, pulmonary edema, increased serum potassium, BUN, creatinine, calcium, sodium, and pH. iii. Diuresis: gradual increased urinary output; may still have uremic symptoms. 1. Indications: increased urinary output, decreased serum sodium, potassium, BUN, creatinine, correction of metabolic acidosis, increased mental and physical activity. iv. Recovery period : 1. Indications: returned to normal functioning while healing takes place. b. Interventions: treat underlying cause, treat fluid and electrolyte imbalance, prevent infection, administer high caloric and low protein diet, possible dialysis c. Nursing Interventions: maintain strict intake and output and compliance with fluid restriction/intake as ordered, daily weights, monitor vital signs closely, assist client with managing anorexia and eating appropriate foods, provide good skin care, monitor for infection, encourage rest, support dialysis if indicated. d. Nephrotic syndrome: Minimal-change nephrotic syndrome (MCNS) most common in type of nephrotic syndrome in children; i. Indications: periorbital or ankle edema, larger than expected weight gain, decreased urinary output, pallor, fatigue, hyperalbuminuria, hypoalbuminemia, ascites, hypovolemia. ii. Treatment: restrict salt, corticosteroid therapy, immunosuppressive therapy iii. Nursing considerations: monitor I/O, daily weights, test urine for albumin, measure abdominal girth, protect from upper respiratory infection, instruct parents about S/S to observe for at home, how to administer steroid therapy, and adverse effects. iv. Diagnostic tests: Urine specimen (reveals low specific gravity, hematuria, proteinuria), Blood studies (reveals elevated BUN, creatinine, potassium), Creatinine Clearance test (measures glomerular filtration rate), and Ultrasonography of kidneys, renal scan and CT scan. 31. Fluids & Electrolytes (3 questions) a. A state of equilibrium in which the amount of fluids and ions remain within normal parameters in the body. This condition of balance is a factor involved in the maintenance of homeostasis. A small variation in the amount of fluid or concentration of ions in the body will create a state of fluid and electrolyte imbalance. Depending on the severity of the fluid loss or gain, or the specific ion which is out of balance, a life threatening condition may exist. b. Body fluid is mostly water, which contains electrolytes. Two major categories of body fluid distribution are intracellular (ICF) and extracellular (ECF), the ECF being further divided into intravascular and interstitial. Important to avoid dehydration and overhydration. Fluid, electrolyte, and acid/base balance are essential for normal body function. Measuring intake and output helps assessment of fluid and electrolyte status. c. Intake includes oral and parenteral fluids. Output includes urine, liquid stool, emesis, drainage. Intake and output should be roughly equal. 1500-2000 mL/day is usually adequate fluid intake. d. Fluid restriction is used when fluids are retained and there is a fluid volume excess. Communicate with the dietary department so that there are not too many fluids on each meal tray. Calculate IV fluids in the total amount. Fluid restriction includes oral and parenteral fluids. e. Deficit is insufficient fluid in the body. Indications of fluid volume deficit include rapid weak pulse, rapid respirations, hypotension, weight loss, emaciation, dry mucous membranes, increased hematocrit, increased urine specific gravity. i. Nursing care → forcing fluids, providing isotonic IV fluids, intake and output, hourly output, daily weights (1L fluid = 1 kg), monitoring vital signs, assessing skin turgor, assessing urine specific gravity. ii. Infants have greater water loss due to the larger amount of extracellular fluid, about 60% of fluid loss comes from the ECF during infancy. iii. Indications of dehydration → tachycardia, dry skin, and mucous membranes, sunken fontanel, loss of skin elasticity. iv. Nursing care → accurate intake and output, offer oral rehydration therapy, administer IV therapy. In the child vomiting and or diarrhea most common causes of dehydration. May be forceful with much vomitus or more gentle with small amount of gastric contents. Fever may also be a cause. v. Treatment of underlying cause most appropriate. Nursing care includes observation and documentation of the behavior and amounts along with associated symptoms, promoting hydration by offering glucose-electrolyte solutions if child is alert, antiemetics, and treatment of underlying cause. vi. Labs → increase concentration in blood f. Overload is created by an isotonic gain, an increase in the interstitial compartment, the intravascular compartment (such as in shock), heart failure, chronic kidney disease, cirrhosis of the liver, excessive ingestion of sodium, or an IV fluid that has been infused too rapidly. i. Signs & Symptoms → slightly increased pulse that is bounding, increased respiratory rate with SOB, crackles on auscultation. JVD, decreased hematocrit and BUN. ii. Nursing Considerations → monitor for signs and symptoms, notify the HCP if necessary, elevate the head of the bed, provide reassurance 32. Multiple Sclerosis (autoimmune disorder) a. Progressive disorder of nerve impulse transmission characterized by demyelination of white matter throughout brain and spinal cord. Periods of exacerbation and remission. Intellect intact. Leads to paraplegia or complete paralysis. b. Indications → patient will present with increasing fatigue and SOB, paresthesias or abnormal sensations in extremities, vision changes, incoordination, bowel and bladder dysfunction, spasticity, intention tremors, chewing and swallowing difficulties, impaired speech, emotional instability, sexual dysfunction. c. Nursing Interventions→ teach exercises related to relaxation, coordination, progressive resistance, range of motion, teach to balance activity and rest, provide warm baths and packs, teach wide-based walk, use of cane or walker, implement bladder and bowel training, teach about self-help devices, instruct in use of eye patch for diplopia, provide emotional support, refer to support groups and organizations d. DX → CT, MRI, CSF increase in gamma globulines 33. Traction a. What is it? → Pull on a body part b. Purpose is to immobilize fracture, alleviate pain and muscle spasm, prevent or correct deformities, promote healing. c. Types: i. Skin (Buck’s extension, Rusell’s, pelvic, or cervical traction) ii. Skeletal (pull applied to skeleton via pins inserted into bone, pins are attached to weights via rope and pulley system [halo, Crutchfield or Barton or Gardner-Wells tongs, 90 degrees - 90 degrees]). iii. Combination of skin and skeletal (balanced suspension with use of Thomas splint and Pearson attachment). d. Nursing Considerations → maintain straight alignment of ropes and pulleys, assure weights hang freely, frequently inspect skin for breakdown, maintain position for countertraction, encourage movement of unaffected areas (do not turn from waist with Russell), (Bucks, if no fracture, may turn to either side, with fracture, turn to unaffected side), (keep heel off bed for skin traction), (Bucks, elevate foot of bed for countertraction, use trapeze for moving; don’t elevate knee gatch), investigate every discomfort immediately and thoroughly, maintain continuous technique. e. Pin Care → clean pins according to institutional policies and procedures, wet swab with solution and wipe once around pin, doing each pin with a new swab. f. Halo Vest → lightweight vest with halo that stabilizes cervical spine. i. Nursing Care → care of insertional sites by cleansing area around pins using sterile technique. Observe pins for loosening, if pins become loose, stabilize head in neutral position and notify health care provider. Inspect skin daily for areas of breakdown under vest 34. Headache → a. Tension: most common headache. i. Indications: mild to moderate pressure or tightness, bilateral, discomfort worse with activity. ii. Nursing Considerations: careful assessment of onset of s/s and triggers, patterns, presence of lethargy, weakness, nausea, vomiting, instruct about analgesics, relaxation techniques, massage, moist hot packs to neck. b. Migraine: recurrent vascular headache, lasts 4-72 hrs. i. Indications: severe pain, throbbing in nature, unilateral, associated with nausea, vomiting, diarrhea. Sometimes prodromal aura present (lights, lines, tastes, odors, tingling, vertigo, tinnitus), blurred vision, photophobia, focal neurological symptoms (vertigo, dysarthria, ataxia, diplopia), scalp tenderness, mood alterations. ii. Interventions: prevention with various medications and modifying trigger factors, treatment of attacks with ergotamine, NSAIDs, antiemetics, sumatriptan, and a quiet dark room and lying down can be helpful. c. Indications for Immediate Follow Up in Children: increased frequency and severity of headache, headaches that awaken a child at night, early morning headaches, headaches that worsen when child gets out of bed in morning, any changes in behavior or personality 35. Meniere’s Disease → ❖ Meniere’s disease is caused by dilation of the endolymphatic system. Meniere’s disease is a disease of the inner ear characterized by too much endolymph fluid in the membranous labyrinth. It can lead to severe hearing loss and debilitating episodes of vertigo. The disease occurs with equal frequency in men and women and may affect either ear or both ears. ➢ S/SX: include tinnitus (ringing in ears), unilateral sensorineural hearing loss, vertigo,Intense vertigo (dizziness), with associated pallor, nausea, vomiting, and sweating, lasting minutes to hours, Feelings of imbalance, Episodic, progressive hearing loss, Pressure in the ear ➢ TX: includes salt and fluid restriction to decrease amount of endolymphatic fluid, antihistamines, antiemetics, corticosteroids, low sodium diet and surgery. ➢ Dx: caloric stimulation test: cold water → eyeball will move and back. Hot water → moves towards and away = positive for meniere’s disease ■ Surgical Tx: ● Endolymphatic sac surgery in which a shunt is installed to drain excess endolymph and to relieve pressure ● Ototoxic medicine (e.g., gentamicin) infusion into the inner ear, to diminish vestibular function and reduce vertigo ● Vestibular nerve section, to relieve vertigo by severing the nerve communication pathway to the brain 36. Shock a. What is it? → decrease in tissue perfusion. Cell metabolism is decreased → cell death and cell dysfunction b. 4 types of shock i. Hypovolemic → loss of fluid volume (most common) 1. Absolute: due to hemorrhage, D/V 2. Relative: 3rd spacing that happens because of sepsis or bowel obstruction ii. Distributive: moves into the ICF due to anaphylaxis, neurogenic, septic shock iii. Cardiogenic → lack of contractility of the heart = decreased cardiac output 1. Due to trauma, MI, heart failure iv. Obstructive → obstruction of filling c. In any emergency situation shock should be anticipated before it develops. d. Stages of shock i. compensatory : body starts to compensate → increase heart rate, holds on to fluid to go to vital organs, decreased urine output ii. Progressive: cardiac output decreases, edema, acidosis iii. Irreversible: no oxygen → body goes into anaerobic state → body starts to die e. Indications → increased pulse, decreased blood pressure, pallor, diaphoresis, moist cold skin, oliguria, hyperpnea, metabolic acidosis, and altered sensorium. f. Treatment → correct physiologic abnormalities and restore and maintain tissue perfusion → isotonic solution and coloids g. RN responsibilities → ensure patent airway, maintaining breathing and circulation, restoring circulating blood volume, inserting indwelling catheter, I/O every 15-30 min, determining the cause of shock, lab tests, elevating feet slightly, administering medications as prescribed, maintaining body temperature, avoiding too much heat. With signs of shock, place patient in modified trendelenburg . 37. CVA (2 questions) → ❖ Sudden disruption in blood supply to brain resulting in sudden loss of brain function that may be temporary or permanent; caused by thrombotic embolism, ischemia, or hemorrhage; indications include loss of movement, thought, memory, speech, or sensation; nursing responsibilities include encouraging the client to attain maximum independence, stimulating multiple senses, repeating directions and breaking down tasks into components, facing the client and speaking clearly slowly, giving the client time to respond, maintaining skin integrity and providing exercises (ROM and facial), self-care activities, and teaching Stating, antihypertensives, and platelet-inhibiting meds decrease incidence of CVA. Recombinant t-PA dissolve obstructive blood clots. t-PA therapy nursing interventions: withhold anticoagulants for next 24hrs, weigh patient to determine dose, and vital signs ( 15min first 2hrs, 30min for next 6hrs, every following hour until 24hrs after treatment). ➢ Transient Ischemic attacks (TIA): transient interruption of blood flow to the brain, it is a warning sign for stroke, repeated TIS can cause brain damage, cause includes clot in the brain, blood vessel injury, blood vessel stenosis. Risk factors: atrial fibrillation, high cholesterol,hypertension, diabetes mellitus, family history, age over 65. ➢ S/SX: they last minutes to hours, include unilateral vision loss, hemiparesis,numbness, loss of sensation, aphasia, dizziness, vertigo, tinnitus, vision changes, dysarthria, dysphagia, coordination problems. ■ Diagnostic tests: CT, MRI, 12 lead electrocardiogram, carotid ultrasound. ➢ TX: Modification of risk factors 38. Meningitis → Infection or inflammation of membranes covering brain and spinal cord; bacterial, viral, or fungal in origin. i. Indications: h/a, fever, photophobia, signs of meningeal irritation (nuchal rigidity, Kernig’s sign, Brudzinski’s sign, opisthotonus position), changes in level of consciousness, seizures; in infants indications include refuse feedings, vomiting, diarrhea, bulging fontanelles, vacant stare, high pitched cry. ii. Diagnostic Tests: Lumbar Puncture to test CSF for increase pressure, increase protein, decrease glucose, + Kernig’s, + Brudzinski's iii. Nursing Interventions: administer antibiotics or antifungals as ordered, observe for increased intracranial pressure, maintain seizure precautions, maintain adequate fluids and electrolyte imbalances. iv. Treatment: 1. Immediate antibiotics to stop the multiplication of bacteria is necessary. IV for 2 wks and orally thereafter. a. Penicillins, Cephalosporins, Vancomycin with rifampin (for resistant strains) b. Dexamethasone as adjunct therapy for bacterial meningitis. c. Supportive care for viral meningitis. d. Digoxin to control arrhythmias. e. Mannitol to decrease cerebral edema. f. Phenytoin (Dilantin) for seizures or sedatives to reduce restlessness. g. Acetaminophen for h/a and fever h. Vaccination as prophylaxis for high risk population i. For contacts of meningitis patients: antimicrobials i. Rifampin ii. Cipro iii. Rocephin 39. Epilepsy → Chronic disorder characterized by recurrent seizure disorder, symptoms of brain or central nervous system (CNS) irritation. Classification generalized seizure: a. tonic-clonic seizure (begins with tonic phase and immediate loss of consciousness, followed by clonic phase, rhythmic jerking of all extremities) i. Signs and Symptoms: 1. Beginning with loud cry 2. Change in LOC 3. Body stiffening- alternating between stiffening and relaxation 4. Tongue biting, incontinence, labored breathing, apnea, cyanosis 5. On wakening: possible confusion, difficulty talking 6. Drowsiness, fatigue, H/A, muscle soreness, weakness b. absence seizures- brief periods of loss of consciousness like day-dreaming, more common in children i. Signs and Symptoms: 1. Blinking or rolling eyes, blank stare 2. Slight mouth movements c. myoclonic seizure- brief jerking of extremities i. Signs and Symptoms: 1. Brief involuntary muscular jerks of the body or extremities d. atonic seizures- sudden loss of muscle tone, client falls; complex partial seizure-client backs out for a few seconds, automatism may occur e. simple partial seizures- remains conscious, often reports aura i. Signs and Symptoms:: 1. sensory(flashing lights, smells, auditory hallucinations) 2. Autonomic (sweating, flushing, pupil dilation) 3. Psychic (dream states, anger, fear) f. idiopathic- occur for no known reason Nursing intv: g. Include observing and documenting type and progress of seizure activity and postictal behavior, O2 and suction at bedside; post-seizure, position on back with head turned to side or position on side to prevent aspiration and promote drainage of secretions; treatment includes medication. TX: h. Medications: valium, phenytoin, carbamazepine, and ethosuximide i. Surgery if meds don’t work j. Emergency tx for status epilepticus consists of diazepam, lorazepam, fosphenytoin, phenobarbital, 50%dextrose I.V., thiamine IV * check blood levels regularly 40. Anemia a. Decrease in red cells or hemoglobin content or altered hemoglobin function. b. Causes → decreased red blood cell production, blood loss, increased destruction of red cells or inadequate intake or excessive loss of iron. c. Signs & Symptoms → tissue hypoxia causing fatigue, pallor of the skin and mucous membranes, increased respiratory rate and depth, dizziness, difficulty concentrating, cold intolerance, compensatory mechanisms cause increased heart rate with possible MI, fluid retention, and increased erythropoietin production; and cardiac failure. d. Complications → high output cardiac failure and heart murmurs. e. Risk factors → menstruating women and children. f. RN care → ID’ing risk factors, administering blood or iron replacement, teaching about diet (women require 15-18 mg daily, men require 10 mg daily; average diet supplies 12-15 mg/day of iron. Beef, lamb, and liver are good sources of iron, absorbed better 41. Thrombophlebitis (2 questions) a. Definition → Inflammation of vein with a clot. A complication of IV therapy. b. Assessment → Pain at or above distal to site, swelling, redness/warmth around site or on path of vein, fever, Leukocytosis (above normal WBC count) c. Nursing Management → Discontinue IV, Apply warm compress, elevate the extremity, restart IV. Heparin may be ordered, check PTT and monitor during administration of Heparin. No sitting or standing for prolonged times —> DVT 42. Tracheostomy (p. 177) a. Surgical incision into trachea, tube inserted through trachea. b. Nursing Considerations: Cuff used to prevent aspiration/facilitate mechanical ventilation, maintain cuff pressure at 14-20 mm Hg, encourage fluids to remove secretions, sterile suctioning if necessary, frequent oral hygiene. c. Indications for suctioning: Noisy respirations, restlessness, increased pulse, increased respirations, presence of mucus. d. Trach Care: Every 8 hours and PRN i. Procedure: Explain it to PT, suction, remove old dressing, open sterile trach care kit, put on sterile gloves, remove inner cannula, clean with Hydrogen peroxide if using a permanent inner cannula, rinse with sterile water/dry, reinsert outer cannula, clean stoma site with Hydrogen peroxide and sterile water/dry, replace ties (keep old ties in place until new ones are secure), apply new sterile dressing (do not cut), document: site, type/quant of secretions, client tolerance of procedure 43. Addison’s Disease → deficiency in adrenocortical hormones a. Addisonian Crisis → acute adrenocortical insufficiency caused by stress, surgery, trauma or infections i. Signs & Symptoms → classic shock symptoms (hypotension & cyanosis), profound weakness & fatigue, severe N/V, dehydration, H/A, confusion, abdominal pain b. Signs & Symptoms → weakness/fatigue, anorexia/weight loss, N/V, constipation/diarrhea, BRONZE skin discoloration, increased pigmentation of the mucous membranes, poor coordination, fasting hypoglycemia, craving salty food, amenorrhea c. Treatment → corticosteroid replacement therapy → cortisone or hydrocortisone i. Fludrocortisone to prevent dehydration & hypotension ii. In crisis → give dexamethasone, hydrocortisone or both d. Nursing Care → monitor vitals & for s/s of shock, hyperkalemia before treatment & hypokalemia after therapy i. Glucose levels checked if patient also has diabetes ii. Diet → sodium & potassium balance iii. Record weight & monitor fluid/electrolyte intake 44. Wound healing (p. 67) a. Dressing: Document amount/character of drainage, HCP changes first post op dressing, aseptic technique, note presence of drains. b. Stages of wound healing i. Inflammatory response ii. Epithelial proliferation iii. Migration iv. Remodeling c. Incision site: Assess: edematous, inflamed, excoriated; drainage: serous, serosanguineous, purulent; Note type of sutures, if edges are well approximated. d. Risk of infection 3-5 days post procedure e. Debride wound if needed to reduce inflammation f. Change dressing frequently to prevent skin breakdown and bacteriac growth i. Types of dressing 1. Dry 2. Open 3. Closed-wet 4. Saline moisturized 5. transparent g. Diet: High calorie, high protein, high in vitamins A & C and mineral zinc 45. Transesophageal Echocardiogram (TEE) a. Diagnostic test using ultrasound to visualize cardiac structures and abnormalities (Cardiac tests) 46. Intracranial Tumor a. Term that describes any intracranial mass. Neoplastic (malignant or benign; secondary or primary), cystic, inflammatory, or syphilic. Types in children: astrocytomas, medulloblastomas, ependymomas, brain stem gliomas and in adults. Gliomas, meningiomas, oligodendrogliomas, acoustic neurons (Schwannomas); b. classified according to location into two types: supratentorial is within the cerebral hemisphere and incision is usually behind hairline; infratentorial is within the brainstem and cerebellum and incision is at nape of neck around occipital lobe. c. Causes → exposure to ionizing radiation; pathophysiology: as mass expands, cerebral tissue is compressed causing cerebral edema and increased intracranial pressure (ICP) d. S/S→ those of ICP and location, size, and degree and speed of invasion of tumor; indications vary depending on location and may include deficits in motor, language, hearing, and visual abilities, dizziness, paresthesias, seizures, personality disturbances, papilledema, nausea and vomiting, drowsiness, changes in level of consciousness, headache, behavioral changes, mental activity changes, weakness, sensory losses, disturbances in speech, vision, gait, or balance, seizures. e. Symptoms for cerebellar tumor include uncoordination of voluntary movements, imbalances, disequilibrium, assessment, headshave, psychological support. f. Symptoms for frontal lobe tumors: include behavioral and emotional changes, impaired judgement, impaired sense of smell, memory loss, paralysis, reduced mental abilities and vision loss. Patients s/s may include personality changes. g. Symptoms of parietal lobe tumors: include impaired speech, inability to write, lack of recognition, and spatial disorders. h. Postoperative nursing interventions include maintain patent airway, elevate head of bed 30 to 45 degrees after supratentorial surgery, position client flat and lateral on either side after infratentorial surgery, monitor vital and neurological signs, observe for complications, administer medications (steroids, diuretics, analgesics, no narcotics; use acetaminophen, anticonvulsants, antibiotics, antipyretics, antiemetics); i. Imaging studies of the brain → radiological method of looking at both structure and function of the brain; can be done with or without contrast medium j. nursing considerations → assess the client for allergies to medium agent if used 47. Culturally Competent Care a. Culturally competent care means planning and implement care that is sensitive to the needs of individual, groups, and families from diverse cultures; it requires cultural sensitivity and cultural awareness; when a nurse from one culture interacts with a client from another culture, b. factors that affect the interaction include: each person’s culture, expectations and beliefs about healthcare, the context of the interaction, the amount of agreement between the two sets of values and beliefs. c. Postmortem Care → all health care team members should be aware of culturally competent care of the body after death; traditions from the orthodox Jewish faith include not touching the body for 30 minutes after death and not leaving the body alone between the time of death and burial; in the Roman Catholic faith, the body is not shrouded until the sacraments are performed; Greek tradition includes the body being washed by a relative or older woman; African Americans prefer that the health team clean and prepare the body; Hispanic families may help with care of the body. 48. Benign Prostate Hypertrophy a. Enlargement of the prostate gland, which surrounds the neck of the bladder and urethra in men. Results in compression and urinary retention b. Pathopys. → testosterone and estrogen impacts DHT (dihydrotestosterone) the growth hormone to BPH c. Risk factors → AGE, family hx, hormonal factors, ethnicity, race, consumption of alcohol and use of cigarettes, HTN, heart disease, diabetes, dietary fat and meal consumption d. Complications → hemorrhage, catheter obstruction, cardiac/resp./renal failure, azotemia (nitrogen waste in blood) e. S/S → generalized SX → fatigue, anorexia, N/V, epigastric discomfort. If obstructing the bladder → dysuria, frequency, urgency, leakage, decreased force of urinary stream, hesitancy, nocturia, recurrent UTI’s, dribbling, sensation that bladder has not been emptied, abdominal straining w/ urination f. RN Interventions → if surgery not indicated include teaching about BPH, encourage fluids, explaining medications catheterizing if ordered, monitor urine output i. Pre op → promoting urinary drainage, discussing concerns (including possible sexual dysfunction), ii. Post op → assessing and maintaining catheter patency, if traction on catheter keep leg straight, monitor drainage, controlling and treating bladder spasms, teaching pelvic exercises, instructing to avoid heavy lifting and prolonged sitting, discussing sexuality concerns g. Tx vary regarding causes and severity of obstruction i. catheterization (a metal catheter with a pronounced prostatic curve is used in more severe cases) ii. Superpubic cystostomy, alphaderenergic blockers, antiandrogen agents, transurethral incision of the prostate (TUIP), transurethral laser resection, transurethral needle ablation, microwave thermotherapy, h. Diagnostic test → digital rectal examination, urinalysis and urodynamic, Creatinine 49. Cataracts a. Opacity of lens that is usually caused by aging. b. Indications → include blurred vision and decreased visual acuity. c. Treatment → removal of the eye lens and cortex by opening the anterior capsule with insertion of new synthetic lens. d. Nursing Responsibilities → antibiotic and steroid ointment and/or drops instilled into eye immediately post-op. e. Eye covered with patch and protective shield, position on the back, in semi-fowler position, or on (floaters, flashing lights, decrease in vision), pain redness, swelling, increase in drainage amount, change in drainage color, injury to eye, infection. f. Client education → wear the eye protective covering until first postoperative visit within 24 hours, wear covering at night up to a month, medicate pain with acetaminophen, vision will clear over several days to weeks, use sunglasses when outside or in bright light, cleanse daily in the morning with wet bath cloth, bathe and shampoo hair with assistance as directed, for 24 hours postoperatively, light activity, resume other activities as directed, no lifting or pushing pulling heavy objects as directed. Lay on the unoperated side. 50. Systemic Lupus a. Chronic, systemic inflammatory autoimmune collagen vascular disease of multiple body systems; indications include arthritis (synovitis), joint swelling, tenderness, and pain on movement, butterfly rash across bridge of nose and cheeks, polymyositis, oral ulcers, pericarditis, pleural effusion, papular, erythematous, purpuric lesions, lymphadenopathy, depression. b. Nursing interventions → maintaining skin integrity, monitoring steroid therapy, monitoring closely for infection and teaching preventive measures, avoid direct sunlight and UV light, relieving pain and discomfort, including NSAID use, advising on lifestyle changes to decrease stress level, decrease risk of coronary artery disease, monitoring for cognitive abilities and emotional stability, providing emotional support. c. Labs → increased ECR and CRP 51. GERD a. Syndrome resulting from esophageal reflux which is backward flow from gastric components into esophagus. b. Esophageal mucosal breaks down often associated with hiatal hernia but not necessarily c. Indications → odynophagia (severe sensation of burning, squeezing pain while swallowing), acid regurgitation, dysphagia, dyspepsia (gastric discomfort after eating, such as fullness, heartburn, bloating, nausea), pain from esophageal spasms, i. Symptoms may mimic heart attack symptoms d. Interventions → may include surgery if client does not respond to medical management i. Administer medications as ordered to decrease reflux (antacids, histamine receptor antagonist, cholinergics, GI stimulants, PPI), ii. instruct about dietary changes (small frequent feedings, adequate fluids with meals, chew slowly and thoroughly, avoid irritating foods such as very hot or cold, spicy, fatty, citrus juices, coffee), iii. NPO for 3 hours before sleep iv. instruct about lifestyle changes (elevate head 6-8 inches at night, lose weight if overweight, avoid tobacco, salicylate, alcohol), use pillows under shoulder and head at night time e. Tx → to reduce intra abdominal pressure sleep in trendelenburg position, avoid lying down after meals and late night snacks, antacids given 1 hr and 3 hrs after meals and at bedtime, PPI, surgery f. Risk Factors → incompetent LES, pyloric stenosis, pyloric surgery, motility disorder, increased age, long term NG tube intubation (>5 days), g. Dx Test → endoscopy or barium swallow, ambulatory 12 to 36 hour esophageal pH monitoring, Bilirubin monitoring h. Complications: Pulmonary symptoms from aspiration of gastric contents into throat, with subsequent aspiration: i. Chronic pulmonary disease or nocturnal wheezing ii. Bronchitis iii. Asthma iv. Morning hoarseness and cough 52. Arthroplasty a. Surgical replacement of a joint with an artificial joint. i. Hip -- the head of the femur and acetabulum. 1. Hemiarthroplasty→ replacement of the head of the femur. Used for diseased femoral joint or fracture of the head of the femur or femoral neck; a. complications→ dislocation of hip prosthesis, excessive wound drainage, thromboembolism, infection. b. Nursing responsibilities → position leg in abduction using splints or wedge or 2 to 3 pillows between the legs, flex hip no more than 90 degrees, elevate head of the bed no more than 45 degrees, turn from back to unaffected side, use a fracture bedpan by having the client flex the nonoperative hip while using a trapeze to lift the pelvis or have the client ambulate to the bathroom or use a bedside commode, use of overbed trapeze to reposition in bed, use incision care, prevent complications of immobility by early ambulation, use semi-reclining or elevated toilet seats and semi-recliner wheelchairs to prevent hip joint flexion, maintain hip precautions as prescribed by health care provider. ii. Knee -- replace, reconstruct, or reshape a diseased knee joint. Done to alleviate pain, restore normal function, or correct an accident of congenital joint defect. 1. Nursing interventions: a. preoperative preparation and teaching. b. Postoperative nursing interventions: monitor skin under knee immobilizer, ambulate as ordered, perform neurovascular checks to monitor circulation and motion and sensation, provide pain management medications and nonpharmacologic means, monitor for venous thrombosis and fat embolism and or pulmonary embolism, encourage deep breathing and coughing. 2. Client teaching: signs and symptoms of infections. 53. Inflammatory Bowel Disease → Includes Crohn’s disease and ulcerative colitis a. Indications: abdominal pain, diarrhea, fluid imbalance, weight loss. Diarrhea in Crohn’s disease is less severe than in ulcerative colitis. b. Nursing Considerations: include high-protein, high-calorie, low-fat, low-fiber diet, may require TPN to rest the bowel, administer analgesics, anticholinergics, sulfonamides (gentamicin), corticosteroids, antidiarrheals, and anti peristaltics, maintain fluid/electrolyte balance, monitor electrolytes, promote rest, relieve anxiety. i. Crohn’s Disease: Subacute and chronic inflammatory bowel disease involving segments of the terminal ileum and proximal colon; extends through all layers of the bowel wall; restricts absorption of nutrients. 1. Symptoms: colicky lower right quadrant pain not relieved by defecation, diarrhea, weight loss, low-grade fever, nutritional deficit, anemia, dehydrations; fistulas, anorectal fissure or fistula. 2. Treatment: medications→antidiarrheals, antispasmodics, anticholinergics, sulfonamides, steroids. 3. Diet: High calorie, high protein, parenteral nutrition used for bowel rest. NO cocoa, chocolate, citrus juices, cold or carbonated drinks, nuts seeds, popcorn or alcohol. 4. Nursing considerations: High-Protein, high-calorie, low-fat, low-fiber diet, administer medications, maintain fluid and electrolyte balance. ii. Ulcerative colitis: Inflammatory condition of colon characterized by eroded areas of mucous membrane and tissue beneath it. 1. Indications: urge to defecate, abdominal cramping, rectal bleeding, blood, pus, mucus in stool, abdominal pain occurs pre defecation, may have 20 to 30 diarrhea stools daily, nutrition deficit, weight loss, anemia, dehydration. 2. Diet: High-protein, high-calorie, low-fat, low-fiber diet, TPN used for bowel rest, analgesics, anticholinergics, antibiotics, corticosteroids to reduce inflammation, ileostomy. 3. Nursing Considerations: Instruct client about medications and diet, maintain fluid/electrolyte balance, monitor electrolytes, promote rest, relieve anxiety. 54. Respiratory: Chronic Obstructive Disorders (2 questions) ❖ Illnesses or disorders occurring in respiratory tract. Starts in the nose and mouth and continues into the lungs, may involve part of all of the respiratory tract. It includes infectious processes as well as abnormalities. ➢ Asthma: ■ Chronic inflammatory disease of the airways caused by increased responsiveness of tracheobronchial tree to various stimuli. ■ S/SX: cough, dyspnea, wheezing, ■ TX: assess respiratory status, administer medications, use peak flow meter, MDI, avoid asthma triggers. May be on theophylline: check theophylline levels often. ➢ Status Asthmaticus is a medical emergency: ■ Nursing Intv: correcting dehydration, and acidosis, improving ventilation, assessing color, respiratory effort, LOC, pulse oximetry, frequent blood gases, SaO2 90%, IV therapy, inhale short acting beta2 agonists. ➢ Bronchiectasis: ■ Chronic dilation of bronchi, frequently on the lower portion of the lung caused by long standing infection. May be acquired or congenital. Involves one or both lungs. ■ S/SX: cough, dyspnea, increased sputum production and wheezing ■ TX: antibiotics, postural drainage, possible resection of diseased areas of lung, ■ Nursing Intv: thorough assessment of respiratory system, O2 sat, elevation of ABGs, increase oral intake, patent airway, sterile suctioning with strict hyperoxygenation prior to suctioning, restrictions on patients activity levels. ➢ Bronchospasm: ■ Narrowing of lumen of bronchi due to muscle spasm. Is frequently associated with reactive airway diseases such as asthma and bronchitis ■ S/SX: coughing frequently and wheezing ■ TX: steroids, bronchodilator, maintain airway ➢ Occupational Lung Disease: pneumoconioses- Silicosis, asbestosis, coal miners,(black lung disease, coal workers lung disease) farmer’s lung, histoplasmosis related to inhaling mineral or inorganic dust, manufactured fibers, metal dusts, biological dusts, or toxic fumes in workplace. Causes lung fibrosis and changes within the lung that lead to dyspnea, respiratory distress, respiratory failure and death. ■ TX → similar to COPD and/or lung transplant 55. Infection Precautions: Contact-Based a. Required with client care activities that require physical skin to skin contact or those that occur between two clients or occur by contact with contaminated inanimate objects in client’s environment. Private room or with client with same infection but no other infection. i. Clean, nonsterile gloves when entering room, ii. change gloves after client contact with fecal material or wound drainage, iii. remove gloves before leaving the client's environment and wash hands with antimicrobial agent iv. wear gown when entering room if clothing has contact with client, environmental surfaces, or if client is incontinent, has diarrhea, an ileostomy, colostomy, or wound drainage. 56. Detached Retina a. Retina is a nervous tissue membrane of the eye that perceives light images of external objects and transmits impulses to the optic nerve. Detachment is separation of retina form choroid, resulting from trauma to the eye, aging process, diabetes or tumors. b. Indications → flashes of light, blurred or “sooty” vision, sensation of particles moving in line of vision, delineated areas of vision blank, feeling of a curtain coming up or down, loss of vision, confusion, apprehension. c. Treatment → surgery to reattach the retina by laser, scleral buckling, or other intraocular procedures. d. Interventions → maintain bed rest. Patch for affected eye or both eyes (as ordered by health care provider), positioning based on surgical procedure performed and location of detachment, and as prescribed by health care provider. e. Client Education → prevent bumping head, do not move eyes rapidly, avoid rapidly jerking head, delay hair washing for 1 week, do not perform strenuous activity for 3 months, use of stool softeners to avoid straining at stool, maintain head in position as ordered by health care provider 57. Respiratory: Acute Disorders ❖ Atelectasis: collapsed or airless lung condition (alveoli collapsed); indications include dyspnea, cyanosis, cough tachycardia, pleuritic chest pain; nursing considerations include suctioning, postural drainage, antibiotics, turn, cough and deep breathe ❖ Pulmonary Embolism: an obstruction of the pulmonary artery, usually caused by embolism from lower extremity thrombosis; indications include pleuritic or anginal chest pain, acute dyspnea, restlessness and apprehension; nursing care includes administering IV heparin, elevating head of bed, administering prescribed oxygen ❖ Flail chest: abnormality of the chest wall occurring when two or more ribs fracture which creates a segment of rib that is not attached on either end;these fractures cause chest wall to become unstable and respond paradoxically; flail area moves in with inspiration and out with expiration; immediate respiratory failure may result and mechanical ventilation may be required with the use of high inspiratory pressures; nursing considerations: monitor for shock, administer humidified oxygen, pain management, monitor ABGs, encourage turning, deep breathing, coughing ❖ Pleurisy: inflammation of the pleura; nursing care: position semi-Fowler’s to high-Fowler’s to aid breathing, encourage respiratory toilet hourly, treat pain as ordered ❖ Pneumothorax: lung collapse caused by accumulation of air or fluid in the pleural cavity; indications include pleuritic pain, tachypnea and shallow breathing, diminished breath sounds; treatment includes chest tubes. ➢ Nursing intervention: insert the chest tube ASAP to remove fluids 58. Lung Cancer a. Malignancy in epithelium of respiratory tract; cigarette smoking is the primary risk factor; no effective screening test, limited treatment options, usually poor prognosis; b. Indications → change in respiratory patterns, persistent cough, bloody or purulent sputum, unexplained dyspnea, unexplained weight loss, recurrent pulmonary system problems, pain in arm or shoulder or chest or back. c. Interventions → surgery, chemotherapy, radiation. d. Nursing Interventions Related to Surgery → usual preoperative and postoperative teaching (especially related to respiration), maintenance of chest tube drainage system. e. Nursing Interventions Related to Chemotherapy and Radiation → gentle and careful skin care, administration of antiemetics and analgesics, provide mouth care, appealing small frequent meals high in calories and protein, hair care, including coping with alopecia, balance rest with activity 59. Bell’s Palsy a. https://www.youtube.com/watch?v=aDkofQthvt0 ❖ Unilateral facial paralysis involving seventh cranial nerve; usually temporary; indications include inability to close eye, decreased corneal reflex, increased lacrimation, drooping mouth, speech difficulty; eating difficulty; nursing interventions include protect head from cold and drafts, administer analgesics, assist with electrical stimulation, teach isometric exercises for facial muscles and also gentle massage and warm packs, prevent corneal abrasions ( artificial tears), sunglasses during the day, eye patch at night, reassure client that client has not had a stroke, provide emotional support for altered body image. ➢ Treatment: ■ Prednisone (to reduce edema), specific antiviral agents, electrotherapy may help prevent atrophy of facial muscles. ➢ Nursing Interventions: ■ Apply moist heat to affected area (for pain), massage pt’s face with a gentle upward motion 2-3 times a day for 5-10min, apply fascial sling to improve lip alignment, provide frequent oral care, provide support. Provide thickened liquids due to difficulty swallowing 60. UTI → infection that begins in the urethra, bladder, ureters or bladder usually caused by Gram negative bacteria, more common in females than males a. Cystitis → bladder inflammation b. Pyelonephritis → inflammation of the kidney c. Signs & Symptoms → frequent urination, urges, pain/burning when urinating, nocturia, pain/tenderness over bladder, cloudy or foul smelling urine, fever, retroperitoneal pain & N/V, confusion in the elderly d. Diagnostic Tests → Clean-catch mid-stream UA, culture & sensitivity e. Treatment → antibiotics, pyridium, vaginal estrogen therapy, ↑ fluid intake to 3000 mL/day, vitamin C & cranberry juice f. Nursing Care → preventative education, empty bladder after sex, avoid douche/powders, wipe from front to back, in children avoid bubble baths. 61. Cystic Fibrosis- (pg. 171, 500) autosomal recessive trait characterized by generalized involvement of exocrine glands, causing production of abnormally thick viscous mucus secretions in the lungs, pancreas, liver, intestine, and reproductive tract. I. Causes- sweat gland dysfunction, resp. dysfunction, GI dysfunction genetic disease (when both parents have it) II. S&S → resp. And GI A. Bronchial obstruction → thick mucus → bacterial infections → COPD sx’s B. Chronic hypoxia C. Hyperinflation of alveoli D. Ciliary destruction → infections E. Pancreatic degeneration → due to thick mucus clog → diabetes F. Biliary cirrhosis (destruction of bile ducts) G. Bowel obstruction in newborns H. Malabsorption I. Failure to thrive III. Risk factors → caucasian children (95%) IV. Diagnostic Tests- Sweat chloride analysis- elevated levels of Na+ and Cl- and above 60; GI enzyme evaluation- pancreatic enzyme deficiency V. Treatment- bronchodilators, mucolytics, corticosteroids, anticholinergics, leukotriene inhibitors, influenza and pneumococcal vaccines; nebulized antibiotics, oral antibiotics, inhaled hypertonic saline, anti-inflammatory agents, pancreatic enzyme supplementation w/ meals, nutritional support, and exercise. Supplements of fat-sol vitamins A, D, E, & K. VI. Nursing Mgmt.- assess airway clearance & VS; admin low flow O2; removal of pulmonary secretions, chest physiotherapy (postural drainage, chest percussion, and vibrations → always done before meals or 1.5 hours after meals), promote adequate fluid(3000 mL/24 hr) and nutritional intake (high calorie). VII. Client Teaching- breathing exercises; stop smoking; avoid hot/cold extremes as well or allergens as well as dampness & drafts; infection control-avoid close contact w/ those that have respiratory infections or the flu; avoid crowds; avoid stress; adequate rest; nourishing diet; good oral hygiene; observe sputum for indications of infection. 62. Esophagoduodenoscopy a. Visualization of esophagus, stomach, and duodenal mucosa through light, flexible fiberoptic tube. Identifies ulcerations, tumors, and obtains tissue biopsy (detect presence of Helicobacter pylori or to rule out gastric carcinoma) or fluid samples. i. Preparation: verify informed consent has been obtained, maintain NPO at least 8 hours before procedure, teach client about numbness of throat due to local anesthetic applied to posterior pharynx. ii. Post Procedure: maintain NPO until gag reflex returns, observe for vomiting of blood, respiratory distress, inform client to expect sore throat for 3-4 days after procedure. b. Description of Procedure: i. Patient is sedated ii. Lubricated endoscope is passed through the mouth and into the esophagus for visualization of the gastric wall and sphincters. iii. Endoscope is advanced to duodenum iv. Still and video images are taken, or images are shown on a monitor for continuous viewing during the procedure. v. Biopsy forceps are passed through the scope to obtain any necessary tissue samples 63. Pressure Ulcer → localized area of necrotic tissue that develops when soft tissue is compressed over a bony prominence a. Pathophysiology → external pressure compresses blood vessels leading to necrosis & friction/shearing forces tear & injure blood vessels & abrade top layer of skin b. Risk Factors → impaired sensory perception /mobility, ALOC, shear, friction & moisture, protein-calorie malnutrition, Old age, dehydration, diabetes, fractures, history of corticosteroid therapy, immunosuppression, poor circulation, multi-system trauma, previous pressure ulcers & significant obesity or thinness c. Prevention → frequent assessment of pressure areas for non-blanching reactive hyperemia especially the coccyx and boney prominences, keeping moisture away from clients skin, repositioning client using draw-sheet, using a turning schedule & providing adequate nutrition & fluids Stages & Treatments 1. Stage 1 → Observable pressure related alteration of skin a. Indicators → change in skin temperature (warm or cool), tissue consistency (firm or boggy) & sensation (pain or itching) b. Treatment → pressure relieving measures → frequent turning, pressure relieving devices & re-positioning 2. Stage 2 → partial thickness skin loss (involves epidermis & dermis) a. Ulcer is superficial → abrasion, blister or shallow crater b. Treatment → maintenance of moist, healing environment i. Saline ii. Occlusive dressing that prevents natural healing but prevents scar formation 3. Stage 3 → full thickness skin loss with tissue damage or necrosis of subcutaneous tissue that may extend down to but not through underlying fascia a. Presentation → deep crater without undermining of adjacent tissue b. Treatment → Debridement i. Wet-to-dry dressings ii. Surgical Intervention iii. Proteolytic Enzymes 4. Stage 4 → full thickness skin loss with extensive destruction, tissue necrosis, or damage to muscle, bone & supporting structures a. Presentation → may have sinus tracts b. Treatment → covered with nonadherent dressing, dressing changed every 8-12 hours i. May require skin grafts! Nursing Considerations to Prevent Pressure Ulcer ❏ Assess for risk factors ❏ Prevent ulcer formation by checking skin & bony prominences daily ❏ Clean skin routinely especially when soiled ❏ Maintain ↑ humidity in environment & use lotion to prevent dry skin ❏ Avoid massaging over bony areas ❏ Protect skin from moisture → incontinence & wound drainage ❏ Use proper turning/ re-positioning techniques to prevent friction & shearing ❏ Try to improve mobility ❏ Document efforts to prevent pressure ulcers & results Nursing Considerations for Patient who has Pressure Ulcer ❏ Assess → ulcer history, stage, location, size, sinus tract presence, visible necrotic tissue, presence of exudate or granulation tissue & evidence of epithelialization ❏ Assess pain status ❏ Debride necrotic tissue & clean wound to remove debris ❏ Provide moist wound-healing environment using proper dressings ❏ Protect wound from further injury ❏ Provide nutrition for wound healing ❏ Apply topical treatment as ordered ❏ Identify cause to promote healing & prevent further development 64. Brachytherapy ❖ Implants (aka seeds, internal radium implants, internal radiation) that are radioactive that are used at tx site, usually a malignant lesion. Seeds are usually placed in body tumor and source is then sealed. If seed becomes dislodged, radiology should be called immediately. ➢ Nursing Interventions: ■ save all dressings and bed linens until the source is removed and then discard the dressings and linen as usual.This is done to ensure that no radiation source is in linen or dressings: urine, feces, and linen are not radioactive ■ Nurse should not stand close or in line with radioactive source. ■ Organize care so limited time is spent in pt.s room (nurses should switch to prevent prolonged exposure per nurse → 30 minutes per shift) ■ Encourage pt. to do own care, pt must stay in bed while implant is in place, position source of radiation is verified by radiography 65. Dumping Syndrome → rapid passage of food passing through stomach causing diaphoresis, diarrhea & hypotension a. Nursing Actions i. Restrict Fluids with meals ii. Avoid Stress after eating → lie down iii. Eat smaller, more frequent meals iv. ↓ Carb & fiber diet [Show More]
Last updated: 1 year ago
Preview 1 out of 83 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Feb 10, 2021
Number of pages
83
Written in
Additional information
This document has been written for:
Uploaded
Feb 10, 2021
Downloads
0
Views
35












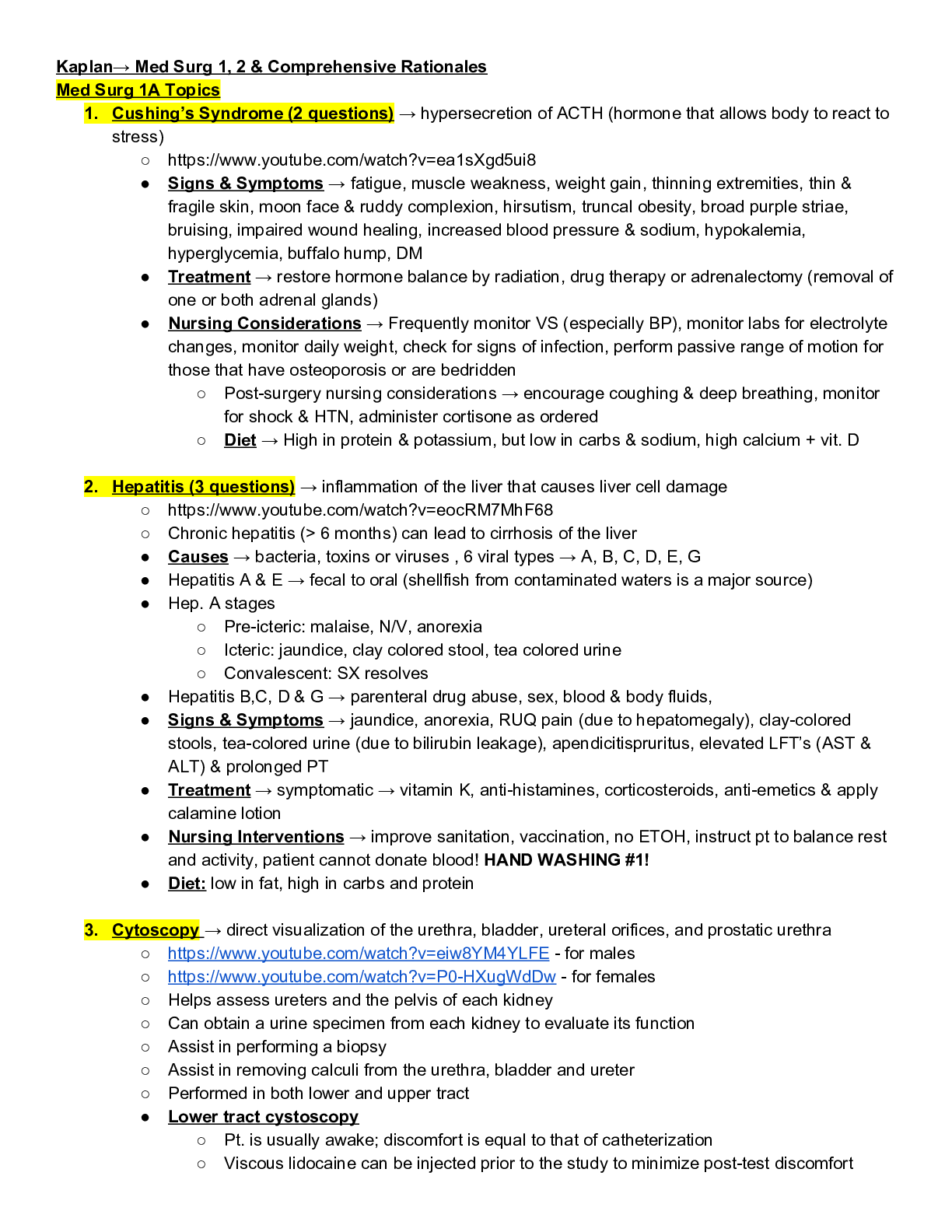
.png)
.png)