*NURSING > QUESTIONS & ANSWERS > Med Surg Test Bank - Summary Primary Concepts Of Adult Nursing. Q&A and the Rationale (1386 Pages) (All)
Med Surg Test Bank - Summary Primary Concepts Of Adult Nursing. Q&A and the Rationale (1386 Pages)
Document Content and Description Below
Table of Contents Table of Contents 1 Chapter 01: Health Care Delivery and Evidence-Based Nursing Practice Chapter 02: Community-Based Nursing Practice Chapter 03: Critical Thinking, Ethical... Decision Making and the Nursing Process Chapter 04: Health Education and Promotion Chapter 05: Adult Health and Nutritional Assessment Chapter 06: Individual and Family Homeostasis, Stress, and Adaptation Chapter 07: Overview of Transcultural Nursing Chapter 08: Overview of Genetics and Genomics in Nursing Chapter 09: Chronic Illness and Disability Chapter 10: Principles and Practices of Rehabilitation Chapter 11: Health Care of the Older Adult Chapter 12: Pain Management Chapter 13: Fluid and Electrolytes: Balance and Disturbance Chapter 14: Shock and Multiple Organ Dysfunction Syndrome Chapter 15: Management of Patients with Oncologic Disorders Chapter 16: End-of-Life Care Chapter 17: Preoperative Nursing Management Chapter 18: Intraoperative Nursing Management Chapter 19: Postoperative Nursing Management Chapter 20: Assessment of Respiratory Function Chapter 21: Respiratory Care Modalities Chapter 22: Management of Patients With Upper Respiratory Tract Disorders Chapter 23: Management of Patients with Chest and Lower Respiratory Tract Disorders Chapter 24: Management of Patients With Chronic Pulmonary Disease Chapter 25: Assessment of Cardiovascular Function Chapter 26: Management of Patients With Dysrhythmias and Conduction Problems Chapter 27: Management of Patients With Coronary Vascular Disorders Chapter 28: Management of Patients With Structural, Infectious, and Inflammatory Cardiac Disorders Chapter 29: Management of Patients With Complications from Heart Disease Chapter 30: Assessment and Management of Patients With Vascular Disorders and Problems of Peripheral Circulation Chapter 31: Assessment and Management of Patients With Hypertension Chapter 32: Assessment of Hematologic Function and Treatment Modalities Chapter 33: Management of Patients With Nonmalignant Hematologic Disorders Chapter 34: Management of Patients With Hematologic Neoplasms Chapter 35: Assessment of Immune Function Chapter 36: Management of Patients With Immune Deficiency Disorders Chapter 37: Assessment and Management of Patients With Allergic Disorders Chapter 38: Assessment and Management of Patients With Rheumatic Disorders Chapter 39: Assessment of Musculoskeletal Function Chapter 40: Musculoskeletal Care Modalities Chapter 41: Management of Patients With Musculoskeletal Disorders Chapter 42: Management of Patients With Musculoskeletal Trauma Chapter 43: Assessment of Digestive and Gastrointestinal Function Chapter 44: Digestive and Gastrointestinal Treatment Modalities Chapter 45: Management of Patients with Oral and Esophageal Disorders Chapter 46: Management of Patients with Gastric and Duodenal Disorders Chapter 47: Management of Patients With Intestinal and Rectal Disorders Chapter 48: Assessment and Management of Patients with Obesity Chapter 49: Assessment and Management of Patients with Hepatic Disorders Chapter 50: Assessment and Management of Patients with Biliary Disorders Chapter 51: Assessment and Management of Patients with Diabetes Chapter 52: Assessment and Management of Patients with Endocrine Disorders Chapter 53: Assessment of Kidney and Urinary Function Chapter 54: Management of Patients with Kidney Disorders Chapter 55: Management of Patients with Urinary Disorders Chapter 56: Assessment and Management of Patients With Female Physiologic Processes Chapter 57: Management of Patients with Female Reproductive Disorders Chapter 58: Assessment and Management of Patients with Breast Disorders Chapter 59: Assessment and Management of Patients With Male Reproductive Disorders Chapter 60: Assessment of Integumentary Function Chapter 61: Managements of Patients with Dermatologic Problems Chapter 62: Managements of Patients with Burn Injury Chapter 63: Assessment and Management of Patients with Eye and Vision Disorders Chapter 64: Assessment and Management of Patients with Hearing and Balance Disorders 1203 Chapter 65: Assessment of Neurologic Function Chapter 66: Management of Patients with Neurologic Dysfunction Chapter 67: Management of Patients with Cerebrovascular Disorders Chapter 68: Management of Patients with Neurologic Trauma Chapter 69: Management of Patients with Neurologic Infections, Autoimmune Disorders, and Neuropathies 1294 Chapter 70: Management of Patients With Oncologic or Degenerative Neurologic Disorders 1312 Chapter 71: Management of Patients With Infectious Diseases Chapter 72: Emergency Nursing Chapter 73: Terrorism, Mass Casualty, and Disaster Nursing Chapter 1 1. The public health nurse is presenting a health promotion class to a group of new mothers. How should the nurse best define health? A) Health is being disease free. B) Health is having fulfillment in all domains of life. C) Health is having psychological and physiological harmony. D) Health is being connected in body, mind, and spirit. 2. A nurse is speaking to a group of prospective nursing students about what it is like to be a nurse. What is one characteristic the nurse would cite as necessary to possess to be an effective nurse? A) Sensitivity to cultural differences B) Team-focused approach to problem-solving C) Strict adherence to routine D) Ability to face criticism 3. With increases in longevity, people have had to become more knowledgeable about their health and the professional health care that they receive. One outcome of this phenomenon is the development of organized self-care education programs. Which of the following do these programs prioritize? A) Adequate prenatal care B) Government advocacy and lobbying C) Judicious use of online communities D) Management of illness 4. The home health nurse is assisting a patient and his family in planning the patient’s return to work after surgery and the development of postsurgical complications. The nurse is preparing a plan of care that addresses the patient’s multifaceted needs. To which level of Maslow’s hierarchy of basic needs does the patient’s need for self-fulfillment relate? A) Physiologic B) Transcendence C) Love and belonging D) Self-actualization 5. The view that health and illness are not static states but that they exist on a continuum is central to professional health care systems. When planning care, this view aids the nurse in appreciating which of the following? A) Care should focus primarily on the treatment of disease. B) A person’s state of health is ever-changing. C) A person can transition from health to illness rapidly. D) Care should focus on the patient’s compliance with interventions. 6. A group of nursing students are participating in a community health clinic. When providing care in this context, what should the students teach participants about disease prevention? A) It is best achieved through attending self-help groups. B) It is best achieved by reducing psychological stress. C) It is best achieved by being an active participant in the community. D) It is best achieved by exhibiting behaviors that promote health. 7. A nurse on a medical-surgical unit has asked to represent the unit on the hospital’s quality committee. When describing quality improvement programs to nursing colleagues and members of other health disciplines, what characteristic should the nurse cite? A) These programs establish consequences for health care professionals’ actions. B) These programs focus on the processes used to provide care. C) These programs identify specific incidents related to quality. D) These programs seek to justify health care costs and systems. 8. Nurses in acute care settings must work with other health care team members to maintain quality care while facing pressures to care for patients who are hospitalized for shorter periods of time than in the past. To ensure positive health outcomes when patients return to their homes, what action should the nurse prioritize? A) Promotion of health literacy during hospitalization B) Close communication with insurers C) Thorough and evidence-based discharge planning D) Participation in continuing education initiatives 9. You are admitting a patient to your medical unit after the patient has been transferred from the emergency department. What is your priority nursing action at this time? A) Identifying the immediate needs of the patient B) Checking the admitting physician’s orders C) Obtaining a baseline set of vital signs D) Allowing the family to be with the patient 10. A nurse on a postsurgical unit is providing care based on a clinical pathway. When performing assessments and interventions with the aid of a pathway, the nurse should prioritize what goal? A) Helping the patient to achieve specific outcomes B) Balancing risks and benefits of interventions C) Documenting the patient’s response to therapy D) Staying accountable to the interdisciplinary team Chapter 2 1. A community health nurse has scheduled a hypertension clinic in a local shopping mall in which shoppers have the opportunity to have their blood pressure measured and learn about hypertension. This nursing activity would be an example of which type of prevention activity? A) Tertiary prevention B) Secondary prevention C) Primary prevention D) Disease prevention 2. The nursing instructor is preparing a group of students for their home care rotation. In preparation, the group discusses the patients that they are most likely to care for in the home. Which of the following groups are the most common recipients of home care services? A) Mentally ill patients B) Patients receiving rehabilitation after surgery C) Terminally ill and palliative patients D) Elderly patients 3. A recent nursing graduate has been surprised at the sharp contrast between some patients’ lifestyles in their homes and the nurse’s own practices and beliefs. To work therapeutically with the patient, what must the nurse do? A) Request another assignment if there is dissonance with the patient’s lifestyle. B) Ask the patient to come to the agency to receive treatment, if possible. C) Resolve to convey respect for the patient’s beliefs and choices. D) Try to adapt the patient’s home to the norms of a hospital environment. 4. Infection control is a high priority in every setting where nursing care is provided. When performing a home visit, how should the nurse best implement the principles of infection control? A) Perform hand hygiene before and after giving direct patient care. B) Remove the patient’s wound dressings from the home promptly. C) Disinfect the patient’s syringes prior to disposal. D) Establish a sterile field in the patient’s home before providing care. 5. An adult patient is ready to be discharged from the hospital after undergoing a transmetatarsal amputation. When should your patient’s discharge planning begin? A) The day prior to discharge B) The day of estimated discharge C) The day that the patient is admitted D) Once the nursing care plan has been finalized 6. A home health nurse is preparing to make the initial visit to a new patient’s home. When planning educational interventions, what information should the nurse provide to the patient and his or her family? A) Available community resources to meet their needs B) Information on other patients in the area with similar health care needs C) The nurse’s contact information and credentials D) Dates and times of all scheduled home care visits 7. The home health nurse receives a referral from the hospital for a patient who needs a home visit for wound care. After obtaining the referral, what would be the first action the nurse should take? A) Have community services make contact with the patient. B) Obtain a physician’s order for the visit. C) Call the patient to obtain permission to visit. D) Arrange for a home health aide to initially visit the patient. 8. At the beginning of a day that will involve several home visits, the nurse has ensured that the health care agency has a copy of her daily schedule. What is the rationale for the nurse’s action? A) It allows the agency to keep track for payment to the nurse. B) It supports safety precautions for the nurse when making a home care visit. C) It allows for greater flexibility for the nurse and his or her colleagues for changes in assignments. D) It allows the patient to cancel appointments with minimal inconvenience. 9. There are specific legal guidelines and regulations for the documentation related to home care. When providing care for a patient who is a Medicaid recipient, what is most important for the nurse to document? A) The medical diagnosis and the supplies needed to care for the patient B) A summary of the patient’s income tax paid during the previous year C) The specific quality of nursing care that is needed D) The patient’s homebound status and the specific need for skilled nursing care 10. Your patient has had a total knee replacement and will need to walk with a two-wheeled walker for 6 weeks. He is being discharged home with a referral for home health care. What will the home care nurse need to assess during the initial nursing assessment in the home? A) Assistance of neighbors B) Qualification for Medicare and Medicaid C) Costs related to the visits D) Characteristics of the home environment Chapter 3 1. A nurse has been offered a position on an obstetric unit and has learned that the unit offers therapeutic abortions, a procedure which contradicts the nurse’s personal beliefs. What is the nurse’s ethical obligation to these patients? A) The nurse should adhere to professional standards of practice and offer service to these patients. B) The nurse should make the choice to decline this position and pursue a different nursing role. C) The nurse should decline to care for the patients considering abortion. D) The nurse should express alternatives to women considering terminating their pregnancy. 2. A terminally ill patient you are caring for is complaining of pain. The physician has ordered a large dose of intravenous opioids by continuous infusion. You know that one of the adverse effects of this medicine is respiratory depression. When you assess your patient’s respiratory status, you find that the rate has decreased from 16 breaths per minute to 10 breaths per minute. What action should you take? A) Decrease the rate of IV infusion. B) Stimulate the patient in order to increase respiratory rate. C) Report the decreased respiratory rate to the physician. D) Allow the patient to rest comfortably. 3. An adult patient has requested a do not resuscitate (DNR) order in light of his recent diagnosis with late stage pancreatic cancer. The patient’s son and daughter-in-law are strongly opposed to the patient’s request. What is the primary responsibility of the nurse in this situation? A) Perform a slow code until a decision is made. B) Honor the request of the patient. C) Contact a social worker or mediator to intervene. D) Temporarily withhold nursing care until the physician talks to the family. 4. An elderly patient is admitted to your unit with a diagnosis of community-acquired pneumonia. During admission the patient states, I have a living will. What implication of this should the nurse recognize? A) This document is always honored, regardless of circumstances. B) This document specifies the patient’s wishes before hospitalization. C) This document that is binding for the duration of the patient’s life. D) This document has been drawn up by the patient’s family to determine DNR status. 5. A nurse has been providing ethical care for many years and is aware of the need to maintain the ethical principle of nonmaleficence. Which of the following actions would be considered a contradiction of this principle? A) Discussing a DNR order with a terminally ill patient B) Assisting a semi-independent patient with ADLs C) Refusing to administer pain medication as ordered D) Providing more care for one patient than for another 6. You have just taken report for your shift and you are doing your initial assessment of your patients. One of your patients asks you if an error has been made in her medication. You know that an incident report was filed yesterday after a nurse inadvertently missed a scheduled dose of the patient’s antibiotic. Which of the following principles would apply if you give an accurate response? A) Veracity B) Confidentiality C) Respect D) Justice 7. A nurse has begun creating a patient’s plan of care shortly after the patient’s admission. It is important that the wording of the chosen nursing diagnoses falls within the taxonomy of nursing. Which organization is responsible for developing the taxonomy of a nursing diagnosis? A) American Nurses Association (ANA) B) NANDA C) National League for Nursing (NLN) D) Joint Commission 8. In response to a patient’s complaint of pain, the nurse administered a PRN dose of hydromorphone (Dilaudid). In what phase of the nursing process will the nurse determine whether this medication has had the desired effect? A) Analysis B) Evaluation C) Assessment D) Data collection 9. A medical nurse has obtained a new patient’s health history and completed the admission assessment. The nurse has followed this by documenting the results and creating a care plan for the patient. Which of the following is the most important rationale for documenting the patient’s care? A) It provides continuity of care. B) It creates a teaching log for the family. C) It verifies appropriate staffing levels. D) It keeps the patient fully informed. 10. The nurse is caring for a patient who is withdrawing from heavy alcohol use and who is consequently combative and confused, despite the administration of benzodiazepines. The patient has a fractured hip that he suffered in a traumatic accident and is trying to get out of bed. What is the most appropriate action for the nurse to take? A) Leave the patient and get help. B) Obtain a physician’s order to restrain the patient. C) Read the facility’s policy on restraints. D) Order soft restraints from the storeroom. Chapter 4 1. A nurse has been working with Mrs. Griffin, a 71-year-old patient whose poorly controlled type 1 diabetes has led to numerous health problems. Over the past several years Mrs. Griffin has had several admissions to the hospital medical unit, and the nurse has often carried out health promotion interventions. Who is ultimately responsible for maintaining and promoting Mrs. Griffin’s health? A) The medical nurse B) The community health nurse who has also worked with Mrs. Griffin C) Mrs. Griffin’s primary care provider D) Mrs. Griffin 2. An elderly female patient has come to the clinic for a scheduled follow-up appointment. The nurse learns from the patient’s daughter that the patient is not following the instructions she received upon discharge from the hospital last month. What is the most likely factor causing the patient not to adhere to her therapeutic regimen? A) Ethnic background of health care provider B) Costs of the prescribed regimen C) Presence of a learning disability D) Personality of the physician 3. A gerontologic nurse has observed that patients often fail to adhere to a therapeutic regimen. What strategy should the nurse adopt to best assist an older adult in adhering to a therapeutic regimen involving wound care? A) Demonstrate a dressing change and allow the patient to practice. B) Provide a detailed pamphlet on a dressing change. C) Verbally instruct the patient how to change a dressing and check for comprehension. D) Delegate the dressing change to a trusted family member. 4. A 20-year-old man newly diagnosed with type 1 diabetes needs to learn how to self-administer insulin. When planning the appropriate educational interventions and considering variables that will affect his learning, the nurse should prioritize which of the following factors? A) Patient’s expected lifespan B) Patient’s gender C) Patient’s occupation D) Patient’s culture 5. The nurse is planning to teach a 75-year-old patient with coronary artery disease about administering her prescribed antiplatelet medication. How can the nurse best enhance the patient’s ability to learn? A) Provide links to Web sites that contain evidence-based information. B) Exclude family members from the session to prevent distraction. C) Use color-coded materials that are succinct and engaging. D) Make the information directly relevant to the patient’s condition. 6. A nurse is planning care for an older adult who lives with a number of chronic health problems. For which of the following nursing diagnoses would education of the patient be the nurse’s highest priority? A) Risk for impaired physical mobility related to joint pain B) Functional urinary incontinence related decreased mobility C) Activity intolerance related to contractures D) Risk for ineffective health maintenance related to nonadherence to therapeutic regimen 7. The nursing instructor has given an assignment to a group of certified nurse practitioner (CNP) students. They are to break into groups of four and complete a health-promotion teaching project and present a report to their fellow students. What project most clearly demonstrates the principles of health-promotion teaching? A) Demonstrating an injection technique to a patient for anticoagulant therapy B) Explaining the side effects of a medication to an adult patient C) Discussing the importance of preventing sexually transmitted infections (STI) to a group of high school students D) Instructing an adolescent patient about safe and nutritious food preparation 8. Health promotion ranks high on the list of health-related concerns of the American public. Based on current knowledge, what factor should the nurse prioritize in an effort to promote health, longevity, and weight control in patients? A) Good nutrition B) Stress reduction C) Use of vitamins D) Screening for health risks 9. The nursing profession and nurses as individuals have a responsibility to promote activities that foster well-being. What factor has most influenced nurses’ abilities to play this vital role? A) Nurses are seen as nurturing professionals. B) Nurses possess a baccalaureate degree as the entry to practice. C) Nurses possess an authentic desire to help others. D) Nurses have long-established credibility with the public. 10. The nurse is teaching a local community group about the importance of disease prevention. Why is the nurse justified in emphasizing disease prevention as a component of health promotion? A) Prevention is emphasized as the link between personal behavior and health. B) Most Americans die of preventable causes. C) Health maintenance organizations (HMOs) now emphasize prevention as the main criterion of health care. D) External environment affects the outcome of most disease processes. Chapter 5 1. A school nurse is teaching a 14-year-old girl of normal weight some of the key factors necessary to maintain good nutrition in this stage of her growth and development. What interventions should the nurse most likely prioritize? A) Decreasing her calorie intake and encouraging her to maintain her weight to avoid obesity B) Increasing her BMI, taking a multivitamin, and discussing body image C) Increasing calcium intake, eating a balanced diet, and discussing eating disorders D) Obtaining a food diary along with providing close monitoring for anorexia 2. A nurse is conducting a health assessment of an adult patient when the patient asks, “Why do you need all this health information and who is going to see it?” What is the nurse’s best response? A) “Please do not worry. It is safe and will be used only to help us with your care. It’s accessible to a wide variety of people who are invested in your health.” B) “It is good you asked and you have a right to know; your information helps us to provide you with the best possible care, and your records are in a secure place.” C) “Your health information is placed on secure Web sites to provide easy access to anyone wishing to see your medical records. This ensures continuity of care.” D) “Health information becomes the property of the hospital and we will make sure that no one sees it. Then, in 2 years, we destroy all records and the process starts over.” 3. The nurse is performing an admission assessment of a 72-year-old female patient who understands minimal English. An interpreter who speaks the patient’s language is unavailable and no members of the care team speak the language. How should the nurse best perform data collection? A) Have a family member provide the data. B) Obtain the data from the old chart and physician’s assessment. C) Obtain the data only from the patient, prioritizing aspects that the patient understands. D) Collect all possible data from the patient and have the family supplement missing details. 4. You are the nurse assessing a 28-year-old woman who has presented to the emergency department with vague complaints of malaise. You note bruising to the patient’s upper arm that correspond to the outline of fingers as well as yellow bruising around her left eye. The patient makes minimal eye contact during the assessment. How might you best inquire about the bruising? A) “Is anyone physically hurting you?” B) “Tell me about your relationships.” C) “Do you want to see a social worker?” D) “Is there something you want to tell me?” 5. You are the nurse performing a health assessment of an adult male patient. The man states, “The doctor has already asked me all these questions. Why are you asking them all over again?” What is your best response? A) “This history helps us determine what your needs may be for nursing care.” B) “You are right; this may seem redundant and I’m sure that it’s frustrating for you.” C) “I want to make sure your doctor has covered everything that’s important for your treatment.” D) “I am a member of your health care team and we want to make sure that nothing falls through the cracks.” 6. You are taking a health history on an adult patient who is new to the clinic. While performing your assessment, the patient informs you that her mother has type 1 diabetes. What is the primary significance of this information to the health history? A) The patient may be at risk for developing diabetes. B) The patient may need teaching on the effects of diabetes. C) The patient may need to attend a support group for individuals with diabetes. D) The patient may benefit from a dietary regimen that tracks glucose intake. 7. A registered nurse is performing the admission assessment of a 37-year-old man who will be treated for pancreatitis on the medical unit. During the nursing assessment, the nurse asks the patient questions related to his spirituality. What is the primary rationale for this aspect of the nurse’s assessment? A) The patient’s spiritual environment can affect his physical activity. B) The patient’s spiritual environment can affect his ability to communicate. C) The patient’s spiritual environment can affect his quality of sexual relationships. D) The patient’s spiritual environment can affect his response to illness. 8. A nurse on a medical unit is conducting a spiritual assessment of a patient who is newly admitted. In the course of this assessment, the patient indicates that she does not eat meat. Which of the following is the most likely significance of this patient’s statement? A) The patient does not understand the principles of nutrition. B) This is an aspect of the patient’s religious practice. C) This constitutes a nursing diagnosis of Risk for Imbalanced Nutrition. D) This is an example of the patient’s coping strategies. 9. You are beginning your shift on a medical unit and are performing assessments appropriate to each patient’s diagnosis and history. When assessing a patient who has an acute staphylococcal infection, what is the most effective technique for assessing the lymph nodes of the patient’s neck? A) Inspection B) Auscultation C) Palpation D) Percussion 10. In your role as a school nurse, you are working with a female high school junior whose BMI is 31. When planning this girl’s care, you should identify what goal? A) Continuation of current diet and activity level B) Increase in exercise and reduction in calorie intake C) Possible referral to an eating disorder clinic D) Increase in daily calorie intake Chapter 6 1. A nurse is meeting with a young woman who has recently lost her job after moving with her husband to a new city. She describes herself as being anxious and pretty depressed. What principle of stress and adaptation should be integrated into the nurse’s plan of care for this patient? A) Adaptation often fails during stressful events and results in homeostasis. B) Stress is a part of all lives, and, eventually, this young woman will adapt. C) Acute anxiety and depression can be adaptations that alleviate stress in some individuals. D) An accumulation of stressors can disrupt homeostasis and result in disease. 2. You are the nurse caring for an adult patient who has just received a diagnosis of prostate cancer. The patient states that he will never be able to cope with this situation. How should you best understand the concept of coping when attempting to meet this patient’s needs? A) Coping is a physiologic measure used to deal with change, and he will physically adapt. B) Coping is composed of the physiologic and psychological processes that people use to adapt to change. C) Coping is the human need for faith and hope, both of which create change. D) Coping is a social strategy that is used to deal with change and loss. 3. The nurse is with a patient who has learned that he has glioblastoma multiforme, a brain tumor associated with an exceptionally poor prognosis. His heart rate increases, his eyes dilate, and his blood pressure increases. The nurse recognizes these changes as being attributable to what response? A) Part of the limbic system response B) Sympathetic nervous response C) Hypothalamic-pituitary response D) Local adaptation syndrome 4. You are the nurse caring for a 72-year-old woman who is recovering from a hemicolectomy on the postsurgical unit. The surgery was very stressful and prolonged, and you note on the chart that her blood sugars are elevated, yet diabetes does not appear in her previous medical history. To what do you attribute this elevation in blood sugars? A) It is a temporary result of increased secretion of antidiuretic hormone. B) She must have had diabetes prior to surgery that was undiagnosed. C) She has suffered pancreatic trauma during her abdominal surgery. D) The blood sugars are probably a result of the fight-or-flight reaction. 5. A patient tells the nurse that she does not like to go to the doctor and is feeling anxious about being in this place. When the nurse checks her blood pressure, it is elevated along with her heart rate. The nurse rechecks her blood pressure about 10 minutes later and it is normal. The patient asks the nurse if she should be concerned that she may have hypertension. What statement should guide the nurse’s response? A) She should not worry; it was stress related and her regular blood pressure is good. B) The first blood pressure was part of a simple stress response; our long-term blood pressure is controlled by negative feedback systems. C) Blood pressure is only one measure of hypertension; she should review this with the doctor and plan to recheck it on a regular basis. D) The respiratory infection is the probably the cause of the elevated blood pressure, and, with treatment, her blood pressure should remain normal. 6. A patient presents to the health center and the nurse practitioner’s assessment reveals an enlarged thyroid. The nurse practitioner believes the thyroid cells may be undergoing hyperplasia. How would the nurse practitioner explain this condition to the patient? A) Hyperplasia is the abnormal decrease in cell and organ size and is a precursor to cancer. B) Hyperplasia is an abnormal increase in new cells and is reversible with the stimulus for cell growth removed. C) Hyperplasia is the change in appearance of the thyroid due to a chronic irritation and will reverse with the stimulus removed. D) Hyperplasia is a cancerous growth and will be removed surgically. 7. A mother has brought her young son to the emergency department (ED). The mother tells the triage nurse that the boy was stung by a bee about an hour ago. The mother explains to the nurse, It hurts him so bad and it looks swollen, red, and infected. What can the triage nurse teach the mother? A) The pain, redness, and swelling are part of the inflammatory process, but it is probably too early for an infection. B) Bee stings frequently cause infection, pain, and swelling, and, with treatment, the infection should begin to subside late today. C) The infection was probably caused by the stinger, which may still be in the wound. D) The mother’s assessment is accurate and the ED doctor will probably prescribe antibiotics to fix the problem. 8. You are caring for an older female patient who is being treated for acute anxiety. She has a nursing diagnosis of Ineffective Coping related to a feeling of helplessness. What would be the most appropriate nursing intervention? A) Put the primary onus for planning care on the patient herself. B) Assess and provide constructive outlets for anger and hostility. C) Assess the patient’s sources of social support. D) Encourage an attitude of realistic hope to help her deal with helpless feelings. 9. A 35-year-old woman comes to the local health center with a large mass in her right breast. She has felt the lump for about a year, but was afraid to come to the clinic because she was sure it was cancer. What is the most appropriate nursing diagnosis for this patient? A) Self-esteem disturbance related to late diagnosis B) Ineffective individual coping related to reluctance to seek care C) Altered family process related to inability to obtain treatment D) Ineffective denial related to reluctance to seek care 10. The nurse at the student health center is seeing a group of students who are interested in reducing their stress level. The nurse identifies guided imagery as an appropriate intervention. What will be included in the nurse’s intervention? A) The use of progressive tensing and relaxing of muscles to release tension in each muscle group B) Using a positive self-image to increase and intensify physical exercise, which decreases stress C) The mindful use of a word, phrase, or visual, which allows oneself to be distracted and temporarily escape from stressful situations D) The use of music and humor to create a calm and relaxed demeanor, which allows escape from stressful situations Chapter 7 1. In a small, rural hospital the nurse is caring for a patient who speaks a language other than English. The nurse needs to use an interpreter to communicate but the hospital does not have access to an interpreter who speaks the patient’s language. When choosing another individual to interpret for this patient, what characteristic should the nurse prioritize? A) Interpreter should recognize the need to speak in a loud voice. B) Interpreter should be able to conduct the conversation quickly to avoid misinterpretation. C) Interpreter should be fluent in several dialects of the patient’s language. D) Interpreter should know that repetition must be avoided while interpreting. 2. You are a community health nurse who provides care to a group of Hispanic people living in an area that is predominantly populated by Caucasian people. How would you characterize the Hispanic people in this community? A) An underclass B) A subgroup C) A minority D) An exception 3. A nurse is caring for an elderly woman who predominantly identifies with an East Asian culture. How can the nurse best demonstrate an awareness of culturally congruent care? A) Maintain eye contact at all times. B) Try to speak the patient’s native language. C) Use touch when communicating. D) Establish effective communication. 4. Most nurses have been taught to maintain direct eye contact when communicating with patients. However, some cultural groups do not usually value direct eye contact when communicating with the nurse. Which cultural group would most likely consider the direct eye contact impolite? A) African Americans B) Hispanics C) Canadians D) Native Americans 5. An emergency department nurse is preparing to inspect and palpate the head and scalp of an older adult who experienced a fall. A member of which group would most likely consider this examination as a violation of norms? A) Jewish B) Asian American C) Islamic D) African American 6. The nurse is helping a patient choose her menu options for the following day. The nurse reads out the option of ham with scalloped potatoes and the patient states that her religion does not allow this. Which of the following is most likely the patient’s religion? A) Roman Catholicism B) Buddhism C) Islam D) Mormonism 7. The nurse is preparing a discharge teaching session with an Asian patient to evaluate the patient’s ability to change a dressing. The patient speaks and understands minimal English. What would be the best way to promote understanding during the teaching session? A) Ask the patient to repeat the instructions carefully. B) Write the procedure out for the patient in simple language. C) Use an interpreter during the teaching session. D) Have the patient demonstrate the dressing change. 8. You are the nurse caring for a patient who is a recent immigrant to the United States from Mexico. Which of the following variables would you prioritize when performing an assessment of the patient’s cultural beliefs? A) Patient’s previous medical history B) Patient’s marital status C) Patient’s age D) Patient’s communication style 9. You are caring for a patient who is terminally ill whose family has requested to hold a spiritual ceremony during which they will be using incense. What would be the best intervention you could make on behalf of this patient? A) Discourage the use of incense in the hospital. B) Ask the family to have the ceremony off the unit. C) Arrange for the ceremony to occur after notifying all departments affected. D) Encourage the family to conduct the ceremony elsewhere because it may affect other patients in the unit. 10. A parent informs the nurse that immunizations are contrary to her religious beliefs, and she does not want her child to receive immunizations. The nurse proceeds to inform the parent that the child will be in grave danger of illness all her life and will not be allowed to start school unless she is immunized. The nurse also informs the parent that she had all of her own children vaccinated with no adverse effects. The nurse’s behavior is an example of what? A) Acculturation B) Cultural blindness C) Cultural imposition D) Cultural taboos Chapter 8 1. A baby is born with what the physician believes is a diagnosis of trisomy 21. This means that the infant has three number 21 chromosomes. What factor describes the etiology of this genetic change? A) The mother also has genetic mutation of chromosome 21. B) The patient has a nondisjunction occurring during meiosis. C) During meiosis, a reduction of chromosomes resulted in 23. D) The patient will have a single X chromosome and infertility. 2. The nurse reviews a patient’s chart and notes that the patient has a gene mutation that affects protein structure, producing hemoglobin S. The nurse knows that with this gene mutation, the patient will experience symptoms of what? A) Peripheral and pulmonary edema B) Thrombotic organ damage C) Metastasis of a glioblastoma D) Amyotrophic lateral sclerosis 3. During the admission assessment, the nurse notes many café-au-lait spots on the patient’s trunk, back, neck, and legs and suspects that the patient has neurofibromatosis. Based on the nurse’s knowledge of neurofibromatosis, the nurse understands that a single family member has which of the following? A) A spontaneous mutation B) A germline mutation C) A nondisjunction D) A monosomy 4. A 45-year-old man has just been diagnosed with Huntington disease. He and his wife are concerned about their four children. What will the nurse understand about the children’s possibility of inheriting the gene for the disease? A) Each child will have a 25% chance of inheriting the disease. B) Each child will have a 50% chance of inheriting the disease. C) Each child will have a 75% chance of inheriting the disease. D) Each child will have no chance of inheriting the disease. 5. A young woman and her husband want to start a family. The young woman explains to the nurse that she had a retinoblastoma as a child. The woman and her husband are concerned about the chances of their son or daughter developing a retinoblastoma. What is important for the nurse to explain to the couple? A) Retinoblastoma is an autosomal recessive inheritance in which each parent carries the gene mutation. B) Retinoblastoma is an X-linked inheritance and all males inherit an X chromosome from their mothers. C) Retinoblastoma is an autosomal dominant inheritance that has incomplete penetrance and can skip a generation. D) Retinoblastoma is a pattern that is more horizontal than vertical; relatives of a single generation tend to have the condition. 6. A 47-year-old patient with osteoarthritis and hypertension is diagnosed with breast cancer. She tells the nurse that her mother also suffered from osteoarthritis and hypertension, and she developed breast cancer at the age of 51 years. The nurse should recognize that this patient’s health status may be the result of what phenomenon? A) X-linked inheritance B) Autosomal recessive inheritance C) Autosomal dominant inheritance D) Multifactorial inheritance 7. While the nurse is taking the patient’s history, the patient tells the nurse she is trying to get pregnant and she is very fearful she will have another miscarriage. She states she has lost two pregnancies and she shares with the nurse that she does not know why she lost the babies. Based on this patient’s history, what recommendation should the nurse make at the present time? A) Instruct her to continue to try to get pregnant B) Let the patient know that her loss may not occur again C) Encourage her explore the possibility of chromosome testing studies D) Instruct her to have an amniocentesis with the next pregnancy 8. A perinatal nurse is providing care for a primiparous woman who gave birth to a healthy infant yesterday. The nurse explains to the patient the genetic screening that is mandated. What is the nurse’s best rationale for this? A) “Genetic screening is a way to determine the rate of infectious disease in babies during this vulnerable time in their lives.” B) “It is important to screen newborns to determine their future cancer risk and appraise the quality of prenatal care they received.” C) “This is a way to assess your infant’s risk for illnesses called phenylketonuria (PKU), congenital hypothyroidism, and galactosemia.” D) “This testing is required and you will not be able to refuse it. It usually is free so there is no reason to refuse it.” 9. A 50-year-old woman presents at the clinic with complaints of recent episodes of forgetfulness and “jerky” head movements. She states her mother had some kind of illness in which she had to be institutionalized at age 42 and passed away at age 45. She stated, “My mother forgot who we were when she was institutionalized.” Based on this information, what does the nurse suspect? A) Huntington disease B) Schizophrenia C) Cerebrovascular accident D) Alzheimer’s disease 10. The occupational health nurse is conducting yearly health screenings. A 50-year-old man states, “My father had colon cancer, but I really don’t understand why that means that I need a colonoscopy.” What could the nurse do to disseminate information about screening to more individuals? A) Plan a health fair for the employees that provides information about screening for diseases that have an inheritance pattern. B) Refer each employee over the age of 50 to a gastroenterologist. C) Create a Web site on diet and exercise as it relates to the prevention of colon cancer in people over 50. D) Place brochures in the nurses’ facility for the employees to access in answering their questions. Chapter 9 1. An elderly patient has presented to the clinic with a new diagnosis of osteoarthritis. The patient’s daughter is accompanying him and you have explained why the incidence of chronic diseases tends to increase with age. What rationale for this phenomenon should you describe? A) With age, biologic changes reduce the efficiency of body systems. B) Older adults often have less support and care from their family, resulting in illness. C) There is an increased morbidity of peers in this age group, and this leads to the older adult’s desire to also assume the “sick role.” D) Chronic illnesses are diagnosed more often in older adults because they have more contact with the health care system. 2. A patient tells the nurse that her doctor just told her that her new diagnosis of rheumatoid arthritis is considered to be a “chronic condition.” She asks the nurse what “chronic condition” means. What would be the nurse’s best response? A) “Chronic conditions are defined as health problems that require management of several months or longer.” B) “Chronic conditions are diseases that come and go in a relatively predictable cycle.” C) “Chronic conditions are medical conditions that culminate in disabilities that require hospitalization.” D) “Chronic conditions are those that require short-term management in extended-care facilities.” 3. A medical-surgical nurse is teaching a patient about the health implications of her recently diagnosed type 2 diabetes. The nurse should teach the patient to be proactive with her glycemic control in order to reduce her risk of what health problem? A) Arthritis B) Renal failure C) Pancreatic cancer D) Asthma 4. A patient who undergoes hemodialysis three times weekly is on a fluid restriction of 1000 mL/day. The nurse sees the patient drinking a 355-mL (12 ounce) soft drink after the patient has already reached the maximum intake of fluid for the day. What action should the nurse take? A) Take the soft drink away from the patient and inform the dialysis nurse to remove extra fluid from the patient during the next dialysis treatment B) Document the patient’s behavior as noncompliant and notify the physician C) Further restrict the patient’s fluid for the following day and communicate this information to the charge nurse D) Reinforce the importance of the fluid restriction and document the teaching and the intake of extra fluid 5. A patient with end-stage lung cancer has been admitted to hospice care. The hospice team is meeting with the patient and her family to establish goals for care. What is likely to be a first priority in goal setting for the patient? A) Maintenance of activities of daily living B) Pain control C) Social interaction D) Promotion of spirituality 6. An international nurse has noted that a trend in developing countries is a decrease in mortality from some acute conditions. This has corresponded with an increase in the incidence and prevalence of chronic diseases. What has contributed to this decrease in mortality from some acute conditions? A) Improved nutrition B) Integration of alternative health practices C) Stronger international security measures D) Decrease in obesity 7. A 37-year-old woman with multiple sclerosis is married and has three children. The nurse has worked extensively with the woman and her family to plan appropriate care. What is the nurse’s most important role with this patient? A) Ensure the patient adheres to all treatments B) Provide the patient with advice on alternative treatment options C) Provide a detailed plan of activities of daily living (ADLs) for the patient D) Help the patient develop strategies to implement treatment regimens 8. A patient has recently been diagnosed with type 2 diabetes. The patient is clinically obese and has a sedentary lifestyle. How can the nurse best begin to help the patient increase his activity level? A) Set up appointment times at a local fitness center for the patient to attend. B) Have a family member ensure the patient follows a suggested exercise plan. C) Construct an exercise program and have the patient follow it. D) Identify barriers with the patient that inhibit his lifestyle change. 9. A home care nurse is making an initial visit to a 68-year-old man. The nurse finds the man tearful and emotionally withdrawn. Even though the man lives alone and has no family, he has been managing well at home until now. What would be the most appropriate action for the nurse to take? A) Reassess the patient’s psychosocial status and make the necessary referrals B) Have the patient volunteer in the community for social contact C) Arrange for the patient to be reassessed by his social worker D) Encourage the patient to focus on the positive aspects of his life 10. You are caring for a patient with a history of chronic angina. The patient tells you that after breakfast he usually takes a shower and shaves. It is at this time, the patient says, that he tends to experience chest pain. What might you counsel the patient to do to decrease the likelihood of angina in the morning? A) Shower in the evening and shave before breakfast. B) Skip breakfast and eat an early lunch. C) Take a nitro tab prior to breakfast. D) Shower once a week and shave prior to breakfast. Chapter 10 1. The nurse is providing care for an older adult man whose diagnosis of dementia has recently led to urinary incontinence. When planning this patient’s care, what intervention should the nurse avoid? A) Scheduled toileting B) Indwelling catheter C) External condom catheter D) Incontinence pads 2. You are the nurse caring for a female patient who developed a pressure ulcer as a result of decreased mobility. The nurse on the shift before you has provided patient teaching about pressure ulcers and healing promotion. You assess that the patient has understood the teaching by observing what? A) Patient performs range-of-motion exercises. B) Patient avoids placing her body weight on the healing site. C) Patient elevates her body parts that are susceptible to edema. D) Patient demonstrates the technique for massaging the wound site. 3. An elderly female patient who is bedridden is admitted to the unit because of a pressure ulcer that can no longer be treated in a community setting. During your assessment of the patient, you find that the ulcer extends into the muscle and bone. At what stage would document this ulcer? A) I B) II C) III D) IV 4. A 74-year-old woman experienced a cerebrovascular accident 6 weeks ago and is currently receiving inpatient rehabilitation. You are coaching the patient to contract and relax her muscles while keeping her extremity in a fixed position. Which type of exercise is the patient performing? A) Passive B) Isometric C) Resistive D) Abduction 5. An interdisciplinary team has been working collaboratively to improve the health outcomes of a young adult who suffered a spinal cord injury in a workplace accident. Which member of the rehabilitation team is the one who determines the final outcome of the process? A) Most-responsible nurse B) Patient C) Patient’s family D) Primary care physician 6. A school nurse is providing health promotion teaching to a group of high school seniors. The nurse should highlight what salient risk factor for traumatic brain injury? A) Substance abuse B) Sports participation C) Anger mismanagement D) Lack of community resources 7. A nurse is giving a talk to a local community group whose members advocate for disabled members of the community. The group is interested in emerging trends that are impacting the care of people who are disabled in the community. The nurse should describe an increasing focus on what aspect of care? A) Extended rehabilitation care B) Independent living C) Acute-care center treatment D) State institutions that provide care for life 8. The nurse is caring for an older adult patient who is receiving rehabilitation following an ischemic stroke. A review of the patient’s electronic health record reveals that the patient usually defers her self-care to family members or members of the care team. What should the nurse include as an initial goal when planning this patient’s subsequent care? A) The patient will demonstrate independent self-care. B) The patient’s family will collaboratively manage the patient’s care. C) The nurse will delegate the patient’s care to a nursing assistant. D) The patient will participate in a life skills program. 9. You are caring for a 35-year-old man whose severe workplace injuries necessitate bilateral below-the-knee amputations. How can you anticipate that the patient will respond to this news? A) The patient will go through the stages of grief over the next week to 10 days. B) The patient will progress sequentially through five stages of the grief process. C) The patient will require psychotherapy to process his grief. D) The patient will experience grief in an individualized manner. 10. An elderly woman diagnosed with osteoarthritis has been referred for care. The patient has difficulty ambulating because of chronic pain. When creating a nursing care plan, what intervention may the nurse use to best promote the patient’s mobility? A) Motivate the patient to walk in the afternoon rather than the morning. B) Encourage the patient to push through the pain in order to gain further mobility. C) Administer an analgesic as ordered to facilitate the patient’s mobility. D) Have another person with osteoarthritis visit the patient. Chapter 11 1. You are providing care for an 82-year-old man whose signs and symptoms of Parkinson disease have become more severe over the past several months. The man tells you that he can no longer do as many things for himself as he used to be able to do. What factor should you recognize as impacting your patient’s life most significantly? A) Neurologic deficits B) Loss of independence C) Age-related changes D) Tremors and decreased mobility 2. A gerontologic nurse practitioner provides primary care for a large number of older adults who are living with various forms of cardiovascular disease. This nurse is well aware that heart disease is the leading cause of death in the aged. What is an age-related physiological change that contributes to this trend? A) Heart muscle and arteries lose their elasticity. B) Systolic blood pressure decreases. C) Resting heart rate decreases with age. D) Atrial-septal defects develop with age. 3. An occupational health nurse overhears an employee talking to his manager about a 65-year-old coworker. What phenomenon would the nurse identify when hearing the employee state, “He should just retire and make way for some new blood.”? A) Intolerance B) Ageism C) Dependence D) Nonspecific prejudice 4. The nurse is caring for a 65-year-old patient who has previously been diagnosed with hypertension. Which of the following blood pressure readings represents the threshold between high-normal blood pressure and hypertension? A) 140/90 mm Hg B) 145/95 mm Hg C) 150/100 mm Hg D) 160/100 mm Hg 5. You are the nurse caring for an 85-year-old patient who has been hospitalized for a fractured radius. The patient’s daughter has accompanied the patient to the hospital and asks you what her father can do for his very dry skin, which has become susceptible to cracking and shearing. What would be your best response? A) “He should likely take showers rather than baths, if possible.” B) “Make sure that he applies sunscreen each morning.” C) “Dry skin is an age-related change that is largely inevitable.” D) “Try to help your father increase his intake of dairy products.” 6. An elderly patient has come in to the clinic for her twice-yearly physical. The patient tells the nurse that she is generally enjoying good health, but that she has been having occasional episodes of constipation over the past 6 months. What intervention should the nurse first suggest? A) Reduce the amount of stress she currently experiences. B) Increase carbohydrate intake and reduce protein intake. C) Take herbal laxatives, such as senna, each night at bedtime. D) Increase daily intake of water. 7. An 84-year-old patient has returned from the post-anesthetic care unit (PACU) following hip arthroplasty. The patient is oriented to name only. The patient’s family is very upset because, before having surgery, the patient had no cognitive deficits. The patient is subsequently diagnosed with postoperative delirium. What should the nurse explain to the patient’s family? A) This problem is self-limiting and there is nothing to worry about. B) Delirium involves a progressive decline in memory loss and overall cognitive function. C) Delirium of this type is treatable and her cognition will return to previous levels. D) This problem can be resolved by administering antidotes to the anesthetic that was used in surgery. 8. The nurse is providing patient teaching to a patient with early stage Alzheimer’s disease (AD) and her family. The patient has been prescribed donepezil hydrochloride (Aricept). What should the nurse explain to the patient and family about this drug? A) It slows the progression of AD. B) It cures AD in a small minority of patients. C) It removes the patient’s insight that he or she has AD. D) It limits the physical effects of AD and other dementias. 9. A nurse is caring for an 86-year-old female patient who has become increasingly frail and unsteady on her feet. During the assessment, the patient indicates that she has fallen three times in the month, though she has not yet suffered an injury. The nurse should take action in the knowledge that this patient is at a high risk for what health problem? A) A hip fracture B) A femoral fracture C) Pelvic dysplasia D) Tearing of a meniscus or bursa 10. The case manager is working with an 84-year-old patient newly admitted to a rehabilitation facility. When developing a care plan for this older adult, which factors should the nurse identify as positive attributes that benefit coping in this age group? Select all that apply. A) Decreased risk taking B) Effective adaptation skills C) Avoiding participation in untested roles D) Increased life experience E) Resiliency during change Chapter 12 1. The nurse who is a member of the palliative care team is assessing a patient. The patient indicates that he has been saving his PRN analgesics until the pain is intense because his pain control has been inadequate. What teaching should the nurse do with this patient? A) Medication should be taken when pain levels are low so the pain is easier to reduce. B) Pain medication can be increased when the pain becomes intense. C) It is difficult to control chronic pain, so this is an inevitable part of the disease process. D) The patient will likely benefit more from distraction than pharmacologic interventions. 2. Two patients on your unit have recently returned to the postsurgical unit after knee arthroplasty. One patient is reporting pain of 8 to 9 on a 0-to-10 pain scale, whereas the other patient is reporting a pain level of 3 to 4 on the same pain scale. What is the nurse’s most plausible rationale for understanding the patients’ different perceptions of pain? A) Endorphin levels may vary between patients, affecting the perception of pain. B) One of the patients is exaggerating his or her sense of pain. C) The patients are likely experiencing a variance in vasoconstriction. D) One of the patients may be experiencing opioid tolerance. 3. You are frequently assessing an 84-year-old woman’s pain after she suffered a humeral fracture in a fall. When applying the nursing process in pain management for a patient of this age, what principle should you best apply? A) Monitor for signs of drug toxicity due to a decrease in metabolism. B) Monitor for an increase in absorption of the drug due to age-related changes. C) Monitor for a paradoxical increase in pain with opioid administration. D) Administer analgesics every 4 to 6 hours as ordered to control pain. 4. The nurse is assessing a patient’s pain while the patient awaits a cholecystectomy. The patient is tearful, hesitant to move, and grimacing. When asked, the patient rates his pain as a 2 at this time using a 0-to-10 pain scale. How should the nurse best respond to this assessment finding? A) Remind the patient that he is indeed experiencing pain. B) Reinforce teaching about the pain scale number system. C) Reassess the patient’s pain in 30 minutes. D) Administer an analgesic and then reassess. 5. You are creating a nursing care plan for a patient with a primary diagnosis of cellulitis and a secondary diagnosis of chronic pain. What common trait of patients who live with chronic pain should inform your care planning? A) They are typically more comfortable with underlying pain than patients without chronic pain. B) They often have a lower pain threshold than patients without chronic pain. C) They often have an increased tolerance of pain. D) They can experience acute pain in addition to chronic pain. 6. The nurse is caring for a 51-year-old female patient whose medical history includes chronic fatigue and poorly controlled back pain. These medical diagnoses should alert the nurse to the possibility of what consequent health problem? A) Anxiety B) Skin breakdown C) Depression D) Hallucinations 7. Your patient has just returned from the postanesthetic care unit (PACU) following left tibia open reduction internal fixation (ORIF). The patient is complaining of pain, and you are preparing to administer the patient’s first scheduled dose of hydromorphone (Dilaudid). Prior to administering the drug, you would prioritize which of the following assessments? A) The patient’s electrolyte levels B) The patient’s blood pressure C) The patient’s allergy status D) The patient’s hydration status 8. Your patient is receiving postoperative morphine through a patient-controlled analgesic (PCA) pump and the patient’s orders specify an initial bolus dose. What is your priority assessment? A) Assessment for decreased level of consciousness (LOC) B) Assessment for respiratory depression C) Assessment for fluid overload D) Assessment for paradoxical increase in pain 9. Your patient is 12-hours post ORIF right ankle. The patient is asking for a breakthrough dose of analgesia. The pain-medication orders are written as a combination of an opioid analgesic and a nonsteroidal anti-inflammatory drug (NSAID) given together. What is the primary rationale for administering pain medication in this manner? A) To prevent respiratory depression from the opioid B) To eliminate the need for additional medication during the night C) To achieve better pain control than with one medication alone D) To eliminate the potentially adverse effects of the opioid 10. The nurse is caring for a patient with metastatic bone cancer. The patient asks the nurse why he has had to keep getting larger doses of his pain medication, although they do not seem to affect him. What is the nurse’s best response? A) Over time you become more tolerant of the drug. B) You may have become immune to the effects of the drug. C) You may be developing a mild addiction to the drug. D) Your body absorbs less of the drug due to the cancer. Chapter 13 1. You are caring for a patient who has a diagnosis of syndrome of inappropriate antidiuretic hormone secretion (SIADH). Your patient’s plan of care includes assessment of specific gravity every 4 hours. The results of this test will allow the nurse to assess what aspect of the patient’s health? A) Nutritional status B) Potassium balance C) Calcium balance D) Fluid volume status 2. You are caring for a patient admitted with a diagnosis of acute kidney injury. When you review your patient’s most recent laboratory reports, you note that the patient’s magnesium levels are high. You should prioritize assessment for which of the following health problems? A) Diminished deep tendon reflexes B) Tachycardia C) Cool, clammy skin D) Acute flank pain 3. You are working on a burns unit and one of your acutely ill patients is exhibiting signs and symptoms of third spacing. Based on this change in status, you should expect the patient to exhibit signs and symptoms of what imbalance? A) Metabolic alkalosis B) Hypermagnesemia C) Hypercalcemia D) Hypovolemia 4. A patient with a longstanding diagnosis of generalized anxiety disorder presents to the emergency room. The triage nurse notes upon assessment that the patient is hyperventilating. The triage nurse is aware that hyperventilation is the most common cause of which acidbase imbalance? A) Respiratory acidosis B) Respiratory alkalosis C) Increased PaCO2 D) CNS disturbances 5. You are an emergency-room nurse caring for a trauma patient. Your patient has the following arterial blood gas results: pH 7.26, PaCO2 28, HCO3 11 mEq/L. How would you interpret these results? A) Respiratory acidosis with no compensation B) Metabolic alkalosis with a compensatory alkalosis C) Metabolic acidosis with no compensation D) Metabolic acidosis with a compensatory respiratory alkalosis 6. You are making initial shift assessments on your patients. While assessing one patient’s peripheral IV site, you note edema around the insertion site. How should you document this complication related to IV therapy? A) Air emboli B) Phlebitis C) Infiltration D) Fluid overload 7. You are performing an admission assessment on an older adult patient newly admitted for end-stage liver disease. What principle should guide your assessment of the patient’s skin turgor? A) Overhydration is common among healthy older adults. B) Dehydration causes the skin to appear spongy. C) Inelastic skin turgor is a normal part of aging. D) Skin turgor cannot be assessed in patients over 70. 8. The physician has ordered a peripheral IV to be inserted before the patient goes for computed tomography. What should the nurse do when selecting a site on the hand or arm for insertion of an IV catheter? A) Choose a hairless site if available. B) Consider potential effects on the patient’s mobility when selecting a site. C) Have the patient briefly hold his arm over his head before insertion. D) Leave the tourniquet on for at least 3 minutes. 9. A nurse in the neurologic ICU has orders to infuse a hypertonic solution into a patient with increased intracranial pressure. This solution will increase the number of dissolved particles in the patient’s blood, creating pressure for fluids in the tissues to shift into the capillaries and increase the blood volume. This process is best described as which of the following? A) Hydrostatic pressure B) Osmosis and osmolality C) Diffusion D) Active transport 10. You are the surgical nurse caring for a 65-year-old female patient who is postoperative day 1 following a thyroidectomy. During your shift assessment, the patient complains of tingling in her lips and fingers. She tells you that she has an intermittent spasm in her wrist and hand and she exhibits increased muscle tone. What electrolyte imbalance should you first suspect? A) Hypophosphatemia B) Hypocalcemia C) Hypermagnesemia D) Hyperkalemia Chapter 14 1. A nurse in the ICU is planning the care of a patient who is being treated for shock. Which of the following statements best describes the pathophysiology of this patient’s health problem? A) Blood is shunted from vital organs to peripheral areas of the body. B) Cells lack an adequate blood supply and are deprived of oxygen and nutrients. C) Circulating blood volume is decreased with a resulting change in the osmotic pressure gradient. D) Hemorrhage occurs as a result of trauma, depriving vital organs of adequate perfusion. 2. In an acute care setting, the nurse is assessing an unstable patient. When prioritizing the patient’s care, the nurse should recognize that the patient is at risk for hypovolemic shock in which of the following circumstances? A) Fluid volume circulating in the blood vessels decreases. B) There is an uncontrolled increase in cardiac output. C) Blood pressure regulation becomes irregular. D) The patient experiences tachycardia and a bounding pulse. 3. The emergency nurse is admitting a patient experiencing a GI bleed who is believed to be in the compensatory stage of shock. What assessment finding would be most consistent with the early stage of compensation? A) Increased urine output B) Decreased heart rate C) Hyperactive bowel sounds D) Cool, clammy skin 4. The nurse is caring for a patient who is exhibiting signs and symptoms of hypovolemic shock following injuries suffered in a motor vehicle accident. The nurse anticipates that the physician will promptly order the administration of a crystalloid IV solution to restore intravascular volume. In addition to normal saline, which crystalloid fluid is commonly used to treat hypovolemic shock? A) Lactated Ringer’s B) Albumin C) Dextran D) 3% NaCl 5. A patient who is in shock is receiving dopamine in addition to IV fluids. What principle should inform the nurse’s care planning during the administration of a vasoactive drug? A) The drug should be discontinued immediately after blood pressure increases. B) The drug dose should be tapered down once vital signs improve. C) The patient should have arterial blood gases drawn every 10 minutes during treatment. D) The infusion rate should be titrated according the patient’s subjective sensation of adequate perfusion. 6. A nurse in the ICU receives report from the nurse in the ED about a new patient being admitted with a neck injury he received while diving into a lake. The ED nurse reports that his blood pressure is 85/54, heart rate is 53 beats per minute, and his skin is warm and dry. What does the ICU nurse recognize that that patient is probably experiencing? A) Anaphylactic shock B) Neurogenic shock C) Septic shock D) Hypovolemic shock 7. The intensive care nurse caring for a patient in shock is planning assessments and interventions related to the patient’s nutritional needs. What physiologic process contributes to these increased nutritional needs? A) The use of albumin as an energy source by the body because of the need for increased adenosine triphosphate (ATP) B) The loss of fluids due to decreased skin integrity and decreased stomach acids due to increased parasympathetic activity C) The release of catecholamines that creates an increase in metabolic rate and caloric requirements D) The increase in GI peristalsis during shock and the resulting diarrhea 8. The nurse is transferring a patient who is in the progressive stage of shock into ICU from the medical unit. The medical nurse is aware that shock affects many organ systems and that nursing management of the patient will focus on what intervention? A) Reviewing the cause of shock and prioritizing the patient’s psychosocial needs B) Assessing and understanding shock and the significant changes in assessment data to guide the plan of care C) Giving the prescribed treatment, but shifting focus to providing family time as the patient is unlikely to survive D) Promoting the patient’s coping skills in an effort to better deal with the physiologic changes accompanying shock 9. When caring for a patient in shock, one of the major nursing goals is to reduce the risk that the patient will develop complications of shock. How can the nurse best achieve this goal? A) Provide a detailed diagnosis and plan of care in order to promote the patient’s and family’s coping. B) Keep the physician updated with the most accurate information because in cases of shock the nurse often cannot provide relevant interventions. C) Monitor for significant changes and evaluate patient outcomes on a scheduled basis focusing on blood pressure and skin temperature. D) Understand the underlying mechanisms of shock, recognize the subtle and more obvious signs, and then provide rapid assessment. 10. The nurse is caring for a patient in the ICU who has been diagnosed with multiple organ dysfunction syndrome (MODS). The nurse’s plan of care should include which of the following interventions? A) Encouraging the family to stay hopeful and educating them to the fact that, in nearly all cases, the prognosis is good B) Encouraging the family to leave the hospital and to take time for themselves as acute care of MODS patients may last for several months C) Promoting communication with the patient and family along with addressing end-of-life issues D) Discussing organ donation on a number of different occasions to allow the family time to adjust to the idea Chapter 15 1. The public health nurse is presenting a health-promotion class to a group at a local community center. Which intervention most directly addresses the leading cause of cancer deaths in North America? A) Monthly self-breast exams B) Smoking cessation C) Annual colonoscopies D) Monthly testicular exams 2. A nurse who works in an oncology clinic is assessing a patient who has arrived for a 2-month follow-up appointment following chemotherapy. The nurse notes that the patient’s skin appears yellow. Which blood tests should be done to further explore this clinical sign? A) Liver function tests (LFTs) B) Complete blood count (CBC) C) Platelet count D) Blood urea nitrogen and creatinine 3. The school nurse is teaching a nutrition class in the local high school. One student states that he has heard that certain foods can increase the incidence of cancer. The nurse responds, Research has shown that certain foods indeed appear to increase the risk of cancer. Which of the following menu selections would be the best choice for potentially reducing the risks of cancer? A) Smoked salmon and green beans B) Pork chops and fried green tomatoes C) Baked apricot chicken and steamed broccoli D) Liver, onions, and steamed peas 4. Traditionally, nurses have been involved with tertiary cancer prevention. However, an increasing emphasis is being placed on both primary and secondary prevention. What would be an example of primary prevention? A) Yearly Pap tests B) Testicular self-examination C) Teaching patients to wear sunscreen D) Screening mammograms 5. The nurse is caring for a 39-year-old woman with a family history of breast cancer. She requested a breast tumor marking test and the results have come back positive. As a result, the patient is requesting a bilateral mastectomy. This surgery is an example of what type of oncologic surgery? A) Salvage surgery B) Palliative surgery C) Prophylactic surgery D) Reconstructive surgery 6. The nurse is caring for a patient who is to begin receiving external radiation for a malignant tumor of the neck. While providing patient education, what potential adverse effects should the nurse discuss with the patient? A) Impaired nutritional status B) Cognitive changes C) Diarrhea D) Alopecia 7. While a patient is receiving IV doxorubicin hydrochloride for the treatment of cancer, the nurse observes swelling and pain at the IV site. The nurse should prioritize what action? A) Stopping the administration of the drug immediately B) Notifying the patient’s physician C) Continuing the infusion but decreasing the rate D) Applying a warm compress to the infusion site 8. A patient newly diagnosed with cancer is scheduled to begin chemotherapy treatment and the nurse is providing anticipatory guidance about potential adverse effects. When addressing the most common adverse effect, what should the nurse describe? A) Pruritis (itching) B) Nausea and vomiting C) Altered glucose metabolism D) Confusion 9. A patient on the oncology unit is receiving carmustine, a chemotherapy agent, and the nurse is aware that a significant side effect of this medication is thrombocytopenia. Which symptom should the nurse assess for in patients at risk for thrombocytopenia? A) Interrupted sleep pattern B) Hot flashes C) Epistaxis (nose bleed) D) Increased weight 10. The nurse is orienting a new nurse to the oncology unit. When reviewing the safe administration of antineoplastic agents, what action should the nurse emphasize? A) Adjust the dose to the patient’s present symptoms. B) Wash hands with an alcohol-based cleanser following administration. C) Use gloves and a lab coat when preparing the medication. D) Dispose of the antineoplastic wastes in the hazardous waste receptacle. Chapter 16 1. In the past three to four decades, nursing has moved into the forefront in providing care for the dying. Which phenomenon has most contributed to this increased focus of care of the dying? A) Increased incidence of infections and acute illnesses B) Increased focus of health care providers on disease prevention C) Larger numbers of people dying in hospital settings D) Demographic changes in the population 2. A nurse who works in the specialty of palliative care frequently encounters issues and situations that constitute ethical dilemmas. What issue has most often presented challenging ethical issues, especially in the context of palliative care? A) The increase in cultural diversity in the United States B) Staffing shortages in health care and questions concerning quality of care C) Increased costs of health care coupled with inequalities in access D) Ability of technology to prolong life beyond meaningful quality of life 3. The nurse is caring for a patient who has been recently diagnosed with late stage pancreatic cancer. The patient refuses to accept the diagnosis and refuses to adhere to treatment. What is the most likely psychosocial purpose of this patient’s strategy? A) The patient may be trying to protect loved ones from the emotional effects of the illness. B) The patient is being noncompliant in order to assert power over caregivers. C) The patient may be skeptical of the benefits of the Western biomedical model of health. D) The patient thinks that treatment does not provide him comfort. 4. A nurse who sits on the hospital’s ethics committee is reviewing a complex case that has many of the hallmarks of assisted suicide. Which of the following would be an example of assisted suicide? A) Administering a lethal dose of medication to a patient whose death is imminent B) Administering a morphine infusion without assessing for respiratory depression C) Granting a patient’s request not to initiate enteral feeding when the patient is unable to eat D) Neglecting to resuscitate a patient with a “do not resuscitate” order 5. A medical nurse is providing palliative care to a patient with a diagnosis of end-stage chronic obstructive pulmonary disease (COPD). What is the primary goal of this nurse’s care? A) To improve the patient’s and family’s quality of life B) To support aggressive and innovative treatments for cure C) To provide physical support for the patient D) To help the patient develop a separate plan with each discipline of the health care team 6. After contributing to the care of several patients who died in the hospital, the nurse has identified some lapses in the care that many of these patients received toward the end of their lives. What have research studies identified as a potential deficiency in the care of the dying in hospital settings? A) Families’ needs for information and support often go unmet. B) Patients are too sedated to achieve adequate pain control. C) Patients are not given opportunities to communicate with caregivers. D) Patients are ignored by the care team toward the end of life. 7. An adult oncology patient has a diagnosis of bladder cancer with metastasis and the patient has asked the nurse about the possibility of hospice care. Which principle is central to a hospice setting? A) The patient and family should be viewed as a single unit of care. B) Persistent symptoms of terminal illness should not be treated. C) Each member of the interdisciplinary team should develop an individual plan of care. D) Terminally ill patients should die in the hospital whenever possible. 8. A clinic nurse is providing patient education prior to a patient’s scheduled palliative radiotherapy to her spine. At the completion of the patient teaching, the patient continues to ask the same questions that the nurse has already addressed. What is the plausible conclusion that the nurse should draw from this? A) The patient is not listening effectively. B) The patient is noncompliant with the plan of care. C) The patient may have a low intelligence quotient or a cognitive deficit. D) The patient has not achieved the desired learning outcomes. 9. The nurse is part of the health care team at an oncology center. A patient has been diagnosed with leukemia and the prognosis is poor, but the patient is not yet aware of the prognosis. How can the bad news best be conveyed to the patient? A) Family should be given the prognosis first. B) The prognosis should be delivered with the patient at eye level. C) The physician should deliver the news to the patient alone. D) The appointment should be scheduled at the end of the day. 10. A patient has just been told that her illness is terminal. The patient tearfully states, “I can’t believe I am going to die. Why me?” What is your best response? A) “I know how you are feeling.” B) “You have lived a long life.” C) “This must be very difficult for you.” D) “Life can be so unfair.” Chapter 17 1. A patient is admitted to the ED complaining of severe abdominal pain, stating that he has been vomiting coffee-ground like emesis. The patient is diagnosed with a perforated gastric ulcer and is informed that he needs surgery. When can the patient most likely anticipate that the surgery will be scheduled? A) Within 24 hours B) Within the next week C) Without delay because the bleed is emergent D) As soon as all the day’s elective surgeries have been completed 2. The nurse is performing a preoperative assessment on a patient going to surgery. The patient informs the nurse that he drinks approximately two bottles of wine each day and has for the last several years. What postoperative difficulties can the nurse anticipate for this patient? A) Alcohol withdrawal syndrome immediately following surgery B) Alcohol withdrawal syndrome 2 to 4 days after his last alcohol drink C) Alcohol withdrawal syndrome upon administration of general anesthesia D) Alcohol withdrawal syndrome 1 week after his last alcohol drink 3. In anticipation of a patient’s scheduled surgery, the nurse is teaching her to perform deep breathing and coughing to use postoperatively. What action should the nurse teach the patient? A) The patient should take three deep breaths and cough hard three times, at least every 15 minutes for the immediately postoperative period. B) The patient should take three deep breaths and exhale forcefully and then take a quick short breath and cough from deep in the lungs. C) The patient should take a deep breath in through the mouth and exhale through the mouth, take a short breath, and cough from deep in the lungs. D) The patient should rapidly inhale, hold for 30 seconds or as long as possible, and exhale slowly. 4. The nurse is preparing a patient for surgery prior to her hysterectomy without oophorectomy. The nurse is witnessing the patient’s signature on a consent form. Which comment by the patient would best indicate informed consent? A) I know I’ll be fine because the physician said he has done this procedure hundreds of times. B) I know I’ll have pain after the surgery but they’ll do their best to keep it to a minimum. C) The physician is going to remove my uterus and told me about the risk of bleeding. D) Because the physician isn’t taking my ovaries, I’ll still be able to have children. 5. The nurse is planning patient teaching for a patient who is scheduled for an open hemicolectomy. The nurse intends to address the topics of incision splinting and leg exercises during this teaching session. When is the best time for the nurse to provide teaching? A) Upon the patient’s admission to the postanesthesia care unit (PACU) B) When the patient returns from the PACU C) During the intraoperative period D) As soon as possible before the surgical procedure 6. The nurse is caring for a hospice patient who is scheduled for a surgical procedure to reduce the size of his spinal tumor in an effort to relieve his pain. The nurse should plan this patient care with the knowledge that his surgical procedure is classified as which of the following? A) Diagnostic B) Laparoscopic C) Curative D) Palliative 7. A nurse is providing preoperative teaching to a patient who will soon undergo a cardiac bypass. The nurse’s teaching plan includes exercises of the extremities. What is the purpose of teaching a patient leg exercises prior to surgery? A) Leg exercises increase the patient’s muscle mass postoperatively. B) Leg exercises improve circulation and prevent venous thrombosis. C) Leg exercises help to prevent pressure sores to the sacrum and heels. D) Leg exercise help increase the patient’s level of consciousness after surgery. 8. During the care of a preoperative patient, the nurse has given the patient a preoperative benzodiazepine. The patient is now requesting to void. What action should the nurse take? A) Assist the patient to the bathroom. B) Offer the patient a bedpan or urinal. C) Wait until the patient gets to the operating room and is catheterized. D) Have the patient go to the bathroom. 9. The nurse is preparing a patient for surgery. The patient states that she is very nervous and really does not understand what the surgical procedure is for or how it will be performed. What is the most appropriate nursing action for the nurse to take? A) Have the patient sign the informed consent and place it in the chart. B) Call the physician to review the procedure with the patient. C) Explain the procedure clearly to the patient and her family. D) Provide the patient with a pamphlet explaining the procedure. 10. The nurse is caring for a patient who is admitted to the ER with the diagnosis of acute appendicitis. The nurse notes during the assessment that the patient’s ribs and xiphoid process are prominent. The patient states she exercises two to three times daily and her mother indicates that she is being treated for anorexia nervosa. How should the nurse best follow up these assessment data? A) Inform the postoperative team about the patient’s risk for wound dehiscence. B) Evaluate the patient’s ability to manage her pain level. C) Facilitate a detailed analysis of the patient’s electrolyte levels. D) Instruct the patient on the need for a high-sodium diet to promote healing. Chapter 18 1. The nurse is preparing an elderly patient for a scheduled removal of orthopedic hardware, a procedure to be performed under general anesthetic. For which adverse effect should the nurse most closely monitor the patient? A) Hypothermia B) Pulmonary edema C) Cerebral ischemia D) Arthritis 2. The OR nurse acts in the circulating role during a patient’s scheduled cesarean section. For what task is this nurse solely responsible? A) Performing documentation B) Estimating the patient’s blood loss C) Setting up the sterile tables D) Keeping track of drains and sponges 3. A 21-year-old patient is positioned on the OR bed prior to knee surgery to correct a sports-related injury. The anesthesiologist administers the appropriate anesthetic. The OR nurse should anticipate which of the following events as the team’s next step in the care of this patient? A) Grounding B) Making the first incision C) Giving blood D) Intubating 4. A circulating nurse provides care in a surgical department that has multiple surgeries scheduled for the day. The nurse should know to monitor which patient most closely during the intraoperative period because of the increased risk for hypothermia? A) A 74-year-old woman with a low body mass index B) A 17-year-old boy with traumatic injuries C) A 45-year-old woman having an abdominal hysterectomy D) A 13-year-old girl undergoing craniofacial surgery 5. The anesthetist is coming to the surgical admissions unit to see a patient prior to surgery scheduled for tomorrow morning. Which of the following is the priority information that the nurse should provide to the anesthetist during the visit? A) Last bowel movement B) Latex allergy C) Number of pregnancies D) Difficulty falling asleep 6. An OR nurse is teaching a nursing student about the principles of surgical asepsis as a requirement in the restricted zone of the operating suite. What personal protective equipment should the nurse wear at all times in the restricted zone of the OR? A) Reusable shoe covers B) Mask covering the nose and mouth C) Goggles D) Gloves 7. An OR nurse is participating in an interdisciplinary audit of infection control practices in the surgical department. The nurse should know that a basic guideline for maintaining surgical asepsis is what? A) Sterile surfaces or articles may touch other sterile surfaces. B) Sterile supplies can be used on another patient if the packages are intact. C) The outer lip of a sterile solution is considered sterile. D) The scrub nurse may pour a sterile solution from a nonsterile bottle. 8. The surgical patient is a 35-year-old woman who has been administered general anesthesia. The nurse recognizes that the patient is in stage II (the excitement stage) of anesthesia. Which intervention would be most appropriate for the nurse to implement during this stage? A) Rub the patient’s back. B) Restrain the patient. C) Encourage the patient to express feelings. D) Stroke the patient’s hand. 9. A patient waiting in the presurgical holding area asks the nurse, “Why exactly do they have to put a breathing tube into me? My surgery is on my knee.” What is the best rationale for intubation during a surgical procedure that the nurse should describe? A) The tube provides an airway for ventilation. B) The tube protects the patient’s esophagus from trauma. C) The patient may receive an antiemetic through the tube. D) The patient’s vital signs can be monitored with the tube. 10. The circulating nurse in an outpatient surgery center is assessing a patient who is scheduled to receive moderate sedation. What principle should guide the care of a patient receiving this form of anesthesia? A) The patient must never be left unattended by the nurse. B) The patient should begin a course of antiemetics the day before surgery. C) The patient should be informed that he or she will remember most of the procedure. D) The patient must be able to maintain his or her own airway. Chapter 19 1. The recovery room nurse is admitting a patient from the OR following the patient’s successful splenectomy. What is the first assessment that the nurse should perform on this newly admitted patient? A) Heart rate and rhythm B) Skin integrity C) Core body temperature D) Airway patency 2. An adult patient is in the recovery room following a nephrectomy performed for the treatment of renal cell carcinoma. The patient’s vital signs and level of consciousness stabilized, but the patient then complains of severe nausea and begins to retch. What should the nurse do next? A) Administer a dose of IV analgesic. B) Apply a cool cloth to the patient’s forehead. C) Offer the patient a small amount of ice chips. D) Turn the patient completely to one side. 3. The perioperative nurse is preparing to discharge a female patient home from day surgery performed under general anesthetic. What instruction should the nurse give the patient prior to the patient leaving the hospital? A) The patient should not drive herself home. B) The patient should take an OTC sleeping pill for 2 nights. C) The patient should attempt to eat a large meal at home to aid wound healing. D) The patient should remain in bed for the first 48 hours postoperative. 4. The nurse is caring for a 78-year-old man who has had an outpatient cholecystectomy. The nurse is getting him up for his first walk postoperatively. To decrease the potential for orthostatic hypotension and consequent falls, what should the nurse have the patient do? A) Sit in a chair for 10 minutes prior to ambulating. B) Drink plenty of fluids to increase circulating blood volume. C) Stand upright for 2 to 3 minutes prior to ambulating. D) Perform range-of-motion exercises for each joint. 5. The perioperative nurse is providing care for a patient who is recovering on the postsurgical unit following a transurethral prostate resection (TUPR). The patient is reluctant to ambulate, citing the need to recover in bed. For what complication is the patient most at risk? A) Atelectasis B) Anemia C) Dehydration D) Peripheral edema 6. The nurse is caring for a patient on the medicalsurgical unit postoperative day 5. During each patient assessment, the nurse evaluates the patient for infection. Which of the following would be most indicative of infection? A) Presence of an indwelling urinary catheter B) Rectal temperature of 99.5ºF (37.5ºC) C) Red, warm, tender incision D) White blood cell (WBC) count of 8,000/mL 7. The nurse is preparing to change a patient’s abdominal dressing. The nurse recognizes the first step is to provide the patient with information regarding the procedure. Which of the following explanations should the nurse provide to the patient? A) The dressing change is often painful, and we will be giving you pain medication prior to the procedure so you do not have to worry. B) During the dressing change, I will provide privacy at a time of your choosing, it should not be painful, and you can look at the incision and help with the procedure if you want to. C) The dressing change should not be painful, but you can never be sure, and infection is always a concern. D) The best time for doing a dressing change is during lunch so we are not interrupted. I will provide privacy, and it should not be painful. 8. A patient is 2 hours postoperative with a Foley catheter in situ. The last hourly urine output recorded for this patient was 10 mL. The tubing of the Foley is patent. What should the nurse do? A) Irrigate the Foley with 30 mL normal saline. B) Notify the physician and continue to monitor the hourly urine output closely. C) Decrease the IV fluid rate and massage the patient’s abdomen. D) Have the patient sit in high-Fowler’s position. 9. The nurse is caring for a 79-year-old man who has returned to the postsurgical unit following abdominal surgery. The patient is unable to ambulate and is now refusing to wear an external pneumatic compression stocking. The nurse should explain that refusing to wear external pneumatic compression stockings increases his risk of what postsurgical complication? A) Sepsis B) Infection C) Pulmonary embolism D) Hematoma 10. The nurse admits a patient to the PACU with a blood pressure of 132/90 mm Hg and a pulse of 68 beats per minute. After 30 minutes, the patient’s blood pressure is 94/47 mm Hg, and the pulse is 110. The nurse documents that the patient’s skin is cold, moist, and pale. Of what is the patient showing signs? A) Hypothermia B) Hypovolemic shock C) Neurogenic shock D) Malignant hyperthermia Chapter 20 1. A patient is having her tonsils removed. The patient asks the nurse what function the tonsils normally serve. Which of the following would be the most accurate response? A) The tonsils separate your windpipe from your throat when you swallow. B) The tonsils help to guard the body from invasion of organisms. C) The tonsils make enzymes that you swallow and which aid with digestion. D) The tonsils help with regulating the airflow down into your lungs. 2. The nurse is caring for a patient who has just returned to the unit after a colon resection. The patient is showing signs of hypoxia. The nurse knows that this is probably caused by what? A) Nitrogen narcosis B) Infection C) Impaired diffusion D) Shunting 3. The nurse is assessing a patient who frequently coughs after eating or drinking. How should the nurse best follow up this assessment finding? A) Obtain a sputum sample. B) Perform a swallowing assessment. C) Inspect the patient’s tongue and mouth. D) Assess the patient’s nutritional status. 4. The ED nurse is assessing a patient complaining of dyspnea. The nurse auscultates the patient’s chest and hears wheezing throughout the lung fields. What might this indicate? A) The patient has a narrowed airway. B) The patient has pneumonia. C) The patient needs physiotherapy. D) The patient has a hemothorax. 5. The nurse is caring for a patient admitted with an acute exacerbation of chronic obstructive pulmonary disease. During assessment, the nurse finds that the patient is experiencing increased dyspnea. What is the most accurate measurement of the concentration of oxygen in the patient’s blood? A) A capillary blood sample B) Pulse oximetry C) An arterial blood gas (ABG) study D) A complete blood count (CBC) 6. The nurse is caring for a patient who has returned to the unit following a bronchoscopy. The patient is asking for something to drink. Which criterion will determine when the nurse should allow the patient to drink fluids? A) Presence of a cough and gag reflex B) Absence of nausea C) Ability to demonstrate deep inspiration D) Oxygen saturation of ³92% 7. A patient with chronic lung disease is undergoing lung function testing. What test result denotes the volume of air inspired and expired with a normal breath? A) Total lung capacity B) Forced vital capacity C) Tidal volume D) Residual volume 8. In addition to heart rate, blood pressure, respiratory rate, and temperature, the nurse needs to assess a patient’s arterial oxygen saturation (SaO2). What procedure will best accomplish this? A) Incentive spirometry B) Arterial blood gas (ABG) measurement C) Peak flow measurement D) Pulse oximetry 9. A patient asks the nurse why an infection in his upper respiratory system is affecting the clarity of his speech. Which structure serves as the patient’s resonating chamber in speech? A) Trachea B) Pharynx C) Paranasal sinuses D) Larynx 10. A patient with a decreased level of consciousness is in a recumbent position. How should the nurse best assess the lung fields for a patient in this position? A) Inform that physician that the patient is in a recumbent position and anticipate an order for a portable chest x-ray. B) Turn the patient to enable assessment of all the patient’s lung fields. C) Avoid turning the patient, and assess the accessible breath sounds from the anterior chest wall. D) Obtain a pulse oximetry reading, and, if the reading is low, reposition the patient and auscultate breath sounds. [Show More]
Last updated: 1 year ago
Preview 1 out of 1386 pages
Instant download
Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Apr 22, 2020
Number of pages
1386
Written in
Additional information
This document has been written for:
Uploaded
Apr 22, 2020
Downloads
0
Views
78

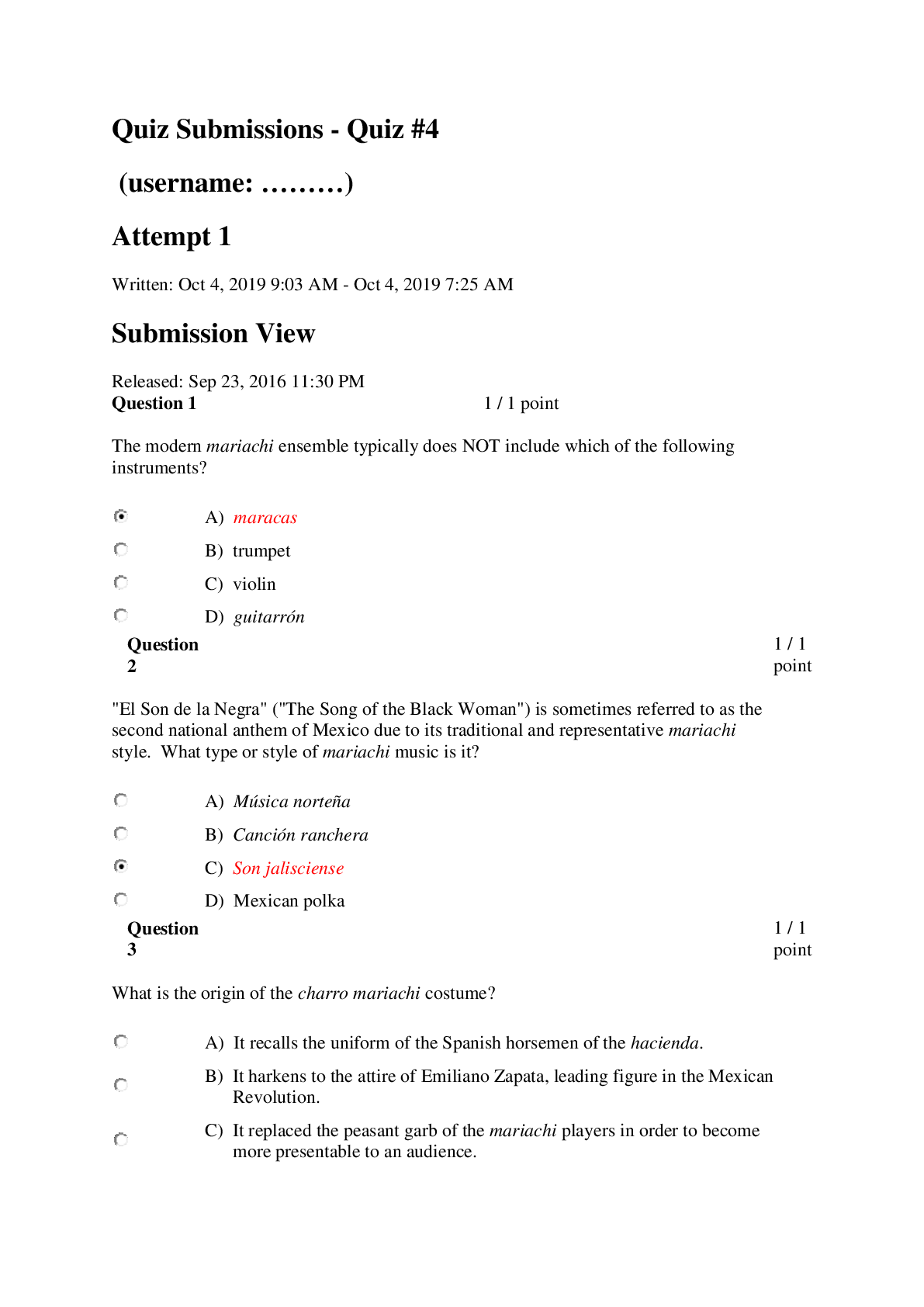
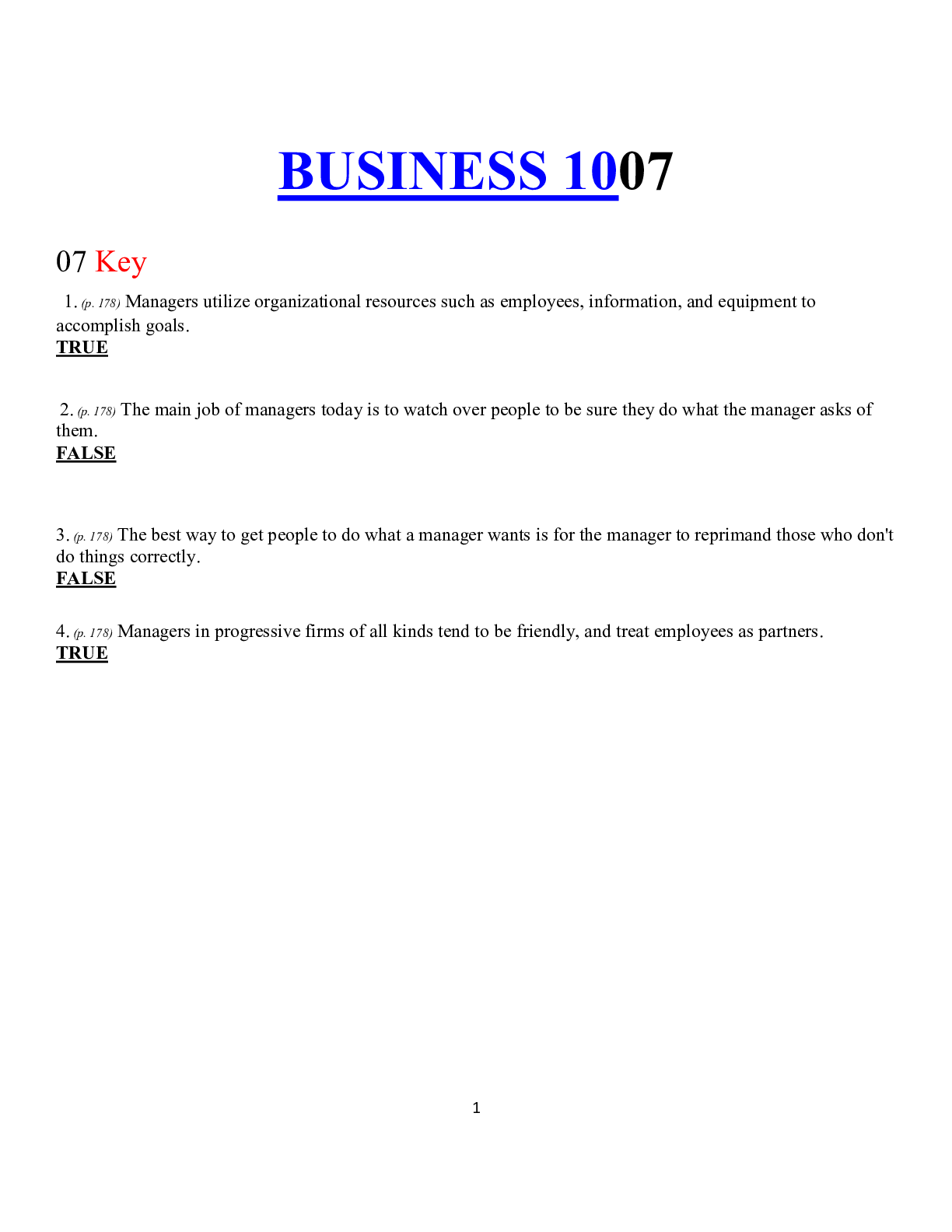
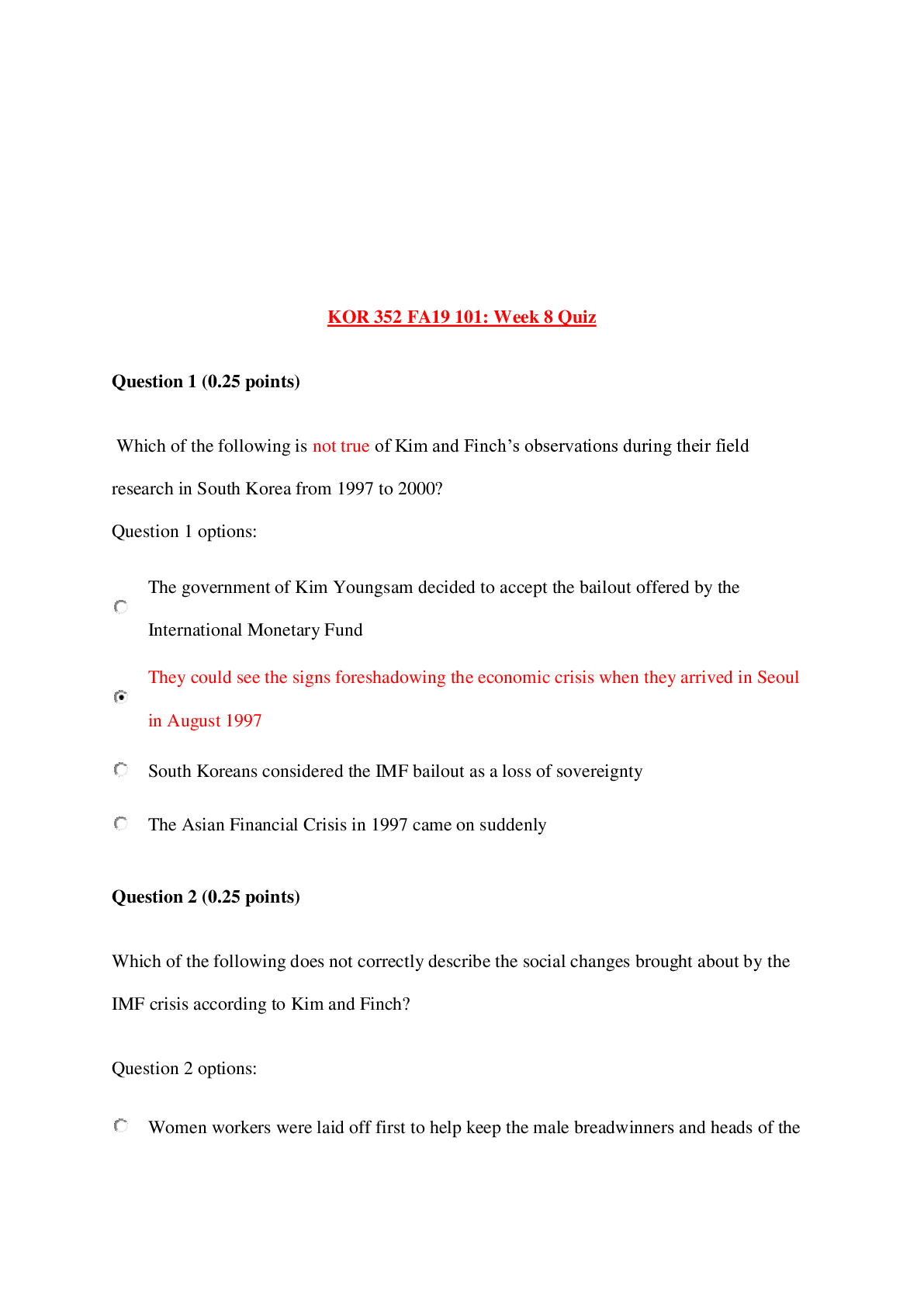
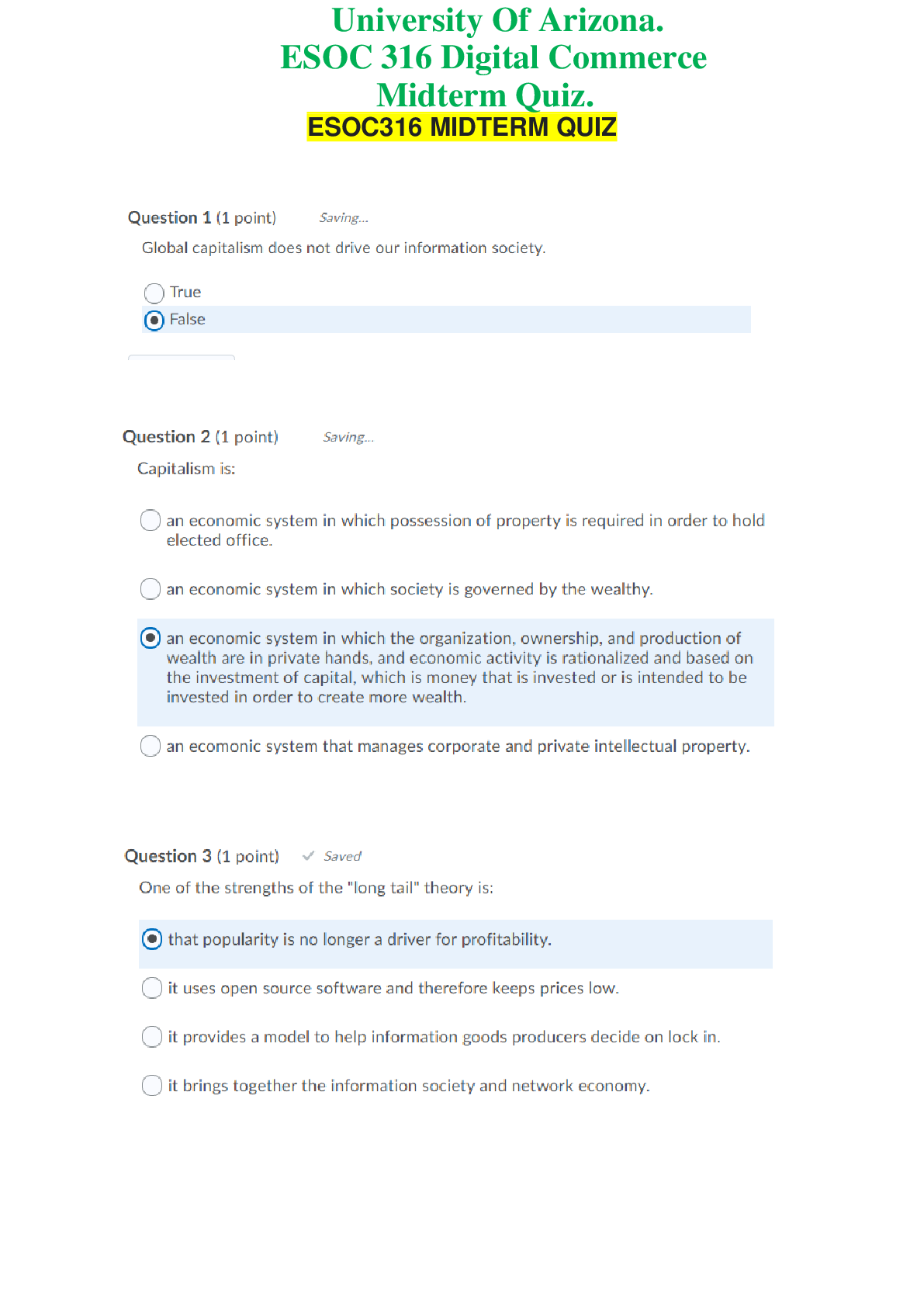
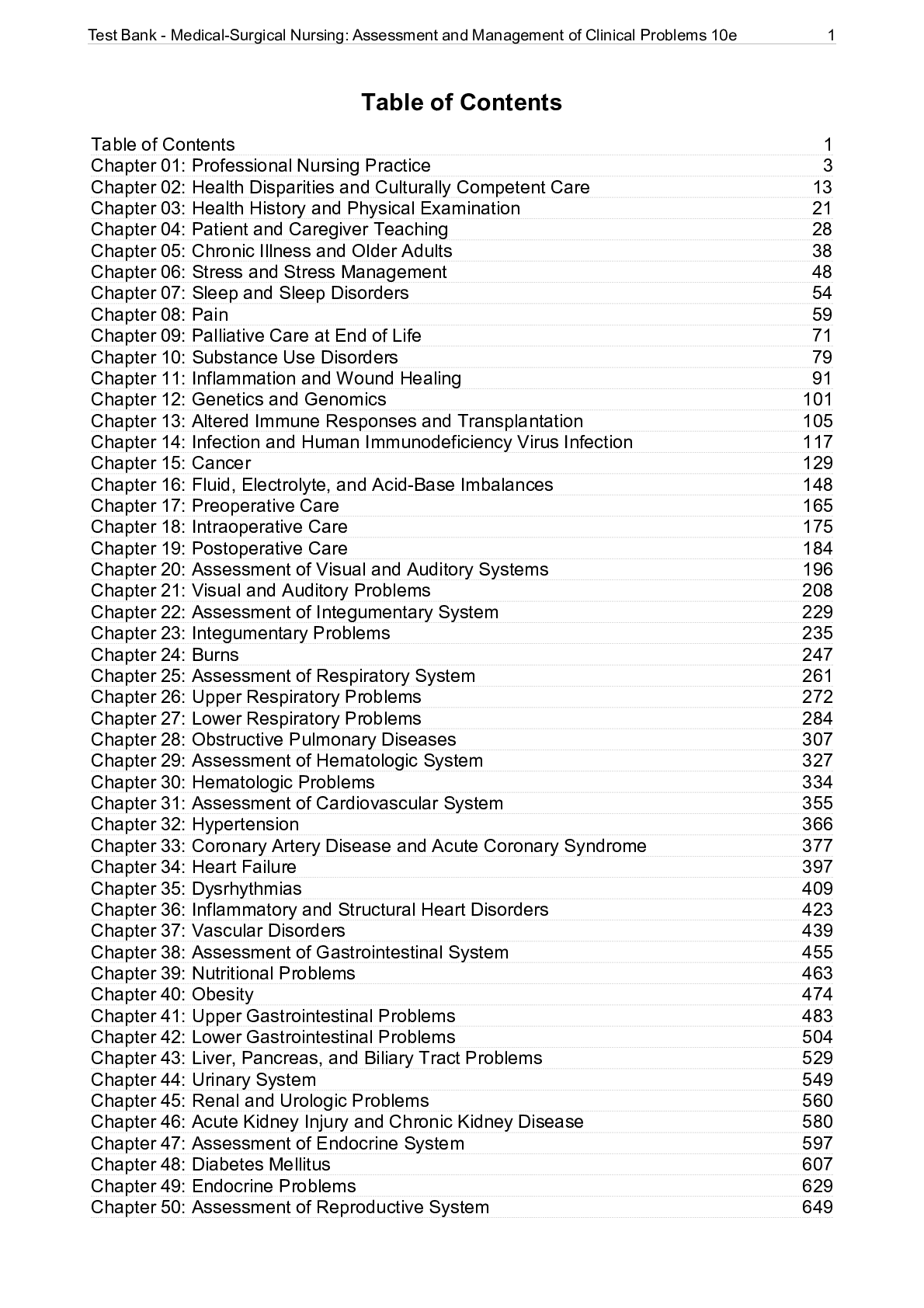
.png)

