*NURSING > QUESTIONS & ANSWERS > Med Surg Test Bank - Summary Primary Concepts Of Adult Nursing. Q&A and the Rationale (1386 Pages) (All)
Med Surg Test Bank - Summary Primary Concepts Of Adult Nursing. Q&A and the Rationale (1386 Pages)
Document Content and Description Below
Med Surg Test Bank - Summary Primary Concepts Of Adult Nursing Chapter 41: Management of Patients With Musculoskeletal Disorders 1. A nurse is caring for an adult patient diagnos... ed with a back strain. What health education should the nurse provide to this patient? A) Avoid lifting more than one-third of body weight without assistance. B) Focus on using back muscles efficiently when lifting heavy objects. C) Lift objects while holding the object a safe distance from the body. D) Tighten the abdominal muscles and lock the knees when lifting of an object. A The nurse will instruct the patient on the safe and correct way to lift objectsusing the strong quadriceps muscles of the thighs, with minimal use of the weak back muscles. To prevent recurrence of acute low back pain, the nurse may instruct the patient to avoid lifting more than one-third of his weight without help. The patient should be informed to place the feet a hip-width apart to provide a wide base of support, the person should bend the knees, tighten the abdominal muscles, and lift the object close to the body with a smooth motion, avoiding twisting and jerking. 2. A nurse is discussing conservative management of tendonitis with a patient. Which of the following may be an effective approach to managing tendonitis? A) Weight reduction B) Use of oral opioid analgesics C) Intermittent application of ice and heat D) Passive range of motion exercises C Conservative management of tendonitis includes rest of the extremity, intermittent ice and heat to the joint, and NSAIDs. Weight reduction may prevent future injuries but will not relieve existing tendonitis. Range-of-motion exercises may exacerbate pain. Opioids would not be considered a conservative treatment measure. 3. A patient presents at a clinic complaining of pain in his heel so bad that it inhibits his ability to walk. The patient is subsequently diagnosed with plantar fasciitis. This patients plan of care should include what intervention? A) Wrapping the affected area in lambs wool or gauze to relieve pressure B) Gently stretching the foot and the Achilles tendon C) Wearing open-toed shoes at all times D) Applying topical analgesic ointment to plantar surface each morning B Feedback: Plantar fasciitis leads to pain that is localized to the anterior medial aspect of the heel and diminishes with gentle stretching of the foot and Achilles tendon. Dressings of any kind are not of therapeutic benefit and analgesic ointments do not address the pathology of the problem. Open-toed shoes are of no particular benefit. A nurse is providing an educational class to a group of older adults at a community senior center. In an effort to prevent osteoporosis, the nurse should encourage participants to ensure that they consume the recommended adequate intake of what nutrients? Select all that apply. A) Vitamin B12 B) Potassium C) Calcitonin D) Calcium E) Vitamin D D, E Feedback: A diet rich in calcium and vitamin D protects against skeletal demineralization. Intake of vitamin B12and potassium does not directly influence the risk for osteoporosis. Calcitonin is not considered to be a dietary nutrient. 5. A nurse is providing a class on osteoporosis at the local seniors center. Which of the following statements related to osteoporosis is most accurate? A) Osteoporosis is categorized as a disease of the elderly. B) A nonmodifiable risk factor for osteoporosis is a persons level of activity. C) Secondary osteoporosis occurs in women after menopause. D) Slow discontinuation of corticosteroid therapy can halt the progression of the osteoporosis. D Feedback: When corticosteroid therapy is discontinued, the progression of osteoporosis is halted, but restoration of lost bone mass does not occur. Osteoporosis is not a disease of the elderly because its onset occurs earlier in life, when bone mass peaks and then begins to decline. A persons level of physical activity is a modifiable factor that influences peak bone mass. Lack of activity increases the risk for the development of osteoporosis. Primary osteoporosis occurs in women after menopause. 6. A nurse is teaching a patient with osteomalacia about the role of diet. What would be the best choice for breakfast for a patient with osteomalacia? A) Cereal with milk, a scrambled egg, and grapefruit B) Poached eggs with sausage and toast C) Waffles with fresh strawberries and powdered sugar D) A bagel topped with butter and jam with a side dish of grapes A Feedback: The best meal option is the one that contains the highest dietary sources of calcium and vitamin D. The best selection among those listed is cereal with milk, and eggs, as these foods contain calcium and vitamin D in a higher quantity over the other menu options. 7. A nurse is caring for a patient with Pagets disease and is reviewing the patients most recent laboratory values. Which of the following values is most characteristic of Pagets disease? A) An elevated level of parathyroid hormone and low calcitonin levels B) A low serum alkaline phosphatase level and a low serum calcium level C) An elevated serum alkaline phosphatase level and a normal serum calcium level D) An elevated calcitonin level and low levels of parathyroid hormone C Feedback: Patients with Pagets disease have normal blood calcium levels. Elevated serum alkaline phosphatase concentration and urinary hydroxyproline excretion reflect the increased osteoblastic activity associated with this condition. Alterations in PTH and calcitonin levels are atypical. 8. Which of the following patients should the nurse recognize as being at the highest risk for the development of osteomyelitis? A) A middle-age adult who takes ibuprofen daily for rheumatoid arthritis B) An elderly patient with an infected pressure ulcer in the sacral area C) A 17-year-old football player who had orthopedic surgery 6 weeks prior D) An infant diagnosed with jaundice B Feedback: Patients who are at high risk of osteomyelitis include those who are poorly nourished, elderly, and obese. The elderly patient with an infected sacral pressure ulcer is at the greatest risk for the development of osteomyelitis, as this patient has two risk factors: age and the presence of a soft-tissue infection that has the potential to extend into the bone. The patient with rheumatoid arthritis has one risk factor and the infant with jaundice has no identifiable risk factors. The patient 6 weeks postsurgery is beyond the usual window of time for the development of a postoperative surgical wound infection. 9. A nurse is caring for a patient with a bone tumor. The nurse is providing education to help the patient reduce the risk for pathologic fractures. What should the nurse teach the patient? A) Strive to achieve maximum weight-bearing capabilities. B) Gradually strengthen the affected muscles through weight training. C) Support the affected extremity with external supports such as splints. D) Limit reliance on assistive devices in order to build strength. C Feedback: During nursing care, the affected extremities must be supported and handled gently. External supports (splints) may be used for additional protection. Prescribed weight-bearing restrictions must be followed. Assistive devices should be used to strengthen the unaffected extremities. 10. A patient presents at a clinic complaining of back pain that goes all the way down the back of the leg to the foot. The nurse should document the presence of what type of pain? A) Bursitis B) Radiculopathy C) Sciatica D) Tendonitis C Feedback: Sciatica nerve pain travels down the back of the thigh to the foot of the affected leg. Bursitis is inflammation of a fluid-filled sac in a joint. Radiculopathy is disease of a nerve root. Tendonitis is inflammation of muscle tendons. 11. A patient tells the nurse that he has pain and numbness to his thumb, first finger, and second finger of the right hand. The nurse discovers that the patient is employed as an auto mechanic, and that the pain is increased while working. This may indicate that the patient could possibly have what health problem? A) Carpel tunnel syndrome B) Tendonitis C) Impingement syndrome D) Dupuytrens contracture A Feedback: Carpel tunnel syndrome may be manifested by numbness, pain, paresthesia, and weakness along the median nerve. Tendonitis is inflammation of muscle tendons. Impingement syndrome is a general term that describes all lesions that involve the rotator cuff of the shoulder. Dupuytrens contracture is a slowly progressive contracture of the palmar fascia. 12. A nurse is assessing a patient who reports a throbbing, burning sensation in the right foot. The patient states that the pain is worst during the day but notes that the pain is relieved with rest. The nurse should recognize the signs and symptoms of what health problem? A) Mortons neuroma B) Pescavus C) Hallux valgus D) Onychocryptosis A Feedback: Mortons neuroma is a swelling of the third (lateral) branch of the median plantar nerve, which causes a throbbing, burning pain, usually relieved with rest. Pescavus refers to a foot with an abnormally high arch and a fixed equinus deformity of the forefoot. Hallux valgus (bunion) is a deformity in which the great toe deviates laterally and there is a marked prominence of the medial aspect of the first metatarsal- phalangeal joint and exostosis. Onychocryptosis (ingrown toenail) occurs when the free edge of a nail plate penetrates the surrounding skin, laterally or anteriorly. 13. A nurse is reviewing the pathophysiology that may underlie a patients decreased bone density. What hormone should the nurse identify as inhibiting bone resorption and promoting bone formation? A) Estrogen B) Parathyroid hormone (PTH) C) Calcitonin D) Progesterone C Feedback: Calcitonin inhibits bone resorption and promotes bone formation, estrogen inhibits bone breakdown, and parathyroid increases bone resorption. Estrogen, which inhibits bone breakdown, decreases with aging. Parathyroid hormone (PTH) increases with aging, increasing bone turnover and resorption. Progesterone is the major naturally occurring human progestogen and plays a role in the female menstrual cycle. 14. A patient is undergoing diagnostic testing for osteomalacia. Which of the following laboratory results is most suggestive of this diagnosis? A) High chloride, calcium, and magnesium B) High parathyroid and calcitonin levels C) Low serum calcium and magnesium levels D) Low serum calcium and low phosphorus level D Feedback: Laboratory studies will reveal a low serum calcium and low phosphorus level. 15. An 80-year-old man in a long-term care facility has a chronic leg ulcer and states that the area has become increasingly painful in recent days. The nurse notes that the site is now swollen and warm to the touch. The patient should undergo diagnostic testing for what health problem? A) Osteomyelitis B) Osteoporosis C) Osteomalacia D) Septic arthritis A Feedback: When osteomyelitis develops from the spread of an adjacent infection, no signs of septicemia are present, but the area becomes swollen, warm, painful, and tender to touch. Osteoporosis is the most prevalent bone disease in the world. Osteomalacia is a metabolic bone disease characterized by inadequate mineralization of bone. Septicarthritis occurs when joints become infected through spread of infection from other parts of the body (hematogenous spread) or directly through trauma or surgical instrumentation. 16. A patient has returned to the unit after undergoing limb-sparing surgery to remove a metastatic bone tumor. The nurse providing postoperative care in the days following surgery assesses for what complication from surgery? A) Deficient fluid volume B) Delayed wound healing C) Hypocalcemia D) Pathologic fractures B Feedback: Delayed wound healing is a complication of surgery due to tissue trauma from the surgery. Nutritional deficiency is usually due to the effects of chemotherapy and radiation therapy, which may cause weight loss. Pathologic fractures are not a complication of surgery. 17. A nurse is caring for a patient who is 12 hours postoperative following foot surgery. The nurse assesses the presence of edema in the foot. What nursing measure will the nurse implement to control the edema? A) Elevate the foot on several pillows. B) Apply warm compresses intermittently to the surgical area. C) Administer a loop diuretic as ordered. D) Increase circulation through frequent ambulation. A Feedback: To control the edema in the foot of a patient who experienced foot surgery, the nurse will elevate the foot on several pillows when the patient is sitting or lying. Diuretic therapy is not an appropriate intervention for edema related to inflammation. Intermittent ice packs should be applied to the surgical area during the first 24 to 48 hours after surgery to control edema and provide some pain relief. Ambulation will gradually be resumed based on the guidelines provided by the surgeon. 18. A patient with diabetes is attending a class on the prevention of associated diseases. What action should the patient perform to reduce the risk of osteomyelitis? A) Increase calcium and vitamin intake. B) Perform meticulous foot care. C) Exercise 3 to 4 times weekly for at least 30 minutes. D) Take corticosteroids as ordered. B Feedback: Diabetic foot ulcers have a high potential for progressing to osteomyelitis. Meticulous foot care can help mitigate this risk. Corticosteroids can exacerbate the risk of osteomyelitis. Increased intake of calcium and vitamins as well as regular exercise are beneficial health promotion exercises, but they do not directly reduce the risk of osteomyelitis. 19. A nurse is planning the care of an older adult patient with osteomalacia. What action should the nurse recommend in order to promote vitamin D synthesis? A) Ensuring adequate exposure to sunlight B) Eating a low-purine diet C) Performing cardiovascular exercise while avoiding weight-bearing exercises D) Taking thyroid supplements as ordered A Feedback: Because sunlight is necessary for synthesizing vitamin D, patients should be encouraged to spend some time in the sun. A low-purine diet is not a relevant action and thyroid supplements do not directly affect bone function. Action must be taken to prevent fractures, but weight-bearing exercise within safe parameters is not necessarily contraindicated. 20. A patient presents to a clinic complaining of a leg ulcer that isnt healing; subsequent diagnostic testing suggests osteomyelitis. The nurse is aware that the most common pathogen to cause osteomyelitis is what? A) Staphylococcus aureus B) Proteus C) Pseudomonas D) Escherichia coli A Feedback: S. aureus causes over 50% of bone infections. Proteus, Pseudomonas, and E. coli are also causes, but to a lesser extent. 21. A nurse is providing care for a patient who has a recent diagnosis of Pagets disease. When planning this patients nursing care, interventions should address what nursing diagnoses? Select all that apply. A) Impaired Physical Mobility B) Acute Pain C) Disturbed Auditory Sensory Perception D) Risk for Injury E) Risk for Unstable Blood Glucose A, B, C, D Feedback: Patients with Pagets disease are at risk of decreased mobility, pain, hearing loss, and injuries resulting from decreased bone density. Pagets disease does not affect blood glucose levels. A nurse is caring for a patient who is being assessed following complaints of severe and persistent low back pain. The patient is scheduled for diagnostic testing in the morning. Which of the following are appropriate diagnostic tests for assessing low back pain? that apply. A) Computed tomography (CT) B) Angiography C) Magnetic resonance imaging (MRI) D) Ultrasound E) X-ray A, C, D, E Feedback: A variety of diagnostic tests can be used to address lower back pain, including CT, MRI, ultrasound, and X-rays. Angiography is not related to the etiology of back pain. 23. A nurse is reviewing the care of a patient who has a long history of lower back pain that has not responded to conservative treatment measures. The nurse should anticipate the administration of what drug? A) Calcitonin B) Prednisone C) Aspirin D) Cyclobenzaprine D Feedback: Short-term prescription muscle relaxants (e.g., cyclobenzaprine [Flexeril]) are effective in relieving acute low back pain. ASA is not normally used for pain control, due to its antiplatelet action and associated risk for bleeding. Calcitonin and corticosteroids are not used in the treatment of lower back pain. 24. A nurse is collaborating with the physical therapist to plan the care of a patient with osteomyelitis. What principle should guide the management of activity and mobility in this patient? A) Stress on the weakened bone must be avoided. B) Increased heart rate enhances perfusion and bone healing. C) Bed rest results in improved outcomes in patients with osteomyelitis. D) Maintenance of baseline ADLs is the primary goal during osteomyelitis treatment. A Feedback: The patient with osteomyelitis has bone that is weakened by the infective process and must be protected by avoidance of stress on the bone.This risk guides the choice of activity in a patient with osteomyelitis. Bed rest is not normally indicated, however. Maintenance of prediagnosis ADLs may be an unrealistic short-term goal for many patients. 25. A 32-year-old patient comes to the clinic complaining of shoulder tenderness, pain, and limited movement. Upon assessment the nurse finds edema. An MRI shows hemorrhage of the rotator cuff tendons and the patient is diagnosed with impingement syndrome. What action should the nurse recommend in order to promote healing? A) Support the affected arm on pillows at night. B) Take prescribed corticosteroids as ordered. C) Put the shoulder through its full range of motion 3 times daily. D) Keep the affected arm in a sling for 2 to 4 weeks. A Feedback: The patient should support the affected arm on pillows while sleeping to keep from turning onto the shoulder. Corticosteroids are not commonly prescribed and a sling is not normally necessary. ROM exercises are indicated, but putting the arm through its full ROM may cause damage during the healing process. 26. A patient presents at the clinic with complaints of morning numbness, cramping, and stiffness in his fourth and fifth fingers. What disease process should the nurse suspect? A) Tendonitis B) A ganglion C) Carpal tunnel syndrome D) Dupuytrens disease D Feedback: In cases of Dupuytrens disease, the patient may experience dull, aching discomfort, morning numbness, cramping, and stiffness in the affected fingers. This condition starts in one hand, but eventually both hands are affected. This clinical scenario does not describe tendonitis, a ganglion, or carpal tunnel syndrome. 27. A patients electronic health record notes that the patient has hallux valgus. What signs and symptoms would the nurse expect this patient to manifest? A) Deviation of a great toe laterally B) Abnormal flexion of the great toe C) An exaggerated arch of the foot D) Fusion of the toe joints A Feedback: A deformity in which the great toe deviates laterally and there is a marked prominence of the medial aspect of the first metatarsal-phalangeal joint and exostosis is referred to as hallux valgus (bunion). Hallux valgus does not result in abnormal flexion, abnormalities of the arch, or joint fusion. 28. An older adult womans current medication regimen includes alendronate (Fosamax). What outcome would indicate successful therapy? A) Increased bone mass B) Resolution of infection C) Relief of bone pain D) Absence of tumor spread A Feedback: Bisphosphonates such as Fosamax increase bone mass and decrease bone loss by inhibiting osteoclast function. These drugs do not treat infection, pain, or tumors. 29. A nurse is caring for a patient who is being treated in the hospital for a spontaneous vertebral fracture related to osteoporosis. The nurse should address the nursing diagnosis of Acute Pain Related to Fracture by implementing what intervention? A) Maintenance of high Fowlers positioning whenever possible B) Intermittent application of heat to the patients back C) Use of a pressure-reducing mattress D) Passive range of motion exercises B Feedback: Intermittent local heat and back rubs promote muscle relaxation following osteoporotic vertebral fractures. High Fowlers positioning is likely to exacerbate pain. The mattress must be adequately supportive, but pressure reduction is not necessarily required. Passive range of motion exercises to the back would cause pain and impair healing. 30. A patient has been admitted to the hospital with a spontaneous vertebral fracture related to osteoporosis. Which of the following nursing diagnoses must be addressed in the plan of care? A) Risk for Aspiration Related to Vertebral Fracture B) Constipation Related to Vertebral Fracture C) Impaired Swallowing Related to Vertebral Fracture D) Decreased Cardiac Output Related to Vertebral Fracture B Feedback: Constipation is a problem related to immobility and medications used to treat vertebral fractures. The patients risks of aspiration, dysphagia, and decreased cardiac output are not necessarily heightened. 31. A nursing educator is reviewing the risk factors for osteoporosis with a group of recent graduates. What risk factor of the following should the educator describe? A) Recurrent infections and prolonged use of NSAIDs B) High alcohol intake and low body mass index C) Small frame, female gender, and Caucasian ethnicity D) Male gender, diabetes, and high protein intake C Feedback: Small-framed, nonobese Caucasian women are at greatest risk for osteoporosis. Diabetes, high protein intake, alcohol use, and infections are not among the most salient risk factors for osteoporosis. 32. A nurse is providing care for a patient who has osteomalacia. What major goal will guide the choice of medical and nursing interventions? A) Maintenance of skin integrity B) Prevention of bone metastasis C) Maintenance of adequate levels of activated vitamin D D) Maintenance of adequate parathyroid hormone function C Feedback: The primary defect in osteomalacia is a deficiency of activated vitamin D, which promotes calcium absorption from the gastrointestinal tract and facilitates mineralization of bone. Interventions are aimed at resolving the processes underlying this deficiency. Maintenance of skin integrity is important, but is not the primary goal in care. Osteomalacia is not a malignant process. Overproduction (not underproduction) of PTH can cause the disease. A patient has been admitted to the medical unit for the treatment of Pagets disease. When reviewing the medication administration record, the nurse should anticipate what medications? Select all that apply. A) Calcitonin B) Bisphosphonates C) Alkaline phosphatase D) Calcium gluconate E) Estrogen A, B Feedback: Bisphosphonates are the cornerstone of Paget therapy in that they stabilize the rapid bone turnover. Calcitonin is also used because it retards bone resorption by decreasing the number and availability of osteoclasts. Alkaline phosphatase is a naturally occurring enzyme, not a drug. Calcium gluconate and estrogen are not used in the treatment of Pagets disease. The health care team is caring for a patient with osteomalacia. It has been determined that the osteomalacia is caused by malabsorption. What is the usual treatment for osteomalacia caused by malabsorption? A) Supplemental calcium and increased doses of vitamin D B) Exogenous parathyroid hormone and multivitamins C) Colony-stimulating factors and calcitonin D) Supplemental potassium and pancreatic enzymes A Feedback: If osteomalacia is caused by malabsorption, increased doses of vitamin D, along with supplemental calcium, are usually prescribed. 35. A patient with diabetes has been diagnosed with osteomyelitis. The nurse notes that the patients right foot is pale and mottled, cool to touch, with a capillary refill of greater than 3 seconds. The nurse should suspect what type of osteomyelitis? A) Hematogenous osteomyelitis B) Osteomyelitis with vascular insufficiency C) Contiguous-focus osteomyelitis D) Osteomyelitis with muscular deterioration B Feedback: Osteomyelitis is classified as hematogenous osteomyelitis (i.e., due to blood-borne spread of infection); contiguous-focus osteomyelitis, from contamination from bone surgery, open fracture, or traumatic injury (e.g., gunshot wound); and osteomyelitis with vascular insufficiency, seen most commonly among patients with diabetes and peripheral vascular disease, most commonly affecting the feet. Osteomyelitis with muscular deterioration does not exist. 36. An orthopedic nurse is caring for a patient who is postoperative day one following foot surgery. What nursing intervention should be included in the patients subsequent care? A) Dressing changes should not be performed unless there are clear signs of infection. B) The surgical site can be soaked in warm bath water for up to 5 minutes. C) The surgical site should be cleansed with hydrogen peroxide once daily. D) The foot should be elevated in order to prevent edema. D Feedback: Pain experienced by patients who undergo foot surgery is related to inflammation and edema. To control the anticipated edema, the foot should be elevated on several pillows when the patient is sitting or lying. Regular dressing changes are performed and the wound should be kept dry. Hydrogen peroxide is not used to cleanse surgical wounds. 37. A nurse is providing discharge teaching for a patient who underwent foot surgery. The nurse is collaborating with the occupational therapist and discussing the use of assistive devices. On what variables does the choice of assistive devices primarily depend? A) Patients general condition, balance, and weight-bearing prescription B) Patients general condition, strength, and gender C) Patients motivation, age, and weight-bearing prescription D) Patients occupation, motivation, and age A Feedback: Assistive devices (e.g., crutches, walker) may be needed. The choice of the devices depends on the patients general condition and balance, and on the weight-bearing prescription. The patients strength, motivation, and weight restrictions are not what the choice of assistive devices is based on. 38. A patient has come to the clinic for a routine annual physical. The nurse practitioner notes a palpable, painless projection of bone at the patients shoulder. The projection appears to be at the distal end of the humerus. The nurse should suspect the presence of which of the following? A) Osteomyelitis B) Osteochondroma C) Osteomalacia D) Pagets disease B Feedback: Osteochondroma is the most common benign bone tumor. It usually occurs as a large projection of bone at the end of long bones (at the knee or shoulder). Osteomyelitis, osteomalacia, and Pagets disease do not involve the development of excess bone tissue. 39. An elderly female with osteoporosis has been hospitalized. Prior to discharge, when teaching the patient, the nurse should include information about which major complication of osteoporosis? A) Bone fracture B) Loss of estrogen C) Negative calcium balance D) Dowagers hump A Feedback: Bone fracture is a major complication of osteoporosis that results when loss of calcium and phosphate increases the fragility of bones. Estrogen deficiencies result from menopause, not osteoporosis. Calcium and vitamin D supplements may be used to support normal bone metabolism, but a negative calcium balance is not a complication of osteoporosis. Dowagers hump results from bone fractures. It develops when repeated vertebral fractures increase spinal curvature. 40. An older adult patient sought care for the treatment of a swollen, painful knee joint. Diagnostic imaging and culturing of synovial fluid resulted in a diagnosis of septic arthritis. The nurse should prioritize which of the following aspects of care? A) Administration of oral and IV corticosteroids as ordered B) Prevention of falls and pathologic fractures C) Maintenance of adequate serum levels of vitamin D D) Intravenous administration of antibiotics D Feedback: IV antibiotics are the major treatment modality for septic arthritis; the nurse must ensure timely administration of these drugs. Corticosteroids are not used to treat septic arthritis and vitamin D levels are not necessarily affected. Falls prevention is important, but septic arthritis does not constitute the same fracture risk as diseases with decreased bone density. Chapter 42: Management of Patients With Musculoskeletal Trauma 1. A nurse admits a patient who has a fracture of the nose that has resulted in a skin tear and involvement of the mucous membranes of the nasal passages. The orthopedic nurse is aware that this description likely indicates which type of fracture? A) Compression B) Compound C) Impacted D) Transverse B Feedback: A compound fracture involves damage to the skin or mucous membranes and is also called an open fracture. A compression fracture involves compression of bone and is seen in vertebral fractures. An impacted fracture occurs when a bone fragment is driven into another bone fragment. A transverse fracture occurs straight across the bone shaft. 2. A patient has sustained a long bone fracture and the nurse is preparing the patients care plan. Which of the following should the nurse include in the care plan? A) Administer vitamin D and calcium supplements as ordered. B) Monitor temperature and pulses of the affected extremity. C) Perform passive range of motion exercises as tolerated. D) Administer corticosteroids as ordered. B Feedback: The nurse should include monitoring for sufficient blood supply by assessing the color, temperature, and pulses of the affected extremity. Weight-bearing exercises are encouraged, but passive ROM exercises have the potential to cause pain and inhibit healing. Corticosteroids, vitamin D, and calcium are not normally administered. 3. A nurses assessment of a patients knee reveals edema, tenderness, muscle spasms, and ecchymosis. The patient states that 2 days ago he ran 10 miles and now it really hurts to stand up. The nurse should plan care based on the belief that the patient has experienced what? A) A first-degree strain B) A second-degree strain C) A first-degree sprain D) A second-degree sprain B Feedback: A second-degree strain involves tearing of muscle fibers and is manifested by notable loss of load- bearing strength with accompanying edema, tenderness, muscle spasm, and ecchymosis. A first-degree strain reflects tearing of a few muscle fibers and is accompanied by minor edema, tenderness, and mild muscle spasm, without noticeable loss of function. However, this patient states a loss of function. A sprain normally involves twisting, which is inconsistent with the patients overuse injury. 4. A nurse is preparing to discharge a patient from the emergency department after receiving treatment for an ankle sprain. While providing discharge education, the nurse should encourage which of the following? A) Apply heat for the first 24 to 48 hours after the injury. B) Maintain the ankle in a dependent position. C) Exercise hourly by performing rotation exercises of the ankle. D) Keep an elastic compression bandage on the ankle. D Feedback: Treatment of a sprain consists of resting and elevating the affected part, applying cold, and using a compression bandage. After the acute inflammatory stage (usually 24 to 48 hours after injury), heat may be applied intermittently. Rotation exercises would likely be painful. 5. A nurse is writing a care plan for a patient admitted to the emergency department (ED) with an open fracture. The nurse will assign priority to what nursing diagnosis for a patient with an open fracture of the radius? A) Risk for Infection B) Risk for Ineffective Role Performance C) Risk for Perioperative Positioning Injury D) Risk for Powerlessness A Feedback: The patient has a significant risk for osteomyelitis and tetanus due to the fact that the fracture is open. Powerlessness and ineffective role performance are psychosocial diagnoses that may or may not apply, and which would be superseded by immediate physiologic threats such as infection. Surgical positioning injury is not plausible, since surgery is not likely indicated. 6. A nurse is caring for a patient who has suffered a hip fracture and who will require an extended hospital stay. The nurse should ensure that the patient does which of the following in order to prevent common complications associated with a hip fracture? A) Avoid requesting analgesia unless pain becomes unbearable. B) Use supplementary oxygen when transferring or mobilizing. C) Increase fluid intake and perform prescribed foot exercises. D) Remain on bed rest for 14 days or until instructed by the orthopedic surgeon. C Feedback: Deep vein thrombosis (DVT) is among the most common complications related to a hip fracture. To prevent DVT, the nurse encourages intake of fluids and ankle and foot exercises. The patient should not be told to endure pain; a proactive approach to pain control should be adopted. While respiratory complications commonly include atelectasis and pneumonia, the use of deep-breathing exercises, changes in position at least every 2 hours, and the use of incentive spirometry help prevent the respiratory complications more than using supplementary oxygen. Bed rest may be indicated in the short term, but is not normally required for 14 days. 7. A nurse is caring for a patient who has suffered an unstable thoracolumbar fracture. Which of the following is the priority during nursing care? A) Preventing infection B) Maintaining spinal alignment C) Maximizing function D) Preventing increased intracranial pressure B Feedback: Patients with an unstable fracture must have their spine in alignment at all times in order to prevent neurologic damage. This is a greater threat, and higher priority, than promoting function and preventing infection, even though these are both valid considerations. Increased ICP is not a high risk. 8. The patient scheduled for a Syme amputation is concerned about the ability to eventually stand on the amputated extremity. How should the nurse best respond to the patients concern? A) You will eventually be able to withstand full weight-bearing after the amputation. B) You will have minimal weight-bearing on this extremity but youll be taught how to use an assistive device. C) You likely will not be able to use this extremity but you will receive teaching on use of a wheelchair. D) You will be fitted for a prosthesis which may or may not allow you to walk. A Feedback: Syme amputation (modified ankle disarticulation amputation) is performed most frequently for extensive foot trauma and produces a painless, durable extremity end that can withstand full weight-bearing. Therefore, each of the other teaching statements is incorrect. 9. A patient with a simple arm fracture is receiving discharge education from the nurse. What would the nurse instruct the patient to do? A) Elevate the affected extremity to shoulder level when at rest. B) Engage in exercises that strengthen the unaffected muscles. C) Apply topical anesthetics to accessible skin surfaces as needed. D) Avoid using analgesics so that further damage is not masked. B Feedback: The nurse will encourage the patient to engage in exercises that strengthen the unaffected muscles. Comfort measures may include appropriate use of analgesics and elevation of the affected extremity to the heart level. Topical anesthetics are not typically used. 10. Six weeks after an above-the-knee amputation (AKA), a patient returns to the outpatient office for a routine postoperative checkup. During the nurses assessment, the patient reports symptoms of phantom pain. What should the nurse tell the patient to do to reduce the discomfort of the phantom pain? A) Apply intermittent hot compresses to the area of the amputation. B) Avoid activity until the pain subsides. C) Take opioid analgesics as ordered. D) Elevate the level of the amputation site. C Feedback: Opioid analgesics may be effective in relieving phantom pain. Heat, immobility, and elevation are not noted to relieve this form of pain. A nurse is caring for a patient who had a right below-the-knee amputation (BKA). The nurse recognizes the importance of implementing measures that focus on preventing flexion contracture of the hip and maintaining proper positioning. Which of the following measures will best achieve these goals? A) Encouraging the patient to turn from side to side and to assume a prone position B) Initiating ROM exercises of the hip and knee 10 to 12 weeks after the amputation C) Minimizing movement of the flexor muscles of the hip D) Encouraging the patient to sit in a chair for at least 8 hours a day A Feedback: The nurse encourages the patient to turn from side to side and to assume a prone position, if possible, to stretch the flexor muscles and to prevent flexion contracture of the hip. Postoperative ROM exercises are started early, because contracture deformities develop rapidly. ROM exercises include hip and knee exercises for patients with BKAs. The nurse also discourages sitting for prolonged periods of time. 12. A nurse is preparing to discharge an emergency department patient who has been fitted with a sling to support her arm after a clavicle fracture. What should the nurse instruct the patient to do? A) Elevate the arm above the shoulder 3 to 4 times daily. B) Avoid moving the elbow, wrist, and fingers until bone remodeling is complete. C) Engage in active range of motion using the affected arm. D) Use the arm for light activities within the range of motion. D Feedback: A patient with a clavicle fracture may use a sling to support the arm and relieve the pain. The patient may be permitted to use the arm for light activities within the range of comfort. The patient should not elevate the arm above the shoulder level until the ends of the bones have united, but the nurse should encourage the patient to exercise the elbow, wrist, and fingers. 13. The orthopedic nurse should assess for signs and symptoms of Volkmanns contracture if a patient has fractured which of the following bones? A) Femur B) Humerus C) Radial head D) Clavicle B Feedback: The most serious complication of a supracondylar fracture of the humerus is Volkmanns ischemic contracture, which results from antecubital swelling or damage to the brachial artery. This complication is specific to humeral fractures. An emergency department nurse is assessing a 17-year-old soccer player who presented with a knee injury. The patients description of the injury indicates that his knee was struck medially while his foot was on the ground. The nurse knows that the patient likely has experienced what injury? A) Lateral collateral ligament injury B) Medial collateral ligament injury C) Anterior cruciate ligament injury D) Posterior cruciate ligament injury A Feedback: When the knee is struck medially, damage may occur to the lateral collateral ligament. If the knee is struck laterally, damage may occur to the medial collateral ligament. The ACL and PCL are not typically injured in this way. 15. A school nurse is assessing a student who was kicked in the shin during a soccer game. The area of the injury has become swollen and discolored. The triage nurse recognizes that the patient has likely sustained what? A) Sprain B) Strain C) Contusion D) Dislocation C Feedback: A contusion is a soft-tissue injury that results in bleeding into soft tissues, creating a hematoma and ecchymosis. A sprain is an injury to ligaments caused by wrenching or twisting. A strain is a muscle pull from overuse, overstretching, or excessive stress. A dislocation is a condition in which the articular surfaces of the bones forming a joint are no longer in anatomic contact. Because the injury is not at the site of a joint, the patient has not experienced a sprain, strain, or dislocation. 16. Radiographs of a boys upper arm show that the humerus appears to be fractured on one side and slightly bent on the other. This diagnostic result suggests what type of fracture? A) Impacted B) Compound C) Compression D) Greenstick D Feedback: Greenstick fractures are an incomplete fracture that results in the bone being broken on one side, while the other side is bent. This is not characteristic of an impacted, compound, or compression fracture. 17. A nurse is performing a shift assessment on an elderly patient who is recovering after surgery for a hip fracture. The nurse notes that the patient is complaining of chest pain, has an increased heart rate, and increased respiratory rate. The nurse further notes that the patient is febrile and hypoxic, coughing, and producing large amounts of thick, white sputum. The nurse recognizes that this is a medical emergency and calls for assistance, recognizing that this patient is likely demonstrating symptoms of what complication? A) Avascular necrosis of bone B) Compartment syndrome C) Fat embolism syndrome D) Complex regional pain syndrome C Feedback: Fat embolism syndrome occurs most frequently in young adults and elderly patients who experience fractures of the proximal femur (i.e., hip fracture). Presenting features of fat embolism syndrome include hypoxia, tachypnea, tachycardia, and pyrexia. The respiratory distress response includes tachypnea, dyspnea, wheezes, precordial chest pain, cough, large amounts of thick, white sputum, and tachycardia. Avascular necrosis (AVN) occurs when the bone loses its blood supply and dies. This does not cause coughing. Complex regional pain syndrome does not have cardiopulmonary involvement. 18. A young patient is being treated for a femoral fracture suffered in a snowboarding accident. The nurses most recent assessment reveals that the patient is uncharacteristically confused. What diagnostic test should be performed on this patient? A) Electrolyte assessment B) Electrocardiogram C) Arterial blood gases D) Abdominal ultrasound C Feedback: Subtle personality changes, restlessness, irritability, or confusion in a patient who has sustained a fracture are indications for immediate arterial blood gas studies due to the possibility of fat embolism syndrome. This assessment finding does not indicate an immediate need for electrolyte levels, an ECG, or abdominal ultrasound. 19. Which of the following is the most appropriate nursing intervention to facilitate healing in a patient who has suffered a hip fracture? A) Administer analgesics as required. B) Place a pillow between the patients legs when turning. C) Maintain prone positioning at all times. D) Encourage internal and external rotation of the affected leg. B Feedback: Placing a pillow between the patients legs when turning prevents adduction and supports the patients legs. Administering analgesics addresses pain but does not directly protect bone remodeling and promote healing. Rotation of the affected leg can cause dislocation and must be avoided. Prone positioning does not need to be maintained at all times. 20. A nurse is planning the care of an older adult patient who will soon be discharged home after treatment for a fractured hip. In an effort to prevent future fractures, the nurse should encourage which of the following? Select all that apply. A) Regular bone density testing B) A high-calcium diet C) Use of falls prevention precautions D) Use of corticosteroids as ordered E) Weight-bearing exercise A, B, C, E Feedback: Health promotion measures after an older adults hip fracture include weight-bearing exercise, promotion of a healthy diet, falls prevention, and bone density testing. Corticosteroids have the potential to reduce bone density and increase the risk for fractures. 21. A patient is brought to the emergency department by ambulance after stepping in a hole and falling. While assessing him the nurse notes that his right leg is shorter than his left leg; his right hip is noticeably deformed and he is in acute pain. Imaging does not reveal a fracture. Which of the following is the most plausible explanation for this patients signs and symptoms? A) Subluxated right hip B) Right hip contusion C) Hip strain D) Traumatic hip dislocation D Feedback: Signs and symptoms of a traumatic dislocation include acute pain, change in positioning of the joint, shortening of the extremity, deformity, and decreased mobility. A subluxation would cause moderate deformity, or possibly no deformity. A contusion or strain would not cause obvious deformities. 22. An emergency department patient is diagnosed with a hip dislocation. The patients family is relieved that the patient has not suffered a hip fracture, but the nurse explains that this is still considered to be a medical emergency. What is the rationale for the nurses statement? A) The longer the joint is displaced, the more difficult it is to get it back in place. B) The patients pain will increase until the joint is realigned. C) Dislocation can become permanent if the process of bone remodeling begins. D) Avascular necrosis may develop at the site of the dislocation if it is not promptly resolved. D Feedback: If a dislocation or subluxation is not reduced immediately, avascular necrosis (AVN) may develop. Bone remodeling does not take place because a fracture has not occurred. Realignment does not become more difficult with time and pain would subside with time, not become worse. 23. The surgical nurse is admitting a patient from postanesthetic recovery following the patients below-the- knee amputation. The nurse recognizes the patients high risk for postoperative hemorrhage and should keep which of the following at the bedside? A) A tourniquet B) A syringe preloaded with vitamin K C) A unit of packed red blood cells, placed on ice D) A dose of protamine sulfate A Feedback: Immediate postoperative bleeding may develop slowly or may take the form of massive hemorrhage resulting from a loosened suture. A large tourniquet should be in plain sight at the patients bedside so that, if severe bleeding occurs, it can be applied to the residual limb to control the hemorrhage. PRBCs cannot be kept at the bedside. Vitamin K and protamine sulfate are antidotes to warfarin and heparin, but are not administered to treat active postsurgical bleeding. 24. An elite high school football player has been diagnosed with a shoulder dislocation. The patient has been treated and is eager to resume his role on his team, stating that he is not experiencing pain. What should the nurse emphasize during health education? A) The need to take analgesia regardless of the short-term absence of pain B) The importance of adhering to the prescribed treatment and rehabilitation regimen C) The fact that he has a permanently increased risk of future shoulder dislocations D) The importance of monitoring for intracapsular bleeding once he resumes playing B Feedback: Patients who have experienced sports-related injuries are often highly motivated to return to their previous level of activity. Adherence to restriction of activities and gradual resumption of activities needs to be reinforced. Appropriate analgesia use must be encouraged, but analgesia does not necessarily have to be taken in the absence of pain. If healing is complete, the patient does not likely have a greatly increased risk of reinjury. Dislocations rarely cause bleeding after the healing process. 25. A patient has presented to the emergency department with an injury to the wrist. The patient is diagnosed with a third-degree strain. Why would the physician order an x-ray of the wrist? A) Nerve damage is associated with third-degree strains. B) Compartment syndrome is associated with third-degree strains. C) Avulsion fractures are associated with third-degree strains. D) Greenstick fractures are associated with third-degree strains. C Feedback: An x-ray should be obtained to rule out bone injury, because an avulsion fracture (in which a bone fragment is pulled away from the bone by a tendon) may be associated with a third-degree strain. Nerve damage, compartment syndrome, and greenstick fractures are not associated with third-degree strains. 26. A 20 year-old is brought in by ambulance to the emergency department after being involved in a motorcycle accident. The patient has an open fracture of his tibia. The wound is highly contaminated and there is extensive soft-tissue damage. How would this patients fracture likely be graded? A) Grade I B) Grade II C) Grade III D) Grade IV C Feedback: Open fractures are graded according to the following criteria. Grade I is a clean wound less than 1 cm long. Grade II is a larger wound without extensive soft-tissue damage. Grade III is highly contaminated, has extensive soft-tissue damage, and is the most severe. There is no grade IV fracture. 27. A 25-year-old man is involved in a motorcycle accident and injures his arm. The physician diagnoses the man with an intra-articular fracture and splints the injury. The nurse implements the teaching plan developed for this patient. What sequela of intra-articular fractures should the nurse describe regarding this patient? A) Post-traumatic arthritis B) Fat embolism syndrome (FES) C) Osteomyelitis D) Compartment syndrome A Feedback: Intra-articular fractures often lead to post-traumatic arthritis. Research does not indicate a correlation between intra-articular fractures and FES, osteomyelitis, or compartment syndrome. 28. A nurse is planning the care of a patient with osteomyelitis that resulted from a diabetic foot ulcer. The patient requires a transmetatarsal amputation. When planning the patients postoperative care, which of the following nursing diagnoses should the nurse most likely include in the plan of care? A) Ineffective Thermoregulation B) Risk-Prone Health Behavior C) Disturbed Body Image D) Deficient Diversion Activity C Feedback: Amputations present a serious threat to any patients body image. None of the other listed diagnoses is specifically associated with amputation. 29. A patient is admitted to the orthopedic unit with a fractured femur after a motorcycle accident. The patient has been placed in traction until his femur can be rodded in surgery. For what early complications should the nurse monitor this patient? Select all that apply. A) Systemic infection B) Complex regional pain syndrome C) Deep vein thrombosis D) Compartment syndrome E) Fat embolism C, D, E Feedback: Early complications include shock, fat embolism, compartment syndrome, and venous thromboemboli (deep vein thrombosis [DVT], pulmonary embolism [PE]). Infection and CRPS are later complications of fractures. 30. A patient has come to the orthopedic clinic for a follow-up appointment 6 weeks after fracturing his ankle. Diagnostic imaging reveals that bone union is not taking place. What factor may have contributed to this complication? A) Inadequate vitamin D intake B) Bleeding at the injury site C) Inadequate immobilization D) Venous thromboembolism (VTE) C Feedback: Inadequate fracture immobilization can delay or prevent union. A short-term vitamin D deficiency would not likely prevent bone union. VTE is a serious complication but would not be a cause of nonunion. Similarly, bleeding would not likely delay union. 31. An older adult patient has fallen in her home and is brought to the emergency department by ambulance with a suspected fractured hip. X-rays confirm a fracture of the left femoral neck. When planning assessments during the patients presurgical care, the nurse should be aware of the patients heightened risk of what complication? A) Osteomyelitis B) Avascular necrosis C) Phantom pain D) Septicemia B Feedback: Fractures of the neck of the femur may damage the vascular system that supplies blood to the head and the neck of the femur, and the bone may become ischemic. For this reason, AVN is common in patients with femoral neck fractures. Infections are not immediate complications and phantom pain applies to patients with amputations, not hip fractures. 32. A patient is being treated for a fractured hip and the nurse is aware of the need to implement interventions to prevent muscle wasting and other complications of immobility. What intervention best addresses the patients need for exercise? A) Performing gentle leg lifts with both legs B) Performing massage to stimulate circulation C) Encouraging frequent use of the overbed trapeze D) Encouraging the patient to log roll side to side once per hour C Feedback: The patient is encouraged to exercise as much as possible by means of the overbed trapeze. This device helps strengthen the arms and shoulders in preparation for protected ambulation. Independent logrolling may result in injury due to the location of the fracture. Leg lifts would be contraindicated for the same reason. Massage by the nurse is not a substitute for exercise. 33. A patient who has had an amputation is being cared for by a multidisciplinary rehabilitation team. What is the primary goal of this multidisciplinary team? A) Maximize the efficiency of care B) Ensure that the patients health care is holistic C) Facilitate the patients adjustment to a new body image D) Promote the patients highest possible level of function D Feedback: The multidisciplinary rehabilitation team helps the patient achieve the highest possible level of function and participation in life activities. The team is not primarily motivated by efficiency, the need for holistic care, or the need to foster the patients body image, despite the fact that each of these are valid goals. 34. A rehabilitation nurse is working with a patient who has had a below-the-knee amputation. The nurse knows the importance of the patients active participation in self-care. In order to determine the patients ability to be an active participant in self-care, the nurse should prioritize assessment of what variable? A) The patients attitude B) The patients learning style C) The patients nutritional status D) The patients presurgical level of function A Feedback: Amputation of an extremity affects the patients ability to provide adequate self-care. The patient is encouraged to be an active participant in self-care. The patient and the nurse need to maintain positive attitudes and to minimize fatigue and frustration during the learning process. Balanced nutrition and the patients learning style are important variables in the rehabilitation process but the patients attitude is among the most salient variables. The patients presurgical level of function may or may not affect participation in rehabilitation. 35. The nurse is providing care for a patient who has had a below-the-knee amputation. The nurse enters the patients room and finds him resting in bed with his residual limb supported on pillow. What is the nurses most appropriate action? A) Inform the surgeon of this finding. B) Explain the risks of flexion contracture to the patient. C) Transfer the patient to a sitting position. D) Encourage the patient to perform active ROM exercises with the residual limb. B Feedback: The residual limb should not be placed on a pillow, because a flexion contracture of the hip may result. There is no acute need to contact the patients surgeon. Encouraging exercise or transferring the patient does not address the risk of flexion contracture. A patient has returned to the postsurgical unit from the PACU after an above-the-knee amputation of the right leg. Results of the nurses initial postsurgical assessment were unremarkable but the patient has called out. The nurse enters the room and observes copious quantities of blood at the surgical site. What should be the nurses initial action? A) Apply a tourniquet. B) Elevate the residual limb. C) Apply sterile gauze. D) Call the surgeon. A Feedback: The nurse should apply a tourniquet in the event of postsurgical hemorrhage. Elevating the limb and applying sterile gauze are likely insufficient to stop the hemorrhage. The nurse should attempt to control the immediate bleeding before contacting the surgeon. 37. A nurse in a busy emergency department provides care for many patients who present with contusions, strains, or sprains. Treatment modalities that are common to all of these musculoskeletal injuries include which of the following? Select all that apply. A) Massage B) Applying ice C) Compression dressings D) Resting the affected extremity E) Corticosteroids F) Elevating the injured limb B, C, D, F Feedback: Treatment of contusions, strains, and sprains consists of resting and elevating the affected part, applying cold, and using a compression bandage. Massage and corticosteroids are not used to treat these injuries. 38. A patient who has undergone a lower limb amputation is preparing to be discharged home. What outcome is necessary prior to discharge? A) Patient can demonstrate safe use of assistive devices. B) Patient has a healed, nontender, nonadherent scar. C) Patient can perform activities of daily living independently. D) Patientis free of pain. A Feedback: A patient should be able to use assistive devices appropriately and safely prior to discharge. Scar formation will not be complete at the time of hospital discharge. It is anticipated that the patient will require some assistance with ADLs postdischarge. Pain should be well managed, but may or may not be wholly absent. An older adult patient experienced a fall and required treatment for a fractured hip on the orthopedic unit. Which of the following are contributory factors to the incidence of falls and fractured hips among the older adult population? Select all that apply. A) Loss of visual acuity B) Adverse medication effects C) Slowed reflexes D) Hearing loss E) Muscle weakness A, B, C, E Feedback: Older adults are generally vulnerable to falls and have a high incidence of hip fracture. Weak quadriceps muscles, medication effects, vision loss, and slowed reflexes are among the factors that contribute to the incidence of falls. Decreased hearing is not noted to contribute to the incidence of falls. 40. A patient was fitted with an arm cast after fracturing her humerus. Twelve hours after the application of the cast, the patient tells the nurse that her arm hurts. Analgesics do not relieve the pain. What would be the most appropriate nursing action? A) Prepare the patient for opening or bivalving of the cast. B) Obtain an order for a different analgesic. C) Encourage the patient to wiggle and move the fingers. D) Petal the edges of the patients cast. A Feedback: Acute compartment syndrome involves a sudden and severe decrease in blood flow to the tissues distal to an area of injury that results in ischemic necrosis if prompt, decisive intervention does not occur. Removing or bivalving the cast is necessary to relieve pressure. Ordering different analgesics does not address the underlying problem. Encouraging the patient to move the fingers or perform range-of-motion exercises will not treat or prevent compartment syndrome. Petaling the edges of a cast with tape prevents abrasions and skin breakdown, not compartment syndrome. Chapter 43: Assessment of Digestive and Gastrointestinal Function 1. A nurse is caring for a patient who is scheduled for a colonoscopy and whose bowel preparation will include polyethylene glycol electrolyte lavage prior to the procedure. The presence of what health problem would contraindicate the use of this form of bowel preparation? A) Inflammatory bowel disease B) Intestinal polyps C) Diverticulitis D) Colon cancer A Feedback: The use of a lavage solution is contraindicated in patients with intestinal obstruction or inflammatory bowel disease. It can safely be used with patients who have polyps, colon cancer, or diverticulitis. 2. A nurse is promoting increased protein intake to enhance a patients wound healing. The nurse knows that enzymes are essential in the digestion of nutrients such as protein. What is the enzyme that initiates the digestion of protein? A) Pepsin B) Intrinsic factor C) Lipase D) Amylase A Feedback: The enzyme that initiates the digestion of protein is pepsin. Intrinsic factor combines with vitamin B12 for absorption by the ileum. Lipase aids in the digestion of fats and amylase aids in the digestion of starch. 3. A patient has been brought to the emergency department with abdominal pain and is subsequently diagnosed with appendicitis. The patient is scheduled for an appendectomy but questions the nurse about how his health will be affected by the absence of an appendix. How should the nurse best respond? A) Your appendix doesnt play a major role, so you wont notice any difference after you recovery from surgery. B) The surgeon will encourage you to limit your fat intake for a few weeks after the surgery, but your body will then begin to compensate. C) Your body will absorb slightly fewer nutrients from the food you eat, but you wont be aware of this. D) Your large intestine will adapt over time to the absence of your appendix. A Feedback: The appendix is an appendage of the cecum (not the large intestine) that has little or no physiologic function. Its absence does not affect digestion or absorption. 4. A patient asks the nursing assistant for a bedpan. When the patient is finished, the nursing assistant notifies the nurse that the patient has bright red streaking of blood in the stool. What is this most likely a result of? A) Diet high in red meat B) Upper GI bleed C) Hemorrhoids D) Use of iron supplements C Feedback: Lower rectal or anal bleeding is suspected if there is streaking of blood on the surface of the stool. Hemorrhoids are often a cause of anal bleeding since they occur in the rectum. Blood from an upper GI bleed would be dark rather than frank. Iron supplements make the stool dark, but not bloody and red meat consumption would not cause frank blood. 5. An adult patient is scheduled for an upper GI series that will use a barium swallow. What teaching should the nurse include when the patient has completed the test? A) Stool will be yellow for the first 24 hours postprocedure. B) The barium may cause diarrhea for the next 24 hours. C) Fluids must be increased to facilitate the evacuation of the stool. D) Slight anal bleeding may be noted as the barium is passed. C Feedback: Postprocedural patient education includes information about increasing fluid intake; evaluating bowel movements for evacuation of barium; and noting increased number of bowel movements, because barium, due to its high osmolarity, may draw fluid into the bowel, thus increasing the intraluminal contents and resulting in greater output. Yellow stool, diarrhea, and anal bleeding are not expected. 6. A patient has come to the outpatient radiology department for diagnostic testing. Which of the following diagnostic procedures will allow the care team to evaluate and remove polyps? A) Colonoscopy B) Barium enema C) ERCP D) Upper gastrointestinal fibroscopy A Feedback: During colonoscopy, tissue biopsies can be obtained as needed, and polyps can be removed and evaluated. This is not possible during a barium enema, ERCP, or gastroscopy. 7. A nurse is caring for a patient with recurrent hematemesis who is scheduled for upper gastrointestinal fibroscopy (UGF). How should the nurse in the radiology department prepare this patient? A) Insert a nasogastric tube. B) Administer a micro Fleet enema at least 3 hours before the procedure. C) Have the patient lie in a supine position for the procedure. D) Apply local anesthetic to the back of the patients throat. D Feedback: Preparation for UGF includes spraying or gargling with a local anesthetic. A nasogastric tube or a micro Fleet enema is not required for this procedure. The patient should be positioned in a side-lying position in case of emesis. 8. The nurse is providing health education to a patient scheduled for a colonoscopy. The nurse should explain that she will be placed in what position during this diagnostic test? A) In a knee-chest position (lithotomy position) B) Lying prone with legs drawn toward the chest C) Lying on the left side with legs drawn toward the chest D) In a prone position with two pillows elevating the buttocks C Feedback: For best visualization, colonoscopy is performed while the patient is lying on the left side with the legs drawn up toward the chest. A kneechest position, lying on the stomach with legs drawn to the chest, and a prone position with two pillows elevating the legs do not allow for the best visualization. 9. A patient has sought care because of recent dark-colored stools. As a result, a fecal occult blood test has been ordered. The nurse should instruct the patient to avoid which of the following prior to collecting a stool sample? A) NSAIDs B) Acetaminophen C) OTC vitamin D supplements D) Fiber supplements A Feedback: NSAIDs can cause a false-positive fecal occult blood test. Acetaminophen, vitamin D supplements, and fiber supplements do not have this effect. 10. The nurse is preparing to perform a patients abdominal assessment. What examination sequence should the nurse follow? A) Inspection, auscultation, percussion, and palpation B) Inspection, palpation, auscultation, and percussion C) Inspection, percussion, palpation, and auscultation D) Inspection, palpation, percussion, and auscultation A Feedback: When performing a focused assessment of the patients abdomen, auscultation should always precede percussion and palpation because they may alter bowel sounds. The traditional sequence for all other focused assessments is inspection, palpation, percussion, and auscultation. 11. A patient who has been experiencing changes in his bowel function is scheduled for a barium enema. What instruction should the nurse provide for postprocedure recovery? A) Remain NPO for 6 hours postprocedure. B) Administer a Fleet enema to cleanse the bowel of the barium. C) Increase fluid intake to evacuate the barium. D) Avoid dairy products for 24 hours postprocedure. C Feedback: Adequate fluid intake is necessary to rid the GI tract of barium. The patient must not remain NPO after the test and enemas are not used to cleanse the bowel of barium. There is no need to avoid dairy products. 12. A nurse is caring for a newly admitted patient with a suspected GI bleed. The nurse assesses the patients stool after a bowel movement and notes it to be a tarry-black color. This finding is suggestive of bleeding from what location? A) Sigmoid colon B) Upper GI tract C) Large intestine D) Anus or rectum B Feedback: Blood shed in sufficient quantities in the upper GI tract will produce a tarry-black color (melena). Blood entering the lower portion of the GI tract or passing rapidly through it will appear bright or dark red. Lower rectal or anal bleeding is suspected if there is streaking of blood on the surface of the stool or if blood is noted on toilet tissue. 13. A nursing student has auscultated a patients abdomen and noted one or two bowel sounds in a 2-minute period of time. How would you tell the student to document the patients bowel sounds? A) Normal B) Hypoactive C) Hyperactive D) Paralytic ileus B Feedback: Documenting bowel sounds is based on assessment findings. The terms normal (sounds heard about every 5 to 20 seconds), hypoactive (one or two sounds in 2 minutes), hyperactive (5 to 6 sounds heard in less than 30 seconds), or absent (no sounds in 3 to 5 minutes) are frequently used in documentation. Paralytic ileus is a medical diagnosis that may cause absent or hypoactive bowel sounds, but the nurse would not independently document this diagnosis. 14. An advanced practice nurse is assessing the size and density of a patients abdominal organs. If the results of palpation are unclear to the nurse, what assessment technique should be implemented? A) Percussion B) Auscultation C) Inspection D) Rectal examination A Feedback: Percussion is used to assess the size and density of the abdominal organs and to detect the presence of air-filled, fluid-filled, or solid masses. Percussion is used either independently or concurrently with palpation because it can validate palpation findings. 15. A nurse is caring for a patient with biliary colic and is aware that the patient may experience referred abdominal pain. Where would the nurse most likely expect this patient to experience referred pain? A) Midline near the umbilicus B) Below the right nipple C) Left groin area D) Right lower abdominal quadrant B Feedback: Patients with referred abdominal pain associated with biliary colic complain of pain below the right nipple. Referred pain above the left nipple may be associated with the heart. Groin pain may be referred pain from ureteral colic. 16. An inpatient has returned to the medical unit after a barium enema. When assessing the patients subsequent bowel patterns and stools, what finding should the nurse report to the physician? A) Large, wide stools B) Milky white stools C) Three stools during an 8-hour period of time D) Streaks of blood present in the stool D Feedback: Barium has a high osmolarity and may draw fluid into the bowel, thus increasing the intraluminal contents and resulting in greater output (large stools). The barium will give the stools a milky white appearance, and it is not uncommon for the patient to experience an increase in the number of bowel movements. Blood in fecal matter is not an expected finding and the nurse should notify the physician. 17. A nurse in a stroke rehabilitation facility recognizes that the brain regulates swallowing. Damage to what area of the brain will most affect the patients ability to swallow? A) Temporal lobe B) Medulla oblongata C) Cerebellum D) Pons B Feedback: Swallowing is a voluntary act that is regulated by a swallowing center in the medulla oblongata of the central nervous system. Swallowing is not regulated by the temporal lobe, cerebellum, or pons. 18. A patient is being assessed for a suspected deficit in intrinsic factor synthesis. What diagnostic or assessment finding is the most likely rationale for this examination of intrinsic factor production? A) Muscle wasting B) Chronic jaundice in the absence of liver disease C) The presence of fat in the patients stool D) Persistently low hemoglobin and hematocrit D Feedback: In the absence of intrinsic factor, vitamin B12 cannot be absorbed, and pernicious anemia results. This would result in a marked reduction in hemoglobin and hematocrit. 19. A patient with a recent history of intermittent bleeding is undergoing capsule endoscopy to determine the source of the bleeding. When explaining this diagnostic test to the patient, what advantage should the nurse describe? A) The test allows visualization of the entire peritoneal cavity. B) The test allows for painless biopsy collection. C) The test does not require fasting. D) The test is noninvasive. D Feedback: Capsule endoscopy allows the noninvasive visualization of the mucosa throughout the entire small intestine. Bowel preparation is necessary and biopsies cannot be collected. This procedure allows visualization of the entire GI tract, but not the peritoneal cavity. 20. A nurse is caring for a patient admitted with a suspected malabsorption disorder. The nurse knows that one of the accessory organs of the digestive system is the pancreas. What digestive enzymes does the pancreas secrete? Select all that apply. A) Pepsin B) Lipase C) Amylase D) Trypsin E) Ptyalin B, C, D Feedback: Digestive enzymes secreted by the pancreas include trypsin, which aids in digesting protein; amylase, which aids in digesting starch; and lipase, which aids in digesting fats. Pepsin is secreted by the stomach and ptyalin is secreted in the saliva. 21. The nurse is caring for a patient with a duodenal ulcer and is relating the patients symptoms to the physiologic functions of the small intestine. What do these functions include? Select all that apply. A) Secretion of hydrochloric acid (HCl) B) Reabsorption of water C) Secretion of mucus D) Absorption of nutrients E) Movement of nutrients into the bloodstream C, D, E Feedback: The small intestine folds back and forth on itself, providing approximately 7000 cm2 (70 m2) of surface area for secretion and absorption, the process by which nutrients enter the bloodstream through the intestinal walls. Water reabsorption primarily takes place in the large bowel. HCl is secreted by the stomach. 22. A nurse is performing an abdominal assessment of an older adult patient. When collecting and analyzing data, the nurse should be cognizant of what age-related change in gastrointestinal structure and function? A) Increased gastric motility B) Decreased gastric pH C) Increased gag reflex D) Decreased mucus secretion D Feedback: Older adults tend to secrete less mucus than younger adults. Gastric motility slows with age and gastric pH rises due to decreased secretion of gastric acids. Older adults tend to have a blunted gag reflex compared to younger adults. The nurse educator is reviewing the blood supply of the GI tract with a group of medical nurses. The nurse is explaining the fact that the veins that return blood from the digestive organs and the spleen form the portal venous system. What large veins will the nurse list when describing this system? Select all that apply. A) Splenic vein B) Inferior mesenteric vein C) Gastric vein D) Inferior vena cava E) Saphenous vein A, B, C Feedback: This portal venous system is composed of five large veins: the superior mesenteric, inferior mesenteric, gastric, splenic, and cystic veins, which eventually form the vena portae that enters the liver. The inferior vena cava is not part of the portal system. The saphenous vein is located in the leg. 24. The physiology instructor is discussing the GI system with the pre-nursing class. What should the instructor describe as a major function of the GI tract? A) The breakdown of food particles into cell form for digestion B) The maintenance of fluid and acid-base balance C) The absorption into the bloodstream of nutrient molecules produced by digestion D) The control of absorption and elimination of electrolytes C Feedback: Primary functions of the GI tract include the breakdown of food particles into molecular form for digestion; the absorption into the bloodstream of small nutrient molecules produced by digestion; and the elimination of undigested unabsorbed food stuffs and other waste products. Nutrients must be broken down into molecular form, not cell form. Fluid, electrolyte, and acid-base balance are primarily under the control of the kidneys. 25. A nurse is providing preprocedure education for a patient who will undergo a lower GI tract study the following week. What should the nurse teach the patient about bowel preparation? A) Youll need to fast for at least 18 hours prior to your test. B) Starting today, take over-the-counter stool softeners twice daily. C) Youll need to have enemas the day before the test. D) For 24 hours before the test, insert a glycerin suppository every 4 hours. C Feedback: Preparation of the patient includes emptying and cleansing the lower bowel. This often necessitates a low-residue diet 1 to 2 days before the test; a clear liquid diet and a laxative the evening before; NPO after midnight; and cleansing enemas until returns are clear the following morning. 26. A patient presents at the walk-in clinic complaining of recurrent sharp stomach pain that is relieved by eating. The nurse suspects that the patient may have an ulcer. How would the nurse explain the formation and role of acid in the stomach to the patient? A) Hydrochloric acid is secreted by glands in the stomach in response to the actual or anticipated presence of food. B) As digestion occurs in the stomach, the stomach combines free hydrogen ions from the food to form acid. C) The body requires an acidic environment in order to synthesize pancreatic digestive enzymes; the stomach provides this environment. D) The acidic environment in the stomach exists to buffer the highly alkaline environment in the esophagus. A Feedback: The stomach, which stores and mixes food with secretions, secretes a highly acidic fluid in response to the presence or anticipated ingestion of food. The stomach does not turn food directly into acid and the esophagus is not highly alkaline. Pancreatic enzymes are not synthesized in a highly acidic environment. 27. Results of a patients preliminary assessment prompted an examination of the patients carcinoembryonic antigen (CEA) levels, which have come back positive. What is the nurses most appropriate response to this finding? A) Perform a focused abdominal assessment. B) Prepare to meet the patients psychosocial needs. C) Liaise with the nurse practitioner to perform an anorectal examination. D) Encourage the patient to adhere to recommended screening protocols. B Feedback: CEA is a protein that is normally not detected in the blood of a healthy person; therefore, when detected it indicates that cancer is present, but not what type of cancer is present. The patient would likely be learning that he or she has cancer, so the nurse must prioritize the patients immediate psychosocial needs, not abdominal assessment. Future screening is not a high priority in the short term. 28. A clinic patient has described recent dark-colored stools;the nurse recognizes the need for fecal occult blood testing (FOBT). What aspect of the patients current health status would contraindicate FOBT? A) Gastroesophageal reflux disease (GERD) B) Peptic ulcers C) Hemorrhoids D) Recurrent nausea and vomiting C Feedback: FOBT should not be performed when there is hemorrhoidal bleeding. GERD, peptic ulcers and nausea and vomiting do not contraindicate the use of FOBT as a diagnostic tool. 29. A patient will be undergoing abdominal computed tomography (CT) with contrast. The nurse has administered IV sodium bicarbonate and oral acetylcysteine (Mucomyst) before the study as ordered. What would indicate that these medications have had the desired therapeutic effect? A) The patients BUN and creatinine levels are within reference range following the CT. B) The CT yields high-quality images. C) The patients electrolytes are stable in the 48 hours following the CT. D) The patients intake and output are in balance on the day after the CT. A Feedback: Both sodium bicarbonate and Mucomyst are free radical scavengers that sequester the contrast byproducts that are destructive to renal cells. Kidney damage would be evident by increased BUN and creatinine levels. These medications are unrelated to electrolyte or fluid balance and they play no role in the results of the CT. 30. A medical patients CA 19-9 levels have become available and they are significantly elevated. How should the nurse best interpret this diagnostic finding? A) The patient may have cancer, but other GI disease must be ruled out. B) The patient most likely has early-stage colorectal cancer. C) The patient has a genetic predisposition to gastric cancer. D) The patient has cancer, but the site is unknown. A Feedback: CA 19-9 levels are elevated in most patients with advanced pancreatic cancer, but they may also be elevated in other conditions such as colorectal, lung, and gallbladder cancers; gallstones; pancreatitis; cystic fibrosis; and liver disease. A cancer diagnosis cannot be made solely on CA 19-9 results. 31. A patient has come to the clinic complaining of blood in his stool. A FOBT test is performed but is negative. Based on the patients history, the physician suggests a colonoscopy, but the patient refuses, citing a strong aversion to the invasive nature of the test. What other test might the physician order to check for blood in the stool? A) A laparoscopic intestinal mucosa biopsy B) A quantitative fecal immunochemical test C) Computed tomography (CT) D) Magnetic resonance imagery (MRI) B Feedback: Quantitative fecal immunochemical tests may be more accurate than guaiac testing and useful for patients who refuse invasive testing. CT or MRI cannot detect blood in stool. Laparoscopic intestinal mucosa biopsy is not performed. 32. A nurse is assessing the abdomen of a patient just admitted to the unit with a suspected GI disease. Inspection reveals several diverse lesions on the patients abdomen. How should the nurse best interpret this assessment finding? A) Abdominal lesions are usually due to age-related skin changes. B) Integumentary diseases often cause GI disorders. C) GI diseases often produce skin changes. D) The patient needs to be assessed for self-harm. C Feedback: Abdominal lesions are of particular importance, because GI diseases often produce skin changes. Skin problems do not normally cause GI disorders. Age-related skin changes do not have a pronounced effect on the skin of the abdomen when compared to other skin surfaces. Self-harm is a less likely explanation for skin lesions on the abdomen. 33. Probably the most widely used in-office or at-home occult blood test is the Hemoccult II. The patient has come to the clinic because he thinks there is blood in his stool. When you reviewed his medications, you noted he is on antihypertensive drugs and NSAIDs for early arthritic pain. You are sending the patient home with the supplies necessary to perform 2 hemoccult tests on his stool and mail the samples back to the clinic. What instruction would you give this patient? A) Take all your medications as usual. B) Take all your medications except the antihypertensive medications. C) Dont eat highly acidic foods 72 hours before you start the test. D) Avoid vitamin C for 72 hours before you start the test. D Feedback: Red meats, aspirin, nonsteroidal anti-inflammatory drugs, turnips, and horseradish should be avoided for 72 hours prior to the study, because they may cause a false-positive result. Also, ingestion of vitamin C from supplements or foods can cause a false-negative result. Acidic foods do not need to be avoided. 34. A patients sigmoidoscopy has been successfully completed and the patient is preparing to return home. Which of the following teaching points should the nurse include in the patients discharge education? A) The patient should drink at least 2 liters of fluid in the next 12 hours. B) The patient can resume a normal routine immediately. C) The patient should expect fecal urgency for several hours. D) The patient can expect some scant rectal bleeding. B Feedback: Following sigmoidoscopy, patients can resume their regular activities and diet. There is no need to push fluids and neither fecal urgency nor rectal bleeding is expected. 35. A nurse is caring for an 83-year-old patient who is being assessed for recurrent and intractable nausea. What age-related change to the GI system may be a contributor to the patients health complaint? A) Stomach emptying takes place more slowly. B) The villi and epithelium of the small intestine become thinner. C) The esophageal sphincter becomes incompetent. D) Saliva production decreases. A Feedback: Delayed gastric emptying occurs in older adults and may contribute to nausea. Changes to the small intestine and decreased saliva production would be less likely to contribute to nausea. Loss of esophageal sphincter function is pathologic and is not considered an age-related change. 36. A patient has been experiencing significant psychosocial stress in recent weeks. The nurse is aware of the hormonal effects of stress, including norepinephrine release. Release of this substance would have what effect on the patients gastrointestinal function? Select all that apply. A) Decreased motility B) Increased sphincter tone C) Increased enzyme release D) Inhibition of secretions E) Increased peristalsis A Feedback: Norepinephrine generally decreases GI motility and secretions, but increases muscle tone of sphincters. Norepinephrine does not increase the release of enzymes. 37. A patient with cystic fibrosis takes pancreatic enzyme replacements on a regular basis. The patients intake of trypsin facilitates what aspect of GI function? A) Vitamin D synthesis B) Digestion of fats C) Maintenance of peristalsis D) Digestion of proteins D Feedback: Trypsin facilitates the digestion of proteins. It does not influence vitamin D synthesis, the digestion of fats, or peristalsis. 38. The nurse is caring for a patient who has a diagnosis of AIDS. Inspection of the patients mouth reveals the new presence of white lesions on the patients oral mucosa. What is the nurses most appropriate response? A) Encourage the patient to gargle with salt water twice daily. B) Attempt to remove the lesions with a tongue depressor. C) Make a referral to the units dietitian. D) Inform the primary care provider of this finding. D Feedback: The nurse should inform the primary care provider of this abnormal finding in the patients oral cavity, since it necessitates medical treatment. It would be inappropriate to try to remove skin lesions from a patients mouth and salt water will not resolve this problem, which is likely due to candidiasis. A dietitian referral is unnecessary. 39. A patient has been scheduled for a urea breath test in one months time. What nursing diagnosis most likely prompted this diagnostic test? A) Impaired Dentition Related to Gingivitis B) Risk For Impaired Skin Integrity Related to Peptic Ulcers C) Imbalanced Nutrition: Less Than Body Requirements Related to Enzyme Deficiency D) Diarrhea Related to Clostridium Difficile Infection B Feedback: Urea breath tests detect the presence of Helicobacter pylori, the bacteria that can live in the mucosal lining of the stomach and cause peptic ulcer disease. This test does not address fluid volume, nutritional status, or dentition. 40. A female patient has presented to the emergency department with right upper quadrant pain; the physician has ordered abdominal ultrasound to rule out cholecystitis (gallbladder infection). The patient expresses concern to the nurse about the safety of this diagnostic procedure. How should the nurse best respond? A) Abdominal ultrasound is very safe, but it cant be performed if youre pregnant. B) Abdominal ultrasound poses no known safety risks of any kind. C) Current guidelines state that a person can have up to 3 ultrasounds per year. D) Current guidelines state that a person can have up to 6 ultrasounds per year. B Feedback: An ultrasound produces no ill effects and there are not specific limits on its use, even during pregnancy. Chapter 44: Digestive and Gastrointestinal Treatment Modalities 1. A nurse is preparing to place a patients ordered nasogastric tube. How should the nurse best determine the correct length of the nasogastric tube? A) Place distal tip to nose, then ear tip and end of xiphoid process. B) Instruct the patient to lie prone and measure tip of nose to umbilical area. C) Insert the tube into the patients nose until secretions can be aspirated. D) Obtain an order from the physician for the length of tube to insert. A Feedback: Tube length is traditionally determined by (1) measuring the distance from the tip of the nose to the earlobe and from the earlobe to the xiphoid process, and (2) adding up to 6 inches for NG placement or at least 8 to 10 inches or more for intestinal placement, although studies do not necessarily confirm that this is a reliable technique. The physician would not prescribe a specific length and the umbilicus is not a landmark for this process. Length is not determined by aspirating from the tube. 2. A patient is concerned about leakage of gastric contents out of the gastric sump tube the nurse has just inserted. What would the nurse do to prevent reflux gastric contents from coming through the blue vent of a gastric sump tube? A) Prime the tubing with 20 mL of normal saline. B) Keep the vent lumen above the patients waist. C) Maintain the patient in a high Fowlers position. D) Have the patient pin the tube to the thigh. B Feedback: The blue vent lumen should be kept above the patients waist to prevent reflux of gastric contents through it; otherwise it acts as a siphon. A one-way anti-reflux valve seated in the blue pigtail can prevent the reflux of gastric contents out the vent lumen. To prevent reflux, the nurse does not prime the tubing, maintain the patient in a high Fowlers position, or have the patient pin the tube to the thigh. 3. A patient receiving tube feedings is experiencing diarrhea. The nurse and the physician suspect that the patient is experiencing dumping syndrome. What intervention is most appropriate? A) Stop the tube feed and aspirate stomach contents. B) Increase the hourly feed rate so it finishes earlier. C) Dilute the concentration of the feeding solution. D) Administer fluid replacement by IV. C Feedback: Dumping syndrome can generally be alleviated by starting with a dilute solution and then increasing the concentration of the solution over several days. Fluid replacement may be necessary but does not prevent or treat dumping syndrome. There is no need to aspirate stomach contents. Increasing the rate will exacerbate the problem. 4. A nurse is admitting a patient to the postsurgical unit following a gastrostomy. When planning assessments, the nurse should be aware of what potential postoperative complication of a gastrostomy? A) Premature removal of the G tube B) Bowel perforation C) Constipation D) Development of peptic ulcer disease (PUD) A Feedback: A significant postoperative complication of a gastrostomy is premature removal of the G tube. Constipation is a less immediate threat and bowel perforation and PUD are not noted to be likely complications. 5. A nursing educator is reviewing the care of patients with feeding tubes and endotracheal tubes (ET). The educator has emphasized the need to check for tube placement in the stomach as well as residual volume. What is the main purpose of this nursing action? A) Prevent gastric ulcers B) Prevent aspiration C) Prevent abdominal distention D) Prevent diarrhea B Feedback: Protecting the client from aspirating is essential because aspiration can cause pneumonia, a potentially life-threatening disorder. Gastric ulcers are not a common complication of tube feeding in clients with ET tubes. Abdominal distention and diarrhea can both be associated with tube feeding, but prevention of these problems is not the primary rationale for confirming placement. 6. The nurse is administering total parenteral nutrition (TPN) to a client who underwent surgery for gastric cancer. Which of the nurses assessments most directly addresses a major complication of TPN? A) Checking the patients capillary blood glucose levels regularly B) Having the patient frequently rate his or her hunger on a 10-point scale C) Measuring the patients heart rhythm at least every 6 hours D) Monitoring the patients level of consciousness each shift A Feedback: The solution, used as a base for most TPN, consists of a high dextrose concentration and may raise blood glucose levels significantly, resulting in hyperglycemia. This is a more salient threat than hunger, though this should be addressed. Dysrhythmias and decreased LOC are not among the most common complications. 7. A critical care nurse is caring for a patient diagnosed with acute pancreatitis. The nurse knows that the indications for starting parenteral nutrition (PN) for this patient are what? A) 5% deficit in body weight compared to preillness weight and increased caloric need B) Calorie deficit and muscle wasting combined with low electrolyte levels C) Inability to take in adequate oral food or fluids within 7 days D) Significant risk of aspiration coupled with decreased level of consciousness C Feedback: The indications for PN include an inability to ingest adequate oral food or fluids within 7 days. Weight loss, muscle wasting combined with electrolyte imbalances, and aspiration indicate a need for nutritional support, but this does not necessary have to be parenteral. 8. A nurse is preparing to administer a patients intravenous fat emulsion simultaneously with parenteral nutrition (PN). Which of the following principles should guide the nurses action? A) Intravenous fat emulsions may be infused simultaneously with PN through a Y-connector close to the infusion site and should not be filtered. B) The nurse should prepare for placement of another intravenous line, as intravenous fat emulsions may not be infused simultaneously through the line used for PN. C) Intravenous fat emulsions may be infused simultaneously with PN through a Y-connector close to the infusion site after running the emulsion through a filter. D) The intravenous fat emulsions can be piggy-backed into any existing IV solution that is infusing. A Feedback: Intravenous fat emulsions may be infused simultaneously with PN through a Y-connector close to the infusion site and should not be filtered. The patient does not need another intravenous line for the fat emulsion. The IVFE cannot be piggy-backed into any existing IV solution that is infusing. 9. A nurse is participating in a patients care conference and the team is deciding between parenteral nutrition (PN) and a total nutritional admixture (TNA). What advantages are associated with providing TNA rather than PN? A) TNA can be mixed by a certified registered nurse. B) TNA can be administered over 8 hours, while PN requires 24-hour administration. C) TNA is less costly than PN. D) TNA does not require the use of a micron filter. C Feedback: TNA is mixed in one container and administered to the patient over a 24-hour period. A 1.5-micron filter is used with the TNA solution. Advantages of the TNA over PN include cost savings. Pharmacy staff must prepare both solutions. 10. A nurse is initiating parenteral nutrition (PN) to a postoperative patient who has developed complications. The nurse should initiate therapy by performing which of the following actions? A) Starting with a rapid infusion rate to meet the patients nutritional needs as quickly as possible B) Initiating the infusion slowly and monitoring the patients fluid and glucose tolerance C) Changing the rate of administration every 2 hours based on serum electrolyte values D) Increasing the rate of infusion at mealtimes to mimic the circadian rhythm of the body B Feedback: PN solutions are initiated slowly and advanced gradually each day to the desired rate as the patients fluid and glucose tolerance permits. The formulation of the PN solutions is calculated carefully each day to meet the complete nutritional needs of the individual patient based on clinical findings and laboratory data. It is not infused more quickly at mealtimes. 11. A patients physician has determined that for the next 3 to 4 weeks the patient will require parenteral nutrition (PN). The nurse should anticipate the placement of what type of venous access device? A) Peripheral catheter B) Nontunneled central catheter C) Implantable port D) Tunneled central catheter B Feedback: Nontunneled central catheters are used for short-term (less than 6 weeks) IV therapy. A peripheral catheter can be used for the administration of peripheral parenteral nutrition for 5 to 7 days. Implantable ports and tunneled central catheters are for long-term use and may remain in place for many years. Peripherally inserted central catheters (PICCs) are another potential option. 12. A nurse is caring for a patient who has an order to discontinue the administration of parenteral nutrition. What should the nurse do to prevent the occurrence of rebound hypoglycemia in the patient? A) Administer an isotonic dextrose solution for 1 to 2 hours after discontinuing the PN. B) Administer a hypertonic dextrose solution for 1 to 2 hours after discontinuing the PN. C) Administer 3 ampules of dextrose 50% immediately prior to discontinuing the PN. D) Administer 3 ampules of dextrose 50% 1 hour after discontinuing the PN. A Feedback: After administration of the PN solution is gradually discontinued, an isotonic dextrose solution is administered for 1 to 2 hours to protect against rebound hypoglycemia. The other listed actions would likely cause hyperglycemia. 13. A nurse is caring for a patient with a subclavian central line who is receiving parenteral nutrition (PN). In preparing a care plan for this patient, what nursing diagnosis should the nurse prioritize? A) Risk for Activity Intolerance Related to the Presence of a Subclavian Catheter B) Risk for Infection Related to the Presence of a Subclavian Catheter C) Risk for Functional Urinary Incontinence Related to the Presence of a Subclavian Catheter D) Risk for Sleep Deprivation Related to the presence of a Subclavian Catheter B Feedback: The high glucose content of PN solutions makes the solutions an idea culture media for bacterial and fungal growth, and the central venous access devices provide a port of entry. Prevention of infection is consequently a high priority. The patient will experience some inconveniences with regard to toileting, activity, and sleep, but the infection risk is a priority over each of these. A patients health decline necessitates the use of total parenteral nutrition. The patient has questioned the need for insertion of a central venous catheter, expressing a preference for a normal IV. The nurse should know that peripheral administration of high-concentration PN formulas is contraindicated because of the risk for what complication? A) Chemical phlebitis B) Hyperglycemia C) Dumping syndrome D) Line sepsis A Feedback: Formulations with dextrose concentrations of more than 10% should not be administered through peripheral veins because they irritate the intima (innermost walls) of small veins, causing chemical phlebitis. Hyperglycemia and line sepsis are risks with both peripheral and central administration of PN. PN is not associated with dumping syndrome. A nurse is providing care for a patient with a diagnosis of late-stage Alzheimers disease. The patient has just returned to the medical unit to begin supplemental feedings through an NG tube. Which of the nurses assessments addresses this patients most significant potential complication of feeding? A) Frequent assessment of the patients abdominal girth B) Assessment for hemorrhage from the nasal insertion site C) Frequent lung auscultation D) Vigilant monitoring of the frequency and character of bowel movements C Feedback: Aspiration is a risk associated with tube feeding; this risk may be exacerbated by the patients cognitive deficits. Consequently, the nurse should auscultate the patients lungs and monitor oxygen saturation closely. Bowel function is important, but the risk for aspiration is a priority. Hemorrhage is highly unlikely and the patients abdominal girth is not a main focus of assessment. 16. The management of the patients gastrostomy is an assessment priority for the home care nurse. What statement would indicate that the patient is managing the tube correctly? A) I clean my stoma twice a day with alcohol. B) The only time I flush my tube is when Im putting in medications. C) I flush my tube with water before and after each of my medications. D) I try to stay still most of the time to avoid dislodging my tube. C Feedback: Frequent flushing is needed to prevent occlusion, and should not just be limited to times of medication administration. Alcohol will irritate skin surrounding the insertion site and activity should be maintained as much as possible. 17. A nurse is caring for a patient with a nasogastric tube for feeding. During shift assessment, the nurse auscultates a new onset of bilateral lung crackles and notes a respiratory rate of 30 breaths per minute. The patients oxygen saturation is 89% by pulse oximetry. After ensuring the patients immediate safety, what is the nurses most appropriate action? A) Perform chest physiotherapy. B) Reduce the height of the patients bed and remove the NG tube. C) Liaise with the dietitian to obtain a feeding solution with lower osmolarity. D) Report possible signs of aspiration pneumonia to the primary care provider. D Feedback: The patient should be assessed for further signs of aspiration pneumonia. It is unnecessary to remove the NG tube and chest physiotherapy is not indicated. A different feeding solution will not resolve this complication. 18. A nurse is creating a care plan for a patient with a nasogastric tube. How should the nurse direct other members of the care team to check correct placement of the tube? A) Auscultate the patients abdomen after injecting air through the tube. B) Assess the color and pH of aspirate. C) Locate the marking made after the initial x-ray confirming placement. D) Use a combination of at least two accepted methods for confirming placement. D Feedback: There are a variety of methods to check tube placement. The safest way to confirm placement is to utilize a combination of assessment methods. 19. The nurse is assessing placement of a nasogastric tube that the patient has had in place for 2 days. The tube is draining green aspirate. What is the nurses most appropriate action? A) Inform the physician that the tube may be in the patients pleural space. B) Withdraw the tube 2 to 4 cm. C) Leave the tube in its present position. D) Advance the tube up to 8 cm. C Feedback: The patients aspirate is from the gastric area when the nurse observes that the color of the aspirate is green. Further confirmation of placement is necessary, but there is likely no need for repositioning. Pleural secretions are pale yellow. 20. A patients new onset of dysphagia has required insertion of an NG tube for feeding; the nurse has modified the patients care plan accordingly. What intervention should the nurse include in the patients plan of care? A) Confirm placement of the tube prior to each medication administration. B) Have the patient sip cool water to stimulate saliva production. C) Keep the patient in a low Fowlers position when at rest. D) Connect the tube to continuous wall suction when not in use. A Feedback: Each time liquids or medications are administered, and once a shift for continuous feedings, the tube must be checked to ensure that it remains properly placed. If the NG tube is used for decompression, it is attached to intermittent low suction. During the placement of a nasogastric tube the patient should be positioned in a Fowlers position. Oral fluid administration is contraindicated by the patients dysphagia. 21. A patient has been brought to the emergency department by EMS after telling a family member that he deliberately took an overdose of NSAIDs a few minutes earlier. If lavage is ordered, the nurse should prepare to assist with the insertion of what type of tube? A) Nasogastric tube B) Levin tube C) Gastric sump D) Orogastric tube D Feedback: An orogastric tube is a large-bore tube inserted through the mouth with a wide outlet for removal of gastric contents; it is used primarily in the emergency department or an intensive care setting. Nasogastric, Levin, and gastric sump tubes are not used for this specific purpose. 22. A patients NG tube has become clogged after the nurse instilled a medication that was insufficiently crushed. The nurse has attempted to aspirate with a large-bore syringe, with no success. What should the nurse do next? A) Withdraw the NG tube 3 to 5 cm and reattempt aspiration. B) Attach a syringe filled with warm water and attempt an in-and-out motion of instilling and aspirating. C) Withdraw the NG tube slightly and attempt to dislodge by flicking the tube with the fingers. D) Remove the NG tube promptly and obtain an order for reinsertion from the primary care provider. B Feedback: When a tube is first noted to be clogged, a 30- to 60-mL syringe should be attached to the end of the tube and any contents aspirated and discarded. Then the syringe should be filled with warm water, attached to the tube again, and a back-and-forth motion initiated to help loosen the clog. Removal is not warranted at this early stage and a flicking motion is not recommended. The tube should not be withdrawn, even a few centimeters. A nurse has obtained an order to remove a patients NG tube and has prepared the patient accordingly. After flushing the tube and removing the nasal tape, the nurse attempts removal but is met with resistance. Because the nurse is unable to overcome this resistance, what is the most appropriate action? A) Gently twist the tube before pulling. B) Instill a digestive enzyme solution and reattempt removal in 10 to 15 minutes. C) Flush the tube with hot tap water and reattempt removal. D) Report this finding to the patients primary care provider. D Feedback: If the tube does not come out easily, force should not be used, and the problem should be reported to the primary provider. Enzymes are used to resolve obstructions, not to aid removal. For safety reasons, hot water is never instilled into a tube. Twisting could cause damage to the mucosa. 24. A nurse is writing a care plan for a patient with a nasogastric tube in place for gastric decompression. What risk nursing diagnosis is the most appropriate component of the care plan? A) Risk for Excess Fluid Volume Related to Enteral Feedings B) Risk for Impaired Skin Integrity Related to the Presence of NG Tube C) Risk for Unstable Blood Glucose Related to Enteral Feedings D) Risk for Impaired Verbal Communication Related to Presence of NG Tube B Feedback: NG tubes can easily damage the delicate mucosa of the nose, sinuses, and upper airway. An NG tube does not preclude verbal communication. This patients NG tube is in place for decompression, so complications of enteral feeding do not apply. 25. A patients enteral feedings have been determined to be too concentrated based on the patients development of dumping syndrome. What physiologic phenomenon caused this patients complication of enteral feeding? A) Increased gastric secretion of HCl and gastrin because of high osmolality of feeds B) Entry of large amounts of water into the small intestine because of osmotic pressure C) Mucosal irritation of the stomach and small intestine by the high concentration of the feed D) Acidbase imbalance resulting from the high volume of solutes in the feed B Feedback: When a concentrated solution of high osmolality entering the intestines is taken in quickly or in large amounts, water moves rapidly into the intestinal lumen from fluid surrounding the organs and the vascular compartment. This results in dumping syndrome. Dumping syndrome is not the result of changes in HCl or gastrin levels. It is not caused by an acidbase imbalance or direct irritation of the GI mucosa. A nurse is creating a care plan for a patient who is receiving parenteral nutrition. The patients care plan should include nursing actions relevant to what potential complications? Select all that apply. A) Dumping syndrome B) Clotted or displaced catheter C) Pneumothorax D) Hyperglycemia E) Line sepsis B, C, D, E Feedback: Common complications of PN include a clotted or displaced catheter, pneumothorax, hyperglycemia, and infection from the venous access device (line sepsis). Dumping syndrome applies to enteral nutrition, not PN. A nurse is caring for a patient who has a gastrointestinal tube in place. Which of the following are indications for gastrointestinal intubation? Select all that apply. A) To remove gas from the stomach B) To administer clotting factors to treat a GI bleed C) To remove toxins from the stomach D) To open sphincters that are closed E) To diagnose GI motility disorders A, C, E Feedback: GI intubation may be performed to decompress the stomach and remove gas and fluid, lavage (flush with water or other fluids) the stomach and remove ingested toxins or other harmful materials, diagnose disorders of GI motility and other disorders, administer medications and feedings, compress a bleeding site, and aspirate gastric contents for analysis. GI intubation is not used for opening sphincters that are not functional or for administering clotting factors. 28. A patient with dysphagia is scheduled for PEG tube insertion and asks the nurse how the tube will stay in place. What is the nurses best response? A) Adhesive holds a flange in place against the abdominal skin. B) A stitch holds the tube in place externally. C) The tube is stitched to the abdominal skin externally and the stomach wall internally. D) An internal retention disc secures the tube against the stomach wall. D Feedback: A PEG tube is held in place by an internal retention disc (flange) that holds it against the stomach wall. It is not held in place by stitches or adhesives. 29. A patient is postoperative day 1 following gastrostomy. The nurse is planning interventions to address the nursing diagnosis of Risk for Infection Related to Presence of Wound and Tube. What intervention is most appropriate? A) Administer antibiotics via the tube as ordered. B) Wash the area around the tube with soap and water daily. C) Cleanse the skin within 2 cm of the insertion site with hydrogen peroxide once per shift. D) Irrigate the skin surrounding the insertion site with normal saline before each use. B Feedback: Infection can be prevented by keeping the skin near the insertion site clean using soap and water. Hydrogen peroxide is not used, due to associated skin irritation. The skin around the site is not irrigated with normal saline and antibiotics are not administered to prevent site infection. 30. The nurse is preparing to insert a patients ordered NG tube. What factor should the nurse recognize as a risk for incorrect placement? A) The patient is obese and has a short neck. B) The patient is agitated. C) The patient has a history of gastroesophageal reflux disease (GERD). D) The patient is being treated for pneumonia. B Feedback: Inappropriate placement may occur in patients with decreased levels of consciousness, confused mental states, poor or absent cough and gag reflexes, or agitation during insertion. A short neck, GERD, and pneumonia are not linked to incorrect placement. 31. Prior to a patients scheduled jejunostomy, the nurse is performing the preoperative assessment. What goal should the nurse prioritize during the preoperative assessment? A) Determining the patients nutritional needs B) Determining that the patient fully understands the postoperative care required C) Determining the patients ability to understand and cooperate with the procedure D) Determining the patients ability to cope with an altered body image C Feedback: The major focus of the preoperative assessment is to determine the patients ability both to understand and cooperate with the procedure. Body image, nutritional needs, and postoperative care are all important variables, but they are not the main focuses of assessment during the immediate preoperative period. 32. You are caring for a patient who was admitted to have a low-profile gastrostomy device (LPGD) placed. How soon after the original gastrostomy tube placement can an LPGD be placed? A) 2 weeks B) 4 to 6 weeks C) 2 to 3 months D) 4 to 6 months C Feedback: An alternative to the PEG device is a low-profile gastrostomy device (LPGD). LPGDs may be inserted 2 to 3 months after initial gastrostomy tube placement. 33. A nurse is caring for a patient who is receiving parenteral nutrition. When writing this patients plan of care, which of the following nursing diagnoses should be included? A) Risk for Peripheral Neurovascular Dysfunction Related to Catheter Placement B) Ineffective Role Performance Related to Parenteral Nutrition C) Bowel Incontinence Related to Parenteral Nutrition D) Chronic Pain Related to Catheter Placement B Feedback: The limitations associated with PN can make it difficult for patients to maintain their usual roles. PN does not normally cause bowel incontinence and catheters are not associated with chronic pain or neurovascular dysfunction. 34. A nurse is aware of the high incidence of catheter-related bloodstream infections in patients receiving parenteral nutrition. What nursing action has the greatest potential to reduce catheter-related bloodstream infections? A) Use clean technique and wear a mask during dressing changes. B) Change the dressing no more than weekly. C) Apply antibiotic ointment around the site with each dressing change. D) Irrigate the insertion site with sterile water during each dressing change. B Feedback: The CDC (2011) recommends changing CVAD dressings not more than every 7 days unless the dressing is damp, bloody, loose, or soiled. Sterile technique (not clean technique) is used. Irrigation and antibiotic ointments are not used. A patient who suffered a stroke had an NG tube inserted to facilitate feeding shortly after admission. The patient has since become comatose and the patients family asks the nurse why the physician is recommending the removal of the patients NG tube and the insertion of a gastrostomy tube. What is the nurses best response? A) It eliminates the risk for infection. B) Feeds can be infused at a faster rate. C) Regurgitation and aspiration are less likely. D) It allows caregivers to provide personal hygiene more easily. C Feedback: Gastrostomy is preferred over NG feedings in the patient who is comatose because the gastroesophageal sphincter remains intact, making regurgitation and aspiration less likely than with NG feedings. Both tubes carry a risk for infection; this change in care is not motivated by the possibility of faster infusion or easier personal care. A patient has been discharged home on parenteral nutrition (PN). Much of the nurses discharge education focused on coping. What must a patient on PN likely learn to cope with? Select all that apply. A) Changes in lifestyle B) Loss of eating as a social behavior C) Chronic bowel incontinence from GI changes D) Sleep disturbances related to frequent urination during nighttime infusions E) Stress of choosing the correct PN formulation A, B, D Feedback: Patients must cope with the loss of eating as a social behavior and with changes in lifestyle brought on by sleep disturbances related to frequent urination during night time infusions. PN is not associated with bowel incontinence and the patient does not select or adjust the formulation of PN. 37. A patient has a gastrostomy tube that has been placed to drain stomach contents by low intermittent suction. What is the nurses priority during this aspect of the patients care? A) Measure and record drainage. B) Monitor drainage for change in color. C) Titrate the suction every hour. D) Feed the patient via the G tube as ordered. A Feedback: This drainage should be measured and recorded because it is a significant indicator of GI function. The nurse should indeed monitor the color of the output, but fluid balance is normally the priority. Frequent titration of the suction should not be necessary and feeding is contraindicated if the G tube is in place for drainage. A nurse is preparing to discharge a patient home on parenteral nutrition. What should an effective home care teaching program address? Select all that apply. A) Preparing the patient to troubleshoot for problems B) Teaching the patient and family strict aseptic technique C) Teaching the patient and family how to set up the infusion D) Teaching the patient to flush the line with sterile water E) Teaching the patient when it is safe to leave the access site open to air A, B, C Feedback: An effective home care teaching program prepares the patient to store solutions, set up the infusion, flush the line with heparin, change the dressings, and troubleshoot for problems. The most common complication is sepsis. Strict aseptic technique is taught for hand hygiene, handling equipment, changing the dressing, and preparing the solution. Sterile water is never used for flushes and the access site must never be left open to air. 39. The nurse is caring for a patient who is postoperative from having a gastrostomy tube placed. What should the nurse do on a daily basis to prevent skin breakdown? A) Verify tube placement. B) Loop adhesive tape around the tube and connect it securely to the abdomen. C) Gently rotate the tube. D) Change the wet-to-dry dressing. C Feedback: The nurse verifies the tubes placement and gently rotates the tube once daily to prevent skin breakdown. Verifying tube placement and taping the tube to the abdomen do not prevent skin breakdown. A gastrostomy wound does not have a wet-to-dry dressing. 40. A nurse is preparing to administer a patients scheduled parenteral nutrition (PN). Upon inspecting the bag, the nurse notices that the presence of small amounts of white precipitate are present in the bag. What is the nurses best action? A) Recognize this as an expected finding. B) Place the bag in a warm environment for 30 minutes. C) Shake the bag vigorously for 10 to 20 seconds. D) Contact the pharmacy to obtain a new bag of PN. D Feedback: Before PN infusion is administered, the solution must be inspected for separation, oily appearance (also known as a cracked solution), or any precipitate (which appears as white crystals). If any of these are present, it is not used. Warming or shaking the bag is inappropriate and unsafe. Chapter 45: Management of Patients with Oral and Esophageal Disorders 1. A nurse is providing oral care to a patient who is comatose. What action best addresses the patients risk of tooth decay and plaque accumulation? A) Irrigating the mouth using a syringe filled with a bacteriocidal mouthwash B) Applying a water-soluble gel to the teeth and gums C) Wiping the teeth and gums clean with a gauze pad D) Brushing the patients teeth with a toothbrush and small amount of toothpaste D Feedback: Application of mechanical friction is the most effective way to cleanse the patients mouth. If the patient is unable to brush teeth, the nurse may brush them, taking precautions to prevent aspiration; or as a substitute, the nurse can achieve mechanical friction by wiping the teeth with a gauze pad. Bacteriocidal mouthwash does reduce plaque-causing bacteria; however, it is not as effective as application of mechanical friction. Water-soluble gel may be applied to lubricate dry lips, but it is not part of oral care. 2. An elderly patient comes into the emergency department complaining of an earache. The patient and has an oral temperature of 100.2F and otoscopic assessment of the ear reveals a pearly gray tympanic membrane with no evidence of discharge or inflammation. Which action should the triage nurse take next? A) Palpate the patients parotid glands to detect swelling and tenderness. B) Assess the temporomandibular joint for evidence of a malocclusion. C) Test the integrity of cranial nerve XII by asking the patient to protrude the tongue. D) Inspect the patients gums for bleeding and hyperpigmentation. A Feedback: Older adults and debilitated patients of any age who are dehydrated or taking medications that reduce saliva production are at risk for parotitis. Symptoms include fever and tenderness, as well as swelling of the parotid glands. Pain radiates to the ear. Pain associated with malocclusion of the temporomandibular joint may also radiate to the ears; however, a temperature elevation would not be associated with malocclusion. The 12th cranial nerve is not associated with the auditory system. Bleeding and hyperpigmented gums may be caused by pyorrhea or gingivitis. These conditions do not cause earache; fever would not be present unless the teeth were abscessed. 3. A patient who had a hemiglossectomy earlier in the day is assessed postoperatively, revealing a patent airway, stable vital signs, and no bleeding or drainage from the operative site. The nurse notes the patient is alert. What is the patients priority need at this time? A) Emotional support from visitors and staff B) An effective means of communicating with the nurse C) Referral to a speech therapist D) Dietary teaching focused on consistency of food and frequency of feedings B Feedback: Verbal communication may be impaired by radical surgery for oral cancer. It is therefore vital to assess the patients ability to communicate in writing before surgery. Emotional support and dietary teaching are critical aspects of the plan of care; however, the patients ability to communicate would be essential for both. Referral to a speech therapist will be required as part of the patients rehabilitation; however, it is not a priority at this particular time. Communication with the nurse is crucial for the delivery of safe and effective care. 4. The nurse notes that a patient who has undergone skin, tissue, and muscle grafting following a modified radical neck dissection requires suctioning. What is the most important consideration for the nurse when suctioning this patient? A) Avoid applying suction on or near the suture line. B) Position patient on the non operative side with the head of the bed down. C) Assess the patients ability to perform self-suctioning. D) Evaluate the patients ability to swallow saliva and clear fluids. A Feedback: The nurse should avoid positioning the suction catheter on or near the graft suture lines. Application of suction in these areas could damage the graft. Self-sectioning may be unsafe because the patient may damage the suture line. Following a modified radical neck dissection with graft, the patient is usually positioned with the head of the bed elevated to promote drainage and reduce edema. Assessing viability of the graft is important but is not part of the suctioning procedure and may delay initiating suctioning. Maintenance of a patent airway is a nursing priority. Similarly, the patients ability to swallow is an important assessment for the nurse to make; however, it is not directly linked to the patients need for suctioning. 5. A patient with gastroesophageal reflux disease (GERD) has a diagnosis of Barretts esophagus with minor cell changes. Which of the following principles should be integrated into the patients subsequent care? A) The patient will require an upper endoscopy every 6 months to detect malignant changes. B) Liver enzymes must be checked regularly, as H2 receptor antagonists may cause hepatic damage. C) Small amounts of blood are likely to be present in the stools and are not cause for concern. D) Antacids may be discontinued when symptoms of heartburn subside. A Feedback: In the patient with Barretts esophagus, the cells lining the lower esophagus have undergone change and are no longer squamous cells. The altered cells are considered precancerous and are a precursor to esophageal cancer. In order to facilitate early detection of malignant cells, an upper endoscopy is recommended every 6 months. H2 receptor antagonists are commonly prescribed for patients with GERD; however, monitoring of liver enzymes is not routine. Stools that contain evidence of frank bleeding or that are tarry are not expected and should be reported immediately. When antacids are prescribed for patients with GERD, they should be taken as ordered whether or not the patient is symptomatic. 6. The school nurse is planning a health fair for a group of fifth graders and dental health is one topic that the nurse plans to address. What would be most likely to increase the risk of tooth decay? A) Organic fruit juice B) Roasted nuts C) Red meat that is high in fat D) Cheddar cheese A Feedback: Dental caries may be prevented by decreasing the amount of sugar and starch in the diet. Patients who snack should be encouraged to choose less cariogenic alternatives, such as fruits, vegetables, nuts, cheeses, or plain yogurt. Fruit juice is high in sugar, regardless of whether it is organic. 7. The nurses comprehensive assessment of a patient includes inspection for signs of oral cancer. What assessment finding is most characteristic of oral cancer in its early stages? A) Dull pain radiating to the ears and teeth B) Presence of a painless sore with raised edges C) Areas of tenderness that make chewing difficult D) Diffuse inflammation of the buccal mucosa B Feedback: Malignant lesions of the oral cavity are most often painless lumps or sores with raised borders. Because they do not bother the patient, delay in seeking treatment occurs frequently, and negatively affects prognosis. Dull pain radiating to the ears and teeth is characteristic of malocclusion. Inflammation of the buccal mucosa causes discomfort and often occurs as a side effect of chemotherapy. Tenderness resulting in pain on chewing may be associated with gingivitis, abscess, irritation from dentures, and other causes. Pain related to oral cancer is a late symptom. 8. A medical nurse who is caring for a patient being discharged home after a radical neck dissection has collaborated with the home health nurse to develop a plan of care for this patient. What is a priority psychosocial outcome for a patient who has had a radical neck dissection? A) Indicates acceptance of altered appearance and demonstrates positive self-image B) Freely expresses needs and concerns related to postoperative pain management C) Compensates effectively for alteration in ability to communicate related to dysarthria D) Demonstrates effective stress management techniques to promote muscle relaxation A Feedback: Since radical neck dissection involves removal of the sternocleidomastoid muscle, spinal accessory muscles, and cervical lymph nodes on one side of the neck, the patients appearance is visibly altered. The face generally appears asymmetric, with a visible neck depression; shoulder drop also occurs frequently. These changes have the potential to negatively affect self-concept and body image. Facilitating adaptation to these changes is a crucial component of nursing intervention. Patients who have had head and neck surgery generally report less pain as compared with other postoperative patients; however, the nurse must assess each individual patients level of pain and response to analgesics. Patients may experience transient hoarseness following a radical neck dissection; however, their ability to communicate is not permanently altered. Stress management is beneficial but would not be considered the priority in this clinical situation. 9. A patient has been diagnosed with an esophageal diverticulum after undergoing diagnostic imaging. When taking the health history, the nurse should expect the patient to describe what sign or symptom? A) Burning pain on swallowing B) Regurgitation of undigested food C) Symptoms mimicking a heart attack D) Chronic parotid abscesses B Feedback: An esophageal diverticulum is an outpouching of mucosa and submucosa that protrudes through the esophageal musculature. Food becomes trapped in the pouch and is frequently regurgitated when the patient assumes a recumbent position. The patient may experience difficulty swallowing; however, burning pain is not a typical finding. Symptoms mimicking a heart attack are characteristic of GERD. Chronic parotid abscesses are not associated with a diagnosis of esophageal diverticulum. 10. A nurse is caring for a patient who is acutely ill and has included vigilant oral care in the patients plan of care. Why are patients who are ill at increased risk for developing dental caries? A) Hormonal changes brought on by the stress response cause an acidic oral environment B) Systemic infections frequently migrate to the teeth C) Hydration that is received intravenously lacks fluoride D) Inadequate nutrition and decreased saliva production can cause cavities D Feedback: Many ill patients do not eat adequate amounts of food and therefore produce less saliva, which in turn reduces the natural cleaning of the teeth. Stress response is not a factor, infections generally do not attack the enamel of the teeth, and the fluoride level of the patient is not significant in the development of dental caries in the ill patient. 11. A nurse who provides care in an ambulatory clinic integrates basic cancer screening into admission assessments. What patient most likely faces the highest immediate risk of oral cancer? A) A 65-year-old man with alcoholism who smokes B) A 45-year-old woman who has type 1 diabetes and who wears dentures C) A 32-year-old man who is obese and uses smokeless tobacco D) A 57-year-old man with GERD and dental caries A Feedback: Oral cancers are often associated with the use of alcohol and tobacco, which when used together have a synergistic carcinogenic effect. Most cases of oral cancers occur in people over the age of 60 and a disproportionate number of cases occur in men. Diabetes, dentures, dental caries, and GERD are not risk factors for oral cancer. 12. A nurse is caring for a patient who has undergone neck resection with a radial forearm free flap. The nurses most recent assessment of the graft reveals that it has a bluish color and that mottling is visible. What is the nurses most appropriate action? A) Document the findings as being consistent with a viable graft. B) Promptly report these indications of venous congestion. C) Closely monitor the patient and reassess in 30 minutes. D) Reposition the patient to promote peripheral circulation. B Feedback: A graft that is blue with mottling may indicate venous congestion. This finding constitutes a risk for tissue ischemia and necrosis; prompt referral is necessary. 13. A nurse is assessing a patient who has just been admitted to the postsurgical unit following surgical resection for the treatment of oropharyngeal cancer. What assessment should the nurse prioritize? A) Assess ability to clear oral secretions. B) Assess for signs of infection. C) Assess for a patent airway. D) Assess for ability to communicate. C Feedback: Postoperatively, the nurse assesses for a patent airway. The patients ability to manage secretions has a direct bearing on airway patency. However, airway patency is the overarching goal. This immediate physiologic need is prioritized over communication, though this is an important consideration. Infection is not normally a threat in the immediate postoperative period. 14. A patient has been diagnosed with achalasia based on his history and diagnostic imaging results. The nurse should identify what risk diagnosis when planning the patients care? A) Risk for Aspiration Related to Inhalation of Gastric Contents B) Risk for Imbalanced Nutrition: Less than Body Requirements Related to Impaired Absorption C) Risk for Decreased Cardiac Output Related to Vasovagal Response D) Risk for Impaired Verbal Communication Related to Oral Trauma A Feedback: Achalasia can result in the aspiration of gastric contents. It is not normally an acute risk to the patients nutritional status and does not affect cardiac output or communication. 15. A nurse is providing health promotion education to a patient diagnosed with an esophageal reflux disorder. What practice should the nurse encourage the patient to implement? A) Keep the head of the bed lowered. B) Drinka cup of hot tea before bedtime. C) Avoid carbonated drinks. D) Eat a low-protein diet. C Feedback: For a patient diagnosed with esophageal reflux disorder, the nurse should instruct the patient to keep the head of the bed elevated. Carbonated drinks, caffeine, and tobacco should be avoided. Protein limitation is not necessary. A staff educator is reviewing the causes of gastroesophageal reflux disease (GERD) with new staff nurses. What area of the GI tract should the educator identify as the cause of reduced pressure associated with GERD? A) Pyloric sphincter B) Lower esophageal sphincter C) Hypopharyngeal sphincter D) Upper esophageal sphincter B Feedback: The lower esophageal sphincter, also called the gastroesophageal sphincter or cardiac sphincter, is located at the junction of the esophagus and the stomach. An incompetent lower esophageal sphincter allows reflux (backward flow) of gastric contents. The upper esophageal sphincter and the hypopharyngeal sphincter are synonymous and are not responsible for the manifestations of GERD. The pyloric sphincter exists between the stomach and the duodenum. 17. A patient who has had a radical neck dissection is being prepared for discharge. The discharge plan includes referral to an outpatient rehabilitation center for physical therapy. What would the goals of physical therapy for this patient include? A) Muscle training to relieve dysphagia B) Relieving nerve paralysis in the cervical plexus C) Promoting maximum shoulder function D) Alleviating achalasia by decreasing esophageal peristalsis C Feedback: Shoulder drop occurs as a result of radical neck dissection. Shoulder function can be improved by rehabilitation exercises. Rehabilitation would not be initiated until the patients neck incision and graft, if present, were sufficiently healed. Nerve paralysis in the cervical plexus and other variables affecting swallowing would be managed by a speech therapist rather than a physical therapist. 18. A nurse is addressing the prevention of esophageal cancer in response to a question posed by a participant in a health promotion workshop. What action has the greatest potential to prevent esophageal cancer? A) Promotion of a nutrient-dense, low-fat diet B) Annual screening endoscopy for patients over 50 with a family history of esophageal cancer C) Early diagnosis and treatment of gastroesophageal reflux disease D) Adequate fluid intake and avoidance of spicy foods C Feedback: There are numerous risk factors for esophageal cancer but chronic esophageal irritation or GERD is among the most significant. This is a more significant risk factor than dietary habits. Screening endoscopies are not recommended solely on the basis of family history. 19. An emergency department nurse is admitting a 3-year-old brought in after swallowing a piece from a wooden puzzle. The nurse should anticipate the administration of what medication in order to relax the esophagus to facilitate removal of the foreign body? A) Haloperidol B) Prostigmine C) Epinephrine D) Glucagon D Feedback: Glucagon is administered prior to removal of a foreign body because it relaxes the smooth muscle of the esophagus, facilitating insertion of the endoscope. Haloperidol is an antipsychotic drug and is not indicated. Prostigmine is prescribed for patients with myastheniagravis. It increases muscular contraction, an effect opposite that which is desired to facilitate removal of the foreign body. Epinephrine is indicated in asthma attack and bronchospasm. 20. A nurse in an oral surgery practice is working with a patient scheduled for removal of an abscessed tooth. When providing discharge education, the nurse should recommend which of the following actions? A) Rinse the mouth with alcohol before bedtime for the next 7 days. B) Use warm saline to rinse the mouth as needed. C) Brush around the area with a firm toothbrush to prevent infection. D) Use a toothpick to dislodge any debris that gets lodged in the socket. B Feedback: The patient should be assessed for bleeding after the tooth is extracted. The mouth can be rinsed with warm saline to keep the area clean. A firm toothbrush or toothpick could injure the tissues around the extracted area. Alcohol would injure tissues that are healing. 21. A patient has been diagnosed with a malignancy of the oral cavity and is undergoing oncologic treatment. The oncologic nurse is aware that the prognosis for recovery from head and neck cancers is often poor because of what characteristic of these malignancies? A) Radiation therapy often results in secondary brain tumors. B) Surgical complications are exceedingly common. C) Diagnosis rarely occurs until the cancer is endstage. D) Metastases are common and respond poorly to treatment. D Feedback: Deaths from malignancies of the head and neck are primarily attributable to local-regional metastasis to the cervical lymph nodes in the neck. This often occurs by way of the lymphatics before the primary lesion has been treated. This local-regional metastasis is not amenable to surgical resection and responds poorly to chemotherapy and radiation therapy. This high mortality rate is not related to surgical complications, late diagnosis, or the development of brain tumors. 22. A patient has undergone surgery for oral cancer and has just been extubated in postanesthetic recovery. What nursing action best promotes comfort and facilitates spontaneous breathing for this patient? A) Placing the patient in a left lateral position B) Administering opioids as ordered C) Placing the patient in Fowlers position D) Teaching the patient to use the patient-controlled analgesia (PCA) system C Feedback: After the endotracheal tube or airway has been removed and the effects of the anesthesia have worn off, the patient may be placed in Fowlers position to facilitate breathing and promote comfort. Lateral positioning does not facilitate oxygenation or comfort. Medications do not facilitate spontaneous breathing. 23. A nurse is performing health education with a patient who has a history of frequent, serious dental caries. When planning educational interventions, the nurse should identify a risk for what nursing diagnosis? A) Ineffective Tissue Perfusion B) Impaired Skin Integrity C) Aspiration D) Imbalanced Nutrition: Less Than Body Requirements D Feedback: Because digestion normally begins in the mouth, adequate nutrition is related to good dental health and the general condition of the mouth. Any discomfort or adverse condition in the oral cavity can affect a persons nutritional status. Dental caries do not typically affect the patients tissue perfusion or skin integrity. Aspiration is not a likely consequence of dental caries. 24. A patient has undergone rigid fixation for the correction of a mandibular fracture suffered in a fight. What area of care should the nurse prioritize when planning this patients discharge education? A) Resumption of activities of daily living B) Pain control C) Promotion of adequate nutrition D) Strategies for promoting communication C Feedback: The patient who has had rigid fixation should be instructed not to chew food in the first 1 to 4 weeks after surgery. A liquid diet is recommended, and dietary counseling should be obtained to ensure optimal caloric and protein intake. The nature of this surgery threatens the patients nutritional status; this physiologic need would likely supersede the resumption of ADLs. Pain should be under control prior to discharge and communication is not precluded by this surgery. 25. A radial graft is planned in the treatment of a patients oropharyngeal cancer. In order to ensure that the surgery will be successful, the care team must perform what assessment prior to surgery? A) Assessing function of cranial nerves V, VI, and IX B) Assessing for a history of GERD C) Assessing for signs or symptoms of atherosclerosis D) Assessing the patency of the ulnar artery D Feedback: If a radial graft is to be performed, an Allen test on the donor arm must be performed to ensure that the ulnar artery is patent and can provide blood flow to the hand after removal of the radial artery. The success of this surgery is not primarily dependent on CN function or the absence of GERD and atherosclerosis. 26. A nurse is caring for a patient who is postoperative day 1 following neck dissection surgery. The nurse is performing an assessment of the patient and notes the presence of high-pitched adventitious sounds over the patients trachea on auscultation. The patients oxygen saturation is 90% by pulse oximetry with a respiratory rate of 31 breaths per minute. What is the nurses most appropriate action? A) Encourage the patient to perform deep breathing and coughing exercises hourly. B) Reposition the patient into a prone or semi-Fowlers position and apply supplementary oxygen by nasal cannula. C) Activate the emergency response system. D) Report this finding promptly to the physician and remain with the patient. D Feedback: In the immediate postoperative period, the nurse assesses for stridor (coarse, high-pitched sound on inspiration) by listening frequently over the trachea with a stethoscope. This finding must be reported immediately because it indicates obstruction of the airway. The patients current status does not warrant activation of the emergency response system, and encouraging deep breathing and repositioning the patient are inadequate responses. 27. A nurse is caring for a patient who has just had a rigid fixation of a mandibular fracture. When planning the discharge teaching for this patient, what would the nurse be sure to include? A) Increasing calcium intake to promote bone healing B) Avoiding chewing food for the specified number of weeks after surgery C) Techniques for managing parenteral nutrition in the home setting D) Techniques for managing a gastrostomy B Feedback: The patient who has had rigid fixation should be instructed not to chew food in the first 1 to 4 weeks after surgery. A liquid diet is recommended, and dietary counseling should be obtained to ensure optimal caloric and protein intake. Increased calcium intake will not have an appreciable effect on healing. Enteral and parenteral nutrition are rarely necessary. 28. A community health nurse serves a diverse population. What individual would likely face the highest risk for parotitis? A) A patient who is receiving intravenous antibiotic therapy in the home setting B) A patient who has a chronic venous ulcer C) An older adult whose medication regimen includes an anticholinergic D) A patient with poorly controlled diabetes who receives weekly wound care C Feedback: Elderly, acutely ill, or debilitated people with decreased salivary flow from general dehydration or medications are at high risk for parotitis. Anticholinergic medications inhibit saliva production. Antibiotics, diabetes, and wounds are not risk factors for parotitis. 29. A nurse is providing care for a patient whose neck dissection surgery involved the use of a graft. When assessing the graft, the nurse should prioritize data related to what nursing diagnosis? A) Risk for Disuse Syndrome B) Unilateral Neglect C) Risk for Trauma D) Ineffective Tissue Perfusion D Feedback: Grafted skin is highly vulnerable to inadequate perfusion and subsequent ischemia and necrosis. This is a priority over chronic pain, which is unlikely to be a long-term challenge. Neglect and disuse are not risks related to the graft site. 30. A patients neck dissection surgery resulted in damage to the patients superior laryngeal nerve. What area of assessment should the nurse consequently prioritize? A) The patients swallowing ability B) The patients ability to speak C) The patients management of secretions D) The patients airway patency A Feedback: If the superior laryngeal nerve is damaged, the patient may have difficulty swallowing liquids and food because of the partial lack of sensation of the glottis. Damage to this particular nerve does not inhibit speech and only affects management of secretions and airway patency indirectly. 31. A patient who underwent surgery for esophageal cancer is admitted to the critical care unit following postanesthetic recovery. Which of the following should be included in the patients immediate postoperative plan of care? A) Teaching the patient to self-suction B) Performing chest physiotherapy to promote oxygenation C) Positioning the patient to prevent gastric reflux D) Providing a regular diet as tolerated C Feedback: After recovering from the effects of anesthesia, the patient is placed in a low Fowlers position, and later in a Fowlers position, to help prevent reflux of gastric secretions. The patient is observed carefully for regurgitation and dyspnea because a common postoperative complication is aspiration pneumonia. In this period of recovery, self-suctioning is also not likely realistic or safe. Chest physiotherapy is contraindicated because of the risk of aspiration. Nutrition is prioritized, but a regular diet is contraindicated in the immediate recovery from esophageal surgery. 32. A patient has received treatment for oral cancer. The combination of medications and radiotherapy has resulted in leukopenia. Which of the following is an appropriate response to this change in health status? A) Ensure that none of the patients visitors has an infection. B) Arrange for a diet that is high in protein and low in fat. C) Administer colony stimulating factors (CSFs) as ordered. D) Prepare to administer chemotherapeutics as ordered. A Feedback: Leukopenia reduces defense mechanisms, increasing the risk of infections. Visitors who might transmit microorganisms are prohibited if the patients immunologic system is depressed. Changes in diet, CSFs, and the use of chemotherapy do not resolve leukopenia. 33. A nurse is caring for a patient who has had surgery for oral cancer. When addressing the patients long- term needs, the nurse should prioritize interventions and referrals with what goal? A) Enhancement of verbal communication B) Enhancement of immune function C) Maintenance of adequate social support D) Maintenance of fluid balance A Feedback: Verbal communication may be impaired by radical surgery for oral cancer. Addressing this impairment often requires a long-term commitment. Immune function, social support, and fluid balance are all necessary, but communication is a priority issue for patients recovering from this type of surgery. 34. A patient with cancer of the tongue has had a radical neck dissection. What nursing assessment would be a priority for this patient? A) Presence of acute pain and anxiety B) Tissue integrity and color of the operative site C) Respiratory status and airway clearance D) Self-esteem and body image C Feedback: Postoperatively, the patient is assessed for complications such as altered respiratory status, wound infection, and hemorrhage. The other assessments are part of the plan of care for a patient who has had a radical neck dissection, but are not the nurses chief priority. 35. A patient returns to the unit after a neck dissection. The surgeon placed a Jackson Pratt drain in the wound. When assessing the wound drainage over the first 24 postoperative hours the nurse would notify the physician immediately for what? A) Presence of small blood clots in the drainage B) 60 mL of milky or cloudy drainage C) Spots of drainage on the dressings surrounding the drain D) 120 mL of serosanguinous drainage B Feedback: Between 80 and 120 mL of serosanguineous secretions may drain over the first 24 hours. Milky drainage is indicative of a chyle fistula, which requires prompt treatment. 36. A nurse is caring for a patient who is postoperative from a neck dissection. What would be the most appropriate nursing action to enhance the patients appetite? A) Encourage the family to bring in the patients favored foods. B) Limit visitors at mealtimes so that the patient is not distracted. C) Avoid offering food unless the patient initiates. D) Provide thorough oral care immediately after the patient eats. A Feedback: Family involvement and home-cooked favorite foods may help the patient to eat. Having visitors at mealtimes may make eating more pleasant and increase the patients appetite. The nurse should not place the complete onus for initiating meals on the patient. Oral care after meals is necessary, but does not influence appetite. 37. A patient with GERD has undergone diagnostic testing and it has been determined that increasing the pace of gastric emptying may help alleviate symptoms. The nurse should anticipate that the patient may be prescribed what drug? A) Metoclopramide (Reglan) B) Omeprazole (Prilosec) C) Lansoprazole (Prevacid) D) Famotidine (Pepcid) A Feedback: Metoclopramide (Reglan) is useful in promoting gastric motility. Omeprazole and lansoprozole are proton pump inhibitors that reduce gastric acid secretion. Famotidine (Pepcid) is an H2receptor antagonist, which has a similar effect. 38. Results of a patient barium swallow suggest that the patient has GERD. The nurse is planning health education to address the patients knowledge of this new diagnosis. Which of the following should the nurse encourage? A) Eating several small meals daily rather than 3 larger meals B) Keeping the head of the bed slightly elevated C) Drinking carbonated mineral water rather than soft drinks D) Avoiding food or fluid intake after 6:00 p.m. B Feedback: The patient with GERD is encouraged to elevate the head of the bed on 6- to 8-inch (15- to 20-cm) blocks. Frequent meals are not specifically encouraged and the patient should avoid food and fluid within 2 hours of bedtime. All carbonated beverages should be avoided. 39. A nurse is caring for a patient in the late stages of esophageal cancer. The nurse should plan to prevent or address what characteristics of this stage of the disease? Select all that apply. A) Perforation into the mediastinum B) Development of an esophageal lesion C) Erosion into the great vessels D) Painful swallowing E) Obstruction of the esophagus A, C, E Feedback: In the later stages of esophageal cancer, obstruction of the esophagus is noted, with possible perforation into the mediastinum and erosion into the great vessels. Painful swallowing and the emergence of a lesion are early signs of esophageal cancer. 40. A patient seeking care because of recurrent heartburn and regurgitation is subsequently diagnosed with a hiatal hernia. Which of the following should the nurse include in health education? A) Drinking beverages after your meal, rather than with your meal, may bring some relief. B) Its best to avoid dry foods, such as rice and chicken, because theyre harder to swallow. C) Many patients obtain relief by taking over-the-counter antacids 30 minutes before eating. D) Instead of eating three meals a day, try eating smaller amounts more often. D Feedback: Management for a hiatal hernia includes frequent, small feedings that can pass easily through the esophagus. Avoiding beverages and particular foods or taking OTC antacids are not noted to be beneficial. Chapter 46: Management of Patients with Gastric and Duodenal Disorders 1. A nurse is caring for a patient who just has been diagnosed with a peptic ulcer. When teaching the patient about his new diagnosis, how should the nurse best describe a peptic ulcer? A) Inflammation of the lining of the stomach B) Erosion of the lining of the stomach or intestine C) Bleeding from the mucosa in the stomach D) Viral invasion of the stomach wall B Feedback: A peptic ulcer is erosion of the lining of the stomach or intestine. Peptic ulcers are often accompanied by bleeding and inflammation, but these are not the definitive characteristics. 2. A patient comes to the clinic complaining of pain in the epigastric region. What assessment question during the health interview would most help the nurse determine if the patient has a peptic ulcer? A) Does your pain resolve when you have something to eat? B) Do over-the-counter pain medications help your pain? C) Does your pain get worse if you get up and do some exercise? D) Do you find that your pain is worse when you need to have a bowel movement? A Feedback: Pain relief after eating is associated with duodenal ulcers. The pain of peptic ulcers is generally unrelated to activity or bowel function and may or may not respond to analgesics. 3. A patient with a diagnosis of peptic ulcer disease has just been prescribed omeprazole (Prilosec). How should the nurse best describe this medications therapeutic action? A) This medication will reduce the amount of acid secreted in your stomach. B) This medication will make the lining of your stomach more resistant to damage. C) This medication will specifically address the pain that accompanies peptic ulcer disease. D) This medication will help your stomach lining to repair itself. A Feedback: Proton pump inhibitors like Prilosec inhibit the synthesis of stomach acid. PPIs do not increase the durability of the stomach lining, relieve pain, or stimulate tissue repair. 4. A nurse is admitting a patient diagnosed with late-stage gastric cancer. The patients family is distraught and angry that she was not diagnosed earlier in the course of her disease. What factor contributes to the fact that gastric cancer is often detected at a later stage? A) Gastric cancer does not cause signs or symptoms until metastasis has occurred. B) Adherence to screening recommendations for gastric cancer is exceptionally low. C) Early symptoms of gastric cancer are usually attributed to constipation. D) The early symptoms of gastric cancer are usually not alarming or highly unusual. D Feedback: Symptoms of early gastric cancer, such as pain relieved by antacids, resemble those of benign ulcers and are seldom definitive. Symptoms are rarely a cause for alarm or for detailed diagnostic testing. Symptoms precede metastasis, however, and do not include constipation. 5. A nurse is preparing to discharge a patient after recovery from gastric surgery. What is an appropriate discharge outcome for this patient? A) The patients bowel movements maintain a loose consistency. B) The patient is able to tolerate three large meals a day. C) The patient maintains or gains weight. D) The patient consumes a diet high in calcium. C Feedback: Expected outcomes for the patient following gastric surgery include ensuring that the patient is maintaining or gaining weight (patient should be weighed daily), experiencing no excessive diarrhea, and tolerating six small meals a day. Patients may require vitamin B12 supplementation by the intramuscular route and do not require a diet excessively rich in calcium. 6. A nurse caring for a patient who has had bariatric surgery is developing a teaching plan in anticipation of the patients discharge. Which of the following is essential to include? A) Drink a minimum of 12 ounces of fluid with each meal. B) Eat several small meals daily spaced at equal intervals. C) Choose foods that are high in simple carbohydrates. D) Sit upright when eating and for 30 minutes afterward. B Feedback: Due to decreased stomach capacity, the patient must consume small meals at intervals to meet nutritional requirements while avoiding a feeling of fullness and complications such as dumping syndrome. The patient should not consume fluids with meals and low-Fowlers positioning is recommended during and after meals. Carbohydrates should be limited. 7. A nurse is completing a health history on a patient whose diagnosis is chronic gastritis. Which of the data should the nurse consider most significantly related to the etiology of the patients health problem? A) Consumes one or more protein drinks daily. B) Takes over-the-counter antacids frequently throughout the day. C) Smokes one pack of cigarettes daily. D) Reports a history of social drinking on a weekly basis. C Feedback: Nicotine reduces secretion of pancreatic bicarbonate, which inhibits neutralization of gastric acid and can underlie gastritis. Protein drinks do not result in gastric inflammation. Antacid use is a response to experiencing symptoms of gastritis, not the etiology of gastritis. Alcohol ingestion can lead to gastritis; however, this generally occurs in patients with a history of consumption of alcohol on a daily basis. 8. A nurse in the postanesthesia care unit admits a patient following resection of a gastric tumor. Following immediate recovery, the patient should be placed in which position to facilitate patient comfort and gastric emptying? A) Fowlers B) Supine C) Left lateral D) Left Sims A Feedback: Positioning the patient in a Fowlers position postoperatively promotes comfort and facilitates emptying of the stomach following gastric surgery. Any position that involves lying down delays stomach emptying and is not recommended for this type of patient. Supine positioning and the left lateral (left Sims) position do not achieve this goal. 9. A community health nurse is preparing for an initial home visit to a patient discharged following a total gastrectomy for treatment of gastric cancer. What would the nurse anticipate that the plan of care is most likely to include? A) Enteral feeding via gastrostomy tube (G tube) B) Gastrointestinal decompression by nasogastric tube C) Periodic assessment for esophageal distension D) Monthly administration of injections of vitamin B12 D Feedback: Since vitamin B12 is absorbed in the stomach, the patient requires vitamin B12 replacement to prevent pernicious anemia. A gastrectomy precludes the use of a G tube. Since the stomach is absent, a nasogastric tube would not be indicated. As well, this is not possible in the home setting. Since there is no stomach to act as a reservoir and fluids and nutrients are passing directly into the jejunum, distension is unlikely. 10. A nurse is assessing a patient who has peptic ulcer disease. The patient requests more information about the typical causes of Helicobacter pylori infection. What would it be appropriate for the nurse to instruct the patient? A) Most affected patients acquired the infection during international travel. B) Infection typically occurs due to ingestion of contaminated food and water. C) Many people possess genetic factors causing a predisposition to H. pylori infection. D) The H. pylori microorganism is endemic in warm, moist climates. B Feedback: Most peptic ulcers result from infection with the gram-negative bacteria H. pylori, which may be acquired through ingestion of food and water. The organism is endemic to all areas of the United States. Genetic factors have not been identified. 11. A patient who experienced an upper GI bleed due to gastritis has had the bleeding controlled and the patients condition is now stable. For the next several hours, the nurse caring for this patient should assess for what signs and symptoms of recurrence? A) Tachycardia, hypotension, and tachypnea B) Tarry, foul-smelling stools C) Diaphoresis and sudden onset of abdominal pain D) Sudden thirst, unrelieved by oral fluid administration A Feedback: Tachycardia, hypotension, and tachypnea are signs of recurrent bleeding. Patients who have had one GI bleed are at risk for recurrence. Tarry stools are expected short-term findings after a hemorrhage. Hemorrhage is not normally associated with sudden thirst or diaphoresis. 12. A patient presents to the walk-in clinic complaining of vomiting and burning in her mid-epigastria. The nurse knows that in the process of confirming peptic ulcer disease, the physician is likely to order a diagnostic test to detect the presence of what? A) Infection with Helicobacter pylori B) Excessive stomach acid secretion C) An incompetent pyloric sphincter D) A metabolic acidbase imbalance A Feedback: H. pylori infection may be determined by endoscopy and histologic examination of a tissue specimen obtained by biopsy, or a rapid urease test of the biopsy specimen. Excessive stomach acid secretion leads to gastritis; however, peptic ulcers are caused by colonization of the stomach by H. pylori. Sphincter dysfunction and acidbase imbalances do not cause peptic ulcer disease. 13. A patient with a peptic ulcer disease has had metronidazole (Flagyl) added to his current medication regimen. What health education related to this medication should the nurse provide? A) Take the medication on an empty stomach. B) Take up to one extra dose per day if stomach pain persists. C) Take at bedtime to mitigate the effects of drowsiness. D) Avoid drinking alcohol while taking the drug. D Feedback: Alcohol must be avoided when taking Flagyl and the medication should be taken with food. This drug does not cause drowsiness and the dose should not be adjusted by the patient. 14. A patient was treated in the emergency department and critical care unit after ingesting bleach. What possible complication of the resulting gastritis should the nurse recognize? A) Esophageal or pyloric obstruction related to scarring B) Uncontrolled proliferation of H. pylori C) Gastric hyperacidity related to excessive gastrin secretion D) Chronic referred pain in the lower abdomen A Feedback: A severe form of acute gastritis is caused by the ingestion of strong acid or alkali, which may cause the mucosa to become gangrenous or to perforate. Scarring can occur, resulting in pyloric stenosis (narrowing or tightening) or obstruction. Chronic referred pain to the lower abdomen is a symptom of peptic ulcer disease, but would not be an expected finding for a patient who has ingested a corrosive substance. Bacterial proliferation and hyperacidity would not occur. 15. A patient who underwent gastric banding 3 days ago is having her diet progressed on a daily basis. Following her latest meal, the patient complains of dizziness and palpitations. Inspection reveals that the patient is diaphoretic. What is the nurses best action? A) Insert a nasogastric tube promptly. B) Reposition the patient supine. C) Monitor the patient closely for further signs of dumping syndrome. D) Assess the patient for signs and symptoms of aspiration. C Feedback: The patients symptoms are characteristic of dumping syndrome, which results in a sensation of fullness, weakness, faintness, dizziness, palpitations, diaphoresis, cramping pains, and diarrhea. Aspiration is a less likely cause for the patients symptoms. Supine positioning will likely exacerbate the symptoms and insertion of an NG tube is contraindicated due to the nature of the patients surgery. 16. A patient is one month postoperative following restrictive bariatric surgery. The patient tells the clinic nurse that he has been having trouble swallowing for the past few days. What recommendation should the nurse make? A) Eating more slowly and chewing food more thoroughly B) Taking an OTC antacid or drinking a glass of milk prior to each meal C) Chewing gum to cause relaxation of the lower esophageal sphincter D) Drinking at least 12 ounces of liquid with each meal A Feedback: Dysphagia may be prevented by educating patients to eat slowly, to chew food thoroughly, and to avoid eating tough foods such as steak or dry chicken or doughy bread. After bariatric procedures, patients should normally not drink beverages with meals. Medications or chewing gum will not alleviate this problem. 17. A patient is receiving education about his upcoming Billroth I procedure (gastroduodenostomy). This patient should be informed that he may experience which of the following adverse effects associated with this procedure? A) Persistent feelings of hunger and thirst B) Constipation or bowel incontinence C) Diarrhea and feelings of fullness D) Gastric reflux and belching C Feedback: Following a Billroth I, the patient may have problems with feelings of fullness, dumping syndrome, and diarrhea. Hunger and thirst, constipation, and gastric reflux are not adverse effects associated with this procedure. 18. A patient has experienced symptoms of dumping syndrome following bariatric surgery. To what physiologic phenomenon does the nurse attribute this syndrome? A) Irritation of the phrenic nerve due to diaphragmatic pressure B) Chronic malabsorption of iron and vitamins A and C C) Reflux of bile into the distal esophagus D) A sudden release of peptides D Feedback: For many years, it had been theorized that the hypertonic gastric food boluses that quickly transit into the intestines drew extracellular fluid from the circulating blood volume into the small intestines to dilute the high concentration of electrolytes and sugars, resulting in symptoms. Now, it is thought that this rapid transit of the food bolus from the stomach into the small intestines instead causes a rapid and exuberant release of metabolic peptides that are responsible for the symptoms of dumping syndrome. It is not a result of phrenic nerve irritation, malabsorption, or bile reflux. 19. A patient comes to the bariatric clinic to obtain information about bariatric surgery. The nurse assesses the obese patient knowing that in addition to meeting the criterion of morbid obesity, a candidate for bariatric surgery must also demonstrate what? A) Knowledge of the causes of obesity and its associated risks B) Adequate understanding of required lifestyle changes C) Positive body image and high self-esteem D) Insight into why past weight loss efforts failed B Feedback: Patients seeking bariatric surgery should be free of serious mental disorders and motivated to comply with lifestyle changes related to eating patterns, dietary choices, and elimination. While assessment of knowledge about causes of obesity and its associated risks as well as insight into the reasons why previous diets have been ineffective are included in the clients plan of care, these do not predict positive client outcomes following bariatric surgery. Most obese patients have an impaired body image and alteration in self-esteem. An obese patient with a positive body image would be unlikely to seek this surgery unless he or she was experiencing significant comorbidities. 20. A nurse is providing patient education for a patient with peptic ulcer disease secondary to chronic nonsteroidal anti-inflammatory drug (NSAID) use. The patient has recently been prescribed misoprostol (Cytotec). What would the nurse be most accurate in informing the patient about the drug? A) It reduces the stomachs volume of hydrochloric acid B) It increases the speed of gastric emptying C) It protects the stomachs lining D) It increases lower esophageal sphincter pressure C Feedback: Misoprostol is a synthetic prostaglandin that, like prostaglandin, protects the gastric mucosa. NSAIDs decrease prostaglandin production and predispose the patient to peptic ulceration. Misoprostol does not reduce gastric acidity, improve emptying of the stomach, or increase lower esophageal sphincter pressure. 21. A nurse is providing anticipator guidance to a patient who is preparing for bariatric surgery. The nurse learns that the patient is anxious about numerous aspects of the surgery. What intervention is most appropriate to alleviate the patients anxiety? A) Emphasize the fact that bariatric surgery has a low risk of complications. B) Encourage the patient to focus on the benefits of the surgery. C) Facilitate the patients contact with a support group. D) Obtain an order for a PRN benzodiazepine. C Feedback: Support groups can be highly beneficial in relieving preoperative and postoperative anxiety and in promoting healthy coping. This is preferable to antianxiety medications. Downplaying the risks of surgery or focusing solely on the benefits is a simplistic and patronizing approach. 22. A patient has just been diagnosed with acute gastritis after presenting in distress to the emergency department with abdominal symptoms. What would be the nursing care most needed by the patient at this time? A) Teaching the patient about necessary nutritional modification B) Helping the patient weigh treatment options C) Teaching the patient about the etiology of gastritis D) Providing the patient with physical and emotional support D Feedback: For acute gastritis, the nurse provides physical and emotional support and helps the patient manage the symptoms, which may include nausea, vomiting, heartburn, and fatigue. The scenario describes a newly diagnosed patient; teaching about the etiology of the disease, lifestyle modifications, or various treatment options would be best provided at a later time. A nurse is providing care for a patient who is postoperative day 2 following gastric surgery. The nurses assessment should be planned in light of the possibility of what potential complications? Select all that apply. A) Malignant hyperthermia B) Atelectasis C) Pneumonia D) Metabolic imbalances E) Chronic gastritis B, C, D Feedback: After surgery, the nurse assesses the patient for complications secondary to the surgical intervention, such as pneumonia, atelectasis, or metabolic imbalances resulting from the GI disruption. Malignant hyperthermia is an intraoperative complication. Chronic gastritis is not a surgical complication. 24. A patient is undergoing diagnostic testing for a tumor of the small intestine. What are the most likely symptoms that prompted the patient to first seek care? A) Hematemesis and persistent sensation of fullness B) Abdominal bloating and recurrent constipation C) Intermittent pain and bloody stool D) Unexplained bowel incontinence and fatty stools C Feedback: When the patient is symptomatic from a tumor of the small intestine, benign tumors often present with intermittent pain. The next most common presentation is occult bleeding. The other listed signs and symptoms are not normally associated with the presentation of small intestinal tumors. 25. A patient is recovering in the hospital following gastrectomy. The nurse notes that the patient has become increasingly difficult to engage and has had several angry outbursts at various staff members in recent days. The nurses attempts at therapeutic dialogue have been rebuffed. What is the nurses most appropriate action? A) Ask the patients primary care provider to liaise between the nurse and the patient. B) Delegate care of the patient to a colleague. C) Limit contact with the patient in order to provide privacy. D) Make appropriate referrals to services that provide psychosocial support. D Feedback: The nurse should enlist the services of clergy, psychiatric clinical nurse specialists, psychologists, social workers, and psychiatrists, if needed. This is preferable to delegating care, since the patient has become angry with other care providers as well. It is impractical and inappropriate to expect the primary care provider to act as a liaison. It would be inappropriate and unsafe to simply limit contact with the patient. 26. A patient has been admitted to the hospital after diagnostic imaging revealed the presence of a gastric outlet obstruction (GOO). What is the nurses priority intervention? A) Administration of antiemetics B) Insertion of an NG tube for decompression C) Infusion of hypotonic IV solution D) Administration of proton pump inhibitors as ordered B Feedback: In treating the patient with gastric outlet obstruction, the first consideration is to insert an NG tube to decompress the stomach. This is a priority over fluid or medication administration. 27. A patient with a history of peptic ulcer disease has presented to the emergency department (ED) in distress. What assessment finding would lead the ED nurse to suspect that the patient has a perforated ulcer? A) The patient has abdominal bloating that developed rapidly. B) The patient has a rigid, boardlike abdomen that is tender. C) The patient is experiencing intense lower right quadrant pain. D) The patient is experiencing dizziness and confusion with no apparent hemodynamic changes. B Feedback: An extremely tender and rigid (boardlike) abdomen is suggestive of a perforated ulcer. None of the other listed signs and symptoms is suggestive of a perforated ulcer. 28. Diagnostic imaging and physical assessment have revealed that a patient with peptic ulcer disease has suffered a perforated ulcer. The nurse recognizes that emergency interventions must be performed as soon as possible in order to prevent the development of what complication? A) Peritonitis B) Gastritis C) Gastroesophageal reflux D) Acute pancreatitis A Feedback: Perforation is the erosion of the ulcer through the gastric serosa into the peritoneal cavity without warning. Chemical peritonitis develops within a few hours of perforation and is followed by bacterial peritonitis. Gastritis, reflux, and pancreatitis are not acute complications of a perforated ulcer. 29. A nurse is performing the admission assessment of a patient whose high body mass index (BMI) corresponds to class III obesity. In order to ensure empathic and patient-centered care, the nurse should do which of the following? A) Examine ones own attitudes towards obesity in general and the patient in particular. B) Dialogue with the patient about the lifestyle and psychosocial factors that resulted in obesity. C) Describe ones own struggles with weight gain and weight loss to the patient. D) Elicit the patients short-term and long-term goals for weight loss. A Feedback: Studies suggest that health care providers, including nurses, harbor negative attitudes towards obese patients. Nurses have a responsibility to examine these attitudes and change them accordingly. This is foundational to all other areas of assessing this patient. 30. A patient has been prescribed orlistat (Xenical) for the treatment of obesity. When providing relevant health education for this patient, the nurse should ensure the patient is aware of what potential adverse effect of treatment? A) Bowel incontinence B) Flatus with oily discharge C) Abdominal pain D) Heat intolerance B Feedback: Side effects of orlistat include increased frequency of bowel movements, gas with oily discharge, decreased food absorption, decreased bile flow, and decreased absorption of some vitamins. This drug does not cause bowel incontinence, abdominal pain, or heat intolerance. 31. A patient who is obese has been unable to lose weight successfully using lifestyle modifications and has mentioned the possibility of using weight-loss medications. What should the nurse teach the patient about pharmacologic interventions for the treatment of obesity? A) Weight loss drugs have many side effects, and most doctors think theyll all be off the market in a few years. B) There used to be a lot of hope that medications would help people lose weight, but its been shown to be mostly a placebo effect. C) Medications can be helpful, but few people achieve and maintain their desired weight loss with medications alone. D) Medications are rapidly become the preferred method of weight loss in people for whom diet and exercise have not worked. C Feedback: Though antiobesity drugs help some patients lose weight, their use rarely results in loss of more than 10% of total body weight. Patients are consequently unlikely to attain their desired weight through medication alone. They are not predicted to disappear from the market and results are not attributed to a placebo effect. 32. A patient has been diagnosed with peptic ulcer disease and the nurse is reviewing his prescribed medication regimen with him. What is currently the most commonly used drug regimen for peptic ulcers? A) Bismuth salts, antivirals, and histamine-2 (H2) antagonists B) H2 antagonists, antibiotics, and bicarbonate salts C) Bicarbonate salts, antibiotics, and ZES D) Antibiotics, proton pump inhibitors, and bismuth salts D Feedback: Currently, the most commonly used therapy for peptic ulcers is a combination of antibiotics, proton pump inhibitors, and bismuth salts that suppress or eradicate H. pylori. H2 receptor antagonists are used to treat NSAID-induced ulcers and other ulcers not associated with H. pylori infection, but they are not the drug of choice. Bicarbonate salts are not used. ZES is the Zollinger-Ellison syndrome and not a drug. 33. A patient who is obese is exploring bariatric surgery options and presented to a bariatric clinic for preliminary investigation. The nurse interviews the patient, analyzing and documenting the data. Which of the following nursing diagnoses may be a contraindication for bariatric surgery? A) Disturbed Body Image Related to Obesity B) Deficient Knowledge Related to Risks and Expectations of Surgery C) Anxiety Related to Surgery D) Chronic Low Self-Esteem Related to Obesity B Feedback: It is expected that patients seeking bariatric surgery may have challenges with body image and self- esteem related to their obesity. Anxiety is also expected when facing surgery. However, if the patients knowledge remains deficient regarding the risks and realistic expectations for surgery, this may show that the patient is not an appropriate surgical candidate. A patient has recently received a diagnosis of gastric cancer; the nurse is aware of the importance of assessing the patients level of anxiety. Which of the following actions is most likely to accomplish this? A) The nurse gauges the patients response to hypothetical outcomes. B) The patient is encouraged to express fears openly. C) The nurse provides detailed and accurate information about the disease. D) The nurse closely observes the patients body language. B Feedback: Encouraging the patient to discuss his or her fears and anxieties is usually the best way to assess a patients anxiety. Presenting hypothetical situations is a surreptitious and possibly inaccurate way of assessing anxiety. Observing body language is part of assessment, but it is not the complete assessment. Presenting information may alleviate anxiety for some patients, but it is not an assessment. 35. A patient has received a diagnosis of gastric cancer and is awaiting a surgical date. During the preoperative period, the patient should adopt what dietary guidelines? A) Eat small, frequent meals with high calorie and vitamin content. B) Eat frequent meals with an equal balance of fat, carbohydrates, and protein. C) Eat frequent, low-fat meals with high protein content. D) Try to maintain the pre-diagnosis pattern of eating. A Feedback: The nurse encourages the patient to eat small, frequent portions of nonirritating foods to decrease gastric irritation. Food supplements should be high in calories, as well as vitamins A and C and iron, to enhance tissue repair. 36. A nurse is caring for a patient who has a diagnosis of GI bleed. During shift assessment, the nurse finds the patient to betachycardic and hypotensive, and the patient has an episode of hematemesis while the nurse is in the room. In addition to monitoring the patients vital signs and level of conscious, what would be a priority nursing action for this patient? A) Place the patient in a prone position. B) Provide the patient with ice water to slow any GI bleeding. C) Prepare for the insertion of an NG tube. D) Notify the physician. D Feedback: The nurse must always be alert for any indicators of hemorrhagic gastritis, which include hematemesis (vomiting of blood), tachycardia, and hypotension. If these occur, the physician is notified and the patients vital signs are monitored as the patients condition warrants. Putting the patient in a prone position could lead to aspiration. Giving ice water is contraindicated as it would stimulate more vomiting. 37. A nurse is caring for a patient hospitalized with an exacerbation of chronic gastritis. What health promotion topic should the nurse emphasize? A) Strategies for maintaining an alkaline gastric environment B) Safe technique for self-suctioning C) Techniques for positioning correctly to promote gastric healing D) Strategies for avoiding irritating foods and beverages D Feedback: Measures to help relieve pain include instructing the patient to avoid foods and beverages that may be irritating to the gastric mucosa and instructing the patient about the correct use of medications to relieve chronic gastritis. An alkaline gastric environment is neither possible nor desirable. There is no plausible need for self-suctioning. Positioning does not have a significant effect on the presence or absence of gastric healing. 38. A patient with gastritis required hospital treatment for an exacerbation of symptoms and receives a subsequent diagnosis of pernicious anemia due to malabsorption. When planning the patients continuing care in the home setting, what assessment question is most relevant? A) Does anyone in your family have experience at giving injections? B) Are you going to be anywhere with strong sunlight in the next few months? C) Are you aware of your blood type? D) Do any of your family members have training in first aid? A Feedback: Patients with malabsorption of vitamin B12 need information about lifelong vitamin B12injections; the nurse may instruct a family member or caregiver how to administer the injections or make arrangements for the patient to receive the injections from a health care provider. Questions addressing sun exposure, blood type and first aid are not directly relevant. 39. A nurse is presenting a class at a bariatric clinic about the different types of surgical procedures offered by the clinic. When describing the implications of different types of surgeries, the nurse should address which of the following topics? Select all that apply. A) Specific lifestyle changes associated with each procedure B) Implications of each procedure for eating habits C) Effects of different surgeries on bowel function D) Effects of various bariatric surgeries on fertility E) Effects of different surgeries on safety of future immunizations A, B, C Feedback: Different bariatric surgical procedures entail different lifestyle modifications; patients must be well informed about the specific lifestyle changes, eating habits, and bowel habits that may result from a particular procedure. Bariatric surgeries do not influence the future use of immunizations or fertility, though pregnancy should be avoided for 18 months after bariatric surgery. 40. A patient has come to the clinic complaining of pain just above her umbilicus. When assessing the patient, the nurse notes Sister Mary Josephs nodules. The nurse should refer the patient to the primary care provider to be assessed for what health problem? A) A GI malignancy B) Dumping syndrome C) Peptic ulcer disease D) Esophageal/gastric obstruction A Feedback: Palpable nodules around the umbilicus, called Sister Mary Josephs nodules, are a sign of a GI malignancy, usually a gastric cancer. This would not be a sign of dumping syndrome, peptic ulcer disease, or esophageal/gastric obstruction. Chapter 47: Management of Patients With Intestinal and Rectal Disorders 1. A nurse is working with a patient who has chronic constipation. What should be included in patient teaching to promote normal bowel function? A) Use glycerin suppositories on a regular basis. B) Limit physical activity in order to promote bowel peristalsis. C) Consume high-residue, high-fiber foods. D) Resist the urge to defecate until the urge becomes intense. C Feedback: Goals for the patient include restoring or maintaining a regular pattern of elimination by responding to the urge to defecate, ensuring adequate intake of fluids and high-fiber foods, learning about methods to avoid constipation, relieving anxiety about bowel elimination patterns, and avoiding complications. Ongoing use of pharmacologic aids should not be promoted, due to the risk of dependence. Increased mobility helps to maintain a regular pattern of elimination. The urge to defecate should be heeded. 2. A nurse is preparing to provide care for a patient whose exacerbation of ulcerative colitis has required hospital admission. During an exacerbation of this health problem, the nurse would anticipate that the patients stools will have what characteristics? A) Watery with blood and mucus B) Hard and black or tarry C) Dry and streaked with blood D) Loose with visible fatty streaks A Feedback: The predominant symptoms of ulcerative colitis are diarrhea and abdominal pain. Stools may be bloody and contain mucus. Stools are not hard, dry, tarry, black or fatty in patients who have ulcerative colitis. 3. A patient has had an ileostomy created for the treatment of irritable bowel disease and the patient is now preparing for discharge. What should the patient be taught about changing this device in the home setting? A) Apply antibiotic ointment as ordered after cleaning the stoma. B) Apply a skin barrier to the peristomal skin prior to applying the pouch. C) Dispose of the clamp with each bag change. D) Cleanse the area surrounding the stoma with alcohol or chlorhexidine. B Feedback: Guidelines for changing an ileostomy appliance are as follows. Skin should be washed with soap and water, and dried. A skin barrier should be applied to the peristomal skin prior to applying the pouch. Clamps are supplied one per box and should be reused with each bag change. Topical antibiotics are not utilized, but an antifungal spray or powder may be used. 4. A patient admitted with acute diverticulitis has experienced a sudden increase in temperature and complains of a sudden onset of exquisite abdominal tenderness. The nurses rapid assessment reveals that the patients abdomen is uncharacteristically rigid on palpation. What is the nurses best response? A) Administer a Fleet enema as ordered and remain with the patient. B) Contact the primary care provider promptly and report these signs of perforation. C) Position the patient supine and insert an NG tube. D) Page the primary care provider and report that the patient may be obstructed. B Feedback: The patients change in status is suggestive of perforation, which is a surgical emergency. Obstruction does not have this presentation involving fever and abdominal rigidity. An enema would be strongly contraindicated. An order is needed for NG insertion and repositioning is not a priority. 5. A 35-year-old male patient presents at the emergency department with symptoms of a small bowel obstruction. In collaboration with the primary care provider, what intervention should the nurse prioritize? A) Insertion of a nasogastric tube B) Insertion of a central venous catheter C) Administration of a mineral oil enema D) Administration of a glycerin suppository and an oral laxative A Feedback: Decompression of the bowel through a nasogastric tube is necessary for all patients with small bowel obstruction. Peripheral IV access is normally sufficient. Enemas, suppositories, and laxatives are not indicated if an obstruction is present. 6. A patient admitted with inflammatory bowel disease asks the nurse for help with menu selections. What menu selection is most likely the best choice for this patient? A) Spinach B) Tofu C) Multigrain bagel D) Blueberries B Feedback: Nutritional management of inflammatory bowel disease requires ingestion of a diet that is bland, low- residue, high-protein, and high-vitamin. Tofu meets each of the criteria. Spinach, multigrain bagels, and blueberries are not low-residue. 7. A patient is admitted to the medical unit with a diagnosis of intestinal obstruction. When planning this patients care, which of the following nursing diagnoses should the nurse prioritize? A) Ineffective Tissue Perfusion Related to Bowel Ischemia B) Imbalanced Nutrition: Less Than Body Requirements Related to Impaired Absorption C) Anxiety Related to Bowel Obstruction and Subsequent Hospitalization D) Impaired Skin Integrity Related to Bowel Obstruction A Feedback: When the bowel is completely obstructed, the possibility of strangulation and tissue necrosis (i.e., tissue death) warrants surgical intervention. As such, this immediate physiologic need is a nursing priority. Nutritional support and management of anxiety are necessary, but bowel ischemia is a more immediate threat. Skin integrity is not threatened. 8. A nurse is presenting an educational event to a local community group. When speaking about colorectal cancer, what risk factor should the nurse cite? A) High levels of alcohol consumption B) History of bowel obstruction C) History of diverticulitis D) Longstanding psychosocial stress A Feedback: Risk factors include high alcohol intake; cigarette smoking; and high-fact, high-protein, low-fiber diet. Diverticulitis, obstruction, and stress are not noted as risk factors for colorectal cancer. 9. A patients screening colonoscopy revealed the presence of numerous polyps in the large bowel. What principle should guide the subsequent treatment of this patients health problem? A) Adherence to a high-fiber diet will help the polyps resolve. B) The patient should be assured that these are a normal, age-related physiologic change. C) The patients polyps constitute a risk factor for cancer. D) The presence of polyps is associated with an increased risk of bowel obstruction. C Feedback: Although most polyps do not develop into invasive neoplasms, they must be identified and followed closely. They are very common, but are not classified as a normal, age-related physiologic change. Diet will not help them resolve and they do not typically lead to obstructions. 10. A nursing instructor is discussing hemorrhoids with the nursing class. Which patients would the nursing instructor identify as most likely to develop hemorrhoids? A) A 45-year-old teacher who stands for 6 hours per day B) A pregnant woman at 28 weeks gestation C) A 37-year-old construction worker who does heavy lifting D) A 60-year-old professional who is under stress B Feedback: Hemorrhoids commonly affect 50% of patients after the age of 50. Pregnancy may initiate hemorrhoids or aggravate existing ones. This is due to increased constipation during pregnancy. The significance of pregnancy is greater than that of standing, lifting, or stress in the development of hemorrhoids. A nurse is planning discharge teaching for a 21-year-old patient with a new diagnosis of ulcerative colitis. When planning family assessment, the nurse should recognize that which of the following factors will likely have the greatest impact on the patients coping after discharge? A) The familys ability to take care of the patients special diet needs B) The familys ability to monitor the patients changing health status C) The familys ability to provide emotional support D) The familys ability to manage the patients medication regimen C Feedback: Emotional support from the family is key to the patients coping after discharge. A 21-year-old would be expected to self-manage the prescribed medication regimen and the family would not be primarily responsible for monitoring the patients health status. It is highly beneficial if the family is willing and able to accommodate the patients dietary needs, but emotional support is paramount and cannot be solely provided by the patient alone. 12. An older adult who resides in an assisted living facility has sought care from the nurse because of recurrent episodes of constipation. Which of the following actions should the nurse first perform? A) Encourage the patient to take stool softener daily. B) Assess the patients food and fluid intake. C) Assess the patients surgical history. D) Encourage the patient to take fiber supplements. B Feedback: The nurse should follow the nursing process and perform an assessment prior to interventions. The patients food and fluid intake is more likely to affect bowel function than surgery. 13. A 16-year-old presents at the emergency department complaining of right lower quadrant pain and is subsequently diagnosed with appendicitis. When planning this patients nursing care, the nurse should prioritize what nursing diagnosis? A) Imbalanced Nutrition: Less Than Body Requirements Related to Decreased Oral Intake B) Risk for Infection Related to Possible Rupture of Appendix C) Constipation Related to Decreased Bowel Motility and Decreased Fluid Intake D) Chronic Pain Related to Appendicitis B Feedback: The patient with a diagnosis of appendicitis has an acute risk of infection related to the possibility of rupture. This immediate physiologic risk is a priority over nutrition and constipation, though each of these concerns should be addressed by the nurse. The pain associated with appendicitis is acute, not chronic. 14. A nurse is talking with a patient who is scheduled to have a hemicolectomy with the creation of a colostomy. The patient admits to being anxious, and has many questions concerning the surgery, the care of a stoma, and necessary lifestyle changes. Which of the following nursing actions is most appropriate? A) Reassure the patient that the procedure is relatively low risk and that patients are usually successful in adjusting to an ostomy. B) Provide the patient with educational materials that match the patients learning style. C) Encourage the patient to write down these concerns and questions to bring forward to the surgeon. D) Maintain an open dialogue with the patient and facilitate a referral to the wound-ostomy- continence (WOC) nurse. D Feedback: A wound-ostomy-continence (WOC) nurse is a registered nurse who has received advanced education in an accredited program to care for patients with stomas. The enterostomal nurse therapist can assist with the selection of an appropriate stoma site, teach about stoma care, and provide emotional support. The surgeon is less likely to address the patients psychosocial and learning needs. Reassurance does not address the patients questions, and education may or may not alleviate anxiety. 15. A nurse is caring for a patient with constipation whose primary care provider has recommended senna (Senokot) for the management of this condition. The nurse should provide which of the following education points? A) Limit your fluid intake temporarily so you dont get diarrhea. B) Avoid taking the drug on a long-term basis. C) Make sure to take a multivitamin with each dose. D) Take this on an empty stomach to ensure maximum effect. B Feedback: Laxatives should not be taken on an ongoing basis in order to reduce the risk of dependence. Fluid should be increased, not limited, and there is no need to take each dose with a multivitamin. Senna does not need to be taken on an empty stomach. 16. The nurse is caring for a patient who is undergoing diagnostic testing for suspected malabsorption. When taking this patients health history and performing the physical assessment, the nurse should recognize what finding as most consistent with this diagnosis? A) Recurrent constipation coupled with weight loss B) Foul-smelling diarrhea that contains fat C) Fever accompanied by a rigid, tender abdomen D) Bloody bowel movements accompanied by fecal incontinence B Feedback: The hallmarks of malabsorption syndrome from any cause are diarrhea or frequent, loose, bulky, foul- smelling stools that have increased fat content and are often grayish (steatorrhea). Constipation and bloody bowel movements are not suggestive of malabsorption syndromes. Fever and a tender, rigid abdomen are associated with peritonitis. 17. A nurse is caring for a patient admitted with symptoms of an anorectal infection; cultures indicate that the patient has a viral infection. The nurse should anticipate the administration of what drug? A) Acyclovir (Zovirax) B) Doxycycline (Vibramycin) C) Penicillin (penicillin D) Metronidazole (Flagyl) A Feedback: Acyclovir (Zovirax) is often given to patients with viral anorectal infections. Doxycycline (Vibramycin) and penicillin (penicillin G) are drugs of choice for bacterial infections. Metronidazole (Flagyl) is used for other infections with a bacterial etiology; it is ineffective against viruses. 18. A nurse caring for a patient with colorectal cancer is preparing the patient for upcoming surgery. The nurse administers cephalexin (Keflex) to the patient and explains what rationale? A) To treat any undiagnosed infections B) To reduce intestinal bacteria levels C) To reduce bowel motility D) To reduce abdominal distention postoperatively B Feedback: Antibiotics such a kanamycin (Kantrex), neomycin (Mycifradin), and cephalexin (Keflex) are administered orally the day before surgery to reduce intestinal bacterial. Preoperative antibiotics are not given to treat undiagnosed infections, reduce motility, or prevent abdominal distention. 19. A nurse is teaching a group of adults about screening and prevention of colorectal cancer. The nurse should describe which of the following as the most common sign of possible colon cancer? A) Development of new hemorrhoids B) Abdominal bloating and flank pain C) Unexplained weight gain D) Change in bowel habits D Feedback: The most common presenting symptom associated with colorectal cancer is a change in bowel habits. The passage of blood is the second most common symptom. Symptoms may also include unexplained anemia, anorexia, weight loss, and fatigue. Hemorrhoids and bloating are atypical. 20. A nurse caring for a patient with a newly created ileostomy assesses the patient and notes that the patient has had not ostomy output for the past 12 hours. The patient also complains of worsening nausea. What is the nurses priority action? A) Facilitate a referral to the wound-ostomy-continence (WOC) nurse. B) Report signs and symptoms of obstruction to the physician. C) Encourage the patient to mobilize in order to enhance motility. D) Contact the physician and obtain a swab of the stoma for culture. B Feedback: It is important to report nausea and abdominal distention, which may indicate intestinal obstruction. This requires prompt medical intervention. Referral to the WOC nurse is not an appropriate short-term response, since medical treatment is necessary. Physical mobility will not normally resolve an obstruction. There is no need to collect a culture from the stoma, because infection is unrelated to this problem. 21. A nurse is working with a patient who is learning to care for a continent ileostomy (Kock pouch). Following the initial period of healing, the nurse is teaching the patient how to independently empty the ileostomy. The nurse should teach the patient to do which of the following actions? A) Aim to eventually empty the pouch every 90 minutes. B) Avoid emptying the pouch until it is visibly full. C) Insert the catheter approximately 5 cm into the pouch. D) Aspirate the contents of the pouch using a 60 mL piston syringe. C Feedback: To empty a Kock pouch, the catheter is gently inserted approximately 5 cm to the point of the valve or nipple. The length of time between drainage periods is gradually increased until the reservoir needs to be drained only every 4 to 6 hours and irrigated once each day. It is not appropriate to wait until the pouch is full, and this would not be visible. The contents of the pouch are not aspirated. 22. A nurse is providing care for a patient who has a diagnosis of irritable bowel syndrome (IBS). When planning this patients care, the nurse should collaborate with the patient and prioritize what goal? A) Patient will accurately identify foods that trigger symptoms. B) Patient will demonstrate appropriate care of his ileostomy. C) Patient will demonstrate appropriate use of standard infection control precautions. D) Patient will adhere to recommended guidelines for mobility and activity. A Feedback: A major focus of nursing care for the patient with IBS is to identify factors that exacerbate symptoms. Surgery is not used to treat this health problem and infection control is not a concern that is specific to this diagnosis. Establishing causation likely is more important to the patient than managing physical activity. A patient has been experiencing disconcerting GI symptoms that have been worsening in severity. Following medical assessment, the patient has been diagnosed with lactose intolerance. The nurse should recognize an increased need for what form of health promotion? A) Annual screening colonoscopies B) Adherence to recommended immunization schedules C) Regular blood pressure monitoring D) Frequent screening for osteoporosis D Feedback: Persons with lactose intolerance often experience hypocalcemia and a consequent risk of osteoporosis related to malabsorption of calcium. Lactose intolerance does not create an increased need for screening for colorectal cancer, immunizations, or blood pressure monitoring. 24. An older adult has a diagnosis of Alzheimers disease and has recently been experiencing fecal incontinence. However, the nurse has observed no recent change in the character of the patients stools. What is the nurses most appropriate intervention? A) Keep a food diary to determine the foods that exacerbate the patients symptoms. B) Provide the patient with a bland, low-residue diet. C) Toilet the patient on a frequent, scheduled basis. D) Liaise with the primary care provider to obtain an order for loperamide. C Feedback: Because the patients fecal incontinence is most likely attributable to cognitive decline, frequent toileting is an appropriate intervention. Loperamide is unnecessary in the absence of diarrhea. Specific foods are not likely to be a cause of, or solution to, this patients health problem. 25. An adult patient has been diagnosed with diverticular disease after ongoing challenges with constipation. The patient will be treated on an outpatient basis. What components of treatment should the nurse anticipate? Select all that apply. A) Anticholinergic medications B) Increased fiber intake C) Enemas on alternating days D) Reduced fat intake E) Fluid reduction B, D Feedback: Patients whose diverticular disease does not warrant hospital treatment often benefit from a high-fiber, low-fat diet. Neither enemas nor anticholinergics are indicated, and fluid intake is encouraged. 26. A patients health history is suggestive of inflammatory bowel disease. Which of the following would suggest Crohns disease, rather that ulcerative colitis, as the cause of the patients signs and symptoms? A) A pattern of distinct exacerbations and remissions B) Severe diarrhea C) An absence of blood in stool D) Involvement of the rectal mucosa C Feedback: Bloody stool is far more common in cases of UC than in Crohns. Rectal involvement is nearly 100% in cases of UC (versus 20% in Crohns) and patients with UC typically experience severe diarrhea. UC is also characterized by a pattern of remissions and exacerbations, while Crohns often has a more prolonged and variable course. 27. During a patients scheduled home visit, an older adult patient has stated to the community health nurse that she has been experiencing hemorrhoids of increasing severity in recent months. The nurse should recommend which of the following? A) Regular application of an OTC antibiotic ointment B) Increased fluid and fiber intake C) Daily use of OTC glycerin suppositories D) Use of an NSAID to reduce inflammation B Feedback: Hemorrhoid symptoms and discomfort can be relieved by good personal hygiene and by avoiding excessive straining during defecation. A high-residue diet that contains fruit and bran along with an increased fluid intake may be all the treatment that is necessary to promote the passage of soft, bulky stools to prevent straining. Antibiotics, regular use of suppositories, and NSAIDs are not recommended, as they do not address the etiology of the health problem. 28. A nurse is providing care for a patient whose recent colostomy has contributed to a nursing diagnosis of Disturbed Body Image Related to Colostomy. What intervention best addresses this diagnosis? A) Encourage the patient to conduct online research into colostomies. B) Engage the patient in the care of the ostomy to the extent that the patient is willing. C) Emphasize the fact that the colostomy was needed to alleviate a much more serious health problem. D) Emphasize the fact that the colostomy is temporary measure and is not permanent. B Feedback: For some patients, becoming involved in the care of the ostomy helps to normalize it and enhance familiarity. Emphasizing the benefits of the intervention is unlikely to improve the patients body image, since the benefits are likely already known. Online research is not likely to enhance the patients body image and some ostomies are permanent. 29. A nurse is caring for a patient who has been admitted to the hospital with diverticulitis. Which of the following would be appropriate nursing diagnoses for this patient? Select all that apply. A) Acute Pain Related to Increased Peristalsis and GI Inflammation B) Activity Intolerance Related to Generalized Weakness C) Bowel Incontinence Related to Increased Intestinal Peristalsis D) Deficient Fluid Volume Related to Anorexia, Nausea, and Diarrhea E) Impaired Urinary Elimination Related to GI Pressure on the Bladder A, B, D Feedback: Patients with diverticulitis are likely to experience pain and decreased activity levels, and are at risk of fluid volume deficit. The patient is unlikely to experience fecal incontinence and urinary function is not directly influenced. 30. The nurse is providing care for a patient whose inflammatory bowel disease has necessitated hospital treatment. Which of the following would most likely be included in the patients medication regimen? A) Anticholinergic medications 30 minutes before a meal B) Antiemetics on a PRN basis C) Vitamin B12 injections to prevent pernicious anemia D) Beta adrenergic blockers to reduce bowel motility A Feedback: The nurse administers anticholinergic medications 30 minutes before a meal as prescribed to decrease intestinal motility and administers analgesics as prescribed for pain. Antiemetics, vitamin B12 injections and beta blockers do not address the signs, symptoms, or etiology of inflammatory bowel disease. 31. A patients colorectal cancer has necessitated a hemicolectomy with the creation of a colostomy. In the 4 days since the surgery, the patient has been unwilling to look at the ostomy or participate in any aspects of ostomy care. What is the nurses most appropriate response to this observation? A) Ensure that the patient knows that he or she will be responsible for care after discharge. B) Reassure the patient that many people are fearful after the creation of an ostomy. C) Acknowledge the patients reluctance and initiate discussion of the factors underlying it. D) Arrange for the patient to be seen by a social worker or spiritual advisor. C Feedback: If the patient is reluctant to participate in ostomy care, the nurse should attempt to dialogue about this with the patient and explore the factors that underlie it. It is presumptive to assume that the patients behavior is motivated by fear. Assessment must precede referrals and emphasizing the patients responsibilities may or may not motivate the patient. 32. A nurse is caring for an older adult who has been experiencing severe Clostridium difficile-related diarrhea. When reviewing the patients most recent laboratory tests, the nurse should prioritize which of the following? A) White blood cell level B) Creatinine level C) Hemoglobin level D) Potassium level D Feedback: In elderly patients, it is important to monitor the patients serum electrolyte levels closely. Diarrhea is less likely to cause an alteration in white blood cell, creatinine, and hemoglobin levels. 33. A nurse is assessing a patients stoma on postoperative day 3. The nurse notes that the stoma has a shiny appearance and a bright red color. How should the nurse best respond to this assessment finding? A) Irrigate the ostomy to clear a possible obstruction. B) Contact the primary care provider to report this finding. C) Document that the stoma appears healthy and well perfused. D) Document a nursing diagnosis of Impaired Skin Integrity. C Feedback: A healthy, viable stoma should be shiny and pink to bright red. This finding does not indicate that the stoma is blocked or that skin integrity is compromised. 34. A patient has been diagnosed with a small bowel obstruction and has been admitted to the medical unit. The nurses care should prioritize which of the following outcomes? A) Preventing infection B) Maintaining skin and tissue integrity C) Preventing nausea and vomiting D) Maintaining fluid and electrolyte balance D Feedback: All of the listed focuses of care are important for the patient with a small bowel obstruction. However, the patients risk of fluid and electrolyte imbalances is an immediate threat to safety, and is a priority in nursing assessment and interventions. 35. A patients large bowel obstruction has failed to resolve spontaneously and the patients worsening condition has warranted admission to the medical unit. Which of the following aspects of nursing care is most appropriate for this patient? A) Administering bowel stimulants as ordered B) Administering bulk-forming laxatives as ordered C) Performing deep palpation as ordered to promote peristalsis D) Preparing the patient for surgical bowel resection D Feedback: The usual treatment for a large bowel obstruction is surgical resection to remove the obstructing lesion. Administration of laxatives or bowel stimulants are contraindicated if the bowel is obstructed. Palpation would be painful and has no therapeutic benefit. 36. A patient has been experiencing occasional episodes of constipation and has been unable to achieve consistent relief by increasing physical activity and improving his diet. What pharmacologic intervention should the nurse recommend to the patient for ongoing use? A) Mineral oil enemas B) Bisacodyl (Dulcolax) C) Senna (Senokot) D) Psyllium hydrophilic mucilloid (Metamucil) D Feedback: Psyllium hydrophilic mucilloid (Metamucil) is a bulk-forming laxative that is safe for ongoing use. None of the other listed laxatives should be used on an ongoing basis because of the risk of dependence. 37. A patient with a diagnosis of colon cancer is 2 days postoperative following bowel resection and anastomosis. The nurse has planned the patients care in the knowledge of potential complications. What assessment should the nurse prioritize? A) Close monitoring of temperature B) Frequent abdominal auscultation C) Assessment of hemoglobin, hematocrit, and red blood cell levels D) Palpation of peripheral pulses and leg girth B Feedback: After bowel surgery, it is important to frequently assess the abdomen, including bowel sounds and abdominal girth, to detect bowel obstruction. The resumption of bowel motility is a priority over each of the other listed assessments, even though each should be performed by the nurse. A teenage patient with a pilonidal cyst has been brought for care by her mother. The nurse who is contributing to the patients care knows that treatment will be chosen based on what risk? A) Risk for infection B) Risk for bowel incontinence C) Risk for constipation D) Risk for impaired tissue perfusion A Feedback: Pilonidal cysts frequently develop into an abscess, necessitating surgical repair. These cysts do not contribute to bowel incontinence, constipation, or impaired tissue perfusion. 39. A nurse at an outpatient surgery center is caring for a patient who had a hemorrhoidectomy. What discharge education topics should the nurse address with this patient? A) The appropriate use of antibiotics to prevent postoperative infection B) The correct procedure for taking a sitz bath C) The need to eat a low-residue, low-fat diet for the next 2 weeks D) The correct technique for keeping the perianal region clean without the use of water B Feedback: Sitz baths are usually indicated after perianal surgery. A low-residue, low-fat diet is not necessary and water is used to keep the region clean. Postoperative antibiotics are not normally prescribed. 40. Which of the following is the most plausible nursing diagnosis for a patient whose treatment for colon cancer has necessitated a colonostomy? A) Risk for Unstable Blood Glucose Due to Changes in Digestion and Absorption B) Unilateral Neglect Related to Decreased Physical Mobility C) Risk for Excess Fluid Volume Related to Dietary Changes and Changes In Absorption D) Ineffective Sexuality Patterns Related to Changes in Self-Concept D Feedback: The presence of an ostomy frequently has an effect on sexuality; this should be addressed thoughtfully in nursing care. None of the other listed diagnoses reflects the physiologic changes that result from colorectal surgery. Chapter 48: Assessment and Management of Patients with Obesity 1. Which statement by the nurse is most likely to help a morbidly obese 22-year-old man in losing weight on a 1000-calorie diet? A) It will be necessary to change lifestyle habits permanently to maintain weight loss. B) You will decrease your risk for future health problems such as diabetes by losing weight now. C) You are likely to notice changes in how you feel with just a few weeks of diet and exercise. D) Most of the weight that you lose during the first weeks of dieting is water weight rather than fat. C Feedback: Motivation is a key factor in successful weight loss and a short-term outcome provides a higher motivation. A 22-year-old patient is unlikely to be motivated by future health problems. Telling a patient that the initial weight loss is water will be discouraging, although this may be correct. Changing lifestyle habits is necessary, but this process occurs over time and discussing this is not likely to motivate the patient. 2. After the nurse teaches a patient about the recommended amounts of foods from animal and plant sources, which menu selections indicate that the initial instructions about diet have been understood? A) 3 oz of lean beef, 2 oz of low-fat cheese, and a tomato slice B) 3 oz of roasted pork, a cup of corn, and a cup of carrot sticks C) Cup of tossed salad and nonfat dressing topped with a chicken breast D) Half cup of tuna mixed with nonfat mayonnaise and a half cup of celery B Feedback: This selection is most consistent with the recommendation of the American Institute for Cancer Research that one third of the diet should be from animal sources and two thirds from plant source foods. The other choices all have higher ratios of animal origin foods to plant source foods than would be recommended. 3. Which nursing action is appropriate when coaching obese adults enrolled in a behavior modification program? A) Having the adults write down the caloric intake of each meal B) Asking the adults about situations that tend to increase appetite C) Suggesting that the adults plan rewards, such as sugarless candy, for achieving their goals D) Encouraging the adults to eat small amounts frequently rather than having scheduled meals B Feedback: Behavior modification programs focus on how and when the person eats and de-emphasize aspects such as calorie counting. Nonfood rewards are recommended for achievement of weight-loss goals. Patients are often taught to restrict eating to designated meals when using behavior modification. 4. The nurse is coaching a community group for individuals who are overweight. Which participant behavior is an example of the best exercise plan for weight loss? A) Walking for 40 minutes 6 or 7 days/week B) Lifting weights with friends 3 times/week C) Playing soccer for an hour on the weekend D) Running for 10 to 15 minutes 3 times/week A Feedback: Exercise should be done daily for 30 minutes to an hour. Exercising in highly aerobic activities for short bursts or only once a week is not helpful and may be dangerous in an individual who has not been exercising. Running may be appropriate, but a patient should start with an exercise that is less stressful and can be done for a longer period. Weight lifting is not as helpful as aerobic exercise in weight loss. 5. A few months after bariatric surgery, a 56-year-old man tells the nurse, My skin is hanging in folds. I think I need cosmetic surgery. Which response by the nurse is most appropriate? A) The important thing is that you are improving your health. B) The skinfolds will disappear once most of the weight is lost. C) Cosmetic surgery is a possibility once your weight has stabilized. D) Perhaps you would like to talk to a counselor about your body image. C Feedback: Reconstructive surgery may be used to eliminate excess skinfolds after at least a year has passed since the surgery. Skinfolds may not disappear over time, especially in older patients. The response, The important thing is that your weight loss is improving your health, ignores the patients concerns about appearance and implies that the nurse knows what is important. Whereas it may be helpful for the patient to talk to a counselor, it is more likely to be helpful to know that cosmetic surgery is available. 6. After vertical banded gastroplasty, a 42-year-old male patient returns to the surgical nursing unit with a nasogastric tube to low, intermittent suction and a patient-controlled analgesia (PCA) machine for pain control. Which nursing action should be included in the postoperative plan of care? A) Offer sips of fruit juices at frequent intervals. B) Irrigate the nasogastric (NG) tube frequently. C) Remind the patient that PCA use may slow the return of bowel function. D) Support the surgical incision during patient coughing and turning in bed. D Feedback: The incision should be protected from strain to decrease the risk for wound dehiscence. The patient should be encouraged to use the PCA because pain control will improve the cough effort and patient mobility. NG irrigation may damage the suture line or overfill the stomach pouch. Sugar-free clear liquids are offered during the immediate postoperative time to decrease the risk for dumping syndrome. 7. The nurse will be teaching self-management to patients after gastric bypass surgery. Which information will the nurse plan to include? A) Drink fluids between meals but not with meals. B) Choose high-fat foods for at least 30% of intake. C) Developing flabby skin can be prevented by exercise. D) Choose foods high in fiber to promote bowel function. A Feedback: Intake of fluids with meals tends to cause dumping syndrome and diarrhea. Food choices should be low in fat and fiber. Exercise does not prevent the development of flabby skin. 8. Which assessment action will help the nurse determine if an obese patient has metabolic syndrome? A) Take the patients apical pulse. B) Check the patients blood pressure. C) Ask the patient about dietary intake. D) Dipstick the patients urine for protein. B Feedback: Elevated blood pressure is one of the characteristics of metabolic syndrome. The other information also may be obtained by the nurse, but it will not assist with the diagnosis of metabolic syndrome. 9. When teaching a patient about testing to diagnose metabolic syndrome, which topic would the nurse include? A) Blood glucose test B) Cardiac enzyme tests C) Postural blood pressures D) Resting electrocardiogram A Feedback: A fasting blood glucose test >100 mg/dL is one of the diagnostic criteria for metabolic syndrome. The other tests are not used to diagnose metabolic syndrome although they may be used to check for cardiovascular complications of the disorder. 10. What information will the nurse include for an overweight 35-year-old woman who is starting a weight- loss plan? A) Weigh yourself at the same time every morning and evening. B) Stick to a 600- to 800-calorie diet for the most rapid weight loss. C) Low carbohydrate diets lead to rapid weight loss but are difficult to maintain. D) Weighing all foods on a scale is necessary to choose appropriate portion sizes. C Feedback: The restrictive nature of fad diets makes the weight loss achieved by the patient more difficult to maintain. Portion size can be estimated in other ways besides weighing. Severely calorie-restricted diets are not necessary for patients in the overweight category of obesity and need to be closely supervised. Patients should weigh weekly rather than daily. 11. Which adult will the nurse plan to teach about risks associated with obesity? A) Man who has a BMI of 18 kg/m2 B) Man with a 42 in waist and 44 in hips C) Woman who has a body mass index (BMI) of 24 kg/m2 D) Woman with a waist circumference of 34 inches (86 cm) B Feedback: The waist-to-hip ratio for this patient is 0.95, which exceeds the recommended level of <0.80. A patient with a BMI of 18 kg/m2 is considered underweight. A BMI of 24 kg/m2 is normal. Health risks associated with obesity increase in women with a waist circumference larger than 35 in (89 cm) and men with a waist circumference larger than 40 in (102 cm). 12. A 61-year-old man is being admitted for bariatric surgery. Which nursing action can the nurse delegate to unlicensed assistive personnel (UAP)? A) Demonstrate use of the incentive spirometer. B) Plan methods for bathing and turning the patient. C) Assist with IV insertion by holding adipose tissue out of the way. D) Develop strategies to provide privacy and decrease embarrassment. C Feedback: UAP can assist with IV placement by assisting with patient positioning or holding skinfolds aside. Planning for care and patient teaching require registered nurse (RN)level education and scope of practice. 13. After successfully losing 1 lb weekly for several months, a patient at the clinic has not lost any weight for the last month. The nurse should first A) review the diet and exercise guidelines with the patient. B) instruct the patient to weigh and record weights weekly. C) ask the patient whether there have been any changes in exercise or diet patterns. D) discuss the possibility that the patient has reached a temporary weight loss plateau. C Feedback: The initial nursing action should be assessment of any reason for the change in weight loss. The other actions may be needed, but further assessment is required before any interventions are planned or implemented. 14. Which finding for a patient who has been taking orlistat (Xenical) is most important to report to the health care provider? A) The patient frequently has liquid stools. B) The patient is pale and has many bruises. C) The patient complains of bloating after meals. D) The patient is experiencing a weight loss plateau. B Feedback: Because orlistat blocks the absorption of fat-soluble vitamins, the patient may not be receiving an adequate amount of vitamin K, resulting in a decrease in clotting factors. Abdominal bloating and liquid stools are common side effects of orlistat and indicate that the nurse should remind the patient that fat in the diet may increase these side effects. Weight loss plateaus are normal during weight reduction. 15. A 40-year-old obese woman reports that she wants to lose weight. Which question should the nurse ask first? A) What factors led to your obesity? B) Which types of food do you like best? C) How long have you been overweight? D) What kind of activities do you enjoy? A Feedback: The nurse should obtain information about the patients perceptions of the reasons for the obesity to develop a plan individualized to the patient. The other information also will be obtained from the patient, but the patient is more likely to make changes when the patients beliefs are considered in planning. 16. The nurse is caring for a 54-year-old female patient on the first postoperative day after a Roux-en-Y gastric bypass procedure. Which assessment finding should be reported immediately to the surgeon? A) Bilateral crackles audible at both lung bases B) Redness, irritation, and skin breakdown in skinfolds C) Emesis of bile-colored fluid past the nasogastric (NG) tube D) Use of patient-controlled analgesia (PCA) several times an hour for pain C Feedback: Vomiting with an NG tube in place indicates that the NG tube needs to be repositioned by the surgeon to avoid putting stress on the gastric sutures. The nurse should implement actions to decrease skin irritation and have the patient cough and deep breathe, but these do not indicate a need for rapid notification of the surgeon. Frequent PCA use after bariatric surgery is expected. 17. Which information will the nurse prioritize in planning preoperative teaching for a patient undergoing a Roux-en-Y gastric bypass? A) Educating the patient about the nasogastric (NG) tube B) Instructing the patient on coughing and breathing techniques C) Discussing necessary postoperative modifications in lifestyle D) Demonstrating passive range-of-motion exercises for the legs B Feedback: Coughing and deep breathing can prevent major postoperative complications such as carbon monoxide retention and hypoxemia. Information about passive range of motion, the NG tube, and postoperative modifications in lifestyle will also be discussed, but avoidance of respiratory complications is the priority goal after surgery. 18. After bariatric surgery, a patient who is being discharged tells the nurse, I prefer to be independent. I am not interested in any support groups. Which response by the nurse is best? A) I hope you change your mind so that I can suggest a group for you. B) Tell me what types of resources you think you might use after this surgery. C) Support groups have been found to lead to more successful weight loss after surgery. D) Because there are many lifestyle changes after surgery, we recommend support groups. B Feedback: This statement allows the nurse to assess the individual patients potential needs and preferences. The other statements offer the patient more information about the benefits of support groups, but fail to acknowledge the patients preferences. 19. A client has been prescribed lorcaserin (Belviq). What teaching is most appropriate? A) Increase the fiber and water in your diet. B) Reduce fat to less than 30% each day. C) Report dry mouth and decreased sweating. D) Lorcaserin may cause loose stools for a few days. A Feedback: This drug can cause constipation, so the client should increase fiber and water in the diet to prevent this from occurring. Reducing fat in the diet is important with orlistat. Lorcaserin can cause dry mouth but not decreased sweating. Loose stools are common with orlistat. 20. A client just returned to the surgical unit after a gastric bypass. What action by the nurse is the priority? A) Assess the clients pain. B) Check the surgical incision. C) Ensure an adequate airway. D) Program the morphine pump. C Feedback: All actions are appropriate care measures for this client; however, airway is always the priority. Bariatric clients tend to have short, thick necks that complicate airway management. 21. A client is in the bariatric clinic 1 month after having gastric bypass surgery. The client is crying and says I didnt know it would be this hard to live like this. What response by the nurse is best? A) Assess the clients coping and support systems. B) Inform the client that things will get easier. C) Re-educate the client on needed dietary changes. D) Tell the client lifestyle changes are always hard. A Feedback: The nurse should assess this clients coping styles and support systems in order to provide holistic care. The other options do not address the clients distress. 22. A client is awaiting bariatric surgery in the morning. What action by the nurse is most important? A) Answering questions the client has about surgery B) Beginning venous thromboembolism prophylaxis C) Informing the client that he or she will be out of bed tomorrow D) Teaching the client about needed dietary changes B Feedback: Morbidly obese clients are at high risk of venous thromboembolism and should be started on a regimen to prevent this from occurring as a priority. Answering questions about the surgery is done by the surgeon. Teaching is important, but safety comes first. Chapter 49: Assessment and Management of Patients with Hepatic Disorders 1. A nurse is caring for a patient with liver failure and is performing an assessment in the knowledge of the patients increased risk of bleeding. The nurse recognizes that this risk is related to the patients inability to synthesize prothrombin in the liver. What factor most likely contributes to this loss of function? A) Alterations in glucose metabolism B) Retention of bile salts C) Inadequate production of albumin by hepatocytes D) Inability of the liver to use vitamin K D Feedback: Decreased production of several clotting factors may be partially due to deficient absorption of vitamin K from the GI tract. This probably is caused by the inability of liver cells to use vitamin K to make prothrombin. This bleeding risk is unrelated to the roles of glucose, bile salts, or albumin. 2. A nurse is performing an admission assessment of a patient with a diagnosis of cirrhosis. What technique should the nurse use to palpate the patients liver? A) Place hand under the right lower abdominal quadrant and press down lightly with the other hand. B) Place the left hand over the abdomen and behind the left side at the 11th rib. C) Place hand under right lower rib cage and press down lightly with the other hand. D) Hold hand 90 degrees to right side of the abdomen and push down firmly. C Feedback: To palpate the liver, the examiner places one hand under the right lower rib cage and presses downward with light pressure with the other hand. The liver is not on the left side or in the right lower abdominal quadrant. 3. A patient with portal hypertension has been admitted to the medical floor. The nurse should prioritize which of the following assessments related to the manifestations of this health problem? A) Assessment of blood pressure and assessment for headaches and visual changes B) Assessments for signs and symptoms of venous thromboembolism C) Daily weights and abdominal girth measurement D) Blood glucose monitoring q4h C Feedback: Obstruction to blood flow through the damaged liver results in increased blood pressure (portal hypertension) throughout the portal venous system. This can result in varices and ascites in the abdominal cavity. Assessments related to ascites are daily weights and abdominal girths. Portal hypertension is not synonymous with cardiovascular hypertension and does not create a risk for unstable blood glucose or VTE. 4. A nurse educator is teaching a group of recent nursing graduates about their occupational risks for contracting hepatitis B. What preventative measures should the educator promote? Select all that apply. A) Immunization B) Use of standard precautions C) Consumption of a vitamin-rich diet D) Annual vitamin K injections E) Annual vitamin B12 injections A, B Feedback: People who are at high risk, including nurses and other health care personnel exposed to blood or blood products, should receive active immunization. The consistent use of standard precautions is also highly beneficial. Vitamin supplementation is unrelated to an individuals risk of HBV. 5. A nurse is caring for a patient with cancer of the liver whose condition has required the insertion of a percutaneous biliary drainage system. The nurses most recent assessment reveals the presence of dark green fluid in the collection container. What is the nurses best response to this assessment finding? A) Document the presence of normal bile output. B) Irrigate the drainage system with normal saline as ordered. C) Aspirate a sample of the drainage for culture. D) Promptly report this assessment finding to the primary care provider. A Feedback: Bile is usually a dark green or brownish-yellow color, so this would constitute an expected assessment finding, with no other action necessary. 6. A patient who has undergone liver transplantation is ready to be discharged home. Which outcome of health education should the nurse prioritize? A) The patient will obtain measurement of drainage from the T-tube. B) The patient will exercise three times a week. C) The patient will take immunosuppressive agents as required. D) The patient will monitor for signs of liver dysfunction. C Feedback: The patient is given written and verbal instructions about immunosuppressive agent doses and dosing schedules. The patient is also instructed on steps to follow to ensure that an adequate supply of medication is available so that there is no chance of running out of the medication or skipping a dose. Failure to take medications as instructed may precipitate rejection. The nurse would not teach the patient to measure drainage from a T-tube as the patient wouldnt go home with a T-tube. The nurse may teach the patient about the need to exercise or what the signs of liver dysfunction are, but the nurse would not stress these topics over the immunosuppressive drug regimen. 7. A triage nurse in the emergency department is assessing a patient who presented with complaints of general malaise. Assessment reveals the presence of jaundice and increased abdominal girth. What assessment question best addresses the possible etiology of this patients presentation? A) How many alcoholic drinks do you typically consume in a week? B) To the best of your knowledge, are your immunizations up to date? C) Have you ever worked in an occupation where you might have been exposed to toxins? D) Has anyone in your family ever experienced symptoms similar to yours? A Feedback: Signs or symptoms of hepatic dysfunction indicate a need to assess for alcohol use. Immunization status, occupational risks, and family history are also relevant considerations, but alcohol use is a more common etiologic factor in liver disease. 8. A nurse is participating in the emergency care of a patient who has just developed variceal bleeding. What intervention should the nurse anticipate? A) Infusion of intravenous heparin B) IV administration of albumin C) STAT administration of vitamin K by the intramuscular route D) IV administration of octreotide (Sandostatin) D Feedback: Octreotide (Sandostatin)a synthetic analog of the hormone somatostatinis effective in decreasing bleeding from esophageal varices, and lacks the vasoconstrictive effects of vasopressin. Because of this safety and efficacy profile, octreotide is considered the preferred treatment regimen for immediate control of variceal bleeding. Vitamin K and albumin are not administered and heparin would exacerbate, not alleviate, bleeding. 9. A nurse is caring for a patient with hepatic encephalopathy. While making the initial shift assessment, the nurse notes that the patient has a flapping tremor of the hands. The nurse should document the presence of what sign of liver disease? A) Asterixis B) Constructional apraxia C) Fetor hepaticus D) Palmar erythema A Feedback: The nurse will document that a patient exhibiting a flapping tremor of the hands is demonstrating asterixis. While constructional apraxia is a motor disturbance, it is the inability to reproduce a simple figure. Fetor hepaticus is a sweet, slightly fecal odor to the breath and not associated with a motor disturbance. Skin changes associated with liver dysfunction may include palmar erythema, which is a reddening of the palms, but is not a flapping tremor. 10. A local public health nurse is informed that a cook in a local restaurant has been diagnosed with hepatitis A. What should the nurse advise individuals to obtain who ate at this restaurant and have never received the hepatitis A vaccine? A) The hepatitis A vaccine B) Albumin infusion C) The hepatitis A and B vaccines D) An immune globulin injection D Feedback: For people who have not been previously vaccinated, hepatitis A can be prevented by the intramuscular administration of immune globulin during the incubation period, if given within 2 weeks of exposure. Administration of the hepatitis A vaccine will not protect the patient exposed to hepatitis A, as protection will take a few weeks to develop after the first dose of the vaccine. The hepatitis B vaccine provides protection again the hepatitis B virus, but plays no role in protection for the patient exposed to hepatitis A. Albumin confers no therapeutic benefit. 11. A participant in a health fair has asked the nurse about the role of drugs in liver disease. What health promotion teaching has the most potential to prevent drug-induced hepatitis? A) Finish all prescribed courses of antibiotics, regardless of symptom resolution. B) Adhere to dosing recommendations of OTC analgesics. C) Ensure that expired medications are disposed of safely. D) Ensure that pharmacists regularly review drug regimens for potential interactions. B Feedback: Although any medication can affect liver function, use of acetaminophen (found in many over-the- counter medications used to treat fever and pain) has been identified as the leading cause of acute liver failure. Finishing prescribed antibiotics and avoiding expired medications are unrelated to this disease. Drug interactions are rarely the cause of drug-induced hepatitis. 12. Diagnostic testing has revealed that a patients hepatocellular carcinoma (HCC) is limited to one lobe. The nurse should anticipate that this patients plan of care will focus on what intervention? A) Cryosurgery B) Liver transplantation C) Lobectomy D) Laser hyperthermia C Feedback: Surgical resection is the treatment of choice when HCC is confined to one lobe of the liver and the function of the remaining liver is considered adequate for postoperative recovery. Removal of a lobe of the liver (lobectomy) is the most common surgical procedure for excising a liver tumor. While cryosurgery and liver transplantation are other surgical options for management of liver cancer, these procedures are not performed at the same frequency as a lobectomy. Laser hyperthermia is a nonsurgical treatment for liver cancer. 13. A patient has been diagnosed with advanced stage breast cancer and will soon begin aggressive treatment. What assessment findings would most strongly suggest that the patient may have developed liver metastases? A) Persistent fever and cognitive changes B) Abdominal pain and hepatomegaly C) Peripheral edema unresponsive to diuresis D) Spontaneous bleeding and jaundice B Feedback: The early manifestations of malignancy of the liver include paina continuous dull ache in the right upper quadrant, epigastrium, or back. Weight loss, loss of strength, anorexia, and anemia may also occur. The liver may be enlarged and irregular on palpation. Jaundice is present only if the larger bile ducts are occluded by the pressure of malignant nodules in the hilum of the liver. Fever, cognitive changes, peripheral edema, and bleeding are atypical signs. 14. A patient is being discharged after a liver transplant and the nurse is performing discharge education. When planning this patients continuing care, the nurse should prioritize which of the following risk diagnoses? A) Risk for Infection Related to Immunosuppressant Use B) Risk for Injury Related to Decreased Hemostasis C) Risk for Unstable Blood Glucose Related to Impaired Gluconeogenesis D) Risk for Contamination Related to Accumulation of Ammonia A Feedback: Infection is the leading cause of death after liver transplantation. Pulmonary and fungal infections are common; susceptibility to infection is increased by the immunosuppressive therapy that is needed to prevent rejection. This risk exceeds the threats of injury and unstable blood glucose. The diagnosis of Risk for Contamination relates to environmental toxin exposure. 15. A patient with a liver mass is undergoing a percutaneous liver biopsy. What action should the nurse perform when assisting with this procedure? A) Position the patient on the right side with a pillow under the costal margin after the procedure. B) Administer 1 unit of albumin 90 minutes before the procedure as ordered. C) Administer at least 1 unit of packed red blood cells as ordered the day before the scheduled procedure. D) Confirm that the patients electrolyte levels have been assessed prior to the procedure. A Feedback: Immediately after a percutaneous liver biopsy, assist the patient to turn onto the right side and place a pillow under the costal margin. Prior administration of albumin or PRBCs is unnecessary. Coagulation tests should be performed, but electrolyte analysis is not necessary. 16. A nurse is caring for a patient with hepatic encephalopathy. The nurses assessment reveals that the patient exhibits episodes of confusion, is difficult to arouse from sleep and has rigid extremities. Based on these clinical findings, the nurse should document what stage of hepatic encephalopathy? A) Stage 1 B) Stage 2 C) Stage 3 D) Stage 4 C Feedback: Patients in the third stage of hepatic encephalopathy exhibit the following symptoms: stuporous, difficult to arouse, sleeps most of the time, exhibits marked confusion, incoherent in speech, asterixis, increased deep tendon reflexes, rigidity of extremities, marked EEG abnormalities. Patients in stages 1 and 2 exhibit clinical symptoms that are not as advanced as found in stage 3, and patients in stage 4 are comatose. In stage 4, there is an absence of asterixis, absence of deep tendon reflexes, flaccidity of extremities, and EEG abnormalities. 17. A patient has developed hepatic encephalopathy secondary to cirrhosis and is receiving care on the medical unit. The patients current medication regimen includes lactulose (Cephulac) four times daily. What desired outcome should the nurse relate to this pharmacologic intervention? A) Two to 3 soft bowel movements daily B) Significant increase in appetite and food intake C) Absence of nausea and vomiting D) Absence of blood or mucus in stool A Feedback: Lactulose (Cephulac) is administered to reduce serum ammonia levels. Two or three soft stools per day are desirable; this indicates that lactulose is performing as intended. Lactulose does not address the patients appetite, symptoms of nausea and vomiting, or the development of blood and mucus in the stool. 18. A nurse is performing an admission assessment for an 81-year-old patient who generally enjoys good health. When considering normal, age-related changes to hepatic function, the nurse should anticipate what finding? A) Similar liver size and texture as in younger adults B) A nonpalpable liver C) A slightly enlarged liver with palpably hard edges D) A slightly decreased size of the liver D Feedback: The most common age-related change in the liver is a decrease in size and weight. The liver is usually still palpable, however, and is not expected to have hardened edges. 19. A nurse is caring for a patient with a blocked bile duct from a tumor. What manifestation of obstructive jaundice should the nurse anticipate? A) Watery, blood-streaked diarrhea B) Orange and foamy urine C) Increased abdominal girth D) Decreased cognition B Feedback: If the bile duct is obstructed, the bile will be reabsorbed into the blood and carried throughout the entire body. It is excreted in the urine, which becomes deep orange and foamy. Bloody diarrhea, ascites, and cognitive changes are not associated with obstructive jaundice. 20. During a health education session, a participant has asked about the hepatitis E virus. What prevention measure should the nurse recommend for preventing infection with this virus? A) Following proper hand-washing techniques B) Avoiding chemicals that are toxic to the liver C) Wearing a condom during sexual contact D) Limiting alcohol intake A Feedback: Avoiding contact with the hepatitis E virus through good hygiene, including hand-washing, is the major method of prevention. Hepatitis E is transmitted by the fecaloral route, principally through contaminated water in areas with poor sanitation. Consequently, none of the other listed preventative measures is indicated. 21. A patients physician has ordered a liver panel in response to the patients development of jaundice. When reviewing the results of this laboratory testing, the nurse should expect to review what blood tests? Select all that apply. A) Alanine aminotransferase (ALT) B) C-reactive protein (CRP) C) Gamma-glutamyl transferase (GGT) D) Aspartate aminotransferase (AST) E) B-type natriuretic peptide (BNP) A, C, D Feedback: Liver function testing includes GGT, ALT, and AST. CRP addresses the presence of generalized inflammation and BNP is relevant to heart failure; neither is included in a liver panel. 22. A patient with liver disease has developed jaundice; the nurse is collaborating with the patient to develop a nutritional plan. The nurse should prioritize which of the following in the patients plan? A) Increased potassium intake B) Fluid restriction to 2 L per day C) Reduction in sodium intake D) High-protein, low-fat diet C Feedback: Patients with ascites require a sharp reduction in sodium intake. Potassium intake should not be correspondingly increased. There is no need for fluid restriction or increased protein intake. 23. A nurse is amending a patients plan of care in light of the fact that the patient has recently developed ascites. What should the nurse include in this patients care plan? A) Mobilization with assistance at least 4 times daily B) Administration of beta-adrenergic blockers as ordered C) Vitamin B12 injections as ordered D) Administration of diuretics as ordered D Feedback: Use of diuretics along with sodium restriction is successful in 90% of patients with ascites. Beta- blockers are not used to treat ascites and bed rest is often more beneficial than increased mobility. Vitamin B12 injections are not necessary. 24. A nurse is caring for a patient who has been admitted for the treatment of advanced cirrhosis. What assessment should the nurse prioritize in this patients plan of care? A) Measurement of abdominal girth and body weight B) Assessment for variceal bleeding C) Assessment for signs and symptoms of jaundice D) Monitoring of results of liver function testing B Feedback: Esophageal varices are a major cause of mortality in patients with uncompensated cirrhosis. Consequently, this should be a focus of the nurses assessments and should be prioritized over the other listed assessments, even though each should be performed. 25. A patient with a diagnosis of cirrhosis has developed variceal bleeding and will imminently undergo variceal banding. What psychosocial nursing diagnosis should the nurse most likely prioritize during this phase of the patients treatment? A) Decisional Conflict B) Deficient Knowledge C) Death Anxiety D) Disturbed Thought Processes C Feedback: The sudden hemorrhage that accompanies variceal bleeding is intensely anxiety-provoking. The nurse must address the patients likely fear of death, which is a realistic possibility. For most patients, anxiety is likely to be a more acute concern than lack of knowledge or decisional conflict. The patient may or may not experience disturbances in thought processes. 26. A patient with a diagnosis of esophageal varices has undergone endoscopy to gauge the progression of this complication of liver disease. Following the completion of this diagnostic test, what nursing intervention should the nurse perform? A) Keep patient NPO until the results of test are known. B) Keep patient NPO until the patients gag reflex returns. C) Administer analgesia until post-procedure tenderness is relieved. D) Give the patient a cold beverage to promote swallowing ability. B Feedback: After the examination, fluids are not given until the patients gag reflex returns. Lozenges and gargles may be used to relieve throat discomfort if the patients physical condition and mental status permit. The result of the test is known immediately. Food and fluids are contraindicated until the gag reflex returns. 27. A patient with esophageal varices is being cared for in the ICU. The varices have begun to bleed and the patient is at risk for hypovolemia. The patient has Ringers lactate at 150 cc/hr infusing. What else might the nurse expect to have ordered to maintain volume for this patient? A) Arterial line B) Diuretics C) Foley catheter D) Volume expanders D Feedback: Because patients with bleeding esophageal varices have intravascular volume depletion and are subject to electrolyte imbalance, IV fluids with electrolytes and volume expanders are provided to restore fluid volume and replace electrolytes. Diuretics would reduce vascular volume. An arterial line and Foley catheter are likely to be ordered, but neither actively maintains the patients volume. 28. A patient with a history of injection drug use has been diagnosed with hepatitis C. When collaborating with the care team to plan this patients treatment, the nurse should anticipate what intervention? A) Administration of immune globulins B) A regimen of antiviral medications C) Rest and watchful waiting D) Administration of fresh-frozen plasma (FFP) B Feedback: There is no benefit from rest, diet, or vitamin supplements in HCV treatment. Studies have demonstrated that a combination of two antiviral agents, Peg-interferon and ribavirin (Rebetol), is effective in producing improvement in patients with hepatitis C and in treating relapses. Immune globulins and FFP are not indicated. 29. A group of nurses have attended an inservice on the prevention of occupationally acquired diseases that affect healthcare providers. What action has the greatest potential to reduce a nurses risk of acquiring hepatitis C in the workplace? A) Disposing of sharps appropriately and not recapping needles B) Performing meticulous hand hygiene at the appropriate moments in care C) Adhering to the recommended schedule of immunizations D) Wearing an N95 mask when providing care for patients on airborne precautions A Feedback: HCV is bloodborne. Consequently, prevention of needlestick injuries is paramount. Hand hygiene, immunizations and appropriate use of masks are important aspects of overall infection control, but these actions do not directly mitigate the risk of HCV. 30. A patient has been admitted to the critical care unit with a diagnosis of toxic hepatitis. When planning the patients care, the nurse should be aware of what potential clinical course of this health problem? Place the following events in the correct sequence. 1. Fever rises. 2. Hematemesis. 3. Clotting abnormalities. 4. Vascular collapse. 5. Coma. A) 1, 2, 5, 4, 3 B) 1, 2, 3, 4, 5 C) 2, 3, 1, 4, 5 D) 3, 1, 2, 5, 4 B Feedback: Recovery from acute toxic hepatitis is rapid if the hepatotoxin is identified early and removed or if exposure to the agent has been limited. Recovery is unlikely if there is a prolonged period between exposure and onset of symptoms. There are no effective antidotes. The fever rises; the patient becomes toxic and prostrated. Vomiting may be persistent, with the emesis containing blood. Clotting abnormalities may be severe, and hemorrhages may appear under the skin. The severe GI symptoms may lead to vascular collapse. Delirium, coma, and seizures develop, and within a few days the patient may die of fulminant hepatic failure unless he or she receives a liver transplant. 31. A previously healthy adults sudden and precipitous decline in health has been attributed to fulminant hepatic failure, and the patient has been admitted to the intensive care unit. The nurse should be aware that the treatment of choice for this patient is what? A) IV administration of immune globulins B) Transfusion of packed red blood cells and fresh-frozen plasma (FFP) C) Liver transplantation D) Lobectomy C Feedback: Liver transplantation carries the highest potential for the resolution of fulminant hepatic failure. This is preferred over other interventions, such as pharmacologic treatments, transfusions, and surgery. 32. A nurse is caring for a patient with cirrhosis secondary to heavy alcohol use. The nurses most recent assessment reveals subtle changes in the patients cognition and behavior. What is the nurses most appropriate response? A) Ensure that the patients sodium intake does not exceed recommended levels. B) Report this finding to the primary care provider due to the possibility of hepatic encephalopathy. C) Inform the primary care provider that the patient should be assessed for alcoholic hepatitis. D) Implement interventions aimed at ensuring a calm and therapeutic care environment. B Feedback: Monitoring is an essential nursing function to identify early deterioration in mental status. The nurse monitors the patients mental status closely and reports changes so that treatment of encephalopathy can be initiated promptly. This change in status is likely unrelated to sodium intake and would not signal the onset of hepatitis. A supportive care environment is beneficial, but does not address the patients physiologic deterioration. A patient with end-stage liver disease has developed hypervolemia. What nursing interventions would be most appropriate when addressing the patients fluid volume excess? Select all that apply. A) Administering diuretics B) Administering calcium channel blockers C) Implementing fluid restrictions D) Implementing a 1500 kcal/day restriction E) Enhancing patient positioning A, C, E Feedback: Administering diuretics, implementing fluid restrictions, and enhancing patient positioning can optimize the management of fluid volume excess. Calcium channel blockers and calorie restriction do not address this problem. 34. A patient with liver cancer is being discharged home with a biliary drainage system in place. The nurse should teach the patients family how to safely perform which of the following actions? A) Aspirating bile from the catheter using a syringe B) Removing the catheter when output is 15 mL in 24 hours C) Instilling antibiotics into the catheter D) Assessing the patency of the drainage catheter D Feedback: Families should be taught to provide basic catheter care, including assessment of patency. Antibiotics are not instilled into the catheter and aspiration using a syringe is contraindicated. The family would not independently remove the catheter; this would be done by a member of the care team when deemed necessary. 35. A patient with cirrhosis has experienced a progressive decline in his health; and liver transplantation is being considered by the interdisciplinary team. How will the patients prioritization for receiving a donor liver be determined? A) By considering the patients age and prognosis B) By objectively determining the patients medical need C) By objectively assessing the patients willingness to adhere to post-transplantation care D) By systematically ruling out alternative treatment options B Feedback: The patient would undergo a classification of the degree of medical need through an objective determination known as the Model of End-Stage Liver Disease (MELD) classification, which stratifies the level of illness of those awaiting a liver transplant. This algorithm considers multiple variables, not solely age, prognosis, potential for adherence, and the rejection of alternative options. 36. A nurse has entered the room of a patient with cirrhosis and found the patient on the floor. The patient states that she fell when transferring to the commode. The patients vital signs are within reference ranges and the nurse observes no apparent injuries. What is the nurses most appropriate action? A) Remove the patients commode and supply a bedpan. B) Complete an incident report and submit it to the unit supervisor. C) Have the patient assessed by the physician due to the risk of internal bleeding. D) Perform a focused abdominal assessment in order to rule out injury. C Feedback: A fall would necessitate thorough medical assessment due to the patients risk of bleeding. The nurses abdominal assessment is an appropriate action, but is not wholly sufficient to rule out internal injury. Medical assessment is a priority over removing the commode or filling out an incident report, even though these actions are appropriate. 37. A patient with liver cancer is being discharged home with a hepatic artery catheter in place. The nurse should be aware that this catheter will facilitate which of the following? A) Continuous monitoring for portal hypertension B) Administration of immunosuppressive drugs during the first weeks after transplantation C) Real-time monitoring of vascular changes in the hepatic system D) Delivery of a continuous chemotherapeutic dose D Feedback: In most cases, the hepatic artery catheter has been inserted surgically and has a prefilled infusion pump that delivers a continuous chemotherapeutic dose until completed. The hepatic artery catheter does not monitor portal hypertension, deliver immunosuppressive drugs, or monitor vascular changes in the hepatic system. 38. A nurse on a solid organ transplant unit is planning the care of a patient who will soon be admitted upon immediate recovery following liver transplantation. What aspect of nursing care is the nurses priority? A) Implementation of infection-control measures B) Close monitoring of skin integrity and color C) Frequent assessment of the patients psychosocial status D) Administration of antiretroviral medications A Feedback: Infection control is paramount following liver transplantation. This is a priority over skin integrity and psychosocial status, even though these are valid areas of assessment and intervention. Antiretrovirals are not indicated. 39. A 55-year-old female patient with hepatocellular carcinoma (HCC) is undergoing radiofrequency ablation. The nurse should recognize what goal of this treatment? A) Destruction of the patients liver tumor B) Restoration of portal vein patency C) Destruction of a liver abscess D) Reversal of metastasis A Feedback: Using radiofrequency ablation, a tumor up to 5 cm in size can be destroyed in one treatment session. This technique does not address circulatory function or abscess formation. It does not allow for the reversal of metastasis. 40. A nurse is caring for a patient with severe hemolytic jaundice. Laboratory tests show free bilirubin to be 24 mg/dL. For what complication is this patient at risk? A) Chronic jaundice B) Pigment stones in portal circulation C) Central nervous system damage D) Hepatomegaly C Feedback: Prolonged jaundice, even if mild, predisposes to the formation of pigment stones in the gallbladder, and extremely severe jaundice (levels of free bilirubin exceeding 20 to 25 mg/dL) poses a risk for CNS damage. There are not specific risks of hepatomegaly or chronic jaundice resulting from high bilirubin. Chapter 50: Assessment and Management of Patients with Biliary Disorders 1. A nurse is assessing a patient who has been diagnosed with cholecystitis, and is experiencing localized abdominal pain. When assessing the characteristics of the patients pain, the nurse should anticipate that it may radiate to what region? A) Left upper chest B) Inguinal region C) Neck or jaw D) Right shoulder D Feedback: The patient may have biliary colic with excruciating upper right abdominal pain that radiates to the back or right shoulder. Pain from cholecystitis does not typically radiate to the left upper chest, inguinal area, neck, or jaw. 2. A 55-year-old man has been newly diagnosed with acute pancreatitis and admitted to the acute medical unit. How should the nurse most likely explain the pathophysiology of this patients health problem? A) Toxins have accumulated and inflamed your pancreas. B) Bacteria likely migrated from your intestines and became lodged in your pancreas. C) A virus that was likely already present in your body has begun to attack your pancreatic cells. D) The enzymes that your pancreas produces have damaged the pancreas itself. D Feedback: Although the mechanisms causing pancreatitis are unknown, pancreatitis is commonly described as the autodigestion of the pancreas. Less commonly, toxic substances and microorganisms are implicated as the cause of pancreatitis. 3. A patients assessment and diagnostic testing are suggestive of acute pancreatitis. When the nurse is performing the health interview, what assessment questions address likely etiologic factors? Select all that apply. A) How many alcoholic drinks do you typically consume in a week? B) Have you ever been tested for diabetes? C) Have you ever been diagnosed with gallstones? D) Would you say that you eat a particularly high-fat diet? E) Does anyone in your family have cystic fibrosis? A, C Feedback: Eighty percent of patients with acute pancreatitis have biliary tract disease such as gallstones or a history of long-term alcohol abuse. Diabetes, high-fat consumption, and cystic fibrosis are not noted etiologic factors. 4. A patients abdominal ultrasound indicates cholelithiasis. When the nurse is reviewing the patients laboratory studies, what finding is most closely associated with this diagnosis? A) Increased bilirubin B) Decreased serum cholesterol C) Increased blood urea nitrogen (BUN) D) Decreased serum alkaline phosphatase level A Feedback: If the flow of blood is impeded, bilirubin, a pigment derived from the breakdown of red blood cells, does not enter the intestines. As a result, bilirubin levels in the blood increase. Cholesterol, BUN, and alkaline phosphatase levels are not typically affected. 5. A nurse who provides care in a walk-in clinic assesses a wide range of individuals. The nurse should identify which of the following patients as having the highest risk for chronic pancreatitis? A) A 45-year-old obese woman with a high-fat diet B) An 18-year-old man who is a weekend binge drinker C) A 39-year-old man with chronic alcoholism D) A 51-year-old woman who smokes one-and-a-half packs of cigarettes per day C Feedback: Excessive and prolonged consumption of alcohol accounts for approximately 70% to 80% of all cases of chronic pancreatitis. 6. A 37-year-old male patient presents at the emergency department (ED) complaining of nausea and vomiting and severe abdominal pain. The patients abdomen is rigid, and there is bruising to the patients flank. The patients wife states that he was on a drinking binge for the past 2 days. The ED nurse should assist in assessing the patient for what health problem? A) Severe pancreatitis with possible peritonitis B) Acute cholecystitis C) Chronic pancreatitis D) Acute appendicitis with possible perforation A Feedback: Severe abdominal pain is the major symptom of pancreatitis that causes the patient to seek medical care. Pain in pancreatitis is accompanied by nausea and vomiting that does not relieve the pain or nausea. Abdominal guarding is present and a rigid or board-like abdomen may be a sign of peritonitis. Ecchymosis (bruising) to the flank or around the umbilicus may indicate severe peritonitis. Pain generally occurs 24 to 48 hours after a heavy meal or alcohol ingestion. The link with alcohol intake makes pancreatitis a more likely possibility than appendicitis or cholecystitis. 7. A patient has been scheduled for an ultrasound of the gallbladder the following morning. What should the nurse do in preparation for this diagnostic study? A) Have the patient refrain from food and fluids after midnight. B) Administer the contrast agent orally 10 to 12 hours before the study. C) Administer the radioactive agent intravenously the evening before the study. D) Encourage the intake of 64 ounces of water 8 hours before the study. A Feedback: An ultrasound of the gallbladder is most accurate if the patient fasts overnight, so that the gallbladder is distended. Contrast and radioactive agents are not used when performing ultrasonography of the gallbladder, as an ultrasound is based on reflected sound waves. 8. A patient who had surgery for gallbladder disease has just returned to the postsurgical unit from postanesthetic recovery. The nurse caring for this patient knows to immediately report what assessment finding to the physician? A) Decreased breath sounds B) Drainage of bile-colored fluid onto the abdominal dressing C) Rigidity of the abdomen D) Acute pain with movement C Feedback: The location of the subcostal incision will likely cause the patient to take shallow breaths to prevent pain, which may result in decreased breath sounds. The nurse should remind patients to take deep breaths and cough to expand the lungs fully and prevent atelectasis. Acute pain is an expected assessment finding following surgery; analgesics should be administered for pain relief. Abdominal splinting or application of an abdominal binder may assist in reducing the pain. Bile may continue to drain from the drainage tract after surgery, which will require frequent changes of the abdominal dressing. Increased abdominal tenderness and rigidity should be reported immediately to the physician, as it may indicate bleeding from an inadvertent puncture or nicking of a major blood vessel during the surgical procedure. 9. A patient with chronic pancreatitis had a pancreaticojejunostomy created 3 months ago for relief of pain and to restore drainage of pancreatic secretions. The patient has come to the office for a routine postsurgical appointment. The patient is frustrated that the pain has not decreased. What is the most appropriate initial response by the nurse? A) The majority of patients who have a pancreaticojejunostomy have their normal digestion restored but do not achieve pain relief. B) Pain relief occurs by 6 months in most patients who undergo this procedure, but some people experience a recurrence of their pain. C) Your physician will likely want to discuss the removal of your gallbladder to achieve pain relief. D) You are probably not appropriately taking the medications for your pancreatitis and pain, so we will need to discuss your medication regimen in detail. B Feedback: Pain relief from a pancreaticojejunostomy often occurs by 6 months in more than 85% of the patients who undergo this procedure, but pain returns in a substantial number of patients as the disease progresses. This patient had surgery 3 months ago; the patient has 3 months before optimal benefits of the procedure may be experienced. There is no obvious indication for gallbladder removal and nonadherence is not the most likely factor underlying the pain. 10. A nurse is caring for a patient who has been scheduled for endoscopic retrograde cholangiopancreatography (ERCP) the following day. When providing anticipatory guidance for this patient, the nurse should describe what aspect of this diagnostic procedure? A) The need to protect the incision postprocedure B) The use of moderate sedation C) The need to infuse 50% dextrose during the procedure D) The use of general anesthesia B Feedback: Moderate sedation, not general anesthesia, is used during ERCP. D50 is not administered and the procedure does not involve the creation of an incision. 11. A patient has undergone a laparoscopic cholecystectomy and is being prepared for discharge home. When providing health education, the nurse should prioritize which of the following topics? A) Management of fluid balance in the home setting B) The need for blood glucose monitoring for the next week C) Signs and symptoms of intra-abdominal complications D) Appropriate use of prescribed pancreatic enzymes C Feedback: Because of the early discharge following laparoscopic cholecystectomy, the patient needs thorough education in the signs and symptoms of complications. Fluid balance is not typically a problem in the recovery period after laparoscopic cholecystectomy. There is no need for blood glucose monitoring or pancreatic enzymes. 12. A nurse is preparing a plan of care for a patient with pancreatic cysts that have necessitated drainage through the abdominal wall. What nursing diagnosis should the nurse prioritize? A) Disturbed Body Image B) Impaired Skin Integrity C) Nausea D) Risk for Deficient Fluid Volume B Feedback: While each of the diagnoses may be applicable to a patient with pancreatic drainage, the priority nursing diagnosis is Impaired Skin Integrity. The drainage is often perfuse and destructive to tissue because of the enzyme contents. Nursing measures must focus on steps to protect the skin near the drainage site from excoriation. The application of ointments or the use of a suction apparatus protects the skin from excoriation. 13. A home health nurse is caring for a patient discharged home after pancreatic surgery. The nurse documents the nursing diagnosis Risk for Imbalanced Nutrition: Less than Body Requirements on the care plan based on the potential complications that may occur after surgery. What are the most likely complications for the patient who has had pancreatic surgery? A) Proteinuria and hyperkalemia B) Hemorrhage and hypercalcemia C) Weight loss and hypoglycemia D) Malabsorption and hyperglycemia D Feedback: The nurse arrives at this diagnosis based on the complications of malabsorption and hyperglycemia. These complications often lead to the need for dietary modifications. Pancreatic enzyme replacement, a low-fat diet, and vitamin supplementation often are also required to meet the patients nutritional needs and restrictions. Electrolyte imbalances often accompany pancreatic disorders and surgery, but the electrolyte levels are more often deficient than excessive. Hemorrhage is a complication related to surgery, but not specific to the nutritionally based nursing diagnosis. Weight loss is a common complication, but hypoglycemia is less likely. 14. A patient has had a laparoscopic cholecystectomy. The patient is now complaining of right shoulder pain. What should the nurse suggest to relieve the pain? A) Aspirin every 4 to 6 hours as ordered B) Application of heat 15 to 20 minutes each hour C) Application of an ice pack for no more than 15 minutes D) Application of liniment rub to affected area B Feedback: If pain occurs in the right shoulder or scapular area (from migration of the CO2 used to insufflate the abdominal cavity during the procedure), the nurse may recommend use of a heating pad for 15 to 20 minutes hourly, walking, and sitting up when in bed. Aspirin would constitute a risk for bleeding. 15. A patient returns to the floor after a laparoscopic cholecystectomy. The nurse should assess the patient for signs and symptoms of what serious potential complication of this surgery? A) Diabetic coma B) Decubitus ulcer C) Wound evisceration D) Bile duct injury D Feedback: The most serious complication after laparoscopic cholecystectomy is a bile duct injury. Patients do not face a risk of diabetic coma. A decubitus ulcer is unlikely because immobility is not expected. Evisceration is highly unlikely, due to the laparoscopic approach. 16. A patient has been treated in the hospital for an episode of acute pancreatitis. The patient has acknowledged the role that his alcohol use played in the development of his health problem, but has not expressed specific plans for lifestyle changes after discharge. What is the nurses most appropriate response? A) Educate the patient about the link between alcohol use and pancreatitis. B) Ensure that the patient knows the importance of attending follow-up appointments. C) Refer the patient to social work or spiritual care. D) Encourage the patient to connect with a community-based support group. D Feedback: After the acute attack has subsided, some patients may be inclined to return to their previous drinking habits. The nurse provides specific information about resources and support groups that may be of assistance in avoiding alcohol in the future. Referral to Alcoholics Anonymous as appropriate or other support groups is essential. The patient already has an understanding of the effects of alcohol, and follow-up appointments will not necessarily result in lifestyle changes. Social work and spiritual care may or may not be beneficial. 17. A patient is being treated on the acute medical unit for acute pancreatitis. The nurse has identified a diagnosis of Ineffective Breathing Pattern Related to Pain. What intervention should the nurse perform in order to best address this diagnosis? A) Position the patient supine to facilitate diaphragm movement. B) Administer corticosteroids by nebulizer as ordered. C) Perform oral suctioning as needed to remove secretions. D) Maintain the patient in a semi-Fowlers position whenever possible. D Feedback: The nurse maintains the patient in a semi-Fowlers position to decrease pressure on the diaphragm by a distended abdomen and to increase respiratory expansion. A supine position will result in increased pressure on the diaphragm and potentially decreased respiratory expansion. Steroids and oral suctioning are not indicated. 18. A patient with gallstones has been prescribed ursodeoxycholic acid (UDCA). The nurse understands that additional teaching is needed regarding this medication when the patient states: A) It is important that I see my physician for scheduled follow-up appointments while taking this medication. B) I will take this medication for 2 weeks and then gradually stop taking it. C) If I lose weight, the dose of the medication may need to be changed. D) This medication will help dissolve small gallstones made of cholesterol. B Feedback: Ursodeoxycholic acid (UDCA) has been used to dissolve small, radiolucent gallstones composed primarily of cholesterol. This drug can reduce the size of existing stones, dissolve small stones, and prevent new stones from forming. Six to 12 months of therapy is required in many patients to dissolve stones, and monitoring of the patient is required during this time. The effective dose of medication depends on body weight. 19. A nurse is assisting with serving dinner trays on the unit. Upon receiving the dinner tray for a patient admitted with acute gallbladder inflammation, the nurse will question which of the following foods on the tray? A) Fried chicken B) Mashed potatoes C) Dinner roll D) Tapioca pudding A Feedback: The diet immediately after an episode of acute cholecystitis is initially limited to low-fat liquids. Cooked fruits, rice or tapioca, lean meats, mashed potatoes, bread, and coffee or tea may be added as tolerated. The patient should avoid fried foods such as fried chicken, as fatty foods may bring on an episode of cholecystitis. 20. A nurse is assessing an elderly patient with gallstones. The nurse is aware that the patient may not exhibit typical symptoms, and that particular symptoms that may be exhibited in the elderly patient may include what? A) Fever and pain B) Chills and jaundice C) Nausea and vomiting D) Signs and symptoms of septic shock D Feedback: The elderly patient may not exhibit the typical symptoms of fever, pain, chills jaundice, and nausea and vomiting. Symptoms of biliary tract disease in the elderly may be accompanied or preceded by those of septic shock, which include oliguria, hypotension, change in mental status, tachycardia, and tachypnea. 21. A nurse is creating a care plan for a patient with acute pancreatitis. The care plan includes reduced activity. What rationale for this intervention should be cited in the care plan? A) Bed rest reduces the patients metabolism and reduces the risk of metabolic acidosis. B) Reduced activity protects the physical integrity of pancreatic cells. C) Bed rest lowers the metabolic rate and reduces enzyme production. D) Inactivity reduces caloric need and gastrointestinal motility. C Feedback: The acutely ill patient is maintained on bed rest to decrease the metabolic rate and reduce the secretion of pancreatic and gastric enzymes. Staying in bed does not release energy from the body to fight the disease. 22. The nurse is caring for a patient who has just returned from the ERCP removal of gallstones. The nurse should monitor the patient for signs of what complications? A) Pain and peritonitis B) Bleeding and perforation C) Acidosis and hypoglycemia D) Gangrene of the gallbladder and hyperglycemia B Feedback: Following ERCP removal of gallstones, the patient is observed closely for bleeding, perforation, and the development of pancreatitis or sepsis. Blood sugar alterations, gangrene, peritonitis, and acidosis are less likely complications. 23. A patient with pancreatic cancer has been scheduled for a pancreaticoduodenectomy (Whipple procedure). During health education, the patient should be informed that this procedure will involve the removal of which of the following? Select all that apply. A) Gallbladder B) Part of the stomach C) Duodenum D) Part of the common bile duct E) Part of the rectum A, B, C, D Feedback: A pancreaticoduodenectomy (Whipple procedure or resection) is used for potentially resectable cancer of the head of the pancreas (Fig. 50-7). This procedure involves removal of the gallbladder, a portion of the stomach, duodenum, proximal jejunum, head of the pancreas, and distal common bile duct. The rectum is not affected. 24. An adult patient has been admitted to the medical unit for the treatment of acute pancreatitis. What nursing action should be included in this patients plan of care? A) Measure the patients abdominal girth daily. B) Limit the use of opioid analgesics. C) Monitor the patient for signs of dysphagia. D) Encourage activity as tolerated. A Feedback: Due to the risk of ascites, the nurse should monitor the patients abdominal girth. There is no specific need to avoid the use of opioids or to monitor for dysphagia, and activity is usually limited. 25. A community health nurse is caring for a patient whose multiple health problems include chronic pancreatitis. During the most recent visit, the nurse notes that the patient is experiencing severe abdominal pain and has vomited 3 times in the past several hours. What is the nurses most appropriate action? A) Administer a PRN dose of pancreatic enzymes as ordered. B) Teach the patient about the importance of abstaining from alcohol. C) Arrange for the patient to be transported to the hospital. D) Insert an NG tube, if available, and stay with the patient. C Feedback: Chronic pancreatitis is characterized by recurring attacks of severe upper abdominal and back pain, accompanied by vomiting. The onset of these acute symptoms warrants hospital treatment. Pancreatic enzymes are not indicated and an NG tube would not be inserted in the home setting. Patient education is a later priority that may or may not be relevant. 26. A student nurse is caring for a patient who has a diagnosis of acute pancreatitis and who is receiving parenteral nutrition. The student should prioritize which of the following assessments? A) Fluid output B) Oral intake C) Blood glucose levels D) BUN and creatinine levels C Feedback: In addition to administering enteral or parenteral nutrition, the nurse monitors serum glucose levels every 4 to 6 hours. Output should be monitored but in most cases it is not more important than serum glucose levels. A patient on parenteral nutrition would have no oral intake to monitor. Blood sugar levels are more likely to be unstable than indicators of renal function. 27. A patient has a recent diagnosis of chronic pancreatitis and is undergoing diagnostic testing to determine pancreatic islet cell function. The nurse should anticipate what diagnostic test? A) Glucose tolerance test B) ERCP C) Pancreatic biopsy D) Abdominal ultrasonography A Feedback: A glucose tolerance test evaluates pancreatic islet cell function and provides necessary information for making decisions about surgical resection of the pancreas. This specific clinical information is not provided by ERCP, biopsy, or ultrasound. 28. A patient has been admitted to the hospital for the treatment of chronic pancreatitis. The patient has been stabilized and the nurse is now planning health promotion and educational interventions. Which of the following should the nurse prioritize? A) Educating the patient about expectations and care following surgery B) Educating the patient about the management of blood glucose after discharge C) Educating the patient about postdischarge lifestyle modifications D) Educating the patient about the potential benefits of pancreatic transplantation C Feedback: The patients lifestyle (especially regarding alcohol use) is a major determinant of the course of chronic pancreatitis. The disease is not often managed by surgery and blood sugar monitoring is not necessarily indicated for every patient after hospital treatment. Transplantation is not an option. 29. The family of a patient in the ICU diagnosed with acute pancreatitis asks the nurse why the patient has been moved to an air bed. What would be the nurses best response? A) Air beds allow the care team to reposition her more easily while shes on bed rest. B) Air beds are far more comfortable than regular beds and shell likely have to be on bed rest a long time. C) The bed automatically moves, so shes less likely to develop pressure sores while shes in bed. D) The bed automatically moves, so she is likely to have less pain. C Feedback: It is important to turn the patient every 2 hours; use of specialty beds may be indicated to prevent skin breakdown. The rationale for a specialty bed is not related to repositioning, comfort, or ease of movement. 30. A patient is receiving care in the intensive care unit for acute pancreatitis. The nurse is aware that pancreatic necrosis is a major cause of morbidity and mortality in patients with acute pancreatitis. Consequently, the nurse should assess for what signs or symptoms of this complication? A) Sudden increase in random blood glucose readings B) Increased abdominal girth accompanied by decreased level of consciousness C) Fever, increased heart rate and decreased blood pressure D) Abdominal pain unresponsive to analgesics C Feedback: Pancreatic necrosis is a major cause of morbidity and mortality in patients with acute pancreatitis because of resulting hemorrhage, septic shock, and multiple organ dysfunction syndrome (MODS). Signs of shock would include hypotension, tachycardia and fever. Each of the other listed changes in status warrants intervention, but none is clearly suggestive of an onset of pancreatic necrosis. 31. A patient has been diagnosed with acute pancreatitis. The nurse is addressing the diagnosis of Acute Pain Related to Pancreatitis. What pharmacologic intervention is most likely to be ordered for this patient? A) Oral oxycodone B) IV hydromorphone (Dilaudid) C) IM meperidine (Demerol) D) Oral naproxen (Aleve) B Feedback: The pain of acute pancreatitis is often very severe and pain relief may require parenteral opioids such as morphine, fentanyl (Sublimaze), or hydromorphone (Dilaudid). There is no clinical evidence to support the use of meperidine for pain relief in pancreatitis. Opioids are preferred over NSAIDs. 32. A patient has just been diagnosed with chronic pancreatitis. The patient is underweight and in severe pain and diagnostic testing indicates that over 80% of the patients pancreas has been destroyed. The patient asks the nurse why the diagnosis was not made earlier in the disease process. What would be the nurses best response? A) The symptoms of pancreatitis mimic those of much less serious illnesses. B) Your body doesnt require pancreatic function until it is under great stress, so it is easy to go unnoticed. C) Chronic pancreatitis often goes undetected until a large majority of pancreatic function is lost. D) Its likely that your other organs were compensating for your decreased pancreatic function. C Feedback: By the time symptoms occur in chronic pancreatitis, approximately 90% of normal acinar cell function (exocrine function) has been lost. Late detection is not usually attributable to the vagueness of symptoms. The pancreas contributes continually to homeostasis and other organs are unable to perform its physiologic functions. 33. A patient has been diagnosed with pancreatic cancer and has been admitted for care. Following initial treatment, the nurse should be aware that the patient is most likely to require which of the following? A) Inpatient rehabilitation B) Rehabilitation in the home setting C) Intensive physical therapy D) Hospice care D Feedback: Pancreatic carcinoma has only a 5% survival rate at 5 years regardless of the stage of disease at diagnosis or treatment. As a result, there is a higher likelihood that the patient will require hospice care than physical therapy and rehabilitation. 34. A patient is admitted to the ICU with acute pancreatitis. The patients family asks what causes acute pancreatitis. The critical care nurse knows that a majority of patients with acute pancreatitis have what? A) Type 1 diabetes B) An impaired immune system C) Undiagnosed chronic pancreatitis D) An amylase deficiency C Feedback: Eighty percent of patients with acute pancreatitis have biliary tract disease or a history of long-term alcohol abuse. These patients usually have had undiagnosed chronic pancreatitis before their first episode of acute pancreatitis. Diabetes, an impaired immune function, and amylase deficiency are not specific precursors to acute pancreatitis. 35. A patient is admitted to the unit with acute cholecystitis. The physician has noted that surgery will be scheduled in 4 days. The patient asks why the surgery is being put off for a week when he has a sick gallbladder. What rationale would underlie the nurses response? A) Surgery is delayed until the patient can eat a regular diet without vomiting. B) Surgery is delayed until the acute symptoms subside. C) The patient requires aggressive nutritional support prior to surgery. D) Time is needed to determine whether a laparoscopic procedure can be used. B Feedback: Unless the patients condition deteriorates, surgical intervention is delayed just until the acute symptoms subside (usually within a few days). There is no need to delay surgery pending an improvement in nutritional status, and deciding on a laparoscopic approach is not a lengthy process. 36. A patient with a cholelithiasis has been scheduled for a laparoscopic cholecystectomy. Why is laparoscopic cholecystectomy preferred by surgeons over an open procedure? A) Laparoscopic cholecystectomy poses fewer surgical risks than an open procedure. B) Laparoscopic cholecystectomy can be performed in a clinic setting, while an open procedure requires an OR. C) A laparoscopic approach allows for the removal of the entire gallbladder. D) A laparoscopic approach can be performed under conscious sedation. A Feedback: Open surgery has largely been replaced by laparoscopic cholecystectomy (removal of the gallbladder through a small incision through the umbilicus). As a result, surgical risks have decreased, along with the length of hospital stay and the long recovery period required after standard surgical cholecystectomy. Both approaches allow for removal of the entire gallbladder and must be performed under general anesthetic in an operating theater. 37. A patient with ongoing back pain, nausea, and abdominal bloating has been diagnosed with cholecystitis secondary to gallstones. The nurse should anticipate that the patient will undergo what intervention? A) Laparoscopic cholecystectomy B) Methyl tertiary butyl ether (MTBE) infusion C) Intracorporeal lithotripsy D) Extracorporeal shock wave therapy (ESWL) A Feedback: Most of the nonsurgical approaches, including lithotripsy and dissolution of gallstones, provide only temporary solutions to gallstone problems and are infrequently used in the United States. Cholecystectomy is the preferred treatment. A nurse is caring for a patient with gallstones who has been prescribed ursodeoxycholic acid (UDCA). The patient askshow this medicine is going to help his symptoms. The nurse should be aware of what aspect of this drugs pharmacodynamics? A) It inhibits the synthesis of bile. B) It inhibits the synthesis and secretion of cholesterol. C) It inhibits the secretion of bile. D) It inhibits the synthesis and secretion of amylase. B Feedback: UDCA acts by inhibiting the synthesis and secretion of cholesterol, thereby desaturating bile. UDCA does not directly inhibit either the synthesis or secretion of bile or amylase. 39. A nurse is providing discharge education to a patient who has undergone a laparoscopic cholecystectomy. During the immediate recovery period, the nurse should recommend what foods? A) High-fiber foods B) Low-purine, nutrient-dense foods C) Low-fat foods high in proteins and carbohydrates D) Foods that are low-residue and low in fat C Feedback: The nurse encourages the patient to eat a diet that is low in fats and high in carbohydrates and proteins immediately after surgery. There is no specific need to increase fiber or avoid purines. A low-residue diet is not indicated. 40. A patient presents to the emergency department (ED) complaining of severe right upper quadrant pain. The patient states that his family doctor told him he had gallstones. The ED nurse should recognize what possible complication of gallstones? A) Acute pancreatitis B) Atrophy of the gallbladder C) Gallbladder cancer D) Gangrene of the gallbladder D Feedback: In calculous cholecystitis, a gallbladder stone obstructs bile outflow. Bile remaining in the gallbladder initiates a chemical reaction; autolysis and edema occur; and the blood vessels in the gallbladder are compressed, compromising its vascular supply. Gangrene of the gallbladder with perforation may result. Pancreatitis, atrophy, and cancer of the gallbladder are not plausible complications. Chapter 51: Assessment and Management of Patients with Diabetes 1. A patient with type 1 diabetes has told the nurse that his most recent urine test for ketones was positive. What is the nurses most plausible conclusion based on this assessment finding? A) The patient should withhold his next scheduled dose of insulin. B) The patient should promptly eat some protein and carbohydrates. C) The patients insulin levels are inadequate. D) The patient would benefit from a dose of metformin (Glucophage). C Feedback: Ketones in the urine signal that there is a deficiency of insulin and that control of type 1 diabetes is deteriorating. Withholding insulin or eating food would exacerbate the patients ketonuria. Metformin will not cause short-term resolution of hyperglycemia. 2. A patient presents to the clinic complaining of symptoms that suggest diabetes. What criteria would support checking blood levels for the diagnosis of diabetes? A) Fasting plasma glucose greater than or equal to 126 mg/dL B) Random plasma glucose greater than 150 mg/dL C) Fasting plasma glucose greater than 116 mg/dL on 2 separate occasions D) Random plasma glucose greater than 126 mg/dL A Feedback: Criteria for the diagnosis of diabetes include symptoms of diabetes plus random plasma glucose greater than or equal to 200 mg/dL, or a fasting plasma glucose greater than or equal to 126 mg/dL. 3. A patient newly diagnosed with type 2 diabetes is attending a nutrition class. What general guideline would be important to teach the patients at this class? A) Low fat generally indicates low sugar. B) Protein should constitute 30% to 40% of caloric intake. C) Most calories should be derived from carbohydrates. D) Animal fats should be eliminated from the diet. C Feedback: Currently, the ADA and the Academy of Nutrition and Dietetics (formerly the American Dietetic Association) recommend that for all levels of caloric intake, 50% to 60% of calories should be derived from carbohydrates, 20% to 30% from fat, and the remaining 10% to 20% from protein.Low fat does not automatically mean low sugar. Dietary animal fat does not need to be eliminated from the diet. 4. A nurse is providing health education to an adolescent newly diagnosed with type 1 diabetes mellitus and her family. The nurse teaches the patient and family that which of the following nonpharmacologic measures will decrease the bodys need for insulin? A) Adequate sleep B) Low stimulation C) Exercise D) Low-fat diet C Feedback: Exercise lowers blood glucose, increases levels of HDLs, and decreases total cholesterol and triglyceride levels. Low fat intake and low levels of stimulation do not reduce a patients need for insulin. Adequate sleep is beneficial in reducing stress, but does not have an effect that is pronounced as that of exercise. 5. A medical nurse is caring for a patient with type 1 diabetes. The patients medication administration record includes the administration of regular insulin three times daily. Knowing that the patients lunch tray will arrive at 11:45, when should the nurse administer the patients insulin? A) 10:45 B) 11:15 C) 11:45 D) 11:50 B Feedback: Regular insulin is usually administered 2030 min before a meal. Earlier administration creates a risk for hypoglycemia; later administration creates a risk for hyperglycemia. 6. A patient has just been diagnosed with type 2 diabetes. The physician has prescribed an oral antidiabetic agent that will inhibit the production of glucose by the liver and thereby aid in the control of blood glucose. What type of oral antidiabetic agent did the physician prescribe for this patient? A) A sulfonylurea B) A biguanide C) A thiazolidinedione D) An alpha glucosidase inhibitor B Feedback: Sulfonylureas exert their primary action by directly stimulating the pancreas to secrete insulin and therefore require a functioning pancreas to be effective. Biguanides inhibit the production of glucose by the liver and are in used in type 2 diabetes to control blood glucose levels. Thiazolidinediones enhance insulin action at the receptor site without increasing insulin secretion from the beta cells of the pancreas. Alpha glucosidase inhibitors work by delaying the absorption of glucose in the intestinal system, resulting in a lower postprandial blood glucose level. 7. A diabetes nurse educator is teaching a group of patients with type 1 diabetes about sick day rules. What guideline applies to periods of illness in a diabetic patient? A) Do not eliminate insulin when nauseated and vomiting. B) Report elevated glucose levels greater than 150 mg/dL. C) Eat three substantial meals a day, if possible. D) Reduce food intake and insulin doses in times of illness. A Feedback: The most important issue to teach patients with diabetes who become ill is not to eliminate insulin doses when nausea and vomiting occur. Rather, they should take their usual insulin or oral hypoglycemic agent dose, then attempt to consume frequent, small portions of carbohydrates. In general, blood sugar levels will rise but should be reported if they are greater than 300 mg/dL. 8. The nurse is discussing macrovascular complications of diabetes with a patient. The nurse would address what topic during this dialogue? A) The need for frequent eye examinations for patients with diabetes B) The fact that patients with diabetes have an elevated risk of myocardial infarction C) The relationship between kidney function and blood glucose levels D) The need to monitor urine for the presence of albumin B Feedback: Myocardial infarction and stroke are considered macrovascular complications of diabetes, while the effects on vision and renal function are considered to be microvascular. 9. A school nurse is teaching a group of high school students about risk factors for diabetes. Which of the following actions has the greatest potential to reduce an individuals risk for developing diabetes? A) Have blood glucose levels checked annually. B) Stop using tobacco in any form. C) Undergo eye examinations regularly. D) Lose weight, if obese. D Feedback: Obesity is a major modifiable risk factor for diabetes. Smoking is not a direct risk factor for the disease. Eye examinations are necessary for persons who have been diagnosed with diabetes, but they do not screen for the disease or prevent it. Similarly, blood glucose checks do not prevent the diabetes. 10. A 15-year-old child is brought to the emergency department with symptoms of hyperglycemia and is subsequently diagnosed with diabetes. Based on the fact that the childs pancreatic beta cells are being destroyed, the patient would be diagnosed with what type of diabetes? A) Type 1 diabetes B) Type 2 diabetes C) Noninsulin-dependent diabetes D) Prediabetes A Feedback: Beta cell destruction is the hallmark of type 1 diabetes. Noninsulin-dependent diabetes is synonymous with type 2 diabetes, which involves insulin resistance and impaired insulin secretion, but not beta cell destruction. Prediabetes is characterized by normal glucose metabolism, but a previous history of hyperglycemia, often during illness or pregnancy. 11. A newly admitted patient with type 1 diabetes asks the nurse what caused her diabetes. When the nurse is explaining to the patient the etiology of type 1 diabetes, what process should the nurse describe? A) The tissues in your body are resistant to the action of insulin, making the glucose levels in your blood increase. B) Damage to your pancreas causes an increase in the amount of glucose that it releases, and there is not enough insulin to control it. C) The amount of glucose that your body makes overwhelms your pancreas and decreases your production of insulin. D) Destruction of special cells in the pancreas causes a decrease in insulin production. Glucose levels rise because insulin normally breaks it down. D Feedback: Type 1 diabetes is characterized by the destruction of pancreatic beta cells, resulting in decreased insulin production, unchecked glucose production by the liver, and fasting hyperglycemia. Also, glucose derived from food cannot be stored in the liver and remains circulating in the blood, which leads to postprandial hyperglycemia. Type 2 diabetes involves insulin resistance and impaired insulin secretion. The body does not make glucose. 12. An occupational health nurse is screening a group of workers for diabetes. What statement should the nurse interpret as suggestive of diabetes? A) Ive always been a fan of sweet foods, but lately Im turned off by them. B) Lately, I drink and drink and cant seem to quench my thirst. C) No matter how much sleep I get, it seems to take me hours to wake up. D) When I went to the washroom the last few days, my urine smelled odd. B Feedback: Classic clinical manifestations of diabetes include the three Ps: polyuria, polydipsia, and polyphagia. Lack of interest in sweet foods, fatigue, and foul-smelling urine are not suggestive of diabetes. 13. A diabetes educator is teaching a patient about type 2 diabetes. The educator recognizes that the patient understands the primary treatment for type 2 diabetes when the patient states what? A) I read that a pancreas transplant will provide a cure for my diabetes. B) I will take my oral antidiabetic agents when my morning blood sugar is high. C) I will make sure to follow the weight loss plan designed by the dietitian. D) I will make sure I call the diabetes educator when I have questions about my insulin. C Feedback: Insulin resistance is associated with obesity; thus the primary treatment of type 2 diabetes is weight loss. Oral antidiabetic agents may be added if diet and exercise are not successful in controlling blood glucose levels. If maximum doses of a single category of oral agents fail to reduce glucose levels to satisfactory levels, additional oral agents may be used. Some patients may require insulin on an ongoing basis or on a temporary basis during times of acute psychological stress, but it is not the central component of type 2 treatment. Pancreas transplantation is associated with type 1 diabetes. 14. A diabetes nurse educator is presenting the American Diabetes Association (ADA) recommendations for levels of caloric intake. What do the ADAs recommendations include? A) 10% of calories from carbohydrates, 50% from fat, and the remaining 40% from protein B) 10% to 20% of calories from carbohydrates, 20% to 30% from fat, and the remaining 50% to 60% from protein C) 20% to 30% of calories from carbohydrates, 50% to 60% from fat, and the remaining 10% to 20% from protein D) 50% to 60% of calories from carbohydrates, 20% to 30% from fat, and the remaining 10% to 20% from protein D Feedback: Currently, the ADA and the Academy of Nutrition and Dietetics (formerly the American Dietetic Association) recommend that for all levels of caloric intake, 50% to 60% of calories come from carbohydrates, 20% to 30% from fat, and the remaining 10% to 20% from protein. 15. An older adult patient with type 2 diabetes is brought to the emergency department by his daughter. The patient is found to have a blood glucose level of 623 mg/dL. The patients daughter reports that the patient recently had a gastrointestinal virus and has been confused for the last 3 hours. The diagnosis of hyperglycemic hyperosmolar syndrome (HHS) is made. What nursing action would be a priority? A) Administration of antihypertensive medications B) Administering sodium bicarbonate intravenously C) Reversing acidosis by administering insulin D) Fluid and electrolyte replacement D Feedback: The overall approach to HHS includes fluid replacement, correction of electrolyte imbalances, and insulin administration. Antihypertensive medications are not indicated, as hypotension generally accompanies HHS due to dehydration. Sodium bicarbonate is not administered to patients with HHS, as their plasma bicarbonate level is usually normal. Insulin administration plays a less important role in the treatment of HHS because it is not needed for reversal of acidosis, as in diabetic ketoacidosis (DKA). 16. A nurse is caring for a patient with type 1 diabetes who is being discharged home tomorrow. What is the best way to assess the patients ability to prepare and self-administer insulin? A) Ask the patient to describe the process in detail. B) Observe the patient drawing up and administering the insulin. C) Provide a health education session reviewing the main points of insulin delivery. D) Review the patients first hemoglobin A1C result after discharge. B Feedback: Nurses should assess the patients ability to perform diabetes related self-care as soon as possible during the hospitalization or office visit to determine whether the patient requires further diabetes teaching. While consulting a home care nurse is beneficial, an initial assessment should be performed during the hospitalization or office visit. Nurses should directly observe the patient performing the skills such as insulin preparation and infection, blood glucose monitoring, and foot care. Simply questioning the patient about these skills without actually observing performance of the skill is not sufficient. Further education does not guarantee learning. 17. An elderly patient comes to the clinic with her daughter. The patient is a diabetic and is concerned about foot care. The nurse goes over foot care with the patient and her daughter as the nurse realizes that foot care is extremely important. Why would the nurse feel that foot care is so important to this patient? A) An elderly patient with foot ulcers experiences severe foot pain due to the diabetic polyneuropathy. B) Avoiding foot ulcers may mean the difference between institutionalization and continued independent living. C) Hypoglycemia is linked with a risk for falls; this risk is elevated in older adults with diabetes. Oral antihyperglycemics have the possible adverse effect of decreased circulation to the lower extremities. B Feedback: The nurse recognizes that providing information on the long-term complicationsespecially foot and eye problemsassociated with diabetes is important. Avoiding amputation through early detection of foot ulcers may mean the difference between institutionalization and continued independent living for the elderly person with diabetes. While the nurse recognizes that hypoglycemia is a dangerous situation and may lead to falls, hypoglycemia is not directly connected to the importance of foot care. Decrease in circulation is related to vascular changes and is not associated with drugs administered for diabetes. 18. A diabetic educator is discussing sick day rules with a newly diagnosed type 1 diabetic. The educator is aware that the patient will require further teaching when the patient states what? A) I will not take my insulin on the days when I am sick, but I will certainly check my blood sugar every 2 hours. B) If I cannot eat a meal, I will eat a soft food such as soup, gelatin, or pudding six to eight times a day. C) I will call the doctor if I am not able to keep liquids in my body due to vomiting or diarrhea. D) I will call the doctor if my blood sugar is over 300 mg/dL or if I have ketones in my urine. A Feedback: The nurse must explanation the sick day rules again to the patient who plans to stop taking insulin when sick. The nurse should emphasize that the patient should take insulin agents as usual and test ones blood sugar and urine ketones every 3 to 4 hours. In fact, insulin-requiring patients may need supplemental doses of regular insulin every 3 to 4 hours. The patient should report elevated glucose levels (greater than 300 mg/dL or as otherwise instructed) or urine ketones to the physician. If the patient is not able to eat normally, the patient should be instructed to substitute soft foods such a gelatin, soup, and pudding. If vomiting, diarrhea, or fever persists, the patient should have an intake of liquids every 30 to 60 minutes to prevent dehydration. 19. Which of the following patients with type 1 diabetes is most likely to experience adequate glucose control? A) A patient who skips breakfast when his glucose reading is greater than 220 mg/dL B) A patient who never deviates from her prescribed dose of insulin C) A patient who adheres closely to a meal plan and meal schedule D) A patient who eliminates carbohydrates from his daily intake C Feedback: The therapeutic goal for diabetes management is to achieve normal blood glucose levels without hypoglycemia. Therefore, diabetes management involves constant assessment and modification of the treatment plan by health professionals and daily adjustments in therapy (possibly including insulin) by patients. For patients who require insulin to help control blood glucose levels, maintaining consistency in the amount of calories and carbohydrates ingested at meals is essential. In addition, consistency in the approximate time intervals between meals, and the snacks, help maintain overall glucose control. Skipping meals is never advisable for person with type 1 diabetes. 20. A 28-year-old pregnant woman is spilling sugar in her urine. The physician orders a glucose tolerance test, which reveals gestational diabetes. The patient is shocked by the diagnosis, stating that she is conscientious about her health, and asks the nurse what causes gestational diabetes. The nurse should explain that gestational diabetes is a result of what etiologic factor? A) Increased caloric intake during the first trimester B) Changes in osmolality and fluid balance C) The effects of hormonal changes during pregnancy D) Overconsumption of carbohydrates during the first two trimesters C Feedback: Hyperglycemia and eventual gestational diabetes develops during pregnancy because of the secretion of placental hormones, which causes insulin resistance. The disease is not the result of food intake or changes in osmolality. 21. A medical nurse is aware of the need to screen specific patients for their risk of hyperglycemic hyperosmolar syndrome (HHS). In what patient population does hyperosmolar nonketotic syndrome most often occur? A) Patients who are obese and who have no known history of diabetes B) Patients with type 1 diabetes and poor dietary control C) Adolescents with type 2 diabetes and sporadic use of antihyperglycemics D) Middle-aged or older people with either type 2 diabetes or no known history of diabetes D Feedback: HHS occurs most often in older people (50 to 70 years of age) who have no known history of diabetes or who have type 2 diabetes. 22. A nurse is caring for a patient newly diagnosed with type 1 diabetes. The nurse is educating the patient about self-administration of insulin in the home setting. The nurse should teach the patient to do which of the following? A) Avoid using the same injection site more than once in 2 to 3 weeks. B) Avoid mixing more than one type of insulin in a syringe. C) Cleanse the injection site thoroughly with alcohol prior to injecting. D) Inject at a 45 angle. A Feedback: To prevent lipodystrophy, the patient should try not to use the same site more than once in 2 to 3 weeks. Mixing different types of insulin in a syringe is acceptable, within specific guidelines, and the needle is usually inserted at a 90 angle. Cleansing the injection site with alcohol is optional. 23. A patient with type 2 diabetes achieves adequate glycemic control through diet and exercise. Upon being admitted to the hospital for a cholecystectomy, however, the patient has required insulin injections on two occasions. The nurse would identify what likely cause for this short-term change in treatment? A) Alterations in bile metabolism and release have likely caused hyperglycemia. B) Stress has likely caused an increase in the patients blood sugar levels. C) The patient has likely overestimated her ability to control her diabetes using nonpharmacologic measures. D) The patients volatile fluid balance surrounding surgery has likely caused unstable blood sugars. B Feedback: During periods of physiologic stress, such as surgery, blood glucose levels tend to increase, because levels of stress hormones (epinephrine, norepinephrine, glucagon, cortisol, and growth hormone) increase. The patients need for insulin is unrelated to the action of bile, the patients overestimation of previous blood sugar control, or fluid imbalance. 24. A physician has explained to a patient that he has developed diabetic neuropathy in his right foot. Later that day, the patient asks the nurse what causes diabetic neuropathy. What would be the nurses best response? A) Research has shown that diabetic neuropathy is caused by fluctuations in blood sugar that have gone on for years. B) The cause is not known for sure but it is thought to have something to do with ketoacidosis. C) The cause is not known for sure but it is thought to involve elevated blood glucose levels over a period of years. D) Research has shown that diabetic neuropathy is caused by a combination of elevated glucose levels and elevated ketone levels. C Feedback: The etiology of neuropathy may involve elevated blood glucose levels over a period of years. High blood sugars (rather than fluctuations or variations in blood sugars) are thought to be responsible. Ketones and ketoacidosis are not direct causes of neuropathies. 25. A patient with type 2 diabetes has been managing his blood glucose levels using diet and metformin (Glucophage). Following an ordered increase in the patients daily dose of metformin, the nurse should prioritize which of the following assessments? A) Monitoring the patients neutrophil levels B) Assessing the patient for signs of impaired liver function C) Monitoring the patients level of consciousness and behavior D) Reviewing the patients creatinine and BUN levels D Feedback: Metformin has the potential to be nephrotoxic; consequently, the nurse should monitor the patients renal function. This drug does not typically affect patients neutrophils, liver function, or cognition. 26. A patient with a longstanding diagnosis of type 1 diabetes has a history of poor glycemic control. The nurse recognizes the need to assess the patient for signs and symptoms of peripheral neuropathy. Peripheral neuropathy constitutes a risk for what nursing diagnosis? A) Infection B) Acute pain C) Acute confusion D) Impaired urinary elimination A Feedback: Decreased sensations of pain and temperature place patients with neuropathy at increased risk for injury and undetected foot infections. The neurologic changes associated with peripheral neuropathy do not normally result in pain, confusion, or impairments in urinary function. 27. A patient has been brought to the emergency department by paramedics after being found unconscious. The patients Medic Alert bracelet indicates that the patient has type 1 diabetes and the patients blood glucose is 22 mg/dL (1.2 mmol/L). The nurse should anticipate what intervention? A) IV administration of 50% dextrose in water B) Subcutaneous administration of 10 units of Humalog C) Subcutaneous administration of 12 to 15 units of regular insulin D) IV bolus of 5% dextrose in 0.45% NaCl A Feedback: In hospitals and emergency departments, for patients who are unconscious or cannot swallow, 25 to 50 mL of 50% dextrose in water (D50W) may be administered IV for the treatment of hypoglycemia. Five percent dextrose would be inadequate and insulin would exacerbate the patients condition. 28. A diabetic nurse is working for the summer at a camp for adolescents with diabetes. When providing information on the prevention and management of hypoglycemia, what action should the nurse promote? A) Always carry a form of fast-acting sugar. B) Perform exercise prior to eating whenever possible. C) Eat a meal or snack every 8 hours. D) Check blood sugar at least every 24 hours. A Feedback: The following teaching points should be included in information provided to the patient on how to prevent hypoglycemia: Always carry a form of fast-acting sugar, increase food prior to exercise, eat a meal or snack every 4 to 5 hours, and check blood sugar regularly. 29. A nurse is teaching basic survival skills to a patient newly diagnosed with type 1 diabetes. What topic should the nurse address? A) Signs and symptoms of diabetic nephropathy B) Management of diabetic ketoacidosis C) Effects of surgery and pregnancy on blood sugar levels D) Recognition of hypoglycemia and hyperglycemia D Feedback: It is imperative that newly diagnosed patients know the signs and symptoms and management of hypo- and hyperglycemia. The other listed topics are valid points for education, but are not components of the patients immediate survival skills following a new diagnosis. 30. A nurse is conducting a class on how to self-manage insulin regimens. A patient asks how long a vial of insulin can be stored at room temperature before it goes bad. What would be the nurses best answer? A) If you are going to use up the vial within 1 month it can be kept at room temperature. B) If a vial of insulin will be used up within 21 days, it may be kept at room temperature. C) If a vial of insulin will be used up within 2 weeks, it may be kept at room temperature. D) If a vial of insulin will be used up within 1 week, it may be kept at room temperature. A Feedback: If a vial of insulin will be used up within 1 month, it may be kept at room temperature. 31. A patient has received a diagnosis of type 2 diabetes. The diabetes nurse has made contact with the patient and will implement a program of health education. What is the nurses priority action? A) Ensure that the patient understands the basic pathophysiology of diabetes. B) Identify the patients body mass index. C) Teach the patient survival skills for diabetes. D) Assess the patients readiness to learn. D Feedback: Before initiating diabetes education, the nurse assesses the patients (and familys) readiness to learn. This must precede other physiologic assessments (such as BMI) and providing health education. 32. A student with diabetes tells the school nurse that he is feeling nervous and hungry. The nurse assesses the child and finds he has tachycardia and is diaphoretic with a blood glucose level of 50 mg/dL (2.8 mmol/L). What should the school nurse administer? A) A combination of protein and carbohydrates, such as a small cup of yogurt B) Two teaspoons of sugar dissolved in a cup of apple juice C) Half of a cup of juice, followed by cheese and crackers D) Half a sandwich with a protein-based filling C Feedback: Initial treatment for hypoglycemia is 15 g concentrated carbohydrate, such as two or three glucose tablets, 1 tube glucose gel, or 0.5 cup juice. After initial treatment, the nurse should follow with a snack including starch and protein, such as cheese and crackers, milk and crackers, or half of a sandwich. It is unnecessary to add sugar to juice, even it if is labeled as unsweetened juice, because the fruit sugar in juice contains enough simple carbohydrate to raise the blood glucose level and additional sugar may result in a sharp rise in blood sugar that will last for several hours. 33. A patient with a history of type 1 diabetes has just been admitted to the critical care unit (CCU) for diabetic ketoacidosis. The CCU nurse should prioritize what assessment during the patients initial phase of treatment? A) Monitoring the patient for dysrhythmias B) Maintaining and monitoring the patients fluid balance C) Assessing the patients level of consciousness D) Assessing the patient for signs and symptoms of venous thromboembolism B Feedback: In addition to treating hyperglycemia, management of DKA is aimed at correcting dehydration, electrolyte loss, and acidosis before correcting the hyperglycemia with insulin. The nurse should monitor the patient for dysrhythmias, decreased LOC and VTE, but restoration and maintenance of fluid balance is the highest priority. 34. A patient has been living with type 2 diabetes for several years, and the nurse realizes that the patient is likely to have minimal contact with the health care system. In order to ensure that the patient maintains adequate blood sugar control over the long term, the nurse should recommend which of the following? A) Participation in a support group for persons with diabetes B) Regular consultation of websites that address diabetes management C) Weekly telephone check-ins with an endocrinologist D) Participation in clinical trials relating to antihyperglycemics A Feedback: Participation in support groups is encouraged for patients who have had diabetes for many years as well as for those who are newly diagnosed. This is more interactive and instructive than simply consulting websites. Weekly telephone contact with an endocrinologist is not realistic in most cases. Participation in research trials may or may not be beneficial and appropriate, depending on patients circumstances. 35. A patient with type 1 diabetes mellitus is seeing the nurse to review foot care. What would be a priority instruction for the nurse to give the patient? A) Examine feet weekly for redness, blisters, and abrasions. B) Avoid the use of moisturizing lotions. C) Avoid hot-water bottles and heating pads. D) Dry feet vigorously after each bath. C Feedback: High-risk behaviors, such as walking barefoot, using heating pads on the feet, wearing open-toed shoes, soaking the feet, and shaving calluses, should be avoided. Socks should be worn for warmth. Feet should be examined each day for cuts, blisters, swelling, redness, tenderness, and abrasions. Lotion should be applied to dry feet but never between the toes. After a bath, the patient should gently, not vigorously, pat feet dry to avoid injury. 36. A diabetes nurse is assessing a patients knowledge of self-care skills. What would be the most appropriate way for the educator to assess the patients knowledge of nutritional therapy in diabetes? A) Ask the patient to describe an optimally healthy meal. B) Ask the patient to keep a food diary and review it with the nurse. C) Ask the patients family what he typically eats. D) Ask the patient to describe a typical days food intake. B Feedback: Reviewing the patients actual food intake is the most accurate method of gauging the patients diet. 37. The most recent blood work of a patient with a longstanding diagnosis of type 1 diabetes has shown the presence of microalbuminuria. What is the nurses most appropriate action? A) Teach the patient about actions to slow the progression of nephropathy. B) Ensure that the patient receives a comprehensive assessment of liver function. C) Determine whether the patient has been using expired insulin. D) Administer a fluid challenge and have the test repeated. A Feedback: Clinical nephropathy eventually develops in more than 85% of people with microalbuminuria. As such, educational interventions addressing this microvascular complication are warranted. Expired insulin does not cause nephropathy, and the patients liver function is not likely affected. There is no indication for the use of a fluid challenge. 38. A nurse is assessing a patient who has diabetes for the presence of peripheral neuropathy. The nurse should question the patient about what sign or symptom that would suggest the possible development of peripheral neuropathy? A) Persistently cold feet B) Pain that does not respond to analgesia C) Acute pain, unrelieved by rest D) The presence of a tingling sensation D Feedback: Although approximately half of patients with diabetic neuropathy do not have symptoms, initial symptoms may include paresthesias (prickling, tingling, or heightened sensation) and burning sensations (especially at night). Cold and intense pain are atypical early signs of this complication. 39. A diabetic patient calls the clinic complaining of having a flu bug. The nurse tells him to take his regular dose of insulin. What else should the nurse tell the patient? A) Make sure to stick to your normal diet. B) Try to eat small amounts of carbs, if possible. C) Ensure that you check your blood glucose every hour. D) For now, check your urine for ketones every 8 hours. B Feedback: For prevention of DKA related to illness, the patient should attempt to consume frequent small portions of carbohydrates (including foods usually avoided, such as juices, regular sodas, and gelatin). Drinking fluids every hour is important to prevent dehydration. Blood glucose and urine ketones must be assessed every 3 to 4 hours. 40. A patient is brought to the emergency department by the paramedics. The patient is a type 2 diabetic and is experiencing HHS. The nurse should identify what components of HHS? Select all that apply. A) Leukocytosis B) Glycosuria C) Dehydration D) Hypernatremia E) Hyperglycemia B, C, D, E Feedback: In HHS, persistent hyperglycemia causes osmotic diuresis, which results in losses of water and electrolytes. To maintain osmotic equilibrium, water shifts from the intracellular fluid space to the extracellular fluid space. With glycosuria and dehydration, hypernatremia and increased osmolarity occur. Leukocytosis does not take place. Chapter 52: Assessment and Management of Patients with Endocrine Disorders 1. The nurse is caring for a patient diagnosed with hypothyroidism secondary to Hashimotos thyroiditis. When assessing this patient, what sign or symptom would the nurse expect? A) Fatigue B) Bulging eyes C) Palpitations D) Flushed skin A Feedback: Symptoms of hypothyroidism include extreme fatigue, hair loss, brittle nails, dry skin, voice huskiness or hoarseness, menstrual disturbance, and numbness and tingling of the fingers. Bulging eyes, palpitations, and flushed skin would be signs and symptoms of hyperthyroidism. 2. A patient has been admitted to the post-surgical unit following a thyroidectomy. To promote comfort and safety, how should the nurse best position the patient? A) Side-lying (lateral) with one pillow under the head B) Head of the bed elevated 30 degrees and no pillows placed under the head C) Semi-Fowlers with the head supported on two pillows D) Supine, with a small roll supporting the neck C Feedback: When moving and turning the patient, the nurse carefully supports the patients head and avoids tension on the sutures. The most comfortable position is the semi-Fowlers position, with the head elevated and supported by pillows. 3. A patient with thyroid cancer has undergone surgery and a significant amount of parathyroid tissue has been removed. The nurse caring for the patient should prioritize what question when addressing potential complications? A) Do you feel any muscle twitches or spasms? B) Do you feel flushed or sweaty? C) Are you experiencing any dizziness or lightheadedness? D) Are you having any pain that seems to be radiating from your bones? A Feedback: As the blood calcium level falls, hyperirritability of the nerves occurs, with spasms of the hands and feet and muscle twitching. This is characteristic of hypoparathyroidism. Flushing, diaphoresis, dizziness, and pain are atypical signs of the resulting hypocalcemia. 4. The nurse is caring for a patient with a diagnosis of Addisons disease. What sign or symptom is most closely associated with this health problem? A) Truncal obesity B) Hypertension C) Muscle weakness D) Moon face C Feedback: Patients with Addisons disease demonstrate muscular weakness, anorexia, gastrointestinal symptoms, fatigue, emaciation, dark pigmentation of the skin, and hypotension. Patients with Cushing syndrome demonstrate truncal obesity, moon face, acne, abdominal striae, and hypertension. 5. The nurse is caring for a patient with Addisons disease who is scheduled for discharge. When teaching the patient about hormone replacement therapy, the nurse should address what topic? A) The possibility of precipitous weight gain B) The need for lifelong steroid replacement C) The need to match the daily steroid dose to immediate symptoms D) The importance of monitoring liver function B Feedback: Because of the need for lifelong replacement of adrenal cortex hormones to prevent addisonian crises, the patient and family members receive explicit education about the rationale for replacement therapy and proper dosage. Doses are not adjusted on a short-term basis. Weight gain and hepatotoxicity are not common adverse effects. 6. The nurse is teaching a patient that the body needs iodine for the thyroid to function. What food would be the best source of iodine for the body? A) Eggs B) Shellfish C) Table salt D) Red meat C Feedback: The major use of iodine in the body is by the thyroid. Iodized table salt is the best source of iodine. 7. A patient is prescribed corticosteroid therapy. What would be priority information for the nurse to give the patient who is prescribed long-term corticosteroid therapy? A) The patients diet should be low protein with ample fat. B) The patient may experience short-term changes in cognition. C) The patient is at an increased risk for developing infection. D) The patient is at a decreased risk for development of thrombophlebitis and thromboembolism. C Feedback: The patient is at increased risk of infection and masking of signs of infection. The cardiovascular effects of corticosteroid therapy may result in development of thrombophlebitis or thromboembolism. Diet should be high in protein with limited fat. Changes in appearance usually disappear when therapy is no longer necessary. Cognitive changes are not common adverse effects. 8. A nurse caring for a patient with diabetes insipidus is reviewing laboratory results. What is an expected urinalysis finding? A) Glucose in the urine B) Albumin in the urine C) Highly dilute urine D) Leukocytes in the urine C Feedback: Patients with diabetes insipidus produce an enormous daily output of very dilute, water-like urine with a specific gravity of 1.001 to 1.005. The urine contains no abnormal substances such as glucose or albumin. Leukocytes in the urine are not related to the condition of diabetes insipidus, but would indicate a urinary tract infection, if present in the urine. 9. The nurse caring for a patient with Cushing syndrome is describing the dexamethasone suppression test scheduled for tomorrow. What does the nurse explain that this test will involve? A) Administration of dexamethasone orally, followed by a plasma cortisol level every hour for 3 hours B) Administration of dexamethasone IV, followed by an x-ray of the adrenal glands C) Administration of dexamethasone orally at 11 PM, and a plasma cortisol level at 8 AM the next morning D) Administration of dexamethasone intravenously, followed by a plasma cortisol level 3 hours after the drug is administered C Feedback: Dexamethasone (1 mg) is administered orally at 11 PM, and a plasma cortisol level is obtained at 8 AM the next morning. This test can be performed on an outpatient basis and is the most widely used and sensitive screening test for diagnosis of pituitary and adrenal causes of Cushing syndrome. 10. You are developing a care plan for a patient with Cushing syndrome. What nursing diagnosis would have the highest priority in this care plan? A) Risk for injury related to weakness B) Ineffective breathing pattern related to muscle weakness C) Risk for loneliness related to disturbed body image D) Autonomic dysreflexia related to neurologic changes A Feedback: The nursing priority is to decrease the risk of injury by establishing a protective environment. The patient who is weak may require assistance from the nurse in ambulating to prevent falls or bumping corners or furniture. The patients breathing will not be affected and autonomic dysreflexia is not a plausible risk. Loneliness may or may not be an issue for the patient, but safety is a priority. 11. The nurse is performing a shift assessment of a patient with aldosteronism. What assessments should the nurse include? Select all that apply. A) Urine output B) Signs or symptoms of venous thromboembolism C) Peripheral pulses D) Blood pressure E) Skin integrity A, D Feedback: The principal action of aldosterone is to conserve body sodium. Alterations in aldosterone levels consequently affect urine output and BP. The patients peripheral pulses, risk of VTE, and skin integrity are not typically affected by aldosteronism. 12. The home care nurse is conducting patient teaching with a patient on corticosteroid therapy. To achieve consistency with the bodys natural secretion of cortisol, when would the home care nurse instruct the patient to take his or her corticosteroids? A) In the evening between 4 PM and 6 PM B) Prior to going to sleep at night C) At noon every day D) In the morning between 7 AM and 8 AM D Feedback: In keeping with the natural secretion of cortisol, the best time of day for the total corticosteroid dose is in the morning from 7 to 8 AM. Large-dose therapy at 8 AM, when the adrenal gland is most active, produces maximal suppression of the gland. Also, a large 8 AM dose is more physiologic because it allows the body to escape effects of the steroids from 4 PM to 6 AM, when serum levels are normally low, thus minimizing cushingoid effects. 13. A patient presents at the walk-in clinic complaining of diarrhea and vomiting. The patient has a documented history of adrenal insufficiency. Considering the patients history and current symptoms, the nurse should anticipate that the patient will be instructed to do which of the following? A) Increase his intake of sodium until the GI symptoms improve. B) Increase his intake of potassium until the GI symptoms improve. C) Increase his intake of glucose until the GI symptoms improve. D) Increase his intake of calcium until the GI symptoms improve. A Feedback: The patient will need to supplement dietary intake with added salt during episodes of GI losses of fluid through vomiting and diarrhea to prevent the onset of addisonian crisis. While the patient may experience the loss of other electrolytes, the major concern is the replacement of lost sodium. 14. The nurse is caring for a patient with hyperparathyroidism. What level of activity would the nurse expect to promote? A) Complete bed rest B) Bed rest with bathroom privileges C) Out of bed (OOB) to the chair twice a day D) Ambulation and activity as tolerated D Feedback: Mobility, with walking or use of a rocking chair for those with limited mobility, is encouraged as much as possible because bones subjected to normal stress give up less calcium. Best rest should be discouraged because it increases calcium excretion and the risk of renal calculi. Limiting the patient to getting out of bed only a few times a day also increases calcium excretion and the associated risks. 15. While assisting with the surgical removal of an adrenal tumor, the OR nurse is aware that the patients vital signs may change upon manipulation of the tumor. What vital sign changes would the nurse expect to see? A) Hyperthermia and tachypnea B) Hypertension and heart rate changes C) Hypotension and hypothermia D) Hyperthermia and bradycardia B Feedback: Manipulation of the tumor during surgical excision may cause release of stored epinephrine and norepinephrine, with marked increases in BP and changes in heart rate. The use of sodium nitroprusside and alpha-adrenergic blocking agents may be required during and after surgery. While other vital sign changes may occur related to surgical complications, the most common changes are related to hypertension and changes in the heart rate. 16. A patient has returned to the floor after having a thyroidectomy for thyroid cancer. The nurse knows that sometimes during thyroid surgery the parathyroid glands can be injured or removed. What laboratory finding may be an early indication of parathyroid gland injury or removal? A) Hyponatremia B) Hypophosphatemia C) Hypocalcemia D) Hypokalemia C Feedback: Injury or removal of the parathyroid glands may produce a disturbance in calcium metabolism and result in a decline of calcium levels (hypocalcemia). As the blood calcium levels fall, hyperirritability of the nerves occurs, with spasms of the hands and feet and muscle twitching. This group of symptoms is known as tetany and must be reported to the physician immediately, because laryngospasm may occur and obstruct the airway. Hypophosphatemia, hyponatremia, and hypokalemia are not expected responses to parathyroid injury or removal. In fact, parathyroid removal or injury that results in hypocalcemia may lead to hyperphosphatemia. 17. The nurse is planning the care of a patient with hyperthyroidism. What should the nurse specify in the patients meal plan? A) A clear liquid diet, high in nutrients B) Small, frequent meals, high in protein and calories C) Three large, bland meals a day D) A diet high in fiber and plant-sourced fat B Feedback: A patient with hyperthyroidism has an increased appetite. The patient should be counseled to consume several small, well-balanced meals. High-calorie, high-protein foods are encouraged. A clear liquid diet would not satisfy the patients caloric or hunger needs. A diet rich in fiber and fat should be avoided because these foods may lead to GI upset or increase peristalsis. 18. A patient with a diagnosis of syndrome of inappropriate antidiuretic hormone secretion (SIADH) is being cared for on the critical care unit. The priority nursing diagnosis for a patient with this condition is what? A) Risk for peripheral neurovascular dysfunction B) Excess fluid volume C) Hypothermia D) Ineffective airway clearance B Feedback: The priority nursing diagnosis for a patient with SIADH is excess fluid volume, as the patient retains fluids and develops a sodium deficiency. Restricting fluid intake is a typical intervention for managing this syndrome. Temperature imbalances are not associated with SIADH. The patient is not at risk for neurovascular dysfunction or a compromised airway. 19. A patient with hypofunction of the adrenal cortex has been admitted to the medical unit. What would the nurse most likely find when assessing this patient? A) Increased body temperature B) Jaundice C) Copious urine output D) Decreased BP D Feedback: Decreased BP may occur with hypofunction of the adrenal cortex. Decreased function of the adrenal cortex does not affect the patients body temperature, urine output, or skin tone. 20. The nurse is assessing a patient diagnosed with Graves disease. What physical characteristics of Graves disease would the nurse expect to find? A) Hair loss B) Moon face C) Bulging eyes D) Fatigue C Feedback: Clinical manifestations of the endocrine disorder Graves disease include exophthalmos (bulging eyes) and fine tremor in the hands. Graves disease is not associated with hair loss, a moon face, or fatigue. 21. A patient with suspected adrenal insufficiency has been ordered an adrenocorticotropic hormone (ACTH) stimulation test. Administration of ACTH caused a marked increase in cortisol levels. How should the nurse interpret this finding? A) The patients pituitary function is compromised. B) The patients adrenal insufficiency is not treatable. C) The patient has insufficient hypothalamic function. D) The patient would benefit from surgery. A Feedback: An adrenal response to the administration of a stimulating hormone suggests inadequate production of the stimulating hormone. In this case, ACTH is produced by the pituitary and, consequently, pituitary hypofunction is suggested. Hypothalamic function is not relevant to the physiology of this problem. Treatment exists, although surgery is not likely indicated. 22. The physician has ordered a fluid deprivation test for a patient suspected of having diabetes insipidus. During the test, the nurse should prioritize what assessments? A) Temperature and oxygen saturation B) Heart rate and BP C) Breath sounds and bowel sounds D) Color, warmth, movement, and sensation of extremities B Feedback: The fluid deprivation test is carried out by withholding fluids for 8 to 12 hours or until 3% to 5% of the body weight is lost. The patients condition needs to be monitored frequently during the test, and the test is terminated if tachycardia, excessive weight loss, or hypotension develops. Consequently, BP and heart rate monitoring are priorities over the other listed assessments. 23. A nurse works in a walk-in clinic. The nurse recognizes that certain patients are at higher risk for different disorders than other patients. What patient is at a greater risk for the development of hypothyroidism? A) A 75-year-old female patient with osteoporosis B) A 50-year-old male patient who is obese C) A 45-year-old female patient who used oral contraceptives D) A 25-year-old male patient who uses recreational drugs A Feedback: Even though osteoporosis is not a risk factor for hypothyroidism, the condition occurs most frequently in older women. 24. A patient with a recent diagnosis of hypothyroidism is being treated for an unrelated injury. When administering medications to the patient, the nurse should know that the patients diminished thyroid function may have what effect? A) Anaphylaxis B) Nausea and vomiting C) Increased risk of drug interactions D) Prolonged duration of effect D Feedback: In all patients with hypothyroidism, the effects of analgesic agents, sedatives, and anesthetic agents are prolonged. There is no direct increase in the risk of anaphylaxis, nausea, or drug interactions, although these may potentially result from the prolonged half-life of drugs. 25. A patient has been admitted to the critical care unit with a diagnosis of thyroid storm. What interventions should the nurse include in this patients immediate care? Select all that apply. A) Administering diuretics to prevent fluid overload B) Administering beta blockers to reduce heart rate C) Administering insulin to reduce blood glucose levels D) Applying interventions to reduce the patients temperature E) Administering corticosteroids B, D Feedback: Thyroid storm necessitates interventions to reduce heart rate and temperature. Diuretics, insulin, and steroids are not indicated to address the manifestations of this health problem. 26. The nurses assessment of a patient with thyroidectomy suggests tetany and a review of the most recent blood work corroborate this finding. The nurse should prepare to administer what intervention? A) Oral calcium chloride and vitamin D B) IV calcium gluconate C) STAT levothyroxine D) Administration of parathyroid hormone (PTH) B Feedback: When hypocalcemia and tetany occur after a thyroidectomy, the immediate treatment is administration of IV calcium gluconate. This has a much faster therapeutic effect than PO calcium or vitamin D supplements. PTH and levothyroxine are not used to treat this complication. 27. A patient has been taking prednisone for several weeks after experiencing a hypersensitivity reaction. To prevent adrenal insufficiency, the nurse should ensure that the patient knows to do which of the following? A) Take the drug concurrent with levothyroxine (Synthroid). B) Take each dose of prednisone with a dose of calcium chloride. C) Gradually replace the prednisone with an OTC alternative. D) Slowly taper down the dose of prednisone, as ordered. D Feedback: Corticosteroid dosages are reduced gradually (tapered) to allow normal adrenal function to return and to prevent steroid-induced adrenal insufficiency. There are no OTC substitutes for prednisone and neither calcium chloride nor levothyroxine addresses the risk of adrenal insufficiency. 28. Following an addisonian crisis, a patients adrenal function has been gradually regained. The nurse should ensure that the patient knows about the need for supplementary glucocorticoid therapy in which of the following circumstances? A) Episodes of high psychosocial stress B) Periods of dehydration C) Episodes of physical exertion D) Administration of a vaccine A Feedback: During stressful procedures or significant illnesses, additional supplementary therapy with glucocorticoids is required to prevent addisonian crisis. Physical activity, dehydration and vaccine administration would not normally be sufficiently demanding such to require glucocorticoids. 29. A 30 year-old female patient has been diagnosed with Cushing syndrome. What psychosocial nursing diagnosis should the nurse most likely prioritize when planning the patients care? A) Decisional conflict related to treatment options B) Spiritual distress related to changes in cognitive function C) Disturbed body image related to changes in physical appearance D) Powerlessness related to disease progression C Feedback: Cushing syndrome causes characteristic physical changes that are likely to result in disturbed body image. Decisional conflict and powerless may exist, but disturbed body image is more likely to be present. Cognitive changes take place in patients with Cushing syndrome, but these may or may not cause spiritual distress. 30. A patient with pheochromocytoma has been admitted for an adrenalectomy to be performed the following day. To prevent complications, the nurse should anticipate preoperative administration of which of the following? A) IV antibiotics B) Oral antihypertensives C) Parenteral nutrition D) IV corticosteroids D Feedback: IV administration of corticosteroids (methylprednisolone sodium succinate [Solu-Medrol]) may begin on the evening before surgery and continue during the early postoperative period to prevent adrenal insufficiency. Antibiotics, antihypertensives, and parenteral nutrition do not prevent adrenal insufficiency or other common complications of adrenalectomy. 31. A patient is undergoing testing for suspected adrenocortical insufficiency. The care team should ensure that the patient has been assessed for the most common cause of adrenocortical insufficiency. What is the most common cause of this health problem? A) Therapeutic use of corticosteroids B) Pheochromocytoma C) Inadequate secretion of ACTH D) Adrenal tumor A Feedback: Therapeutic use of corticosteroids is the most common cause of adrenocortical insufficiency. The other options also cause adrenocortical insufficiency, but they are not the most common causes. 32. The nurse providing care for a patient with Cushing syndrome has identified the nursing diagnosis of risk for injury related to weakness. How should the nurse best reduce this risk? A) Establish falls prevention measures. B) Encourage bed rest whenever possible. C) Encourage the use of assistive devices. D) Provide constant supervision. A Feedback: The nurse should take action to prevent the patients risk for falls. Bed rest carries too many harmful effects, however, and assistive devices may or may not be necessary. Constant supervision is not normally required or practicable. 33. A patient with Cushing syndrome has been hospitalized after a fall. The dietician consulted works with the patient to improve the patients nutritional intake. What foods should a patient with Cushing syndrome eat to optimize health? Select all that apply. A) Foods high in vitamin D B) Foods high in calories C) Foods high in protein D) Foods high in calcium E) Foods high in sodium A, C, D Feedback: Foods high in vitamin D, protein, and calcium are recommended to minimize muscle wasting and osteoporosis. Referral to a dietitian may assist the patient in selecting appropriate foods that are also low in sodium and calories. 34. A patient on corticosteroid therapy needs to be taught that a course of corticosteroids of 2 weeks duration can suppress the adrenal cortex for how long? A) Up to 4 weeks B) Up to 3 months C) Up to 9 months D) Up to 1 year D Feedback: Suppression of the adrenal cortex may persist up to 1 year after a course of corticosteroids of only 2 weeks duration. 35. A patient with Cushing syndrome as a result of a pituitary tumor has been admitted for a transsphenoidal hypophysectomy. What would be most important for the nurse to monitor before, during, and after surgery? A) Blood glucose B) Assessment of urine for blood C) Weight D) Oral temperature A Feedback: Before, during, and after this surgery, blood glucose monitoring and assessment of stools for blood are carried out. The patients blood sugar is more likely to be volatile than body weight or temperature. Hematuria is not a common complication. 36. What should the nurse teach a patient on corticosteroid therapy in order to reduce the patients risk of adrenal insufficiency? A) Take the medication late in the day to mimic the bodys natural rhythms. B) Always have enough medication on hand to avoid running out. C) Skip up to 2 doses in cases of illness involving nausea. D) Take up to 1 extra dose per day during times of stress. B Feedback: The patient and family should be informed that acute adrenal insufficiency and underlying symptoms will recur if corticosteroid therapy is stopped abruptly without medical supervision. The patient should be instructed to have an adequate supply of the corticosteroid medication always available to avoid running out. Doses should not be skipped or added without explicit instructions to do so. Corticosteroids should normally be taken in the morning to mimic natural rhythms. 37. The nurse is caring for a patient at risk for an addisonian crisis. For what associated signs and symptoms should the nurse monitor the patient? Select all that apply. A) Epistaxis B) Pallor C) Rapid respiratory rate D) Bounding pulse E) Hypotension B, C, E Feedback: The patient at risk is monitored for signs and symptoms indicative of addisonian crisis, which can include shock; hypotension; rapid, weak pulse; rapid respiratory rate; pallor; and extreme weakness. Epistaxis and a bounding pulse are not symptoms or signs of an addisonian crisis. 38. A patient has been assessed for aldosteronism and has recently begun treatment. What are priority areas for assessment that the nurse should frequently address? Select all that apply. A) Pupillary response B) Creatinine and BUN levels C) Potassium level D) Peripheral pulses E) BP C, E Feedback: Patients with aldosteronism exhibit a profound decline in the serum levels of potassium, and hypertension is the most prominent and almost universal sign of aldosteronism. Pupillary response, peripheral pulses, and renal function are not directly affected. 39. A patient who has been taking corticosteroids for several months has been experiencing muscle wasting. The patient has asked the nurse for suggestions to address this adverse effect. What should the nurse recommend? A) Activity limitation to conserve energy B) Consumption of a high-protein diet C) Use of OTC vitamin D and calcium supplements D) Passive range-of-motion exercises B Feedback: Muscle wasting can be partly addressed through increased protein intake. Passive ROM exercises maintain flexibility, but do not build muscle mass. Vitamin D and calcium supplements do not decrease muscle wasting. Activity limitation would exacerbate the problem. 40. The nurse is providing care for an older adult patient whose current medication regimen includes levothyroxine (Synthroid). As a result, the nurse should be aware of the heightened risk of adverse effects when administering an IV dose of what medication? A) A fluoroquinalone antibiotic B) A loop diuretic C) A proton pump inhibitor (PPI) D) A benzodiazepine D Feedback: Oral thyroid hormones interact with many other medications.Even in small IV doses, hypnotic and sedative agents may induce profound somnolence, lasting far longer than anticipated and leading to narcosis (stupor like condition). Furthermore, they are likely to cause respiratory depression, which can easily be fatal because of decreased respiratory reserve and alveolar hypoventilation. Antibiotics, PPIs and diuretics do not cause the same risk. Chapter 53: Assessment of Kidney and Urinary Function 1. The care team is considering the use of dialysis in a patient whose renal function is progressively declining. Renal replacement therapy is indicated in which of the following situations? A) When the patients creatinine level drops below 1.2 mg/dL (110 mmol/L) B) When the patients blood urea nitrogen (BUN) is above 15 mg/dL C) When approximately 40% of nephrons are not functioning D) When about 80% of the nephrons are no longer functioning D Feedback: When the total number of functioning nephrons is less than 20%, renal replacement therapy needs to be considered. Dialysis is an example of a renal replacement therapy. Prior to the loss of about 80% of the nephron functioning ability, the patient may have mild symptoms of compromised renal function, but symptom management is often obtained through dietary modifications and drug therapy. The listed creatinine and BUN levels are within reference ranges. 2. A nurse knows that specific areas in the ureters have a propensity for obstruction. Prompt management of renal calculi is most important when the stone is located where? A) In the ureteropelvic junction B) In the ureteral segment near the sacroiliac junction C) In the ureterovesical junction D) In the urethra A Feedback: The three narrowed areas of each ureter are the ureteropelvic junction, the ureteral segment near the sacroiliac junction, and the ureterovescial junction. These three areas of the ureters have a propensity for obstruction by renal calculi or stricture. Obstruction of the ureteropelvic junction is most serious because of its close proximity to the kidney and the risk of associated kidney dysfunction. The urethra is not part of the ureter. 3. A nurse is caring for a patient with impaired renal function. A creatinine clearance measurement has been ordered. The nurse should facilitate collection of what samples? A) A fasting serum potassium level and a random urine sample B) A 24-hour urine specimen and a serum creatinine level midway through the urine collection process C) A BUN and serum creatinine level on three consecutive mornings D) A sterile urine specimen and an electrolyte panel, including sodium, potassium, calcium, and phosphorus values B Feedback: To calculate creatinine clearance, a 24-hour urine specimen is collected. Midway through the collection, the serum creatinine level is measured. 4. The nurse is assessing a patients bladder by percussion. The nurse elicits dullness after the patient has voided. How should the nurse interpret this assessment finding? A) The patients bladder is not completely empty. B) The patient has kidney enlargement. C) The patient has a ureteral obstruction. D) The patient has a fluid volume deficit. A Feedback: Dullness to percussion of the bladder following voiding indicates incomplete bladder emptying. Enlargement of the kidneys can be attributed to numerous conditions such as polycystic kidney disease or hydronephrosis and is not related to bladder fullness. Dehydration and ureteral obstruction are not related to bladder fullness; in fact, these conditions result in decreased flow of urine to the bladder. 5. The nurse is providing pre-procedure teaching about an ultrasound. The nurse informs the patient that in preparation for an ultrasound of the lower urinary tract the patient will require what? A) Increased fluid intake to produce a full bladder B) IV administration of radiopaque contrast agent C) Sedation and intubation D) Injection of a radioisotope A Feedback: Ultrasonography requires a full bladder; therefore, fluid intake should be encouraged before the procedures. The administration of a radiopaque contrast agent is required to perform IV urography studies, such as an IV pyelogram. Ultrasonography is a quick and painless diagnostic test and does not require sedation or intubation. The injection of a radioisotope is required for nuclear scan and ultrasonography is not in this category of diagnostic studies. 6. The nurse is caring for a patient who has a fluid volume deficit. When evaluating this patients urinalysis results, what should the nurse anticipate? A) A fluctuating urine specific gravity B) A fixed urine specific gravity C) A decreased urine specific gravity D) An increased urine specific gravity D Feedback: Urine specific gravity depends largely on hydration status. A decrease in fluid intake will lead to an increase in the urine specific gravity. With high fluid intake, specific gravity decreases. In patients with kidney disease, urine specific gravity does not vary with fluid intake, and the patients urine is said to have a fixed specific gravity. 7. A geriatric nurse is performing an assessment of body systems on an 85-year-old patient. The nurse should be aware of what age-related change affecting the renal or urinary system? A) Increased ability to concentrate urine B) Increased bladder capacity C) Urinary incontinence D) Decreased glomerular filtration rate D Feedback: Many age-related changes in the renal and urinary systems should be taken into consideration when taking a health history of the older adult. One change includes a decreased glomerular surface area resulting in a decreased glomerular filtration rate. Other changes include the decreased ability to concentrate urine and a decreased bladder capacity. It also should be understood that urinary incontinence is not a normal age-related change, but is common in older adults, especially in women because of the loss of pelvic muscle tone. 8. A nurse is preparing a patient diagnosed with benign prostatic hypertrophy (BPH) for a lower urinary tract cystoscopic examination. The nurse informs the patient that the most common temporary complication experienced after this procedure is what? A) Urinary retention B) Bladder perforation C) Hemorrhage D) Nausea A Feedback: After a cystoscopic examination, the patient with obstructive pathology may experience urine retention if the instruments used during the examination caused edema. The nurse will carefully monitor the patient with prostatic hyperplasia for urine retention. Post-procedure, the patient will experience some hematuria, but is not at great risk for hemorrhage. Unless the condition is associated with another disorder, nausea is not commonly associated with this diagnostic study. Bladder perforation is rare. 9. A patient with renal failure secondary to diabetic nephropathy has been admitted to the medical unit. What is the most life-threatening effect of renal failure for which the nurse should monitor the patient? A) Accumulation of wastes B) Retention of potassium C) Depletion of calcium D) Lack of BP control B Feedback: Retention of potassium is the most life-threatening effect of renal failure. Aldosterone causes the kidney to excrete potassium, in contrast to aldosterones effects on sodium described previously. Acidbase balance, the amount of dietary potassium intake, and the flow rate of the filtrate in the distal tubule also influence the amount of potassium secreted into the urine. Hypocalcemia, the accumulation of wastes, and lack of BP control are complications associated with renal failure, but do not have same level of threat to the patients well-being as hyperkalemia. 10. A kidney biopsy has been scheduled for a patient with a history of acute renal failure. The patient asks the nurse why this test has been scheduled. What is the nurses best response? A) A biopsy is routinely ordered for all patients with renal disorders. B) A biopsy is generally ordered following abnormal x-ray findings of the renal pelvis. C) A biopsy is often ordered for patients before they have a kidney transplant. D) A biopsy is sometimes necessary for diagnosing and evaluating the extent of kidney disease. D Feedback: Biopsy of the kidney is used in diagnosing and evaluating the extent of kidney disease. Indications for biopsy include unexplained acute renal failure, persistent proteinuria or hematuria, transplant rejection, and glomerulopathies. 11. The nurse is caring for a patient suspected of having renal dysfunction. When reviewing laboratory results for this patient, the nurse interprets the presence of which substances in the urine as most suggestive of pathology? A) Potassium and sodium B) Bicarbonate and urea C) Glucose and protein D) Creatinine and chloride C Feedback: The various substances normally filtered by the glomerulus, reabsorbed by the tubules, and excreted in the urine include sodium, chloride, bicarbonate, potassium, glucose, urea, creatinine, and uric acid. Within the tubule, some of these substances are selectively reabsorbed into the blood. Glucose is completely reabsorbed in the tubule and normally does not appear in the urine. However, glucose is found in the urine if the amount of glucose in the blood and glomerular filtrate exceeds the amount that the tubules are able to reabsorb. Protein molecules are also generally not found in the urine because amino acids are also filtered at the level of the glomerulus and reabsorbed so that it is not excreted in the urine. 12. The nurse caring for a patient with suspected renal dysfunction calculates that the patients weight has increased by 5 pounds in the past 24 hours. The nurse estimates that the patient has retained approximately how much fluid? A) 1,300 mL of fluid in 24 hours B) 2,300 mL of fluid in 24 hours C) 3,100 mL of fluid in 24 hours D) 5,000 mL of fluid in 24 hours B Feedback: An increase in body weight commonly accompanies edema. To calculate the approximate weight gain from fluid retention, remember that 1 kg of weight gain equals approximately 1,000 mL of fluid. Five lbs = 2.27 kg = 2,270 mL. 13. The nurse is performing a focused genitourinary and renal assessment of a patient. Where should the nurse assess for pain at the costovertebral angle? A) At the umbilicus and the right lower quadrant of the abdomen B) At the suprapubic region and the umbilicus C) At the lower border of the 12th rib and the spine D) At the 7th rib and the xyphoid process C Feedback: The costovertebral angle is the angle formed by the lower border of the 12th rib and the spine. Renal dysfunction may produce tenderness over the costovertebral angle. 14. The staff educator is giving a class for a group of nurses new to the renal unit. The educator is discussing renal biopsies. In what patient would the educator tell the new nurses that renal biopsies are contraindicated? A) A 64-year-old patient with chronic glomerulonephritis B) A 57-year-old patient with proteinuria C) A 42-year-old patient with morbid obesity D) A 16-year-old patient with signs of kidney transplant rejection C Feedback: There are several contraindications to a kidney biopsy, including bleeding tendencies, uncontrolled hypertension, a solitary kidney, and morbid obesity. Indications for a renal biopsy include unexplained acute renal failure, persistent proteinuria or hematuria, transplant rejection, and glomerulopathies. 15. The nurse is caring for a patient who describes changes in his voiding patterns. The patient states, I feel the urge to empty my bladder several times an hour and when the urge hits me I have to get to the restroom quickly. But when I empty my bladder, there doesnt seem to be a great deal of urine flow. What would the nurse expect this patients physical assessment to reveal? A) Hematuria B) Urine retention C) Dehydration D) Renal failure B Feedback: Increased urinary urgency and frequency coupled with decreasing urine volumes strongly suggest urine retention. Hematuria may be an accompanying symptom, but is likely related to a urinary tract infection secondary to the retention of urine. Dehydration and renal failure both result in a decrease in urine output, but the patient with these conditions does not have normal urine production and decreased or minimal flow of urine to the bladder. The symptoms of urgency and frequency do not accompany renal failure and dehydration due to decreased urine production. 16. The nurse is caring for a patient with a nursing diagnosis of deficient fluid volume. The nurses assessment reveals a BP of 98/52 mm Hg. The nurse should recognize that the patients kidneys will compensate by secreting what substance? A) Antidiuretic hormone (ADH) B) Aldosterone C) Renin D) Angiotensin C Feedback: When the vasa recta detect a decrease in BP, specialized juxtaglomerular cells near the afferent arteriole, distal tubule, and efferent arteriole secrete the hormone renin. Renin converts angiotensinogen to angiotensin I, which is then converted to angiotensin II. The vasoconstriction causes the BP to increase. The adrenal cortex secretes aldosterone in response to stimulation by the pituitary gland, which in turn is in response to poor perfusion or increasing serum osmolality. The result is an increase in BP. 17. A nurse is caring for a 73-year-old patient with a urethral obstruction related to prostatic enlargement. When planning this patients care, the nurse should be aware of the consequent risk of what complication? A) Urinary tract infection B) Enuresis C) Polyuria D) Proteinuria A Feedback: An obstruction of the bladder outlet, such as in advanced benign prostatic hyperplasia, results in abnormally high voiding pressure with a slow, prolonged flow of urine. The urine may remain in the bladder, which increases the potential of a urinary tract infection. Older male patients are at risk for prostatic enlargement, which causes urethral obstruction and can result in hydronephrosis, renal failure, and urinary tract infections. 18. A patient with elevated BUN and creatinine values has been referred by her primary physician for further evaluation. The nurse should anticipate the use of what initial diagnostic test? A) Ultrasound B) X-ray C) Computed tomography (CT) D) Nuclear scan A Feedback: Ultrasonography is a noninvasive procedure that passes sound waves into the body through a transducer to detect abnormalities of internal tissues and organs. Structures of the urinary system create characteristic ultrasonographic images. Because of its sensitivity, ultrasonography has replaced many other diagnostic tests as the initial diagnostic procedure. 19. A patient admitted to the medical unit with impaired renal function is complaining of severe, stabbing pain in the flank and lower abdomen. The patient is being assessed for renal calculi. The nurse recognizes that the stone is most likely in what anatomic location? A) Meatus B) Bladder C) Ureter D) Urethra C Feedback: Ureteral pain is characterized as a dull continuous pain that may be intense with voiding. The pain may be described as sharp or stabbing if the bladder is full. This type of pain is inconsistent with a stone being present in the bladder. Stones are not normally situated in the urethra or meatus. 20. The nurse is caring for a patient who had a brush biopsy 12 hours ago. The presence of what assessment finding should prompt the nurse to notify the physician? A) Scant hematuria B) Renal colic C) Temperature 100.2F orally D) Infiltration of the patients intravenous catheter C Feedback: Hematuria and renal colic are common and expected findings after the performance of a renal brush biopsy. The physician should be notified of the patients body temperature, which likely indicates the onset of an infectious process. IV infiltration does not warrant notification of the primary care physician. 21. A patient with recurrent urinary tract infections has just undergone a cystoscopy and complains of slight hematuria during the first void after the procedure. What is the nurses most appropriate action? A) Administer a STAT dose of vitamin K, as ordered. B) Reassure the patient that this is not unexpected and then monitor the patient for further bleeding. C) Promptly inform the physician of this assessment finding. D) Position the patient supine and insert a Foley catheter, as ordered. B Feedback: Some burning on voiding, blood-tinged urine, and urinary frequency from trauma to the mucous membranes can be expected after cystoscopy. The nurse should explain this to the patient and ensure that the bleeding resolves. No clear need exists to report this finding and it does not warrant insertion of a Foley catheter or vitamin K administration. 22. A patient is complaining of genitourinary pain shortly after returning to the unit from a scheduled cystoscopy. What intervention should the nurse perform? A) Encourage mobilization. B) Apply topical lidocaine to the patients meatus, as ordered. C) Apply moist heat to the patients lower abdomen. D) Apply an ice pack to the patients perineum. C Feedback: Following cystoscopy, moist heat to the lower abdomen and warm sitz baths are helpful in relieving pain and relaxing the muscles. Ice, lidocaine, and mobilization are not recommended interventions. 23. The nurse is caring for a patient who is going to have an open renal biopsy. What would be an important nursing action in preparing this patient for the procedure? A) Discuss the patients diagnosis with the family. B) Bathe the patient before the procedure with antiseptic skin wash. C) Administer antivirals before sending the patient for the procedure. D) Keep the patient NPO prior to the procedure. D Feedback: Preparation for an open biopsy is similar to that for any major abdominal surgery. When preparing the patient for an open biopsy you would keep the patient NPO. You may discuss the diagnosis with the family, but that is not a preparation for the procedure. A pre-procedure wash is not normally ordered and antivirals are not administered in anticipation of a biopsy. 24. The nurse is caring for a patient scheduled for renal angiography following a motor vehicle accident. What patient preparation should the nurse most likely provide before this test? A) Administration of IV potassium chloride B) Administration of a laxative C) Administration of Gastrografin D) Administration of a 24-hour urine test B Feedback: Before the procedure, a laxative may be prescribed to evacuate the colon so that unobstructed x-rays can be obtained. A 24-hour urine test is not necessary prior to the procedure. Gastrografin and potassium chloride are not administered prior to renal angiography. 25. Diagnostic testing of an adult patient reveals renal glycosuria. The nurse should recognize the need for the patient to be assessed for what health problem? A) Diabetes insipidus B) Syndrome of inappropriate antidiuretic hormone secretion (SIADH) C) Diabetes mellitus D) Renal carcinoma C Feedback: Renal glycosuria can occur on its own as a benign condition. It also occurs in poorly controlled diabetes, the most common condition that causes the blood glucose level to exceed the kidneys reabsorption capacity. Glycosuria is not associated with SIADH, diabetes insipidus, or renal carcinoma. 26. A patient with a diagnosis of respiratory acidosis is experiencing renal compensation. What function does the kidney perform to assist in restoring acidbase balance? A) Sequestering free hydrogen ions in the nephrons B) Returning bicarbonate to the bodys circulation C) Returning acid to the bodys circulation D) Excreting bicarbonate in the urine B Feedback: The kidney performs two major functions to assist in acidbase balance. The first is to reabsorb and return to the bodys circulation any bicarbonate from the urinary filtrate; the second is to excrete acid in the urine. Retaining bicarbonate will counteract an acidotic state. The nephrons do not sequester free hydrogen ions. 27. A patients most recent laboratory findings indicate a glomerular filtration rate (GFR) of 58 mL/min. The nurse should recognize what implication of this diagnostic finding? A) The patient is likely to have a decreased level of blood urea nitrogen (BUN). B) The patient is at risk for hypokalemia. C) The patient is likely to have irregular voiding patterns. D) The patient is likely to have increased serum creatinine levels. D Feedback: The adult GFR can vary from a normal of approximately 125 mL/min (1.67 to 2.0 mL/sec) to a high of 200 mL/min. A low GFR is associated with increased levels of BUN, creatinine, and potassium. 28. A patient has experienced excessive losses of bicarbonate and has subsequently developed an acidbase imbalance. How will this lost bicarbonate be replaced? A) The kidneys will excrete increased quantities of acid. B) Bicarbonate will be released from the adrenal medulla. C) Alveoli in the lungs will synthesize new bicarbonate. D) Renal tubular cells will generate new bicarbonate. D Feedback: To replace any lost bicarbonate, the renal tubular cells generate new bicarbonate through a variety of chemical reactions. This newly generated bicarbonate is then reabsorbed by the tubules and returned to the body. The lungs and adrenal glands do not synthesize bicarbonate. Excretion of acid compensates for a lack of bicarbonate, but it does not actively replace it. 29. A nurse is aware of the high incidence and prevalence of fluid volume deficit among older adults. What related health education should the nurse provide to an older adult? A) If possible, try to drink at least 4 liters of fluid daily. B) Ensure that you avoid replacing water with other beverages. C) Remember to drink frequently, even if you dont feel thirsty. D) Make sure you eat plenty of salt in order to stimulate thirst. C Feedback: The nurse emphasizes the need to drink throughout the day even if the patient does not feel thirsty, because the thirst stimulation is decreased. Four liters of daily fluid intake is excessive and fluids other than water are acceptable in most cases. Additional salt intake is not recommended as a prompt for increased fluid intake. 30. A patient is scheduled for a diagnostic MRI of the lower urinary system. What pre-procedure education should the nurse include? A) The need to be NPO for 12 hours prior to the test B) Relaxation techniques to apply during the test C) The need for conscious sedation prior to the test D) The need to limit fluid intake to 1 liter in the 24 hours before the test B Feedback: Patient preparation should include teaching relaxation techniques because the patient needs to remain still during an MRI. The patient does not normally need to be NPO or fluid-restricted before the test and conscious sedation is not usually implemented. 31. Results of a patients 24-hour urine sample indicate osmolality of 510 mOsm/kg, which is within reference range. What conclusion can the nurse draw from this assessment finding? A) The patients kidneys are capable of maintaining acidbase balance. B) The patients kidneys reabsorb most of the potassium that the patient ingests. C) The patients kidneys can produce sufficiently concentrated urine. D) The patients kidneys are producing sufficient erythropoietin. C Feedback: Osmolality is the most accurate measurement of the kidneys ability to dilute and concentrate urine. Osmolality is not a direct indicator of renal function as it relates to erythropoietin synthesis or maintenance of acidbase balance. It does not indicate the maintenance of healthy levels of potassium, the vast majority of which is excreted. 32. A patient is scheduled for diagnostic testing to address prolonged signs and symptoms of genitourinary dysfunction. What signs and symptoms are particularly suggestive of urinary tract disease? Select all that apply. A) Petechiae B) Pain C) Gastrointestinal symptoms D) Changes in voiding E) Jaundice B, C, D Feedback: Dysfunction of the kidney can produce a complex array of symptoms throughout the body. Pain, changes in voiding, and gastrointestinal symptoms are particularly suggestive of urinary tract disease. Jaundice and petechiae are not associated with genitourinary health problems. 33. A patient asks the nurse why kidney problems can cause gastrointestinal disturbances. What relationship should the nurse describe? A) The right kidneys proximity to the pancreas, liver, and gallbladder B) The indirect impact of digestive enzymes on renal function C) That the peritoneum encapsulates the GI system and the kidneys D) The left kidneys connection to the common bile duct A Feedback: The proximity of the right kidney to the colon, duodenum, head of the pancreas, common bile duct, liver, and gallbladder may cause GI disturbances. The proximity of the left kidney to the colon (splenic flexure), stomach, pancreas, and spleen may also result in intestinal symptoms. Digestive enzymes do not affect renal function and the left kidney is not connected to the common bile duct. 34. A patient with a history of progressively worsening fatigue is undergoing a comprehensive assessment which includes test of renal function relating to erythropoiesis. When assessing the oxygen transport ability of the blood, the nurse should prioritize the review of what blood value? A) Hematocrit B) Hemoglobin C) Erythrocyte sedimentation rate (ESR) D) Serum creatinine B Feedback: Although historically hematocrit has been the blood test of choice when assessing a patient for anemia, use of the hemoglobin level rather than hematocrit is currently recommended, because that measurement is a better assessment of the oxygen transport ability of the blood. ESR and creatinine levels are not indicative of oxygen transport ability. 35. The nurse is reviewing the electronic health record of a patient with a history of incontinence. The nurse reads that the physician assessed the patients deep tendon reflexes. What condition of the urinary/renal system does this assessment address? A) Renal calculi B) Bladder dysfunction C) Benign prostatic hyperplasia (BPH) D) Recurrent urinary tract infections (UTIs) B Feedback: The deep tendon reflexes of the knee are examined for quality and symmetry. This is an important part of testing for neurologic causes of bladder dysfunction, because the sacral area, which innervates the lower extremities, is in the same peripheral nerve area responsible for urinary continence. Neurologic function does not directly influence the course of renal calculi, BPH or UTIs. 36. A patient with a history of incontinence will undergo urodynamic testing in the physicians office. Because voiding in the presence of others can cause situational anxiety, the nurse should perform what action? A) Administer diuretics as ordered. B) Push fluids for several hours prior to the test. C) Discuss possible test results as the patient voids. D) Help the patient to relax before and during the test. D Feedback: Voiding in the presence of others can frequently cause guarding, a natural reflex that inhibits voiding due to situational anxiety. Because the outcomes of these studies determine the plan of care, the nurse must help the patient relax by providing as much privacy and explanation about the procedure as possible. Diuretics and increased fluid intake would not address the patients anxiety. It would be inappropriate and anxiety-provoking to discuss test results during the performance of the test. 37. A nurse is working with a patient who will undergo invasive urologic testing. The nurse has informed the patient that slight hematuria may occur after the testing is complete. The nurse should recommend what action to help resolve hematuria? A) Increased fluid intake following the test B) Use of an OTC diuretic after the test C) Gentle massage of the lower abdomen D) Activity limitation for the first 12 hours after the test A Feedback: Drinking fluids can help to clear hematuria. Diuretics are not used for this purpose. Activity limitation and massage are unlikely to resolve this expected consequence of testing. 38. The nurse is preparing to collect an ordered urine sample for urinalysis. The nurse should be aware that this test will include what assessment parameters? Select all that apply. A) Specific gravity of the patients urine B) Testing for the presence of glucose in the patients urine C) Microscopic examination of urine sediment for RBCs D) Microscopic examination of urine sediment for casts E) Testing for BUN and creatinine in the patients urine A, B, C, D Feedback: Urine testing includes testing for specific gravity, glucose, RBCs, and casts. BUN and creatinine are components of serum, not urine. 39. Dipstick testing of an older adult patients urine indicates the presence of protein. Which of the following statements is true of this assessment finding? A) This finding needs to be considered in light of other forms of testing. B) This finding is a risk factor for urinary incontinence. C) This finding is likely the result of an age-related physiologic change. D) This result confirms that the patient has diabetes. Select all that apply. B, C, D Feedback: A dipstick examination, which can detect from 30 to 1000 mg/dL of protein, should be used as a screening test only, because urine concentration, pH, hematuria, and radiocontrast materials all affect the results. Proteinuria is not diagnostic of diabetes and it is neither an age-related change nor a risk factor for incontinence. 40. What nursing action should the nurse perform when caring for a patient undergoing diagnostic testing of the renal-urologic system? A) Withhold medications until 12 hours post-testing. B) Ensure that the patient knows the importance of temporary fluid restriction after testing. C) Inform the patient of his or her medical diagnosis after reviewing the results. D) Assess the patients understanding of the test results after their completion. D Feedback: The nurse should ensure that the patient understands the results that are presented by the physician. Informing the patient of a diagnosis is normally the primary care providers responsibility. Withholding fluids or medications is not normally required after testing. Chapter 54: Management of Patients with Kidney Disorders 1. The nurse is assessing a patient suspected of having developed acute glomerulonephritis. The nurse should expect to address what clinical manifestation that is characteristic of this health problem? A) Hematuria B) Precipitous decrease in serum creatinine levels C) Hypotension unresolved by fluid administration D) Glucosuria A Feedback: The primary presenting feature of acute glomerulonephritis is hematuria (blood in the urine), which may be microscopic (identifiable through microscopic examination) or macroscopic or gross (visible to the eye). Proteinuria, primarily albumin, which is present, is due to increased permeability of the glomerular membrane. Blood urea nitrogen (BUN) and serum creatinine levels may rise as urine output drops. Some degree of edema and hypertension is noted in most patients. 2. The nurse is caring for acutely ill patient. What assessment finding should prompt the nurse to inform the physician that the patient may be exhibiting signs of acute kidney injury (AKI)? A) The patient is complains of an inability to initiate voiding. B) The patients urine is cloudy with a foul odor. C) The patients average urine output has been 10 mL/hr for several hours. D) The patient complains of acute flank pain. C Feedback: Oliguria (<500 mL/d of urine) is the most common clinical situation seen in AKI. Flank pain and inability to initiate voiding are not characteristic of AKI. Cloudy, foul-smelling urine is suggestive of a urinary tract infection. 3. The nurse is caring for a patient with a history of systemic lupus erythematosus who has been recently diagnosed with end-stage kidney disease (ESKD). The patient has an elevated phosphorus level and has been prescribed calcium acetate to bind the phosphorus. The nurse should teach the patient to take the prescribed phosphorus-binding medication at what time? A) Only when needed B) Daily at bedtime C) First thing in the morning D) With each meal D Feedback: Both calcium carbonate and calcium acetate are medications that bind with the phosphate and assist in excreting the phosphate from the body, in turn lowering the phosphate levels. Phosphate-binding medications must be administered with food to be effective. 4. The nurse is working on the renal transplant unit. To reduce the risk of infection in a patient with a transplanted kidney, it is imperative for the nurse to do what? A) Wash hands carefully and frequently. B) Ensure immediate function of the donated kidney. C) Instruct the patient to wear a face mask. D) Bar visitors from the patients room. A Feedback: The nurse ensures that the patient is protected from exposure to infection by hospital staff, visitors, and other patients with active infections. Careful handwashing is imperative; face masks may be worn by hospital staff and visitors to reduce the risk for transmitting infectious agents while the patient is receiving high doses of immunosuppressants. Visitors may be limited, but are not normally barred outright. Ensuring kidney function is vital, but does not prevent infection. 5. The nurse is caring for a patient receiving hemodialysis three times weekly. The patient has had surgery to form an arteriovenous fistula. What is most important for the nurse to be aware of when providing care for this patient? A) Using a stethoscope for auscultating the fistula is contraindicated. B) The patient feels best immediately after the dialysis treatment. C) Taking a BP reading on the affected arm can damage the fistula. D) The patient should not feel pain during initiation of dialysis. C Feedback: When blood flow is reduced through the access for any reason (hypotension, application of BP cuff/tourniquet), the access site can clot. Auscultation of a bruit in the fistula is one way to determine patency. Typically, patients feel fatigued immediately after hemodialysis because of the rapid change in fluid and electrolyte status. Although the area over the fistula may have some decreased sensation, a needle stick is still painful. 6. A patient has a glomerular filtration rate (GFR) of 43 mL/min/1.73 m2. Based on this GFR, the nurse interprets that the patients chronic kidney disease is at what stage? A) Stage 1 B) Stage 2 C) Stage 3 D) Stage 4 C Feedback: Stages of chronic renal failure are based on the GFR. Stage 3 is defined by a GFR in the range of 30 to 59 mL/min/1.73 m2. This is considered a moderate decrease in GFR. 7. A football player is thought to have sustained an injury to his kidneys from being tackled from behind. The ER nurse caring for the patient reviews the initial orders written by the physician and notes that an order to collect all voided urine and send it to the laboratory for analysis. The nurse understands that this nursing intervention is important for what reason? A) Hematuria is the most common manifestation of renal trauma and blood losses may be microscopic, so laboratory analysis is essential. B) Intake and output calculations are essential and the laboratory will calculate the precise urine output produced by this patient. C) A creatinine clearance study may be ordered at a later time and the laboratory will hold all urine until it is determined if the test will be necessary. D) There is great concern about electrolyte imbalances and the laboratory will monitor the urine for changes in potassium and sodium concentrations. A Feedback: Hematuria is the most common manifestation of renal trauma; its presence after trauma suggests renal injury. Hematuria may not occur, or it may be detectable only on microscopic examination. All urine should be saved and sent to the laboratory for analysis to detect RBCs and to evaluate the course of bleeding. Measuring intake and output is not a function of the laboratory. The laboratory does not save urine to test creatinine clearance at a later time. The laboratory does not monitor the urine for sodium or potassium concentrations. 8. A patient admitted with nephrotic syndrome is being cared for on the medical unit. When writing this patients care plan, based on the major clinical manifestation of nephrotic syndrome, what nursing diagnosis should the nurse include? A) Constipation related to immobility B) Risk for injury related to altered thought processes C) Hyperthermia related to the inflammatory process D) Excess fluid volume related to generalized edema D Feedback: The major clinical manifestation of nephrotic syndrome is edema, so the appropriate nursing diagnosis is Excess fluid volume related to generalized edema. Edema is usually soft, pitting, and commonly occurs around the eyes, in dependent areas, and in the abdomen. 9. The nurse coming on shift on the medical unit is taking a report on four patients. What patient does the nurse know is at the greatest risk of developing ESKD? A) A patient with a history of polycystic kidney disease B) A patient with diabetes mellitus and poorly controlled hypertension C) A patient who is morbidly obese with a history of vascular disorders D) A patient with severe chronic obstructive pulmonary disease B Feedback: Systemic diseases, such as diabetes mellitus (leading cause); hypertension; chronic glomerulonephritis; pyelonephritis; obstruction of the urinary tract; hereditary lesions, such as in polycystic kidney disease; vascular disorders; infections; medications; or toxic agents may cause ESKD. A patient with more than one of these risk factors is at the greatest risk for developing ESKD. Therefore, the patient with diabetes and hypertension is likely at highest risk for ESKD. 10. The nurse is caring for a patient postoperative day 4 following a kidney transplant. When assessing for potential signs and symptoms of rejection, what assessment should the nurse prioritize? A) Assessment of the quantity of the patients urine output B) Assessment of the patients incision C) Assessment of the patients abdominal girth D) Assessment for flank or abdominal pain A Feedback: After kidney transplantation, the nurse should perform all of the listed assessments. However, oliguria is considered to be more suggestive of rejection than changes to the patients abdomen or incision. 11. The nurse is caring for a patient in acute kidney injury. Which of the following complications would most clearly warrant the administration of polystyrene sulfonate (Kayexalate)? A) Hypernatremia B) Hypomagnesemia C) Hyperkalemia D) Hypercalcemia C Feedback: Hyperkalemia, a common complication of acute kidney injury, is life-threatening if immediate action is not taken to reverse it. The administration of polystyrene sulfonate reduces serum potassium levels. 12. Renal failure can have prerenal, renal, or postrenal causes. A patient with acute kidney injury is being assessed to determine where, physiologically, the cause is. If the cause is found to be prerenal, which condition most likely caused it? A) Heart failure B) Glomerulonephritis C) Ureterolithiasis D) Aminoglycoside toxicity A Feedback: By causing inadequate renal perfusion, heart failure can lead to prerenal failure. Glomerulonephritis and aminoglycoside toxicity are renal causes, and ureterolithiasis is a postrenal cause. 13. A 45-year-old man with diabetic nephropathy has ESKD and is starting dialysis. What should the nurse teach the patient about hemodialysis? A) Hemodialysis is a treatment option that is usually required three times a week. B) Hemodialysis is a program that will require you to commit to daily treatment. C) This will require you to have surgery and a catheter will need to be inserted into your abdomen. D) Hemodialysis is a treatment that is used for a few months until your kidney heals and starts to produce urine again. A Feedback: Hemodialysis is the most commonly used method of dialysis. Patients receiving hemodialysis must undergo treatment for the rest of their lives or until they undergo successful kidney transplantation. Treatments usually occur three times a week for at least 3 to 4 hours per treatment. 14. A patient with ESKD receives continuous ambulatory peritoneal dialysis. The nurse observes that the dialysate drainage fluid is cloudy. What is the nurses most appropriate action? A) Inform the physician and assess the patient for signs of infection. B) Flush the peritoneal catheter with normal saline. C) Remove the catheter promptly and have the catheter tip cultured. D) Administer a bolus of IV normal saline as ordered. A Feedback: Peritonitis is the most common and serious complication of peritoneal dialysis. The first sign of peritonitis is cloudy dialysate drainage fluid, so prompt reporting to the primary care provider and rapid assessment for other signs of infection are warranted. Administration of an IV bolus is not necessary or appropriate and the physician would determine whether removal of the catheter is required. Flushing the catheter does not address the risk for infection. 15. The nurse is planning patient teaching for a patient with ESKD who is scheduled for the creation of a fistula. The nurse would include which of the following in teaching the patient about the fistula? A) A vein and an artery in your arm will be attached surgically. B) The arm should be immobilized for 4 to 6 days. C) One needle will be inserted into the fistula for each dialysis treatment. D) The fistula can be used 2 days after the surgery for dialysis treatment. A Feedback: The fistula joins an artery and a vein, either side-to-side or end-to-end. This access will need time, usually 2 to 3 months, to mature before it can be used. The patient is encouraged to perform exercises to increase the size of the affected vessels (e.g., squeezing a rubber ball for forearm fistulas). Two needles will be inserted into the fistula for each dialysis treatment. 16. A patient with ESKD is scheduled to begin hemodialysis. The nurse is working with the patient to adapt the patients diet to maximize the therapeutic effect and minimize the risks of complications. The patients diet should include which of the following modifications? Select all that apply. A) Decreased protein intake B) Decreased sodium intake C) Increased potassium intake D) Fluid restriction E) Vitamin D supplementation A, B, D Feedback: Restricting dietary protein decreases the accumulation of nitrogenous wastes, reduces uremic symptoms, and may even postpone the initiation of dialysis for a few months. Restriction of fluid is also part of the dietary prescription because fluid accumulation may occur. As well, sodium is usually restricted to 2 to 3 g/day. Potassium intake is usually limited, not increased, and there is no particular need for vitamin D supplementation. 17. A patient on the critical care unit is postoperative day 1 following kidney transplantation from a living donor. The nurses most recent assessments indicate that the patient is producing copious quantities of dilute urine. What is the nurses most appropriate response? A) Assess the patient for further signs or symptoms of rejection. B) Recognize this as an expected finding. C) Inform the primary care provider of this finding. D) Administer exogenous antidiuretic hormone as ordered. B Feedback: A kidney from a living donor related to the patient usually begins to function immediately after surgery and may produce large quantities of dilute urine. This is not suggestive of rejection and treatment is not warranted. There is no obvious need to report this finding. 18. A patient is scheduled for a CT scan of the abdomen with contrast. The patient has a baseline creatinine level of 2.3 mg/dL. In preparing this patient for the procedure, the nurse anticipates what orders? A) Monitor the patients electrolyte values every hour before the procedure. B) Preprocedure hydration and administration of acetylcysteine C) Hemodialysis immediately prior to the CT scan D) Obtain a creatinine clearance by collecting a 24-hour urine specimen. B Feedback: Radiocontrast-induced nephropathy is a major cause of hospital-acquired acute kidney injury. Baseline levels of creatinine greater than 2 mg/dL identify the patient as being high risk. Preprocedure hydration and prescription of acetylcysteine (Mucomyst) the day prior to the test is effective in prevention. The nurse would not monitor the patients electrolytes every hour preprocedure. Nothing in the scenario indicates the need for hemodialysis. A creatinine clearance is not necessary prior to a CT scan with contrast. 19. The nurse is caring for a patient with acute glomerular inflammation. When assessing for the characteristic signs and symptoms of this health problem, the nurse should include which assessments? Select all that apply. A) Percuss for pain in the right lower abdominal quadrant. B) Assess for the presence of peripheral edema. C) Auscultate the patients apical heart rate for dysrhythmias. D) Assess the patients BP. E) Assess the patients orientation and judgment. B, D Feedback: Most patients with acute glomerular inflammation have some degree of edema and hypertension. Dysrhythmias, RLQ pain, and changes in mental status are not among the most common manifestations of acute glomerular inflammation. 20. A patient is admitted to the ICU after a motor vehicle accident. On the second day of the hospital admission, the patient develops acute kidney injury. The patient is hemodynamically unstable, but renal replacement therapy is needed to manage the patients hypervolemia and hyperkalemia. Which of the following therapies will the patients hemodynamic status best tolerate? A) Hemodialysis B) Peritoneal dialysis C) Continuous venovenous hemodialysis (CVVHD) D) Plasmapheresis C Feedback: CVVHD facilitates the removal of uremic toxins and fluid. The hemodynamic effects of CVVHD are usually mild in comparison to hemodialysis, so CVVHD is best tolerated by an unstable patient. Peritoneal dialysis is not the best choice, as the patient may have sustained abdominal injuries during the accident and catheter placement would be risky. Plasmapheresis does not achieve fluid removal and electrolyte balance. 21. A patient has presented with signs and symptoms that are characteristic of acute kidney injury, but preliminary assessment reveals no obvious risk factors for this health problem. The nurse should recognize the need to interview the patient about what topic? A) Typical diet B) Allergy status C) Psychosocial stressors D) Current medication use D Feedback: The kidneys are susceptible to the adverse effects of medications because they are repeatedly exposed to substances in the blood. Nephrotoxic medications are a more likely cause of AKI than diet, allergies, or stress. 22. An 84-year-old woman diagnosed with cancer is admitted to the oncology unit for surgical treatment. The patient has been on chemotherapeutic agents to decrease the tumor size prior to the planned surgery. The nurse caring for the patient is aware that what precipitating factors in this patient may contribute to AKI? Select all that apply. A) Anxiety B) Low BMI C) Age-related physiologic changes D) Chronic systemic disease E) NPO status C, D Feedback: Changes in kidney function with normal aging increase the susceptibility of elderly patients to kidney dysfunction and renal failure. In addition, the presence of chronic, systemic diseases increases the risk of AKI. Low BMI and anxiety are not risk factors for acute renal disease. NPO status is not a risk, provided adequate parenteral hydration is administered. 23. A patient is being treated for AKI and the patient daily weights have been ordered. The nurse notes a weight gain of 3 pounds over the past 48 hours. What nursing diagnosis is suggested by this assessment finding? A) Imbalanced nutrition: More than body requirements B) Excess fluid volume C) Sedentary lifestyle D) Adult failure to thrive B Feedback: If the patient with AKI gains or does not lose weight, fluid retention should be suspected. Short-term weight gain is not associated with excessive caloric intake or a sedentary lifestyle. Failure to thrive is not associated with weight gain. 24. A 15-year-old is admitted to the renal unit with a diagnosis of postinfectious glomerular disease. The nurse should recognize that this form of kidney disease may have been precipitated by what event? A) Psychosocial stress B) Hypersensitivity to an immunization C) Menarche D) Streptococcal infection D Feedback: Postinfectious causes of postinfectious glomerular disease are group A beta-hemolytic streptococcal infection of the throat that precedes the onset of glomerulonephritis by 2 to 3 weeks. Menarche, stress, and hypersensitivity are not typical causes. 25. A patient on the medical unit has a documented history of polycystic kidney disease (PKD). What principle should guide the nurses care of this patient? A) The disease is self-limiting and cysts usually resolve spontaneously in the fifth or sixth decade of life. B) The patients disease is incurable and the nurses interventions will be supportive. C) The patient will eventually require surgical removal of his or her renal cysts. D) The patient is likely to respond favorably to lithotripsy treatment of the cysts. B Feedback: PKD is incurable and care focuses on support and symptom control. It is not self-limiting and is not treated surgically or with lithotripsy. 26. The nurse is providing a health education workshop to a group of adults focusing on cancer prevention. The nurse should emphasize what action in order to reduce participants risks of renal carcinoma? A) Avoiding heavy alcohol use B) Control of sodium intake C) Smoking cessation D) Adherence to recommended immunization schedules C Feedback: Tobacco use is a significant risk factor for renal cancer, surpassing the significance of high alcohol and sodium intake. Immunizations do not address an individuals risk of renal cancer. 27. The nurse performing the health interview of a patient with a new onset of periorbital edema has completed a genogram, noting the health history of the patients siblings, parents, and grandparents. This assessment addresses the patients risk of what kidney disorder? A) Nephritic syndrome B) Acute glomerulonephritis C) Nephrotic syndrome D) Polycystic kidney disease (PKD) D Feedback: PKD is a genetic disorder characterized by the growth of numerous cysts in the kidneys. Nephritic syndrome, acute glomerulonephritis, and nephrotic syndrome are not genetic disorders. 28. A patient is brought to the renal unit from the PACU status post resection of a renal tumor. Which of the following nursing actions should the nurse prioritize in the care of this patient? A) Increasing oral intake B) Managing postoperative pain C) Managing dialysis D) Increasing mobility B Feedback: The patient requires frequent analgesia during the postoperative period and assistance with turning, coughing, use of incentive spirometry, and deep breathing to prevent atelectasis and other pulmonary complications. Increasing oral intake and mobility are not priority nursing actions in the immediate postoperative care of this patient. Dialysis is not necessary following kidney surgery. 29. A nurse is caring for a patient who is in the diuresis phase of AKI. The nurse should closely monitor the patient for what complication during this phase? A) Hypokalemia B) Hypocalcemia C) Dehydration D) Acute flank pain C Feedback: The diuresis period is marked by a gradual increase in urine output, which signals that glomerular filtration has started to recover. The patient must be observed closely for dehydration during this phase; if dehydration occurs, the uremic symptoms are likely to increase. Excessive losses of potassium and calcium are not typical during this phase, and diuresis does not normally result in pain. 30. The nurse is caring for a patient status after a motor vehicle accident. The patient has developed AKI. What is the nurses role in caring for this patient? Select all that apply. A) Providing emotional support for the family B) Monitoring for complications C) Participating in emergency treatment of fluid and electrolyte imbalances D) Providing nursing care for primary disorder (trauma) E) Directing nutritional interventions A, B, C, D Feedback: The nurse has an important role in caring for the patient with AKI. The nurse monitors for complications, participates in emergency treatment of fluid and electrolyte imbalances, assesses the patients progress and response to treatment, and provides physical and emotional support. Additionally, the nurse keeps family members informed about the patients condition, helps them understand the treatments, and provides psychological support. Although the development of AKI may be the most serious problem, the nurse continues to provide nursing care indicated for the primary disorder (e.g., burns, shock, trauma, obstruction of the urinary tract). The nurse does not direct the patients nutritional status; the dietician and the physician normally collaborate on directing the patients nutritional status. 31. A 71-year-old patient with ESKD has been told by the physician that it is time to consider hemodialysis until a transplant can be found. The patient tells the nurse she is not sure she wants to undergo a kidney transplant. What would be an appropriate response for the nurse to make? A) The decision is certainly yours to make, but be sure not to make a mistake. B) Kidney transplants in patients your age are as successful as they are in younger patients. C) I understand your hesitancy to commit to a transplant surgery. Success is comparatively rare. D) Have you talked this over with your family? B Feedback: Although there is no specific age limitation for renal transplantation, concomitant disorders (e.g., coronary artery disease, peripheral vascular disease) have made it a less common treatment for the elderly. However, the outcome is comparable to that of younger patients. The other listed options either belittle the patient or give the patient misinformation. 32. The nurse has identified the nursing diagnosis of risk for infection in a patient who undergoes peritoneal dialysis. What nursing action best addresses this risk? A) Maintain aseptic technique when administering dialysate. B) Wash the skin surrounding the catheter site with soap and water prior to each exchange. C) Add antibiotics to the dialysate as ordered. D) Administer prophylactic antibiotics by mouth or IV as ordered. A Feedback: Aseptic technique is used to prevent peritonitis and other infectious complications of peritoneal dialysis. It is not necessary to cleanse the skin with soap and water prior to each exchange. Antibiotics may be added to dialysate to treat infection, but they are not used to prevent infection. 33. The nurse is caring for a patient who has returned to the postsurgical suite after post-anesthetic recovery from a nephrectomy. The nurses most recent hourly assessment reveals a significant drop in level of consciousness and BP as well as scant urine output over the past hour. What is the nurses best response? A) Assess the patient for signs of bleeding and inform the physician. B) Monitor the patients vital signs every 15 minutes for the next hour. C) Reposition the patient and reassess vital signs. D) Palpate the patients flanks for pain and inform the physician. A Feedback: Bleeding may be suspected when the patient experiences fatigue and when urine output is less than 30 mL/h. The physician must be made aware of this finding promptly. Palpating the patients flanks would cause intense pain that is of no benefit to assessment. 34. The critical care nurse is monitoring the patients urine output and drains following renal surgery. What should the nurse promptly report to the physician? A) Increased pain on movement B) Absence of drain output C) Increased urine output D) Blood-tinged serosanguineous drain output B Feedback: Urine output and drainage from tubes inserted during surgery are monitored for amount, color, and type or characteristics. Decreased or absent drainage is promptly reported to the physician because it may indicate obstruction that could cause pain, infection, and disruption of the suture lines. Reporting increased pain on movement has nothing to do with the scenario described. Increased urine output and serosanguineous drainage are expected. 35. The nurse is creating an education plan for a patient who underwent a nephrectomy for the treatment of a renal tumor. What should the nurse include in the teaching plan? A) The importance of increased fluid intake B) Signs and symptoms of rejection C) Inspection and care of the incision D) Techniques for preventing metastasis C Feedback: The nurse teaches the patient to inspect and care for the incision and perform other general postoperative care, including activity and lifting restrictions, driving, and pain management. There would be no need to teach the signs or symptoms of rejection as there has been no transplant. Increased fluid intake is not normally recommended and the patient has minimal control on the future risk for metastasis. 36. A patient with chronic kidney disease has been hospitalized and is receiving hemodialysis on a scheduled basis. The nurse should include which of the following actions in the plan of care? A) Ensure that the patient moves the extremity with the vascular access site as little as possible. B) Change the dressing over the vascular access site at least every 12 hours. C) Utilize the vascular access site for infusion of IV fluids. D) Assess for a thrill or bruit over the vascular access site each shift. D Feedback: The bruit, or thrill, over the venous access site must be evaluated at least every shift. Frequent dressing changes are unnecessary and the patient does not normally need to immobilize the site. The site must not be used for purposes other than dialysis. 37. The nurse is caring for a patient who has just returned to the post-surgical unit following renal surgery. When assessing the patients output from surgical drains, the nurse should assess what parameters? Select all that apply. A) Quantity of output B) Color of the output C) Visible characteristics of the output D) Odor of the output E) pH of the output A, B, C Feedback: Urine output and drainage from tubes inserted during surgery are monitored for amount, color, and type or characteristics. Odor and pH are not normally assessed. 38. The nurse is caring for a patient after kidney surgery. The nurse is aware that bleeding is a major complication of kidney surgery and that if it goes undetected and untreated can result in hypovolemia and hemorrhagic shock in the patient. When assessing for bleeding, what assessment parameter should the nurse evaluate? A) Oral intake B) Pain intensity C) Level of consciousness D) Radiation of pain C Feedback: Bleeding is a major complication of kidney surgery. If undetected and untreated, this can result in hypovolemia and hemorrhagic shock. The nurses role is to observe for these complications, to report their signs and symptoms, and to administer prescribed parenteral fluids and blood and blood components. Monitoring of vital signs, skin condition, the urinary drainage system, the surgical incision, and the level of consciousness is necessary to detect evidence of bleeding, decreased circulating blood, and fluid volume and cardiac output. Bleeding is not normally evidenced by changes in pain or oral intake. 39. A nurse on the renal unit is caring for a patient who will soon begin peritoneal dialysis. The family of the patient asks for education about the peritoneal dialysis catheter that has been placed in the patients peritoneum. The nurse explains the three sections of the catheter and talks about the two cuffs on the dialysis catheter. What would the nurse explain about the cuffs? Select all that apply. A) The cuffs are made of Dacron polyester. B) The cuffs stabilize the catheter. C) The cuffs prevent the dialysate from leaking. D) The cuffs provide a barrier against microorganisms. E) The cuffs absorb dialysate A, B, C, D Feedback: Most of these catheters have two cuffs, which are made of Dacron polyester. The cuffs stabilize the catheter, limit movement, prevent leaks, and provide a barrier against microorganisms. They do not absorb dialysate. 40. A patient with chronic kidney disease is completing an exchange during peritoneal dialysis. The nurse observes that the peritoneal fluid is draining slowly and that the patients abdomen is increasing in girth. What is the nurses most appropriate action? A) Advance the catheter 2 to 4 cm further into the peritoneal cavity. B) Reposition the patient to facilitate drainage. C) Aspirate from the catheter using a 60-mL syringe. D) Infuse 50 mL of additional dialysate. B Feedback: If the peritoneal fluid does not drain properly, the nurse can facilitate drainage by turning the patient from side to side or raising the head of the bed. The catheter should never be pushed further into the peritoneal cavity. It would be unsafe to aspirate or to infuse more dialysate. Chapter 55: Management of Patients with Urinary Disorders 1. A female patient has been experiencing recurrent urinary tract infections. What health education should the nurse provide to this patient? A) Bathe daily and keep the perineal region clean. B) Avoid voiding immediately after sexual intercourse. C) Drink liberal amounts of fluids. D) Void at least every 6 to 8 hours. C Feedback: The patient is encouraged to drink liberal amounts of fluids (water is the best choice) to increase urine production and flow, which flushes the bacteria from the urinary tract. Frequent voiding (every 2 to 3 hours) is encouraged to empty the bladder completely because this can significantly lower urine bacterial counts, reduce urinary stasis, and prevent reinfection. The patient should be encouraged to shower rather than bathe. 2. A 42-year-old woman comes to the clinic complaining of occasional urinary incontinence when she sneezes. The clinic nurse should recognize what type of incontinence? A) Stress incontinence B) Reflex incontinence C) Overflow incontinence D) Functional incontinence A Feedback: Stress incontinence is the involuntary loss of urine through an intact urethra as a result of sudden increase in intra-abdominal pressure. Reflex incontinence is loss of urine due to hyperreflexia or involuntary urethral relaxation in the absence of normal sensations usually associated with voiding. Overflow incontinence is an involuntary urine loss associated with overdistension of the bladder. Functional incontinence refers to those instances in which the function of the lower urinary tract is intact, but other factors (outside the urinary system) make it difficult or impossible for the patient to reach the toilet in time for voiding. 3. A nurse is caring for a female patient whose urinary retention has not responded to conservative treatment. When educating this patient about self-catheterization, the nurse should encourage what practice? A) Assuming a supine position for self-catheterization B) Using clean technique at home to catheterize C) Inserting the catheter 1 to 2 inches into the urethra D) Self-catheterizing every 2 hours at home B Feedback: The patient may use a clean (nonsterile) technique at home, where the risk of cross-contamination is reduced. The average daytime clean intermittent catheterization schedule is every 4 to 6 hours and just before bedtime. The female patient assumes a Fowlers position and uses a mirror to help locate the urinary meatus. The nurse teaches her to catheterize herself by inserting a catheter 7.5 cm (3 inches) into the urethra, in a downward and backward direction. 4. A 52-year-old patient is scheduled to undergo ileal conduit surgery. When planning this patients discharge education, what is the most plausible nursing diagnosis that the nurse should address? A) Impaired mobility related to limitations posed by the ileal conduit B) Deficient knowledge related to care of the ileal conduit C) Risk for deficient fluid volume related to urinary diversion D) Risk for autonomic dysreflexia related to disruption of the sacral plexus B Feedback: The patient will most likely require extensive teaching about the care and maintenance of a new urinary diversion. A diversion does not create a serious risk of fluid volume deficit. Mobility is unlikely to be impaired after the immediate postsurgical recovery. The sacral plexus is not threatened by the creation of a urinary diversion. 5. The nurse on a urology unit is working with a patient who has been diagnosed with oxalate renal calculi. When planning this patients health education, what nutritional guidelines should the nurse provide? A) Restrict protein intake as ordered. B) Increase intake of potassium-rich foods. C) Follow a low-calcium diet. D) Encourage intake of food containing oxalates. A Feedback: Protein is restricted to 60 g/d, while sodium is restricted to 3 to 4 g/d. Low-calcium diets are generally not recommended except for true absorptive hypercalciuria. The patient should avoid intake of oxalate- containing foods and there is no need to increase potassium intake. 6. The nurse is caring for a patient who underwent percutaneous lithotripsy earlier in the day. What instruction should the nurse give the patient? A) Limit oral fluid intake for 1 to 2 days. B) Report the presence of fine, sand like particles through the nephrostomy tube. C) Notify the physician about cloudy or foul-smelling urine. D) Report any pink-tinged urine within 24 hours after the procedure. C Feedback: The patient should report the presence of foul-smelling or cloudy urine since this is suggestive of a UTI. Unless contraindicated, the patient should be instructed to drink large quantities of fluid each day to flush the kidneys. Sand like debris is normal due to residual stone products. Hematuria is common after lithotripsy. 7. A female patients most recent urinalysis results are suggestive of bacteriuria. When assessing this patient, the nurses data analysis should be informed by what principle? A) Most UTIs in female patients are caused by viruses and do not cause obvious symptoms. B) A diagnosis of bacteriuria requires three consecutive positive results. C) Urine contains varying levels of healthy bacterial flora. D) Urine samples are frequently contaminated by bacteria normally present in the urethral area. D Feedback: Because urine samples (especially in women) are commonly contaminated by the bacteria normally present in the urethral area, a bacterial count exceeding 105 colonies/mL of clean-catch, midstream urine is the measure that distinguishes true bacteriuria from contamination. A diagnosis does not require three consecutive positive results and urine does not contain a normal flora in the absence of a UTI. Most UTIs have a bacterial etiology. 8. The clinic nurse is preparing a plan of care for a patient with a history of stress incontinence. What role will the nurse have in implementing a behavioral therapy approach? A) Provide medication teaching related to pseudoephedrine sulfate. B) Teach the patient to perform pelvic floor muscle exercises. C) Prepare the patient for an anterior vaginal repair procedure. D) Provide information on periurethral bulking. B Feedback: Pelvic floor muscle exercises (sometimes called Kegel exercises) represent the cornerstone of behavioral intervention for addressing symptoms of stress, urge, and mixed incontinence. None of the other listed interventions has a behavioral approach. 9. The nurse and urologist have both been unsuccessful in catheterizing a patient with a prostatic obstruction and a full bladder. What approach does the nurse anticipate the physician using to drain the patients bladder? A) Insertion of a suprapubic catheter B) Scheduling the patient immediately for a prostatectomy C) Application of warm compresses to the perineum to assist with relaxation D) Medication administration to relax the bladder muscles and reattempting catheterization in 6 hours A Feedback: When the patient cannot void, catheterization is used to prevent overdistention of the bladder. In the case of prostatic obstruction, attempts at catheterization by the urologist may not be successful, requiring insertion of a suprapubic catheter. A prostatectomy may be necessary, but would not be undertaken for the sole purpose of relieving a urethral obstruction. Delaying by applying compresses or administering medications could result in harm. 10. The nurse has implemented a bladder retraining program for an older adult patient. The nurse places the patient on a timed voiding schedule and performs an ultrasonic bladder scan after each void. The nurse notes that the patient typically has approximately 50 mL of urine remaining in her bladder after voiding. What would be the nurses best response to this finding? A) Perform a straight catheterization on this patient. B) Avoid further interventions at this time, as this is an acceptable finding. C) Place an indwelling urinary catheter. D) Press on the patients bladder in an attempt to encourage complete emptying. B Feedback: In adults older than 60 years of age, 50 to 100 mL of residual urine may remain after each voiding because of the decreased contractility of the detrusor muscle. Consequently, further interventions are not likely warranted. 11. The nurse is caring for a patient recently diagnosed with renal calculi. The nurse should instruct the patient to increase fluid intake to a level where the patient produces at least how much urine each day? A) 1,250 mL B) 2,000 mL C) 2,750 mL D) 3,500 mL B Feedback: Unless contraindicated by renal failure or hydronephrosis, patients with renal stones should drink at least eight 8-ounce glasses of water daily or have IV fluids prescribed to keep the urine dilute. A urine output exceeding 2 L a day is advisable. 12. A patient with cancer of the bladder has just returned to the unit from the PACU after surgery to create an ileal conduit. The nurse is monitoring the patients urine output hourly and notifies the physician when the hourly output is less than what? A) 30 mL B) 50 mL C) 100 mL D) 125 mL A Feedback: A urine output below 30 mL/hr may indicate dehydration or an obstruction in the ileal conduit, with possible backflow or leakage from the ureteroileal anastomosis. 13. The nurse is caring for a patient with an indwelling urinary catheter. The nurse is aware that what nursing action helps prevent infection in a patient with an indwelling catheter? A) Vigorously clean the meatus area daily. B) Apply powder to the perineal area twice daily. C) Empty the drainage bag at least every 8 hours. D) Irrigate the catheter every 8 hours with normal saline. C Feedback: To reduce the risk of bacterial proliferation, the nurse should empty the collection bag at least every 8 hours through the drainage spout, and more frequently if there is a large volume of urine. Vigorous cleaning of the meatus while the catheter is in place is discouraged, because the cleaning action can move the catheter, increasing the risk of infection. The spout (or drainage port) of any urinary drainage bag can become contaminated when opened to drain the bag. Irrigation of the catheter opens the closed system, increasing the likelihood of infection. 14. The nurse is teaching a health class about UTIs to a group of older adults. What characteristic of UTIs should the nurse cite? A) Men over age 65 are equally prone to UTIs as women, but are more often asymptomatic. B) The prevalence of UTIs in men older than 50 years of age approaches that of women in the same age group. C) Men of all ages are less prone to UTIs, but typically experience more severe symptoms. D) The prevalence of UTIs in men cannot be reliably measured, as men generally do not report UTIs. B Feedback: The antibacterial activity of the prostatic secretions that protect men from bacterial colonization of the urethra and bladder decreases with aging. The prevalence of infection in men older than 50 years of age approaches that of women in the same age group. Men are not more likely to be asymptomatic and are not known to be reluctant to report UTIs. 15. A patient has been admitted to the postsurgical unit following the creation of an ileal conduit. What should the nurse measure to determine the size of the appliance needed? A) The circumference of the stoma B) The narrowest part of the stoma C) The widest part of the stoma D) Half the width of the stoma C Feedback: The correct appliance size is determined by measuring the widest part of the stoma with a ruler. The permanent appliance should be no more than 1.6 mm (1/8 inch) larger than the diameter of the stoma and the same shape as the stoma to prevent contact of the skin with drainage. 16. A patient being treated in the hospital has been experiencing occasional urinary retention. What nursing action should the nurse take to encourage a patient who is having difficulty voiding? A) Use a slipper bedpan. B) Apply a cold compress to the perineum. C) Have the patient lie in a supine position. D) Provide privacy for the patient. D Feedback: Nursing measures to encourage normal voiding patterns include providing privacy, ensuring an environment and body position conducive to voiding, and assisting the patient with the use of the bathroom or bedside commode, rather than a bedpan, to provide a more natural setting for voiding. Most people find supine positioning not conducive to voiding. 17. A nurses colleague has applied an incontinence pad to an older adult patient who has experienced occasional episodes of functional incontinence. What principle should guide the nurses management of urinary incontinence in older adults? A) Diuretics should be promptly discontinued when an older adult experiences incontinence. B) Restricting fluid intake is recommended for older adults experiencing incontinence. C) Urinary catheterization is a first-line treatment for incontinence in older adults with incontinence. D) Urinary incontinence is not considered a normal consequence of aging. D Feedback: Nursing management is based on the premise that incontinence is not inevitable with illness or aging and that it is often reversible and treatable. Diuretics cannot always be safely discontinued. Fluid restriction and catheterization are not considered to be safe, first-line interventions for the treatment of incontinence. 18. The nurse is working with a patient who has been experiencing episodes of urinary retention. What assessment finding would suggest that the patient is experiencing retention? A) The patients suprapubic region is dull on percussion. B) The patient is uncharacteristically drowsy. C) The patient claims to void large amounts of urine 2 to 3 times daily. D) The patient takes a beta adrenergic blocker for the treatment of hypertension. A Feedback: Dullness on percussion of the suprapubic region is suggestive of urinary retention. Patients retaining urine are typically restless, not drowsy. A patient experiencing retention usually voids frequent, small amounts of urine and the use of beta-blockers is unrelated to urinary retention. 19. A patient with kidney stones is scheduled for extracorporeal shock wave lithotripsy (ESWL). What should the nurse include in the patients post-procedure care? A) Strain the patients urine following the procedure. B) Administer a bolus of 500 mL normal saline following the procedure. C) Monitor the patient for fluid overload following the procedure. D) Insert a urinary catheter for 24 to 48 hours after the procedure. A Feedback: Following ESWL, the nurse should strain the patients urine for gravel or sand. There is no need to administer an IV bolus after the procedure and there is not a heightened risk of fluid overload. Catheter insertion is not normally indicated following ESWL. 20. The nurse is caring for a patient who has undergone creation of a urinary diversion. Forty-eight hours postoperatively, the nurses assessment reveals that the stoma is a dark purplish color. What is the nurses most appropriate response? A) Document the presence of a healthy stoma. B) Assess the patient for further signs and symptoms of infection. C) Inform the primary care provider that the vascular supply may be compromised. D) Liaise with the wound-ostomy-continence (WOC) nurse because the ostomy appliance around the stoma may be too loose. C Feedback: A healthy stoma is pink or red. A change from this normal color to a dark purplish color suggests that the vascular supply may be compromised. A loose ostomy appliance and infections do not cause a dark purplish stoma. 21. A patient is undergoing diagnostic testing for a suspected urinary obstruction. The nurse should know that incomplete emptying of the bladder due to bladder outlet obstruction can cause what? A) Hydronephrosis B) Nephritic syndrome C) Pylonephritis D) Nephrotoxicity A Feedback: If voiding dysfunction goes undetected and untreated, the upper urinary system may become compromised. Chronic incomplete bladder emptying from poor detrusor pressure results in recurrent bladder infection. Incomplete bladder emptying due to bladder outlet obstruction, causing high-pressure detrusor contractions, can result in hydronephrosis from the high detrusor pressure that radiates up the ureters to the renal pelvis. This problem does not normally cause nephritic syndrome or pyelonephritis. Nephrotoxicity results from chemical causes. 22. The nurse is assessing a patient admitted with renal stones. During the admission assessment, what parameters would be priorities for the nurse to address? Select all that apply. A) Dietary history B) Family history of renal stones C) Medication history D) Surgical history E) Vaccination history A, B, C Feedback: Dietary and medication histories and family history of renal stones are obtained to identify factors predisposing the patient to stone formation. When caring for a patient with renal stones it would not normally be a priority to assess the vaccination history or surgical history, since these factors are not usually related to the etiology of kidney stones. 23. A nurse who provides care in a long-term care facility is aware of the high incidence and prevalence of urinary tract infections among older adults. What action has the greatest potential to prevent UTIs in this population? A) Administer prophylactic antibiotics as ordered. B) Limit the use of indwelling urinary catheters. C) Encourage frequent mobility and repositioning. D) Toilet residents who are immobile on a scheduled basis. B Feedback: When indwelling catheters are used, the risk of UTI increases dramatically. Limiting their use significantly reduces an older adults risk of developing a UTI. Regular toileting promotes continence, but has only an indirect effect on the risk of UTIs. Prophylactic antibiotics are not normally administered. Mobility does not have a direct effect on UTI risk. 24. A gerontologic nurse is assessing a patient who has numerous comorbid health problems. What assessment findings should prompt the nurse to suspect a UTI? Select all that apply. A) Food cravings B) Upper abdominal pain C) Insatiable thirst D) Uncharacteristic fatigue E) New onset of confusion D Feedback: The most common subjective presenting symptom of UTI in older adults is generalized fatigue. The most common objective finding is a change in cognitive functioning. Food cravings, increased thirst, and upper abdominal pain necessitate further assessment and intervention, but none is directly suggestive of a UTI. 25. A female patient has been prescribed a course of antibiotics for the treatment of a UTI. When providing health education for the patient, the nurse should address what topic? A) The risk of developing a vaginal yeast infection as a consequent of antibiotic therapy B) The need to expect a heavy menstrual period following the course of antibiotics C) The risk of developing antibiotic resistance after the course of antibiotics D) The need to undergo a series of three urine cultures after the antibiotics have been completed A Feedback: Yeast vaginitis occurs in as many as 25% of patients treated with antimicrobial agents that affect vaginal flora. Yeast vaginitis can cause more symptoms and be more difficult and costly to treat than the original UTI. Antibiotics do not affect menstrual periods and serial urine cultures are not normally necessary. Resistance is normally a result of failing to complete a prescribed course of antibiotics. 26. An adult patient has been hospitalized with pyelonephritis. The nurses review of the patients intake and output records reveals that the patient has been consuming between 3 L and 3.5 L of oral fluid each day since admission. How should the nurse best respond to this finding? A) Supplement the patients fluid intake with a high-calorie diet. B) Emphasize the need to limit intake to 2 L of fluid daily. C) Obtain an order for a high-sodium diet to prevent dilutional hyponatremia. D) Encourage the patient to continue this pattern of fluid intake. D Feedback: Unless contraindicated, 3 to 4 L of fluids per day is encouraged to dilute the urine, decrease burning on urination, and prevent dehydration. No need to supplement this fluid intake with additional calories or sodium. 27. An older adult has experienced a new onset of urinary incontinence and family members identify this problem as being unprecedented. When assessing the patient for factors that may have contributed to incontinence, the nurse should prioritize what assessment? A) Reviewing the patients 24-hour food recall for changes in diet B) Assessing for recent contact with individuals who have UTIs C) Assessing for changes in the patients level of psychosocial stress D) Reviewing the patients medication administration record for recent changes D Feedback: Many medications affect urinary continence in addition to causing other unwanted or unexpected effects. Stress and dietary changes could potentially affect the patients continence, but medications are more frequently causative of incontinence. UTIs can cause incontinence, but these infections do not result from contact with infected individuals. 28. A nurse is working with a female patient who has developed stress urinary incontinence. Pelvic floor muscle exercises have been prescribed by the primary care provider. How can the nurse best promote successful treatment? A) Clearly explain the potential benefits of pelvic floor muscle exercises. B) Ensure the patient knows that surgery will be required if the exercises are unsuccessful. C) Arrange for biofeedback when the patient is learning to perform the exercises. D) Contact the patient weekly to ensure that she is performing the exercises consistently. C Feedback: Research shows that written or verbal instruction alone is usually inadequate to teach an individual how to identify and strengthen the pelvic floor for sufficient bladder and bowel control. Biofeedback-assisted pelvic muscle exercise (PME) uses either electromyography or manometry to help the individual identify the pelvic muscles as he or she attempts to learn which muscle group is involved when performing PME. This objective assessment is likely superior to weekly contact with the patient. Surgery is not necessarily indicated if behavioral techniques are unsuccessful. 29. A patient has a flaccid bladder secondary to a spinal cord injury. The nurse recognizes this patients high risk for urinary retention and should implement what intervention in the patients plan of care? A) Relaxation techniques B) Sodium restriction C) Lower abdominal massage D) Double voiding D Feedback: To enhance emptying of a flaccid bladder, the patient may be taught to double void. After each voiding, the patient is instructed to remain on the toilet, relax for 1 to 2 minutes, and then attempt to void again in an effort to further empty the bladder. Relaxation does not affect the neurologic etiology of a flaccid bladder. Sodium restriction and massage are similarly ineffective. 30. A patient with a sacral pressure ulcer has had a urinary catheter inserted. As a result of this new intervention, the nurse should prioritize what nursing diagnosis in the patients plan of care? A) Impaired physical mobility related to presence of an indwelling urinary catheter B) Risk for infection related to presence of an indwelling urinary catheter C) Toileting self-care deficit related to urinary catheterization D) Disturbed body image related to urinary catheterization B Feedback: Catheters create a high risk for UTIs. Because of this acute physiologic threat, the patients risk for infection is usually prioritized over functional and psychosocial diagnoses. 31. A patient has had her indwelling urinary catheter removed after having it in place for 10 days during recovery from an acute illness. Two hours after removal of the catheter, the patient informs the nurse that she is experiencing urinary urgency resulting in several small-volume voids. What is the nurses best response? A) Inform the patient that urgency and occasional incontinence are expected for the first few weeks post-removal. B) Obtain an order for a loop diuretic in order to enhance urine output and bladder function. C) Inform the patient that this is not unexpected in the short term and scan the patients bladder following each void. D) Obtain an order to reinsert the patients urinary catheter and attempt removal in 24 to 48 hours. C Feedback: Immediately after the indwelling catheter is removed, the patient is placed on a timed voiding schedule, usually every 2 to 3 hours. At the given time interval, the patient is instructed to void. The bladder is then scanned using a portable ultrasonic bladder scanner; if the bladder has not emptied completely, straight catheterization may be performed. An indwelling catheter would not be reinserted to resolve the problem and diuretics would not be beneficial. Ongoing incontinence is not an expected finding after catheter removal. 32. A nurse on a busy medical unit provides care for many patients who require indwelling urinary catheters at some point during their hospital care. The nurse should recognize a heightened risk of injury associated with indwelling catheter use in which patient? A) A patient whose diagnosis of chronic kidney disease requires a fluid restriction B) A patient who has Alzheimers disease and who is acutely agitated C) A patient who is on bed rest following a recent episode of venous thromboembolism D) A patient who has decreased mobility following a transmetatarsal amputation B Feedback: Patients who are confused and agitated risk trauma through the removal of an indwelling catheter which has the balloon still inflated. Recent VTE, amputation, and fluid restriction do not directly create a risk for injury or trauma associated with indwelling catheter use. 33. A patient has been admitted to the medical unit with a diagnosis of ureteral colic secondary to urolithiasis. When planning the patients admission assessment, the nurse should be aware of the signs and symptoms that are characteristic of this diagnosis? Select all that apply. A) Diarrhea B) High fever C) Hematuria D) Urinary frequency E) Acute pain C, D, E Feedback: Stones lodged in the ureter (ureteral obstruction) cause acute, excruciating, colicky, wavelike pain, radiating down the thigh and to the genitalia. Often, the patient has a desire to void, but little urine is passed, and it usually contains blood because of the abrasive action of the stone. This group of symptoms is called ureteral colic. Diarrhea is not associated with this presentation and a fever is usually absent due to the noninfectious nature of the health problem. 34. A patient with a recent history of nephrolithiasis has presented to the ED. After determining that the patients cardiopulmonary status is stable, what aspect of care should the nurse prioritize? A) IV fluid administration B) Insertion of an indwelling urinary catheter C) Pain management D) Assisting with aspiration of the stone C Feedback: The patient with kidney stones is often in excruciating pain, and this is a high priority for nursing interventions. In the short term, this would supersede the patients need for IV fluids or for catheterization. Kidney stones cannot be aspirated. 35. A patient has been successfully treated for kidney stones and is preparing for discharge. The nurse recognizes the risk of recurrence and has planned the patients discharge education accordingly. What preventative measure should the nurse encourage the patient to adopt? A) Increasing intake of protein from plant sources B) Increasing fluid intake C) Adopting a high-calcium diet D) Eating several small meals each day B Feedback: Increased fluid intake is encouraged to prevent the recurrence of kidney stones. Protein intake from all sources should be limited. Most patients do not require a low-calcium diet, but increased calcium intake would be contraindicated for all patients. Eating small, frequent meals does not influence the risk for recurrence. 36. A patient who has recently undergone ESWL for the treatment of renal calculi has phoned the urology unit where he was treated, telling the nurse that he has a temperature of 101.1F (38.4C). How should the nurse best respond to the patient? A) Remind the patient that renal calculi have a noninfectious etiology and that a fever is unrelated to their recurrence. B) Remind the patient that occasional febrile episodes are expected following ESWL. C) Tell the patient to report to the ED for further assessment. D) Tell the patient to monitor his temperature for the next 24 hours and then contact his urologists office. C Feedback: Following ESWL, the development of a fever is abnormal and is suggestive of a UTI; prompt medical assessment and treatment are warranted. It would be inappropriate to delay further treatment. 37. The nurse who is leading a wellness workshop has been asked about actions to reduce the risk of bladder cancer. What health promotion action most directly addresses a major risk factor for bladder cancer? A) Smoking cessation B) Reduction of alcohol intake C) Maintenance of a diet high in vitamins and nutrients D) Vitamin D supplementation A Feedback: People who smoke develop bladder cancer twice as often as those who do not smoke. High alcohol intake and low vitamin intake are not noted to contribute to bladder cancer. 38. Resection of a patients bladder tumor has been incomplete and the patient is preparing for the administration of the first ordered instillation of topical chemotherapy. When preparing the patient, the nurse should emphasize the need to do which of the following? A) Remain NPO for 12 hours prior to the treatment. B) Hold the solution in the bladder for 2 hours before voiding. C) Drink the intravesical solution quickly and on an empty stomach. D) Avoid acidic foods and beverages until the full cycle of treatment is complete. B Feedback: The patient is allowed to eat and drink before the instillation procedure. Once the bladder is full, the patient must retain the intravesical solution for 2 hours before voiding. The solution is instilled through the meatus; it is not consumed orally. There is no need to avoid acidic foods and beverages during treatment. 39. The nurse has tested the pH of urine from a patients newly created ileal conduit and obtained a result of 6.8. What is the nurses best response to this assessment finding? A) Obtain an order to increase the patients dose of ascorbic acid. B) Administer IV sodium bicarbonate as ordered. C) Encourage the patient to drink at least 500 mL of water and retest in 3 hours. D) Irrigate the ileal conduit with a dilute citric acid solution as ordered. A Feedback: Because severe alkaline encrustation can accumulate rapidly around the stoma, the urine pH is kept below 6.5 by administration of ascorbic acid by mouth. An increased pH may suggest a need to increase ascorbic acid dosing. This is not treated by administering bicarbonate or citric acid, nor by increasing fluid intake. 40. A patient is postoperative day 3 following the creation of an ileal conduit for the treatment of invasive bladder cancer. The patient is quickly learning to self-manage the urinary diversion, but expresses concern about the presence of mucus in the urine. What is the nurses most appropriate response? A) Report this finding promptly to the primary care provider. B) Obtain a sterile urine sample and send it for culture. C) Obtain a urine sample and check it for pH. D) Reassure the patient that this is an expected phenomenon. D Feedback: Because mucous membrane is used in forming the conduit, the patient may excrete a large amount of mucus mixed with urine. This causes anxiety in many patients. To help relieve this anxiety, the nurse reassures the patient that this is a normal occurrence after an ileal conduit procedure. Urine testing for culture or pH is not required. 41. The nurse is collaborating with the wound-ostomy-continence (WOC) nurse to teach a patient how to manage her new ileal conduit in the home setting. To prevent leakage or skin breakdown, the nurse should encourage which of the following practices? A) Empty the collection bag when it is between one-half and two-thirds full. B) Limit fluid intake to prevent production of large volumes of dilute urine. C) Reinforce the appliance with tape if small leaks are detected. D) Avoid using moisturizing soaps and body washes when cleaning the peristomal area. D Feedback: The patient is instructed to avoid moisturizing soaps and body washes when cleaning the area because they interfere with the adhesion of the pouch. To maintain skin integrity, a skin barrier or leaking pouch is never patched with tape to prevent accumulation of urine under the skin barrier or faceplate. Fluids should be encouraged, not limited, and the collection bag should not be allowed to become more than one-third full. 42. A patient has undergone the creation of an Indiana pouch for the treatment of bladder cancer. The nurse identified the nursing diagnosis of disturbed body image. How can the nurse best address the effects of this urinary diversion on the patients body image? A) Emphasize that the diversion is an integral part of successful cancer treatment. B) Encourage the patient to speak openly and frankly about the diversion. C) Allow the patient to initiate the process of providing care for the diversion. D) Provide the patient with detailed written materials about the diversion at the time of discharge. B Feedback: Allowing the patient to express concerns and anxious feelings can help with body image, especially in adjusting to the changes in toileting habits. The nurse may have to initiate dialogue about the management of the diversion, especially if the patient is hesitant. Provision of educational materials is rarely sufficient to address a sudden change and profound change in body image. Emphasizing the role of the diversion in cancer treatment does not directly address the patients body image. Chapter 56: Assessment and Management of Patients With Female Physiologic Processes 1. A school nurse is presenting information on human development and sexuality. When describing the role of hormones in sexual development, which hormone does the nurse teach the class is the most important one for developing and maintaining the female reproductive organs? A) Estrogen B) Progesterone C) Androgens D) Follicle-stimulating hormone A Feedback: Estrogens are responsible for developing and maintaining the female reproductive organs. Progesterone is the most important hormone for conditioning the endometrium in preparation for implantation of the fertilized ovum. Androgens, secreted by the ovaries in small amounts, are involved in the early development of the follicle and affect the female libido. Follicle-stimulating hormone is responsible for stimulating the ovaries to secrete estrogen. 2. The nurse is taking the sexual history of an adolescent who has come into the free clinic. What question best assesses the patients need for further information? A) Are you involved in an intimate relationship at this time? B) How many sexual partners have you had? C) What questions or concerns do you have about your sexual health? D) Have you ever been diagnosed with a sexually transmitted infection? C Feedback: An open-ended question related to the patients need for further information should be included while obtaining a sexual history. None of the other listed questions are open-ended. 3. The nurse is being trained to perform assessment screenings for abuse on patients who come into the walk-in clinic where the nurse works. Which of the following assessment questions is most appropriate? A) Would you describe your relationship as healthy and functional? B) Have you ever been forced into sexual activity? C) Do you make your husband uncontrollably angry? D) How is conflict usually handled in your home? B Feedback: Asking about abuse directly is effective in identifying the presence of abuse and should be included in the health history of all women. Oblique questions that relate to the character of the relationship or conflict resolution are less useful clinically. Asking about making a partner angry is not an appropriate way to screen for family violence because it does not directly address the problem. 4. A premenopausal patient is complaining of vaginal spotting and sharp, colicky lower abdominal pain. She informs the nurse that her period is 2 weeks late. The nurse should recognize a need for this patient to be investigated for what health problem? A) Trichomonas vaginalis B) Ectopic pregnancy C) Cervical cancer D) Fibromyalgia B Feedback: Clinical symptoms of an ectopic pregnancy include delay in menstruation of 1 to 2 weeks, vaginal spotting, and sharp, colicky pain. Trichomonas vaginalis causes a vaginal infection. Cervical cancer and fibromyalgia do not affect menstruation. 5. A female patient who has cognitive and physical disabilities has come into the clinic for a routine check- up. When planning this patients assessment, what action should the nurse take? A) Ensure that a chaperone is available to be present during the assessment. B) Limit the length and scope of the health assessment. C) Avoid health promotion or disease prevention education. D) Avoid equating the patient with her disabilities. D Feedback: When working with women who have disabilities, it is important that the nurse avoid equating the woman with her disability; the nurse must make an effort to understand that the patient and the disability are not synonymous. A chaperone is not necessarily required and there may or may not be a need to abbreviate the assessment. The nurse should provide education as needed. 6. A patient calls the clinic and tells the nurse she has thick white, curd-like discharge from her vagina. How should the nurse best interpret this preliminary data? A) The drainage is physiologic and normal. B) The patient may have a Candida species infection. C) The patient needs a Pap smear as soon as possible. D) The patient may have a Trichomonas infection. B Feedback: Drainage caused by Candida is typically curd-like and white. Trichomonas infections usually cause copious, frothy yellowish-green discharge. There is no immediate need for a Pap smear, as malignancy is an unlikely cause. 7. A nurse presenting an educational event for a local community group is addressing premenstrual syndrome (PMS). What treatment guideline should the nurse teach this group? A) Avoid excessive fluid intake. B) Increase the frequency and intensity of exercise. C) Limit psychosocial stressors in order to reduce symptoms. D) Take opioid analgesics as ordered. B Feedback: In general, the patient is encouraged to increase or initiate an exercise program to help relieve symptoms of PMS. Fluid intake should be increased. Opioids are not used to treat PMS. Stress reduction has multiple benefits, but it is not noted to alleviate the symptoms of PMS. 8. A nurse is collecting assessment data from a premenopausal patient who states that she does not have menses. What term should the nurse use to document the absence of menstrual flow? A) Amenorrhea B) Dysmenorrhea C) Menorrhagia D) Metrorrhagia A Feedback: Amenorrhea refers to absence of menstrual flow, whereas dysmenorrhea is painful menstruation. Menorrhagia, also called hypermenorrhea, is defined as prolonged or excessive bleeding at the time of the regular menstrual flow. Metrorrhagia refers to vaginal bleeding between regular menstrual periods. 9. A new patient has come to the clinic seeking an appropriate method of birth control. What would the nurse teach this patient about a diaphragm? A) One size fits all females. B) The diaphragm may be cleaned with soap and water after use. C) A diaphragm eliminates the need for spermicidal jelly. D) The diaphragm should be removed 1 hour following intercourse. B Feedback: The diaphragm may be cleaned with soap and water after use. It must be left in 6 hours after intercourse and should be used with spermicidal jelly. There are different sizes of diaphragms and the patient needs to be fitted by the health care practitioner. 10. A patient who is in the first trimester of pregnancy has experienced an incomplete abortion. The obstetric nurse should prepare the patient for what possible intervention? A) Dilation and evacuation B) Several days of bed rest C) Administration of hydromorphone D) IV administration of clomiphene A Feedback: If only some of the tissue is passed, the abortion is referred to as incomplete. An emptying or evacuation procedure (D&C, or dilation and evacuation [D&E]) or administration of oral misoprostol (Cytotec) is usually required to remove the remaining tissue. Bed rest will not necessarily result in the passing of all the tissue. Clomiphene and hydromorphone are of no therapeutic benefit. 11. A patient in her late fifties has expressed to the nurse her desire to explore hormone replacement therapy (HRT). Based on what aspect of the patients health history is HRT contraindicated? A) History of vaginal dryness B) History of hot flashes and night sweats C) History of vascular thrombosis D) Family history of osteoporosis C Feedback: The use of HRT is contraindicated in women with a history of vascular thrombosis, active liver disease, some cases of uterine cancer, and undiagnosed vaginal bleeding. HRT is beneficial in women with a risk for osteoporosis. Vaginal dryness, hot flashes, and night sweats are symptoms of menopause that may be relieved with HRT. 12. The school nurse is presenting a class on female reproductive health. The nurse should describe what aspect of Pap smears? A) The test may be performed at any time during the patients menstrual cycle. B) The smear should be done every 2 years. C) The test can detect early evidence of cervical cancer. D) Falsepositive Pap smear results occur mostly from not douching before the examination. C Feedback: The test should be performed when the patient is not menstruating. Douching washes away cellular material. The test detects cervical cancer, and falsenegative Pap smear results occur mostly from sampling errors or improper technique. For most women, a Pap smear should be done annually. 13. A nurse practitioner is preparing to perform a patients scheduled Pap smear and the patient asks the nurse to ensure that the speculum is well-lubricated. How should the nurse proceed with assessment? A) Reassure the patient that ample petroleum jelly will be used. B) Reassure that patient that a water-based lubricant will be used. C) Explain to the patient that water is the only lubricant that can be used. D) Explain to the patient why the speculum must be introduced dry. C Feedback: Because lubricants may obscure cells on a Pap smear, warm water is the only lubricant that can be used. 14. A clinic nurse is meeting with a 38-year-old patient who states that she would like to resume using oral contraceptives, which she used for several years during her twenties. What assessment question is most likely to reveal a potential contraindication to oral contraceptive use? A) Have you ever had surgery? B) Have you ever had a sexually transmitted infection? C) When did you last have your blood sugar levels checked? D) Do you smoke? D Feedback: Women who smoke and who are 35 years of age or older should not take oral contraceptives because of an increased risk for cardiac problems. Previous surgeries, STIs, and blood sugar instability do not necessarily contraindicate the use of oral contraceptives. 15. A 17-year-old girl has come to the free clinic for her annual examination. She tells the nurse she uses tampons and asks how long she may safely leave her tampon in place. What is the nurses best response? A) You may leave the tampon in overnight. B) The tampon should be changed at least twice per day. C) Tampons are dangerous and, ideally, you should not be using them. D) Tampons need to be changed every 4 to 6 hours. D Feedback: Tampons should not be used for more than 4 to 6 hours, nor should super-absorbent tampons be used because of the association with toxic shock syndrome. If used appropriately, it is acceptable and safe for the patient to use tampons. 16. A 51-year-old woman has come to the OB/GYN clinic for her annual physical. She tells the nurse that she has been experiencing severe hot flashes, but that she is reluctant to begin hormone therapy (HT). What potential solution should the nurse discuss with the patient? A) Sodium restriction B) Adopting a vegan diet C) Massage therapy D) Vitamin supplements D Feedback: For some women, vitamins B6 and E have proven beneficial for the treatment of hot flashes. Sodium restriction, vegan diet, and massage have not been noted to relieve this symptom of perimenopause. 17. A newly pregnant patient is being assessed in an obstetric clinic. The patient states that she has been experiencing intense abdominal pain and the nurse anticipates that the patient will be assessed for ectopic pregnancy. In addition to ultrasonography, what diagnostic test should the nurse anticipate? A) Computed tomography B) Human chorionic gonadotropin (hCG) testing C) Estrogen and progesterone testing D) Abdominal x-ray B Feedback: If an ectopic pregnancy is suspected, the patient is assessed using ultrasound and hCG testing. CT and x- rays are contraindicated during pregnancy and estrogen and progesterone levels are not diagnostic of ectopic pregnancy. 18. An adolescent is brought to the clinic by her mother because of abnormal uterine bleeding. The nurse should understand that the most likely cause of this dysfunctional bleeding pattern is what? A) Lack of ovulation B) Chronic vaginitis C) A sexually transmitted infection D) Ectopic pregnancy A Feedback: Dysfunctional uterine bleeding can occur at any age, but is most common at opposite ends of the reproductive life span. It is usually secondary to anovulation (lack of ovulation) and is common in adolescents. It is not suggestive of vaginitis, an STI, or ectopic pregnancy. 19. The nurse is planning the sexual assessment of a new adolescent patient. The nurse should include what assessment components? Select all that apply. A) Physical examination findings B) Laboratory results C) Health history D) Interpersonal skills E) Understanding of menopause A, B, C Feedback: A sexual assessment includes both subjective and objective data. Health and sexual histories, physical examination findings, and laboratory results are all part of the database. A sexual assessment would not normally include the patients interpersonal skills. It is not likely to necessary to assess an adolescents understanding of menopause. 20. By initiating an assessment about sexual concerns what does the nurse convey to the patient? Select all that apply. A) That sexual issues are valid health issues B) That it is safe to talk about sexual issues C) That sexual issues are only a minor aspect a persons identity D) That changes or problems in sexual functioning should be discussed E) That changes or problems in sexual functioning are highly atypical A, B, D Feedback: By initiating an assessment about sexual concerns, the nurse communicates to the patient that issues about changes or problems in sexual functioning are valid and significant health issues. The nurse communicates that it is safe to talk about sexual issues and that changes or challenges in sexual function are not unusual. 21. The nurse is utilizing the PLISSIT model of sexual health assessment during an interaction with a new patient. According to this model, the nurse should begin with what action? A) Conducting a preliminary assessment B) Addressing the patients psychosocial status C) Asking the patients permission to discuss sexuality D) Assessing for physiologic problems C Feedback: The PLISSIT model of sexual assessment begins with permission and subsequently includes limited information, specific suggestions, and intensive therapy. 22. During the nurses assessment of a female patient, the patient reveals that she experienced sexual abuse when she was a young woman. What is the nurses most appropriate response to this disclosure? A) Reassure her that this information will be kept a secret. B) Begin the process of intensive psychotherapy. C) Encourage the patient to phone 911. D) Facilitate appropriate resources and referrals. D Feedback: The nurses primary roles in light of this disclosure are to provide empathy and to arrange for appropriate resources and referrals. There is no need to phone 911 and psychotherapy is beyond the nurses scope of practice. The patients confidentiality will be respected, but this does not mean that the nurse can promise to keep it a secret. 23. A 15-year-old girl is brought to the clinic by her mother to see her primary care provider. The mother states that her daughter has not started to develop sexually. The physical examination shows that the patient has no indication of secondary sexual characteristics. What diagnosis should the nurse suspect? A) Primary amenorrhea B) Dyspareunia C) Vaginal atrophy D) Secondary dysmenorrhea A Feedback: Primary amenorrhea (delayed menarche) refers to the situation in which young women older than 16 years of age have not begun to menstruate but otherwise show evidence of sexual maturation, or in which young women have not begun to menstruate and have not begun to show development of secondary sex characteristics by 14 years of age. In secondary dysmenorrhea, pelvic pathology such as endometriosis, tumor, or pelvic inflammatory disease (PID) contributes to symptoms. Dyspareunia is painful intercourse and vaginal atrophy would not contribute to the delayed onset of puberty. 24. A 36-year-old woman comes to the clinic complaining of premenstrual syndrome (PMS) that is disrupting her quality of life. What signs and symptoms are associated with this health problem? Select all that apply. A) Loss of appetite B) Breast tenderness C) Depression D) Fluid retention E) Headache B, C, D, E Feedback: Physiologic symptoms of PMS include headache, breast tenderness, and fluid retention as well as affective symptoms, such as depression. Loss of appetite is not noted to be among the most common symptoms. 25. A patient states that PMS that is significantly disrupting her quality of life and that conservative management has failed to produce relief. What pharmacologic treatment may benefit this patient? A) An opioid analgesic B) A calcium channel blocker C) A monoamine oxidase inhibitor (MAOI) D) A selective serotonin reuptake inhibitor (SSRI) D Feedback: Pharmacologic remedies for PMS include selective serotonin reuptake inhibitors. MAOIs are not used for this purpose. Calcium channel blockers and opioids would not lead to symptom relief. 26. The nurse is assessing a 53-year-old woman who has been experiencing dysmenorrhea. What questions should the nurse include in an assessment of the patients menstrual history? Select all that apply. A) Do you ever experience bleeding after intercourse? B) How long is your typical cycle? C) Did you have any sexually transmitted infections in early adulthood? D) When did your mother and sisters get their first periods? E) Do you experience cramps or pain during your cycle? A, B, E Feedback: Menstrual history addresses such factors as the length of cycles, duration and amount of flow, presence of cramps or pain, and bleeding between periods or after intercourse. Family members menarche and prior STIs are not likely to affect the patients current cycles. 27. The nurse is working with a couple who have been unable to conceive despite more than 2 years of trying to get pregnant. The couple has just learned that in vitro fertilization (IVF) was unsuccessful and they are both tearful. What nursing diagnosis is most likely to apply to this couple? A) Hopelessness related to failed IVF B) Acute confusion related to reasons for failed IVF C) Compromised family coping related to unsuccessful IVF D) Moral distress related to unsuccessful IVF A Feedback: Although further assessment is undoubtedly necessary, it is likely that the couple will be experiencing hopelessness at the news that a potentially promising intervention has failed. Acute confusion denotes a cognitive deficit, not a sense of despair. Sadness at this news is not necessarily suggestive of impaired coping. Moral distress is unlikely because this is not a situation involving morality. 28. A 48-year-old woman presenting for care is seeking information about hormone therapy (HT) for the treatment of her perimenopausal symptoms. The patients need for relief from hot flashes and other symptoms will be weighed carefully against the increased risks of what complications of HT? Select all that apply. A) Anaphylaxis B) Osteoporosis C) Breast cancer D) Cardiovascular disease E) Venous thromboembolism C, D, E Feedback: Although HT decreases hot flashes and reduces the risk of osteoporotic fractures as well as colorectal cancer, studies have shown that it increases the risk of breast cancer, heart attack, stroke, and blood clots. There is no significant risk of anaphylaxis. 29. A 27-year-old primipara presents to the ED with vaginal bleeding and suspected contractions. The woman relates that she is 14 weeks pregnant and she thinks she is losing her baby. Diagnostic testing confirms a spontaneous abortion. What nursing action would be a priority at this time? A) Leave the patient alone so she can grieve in private. B) Teach the patient that this will not affect her future chance of conception. C) Take the patient off the obstetric floor so she will not hear a baby cry. D) Provide opportunities for the patient to talk and express her emotions. D Feedback: Providing opportunities for the patient to talk and express her emotions is helpful and also provides clues for the nurse in planning more specific care. The patient may or may not want to be alone, but the nurse should first determine her wishes. It would be inappropriate to refer to future pregnancies during this acute time of loss. It would not be necessary or practical to remove the patient from the unit. 30. A couple has come to the infertility clinic because they have been unable to get pregnant even though they have been trying for over a year. Diagnostic tests are planned for the woman to ascertain if ovulation is regular and whether her endometrium is adequately supported for implantation. What test would the nurse expect to have ordered for this woman? A) Serum progesterone B) Abdominal CT C) Oocyte viability test D) Urine testosterone A Feedback: Diagnostic studies performed to determine if ovulation is regular and whether the progestational endometrium is adequate for implantation may include a serum progesterone level and an ovulation index. None of the other listed tests is used to investigate infertility. 31. The nurse is caring for a couple trying to get pregnant and have not been able to for over a year. The couple asks what kind of problems a man can have that can cause infertility. What should be the nurses response? A) Men can have increased prolactin levels that decrease sperm viability. B) Men can have problems that increase the temperature around their testicles and decrease the quality of their semen. C) Men may inherit the gene that causes low sperm production. D) Men may produce sperm that are incompatible with the shape of the egg. B Feedback: Men may be affected by varicoceles, varicose veins around the testicle, which decrease semen quality by increasing testicular temperature. Low prolactin levels may contribute to the problem. Genetic factors are not noted to relate to male infertility. Infertility is not normally linked to sperm that are incompatible with the shape of the egg. 32. A couple with a diagnosis of ovarian failure discusses their infertility options with their physician. The nurse should recognize which of the following as the treatment of choice for a patient with ovarian failure? A) Intracytoplasmic sperm injection B) Artificial insemination C) Gamete intrafallopian transfer D) In vitro fertilization C Feedback: Gamete intrafallopian transfer (GIFT), a variation of IVF, is the treatment of choice for patients with ovarian failure. In intracytoplasmic sperm injection (ICSI), an ovum is retrieved as described previously, and a single sperm is injected through the zona pellucida, through the egg membrane, and into the cytoplasm of the oocyte. The fertilized egg is then transferred back to the donor. ICSI is the treatment of choice in severe male factor infertility. IVF involves ovarian stimulation, egg retrieval, fertilization, and embryo transfer. Artificial insemination is the deposit of semen into the female genital tract by artificial means. 33. The nurse is working with a couple who is being evaluated for infertility. What nursing intervention would be most appropriate for this couples likely needs? A) Educating them about parenting techniques in order to foster hope B) Educating them about the benefits of child-free living C) Choosing the most appropriate reproductive technology D) Referring them to appropriate community resources D Feedback: Nursing interventions appropriate when working with couples during infertility evaluations include referring the couple to appropriate resources when necessary. It would likely be considered offensive and insensitive to focus the couple on parenting skills or the benefits of child-free living. Choosing particular reproductive technologies is beyond the nurses scope of practice. 34. A woman presents at the ED with sharp, colicky pain in her right abdomen that radiates to her right shoulder. She tells the nurse that she has been spotting lightly for the past few days. The patient is subsequently diagnosed with an ectopic pregnancy. What major nursing diagnosis most likely relates to this patients needs? A) Anxiety related to potential treatment options and health outcomes B) Chronic sorrow related to spontaneous abortion C) Chronic pain related to genitourinary trauma D) Impaired tissue integrity related to keloid scarring A Feedback: It is highly likely that the woman diagnosed with an ectopic pregnancy will experience intense anxiety. Pain and sorrow are also plausible, but are unlikely to become chronic. Impaired tissue integrity and keloid scarring are atypical. 35. The nurse is assessing a patient who believes that she has recently begun menopause. What principle should inform the nurses interactions with this patient? A) The nurse should express empathy for the patients difficult health situation. B) The nurse should begin by assuring the patient that her health will be much better in a few years. C) The nurse must carefully assess the patients feelings and beliefs surrounding menopause. D) The nurse should encourage the patient to celebrate this life milestone and its accompanying benefits. C Feedback: Women have widely varying views on menopause and the nurse must ascertain these. It is wrong to presume either a positive or negative view of this transition without first performing assessment. 36. A 51-year-old woman is experiencing perimenopausal symptoms and expresses confusion around the possible use of hormone therapy (HT). She explains that her mother and aunts used HT and she is unsure why few of her peers have been prescribed this treatment. What should the nurse explain to the patient? A) Large, long-term health studies have revealed that HT is minimally effective. B) HT has been largely replaced by other nonpharmacologic interventions. C) Research has shown that significant health risks are associated with HT. D) HT has been shown to exacerbate symptoms of menopause in a minority of women. C Feedback: HT is effective, but has been associated with serious adverse effects. However, it does not exacerbate the symptoms of menopause. Nonpharmacologic interventions that address perimenopausal symptoms have not yet been identified. 37. A community health nurse is leading a health education session addressing menopause and other aspects of womens health. What dietary supplements should the nurse recommend to prevent morbidity associated with osteoporotic fractures? A) Vitamin B12 and vitamin C B) Vitamin A and potassium C) Vitamin B6 and phosphorus D) Calcium and vitamin D D Feedback: Calcium and vitamin D supplementation may be helpful in reducing bone loss and preventing the morbidity associated with osteoporotic fractures. Phosphorus, potassium, vitamin B12, vitamin C, and vitamin B6 do not address this risk. 38. The nurse is working with a patient who expects to begin menopause in the next few years. What educational topic should the nurse prioritize when caring for a healthy woman approaching menopause? A) Patient teaching and counseling regarding healthy lifestyles B) Referrals to local support groups C) Nutritional counseling regarding osteoporosis prevention D) Drug therapy options A Feedback: The individual womans evaluation of herself and her worth, now and in the future, is likely to affect her emotional reaction to menopause. Patient teaching and counseling regarding healthy lifestyles, health promotion, and health screening are of paramount importance. This broad goal of fostering healthy lifestyles transcends individual topics such as drug treatment, support groups, and osteoporosis prevention. 39. A womans current health complaints are suggestive of a diagnosis of premenstrual dysphoric disorder (PMDD). The nurse should first do which of the following? A) Assess the patients understanding of HT. B) Assess the patient for risk of suicide. C) Assure the patient that the problem is self-limiting. D) Suggest the use of St. Johns wort. B Feedback: If the patient has severe symptoms of PMS or PMDD, the nurse assesses her for suicidal, uncontrollable, and violent behavior. The problem can escalate and is not necessarily self-limiting. HT is not a relevant intervention and the nurse should not recommend herbal supplements without input from the primary care provider. 40. A 21-year-old woman has sought care because of heavy periods and has subsequently been diagnosed with menorrhagia. The nurse should recognize which of the following as the most likely cause of the patients health problem? A) Hormonal disturbances B) Cervical or uterine cancer C) Pelvic inflammatory disease D) A sexually transmitted infection (STI) A Feedback: Menorrhagia is prolonged or excessive bleeding at the time of the regular menstrual flow. In young women, the cause is usually related to endocrine disturbance; in later life, it usually results from inflammatory disturbances, tumors of the uterus, or hormonal imbalance. STIs, pelvic inflammatory disease, and cancer are less likely causes. Chapter 57: Management of Patients with Female Reproductive Disorders 1. While taking a health history on a 20-year-old female patient, the nurse ascertains that this patient is taking miconazole (Monistat). The nurse is justified in presuming that this patient has what medical condition? A) Bacterial vaginosis B) Human papillomavirus (HPV) C) Candidiasis D) Toxic shock syndrome (TSS) C Feedback: Candidiasis is a fungal or yeast infection caused by strains of Candida. Miconazole (Monistat) is an antifungal medication used in the treatment of candidiasis. This agent is inserted into the vagina with an applicator at bedtime and may be applied to the vulvar area for pruritus. HPV, bacterial vaginosis, and TSS are not treated by Monistat. 2. A patient with genital herpes is having an acute exacerbation. What medication would the nurse expect to be ordered to suppress the symptoms and shorten the course of the infection? A) Clotrimazole (Gyne-Lotrimin) B) Metronidazole (Flagyl) C) Podophyllin (Podofin) D) Acyclovir (Zovirax) D Feedback: Acyclovir (Zovirax) is an antiviral agent that can suppress the symptoms of genital herpes and shorten the course of the infection. It is effective at reducing the duration of lesions and preventing recurrences. Clotrimazole is used in the treatment of yeast infections. Metronidazole is the most effective treatment for trichomoniasis. Posophyllin is used to treat external genital warts. Acyclovir is used in the treatment of genital herpes. 3. A patient with trichomoniasis comes to the walk-in clinic. In developing a care plan for this patient the nurse would know to include what as an important aspect of treating this patient? A) Both partners will be treated with metronidazole (Flagyl). B) Constipation and menstrual difficulties may occur. C) The patient should perform Kegel exercises 30 to 80 times daily. D) Care will involve hormone therapy to control the pain. A Feedback: The most effective treatment for trichomoniasis is metronidazole (Flagyl). Both partners receive a one- time loading dose or a smaller dose three times a day for 1 week. In pelvic inflammatory disease, menstrual difficulties and constipation may occur. Kegel exercises are prescribed to help strengthen weakened muscles associated with cystocele and other structural deficits. Hormone therapy does not address the etiology of trichomoniasis. 4. A student nurse is doing clinical hours at an OB/GYN clinic. The student is helping to develop a plan of care for a patient with gonorrhea who has presented at the clinic. The student should include which of the following in the care plan for this patient? A) The patient may benefit from oral contraceptives. B) The patient must avoid use of tampons. C) The patient is susceptible to urinary incontinence. D) The patient should also be treated for chlamydia. D Feedback: Because of the high incidence of coinfection with chlamydia and gonorrhea, the patient should also be treated for chlamydia. Avoiding the use of tampons is part of the self-care management of a patient with possible toxic shock syndrome (TSS). The patient is not susceptible to incontinence and there is no indication for the use of oral contraceptives. 5. When teaching patients about the risk factors of cervical cancer, what would the nurse identify as the most important risk factor? A) Late childbearing B) Human papillomavirus (HPV) C) Postmenopausal bleeding D) Tobacco use B Feedback: HPV is the most salient risk factor for cervical cancer, exceeding the risks posed by smoking, late childbearing, and postmenopausal bleeding. 6. The nurse is providing preoperative education for a patient diagnosed with endometriosis. A hysterectomy has been scheduled. What education topic should the nurse be sure to include for this patient? A) Menstrual periods will continue to occur for several months, some of them heavy. B) Normal activity will be permitted within 48 hours following surgery. C) After a hysterectomy, hormone levels remain largely unaffected. D) The bladder must be emptied prior to surgery and a catheter may be placed during surgery. D Feedback: The intestinal tract and the bladder need to be empty before the patient is taken to the OR to prevent contamination and injury to the bladder or intestinal tract. The patient is informed that her periods are now over, but she may have a slightly bloody discharge for a few days. The patient is instructed to avoid straining, lifting, or driving until her surgeon permits her to resume these activities. The patients hormonal balance is upset, which usually occurs in reproductive system disturbances. The patient may experience depression and heightened emotional sensitivity to people and situations. 7. A patient has returned to the post-surgical unit after vulvar surgery. What intervention should the nurse prioritize during the initial postoperative period? A) Placing the patient in high Fowlers position B) Administering sitz baths every 4 hours C) Monitoring the integrity of the surgical site D) Avoiding analgesics unless the patients pain is unbearable C Feedback: An important intervention for the patient who has undergone vulvar surgery is to monitor closely for signs of infection in the surgical site, such as redness, purulent drainage, and fever. The patient should be placed in low Fowlers position to reduce pain by relieving tension on the incision. Sitz baths are discouraged after of wide excision of the vulva because of the risk of infection. Analgesics should be administered preventively on a scheduled basis to relieve pain and increase the patients comfort level. 8. A patient comes to the free clinic complaining of a gray-white discharge that clings to her external vulva and vaginal walls. A nurse practitioner assesses the patient and diagnoses Gardnerella vaginalis. What would be the most appropriate nursing action at this time? A) Advise the patient that this is an overgrowth of normal vaginal flora. B) Discuss the effect of this diagnosis on the patients fertility. C) Document the vaginal discharge as normal. D) Administer acyclovir as ordered. A Feedback: Gray-white discharge that clings to the external vulva and vaginal walls is indicative of an overgrowth of Gardnerella vaginalis. The patients discharge is not a normal assessment finding. Antiviral medications are ineffective because of the bacterial etiology. This diagnosis is unlikely to have a long- term bearing on the patients fertility. 9. A female patient with HIV has just been diagnosed with condylomata acuminata (genital warts). What information is most appropriate for the nurse to tell this patient? A) This condition puts her at a higher risk for cervical cancer; therefore, she should have a Papanicolaou (Pap) test annually. B) The most common treatment is metronidazole (Flagyl), which should eradicate the problem within 7 to 10 days. C) The potential for transmission to her sexual partner will be eliminated if condoms are used every time they have sexual intercourse. D) The human papillomavirus (HPV), which causes condylomata acuminata, cannot be transmitted during oral sex. A Feedback: HIV-positive women have a higher rate of HPV. Infections with HPV and HIV together increase the risk of malignant transformation and cervical cancer. Thus, women with HIV infection should have frequent Pap smears. Because condylomata acuminata is a virus, there is no permanent cure. Because condylomata acuminata can occur on the vulva, a condom will not protect sexual partners. HPV can be transmitted to other parts of the body, such as the mouth, oropharynx, and larynx. 10. The nurse is teaching a patient preventative measures regarding vaginal infections. The nurse should include which of the following as an important risk factor? A) High estrogen levels B) Late menarche C) Nonpregnant state D) Frequent douching D Feedback: Risk factors associated with vulvovaginal infections include pregnancy, premenarche, low estrogen levels, and frequent douching. 11. A nurse is caring for a pregnant patient with active herpes. The teaching plan for this patient should include which of the following? A) Babies delivered vaginally may become infected with the virus. B) Recommended treatment is excision of the herpes lesions. C) Pain generally does not occur with a herpes outbreak during pregnancy. D) Pregnancy may exacerbate the mothers symptoms, but poses no risk to the infant. A Feedback: In pregnant women with active herpes, babies delivered vaginally may become infected with the virus. There is a risk for fetal morbidity and mortality if this occurs. Lesions are not controlled with excision. Itching and pain accompany the process as the infected area becomes red and swollen. Aspirin and other analgesics are usually effective in controlling the pain. 12. A patient with ovarian cancer is admitted to the hospital for surgery and the nurse is completing the patients health history. What clinical manifestation would the nurse expect to assess? A) Fish-like vaginal odor B) Increased abdominal girth C) Fever and chills D) Lower abdominal pelvic pain B Feedback: Clinical manifestations of ovarian cancer include enlargement of the abdomen from an accumulation of fluid. Flatulence and feeling full after a light meal are significant symptoms. In bacterial vaginosis, a fish-like odor, which is noticeable after sexual intercourse or during menstruation, occurs as a result of a rise in the vaginal pH. Fever, chills, and abdominal pelvic pain are atypical. 13. A 30-year-old patient has come to the clinic for her yearly examination. The patient asks the nurse about ovarian cancer. What should the nurse state when describing risk factors for ovarian cancer? A) Use of oral contraceptives increases the risk of ovarian cancer. B) Most cases of ovarian cancer are attributed to tobacco use. C) Most cases of ovarian cancer are considered to be random, with no obvious causation. D) The majority of women who get ovarian cancer have a family history of the disease. C Feedback: Most cases of ovarian cancer are random, with only 5% to 10% of ovarian cancers having a familial connection. Contraceptives and tobacco have not been identified as major risk factors. 14. A student nurse is caring for a patient who has undergone a wide excision of the vulva. The student should know that what action is contraindicated in the immediate postoperative period? A) Placing patient in low Fowlers position B) Application of compression stockings C) Ambulation to a chair D) Provision of a low-residue diet C Feedback: Sitting in a chair would not be recommended immediately in the postoperative period. This would place too much tension on the incision site. A low Fowlers position or, occasionally, a pillow placed under the knees, will reduce pain by relieving tension on the incision. Application of compression stocking would prevent a deep vein thrombosis from occurring. A low-residue diet would be ordered to prevent straining on defecation and wound contamination. 15. A female patient tells the nurse that she thinks she has a vaginal infection because she has noted inflammation of her vulva and the presence of a frothy, yellow-green discharge. The nurse recognizes that the clinical manifestations described are typical of what vaginal infection? A) Trichomonas vaginalis B) Candidiasis C) Gardnerella D) Gonorrhea A Feedback: The clinical manifestations indicate T. vaginalis, which is treated with metronidazole in the form of oral tablets. Candidiasis produces a white, cheese-like discharge. Gardnerella is characterized by gray-white to yellow-white discharge clinging to external vulva and vaginal walls. Gonorrhea often produces no symptoms. 16. The nurse notes that a patient has a history of fibroids and is aware that this term refers to a benign tumor of the uterus. What is a more appropriate term for a fibroid? A) Bartholins cyst B) Dermoid cyst C) Hydatidiform mole D) Leiomyoma D Feedback: A leiomyoma is a usually benign tumor of the uterus, commonly referred to as a fibroid. A Bartholins cyst is a cyst in a paired vestibular band in the vulva, whereas a dermoid cyst is a benign tumor that is thought to arise from parts of the ovum and normally disappears with maturation. A hydatidiform mole is a type of gestational neoplasm. 17. A nurse practitioner is examining a patient who presented at the free clinic with vulvar pruritus. For which assessment finding would the practitioner look that may indicate the patient has an infection caused by Candida albicans? A) Cottage cheese-like discharge B) Yellow-green discharge C) Gray-white discharge D) Watery discharge with a fishy odor A Feedback: The symptoms of C. albicans include itching and a scant white discharge that has the consistency of cottage cheese. Yellow-green discharge is a sign of T. vaginalis. Gray-white discharge and a fishy odor are signs of G. vaginalis. 18. The nurse is planning health education for a patient who has experienced a vaginal infection. What guidelines should the nurse include in this program regarding prevention? A) Wear tight-fitting synthetic underwear. B) Use bubble bath to eradicate perineal bacteria. C) Avoid feminine hygiene products, such as sprays. D) Restrict daily bathing. C Feedback: Instead of tight-fitting synthetic, nonabsorbent, heat-retaining underwear, cotton underwear is recommended to prevent vaginal infections. Douching is generally discouraged, as is the use of feminine hygiene products. Daily bathing is not restricted. 19. A patient has herpes simplex 2 viral infection (HSV2). The nurse recognizes that which of the following should be included in teaching the patient? A) The virus causes cold sores of the lips. B) The virus may be cured with antibiotics. C) The virus, when active, may not be contracted during intercourse. D) Treatment is aimed at relieving symptoms. D Feedback: HSV-2 causes genital herpes and is known to ascend the peripheral sensory nerves and remain inactive after infection, becoming active in times of stress. The virus is not curable, but treatment is aimed at controlling symptoms. HSV1 causes cold sores, and varicella zoster causes shingles. 20. You are caring for a patient who has been diagnosed with genital herpes. When preparing a teaching plan for this patient, what general guidelines should be taught? A) Thorough handwashing is essential. B) Sun bathing assists in eradicating the virus. C) Lesions should be massaged with ointment. D) Self-infection cannot occur from touching lesions during a breakout. A Feedback: The risk of reinfection and spread of infection to others or to other structures of the body can be reduced by handwashing, use of barrier methods with sexual contact, and adherence to prescribed medication regimens. The lesions should be allowed to dry. Touching of lesions during an outbreak should be avoided; if touched, appropriate hygiene practices must be followed. 21. A patient comes to the clinic complaining of a tender, inflamed vulva. Testing does not reveal the presence of any known causative microorganism. What aspect of this patients current health status may account for the patients symptoms of vulvitis? A) The patient is morbidly obese. B) The patient has type 1 diabetes. C) The patient has chronic kidney disease. D) The patient has numerous allergies. B Feedback: Vulvitis, an inflammation of the vulva, may occur as a result of other disorders, such as diabetes, dermatologic problems, or poor hygiene. Obesity, kidney disease, and allergies are less likely causes than diabetes. 22. A 14-year-old is brought to the clinic by her mother. The mother explains to the nurse that her daughter has just started using tampons, but is not yet sexually active. The mother states I am very concerned because my daughter is having a lot of stabbing pain and burning. What might the nurse suspect is the problem with the 14-year-old? A) Vulvitis B) Vulvodynia C) Vaginitis D) Bartholins cyst B Feedback: Vulvodynia is a chronic vulvar pain syndrome. Symptoms may include burning, stinging, irritation, or stabbing pain and may follow the initial use of tampons or first sexual experience. Vulvitis is an inflammation of the vulva that is normally infectious. Bartholins cyst results from the obstruction of a duct in one of the paired vestibular glands located in the posterior third of the vulva, near the vestibule. 23. A patient has been diagnosed with polycystic ovary syndrome (PCOS). The nurse should encourage what health promotion activity to address the patients hormone imbalance and infertility? A) Kegel exercises B) Increased fluid intake C) Weight loss D) Topical antibiotics as ordered C Feedback: Lifestyle modification is critical in the treatment of PCOS, and weight management is part of the treatment plan. As little as a weight loss of 5% of total body weight can help with hormone imbalance and infertility. Antibiotics are irrelevant, as PCOS does not have an infectious etiology. Fluid intake and Kegel exercises do not influence the course of the disease. 24. A patient has been diagnosed with endometriosis. When planning this patients care, the nurse should prioritize what nursing diagnosis? A) Anxiety related to risk of transmission B) Acute pain related to misplaced endometrial tissue C) Ineffective tissue perfusion related to hemorrhage D) Excess fluid volume related to abdominal distention B Feedback: Symptoms of endometriosis vary but include dysmenorrhea, dyspareunia, and pelvic discomfort or pain. Dyschezia (pain with bowel movements) and radiation of pain to the back or leg may occur. Ineffective tissue perfusion is not associated with endometriosis and there is no plausible risk of fluid overload. Endometriosis is not transmittable. 25. When reviewing the electronic health record of a female patient, the nurse reads that the patient has a history of adenomyosis. The nurse should be aware that this patient experiences symptoms resulting from what pathophysiologic process? A) Loss of muscle tone in the vaginal wall B) Excessive synthesis and release of unopposed estrogen C) Invasion of the uterine wall by endometrial tissue D) Proliferation of tumors in the uterine wall C Feedback: In adenomyosis, the tissue that lines the endometrium invades the uterine wall. This disease is not characterized by loss of muscle tone, the presence of tumors, or excessive estrogen. 26. Following a recent history of dyspareunia and lower abdominal pain, a patient has received a diagnosis of pelvic inflammatory disease (PID). When providing health education related to self-care, the nurse should address which of the following topics? Select all that apply. A) Use of condoms to prevent infecting others B) Appropriate use of antibiotics C) Taking measures to prevent pregnancy D) The need for a Pap smear every 3 months E) The importance of weight loss in preventing symptoms A, B Feedback: Patients with PID need to take action to avoid infecting others. Antibiotics are frequently required. Pregnancy does not necessarily need to be avoided, but there is a heightened risk of ectopic pregnancy. Weight loss does not directly alleviate symptoms. Regular follow-up is necessary, but Pap smears do not need to be performed every 3 months. 27. A middle-aged female patient has been offered testing for HIV/AIDS upon admission to the hospital for an unrelated health problem. The nurse observes that the patient is visibly surprised and embarrassed by this offer. How should the nurse best respond? A) Most women with HIV dont know they have the disease. If you have it, its important we catch it early. B) This testing is offered to every adolescent and adult regardless of their lifestyle, appearance or history. C) The rationale for this testing is so that you can begin treatment as soon as testing comes back, if its positive. D) Youre being offered this testing because you are actually in the prime demographic for HIV infection. B Feedback: Because patients may be reluctant to discuss risk-taking behavior, routine screening should be offered to all women between the ages of 13 to 64 years in all health care settings. Assuring a woman that the offer of testing is not related to a heightened risk may alleviate her anxiety. Middle-aged women are not the prime demographic for HIV infection. The nurse should avoid causing fear by immediately discussing treatment or the fact that many patients are unaware of their diagnosis. 28. A patient with a genital herpes exacerbation has a nursing diagnosis of acute pain related to the genital lesions. What nursing intervention best addresses this diagnosis? A) Cover the lesions with a topical antibiotic. B) Keep the lesions clean and dry. C) Apply a topical NSAID to the lesions. D) Remain on bed rest until the lesions resolve. B Feedback: To reduce pain, the lesions should be kept clean and proper hygiene practices maintained. Topical ointments are avoided and antibiotics are irrelevant due to the viral etiology. Activity should be maintained as tolerated. 29. The nurse is caring for a patient who has just been told that her ovarian cancer is terminal and that no curative options remain. What would be the priority nursing care for this patient at this time? A) Provide emotional support to the patient and her family. B) Implement distraction and relaxation techniques. C) Offer to inform the patients family of this diagnosis. D) Teach the patient about the importance of maintaining a positive attitude. A Feedback: Emotional support is an integral part of nursing care at this point in the disease progression. It is not normally appropriate for the nurse to inform the family of the patients diagnosis. It may be inappropriate and simplistic to focus on distraction, relaxation, and positive thinking. 30. A public health nurse is participating in a campaign aimed at preventing cervical cancer. What strategies should the nurse include is this campaign? Select all that apply. A) Promotion of HPV immunization B) Encouraging young women to delay first intercourse C) Smoking cessation D) Vitamin D and calcium supplementation E) Using safer sex practices A, B, C, E Feedback: Preventive measures relevant to cervical cancer include regular pelvic examinations and Pap tests for all women, especially older women past childbearing age. Preventive counseling should encourage delaying first intercourse, avoiding HPV infection, participating in safer sex only, smoking cessation, and receiving HPV immunization. Calcium and vitamin D supplementation are not relevant. 31. A patient is being discharged home after a hysterectomy. When providing discharge education for this patient, the nurse has cautioned the patient against sitting for long periods. This advice addresses the patients risk of what surgical complication? A) Pudendal nerve damage B) Fatigue C) Venous thromboembolism D) Hemorrhage C Feedback: The patient should resume activities gradually. This does not mean sitting for long periods, because doing so may cause blood to pool in the pelvis, increasing the risk of thromboembolism. Sitting for long periods after a hysterectomy does not cause postoperative nerve damage; it does not increase the fatigue factor after surgery or the risk of hemorrhage. 32. A 27-year-old female patient is diagnosed with invasive cervical cancer and is told she needs to have a hysterectomy. One of the nursing diagnoses for this patient is disturbed body image related to perception of femininity. What intervention would be most appropriate for this patient? A) Reassure the patient that she will still be able to have children. B) Reassure the patient that she does not have to have sex to be feminine. C) Reassure the patient that you know how she is feeling and that you feel her anxiety and pain. D) Reassure the patient that she will still be able to have intercourse with sexual satisfaction and orgasm. D Feedback: The patient needs reassurance that she will still have a vagina and that she can experience sexual intercourse after temporary postoperative abstinence while tissues heal. Information that sexual satisfaction and orgasm arise from clitoral stimulation rather than from the uterus reassures many women. Most women note some change in sexual feelings after hysterectomy, but they vary in intensity. In some cases, the vagina is shortened by surgery, and this may affect sensitivity or comfort. It would be inappropriate to reassure the patient that she will still be able to have children; there is no reason to reassure the patient about not being able to have sex. There is no way you can know how the patient is feeling and it would be inappropriate to say so. 33. A patient is post-operative day 1 following a vaginal hysterectomy. The nurse notes an increase in the patients abdominal girth and the patient complains of bloating. What is the nurses most appropriate action? A) Provide the patient with an unsweetened, carbonated beverage. B) Apply warm compresses to the patients lower abdomen. C) Provide an ice pack to apply to the perineum and suprapubic region. D) Assist the patient into a prone position. B Feedback: If the patient has abdominal distention or flatus, a rectal tube and application of heat to the abdomen may be prescribed. Ice and carbonated beverages are not recommended and prone positioning would be uncomfortable. 34. A 31-year-old patient has returned to the post-surgical unit following a hysterectomy. The patients care plan addresses the risk of hemorrhage. How should the nurse best monitor the patients postoperative blood loss? A) Have the patient void and have bowel movements using a commode rather than toilet. B) Count and inspect each perineal pad that the patient uses. C) Swab the patients perineum for the presence of blood at least once per shift. D) Leave the patients perineum open to air to facilitate inspection. B Feedback: To detect bleeding, the nurse counts the perineal pads used or checks the incision site, assesses the extent of saturation with blood, and monitors vital signs. The perineum is not swabbed and there is no reason to prohibit the use of the toilet. Absorbent pads are applied to the perineum; it is not open to air. 35. A patient diagnosed with cervical cancer will soon begin a round of radiation therapy. When planning the patients subsequent care, the nurse should prioritize actions with what goal? A) Preventing hemorrhage B) Ensuring the patient knows the treatment is palliative, not curative C) Protecting the safety of the patient, family, and staff D) Ensuring that the patient adheres to dietary restrictions during treatment C Feedback: Care must be taken to protect the safety of patients, family members, and staff during radiation therapy. Hemorrhage is not a common complication of radiation therapy and the treatment can be curative. Dietary restrictions are not normally necessary during treatment. 36. The nurse is caring for a 63-year-old patient with ovarian cancer. The patient is to receive chemotherapy consisting of Taxol and Paraplatin. For what adverse effect of this treatment should the nurse monitor the patient? A) Leukopenia B) Metabolic acidosis C) Hyperphosphatemia D) Respiratory alkalosis A Feedback: Chemotherapy is usually administered IV on an outpatient basis using a combination of platinum and taxane agents. Paclitaxel (Taxol) plus carboplatin (Paraplatin) are most often used because of their excellent clinical benefits and manageable toxicity. Leukopenia, neurotoxicity, and fever may occur. Acidbase imbalances and elevated phosphate levels are not anticipated. 37. The nurse is caring for a patient with a diagnosis of vulvar cancer who has returned from the PACU after undergoing a wide excision of the vulva. How should this patients analgesic regimen be best managed? A) Analgesia should be withheld unless the patients pain becomes unbearable. B) Scheduled analgesia should be administered around-the-clock to prevent pain. C) All analgesics should be given on a PRN, rather than scheduled, basis. D) Opioid analgesics should be avoided and NSAIDs exclusively provided. B Feedback: Because of the wide excision, the patient may experience severe pain and discomfort even with minimal movement. Therefore, analgesic agents are administered preventively (i.e., around the clock at designated times) to relieve pain, increase the patients comfort level, and allow mobility. Opioids are usually required. 38. A 45-year-old woman has just undergone a radical hysterectomy for invasive cervical cancer. Prior to the surgery the physician explained to the patient that after the surgery a source of radiation would be placed near the tumor site to aid in reducing recurrence. What is the placement of the source of radiation called? A) Internal beam radiation B) Trachelectomy C) Brachytherapy D) External radiation C Feedback: Radiation, which is often part of the treatment to reduce recurrent disease, may be delivered by an external beam or by brachytherapy (method by which the radiation source is placed near the tumor) or both. 39. A 25-year-old patient diagnosed with invasive cervical cancer expresses a desire to have children. What procedure might the physician offer as treatment? A) Radical hysterectomy B) Radical culposcopy C) Radical trabeculectomy D) Radical trachelectomy D Feedback: A procedure called a radical trachelectomy is an alternative to hysterectomy in women with invasive cervical cancer who are young and want to have children. In this procedure, the cervix is gripped with retractors and pulled down into the vagina until it is visible. The affected tissue is excised while the rest of the cervix and uterus remain intact. A drawstring suture is used to close the cervix. For a woman who wants to have children, a radical hysterectomy would not provide the option of children. A radical culposcopy and a radical trabeculectomy are simple distracters for this question. 40. A nurse providing prenatal care to a pregnant woman is addressing measures to reduce her postpartum risk of cystocele, rectocele, and uterine prolapse. What action should the nurse recommend? A) Maintenance of good perineal hygiene B) Prevention of constipation C) Increased fluid intake for 2 weeks postpartum D) Performance of pelvic muscle exercises D Feedback: Some disorders related to relaxed pelvic muscles (cystocele, rectocele, and uterine prolapse) may be prevented. During pregnancy, early visits to the primary provider permit early detection of problems. During the postpartum period, the woman can be taught to perform pelvic muscle exercises, commonly known as Kegel exercises, to increase muscle mass and strengthen the muscles that support the uterus and then to continue them as a preventive action. Fluid intake, prevention of constipation, and hygiene do not reduce this risk. Chapter 58: Assessment and Management of Patients with Breast Disorders 1. A 45-year-old woman comes into the health clinic for her annual check-up. She mentions to the nurse that she has noticed dimpling of the right breast that has occurred in a few months. What assessment would be most appropriate for the nurse to make? A) Evaluate the patients milk production. B) Palpate the area for a breast mass. C) Assess the patients knowledge of breast cancer. D) Assure the patient that this likely an age-related change. B Feedback: It would be most important for the nurse to palpate the breast to determine the presence of a mass and to refer the patient to her primary care provider. Edema and pitting of the skin may result from a neoplasm blocking lymphatic drainage, giving the skin an orange-peel appearance (peau dorange), a classic sign of advanced breast cancer. Evaluation of milk production is required in lactating women. There is no indication of lactation in the scenario. The patients knowledge of breast cancer is relevant, but is not a time-dependent priority. This finding is not an age-related change. 2. The nurse leading an educational session is describing self-examination of the breast. The nurse tells the womens group to raise their arms and inspect their breasts in a mirror. A member of the womens group asks the nurse why raising her arms is necessary. What is the nurses best response? A) It helps to spread out the fat that makes up your breast. B) It allows you to simultaneously assess for pain. C) It will help to observe for dimpling more closely. D) This is what the American Cancer Society recommends. C Feedback: The primary reason for raising the arms is to detect any dimpling. To elicit skin dimpling or retraction that may otherwise go undetected, the examiner instructs the patient to raise both arms overhead. Citing American Cancer Society recommendations does not address the womans question. The purpose of raising the arms is not to elicit pain or to redistribute adipose tissue. 3. A woman aged 48 years comes to the clinic because she has discovered a lump in her breast. After diagnostic testing, the woman receives a diagnosis of breast cancer. The woman asks the nurse when her teenage daughters should begin mammography. What is the nurses best advice? A) Age 28 B) Age 35 C) Age 38 D) Age 48 C Feedback: A general guideline is to begin screening 5 to 10 years earlier than the age at which the youngest family member developed breast cancer, but not before age 25 years. In families with a history of breast cancer, a downward shift in age of diagnosis of about 10 years is seen. Because their mother developed breast cancer at age 48 years, the daughters should begin mammography at age 38 to 43 years. 4. A woman scheduled for a simple mastectomy in one week is having her preoperative education provided by the clinic nurse. What educational intervention will be of primary importance to prevent hemorrhage in the postoperative period? A) Limit her intake of green leafy vegetables. B) Increase her water intake to 8 glasses per day. C) Stop taking aspirin. D) Have nothing by mouth for 6 hours before surgery. C Feedback: The nurse should instruct the patient to stop taking aspirin due to its anticoagulant effect. Limiting green leafy vegetables will decrease vitamin K and marginally increase bleeding. Increasing fluid intake or being NPO before surgery will have no effect on bleeding. 5. The nurse is caring for a 52-year-old woman whose aunt and mother died of breast cancer. The patient states, My doctor and I talked about Tamoxifen to help prevent breast cancer. Do you think it will work? What would be the nurses best response? A) Yes, its known to have a slight protective effect. B) Yes, but studies also show an increased risk of osteoporosis. C) You wont need to worry about getting cancer as long as you take Tamoxifen. D) Tamoxifen is known to be a highly effective protective measure. D Feedback: Tamoxifen has been shown to be a highly effective chemopreventive agent. However, it cannot reduce the risk of cancer by 100%. It also acts to prevent osteoporosis. 6. A woman is being treated for a tumor of the left breast. If the patient and her physician opt for prophylactic treatment, the nurse should prepare the woman for what intervention? A) More aggressive chemotherapy B) Left mastectomy C) Radiation therapy D) Bilateral mastectomy D Feedback: Right mastectomy would be considered a prophylactic measure to reduce the risk of cancer in the patients unaffected breast. None of the other listed interventions would be categorized as being prophylactic rather than curative. 7. During a recent visit to the clinic a woman presents with erythema of the nipple and areola on the right breast. She states this started several weeks ago and she was fearful of what would be found. The nurse should promptly refer the patient to her primary care provider because the patients signs and symptoms are suggestive of what health problem? A) Peau dorange B) Nipple inversion C) Pagets disease D) Acute mastitis C Feedback: Pagets disease presents with erythema of the nipple and areola. Peau dorange, which is associated with breast cancer, is caused by interference with lymphatic drainage, but does not cause these specific signs. Nipple inversion is considered normal if long-standing; if it is associated with fibrosis and is a recent development, malignancy is suspected. Acute mastitis is associated with lactation, but it may occur at any age. 8. A patient who came to the clinic after finding a mass in her breast is scheduled for a diagnostic breast biopsy. During the nurses admission assessment, the nurse observes that the patient is distracted and tense. What is it important for the nurse to do? A) Acknowledge the fear the patient is likely experiencing. B) Describe the support groups that exist in the community. C) Assess the patients stress management skills. D) Document a nursing diagnosis of ineffective coping. A Feedback: In the breast cancer diagnostic phase it is appropriate to acknowledge the patients feelings of fear, concern, and apprehension. This must precede interventions such as referrals, if appropriate. Assessment of stress management skills made be necessary, but the nurse should begin by acknowledging the patients feelings. Fear is not necessarily indicative of ineffective coping. 9. A patient has been referred to the breast clinic after her most recent mammogram revealed the presence of a lump. The lump is found to be a small, well-defined nodule in the right breast. The oncology nurse should recognize the likelihood of what treatment? A) Lumpectomy and radiation B) Partial mastectomy and radiation C) Partial mastectomy and chemotherapy D) Total mastectomy and chemotherapy A Feedback: Treatment for breast cancer depends on the disease stage and type, the patients age and menopausal status, and the disfiguring effects of the surgery. For this patient, lumpectomy is the most likely option because the nodule is well-defined. The patient usually undergoes radiation therapy afterward. Because a lumpectomy is possible, mastectomy would not be the treatment of choice. 10. A 23-year-old woman comes to the free clinic stating I think I have a lump in my breast. Do I have cancer? The nurse instructs the patient that a diagnosis of breast cancer is confirmed by what? A) Supervised breast self-examination B) Mammography C) Fine-needle aspiration D) Chest x-ray C Feedback: Fine-needle aspiration and biopsy provide cells for histologic examination to confirm a diagnosis, although falsenegative and falsepositive findings are possibilities. A breast self-examination, if done regularly, is the most reliable method for detecting breast lumps early, but is not diagnostic of cancer. Mammography is used to detect tumors that are too small to palpate. Chest x-rays can be used to pinpoint rib metastasis. Neither test is considered diagnostic of breast cancer, however. 11. A 42 year-old patient tells the nurse that she has found a painless lump in her right breast during her monthly self-examination. She says that she is afraid that she has cancer. Which assessment finding would most strongly suggest that this patients lump is cancerous? A) Eversion of the right nipple and mobile mass B) A nonmobile mass with irregular edges C) A mobile mass that is soft and easily delineated D) Nonpalpable right axillary lymph nodes B Feedback: Breast cancer tumors are typically fixed, hard, and poorly delineated with irregular edges. A mobile mass that is soft and easily delineated is most commonly a fluid-filled benign cyst. Axillary lymph nodes may or may not be palpable on initial detection of a cancerous mass. Nipple retraction, not eversion, may be a sign of cancer. 12. A patient in her 30s has two young children and has just had a modified radical mastectomy with immediate reconstruction. The patient shares with the nurse that she is somewhat worried about her future, but she appears to be adjusting well to her diagnosis and surgery. What nursing intervention is most appropriate to support this patients coping? A) Encourage the patients spouse or partner to be supportive while she recovers. B) Encourage the patient to proceed with the next phase of treatment. C) Recommend that the patient remain optimistic for the sake of her children. D) Arrange a referral to a community-based support program. D Feedback: The patient is not exhibiting clear signs of anxiety or depression. Therefore, the nurse can probably safely approach her about talking with others who have had similar experiences. The nurse may educate the patients spouse or partner to listen for concerns, but the nurse should not tell the patients spouse what to do. The patient must consult with her physician and make her own decisions about further treatment. The patient needs to express her sadness, frustration, and fear. She cannot be expected to be optimistic at all times. 13. The nurse is caring for a patient who has just had a radical mastectomy and axillary node dissection. When providing patient education regarding rehabilitation, what should the nurse recommend? A) Avoid exercise of the arm for next 2 months. B) Keep cuticles clipped neatly. C) Avoid lifting objects heavier than 10 pounds. D) Use a sling until healing is complete. C Feedback: Following an axillary dissection, the patient should avoid lifting objects greater than 5 to 10 pounds, cutting the cuticles, and undergoing venipuncture on the affected side. Exercises of the hand and arm are encouraged and the use of a sling is not necessary. 14. A new mother who is breastfeeding calls the clinic to speak to a nurse. The patient is complaining of pain in her left breast and describes her breast as feeling doughy. The nurse tells her to come into the clinic and be checked. The patient is diagnosed with acute mastitis and placed on antibiotics. What comfort measure should the nurse recommend? A) Apply cold compresses as ordered. B) Avoid wearing a bra until the infection clears. C) Avoid washing the breasts. D) Perform gentle massage to stimulate neutrophil migration. A Feedback: Treatment of mastitis consists of antibiotics and local application of cold compresses to relieve discomfort. A broad-spectrum antibiotic agent may be prescribed for 7 to 10 days. The patient should wear a snug bra and perform personal hygiene carefully. Massage is not recommended. 15. When planning discharge teaching with a patient who has undergone a total mastectomy with axillary dissection, the nurse knows to instruct the patient that she should report what sign or symptom to the physician immediately? A) Fatigue B) Temperature greater than 98.5F C) Sudden cessation of output from the drainage device D) Gradual decline in output from the drain C Feedback: The patient should report sudden cessation of output from the drainage device, which could indicate an occlusion. Gradual decline in output is expected. A temperature of 100.4F or greater should also be reported to rule out postoperative infection, but a temperature of 98.5F is not problematic. Fatigue is expected during the recovery period. 16. A patient newly diagnosed with breast cancer states that her physician suspects regional lymph node involvement and told her that there are signs of metastatic disease. The nurse learns that the patient has been diagnosed with stage IV breast cancer. What is an implication of this diagnosis? A) The patient is not a surgical candidate. B) The patients breast cancer is considered highly treatable. C) There is a 10% chance that the patients cancer will self-resolve. D) The patient has a 15% chance of 5-year survival. D Feedback: The 5-year survival rate is approximately 15% for stage IV breast cancer. Surgery is still a likely treatment, but the disease would not be considered to be highly treatable. Self-resolution of the disease is not a possibility. 17. The nurse is performing a comprehensive health history of a patient who is in her 50s. The nurse should identify what risk factor that may increase this patients risk for breast cancer? A) The patient breastfed each of her children. B) The patient gave birth to her first child at age 38. C) The patient experienced perimenopausal symptoms starting at age 46. D) The patient experienced menarche at age 13. B Feedback: Late age at first pregnancy is a risk factor for breast cancer. None of the other listed aspects of the patients health history is considered to be a risk factor for breast cancer. 18. A nurse is examining a patient who has been diagnosed with a fibroadenoma. The nurse should recognize what implication of this patients diagnosis? A) The patient will be scheduled for radiation therapy. B) The patient might be referred for a biopsy. C) The patients breast mass is considered an age-related change. D) The patients diagnosis is likely related to her use of oral contraceptives. B Feedback: Fibroadenomas are firm, round, movable, benign tumors. These masses are nontender and are sometimes removed for biopsy and definitive diagnosis. They are not considered to be an age-related change, even though they are benign. Radiation therapy is unnecessary and fibroadenomas do not result from oral contraceptive use. 19. The nurse is reviewing the physicians notes from the patient who has just left the clinic. The nurse learns that the physician suspects a malignant breast tumor. On palpation, the mass most likely had what characteristic? A) Nontenderness B) A size of 5 mm C) Softness and a regular shape D) Mobility A Feedback: Generally, the lesions are nontender, fixed rather than mobile, and hard with irregular borders. Small size is not suggestive of malignancy. 20. A patient has presented for her annual mammogram. The patient voices concerns related to exposure to radiation. What should the nurse teach the patient about a mammogram? A) It does not use radiation. B) Radiation levels are safe as long as mammograms are performed only once per year. C) The negative effects of radiation do not accumulate until late in life. D) Radiation from a mammogram is equivalent to an hour of sunlight. D Feedback: The radiation exposure of mammogram is equivalent to about 1 hour of exposure to sunlight. Consequently, the benefits of mammography far outweigh any risks associated with the procedure. Negative consequences are insignificant, and do not accumulate later in life. 21. For which of the following population groups would an annual clinical breast examination be recommended? A) Women over age 21 B) Women over age 25 C) Women over age 40 D) All post-pubescent females with a family history of breast cancer C Feedback: Annual clinical breast examination is recommended for women aged 40 years and older. Younger women may have examinations less frequently. 22. A 42-year-old man has come to the clinic for an annual physical. The nurse notes in the patients history that his father was treated for breast cancer. What should the nurse provide to the patient before he leaves the clinic? A) A referral for a mammogram B) Instructions about breast self-examination (BSE) C) A referral to a surgeon D) A referral to a support group B Feedback: Instructions about BSE should be provided to men if they have a family history of breast cancer, because they may have an increased risk of male breast cancer. It is not within the scope of the practice of a nurse to refer a patient for a mammogram or to a surgeon; these actions are not necessary or recommended. In the absence of symptoms or a diagnosis, referral to a support group is unnecessary. 23. The nurse is teaching breast self-examination (BSE) to a group of women. The nurse should recommend that the women perform BSE at what time? A) At the time of menses B) At any convenient time, regardless of cycles C) Weekly D) Between days 5 and 7 after menses D Feedback: BSE is best performed after menses, on day 5 to day 7, counting the first day of menses as day 1. Monthly performance is recommended. 24. A nurse is teaching a group of women about the potential benefits of breast self-examination (BSE). The nurse should teach the women that effective BSE is dependent on what factor? A) Womens knowledge of how their breasts normally look and feel B) The rapport that exists between the woman and her primary care provider C) Synchronizing womens routines around BSE with the performance of mammograms D) Womens knowledge of the pathophysiology of breast cancer A Feedback: Current practice emphasizes the importance of breast self-awareness, which is a womans attentiveness to the normal appearance and feel of her breasts. BSE does not need to be synchronized with the performance of mammograms. Rapport between the patient and the care provider is beneficial, but does not necessarily determine the effectiveness of BSE. The woman does not need to understand the pathophysiology of breast cancer to perform BSE effectively. 25. A 60-year-old man presents at the clinic complaining that his breasts are tender and enlarging. The patient is subsequently diagnosed with gynecomastia. The patient should be assessed for the possibility of what causative factor? A) Age-related physiologic changes B) Medication adverse effects C) Poor nutrition D) Fluid overload B Feedback: Gynecomastia can also occur in older men and usually presents as a firm, tender mass underneath the areola. In these patients, gynecomastia may be diffuse and related to the use of certain medications. It is unrelated to fluid overload or nutrition and is not considered an age-related change. 26. A woman is considering breast reduction mammoplasty. When weighing the potential risks and benefits of this surgical procedure, the nurse should confirm that the patient is aware of what potential consequence? A) Chronic breast pain B) Unclear mammography results C) Increased risk of breast cancer D) Decreased nipple sensation D Feedback: During the preoperative consultation, the patient should be informed of a possibility that sensory changes of the nipple (e.g., numbness) may occur. There is no consequent increase in breast cancer risk and it does not affect future mammography results. Chronic pain is not an expected complication. 27. A patient is to undergo an ultrasound-guided core biopsy. The patient tells the nurse that a friend of hers had a stereotactic core biopsy. She wants to understand the differences between the two procedures. What would be the nurses best response? A) An ultrasound-guided core biopsy is faster, less expensive, and does not use radiation. B) An ultrasound-guided core biopsy is a little more expensive, but it doesnt use radiation and it is faster. C) An ultrasound-guided core biopsy is a little more expensive, and it also uses radiation but it is faster. D) An ultrasound-guided core biopsy takes more time, and it also uses radiation, but it is less expensive. A Feedback: Ultrasound-guided core biopsy does not use radiation and is also faster and less expensive than stereotactic core biopsy. 28. A patient at high risk for breast cancer is scheduled for an incisional biopsy in the outpatient surgery department. When the nurse is providing preoperative education, the patient asks why an incisional biopsy is being done instead of just removing the mass. What would be the nurses best response? A) An incisional biopsy is performed because its known to be less painful and more accurate than other forms of testing. B) An incisional biopsy is performed to confirm a diagnosis and so that special studies can be done that will help determine the best treatment. C) An incisional biopsy is performed to assess the potential for recovery from a mastectomy. D) An incisional biopsy is performed on patients who are younger than the age of 40 and who are otherwise healthy. B Feedback: Incisional biopsy surgically removes a portion of a mass. This is performed to confirm a diagnosis and to conduct special studies that will aid in determining treatment. Incisional biopsies cannot always remove the whole mass, nor is it always beneficial to the patient to do so. The procedure is not chosen because of the potential for pain, the possibility of recovery from mastectomy, or the patients age. 29. A patient is being discharged home from the ambulatory surgery center after an incisional biopsy of a mass in her left breast. What are the criteria for discharging this patient home? Select all that apply. A) Patient must understand when she can begin ambulating B) Patient must have someone to accompany her home C) Patient must understand activity restrictions D) Patient must understand care of the biopsy site E) Patient must understand when she can safely remove her urinary catheter B, C, D Feedback: Prior to discharge from the ambulatory surgical center or the office, the patient must be able to tolerate fluids, ambulate, and void. The patient must have somebody to accompany her home and would not be discharged with urinary catheter in place. 30. A patient has just been told she needs to have an incisional biopsy of a right breast mass. During preoperative teaching, how could the nurse best assess this patient for specific educational, physical, or psychosocial needs she might have? A) By encouraging her to verbalize her questions and concerns B) By discussing the possible findings of the biopsy C) By discussing possible treatment options if the diagnosis is cancer D) By reviewing her medical history A Feedback: During the preoperative visit, the nurse assesses the patient for any specific educational, physical, or psychosocial needs that she may have. This can be accomplished by encouraging her to verbalize her fears, concerns, and questions. Reviewing her medical history may be beneficial, but it is not the best way to ascertain her needs. Discussing possible findings of the biopsy and possible treatment options is the responsibility of the treating physician. 31. A patient has just returned to the postsurgical unit from post-anesthetic recovery after breast surgery for removal of a malignancy. What is the most likely major nursing diagnosis to include in this patients immediate plan of care? A) Acute pain related to tissue manipulation and incision B) Ineffective coping related to surgery C) Risk for trauma related to post-surgical injury D) Chronic sorrow related to change in body image A Feedback: Although many patients experience minimal pain, it is still important to assess for this postsurgical complication. Sorrow and ineffective coping are possible, but neither is likely to be evident in the immediate postoperative period. There is minimal risk of trauma. 32. A 52-year-old woman has just been told she has breast cancer and is scheduled for a modified mastectomy the following week. The nurse caring for this patient knows that she is anxious and fearful about the upcoming procedure and the newly diagnosed malignancy. How can the nurse most likely alleviate this patients fears? A) Provide written material on the procedure that has been scheduled for the patient. B) Provide the patient with relevant information about expected recovery. C) Give the patient current information on breast cancer survival rates. D) Offer the patient alternative treatment options. B Feedback: Providing the patient with realistic expectations about the healing process and expected recovery can help alleviate fears. Offering the patient alternative treatment options is not within the nurses normal scope of practice. Addressing survival rates may or may not be beneficial for the patient. Written material is rarely sufficient to meet patients needs. 33. A nurse is explaining that each breast contains 12 to 20 cone-shaped lobes. The nurse should explain that each lobe consists of what elements? A) Modified tendons and ligaments B) Connective tissue and smooth muscle C) Lobules and ducts D) Endocrine glands and sebaceous glands C Feedback: Each breast contains 12 to 20 cone-shaped lobes, which are made up of glandular elements (lobules and ducts) and separated by fat and fibrous tissue that binds the lobes together. These breast lobes do not consist of tendons, ligaments, endocrine glands, or smooth muscle. 34. A nurse has assessed that a patient is not yet willing to view her mastectomy site. How should the nurse best assist the patient is developing a positive body image? A) Ask the woman to describe the current appearance of her breast. B) Help the patient to understand that many women have gone through the same unpleasant experience. C) Explain to the patient that her body image does not have to depend on her physical appearance. D) Provide the patient with encouragement in an empathic and thoughtful manner. D Feedback: Gentle encouragement can help the patient progress toward accepting the change in her appearance. The nurse should not downplay the significance of physical appearance. Explaining that others have had similar experiences may or may not benefit the patient. Asking the patient to describe the appearance of her breast is likely to exacerbate the womans reluctance to do so. 35. A patient has had a total mastectomy with immediate reconstruction. The patient asks the nurse when she can take a shower. What should the nurse respond? A) Not until the drain is removed B) On the second postoperative day C) Now, if you wash gently with soap and water D) Seven days after your surgery A Feedback: If immediate reconstruction has been performed, showering may be contraindicated until the drain is removed. 36. A patient has been discharged home after a total mastectomy without reconstruction. The patient lives alone and has a home health referral. When the home care nurse performs the first scheduled visit this patient, what should the nurse assess? Select all that apply. A) Adherence to the exercise plan B) Overall psychological functioning C) Integrity of surgical drains D) Understanding of cancer E) Use of the breast prosthesis A, B, C Feedback: Patients who have difficulty managing their postoperative care at home may benefit from a home health care referral. The home care nurse assesses the patients incision and surgical drain(s), adequacy of pain management, adherence to the exercise plan, and overall physical and psychological functioning. It is unnecessary to assess the patients understanding of cancer at this stage of recovery. Prostheses may be considered later in the recovery process. 37. A patient has just been diagnosed with breast cancer and the nurse is performing a patient interview. In assessing this patients ability to cope with this diagnosis, what would be an appropriate question for the nurse to ask this patient? A) What is your level of education? B) Are you feeling alright these days? C) Is there someone you trust to help you make treatment choices? D) Are you concerned about receiving this diagnosis? C Feedback: A trusted ally to assist in making treatment choices is beneficial to the patients coping ability. It is condescending and inappropriate to ask if the patient is feeling alright these days or is concerned about the diagnosis. The patients education level is irrelevant. 38. A 35-year-old mother of three young children has been diagnosed with stage II breast cancer. After discussing treatment options with her physician, the woman goes home to talk to her husband, later calling the nurse for clarification of some points. The patient tells the nurse that the physician has recommended breast conservation surgery followed by radiation. The patients husband has done some online research and is asking why his wife does not have a modified radical mastectomy to be sure all the cancer is gone. What would be the nurses best response? A) Modified radical mastectomies are very hard on a patient, both physically and emotionally and they really arent necessary anymore. B) According to current guidelines, having a modified radical mastectomy is no longer seen as beneficial. C) Modified radical mastectomies have a poor survival rate because of the risk of cancer recurrence. D) According to current guidelines, breast conservation combined with radiation is as effective as a modified radical mastectomy. D Feedback: Breast conservation along with radiation therapy in stage I and stage II breast cancer results in a survival rate equal to that of modified radical mastectomy. Mastectomies are still necessary in many cases, but are not associated with particular risk of recurrence. 39. A patient who has had a lumpectomy calls the clinic to talk to the nurse. The patient tells the nurse that she has developed a tender area on her breast that is red and warm and looks like someone drew a line with a red marker. What would the nurse suspect is the womans problem? A) Mondor disease B) Deep vein thrombosis (DVT) of the breast C) Recurrent malignancy D) An area of fat necrosis A Feedback: Superficial thrombophlebitis of the breast (Mondor disease) is an uncommon condition that is usually associated with pregnancy, trauma, or breast surgery. Pain and redness occur as a result of a superficial thrombophlebitis in the vein that drains the outer part of the breast. The mass is usually linear, tender, and erythematous. Fat necrosis is a condition of the breast that is often associated with a history of trauma. The scenario described does not indicate a recurrent malignancy. DVTs of the breast do not occur. 40. A woman calls the clinic and tells the nurse she has had bloody drainage from her right nipple. The nurse makes an appointment for this patient, expecting the physician or practitioner to order what diagnostic test on this patient? A) Breast ultrasound B) Radiography C) Positron emission testing (PET) D) Galactography D Feedback: Galactography is a diagnostic procedure that involves injection of less than 1 mL of radiopaque material through a cannula inserted into the ductal opening on the areola, which is followed by mammography. It is performed to evaluate an abnormality within the duct when the patient has bloody nipple discharge on expression, spontaneous nipple discharge, or a solitary dilated duct noted on mammography. X-ray, PET, and ultrasound are not typically used for this purpose. Chapter 59: Assessment and Management of Patients With Male Reproductive Disorders 1. An adolescent is identified as having a collection of fluid in the tunica vaginalis of his testes. The nurse knows that this adolescent will receive what medical diagnosis? A) Cryptorchidism B) Orchitis C) Hydrocele D) Prostatism C Feedback: A hydrocele refers to a collection of fluid in the tunica vaginalis of the testes. Cryptorchidism is the most common congenital defect in males, characterized by failure of one or both of the testes to descend into the scrotum. Orchitis is an inflammation of the testes (testicular congestion) caused by pyogenic, viral, spirochetal, parasitic, traumatic, chemical, or unknown factors. Prostatism is an obstructive and irritative symptom complex that includes increased frequency and hesitancy in starting urination, a decrease in the volume and force of the urinary stream, acute urinary retention, and recurrent urinary tract infections. 2. An uncircumcised 78-year-old male has presented at the clinic complaining that he cannot retract his foreskin over his glans. On examination, it is noted that the foreskin is very constricted. The nurse should recognize the presence of what health problem? A) Bowens disease B) Peyronies disease C) Phimosis D) Priapism C Feedback: Phimosis is the term used to describe a condition in which the foreskin is constricted so that it cannot be retracted over the glans. Bowens disease is an in situ carcinoma of the penis. Peyronies disease is an acquired, benign condition that involves the buildup of fibrous plaques in the sheath of the corpus cavernosum. Priapism is an uncontrolled, persistent erection of the penis from either neural or vascular causes, including medications, sickle cell thrombosis, leukemic cell infiltration, spinal cord tumors, and tumor invasion of the penis or its vessels. 3. A nurse practitioner is assessing a 55-year-old male patient who is complaining of perineal discomfort, burning, urgency, and frequency with urination. The patient states that he has pain with ejaculation. The nurse knows that the patient is exhibiting symptoms of what? A) Varicocele B) Epididymitis C) Prostatitis D) Hydrocele C Feedback: Perineal discomfort, burning, urgency, frequency with urination, and pain with ejaculation is indicative of prostatitis. A varicocele is an abnormal dilation of the pampiniform venous plexus and the internal spermatic vein in the scrotum (the network of veins from the testis and the epididymis that constitute part of the spermatic cord). Epididymitis is an infection of the epididymis that usually descends from an infected prostate or urinary tract; it also may develop as a complication of gonorrhea. A hydrocele is a collection of fluid, generally in the tunica vaginalis of the testis, although it also may collect within the spermatic cord. 4. A patient has been prescribed sildenafil. What should the nurse teach the patient about this medication? A) Sexual stimulation is not needed to obtain an erection. B) The drug should be taken 1 hour prior to intercourse. C) Facial flushing or headache should be reported to the physician immediately. D) The drug has the potential to cause permanent visual changes. B Feedback: The patient must have sexual stimulation to create the erection, and the drug should be taken 1 hour before intercourse. Facial flushing, mild headache, indigestion, and running nose are common side effects of Viagra and do not normally warrant reporting to the physician. Some visual disturbances may occur, but these are transient. 5. A patient is 24 hours postoperative following prostatectomy and the urologist has ordered continuous bladder irrigation. What color of output should the nurse expect to find in the drainage bag? A) Red wine colored B) Tea colored C) Amber D) Light pink D Feedback: The urine drainage following prostatectomy usually begins as a reddish pink, then clears to a light pink 24 hours after surgery. 6. A public health nurse has been asked to provide a health promotion session for men at a wellness center. What should the nurse inform the participants about testicular cancer? A) It is most common among men over 55. B) It is one of the least curable solid tumors. C) It typically does not metastasize. D) It is highly responsive to treatment. D Feedback: Testicular cancer is most common among men 15 to 35 years of age and produces a painless enlargement of the testicle. Testicular cancers metastasize early but are one of the most curable solid tumors, being highly responsive to chemotherapy. 7. A nurse is planning the postoperative care of a patient who is scheduled for radical prostatectomy. What intraoperative position will place the patient at particular risk for the development of deep vein thrombosis postoperatively? A) Fowlers position B) Prone position C) Supine position D) Lithotomy position D Feedback: Elastic compression stockings are applied before surgery and are particularly important for prevention of deep vein thrombosis if the patient is placed in a lithotomy position during surgery. During a prostatectomy, the patient is not placed in the supine, prone, or Fowlers position. 8. A patient has just been diagnosed with prostate cancer and is scheduled for brachytherapy next week. The patient and his wife are unsure of having the procedure because their daughter is 3 months pregnant. What is the most appropriate teaching the nurse should provide to this family? A) The patient should not be in contact with the baby after delivery. B) The patients treatment poses no risk to his daughter or her infant. C) The patients brachytherapy may be contraindicated for safety reasons. D) The patient should avoid close contact with his daughter for 2 months. D Feedback: Brachytherapy involves the implantation of interstitial radioactive seeds under anesthesia. The surgeon uses ultrasound guidance to place about 80 to 100 seeds, and the patient returns home after the procedure. Exposure of others to radiation is minimal, but the patient should avoid close contact with pregnant women and infants for up to 2 months. 9. A patient has presented at the clinic with symptoms of benign prostatic hyperplasia. What diagnostic findings would suggest that this patient has chronic urinary retention? A) Hypertension B) Peripheral edema C) Tachycardia and other dysrhythmias D) Increased blood urea nitrogen (BUN) D Feedback: Hypertension, edema, and tachycardia would not normally be associated with benign prostatic hyperplasia. Azotemia is an accumulation of nitrogenous waste products, and renal failure can occur with chronic urinary retention and large residual volumes. 10. A 55-year-old man presents at the clinic complaining of erectile dysfunction. The patient has a history of diabetes. The physician orders tadalafil (Cialis) to be taken 1 hour before sexual intercourse. The nurse reviews the patients history prior to instructing the patient on the use of this medication. What disorder will contraindicate the use of tadalafil (Cialis)? A) Cataracts B) Retinopathy C) Hypotension D) Diabetic nephropathy B Feedback: Patients with cataracts, hypotension, or nephropathy will be allowed to take tadalafil (Cialis) and sildenafil (Viagra) if needed. However, tadalafil (Cialis) and sildenafil (Viagra) are usually contraindicated with diabetic retinopathy. 11. A nurse is teaching a 53-year-old man about prostate cancer. What information should the nurse provide to best facilitate the early identification of prostate cancer? A) Have a digital rectal examination and prostate-specific antigen (PSA) test done yearly. B) Have a transrectal ultrasound every 5 years. C) Perform monthly testicular self-examinations, especially after age 60. D) Have a complete blood count (CBC), blood urea nitrogen (BUN) and creatinine assessment performed annually. A Feedback: The incidence of prostate cancer increases after age 50. The digital rectal examination, which identifies enlargement or irregularity of the prostate, and the PSA test, a tumor marker for prostate cancer, are effective diagnostic measures that should be done yearly. Testicular self-examinations wont identify changes in the prostate gland due to its location in the body. A transrectal ultrasound and CBC with BUN and creatinine assessment are usually done after diagnosis to identify the extent of disease and potential metastases. 12. A public health nurse is teaching a health class for the male students at the local high school. The nurse is teaching the boys to perform monthly testicular self-examinations. What point would be appropriate to emphasize? A) Testicular cancer is a highly curable type of cancer. B) Testicular cancer is very difficult to diagnose. C) Testicular cancer is the number one cause of cancer deaths in males. D) Testicular cancer is more common in older men. A Feedback: Testicular cancer is highly curable, particularly when its treated in its early stage. Self-examination allows early detection and facilitates the early initiation of treatment. The highest mortality rates from cancer among men are with lung cancer. Testicular cancer is found more commonly in younger men. 13. A patient has just returned to the floor following a transurethral resection of the prostate. A triple-lumen indwelling urinary catheter has been inserted for continuous bladder irrigation. What, in addition to balloon inflation, are the functions of the three lumens? A) Continuous inflow and outflow of irrigation solution B) Intermittent inflow and continuous outflow of irrigation solution C) Continuous inflow and intermittent outflow of irrigation solution D) Intermittent flow of irrigation solution and prevention of hemorrhage A Feedback: For continuous bladder irrigation, a triple-lumen indwelling urinary catheter is inserted. The three lumens provide for balloon inflation and continuous inflow and outflow of irrigation solution. 14. A nurse is assessing a patient who presented to the ED with priapism. The student nurse is aware that this condition is classified as a urologic emergency because of the potential for what? A) Urinary tract infection B) Chronic pain C) Permanent vascular damage D) Future erectile dysfunction C Feedback: The ischemic form of priapism, which is described as nonsexual, persistent erection with little or no cavernous blood flow, must be treated promptly to prevent permanent damage to the penis. Priapism has not been indicated in the development of UTIs, chronic pain, or erectile dysfunction. 15. A man comes to the clinic complaining that he is having difficulty obtaining an erection. When reviewing the patients history, what might the nurse note that contributes to erectile dysfunction? A) The patient has been treated for a UTI twice in the past year. B) The patient has a history of hypertension. C) The patient is 66 years old. D) The patient leads a sedentary lifestyle. B Feedback: Past history of infection and lack of exercise do not contribute to impotence. With advancing age, sexual function and libido and potency decrease somewhat, but this is not the primary reason for impotence. Vascular problems cause about half the cases of impotence in men older than 50 years; hypertension is a major cause of such problems. 16. A 35-year-old man is seen in the clinic because he is experiencing recurring episodes of urinary frequency, dysuria, and fever. The nurse should recognize the possibility of what health problem? A) Chronic bacterial prostatitis B) Orchitis C) Benign prostatic hyperplasia D) Urolithiasis A Feedback: Prostatitis is an inflammation of the prostate gland that is often associated with lower urinary tract symptoms and symptoms of sexual discomfort and dysfunction. Symptoms are usually mild, consisting of frequency, dysuria, and occasionally urethral discharge. Urinary incontinence and retention occur with benign prostatic hyperplasia or hypertrophy. The patient may experience nocturia, urgency, decrease in volume and force of urinary stream. Urolithiasis is characterized by excruciating pain. Orchitis does not cause urinary symptoms. 17. To decrease glandular cellular activity and prostate size, an 83-year-old patient has been prescribed finasteride (Proscar). When performing patient education with this patient, the nurse should be sure to tell the patient what? A) Report the planned use of dietary supplements to the physician. B) Decrease the intake of fluids to prevent urinary retention. C) Abstain from sexual activity for 2 weeks following the initiation of treatment. D) Anticipate a temporary worsening of urinary retention before symptoms subside. A Feedback: Some herbal supplements are contraindicated with Proscar, thus their planned use should be discussed with the physician or pharmacist. The patient should maintain normal fluid intake. There is no need to abstain from sexual activity and a worsening of urinary retention is not anticipated. 18. A nurse is providing an educational event to a local mens group about prostate cancer. The nurse should cite an increased risk of prostate cancer in what ethnic group? A) Native Americans B) Caucasian Americans C) African Americans D) Asian Americans C Feedback: African American men have a high risk of prostate cancer; furthermore, they are more than twice as likely to die from prostate cancer as men of other racial or ethnic groups. 19. A man tells the nurse that his father died of prostate cancer and he is concerned about his own risk of developing the disease, having heard that prostate cancer has a genetic link. What aspect of the pathophysiology of prostate cancer would underlie the nurses response? A) A number of studies have identified an association of BRCA-2 mutation with an increased risk of prostate cancer. B) HNPCC is a mutation of two genes that causes prostate cancer in men and it is autosomal dominant. C) Studies have shown that the presence of the TP53 gene strongly influences the incidence of prostate cancer. D) Recent research has demonstrated that prostate cancer is the result of lifestyle factors and that genetics are unrelated. A Feedback: A number of studies have identified an association of BRCA-2 mutation with an increased risk of prostate cancer. HPNCC is a form of colon cancer. The TP53 gene is associated with breast cancer. 20. A nurse is performing an admission assessment on a 40-year-old man who has been admitted for outpatient surgery on his right knee. While taking the patients family history, he states, My father died of prostate cancer at age 48. The nurse should instruct him on which of the following health promotion activities? A) The patient will need PSA levels drawn starting at age 55. B) The patient should have testing for presence of the CDH1 and STK11 genes. C) The patient should have PSA levels drawn regularly. D) The patient should limit alcohol use due to the risk of malignancy. C Feedback: PSA screening is warranted by the patients family history and should not be delayed until age 55. The CDH1 and STK11 genes do not relate to the risk for prostate cancer. Alcohol consumption by the patient should be limited. However, this is not the most important health promotion intervention. 21. A 35-year-old father of three tells the nurse that he wants information on a vasectomy. What would the nurse tell him about ejaculate after a vasectomy? A) There will be no ejaculate after a vasectomy, though the patients potential for orgasm is unaffected. B) There is no noticeable decrease in the amount of ejaculate even though it contains no sperm. C) There is a marked decrease in the amount of ejaculate after vasectomy, though this does not affect sexual satisfaction. There is no change in the quantity of ejaculate after vasectomy, but the viscosity is somewhat increased. B Feedback: Seminal fluid is manufactured predominantly in the seminal vesicles and prostate gland, which are unaffected by vasectomy, thus no noticeable decrease in the amount of ejaculate occurs (volume decreases approximately 3%), even though it contains no spermatozoa. The viscosity of ejaculate does not change. 22. A 76-year-old with a diagnosis of penile cancer has been admitted to the medical floor. Because the incidence of penile cancer is so low, the staff educator has been asked to teach about penile cancer. What risk factors should the educator cite in this presentation? Select all that apply. A) Phimosis B) Priapism C) Herpes simplex infection D) Increasing age E) Lack of circumcision A, D, E Feedback: Several risk factors for penile cancer have been identified, including lack of circumcision, poor genital hygiene, phimosis, HPV, smoking, ultraviolet light treatment of psoriasis on the penis, increasing age (two-thirds of cases occur in men older than 65 years of age), lichen sclerosus, and balanitis xerotica obliterans. Priapism and HSV are not known risk factors. 23. A 75-year-old male patient is being treated for phimosis. When planning this patients care, what health promotion activity is most directly related to the etiology of the patients health problem? A) Teaching the patient about safer sexual practices B) Teaching the patient about the importance of hygiene C) Teaching the patient about the safe use of PDE-5 inhibitors D) Teaching the patient to perform testicular self-examination B Feedback: Poor hygiene often contributes to cases of phimosis. This health problem is unrelated to sexual practices, the use of PDE-5 inhibitors, or testicular self-examination. A patient who is postoperative day 12 and recovering at home following a laparoscopic prostatectomy has reported that he is experiencing occasional dribbling of urine. How should the nurse best respond to this patients concern? A) Inform the patient that urinary control is likely to return gradually. B) Arrange for the patient to be assessed by his urologist. C) Facilitate the insertion of an indwelling urinary catheter by the home care nurse. D) Teach the patient to perform intermittent self-catheterization. A Feedback: It is important that the patient know that regaining urinary control is a gradual process; he may continue to dribble after being discharged from the hospital, but this should gradually diminish (usually within 1 year). At this point, medical follow-up is likely not necessary. There is no need to perform urinary catheterization. 25. A physician explains to the patient that he has an inflammation of the Cowper glands. Where are the Cowper glands located? A) Within the epididymis B) Below the prostate, within the posterior aspect of the urethra C) On the inner epithelium lining the scrotum, lateral to the testes D) Medial to the vas deferens B Feedback: Cowper glands lie below the prostate, within the posterior aspect of the urethra. This gland empties its secretions into the urethra during ejaculation, providing lubrication. The Cowper glands do not lie within the epididymis, within the scrotum, or alongside the vas deferens. 26. A nursing student is learning how to perform sexual assessments using the PLISSIT model. According to this model, the student should begin an assessment by doing which of the following? A) Briefly teaching the patient about normal sexual physiology B) Assuring the patient that what he says will be confidential C) Asking the patient if he is willing to discuss sexual functioning D) Ensuring patient privacy C Feedback: The PLISSIT (permission, limited information, specific suggestions, intensive therapy) model of sexual assessment and intervention may be used to provide a framework for nursing interventions. By beginning with the patients permission, the nurse establishes a patient-centered focus. 27. A nurse is caring for a 33-year-old male who has come to the clinic for a physical examination. He states that he has not had a routine physical in 5 years. During the examination, the physician finds that digital rectal examination (DRE) reveals stoney hardening in the posterior lobe of the prostate gland that is not mobile. The nurse recognizes that the observation typically indicates what? A) A normal finding B) A sign of early prostate cancer C) Evidence of a more advanced lesion D) Metastatic disease C Feedback: Routine repeated DRE (preferably by the same examiner) is important, because early cancer may be detected as a nodule within the gland or as an extensive hardening in the posterior lobe. The more advanced lesion is stony hard and fixed. This finding is not suggestive of metastatic disease. 28. A patient who is scheduled for an open prostatectomy is concerned about the potential effects of the surgery on his sexual function. What aspect of prostate surgery should inform the nurses response? A) Erectile dysfunction is common after prostatectomy as a result of hormonal changes. B) All prostatectomies carry a risk of nerve damage and consequent erectile dysfunction. C) Erectile dysfunction after prostatectomy is expected, but normally resolves within several months. D) Modern surgical techniques have eliminated the risk of erectile dysfunction following prostatectomy. B Feedback: All prostatectomies carry a risk of impotence because of potential damage to the pudendal nerves. If this damage occurs, the effects are permanent. Hormonal changes do not affect sexual functioning after prostatectomy. 29. A patient has returned to the floor from the PACU after undergoing a suprapubic prostatectomy. The nurse notes significant urine leakage around the suprapubic tube. What is the nurses most appropriate action? A) Cleanse the skin surrounding the suprapubic tube. B) Inform the urologist of this finding. C) Remove the suprapubic tube and apply a wet-to-dry dressing. D) Administer antispasmodic drugs as ordered. B Feedback: The physician should be informed if there is significant leakage around a suprapubic catheter. Cleansing the skin is appropriate but does not resolve the problem. Removing the suprapubic tube is contraindicated because it is unsafe. Administering drugs will not stop the leakage of urine around the tube. 30. A 29-year-old patient has just been told that he has testicular cancer and needs to have surgery. During a presurgical appointment, the patient admits to feeling devastated that he requires surgery, stating that it will leave him emasculated and a shell of a man. The nurse should identify what nursing diagnosis when planning the patients subsequent care? A) Disturbed Body Image Related to Effects of Surgery B) Spiritual Distress Related to Effects of Cancer Surgery C) Social Isolation Related to Effects of Surgery D) Risk for Loneliness Related to Change in Self-Concept A Feedback: The patients statements specifically address his perception of his body as it relates to his identity. Consequently, a nursing diagnosis of Disturbed Body Image is likely appropriate. This patient is at risk for social isolation and loneliness, but theres no indication in the scenario that these diagnoses are present. There is no indication of spiritual element to the patients concerns. 31. A nurse is providing care for a patient who has recently been admitted to the postsurgical unit from PACU following a transuretheral resection of the prostate. The nurse is aware of the nursing diagnosis of Risk for Imbalanced Fluid Volume. In order to assess for this risk, the nurse should prioritize what action? A) Closely monitoring the input and output of the bladder irrigation system B) Administering parenteral nutrition and fluids as ordered C) Monitoring the patients level of consciousness and skin turgor D) Scanning the patients bladder for retention every 2 hours A Feedback: Continuous bladder irrigation effectively reduces the risk of clots in the GU tract but also creates a risk for fluid volume excess if it becomes occluded. The nurse must carefully compare input and output, and ensure that these are in balance. Parenteral nutrition is unnecessary after prostate surgery and skin turgor is not an accurate indicator of fluid status. Frequent bladder scanning is not required when a urinary catheter is in situ. 32. A 22-year-old male is being discharged home after surgery for testicular cancer. The patient is scheduled to begin chemotherapy in 2 weeks. The patient tells the nurse that he doesnt think he can take weeks or months of chemotherapy, stating that he has researched the adverse effects online. What is the most appropriate nursing action for this patient at this time? A) Provide empathy and encouragement in an effort to foster a positive outlook. B) Tell the patient it is his decision whether to accept or reject chemotherapy. C) Report the patients statement to members of his support system. D) Refer the patient to social work. A Feedback: Patients may be required to endure a long course of therapy and will need encouragement to maintain a positive attitude. It is certainly the patients ultimate decision to accept or reject chemotherapy, but the nurse should focus on promoting a positive outlook. It would be a violation of confidentiality to report the patients statement to members of his support system and there is no obvious need for a social work referral. 33. A 57-year-old male comes to the clinic complaining that when he has an erection his penis curves and becomes painful. The patients diagnosis is identified as severe Peyronies disease. The nurse should be aware of what likely treatment modality? A) Physical therapy B) Treatment with PDE-5 inhibitors C) Intracapsular hydrocortisone injections D) Surgery D Feedback: Surgical removal of mature plaques is used to treat severe Peyronies disease. There is no potential benefit to physical therapy and hydrocortisone injections are not normally used. PDE-5 inhibitors would exacerbate the problem. 34. A patient has experienced occasional urinary incontinence in the weeks since his prostatectomy. In order to promote continence, the nurse should encourage which of the following? A) Pelvic floor exercises B) Intermittent urinary catheterization C) Reduced physical activity D) Active range of motion exercises A Feedback: Pelvic floor muscles can promote the resumption of normal urinary function following prostate surgery. Catheterization is normally unnecessary, and it carries numerous risks of adverse effects. Increasing or decreasing physical activity is unlikely to influence urinary function. 35. A clinic nurse is providing preprocedure education for a man who will undergo a vasectomy. Which of the following measures will enhance healing and comfort? Select all that apply. A) Abstaining from sexual intercourse for at least 14 days postprocedure B) Wearing a scrotal support garment C) Using sitz baths D) Applying a heating pad intermittently E) Staying on bed rest for 48 to 72 hours postprocedure B, C Feedback: Applying ice bags intermittently to the scrotum for several hours after surgery can reduce swelling and relieve discomfort, and is preferable to the application of heat. The nurse advises the patient to wear snug, cotton underwear or a scrotal support for added comfort and support. Sitz baths can also enhance comfort. Extended bed rest is unnecessary, and sexual activity can usually be resumed in 1 week. 36. A patient has returned to the floor after undergoing a transurethral resection of the prostate (TURP). The patient has a continuous bladder irrigation system in place. The patient tells you he is experiencing bladder spasms and asks what you can do to relieve his discomfort. What is the most appropriate nursing action to relieve the discomfort of the patient? A) Apply a cold compress to the pubic area. B) Notify the urologist promptly. C) Irrigate the catheter with 30 to 50 mL of normal saline as ordered. D) Administer a smooth-muscle relaxant as ordered. D Feedback: Administering a medication that relaxes smooth muscles can help relieve bladder spasms. Neither a cold compress nor catheter irrigation will alleviate bladder spasms. In most cases, this problem can be relieved without the involvement of the urologist, who will normally order medications on a PRN basis. 37. A patient confides to the nurse that he cannot engage in sexual activity. The patient is 27 years old and has no apparent history of chronic illness that would contribute to erectile dysfunction. What does the nurse know will be ordered for this patient to assess his sexual functioning? A) Sperm count B) Ejaculation capacity tests C) Engorgement tests D) Nocturnal penile tumescence tests D Feedback: Nocturnal penile tumescence tests may be conducted in a sleep laboratory to monitor changes in penile circumference during sleep using various methods to determine number, duration, rigidity, and circumference of penile erections; the results help identify whether the erectile dysfunction is caused by physiologic and/or psychological factors. A sperm count would be done if the patient was complaining of infertility. Ejaculation capacity tests and engorgement tests are not applicable for assessment in this circumstance. 38. The nurse is leading a workshop on sexual health for men. The nurse should teach participants that organic causes of erectile dysfunction include what? Select all that apply. A) Diabetes B) Testosterone deficiency C) Anxiety D) Depression E) Parkinsonism A, B, E Feedback: Organic causes of ED include cardiovascular disease, endocrine disease (diabetes, pituitary tumors, testosterone deficiency, hyperthyroidism, and hypothyroidism), cirrhosis, chronic renal failure, genitourinary conditions (radical pelvic surgery), hematologic conditions (Hodgkin disease, leukemia), neurologic disorders (neuropathies, parkinsonism, spinal cord injury, multiple sclerosis), trauma to the pelvic or genital area, alcohol, smoking, medications, and drug abuse. Anxiety and depression are considered to be psychogenic causes. 39. A patient has been diagnosed with erectile dysfunction; the cause has been determined to be psychogenic. The patients interdisciplinary plan of care should prioritize which of the following interventions? A) Penile implant B) PDE-5 inhibitors C) Physical therapy D) Psychotherapy D Feedback: Patients with erectile dysfunction from psychogenic causes are referred to a health care provider or therapist who specializes in sexual dysfunction. Because of the absence of an organic cause, medications and penile implants are not first-line treatments. Physical therapy is not normally effective in the treatment of ED. 40. A patient presents to the emergency department with paraphimosis. The physician is able to compress the glans and manually reduce the edema. Once the inflammation and edema subside, what is usually indicated? A) Needle aspiration of the corpus cavernosum B) Circumcision C) Abstinence from sexual activity for 6 weeks D) Administration of vardenafil B Feedback: Circumcision is usually indicated after the inflammation and edema subside. Needle aspiration of the corpus cavernosum is indicated in priapism; abstinence from sexual activity for 6 weeks is not indicated. Vardenafil is Levitra and would not be used for paraphimosis. Chapter 60: Assessment of Integumentary Function 1. A nurse is aware that the outer layer of the skin consists of dead cells that contain large amounts of keratin. The physiologic functions of keratin include which of the following? Select all that apply. A) Producing antibodies B) Absorbing electrolytes C) Maintaining acidbase balance D) Physically repelling pathogens E) Preventing fluid loss D, E Feedback: The dead cells of the epidermis contain large amounts of keratin, an insoluble, fibrous protein that forms the outer barrier of the skin. Keratin has the capacity to repel pathogens and prevent excessive fluid loss from the body. It does not contribute directly to antibody production, acidbase balance, or electrolyte levels. 2. When planning the skin care of a patient with decreased mobility, the nurse is aware of the varying thickness of the epidermis. At what location is the epidermal layer thickest? A) The scalp B) The elbows C) The palms of the hands D) The knees C Feedback: The epidermis is the thickest over the palms of the hands and the soles of the feet. 3. A young student is brought to the school nurse after falling off a swing. The nurse is documenting that the child has bruising on the lateral aspect of the right arm. What term will the nurse use to describe bruising on the skin in documentation? A) Telangiectasias B) Ecchymoses C) Purpura D) Urticaria B Feedback: Telangiectasias consists of red marks on the skin caused by stretching of superficial blood vessels. Ecchymoses are bruises, and purpura consists of pinpoint hemorrhages into the skin. Urticariais wheals or hives. 4. The nurse in an ambulatory care center is admitting an older adult patient who has bright red moles on the skin. Benign changes in elderly skin that appear as bright red moles are termed what? A) Cherry angiomas B) Solar lentigo C) Seborrheickeratoses D) Xanthelasma A Feedback: Cherry angiomas appear as bright red moles, while solar lentigo are commonly called liver spots. Seborrheickeratoses are described as crusty brown stuck on patches, while xanthelasma appears as yellowish, waxy deposits on the upper eyelids. 5. While assessing a dark-skinned patient at the clinic, the nurse notes the presence of patchy, milky white spots. The nurse knows that this finding is characteristic of what diagnosis? A) Cyanosis B) Addisons disease C) Polycythemia D) Vitiligo D Feedback: With cyanosis, nail beds are dusky. With polycythemia, the nurse notes ruddy blue face, oral mucosa, and conjunctiva. A bronzed appearance, or external tan, is associated with Addisons disease. Vitiligo is a condition characterized by destruction of the melanocytes in circumscribed areas of skin and appears in light or dark skin as patchy, milky white spots, often symmetric bilaterally. 6. While waiting to see the physician, a patient shows the nurse skin areas that are flat, nonpalpable, and have had a change of color. The nurse recognizes that the patient is demonstrating what? A) Macules B) Papules C) Vesicles D) Pustules A Feedback: A macule is a flat, nonpalpable skin color change, while a papule is an elevated, solid, palpable mass. A vesicle is a circumscribed, elevated, palpable mass containing serous fluid, while a pustule is a pus-filled vesicle. 7. An African American is admitted to the medical unit with liver disease. To correctly assess this patient for jaundice, on what body area should the nurse look for yellow discoloration? A) Elbows B) Lips C) Nail beds D) Sclerae D Feedback: Jaundice, a yellowing of the skin, is directly related to elevations in serum bilirubin and is often first observed in the sclerae and mucous membranes. 8. A nurse is doing a shift assessment on a group of patients after first taking report. An elderly patient is having her second dose of IV antibiotics for a diagnosis of pneumonia. The nurse notices a new rash on the patients chest. The nurse should ask what priority question regarding the presence of a reddened rash? A) Is the rash worse at a particular time or season? B) Are you allergic to any foods or medication? C) Are you having any loss of sensation in that area? D) Is your rash painful? B Feedback: The nurse should suspect an allergic reaction to the antibiotic therapy. Allergies can be a significant threat to the patients immediate health, thus questions addressing this possibility would be prioritized over those addressing sensation. Asking about previous rashes is important, but this should likely be framed in the context of an allergy assessment. 9. A gerontologic nurse is teaching a group of nursing students about integumentary changes that occur in older adults. How should these students best integrate these changes into care planning? A) By avoiding the use of moisturizing lotions on older adults skin B) By protecting older adults against shearing injuries C) By avoiding the use of ice packs to treat muscle pain D) By protecting older adults against excessive sweat accumulation B Feedback: Cellular changes associated with aging include thinning at the junction of the dermis and epidermis, which creates a risk for shearing injuries. Moisturizing lotions can be safely used to address the increased dryness of older adults skin. Ice packs can be used, provided skin is assessed regularly and the patient possesses normal sensation. Older adults perspire much less than younger adults, thus sweat accumulation is rarely an issue. 10. A patient is diagnosed with atrial fibrillation and the physician orders Coumadin (warfarin). For what skin lesion should the nurse monitor this patient? A) Ulcer B) Ecchymosis C) Scar D) Erosion B Feedback: Ecchymosis refers to a round or irregular macular lesion, which is larger than petechiae. This occurs secondary to blood extravasation. It is important to watch for ecchymosis in a patient receiving any type of anticoagulant. An ulcer is an open lesion eroded into the patients flesh. A scar is an area on the skin caused by the healing of an injury. Erosion is loss of superficial epidermis that does not extend to the dermisa depressed, moist area. 11. A new patient has come to the dermatology clinic to be assessed for a reddened rash on his abdomen. What diagnostic test would most likely be ordered to identify the causative allergen? A) Skin scrapings B) Skin biopsy C) Patch testing D) Tzanck smear C Feedback: Patch testing is performed to identify substances to which the patient has developed an allergy. Skin scrapings are done for suspected fungal lesions. A skin biopsy is completed to rule out malignancy and to establish an exact diagnosis of skin lesions. A Tzanck smear is used to examine cells from blistering skin conditions, such as herpes zoster. 12. A patient with a suspected malignant melanoma is referred to the dermatology clinic. The nurse knows to facilitate what diagnostic test to rule out a skin malignancy? A) Tzanck smear B) Skin biopsy C) Patch testing D) Skin scrapings B Feedback: A skin biopsy is done to rule out malignancies of skin lesions. A Tzanck smear is used to examine cells from blistering skin conditions, such as herpes zoster. Patch testing is performed to identify substances to which the patient has developed an allergy. Skin scrapings are done for suspected fungal infections. A nurse is explaining the importance of sunlight on the skin to a woman with decreased mobility who rarely leaves her house. The nurse would emphasize that ultraviolet light helps to synthesize what vitamin? A) E B) D C) A D) C B Feedback: Skin exposed to ultraviolet light can convert substances necessary for synthesizing vitamin D (cholecalciferol). Vitamin D is essential for preventing rickets, a condition that causes bone deformities and results from a deficiency of vitamin D, calcium, and phosphorus. 14. A nurse is working with a patient who has a diagnosis of Cushing syndrome. When completing a physical assessment, the nurse should specifically observe for what integumentary manifestation? A) Alopecia B) Yellowish skin tone C) Patchy, bronze pigmentation D) Hirsutism D Feedback: Cushing syndrome causes excessive hair growth, especially in women. Alopecia is hair loss from the scalp and other parts of the body. Jaundice causes a yellow discoloration in light-skinned patients, but this does not accompany Cushing syndrome. Patients that have Addisons disease exhibit a bronze discoloration to their skin due to increased melanin production. 15. The outer layer of the epidermis provides the most effective barrier to penetration of the skin by environmental factors. Which of the following is an example of penetration by an environmental factor? A) An insect bite B) Dehydration C) Sunburn D) Excessive perspiration A Feedback: The stratum corneum, the outer layer of the epidermis, provides the most effective barrier to both epidermal water loss and penetration of environmental factors, such as chemicals, microbes, insect bites, and other trauma. Dehydration, sunburn, and excessive perspiration are not examples of penetration of an environmental factor. 16. A nurse in a dermatology clinic is reading the electronic health record of a new patient. The nurse notes that the patient has a history of a primary skin lesion. What is an example of a primary skin lesion? A) Crust B) Keloid C) Pustule D) Ulcer C Feedback: A pustule is an example of a primary skin lesion. Primary skin lesions are original lesions arising from previously normal skin. Crusts, keloids and ulcers are secondary lesions. 17. An unresponsive Caucasian patient has been brought to the emergency room by EMS. While assessing this patient, the nurse notes that the patients face is a cherry-red color. What should the nurse suspect? A) Carbon monoxide poisoning B) Anemia C) Jaundice D) Uremia A Feedback: Carbon monoxide poisoning causes a bright cherry red color in the face and upper torso in light-skinned persons. In dark-skinned persons, there will be a cherry red color to nail beds, lips, and oral mucosa. When anemia occurs in light-skinned persons, the skin has generalized pallor. Anemia in dark-skinned persons manifests as a yellow-brown coloration. Jaundice appears as a yellow coloration of the sclerae. Uremia gives a yellow-orange tinge to the skin. 18. A nurse is providing an educational presentation addressing the topic of Protecting Your Skin. When discussing the anatomy of the skin with this group, the nurse should know that what cells are responsible for producing the pigmentation of the skin? A) Islets of Langerhans B) Squamous cells C) T cells D) Melanocytes D Feedback: Melanocytes are the special cells of the epidermis that are primarily responsible for producing the pigment melanin. Islets of Langerhans are clusters of cells in the pancreas. Squamous cells are flat, scaly epithelial cells. T cells function in the immune response. 19. A wound care nurse is reviewing skin anatomy with a group of medical nurses. Which area of the skin would the nurse identify as providing a cushion between the skin layers, muscles, and bones? A) Dermis B) Subcutaneous tissue C) Epidermis D) Stratum corneum B Feedback: The subcutaneous tissue, or hypodermis, is the innermost layer of the skin that is responsible for providing a cushion between the skin layers, muscles, and bones. The dermis is the largest portion of the skin, providing strength and structure. The epidermis is the outermost layer of stratified epithelial cells and composed of keratinocytes. The stratum corneum is the outermost layer of the epidermis, which provides a barrier to prevent epidermal water loss. 20. A young student comes to the school nurse and shows the nurse a mosquito bite. As the nurse expects, the bite is elevated and has serous fluid contained in the dermis. How would the nurse classify this lesion? A) Vesicle B) Macule C) Nodule D) Wheal D Feedback: A wheal is a primary skin lesion that is elevated and has fluid contained in the dermis. An example of a wheal would be an insect bite or hives. Vesicles, macules, and nodules are not characterized by elevation and the presence of serous fluid. 21. While assessing a 25-year-old female, the nurse notes that the patient has hair on her lower abdomen. Earlier in the health interview, the patient stated that her menses are irregular. The nurse should suspect what type of health problem? A) A metabolic disorder B) A malignancy C) A hormonal imbalance D) An infectious process C Feedback: Some women with higher levels of testosterone have hair in the areas generally thought of as masculine, such as the face, chest, and lower abdomen. This is often a normal genetic variation, but if it appears along with irregular menses and weight changes, it may indicate a hormonal imbalance. This combination of irregular menses and hair distribution is inconsistent with metabolic disorders, malignancy, or infection. 22. An 82-year-old patient is being treated in the hospital for a sacral pressure ulcer. What age-related change is most likely to affect the patients course of treatment? A) Increased thickness of the subcutaneous skin layer B) Increased vascular supply to superficial skin layers C) Changes in the character and quantity of bacterial skin flora D) Increased time required for wound healing D Feedback: Wound healing becomes slower with age, requiring more time for older adults to recover from surgical and traumatic wounds. There are no changes in skin flora with increased age. Vascular supply and skin thickness both decrease with age. 23. A nurse is preparing to perform the physical assessment of a newly admitted patient. During which of the following components of the assessment should the nurse wear gloves? Select all that apply. A) Palpation of the patients scalp B) Palpation of the patients upper extremities C) Palpation of a rash on the patients trunk D) Palpation of a lesion on the patients upper back E) Palpation of the patients fingers C, D Feedback: Gloves are worn during skin examination if a rash or lesions are to be palpated. It is not normally necessary to wear gloves to palpate a patients scalp, extremities, or fingers unless contact with body fluids is reasonably foreseeable. 24. A patient with an exceptionally low body mass index has been admitted to the emergency department with signs and symptoms of hypothermia. The nurse should know that this patients susceptibility to heat loss is related to atrophy of what skin component? A) Epidermis B) Merkel cells C) Dermis D) Subcutaneous tissue D Feedback: The subcutaneous tissues and the amount of fat deposits are important factors in body temperature regulation. The epidermis is an outermost layer of stratified epithelial cells. Merkel cells are receptors that transmit stimuli to the axon through a chemical synapse. The dermis makes up the largest portion of the skin, providing strength and structure. It is composed of two layers: papillary and reticular. 25. A nurse is reviewing gerontologic considerations relating to the care of patients with dermatologic problems. What vulnerability results from the age-related loss of subcutaneous tissue? A) Decreased resistance to ultraviolet radiation B) Increased vulnerability to infection C) Diminished protection of tissues and organs D) Increased risk of skin malignancies C Feedback: Loss of the subcutaneous tissue substances of elastin, collagen, and fat diminishes the protection and cushioning of underlying tissues and organs, decreases muscle tone, and results in the loss of the insulating properties of fat. This age-related change does not correlate to an increased vulnerability to sun damage, infection, or cancer. 26. An 80-year-old patient is brought to the clinic by her son. The son asks the nurse why his mother has gotten so many spots on her skin. What would be an appropriate response by the nurse? A) As people age, they normally develop uneven pigmentation in their skin. B) These spots are called liver spots or age spots. C) Older skin is more apt to break down and tear, causing sores. D) These are usually the result of nutritional deficits earlier in life. A Feedback: The major changes in the skin of older people include dryness, wrinkling, uneven pigmentation, and various proliferative lesions. Stating the names of these spots and identifying older adults vulnerability to skin damage do not answer the sons question. These lesions are not normally a result of nutritional imbalances. 27. An older adult patient is diagnosed with a vitamin D deficiency. What would be an appropriate recommendation by the nurse? A) Spend time outdoors at least twice per week B) Increase intake of leafy green vegetables C) Start taking a multivitamin each morning D) Eat red meat at least once per week A Feedback: Skin exposed to ultraviolet light can convert substances necessary for synthesizing vitamin D (cholecalciferol). It is estimated that most people need five to thirty minutes of sun exposure twice a week in order for this synthesis to occur. Multivitamins may not resolve a specific vitamin D deficiency. Vitamin D is unrelated to meat and vegetable intake. 28. The nurse is performing an initial assessment of a patient who has a raised, pruritic rash. The patient denies taking any prescription medication and denies any allergies. What would be an appropriate question to ask this patient at this time? A) Is anyone in your family allergic to anything? B) How long have you had this abrasion? C) Do you take any over-the-counter drugs or herbal preparations? D) What do you do for a living? C Feedback: If suspicious areas are noted, the patient is questioned about nonprescription or herbal preparations that might be in use. Ascertaining a family history of allergies would not give helpful information at this time. The patients lesion is not described as an abrasion. The patients occupation may or may not be relevant; it is more important to assess for herb or drug reactions. 29. A nurse is conducting a health interview and is assessing for integumentary conditions that are known to have a genetic component. What assessment question is most appropriate? A) Does anyone in your family have eczema or psoriasis? B) Have any of your family members been diagnosed with malignant melanoma? C) Do you have a family history of vitiligo or port-wine stains? D) Does any member of your family have a history of keloid scarring? A Feedback: Eczema and psoriasis are known to have a genetic component. This is not true of any of the other listed integumentary disorders. 30. A nurse in the emergency department (ED) is triaging a 5-year-old who has been brought to the ED by her parents for an outbreak of urticaria. What would be the most appropriate question to ask this patient and her family? A) Has she eaten any new foods today? B) Has she bathed in the past 24 hours? C) Did she go to a friends house today? D) Was she digging in the dirt today? A Feedback: Foods can cause skin reactions, especially in children. In most cases, this is a more plausible cause of urticaria than bathing, contact with other children, or soil-borne pathogens. 31. A nurse practitioner working in a dermatology clinic finds an open lesion on a patient who is being assessed. What should the nurse do next? A) Obtain a swab for culture. B) Assess the characteristics of the lesion. C) Obtain a swab for pH testing. D) Apply a test dose of broad-spectrum topical antibiotic. B Feedback: If acute open wounds or lesions are found on inspection of the skin, a comprehensive assessment should be made and documented. Testing for culture and pH are not necessarily required, and assessment should precede these actions. Antibiotics are not applied on an empiric basis. 32. The nurse is performing a comprehensive assessment of a patients skin surfaces and intends to assess moisture, temperature, and texture. The nurse should perform this component of assessment in what way? A) By examining the patient under a Woods light B) By inspecting the patients skin in direct sunlight C) By palpating the patients skin D) By performing percussion of major skin surfaces C Feedback: Inspection and palpation are techniques commonly used in examining the skin. A patient would only be examined under a Woods light if there were indications it could be diagnostic. The patient is examined in a well-lit room, not in direct sunlight. Percussion is not a technique used in assessing the skin. 33. A nurse is assessing the skin of a patient who has been diagnosed with bacterial cellulitis on the dorsal portion of the great toe. When reviewing the patients health history, the nurse should identify what comorbidity as increasing the patients vulnerability to skin infections? A) Chronic obstructive pulmonary disease B) Rheumatoid arthritis C) Gout D) Diabetes D Feedback: Patients with diabetes are particularly susceptible to skin infections. COPD, RA, and gout are less commonly associated with integumentary manifestations. 34. A patient with human immunodeficiency virus (HIV) has sought care because of the recent development of new skin lesions. The nurse should interpret these lesions as most likely suggestive of what? A) A reduction in the patients CD4 count B) A reduction in the patients viral load C) An adverse effect of antiretroviral therapy D) Virus-induced changes in allergy status A Feedback: Cutaneous signs may be the first manifestation of human immunodeficiency virus (HIV), appearing in more than 90% of HIV-infected people as immune function deteriorates. These skin signs correlate with low CD4 counts and may become very atypical in immunocompromised people. Viral load increases, not decreases, as the disease progresses. Antiretrovirals are not noted to cause cutaneous changes and viruses do not change an individuals allergy status. 35. Assessment of a patients leg reveals the presence of a 1.5-cm circular region of necrotic tissue that is deeper than the epidermis. The nurse should document the presence of what type of skin lesion? A) Keloid B) Ulcer C) Fissure D) Erosion B Feedback: An ulcer is skin loss extending past the epidermis with the involvement of necrotic tissue. Keloids lack necrosis and consist of scar tissue. A fissure is linear and erosions do not extend to the dermis. 36. A new patient presents at the clinic and the nurse performs a comprehensive health assessment. The nurse notes that the patients fingernail surfaces are pitted. The nurse should suspect the presence of what health problem? A) Eczema B) Systemic lupus erythematosus (SLE) C) Psoriasis D) Chronic obstructive pulmonary disease (COPD) C Feedback: Pitted surface of the nails is a definite indication of psoriasis. Pitting of the nails does not indicate eczema, SLE, or COPD. 37. A patients health assessment has resulted in a diagnosis of alopecia areata. What nursing diagnosis should the nurse most likely associate with this health problem? A) Chronic Pain B) Impaired Skin Integrity C) Impaired Tissue Integrity D) Disturbed Body Image D Feedback: Alopecia areata causes hair loss in smaller defined areas. As such, it is common for the patient to experience a disturbed body image. Hair loss does not cause pain and does not affect skin or tissue integrity. 38. A patient is suspected of developing an allergy to an environmental substance and has been given a patch test. During the test, the patient develops fine blisters, papules, and severe itching. The nurse knows that this is indicative of what strength reaction? A) Weak positive B) Moderately positive C) Strong positive D) Severely positive B Feedback: The development of redness, fine elevations, or itching is considered a weak positive reaction; fine blisters, papules, and severe itching indicate a moderately positive reaction; and blisters, pain, and ulceration indicate a strong positive reaction. 39. A dermatologist has asked the nurse to assist with examination of a patients skin using a Woods light. This test will allow the physician to assess for which of the following? A) The presence of minute regions of keloid scarring B) Unusual patterns of pigmentation on the patients skin C) Vascular lesions that are not visible to the naked eye D) The presence of parasites on the epidermis B Feedback: Woods light makes it possible to differentiate epidermal from dermal lesions and hypopigmented and hyperpigmented lesions from normal skin. 40. A patient presents at the dermatology clinic with suspected herpes simplex. The nurse knows to prepare what diagnostic test for this condition? A) Skin biopsy B) Patch test C) Tzanck smear D) Examination with a Woods light C Feedback: The Tzanck smear is a test used to examine cells from blistering skin conditions, such as herpes zoster, varicella, herpes simplex, and all forms of pemphigus. The secretions from a suspected lesion are applied to a glass slide, stained, and examined. This is not accomplished by biopsy, patch test, or Woods light. Chapter 61: Managements of Patients with Dermatologic Problems 1. A nurse practitioner is seeing a 16-year-old male patient who has come to the dermatology clinic for treatment of acne. The nurse practitioner would know that the treatment may consist of which of the following medications? A) Acyclovir (Zovirax) B) Benzoyl peroxide and erythromycin (Benzamycin) C) Diphenhydramine (Benadryl) D) Triamcinolone (Kenalog) B Feedback: Benzamycin gel is among the topical treatments available for acne. Zovirax is used in the treatment of herpes zoster as an oral antiviral agent. Benadryl is an oral antihistamine used in the treatment of pruritus. Intralesional injections of Kenalog have been utilized in the treatment of psoriasis. 2. A nurse is caring for a patient who has been diagnosed with psoriasis. The nurse is creating an education plan for the patient. What information should be included in this plan? A) Use caution when taking nonprescription medications. B) Avoid public places until symptoms subside. C) Wash skin frequently to prevent infection. D) Liberally apply corticosteroids as needed. A Feedback: The patient should be cautioned about taking nonprescription medications because some may aggravate mild psoriasis. Psoriasis is not contagious. Many patients need reassurance that the condition is not infectious, not a reflection of poor personal hygiene, and not skin cancer. Excessively frequent washing of skin produces more soreness and scaling. Overuse of topical corticosteroids can result in skin atrophy, striae, and medication resistance. 3. A nurse is planning the care of a patient with herpes zoster. What medication, if administered within the first 24 hours of the initial eruption, can arrest herpes zoster? A) Prednisone (Deltasone) B) Azanthioprine (Imuran) C) Triamcinolone (Kenalog) D) Acyclovir (Zovirax) D Feedback: Acyclovir, if started early, is effective in significantly reducing the pain and halting the progression of the disease. There is evidence that infection is arrested if oral antiviral agents are administered within the first 24 hours. Prednisone is an anti-inflammatory agent used in a variety of skin disorders, but not in the treatment of herpes. Azanthioprine is an immunosuppressive agent used in the treatment of pemphigus. Triamcinolone is utilized in the treatment of psoriasis. 4. A patient with squamous cell carcinoma has been scheduled for treatment of this malignancy. The nurse should anticipate that treatment for this type of cancer will primarily consist of what intervention? A) Chemotherapy B) Radiation therapy C) Surgical excision D) Biopsy of sample tissue C Feedback: The primary goal of surgical management of squamous cell carcinoma is to remove the tumor entirely. Radiation therapy is reserved for older patients, because x-ray changes may be seen after 5 to 10 years, and malignant changes in scars may be induced by irradiation 15 to 30 years later. Obtaining a biopsy would not be a goal of treatment; it may be an assessment. Chemotherapy and radiation therapy are generally reserved for patients who are not surgical candidates. 5. When writing a plan of care for a patient with psoriasis, the nurse would know that an appropriate nursing diagnosis for this patient would be what? A) Impaired Skin Integrity Related to Scaly Lesions B) Acute Pain Related to Blistering and Erosions of the Oral Cavity C) Impaired Tissue Integrity Related to Epidermal Shedding D) Anxiety Related to Risk for Melanoma A Feedback: An appropriate diagnosis for a patient with psoriasis would include Impaired Skin Integrity as it relates to scaly lesions. Psoriasis causes pain but does not normally affect the oral cavity. Similarly, tissue integrity is impaired, but not through the process of epidermal shedding. Psoriasis is not related to an increased risk for melanoma. A patient who has sustained third-degree facial burns and a facial fracture is undergoing reconstructive surgery and implantation of a prosthesis. The nurse has identified a nursing diagnosis of Disturbed Body Image Related to Disfigurement. What would be an appropriate nursing intervention related to this diagnosis? A) Referring the patient to a speech therapist B) Gradually adding soft foods to diet C) Administering analgesics as prescribed D) Teaching the patient how to use and care for the prosthesis D Feedback: The process of facial reconstruction is often slow and tedious. Because a persons facial appearance affects self-esteem so greatly, this type of reconstruction is often a very emotional experience for the patient. Reinforcement of the patients successful coping strategies improves self-esteem. If prosthetic devices are used, the patient is taught how to use and care for them to gain a sense of greater independence. This is an intervention that relates to Disturbed Body Image in these patients. None of the other listed interventions relates directly to the diagnosis of Disturbed Body Image. 7. While performing an initial assessment of a patient admitted with appendicitis, the nurse observes an elevated blue-black lesion on the patients ear. The nurse knows that this lesion is consistent with what type of skin cancer? A) Basal cell carcinoma B) Squamous cell carcinoma C) Dermatofibroma D) Malignant melanoma D Feedback: A malignant melanoma presents itself as a superficial spreading melanoma which may appear in a combination of colors, with hues of tan, brown, and black mixed with gray, blue-black, or white. The lesion tends to be circular, with irregular outer portions. BCC usually begins as a small, waxy nodule with rolled, translucent, pearly borders; telangiectatic vessels may be present. SCC appears as a rough, thickened, scaly tumor that may be asymptomatic or may involve bleeding. A dermatofibroma presents as a firm, dome-shaped papule or nodule that may be skin colored or pinkish-brown. 8. A nurse is providing care for a patient who has developed Kaposis sarcoma secondary to HIV infection. The nurse should be aware that this form of malignancy originates in what part of the body? A) Connective tissue cells in diffuse locations B) Smooth muscle cells of the gastrointestinal and respiratory tract C) Neural tissue of the brain and spinal cord D) Endothelial cells lining small blood vessels D Feedback: Kaposis sarcoma (KS) is a malignancy of endothelial cells that line the small blood vessels. It does not originate in connective tissue, smooth muscle cells of the GI and respiratory tract, or in neural tissue. 9. A patient requires a full-thickness graft to cover a chronic wound. How is the donor site selected? A) The largest area of the body without hair is selected. B) Any area that is not normally visible can be used. C) An area matching the color and texture of the skin at the surgical site is selected. D) An area matching the sensory capability of the skin at the surgical site is selected. C Feedback: The site where the intact skin is harvested is called the donor site. Selection of the donor site is made to match the color and texture of skin at the surgical site and to leave as little scarring as possible. 10. A patient has just been told that he has malignant melanoma. The nurse caring for this patient should anticipate that the patient will undergo what treatment? A) Chemotherapy B) Immunotherapy C) Wide excision D) Radiation therapy C Feedback: Wide excision is the primary treatment for malignant melanoma, which removes the entire lesion and determines the level and staging. Chemotherapy may be used after the melanoma is excised. Immunotherapy is experimental and radiation therapy is palliative. 11. A nurse is leading a health promotion workshop that is focusing on cancer prevention. What action is most likely to reduce participants risks of basal cell carcinoma (BCC)? A) Teaching participants to improve their overall health through nutrition B) Encouraging participants to identify their family history of cancer C) Teaching participants to limit their sun exposure D) Teaching participants to control exposure to environmental and occupational radiation C Feedback: Sun exposure is the best known and most common cause of BCC. BCC is not commonly linked to general health debilitation, family history, or radiation exposure. 12. A patient diagnosed with a stasis ulcer has been hospitalized. There is an order to change the dressing and provide wound care. Which activity should the nurse first perform when providing wound care? A) Assess the drainage in the dressing. B) Slowly remove the soiled dressing. C) Perform hand hygiene. D) Don non-latex gloves. C Feedback: The nurse and physician must adhere to standard precautions and wear gloves when inspecting the skin or changing a dressing. Use of standard precautions and proper disposal of any contaminated dressing is carried out according to Occupational Safety and Health Administration (OSHA) regulations. Hand hygiene must precede other aspects of wound care. 13. A patient comes to the clinic complaining of a red rash of small, fluid-filled blisters and is suspected of having herpes zoster. What presentation is most consistent with herpes zoster? A) Grouped vesicles occurring on lips and oral mucous membranes B) Grouped vesicles occurring on the genitalia C) Rough, fresh, or gray skin protrusions D) Grouped vesicles in linear patches along a dermatome D Feedback: Herpes zoster, or shingles, is an acute inflammation of the dorsal root ganglia, causing localized, vesicular skin lesions following a dermatome. Herpes simplex type 1 is a viral infection affecting the skin and mucous membranes, usually producing cold sores or fever blisters. Herpes simplex type 2 primarily affects the genital area, causing painful clusters of small ulcerations. Warts appear as rough, fresh, or gray skin protrusions. 14. A patient with a chronic diabetic wound is being discharged after receiving a skin graft to aid wound healing. What direction should the nurse include in home care instructions? A) Gently massage the graft site daily to promote perfusion. B) Protect the graft from direct sunlight and temperature extremes. C) Protect the graft site from any form of moisture for at least 12 weeks. D) Apply antibiotic ointment to the graft site and donor site daily. B Feedback: Both the donor site and the grafted area must be protected from exposure to extremes in temperature, external trauma, and sunlight because these areas are sensitive, especially to thermal injuries. Antibiotic ointments are not typically prescribed and massage may damage these fragile sites. There is no need to protect the sites from all forms of moisture for the long term. A patient presents at the free clinic with a black, wart-like lesion on his face, stating, Ive done some research, and Im pretty sure I have malignant melanoma. Subsequent diagnostic testing results in a diagnosis of seborrheic keratosis. The nurse should recognize what significance of this diagnosis? A) The patient requires no treatment unless he finds the lesion to be cosmetically unacceptable. B) The patients lesion will be closely observed for 6 months before a plan of treatment is chosen. C) The patient has one of the few dermatologic malignancies that respond to chemotherapy. D) The patient will likely require wide excision. A Feedback: Seborrheic keratoses are benign, wart like lesions of various sizes and colors, ranging from light tan to black. There is no harm in allowing these growths to remain because there is no medical significance to their presence. 16. A nurse is providing care for a patient who has psoriasis. The nurse is aware of the sequelae that can result from this health problem. Following the appearance of skin lesions, the nurse should prioritize what assessment? A) Assessment of the patients stool for evidence of intestinal sloughing B) Assessment of the patients apical heart rate for dysrhythmias C) Assessment of the patients joints for pain and decreased range of motion D) Assessment for cognitive changes resulting from neurologic lesions C Feedback: Asymmetric rheumatoid factornegative arthritis of multiple joints occurs in up to 30% of people with psoriasis, most typically after the skin lesions appear. The most typical joints affected include those in the hands or feet, although sometimes larger joints such as the elbow, knees, or hips may be affected. As such, the nurse should assess for this musculoskeletal complication. GI, cardiovascular, and neurologic function are not affected by psoriasis. 17. A patient is admitted to the intensive care unit with what is thought to be toxic epidermal necrolysis (TEN). When assessing the health history of the patient, the nurse would be alert to what precipitating factor? A) Recent heavy ultraviolet exposure B) Substandard hygienic conditions C) Recent administration of new medications D) Recent varicella infection C Feedback: In adults, TEN is usually triggered by a reaction to medications. Antibiotics, antiseizure agents, butazones, and sulfonamides are the most frequent medications implicated. TEN is unrelated to UV exposure, hygiene, or varicella infection. 18. A patient has received a diagnosis of irritant contact dermatitis. What action should the nurse prioritize in the patients subsequent care? A) Teaching the patient to safely and effectively administer immunosuppressants B) Helping the patient identify and avoid the offending agent C) Teaching the patient how to maintain meticulous skin hygiene D) Helping the patient perform wound care in the home environment B Feedback: A focus of care for patients with irritant contact dermatitis is identifying and avoiding the offending agent. Immunosuppressants are not used to treat eczema and wound care is not normally required, except in cases of open lesions. Poor hygiene has no correlation with contact dermatitis. 19. A nurse is caring for a patient whose chemical injury has necessitated a skin graft to his left hand. The nurse enters the room and observes that the patient is performing active range of motion (ROM) exercises with the affected hand. How should the nurse best respond? A) Liaise with the physical therapist to ensure that the patient is performing exercises safely. B) Validate the patients efforts to increase blood perfusion to the graft site. C) Remind the patient that ROM exercises should be passive, not active. D) Remind the patient of the need to immobilize the graft to facilitate healing. D Feedback: The nurse should instruct the patient to keep the affected part immobilized as much as possible in order to facilitate healing. Passive ROM exercises can be equally as damaging as active ROM. A school nurse has sent home four children who show evidence of pediculosis capitis. What is an important instruction the nurse should include in the note being sent home to parents? A) The childs scalp should be monitored for 48 to 72 hours before starting treatment. B) Nits may have to be manually removed from the childs hair shafts. C) The disease is self-limiting and symptoms will abate within 1 week. D) Efforts should be made to improve the childs level of hygiene. B Feedback: Treatment for head lice should begin promptly and may require manual removal of nits following medicating shampoo. Head lice are not related to a lack of hygiene. Treatment is necessary because the condition will not likely resolve spontaneously within 1 week. 21. A patient has just been diagnosed with psoriasis and frequently has lesions around his right eye. What should the nurse teach the patient about topical corticosteroid use on these lesions? A) Cataract development is possible. B) The ointment is likely to cause weeping. C) Corticosteroid use is contraindicated on these lesions. D) The patient may develop glaucoma. A Feedback: Patients using topical corticosteroid preparations repeatedly on the face and around the eyes should be aware that cataract development is possible. Weeping and glaucoma are less likely. There is no consequent risk of glaucoma. 22. A nurse is caring for a patient who has a diagnosis of bullous pemphigoid and who is being treated on the medical unit. When providing hygiene for this patient, the nurse should perform which of the following actions? A) After washing, wipe lesions with sterile gauze to remove cellular debris. B) Apply antibiotic ointment to lesions after washing. C) Apply cornstarch to the patients skin after bathing to facilitate mobility. D) Avoid using water to cleanse the patients skin in order to maintain skin integrity. C Feedback: After the patients skin is bathed, it is dried carefully and dusted liberally with nonirritating powder (e.g., cornstarch), which enables the patient to move about freely in bed. Open blisters should not normally be wiped and antibiotics are not applied to wound beds in the absence of a secondary infection. Water can safely be used to provide hygiene. A nurse is caring for a patient admitted to the medical unit with a diagnosis of pemphigus vulgaris. When writing the care plan for this patient, what nursing diagnoses should be included? Select all that apply. A) Risk for Infection Related to Lesions B) Impaired Skin Integrity Related to Epidermal Blisters C) Disturbed Body Image Related to Presence of Skin Lesions D) Acute Pain Related to Disruption in Skin Integrity E) Hyperthermia Related to Disruptions in Thermoregulation A, B, C, D Feedback: Blistering diseases disrupt skin integrity and are associated with pain and a risk for infection. Because of the visibility of blisters, body image is often affected. The patient faces a risk for hypothermia, not hyperthermia. 24. A patients blistering disorder has resulted in the formation of multiple lesions in the patients mouth. What intervention should be included in the patients plan of care? A) Provide chlorhexidine solution for rinsing the patients mouth. B) Avoid providing regular mouth care until the patients lesions heal. C) Liaise with the primary care provider to arrange for parenteral nutrition. D) Encourage the patient to gargle with a hypertonic solution after each meal. A Feedback: Frequent rinsing of the mouth with chlorhexidine solution is prescribed to rid the mouth of debris and to soothe ulcerated areas. A hypertonic solution would be likely to cause pain and further skin disruption. Meticulous mouth care should be provided and there is no reason to provide nutrition parenterally. 25. When caring for a patient with toxic epidermal necrolysis (TEN), the critical care nurse assesses frequently for high fever, tachycardia, and extreme weakness and fatigue. The nurse is aware that these findings are potential indicators of what? Select all that apply. A) Possible malignancy B) Epidermal necrosis C) Neurologic involvement D) Increased metabolic needs E) Possible gastrointestinal mucosal sloughing B, D, E Feedback: Assessment for high fever, tachycardia, and extreme weakness and fatigue is essential because these factors indicate the process of epidermal necrosis, increased metabolic needs, and possible gastrointestinal and respiratory mucosal sloughing. These factors are less likely to suggest malignancy or neurologic involvement, as these are not common complications of TEN. 26. A nurse is assessing a teenage patient with acne vulgaris. The patients mother states, I keep telling him that this is what happens when you eat as much chocolate as he does. What aspect of the pathophysiology of acne should inform the nurses response? A) A sudden change in patients diet may exacerbate, rather than alleviate, the patients symptoms. B) Chocolate is not among the foods that are known to cause acne. C) Elimination of chocolate from the patients diet will likely lead to resolution within several months. D) Diet is thought to play a minimal role in the development of acne. D Feedback: Diet is not believed to play a major role in acne therapy. A change in diet is not known to exacerbate symptoms. 27. A nurse is providing self-care education to a patient who has been receiving treatment for acne vulgaris. What instruction should the nurse provide to the patient? A) Wash your face with water and gentle soap each morning and evening. B) Before bedtime, clean your face with rubbing alcohol on a cotton pad. C) Gently burst new pimples before they form a visible head. D) Set aside time each day to squeeze blackheads and remove the plug. A Feedback: The nurse should inform the patient to wash the face and other affected areas with mild soap and water twice each day to remove surface oils and prevent obstruction of the oil glands. Cleansing with rubbing alcohol is not recommended and all forms of manipulation should be avoided. 28. A nurse is caring for a patient whose skin cancer will soon be removed by excision. Which of the following actions should the nurse perform? A) Teach the patient about early signs of secondary blistering diseases. B) Teach the patient about self-care after treatment. C) Assess the patients risk for recurrent malignancy. D) Assess the patient for adverse effects of radiotherapy. B Feedback: Because many skin cancers are removed by excision, patients are usually treated in outpatient surgical units. The role of the nurse is to teach the patient about prevention of skin cancer and about self-care after treatment. Assessing the patients risk for recurrent malignancy is primarily the role of the physician. Blistering diseases do not result from cancer or subsequent excision. Excision is not accompanied by radiotherapy. 29. A patient has just undergone surgery for malignant melanoma. Which of the following nursing actions should be prioritized? A) Maintain the patient on bed rest for the first 24 hours postoperative. B) Apply distraction techniques to relieve pain. C) Provide soft or liquid diet that is high in protein to assist with healing. D) Anticipate the need for, and administer, appropriate analgesic medications. D Feedback: Nursing interventions after surgery for a malignant melanoma center on promoting comfort, because wide excision surgery may be necessary. Anticipating the need for and administering appropriate analgesic medications are important. Distraction techniques may be appropriate for some patients, but these are not a substitute for analgesia. Bed rest and a modified diet are not necessary. 30. A patient has recently been diagnosed with advanced malignant melanoma and is scheduled for a wide excision of the tumor on her chest. In writing the plan of care for this patient, what major nursing diagnosis should the nurse include? A) Deficient Knowledge about Early Signs of Melanoma B) Chronic Pain Related to Surgical Excision and Grafting C) Depression Related to Reconstructive Surgery D) Anxiety Related to Lack of Social Support A Feedback: The fact that the patients disease was not reported until an advanced stage suggests that the patient lacked knowledge about skin lesions. Excision does not result in chronic pain. Reconstructive surgery is not a certainty, and will not necessarily lead to depression. Anxiety is likely, but this may or may not be related to a lack of social support. 31. A nurse educator is teaching a group of medical nurses about Kaposis sarcoma. What would the educator identify as characteristics of endemic Kaposis sarcoma? Select all that apply. A) Affects people predominantly in the eastern half of Africa B) Affects men more than women C) Does not affect children D) Cannot infiltrate E) Can progress to lymphadenopathic forms A, B, E Feedback: Endemic (African) Kaposis sarcoma affects people predominantly in the eastern half of Africa, near the equator. Men are affected more often than women, and children can be affected as well. The disease may resemble classic KS or it may infiltrate and progress to lymphadenopathic forms. 32. A 35-year-old kidney transplant patient comes to the clinic exhibiting new skin lesions. The diagnosis is Kaposis sarcoma. The nurse caring for this patient recognizes that this is what type of Kaposis sarcoma? A) Classic B) AIDS-related C) Immunosuppression-related D) Endemic C Feedback: Immunosuppression-associated Kaposis sarcoma occurs in transplant recipients and people with AIDS. This form of KS is characterized by local skin lesions and disseminated visceral and mucocutaneous diseases. Classic Kaposis sarcoma occurs predominantly in men of Mediterranean or Jewish ancestry between 40 and 70 years of age. Endemic KS affects people predominantly in the eastern half of Africa. AIDS-related KS is seen in people with AIDS. 33. A 65-year-old man presents at the clinic complaining of nodules on both legs. The man tells the nurse that his son, who is in medical school, encouraged him to seek prompt care and told him that the nodules are related to the fact that he is Jewish. What health problem should the nurse suspect? A) Stasis ulcers B) Bullous pemphigoid C) Psoriasis D) Classic Kaposis sarcoma D Feedback: Classic Kaposis sarcoma occurs predominantly in men of Mediterranean or Jewish ancestry between 40 and 70 years of age. Most patients have nodules or plaques on the lower extremities that rarely metastasize beyond this area. Classic KS is chronic, relatively benign, and rarely fatal. Stasis ulcers do not create nodules. Bullous pemphigoid is characterized by blistering. Psoriasis characteristically presents with silvery plaques. 34. A 55-year-old woman is scheduled to have a chemical face peel. The nurse is aware that the patient is likely seeking treatment for which of the following? A) Wrinkles near the lips and eyes B) Removal of acne scars C) Vascular lesions on the cheeks D) Real or perceived misshaping of the eyes A Feedback: Chemical face peeling is especially useful for wrinkles at the upper and lower lip, forehead, and periorbital areas. Chemical face peeling does not remove acne scars, remove vascular lesions, or reshape the eyes. 35. A patient comes to the dermatology clinic requesting the removal of a port-wine stain on his right cheek. The nurse knows that the procedure especially useful in treating cutaneous vascular lesions such as port- wine stains is what? A) Skin graft B) Laser treatment C) Chemical face peeling D) Free flap B Feedback: Argon lasers are useful in treating cutaneous vascular lesions such as port-wine stains. Skin grafts, chemical face peels, and free flaps would not be used to remove a port-wine stain. A 30-year-old male patient has just returned from the operating room after having a flap done following a motorcycle accident. The patients wife asks the nurse about the major complications following this type of surgery. What would be the nurses best response? A) The major complication is when the patient develops chronic pain. B) The major complication is when the patient loses sensation in the flap. C) The major complication is when the pedicle tears loose and the flap dies. D) The major complication is when the blood supply fails and the tissue in the flap dies. D Feedback: The major complication of a flap is necrosis of the pedicle or base as a result of failure of the blood supply. This is more likely than tearing of the pedicle and chronic pain and is more serious than loss of sensation. 37. A public health nurse is participating in a health promotion campaign that has the goal of improving outcomes related to skin cancer in the community. What action has the greatest potential to achieve this goal? A) Educating participants about the relationship between general health and the risk of skin cancer B) Educating participants about treatment options for skin cancer C) Educating participants about the early signs and symptoms of skin cancer D) Educating participants about the health risks associated with smoking and assisting with smoking cessation C Feedback: The best hope of decreasing the incidence of skin cancer lies in educating patients about the early signs. There is a relationship between general health and skin cancer, but teaching individuals to identify the early signs and symptoms is more likely to benefit overall outcomes related to skin cancer. Teaching about treatment options is not likely to have a major effect on outcomes of the disease. Smoking is not among the major risk factors for skin cancer. 38. An older adult resident of a long-term care facility has been experiencing generalized pruritus that has become more severe in recent weeks. What intervention should the nurse add to this residents plan of care? A) Avoid the application of skin emollients. B) Apply antibiotic ointment as ordered following baths. C) Avoid using hot water during the patients baths. D) Administer acetaminophen 4 times daily as ordered. C Feedback: If baths have been prescribed, the patient is reminded to use tepid (not hot) water and to shake off the excess water and blot between intertriginous areas (body folds) with a towel. Skin emollients should be applied to reduce pruritus. Acetaminophen and antibiotics do not reduce pruritus. 39. A patient has a diagnosis of seborrhea and has been referred to the dermatology clinic, where the nurse contributes to care. When planning this patients care, the nurse should include which of the following nursing diagnoses? A) Risk for Deficient Fluid Volume Related to Excess Sebum Synthesis B) Ineffective Thermoregulation Related to Occlusion of Sebaceous Glands C) Disturbed Body Image Related to Excess Sebum Production D) Ineffective Tissue Perfusion Related to Occlusion of Sebaceous Glands C Feedback: Seborrhea causes highly visible manifestations that are likely to have a negative effect on the patients body image. Seborrhea does not normally affect fluid balance, thermoregulation, or tissue perfusion. 40. A nurse is working with a family whose 5 year-old daughter has been diagnosed with impetigo. What educational intervention should the nurse include in this familys care? A) Ensuring that the family knows that impetigo is not contagious B) Teaching about the safe and effective use of topical corticosteroids C) Teaching about the importance of maintaining high standards of hygiene D) Ensuring that the family knows how to safely burst the childs vesicles C Feedback: Impetigo is associated with unhygienic conditions; educational interventions to address this are appropriate. The disease is contagious, thus vesicles should not be manually burst. Because of the bacterial etiology, corticosteroids are ineffective. Chapter 62: Managements of Patients with Burn Injury 1. A patient is brought to the emergency department from the site of a chemical fire, where he suffered a burn that involves the epidermis, dermis, and the muscle and bone of the right arm. On inspection, the skin appears charred. Based on these assessment findings, what is the depth of the burn on the patients arm? A) Superficial partial-thickness B) Deep partial-thickness C) Full partial-thickness D) Full-thickness D Feedback: A full-thickness burn involves total destruction of the epidermis and dermis and, in some cases, underlying tissue as well. Wound color ranges widely from white to red, brown, or black. The burned area is painless because the nerve fibers are destroyed. The wound can appear leathery; hair follicles and sweat glands are destroyed. Edema may also be present. Superficial partial-thickness burns involve the epidermis and possibly a portion of the dermis; the patient will experience pain that is soothed by cooling. Deep partial-thickness burns involve the epidermis, upper dermis, and portion of the deeper dermis; the patient will complain of pain and sensitivity to cold air. Full partial thickness is not a depth of burn. 2. The current phase of a patients treatment for a burn injury prioritizes wound care, nutritional support, and prevention of complications such as infection. Based on these care priorities, the patient is in what phase of burn care? A) Emergent B) Immediate resuscitative C) Acute D) Rehabilitation C Feedback: The acute or intermediate phase of burn care follows the emergent/resuscitative phase and begins 48 to 72 hours after the burn injury. During this phase, attention is directed toward continued assessment and maintenance of respiratory and circulatory status, fluid and electrolyte balance, and gastrointestinal function. Infection prevention, burn wound care (i.e., wound cleaning, topical antibacterial therapy, wound dressing, dressing changes, wound dbridement, and wound grafting), pain management, and nutritional support are priorities at this stage. Priorities during the emergent or immediate resuscitative phase include first aid, prevention of shock and respiratory distress, detection and treatment of concomitant injuries, and initial wound assessment and care. The priorities during the rehabilitation phase include prevention of scars and contractures, rehabilitation, functional and cosmetic reconstruction, and psychosocial counseling. 3. A patient in the emergent/resuscitative phase of a burn injury has had blood work and arterial blood gases drawn. Upon analysis of the patients laboratory studies, the nurse will expect the results to indicate what? A) Hyperkalemia, hyponatremia, elevated hematocrit, and metabolic acidosis B) Hypokalemia, hypernatremia, decreased hematocrit, and metabolic acidosis C) Hyperkalemia, hypernatremia, decreased hematocrit, and metabolic alkalosis D) Hypokalemia, hyponatremia, elevated hematocrit, and metabolic alkalosis A Feedback: Fluid and electrolyte changes in the emergent/resuscitative phase of a burn injury include hyperkalemia related to the release of potassium into the extracellular fluid, hyponatremia from large amounts of sodium lost in trapped edema fluid, hemoconcentration that leads to an increased hematocrit, and loss of bicarbonate ions that results in metabolic acidosis. 4. A patient has experienced an electrical burn and has developed thick eschar over the burn site. Which of the following topical antibacterial agents will the nurse expect the physician to order for the wound? A) Silver sulfadiazine 1% (Silvadene) water-soluble cream B) Mafenide acetate 10% (Sulfamylon) hydrophilic-based cream C) Silver nitrate 0.5% aqueous solution D) Acticoat B Feedback: Mafenide acetate 10% hydrophilic-based cream is the agent of choice when there is a need to penetrate thick eschar. Silver products do not penetrate eschar; Acticoat is a type of silver dressing. 5. An occupational health nurse is called to the floor of a factory where a worker has sustained a flash burn to the right arm. The nurse arrives and the flames have been extinguished. The next step is to cool the burn. How should the nurse cool the burn? A) Apply ice to the site of the burn for 5 to 10 minutes. B) Wrap the patients affected extremity in ice until help arrives. C) Apply an oil-based substance or butter to the burned area until help arrives. D) Wrap cool towels around the affected extremity intermittently. D Feedback: Once the burn has been sustained, the application of cool water is the best first-aid measure. Soaking the burn area intermittently in cool water or applying cool towels gives immediate and striking relief from pain, and limits local tissue edema and damage. However, never apply ice directly to the burn, never wrap the person in ice, and never use cold soaks or dressings for longer than several minutes; such procedures may worsen the tissue damage and lead to hypothermia in people with large burns. Butter is contraindicated. 6. An emergency department nurse has just admitted a patient with a burn. What characteristic of the burn will primarily determine whether the patient experiences a systemic response to this injury? A) The length of time since the burn B) The location of burned skin surfaces C) The source of the burn D) The total body surface area (TBSA) affected by the burn D Feedback: Systemic effects are a result of several variables. However, TBSA and wound severity are considered the major factors that affect the presence or absence of systemic effects. 7. A nurse on a burn unit is caring for a patient in the acute phase of burn care. While performing an assessment during this phase of burn care, the nurse recognizes that airway obstruction related to upper airway edema may occur up to how long after the burn injury? A) 2 days B) 3 days C) 5 days D) 1 week A Feedback: Airway obstruction caused by upper airway edema can take as long as 48 hours to develop. Changes detected by x-ray and arterial blood gases may occur as the effects of resuscitative fluid and the chemical reaction of smoke ingredients with lung tissues become apparent. 8. A patient has sustained a severe burn injury and is thought to have an impaired intestinal mucosal barrier. Since this patient is considered at an increased risk for infection, what intervention will best assist in avoiding increased intestinal permeability and prevent early endotoxin translocation? A) Early enteral feeding B) Administration of prophylactic antibiotics C) Bowel cleansing procedures D) Administration of stool softeners A Feedback: If the intestinal mucosa receives some type of protection against permeability change, infection could be avoided. Early enteral feeding is one step to help avoid this increased intestinal permeability and prevent early endotoxin translocation. Antibiotics are seldom prescribed prophylactically because of the risk of promoting resistant strains of bacteria. A bowel cleansing procedure would not be ordered for this patient. The administration of stool softeners would not assist in avoiding increased intestinal permeability and prevent early endotoxin translocation. 9. A patient has been admitted to a burn intensive care unit with extensive full-thickness burns over 25% of the body. After ensuring cardiopulmonary stability, what would be the nurses immediate, priority concern when planning this patients care? A) Fluid status B) Risk of infection C) Nutritional status D) Psychosocial coping A Feedback: During the early phase of burn care, the nurse is most concerned with fluid resuscitation, to correct large-volume fluid loss through the damaged skin. Infection control and early nutritional support are important, but fluid resuscitation is an immediate priority. Coping is a higher priority later in the recovery period. 10. The nurse is preparing the patient for mechanical dbridement and informs the patient that this will involve which of the following procedures? A) A spontaneous separation of dead tissue from the viable tissue B) Removal of eschar until the point of pain and bleeding occurs C) Shaving of burned skin layers until bleeding, viable tissue is revealed D) Early closure of the wound B Feedback: Mechanical dbridementcan be achieved through the use of surgical scissors, scalpels, or forceps to remove the eschar until the point of pain and bleeding occurs. Mechanical dbridement can also be accomplished through the use of topical enzymatic dbridement agents. The spontaneous separation of dead tissue from the viable tissue is an example of natural dbridement. Shaving the burned skin layers and early wound closure are examples of surgical dbridement. 11. A patient with a partial-thickness burn injury had Biobrane applied 2 weeks ago. The nurse notices that the Biobrane is separating from the burn wound. What is the nurses most appropriate intervention? A) Reinforce the Biobrane dressing with another piece of Biobrane. B) Remove the Biobrane dressing and apply a new dressing. C) Trim away the separated Biobrane. D) Notify the physician for further emergency-related orders. C Feedback: As the Biobrane gradually separates, it is trimmed, leaving a healed wound. When the Biobrane dressing adheres to the wound, the wound remains stable and the Biobrane can remain in place for 3 to 4 weeks. There is no need to reinforce the Biobrane nor to remove it and apply a new dressing. There is not likely any need to notify the physician for further orders. 12. An emergency department nurse learns from the paramedics that they are transporting a patient who has suffered injury from a scald from a hot kettle. What variables will the nurse consider when determining the depth of burn? A) The causative agent B) The patients preinjury health status C) The patients prognosis for recovery D) The circumstances of the accident A Feedback: The following factors are considered in determining the depth of a burn: how the injury occurred, causative agent (such as flame or scalding liquid), temperature of the burning agent, duration of contact with the agent, and thickness of the skin. The patients preinjury status, circumstances of the accident, and prognosis for recovery are important, but are not considered when determining the depth of the burn. 13. A nurse is caring for a patient who has sustained a deep partial-thickness burn injury. In prioritizing the nursing diagnoses for the plan of care, the nurse will give the highest priority to what nursing diagnosis? A) Activity Intolerance B) Anxiety C) Ineffective Coping D) Acute Pain D Feedback: Pain is inevitable during recovery from any burn injury. Pain in the burn patient has been described as one of the most severe causes of acute pain. Management of the often-severe pain is one of the most difficult challenges facing the burn team. While the other nursing diagnoses listed are valid, the presence of pain may contribute to these diagnoses. Management of the patients pain is the priority, as it may have a direct correlation to the other listed nursing diagnoses. 14. A triage nurse in the emergency department (ED) receives a phone call from a frantic father who saw his 4-year-old child tip a pot of boiling water onto her chest. The father has called an ambulance. What would the nurse in the ED receiving the call instruct the father to do? A) Cover the burn with ice and secure with a towel. B) Apply butter to the area that is burned. C) Immerse the child in a cool bath. D) Avoid touching the burned area under any circumstances. C Feedback: After the flames or heat source have been removed or extinguished, the burned area and adherent clothing are soaked with cool water briefly to cool the wound and halt the burning process. Cool water is the best first-aid measure. Ice and butter are contraindicated. Appropriate first aid necessitates touching the burn. 15. A nurse is teaching a patient with a partial-thickness wound how to wear his elastic pressure garment. How would the nurse instruct the patient to wear this garment? A) 4 to 6 hours a day for 6 months B) During waking hours for 2 to 3 months after the injury C) Continuously D) At night while sleeping for a year after the injury C Feedback: Elastic pressure garments are worn continuously (i.e., 23 hours a day). 16. A patient is brought to the ED by paramedics, who report that the patient has partial-thickness burns on the chest and legs. The patient has also suffered smoke inhalation. What is the priority in the care of a patient who has been burned and suffered smoke inhalation? A) Pain B) Fluid balance C) Anxiety and fear D) Airway management D Feedback: Systemic threats from a burn are the greatest threat to life. The ABCs of all trauma care apply during the early postburn period. While all options should be addressed, pain, fluid balance, and anxiety and fear do not take precedence over airway management. 17. A patient arrives in the emergency department after being burned in a house fire. The patients burns cover the face and the left forearm. What extent of burns does the patient most likely have? A) 13% B) 25% C) 9% D) 18% D Feedback: When estimating the percentage of body area or burn surface area that has been burned, the Rule of Nines is used: the face is 9%, and the forearm is 9% for a total of 18% in this patient. 18. A nurse is caring for a patient in the emergent/resuscitative phase of burn injury. During this phase, the nurse should monitor for evidence of what alteration in laboratory values? A) Sodium deficit B) Decreased prothrombin time (PT) C) Potassium deficit D) Decreased hematocrit A Feedback: Anticipated fluid and electrolyte changes that occur during the emergent/resuscitative phase of burn injury include sodium deficit, potassium excess, base-bicarbonate deficit, and elevated hematocrit. PT does not typically decrease. 19. A nurse is developing a care plan for a patient with a partial-thickness burn, and determines that an appropriate goal is to maintain position of joints in alignment. What is the best rationale for this intervention? A) To prevent neuropathies B) To prevent wound breakdown C) To prevent contractures D) To prevent heterotopic ossification C Feedback: To prevent the complication of contractures, the nurse will establish a goal to maintain position of joints in alignment. Gentle range of motion exercises and a consult to PT and OT for exercises and positioning recommendations are also appropriate interventions for the prevention of contractures. Joint alignment is not maintained specifically for preventing neuropathy, wound breakdown, or heterotopic ossification. 20. A patients burns have required a homograft. During the nurses most recent assessment, the nurse observes that the graft is newly covered with purulent exudate. What is the nurses most appropriate response? A) Perform mechanical dbridement to remove the exudate and prevent further infection. B) Inform the primary care provider promptly because the graft may need to be removed. C) Perform range of motion exercises to increase perfusion to the graft site and facilitate healing. D) Document this finding as an expected phase of graft healing. B Feedback: An infected graft may need to be removed, thus the care provider should be promptly informed. ROM exercises will not resolve this problem and the nurse would not independently perform dbridement. A nurse who is taking care of a patient with burns is asked by a family member why the patient is losing so much weight. The patient is currently in the intermediate phase of recovery. What would be the nurses most appropriate response to the family member? A) Hes on a calorie-restricted diet in order to divert energy to wound healing. B) His body has consumed his fat deposits for fuel because his calorie intake is lower than normal. C) He actually hasnt lost weight. Instead, theres been a change in the distribution of his body fat. D) He lost many fluids while he was being treated in the emergency phase of burn care. B Feedback: Patients lose a great deal of weight during recovery from severe burns. Reserve fat deposits are catabolized as a result of hypermetabolism. Patients are not placed on a calorie restriction during recovery and fluid losses would not account for weight loss later in the recovery period. Changes in the overall distribution of body fat do not occur. 22. A nurse has reported for a shift at a busy burns and plastics unit in a large university hospital. Which patient is most likely to have life-threatening complications? A) A 4-year-old scald victim burned over 24% of the body B) A 27-year-old male burned over 36% of his body in a car accident C) A 39-year-old female patient burned over 18% of her body D) A 60-year-old male burned over 16% of his body in a brush fire A Feedback: Young children and the elderly continue to have increased morbidity and mortality when compared to other age groups with similar injuries and present a challenge for burn care. This is an important factor when determining the severity of injury and possible outcome for the patient. 23. A patient is brought to the emergency department with a burn injury. The nurse knows that the first systemic event after a major burn injury is what? A) Hemodynamic instability B) Gastrointestinal hypermotility C) Respiratory arrest D) Hypokalemia A Feedback: The initial systemic event after a major burn injury is hemodynamic instability, which results from loss of capillary integrity and a subsequent shift of fluid, sodium, and protein from the intravascular space into the interstitial spaces. This precedes GI changes. Respiratory arrest may or may not occur, largely depending on the presence or absence of smoke inhalation. Hypokalemia does not take place in the initial phase of recovery. 24. A patient with severe burns is admitted to the intensive care unit to stabilize and begin fluid resuscitation before transport to the burn center. The nurse should monitor the patient closely for what signs of the onset of burn shock? A) Confusion B) High fever C) Decreased blood pressure D) Sudden agitation C Feedback: As fluid loss continues and vascular volume decreases, cardiac output continues to decrease and the blood pressure drops, marking the onset of burn shock. Shock and the accompanying hemodynamic changes are not normally accompanied by confusion, fever, or agitation. 25. An emergency department nurse has just received a patient with burn injuries brought in by ambulance. The paramedics have started a large-bore IV and covered the burn in cool towels. The burn is estimated as covering 24% of the patients body. How should the nurse best address the pathophysiologic changes resulting from major burns during the initial burn-shock period? A) Administer IV fluids B) Administer broad-spectrum antibiotics C) Administer IV potassium chloride D) Administer packed red blood cells A Feedback: Pathophysiologic changes resulting from major burns during the initial burn-shock period include massive fluid losses. Addressing these losses is a major priority in the initial phase of treatment. Antibiotics and PRBCs are not normally administered. Potassium chloride would exacerbate the patients hyperkalemia. 26. A patients burns are estimated at 36% of total body surface area; fluid resuscitation has been ordered in the emergency department. After establishing intravenous access, the nurse should anticipate the administration of what fluid? A) 0.45% NaCl with 20 mEq/L KCl B) 0.45% NaCl with 40 mEq/L KCl C) Normal saline D) Lactated Ringers D Feedback: Fluid resuscitation with lactated Ringers (LR) should be initiated using the American Burn Associations (ABA) fluid resuscitation formulas. LR is the crystalloid of choice because its composition and osmolality most closely resemble plasma and because use of normal saline is associated with hyperchloremic acidosis. Potassium chloride solutions would exacerbate the hyperkalemia that occurs following burn injuries. 27. A patient is admitted to the burn unit after being transported from a facility 1000 miles away. The patient has burns to the groin area and circumferential burns to both upper thighs. When assessing the patients legs distal to the wound site, the nurse should be cognizant of the risk of what complication? A) Ischemia B) Referred pain C) Cellulitis D) Venous thromboembolism (VTE) A Feedback: As edema increases, pressure on small blood vessels and nerves in the distal extremities causes an obstruction of blood flow and consequent ischemia. This complication is similar to compartment syndrome. Referred pain, cellulitis, and VTE are not noted complications that occur distal to the injury site. 28. A patient experienced a 33% TBSA burn 72 hours ago. The nurse observes that the patients hourly urine output has been steadily increasing over the past 24 hours. How should the nurse best respond to this finding? A) Obtain an order to reduce the rate of the patients IV fluid infusion. B) Report the patients early signs of acute kidney injury (AKI). C) Recognize that the patient is experiencing an expected onset of diuresis. D) Administer sodium chloride as ordered to compensate for this fluid loss. C Feedback: As capillaries regain integrity, 48 or more hours after the burn, fluid moves from the interstitial to the intravascular compartment and diuresis begins. This is an expected development and does not require a reduction in the IV infusion rate or the administration of NaCl. Diuresis is not suggestive of AKI. 29. A public health nurse has reviewed local data about the incidence and prevalence of burn injuries in the community. These data are likely to support what health promotion effort? A) Education about home safety B) Education about safe storage of chemicals C) Education about workplace health threats D) Education about safe driving A Feedback: A large majority of burns occur in the home setting; educational interventions should address this epidemiologic trend. 30. A nurse is performing a home visit to a patient who is recovering following a long course of inpatient treatment for burn injuries. When performing this home visit, the nurse should do which of the following? A) Assess the patient for signs of electrolyte imbalances. B) Administer fluids as ordered. C) Assess the risk for injury recurrence. D) Assess the patients psychosocial state. D Feedback: Recovery from burns can be psychologically challenging; the nurses assessments must address this reality. Fluid and electrolyte imbalances are infrequent during the rehabilitation phase of recovery. Burns are not typically a health problem that tends to recur; the experience of being burned tends to foster vigilance. 31. A patient has experienced burns to his upper thighs and knees. Following the application of new wound dressings, the nurse should perform what nursing action? A) Instruct the patient to keep the wound site in a dependent position. B) Administer PRN analgesia as ordered. C) Assess the patients peripheral pulses distal to the dressing. D) Assist with passive range of motion exercises to set the new dressing. C Feedback: Dressings can impede circulation if they are wrapped too tightly. The peripheral pulses must be checked frequently and burned extremities elevated. Dependent positioning does not need to be maintained. PRN analgesics should be administered prior to the dressing change. ROM exercises do not normally follow a dressing change. 32. A nurse is caring for a patient with burns who is in the later stages of the acute phase of recovery. The plan of nursing care should include which of the following nursing actions? A) Maintenance of bed rest to aid healing B) Choosing appropriate splints and functional devices C) Administration of beta adrenergic blockers D) Prevention of venous thromboembolism D Feedback: Prevention of deep vein thrombosis (DVT) is an important factor in care. Early mobilization of the patient is important. The nurse monitors the splints and functional devices, but these are selected by occupational and physical therapists. The hemodynamic changes accompanying burns do not normally require the use of beta blockers. A patient is in the acute phase of a burn injury. One of the nursing diagnoses in the plan of care is Ineffective Coping Related to Trauma of Burn Injury. What interventions appropriately address this diagnosis? Select all that apply. A) Promote truthful communication. B) Avoid asking the patient to make decisions. C) Teach the patient coping strategies. D) Administer benzodiazepines as ordered. E) Provide positive reinforcement. A, C, E Feedback: The nurse can assist the patient to develop effective coping strategies by setting specific expectations for behavior, promoting truthful communication to build trust, helping the patient practice appropriate strategies, and giving positive reinforcement when appropriate. The patient may benefit from being able to make decisions regarding his or her care. Benzodiazepines may be needed for short-term management of anxiety, but they are not used to enhance coping. 34. A patient who was burned in a workplace accident has completed the acute phase of treatment and the plan of care has been altered to prioritize rehabilitation. What nursing action should be prioritized during this phase of treatment? A) Monitoring fluid and electrolyte imbalances B) Providing education to the patient and family C) Treating infection D) Promoting thermoregulation B Feedback: Patient and family education is a priority during rehabilitation. There should be no fluid and electrolyte imbalances in the rehabilitation phase. The presence of impaired thermoregulation or infection would suggest that the patient is still in the acute phase of burn recovery. 35. A burn patient is transitioning from the acute phase of the injury to the rehabilitation phase. The patient tells the nurse, I cant wait to have surgery to reconstruct my face so I look normal again. What would be the nurses best response? A) Thats something that you and your doctor will likely talk about after your scars mature. B) That is something for you to talk to your doctor about because its not a nursing responsibility. C) I know this is really important to you, but you have to realize that no one can make you look like you used to. D) Unfortunately, its likely that you will have most of these scars for the rest of your life. A Feedback: Burn reconstruction is a treatment option after all scars have matured and is discussed within the first few years after injury. Even though this is not a nursing responsibility, the nurse should still respond appropriately to the patients query. It is true that the patient will not realistically look like he or she used to, but this does not instill hope. 36. A patient who is in the acute phase of recovery from a burn injury has yet to experience adequate pain control. What pain management strategy is most likely to meet this patients needs? A) A patient-controlled analgesia (PCA) system B) Oral opioids supplemented by NSAIDs C) Distraction and relaxation techniques supplemented by NSAIDs D) A combination of benzodiazepines and topical anesthetics A Feedback: The goal of treatment is to provide a long-acting analgesic that will provide even coverage for this long- term discomfort. It is helpful to use escalating doses when initiating the medication to reach the level of pain control that is acceptable to the patient. The use of patient-controlled analgesia (PCA) gives control to the patient and achieves this goal. Patients cannot normally achieve adequate pain control without the use of opioids, and parenteral administration is usually required. 37. The nurse caring for a patient who is recovering from full-thickness burns is aware of the patients risk for contracture and hypertrophic scarring. How can the nurse best mitigate this risk? A) Apply skin emollients as ordered after granulation has occurred. B) Keep injured areas immobilized whenever possible to promote healing. C) Administer oral or IV corticosteroids as ordered. D) Encourage physical activity and range of motion exercises. D Feedback: Exercise and the promotion of mobility can reduce the risk of contracture and hypertrophic scarring. Skin emollients are not normally used in the treatment of burns, and these do not prevent scarring. Steroids are not used to reduce scarring, as they also slow the healing process. 38. While performing a patients ordered wound care for the treatment of a burn, the patient has made a series of sarcastic remarks to the nurse and criticized her technique. How should the nurse best interpret this patients behavior? A) The patient may be experiencing an adverse drug reaction that is affecting his cognition and behavior. B) The patient may be experiencing neurologic or psychiatric complications of his injuries. C) The patient may be experiencing inconsistencies in the care that he is being provided. D) The patient may be experiencing anger about his circumstances that he is deflecting toward the nurse. D Feedback: The patient may experience feelings of anger. The anger may be directed outward toward those who escaped unharmed or toward those who are now providing care. While drug reactions, complications, and frustrating inconsistencies in care cannot be automatically ruled out, it is not uncommon for anger to be directed at caregivers. 39. A home care nurse is performing a visit to a patients home to perform wound care following the patients hospital treatment for severe burns. While interacting with the patient, the nurse should assess for evidence of what complication? A) Psychosis B) Post-traumatic stress disorder C) Delirium D) Vascular dementia B Feedback: Post-traumatic stress disorder (PTSD) is the most common psychiatric disorder in burn survivors, with a prevalence that may be as high as 45%. As a result, it is important for the nurse to assess for this complication of burn injuries. Psychosis, delirium, and dementia are not among the noted psychiatric and psychosocial complications of burns. 40. A nurse who provides care on a burn unit is preparing to apply a patients ordered topical antibiotic ointment. What action should the nurse perform when administering this medication? A) Apply the new ointment without disturbing the existing layer of ointment. B) Apply the ointment using a sterile tongue depressor. C) Apply a layer of ointment approximately 1/16 inch thick. D) Gently irrigate the wound bed after applying the antibiotic ointment. C Feedback: After removing the old ointment from the wound bed, the nurse should apply a layer of ointment 1/16- inch thick using clean gloves. The wound would not be irrigated after application of new ointment. Chapter 63: Assessment and Management of Patients with Eye and Vision Disorders 1. The registered nurse taking shift report learns that an assigned patient is blind. How should the nurse best communicate with this patient? A) Provide instructions in simple, clear terms. B) Introduce herself in a firm, loud voice at the doorway of the room. C) Lightly touch the patients arm and then introduce herself. D) State her name and role immediately after entering the patients room. D Feedback: There are several guidelines to consider when interacting with a person who is blind or has low vision. Identify yourself by stating your name and role, before touching or making physical contact with the patient. When talking to the person, speak directly at him or her using a normal tone of voice. There is no need to raise your voice unless the person asks you to do so and there is no particular need to simplify verbal instructions. 2. The nurse has taken shift report on her patients and has been told that one patient has an ocular condition that has primarily affected the rods in his eyes. Considering this information, what should the nurse do while caring for the patient? A) Ensure adequate lighting in the patients room. B) Provide a dimly lit room to aid vision by limiting contrast. C) Carefully point out color differences for the patient. D) Carefully point out fine details for the patient. A Feedback: The nurse should provide adequate lighting in the patients room, as the rods are mainly responsible for night vision or vision in low light. If the patients rods are impaired, the patient will have difficulty seeing in dim light. The cones in the eyes provide best vision for bright light, color vision, and fine detail. 3. A patient who presents for an eye examination is diagnosed as having a visual acuity of 20/40. The patient asks the nurse what these numbers specifically mean. What is a correct response by the nurse? A) A person whose vision is 20/40 can see an object from 40 feet away that a person with 20/20 vision can see from 20 feet away. B) A person whose vision is 20/40 can see an object from 20 feet away that a person with 20/20 vision can see from 40 feet away. C) A person whose vision is 20/40 can see an object from 40 inches away that a person with 20/20 vision can see from 20 inches away. D) A person whose vision is 20/40 can see an object from 20 inches away that a person with 20/20 vision can see from 40 inches away. B Feedback: The Snellen chart is a tool used to measure visual acuity. It is composed of a series of progressively smaller rows of letters and is used to test distance vision. The fraction 20/20 is considered the standard of normal vision. Most people can see the letters on the line designated as 20/20 from a distance of 20 feet. A person whose vision is 20/40 can see an object from 20 feet away that a person with 20/20 vision can see from 40 feet away. 4. During discharge teaching the nurse realizes that the patient is not able to read medication bottles accurately and has not been taking her medications consistently at home. How should the nurse intervene most appropriately in this situation? A) Ask the social worker to investigate alternative housing arrangements. B) Ask the social worker to investigate community support agencies. C) Encourage the patient to explore surgical corrections for the vision problem. D) Arrange for referral to a rehabilitation facility for vision training. B Feedback: Managing low vision involves magnification and image enhancement through the use of low-vision aids and strategies and referrals to social services and community agencies serving those with visual impairment. Community agencies offer services to patients with low vision, which include training in independent living skills and a variety of assistive devices for vision enhancement, orientation, and mobility, preventing patients from needing to enter a nursing facility. A rehabilitation facility is generally not needed by the patients to learn to use the assistive devices or to gain a greater degree of independence. Surgical options may or may not be available to the patient. 5. The nurse is providing health education to a patient newly diagnosed with glaucoma. The nurse teaches the patient that this disease has a familial tendency. The nurse should encourage the patients immediate family members to undergo clinical examinations how often? A) At least monthly B) At least once every 2 years C) At least once every 5 years D) At least once every 10 years B Feedback: Glaucoma has a family tendency and family members should be encouraged to undergo examinations at least once every 2 years to detect glaucoma early. Testing on a monthly basis is not necessary and excessive. 6. A patient is exploring treatment options after being diagnosed with age-related cataracts that affect her vision. What treatment is most likely to be used in this patients care? A) Antioxidant supplements, vitamin C and E, beta-carotene, and selenium B) Eyeglasses or magnifying lenses C) Corticosteroid eye drops D) Surgical intervention D Feedback: Surgery is the treatment option of choice when the patients functional and visual status is compromised. No nonsurgical (medications, eye drops, eyeglasses) treatment cures cataracts or prevents age-related cataracts. Studies recently have found no benefit from antioxidant supplements, vitamins C and E, beta- carotene, or selenium. Corticosteroid eye drops are prescribed for use after cataract surgery; however, they increase the risk for cataracts if used long-term or in high doses. Eyeglasses and magnification may improve vision in the patient with early stages of cataracts, but have limitations for the patient with impaired functioning. 7. A patient presents at the ED after receiving a chemical burn to the eye. What would be the nurses initial intervention for this patient? A) Generously flush the affected eye with a dilute antibiotic solution. B) Generously flush the affected eye with normal saline or water. C) Apply a patch to the affected eye. D) Apply direct pressure to the affected eye. B Feedback: Chemical burns of the eye should be immediately irrigated with water or normal saline to flush the chemical from the eye. Antibiotic solutions, lubricant drops, and other prescription drops may be prescribed at a later time. Application of direct pressure may extend the damage to the eye tissue and should be avoided. Patching will be incorporated into the treatment plan at a later time to assist with the process of re-epithelialization, but at this point in the care of the patient, patching will prevent irrigation of the eye. 8. The nurse is administering eye drops to a patient with glaucoma. After instilling the patients first medication, how long should the nurse wait before instilling the patients second medication into the same eye? A) 30 seconds B) 1 minute C) 3 minutes D) 5 minutes D Feedback: A 5-minute interval between successive eye drop administrations allows for adequate drug retention and absorption. Any time frame less than 5 minutes will not allow adequate absorption. 9. A patient is being discharged home from the ambulatory surgical center after cataract surgery. In reviewing the discharge instructions with the patient, the nurse instructs the patient to immediately call the office if the patient experiences what? A) Slight morning discharge from the eye B) Any appearance of redness of the eye C) A scratchy feeling in the eye D) A new floater in vision D Feedback: Cataract surgery increases the risk of retinal detachment and the patient must be instructed to notify the surgeon of new floaters in vision, flashing lights, decrease in vision, pain, or increase in redness. Slight morning discharge, some redness, and a scratchy feeling may be expected for a few days after surgery. 10. A patient comes to the ophthalmology clinic for an eye examination. The patient tells the nurse that he often sees floaters in his vision. How should the nurse best interpret this subjective assessment finding? A) This is a normal aging process of the eye. B) Glasses will minimize this phenomenon. C) The patient may be exhibiting signs of glaucoma. D) This may be a result of weakened ciliary muscles. A Feedback: As the body ages, the perfect gel-like characteristics of the vitreous humor are gradually lost, and various cells and fibers cast shadows that the patient perceives as floaters. This is a normal aging process. 11. A patients ocular tumor has necessitated enucleation and the patient will be fitted with a prosthesis. The nurse should address what nursing diagnosis when planning the patients discharge education? A) Disturbed body image B) Chronic pain C) Ineffective protection D) Unilateral neglect A Feedback: The use of an ocular prosthesis is likely to have a significant impact on a patients body image. Prostheses are not associated with chronic pain or ineffective protection. The patient experiences a change in vision, but is usually able to accommodate such changes and prevent unilateral neglect. 12. The nurses assessment of a patient with significant visual losses reveals that the patient cannot count fingers. How should the nurse proceed with assessment of the patients visual acuity? A) Assess the patients vision using a Snellen chart. B) Determine whether the patient is able to see the nurses hand motion. C) Perform a detailed examination of the patients external eye structures. D) Palpate the patients periocular regions. B Feedback: If the patient cannot count fingers, the examiner raises one hand up and down or moves it side to side and asks in which direction the hand is moving. An inability to count fingers precludes the use of a Snellen chart. Palpation and examination cannot ascertain visual acuity. 13. The nurse on the medicalsurgical unit is reviewing discharge instructions with a patient who has a history of glaucoma. The nurse should anticipate the use of what medications? A) Potassium-sparing diuretics B) Cholinergics C) Antibiotics D) Loop diuretics B Feedback: Cholinergics are used in the treatment of glaucoma. The action of this medication is to increase aqueous fluid outflow by contracting the ciliary muscle and causing miosis and opening the trabecular meshwork. Diuretics and antibiotics are not used in the management of glaucoma. 14. A nurse is teaching a patient with glaucoma how to administer eye drops to achieve maximum absorption. The nurse should teach the patient to perform what action? A) Instill the medication in the conjunctival sac. B) Maintain a supine position for 10 minutes after administration. C) Keep the eyes closed for 1 to 2 minutes after administration. D) Apply the medication evenly to the sclera A Feedback: Eye drops should be instilled into the conjunctival sac, where absorption can best take place, rather than distributed over the sclera. It is unnecessary to keep the eyes closed or to maintain a supine position after administration. 15. A patient with chronic open-angle glaucoma is being taught to self-administer pilocarpine. After the patient administers the pilocarpine, the patient states that her vision is blurred. Which nursing action is most appropriate? A) Holding the next dose and notifying the physician B) Treating the patient for an allergic reaction C) Suggesting that the patient put on her glasses D) Explaining that this is an expected adverse effect D Feedback: Pilocarpine, a miotic drug used to treat glaucoma, achieves its effect by constricting the pupil. Blurred vision lasting 1 to 2 hours after instilling the eye drops is an expected adverse effect. The patient may also note difficulty adapting to the dark. Because blurred vision is an expected adverse effect, the drug does not need to be withheld, nor does the physician need to be notified. Likewise, the patient does not need to be treated for an allergic reaction. Wearing glasses will not alter this temporary adverse effect. 16. The nurse should recognize the greatest risk for the development of blindness in which of the following patients? A) A 58-year-old Caucasian woman with macular degeneration B) A 28-year-old Caucasian man with astigmatism C) A 58-year-old African American woman with hyperopia D) A 28-year-old African American man with myopia A Feedback: The most common causes of blindness and visual impairment among adults 40 years of age or older are diabetic retinopathy, macular degeneration, glaucoma, and cataracts. The 58-year-old Caucasian woman with macular degeneration has the greatest risk for the development of blindness related to her age and the presence of macular degeneration. Individuals with hyperopia, astigmatism, and myopia are not in a risk category for blindness. 17. A 6-year-old child is brought to the pediatric clinic for the assessment of redness and discharge from the eye and is diagnosed with viral conjunctivitis. What is the most important information to discuss with the parents and child? A) Handwashing can prevent the spread of the disease to others. B) The importance of compliance with antibiotic therapy C) Signs and symptoms of complications, such as meningitis and septicemia D) The likely need for surgery to prevent scarring of the conjunctiva A Feedback: The nurse must inform the parents and child that viral conjunctivitis is highly contagious and instructions should emphasize the importance of handwashing and avoiding sharing towels, face cloths, and eye drops. Viral conjunctivitis is not responsive to any treatment, including antibiotic therapy. Patients with gonococcal conjunctivitis are at risk for meningitis and generalized septicemia; these conditions do not apply to viral conjunctivitis. Surgery to prevent scarring of the conjunctiva is not associated with viral conjunctivitis. 18. The nurse is admitting a 55-year-old male patient diagnosed with a retinal detachment in his left eye. While assessing this patient, what characteristic symptom would the nurse expect to find? A) Flashing lights in the visual field B) Sudden eye pain C) Loss of color vision D) Colored halos around lights A Feedback: Flashing lights in the visual field is a common symptom of retinal detachment. Patients may also report spots or floaters or the sensation of a curtain being pulled across the eye. Retinal detachment is not associated with eye pain, loss of color vision, or colored halos around lights. 19. Several residents of a long-term care facility have developed signs and symptoms of viral conjunctivitis. What is the most appropriate action of the nurse who oversees care in the facility? A) Arrange for the administration of prophylactic antibiotics to unaffected residents. B) Instill normal saline into the eyes of affected residents two to three times daily. C) Swab the conjunctiva of unaffected residents for culture and sensitivity testing. D) Isolate affected residents from residents who have not developed conjunctivitis. D Feedback: To prevent spread during outbreaks of conjunctivitis caused by adenovirus, health care facilities must set aside specified areas for treating patients diagnosed with or suspected of having conjunctivitis caused by adenovirus. Antibiotics and saline flushes are ineffective and normally no need to perform testing of individuals lacking symptoms. 20. A patient has just returned to the surgical floor after undergoing a retinal detachment repair. The postoperative orders specify that the patient should be kept in a prone position until otherwise ordered. What should the nurse do? A) Call the physician and ask for the order to be confirmed. B) Follow the order because this position will help keep the retinal repair intact. C) Instruct the patient to maintain this position to prevent bleeding. D) Reposition the patient after the first dressing change. B Feedback: For pneumatic retinopexy, postoperative positioning of the patient is critical because the injected bubble must float into a position overlying the area of detachment, providing consistent pressure to reattach the sensory retina. The patient must maintain a prone position that would allow the gas bubble to act as a tamponade for the retinal break. Patients and family members should be made aware of these special needs beforehand so that the patient can be made as comfortable as possible. It would be inappropriate to deviate from this order and there is no obvious need to confirm the order. 21. A patient has informed the home health nurse that she has recently noticed distortions when she looks at the Amsler grid that she has mounted on her refrigerator. What is the nurses most appropriate action? A) Reassure the patient that this is an age-related change in vision. B) Arrange for the patient to have her visual acuity assessed. C) Arrange for the patient to be assessed for macular degeneration. D) Facilitate tonometry testing. C Feedback: 18, The Amsler grid is a test often used for patients with macular problems, such as macular degeneration. Distortions would not be attributed to age-related changes and there is no direct need for testing of intraocular pressure or visual acuity. 22. A 56-year-old patient has come to the clinic for his routine eye examination and is told he needs bifocals. The patient asks the nurse what change in his eyes has caused his need for bifocals. How should the nurse respond? A) You know, you are getting older now and we change as we get older. B) The parts of our eyes age, just like the rest of us, and this is nothing to cause you to worry. C) There is a gradual thickening of the lens of the eye and it can limit the eyes ability for accommodation. D) The eye gets shorter, back to front, as we age and it changes how we see things. C Feedback: As a result of a loss of accommodative power in the lens with age, many adults require bifocals or other forms of visual correction. This is not attributable to a change in the shape of the ocular globe. The nurse should not dismiss or downplay the patients concerns. 23. The nurse is teaching a patient to care for her new ocular prosthesis. What should the nurse emphasize during the patients health education? A) The need to limit exposure to bright light B) The need to maintain a low Fowlers position when removing the prosthesis C) The need to perform thorough hand hygiene before handling the prosthesis D) The need to apply antiviral ointment to the prosthesis daily C Feedback: Proper hand hygiene must be observed before inserting and removing an ocular prosthesis. There is no need for a low Fowlers position or for limiting light exposure. Antiviral ointments are not routinely used. 24. Cytomegalovirus (CMV) is the most common cause of retinal inflammation in patients with AIDS. What drug, surgically implanted, is used for the acute stage of CMV retinitis? A) Pilocarpine B) Penicillin C) Ganciclovir D) Gentamicin C Feedback: The surgically implanted sustained-release insert of ganciclovir enables higher concentrations of ganciclovir to reach the CMV retinitis. Pilocarpine is a muscarinic agent used in open-angle glaucoma. Gentamicin and penicillin are antibiotics that are not used to treat CMV retinitis. 25. A patient got a sliver of glass in his eye when a glass container at work fell and shattered. The glass had to be surgically removed and the patient is about to be discharged home. The patient asks the nurse for a topical anesthetic for the pain in his eye. What should the nurse respond? A) Overuse of these drops could soften your cornea and damage your eye. B) You could lose the peripheral vision in your eye if you used these drops too much. C) Im sorry, this medication is considered a controlled substance and patients cannot take it home. D) I know these drops will make your eye feel better, but I cant let you take them home. A Feedback: Most patients are not allowed to take topical anesthetics home because of the risk of overuse. Patients with corneal abrasions and erosions experience severe pain and are often tempted to overuse topical anesthetic eye drops. Overuse of these drops results in softening of the cornea. Prolonged use of anesthetic drops can delay wound healing and can lead to permanent corneal opacification and scarring, resulting in visual loss. The nurse must explain the rationale for limiting the home use of these medications. 26. A patient has been diagnosed with glaucoma and the nurse is preparing health education regarding the patients medication regimen. The patient states that she is eager to beat this disease and looks forward to the time that she will no longer require medication. How should the nurse best respond? A) You have a great attitude. This will likely shorten the amount of time that you need medications. B) In fact, glaucoma usually requires lifelong treatment with medications. C) Most people are treated until their intraocular pressure goes below 50 mm Hg. D) You can likely expect a minimum of 6 months of treatment. B Feedback: Glaucoma requires lifelong pharmacologic treatment. Normal intraocular pressure is between 10 and 21 mm Hg. 27. An older adult patient has been diagnosed with macular degeneration and the nurse is assessing him for changes in visual acuity since his last clinic visit. When assessing the patient for recent changes in visual acuity, the patient states that he sees the lines on an Amsler grid as being distorted. What is the nurses most appropriate response? A) Ask if the patient has been using OTC vasoconstrictors. B) Instruct the patient to repeat the test at different times of the day when at home. C) Arrange for the patient to visit his ophthalmologist. D) Encourage the patient to adhere to his prescribed drug regimen. C Feedback: With a change in the patients perception of the grid, the patient should notify the ophthalmologist immediately and should arrange to be seen promptly. This is a priority over encouraging drug adherence, even though this is also important. Vasoconstrictors are not a likely cause of this change and repeating the test at different times is not relevant. 28. A public health nurse is teaching a health promotion workshop that focuses on vision and eye health. What should this nurse cite as the most common causes of blindness and visual impairment among adults over the age of 40? Select all that apply. A) Diabetic retinopathy B) Trauma C) Macular degeneration D) Cytomegalovirus E) Glaucoma A, C, E Feedback: The most common causes of blindness and visual impairment among adults 40 years of age or older are diabetic retinopathy, macular degeneration, glaucoma, and cataracts. Therefore, trauma and cytomegalovirus are incorrect. 29. The nurse is providing discharge education to an adult patient who will begin a regimen of ocular medications for the treatment of glaucoma. How can the nurse best determine if the patient is able to self-administer these medications safely and effectively? A) Assess the patient for any previous inability to self-manage medications. B) Ask the patient to demonstrate the instillation of her medications. C) Determine whether the patient can accurately describe the appropriate method of administering her medications. D) Assess the patients functional status. B Feedback: The patient or the caregiver at home should be asked to demonstrate actual eye drop administration. This method of assessment is more accurate than asking the patient to describe the process or determining earlier inabilities to self-administer medications. The patients functional status will not necessarily determine the ability to administer medication safely. 30. A patient with low vision has called the clinic and asked the nurse for help with acquiring some low- vision aids. What else can the nurse offer to help this patient manage his low vision? A) The patient uses OTC NSAIDs. B) The patient has a history of stroke. C) The patient has diabetes. D) The patient has Asian ancestry. C Feedback: Diabetes is a risk factor for glaucoma, but Asian ancestry, NSAIDs, and stroke are not risk factors for the disease. 31. The public health nurse is addressing eye health and vision protection during an educational event. What statement by a participant best demonstrates an understanding of threats to vision? A) Im planning to avoid exposure to direct sunlight on my next vacation. B) Ive never exercised regularly, but Im going to start working out at the gym daily. C) Im planning to talk with my pharmacist to review my current medications. D) Im certainly going to keep a close eye on my blood pressure from now on. D Feedback: Hypertension is a major cause of vision loss, exceeding the significance of inactivity, sunlight, and adverse effects of medications. 32. A patient has had a sudden loss of vision after head trauma. How should the nurse best describe the placement of items on the dinner tray? A) Explain the location of items using clock cues. B) Explain that each of the items on the tray is clearly separated. C) Describe the location of items from the bottom of the plate to the top. D) Ask the patient to describe the location of items before confirming their location. A Feedback: The food trays composition is likened to the face of a clock. It is unreasonable to expect the patient to describe the location of items or to state that items are separated. 33. A hospitalized patient with impaired vision must get a picture in his or her mind of the hospital room and its contents in order to mobilize independently and safely. What must the nurse monitor in the patients room? A) That a commode is always available at the bedside B) That all furniture remains in the same position C) That visitors do not leave items on the bedside table D) That the patients slippers stay under the bed B Feedback: All articles and furniture must remain in the same positions throughout the patients hospitalization. This will reduce the patients risks for falls. Visual impairment does not necessarily indicate a need for a commode. Keeping slippers under the bed and keeping the bedside table clear are also appropriate, but preventing falls by maintaining the room arrangement is a priority. 34. A patient has just arrived to the floor after an enucleation procedure following a workplace accident in which his left eye was irreparably damaged. Which of the following should the nurse prioritize during the patients immediate postoperative recovery? A) Teaching the patient about options for eye prostheses B) Teaching the patient to estimate depth and distance with the use of one eye C) Assessing and addressing the patients emotional needs D) Teaching the patient about his post-discharge medication regimen C Feedback: When surgical eye removal is unexpected, such as in severe ocular trauma, leaving no time for the patient and family to prepare for the loss, the nurses role in providing emotional support is crucial. In the short term, this is a priority over teaching regarding prostheses, medications, or vision adaptation. 35. A patient with a diagnosis of retinal detachment has undergone a vitreoretinal procedure on an outpatient basis. What subject should the nurse prioritize during discharge education? A) Risk factors for postoperative cytomegalovirus (CMV) B) Compensating for vision loss for the next several weeks C) Non-pharmacologic pain management strategies D) Signs and symptoms of increased intraocular pressure D Feedback: Patients must be educated about the signs and symptoms of complications, particularly of increasing IOP and postoperative infection. CMV is not a typical complication and the patient should not expect vision loss. Vitreoretinal procedures are not associated with high levels of pain. 36. A patient is ready to be discharged home after a cataract extraction with intraocular lens implant and the nurse is reviewing signs and symptoms that need to be reported to the ophthalmologist immediately. Which of the patients statements best demonstrates an adequate understanding? A) I need to call the doctor if I get nauseated. B) I need to call the doctor if I have a light morning discharge. C) I need to call the doctor if I get a scratchy feeling. D) I need to call the doctor if I see flashing lights. D Feedback: Postoperatively, the patient who has undergone cataract extraction with intraocular lens implant should report new floaters in vision, flashing lights, decrease in vision, pain, or increase in redness to the ophthalmologist. Slight morning discharge and a scratchy feeling can be expected for a few days. Blurring of vision may be experienced for several days to weeks. 37. A patient has lost most of her vision as a result of macular degeneration. When attempting to meet this patients psychosocial needs, what nursing action is most appropriate? A) Encourage the patient to focus on her use of her other senses. B) Assess and promote the patients coping skills during interactions with the patient. C) Emphasize that her lifestyle will be unchanged once she adapts to her vision loss. D) Promote the patients hope for recovery. B Feedback: The nurse should empathically promote the patients coping with her loss. Focusing on the remaining senses could easily be interpreted as downplaying the patients loss, and recovery is not normally a realistic possibility. Even with successful adaptation, the patients lifestyle will be profoundly affected. 38. When administering a patients eye drops, the nurse recognizes the need to prevent absorption by the nasolacrimal duct. How can the nurse best achieve this goal? A) Ensure that the patient is well hydrated at all times. B) Encourage self-administration of eye drops. C) Occlude the puncta after applying the medication. D) Position the patient supine before administering eye drops. C Feedback: Absorption of eye drops by the nasolacrimal duct is undesirable because of the potential systemic side effects of ocular medications. To diminish systemic absorption and minimize the side effects, it is important to occlude the puncta. Self-administration, supine positioning, and adequate hydration do not prevent this adverse effect. 39. A patient with glaucoma has presented for a scheduled clinic visit and tells the nurse that she has begun taking an herbal remedy for her condition that was recommended by a work colleague. What instruction should the nurse provide to the patient? A) The patient should discuss this new remedy with her ophthalmologist promptly. B) The patient should monitor her IOP closely for the next several weeks. C) The patient should do further research on the herbal remedy. D) The patient should report any adverse effects to her pharmacist. A Feedback: Patients should discuss any new treatments with an ophthalmologist; this should precede the patients own further research or reporting adverse effects to the pharmacist. Self-monitoring of IOP is not possible. 40. A patient is scheduled for enucleation and the nurse is providing anticipatory guidance about postoperative care. What aspects of care should the nurse describe to the patient? Select all that apply. A) Application of topical antibiotic ointment B) Maintenance of a supine position for the first 48 hours postoperative C) Fluid restriction to prevent orbital edema D) Administration of loop diuretics to prevent orbital edema E) Use of an ocular pressure dressing A, E Feedback: Patients who undergo eye removal need to know that they will usually have a large ocular pressure dressing, which is typically removed after a week, and that an ophthalmic topical antibiotic ointment is applied in the socket three times daily. Fluid restriction, supine positioning, and diuretics are not indicated. Chapter 64: Assessment and Management of Patients with Hearing and Balance Disorders 1. The clinic nurse is assessing a child who has been brought to the clinic with signs and symptoms that are suggestive of otitis externa. What assessment finding is characteristic of otitis externa? A) Tophi on the pinna and ear lobe B) Dark yellow cerumen in the external auditory canal C) Pain on manipulation of the auricle D) Air bubbles visible in the middle ear C Feedback: Pain when the nurse pulls gently on the auricle in preparation for an otoscopic examination of the ear canal is a characteristic finding in patients with otitis externa. Tophi are deposits of generally painless uric acid crystals; they are a common physical assessment finding in patients diagnosed with gout. Cerumen is a normal finding during assessment of the ear canal. Its presence does not necessarily indicate that inflammation is present. Air bubbles in the middle ear may be visualized with the otoscope; however, these do not indicate a problem involving the ear canal. 2. While reviewing the health history of an older adult experiencing hearing loss the nurse notes the patient has had no trauma or loss of balance. What aspect of this patients health history is most likely to be linked to the patients hearing deficit? A) Recent completion of radiation therapy for treatment of thyroid cancer B) Routine use of quinine for management of leg cramps C) Allergy to hair coloring and hair spray D) Previous perforation of the eardrum B Feedback: Long-term, regular use of quinine for management of leg cramps is associated with loss of hearing acuity. Radiation therapy for cancer should not affect hearing; however, hearing can be significantly compromised by chemotherapy. Allergy to hair products may be associated with otitis externa; however, it is not linked to hearing loss. An ear drum that perforates spontaneously due to the sudden drop in altitude associated with a high dive usually heals well and is not likely to become infected. Recurrent otitis media with perforation can affect hearing as a result of chronic inflammation of the ossicles in the middle ear. 3. A nurse is planning preoperative teaching for a patient with hearing loss due to otosclerosis. The patient is scheduled for a stapedectomy with insertion of a prosthesis. What information is most crucial to include in the patients preoperative teaching? A) The procedure is an effective, time-tested treatment for sensory hearing loss. B) The patient is likely to experience resolution of conductive hearing loss after the procedure. C) Several months of post-procedure rehabilitation will be needed to maximize benefits. D) The procedure is experimental, but early indications suggest great therapeutic benefits. B Feedback: Stapedectomy is a very successful time-tested procedure, resulting in the restoration of conductive hearing loss. Lengthy rehabilitation is not normally required. 4. Which of the following nursing interventions would most likely facilitate effective communication with a hearing-impaired patient? A) Ask the patient to repeat what was said in order to evaluate understanding. B) Stand directly in front of the patient to facilitate lip reading. C) Reduce environmental noise and distractions before communicating. D) Raise the voice to project sound at a higher frequency. C Feedback: Communication with the hearing impaired can be facilitated by talking in a quiet space free of competing noise stimuli and other distractions. Asking the patient to repeat what was said is likely to provoke frustration in the patient. A more effective strategy would be to repeat the question or statement, choosing different words. Raising the voice to project sound at higher frequency would make understanding more difficult. The nurse cannot assume that the patient reads lips. If the patient does read lips, on average he or she will understand only 50% of words accurately. 5. The nurse is providing discharge education for a patient with a new diagnosis of Mnires disease. What food should the patient be instructed to limit or avoid? A) Sweet pickles B) Frozen yogurt C) Shellfish D) Red meat A Feedback: The patient with Mnires disease should avoid foods high in salt and/or sugar; sweet pickles are high in both. Milk products are not contraindicated. Any type of meat, fish, or poultry is permitted, with the exception of canned or pickled varieties. In general, the patient with Mnires disease should avoid or limit canned and processed foods. 6. Following a motorcycle accident, a 17-year-old man is brought to the ED. What physical assessment findings related to the ear should be reported by the nurse immediately? A) The malleus can be visualized during otoscopic examination. B) The tympanic membrane is pearly gray. C) Tenderness is reported by the patient when the mastoid area is palpated. D) Clear, watery fluid is draining from the patients ear. D Feedback: For the patient experiencing acute head trauma, immediately report the presence of clear, watery drainage from the ear. The fluid is likely to be cerebrospinal fluid associated with skull fracture. The ability to visualize the malleus is a normal physical assessment finding. The tympanic membrane is normally pearly gray in color. Tenderness of the mastoid area usually indicates inflammation. This should be reported, but is not a finding indicating urgent intervention. 7. A patient has been diagnosed with hearing loss related to damage of the end organ for hearing or cranial nerve VIII. What term is used to describe this condition? A) Exostoses B) Otalgia C) Sensorineural hearing loss D) Presbycusis C Feedback: Sensorineural hearing loss is loss of hearing related to damage of the end organ for hearing or cranial nerve VIII. Exostoses refer to small, hard, bony protrusions in the lower posterior bony portion of the ear canal. Otalgia refers to a sensation of fullness or pain in the ear. Presbycusis is the term used to refer to the progressive hearing loss associated with aging. Both middle and inner ear age-related changes result in hearing loss. 8. A group of high school students is attending a concert, which will be at a volume of 80 to 90 dB. What is a health consequence of this sound level? A) Hearing will not be affected by a decibel level in this range. B) Hearing loss may occur with a decibel level in this range. C) Sounds in this decibel level are not perceived to be harsh to the ear. D) Ear plugs will have no effect on these decibel levels. B Feedback: Sound louder than 80 dB is perceived by the human ear to be harsh and can be damaging to the inner ear. Ear protection or plugs do help to minimize the effects of high decibel levels. 9. A patient has undergone diagnostic testing and has been diagnosed with otosclerosis? What ear structure is primarily affected by this diagnosis? A) Malleus B) Stapes C) Incus D) Tympanic membrane B Feedback: Otosclerosis involves the stapes and is thought to result from the formation of new, abnormal bone, especially around the oval window, with resulting fixation of the stapes. 10. A patient with otosclerosis has significant hearing loss. What should the nurse do to best facilitate communication with the patient? A) Sit or stand in front of the patient when speaking. B) Use exaggerated lip and mouth movements when talking. C) Stand in front of a light or window when speaking. D) Say the patients name loudly before starting to talk. A Feedback: Standing directly in front of a hearing-impaired patient allows him or her to lip-read and see facial expressions that offer clues to what is being said. Using exaggerated lip and mouth movements can make lip-reading more difficult by distorting words. Backlighting can create glare, making it difficult for the patient to lip-read. To get the attention of a hearing-impaired patient, gently touch the patients shoulder or stand in front of the patient. 11. The nurse in the ED is caring for a 4 year-old brought in by his parents who state that the child will not stop crying and pulling at his ear. Based on information collected by the nurse, which of the following statements applies to a diagnosis of external otitis? A) External otitis is characterized by aural tenderness. B) External otitis is usually accompanied by a high fever. C) External otitis is usually related to an upper respiratory infection. D) External otitis can be prevented by using cotton-tipped applicators to clean the ear. A Feedback: Patients with otitis externa usually exhibit pain, discharge from the external auditory canal, and aural tenderness. Fever and accompanying upper respiratory infection occur more commonly in conjunction with otitis media (infection of the middle ear). Cotton-tipped applicators can actually cause external otitis so their use should be avoided. 12. A patient diagnosed with arthritis has been taking aspirin and now reports experiencing tinnitus and hearing loss. What should the nurse teach this patient? A) The hearing loss will likely resolve with time after the drug is discontinued. B) The patients hearing loss and tinnitus are irreversible at this point. C) The patients tinnitus is likely multifactorial, and not directly related to aspirin use. D) The patients tinnitus will abate as tolerance to aspirin develops. A Feedback: Tinnitus and hearing loss are signs of ototoxicity, which is associated with aspirin use. In most cases, this will resolve upon discontinuing the aspirin. Many other drugs cause irreversible ototoxicity. 13. A patient is postoperative day 6 following tympanoplasty and mastoidectomy. The patient has phoned the surgical unit and states that she is experiencing occasional sharp, shooting pains in her affected ear. How should the nurse best interpret this patients complaint? A) These pains are an expected finding during the first few weeks of recovery. B) The patients complaints are suggestive of a postoperative infection. C) The patient may have experienced a spontaneous rupture of the tympanic membrane. D) The patients surgery may have been unsuccessful. A Feedback: For 2 to 3 weeks after surgery, the patient may experience sharp, shooting pains intermittently as the eustachian tube opens and allows air to enter the middle ear. Constant, throbbing pain accompanied by fever may indicate infection and should be reported to the primary care provider. The patients pain does not suggest tympanic perforation or unsuccessful surgery. 14. The nurse is discussing the results of a patients diagnostic testing with the nurse practitioner. What Weber test result would indicate the presence of a sensorineural loss? A) The sound is heard better in the ear in which hearing is better. B) The sound is heard equally in both ears. C) The sound is heard better in the ear in which hearing is poorer. D) The sound is heard longer in the ear in which hearing is better. A Feedback: A patient with sensorineural hearing loss hears the sound better in the ear in which hearing is better. The Weber test assesses bone conduction of sound and is used for assessing unilateral hearing loss. A tuning fork is used. A patient with normal hearing hears the sound equally in both ears or describes the sound as centered in the middle of the head. A patient whose hearing loss is conductive hears the sound better in the affected ear. 15. The advanced practice nurse is attempting to examine the patients ear with an otoscope. Because of impacted cerumen, the tympanic membrane cannot be visualized. The nurse irrigates the patients ear with a solution of hydrogen peroxide and water to remove the impacted cerumen. What nursing intervention is most important to minimize nausea and vertigo during the procedure? A) Maintain the irrigation fluid at a warm temperature. B) Instill short, sharp bursts of fluid into the ear canal. C) Follow the procedure with insertion of a cerumen curette to extract missed ear wax. D) Have the patient stand during the procedure. A Feedback: Warm water (never cold or hot) and gentle, not forceful, irrigation should be used to remove cerumen. Too forceful irrigation can cause perforation of the tympanic membrane, and ice water causes vomiting. Cerumen curettes should not be routinely used by the nurse. Special training is required to use a curette safely. It is unnecessary to have the patient stand during the procedure. 16. A patient is scheduled to have an electronystagmography as part of a diagnostic workup for Mnires disease. What question is it most important for the nurse to ask the patient in preparation for this test? A) Have you ever experienced claustrophobia or feelings of anxiety while in enclosed spaces? B) Do you currently take any tranquilizers or stimulants on a regular basis? C) Do you have a history of falls or problems with loss of balance? D) Do you have a history of either high or low blood pressure? B Feedback: Electronystagmography measures changes in electrical potentials created by eye movements during induced nystagmus. Medications such as tranquilizers, stimulants, or antivertigo agents are withheld for 5 days before the test. Claustrophobia is not a significant concern associated with this test; rather, it is most often a concern for patients undergoing magnetic resonance imaging (MRI). Balance is impaired by Mnires disease; therefore, a patient history of balance problems is important, but is not relevant to test preparation. Hypertension or hypotension, while important health problems, should not be affected by this test. 17. The nurse is planning the care of a patient who is adapting to the use of a hearing aid for the first time. What is the most significant challenge experienced by a patient with hearing loss who is adapting to using a hearing aid for the first time? A) Regulating the tone and volume B) Learning to cope with amplification of background noise C) Constant irritation of the external auditory canal D) Challenges in keeping the hearing aid clean while minimizing exposure to moisture B Feedback: Each of the answers represents a common problem experienced by patients using a hearing aid for the first time. However, amplification of background noise is a difficult problem to manage and is the major reason why patients stop using their hearing aid. All patients learning to use a hearing aid require support and coaching by the nurse and other members of the health care team. Patients should be encouraged to discuss their adaptation to the hearing aid with their audiologist. 18. A patient with mastoiditis is admitted to the post-surgical unit after undergoing a radical mastoidectomy. The nurse should identify what priority of postoperative care? A) Assessing for mouth droop and decreased lateral eye gaze B) Assessing for increased middle ear pressure and perforated ear drum C) Assessing for gradual onset of conductive hearing loss and nystagmus D) Assessing for scar tissue and cerumen obstructing the auditory canal A Feedback: The facial nerve runs through the middle ear and the mastoid; therefore, there is risk of injuring this nerve during a mastoidectomy. When injury occurs, the patient may display mouth droop and decreased lateral gaze on the operative side. Scar tissue is a long-term complication of tympanoplasty and therefore would not be evident during the immediate postoperative period. Tympanic perforation is not a common complication of this surgery. 19. The nurse is assessing a patient with multiple sclerosis who is demonstrating involuntary, rhythmic eye movements. What term will the nurse use when documenting these eye movements? A) Vertigo B) Tinnitus C) Nystagmus D) Astigmatism C Feedback: Vertigo is an illusion of movement where the individual or the surroundings are sensed as moving. Tinnitus refers to a subjective perception of sound with internal origin. Nystagmus refers to involuntary rhythmic eye movement. Astigmatism is a defect is visual acuity. 20. The nurse is planning the care of a patient with a diagnosis of vertigo. What nursing diagnosis risk should the nurse prioritize in this patients care? A) Risk for disturbed sensory perception B) Risk for unilateral neglect C) Risk for falls D) Risk for ineffective health maintenance C Feedback: Vertigo is defined as the misperception or illusion of motion, either of the person or the surroundings. A patient suffering from vertigo will be at an increased risk of falls. For most patients, this is likely to exceed the patients risk for neglect, ineffective health maintenance, or disturbed sensation. 21. A patient has been diagnosed with serous otitis media for the third time in the past year. How should the nurse best interpret this patients health status? A) For some patients, these recurrent infections constitute an age-related physiologic change. B) The patient would benefit from a temporary mobility restriction to facilitate healing. C) The patient needs to be assessed for nasopharyngeal cancer. D) Blood cultures should be drawn to rule out a systemic infection. C Feedback: A carcinoma (e.g., nasopharyngeal cancer) obstructing the eustachian tube should be ruled out in adults with persistent unilateral serous otitis media. This phenomenon is not an age-related change and does not indicate a systemic infection. Mobility limitations are unnecessary. 22. A patient with a sudden onset of hearing loss tells the nurse that he would like to begin using hearing aids. The nurse understands that the health professional dispensing hearing aids would have what responsibility? A) Test the patients hearing promptly. B) Perform an otoscopy. C) Measure the width of the patients ear canal. D) Refer the patient to his primary care physician. D Feedback: Health care professionals who dispense hearing aids are required to refer prospective users to a physician if the patient has sudden or rapidly progressive hearing loss. This would be a health priority over other forms of assessment, due to the possible presence of a pathologic process. 23. The nurse is providing care for a patient who has benefited from a cochlear implant. The nurse should understand that this patients health history likely includes which of the following? Select all that apply. A) The patient was diagnosed with sensorineural hearing loss. B) The patients hearing did not improve appreciably with the use of hearing aids. C) The patient has deficits in peripheral nervous function. D) The patients hearing deficit is likely accompanied by a cognitive deficit. E) The patient is unable to lip-read. A, B Feedback: A cochlear implant is an auditory prosthesis used for people with profound sensorineural hearing loss bilaterally who do not benefit from conventional hearing aids. The need for a cochlear implant is not associated with deficits in peripheral nervous function, cognitive deficits, or an inability to lip-read. 24. A patient presents to the ED complaining of a sudden onset of incapacitating vertigo, with nausea and vomiting and tinnitus. The patient mentions to the nurse that she suddenly cannot hear very well. What would the nurse suspect the patients diagnosis will be? A) Ossiculitis B) Mnires disease C) Ototoxicity D) Labyrinthitis D Feedback: Labyrinthitis is characterized by a sudden onset of incapacitating vertigo, usually with nausea and vomiting, various degrees of hearing loss, and possibly tinnitus. None of the other listed diagnosis is characterized by a rapid onset of symptoms. 25. Which of the following nurses actions carries the greatest potential to prevent hearing loss due to ototoxicity? A) Ensure that patients understand the differences between sensory hearing loss and conductive hearing loss. B) Educate patients about expected age-related changes in hearing perception. C) Educate patients about the risks associated with prolonged exposure to environmental noise. D) Be aware of patients medication regimens and collaborate with other professionals accordingly. D Feedback: A variety of medications may have adverse effects on the cochlea, vestibular apparatus, or cranial nerve VIII. All but a few, such as aspirin and quinine, cause irreversible hearing loss. Ototoxicity is not related to age-related changes, noise exposure, or the differences between types of hearing loss. 26. A child goes to the school nurse and complains of not being able to hear the teacher. What test could the school nurse perform that would preliminarily indicate hearing loss? A) Audiometry B) Rinne test C) Whisper test D) Weber test C Feedback: A general estimate of hearing can be made by assessing the patients ability to hear a whispered phrase or a ticking watch, testing one ear at a time. The Rinne and Weber tests distinguish sensorineural from conductive hearing loss. These tests, as well as audiometry, are not usually performed by a registered nurse in a general practice setting. 27. A nurse is teaching preventative measures for otitis externa to a group of older adults. What action should the nurse encourage? A) Rinsing the ears with normal saline after swimming B) Avoiding loud environmental noises C) Instilling antibiotic ointments on a regular basis D) Avoiding the use of cotton swabs D Feedback: Nurses should instruct patients not to clean the external auditory canal with cotton-tipped applicators and to avoid events that traumatize the external canal such as scratching the canal with the fingernail or other objects. Environmental noise should be avoided, but this does not address the risk for ear infection. Routine use of antibiotics is not encouraged and rinsing the ears after swimming is not recommended. 28. The nurse is reviewing the health history of a newly admitted patient and reads that the patient has been previously diagnosed with exostoses. How should the nurse accommodate this fact into the patients plan of care? A) The nurse should perform the Rinne and Weber tests. B) The nurse should arrange for audiometry testing as soon as possible. C) The nurse should collaborate with the pharmacist to assess for potential ototoxic medications. D) No specific assessments or interventions are necessary to addressing exostoses. D Feedback: Exostoses are small, hard, bony protrusions found in the lower posterior bony portion of the ear canal; they usually occur bilaterally. They do not normally impact hearing and no treatments or nursing actions are usually necessary. 29. The nurse is caring for a patient who has undergone a mastoidectomy. In an effort to prevent postoperative infection, what intervention should the nurse implement? A) Teach the patient about the risks of ototoxic medications. B) Instruct the patient to protect the ear from water for several weeks. C) Teach the patient to remove cerumen safely at least once per week. D) Instruct the patient to protect the ear from temperature extremes until healing is complete. B Feedback: To prevent infection, the patient is instructed to prevent water from entering the external auditory canal for 6 weeks. Ototoxic medications and temperature extremes do not present a risk for infection. Removal of cerumen during the healing process should be avoided due to the possibility of trauma. 30. A patient is being discharged home after mastoid surgery. What topic should the nurse address in the patients discharge education? A) Expected changes in facial nerve function B) The need for audiometry testing every 6 months following recovery C) Safe use of analgesics and antivertiginous agents D) Appropriate use of OTC ear drops C Feedback: Patients require instruction about medication therapy, such as analgesics and antivertiginous agents (e.g., antihistamines) prescribed for balance disturbance. OTC ear drops are not recommended and changes in facial nerve function are signs of a complication that needs to be addressed promptly. There is no need for serial audiometry testing. 31. After mastoid surgery, an 81-year-old patient has been identified as needing assistance in her home. What would be a primary focus of this patients home care? A) Preparation of nutritious meals and avoidance of contraindicated foods B) Ensuring the patient receives adequate rest each day C) Helping the patient adapt to temporary hearing loss D) Assisting the patient with ambulation as needed to avoid falling D Feedback: The caregiver and patient are cautioned that the patient may experience some vertigo and will therefore require help with ambulation to avoid falling. The patient should not be expected to experience hearing loss and no foods are contraindicated. Adequate rest is needed, but this is not a primary focus of home care. 32. A hearing-impaired patient is scheduled to have an MRI. What would be important for the nurse to remember when caring for this patient? A) Patient is likely unable to hear the nurse during test. B) A person adept in sign language must be present during test. C) Lip reading will be the method of communication that is necessary. D) The nurse should interact with the patient like any other patient. A Feedback: During health care and screening procedures, the practitioner (e.g., dentist, physician, nurse) must be aware that patients who are deaf or hearing-impaired are unable to read lips, see a signer, or read written materials in the dark rooms required during some diagnostic tests. The same situation exists if the practitioner is wearing a mask or not in sight (e.g., x-ray studies, MRI, colonoscopy). 33. The nurse and a colleague are performing the Epley maneuver with a patient who has a diagnosis of benign paroxysmal positional vertigo. The nurses should begin this maneuver by performing what action? A) Placing the patient in a prone position B) Assisting the patient into a sitting position C) Instilling 15 mL of warm normal saline into one of the patients ears D) Assessing the patients baseline hearing by performing the whisper test B Feedback: The Epley maneuver is performed by placing the patient in a sitting position, turning the head to a 45- degree angle on the affected side, and then quickly moving the patient to the supine position. Saline is not instilled into the ears and there is no need to assess hearing before the test. 34. A 6-month-old infant is brought to the ED by his parents for inconsolable crying and pulling at his right ear. When assessing this infant, the advanced practice nurse is aware that the tympanic membrane should be what color in a healthy ear? A) Yellowish-white B) Pink C) Gray D) Bluish-white C Feedback: The healthy tympanic membrane appears pearly gray and is positioned obliquely at the base of the ear canal. Any other color is suggestive of a pathological process. 35. A child has been experiencing recurrent episodes of acute otitis media (AOM). The nurse should anticipate that what intervention is likely to be ordered? A) Ossiculoplasty B) Insertion of a cochlear implant C) Stapedectomy D) Insertion of a ventilation tube D Feedback: If AOM recurs and there is no contraindication, a ventilating, or pressure-equalizing, tube may be inserted. The ventilating tube, which temporarily takes the place of the eustachian tube in equalizing pressure, is retained for 6 to 18 months. Ossiculoplasty is not used to treat AOM and stapedectomy is performed to treat otosclerosis. Cochlear implants are used to treat sensorineural hearing loss. 36. An older adult with a recent history of mixed hearing loss has been diagnosed with a cholesteatoma. What should this patient be taught about this diagnosis? Select all that apply A) Cholesteatomas are benign and self-limiting, and hearing loss will resolve spontaneously. B) Cholesteatomas are usually the result of metastasis from a distant tumor site. C) Cholesteatomas are often the result of chronic otitis media. D) Cholesteatomas, if left untreated, result in intractable neuropathic pain. E) Cholesteatomas usually must be removed surgically. C, E Feedback: Cholesteatoma is a tumor of the external layer of the eardrum into the middle ear, often resulting from chronic otitis media. They usually do not cause pain; however, if treatment or surgery is delayed, they may burst or destroy the mastoid bone. They are not normally the result of metastasis and are not self- limiting. 37. The nurse is admitting a patient to the unit who is scheduled to have an ossiculoplasty. What postoperative assessment will best determine whether the procedure has been successful? A) Otoscopy B) Audiometry C) Balance testing D) Culture and sensitivity testing of ear discharge B Feedback: Ossiculoplasty is the surgical reconstruction of the middle ear bones to restore hearing. Consequently, results are assessed by testing hearing, not by visualizing the ear, testing balance, or culturing ear discharge. 38. On otoscopy, a red blemish behind the tympanic membrane is suggestive of what diagnosis? A) Acoustic tumor B) Cholesteatoma C) Facial nerve neuroma D) Glomus tympanicum D Feedback: In the case of glomus tympanicum, a red blemish on or behind the tympanic membrane is seen on otoscopy. This assessment finding is not associated with an acoustic tumor, facial nerve neuroma, or cholesteatoma. 39. The nurse is discharging a patient home after mastoid surgery. What should the nurse include in discharge teaching? A) Try to induce a sneeze every 4 hours to equalize pressure. B) Be sure to exercise to reduce fatigue. C) Avoid sleeping in a side-lying position. D) Dont blow your nose for 2 to 3 weeks. D Feedback: The patient is instructed to avoid heavy lifting, straining, exertion, and nose blowing for 2 to 3 weeks after surgery to prevent dislodging the tympanic membrane graft or ossicular prosthesis. Side-lying is not contraindicated; sneezing could cause trauma. 40. An advanced practice nurse has performed a Rinne test on a new patient. During the test, the patient reports that air-conducted sound is louder than bone-conducted sound. How should the nurse best interpret this assessment finding? A) The patients hearing is likely normal. B) The patient is at risk for tinnitus. C) The patient likely has otosclerosis. D) The patient likely has sensorineural hearing loss. A Feedback: The Rinne test is useful for distinguishing between conductive and sensorineural hearing loss. A person with normal hearing reports that air-conducted sound is louder than bone-conducted sound. Chapter 65: Assessment of Neurologic Function 1. A patient is brought to the ER following a motor vehicle accident in which he sustained head trauma. Preliminary assessment reveals a vision deficit in the patients left eye. The nurse should associate this abnormal finding with trauma to which of the following cerebral lobes? A) Temporal B) Occipital C) Parietal D) Frontal B Feedback: The posterior lobe of the cerebral hemisphere is responsible for visual interpretation. The temporal lobe contains the auditory receptive areas. The parietal lobe contains the primary sensory cortex, and is essential to an individuals awareness of the body in space, as well as orientation in space and spatial relations. The frontal lobe functions in concentration, abstract thought, information storage or memory, and motor function. 2. A patient scheduled for magnetic resonance imaging (MRI) has arrived at the radiology department. The nurse who prepares the patient for the MRI should prioritize which of the following actions? A) Withholding stimulants 24 to 48 hours prior to exam B) Removing all metal-containing objects C) Instructing the patient to void prior to the MRI D) Initiating an IV line for administration of contrast B Feedback: Patient preparation for an MRI consists of removing all metal-containing objects prior to the examination. Withholding stimulants would not affect an MRI; this relates to an electroencephalography (EEG). Instructing the patient to void is patient preparation for a lumbar puncture. Initiating an IV line for administration of contrast would be done if the patient was having a CT scan with contrast. 3. A gerontologic nurse planning the neurologic assessment of an older adult is considering normal, age- related changes. Of what phenomenon should the nurse be aware? A) Hyperactive deep tendon reflexes B) Reduction in cerebral blood flow C) Increased cerebral metabolism D) Hypersensitivity to painful stimuli B Feedback: Reduction in cerebral blood flow (CBF) is a change that occurs in the normal aging process. Deep tendon reflexes can be decreased or, in some cases, absent. Cerebral metabolism decreases as the patient advances in age. Reaction to painful stimuli may be decreased with age. Because pain is an important warning signal, caution must be used when hot or cold packs are used. 4. The nurse has admitted a new patient to the unit. One of the patients admitting orders is for an adrenergic medication. The nurse knows that this medication will have what effect on the circulatory system? A) Thin, watery saliva B) Increased heart rate C) Decreased BP D) Constricted bronchioles B Feedback: The term adrenergic refers to the sympathetic nervous system. Sympathetic effects include an increased rate and force of the heartbeat. Cholinergic effects, which correspond to the parasympathetic division of the autonomic nervous system, include thin, watery saliva, decreased rate and force of heartbeat, and decreased BP. 5. A nurse is assessing reflexes in a patient with hyperactive reflexes. When the patients foot is abruptly dorsiflexed, it continues to beat two to three times before settling into a resting position. How would the nurse document this finding? A) Rigidity B) Flaccidity C) Clonus D) Ataxia C Feedback: When reflexes are very hyperactive, a phenomenon called clonus may be elicited. If the foot is abruptly dorsiflexed, it may continue to beat two to three times before it settles into a position of rest. Rigidity is an increase in muscle tone at rest characterized by increased resistance to passive stretch. Flaccidity is lack of muscle tone. Ataxia is the inability to coordinate muscle movements, resulting in difficulty walking, talking, and performing self-care activities. 6. The nurse is doing an initial assessment on a patient newly admitted to the unit with a diagnosis of cerebrovascular accident (CVA). The patient has difficulty copying a figure that the nurse has drawn and is diagnosed with visual-receptive aphasia. What brain region is primarily involved in this deficit? A) Temporal lobe B) Parietal-occipital area C) Inferior posterior frontal areas D) Posterior frontal area B Feedback: Difficulty copying a figure that the nurse has drawn would be considered visual-receptive aphasia, which involves the parietal-occipital area. Expressive aphasia, the inability to express oneself, is often associated with damage to the frontal area. Receptive aphasia, the inability to understand what someone else is saying, is often associated with damage to the temporal lobe area. 7. What term is used to describe the fibrous connective tissue that hugs the brain closely and extends into every fold of the brains surface? A) Dura mater B) Arachnoid C) Fascia D) Pia mater D Feedback: The term meninges describes the fibrous connective tissue that covers the brain and spinal cord. The meninges have three layers, the dura mater, arachnoid, and pia mater. The pia mater is the innermost membrane that hugs the brain closely and extends into every fold of the brains surface. The dura mater, the outermost layer, covers the brain and spinal cord. The arachnoid, the middle membrane, is responsible for the production of cerebrospinal fluid. 8. The nurse is caring for a patient with an upper motor neuron lesion. What clinical manifestations should the nurse anticipate when planning the patients neurologic assessment? A) Decreased muscle tone B) Flaccid paralysis C) Loss of voluntary control of movement D) Slow reflexes C Feedback: Upper motor neuron lesions do not cause muscle atrophy, flaccid paralysis, or slow reflexes. However, upper motor neuron lesions normally cause loss of voluntary control. 9. The nurse is admitting a patient to the unit who is diagnosed with a lower motor neuron lesion. What entry in the patients electronic record is most consistent with this diagnosis? A) Patient exhibits increased muscle tone. B) Patient demonstrates normal muscle structure with no evidence of atrophy. C) Patient demonstrates hyperactive deep tendon reflexes. D) Patient demonstrates an absence of deep tendon reflexes. D Feedback: Lower motor neuron lesions cause flaccid muscle paralysis, muscle atrophy, decreased muscle tone, and loss of voluntary control. 10. An elderly patient is being discharged home. The patient lives alone and has atrophy of his olfactory organs. The nurse tells the patients family that it is essential that the patient have what installed in the home? A) Grab bars B) Nonslip mats C) Baseboard heaters D) A smoke detector D Feedback: The sense of smell deteriorates with age. The olfactory organs are responsible for smell. This may present a safety hazard for the patient because he or she may not smell smoke or gas leaks. Smoke detectors are universally necessary, but especially for this patient. 11. The patient in the ED has just had a diagnostic lumbar puncture. To reduce the incidence of a post- lumbar puncture headache, what is the nurses most appropriate action? A) Position the patient prone. B) Position the patient supine with the head of bed flat. C) Position the patient left side-lying. D) Administer acetaminophen as ordered. A Feedback: The lumbar puncture headache may be avoided if a small-gauge needle is used and if the patient remains prone after the procedure. Acetaminophen is not administered as a preventative measure for post-lumbar puncture headaches. 12. The nurse is conducting a focused neurologic assessment. When assessing the patients cranial nerve function, the nurse would include which of the following assessments? A) Assessment of hand grip B) Assessment of orientation to person, time, and place C) Assessment of arm drift D) Assessment of gag reflex D Feedback: The gag reflex is governed by the glossopharyngeal nerve, one of the cranial nerves. Hand grip and arm drifting are part of motor function assessment. Orientation is an assessment parameter related to a mental status examination. 13. A nurse is caring for a patient diagnosed with Mnires disease. While completing a neurologic examination on the patient, the nurse assesses cranial nerve VIII. The nurse would be correct in identifying the function of this nerve as what? A) Movement of the tongue B) Visual acuity C) Sense of smell D) Hearing and equilibrium D Feedback: Cranial nerve VIII (acoustic) is responsible for hearing and equilibrium. Cranial nerve XII (hypoglossal) is responsible for movement of the tongue. Cranial nerve II (optic) is responsible for visual acuity and visual fields. Cranial nerve I (olfactory) functions in sense of smell. 14. A patient exhibiting an uncoordinated gait has presented at the clinic. Which of the following is the most plausible cause of this patients health problem? A) Cerebellar dysfunction B) A lesion in the pons C) Dysfunction of the medulla D) A hemorrhage in the midbrain A Feedback: The cerebellum controls fine movement, balance, position sense, and integration of sensory input. Portions of the pons control the heart, respiration, and blood pressure. Cranial nerves IX through XII connect to the brain in the medulla. Cranial nerves III and IV originate in the midbrain. 15. The nursing students are learning how to assess function of cranial nerve VIII. To assess the function of cranial nerve VIII the students would be correct in completing which of the following assessment techniques? A) Have the patient identify familiar odors with the eyes closed. B) Assess papillary reflex. C) Utilize the Snellen chart. D) Test for air and bone conduction (Rinne test). D Feedback: Cranial nerve VIII is the acoustic nerve. It functions in hearing and equilibrium. When assessing this nerve, the nurse would test for air and bone conduction (Rinne) with a tuning fork. Assessment of papillary reflex would be completed for cranial nerves III (oculomotor), IV (trochlear), and VI (abducens). The Snellen chart would be used to assess cranial nerve II (optic). 16. A patient is being given a medication that stimulates her parasympathetic system. Following administration of this medication, the nurse should anticipate what effect? A) Constricted pupils B) Dilated bronchioles C) Decreased peristaltic movement D) Relaxed muscular walls of the urinary bladder A Feedback: Parasympathetic stimulation results in constricted pupils, constricted bronchioles, increased peristaltic movement, and contracted muscular walls of the urinary bladder. 17. A patient with lower back pain is scheduled for myelography using metrizamide (a water-soluble contrast dye). After the test, the nurse should prioritize what action? A) Positioning the patient with the head of the bed elevated 45 degrees B) Administering IV morphine sulfate to prevent headache C) Limiting fluids for the next 12 hours D) Helping the patient perform deep breathing and coughing exercises A Feedback: After myelography, the patient lies in bed with the head of the bed elevated 30 to 45 degrees. The patient is advised to remain in bed in the recommended position for 3 hours or as prescribed. Drinking liberal amounts of fluid for rehydration and replacement of CSF may decrease the incidence of postlumbar puncture headache. Deep breathing and coughing exercises are not normally necessary since there is no consequent risk of atelectasis. 18. A patient is having a fight or flight response after receiving bad news about his prognosis. What affect will this have on the patients sympathetic nervous system? A) Constriction of blood vessels in the heart muscle B) Constriction of bronchioles C) Increase in the secretion of sweat D) Constriction of pupils C Feedback: Sympathetic nervous system stimulation results in dilated blood vessels in the heart and skeletal muscle, dilated bronchioles, increased secretion of sweat, and dilated pupils. 19. The nurse educator is reviewing the assessment of cranial nerves. What should the educator identify as the specific instances when cranial nerves should be assessed? Select all that apply. A) When a neurogenic bladder develops B) When level of consciousness is decreased C) With brain stem pathology D) In the presence of peripheral nervous system disease E) When a spinal reflex is interrupted B, C, D Feedback: Cranial nerves are assessed when level of consciousness is decreased, with brain stem pathology, or in the presence of peripheral nervous system disease. Abnormalities in muscle tone and involuntary movements are less likely to prompt the assessment of cranial nerves, since these nerves do not directly mediate most aspects of muscle tone and movement. 20. A patient in the OR goes into malignant hyperthermia due to an abnormal reaction to the anesthetic. The nurse knows that the area of the brain that regulates body temperature is which of the following? A) Cerebellum B) Thalamus C) Hypothalamus D) Midbrain C Feedback: The hypothalamus plays an important role in the endocrine system because it regulates the pituitary secretion of hormones that influence metabolism, reproduction, stress response, and urine production. It works with the pituitary to maintain fluid balance through hormonal release and maintains temperature regulation by promoting vasoconstriction or vasodilatation. The cerebellum, thalamus, and midbrain and not directly involved in temperature regulation. 21. The nurse is planning the care of a patient with Parkinsons disease. The nurse should be aware that treatment will focus on what pathophysiological phenomenon? A) Premature degradation of acetylcholine B) Decreased availability of dopamine C) Insufficient synthesis of epinephrine D) Delayed reuptake of serotonin B Feedback: Parkinsons disease develops from decreased availability of dopamine, not acetylcholine, epinephrine, or serotonin. 22. A patient is admitted to the medical unit with an exacerbation of multiple sclerosis. When assessing this patient, the nurse has the patient stick out her tongue and move it back and forth. What is the nurse assessing? A) Function of the hypoglossal nerve B) Function of the vagus nerve C) Function of the spinal nerve D) Function of the trochlear nerve A Feedback: The hypoglossal nerve is the 12th cranial nerve. It is responsible for movement of the tongue. None of the other listed nerves affects motor function in the tongue. 23. A trauma patient was admitted to the ICU with a brain injury. The patient had a change in level of consciousness, increased vital signs, and became diaphoretic and agitated. The nurse should recognize which of the following syndromes as the most plausible cause of these symptoms? A) Adrenal crisis B) Hypothalamic collapse C) Sympathetic storm D) Cranial nerve deficit C Feedback: Sympathetic storm is a syndrome associated with changes in level of consciousness, altered vital signs, diaphoresis, and agitation that may result from hypothalamic stimulation of the sympathetic nervous system following traumatic brain injury. Alterations in cranial nerve or adrenal function would not have this result. 24. Assessment is crucial to the care of patients with neurologic dysfunction. What does accurate and appropriate assessment require? Select all that apply. A) The ability to select mediations for the neurologic dysfunction B) Understanding of the tests used to diagnose neurologic disorders C) Knowledge of nursing interventions related to assessment and diagnostic testing D) Knowledge of the anatomy of the nervous system E) The ability to interpret the results of diagnostic tests B, C, D Feedback: Assessment requires knowledge of the anatomy and physiology of the nervous system and an understanding of the array of tests and procedures used to diagnose neurologic disorders. Knowledge about the nursing implications and interventions related to assessment and diagnostic testing is also essential. Selecting medications and interpreting diagnostic tests are beyond the normal scope of the nurse. 25. When caring for a patient with an altered level of consciousness, the nurse is preparing to test cranial nerve VII. What assessment technique would the nurse use to elicit a response from cranial nerve VII? A) Palpate trapezius muscle while patient shrugs should against resistance. B) Administer the whisper or watch-tick test. C) Observe for facial movement symmetry, such as a smile. D) Note any hoarseness in the patients voice. C Feedback: Cranial nerve VII is the facial nerve. An appropriate assessment technique for this cranial nerve would include observing for symmetry while the patient performs facial movements: smiles, whistles, elevates eyebrows, and frowns. Palpating and noting strength of the trapezius muscle while the patient shrugs shoulders against resistance would be completed to assess cranial nerve XI (spinal accessory). Assessing cranial nerve VIII (acoustic) would involve using the whisper or watch-tick test to evaluate hearing. Noting any hoarseness in the patients voice would involve assessment of cranial nerve X (vagus). 26. The nurse is caring for a patient who exhibits abnormal results of the Weber test and Rinne test. The nurse should suspect dysfunction involving what cranial nerve? A) Trigeminal B) Acoustic C) Hypoglossal D) Trochlear B Feedback: Abnormal hearing can correlate with damage to cranial nerve VIII (acoustic). The acoustic nerve functions in hearing and equilibrium. The trigeminal nerve functions in facial sensation, corneal reflex, and chewing. The hypoglossal nerve moves the tongue. The trochlear nerve controls muscles that move the eye. 27. The nurse caring for an 80 year-old patient knows that she has a pre-existing history of dulled tactile sensation. The nurse should first consider what possible cause for this patients diminished tactile sensation? A) Damage to cranial nerve VIII B) Adverse medication effects C) Age-related neurologic changes D) An undiagnosed cerebrovascular accident in early adulthood C Feedback: Tactile sensation is dulled in the elderly person due to a decrease in the number of sensory receptors. While thorough assessment is necessary, it is possible that this change is unrelated to pathophysiological processes. 28. A 72-year-old man has been brought to his primary care provider by his daughter, who claims that he has been experiencing uncharacteristic lapses in memory. What principle should underlie the nurses assessment and management of this patient? A) Loss of short-term memory is normal in older adults, but loss of long-term memory is pathologic. B) Lapses in memory in older adults are considered benign unless they have negative consequences. C) Gradual increases in confusion accompany the aging process. D) Thorough assessment is necessary because changes in cognition are always considered to be pathologic. D Feedback: Although mental processing time decreases with age, memory, language, and judgment capacities remain intact. Change in mental status should never be assumed to be a normal part of aging. 29. A gerontologic nurse educator is providing practice guidelines to unlicensed care providers. Because reaction to painful stimuli is sometimes blunted in older adults, what must be used with caution? A) Hot or cold packs B) Analgesics C) Anti-inflammatory medications D) Whirlpool baths A Feedback: Reaction to painful stimuli may be decreased with age. Because pain is an important warning signal, caution must be used when hot or cold packs are used. The older patient may be burned or suffer frostbite before being aware of any discomfort. Any medication is used with caution in the elderly, but not because of the decreased sense of heat or cold. Whirlpool baths are generally not a routine treatment ordered for the elderly. 30. A trauma patient in the ICU has been declared brain dead. What diagnostic test is used in making the determination of brain death? A) Magnetic resonance imaging (MRI) B) Electroencephalography (EEG) C) Electromyelography (EMG) D) Computed tomography (CT) B Feedback: The EEG can be used in determining brain death. MRI, CT, and EMG are not normally used in determining brain death. 31. A patient is scheduled for CT scanning of the head because of a recent onset of neurologic deficits. What should the nurse tell the patient in preparation for this test? A) No metal objects can enter the procedure room. B) You need to fast for 8 hours prior to the test. C) You will need to lie still throughout the procedure. D) There will be a lot of noise during the test. C Feedback: Preparation for CT scanning includes teaching the patient about the need to lie quietly throughout the procedure. If the patient were having an MRI, metal and noise would be appropriate teaching topics. There is no need to fast prior to a CT scan of the brain. 32. A patient for whom the nurse is caring has positron emission tomography (PET) scheduled. In preparation, what should the nurse explain to the patient? A) The test will temporarily limit blood flow through the brain. B) An allergy to iodine precludes getting the radio-opaque dye. C) The patient will need to endure loud noises during the test. D) The test may result in dizziness or lightheadedness. D Feedback: Key nursing interventions for PET scan include explaining the test and teaching the patient about inhalation techniques and the sensations (e.g., dizziness, light-headedness, and headache) that may occur. A PET scan does not impede blood flow through the brain. An allergy to iodine precludes the dye for an MRI, and loud noise is heard in an MRI. 33. A patient is scheduled for a myelogram and the nurse explains to the patient that this is an invasive procedure, which assesses for any lesions in the spinal cord. The nurse should explain that the preparation is similar to which of the following neurologic tests? A) Lumbar puncture B) MRI C) Cerebral angiography D) EEG A Feedback: A myelogram is an x-ray of the spinal subarachnoid space taken after the injection of a contrast agent into the spinal subarachnoid space through a lumbar puncture. Patient preparation for a myelogram would be similar to that for lumbar puncture. The other listed diagnostic tests do not involve lumbar puncture. 34. The physician has ordered a somatosensory evoked responses (SERs) test for a patient for whom the nurse is caring. The nurse is justified in suspecting that this patient may have a history of what type of neurologic disorder? A) Hypothalamic disorder B) Demyelinating disease C) Brainstem deficit D) Diabetic neuropathy B Feedback: SERs are used to detect deficits in the spinal cord or peripheral nerve conduction and to monitor spinal cord function during surgical procedures. The test is also useful in the diagnosis of demyelinating diseases, such as multiple sclerosis and polyneuropathies, where nerve conduction is slowed. The test is not done to diagnose hypothalamic disorders, brainstem deficits, or diabetic neuropathies. 35. A patient had a lumbar puncture performed at the outpatient clinic and the nurse has phoned the patient and family that evening. What does this phone call enable the nurse to determine? A) What are the patients and familys expectations of the test B) Whether the patients family had any questions about why the test was necessary C) Whether the patient has had any complications of the test D) Whether the patient understood accurately why the test was done C Feedback: Contacting the patient and family after diagnostic testing enables the nurse to determine whether they have any questions about the procedure or whether the patient had any untoward results. The other listed information should have been elicited from the patient and family prior to the test. 36. A patient is currently being stimulated by the parasympathetic nervous system. What effect will this nervous stimulation have on the patients bladder? A) The parasympathetic nervous system causes urinary retention. B) The parasympathetic nervous system causes bladder spasms. C) The parasympathetic nervous system causes urge incontinence. D) The parasympathetic nervous system makes the bladder contract. D Feedback: The parasympathetic division of the nervous system causes contraction (stimulation) of the urinary bladder muscles and a decrease (inhibition) in heart rate, whereas the sympathetic division produces relaxation (inhibition) of the urinary bladder and an increase (stimulation) in the rate and force of the heartbeat. 37. The nurse is performing a neurologic assessment of a patient whose injuries have rendered her unable to follow verbal commands. How should the nurse proceed with assessing the patients level of consciousness (LOC)? A) Assess the patients vital signs and correlate these with the patients baselines. B) Assess the patients eye opening and response to stimuli. C) Document that the patient currently lacks a level of consciousness. D) Facilitate diagnostic testing in an effort to obtain objective data. B Feedback: If the patient is not alert or able to follow commands, the examiner observes for eye opening; verbal response and motor response to stimuli, if any; and the type of stimuli needed to obtain a response. Vital signs and diagnostic testing are appropriate, but neither will allow the nurse to gauge the patients LOC. Inability to follow commands does not necessarily denote an absolute lack of consciousness. 38. In the course of a focused neurologic assessment, the nurse is palpating the patients major muscle groups at rest and during passive movement. Data gleaned from this assessment will allow the nurse to describe which of the following aspects of neurologic function? A) Muscle dexterity B) Muscle tone C) Motor symmetry D) Deep tendon reflexes B Feedback: Muscle tone (the tension present in a muscle at rest) is evaluated by palpating various muscle groups at rest and during passive movement. Data from this assessment do not allow the nurse to ascertain the patients dexterity, reflexes, or motor symmetry. 39. The neurologic nurse is testing the function of a patients cerebellum and basal ganglia. What action will most accurately test these structures? A) Have the patient identify the location of a cotton swab on his or her skin with the eyes closed. B) Elicit the patients response to a hypothetical problem. C) Ask the patient to close his or her eyes and discern between hot and cold stimuli. D) Guide the patient through the performance of rapid, alternating movements. D Feedback: Cerebellar and basal ganglia influence on the motor system is reflected in balance control and coordination. Coordination in the hands and upper extremities is tested by having the patient perform rapid, alternating movements and point-to-point testing. The cerebellum and basal ganglia do not mediate cutaneous sensation or judgment. 40. During the performance of the Romberg test, the nurse observes that the patient sways slightly. What is the nurses most appropriate action? A) Facilitate a referral to a neurologist. B) Reposition the patient supine to ensure safety. C) Document successful completion of the assessment. D) Follow up by having the patient perform the Rinne test. C Feedback: Slight swaying during the Romberg test is normal, but a loss of balance is abnormal and is considered a positive Romberg test. Slight swaying is not a significant threat to the patients safety. The Rinne test assesses hearing, not balance. Chapter 66: Management of Patients with Neurologic Dysfunction 1. A patient is being admitted to the neurologic ICU following an acute head injury that has resulted in cerebral edema. When planning this patients care, the nurse would expect to administer what priority medication? A) Hydrochlorothiazide (HydroDIURIL) B) Furosemide (Lasix) C) Mannitol (Osmitrol) D) Spirolactone (Aldactone) C Feedback: The osmotic diuretic mannitol is given to dehydrate the brain tissue and reduce cerebral edema. This drug acts by reducing the volume of brain and extracellular fluid. Spirolactone, furosemide, and hydrochlorothiazide are diuretics that are not typically used in the treatment of increased ICP resulting from cerebral edema. 2. The nurse is providing care for a patient who is unconscious. What nursing intervention takes highest priority? A) Maintaining accurate records of intake and output B) Maintaining a patent airway C) Inserting a nasogastric (NG) tube as ordered D) Providing appropriate pain control B Feedback: Maintaining a patent airway always takes top priority, even though each of the other listed actions is necessary and appropriate. 3. The nurse is caring for a patient in the ICU who has a brain stem herniation and who is exhibiting an altered level of consciousness. Monitoring reveals that the patients mean arterial pressure (MAP) is 60 mm Hg with an intracranial pressure (ICP) reading of 5 mm Hg. What is the nurses most appropriate action? A) Position the patient in the high Fowlers position as tolerated. B) Administer osmotic diuretics as ordered. C) Participate in interventions to increase cerebral perfusion pressure. D) Prepare the patient for craniotomy. C Feedback: The cerebral perfusion pressure (CPP) is 55 mm Hg, which is considered low. The normal CPP is 70 to 100 mm Hg. Patients with a CPP of less than 50 mm Hg experience irreversible neurologic damage. As a result, interventions are necessary. A craniotomy is not directly indicated. Diuretics and increased height of bed would exacerbate the patients condition. 4. The nurse is caring for a patient who is postoperative following a craniotomy. When writing the plan of care, the nurse identifies a diagnosis of deficient fluid volume related to fluid restriction and osmotic diuretic use. What would be an appropriate intervention for this diagnosis? A) Change the patients position as indicated. B) Monitor serum electrolytes. C) Maintain NPO status. D) Monitor arterial blood gas (ABG) values. B Feedback: The postoperative fluid regimen depends on the type of neurosurgical procedure and is determined on an individual basis. The volume and composition of fluids are adjusted based on daily serum electrolyte values, along with fluid intake and output. Fluids may have to be restricted in patients with cerebral edema. Changing the patients position, maintaining an NPO status, and monitoring ABG values do not relate to the nursing diagnosis of deficient fluid volume. 5. A patient with a documented history of seizure disorder experiences a generalized seizure. What nursing action is most appropriate? A) Restrain the patient to prevent injury. B) Open the patients jaws to insert an oral airway. C) Place patient in high Fowlers position. D) Loosen the patients restrictive clothing. D Feedback: An appropriate nursing intervention would include loosening any restrictive clothing on the patient. No attempt should be made to restrain the patient during the seizure because muscular contractions are strong and restraint can produce injury. Do not attempt to pry open jaws that are clenched in a spasm to insert anything. Broken teeth and injury to the lips and tongue may result from such an action. If possible, place the patient on one side with head flexed forward, which allows the tongue to fall forward and facilitates drainage of saliva and mucus. 6. A patient who has been on long-term phenytoin (Dilantin) therapy is admitted to the unit. In light of the adverse of effects of this medication, the nurse should prioritize which of the following in the patients plan of care? A) Monitoring of pulse oximetry B) Administration of a low-protein diet C) Administration of thorough oral hygiene D) Fluid restriction as ordered C Feedback: Gingival hyperplasia (swollen and tender gums) can be associated with long-term phenytoin (Dilantin) use. Thorough oral hygiene should be provided consistently and encouraged after discharge. Fluid and protein restriction are contraindicated and there is no particular need for constant oxygen saturation monitoring. 7. A nurse is admitting a patient with a severe migraine headache and a history of acute coronary syndrome. What migraine medication would the nurse question for this patient? A) Rizatriptan (Maxalt) B) Naratriptan (Amerge) C) Sumatriptan succinate (Imitrex) D) Zolmitriptan (Zomig) C Feedback: Triptans can cause chest pain and are contraindicated in patients with ischemic heart disease. Maxalt, Amerge, and Zomig are triptans used in routine clinical use for the treatment of migraine headaches. 8. The nurse is caring for a patient with increased intracranial pressure (ICP). The patient has a nursing diagnosis of ineffective cerebral tissue perfusion. What would be an expected outcome that the nurse would document for this diagnosis? A) Copes with sensory deprivation. B) Registers normal body temperature. C) Pays attention to grooming. D) Obeys commands with appropriate motor responses. D Feedback: An expected outcome of the diagnosis of ineffective cerebral tissue perfusion in a patient with increased intracranial pressure (ICP) would include obeying commands with appropriate motor responses. Vitals signs and neurologic status are assessed every 15 minutes to every hour. Coping with sensory deprivation would relate to the nursing diagnosis of disturbed sensory perception. The outcome of registers normal body temperature relates to the diagnosis of potential for ineffective thermoregulation. Body image disturbance would have a potential outcome of pays attention to grooming. 9. A patient exhibiting an altered level of consciousness (LOC) due to blunt-force trauma to the head is admitted to the ED. The physician determines the patients injury is causing increased intracranial pressure (ICP). The nurse should gauge the patients LOC on the results of what diagnostic tool? A) Monro-Kellie hypothesis B) Glasgow Coma Scale C) Cranial nerve function D) Mental status examination B Feedback: LOC, a sensitive indicator of neurologic function, is assessed based on the criteria in the Glasgow Coma Scale: eye opening, verbal response, and motor response. The Monro-Kellie hypothesis states that because of the limited space for expansion within the skull, an increase in any one of the components (blood, brain tissue, cerebrospinal fluid) causes a change in the volume of the others. Cranial nerve function and the mental status examination would be part of the neurologic examination for this patient, but would not be the priority in evaluating LOC. 10. While completing a health history on a patient who has recently experienced a seizure, the nurse would assess for what characteristic associated with the postictal state? A) Epileptic cry B) Confusion C) Urinary incontinence D) Body rigidity B Feedback: In the postictal state (after the seizure), the patient is often confused and hard to arouse and may sleep for hours. The epileptic cry occurs from the simultaneous contractions of the diaphragm and chest muscles that occur during the seizure. Urinary incontinence and intense rigidity of the entire body are followed by alternating muscle relaxation and contraction (generalized tonicclonic contraction) during the seizure. 11. A patient with increased ICP has a ventriculostomy for monitoring ICP. The nurses most recent assessment reveals that the patient is now exhibiting nuchal rigidity and photophobia. The nurse would be correct in suspecting the presence of what complication? A) Encephalitis B) CSF leak C) Meningitis D) Catheter occlusion C Feedback: Complications of a ventriculostomy include ventricular infectious meningitis and problems with the monitoring system. Nuchal rigidity and photophobia are clinical manifestations of meningitis, but are not suggestive of encephalitis, a CSF leak, or an occluded catheter. 12. The nurse is participating in the care of a patient with increased ICP. What diagnostic test is contraindicated in this patients treatment? A) Computed tomography (CT) scan B) Lumbar puncture C) Magnetic resonance imaging (MRI) D) Venous Doppler studies B Feedback: A lumbar puncture in a patient with increased ICP may cause the brain to herniate from the withdrawal of fluid and change in pressure during the lumbar puncture. Herniation of the brain is a dire and frequently fatal event. CT, MRI, and venous Doppler are considered noninvasive procedures and they would not affect the ICP itself. 13. The nurse is caring for a patient who is in status epilepticus. What medication does the nurse know may be given to halt the seizure immediately? A) Intravenous phenobarbital (Luminal) B) Intravenous diazepam (Valium) C) Oral lorazepam (Ativan) D) Oral phenytoin (Dilantin) B Feedback: Medical management of status epilepticus includes IV diazepam (Valium) and IV lorazepam (Ativan) given slowly in an attempt to halt seizures immediately. Other medications (phenytoin, phenobarbital) are given later to maintain a seizure-free state. Oral medications are not given during status epilepticus. 14. The nurse has created a plan of care for a patient who is at risk for increased ICP. The patients care plan should specify monitoring for what early sign of increased ICP? A) Disorientation and restlessness B) Decreased pulse and respirations C) Projectile vomiting D) Loss of corneal reflex A Feedback: Early indicators of ICP include disorientation and restlessness. Later signs include decreased pulse and respirations, projectile vomiting, and loss of brain stem reflexes, such as the corneal reflex. 15. The neurologic ICU nurse is admitting a patient following a craniotomy using the supratentorial approach. How should the nurse best position the patient? A) Position the patient supine. B) Maintain head of bed (HOB) elevated at 30 to 45 degrees. C) Position patient in prone position. D) Maintain bed in Trendelenberg position. B Feedback: The patient undergoing a craniotomy with a supratentorial (above the tentorium) approach should be placed with the HOB elevated 30 to 45 degrees, with the neck in neutral alignment. Each of the other listed positions would cause a dangerous elevation in ICP. 16. A clinic nurse is caring for a patient diagnosed with migraine headaches. During the patient teaching session, the patient questions the nurse regarding alcohol consumption. What would the nurse be correct in telling the patient about the effects of alcohol? A) Alcohol causes hormone fluctuations. B) Alcohol causes vasodilation of the blood vessels. C) Alcohol has an excitatory effect on the CNS. D) Alcohol diminishes endorphins in the brain. B Feedback: Alcohol causes vasodilation of the blood vessels and may exacerbate migraine headaches. Alcohol has a depressant effect on the CNS. Alcohol does not cause hormone fluctuations, nor does it decrease endorphins (morphine-like substances produced by the body) in the brain. 17. A patient has developed diabetes insipidus after having increased ICP following head trauma. What nursing assessment best addresses this complication? A) Vigilant monitoring of fluid balance B) Continuous BP monitoring C) Serial arterial blood gases (ABGs) D) Monitoring of the patients airway for patency A Feedback: Diabetes insipidus requires fluid and electrolyte replacement, along with the administration of vasopressin, to replace and slow the urine output. Because of these alterations in fluid balance, careful monitoring is necessary. None of the other listed assessments directly addresses the major manifestations of diabetes insipidus. 18. What should the nurse suspect when hourly assessment of urine output on a patient postcraniotomy exhibits a urine output from a catheter of 1,500 mL for two consecutive hours? A) Cushing syndrome B) Syndrome of inappropriate antidiuretic hormone (SIADH) C) Adrenal crisis D) Diabetes insipidus D Feedback: Diabetes insipidus is an abrupt onset of extreme polyuria that commonly occurs in patients after brain surgery. Cushing syndrome is excessive glucocorticoid secretion resulting in sodium and water retention. SIADH is the result of increased secretion of ADH; the patient becomes volume-overloaded, urine output diminishes, and serum sodium concentration becomes dilute. Adrenal crisis is undersecretion of glucocorticoids resulting in profound hypoglycemia, hypovolemia, and hypotension. 19. During the examination of an unconscious patient, the nurse observes that the patients pupils are fixed and dilated. What is the most plausible clinical significance of the nurses finding? A) It suggests onset of metabolic problems. B) It indicates paralysis on the right side of the body. C) It indicates paralysis of cranial nerve X. D) It indicates an injury at the midbrain level. D Feedback: Pupils that are fixed and dilated indicate injury at the midbrain level. This finding is not suggestive of unilateral paralysis, metabolic deficits, or damage to CN X. 20. Following a traumatic brain injury, a patient has been in a coma for several days. Which of the following statements is true of this patients current LOC? A) The patient occasionally makes incomprehensible sounds. B) The patients current LOC will likely become a permanent state. C) The patient may occasionally make nonpurposeful movements. D) The patient is incapable of spontaneous respirations. C Feedback: Coma is a clinical state of unarousable unresponsiveness in which no purposeful responses to internal or external stimuli occur, although nonpurposeful responses to painful stimuli and brain stem reflexes may be present. Verbal sounds, however, are atypical. Ventilator support may or may not be necessary. Comas are not permanent states. 21. The nurse is caring for a patient with permanent neurologic impairments resulting from a traumatic head injury. When working with this patient and family, what mutual goal should be prioritized? A) Achieve as high a level of function as possible. B) Enhance the quantity of the patients life. C) Teach the family proper care of the patient. D) Provide community assistance. A Feedback: The overarching goals of care are to achieve as high a level of function as possible and to enhance the quality of life for the patient with neurologic impairment and his or her family. This goal encompasses family and community participation. 22. The nurse is providing care for a patient who is withdrawing from heavy alcohol use. The nurse and other members of the care team are present at the bedside when the patient has a seizure. In preparation for documenting this clinical event, the nurse should note which of the following? A) The ability of the patient to follow instructions during the seizure. B) The success or failure of the care team to physically restrain the patient. C) The patients ability to explain his seizure during the postictal period. D) The patients activities immediately prior to the seizure. D Feedback: Before and during a seizure, the nurse observes the circumstances before the seizure, including visual, auditory, or olfactory stimuli; tactile stimuli; emotional or psychological disturbances; sleep; and hyperventilation. Communication with the patient is not possible during a seizure and physical restraint is not attempted. The patients ability to explain the seizure is not clinically relevant. 23. The nurse is caring for a patient whose recent health history includes an altered LOC. What should be the nurses first action when assessing this patient? A) Assessing the patients verbal response B) Assessing the patients ability to follow complex commands C) Assessing the patients judgment D) Assessing the patients response to pain A Feedback: Assessment of the patient with an altered LOC often starts with assessing the verbal response through determining the patients orientation to time, person, and place. In most cases, this assessment will precede each of the other listed assessments, even though each may be indicated. 24. The nurse caring for a patient in a persistent vegetative state is regularly assessing for potential complications. Complications of neurologic dysfunction for which the nurse should assess include which of the following? Select all that apply. A) Contractures B) Hemorrhage C) Pressure ulcers D) Venous thromboembolism E) Pneumonia A, C, D, E Feedback: Based on the assessment data, potential complications may include respiratory distress or failure, pneumonia, aspiration, pressure ulcer, deep vein thrombosis (DVT), and contractures. The pathophysiology of decreased LOC does not normally create a heightened risk for hemorrhage. 25. The nurse is caring for a patient with a brain tumor. What drug would the nurse expect to be ordered to reduce the edema surrounding the tumor? A) Solumedrol B) Dextromethorphan C) Dexamethasone D) Furosemide C Feedback: If a brain tumor is the cause of the increased ICP, corticosteroids (e.g., dexamethasone) help reduce the edema surrounding the tumor. Solumedrol, a steroid, and furosemide, a loop diuretic, are not the drugs of choice in this instance. Dextromethorphan is used in cough medicines. 26. The nurse is caring for a patient who sustained a moderate head injury following a bicycle accident. The nurses most recent assessment reveals that the patients respiratory effort has increased. What is the nurses most appropriate response? A) Inform the care team and assess for further signs of possible increased ICP. B) Administer bronchodilators as ordered and monitor the patients LOC. C) Increase the patients bed height and reassess in 30 minutes. D) Administer a bolus of normal saline as ordered. A Feedback: Increased respiratory effort can be suggestive of increasing ICP, and the care team should be promptly informed. A bolus of IV fluid will not address the problem. Repositioning the patient and administering bronchodilators are insufficient responses, even though these actions may later be ordered. 27. A patient has a poor prognosis after being involved in a motor vehicle accident resulting in a head injury. As the patients ICP increases and condition worsens, the nurse knows to assess for indications of approaching death. These indications include which of the following? A) Hemiplegia B) Dry mucous membranes C) Signs of internal bleeding D) Loss of brain stem reflexes D Feedback: Loss of brain stem reflexes, including pupillary, corneal, gag, and swallowing reflexes, is an ominous sign of approaching death. Dry mucous membranes, hemiplegia, and bleeding must be promptly addressed, but none of these is a common sign of impending death. 28. A patient has experienced a seizure in which she became rigid and then experienced alternating muscle relaxation and contraction. What type of seizure does the nurse recognize? A) Unclassified seizure B) Absence seizure C) Generalized seizure D) Focal seizure C Feedback: Generalized seizures often involve both hemispheres of the brain, causing both sides of the body to react. Intense rigidity of the entire body may occur, followed by alternating muscle relaxation and contraction (generalized tonicclonic contraction). This pattern of rigidity does not occur in patients who experience unclassified, absence, or focal seizures. 29. When caring for a patient with increased ICP the nurse knows the importance of monitoring for possible secondary complications, including syndrome of inappropriate antidiuretic hormone (SIADH). What nursing interventions would the nurse most likely initiate if the patient developed SIADH? A) Fluid restriction B) Transfusion of platelets C) Transfusion of fresh frozen plasma (FFP) D) Electrolyte restriction A Feedback: The nurse also assesses for complications of increased ICP, including diabetes insipidus, and SIADH. SIADH requires fluid restriction and monitoring of serum electrolyte levels. Transfusions are unnecessary. 30. The nurse is admitting a patient to the unit who is scheduled for removal of an intracranial mass. What diagnostic procedures might be included in this patients admission orders? Select all that apply. A) Transcranial Doppler flow study B) Cerebral angiography C) MRI D) Cranial radiography E) Electromyelography (EMG) A, B, C Feedback: Preoperative diagnostic procedures may include a CT scan to demonstrate the lesion and show the degree of surrounding brain edema, the ventricular size, and the displacement. An MRI scan provides information similar to that of a CT scan with improved tissue contrast, resolution, and anatomic definition. Cerebral angiography may be used to study a tumors blood supply or to obtain information about vascular lesions. Transcranial Doppler flow studies are used to evaluate the blood flow within intracranial blood vessels. Regular x-rays of the skull would not be diagnostic for an intracranial mass. An EMG would not be ordered prior to intracranial surgery to remove a mass. 31. A patient is recovering from intracranial surgery performed approximately 24 hours ago and is complaining of a headache that the patient rates at 8 on a 10-point pain scale. What nursing action is most appropriate? A) Administer morphine sulfate as ordered. B) Reposition the patient in a prone position. C) Apply a hot pack to the patients scalp. D) Implement distraction techniques. A Feedback: The patient usually has a headache after a craniotomy as a result of stretching and irritation of nerves in the scalp during surgery. Morphine sulfate may also be used in the management of postoperative pain in patients who have undergone a craniotomy. Prone positioning is contraindicated due to the consequent increase in ICP. Distraction would likely be inadequate to reduce pain and a hot pack may cause vasodilation and increased pain. 32. A patient is recovering from intracranial surgery that was performed using the transsphenoidal approach. The nurse should be aware that the patient may have required surgery on what neurologic structure? A) Cerebellum B) Hypothalamus C) Pituitary gland D) Pineal gland C Feedback: The transsphenoidal approach (through the mouth and nasal sinuses) is often used to gain access to the pituitary gland. This surgical approach would not allow for access to the pineal gland, cerebellum, or hypothalamus. 33. A patient is postoperative day 1 following intracranial surgery. The nurses assessment reveals that the patients LOC is slightly decreased compared with the day of surgery. What is the nurses best response to this assessment finding? A) Recognize that this may represent the peak of post-surgical cerebral edema. B) Alert the surgeon to the possibility of an intracranial hemorrhage. C) Understand that the surgery may have been unsuccessful. D) Recognize the need to refer the patient to the palliative care team. A Feedback: Some degree of cerebral edema occurs after brain surgery; it tends to peak 24 to 36 hours after surgery, producing decreased responsiveness on the second postoperative day. As such, there is not necessarily any need to deem the surgery unsuccessful or to refer the patient to palliative care. A decrease in LOC is not evidence of an intracranial hemorrhage. 34. A school nurse is called to the playground where a 6-year-old girl has been found unresponsive and staring into space, according to the playground supervisor. How would the nurse document the girls activity in her chart at school? A) Generalized seizure B) Absence seizure C) Focal seizure D) Unclassified seizure B Feedback: Staring episodes characterize an absence seizure, whereas focal seizures, generalized seizures, and unclassified seizures involve uncontrolled motor activity. 35. A neurologic nurse is reviewing seizures with a group of staff nurses. How should this nurse best describe the cause of a seizure? A) Sudden electrolyte changes throughout the brain B) A dysrhythmia in the peripheral nervous system C) A dysrhythmia in the nerve cells in one section of the brain D) Sudden disruptions in the blood flow throughout the brain C Feedback: The underlying cause of a seizure is an electrical disturbance (dysrhythmia) in the nerve cells in one section of the brain; these cells emit abnormal, recurring, uncontrolled electrical discharges. Seizures are not caused by changes in blood flow or electrolytes. 36. The nurse is caring for a patient who has undergone supratentorial removal of a pituitary mass. What medication would the nurse expect to administer prophylactically to prevent seizures in this patient? A) Prednisone B) Dexamethasone C) Cafergot D) Phenytoin D Feedback: Antiseizure medication (phenytoin, diazepam) is often prescribed prophylactically for patients who have undergone supratentorial craniotomy because of the high risk of seizures after this procedure. Prednisone and dexamethasone are steroids and do not prevent seizures. Cafergot is used in the treatment of migraines. 37. A hospital patient has experienced a seizure. In the immediate recovery period, what action best protects the patients safety? A) Place the patient in a side-lying position. B) Pad the patients bed rails. C) Administer antianxiety medications as ordered. D) Reassure the patient and family members. A Feedback: To prevent complications, the patient is placed in the side-lying position to facilitate drainage of oral secretions. Suctioning is performed, if needed, to maintain a patent airway and prevent aspiration. None of the other listed actions promotes safety during the immediate recovery period. 38. A nurse is caring for a patient who experiences debilitating cluster headaches. The patient should be taught to take appropriate medications at what point in the course of the onset of a new headache? A) As soon as the patients pain becomes unbearable B) As soon as the patient senses the onset of symptoms C) Twenty to 30 minutes after the onset of symptoms D) When the patient senses his or her symptoms peaking B Feedback: A migraine or a cluster headache in the early phase requires abortive medication therapy instituted as soon as possible. Delaying medication administration would lead to unnecessary pain. 39. A nurse is collaborating with the interdisciplinary team to help manage a patients recurrent headaches. What aspect of the patients health history should the nurse identify as a potential contributor to the patients headaches? A) The patient leads a sedentary lifestyle. B) The patient takes vitamin D and calcium supplements. C) The patient takes vasodilators for the treatment of angina. D) The patient has a pattern of weight loss followed by weight gain. C Feedback: Vasodilators are known to contribute to headaches. Weight fluctuations, sedentary lifestyle, and vitamin supplements are not known to have this effect. 40. An adult patient has sought care for the treatment of headaches that have become increasingly severe and frequent over the past several months. Which of the following questions addresses potential etiological factors? Select all that apply? A) Are you exposed to any toxins or chemicals at work? B) How would you describe your ability to cope with stress? C) What medications are you currently taking? D) When was the last time you were hospitalized? E) Does anyone else in your family struggle with headaches? A, B, C, E Feedback: Headaches are multifactorial, and may involve medications, exposure to toxins, family history, and stress. Hospitalization is an unlikely contributor to headaches. Chapter 67: Management of Patients with Cerebrovascular Disorders 1. A patient has had an ischemic stroke and has been admitted to the medical unit. What action should the nurse perform to best prevent joint deformities? A) Place the patient in the prone position for 30 minutes/day. B) Assist the patient in acutely flexing the thigh to promote movement. C) Place a pillow in the axilla when there is limited external rotation. D) Place patients hand in pronation. C Feedback: A pillow in the axilla prevents adduction of the affected shoulder and keeps the arm away from the chest. The prone position with a pillow under the pelvis, not flat, promotes hyperextension of the hip joints, essential for normal gait. To promote venous return and prevent edema, the upper thigh should not be flexed acutely. The hand is placed in slight supination, not pronation, which is its most functional position. 2. A patient diagnosed with transient ischemic attacks (TIAs) is scheduled for a carotid endarterectomy. The nurse explains that this procedure will be done for what purpose? A) To decrease cerebral edema B) To prevent seizure activity that is common following a TIA C) To remove atherosclerotic plaques blocking cerebral flow D) To determine the cause of the TIA C Feedback: The main surgical procedure for select patients with TIAs is carotid endarterectomy, the removal of an atherosclerotic plaque or thrombus from the carotid artery to prevent stroke in patients with occlusive disease of the extracranial arteries. An endarterectomy does not decrease cerebral edema, prevent seizure activity, or determine the cause of a TIA. 3. The nurse is discharging home a patient who suffered a stroke. He has a flaccid right arm and leg and is experiencing problems with urinary incontinence. The nurse makes a referral to a home health nurse because of an awareness of what common patient response to a change in body image? A) Denial B) Fear C) Depression D) Disassociation C Feedback: Depression is a common and serious problem in the patient who has had a stroke. It can result from a profound disruption in his or her life and changes in total function, leaving the patient with a loss of independence. The nurse needs to encourage the patient to verbalize feelings to assess the effect of the stroke on self-esteem. Denial, fear, and disassociation are not the most common patient response to a change in body image, although each can occur in some patients. 4. When caring for a patient who had a hemorrhagic stroke, close monitoring of vital signs and neurologic changes is imperative. What is the earliest sign of deterioration in a patient with a hemorrhagic stroke of which the nurse should be aware? A) Generalized pain B) Alteration in level of consciousness (LOC) C) Tonicclonic seizures D) Shortness of breath B Feedback: Alteration in LOC is the earliest sign of deterioration in a patient after a hemorrhagic stroke, such as mild drowsiness, slight slurring of speech, and sluggish papillary reaction. Sudden headache may occur, but generalized pain is less common. Seizures and shortness of breath are not identified as early signs of hemorrhagic stroke. 5. The nurse is performing stroke risk screenings at a hospital open house. The nurse has identified four patients who might be at risk for a stroke. Which patient is likely at the highest risk for a hemorrhagic stroke? A) White female, age 60, with history of excessive alcohol intake B) White male, age 60, with history of uncontrolled hypertension C) Black male, age 60, with history of diabetes D) Black male, age 50, with history of smoking B Feedback: Uncontrolled hypertension is the primary cause of a hemorrhagic stroke. Control of hypertension, especially in individuals over 55 years of age, clearly reduces the risk for hemorrhagic stroke. Additional risk factors are increased age, male gender, and excessive alcohol intake. Another high-risk group includes African Americans, where the incidence of first stroke is almost twice that as in Caucasians. 6. A patient who just suffered a suspected ischemic stroke is brought to the ED by ambulance. On what should the nurses primary assessment focus? A) Cardiac and respiratory status B) Seizure activity C) Pain D) Fluid and electrolyte balance A Feedback: Acute care begins with managing ABCs. Patients may have difficulty keeping an open and clear airway secondary to decreased LOC. Neurologic assessment with close monitoring for signs of increased neurologic deficit and seizure activity occurs next. Fluid and electrolyte balance must be controlled carefully with the goal of adequate hydration to promote perfusion and decrease further brain activity. 7. A patient with a cerebral aneurysm exhibits signs and symptoms of an increase in intracranial pressure (ICP). What nursing intervention would be most appropriate for this patient? A) Range-of-motion exercises to prevent contractures B) Encouraging independence with ADLs to promote recovery C) Early initiation of physical therapy D) Absolute bed rest in a quiet, nonstimulating environment D Feedback: The patient is placed on immediate and absolute bed rest in a quiet, nonstressful environment because activity, pain, and anxiety elevate BP, which increases the risk for bleeding. Visitors are restricted. The nurse administers all personal care. The patient is fed and bathed to prevent any exertion that might raise BP. 8. A patient recovering from a stroke has severe shoulder pain from subluxation of the shoulder and is being cared for on the unit. To prevent further injury and pain, the nurse caring for this patient is aware of what principle of care? A) The patient should be fitted with a cast because use of a sling should be avoided due to adduction of the affected shoulder. B) Elevation of the arm and hand can lead to further complications associated with edema. C) Passively exercising the affected extremity is avoided in order to minimize pain. D) The patient should be taught to interlace fingers, place palms together, and slowly bring scapulae forward to avoid excessive force to shoulder. D Feedback: To prevent shoulder pain, the nurse should never lift a patient by the flaccid shoulder or pull on the affected arm or shoulder. The patient is taught how to move and exercise the affected arm/shoulder through proper movement and positioning. The patient is instructed to interlace the fingers, place the palms together, and push the clasped hands slowly forward to bring the scapulae forward; he or she then raises both hands above the head. This is repeated throughout the day. The use of a properly worn sling when the patient is out of bed prevents the paralyzed upper extremity from dangling without support. Range-of-motion exercises are still vitally important in preventing a frozen shoulder and ultimately atrophy of subcutaneous tissues, which can cause more pain. Elevation of the arm and hand is also important in preventing dependent edema of the hand. 9. The patient has been diagnosed with aphasia after suffering a stroke. What can the nurse do to best make the patients atmosphere more conducive to communication? A) Provide a board of commonly used needs and phrases. B) Have the patient speak to loved ones on the phone daily. C) Help the patient complete his or her sentences. D) Speak in a loud and deliberate voice to the patient. A Feedback: The inability to talk on the telephone or answer a question or exclusion from conversation causes anger, frustration, fear of the future, and hopelessness. A common pitfall is for the nurse or other health care team member to complete the thoughts or sentences of the patient. This should be avoided because it may cause the patient to feel more frustrated at not being allowed to speak and may deter efforts to practice putting thoughts together and completing a sentence. The patient may also benefit from a communication board, which has pictures of commonly requested needs and phrases. The board may be translated into several languages. 10. The nurse is assessing a patient with a suspected stroke. What assessment finding is most suggestive of a stroke? A) Facial droop B) Dysrhythmias C) Periorbital edema D) Projectile vomiting A Feedback: Facial drooping or asymmetry is a classic abnormal finding on a physical assessment that may be associated with a stroke. Facial edema is not suggestive of a stroke and patients less commonly experience dysrhythmias or vomiting. 11. The nurse is caring for a patient diagnosed with an ischemic stroke and knows that effective positioning of the patient is important. Which of the following should be integrated into the patients plan of care? A) The patients hip joint should be maintained in a flexed position. B) The patient should be in a supine position unless ambulating. C) The patient should be placed in a prone position for 15 to 30 minutes several times a day. D) The patient should be placed in a Trendelenberg position two to three times daily to promote cerebral perfusion. C Feedback: If possible, the patient is placed in a prone position for 15 to 30 minutes several times a day. A small pillow or a support is placed under the pelvis, extending from the level of the umbilicus to the upper third of the thigh. This helps to promote hyperextension of the hip joints, which is essential for normal gait, and helps prevent knee and hip flexion contractures. The hip joints should not be maintained in flexion and the Trendelenberg position is not indicated. 12. A patient has been admitted to the ICU after being recently diagnosed with an aneurysm and the patients admission orders include specific aneurysm precautions. What nursing action will the nurse incorporate into the patients plan of care? A) Elevate the head of the bed to 45 degrees. B) Maintain the patient on complete bed rest. C) Administer enemas when the patient is constipated. D) Avoid use of thigh-high elastic compression stockings. B Feedback: Cerebral aneurysm precautions are implemented for the patient with a diagnosis of aneurysm to provide a nonstimulating environment, prevent increases in ICP, and prevent further bleeding. The patient is placed on immediate and absolute bed rest in a quiet, nonstressful environment because activity, pain, and anxiety elevate BP, which increases the risk for bleeding. Visitors, except for family, are restricted. The head of the bed is elevated 15 to 30 degrees to promote venous drainage and decrease ICP. Some neurologists, however, prefer that the patient remains flat to increase cerebral perfusion. No enemas are permitted, but stool softeners and mild laxatives are prescribed. Thigh-high elastic compression stockings or sequential compression boots may be ordered to decrease the patients risk for deep vein thrombosis (DVT). 13. A nurse is caring for a patient diagnosed with a hemorrhagic stroke. When creating this patients plan of care, what goal should be prioritized? A) Prevent complications of immobility. B) Maintain and improve cerebral tissue perfusion. C) Relieve anxiety and pain. D) Relieve sensory deprivation. B Feedback: Each of the listed goals is appropriate in the care of a patient recovering from a stroke. However, promoting cerebral perfusion is a priority physiologic need, on which the patients survival depends. 14. The nurse is preparing health education for a patient who is being discharged after hospitalization for a hemorrhagic stroke. What content should the nurse include in this education? A) Mild, intermittent seizures can be expected. B) Take ibuprofen for complaints of a serious headache. C) Take antihypertensive medication as ordered. D) Drowsiness is normal for the first week after discharge. C Feedback: The patient and family are provided with information that will enable them to cooperate with the care and restrictions required during the acute phase of hemorrhagic stroke and to prepare the patient to return home. Patient and family teaching includes information about the causes of hemorrhagic stroke and its possible consequences. Symptoms of hydrocephalus include gradual onset of drowsiness and behavioral changes. Hypertension is the most serious risk factor, suggesting that appropriate antihypertensive treatment is essential for a patient being discharged. Seizure activity is not normal; complaints of a serious headache should be reported to the physician before any medication is taken. Drowsiness is not normal or expected. 15. A patient diagnosed with a cerebral aneurysm reports a severe headache to the nurse. What action is a priority for the nurse? A) Sit with the patient for a few minutes. B) Administer an analgesic. C) Inform the nurse-manager. D) Call the physician immediately. D Feedback: A headache may be an indication that the aneurysm is leaking. The nurse should notify the physician immediately. The physician will decide whether administration of an analgesic is indicated. Informing the nurse-manager is not necessary. Sitting with the patient is appropriate, once the physician has been notified of the change in the patients condition. 16. A patient is brought by ambulance to the ED after suffering what the family thinks is a stroke. The nurse caring for this patient is aware that an absolute contraindication for thrombolytic therapy is what? A) Evidence of hemorrhagic stroke B) Blood pressure of 180/110 mm Hg C) Evidence of stroke evolution D) Previous thrombolytic therapy within the past 12 months A Feedback: Thrombolytic therapy would exacerbate a hemorrhagic stroke with potentially fatal consequences. Stroke evolution, high BP, or previous thrombolytic therapy does not contraindicate its safe and effective use. 17. When caring for a patient who has had a stroke, a priority is reduction of ICP. What patient position is most consistent with this goal? A) Head turned slightly to the right side B) Elevation of the head of the bed C) Position changes every 15 minutes while awake D) Extension of the neck B Feedback: Elevation of the head of the bed promotes venous drainage and lowers ICP; the nurse should avoid flexing or extending the neck or turning the head side to side. The head should be in a neutral midline position. Excessively frequent position changes are unnecessary. 18. A patient who suffered an ischemic stroke now has disturbed sensory perception. What principle should guide the nurses care of this patient? A) The patient should be approached on the side where visual perception is intact. B) Attention to the affected side should be minimized in order to decrease anxiety. C) The patient should avoid turning in the direction of the defective visual field to minimize shoulder subluxation. D) The patient should be approached on the opposite side of where the visual perception is intact to promote recovery. A Feedback: Patients with decreased field of vision should first be approached on the side where visual perception is intact. All visual stimuli should be placed on this side. The patient can and should be taught to turn the head in the direction of the defective visual field to compensate for this loss. The nurse should constantly remind the patient of the other side of the body and should later stand at a position that encourages the patient to move or turn to visualize who and what is in the room. 19. What should be included in the patients care plan when establishing an exercise program for a patient affected by a stroke? A) Schedule passive range of motion every other day. B) Keep activity limited, as the patient may be over stimulated. C) Have the patient perform active range-of-motion (ROM) exercises once a day. D) Exercise the affected extremities passively four or five times a day. D Feedback: The affected extremities are exercised passively and put through a full ROM four or five times a day to maintain joint mobility, regain motor control, prevent development of a contracture in the paralyzed extremity, prevent further deterioration of the neuromuscular system, and enhance circulation. Active ROM exercises should ideally be performed more than once per day. 20. A female patient is diagnosed with a right-sided stroke. The patient is now experiencing hemianopsia. How might the nurse help the patient manage her potential sensory and perceptional difficulties? A) Keep the lighting in the patients room low. B) Place the patients clock on the affected side. C) Approach the patient on the side where vision is impaired. D) Place the patients extremities where she can see them. D Feedback: The patient with homonymous hemianopsia (loss of half of the visual field) turns away from the affected side of the body and tends to neglect that side and the space on that side; this is called amorphosynthesis. In such instances, the patient cannot see food on half of the tray, and only half of the room is visible. It is important for the nurse to remind the patient constantly of the other side of the body, to maintain alignment of the extremities, and if possible, to place the extremities where the patient can see them. Patients with a decreased field of vision should be approached on the side where visual perception is intact. All visual stimuli (clock, calendar, and television) should be placed on this side. The patient can be taught to turn the head in the direction of the defective visual field to compensate for this loss. Increasing the natural or artificial lighting in the room and providing eyeglasses are important in increasing vision. There is no reason to keep the lights dim. The public health nurse is planning a health promotion campaign that reflects current epidemiologic trends. The nurse should know that hemorrhagic stroke currently accounts for what percentage of total strokes in the United States? A) 43% B) 33% C) 23% D) 13% D Feedback: Strokes can be divided into two major categories: ischemic (87%), in which vascular occlusion and significant hypoperfusion occur, and hemorrhagic (13%), in which there is extravasation of blood into the brain or subarachnoid space. 22. A patient who has experienced an ischemic stroke has been admitted to the medical unit. The patients family in adamant that she remain on bed rest to hasten her recovery and to conserve energy. What principle of care should inform the nurses response to the family? A) The patient should mobilize as soon as she is physically able. B) To prevent contractures and muscle atrophy, bed rest should not exceed 4 weeks. C) The patient should remain on bed rest until she expresses a desire to mobilize. D) Lack of mobility will greatly increase the patients risk of stroke recurrence. A Feedback: As soon as possible, the patient is assisted out of bed and an active rehabilitation program is started. Delaying mobility causes complications, but not necessarily stroke recurrence. Mobility should not be withheld until the patient initiates. 23. A patient has recently begun mobilizing during the recovery from an ischemic stroke. To protect the patients safety during mobilization, the nurse should perform what action? A) Support the patients full body weight with a waist belt during ambulation. B) Have a colleague follow the patient closely with a wheelchair. C) Avoid mobilizing the patient in the early morning or late evening. D) Ensure that the patients family members do not participate in mobilization. B Feedback: During mobilization, a chair or wheelchair should be readily available in case the patient suddenly becomes fatigued or feels dizzy. The family should be encouraged to participate, as appropriate, and the nurse should not have to support the patients full body weight. Morning and evening activity are not necessarily problematic. 24. A patient diagnosed with a hemorrhagic stroke has been admitted to the neurologic ICU. The nurse knows that teaching for the patient and family needs to begin as soon as the patient is settled on the unit and will continue until the patient is discharged. What will family education need to include? A) How to differentiate between hemorrhagic and ischemic stroke B) Risk factors for ischemic stroke C) How to correctly modify the home environment D) Techniques for adjusting the patients medication dosages at home C Feedback: For a patient with a hemorrhagic stroke, teaching addresses the use of assistive devices or modification of the home environment to help the patient live with the disability. This is more important to the patients needs than knowing about risk factors for ischemic stroke. It is not necessary for the family to differentiate between different types of strokes. Medication regimens should never be altered without consultation. 25. After a subarachnoid hemorrhage, the patients laboratory results indicate a serum sodium level of less than 126 mEq/L. What is the nurses most appropriate action? A) Administer a bolus of normal saline as ordered. B) Prepare the patient for thrombolytic therapy as ordered. C) Facilitate testing for hypothalamic dysfunction. D) Prepare to administer 3% NaCl by IV as ordered. D Feedback: The patient may be experiencing syndrome of inappropriate antidiuretic hormone (SIADH) or cerebral salt-wasting syndrome. The treatment most often is the use of IV hypertonic 3% saline. A normal saline bolus would exacerbate the problem and there is no indication for tests of hypothalamic function or thrombolytic therapy. 26. A community health nurse is giving an educational presentation about stroke and heart disease at the local senior citizens center. What nonmodifiable risk factor for stroke should the nurse cite? A) Female gender B) Asian American race C) Advanced age D) Smoking C Feedback: Advanced age, male gender, and race are well-known nonmodifiable risk factors for stroke. High-risk groups include people older than 55 years of age; the incidence of stroke more than doubles in each successive decade. Men have a higher rate of stroke than that of women. Another high-risk group is African Americans; the incidence of first stroke in African Americans is almost twice that as in Caucasian Americans; Asian American race is not a risk factor. Smoking is a modifiable risk. 27. A family member brings the patient to the clinic for a follow-up visit after a stroke. The family member asks the nurse what he can do to decrease his chance of having another stroke. What would be the nurses best answer? A) Have your heart checked regularly. B) Stop smoking as soon as possible. C) Get medication to bring down your sodium levels. D) Eat a nutritious diet. B Feedback: Smoking is a modifiable and highly significant risk factor for stroke. The significance of smoking, and the potential benefits of quitting, exceed the roles of sodium, diet, and regular medical assessments. 28. The nurse is reviewing the medication administration record of a female patient who possesses numerous risk factors for stroke. Which of the womans medications carries the greatest potential for reducing her risk of stroke? A) Naproxen 250 PO b.i.d. B) Calcium carbonate 1,000 mg PO b.i.d. C) Aspirin 81 mg PO o.d. D) Lorazepam 1 mg SL b.i.d. PRN C Feedback: Research findings suggest that low-dose aspirin may lower the risk of stroke in women who are at risk. Naproxen, lorazepam, and calcium supplements do not have this effect. 29. A nurse in the ICU is providing care for a patient who has been admitted with a hemorrhagic stroke. The nurse is performing frequent neurologic assessments and observes that the patient is becoming progressively more drowsy over the course of the day. What is the nurses best response to this assessment finding? A) Report this finding to the physician as an indication of decreased metabolism. B) Provide more stimulation to the patient and monitor the patient closely. C) Recognize this as the expected clinical course of a hemorrhagic stroke. D) Report this to the physician as a possible sign of clinical deterioration. D Feedback: Alteration in LOC often is the earliest sign of deterioration in a patient with a hemorrhagic stroke. Drowsiness and slight slurring of speech may be early signs that the LOC is deteriorating. This finding is unlikely to be the result of metabolic changes and it is not expected. Stimulating a patient with an acute stroke is usually contraindicated. 30. Following diagnostic testing, a patient has been admitted to the ICU and placed on cerebral aneurysm precautions. What nursing action should be included in patients plan of care? A) Supervise the patients activities of daily living closely. B) Initiate early ambulation to prevent complications of immobility. C) Provide a high-calorie, low-protein diet. D) Perform all of the patients hygiene and feeding. A Feedback: The patient is placed on immediate and absolute bed rest in a quiet, nonstressful environment, because activity, pain, and anxiety elevate BP, which increases the risk for bleeding. As such, independent ADLs and ambulation are contraindicated. There is no need for a high-calorie or low-protein diet. 31. A preceptor is discussing stroke with a new nurse on the unit. The preceptor would tell the new nurse which cardiac dysrhythmia is associated with cardiogenic embolic strokes? A) Ventricular tachycardia B) Atrial fibrillation C) Supraventricular tachycardia D) Bundle branch block B Feedback: Cardiogenic embolic strokes are associated with cardiac dysrhythmias, usually atrial fibrillation. The other listed dysrhythmias are less commonly associated with this type of stroke. 32. The pathophysiology of an ischemic stroke involves the ischemic cascade, which includes the following steps: 1. Change in pH 2. Blood flow decreases 3. A switch to anaerobic respiration 4. Membrane pumps fail 5. Cells cease to function 6. Lactic acid is generated Put these steps in order in which they occur. A) 635241 B) 352416 C) 236145 D) 162534 C Feedback: The ischemic cascade begins when cerebral blood flow decreases to less than 25 mL per 100 g of blood per minute. At this point, neurons are no longer able to maintain aerobic respiration. The mitochondria must then switch to anaerobic respiration, which generates large amounts of lactic acid, causing a change in the pH. This switch to the less efficient anaerobic respiration also renders the neuron incapable of producing sufficient quantities of adenosine triphosphate (ATP) to fuel the depolarization processes. The membrane pumps that maintain electrolyte balances begin to fail, and the cells cease to function. 33. As a member of the stroke team, the nurse knows that thrombolytic therapy carries the potential for benefit and for harm. The nurse should be cognizant of what contraindications for thrombolytic therapy? Select all that apply. A) INR above 1.0 B) Recent intracranial pathology C) Sudden symptom onset D) Current anticoagulation therapy E) Symptom onset greater than 3 hours prior to admission B, D, E Feedback: Some of the absolute contraindications for thrombolytic therapy include symptom onset greater than 3 hours before admission, a patient who is anticoagulated (with an INR above 1.7), or a patient who has recently had any type of intracranial pathology (e.g., previous stroke, head injury, trauma). 34. After a major ischemic stroke, a possible complication is cerebral edema. Nursing care during the immediate recovery period from an ischemic stroke should include which of the following? A) Positioning to avoid hypoxia B) Maximizing PaCO2 C) Administering hypertonic IV solution D) Initiating early mobilization A Feedback: Interventions during this period include measures to reduce ICP, such as administering an osmotic diuretic (e.g., mannitol), maintaining the partial pressure of carbon dioxide (PaCO2) within the range of 30 to 35 mm Hg, and positioning to avoid hypoxia. Hypertonic IV solutions are not used unless sodium depletion is evident. Mobilization would take place after the immediate threat of increased ICP has past. 35. The nurse is caring for a patient recovering from an ischemic stroke. What intervention best addresses a potential complication after an ischemic stroke? A) Providing frequent small meals rather than three larger meals B) Teaching the patient to perform deep breathing and coughing exercises C) Keeping a urinary catheter in situ for the full duration of recovery D) Limiting intake of insoluble fiber B Feedback: Because pneumonia is a potential complication of stroke, deep breathing and coughing exercises should be encouraged unless contraindicated. No particular need exists to provide frequent meals and normally fiber intake should not be restricted. Urinary catheters should be discontinued as soon as possible. 36. During a patients recovery from stroke, the nurse should be aware of predictors of stroke outcome in order to help patients and families set realistic goals. What are the predictors of stroke outcome? Select all that apply. A) National Institutes of Health Stroke Scale (NIHSS) score B) Race C) LOC at time of admission D) Gender E) Age A, C, E Feedback: It is helpful for clinicians to be knowledgeable about the relative importance of predictors of stroke outcome (age, NIHSS score, and LOC at time of admission) to provide stroke survivors and their families with realistic goals. Race and gender are not predictors of stroke outcome. 37. A nursing student is writing a care plan for a newly admitted patient who has been diagnosed with a stroke. What major nursing diagnosis should most likely be included in the patients plan of care? A) Adult failure to thrive B) Post-trauma syndrome C) Hyperthermia D) Disturbed sensory perception D Feedback: The patient who has experienced a stroke is at a high risk for disturbed sensory perception. Stroke is associated with multiple other nursing diagnoses, but hyperthermia, adult failure to thrive, and post- trauma syndrome are not among these. 38. When preparing to discharge a patient home, the nurse has met with the family and warned them that the patient may exhibit unexpected emotional responses. The nurse should teach the family that these responses are typically a result of what cause? A) Frustration around changes in function and communication B) Unmet physiologic needs C) Changes in brain activity during sleep and wakefulness D) Temporary changes in metabolism A Feedback: Emotional problems associated with stroke are often related to the new challenges around ADLs and communication. These challenges are more likely than metabolic changes, unmet physiologic needs, or changes in brain activity, each of which should be ruled out. 39. A rehabilitation nurse caring for a patient who has had a stroke is approached by the patients family and asked why the patient has to do so much for herself when she is obviously struggling. What would be the nurses best answer? A) We are trying to help her be as useful as she possibly can. B) The focus on care in a rehabilitation facility is to help the patient to resume as much self-care as possible. C) We arent here to care for her the way the hospital staff did; we are here to help her get better so she can go home. D) Rehabilitation means helping patients do exactly what they did before their stroke. B Feedback: In both acute care and rehabilitation facilities, the focus is on teaching the patient to resume as much self-care as possible. The goal of rehabilitation is not to be useful, nor is it to return patients to their prestroke level of functioning, which may be unrealistic. 40. A patient with a new diagnosis of ischemic stroke is deemed to be a candidate for treatment with tissue plasminogen activator (t-PA) and has been admitted to the ICU. In addition to closely monitoring the patients cardiac and neurologic status, the nurse monitors the patient for signs of what complication? A) Acute pain B) Septicemia C) Bleeding D) Seizures C Feedback: Bleeding is the most common side effect of t-PA administration, and the patient is closely monitored for any bleeding. Septicemia, pain, and seizures are much less likely to result from thrombolytic therapy. Chapter 68: Management of Patients with Neurologic Trauma 1. The ED nurse is caring for a patient who has been brought in by ambulance after sustaining a fall at home. What physical assessment finding is suggestive of a basilar skull fracture? A) Epistaxis B) Periorbital edema C) Bruising over the mastoid D) Unilateral facial numbness C Feedback: An area of ecchymosis (bruising) may be seen over the mastoid (Battles sign) in a basilar skull fracture. Numbness, edema, and epistaxis are not directly associated with a basilar skull fracture. 2. A patient is brought to the trauma center by ambulance after sustaining a high cervical spinal cord injury 1 hours ago. Endotracheal intubation has been deemed necessary and the nurse is preparing to assist. What nursing diagnosis should the nurse associate with this procedure? A) Risk for impaired skin integrity B) Risk for injury C) Risk for autonomic dysreflexia D) Risk for suffocation B Feedback: If endotracheal intubation is necessary, extreme care is taken to avoid flexing or extending the patients neck, which can result in extension of a cervical injury. Intubation does not directly cause autonomic dysreflexia and the threat to skin integrity is a not a primary concern. Intubation does not carry the potential to cause suffocation. 3. A nurse is caring for a critically ill patient with autonomic dysreflexia. What clinical manifestations would the nurse expect in this patient? A) Respiratory distress and projectile vomiting B) Bradycardia and hypertension C) Tachycardia and agitation D) Third-spacing and hyperthermia B Feedback: Autonomic dysreflexia is characterized by a pounding headache, profuse sweating, nasal congestion, piloerection (goose bumps), bradycardia, and hypertension. It occurs in cord lesions above T6 after spinal shock has resolved; it does not result in vomiting, tachycardia, or third-spacing. 4. The nurse is caring for a patient with increased intracranial pressure (ICP) caused by a traumatic brain injury. Which of the following clinical manifestations would suggest that the patient may be experiencing increased brain compression causing brain stem damage? A) Hyperthermia B) Tachycardia C) Hypertension D) Bradypnea A Feedback: Signs of increasing ICP include slowing of the heart rate (bradycardia), increasing systolic BP, and widening pulse pressure. As brain compression increases, respirations become rapid, BP may decrease, and the pulse slows further. A rapid rise in body temperature is regarded as unfavorable. Hyperthermia increases the metabolic demands of the brain and may indicate brain stem damage. 5. A patient is brought to the ED by her family after falling off the roof. A family member tells the nurse that when the patient fell she was knocked out, but came to and seemed okay. Now she is complaining of a severe headache and not feeling well. The care team suspects an epidural hematoma, prompting the nurse to prepare for which priority intervention? A) Insertion of an intracranial monitoring device B) Treatment with antihypertensives C) Emergency craniotomy D) Administration of anticoagulant therapy C Feedback: An epidural hematoma is considered an extreme emergency. Marked neurologic deficit or respiratory arrest can occur within minutes. Treatment consists of making an opening through the skull to decrease ICP emergently, remove the clot, and control the bleeding. Antihypertensive medications would not be a priority. Anticoagulant therapy should not be ordered for a patient who has a cranial bleed. This could further increase bleeding activity. Insertion of an intracranial monitoring device may be done during the surgery, but is not priority for this patient. 6. The staff educator is precepting a nurse new to the critical care unit when a patient with a T2 spinal cord injury is admitted. The patient is soon exhibiting manifestations of neurogenic shock. In addition to monitoring the patient closely, what would be the nurses most appropriate action? A) Prepare to transfuse packed red blood cells. B) Prepare for interventions to increase the patients BP. C) Place the patient in the Trendelenberg position. D) Prepare an ice bath to lower core body temperature. B Feedback: Manifestations of neurogenic shock include decreased BP and heart rate. Cardiac markers would be expected to rise in cardiogenic shock. Transfusion, repositioning, and ice baths are not indicated interventions. 7. An ED nurse has just received a call from EMS that they are transporting a 17-year-old man who has just sustained a spinal cord injury (SCI). The nurse recognizes that the most common cause of this type of injury is what? A) Sports-related injuries B) Acts of violence C) Injuries due to a fall D) Motor vehicle accidents D Feedback: The most common causes of SCIs are motor vehicle crashes (46%), falls (22%), violence (16%), and sports (12%). 8. A patient with spinal cord injury has a nursing diagnosis of altered mobility and the nurse recognizes the increased the risk of deep vein thrombosis (DVT). Which of the following would be included as an appropriate nursing intervention to prevent a DVT from occurring? A) Placing the patient on a fluid restriction as ordered B) Applying thigh-high elastic stockings C) Administering an antifibrinolyic agent D) Assisting the patient with passive range of motion (PROM) exercises B Feedback: It is important to promote venous return to the heart and prevent venous stasis in a patient with altered mobility. Applying elastic stockings will aid in the prevention of a DVT. The patient should not be placed on fluid restriction because a dehydrated state will increase the risk of clotting throughout the body. Antifibrinolytic agents cause the blood to clot, which is absolutely contraindicated in this situation. PROM exercises are not an effective protection against the development of DVT. 9. Paramedics have brought an intubated patient to the RD following a head injury due to acceleration- deceleration motor vehicle accident. Increased ICP is suspected. Appropriate nursing interventions would include which of the following? A) Keep the head of the bed (HOB) flat at all times. B) Teach the patient to perform the Valsalva maneuver. C) Administer benzodiazepines on a PRN basis. D) Perform endotracheal suctioning every hour. C Feedback: If the patient with a brain injury is very agitated, benzodiazepines are the most commonly used sedatives and do not affect cerebral blood flow or ICP. The HOB should be elevated 30 degrees. Suctioning should be done a limited basis, due to increasing the pressure in the cranium. The Valsalva maneuver is to be avoided. This also causes increased ICP. 10. A patient who has sustained a nondepressed skull fracture is admitted to the acute medical unit. Nursing care should include which of the following? A) Preparation for emergency craniotomy B) Watchful waiting and close monitoring C) Administration of inotropic drugs D) Fluid resuscitation B Feedback: Nondepressed skull fractures generally do not require surgical treatment; however, close observation of the patient is essential. A craniotomy would not likely be needed if the fracture is nondepressed. Even if treatment is warranted, it is unlikely to include inotropes or fluid resuscitation. 11. A patient who suffered a spinal cord injury is experiencing an exaggerated autonomic response. What aspect of the patients current health status is most likely to have precipitated this event? A) The patient received a blood transfusion. B) The patients analgesia regimen was recent changed. C) The patient was not repositioned during the night shift. D) The patients urinary catheter became occluded. D Feedback: A distended bladder is the most common cause of autonomic dysreflexia. Infrequent positioning is a less likely cause, although pressure ulcers or tactile stimulation can cause it. Changes in mediations or blood transfusions are unlikely causes. 12. A patient is admitted to the neurologic ICU with a spinal cord injury. In writing the patients care plan, the nurse specifies that contractures can best be prevented by what action? A) Repositioning the patient every 2 hours B) Initiating range-of-motion exercises (ROM) as soon as the patient initiates C) Initiating (ROM) exercises as soon as possible after the injury D) Performing ROM exercises once a day C Feedback: Passive ROM exercises should be implemented as soon as possible after injury. It would be inappropriate to wait for the patient to first initiate exercises. Toes, metatarsals, ankles, knees, and hips should be put through a full ROM at least four, and ideally five, times daily. Repositioning alone will not prevent contractures. 13. A patient with a head injury has been increasingly agitated and the nurse has consequently identified a risk for injury. What is the nurses best intervention for preventing injury? A) Restrain the patient as ordered. B) Administer opioids PRN as ordered. C) Arrange for friends and family members to sit with the patient. D) Pad the side rails of the patients bed. D Feedback: To protect the patient from self-injury, the nurse uses padded side rails. The nurse should avoid restraints, because straining against them can increase ICP or cause other injury. Narcotics used to control restless patients should be avoided because these medications can depress respiration, constrict the pupils, and alter the patients responsiveness. Visitors should be limited if the patient is agitated. 14. A patient with a C5 spinal cord injury is tetraplegic. After being moved out of the ICU, the patient complains of a severe throbbing headache. What should the nurse do first? A) Check the patients indwelling urinary catheter for kinks to ensure patency. B) Lower the HOB to improve perfusion. C) Administer analgesia. D) Reassure the patient that headaches are expected after spinal cord injuries. A Feedback: A severe throbbing headache is a common symptom of autonomic dysreflexia, which occurs after injuries to the spinal cord above T6. The syndrome is usually brought on by sympathetic stimulation, such as bowel and bladder distention. Lowering the HOB can increase ICP. Before administering analgesia, the nurse should check the patients catheter, record vital signs, and perform an abdominal assessment. A severe throbbing headache is a dangerous symptom in this patient and is not expected. 15. A patient is admitted to the neurologic ICU with a spinal cord injury. When assessing the patient the nurse notes there is a sudden depression of reflex activity in the spinal cord below the level of injury. What should the nurse suspect? A) Epidural hemorrhage B) Hypertensive emergency C) Spinal shock D) Hypovolemia C Feedback: In spinal shock, the reflexes are absent, BP and heart rate fall, and respiratory failure can occur. Hypovolemia, hemorrhage, and hypertension do not cause this sudden change in neurologic function. 16. An elderly woman found with a head injury on the floor of her home is subsequently admitted to the neurologic ICU. What is the best rationale for the following physician orders: elevate the HOB; keep the head in neutral alignment with no neck flexion or head rotation; avoid sharp hip flexion? A) To decrease cerebral arterial pressure B) To avoid impeding venous outflow C) To prevent flexion contractures D) To prevent aspiration of stomach contents B Feedback: Any activity or position that impedes venous outflow from the head may contribute to increased volume inside the skull and possibly increase ICP. Cerebral arterial pressure will be affected by the balance between oxygen and carbon dioxide. Flexion contractures are not a priority at this time. Stomach contents could still be aspirated in this position. 17. A patient with a T2 injury is in spinal shock. The nurse will expect to observe what assessment finding? A) Absence of reflexes along with flaccid extremities B) Positive Babinskis reflex along with spastic extremities C) Hyperreflexia along with spastic extremities D) Spasticity of all four extremities A Feedback: During the period immediately following a spinal cord injury, spinal shock occurs. In spinal shock, all reflexes are absent and the extremities are flaccid. When spinal shock subsides, the patient demonstrates a positive Babinskis reflex, hyperreflexia, and spasticity of all four extremities. 18. A nurse is reviewing the trend of a patients scores on the Glasgow Coma Scale (GCS). This allows the nurse to gauge what aspect of the patients status? A) Reflex activity B) Level of consciousness C) Cognitive ability D) Sensory involvement B Feedback: The Glasgow Coma Scale (GCS) examines three responses related to LOC: eye opening, best verbal response, and best motor response. 19. The nurse is caring for a patient who is rapidly progressing toward brain death. The nurse should be aware of what cardinal signs of brain death? Select all that apply. A) Absence of pain response B) Apnea C) Coma D) Absence of brain stem reflexes E) Absence of deep tendon reflexes B, C, D Feedback: The three cardinal signs of brain death upon clinical examination are coma, the absence of brain stem reflexes, and apnea. Absences of pain response and deep tendon reflexes are not necessarily indicative of brain death. 20. Following a spinal cord injury a patient is placed in halo traction. While performing pin site care, the nurse notes that one of the traction pins has become detached. The nurse would be correct in implementing what priority nursing action? A) Complete the pin site care to decrease risk of infection. B) Notify the neurosurgeon of the occurrence. C) Stabilize the head in a lateral position. D) Reattach the pin to prevent further head trauma. B Feedback: If one of the pins became detached, the head is stabilized in neutral position by one person while another notifies the neurosurgeon. Reattaching the pin as a nursing intervention would not be done due to risk of increased injury. Pin site care would not be a priority in this instance. Prevention of neurologic injury is the priority. 21. The ED is notified that a 6-year-old is in transit with a suspected brain injury after being struck by a car. The child is unresponsive at this time, but vital signs are within acceptable limits. What will be the primary goal of initial therapy? A) Promoting adequate circulation B) Treating the childs increased ICP C) Assessing secondary brain injury D) Preserving brain homeostasis D Feedback: All therapy is directed toward preserving brain homeostasis and preventing secondary brain injury, which is injury to the brain that occurs after the original traumatic event. The scenario does not indicate the child has increased ICP or a secondary brain injury at this point. Promoting circulation is likely secondary to the broader goal of preserving brain homeostasis. 22. A patient is admitted to the neurologic ICU with a suspected diffuse axonal injury. What would be the primary neuroimaging diagnostic tool used on this patient to evaluate the brain structure? A) MRI B) PET scan C) X-ray D) Ultrasound A Feedback: CT and MRI scans, the primary neuroimaging diagnostic tools, are useful in evaluating the brain structure. Ultrasound would not show the brain nor would an x-ray. A PET scan shows brain function, not brain structure. 23. A 13-year-old was brought to the ED, unconscious, after being hit in the head by a baseball. When the child regains consciousness, 5 hours after being admitted, he cannot remember the traumatic event. MRI shows no structural sign of injury. What injury would the nurse suspect the patient has? A) Diffuse axonal injury B) Grade 1 concussion with frontal lobe involvement C) Contusion D) Grade 3 concussion with temporal lobe involvement D Feedback: In a grade 3 concussion there is a loss of consciousness lasting from seconds to minutes. Temporal lobe involvement results in amnesia. Frontal lobe involvement can cause uncharacteristic behavior and a grade 1 concussion does not involve loss of consciousness. Diagnostic studies may show no apparent structural sign of injury, but the duration of unconsciousness is an indicator of the severity of the concussion. Diffuse axonal injury (DAI) results from widespread shearing and rotational forces that produce damage throughout the brainto axons in the cerebral hemispheres, corpus callosum, and brain stem. In cerebral contusion, a moderate to severe head injury, the brain is bruised and damaged in a specific area because of severe acceleration-deceleration force or blunt trauma. 24. An 82-year-old man is admitted for observation after a fall. Due to his age, the nurse knows that the patient is at increased risk for what complication of his injury? A) Hematoma B) Skull fracture C) Embolus D) Stroke A Feedback: Two major factors place older adults at increased risk for hematomas. First, the dura becomes more adherent to the skull with increasing age. Second, many older adults take aspirin and anticoagulants as part of routine management of chronic conditions. Because of these factors, the patients risk of a hematoma is likely greater than that of stroke, embolism, or skull fracture. 25. A neurologic flow chart is often used to document the care of a patient with a traumatic brain injury. At what point in the patients care should the nurse begin to use a neurologic flow chart? A) When the patients condition begins to deteriorate B) As soon as the initial assessment is made C) At the beginning of each shift D) When there is a clinically significant change in the patients condition B Feedback: Neurologic parameters are assessed initially and as frequently as the patients condition requires. As soon as the initial assessment is made, the use of a neurologic flowchart is started and maintained. A new chart is not begun at the start of every shift. 26. The nurse planning the care of a patient with head injuries is addressing the patients nursing diagnosis of sleep deprivation. What action should the nurse implement? A) Administer a benzodiazepine at bedtime each night. B) Do not disturb the patient between 2200 and 0600. C) Cluster overnight nursing activities to minimize disturbances. D) Ensure that the patient does not sleep during the day. C Feedback: To allow the patient longer times of uninterrupted sleep and rest, the nurse can group nursing care activities so that the patient is disturbed less frequently. However, it is impractical and unsafe to provide no care for an 8-hour period. The use of benzodiazepines should be avoided. 27. The nurse has implemented interventions aimed at facilitating family coping in the care of a patient with a traumatic brain injury. How can the nurse best facilitate family coping? A) Help the family understand that the patient could have died. B) Emphasize the importance of accepting the patients new limitations. C) Have the members of the family plan the patients inpatient care. D) Assist the family in setting appropriate short-term goals. D Feedback: Helpful interventions to facilitate coping include providing family members with accurate and honest information and encouraging them to continue to set well-defined, short-term goals. Stating that a patients condition could be worse downplays their concerns. Emphasizing the importance of acceptance may not necessarily help the family accept the patients condition. Family members cannot normally plan a patients hospital care, although they may contribute to the care in some ways. 28. The school nurse is giving a presentation on preventing spinal cord injuries (SCI). What should the nurse identify as prominent risk factors for SCI? Select all that apply. A) Young age B) Frequent travel C) African American race D) Male gender E) Alcohol or drug use A, D, E Feedback: The predominant risk factors for SCI include young age, male gender, and alcohol and drug use. Ethnicity and travel are not risk factors. 29. The school nurse has been called to the football field where player is immobile on the field after landing awkwardly on his head during a play. While awaiting an ambulance, what action should the nurse perform? A) Ensure that the player is not moved. B) Obtain the players vital signs, if possible. C) Perform a rapid assessment of the players range of motion. D) Assess the players reflexes. A Feedback: At the scene of the injury, the patient must be immobilized on a spinal (back) board, with the head and neck maintained in a neutral position, to prevent an incomplete injury from becoming complete. This is a priority over determining the patients vital signs. It would be inappropriate to test ROM or reflexes. 30. The nurse is caring for a patient whose spinal cord injury has caused recent muscle spasticity. What medication should the nurse expect to be ordered to control this? A) Baclofen (Lioresal) B) Dexamethasone (Decadron) C) Mannitol (Osmitrol) D) Phenobarbital (Luminal) A Feedback: Baclofen is classified as an antispasmodic agent in the treatment of muscles spasms related to spinal cord injury. Decadron is an anti-inflammatory medication used to decrease inflammation in both SCI and head injury. Mannitol is used to decrease cerebral edema in patients with head injury. Phenobarbital is an anticonvulsant that is used in the treatment of seizure activity. 31. The nurse is planning the care of a patient with a T1 spinal cord injury. The nurse has identified the diagnosis of risk for impaired skin integrity. How can the nurse best address this risk? A) Change the patients position frequently. B) Provide a high-protein diet. C) Provide light massage at least daily. D) Teach the patient deep breathing and coughing exercises. A Feedback: Frequent position changes are among the best preventative measures against pressure ulcers. A high- protein diet can benefit wound healing, but does not necessarily prevent skin breakdown. Light massage and deep breathing do not protect or restore skin integrity. 32. A patient with a spinal cord injury has experienced several hypotensive episodes. How can the nurse best address the patients risk for orthostatic hypotension? A) Administer an IV bolus of normal saline prior to repositioning. B) Maintain bed rest until normal BP regulation returns. C) Monitor the patients BP before and during position changes. D) Allow the patient to initiate repositioning. C Feedback: To prevent hypotensive episodes, close monitoring of vital signs before and during position changes is essential. Prolonged bed rest carries numerous risks and it is not possible to provide a bolus before each position change. Following the patients lead may or may not help regulate BP. 33. A nurse on the neurologic unit is providing care for a patient who has spinal cord injury at the level of C4. When planning the patients care, what aspect of the patients neurologic and functional status should the nurse consider? A) The patient will be unable to use a wheelchair. B) The patient will be unable to swallow food. C) The patient will be continent of urine, but incontinent of bowel. D) The patient will require full assistance for all aspects of elimination. D Feedback: Patients with a lesion at C4 are fully dependent for elimination. The patient is dependent for feeding, but is able to swallow. The patient will be capable of using an electric wheelchair. 34. The nurse is providing health education to a patient who has a C6 spinal cord injury. The patient asks why autonomic dysreflexia is considered an emergency. What would be the nurses best answer? A) The sudden increase in BP can raise the ICP or rupture a cerebral blood vessel. B) The suddenness of the onset of the syndrome tells us the body is struggling to maintain its normal state. C) Autonomic dysreflexia causes permanent damage to delicate nerve fibers that are healing. D) The sudden, severe headache increases muscle tone and can cause further nerve damage. A Feedback: The sudden increase in BP may cause a rupture of one or more cerebral blood vessels or lead to increased ICP. Autonomic dysreflexia does not directly cause nerve damage. 35. The nurse caring for a patient with a spinal cord injury notes that the patient is exhibiting early signs and symptoms of disuse syndrome. Which of the following is the most appropriate nursing action? A) Limit the amount of assistance provided with ADLs. B) Collaborate with the physical therapist and immobilize the patients extremities temporarily. C) Increase the frequency of ROM exercises. D) Educate the patient about the importance of frequent position changes. C Feedback: To prevent disuse syndrome, ROM exercises must be provided at least four times a day, and care is taken to stretch the Achilles tendon with exercises. The patient is repositioned frequently and is maintained in proper body alignment whether in bed or in a wheelchair. The patient must be repositioned by caregivers, not just taught about repositioning. It is inappropriate to limit assistance for the sole purpose of preventing disuse syndrome. 36. Splints have been ordered for a patient who is at risk of developing footdrop following a spinal cord injury. The nurse caring for this patient knows that the splints are removed and reapplied when? A) At the patients request B) Each morning and evening C) Every 2 hours D) One hour prior to mobility exercises C Feedback: The feet are prone to footdrop; therefore, various types of splints are used to prevent footdrop. When used, the splints are removed and reapplied every 2 hours. 37. A patient who is being treated in the hospital for a spinal cord injury is advocating for the removal of his urinary catheter, stating that he wants to try to resume normal elimination. What principle should guide the care teams decision regarding this intervention? A) Urinary retention can have serious consequences in patients with SCIs. B) Urinary function is permanently lost following an SCI. C) Urinary catheters should not remain in place for more than 7 days. D) Overuse of urinary catheters can exacerbate nerve damage. A Feedback: Bladder distention, a major cause of autonomic dysreflexia, can also cause trauma. For this reason, removal of a urinary catheter must be considered with caution. Extended use of urinary catheterization is often necessary following SCI. The effect of a spinal cord lesion on urinary function depends on the level of the injury. Catheter use does not cause nerve damage, although it is a major risk factor for UTIs. 38. A patient with spinal cord injury is ready to be discharged home. A family member asks the nurse to review potential complications one more time. What are the potential complications that should be monitored for in this patient? Select all that apply. A) Orthostatic hypotension B) Autonomic dysreflexia C) DVT D) Salt-wasting syndrome E) Increased ICP A, B, C Feedback: For a spinal cord-injured patient, based on the assessment data, potential complications that may develop include DVT, orthostatic hypotension, and autonomic dysreflexia. Salt-wasting syndrome or increased ICP are not typical complications following the immediate recovery period. 39. The nurse recognizes that a patient with a SCI is at risk for muscle spasticity. How can the nurse best prevent this complication of an SCI? A) Position the patient in a high Fowlers position when in bed. B) Support the knees with a pillow when the patient is in bed. C) Perform passive ROM exercises as ordered. D) Administer NSAIDs as ordered. C Feedback: Passive ROM exercises can prevent muscle spasticity following SCI. NSAIDs are not used for this purpose. Pillows and sitting upright do not directly address the patients risk of muscle spasticity. 40. A patient is admitted to the neurologic ICU with a C4 spinal cord injury. When writing the plan of care for this patient, which of the following nursing diagnoses would the nurse prioritize in the immediate care of this patient? A) Risk for impaired skin integrity related to immobility and sensory loss B) Impaired physical mobility related to loss of motor function C) Ineffective breathing patterns related to weakness of the intercostal muscles D) Urinary retention related to inability to void spontaneously C Feedback: A nursing diagnosis related to breathing pattern would be the priority for this patient. A C4 spinal cord injury will require ventilatory support, due to the diaphragm and intercostals being affected. The other nursing diagnoses would be used in the care plan, but not designated as a higher priority than ineffective breathing patterns. Chapter 69: Management of Patients with Neurologic Infections, Autoimmune Disorders, and Neuropathies 1. A patient with possible bacterial meningitis is admitted to the ICU. What assessment finding would the nurse expect for a patient with this diagnosis? A) Pain upon ankle dorsiflexion of the foot B) Neck flexion produces flexion of knees and hips C) Inability to stand with eyes closed and arms extended without swaying D) Numbness and tingling in the lower extremities B Feedback: Clinical manifestations of bacterial meningitis include a positive Brudzinskis sign. Neck flexion producing flexion of knees and hips correlates with a positive Brudzinskis sign. Positive Homans sign (pain upon dorsiflexion of the foot) and negative Rombergs sign (inability to stand with eyes closed and arms extended) are not expected assessment findings for the patient with bacterial meningitis. Peripheral neuropathy manifests as numbness and tingling in the lower extremities. Again, this would not be an initial assessment to rule out bacterial meningitis. 2. The nurse is planning discharge education for a patient with trigeminal neuralgia. The nurse knows to include information about factors that precipitate an attack. What would the nurse be correct in teaching the patient to avoid? A) Washing his face B) Exposing his skin to sunlight C) Using artificial tears D) Drinking large amounts of fluids A Feedback: Washing the face should be avoided if possible because this activity can trigger an attack of pain in a patient with trigeminal neuralgia. Using artificial tears would be an appropriate behavior. Exposing the skin to sunlight would not be harmful to this patient. Temperature extremes in beverages should be avoided. 3. The nurse is caring for a patient with multiple sclerosis (MS). The patient tells the nurse the hardest thing to deal with is the fatigue. When teaching the patient how to reduce fatigue, what action should the nurse suggest? A) Taking a hot bath at least once daily B) Resting in an air-conditioned room whenever possible C) Increasing the dose of muscle relaxants D) Avoiding naps during the day B Feedback: Fatigue is a common symptom of patients with MS. Lowering the body temperature by resting in an air- conditioned room may relieve fatigue; however, extreme cold should be avoided. A hot bath or shower can increase body temperature, producing fatigue. Muscle relaxants, prescribed to reduce spasticity, can cause drowsiness and fatigue. Planning for frequent rest periods and naps can relieve fatigue. Other measures to reduce fatigue in the patient with MS include treating depression, using occupational therapy to learn energy conservation techniques, and reducing spasticity. 4. A patient with Guillain-Barr syndrome has experienced a sharp decline in vital capacity. What is the nurses most appropriate action? A) Administer bronchodilators as ordered. B) Remind the patient of the importance of deep breathing and coughing exercises. C) Prepare to assist with intubation. D) Administer supplementary oxygen by nasal cannula. C Feedback: For the patient with Guillain-Barr syndrome, mechanical ventilation is required if the vital capacity falls, making spontaneous breathing impossible and tissue oxygenation inadequate. Each of the other listed actions is likely insufficient to meet the patients oxygenation needs. 5. A patient diagnosed with Bells palsy is being cared for on an outpatient basis. During health education, the nurse should promote which of the following actions? A) Applying a protective eye shield at night B) Chewing on the affected side to prevent unilateral neglect C) Avoiding the use of analgesics whenever possible D) Avoiding brushing the teeth A Feedback: Corneal irritation and ulceration may occur if the eye is unprotected. While paralysis lasts, the involved eye must be protected. The patient should be encouraged to eat on the unaffected side, due to swallowing difficulties. Analgesics are used to control the facial pain. The patient should continue to provide self-care including oral hygiene. 6. The nurse is working with a patient who is newly diagnosed with MS. What basic information should the nurse provide to the patient? A) MS is a progressive demyelinating disease of the nervous system. B) MS usually occurs more frequently in men. C) MS typically has an acute onset. D) MS is sometimes caused by a bacterial infection. A Feedback: MS is a chronic, degenerative, progressive disease of the central nervous system, characterized by the occurrence of small patches of demyelination in the brain and spinal cord. The cause of MS is not known, and the disease affects twice as many women as men. 7. The nurse is creating a plan of care for a patient who has a recent diagnosis of MS. Which of the following should the nurse include in the patients care plan? A) Encourage patient to void every hour. B) Order a low-residue diet. C) Provide total assistance with all ADLs. D) Instruct the patient on daily muscle stretching. D Feedback: A patient diagnosed with MS should be encouraged to increase the fiber in his or her diet and void 30 minutes after drinking to help train the bladder. The patient should participate in daily muscle stretching to help alleviate and relax muscle spasms. 8. A patient with metastatic cancer has developed trigeminal neuralgia and is taking carbamazepine (Tegretol) for pain relief. What principle applies to the administration of this medication? A) Tegretol is not known to have serious adverse effects. B) The patient should be monitored for bone marrow depression. C) Side effects of the medication include renal dysfunction. D) The medication should be first taken in the maximum dosage form to be effective. B Feedback: The anticonvulsant agents carbamazepine (Tegretol) and phenytoin (Dilantin) relieve pain in most patients diagnosed with trigeminal neuralgia by reducing the transmission of impulses at certain nerve terminals. Side effects include nausea, dizziness, drowsiness, and aplastic anemia. Carbamazepine should be gradually increased until pain relief is obtained. 9. A male patient presents to the clinic complaining of a headache. The nurse notes that the patient is guarding his neck and tells the nurse that he has stiffness in the neck area. The nurse suspects the patient may have meningitis. What is another well-recognized sign of this infection? A) Negative Brudzinskis sign B) Positive Kernigs sign C) Hyperpatellar reflex D) Sluggish pupil reaction B Feedback: Meningeal irritation results in a number of well-recognized signs commonly seen in meningitis, such as a positive Kernigs sign, a positive Brudzinskis sign, and photophobia. Hyperpatellar reflex and a sluggish pupil reaction are not commonly recognized signs of meningitis. 10. The nurse is developing a plan of care for a patient newly diagnosed with Bells palsy. The nurses plan of care should address what characteristic manifestation of this disease? A) Tinnitus B) Facial paralysis C) Pain at the base of the tongue D) Diplopia B Feedback: Bells palsy is characterized by facial dysfunction, weakness, and paralysis. It does not result in diplopia, pain at the base of the tongue, or tinnitus. The nurse caring for a patient diagnosed with Guillain-Barr syndrome is planning care with regard to the clinical manifestations associated this syndrome. The nurses communication with the patient should reflect the possibility of what sign or symptom of the disease? A) Intermittent hearing loss B) Tinnitus C) Tongue enlargement D) Vocal paralysis D Feedback: Guillain-Barr syndrome is a disorder of the vagus nerve. Clinical manifestations include vocal paralysis, dysphagia, and voice changes (temporary or permanent hoarseness). Hearing deficits, tinnitus, and tongue enlargement are not associated with the disease. 12. The nurse is preparing to provide care for a patient diagnosed with myasthenia gravis. The nurse should know that the signs and symptoms of the disease are the result of what? A) Genetic dysfunction B) Upper and lower motor neuron lesions C) Decreased conduction of impulses in an upper motor neuron lesion D) A lower motor neuron lesion D Feedback: Myasthenia gravis is characterized by a weakness of muscles, especially in the face and throat, caused by a lower neuron lesion at the myoneural junction. It is not a genetic disorder. A combined upper and lower neuron lesion generally occurs as a result of spinal injuries. A lesion involving cranial nerves and their axons in the spinal cord would cause decreased conduction of impulses at an upper motor neuron. 13. A patient with suspected Creutzfeldt-Jakob disease (CJD) is being admitted to the unit. The nurse would expect what diagnostic test to be ordered for this patient? A) Cerebral angiography B) ABG analysis C) CT D) EEG D Feedback: The EEG reveals a characteristic pattern over the duration of CJD. A CT scan may be used to rule out disorders that may mimic the symptoms of CJD. ABGs would not be necessary until the later stages of CJD; they would not be utilized as a diagnostic test. Cerebral angiography is not used to diagnose CJD. 14. To alleviate pain associated with trigeminal neuralgia, a patient is taking Tegretol (carbamazepine). What health education should the nurse provide to the patient before initiating this treatment? A) Concurrent use of calcium supplements is contraindicated. B) Blood levels of the drug must be monitored. C) The drug is likely to cause hyperactivity and agitation. D) Tegretol can cause tinnitus during the first few days of treatment. B Feedback: Side effects of Tegretol include nausea, dizziness, drowsiness, and aplastic anemia. The patient must also be monitored for bone marrow depression during long-term therapy. Skin discoloration, insomnia, and tinnitus are not side effects of Tegretol. 15. A patient with herpes simplex virus encephalitis (HSV) has been admitted to the ICU. What medication would the nurse expect the physician to order for the treatment of this disease process? A) Cyclosporine (Neoral) B) Acyclovir (Zovirax) C) Cyclobenzaprine (Flexeril) D) Ampicillin (Prinicpen) B Feedback: Acyclovir (Zovirax) or ganciclovir (Cytovene), antiviral agents, are the medications of choice in the treatment of HSV. The mode of action is the inhibition of viral DNA replication. To prevent relapse, treatment would continue for up to 3 weeks. Cyclosporine is an immunosuppressant and antirheumatic. Cyclobenzaprine is a centrally acting skeletal muscle relaxant. Ampicillin, an antibiotic, is ineffective against viruses. 16. A middle-aged woman has sought care from her primary care provider and undergone diagnostic testing that has resulted in a diagnosis of MS. What sign or symptom is most likely to have prompted the woman to seek care? A) Cognitive declines B) Personality changes C) Contractures D) Difficulty in coordination D Feedback: The primary symptoms of MS most commonly reported are fatigue, depression, weakness, numbness, difficulty in coordination, loss of balance, spasticity, and pain. Cognitive changes and contractures usually occur later in the disease. 17. A nurse is planning the care of a 28-year-old woman hospitalized with a diagnosis of myasthenia gravis. What approach would be most appropriate for the care and scheduling of diagnostic procedures for this patient? A) All at one time, to provide a longer rest period B) Before meals, to stimulate her appetite C) In the morning, with frequent rest periods D) Before bedtime, to promote rest C Feedback: Procedures should be spaced to allow for rest in between. Procedures should be avoided before meals, or the patient may be too exhausted to eat. Procedures should be avoided near bedtime if possible. 18. The nurse is caring for a patient who is hospitalized with an exacerbation of MS. To ensure the patients safety, what nursing action should be performed? A) Ensure that suction apparatus is set up at the bedside. B) Pad the patients bed rails. C) Maintain bed rest whenever possible. D) Provide several small meals each day. A Feedback: Because of the patients risk of aspiration, it is important to have a suction apparatus at hand. Bed rest should be generally be minimized, not maximized, and there is no need to pad the patients bed rails or to provide multiple small meals. 19. A 33-year-old patient presents at the clinic with complaints of weakness, incoordination, dizziness, and loss of balance. The patient is hospitalized and diagnosed with MS. What sign or symptom, revealed during the initial assessment, is typical of MS? A) Diplopia, history of increased fatigue, and decreased or absent deep tendon reflexes B) Flexor spasm, clonus, and negative Babinskis reflex C) Blurred vision, intention tremor, and urinary hesitancy D) Hyperactive abdominal reflexes and history of unsteady gait and episodic paresthesia in both legs C Feedback: Optic neuritis, leading to blurred vision, is a common early sign of MS, as is intention tremor (tremor when performing an activity). Nerve damage can cause urinary hesitancy. In MS, deep tendon reflexes are increased or hyperactive. A positive Babinskis reflex is found in MS. Abdominal reflexes are absent with MS. 20. The nurse is developing a plan of care for a patient with Guillain-Barr syndrome. Which of the following interventions should the nurse prioritize for this patient? A) Using the incentive spirometer as prescribed B) Maintaining the patient on bed rest C) Providing aids to compensate for loss of vision D) Assessing frequently for loss of cognitive function A Feedback: Respiratory function can be maximized with incentive spirometry and chest physiotherapy. Nursing interventions toward enhancing physical mobility should be utilized. Nursing interventions are aimed at preventing a deep vein thrombosis. Guillain-Barr syndrome does not affect cognitive function or vision. 21. A 69-year-old patient is brought to the ED by ambulance because a family member found him lying on the floor disoriented and lethargic. The physician suspects bacterial meningitis and admits the patient to the ICU. The nurse knows that risk factors for an unfavorable outcome include what? Select all that apply. A) Blood pressure greater than 140/90 mm Hg B) Heart rate greater than 120 bpm C) Older age D) Low Glasgow Coma Scale E) Lack of previous immunizations B, C, D Feedback: Risks for an unfavorable outcome of meningitis include older age, a heart rate greater than 120 beats/minute, low Glasgow Coma Scale score, cranial nerve palsies, and a positive Gram stain 1 hour after presentation to the hospital. A BP greater than 140/90 mm Hg is indicative of hypertension, but is not necessarily related to poor outcomes related to meningitis. Immunizations are not normally relevant to the course of the disease. 22. The critical care nurse is caring for 25-year-old man admitted to the ICU with a brain abscess. What is a priority nursing responsibility in the care of this patient? A) Maintaining the patients functional independence B) Providing health education C) Monitoring neurologic status closely D) Promoting mobility C Feedback: Vigilant neurologic monitoring is a key aspect of caring for a patient who has a brain abscess. This supersedes education, ADLs, and mobility, even though these are all valid and important aspects of nursing care. 23. A patient is being admitted to the neurologic ICU with suspected herpes simplex virus encephalitis. What nursing action best addresses the patients complaints of headache? A) Initiating a patient-controlled analgesia (PCA) of morphine sulfate B) Administering hydromorphone (Dilaudid) IV as needed C) Dimming the lights and reducing stimulation D) Distracting the patient with activity C Feedback: Comfort measures to reduce headache include dimming the lights, limiting noise and visitors, grouping nursing interventions, and administering analgesic agents. Opioid analgesic medications may mask neurologic symptoms; therefore, they are used cautiously. Non-opioid analgesics may be preferred. Distraction is unlikely to be effective, and may exacerbate the patients pain. 24. A patient is admitted through the ED with suspected St. Louis encephalitis. The unique clinical feature of St. Louis encephalitis will make what nursing action a priority? A) Serial assessments of hemoglobin levels B) Blood glucose monitoring C) Close monitoring of fluid balance D) Assessment of pain along dermatomes C Feedback: A unique clinical feature of St. Louis encephalitis is SIADH with hyponatremia. As such, it is important to monitor the patients intake and output closely. 25. The nurse is caring for a 77-year-old woman with MS. She states that she is very concerned about the progress of her disease and what the future holds. The nurse should know that elderly patients with MS are known to be particularly concerned about what variables? Select all that apply. A) Possible nursing home placement B) Pain associated with physical therapy C) Increasing disability D) Becoming a burden on the family E) Loss of appetite A, C, D Feedback: Elderly patients with MS are particularly concerned about increasing disability, family burden, marital concern, and the possible future need for nursing home care. Older adults with MS are not noted to have particular concerns regarding the pain of therapy or loss of appetite. 26. You are the clinic nurse caring for a patient with a recent diagnosis of myasthenia gravis. The patient has begun treatment with pyridostigmine bromide (Mestinon). What change in status would most clearly suggest a therapeutic benefit of this medication? A) Increased muscle strength B) Decreased pain C) Improved GI function D) Improved cognition A Feedback: The goal of treatment using pyridostigmine bromide is improvement of muscle strength and control of fatigue. The drug is not intended to treat pain, or cognitive or GI functions. 27. The critical care nurse is admitting a patient in myasthenic crisis to the ICU. The nurse should prioritize what nursing action in the immediate care of this patient? A) Suctioning secretions B) Facilitating ABG analysis C) Providing ventilatory assistance D) Administering tube feedings C Feedback: Providing ventilatory assistance takes precedence in the immediate management of the patient with myasthenic crisis. It may be necessary to suction secretions and/or provide tube feedings, but they are not the priority for this patient. ABG analysis will be done, but this is not the priority. 28. The nurse caring for a patient in ICU diagnosed with Guillain-Barr syndrome should prioritize monitoring for what potential complication? A) Impaired skin integrity B) Cognitive deficits C) Hemorrhage D) Autonomic dysfunction D Feedback: Based on the assessment data, potential complications that may develop include respiratory failure and autonomic dysfunction. Skin breakdown, decreased cognition, and hemorrhage are not complications of Guillain-Barr syndrome. The nurse is teaching a patient with Guillain-Barr syndrome about the disease. The patient asks how he can ever recover if demyelination of his nerves is occurring. What would be the nurses best response? A) Guillain-Barr spares the Schwann cell, which allows for remyelination in the recovery phase of the disease. B) In Guillain-Barr, Schwann cells replicate themselves before the disease destroys them, so remyelination is possible. C) I know you understand that nerve cells do not remyelinate, so the physician is the best one to answer your question. D) For some reason, in Guillain-Barr, Schwann cells become activated and take over the remyelination process. A Feedback: Myelin is a complex substance that covers nerves, providing insulation and speeding the conduction of impulses from the cell body to the dendrites. The cell that produces myelin in the peripheral nervous system is the Schwann cell. In Guillain-Barr syndrome, the Schwann cell is spared, allowing for remyelination in the recovery phase of the disease. The nurse should avoid downplaying the patients concerns by wholly deferring to the physician. 30. A patient diagnosed with myasthenia gravis has been hospitalized to receive plasmapheresis for a myasthenic exacerbation. The nurse knows that the course of treatment for plasmapheresis in a patient with myasthenia gravis is what? A) Every day for 1 week B) Determined by the patients response C) Alternate days for 10 days D) Determined by the patients weight B Feedback: The typical course of plasmapheresis consists of daily or alternate-day treatment, and the number of treatments is determined by the patients response. 31. The nurse is discharging a patient home after surgery for trigeminal neuralgia. What advice should the nurse provide to this patient in order to reduce the risk of injury? A) Avoid watching television or using a computer for more than 1 hour at a time. B) Use OTC antibiotic eye drops for at least 14 days. C) Avoid rubbing the eye on the affected side of the face. D) Rinse the eye on the affected side with normal saline daily for 1 week. C Feedback: If the surgery results in sensory deficits to the affected side of the face, the patient is instructed not to rub the eye because the pain of a resulting injury will not be detected. There is no need to limit TV viewing or to rinse the eye daily. Antibiotics may or may not be prescribed, and these would not reduce the risk of injury. 32. A patient diagnosed with Bells palsy is having decreased sensitivity to touch of the involved nerve. What should the nurse recommend to prevent atrophy of the muscles? A) Blowing up balloons B) Deliberately frowning C) Smiling repeatedly D) Whistling D Feedback: Facial exercises, such as wrinkling the forehead, blowing out the cheeks, and whistling, may be performed with the aid of a mirror to prevent muscle atrophy. Blowing up balloons, frowning, and smiling are not considered facial exercises. 33. A patient with diabetes presents to the clinic and is diagnosed with a mononeuropathy. This patients nursing care should involve which of the following? A) Protection of the affected limb from injury B) Passive and active ROM exercises for the affected limb C) Education about improvements to glycemic control D) Interventions to prevent contractures A Feedback: Nursing care involves protection of the affected limb or area from injury, as well as appropriate patient teaching about mononeuropathy and its treatment. Nursing care for this patient does not likely involve exercises or assistive devices, since these are unrelated to the etiology of the disease. Improvements to diabetes management may or may not be necessary. 34. A patient diagnosed with MS has been admitted to the medical unit for treatment of an MS exacerbation. Included in the admission orders is baclofen (Lioresal). What should the nurse identify as an expected outcome of this treatment? A) Reduction in the appearance of new lesions on the MRI B) Decreased muscle spasms in the lower extremities C) Increased muscle strength in the upper extremities D) Decreased severity and duration of exacerbations B Feedback: Baclofen, a g-aminobutyric acid (GABA) agonist, is the medication of choice in treating spasms. It can be administered orally or by intrathecal injection. Avonex and Betaseron reduce the appearance of new lesions on the MRI. Corticosteroids limit the severity and duration of exacerbations. Anticholinesterase agents increase muscle strength in the upper extremities. 35. A 35-year-old woman is diagnosed with a peripheral neuropathy. When making her plan of care, the nurse knows to include what in patient teaching? Select all that apply. A) Inspect the lower extremities for skin breakdown. B) Footwear needs to be accurately sized. C) Immediate family members should be screened for the disease. D) Assistive devices may be needed to reduce the risk of falls. E) Dietary modifications are likely necessary. A, B, D Feedback: The plan of care includes inspection of the lower extremities for skin breakdown. Footwear should be accurately sized. Assistive devices, such as a walker or cane, may decrease the risk of falls. Bath water temperature is checked to avoid thermal injury. Peripheral neuropathies do not have a genetic component and diet is unrelated. 36. A 73-year-old man comes to the clinic complaining of weakness and loss of sensation in his feet and legs. Assessment of the patient shows decreased reflexes bilaterally. Why would it be a challenge to diagnose a peripheral neuropathy in this patient? A) Older adults are often vague historians. B) The elderly have fewer peripheral nerves than younger adults. C) Many older adults are hesitant to admit that their body is changing. D) Many symptoms can be the result of normal aging process. D Feedback: The diagnosis of peripheral neuropathy in the geriatric population is challenging because many symptoms, such as decreased reflexes, can be associated with the normal aging process. In this scenario, the patient has come to the clinic seeking help for his problem; this does not indicate a desire on the part of the patient to withhold information from the health care giver. The normal aging process does not include a diminishing number of peripheral nerves. 37. A patient with MS has been admitted to the hospital following an acute exacerbation. When planning the patients care, the nurse addresses the need to enhance the patients bladder control. What aspect of nursing care is most likely to meet this goal? A) Establish a timed voiding schedule. B) Avoid foods that change the pH of urine. C) Perform intermittent catheterization q6h. D) Administer anticholinergic drugs as ordered. A Feedback: A timed voiding schedule addresses many of the challenges with urinary continence that face the patient with MS. Interventions should be implemented to prevent the need for catheterization and anticholinergics are not normally used. 38. A patient with MS has developed dysphagia as a result of cranial nerve dysfunction. What nursing action should the nurse consequently perform? A) Arrange for the patient to receive a low residue diet. B) Position the patient upright during feeding. C) Suction the patient following each meal. D) Withhold liquids until the patient has finished eating. B Feedback: Correct, upright positioning is necessary to prevent aspiration in the patient with dysphagia. There is no need for a low-residue diet and suctioning should not be performed unless there is an apparent need. Liquids do not need to be withheld during meals in order to prevent aspiration. 39. A 48-year-old patient has been diagnosed with trigeminal neuralgia following recent episodes of unilateral face pain. The nurse should recognize what implication of this diagnosis? A) The patient will likely require lifelong treatment with anticholinergic medications. B) The patient has a disproportionate risk of developing myasthenia gravis later in life. C) The patient needs to be assessed for MS. D) The disease is self-limiting and the patient will achieve pain relief over time. C Feedback: Patients that develop trigeminal neuralgia before age 50 should be evaluated for the coexistent of MS because trigeminal neuralgia occurs in approximately 5% of patients with MS. Treatment does not include anticholinergics and the disease is not self-limiting. Trigeminal neuralgia is not associated with an increased risk of myasthenia gravis. 40. A patient presents at the clinic complaining of pain and weakness in her hands. On assessment, the nurse notes diminished reflexes in the upper extremities bilaterally and bilateral loss of sensation. The nurse knows that these findings are indicative of what? A) Guillain-Barr syndrome B) Myasthenia gravis C) Trigeminal neuralgia D) Peripheral nerve disorder D Feedback: The major symptoms of peripheral nerve disorders are loss of sensation, muscle atrophy, weakness, diminished reflexes, pain, and paresthesia (numbness, tingling) of the extremities. Trigeminal neuralgia is a condition of the fifth cranial nerve that is characterized by paroxysms of pain in the area innervated by any of the three branches, but most commonly the second and third branches of the trigeminal nerve. Myasthenia gravis, an autoimmune disorder affecting the myoneural junction, is characterized by varying degrees of weakness of the voluntary muscles. Guillain-Barr syndrome is an autoimmune attack on the peripheral nerve myelin. Chapter 70: Management of Patients With Oncologic or Degenerative Neurologic Disorders 1. A nurse is assessing a patient with an acoustic neuroma who has been recently admitted to an oncology unit. What symptoms is the nurse likely to find during the initial assessment? A) Loss of hearing, tinnitus, and vertigo B) Loss of vision, change in mental status, and hyperthermia C) Loss of hearing, increased sodium retention, and hypertension D) Loss of vision, headache, and tachycardia A Feedback: An acoustic neuroma is a tumor of the eighth cranial nerve, the cranial nerve most responsible for hearing and balance. The patient with an acoustic neuroma usually experiences loss of hearing, tinnitus, and episodes of vertigo and staggering gait. Acoustic neuromas do not cause loss of vision, increased sodium retention, or tachycardia. 2. A 25-year-old female patient with brain metastases is considering her life expectancy after her most recent meeting with her oncologist. Based on the fact that the patient is not receiving treatment for her brain metastases, what is the nurses most appropriate action? A) Promoting the patients functional status and ADLs B) Ensuring that the patient receives adequate palliative care C) Ensuring that the family does not tell the patient that her condition is terminal D) Promoting adherence to the prescribed medication regimen B Feedback: Patients with intracerebral metastases who are not treated have a steady downhill course with a limited survival time, whereas those who are treated may survive for slightly longer periods, but for most cure is not possible. Palliative care is thus necessary. This is a priority over promotion of function and the family should not normally withhold information from the patient. Adherence to medications such as analgesics is important, but palliative care is a high priority. 3. The nurse is writing a care plan for a patient with brain metastases. The nurse decides that an appropriate nursing diagnosis is anxiety related to lack of control over the health circumstances. In establishing this plan of care for the patient, the nurse should include what intervention? A) The patient will receive antianxiety medications every 4 hours. B) The patients family will be instructed on planning the patients care. C) The patient will be encouraged to verbalize concerns related to the disease and its treatment. D) The patient will begin intensive therapy with the goal of distraction. C Feedback: Patients need the opportunity to exercise some control over their situation. A sense of mastery can be gained as they learn to understand the disease and its treatment and how to deal with their feelings. Distraction and administering medications will not allow the patient to gain control over anxiety. Delegating planning to the family will not help the patient gain a sense of control and autonomy. 4. A patient with suspected Parkinsons disease is initially being assessed by the nurse. When is the best time to assess for the presence of a tremor? A) When the patient is resting B) When the patient is ambulating C) When the patient is preparing his or her meal tray to eat D) When the patient is participating in occupational therapy A Feedback: The tremor is present while the patient is at rest; it increases when the patient is walking, concentrating, or feeling anxious. Resting tremor characteristically disappears with purposeful movement, but is evident when the extremities are motionless. Consequently, the nurse should assess for the presence of a tremor when the patient is not performing deliberate actions. 5. The clinic nurse caring for a patient with Parkinsons disease notes that the patient has been taking levodopa and carbidopa (Sinemet) for 7 years. For what common side effect of Sinemet would the nurse assesses this patient? A) Pruritus B) Dyskinesia C) Lactose intolerance D) Diarrhea B Feedback: Within 5 to 10 years of taking levodopa, most patients develop a response to the medication characterized by dyskinesia (abnormal involuntary movements). Another potential complication of long- term dopaminergic medication use is neuroleptic malignant syndrome characterized by severe rigidity, stupor, and hyperthermia. Side effects of long-term Sinemet therapy are not pruritus, lactose intolerance, or diarrhea. 6. The nurse is caring for a boy who has muscular dystrophy. When planning assistance with the patients ADLs, what goal should the nurse prioritize? A) Promoting the patients recovery from the disease B) Maximizing the patients level of function C) Ensuring the patients adherence to treatment D) Fostering the familys participation in care B Feedback: Priority for the care of the child with muscular dystrophy is the need to maximize the patients level of function. Family participation is also important, but should be guided by this goal. Adherence is not a central goal, even though it is highly beneficial, and the disease is not curable. 7. A 37-year-old man is brought to the clinic by his wife because he is experiencing loss of motor function and sensation. The physician suspects the patient has a spinal cord tumor and hospitalizes him for diagnostic testing. In light of the need to diagnose spinal cord compression from a tumor, the nurse will most likely prepare the patient for what test? A) Anterior-posterior x-ray B) Ultrasound C) Lumbar puncture D) MRI D Feedback: The MRI scan is the most commonly used diagnostic procedure. It is the most sensitive diagnostic tool that is particularly helpful in detecting epidural spinal cord compression and vertebral bone metastases. 8. A patient with Parkinsons disease is undergoing a swallowing assessment because she has recently developed adventitious lung sounds. The patients nutritional needs should be met by what method? A) Total parenteral nutrition (TPN) B) Provision of a low-residue diet C) Semisolid food with thick liquids D) Minced foods and a fluid restriction C Feedback: A semisolid diet with thick liquids is easier for a patient with swallowing difficulties to consume than is a solid diet. Low-residue foods and fluid restriction are unnecessary and counterproductive to the patients nutritional status. The patients status does not warrant TPN. 9. While assessing the patient at the beginning of the shift, the nurse inspects a surgical dressing covering the operative site after the patients cervical diskectomy. The nurse notes that the drainage is 75% saturated with serosanguineous discharge. What is the nurses most appropriate action? A) Page the physician and report this sign of infection. B) Reinforce the dressing and reassess in 1 to 2 hours. C) Reposition the patient to prevent further hemorrhage. D) Inform the surgeon of the possibility of a dural leak. D Feedback: After a cervical diskectomy, the nurse will monitor the operative site and dressing covering this site. Serosanguineous drainage may indicate a dural leak. This constitutes a risk for meningitis, but is not a direct sign of infection. This should be reported to the surgeon, not just reinforced and observed. 10. A patient, diagnosed with cancer of the lung, has just been told he has metastases to the brain. What change in health status would the nurse attribute to the patients metastatic brain disease? A) Chronic pain B) Respiratory distress C) Fixed pupils D) Personality changes D Feedback: Neurologic signs and symptoms include headache, gait disturbances, visual impairment, personality changes, altered mentation (memory loss and confusion), focal weakness, paralysis, aphasia, and seizures. Pain, respiratory distress, and fixed pupils are not among the more common neurologic signs and symptoms of metastatic brain disease. 11. A patient has just been diagnosed with Parkinsons disease and the nurse is planning the patients subsequent care for the home setting. What nursing diagnosis should the nurse address when educating the patients family? A) Risk for infection B) Impaired spontaneous ventilation C) Unilateral neglect D) Risk for injury D Feedback: Individuals with Parkinsons disease face a significant risk for injury related to the effects of dyskinesia. Unilateral neglect is not characteristic of the disease, which affects both sides of the body. Parkinsons disease does not directly constitute a risk for infection or impaired respiration. 12. The nurse is caring for a patient with Huntington disease who has been admitted to the hospital for treatment of malnutrition. What independent nursing action should be implemented in the patients plan of care? A) Firmly redirect the patients head when feeding. B) Administer phenothiazines after each meal as ordered. C) Encourage the patient to keep his or her feeding area clean. D) Apply deep, gentle pressure around the patients mouth to aid swallowing. D Feedback: Nursing interventions for a patient who has inadequate nutritional intake should include the following: Apply deep gentle pressure around the patients mouth to assist with swallowing, and administer phenothiazines prior to the patients meal as ordered. The nurse should disregard the mess of the feeding area and treat the person with dignity. Stiffness and turning away by the patient during feeding are uncontrollable choreiform movements and should not be interrupted. 13. A patient has been admitted to the neurologic unit for the treatment of a newly diagnosed brain tumor. The patient has just exhibited seizure activity for the first time. What is the nurses priority response to this event? A) Identify the triggers that precipitated the seizure. B) Implement precautions to ensure the patients safety. C) Teach the patients family about the relationship between brain tumors and seizure activity. D) Ensure that the patient is housed in a private room. B Feedback: Patients with seizures are carefully monitored and protected from injury. Patient safety is a priority over health education, even though this is appropriate and necessary. Specific triggers may or may not be evident; identifying these is not the highest priority. A private room is preferable, but not absolutely necessary. 14. A patient diagnosed with a pituitary adenoma has arrived on the neurologic unit. When planning the patients care, the nurse should be aware that the effects of the tumor will primarily depend on what variable? A) Whether the tumor utilizes aerobic or anaerobic respiration B) The specific hormones secreted by the tumor C) The patients pre-existing health status D) Whether the tumor is primary or the result of metastasis B Feedback: Functioning pituitary tumors can produce one or more hormones normally produced by the anterior pituitary and the effects of the tumor depend largely on the identity of these hormones. This variable is more significant than the patients health status or whether the tumor is primary versus secondary. Anaerobic and aerobic respiration is not relevant. 15. A male patient with a metastatic brain tumor is having a generalized seizure and begins vomiting. What should the nurse do first? A) Perform oral suctioning. B) Page the physician. C) Insert a tongue depressor into the patients mouth. D) Turn the patient on his side. D Feedback: The nurses first response should be to place the patient on his side to prevent him from aspirating emesis. Inserting something into the seizing patients mouth is no longer part of a seizure protocol. Obtaining supplies to suction the patient would be a delegated task. Paging or calling the physician would only be necessary if this is the patients first seizure. 16. The nurse in an extended care facility is planning the daily activities of a patient with postpolio syndrome. The nurse recognizes the patient will best benefit from physical therapy when it is scheduled at what time? A) Immediately after meals B) In the morning C) Before bedtime D) In the early evening B Feedback: Important activities for patients with postpolio syndrome should be planned for the morning, as fatigue often increases in the afternoon and evening. 17. A patient newly diagnosed with a cervical disk herniation is receiving health education from the clinic nurse. What conservative management measures should the nurse teach the patient to implement? A) Perform active ROM exercises three times daily. B) Sleep on a firm mattress. C) Apply cool compresses to the back of the neck daily. D) Wear the cervical collar for at least 2 hours at a time. B Feedback: Proper positioning on a firm mattress and bed rest for 1 to 2 days may bring dramatic relief from pain. The patient may need to wear a cervical collar 24 hours a day during the acute phase of pain from a cervical disk herniation. Hot, moist compresses applied to the back of the neck will increase blood flow to the muscles and help relax the spastic muscles. 18. A patient has just returned to the unit from the PACU after surgery for a tumor within the spine. The patient complains of pain. When positioning the patient for comfort and to reduce injury to the surgical site, the nurse will position to patient in what position? A) In the high Fowlers position B) In a flat side-lying position C) In the Trendelenberg position D) In the reverse Trendelenberg position B Feedback: After spinal surgery, the bed is usually kept flat initially. The side-lying position is usually the most comfortable because this position imposes the least pressure on the surgical site. The Fowlers position, Trendelenberg position, and reverse Trendelenberg position are inappropriate for this patient because they would result in increased pain and complications. 19. A patient with Huntington disease has just been admitted to a long-term care facility. The charge nurse is creating a care plan for this patient. Nutritional management for a patient with Huntington disease should be informed by what principle? A) The patient is likely to have an increased appetite. B) The patient is likely to required enzyme supplements. C) The patient will likely require a clear liquid diet. D) The patient will benefit from a low-protein diet. A Feedback: Due to the continuous involuntary movements, patients will have a ravenous appetite. Despite this ravenous appetite, patients usually become emaciated and exhausted. As the disease progresses, patients experience difficulty in swallowing and thin liquids should be avoided. Protein will not be limited with this disease. Enzyme supplements are not normally required. 20. A patient with amyotrophic lateral sclerosis (ALS) is being visited by the home health nurse who is creating a care plan. What nursing diagnosis is most likely for a patient with this condition? A) Chronic confusion B) Impaired urinary elimination C) Impaired verbal communication D) Bowel incontinence C Feedback: Impaired communication is an appropriate nursing diagnosis; the voice in patients with ALS assumes a nasal sound and articulation becomes so disrupted that speech is unintelligible. Intellectual function is marginally impaired in patients with late ALS. Usually, the anal and bladder sphincters are intact because the spinal nerves that control muscles of the rectum and urinary bladder are not affected. 21. The nurse educator is discussing neoplasms with a group of recent graduates. The educator explains that the effects of neoplasms are caused by the compression and infiltration of normal tissue. The physiologic changes that result can cause what pathophysiologic events? Select all that apply. A) Intracranial hemorrhage B) Infection of cerebrospinal fluid C) Increased ICP D) Focal neurologic signs E) Altered pituitary function C, D, E Feedback: The effects of neoplasms are caused by the compression and infiltration of tissue. A variety of physiologic changes result, causing any or all of the following pathophysiologic events: increased ICP and cerebral edema, seizure activity and focal neurologic signs, hydrocephalus, and altered pituitary function. 22. The nurse is caring for a patient newly diagnosed with a primary brain tumor. The patient asks the nurse where his tumor came from. What would be the nurses best response? A) Your tumor originated from somewhere outside the CNS. B) Your tumor likely started out in one of your glands. C) Your tumor originated from cells within your brain itself. D) Your tumor is from nerve tissue somewhere in your body. C Feedback: Primary brain tumors originate from cells and structures within the brain. Secondary brain tumors are metastatic tumors that originate somewhere else in the body. The scenario does not indicate that the patients tumor is a pituitary tumor or a neuroma. 23. A gerontologic nurse is advocating for diagnostic testing of an 81-year-old patient who is experiencing personality changes. The nurse is aware of what factor that is known to affect the diagnosis and treatment of brain tumors in older adults? A) The effects of brain tumors are often attributed to the cognitive effects of aging. B) Brain tumors in older adults do not normally produce focal effects. C) Older adults typically have numerous benign brain tumors by the eighth decade of life. D) Brain tumors cannot normally be treated in patient over age 75. A Feedback: In older adult patients, early signs and symptoms of intracranial tumors can be easily overlooked or incorrectly attributed to cognitive and neurologic changes associated with normal aging. Brain tumors are not normally benign and they produce focal effects in all patients. Treatment options are not dependent primarily on age. 24. A patient who has been experiencing numerous episodes of unexplained headaches and vomiting has subsequently been referred for testing to rule out a brain tumor. What characteristic of the patients vomiting is most consistent with a brain tumor? A) The patients vomiting is accompanied by epistaxis. B) The patients vomiting does not relieve his nausea. C) The patients vomiting is unrelated to food intake. D) The patients emesis is blood-tinged. C Feedback: Vomiting is often unrelated to food intake if caused by a brain tumor. The presence or absence of blood is not related to the possible etiology and vomiting may or may not relieve the patients nausea. 25. A male patient presents at the free clinic with complaints of impotency. Upon physical examination, the nurse practitioner notes the presence of hypogonadism. What diagnosis should the nurse suspect? A) Prolactinoma B) Angioma C) Glioma D) Adrenocorticotropic hormone (ACTH)producing adenoma A Feedback: Male patients with prolactinomas may present with impotence and hypogonadism. An ACTH-producing adenoma would cause acromegaly. The scenario contains insufficient information to know if the tumor is an angioma, glioma, or neuroma. 26. The nurse is planning the care of a patient who has been recently diagnosed with a cerebellar tumor. Due to the location of this patients tumor, the nurse should implement measures to prevent what complication? A) Falls B) Audio hallucinations C) Respiratory depression D) Labile BP A Feedback: A cerebellar tumor causes dizziness, an ataxic or staggering gait with a tendency to fall toward the side of the lesion, and marked muscle incoordination. Because of this, the patient faces a high risk of falls. Hallucinations and unstable vital signs are not closely associated with cerebellar tumors. 27. A patient has been admitted to the neurologic ICU with a diagnosis of a brain tumor. The patient is scheduled to have a tumor resection/removal in the morning. Which of the following assessment parameters should the nurse include in the initial assessment? A) Gag reflex B) Deep tendon reflexes C) Abdominal girth D) Hearing acuity A Feedback: Preoperatively, the gag reflex and ability to swallow are evaluated. In patients with diminished gag response, care includes teaching the patient to direct food and fluids toward the unaffected side, having the patient sit upright to eat, offering a semisoft diet, and having suction readily available. Deep tendon reflexes, abdominal girth, and hearing acuity are less commonly affected by brain tumors and do not affect the risk for aspiration. 28. A patient with a brain tumor has begun to exhibit signs of cachexia. What subsequent assessment should the nurse prioritize? A) Assessment of peripheral nervous function B) Assessment of cranial nerve function C) Assessment of nutritional status D) Assessment of respiratory status C Feedback: Cachexia is a wasting syndrome of weight loss, muscle atrophy, fatigue, weakness, and significant loss of appetite. Consequently, nutritional assessment is paramount. 29. A patient with an inoperable brain tumor has been told that he has a short life expectancy. On what aspects of assessment and care should the home health nurse focus? Select all that apply. A) Pain control B) Management of treatment complications C) Interpretation of diagnostic tests D) Assistance with self-care E) Administration of treatments A, B, D, E Feedback: Home care needs and interventions focus on four major areas: palliation of symptoms and pain control, assistance in self-care, control of treatment complications, and administration of specific forms of treatment, such as parenteral nutrition. Interpretation of diagnostic tests is normally beyond the purview of the nurse. 30. An older adult has encouraged her husband to visit their primary care provider, stating that she is concerned that he may have Parkinsons disease. Which of the wifes descriptions of her husbands health and function is most suggestive of Parkinsons disease? A) Lately he seems to move far more slowly than he ever has in the past. B) He often complains that his joints are terribly stiff when he wakes up in the morning. C) Hes forgotten the names of some people that weve known for years. D) Hes losing weight even though he has a ravenous appetite. A Feedback: Parkinsons disease is characterized by bradykinesia. It does not manifest as memory loss, increased appetite, or joint stiffness. 31. A patient, brought to the clinic by his wife and son, is diagnosed with Huntington disease. When providing anticipatory guidance, the nurse should address the future possibility of what effect of Huntington disease? A) Metastasis B) Risk for stroke C) Emotional and personality changes D) Pathologic bone fractures C Feedback: Huntington disease causes profound changes to personality and behavior. It is a nonmalignant disease and stroke is not a central risk. The disease is not associated with pathologic bone fractures. 32. A patient who was diagnosed with Parkinsons disease several months ago recently began treatment with levodopa-carbidopa. The patient and his family are excited that he has experienced significant symptom relief. The nurse should be aware of what implication of the patients medication regimen? A) The patient is in a honeymoon period when adverse effects of levodopa-carbidopa are not yet evident. B) Benefits of levodopa-carbidopa do not peak until 6 to 9 months after the initiation of treatment. C) The patients temporary improvement in status is likely unrelated to levodopa-carbidopa. D) Benefits of levodopa-carbidopa often diminish after 1 or 2 years of treatment. D Feedback: The beneficial effects of levodopa therapy are most pronounced in the first year or two of treatment. Benefits begin to wane and adverse effects become more severe over time. However, a honeymoon period of treatment is not known. 33. The nurse caring for a patient diagnosed with Parkinsons disease has prepared a plan of care that would include what goal? A) Promoting effective communication B) Controlling diarrhea C) Preventing cognitive decline D) Managing choreiform movements A Feedback: The goals for the patient may include improving functional mobility, maintaining independence in ADLs, achieving adequate bowel elimination, attaining and maintaining acceptable nutritional status, achieving effective communication, and developing positive coping mechanisms. Constipation is more likely than diarrhea and cognition largely remains intact. Choreiform movements are related to Huntington disease. 34. The nurse is caring for a patient diagnosed with Parkinsons disease. The patient is having increasing problems with rising from the sitting to the standing position. What should the nurse suggest to the patient to use that will aid in getting from the sitting to the standing position as well as aid in improving bowel elimination? A) Use of a bedpan B) Use of a raised toilet seat C) Sitting quietly on the toilet every 2 hours D) Following the outlined bowel program B Feedback: A raised toilet seat is useful, because the patient has difficulty in moving from a standing to a sitting position. A handicapped toilet is not high enough and will not aid in improving bowel elimination. Sitting quietly on the toilet every 2 hours will not aid in getting from the sitting to standing position; neither will following the outlined bowel program. 35. A patient with Parkinsons disease is experiencing episodes of constipation that are becoming increasingly frequent and severe. The patient states that he has been achieving relief for the past few weeks by using OTC laxatives. How should the nurse respond? A) Its important to drink plenty of fluids while youre taking laxatives. B) Make sure that you supplement your laxatives with a nutritious diet. C) Lets explore other options, because laxatives can have side effects and create dependency. D) You should ideally be using herbal remedies rather than medications to promote bowel function. C Feedback: Laxatives should be avoided in patients with Parkinsons disease due to the risk of adverse effects and dependence. Herbal bowel remedies are not necessarily less risky. 36. A family member of a patient diagnosed with Huntington disease calls you at the clinic. She is requesting help from the Huntingtons Disease Society of America. What kind of help can this patient and family receive from this organization? Select all that apply. A) Information about this disease B) Referrals C) Public education D) Individual assessments E) Appraisals of research studies A, B, C Feedback: The Huntingtons Disease Society of America helps patients and families by providing information, referrals, family and public education, and support for research. It does not provide individual assessments or appraisals of individual research studies. 37. A patient with a new diagnosis of amyotrophic lateral sclerosis (ALS) is overwhelmed by his diagnosis and the known complications of the disease. How can the patient best make known his wishes for care as his disease progresses? A) Prepare an advance directive. B) Designate a most responsible physician (MRP) early in the course of the disease. C) Collaborate with representatives from the Amyotrophic Lateral Sclerosis Association. D) Ensure that witnesses are present when he provides instruction. A Feedback: Patients with ALS are encouraged to complete an advance directive or living will to preserve their autonomy in decision making. None of the other listed actions constitutes a legally binding statement of end-of-life care. 38. The nurse is caring for a patient who is scheduled for a cervical discectomy the following day. During health education, the patient should be made aware of what potential complications? A) Vertebral fracture B) Hematoma at the surgical site C) Scoliosis D) Renal trauma B Feedback: Based on all the assessment data, the potential complications of diskectomy may include hematoma at the surgical site, resulting in cord compression and neurologic deficit and recurrent or persistent pain after surgery. Renal trauma and fractures are unlikely; scoliosis is a congenital malformation of the spine. 39. The nurse responds to the call light of a patient who has had a cervical diskectomy earlier in the day. The patient states that she is having severe pain that had a sudden onset. What is the nurses most appropriate action? A) Palpate the surgical site. B) Remove the dressing to assess the surgical site. C) Call the surgeon to report the patients pain. D) Administer a dose of an NSAID. C Feedback: If the patient experiences a sudden increase in pain, extrusion of the graft may have occurred, requiring reoperation. A sudden increase in pain should be promptly reported to the surgeon. Administration of an NSAID would be an insufficient response and the dressing should not be removed without an order. Palpation could cause further damage. 40. A nurse is planning discharge education for a patient who underwent a cervical diskectomy. What strategies would the nurse assess that would aid in planning discharge teaching? A) Care of the cervical collar B) Technique for performing neck ROM exercises C) Home assessment of ABGs D) Techniques for restoring nerve function A Feedback: Prior to discharge, the nurse should assess the patients use and care of the cervical collar. Neck ROM exercises would be contraindicated and ABGs cannot be assessed in the home. Nerve function is not compromised by a diskectomy. Chapter 71: Management of Patients With Infectious Diseases 1. A male patient comes to the clinic and is diagnosed with gonorrhea. Which symptom most likely prompted him to seek medical attention? A) Rashes on the palms of the hands and soles of the feet B) Cauliflower-like warts on the penis C) Painful, red papules on the shaft of the penis D) Foul-smelling discharge from the penis D Feedback: Signs and symptoms of gonorrhea in men include purulent, foul-smelling drainage from the penis and painful urination. Rashes on the palms of the hands and soles of the feet are a sign of the secondary stage of syphilis. Cauliflower-like warts on the penis are a sign of human papillomavirus. Painful red papules on the shaft of the penis may be a sign of the first stage of genital herpes. 2. A nurse is caring for a child who was admitted to the pediatric unit with infectious diarrhea. The nurse should be alert to what assessment finding as an indicator of dehydration? A) Labile BP B) Weak pulse C) Fever D) Diaphoresis B Feedback: Assessment of dehydration includes evaluation of thirst, oral mucous membrane dryness, sunken eyes, a weakened pulse, and loss of skin turgor. Diaphoresis, labile BP, and fever are not characteristic signs and symptoms of dehydration. 3. A nursing home patient has been diagnosed with Clostridium difficile. What type of precautions should the nurse implement to prevent the spread of this infectious disease to other residents? A) Contact B) Droplet C) Airborne D) Positive pressure isolation A Feedback: Contact precautions are used for organisms that are spread by skin-to-skin contact, such as antibiotic- resistant organisms or Clostridium difficile. Droplet precautions are used for organisms that can be transmitted by close, face-to-face contact, such as influenza or meningococcal meningitis. Airborne precautions are required for patients with presumed or proven pulmonary TB or chickenpox. Positive pressure isolation is unnecessary and ineffective. 4. A nurse who provides care in a busy ED is in contact with hundreds of patients each year. The nurse has a responsibility to receive what vaccine? A) Hepatitis B vaccine B) Human papillomavirus (HPV) vaccine C) Clostridium difficile vaccine D) Staphylococcus aureus vaccine A Feedback: Nurses should recognize their personal responsibility to receive the hepatitis B vaccine and an annual influenza vaccine to reduce potential transmission to themselves and vulnerable patient groups. HPV is not a threat because it is sexually transmitted. No vaccines are available againstC. difficile and S. aureus. 5. When a disease infects a host a portal of entry is needed for an organism to gain access. What has been identified as the portal of entry for tuberculosis? A) Integumentary system B) Urinary system C) Respiratory system D) Gastrointestinal system C Feedback: The portal of entry for M. tuberculosis is through the respiratory tract. 6. A patient has a concentration of S. aureus located on his skin. The patient is not showing signs of increased temperature, redness, or pain at the site. The nurse is aware that this is a sign of a microorganism at which of the following stages? A) Infection B) Colonization C) Disease D) Bacteremia B Feedback: Colonization refers to the presence of microorganisms without host interference or interaction. Infection is a condition in which the host interacts physiologically and immunologically with a microorganism. Disease is the decline in wellness of a host due to infection. Bacteremia is a condition of bacteria in the blood. 7. An infectious outbreak of unknown origin has occurred in a long-term care facility. The nurse who oversees care at the facility should report the outbreak to what organization? A) Centers for Disease Control and Prevention (CDC) B) American Medical Association (AMA) C) Environmental Protection Agency (EPA) D) American Nurses Association (ANA) A Feedback: The goals of the CDC are to provide scientific recommendations regarding disease prevention and control to reduce disease, which it includes in publications. As such, outbreaks of unknown origin should normally be reported to the CDC. The AMA is the professional organization for medical doctors; the EPA oversees our environment; the ANA is the professional organization for American nurses. 8. The infectious control nurse is presenting a program on West Nile virus for a local community group. To reduce the incidence of this disease, the nurse should recommend what action? A) Covering open wounds at all times B) Vigilant handwashing in home and work settings C) Consistent use of mosquito repellants D) Annual vaccination C Feedback: West Nile virus is transmitted by mosquitoes, which become infected by biting birds that are infected with the virus. Prevention of mosquito bites can reduce the risk of contracting the disease. Handwashing and bandaging open wounds are appropriate general infection control measures, but these actions do not specifically prevent West Nile virus for which no vaccine currently exists. 9. An immunosuppressed patient is receiving chemotherapy treatment at home. What infection-control measure should the nurse recommend to the family? A) Family members should avoid receiving vaccinations until the patient has recovered from his or her illness. B) Wipe down hard surfaces with a dilute bleach solution once per day. C) Maintain cleanliness in the home, but recognize that the home does not need to be sterile. D) Avoid physical contact with the patient unless absolutely necessary. C Feedback: When assessing the risk of the immunosuppressed patient in the home environment for infection, it is important to realize that intrinsic colonizing bacteria and latent viral infections present a greater risk than do extrinsic environmental contaminants. The nurse should reassure the patient and family that their home needs to be clean but not sterile. Common-sense approaches to cleanliness and risk reduction are helpful. The family need not avoid vaccinations and it is unnecessary to avoid all contact or to wipe down surfaces daily. 10. A medical nurse is careful to adhere to infection control protocols, including handwashing. Which statement about handwashing supports the nurses practice? A) Frequent handwashing reduces transmission of pathogens from one patient to another. B) Wearing gloves is known to be an adequate substitute for handwashing. C) Bar soap is preferable to liquid soap. D) Waterless products should be avoided in situations where running water is unavailable. A Feedback: Whether gloves are worn or not, handwashing is required before and after patient contact because thorough handwashing reduces the risk of cross-contamination. Bar soap should not be used because it is a potential carrier of bacteria. Soap dispensers are preferable, but they must also be checked for bacteria. When water is unavailable, the nurse should wash using a liquid hand sanitizer. 11. A male patient with gonorrhea asks the nurse how he can reduce his risk of contracting another sexually transmitted infection. The patient is not in a monogamous relationship. The nurse should instruct the patient to do which of the following? A) Ask all potential sexual partners if they have a sexually transmitted disease. B) Wear a condom every time he has intercourse. C) Consider intercourse to be risk-free if his partner has no visible discharge, lesions, or rashes. D) Aim to limit the number of sexual partners to fewer than five over his lifetime. B Feedback: Wearing a condom during intercourse considerably reduces the risk of contracting STIs. The other options may help reduce the risk for contracting an STI, but not to the extent that wearing a condom will. A monogamous relationship reduces the risk of contracting STIs. 12. The nurse places a patient in isolation. Isolation techniques have the potential to break the chain of infection by interfering with what component of the chain of infection? A) Mode of transmission B) Agent C) Susceptible host D) Portal of entry A Feedback: Isolation techniques attempt to break the chain of infection by interfering with the transmission mode. These techniques do not directly affect the agent, host, or portal of entry. 13. The nurse is caring for a patient who is colonized with methicillin-resistant Staphylococcus aureus (MRSA). What infection control measure has the greatest potential to reduce transmission of MRSA and other nosocomial pathogens in a health care setting? A) Using antibacterial soap when bathing patients with MRSA B) Conducting culture surveys on a regularly scheduled basis C) Performing hand hygiene before and after contact with every patient D) Using aseptic housekeeping practices for environmental cleaning C Feedback: Handwashing is the major infection control measure to reduce the risk of transmission of MRSA and other nosocomial pathogens. No convincing evidence exists to support that bathing patients with antibacterial soap is effective. Culture surveys can help establish the true prevalence of MRSA in a facility, but are used only to help implement where and when infection-control measures are needed. Hand hygiene is known to be more clinically important than housekeeping. 14. A patient on Airborne Precautions asks the nurse to leave his door open. What is the nurses best reply? A) I have to keep your door shut at all times. Ill open the curtains so that you dont feel so closed in. B) Ill keep the door open for you, but please try to avoid moving around the room too much. C) I can open your door if you wear this mask. D) I can open your door, but Ill have to come back and close it in a few minutes. A Feedback: The nurse is placing the patient on airborne precautions, which require that doors and windows be closed at all times. Opening the curtains is acceptable. Antibiotics, wearing a mask, and standard precautions are not sufficient to allow the patients door to be open. 15. Family members are caring for a patient with HIV in the patients home. What should the nurse encourage family members to do to reduce the risk of infection transmission? A) Use caution when shaving the patient. B) Use separate dishes for the patient and family members. C) Use separate bed linens for the patient. D) Disinfect the patients bedclothes regularly. A Feedback: When caring for a patient with HIV at home, family members should use caution when providing care that may expose them to the patients blood, such as shaving. Dishes, bed linens, and bedclothes, unless contaminated with blood, only require the usual cleaning. 16. A nurse is preparing to administer a patients scheduled dose of subcutaneous heparin. To reduce the risk of needlestick injury, the nurse should perform what action? A) Recap the needle before leaving the bedside. B) Recap the needle immediately before leaving the room. C) Avoid recapping the needle before disposing of it. D) Wear gloves when administering the injection. C Feedback: Used needles should not be recapped. Instead, they are placed directly into puncture-resistant containers near the place where they are used. Gloves do not prevent needlestick injuries. 17. A 16-year-old male patient comes to the free clinic and is subsequently diagnosed with primary syphilis. What health problem most likely prompted the patient to seek care? A) The emergence of a chancre on his penis B) Painful urination C) Signs of a systemic infection D) Unilateral testicular swelling A Feedback: Primary syphilis occurs 2 to 3 weeks after initial inoculation with the organism. A painless chancre develops at the site of infection. Initial infection with syphilis is not associated with testicular swelling, painful voiding, or signs of systemic infection. 18. A patient on the medical unit is found to have pulmonary tuberculosis (TB). What is the most appropriate precaution for the staff to take to prevent transmission of this disease? A) Standard precautions only B) Droplet precautions C) Standard and contact precautions D) Standard and airborne precautions D Feedback: Airborne precautions are required for proven or suspected pulmonary TB. Standard precaution techniques are used in conjunction with the transmission-based precautions, regardless of the patients diagnosis. Droplet and contact precautions are insufficient. 19. An adult patient in the ICU has a central venous catheter in place. Over the past 24 hours, the patient has developed signs and symptoms that are suggestive of a central line associated bloodstream infection (CLABSI). What aspect of the patients care may have increased susceptibility to CLABSI? A) The patients central line was placed in the femoral vein. B) The patient had blood cultures drawn from the central line. C) The patient was treated for vancomycin-resistant enterococcus (VRE) during a previous admission. D) The patient has received antibiotics and IV fluids through the same line. A Feedback: In adult patients, the femoral site should be avoided in order to reduce the risk of CLABSI. Drawing blood cultures, receiving treatment for VRE, and receiving fluids and drugs through the same line are not known to increase the risk for CLABSI. 20. What is the best rationale for health care providers receiving the influenza vaccination on a yearly basis? A) To decreased nurses susceptibility to health care-associated infections B) To decrease risk of transmission to vulnerable patients C) To eventually eradicate the influenza virus in the United States D) To prevent the emergence of drug-resistant strains of the influenza virus B Feedback: To reduce the chance of transmission to vulnerable patients, health care workers are advised to obtain influenza vaccinations. The vaccine will not decrease nurses risks of developing health care-associated infections, eradicate the influenza virus, or decrease the risk of developing new strains of the influenza virus. 21. A patient has presented at the ED with copious diarrhea and accompanying signs of dehydration. During the patients health history, the nurse learns that the patient recently ate oysters from the Gulf of Mexico. The nurse should recognize the need to have the patients stool cultured for microorganisms associated with what disease? A) Ebola B) West Nile virus C) Legionnaires disease D) Cholera D Feedback: In the U.S., cholera should be suspected in patients who have watery diarrhea after eating shellfish harvested from the Gulf of Mexico. 22. A patient is alarmed that she has tested positive for MRSA following culture testing during her admission to the hospital. What should the nurse teach the patient about this diagnostic finding? A) There are promising treatments for MRSA, so this is no cause for serious concern. B) This doesnt mean that you have an infection; it shows that the bacteria live on one of your skin surfaces. C) The vast majority of patients in the hospital test positive for MRSA, but the infection doesnt normally cause serious symptoms. D) This finding is only preliminary, and your doctor will likely order further testing. B Feedback: This patients testing results are indicative of colonization, which is not synonymous with infection. The test results are considered reliable, and would not be characterized as preliminary. Treatment is not normally prescribed for colonizations. 23. A patients diagnostic testing revealed that he is colonized with vancomycin-resistantenterococcus (VRE). What change in the patients health status could precipitate an infection? A) Use of a narrow-spectrum antibiotic B) Treatment of a concurrent infection using vancomycin C) Development of a skin break D) Persistent contact of the bacteria with skin surfaces C Feedback: Colonization can progress to infection if there is a portal of entry by which bacteria can invade body tissues. The use of vancomycin, or any other antibiotic, would not necessarily precipitate a VRE infection. Prolonged skin contact is similarly unlikely to cause infection, provided the skin remains intact. 24. A clinic nurse is caring for a male patient diagnosed with gonorrhea who has been prescribed ceftriaxone and doxycycline. The patient asks why he is receiving two antibiotics. What is the nurses best response? A) There are many drug-resistant strains of gonorrhea, so more than one antibiotic may be required for successful treatment. B) The combination of these two antibiotics reduces the later risk of reinfection. C) Many people infected with gonorrhea are infected with chlamydia as well. D) This combination of medications will eradicate the infection twice as fast than a single antibiotic. C Feedback: Because patients are often coinfected with both gonorrhea and chlamydia, the CDC recommends dual therapy even if only gonorrhea has been laboratory proven. Although the number of resistant strains of gonorrhea has increased, that is not the reason for use of combination antibiotic therapy. Dual therapy is prescribed to treat both gonorrhea and chlamydia, because many patients with gonorrhea have a coexisting chlamydial infection. This combination of antibiotics does not reduce the risk of reinfection or provide a faster cure. 25. A student nurse completing a preceptorship is reviewing the use of standard precautions. Which of the following practices is most consistent with standard precautions? A) Wearing a mask and gown when starting an IV line B) Washing hands immediately after removing gloves C) Recapping all needles promptly after use to prevent needlestick injuries D) Double-gloving when working with a patient who has a blood-borne illness B Feedback: Standard precautions are used to prevent contamination from blood and body fluids. Gloves are worn whenever exposure is possible, and hands should be washed after removing gloves. Needles are never recapped after use because this increases the risk of accidental needlesticks. Under ordinary circumstances, masks and gowns are not necessary for starting an IV line. Double-gloving is not a recognized component of standard precautions. 26. A patient is admitted from the ED diagnosed with Neisseria meningitides. What type of isolation precautions should the nurse institute? A) Contact precautions B) Droplet precautions C) Airborne precautions D) Observation precautions B Feedback: This patient requires droplet precautions because the organism can be transmitted through large airborne droplets when the patient coughs, sneezes, or fails to cover the mouth. Smaller droplets can be addressed by airborne precautions, but this is insufficient for this microorganism. 27. During a health education session, a participant asks the nurse how a vaccine can protect from future exposures to diseases against which she is vaccinated. What would be the nurses best response? A) The vaccine causes an antibody response in the body. B) The vaccine responds to an infection in the body after it occurs. C) The vaccine is similar to an antibiotic that is used to treat an infection. D) The vaccine actively attacks the microorganism. A Feedback: Vaccines are an antigen preparation that produces an antibody response in a human to protect him or her from future exposure to the vaccinated organism. A vaccine does not respond to an infection after it occurs; it does not act like an antibiotic and does not actively attack the microorganism. 28. A 2-year-old is brought to the clinic by her mother who tells the nurse her daughter has diarrhea and the child is complaining of pain in her stomach. The mother says that the little girl had not eaten anything unusual, consuming homemade chicken strips and carrot sticks the evening prior. Which bacterial infection would the nurse suspect this little girl of contracting? A) Escherichia coli B) Salmonella C) Shigella D) Giardia lamblia B Feedback: Annually in the United States, Salmonella species contaminate approximately 2.2 million eggs (1 in 20,000 eggs) and one in eight chickens raised as meat. Diarrhea with gastroenteritis is a common manifestation associated with Salmonella. Recent outbreaks of E. coli have been associated with ingestion of undercooked beef. Shigella spreads through the fecaloral route, with easy transmission from one person to another. People infected with Giardia lambliacontract the disease by drinking contaminated water. 29. A public health nurse is teaching a mother about vaccinations prior to obtaining informed consent for her childs vaccination. What should the nurse cite as the most common adverse effect of vaccinations? A) Temporary sensitivity to the sun B) Allergic reactions to the antigen or carrier solution C) Nausea and vomiting D) Joint pain near the injection site B Feedback: The most common adverse effects are an allergic reaction to the antigen or carrier solution and the occurrence of the actual disease (often in modified form) when live vaccine is used. Reactions to vaccines do not typically include sensitivity to the sun, nausea and vomiting, or joint pain. 30. A mother brings her 12 month-old son into the clinic for his measles-mumps-rubella (MMR) vaccination. What would the clinic nurse advise the mother about the MMR vaccine? A) Photophobia and hives might occur. B) There are no documented reactions to an MMR. C) Fever and hypersensitivity reaction might occur. D) Hypothermia might occur. C Feedback: Patients should be advised that fever, transient lymphadenopathy, or a hypersensitivity reaction might occur following an MMR vaccination. Reactions to an MMR do not include photophobia or hypothermia. 31. An older adult patient tells the nurse that she had chicken pox as a child and is eager to be vaccinated against shingles. What should the nurse teach the patient about this vaccine? A) Vaccination against shingles is contraindicated in patients over the age of 80. B) Vaccination can reduce her risk of shingles by approximately 50%. C) Vaccination against shingles involves a series of three injections over the course of 6 months. D) Vaccination against shingles is only effective if preceded by a childhood varicella vaccination. B Feedback: Zostavax, a vaccine to reduce the risk of shingles, is recommended for people older than 60 years of age because it reduces the risk of shingles by approximately 50%. It does not need to be preceded by childhood varicella vaccine. The vaccine consists of a single injection. 32. The nurse educator is discussing emerging diseases with a group of nurses. The educator should cite what causes of emerging diseases? Select all that apply. A) Progressive weakening of human immune systems B) Use of extended-spectrum antibiotics C) Population movements D) Increased global travel E) Globalization of food supplies B, C, D, E Feedback: Many factors contribute to newly emerging or re-emerging infectious diseases. These include travel, globalization of food supply and central processing of food, population growth, increased urban crowding, population movements (e.g., those that result from war, famine, or man-made or natural disasters), ecologic changes, human behavior (e.g., risky sexual behavior, IV/injection drug use), antimicrobial resistance, and breakdown in public health measures. Not noted is an overall decline in human immunity. 33. An older adult patient has been diagnosed with Legionella infection. When planning this patients care, the nurse should prioritize which of the following nursing actions? A) Monitoring for evidence of skin breakdown B) Emotional support and promotion of coping C) Assessment for signs of internal hemorrhage D) Vigilant monitoring of respiratory status D Feedback: The lungs are the principal organs of Legionella infection. The patient develops increasing pulmonary symptoms, including productive cough, dyspnea, and chest pain. Consequently, respiratory support is vital. Hemorrhage and skin breakdown are not central manifestations of the disease. Preservation of the patients airway is a priority over emotional support, even though this aspect of care is important. 34. The nurse is caring for a patient with secondary syphilis. What intervention should the nurse institute when caring for this patient? A) Ensure that the patient is housed in a private room. B) Administer hydrocortisone ointment to the lesions as ordered. C) Administer combination therapy with antiretrovirals as ordered. D) Wear gloves if contact with lesions is possible. D Feedback: Lesions of primary and secondary syphilis may be highly infective. Gloves are worn when direct contact with lesions is likely, and hand hygiene is performed after gloves are removed. Isolation in a private room is not required. Corticosteroids antiviral medications are not indicated. 35. A long-term care facility is the site of an outbreak of infectious diarrhea. The nurse educator has emphasized the importance of hand hygiene to staff members. The use of alcohol-based cleansers may be ineffective if the causative microorganism is identified as what? A) Shigella B) Escherichia coli C) Clostridium difficile D) Norovirus C Feedback: The spore form of the bacterium C. difficile is resistant to alcohol and other hand disinfectants; therefore, the use of gloves and handwashing (soap and water for physical removal) are required when C. difficile has been identified. Each of the other listed microorganisms is susceptible to alcohol-based cleansers. 36. The nurse is providing care for an older adult patient who has developed signs and symptoms ofCalicivirus (Norovirus). What assessment should the nurse prioritize when planning this patients care? A) Respiratory status B) Pain C) Fluid intake and output D) Deep tendon reflexes and neurological status C Feedback: The vomiting and diarrhea that accompany Norovirus create a severe risk of fluid volume deficit. For this reason, assessments relating to fluid balance should be prioritized, even though each of the listed assessments should be included in the plan of care. 37. The nurse who provides care at a wilderness camp is teaching staff members about measures that reduce campers and workers risks of developing Giardia infections. The nurse should emphasize which of the following practices? A) Making sure not to drink water that has not been purified B) Avoiding the consumption of wild berries C) Removing ticks safely and promptly D) Using mosquito repellant consistently D Feedback: Transmission of the protozoan Giardia lamblia occurs when food or drink is contaminated with viable cysts of the organism. People often become infected while traveling to endemic areas or by drinking contaminated water from mountain streams within the United States. Berries, mosquitoes, and ticks are not sources of this microorganism. 38. A nurse is participating in a vaccination clinic at the local public health clinic. The nurse is describing the public health benefits of vaccinations to participants. Vaccine programs addressing which of the following diseases have been deemed successful? Select all that apply. A) Polio B) Diphtheria C) Hepatitis D) Tuberculosis E) Pertussis A, B, E Feedback: The most successful vaccine programs have been ones for the prevention of smallpox, measles, mumps, rubella, polio, diphtheria, pertussis, and tetanus. There is no vaccine for tuberculosis. Hepatitis is not counted as one of the most successful vaccination programs, because vaccination rates for hepatitis leave room for improvement. 39. A public health nurse promoting the annual influenza vaccination is focusing health promotion efforts on the populations most vulnerable to death from influenza. The nurse should focus on which of the following groups? A) Preschool-aged children B) Adults with diabetes and/or renal failure C) Older adults with compromised health status D) Infants under the age of 12 months C Feedback: Influenza vaccination is particularly beneficial in preventing death among older adults, especially those with compromised health status or those who live in institutional settings. It is recommended for children and adults, but carries the greatest reduction in morbidity and mortality in older adults. 40. The nurse receives a phone call from a clinic patient who experienced fever and slight dyspnea several hours after receiving the pneumococcus vaccine. What is the nurses most appropriate action? A) Instruct the patient to call 911. B) Inform the patient that this is an expected response to vaccination. C) Encourage the patient to take NSAIDs until symptoms are relieved. D) Ensure that the adverse reaction is reported. D Feedback: Nurses should ask adult vaccine recipients to provide information about any problems encountered after vaccination. As mandated by law, a Vaccine Adverse Event Reporting System (VAERS) form must be completed with the following information: type of vaccine received, timing of vaccination, onset of the adverse event, current illnesses or medication, history of adverse events after vaccination, and demographic information about the recipient. NSAIDs are not necessarily required and no evidence of distress warrants a call to 911. This is not an expected response to vaccination. Chapter 72: Emergency Nursing 1. Which patient should the nurse prioritize as needing emergent treatment, assuming no other injuries are present except the ones outlined below? A) A patient with a blunt chest trauma with some difficulty breathing B) A patient with a sore neck who was immobilized in the field on a backboard with a cervical collar C) A patient with a possible fractured tibia with adequate pedal pulses D) A patient with an acute onset of confusion A Feedback: The patient with blunt chest trauma possibly has a compromised airway. Establishment and maintenance of a patent airway and adequate ventilation is prioritized over other health problems, including skeletal injuries and changes in cognition. 2. The nurse observes that the family members of a patient who was injured in an accident are blaming each other for the circumstances leading up to the accident. The nurse appropriately lets the family members express their feelings of responsibility, while explaining that there was probably little they could do to prevent the injury. In what stage of crisis is this family? A) Anxiety and denial B) Remorse and guilt C) Anger D) Grief B Feedback: Remorse and guilt are natural processes of the stages of a crisis and should be facilitated for the family members to process the crisis. The familys sense of blame and responsibility are more suggestive of guilt than anger, grief, or anxiety. 3. A patient is brought to the ED by ambulance with a gunshot wound to the abdomen. The nurse knows that the most common hollow organ injured in this type of injury is what? A) Liver B) Small bowel C) Stomach D) Large bowel B Feedback: Penetrating abdominal wounds have a high incidence of injury to hollow organs, especially the small bowel. The liver is also injured frequently, but it is a solid organ. 4. A patient has been brought to the ED with multiple trauma after a motor vehicle accident. After immediate threats to life have been addressed, the nurse and trauma team should take what action? A) Perform a rapid physical assessment. B) Initiate health education. C) Perform diagnostic imaging. D) Establish the circumstances of the accident. A Feedback: Once immediate threats to life have been corrected, a rapid physical examination is done to identify injuries and priorities of treatment. Health education is initiated later in the care process and diagnostic imaging would take place after a rapid physical assessment. It is not the care teams responsibility to determine the circumstances of the accident. 5. The nursing educator is reviewing the signs and symptoms of heat stroke with a group of nurses who provide care in a desert region. The educator should describe what sign or symptom? A) Hypertension with a wide pulse pressure B) Anhidrosis C) Copious diuresis D) Cheyne-Stokes respirations B Feedback: Heat stroke is manifested by anhidrosis confusion, bizarre behavior, coma, elevated body temperature, hot dry skin, tachypnea, hypotension, and tachycardia. This health problem is not associated with anhidrosis or Cheyne-Stokes respirations. 6. A patient is brought to the ED by ambulance after swallowing highly acidic toilet bowl cleaner 2 hours earlier. The patient is alert and oriented. What is the care teams most appropriate treatment? A) Administering syrup of ipecac B) Performing a gastric lavage C) Giving milk to drink D) Referring to psychiatry C Feedback: A patient who has swallowed an acidic substance, such as toilet bowl cleaner, may be given milk or water to drink for dilution. Gastric lavage must be performed within 1 hour of ingestion. A psychiatric consult may be considered once the patient is physically stable and it is deemed appropriate by the physician. Syrup of ipecac is no longer used in clinical settings. 7. A patient is admitted to the ED with suspected alcohol intoxication. The ED nurse is aware of the need to assess for conditions that can mimic acute alcohol intoxication. In light of this need, the nurse should perform what action? A) Check the patients blood glucose level. B) Assess for a documented history of major depression. C) Determine whether the patient has ingested a corrosive substance. D) Arrange for assessment of serum potassium levels. A Feedback: Hypoglycemia can mimic alcohol intoxication and should be assessed in a patient suspected of alcohol intoxication. Potassium imbalances, depression, and poison ingestion are not noted to mimic the characteristic signs and symptoms of alcohol intoxication. 8. The paramedics bring a patient who has suffered a sexual assault to the ED. What is important for the sexual assault nurse examiner to do when assessing a sexual assault victim? A) Respect the patients privacy during assessment. B) Shave all pubic hair for laboratory analysis. C) Place items for evidence in plastic bags. D) Bathe the patient before the examination. A Feedback: The patients privacy and sensitivity must be respected, because the patient will be experiencing a stress response to the assault. Pubic hair is combed or trimmed for sampling. Paper bags are used for evidence collection because plastic bags retain moisture, which promotes mold and mildew that can destroy evidence. Bathing the patient before the examination would destroy or remove key evidence. 9. A patient with a history of major depression is brought to the ED by her parents. Which of the following nursing actions is most appropriate? A) Noting that symptoms of physical illness are not relevant to the current diagnosis B) Asking the patient if she has ever thought about taking her own life C) Conducting interviews in a brief and direct manner D) Arranging for the patient to spend time alone to consider her feelings B Feedback: Establishing if the patient has suicidal thoughts or intents helps identify the level of depression and intervention. Physical symptoms are relevant and should be explored. Allow the patient to express feelings, and conduct the interview at a comfortable pace for the patient. Never leave the patient alone, because suicide is usually committed in solitude. 10. A triage nurse is talking to a patient when the patient begins choking on his lunch. The patient is coughing forcefully. What should the nurse do? A) Stand him up and perform the abdominal thrust maneuver from behind. B) Lay him down, straddle him, and perform the abdominal thrust maneuver. C) Leave him to get assistance. D) Stay with him and encourage him, but not intervene at this time. D Feedback: If the patient is coughing, he should be able to dislodge the object or cause a complete obstruction. If complete obstruction occurs, the nurse should perform the abdominal thrust maneuver with the patient standing. If the patient is unconscious, the nurse should lay the patient down. A nurse should never leave a choking patient alone. 11. You are a floor nurse caring for a patient with alcohol withdrawal syndrome. What would be an appropriate nursing action to minimize the potential for hallucinations? A) Engage the patient in a process of health education. B) Administer opioid analgesics as ordered. C) Place the patient in a private, well-lit room. D) Provide television or a radio as therapeutic distraction C Feedback: The patient should be placed in a quiet single room with lights on and in a calm nonstressful environment. TV and radio stimulation should be avoided. Analgesics are not normally necessary, and would potentially contribute to hallucinations. Health education would be inappropriate while the patient is experiencing acute withdrawal. 12. An obtunded patient is admitted to the ED after ingesting bleach. The nurse should prepare to assist with what intervention? A) Prompt administration of an antidote B) Gastric lavage C) Administration of activated charcoal D) Helping the patient drink large amounts of water D Feedback: The patient who has ingested a corrosive poison, such as bleach, is given water or milk to drink for dilution. Gastric lavage is not used to treat ingestion of corrosives and activated charcoal is ineffective. There is no antidote for a corrosive substance such as bleach. 13. A 6-year-old is admitted to the ED after being rescued from a pond after falling through the ice while ice skating. What action should the nurse perform while rewarming the patient? A) Assessing the patients oral temperature frequently B) Ensuring continuous ECG monitoring C) Massaging the patients skin surfaces to promote circulation D) Administering bronchodilators by nebulizer B Feedback: A hypothermic patient requires continuous ECG monitoring and assessment of core temperatures with an esophageal probe, bladder, or rectal thermometer. Massage is not performed and bronchodilators would normally be insufficient to meet the patients respiratory needs. 14. A male patient with multiple injuries is brought to the ED by ambulance. He has had his airway stabilized and is breathing on his own. The ED nurse does not see any active bleeding, but should suspect internal hemorrhage based on what finding? A) Absence of bruising at contusion sites B) Rapid pulse and decreased capillary refill C) Increased BP with narrowed pulse pressure D) Sudden diaphoresis B Feedback: The nurse would anticipate that the pulse would increase and BP would decrease. Urine output would also decrease. An absence of bruising and the presence of diaphoresis would not suggest internal hemorrhage. 15. A 13-year-old is being admitted to the ED after falling from a roof and sustaining blunt abdominal injuries. To assess for internal injury in the patients peritoneum, the nurse should anticipate what diagnostic test? A) Radiograph B) Computed tomography (CT) scan C) Complete blood count (CBC) D) Barium swallow B Feedback: CT scan of the abdomen, diagnostic peritoneal lavage, and abdominal ultrasound are appropriate diagnostic tools to assess intra-abdominal injuries. X-rays do not yield sufficient data and a CBC would not reveal the presence of intraperitoneal injury. 16. A patient is brought to the ER in an unconscious state. The physician notes that the patient is in need of emergency surgery. No family members are present, and the patient does not have identification. What action by the nurse is most important regarding consent for treatment? A) Ask the social worker to come and sign the consent. B) Contact the police to obtain the patients identity. C) Obtain a court order to treat the patient. D) Clearly document LOC and health status on the patients chart. D Feedback: When patients are unconscious and in critical condition, the condition and situation should be documented to administer treatment quickly and timely when no consent can be obtained by usual routes. A social worker is not asked to sign the consent. Finding the patients identity is not a priority. Obtaining a court order would take too long. 17. A patient is experiencing respiratory insufficiency and cannot maintain spontaneous respirations. The nurse suspects that the physician will perform which of the following actions? A) Insert an oropharyngeal airway. B) Perform the jaw thrust maneuver. C) Perform endotracheal intubation. D) Perform a cricothyroidotomy. C Feedback: Endotracheal tubes are used in cases when the patient cannot be ventilated with an oropharyngeal airway, which is used in patients who are breathing spontaneously. The jaw thrust maneuver does not establish an airway and cricothyroidotomy would be performed as a last resort. 18. A patient is brought by friends to the ED after being involved in a motor vehicle accident. The patient sustained blunt trauma to the abdomen. What nursing action would be most appropriate for this patient? A) Ambulate the patient to expel flatus. B) Place the patient in a high Fowlers position. C) Immobilize the patient on a backboard. D) Place the patient in a left lateral position. C Feedback: When admitted for blunt trauma, patients must be immobilized until spinal injury is ruled out. Ambulation, side-lying, and upright positioning would be contraindicated until spinal injury is ruled out. 19. A backcountry skier has been airlifted to the ED after becoming lost and developing hypothermia and frostbite. How should the nurse best manage the patients frostbite? A) Immerse affected extremities in water slightly above normal body temperature. B) Immerse the patients frostbitten extremities in the warmest water the patient can tolerate. C) Gently massage the patients frozen extremities in between water baths. D) Perform passive range-of-motion exercises of the affected extremities to promote circulation. A Feedback: Frozen extremities are usually placed in a 37C to 40C (98.6F to 104F) circulating bath for 30- to 40- minute spans. To avoid further mechanical injury, the body part is not handled. Massage is contraindicated. 20. A patient with a fractured femur presenting to the ED exhibits cool, moist skin, increased heart rate, and falling BP. The care team should consider the possibility of what complication of the patients injuries? A) Myocardial infarction B) Hypoglycemia C) Hemorrhage D) Peritonitis C Feedback: The signs and symptoms the patient is experiencing suggest a volume deficit from an internal bleed. That the symptoms follow an acute injury suggests hemorrhage rather than myocardial infarction or hypoglycemia. Peritonitis would be an unlikely result of a femoral fracture. 21. A patient who has been diagnosed with cholecystitis is being discharged home from the ED to be scheduled for surgery later. The patient received morphine during the present ED admission and is visibly drowsy. When providing health education to the patient, what would be the most appropriate nursing action? A) Give written instructions to patient. B) Give verbal instructions to one of the patients family members. C) Telephone the patient the next day with verbal instructions. D) Give verbal and written instructions to patient and a family member. D Feedback: Before discharge, verbal and written instructions for continuing care are given to the patient and the family or significant others. Discharge teaching is completed prior to the patient leaving the ED, so phoning the patient the next day in not acceptable. 22. A patient is admitted to the ED complaining of abdominal pain. Further assessment of the abdomen reveals signs of peritoneal irritation. What assessment findings would corroborate this diagnosis? Select all that apply. A) Ascites B) Rebound tenderness C) Changes in bowel sounds D) Muscular rigidity E) Copious diarrhea B, C, D Feedback: Signs of peritoneal irritation include abdominal distention, involuntary guarding, tenderness, pain, muscular rigidity, or rebound tenderness along with changes in bowel sounds. Diarrhea and ascites are not signs of peritoneal irritation. 23. A patient who attempted suicide being treated in the ED is accompanied by his mother, father, and brother. When planning the nursing care of this family, the nurse should perform which of the following action? A) Refer the family to psychiatry in order to provide them with support. B) Explore the causes of the patients suicide attempt with the family. C) Encourage the family to participate in the bedside care of the patient. D) Ensure that the family receives appropriate crisis intervention services. D Feedback: It is essential that family crisis intervention services are available for families of ED patients. It would be inappropriate and insensitive to explore causes of the patients suicide attempt with the family. Family participation in bedside care is often impractical in the ED setting. Psychiatry is not the normal source of psychosocial support and crisis intervention. 24. A patient is admitted to the ED after being involved in a motor vehicle accident. The patient has multiple injuries. After establishing an airway and adequate ventilation, the ED team should prioritize what aspect of care? A) Control the patients hemorrhage. B) Assess for cognitive effects of the injury. C) Splint the patients fractures. D) Assess the patients neurologic status. A Feedback: After establishing airway and ventilation, the team should evaluate and restore cardiac output by controlling hemorrhage. This must precede neurologic assessments and treatment of skeletal injuries. 25. A patient with multiple trauma is brought to the ED by ambulance after a fall while rock climbing. What is a responsibility of the ED nurse in this patients care? A) Intubating the patient B) Notifying family members C) Ensuring IV access D) Delivering specimens to the laboratory C Feedback: ED nursing responsibilities include ensuring airway and IV access. Nurses are not normally responsible for notifying family members. Nurses collect specimens, but are not responsible for their delivery. Physicians or other team members with specialized training intubate the patient. 26. A patient has been brought to the ED after suffering genitourinary trauma in an assault. Initial assessment reveals that the patients bladder is distended. What is the nurses most appropriate action? A) Withhold fluids from the patient. B) Perform intermittent urinary catheterization. C) Insert a narrow-gauge indwelling urinary catheter. D) Await orders following the urologists assessment. D Feedback: Urethral catheter insertion when a possible urethral injury is present is contraindicated; a urology consultation and further evaluation of the urethra are required. The nurse would withhold fluids, but urologic assessment is the priority. 27. The triage nurse is working in the ED. A homeless person is admitted during a blizzard with complaints of being unable to feel his feet and lower legs. Core temperature is noted at 33.2C (91.8F). The patient is intoxicated with alcohol at the time of admission and is visibly malnourished. What is the triage nurses priority in the care of this patient? A) Addressing the patients hypothermia B) Addressing the patients frostbite in his lower extremities C) Addressing the patients alcohol intoxication D) Addressing the patients malnutrition A Feedback: The patient may also have frostbite, but hypothermia takes precedence in treatment because it is systemic rather than localized. The alcohol abuse and the alteration in nutrition do not take precedence over the treatment of hypothermia because both problems are a less acute threat to the patients survival. 28. A patient is brought to the ED by friends. The friends tell the nurse that the patient was using cocaine at a party. On arrival to the ED the patient is in visible distress with an axillary temperature of 40.1C (104.2F). What would be the priority nursing action for this patient? A) Monitor cardiovascular effects. B) Administer antipyretics. C) Ensure airway and ventilation. D) Prevent seizure activity. C Feedback: Although all of the listed actions may be necessary for this patients care, the priority is to establish a patent airway and adequate ventilation. 29. A patient admitted to the ED with severe diarrhea and vomiting is subsequently diagnosed with food poisoning. The nurse caring for this patient assesses for signs and symptoms of fluid and electrolyte imbalances. For what signs and symptoms would this nurse assess? Select all that apply. A) Dysrhythmias B) Hypothermia C) Hypotension D) Hyperglycemia E) Delirium A, C, E Feedback: The patient is assessed for signs and symptoms of fluid and electrolyte imbalances, including lethargy, rapid pulse rate, fever, oliguria, anuria, hypotension, and delirium. Hyperglycemia and hypothermia are not typically associated with fluid and electrolyte imbalances. 30. The nurse is caring for a patient admitted with a drug overdose. What is the nurses priority responsibility in caring for this patient? A) Support the patients respiratory and cardiovascular function. B) Provide for the safety of the patient. C) Enhance clearance of the offending agent. D) Ensure the safety of the staff. A Feedback: Treatment goals for a patient with a drug overdose are to support the respiratory and cardiovascular functions, to enhance clearance of the agent, and to provide for safety of the patient and staff. Of these responsibilities, however, support of vital physiologic function is a priority. 31. A patient is admitted to the ED with an apparent overdose of IV heroin. After stabilizing the patients cardiopulmonary status, the nurse should prepare to perform what intervention? A) Administer a bolus of lactated Ringers. B) Administer naloxone hydrochloride (Narcan). C) Insert an indwelling urinary catheter. D) Perform a focused neurologic assessment. B Feedback: Narcan is an opioid antagonist that is administered for the treatment of narcotic overdoses. There is no definitive need for a urinary catheter or for a bolus of lactated Ringers. The patients basic neurologic status should be ascertained during the rapid assessment, but a detailed examination would be take precedence over administration of an antidote. 32. A patient is being treated for bites that she suffered during an assault. After the bites have been examined and documented by a forensic examiner, the nurse should perform what action? A) Apply a dressing saturated with chlorhexidine. B) Wash the bites with soap and water. C) Arrange for the patient to receive a hepatitis B vaccination. D) Assess the patients immunization history. B Feedback: After forensic evidence has been gathered, cleansing with soap and water is necessary, followed by the administration of antibiotics and tetanus toxoid as prescribed. The patients immunization history does not directly influence the course of treatment and hepatitis B vaccination is not indicated. Chlorhexidine bandages are not recommended. 33. A nurse is caring for a patient who has been the victim of sexual assault. The nurse documents that the patient appears to be in a state of shock, verbalizing fear, guilt, and humiliation. What phase of rape trauma syndrome is this patient most likely experiencing? A) Reorganization phase B) Denial phase C) Heightened anxiety phase D) Acute disorganization phase D Feedback: The acute disorganization phase may manifest as an expressed state in which shock, disbelief, fear, guilt, humiliation, anger, and other such emotions are encountered. These varied responses to the assault are not associated with a denial, heightened anxiety, or reorganization phase. 34. The ED nurse is planning the care of a patient who has been admitted following a sexual assault. The nurse knows that all of the nursing interventions are aimed at what goal? A) Encouraging the patient to gain a sense of control over his or her life B) Collecting sufficient evidence to secure a criminal conviction C) Helping the patient understand that this will not happen again D) Encouraging the patient to verbalize what happened during the assault A Feedback: The goals of management are to provide support, to reduce the patients emotional trauma, and to gather available evidence for possible legal proceedings. All of the interventions are aimed at encouraging the patient to gain a sense of control over his or her life. The patients well-being should be considered a priority over criminal proceedings. No health professional can guarantee the patients future safety and having the patient verbalize the event is not a priority. 35. The ED nurse admitting a patient with a history of depression is screening the patient for suicide risk. What assessment question should the nurse ask when screening the patient? A) How would you describe your mood over the past few days? B) Have you ever thought about taking your own life? C) How do you think that your life is most likely to end? D) How would you rate the severity of your depression right now on a 10-point scale? B Feedback: The nurse should address the patients possible plans for suicide in a direct yet empathic manner. The nurse should avoid oblique or indirect references to suicide and should not limit questions to the patients depression. 36. A patient is brought to the ED by family members who tell the nurse that the patient has been exhibiting paranoid, agitated behavior. What should the nurse do when interacting with this patient? A) Keep the patient in a confined space. B) Use therapeutic touch appropriately. C) Give the patient honest answers about likely treatment. D) Attempt to convince the patient that his or her fears are unfounded. C Feedback: The nurse should offer appropriate and honest explanations in order to foster rapport and trust. Confinement is likely to cause escalation, as is touching the patient. The nurse should not normally engage in trying to convince the patient that his or her fears are unjustified, as this can also cause escalation. 37. A patient is brought to the ED by two police officers. The patient was found unconscious on the sidewalk, with his face and hands covered in blood. At present, the patient is verbally abusive and is fighting the staff in the ED, but appears medically stable. The decision is made to place the patient in restraints. What action should the nurse perform when the patient is restrained? A) Frequently assess the patients skin integrity. B) Inform the patient that he is likely to be charged with assault. C) Avoid interacting with the patient until the restraints are removed. D) Take the opportunity to perform a full physical assessment. A Feedback: It is important to assess skin integrity when physical restraints are used. Criminal charges are not the responsibility of the nurse and the nurse should still interact with the patient. A full physical assessment, however, would likely be delayed until the patient is not combative. 38. An 83-year-old patient is brought in by ambulance from a long-term care facility. The patients symptoms are weakness, lethargy, incontinence, and a change in mental status. The nurse knows that emergencies in older adults may be more difficult to manage. Why would this be true? A) Older adults may have an altered response to treatment. B) Older adults are often reluctant to adhere to prescribed treatment. C) Older adults have difficulty giving a health history. D) Older adults often stigmatize their peers who use the ED. A Feedback: Emergencies in this age group may be more difficult to manage because elderly patients may have an atypical presentation, an altered response to treatment, a greater risk of developing complications, or a combination of these factors. The elderly patient may perceive the emergency as a crisis signaling the end of an independent lifestyle or even resulting in death. Stigmatization and nonadherence to treatment are not commonly noted. Older adults do not necessarily have difficulty giving a health history. 39. An ED nurse is triaging patients according to the Emergency Severity Index (ESI). When assigning patients to a triage level, the nurse will consider the patients acuity as well as what other variable? A) The likelihood of a repeat visit to the ED in the next 7 days B) The resources that the patient is likely to require C) The patients or insurers ability to pay for care D) Whether the patient is known to ED staff from previous visits B Feedback: With the ESI, patients are assigned to triage levels based on both their acuity and their anticipated resource needs. Ability to pay, the likelihood of repeat visits, and the history of prior visits are not explicitly considered. 40. A 23-year-old woman is brought to the ED complaining of stomach cramps, nausea, vomiting, and diarrhea. The care team suspects food poisoning. What is the key to treatment in food poisoning? A) Administering IV antibiotics B) Assessing immunization status C) Determining the source and type of food poisoning D) Determining if anyone else in the family is ill C Feedback: Determining the source and type of food poisoning is essential to treatment, and is more important than determining other sick family members. Antibiotics are not normally indicated and immunizations are not relevant to diagnosis or treatment of food poisoning. Chapter 73: Terrorism, Mass Casualty, and Disaster Nursing 1. The nurse manager in the ED receives information that a local chemical plant has had a chemical leak. This disaster is assigned a status of level II. What does this classification indicate? A) First responders can manage the situation. B) Regional efforts and aid from surrounding communities can manage the situation. C) Statewide or federal assistance is required. D) The area must be evacuated immediately. B Feedback: Level II disasters indicate that regional efforts and aid from the surrounding communities will be able to manage the situation. Local efforts are likely to be overwhelmed, while state and federal assistance are not likely necessary. The disaster level does not indicate the necessity of evacuation. 2. A workplace explosion has left a 40-year-old man burned over 65% of his body. His burns are second- and third-degree burns, but he is conscious. How would this person be triaged? A) Green B) Yellow C) Red D) Black D Feedback: The purpose of triaging in a disaster is to do the greatest good for the greatest number of people. The patient would be triaged as black due to the unlikelihood of survival. Persons triaged as green, yellow, or red have a higher chance of recovery. 3. A patient has been witness to a disaster involving a large number of injuries. The patient appears upset, but states that he feels capable of dealing with his emotions. What is the nurses most appropriate intervention? A) Educate the patient about the potential harm in denying his emotions. B) Refer the patient to social work or spiritual care. C) Encourage the patient to take a leave of absence from his job to facilitate emotional healing. D) Encourage the patient to return to normal social roles when appropriate. D Feedback: The patient should be encouraged to return to normal social roles when appropriate if he is confident and genuine about his ability to cope. The nurse should use active listening to the patients concerns and emotions to enable the patient to process the situation. The patient is not necessarily being unrealistic or dishonest. As a result, social work or spiritual care may not be needed. Time away from work may not be required. 4. A nurse is caring for patients exposed to a terrorist attack involving chemicals. The nurse has been advised that personal protective equipment must be worn in order to give the highest level of respiratory protection with a lesser level of skin and eye protection. What level protection is this considered? A) Level A B) Level B C) Level C D) Level D B Feedback: Level B personal protective equipment provides the highest level of respiratory protection, with a lesser level of skin and eye protection. Level A provides the highest level of respiratory, mucous membrane, skin, and eye protection. Level C incorporates the use of an air-purified respirator, a chemical resistant coverall with splash hood, chemical resistant gloves, and boots. Level D is the same as a work uniform. 5. A patient who has been exposed to anthrax is being treated in the local hospital. The nurse should prioritize what health assessments? A) Integumentary assessment B) Assessment for signs of hemorrhage C) Neurologic assessment D) Assessment of respiratory status D Feedback: The second stage of anthrax infection by inhalation includes severe respiratory distress, including stridor, cyanosis, hypoxia, diaphoresis, hypotension, and shock. The first stage includes flu-like symptoms. The second stage of infection by inhalation does not include headache, vomiting, or syncope. 6. When assessing patients who are victims of a chemical agent attack, the nurse is aware that assessment findings vary based on the type of chemical agent. The chemical sulfur mustard is an example of what type of chemical warfare agent? A) Nerve agent B) Blood agent C) Pulmonary agent D) Vesicant D Feedback: Sulfur mustard is a vesicant chemical that causes blistering and results in burning, conjunctivitis, bronchitis, pneumonia, hematopoietic suppression, and death. Nerve agents include sarin, soman, tabun, VX, and organophosphates (pesticides). Hydrogen cyanide is a blood agent that has a direct effect on cellular metabolism, resulting in asphyxiation through alterations in hemoglobin. Chlorine is a pulmonary agent, which destroys the pulmonary membrane that separates the alveolus from the capillary bed. 7. A major earthquake has occurred within the vicinity of the local hospital. The nursing supervisor working the night shift at the hospital receives information that the hospital disaster plan will be activated. The supervisor will need to work with what organization responsible for coordinating interagency relief assistance? A) Office of Emergency Management B) Incident Command System C) Centers for Disease Control and Prevention (CDC) D) American Red Cross A Feedback: The Office of Emergency Management coordinates the disaster relief efforts at state and local levels. The Incident Command System is a management tool to organize personnel, facilities, equipment, and communication in an emergency situation. The CDC is the agency for disease prevention and control and it supports state and local health departments. The American Red Cross provides additional support. 8. While developing an emergency operations plan (EOP), the committee is discussing the components of the EOP. During the post-incident response of an emergency operations plan, what activity will take place? A) Deciding when the facility will go from disaster response to daily activities B) Conducting practice drills for the community and facility C) Conducting a critique and debriefing for all involved in the incident D) Replacing the resources in the facility C Feedback: A post-incident response includes critiquing and debriefing all parties involved immediately and at later dates. It does not include the decision to go from disaster response to daily activities; it does not include practice drills; and it does not include replacement of resources in the facility. 9. The announcement is made that the facility may return to normal functioning after a local disaster. In the emergency operations plan, what is this referred to as? A) Demobilization response B) Post-incident response C) Crisis diffusion D) Reversion A Feedback: The demobilization response occurs when it is deemed that the facility may return to normal daily functioning. This is not known as the post-incident response, crisis diffusion or reversion. 10. A group of disaster survivors is working with the critical incident stress management (CISM) team. Members of this team should be guided by what goal? A) Determining whether the incident was managed effectively B) Educating survivors on potential coping strategies for future disasters C) Providing individuals with education about recognizing stress reactions D) Determining if individuals responded appropriately during the incident C Feedback: In defusing, patients are given information about recognizing stress reactions and how to deal with handling the stress they may experience. Debriefing involves asking patients about their current emotional coping and symptoms, following up, and identifying patients who require further assessment and assistance in dealing with the stress experienced. The CISM team does not focus primarily on the management of the incident or on providing skills for future incidents. 11. Level C personal protective equipment has been deemed necessary in the response to an unknown substance. The nurse is aware that the equipment will include what? A) A self-contained breathing apparatus B) A vapor-tight, chemical-resistant suit C) A uniform only D) An air-purified respirator D Feedback: Level C incorporates the use of an air-purified respirator, a chemical resistant coverall with splash hood, chemical-resistant gloves, and boots. Level A provides the highest level of respiratory, mucous membrane, skin, and eye protection, incorporating a vapor-tight, chemical-resistant suit and self- contained breathing apparatus (SCBA). Level B personal protective equipment provides the highest level of respiratory protection, with a lesser level of skin and eye protection, incorporating a chemical- resistant suit and SCBA. Level D is the same as a work uniform. 12. Emergency department (ED) staff members have been trained to follow steps that will decrease the risk of secondary exposure to a chemical. When conducting decontamination, staff members should remove the patients clothing and then perform what action? A) Rinse the patient with water. B) Wash the patient with a dilute bleach solution. C) Wash the patient chlorhexidine. D) Rinse the patient with hydrogen peroxide. A Feedback: The first step in decontamination is removal of the patients clothing and jewelry and then rinsing the patient with water. This is usually followed by a wash with soap and water, not chlorhexidine, bleach, or hydrogen peroxide. 13. A nurse takes a shift report and finds he is caring for a patient who has been exposed to anthrax by inhalation. What precautions does the nurse know must be put in place when providing care for this patient? A) Standard precautions B) Airborne precautions C) Droplet precautions D) Contact precautions A Feedback: The patient is not contagious, and anthrax cannot be spread from person to person, so standard precautions are initiated. Airborne, contact, and droplet precautions are not necessary. 14. A group of medical nurses are being certified in their response to potential bioterrorism. The nurses learn that if a patient is exposed to the smallpox virus he or she becomes contagious at what time? A) 6 to 12 hours after exposure B) When pustules form C) After a rash appears D) When the patient becomes febrile C Feedback: A patient is contagious after a rash develops, which initially develops on the face, mouth, pharynx, and forearms. The patient exposed to the smallpox virus is not contagious immediately after exposure; only when pustules form, or with a body temperature of 38C. 15. A patient is being treated in the ED following a terrorist attack. The patient is experiencing visual disturbances, nausea, vomiting, and behavioral changes. The nurse suspects this patient has been exposed to what chemical agent? A) Nerve agent B) Pulmonary agent C) Vesicant D) Blood agent A Feedback: Nerve agent exposure results in visual disturbances, nausea and vomiting, forgetfulness, irritability, and impaired judgment. This presentation is not suggestive of vesicants, pulmonary agents, or blood agents. 16. A patient is admitted to the ED who has been exposed to a nerve agent. The nurse should anticipate the STAT administration of what drug? A) Amyl nitrate B) Dimercaprol C) Erythromycin D) Atropine D Feedback: Atropine is administered when a patient is exposed to a nerve agent. Exposure to blood agents, such as cyanide, requires treatment with amyl nitrate, sodium nitrite, and sodium thiosulfate. Dimercaprol is administered IV for systemic toxicity and topically for skin lesions when exposed to vesicants. Erythromycin is an antibiotic, which is ineffective against nerve agents. 17. A patient was exposed to a dose of more than 5,000 rads of radiation during a terrorist attack. The patients skin will eventually show what manifestation? A) Erythema B) Ecchymosis C) Desquamation D) Necrosis D Feedback: Necrosis of the skin will become evident within a few days to months at doses of more than 5,000 rads. With 600 to 1,000 rads, erythema will occur; it can disappear within hours and then reappear. At greater than 1,000 rads, desquamation (radiation dermatitis) of the skin will occur. Ecchymosis does not occur. 18. There has been a radiation-based terrorist attack and a patient is experiencing vomiting, diarrhea, and shock after the attack. How will the patients likelihood of survival be characterized? A) Probable B) Possible C) Improbable D) Extended C Feedback: Patients who experience vomiting, diarrhea, and shock after radiation exposure are categorized as improbable survival, because they are demonstrating symptoms of exposure levels of more than 800 rads of total body-penetrating irradiation. 19. A 44-year-old male patient has been exposed to severe amount of radiation after a leak in a reactor plant. When planning this patients care, the nurse should implement what action? A) The patient should be scrubbed with alcohol and iodine. B) The patient should be carefully protected from infection. C) The patients immunization status should be promptly assessed. D) The patients body hair should be removed to prevent secondary contamination. B Feedback: Damage to the hematopoietic system following radiation exposure creates a serious risk for infection. There is no need to remove the patients hair and the patients immunization status is not significant. Alcohol and iodine are ineffective against radiation. 20. The nurse is coordinating the care of victims who arrive at the ED after a radiation leak at a nearby nuclear plant. What would be the first intervention initiated when victims arrive at the hospital? A) Administer prophylactic antibiotics. B) Survey the victims using a radiation survey meter. C) Irrigate victims open wounds. D) Perform soap and water decontamination. B Feedback: Each patient arriving at the hospital should first be surveyed with the radiation survey meter for external contamination and then directed toward the decontamination area as needed. This survey should precede decontamination efforts or irrigation of wounds. Antibiotics are not indicated. 21. An industrial site has experienced a radiation leak and workers who have been potentially affected are en route to the hospital. To minimize the risks of contaminating the hospital, managers should perform what action? A) Place all potential victims on reverse isolation. B) Establish a triage outside the hospital. C) Have hospital staff put on personal protective equipment. D) Place hospital staff on abbreviated shifts of no more than 4 hours. B Feedback: Triage outside the hospital is the most effective means of preventing contamination of the facility itself. None of the other listed actions has the potential to prevent the contamination of the hospital itself. 22. After a radiation exposure, a patient has been assessed and determined to be a possible survivor. Following the resolution of the patients initial symptoms, the care team should anticipate what event? A) A return to full health B) Internal bleeding C) A latent phase D) Massive tissue necrosis C Feedback: A latent phase commonly follows the prodromal phase of radiation exposure. The patient is deemed a possible survivor, not a probable survivor, so an immediate return to health is unlikely. However, internal bleeding and massive tissue necrosis would not be expected in a patient categorized as a possible survivor. 23. A hospitals emergency operations plan has been enacted following an industrial accident. While one nurse performs the initial triage, what should other emergency medical services personnel do? A) Perform life-saving measures. B) Classify patients according to acuity. C) Provide health promotion education. D) Modify the emergency operations plan. A Feedback: In an emergency, patients are immediately tagged and transported or given life-saving interventions. One person performs the initial triage while other emergency medical services (EMS) personnel perform life- saving measures and transport patients. Health promotion is not a priority during the acute stage of the crisis. Classifying patients is the task of the triage nurse. EMS personnel prioritize life-saving measures; they do not modify the operations plan. 24. A nurse is triaging patients after a chemical leak at a nearby fertilizer factory. The guiding principle of this activity is what? A) Assigning a high priority to the most critical injuries B) Doing the greatest good for the greatest number of people C) Allocating resources to the youngest and most critical D) Allocating resources on a first come, first served basis B Feedback: In nondisaster situations, health care workers assign a high priority and allocate the most resources to those who are the most critically ill. However, in a disaster, when health care providers are faced with a large number of casualties, the fundamental principle guiding resource allocation is to do the greatest good for the greatest number of people. A first come, first served approach is unethical. 25. A nurse has been called for duty during a response to a natural disaster. In this context of care, the nurse should expect to do which of the following? A) Practice outside of her normal area of clinical expertise. B) Perform interventions that are not based on assessment data. C) Prioritize psychosocial needs over physiologic needs. D) Prioritize the interests of older adults over younger patients. A Feedback: During a disaster, nurses may be asked to perform duties outside their areas of expertise and may take on responsibilities normally held by physicians or advanced practice nurses. 26. A nurse is participating in the planning of a hospitals emergency operations plan. The nurse is aware of the potential for ethical dilemmas during a disaster or other emergency. Ethical dilemmas in these contexts are best addressed by which of the following actions? A) Having an ethical framework in place prior to an emergency B) Allowing staff to provide care anonymously during an emergency C) Assuring staff that they are not legally accountable for care provided during an emergency D) Teaching staff that principles of ethics do not apply in an emergency situation A Feedback: Nurses can plan for the ethical dilemmas they may face during disasters by establishing a framework for evaluating ethical questions before they arise and by identifying and exploring possible responses to difficult clinical situations. Ethical principles do not become wholly irrelevant in emergencies. Care cannot be given anonymously and accountability for practice always exists, even in an emergency. 27. A nurse is undergoing debriefing with the critical incident stress management (CISM) team after participating in the response to a disaster. During this process, the nurse will do which of the following? A) Evaluate the care that he or she provided during the disaster. B) Discuss own emotional responses to the disaster. C) Explore the ethics of the care provided during the disaster. D) Provide suggestions for improving the emergency operations plan. B Feedback: In debriefing, participants are asked about their emotional reactions to the incident, what symptoms they may be experiencing (e.g., flashbacks, difficulty sleeping, intrusive thoughts), and other psychological ramifications. The EOP and the care the nurse provided are not evaluated. 28. A man survived a workplace accident that claimed the lives of many of his colleagues several months ago. The man has recently sought care for the treatment of depression. How should the nurse best understand the mans current mental health problem? A) The man is experiencing a common response following a disaster. B) The man fails to appreciate the fact that he survived the disaster. C) The man most likely feels guilty about his actions during the disaster. D) The mans depression most likely predated the disaster. A Feedback: Depression is a common response to disaster. It does not suggest that the patient feels guilty about his actions or that he does not appreciate the fact that he survived. It is possible, but less likely, that the patient was depressed prior to the disaster. 29. The nurse has been notified that the ED is expecting terrorist attack victims and that level D personal protective equipment is appropriate. What does level D PPE include? A) A chemical-resistant coverall with splash hood, chemical-resistant gloves, and boots B) A self-contained breathing apparatus (SCBA) and a fully encapsulating, vapor-tight, chemical- resistant suit with chemical-resistant gloves and boots. C) The SCBA and a chemical-resistant suit, but the suit is not vapor tight D) The nurses typical work uniform D Feedback: The typical work uniform is appropriate for Level D protection 30. The nurse is preparing to admit patients who have been the victim of a blast injury. The nurse should expect to treat a large number of patients who have experienced what type of injury? A) Chemical burns B) Spinal cord injury C) Meningeal tears D) Tympanic membrane rupture D Feedback: Tympanic membrane (TM) rupture is the most frequent injury after subjection to a pressure wave resulting from a blast injury because the TM is the bodys most sensitive organ to pressure. In most cases, other injuries such as meningeal tears, spinal cord injury, and chemical injuries are likely to be less common. 31. A nurse who is a member of the local disaster response team is learning about blast injuries. The nurse should plan for what event that occurs in the tertiary phase of the blast injury? A) Victims pre-existing medical conditions are exacerbated. B) Victims are thrown by the pressure wave. C) Victims experience burns from the blast. D) Victims suffer injuries caused by debris or shrapnel from the blast. B Feedback: The tertiary phase of the blast injury results from the pressure wave that causes the victims to be thrown, resulting in traumatic injury. None of the other listed events occurs in this specific phase of a blast. 32. A patient suffering from blast lung has been admitted to the hospital and is exhibiting signs and symptoms of an air embolus. What is the nurses most appropriate action? A) Place the patient in the Trendelenberg position. B) Assess the patients airway and begin chest compressions. C) Position the patient in the prone, left lateral position. D) Encourage the patient to perform deep breathing and coughing exercises. C Feedback: In the event of an air embolus, the patient should be placed immediately in the prone left lateral position to prevent migration of the embolus and will require emergent treatment in a hyperbaric chamber. Chest compressions, deep breathing, and coughing would exacerbate the patients condition. Trendelenberg positioning is not recommended. 33. A patient has been admitted to the medical unit with signs and symptoms that are suggestive of anthrax infection. The nurse should anticipate what intervention? A) Administration of acyclovir B) Hematopoietic stem cell transplantation (HSCT) C) Administration of penicillin D) Hemodialysis C Feedback: Anthrax infection is treated with penicillin. Acyclovir is ineffective because anthrax is a bacterium. Dialysis and HSCT are not indicated. 34. The ED staff has been notified of the imminent arrival of a patient who has been exposed to chlorine. The nurse should anticipate the need to address what nursing diagnosis? A) Impaired gas exchange B) Decreased cardiac output C) Chronic pain D) Excess fluid volume A Feedback: Pulmonary agents, such as phosgene and chlorine, destroy the pulmonary membrane that separates the alveolus from the capillary bed, disrupting alveolarcapillary oxygen transport mechanisms. Capillary leakage results in fluid-filled alveoli and gas exchange ceases to occur. Pain is likely, but is acute rather than chronic. Fluid volume excess is unlikely to be a priority diagnosis and cardiac output will be secondarily affected by the pulmonary effects. 35. The nursing supervisor at the local hospital is advised that your hospital will be receiving multiple trauma victims from a blast that occurred at a local manufacturing plant. The paramedics call in a victim of the blast with injuries including a head injury and hemorrhage. What phase of blast injury should the nurse expect to treat in this patient? A) Primary phase B) Secondary phase C) Tertiary phase D) Quaternary phase A Feedback: Pulmonary barotraumas, including pulmonary contusions; head injuries, including concussion, other severe brain injuries; tympanic membrane rupture, middle ear injury; abdominal hollow organ perforation; and hemorrhage are all injuries that can occur in the primary phase of a blast. These particular injuries are not characteristic of the subsequent phases. 36. A nurse has had contact with a patient who developed smallpox and became febrile after a terrorist attack. This nurse will require what treatment? A) Watchful waiting B) Treatment with colony-stimulating factors (CSFs) C) Vaccination D) Treatment with ceftriaxone C Feedback: All people who have had household or face-to-face contact with a patient with small pox after the fever begins should be vaccinated within 4 days to prevent infection and death. Watchful waiting would be inappropriate and CSFs are not used for treatment. Vaccination, rather than antibiotics, is the treatment of choice. 37. The emergency response team is dealing with a radiation leak at the hospital. What action should be performed to prevent the spread of the contaminants? A) Floors must be scrubbed with undiluted bleach. B) Waste must be promptly incinerated. C) The ventilation system should be deactivated. D) Air ducts and vents should be sealed. D Feedback: All air ducts and vents must be sealed to prevent spread. Waste is controlled through double-bagging and the use of plastic-lined containers outside of the facility rather than incineration. Bleach would be ineffective against radiation and the ventilation system may or may not be deactivated. 38. A patient has been exposed to a nerve agent in a biochemical terrorist attack. This type of agent bonds with acetylcholinesterase, so that acetylcholine is not inactivated. What is the pathologic effect of this type of agent? A) Hyperstimulation of the nerve endings B) Temporary deactivation of the nerve endings C) Binding of the nerve endings D) Destruction of the nerve endings A Feedback: Nerve agents can be inhaled or absorbed percutaneously or subcutaneously. These agents bond with acetylcholinesterase, so that acetylcholine is not inactivated; the adverse result is continuous stimulation (hyperstimulation) of the nerve endings. Nerve endings are not deactivated, bound, or destroyed. 39. A group of military nurses are reviewing the care of victims of biochemical terrorist attacks. The nurses should identify what agents as having the shortest latency? A) Viral agents B) Nerve agents C) Pulmonary agents D) Blood agents B Feedback: Latency is the time from absorption to the appearance of signs and symptoms. Sulfur mustards and pulmonary agents have the longest latency, whereas vesicants, nerve agents, and cyanide produce signs and symptoms within seconds. 40. A nurse is giving an educational class to members of the local disaster team. What should the nurse instruct members of the disaster team to do in a chemical bioterrorist attack? A) Cover their eyes. B) Put on a personal protective equipment mask. C) Stand up. D) Crawl to an exit. C Feedback: Most chemicals are heavier than air, except for hydrogen cyanide. Therefore, in the presence of most chemicals, people should stand up to avoid heavy exposure because the chemical will sink toward the floor or ground. For this reason, covering their eyes, putting on a PPE mask, or crawling to an exit will not decrease exposure. [Show More]
Last updated: 1 year ago
Preview 1 out of 1386 pages
Instant download
Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Apr 22, 2020
Number of pages
1386
Written in
Additional information
This document has been written for:
Uploaded
Apr 22, 2020
Downloads
0
Views
243

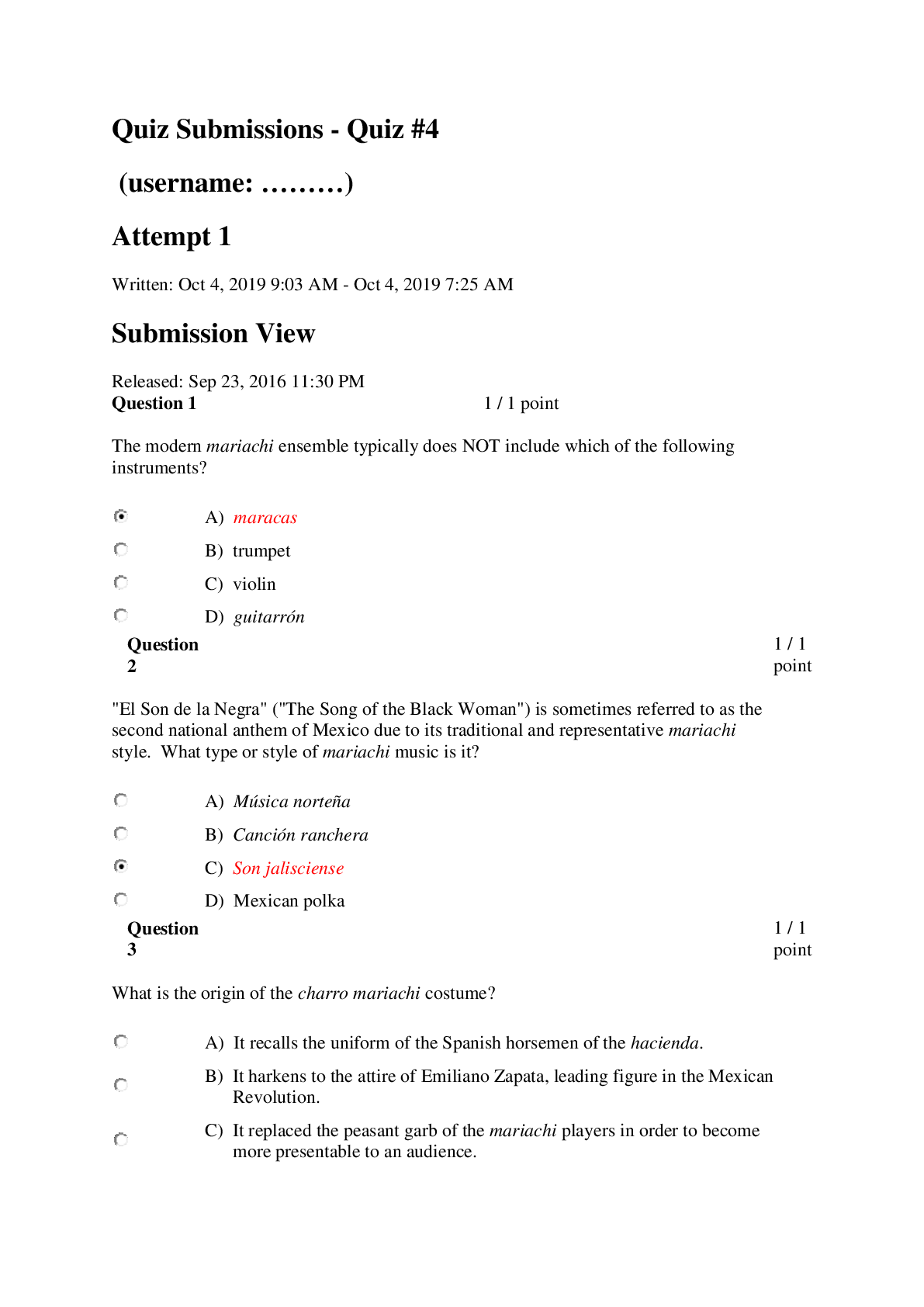
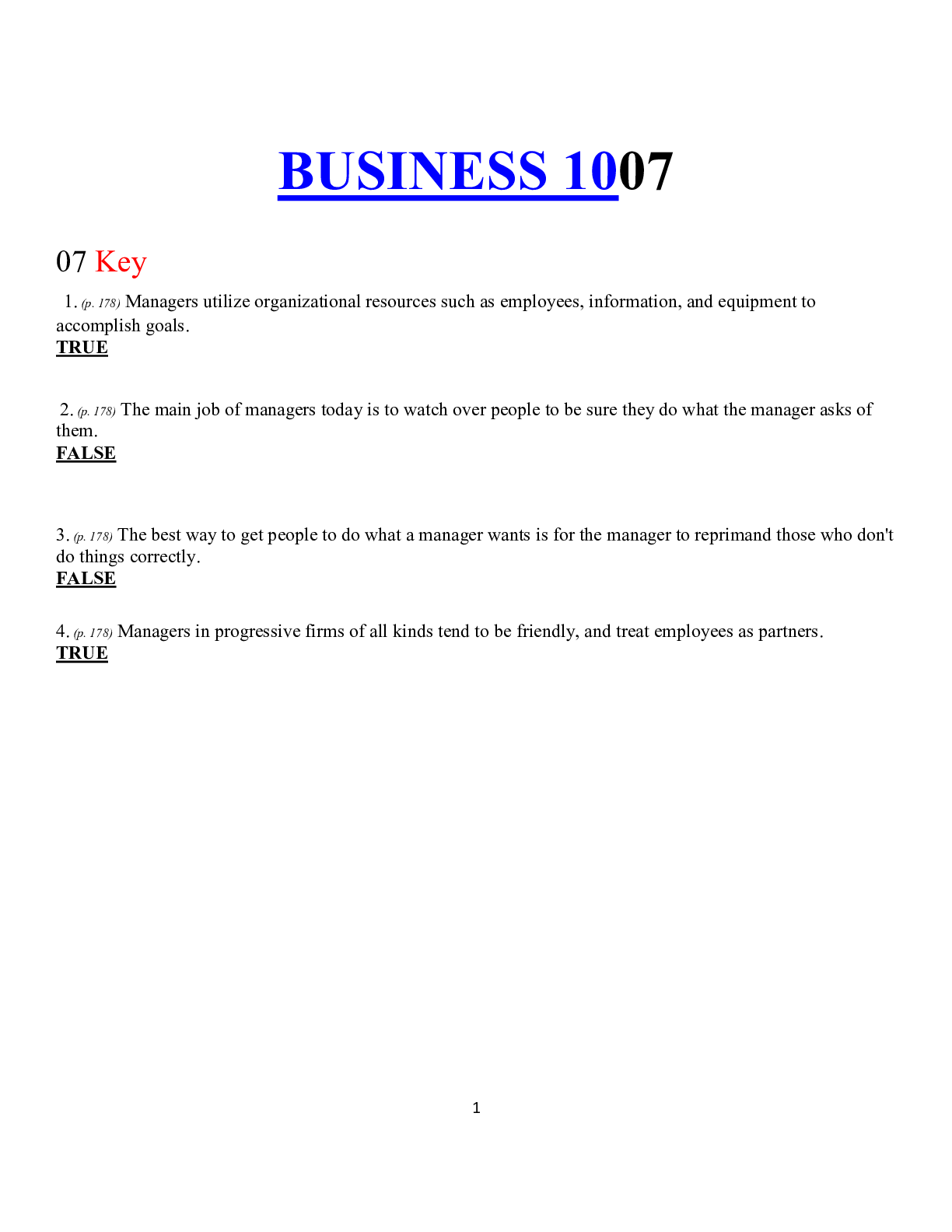
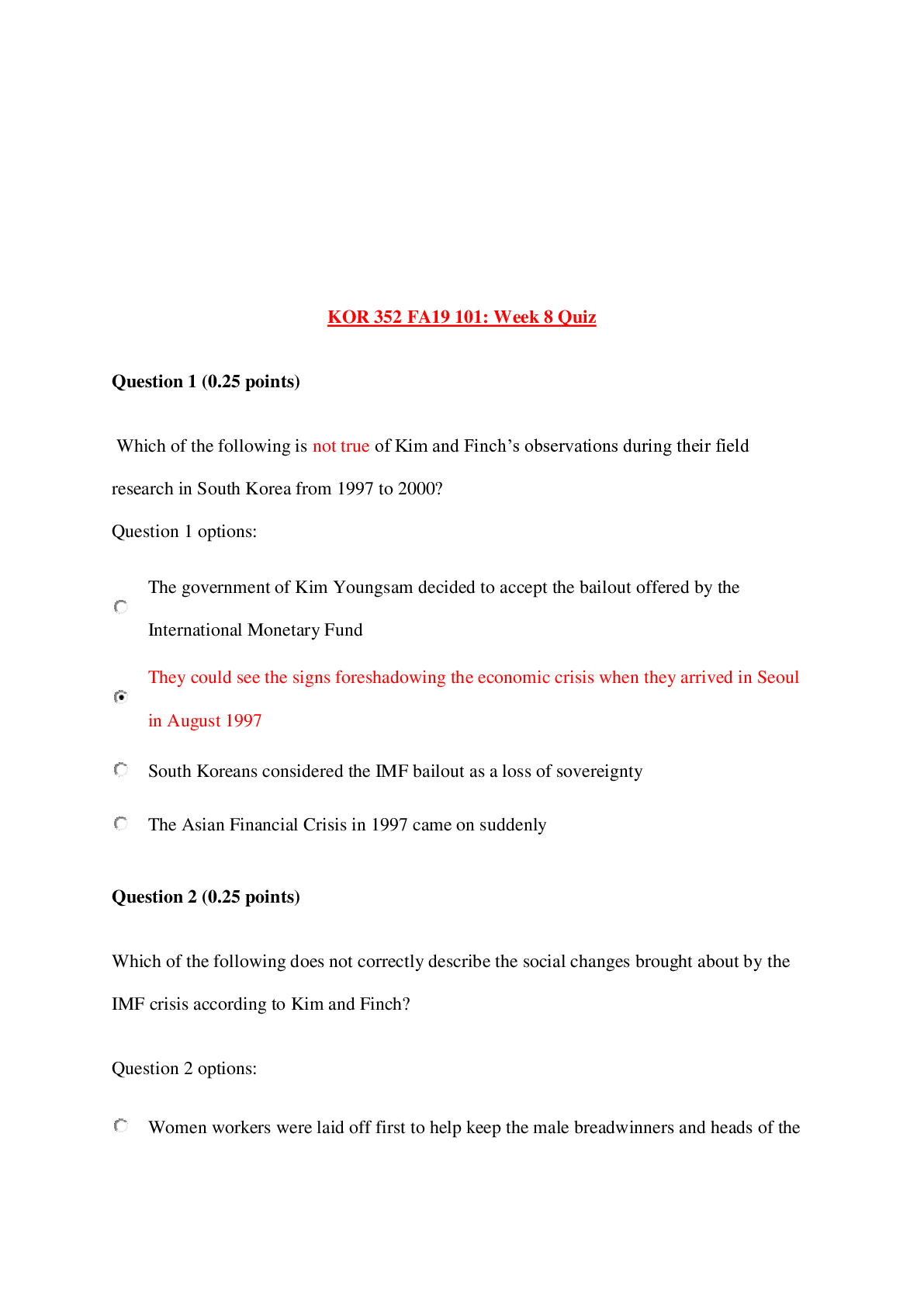
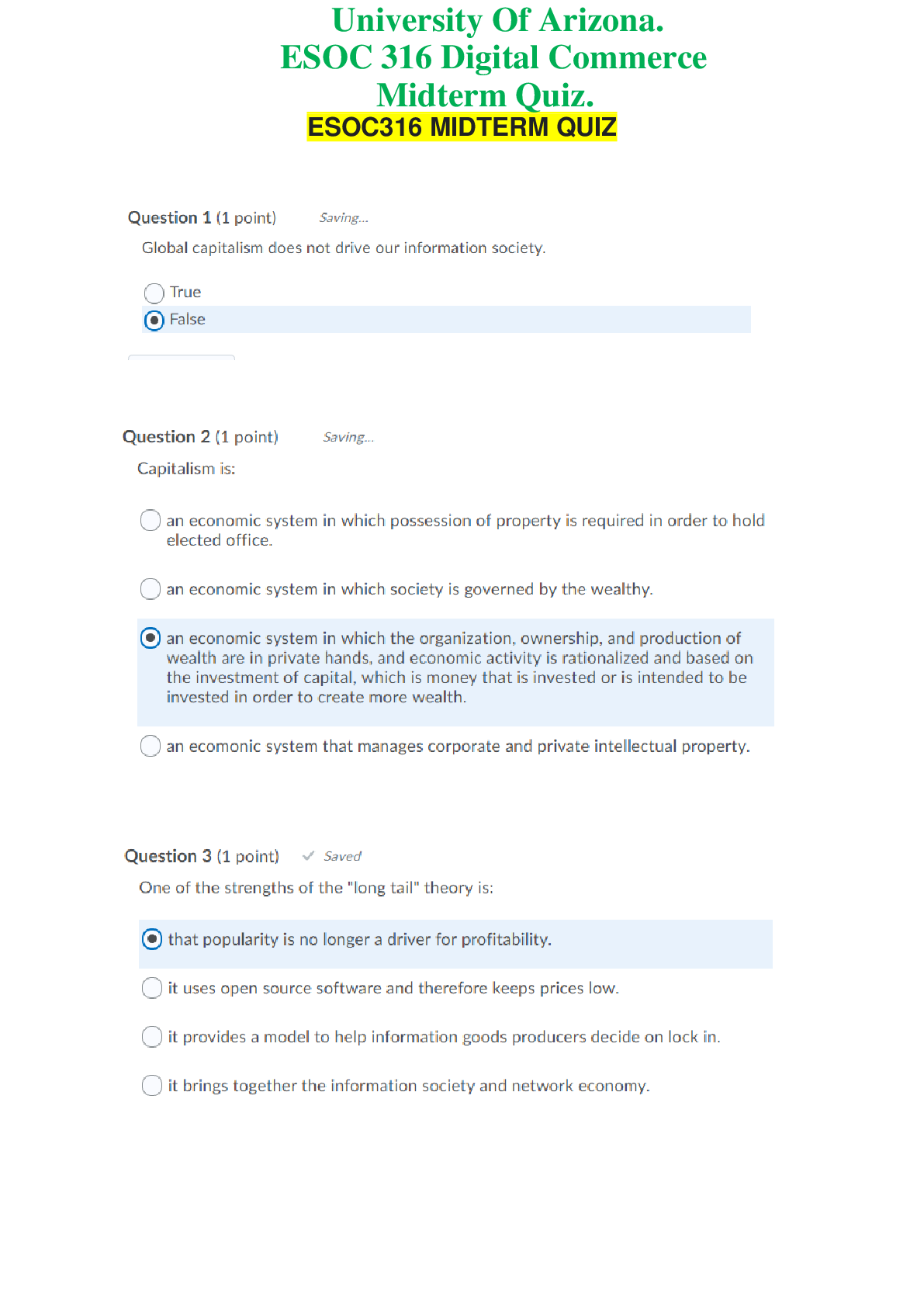
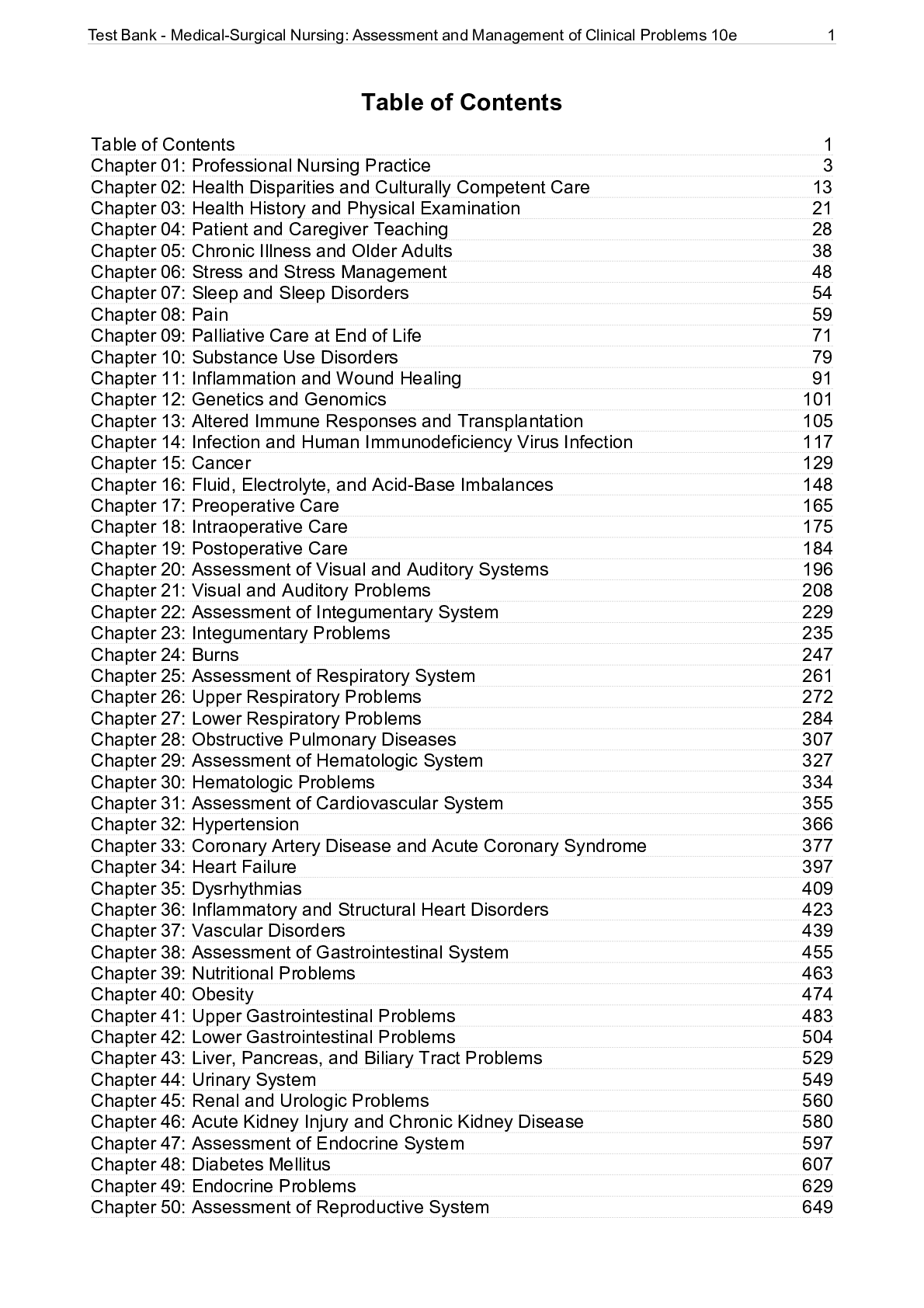
.png)

