Health Care > EXAM > COC 2020 Final Exam Study Questions - Set 7 (Complete Solutions, Answered) (All)
COC 2020 Final Exam Study Questions - Set 7 (Complete Solutions, Answered)
Document Content and Description Below
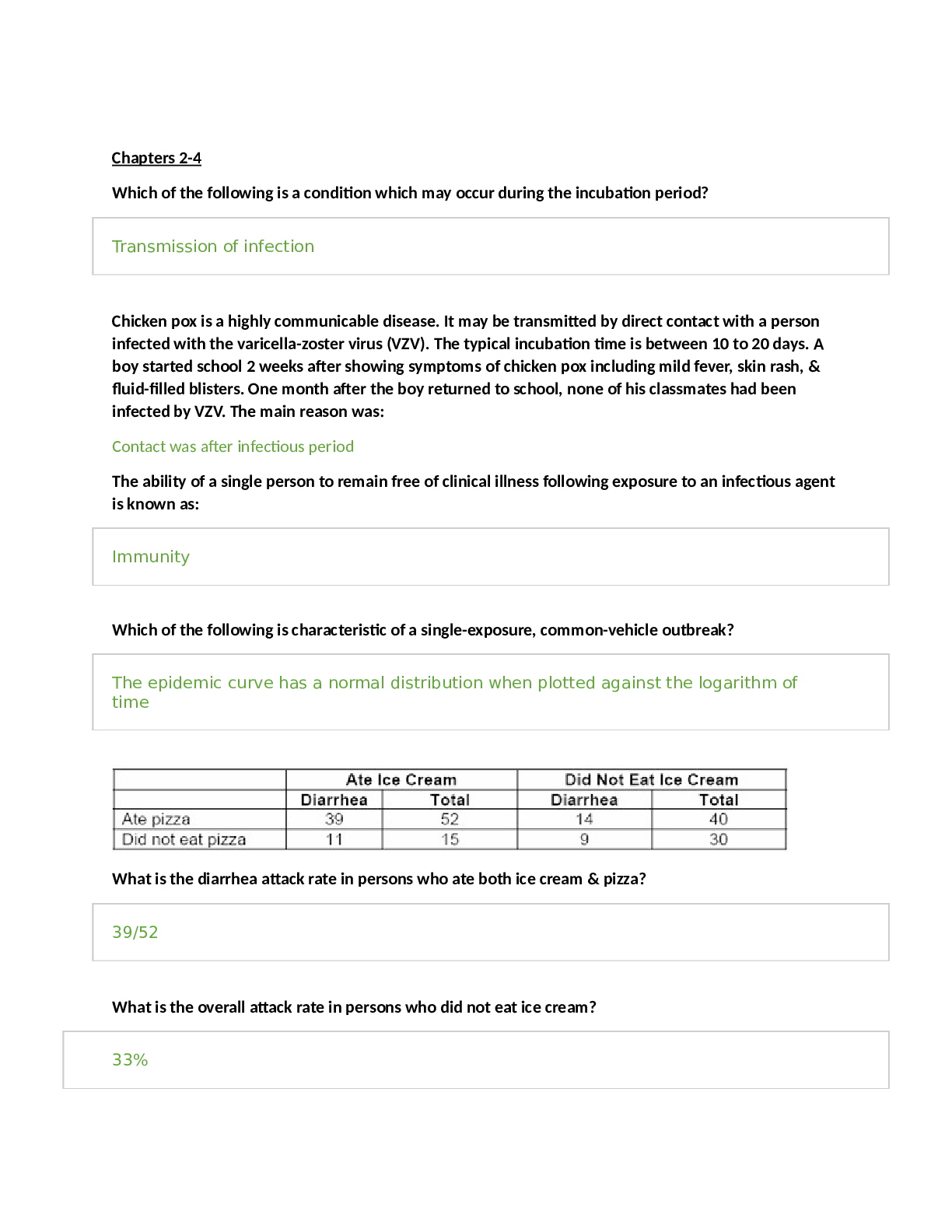
COC 2020 Final Exam Study Questions - Set 7 (Complete Solutions, Answered) Medicare payment for inPt eligible new tech is based on the cost to the hospital for the new tech. Medicare pays: 50% for t... he costs of the new tech in excess of the full MS-DRG payment Medicare reimbursable drugs are found in this code book. HCPCS Level II Rationale: Medicare reimbursable drugs are found in the HCPCS Level II code book. Medicare reimbursable drugs must be billed in the appropriate dosage amount defined by the long descriptor of their respective HCPCS Level II codes and adjusted for the units to reflect the amount of drug administered. MeV: Radiation dosage in million electron volts = maximum energy level of the X-ray beam Modifier TC is reported on the UB-04 claim form. True or False? Why? False. Modifier TC indicates the technical component. This is understood in the facility setting and is not reported on the UB-04. Mr. Elliot visits the surgeon for evaluation for a wedge resection ofleft lung cancer. During the admission, the patient reports pain in the chest due to the malignancy. Applying the coding concept from ICD-10-CM guideline I.C.6.b.5, what ICD-10-CM code(s) should be reported? C34.92, G89.3 Mr. McFarland visits his oncologist for prostate cancer. He is reporting more fatigue than usual. Lab tests determine the patient has anemia due to the cancer. Applying the coding concept from ICD-10-CM guideline I.C.2.c.l, what ICD-10-CM codes should be reported for the visit? C61, D63.0 Mr. Smith is scheduled for a splenectomy for hypersplenism. Before his splenectomy, he is required to have clearance from his pulmonologist. The pulmonologist performs a pre-operative screening. Applying the coding concept from ICD-10-CM guideline IV.M, which ICD-10-CM codes would be reported for the pre-operative clearance? Z01.811, D73.1 Mr. Smith presents to the office for a screening test to detect sickle cell disorder. What ICD-10-CM code(s) is/are reported? Z13.0 Mr. Timmins fell off a roof and suffered a spinal injury. As a result of the injury, he has been suffering from chronic pain in his lower back for several years. Today, he presents for insertion of a neurostimulator for pain control. Applying the coding concept from ICD-10-CM guidelines I.C.6.b.l.a and I.C.6.b.l.b.ii, what ICD-10-CM codes should be reported for the pain? (Do not code the external cause.) G89.21, M54.5 Mrs. Bixby, 83, is being admitted for dehydration and anorexia. The probable cause is dementia. She was brought in by her daughter who is visiting from out of town. Her daughter will take her from our office to St. Mary's. The gerontology unit will evaluate her mental condition tomorrow after she is stabilized. How would you code the diagnoses? R63.0, E86.0 Mrs. Fryer visits her nephrologist for an erythropoietin (EPO) injection for her anemia. She has Stage 3 chronic kidney disease, which is the cause of the anemia. Applying the coding concept from ICD-10-CM guideline I.A.13, what ICD- 10-CM code(s) should be reported for the EPO injection? N18.3,D63.1 Mrs. Johnson is here today to receive an intercostal nerve block to mitigate the debilitating pain of her malignancy. Her cancer has metastasized to her bones in her thoracic spine Primary cancer is unknown. What ICD-10-CM codes are reported? G89.3, C79.51,C80.1 Mrs. Smith is visiting her mother and is 150 miles away from home. She is in the 26th week of pregnancy. In the late afternoon she suddenly feels a gush of fluid followed by strong uterine contractions. She is rushed to the hospital but the baby is born before they arrive. In the ED, she and the baby are examined, and the retained placenta is delivered. The baby is in the neonatal nursery doing okay. Mrs. Smith has a 2nd degree perineal laceration secondary to precipitous delivery, which was repaired by the ED physician. She will return home for her postpartum care. What codes does the facility ED report (CPT® and ICD-10-CM codes)? 59414, 59300, O73.0, O70.1, Z37.0, Z3A.26 Multifield: Use of three or more fields to deliver dosage Muscle is attached to bone by what method? Tendons, aponeurosis and directly to the bone Myocardial Perfusion Imaging Indications: Chest pain. Procedure: Resting tomographic myocardial perfusion images were obtained following injection of 10 mCi of intravenous Cardiolite (technetium tc 99 sestamibi for injection). At peak exercise, 30 mCi of intravenous Cardiolite was injected, and post-stress tomographic myocardial perfusion images were obtained. Post stress gated images of the left ventricle were also acquired. Myocardial perfusion images were compared in the standard fashion. Findings: This is a technically fair study. No stress induced electrocardiographic changes noted. There are no significant reversible or fixed perfusion defects noted. Gated images of the left ventricle reveal normal left ventricular volumes, normal left ventricular wall motion, and an estimated left ventricular ejection fraction of 50%.Impression: No evidence of myocardial ischemia or infarction. Normal left ventricular ejection fraction. What CPT ® and ICD-10-CM codes are reported by the facility? 78452, 93017, A9500, R07.9 Name an example of when a problem caused by diabetes is NOT sequenced after the code for diabetes. Refer to ICD- 10-CM guideline I.C.4.a.5.a. When a patient's insulin pump malfunctions Name four reasons why chronological documentation of patient care is important. 1. Enable the physician and other healthcare professionals to plan and evaluate the patient's immediate treatment, and to monitor his or her healthcare.; 2. Enhance communication and promote continuity of care among physicians and other healthcare professionals involved in the patient's care.; 3. Facilitate claims review and payments.; 4. Assist in utilization review and quality of care evaluations.; 5. Reduce complicated medical reviews.; 6. Provide clinical data for research and education.; 7. Serve as a legal document to verify the services (for example, in defense of an alleged professional liability claim). Name three benefits of an effective compliance plan. Faster, more accurate payment of claims, Fewer billing mistakes, Diminished chances of payer audit, Last chance of running afoul of self-referral and anti-kickback statutes Neuroendocrine glands Exerts chemical control over the human body by maintaining homeostasis NI is a: Payment indicator Oblique: Body part is rotated so it does not produce an AP/PA projection. The X-ray beam enters at an angle that is neither frontal (AP or PA) nor lateral. Observation services provided for more than 8 hours are considered packaged in which circumstance? When reported with a procedure assigned a status indicator T. OCE Edit 22-Invalid modifier is applied to a facility claim. The claim has modifier 63 appended to one of the procedure codes. Which appendix might help determine the reason for this edit? Appendix F OCE is an abbreviation for: Outpatient Code Editor Oculomotor Controls movement of four of the six muscles of the eyeball, the upper eyelid, and the muscles that constrict the pupils Olfactory Sense of smell On the UB-04 claim form: Sequence by revenue codes in ascending order OPER ATION: Left stapedotomy for conductive hearing loss. Operating microscope. SURGEON: ANESTHESIA: General. FINDINGS AT SURGERY: The patient had intact tympanic membrane. The incus and malleus were intact and mobile. The superstructure was absent, the footplate was not mobile. A 4.5 x 0.6 smart piston was used. DESCRIPTION OF OPERATION: After the establishment of general anesthesia and administration of appropriate IV antibiotics, the left ear was prepped and draped in the usual fashion, with a microscope and a canal knife, a tympanome-atal flap was incised and elevated. The middle ear was entered with a Rosen needle. The middle ear was explored with the previous mentioned findings. A measurement was taken, and then a fenestra was created in the footplate with a laser. A 4.5x 0.6 SMart stapes piston prosthesis was placed through the fenestra and crimped with a laser to the incus. It was mobile. The oval window was sealed with autologous venous blood. The eardrum was returned to the original position and packed with Gelfoam packing. A sterile dressing was placed upon the wound. What CPT® code and ICD-10-CM code is reported by the facility for the surgery? 69660-LT, H90.12 Operative Note Indications: This 67 year-old man with some compressive symptoms. A large left thyroid goiter was brought to surgery today for a left total thyroid lobectomy. He understood the risks of the procedure including nerve injury and bleeding and hypoparathyroidism. Procedure: After induction of anesthesia by the anesthesiologist, the neck was prepped and draped. A low collar incision was made and subplatysmal flaps were raised. The midline fascia was divided and retracted. The right lobe was essentially normal along with the isthmus; however, there was a huge fist-sized multiple colloid nodule goiter in the left thyroid lobe. This was mobilized. Care was taken to protect the recurrent nerve in the parathyroid. The superior pole was ligated between heavy silks along with the middle thyroid vein and inferior thyroid artery. A total left thyroid lobectomy was performed using hemostat and silk ligatures. This was confirmed as benign histologically. After checking for hemostasis, the neck was drained with a Jackson-Pratt and closed in layers with Vicryl and PDS. He tolerated this well and returned to the PACU in stable condition. Needle and sponge counts were correct. What CPT® code is reported? 60220-LT Operative Note Preoperative Diagnosis: Abdominal pain, thrombocytopenia, eosinophilia Postoperative Diagnosis: Acute gastritis, rule out eosinophilic gastritis Anesthesia: Demerol 100 mg, Versed 4 mg The patient's pulse, blood pressure, and pulse oximetry were monitored continuously and remained stable throughout the procedure and medication was administered by the anesthesia team. With the patient in the left lateral position, the endoscope was placed in the oropharynx. My visualization of larynx and laryngeal structures was good and these appeared normal. The esophagus was readily intubated and the proximal, mid, and distal esophageal mucosa appeared essentially unremarkable. There was perhaps some subtle felinization, but it was within normal limits. With the stomach, however, there were patches of erythema in the antrum and body and these were photographed and subsequently biopsied. In the more proximal body, there was subtle edema. This was photographed. Careful inspection of the stomach was made in forward and in retroflexed views, looking at cardia, fundus, annulus, body, antrum, and pylorus. The duodenal bulb and second portion of the duodenum appeared entirely normal. I await the biopsies with interest. The patient did have HIDA scan imaging and his gallbladder ejection fraction seems low at 31 percent, which in someone with biliary colic is highly suggestive of dysfunctional gallbladder. I will follow him into the GI hospital clinic. I am awaiting the results of the hematology assessment with interest, along with the biopsies and we will tie everything together when I see him again. What CPT® and ICD-10-CM codes are reported? 43239, K29.00 Operative Note Preoperative Diagnosis: History of anal ulcerations, hemorrhoids Postoperative Diagnosis: Hemorrhoids present posterior aspect, small and stable Procedure Performed: Anoscopy was performed. No ulcerations, no fissures, hemorrhoids present posterior aspect, small. Hemorrhoids are stable. Plan: 1- Continue avoiding foods and liquids as recommended in the first visit. 2- Stop Anusol suppositories.3-Can restart suspended food and liquids, one at a time, for ten days. If there is no recurrence, add a second food, and so forth. 4-Follow-up visit in two months. Select the correct ICD-10-CM and CPT® codes. 46600, K64.8, Z87.19 Operative Note Preoperative Diagnosis: Hypertrophic obstruction tonsils and adenoids. Postoperative Diagnosis: Same. The 27 year-old patient was intubated and the airway was secured. The adenoid region was palpated and the adenoid tissue was found to be obstructive and encroaching on the Eustachian tube orifices and the posterior choana. The palate was also palpated. The muscular sling was intact and the palate was felt to be of adequate length to result in good closure. The uvula was normal. The adenoids were gently removed with the curette. I did not disturb the Passavant's ridge. Only superior lymphoid tissue was removed. Hemostasis was achieved with a tonsillar pack. The tonsils were removed with blunt dissection, followed by selective electrocautery to prominent vessels in each fossa. Good hemostasis was achieved. Packing was removed at the end of the case at the time of extubation. The patient was in good cardiac and pulmonary condition without significant bleeding. What CPT® and ICD-10-CM codes are reported? 42821, J35.3 [Show More]
Last updated: 1 week ago
Preview 1 out of 17 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Apr 24, 2024
Number of pages
17
Written in
Additional information
This document has been written for:
Uploaded
Apr 24, 2024
Downloads
0
Views
2