*NURSING > STUDY GUIDE > NURSING 266 Med-Surg (Exam One) Study Guide Final | University of California, Los Angeles | DETAILED (All)
NURSING 266 Med-Surg (Exam One) Study Guide Final | University of California, Los Angeles | DETAILED SOLUTION
Document Content and Description Below
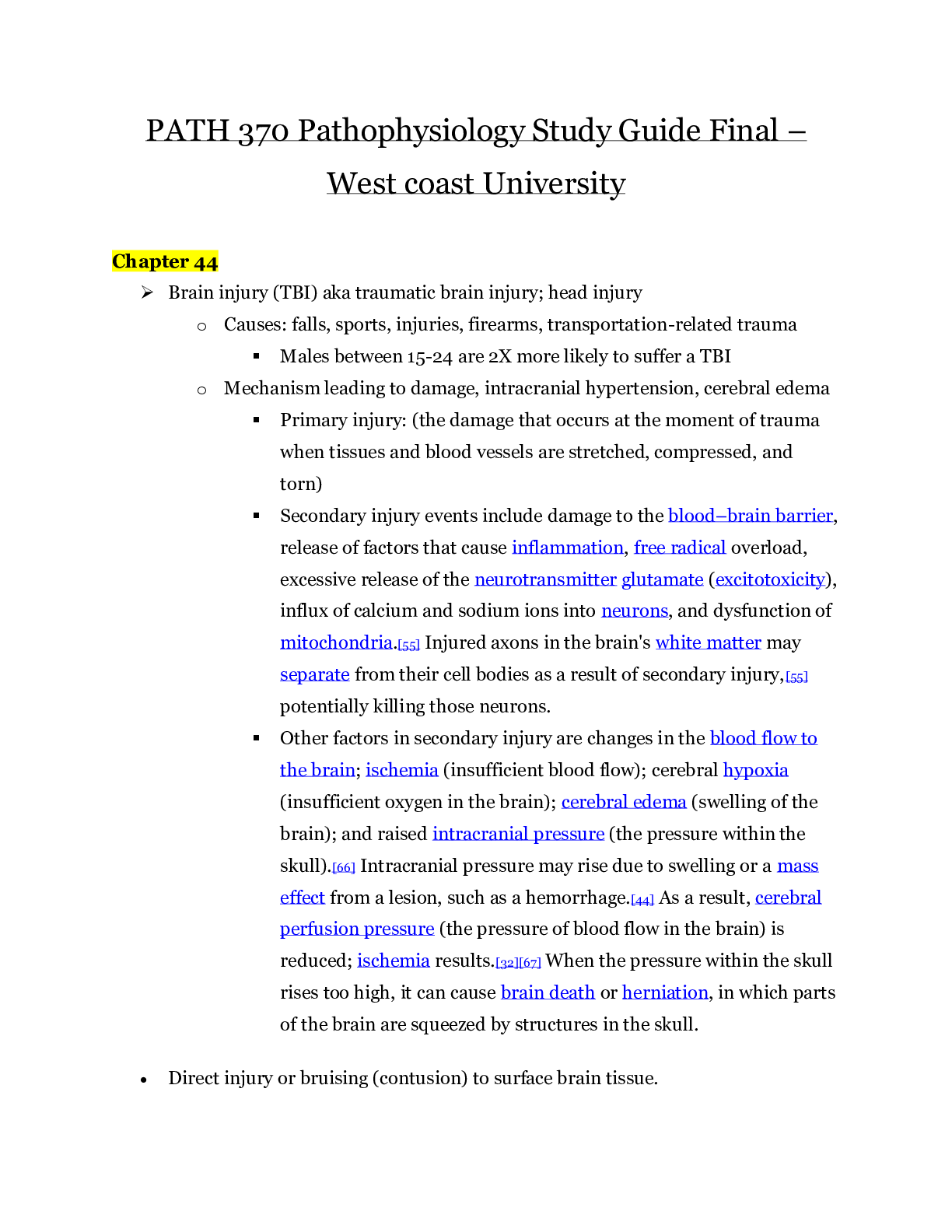
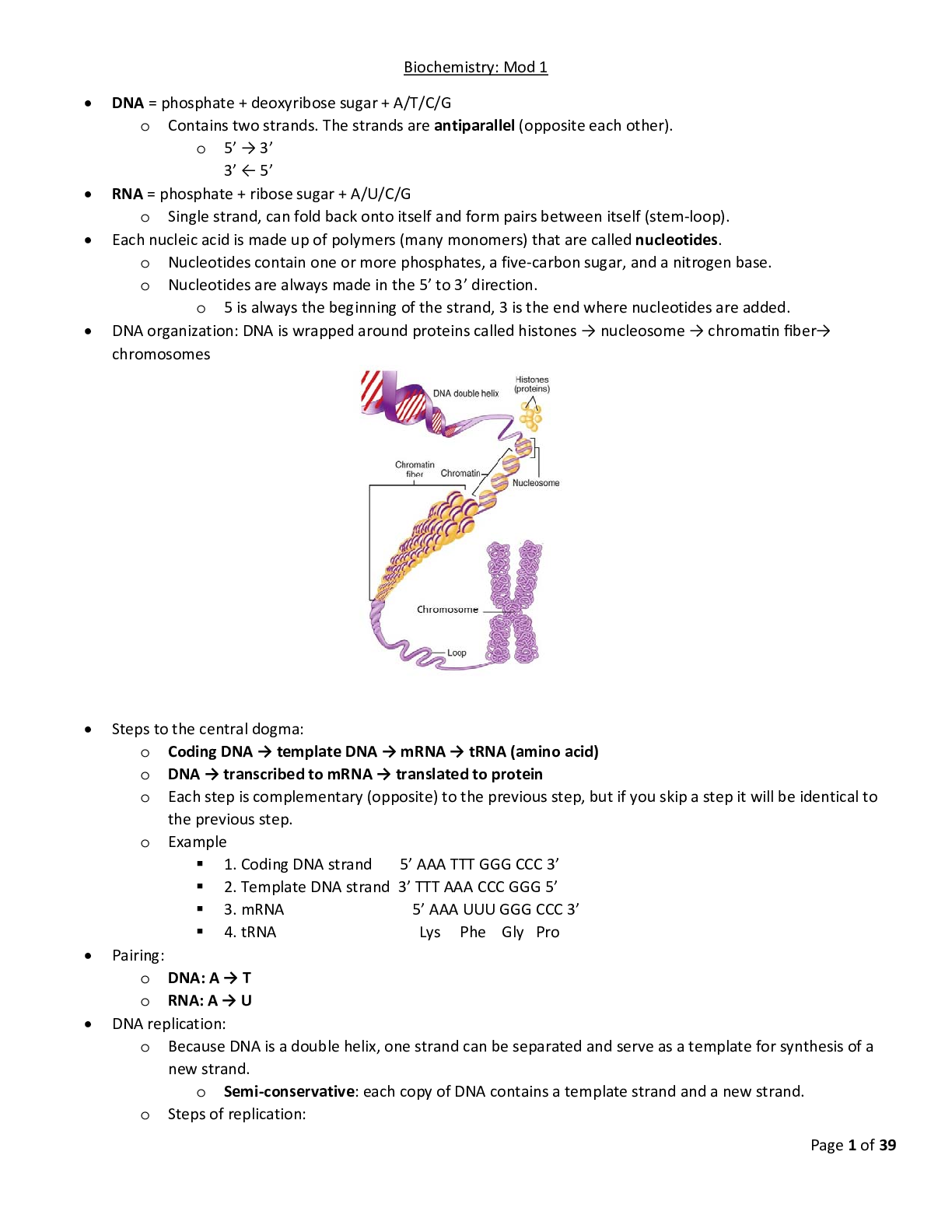
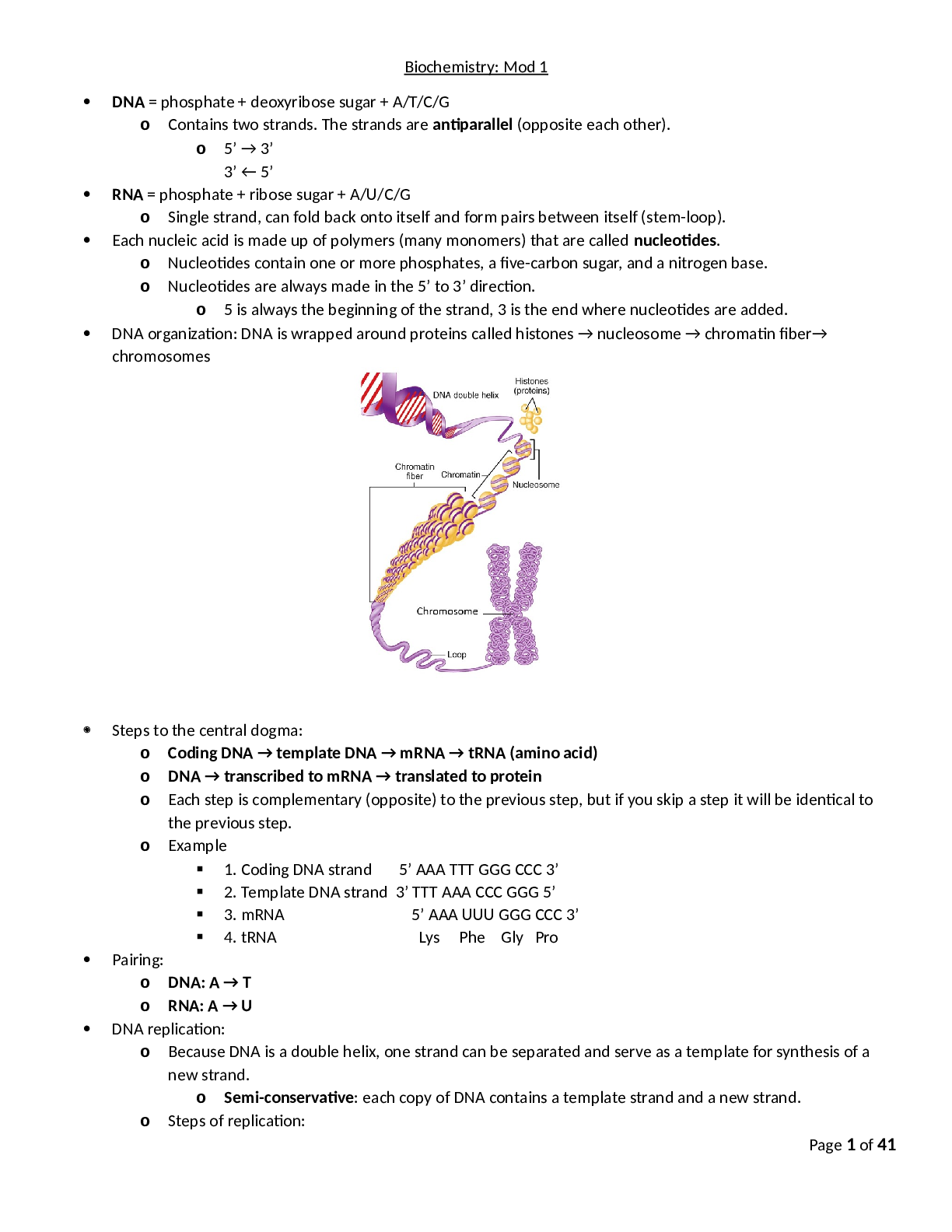
Med-Surg Exam One Study Guide (Fox) What to Know For Exams: ● Test Yourself NCLEX Examination Challenge ● Know Nursing Safety Priority QSEN for the chapters (starts after multiple ... choice study guides-below) ● Know the type of IV to infuse for a patient with hypovolemia (in chart and in youtube link) ● The RN should assess patient manifestations for what in the patient with fluid volume deficit? ○ Loss of extracellular fluid volume exceeds intake of fluid ○ This is not dehydration ○ Urine output <30 mL/hr ○ Acute daily loss of 1 pound ○ Monitor fluid overload: shoes, belt, abdominal girth ○ Weak, rapid pulse, and postural hypotension ○ Tissue turgor decreased (not accurate in elderly) ○ Urine specific gravity: >1.020 ○ Increased BUN ○ Increased creatinine (normal = 0.7-1.4) better indicator of renal function than BUN ● The highest priority nursing for a patient with a serum potassium level of 2.2 mEq/L (Initiate cardiac monitoring) ● RN Pharmacology for Nursing ATI book (Chapter 27) will be on exam ● RN Medical Surgical Nursing will be on Exam 1 (2 ATI Chapters to study, BOTH are Chapter 27 but 2 ATI books=Pharmacology and Med-Surg, also see the beginning of each powerpoint for information to review for exams) Left VS Right Sided-Heart Failure Video: (Video to Help Explain Left VS Right-Sided Heart Failure) https://www.youtube.com/watch?v=Y1IUFGh2T_E TACO (transfusion associated circulatory overload) TRALI (transfusion related acute lung injury) What Is It? -Hydrostatic pulmonary edema due to transfusion (too much blood and non-sanguineous fluid, transfused too rapidly): -High rates of volume infusion -Underlying cardiac or pulmonary pathology Risk Factors: ● Very young/old ● Onset: <2 hours of transfusion Signs: ● Increased BP ● Tachycardia ● Gallop, JVD, systolic/diastolic HTN ● Pulmonary edema ● Increased BNP Diagnosis: ● EKG-new ST segment and T wave changes ● Lab-troponin T >0.1 ng.mL ● Hemodynamic-PAOP >18 mmHg, CVP (central venous pressure) >12 Treatment: ● Diuretics ● Inotropic agents ● Supplemental oxygen therapy ● Nitrates Role of BNP: ● Neurohormone released from ventricular myocardium in response to ventricular volume ● First introduced to diagnose CHF Summary: ● Associated with significant morbidity ● “New” complication of importance What Is It? -Acute respiratory distress Risk Factors: ● Onset: within 6 hours of a plasma containing transfusion Signs: ● Fever (1-2 degrees) ● Hypotension (DO NOT GIVE DIURETICS-COULD WORSEN) ● Hypoxemia (oxygen sat <90% on room air) ● Bilateral pulmonary edema (rapid onset) ● No evidence of circulatory overload ● May be accompanied by: -Fever, hypothermia, BP instability Diagnosis: ● Bilateral infiltrates on chest X-ray Treatment: ● Aggressive respiratory support ● Mechanical ventilation ● Applying restrictive tidal volume ● Fluid restriction ● Under-recognized, under-reported ● Confused with TRALI IV FLUID REPLACEMENT IV Solutions Made Easy (Video) https://www.youtube.com/watch?v=51FkahHUBwc *Remember that Na+ is the popular kid, and water is the quiet kid. Water follows wherever Na+ goes* Isotonic Hypotonic Hypertonic Iso means equal Tonic-concentration of a solution Hypo means below/beneath Tonic-concentration of solution Hyper means excessive Tonic-concentration of solution ● 0.9% saline ● 5% Dextrose in water (D5W) - can be hypotonic too once the body absorbs the dextrose, it becomes a hypotonic solution ● 5% Dextrose in 0.225 saline ● Lactated Ringers Side Effects of having hypotonic cells: -Cell lyses, depletes circulatory system fluid (hypovolemic) ● 0.45% saline (½ NS) ● 0.2225 saline (¼ NS) ● 0.33% saline (⅓ NS) Side Effect of having hypertonic cells: -Cells will shrink! ● 3% saline ● 5% saline ● 10% dextrose in water ● 5% dextrose in 0.9% saline ● 5% dextrose in ½ NS ● 5% dextrose in Lactated Ringers **Given in central line. Also, watch closely, can quickly cause overload, which leads to pulmonary edema** To increase extracellular fluid volume when a patient has decreased extracellular volume) -Does NOT cause shift -Used in: ● Blood loss ● Dehydration ● Surgery To rehydrate cell, moves more fluid into the cell -Used in: ● DKA, hyperglycemia -DO NOT USE WITH: increased intracranial pressure, can shift fluid into brain tissue, burns, and trauma Pushes Na+ back into the intravascular system ● Hyponatremia ● Cerebral edema (decreases swelling by removing fluid off the brain) ***Causes cell dehydration and helps increase fluid in the extracellular space*** Isotonic crystalloid solutions (0.9% NaCl, lactated Ringer) ● Osmolality is 250-375 mOsm/L; concentration is same as plasma & extracellular fluid (285-295 mOsm/L) ● When fluid is infused into extracellular vascular compartment, it remains there because no concentration gradient is present Hypotonic crystalloid solutions (2.5% dextrose & water, 0.45% NaCl) ● Osmolality is less than that of extracellular fluid (<250 mOsm/L) ● When infused into extracellular vascular compartment, body fluids shift out of intravascular compartments into interstitial tissue & cells Hypertonic solutions (dextrose 5% & 0.9% NaCl, 5% dextrose & lactated Ringer) & colloid solutions (dextran, albumin) ● Osmolality is more than that of extracellular fluid (>375 mOsm/L) ● When infused into vascular compartment, body fluids shift from intracellular compartment into extracellular vascular compartment Circle the Correct Answer: 1. The movement of water through a semipermeable membrane is called diffusion/osmosis. (This is the principle of dialysis) 2. The higher the osmolality (concentration) of a solution, the greater/lesser its pulling power for water. 3. Two-thirds of fluid within the body is held in the intravascular/intracellular compartment. 4. If an intravenous solution has a lesser osmolality than normal plasma, it is a isotonic/hypotonic solution. 5. Hypotonic/hypertonic fluids are contraindicated in acute brain injuries because the cells are very sensitive to free water increasing cerebral edema. 6. Colloid osmotic pressure/hydrostatic pressure is the pushing force of a fluid against the walls of the space it occupies. (In the shock patient experiencing third-spacing) 7. Aldosterone is a hormone produced by the adrenal/thyroid gland that conserves sodium/potassium by causing the kidneys to retain this ion. 8. An example of isotonic dehydration would be a patient suffering a traumatic hemorrhage/dysphagic client. 9. A patient suffering from dehydration would have an increased/decreased urine specific gravity. 10. Edema occurs when there is an increased hydrostatic/oncotic pressure forcing fluid to be pushed into tissues. 11. Sodium (Na+) is found predominantly in the intracellular/intravascular compartment. 12. Sodium (Na+) is a(n) anion/cation. 13. A patient with a Na+ level less than 135 mEq/L would be hyponatremic/hypernatremic. 14. 3% NaCl is a hypotonic/hypertonic solution 15. K+ is primarily an intracellular/extracellular cation. 16. A “tented T wave” on an ECG is indicative of hypokalemia/hyperkalemia. 17. Release of parathyroid hormone (PTH) raises/lowers the plasma calcium level by promoting the transfer of calcium from bone to plasma. 18. The active form of calcium is ionized/protein-bound calcium. 19. Massive blood transfusions may result in hypokalemia/hyperkalemia. 20. Massive blood transfusions may result in hypocalcemia/hypercalcemia. (99% of the calcium is in the skeletal system) 21. Signs of hypocalcemia occur when levels of total serum calcium/ionized calcium fall below normal. (Ideally ionized calcium levels should be measured since this is the physiologically active form but often times the serum calcium level available is used) fall below normal, clinically the ionized level is often reported in the arterial blood gas analysis) 22. A positive Chvostek’s/Trousseau’s sign is recorded when inflation of a blood pressure cuff on the upper arm to 20 mm above the systolic BP for about three minutes results in carpopedal spasm. 23. Chronic alcoholism is the most common cause of hypomagnesemia/hypermagnesemia. 24. Overuse of antacids, cathartics or enemas may result in hypomagnesemia/hypermagnesemia. 25. The normal specific gravity range of a urinalysis is 1.003-1.030/ 1.030-1.300 26. Phosphorus is found in high/low amounts in red and organ meats, fish, poultry, eggs, milk and milk products, legumes, whole grains and nuts. 27. Normal adult serum Osmolarity in the body is 270 to 300mOsm/L / 270 to 360 mOsm/L 28. Thrombus is an inflammation of the vein / a blood clot in the vein 29. TPN solutions have a osmolarity greater than 600 mOsm/L / 1400 mOsm/L 30. When placing peripheral IVs in adults it is best to avoid this area due to risk of deep vein thrombosis and infiltration: Lower extremeties / Wrist 31. A PICC can be used for blood draws but the lumen size should be (<4 French/ > 4 French) 32. It is best to choose the smallest / largest gauge catheter capable of delivering the prescribed infusion therapy. Fill in the Blank: 33. The end product of muscle metabolism is lactic acid . 34. 5 percentage of body weight is contained in the intravascular space. 35. 15 percentage of body weight is contained within the interstitum. 36. 40 percentage of body weight is contained in the intracellular space. 37. 25% Albumin IV fluid is a hypotonic / hypertonic solution. 38. Kidney is the body organ most important for maintenance of fluid and electrolytes. Matching: 39. Sodium B A) Maintains body osmolality with Na+ 40. Potassium C B) Maintains extracellular osmolality 41. Chloride A 42. Bicarbonate D C) Promotes transmission of nerve impulses and causes contractility of muscle tissue 43. Calcium E D) Buffers the acidity of body fluids 44. Magnesium F E) Contracts heart muscle F) Aids in neuromuscular transmission and heart muscle contraction Some More Matching:(match correct values with labs): 45. Sodium B A) 3.5-5.0 mEq/L 46. Potassium A B) 135-145 mEq/L 47. Chloride F C) 1.5-2.5 mEq/L 48. Bicarbonate E D) 2.5-4.5 mg/dL 49. Calcium G E) 22-30 mEq/L 50. Magnesium C F) 95-105 mEq/L 51. Phosphorus D G) 9-11 mg/dL 52. Chvostek’s sign is positive when skin turgor remains tented in hypocalcemic states / the facial nerve twitches in hypocalcemic states 53. Kayexalate is given to a person in renal failure for the purpose of excretion of calcium / potassium 54. The following are causes of hyperkalemia : burns, crushing injuries & renal failure / loop diuretics, steroid use, & Cushing’s syndrome. 55. A patient arrives in the emergency department following a motor vehicle accident with fluid volume deficit. The patient is a 45 yr. old male with history of Hepatitis. You need to start an IV for fluid replacement and choose from the following: 5% Dextrose in Lactated Ringers, 5% Dextrose and Water, Lactated Ringers, 0.9% Normal Saline. You select the IV bag labeled 0.9% Normal Saline . 56. You are the admitting RN for a Post operative patient and begin to gather the necessary IV equipment for the patient knowing that most Post-op patients in a general medical surgical unit are administered (hypertonic/hypotonic circle correct answer) IV solutions. 57. You are the RN caring for a previously healthy 27 year old patient with severe acidosis and choose from the following IV bags (5% Dextrose and Water, Lactated Ringers, 0.9% Normal Saline). You select the IV bag labeled Lactated Ringers . 58. You are the RN caring for a patient newly diagnosed during your shift with mild hypernatremia and know that you will need to check your IV fluid stock to make sure that you the following is present in your stock and find the following: 0.45 Normal Saline, 0.9% Normal Saline, 5% albumin, 5% Normal Saline. You select the appropriate IV fluid for this patient and it is 0.45% Normal Saline . “Transfusion responsibilities” of the RN include the Following; True or False 59. The transfusion of blood needs to be completed within 5 hours of removal from refrigeration. a. True b. False 60. Verifying the patient with the patient’s room number a. True b. False 61. Begin transfusion slowly, stay with the patient the first 15 to 30 minutes a. True b. False Watch the Blood Administration video and be able to answer: The universal blood donor type (O Negative) , IV solution best for running with blood administration set (Normal Saline because it can cause cells to clump if you don’t use it!), When an ABO Hemolytic Reaction occurs. The correct administration procedures and supplies for administering PRBCs. 62. Critical Thinking: You know the gauge size of needle for the patient means the : diameter bore is smaller / larger as the gauge number increases 63. The appropriate size of needle for blood administration according to your Medical-Surgical textbook is: (Larger bore diameter 20 gauge or greater / Smaller bore diameter 22 gauge or less) circle the correct answer. (Diameter 18 preferred but depending on the integrity of the vein may go to 22 gauge) 64. Surgery most often uses this gauge for blood administration? _18 gauge_ Blood Transfusion 1. Each year in the US, about how many millions of patients receive transfusions of blood components? ● 4.5 million 2. Patients with acute burn injuries may require up to how many units of platelets? ● 20 units 3. Which is the most commonly transfused of all blood products? ● Packed red blood cells 4. Fresh frozen plasma is transfused primarily to: ● Treat coagulation deficiencies 5. Thawed plasma must be discarded if it is not transfused within how many hours of preparation? ● 36 hours 6. Cryoprecipitate is used to treat deficiency of which of the following? ● Fibrinogen 7. People with Type O blood express which of the following antigens on their RBCs? ● Neither A nor B 8. An example of a delayed transfusion reaction is: ● Post Transfusion purpura 9. A manifestation of acute hemolytic transfusion reaction is: ● Chest pain 10. In response to any acute transfusion reaction, which action should the nurse take first? ● Stop the blood transfusion 11. A clinical manifestation of a severe systemic allergic reaction is: ● Abdominal pain 12. Which of the following medications treats an anaphylactic transfusion reaction? ● Epinephrine 13. Which of the following medications should the patient who requires transfusion therapy and are at risk for transfusion-associated circulatory overload receive? ● Diuretics 14. Patients who develop TRALI have an acute onset of respiratory distress and pulmonary edema within how many hours of transfusion? ● 6 hours 15. With TRALI, immune mediators may produce: ● Blood pressure instability 16. Treatment for TRALI calls for aggressive respiratory support, possibly along with: ● Fluid restriction 17. A clinical manifestation of transfusion-associated graft vs. host disease is: ● Diarrhea 18. Prior to transfusion, which of the following is a preventative strategy for TA-GVHD? ● Irradiating donor lymphocytes 19. Several of the additive solutions that preserve and store blood products put patients at risk for various imbalances including: ● Metabolic acidosis Cardiac Review Questions 1. The tricuspid valve is located between the right atrium and right ventricle. 2. The AV node is the part of the heart’s conduction system that has an inherent rate of 40-60 BPM. 3. A normal cardiac output is 4 L/min to 8 L/min. 4. The component of stroke volume that is the amount of tension on the ventricles at the end of diastole is called preload . 5. The Sympathetic nervous system has a positive chronotropic effect on the heart. 6. The Purkinje system has an inherent heart rate of 20-40 BPM. 7. The Pulmonary artery carries deoxygenated blood. 8. The inner layer of the heart muscle is called the endocardium . 9. The primary job of the AV node is to delay the electrical depolarization of the SA node to the ventricles. 10. The representation of atrial depolarization on an ECG is the P wave. 11. A prolonged QT interval increases the relative refractory period of the heart. 12. The left coronary artery supplies the anterior wall of the left ventricle. 13. The posterior descending artery (PDA) branches off the right coronary artery. 14. Small capillaries that provide coronary bloodflow during ischemic periods is called collateral circulation. 15. Afterload is the amount of resistance on the ventricles during systole. 16. The parasympathetic nervous system innervates the SA node, atria and AV node, but does not innervate the ventricles. 17. The T wave on the ECG represents ventricular repolarization. 18. Cardiac index is cardiac output divided by body surface area and accounts for different sizes of individuals. 19. Venous return is the primary component of ventricular preload. 20. Normal sinus rhythm has a heart rate between 60 and 100 BPM. Circle the appropriate bracketed option to complete the sentence correctly. 21. The sympathetic nervous system [increases/decreases] the inotropic effect on the heart. 22. Preload is [increased/decreased] if the patient has lost most of their blood volume on the ER floor. 23. The QRS complex represents ventricular [depolarization/repolarization] on the ECG. 24. The SA node is located in the [right/left] atrium. 25. The valve that is located between the left atrium and left ventricle is the [mitral/tricuspid] valve. 26. Lanoxin will [increase/decrease] the PR interval on an ECG. 27. If we place a patient in Trendelenburg position, we [increase/decrease] ventricular preload. 28. Hypothermia would [increase/decrease] ventricular afterload. 29. Primary hypertension would [increase/decrease] ventricular afterload. 30. If heart rate is decreased and stroke volume is unchanged, cardiac output would be [increased/decreased]. 31. Coarctation of the aorta [increases/decreases] afterload. 32. Beta blockers [increase/decrease] contractility of the heart. 33. A myocardial infarction (MI) that encompasses the entire wall of the heart muscle is called a subendocardial/transmural] MI. 34. ST segment elevation on the ECG is indicative of [injury/ischemia]. 35. ST segment depression and/or inverted T waves are signs of ischemia and are considered [normal/abnormal] with exercise. 36. There are five basic steps in arrhythmia interpretation including: 1) rhythm, 2) rate, 3) P wave presence, 4) PR interval and 5) [QRS complex duration/QT interval duration]. 37. Atropine is an anticholenergic medication that affects the [sympathetic/parasympathetic] nervous system. 38. In anaphylaxis, the afterload is [increased/decreased]. 39. Ventricular preload of the right ventricle is called the [CVP-central venous pressure/PCWP]. 40. Left ventricular afterload is called the [PVR/SVR-systemic vascular resistance]. 41. Antihypertensive medications are often given to [increase/decrease] afterload. 42. A drug that increases the heart rate is said to have a [positive/negative] chronotropic effect. 43. A normal CVP is [1-10 mm Hg/ 4-12 mm Hg]. 44. Any heart rate greater than 100BPM is said to be [bradycardia/tachycardia]. 45. The P wave represents [atrial/ventricular] depolarization. 46. The QRS complex represents ventricular [depolarization/repolarization]. 47. The T wave represents ventricular [depolarization/repolarization]. 48. The valve located between the right ventricle and the pulmonary artery is the [tricuspid/pulmonic] valve. 49. The [left/right] coronary artery supplies the greater mass of myocardium with its blood flow, thus any lesion may be significant. 50. A medication that increases the force of contraction is said to have a positive [inotropic/chronotropic] effect. 51. The most common rhythm associated with Sudden Cardiac Arrest (SCA) is [atrial fibrillation/ventricular fibrillation]. 52. Data suggests that the caregiver immediately resuming chest compressions after a shock [will/will not] trigger another bout of ventricular fibrillation. Fill in the blanks 53. The RN should thoroughly evaluate the nature and characteristics of chest pain. Ask the patient if he or she has discomfort , heaviness, _pressure_, and indigestion. 54. Following a cardiac catheterization the rapid response team or physician should be called if the patient experiences symptoms of cardiac ischemia such as, dysrhythmias, bleeding, hematoma, or a dramatic change in peripheral pulses of extremity_. 55. For patients with sinus tachycardia, assess for fatigue, weakness, shortness of breath, orthopnea, decreased oxygen saturation and decreased blood pressure_. 56. Palpate the femoral arteries while observing the monitor for widened complexes or auscultating apical heart sounds. Acute MI PVCs may be a warning , possibly triggering life-threatening VT or VF . 57. In some patients , _VT_ causes cardiac arrest. 58. In the above patient it is important for the RN to assess the patient’s airway, breathing , circulation, LOC, and oxygenation level . 59. The next step for the patient in #57 if the patient is stable is to administer and confirm the rhythm via a 12 Lead EKG . 60. Defibrillation (asynchronous counter-shock) is the treatment of choice for unstable supraventricular tachycardia. True or False-cardioversion-synchronous 61. You are caring for a patient with heart valve disease, thus RN teaching prior to dental procedures includes stressing the importance of prophylactic antibiotic therapy . 62. You are an RN caring for a patient post op with an aortic valve replacement. You know this group of patients has a higher risk of post-op hemorrhage. Therefore you will immediately call the Rapid Response Team or other healthcare provider immediately if _heart rate_or _blood pressure_decreases. 63. Bleeding after CABG surgery requires monitoring by the RN. Measure mediastinal and pleural chest tube drainage at least hourly. Report amounts over >150 cc per hour or drastic decreases abruptly to the surgeon. 64. Check CABG patient’s neurologic status every _30_ to _60_ minutes until awakened from anesthesia. Then check patient per agency policy. Cardiac Auscultation Pages: Assessment of the Jugular Venous Pressure (Easy To Assess JVD Video) https://www.youtube.com/watch?v=c2ZOkXthcV0 ● Always observe the venous pulsations in the neck to assess the adequacy of blood volume and central venous pressure (JVP). Nurses can also assess JVP to estimate the filling volume and pressure on the right side of the heart. An increase in JVP causes JVD ● Increases in JVP are usually caused by right ventricular failure. Other causes include tricuspid regurgitation or stenosis, pulmonary hypertension, cardiac tamponade, constrictive pericarditis, hypervolemia, and superior vena cava obstruction. ● Hypokinetic pulse: weak pulse, is indicative of narrow pulse pressure ● Hyperkinetic pulse: large, bounding pulse, caused by increased ejection of the blood (sepsis, exercise, pain, fever, anxiety) ● Assess for: -Bruits: swishing sounds that may occur from turbulent blood flow in narrowed or atherosclerotic arteries -Assess for absence or presence using bell technique of the stethoscope on the neck over the carotid artery while the patient hold their breath -Once the vessel is blocked 90% or greater, the bruit cannot be heard anymore Chapter 13: Nursing Safety Priority QSEN (Concepts of Infusion Therapy) 1. Drugs such as amiodarone (Cordarone), vancomycin (Vancocin), and ciprofloxacin (Cipro IV) are venous irritants that have a pH less than 5.0 (Normal pH is 7.35-7.45). Phlebitis occurs when patients require long-term infusion of these drugs in peripheral circulation. Drugs with vasoconstrictive action (dopamine or chemotherapeutic drugs) are vesicants (chemicals that damage the body tissue on direct contact) that can cause extravasation. Extravasation results in severe tissue integrity impairment as manifested by blistering, tissue sloughing, or necrosis from infiltration into the surrounding tissues. Monitor the IV insertion site carefully for early manifestations of infiltration, including swelling, coolness, or redness. If any of these symptoms are present, discontinue the drug therapy, and notify the infusion team. If an infusion specialist is not available, contact the HCP and remove IV catheter. 2. Determine that the IV prescription is appropriate for the patient and clarify any questions with the primary health care provider before administration. Be sure to check for the accuracy and completeness of the treatment prescription. An example of an incomplete one is 5% dextrose in water to keep the vein open. This statement does not specify the rate of infusion and is not considered complete. 3. Avoid veins on the palmar side of the wrist because the median nerve is located close to the veins in this area, making the venipuncture more painful and difficult to stabilize. The cephalic vein begins above the thumb and extends up the entire length of the arm. The vein is usually large and prominent, appearing as a prime site for catheter insertion. Damage to the nerve from any injury can result in permanent loss of function or complex regional pain syndrome, type 2. Reports of tingling, feelings pins and needles in the extremity, or numbness during the venipuncture can indicate nerve puncture. If any of these symptoms occur, stop the IV insertion procedure immediately, remove the catheter, and choose a new site. 4. The INS recommendation for flushing PICC lines not actively used is 5 mL of heparin in a 10 mL syringe at least daily when using a non valved catheter and at least weekly with a valved catheter. Use 10 mL of sterile saline to flush before and after medication administration; 20 mL of sterile saline is flushed after drawing blood. Always use 10 mL barrel syringes to flush any central line because the pressure exerted by a smaller barrel poses a risk for rupturing the catheter. 5. Before giving a drug through an implanted port, always check for blood return. If there is no blood return, withhold the drug until patency and adequate non coring needle placement of the port are established. Serious extravasation of vesicant drugs can occur because a fibrin sheath may occur at the tip of the catheter, clot it, and cause retrograde subcutaneous leakage. 6. Regardless of the type of fluid container being used, check it for cracks or pinholes before use. Always observe the fluid for turbidity (cloudiness) or any unusual color that could indicate contamination. 7. Remind UAP (unlicensed assistive personnel) to avoid taking blood pressures in an extremity with any type of catheter in place. If a short peripheral catheter is being used, for continuous infusion, the compression while taking BP can increase venous pressure causing fluid to overflow from the puncture site and cause infiltration. When a midline catheter or PICC is being used, compression from the BP could increase vein irritation and lead to phlebitis. ● Draw blood samples in the extremity opposite from all catheters. Blood should not be drawn from a venipuncture site proximal (above) an infusing peripheral catheter because the infusing fluid could alter the results of the test being performed. Venipuncture at or near the insertion site of a midline catheter or PICC could damage the catheter, add to areas of venous inflammation, and decreased perfusion. 8. Site protection may be needed for short peripheral catheters or for port access needles. Plastic shields can be placed over the site to prevent accidental bumping or pressure from clothing. Make sure that you can easily access the site frequently. Never place a restraint or opaque dressing over a peripheral IV site, especially when infusing an irritant or vesicant. 9. Assess catheter patency carefully before each use. Use sterile technique to flush with normal saline while applying slow, gentle pressure to the syringe plunger. If you feel any resistance, stop the procedure immediately! If you continue, catheter rupture or forcing a blood clot into circulation could result. During the flushing procedure always aspirate for a brisk blood return from the catheter lumen. ● If the catheter will not yield a blood return, further diagnostic studies may be needed to determine the cause of the problems. Thrombolytic agents such as alteplase (Cathflo Activase) may be used to dissolve blood clots in venous catheters. 10. Catheter securement may mean that administration sets are placed out of easy reach of a confused patient. Use flexible netting over the extremity to help prevent the patient from pulling at the dressing or tubing, while allowing easy access to the site. A device such as the IV House UltraDressing can also protect the site. Do not use rolled bandages to cover the extremity because they prevent insertion site assessment. Complications may progress to an advanced state before they are noticed. 11. Carefully secure all junctions on the administration sets with Luer-Lok devices. Life-threatening hemorrhage can occur if an accidental disconnection occurs! When an infusion pump is used, be sure that it has a pressure high enough to overcome arterial pressure. Closely monitor the arterial insertion site and affected extremity. Assess the extremity for warmth, sensation, cap refill, and pulse. Chapter 33: Nursing Safety Priority QSEN (Assessment of the Cardiovascular System) 1. Thoroughly evaluate the nature and characteristics of the chest pain. Because pain resulting from MI is life threatening and can lead to serious complications, its cause should be considered ischemic until proven otherwise. When assessing for symptoms, ask the patient if he or she has discomfort, heaviness, pressure, and/or indigestion. It is important to note that chest pain can occur in any setting. Proper assessment of the pain can decrease the potential for serious complications. 2. If the patient experiences symptoms of MI such as chest pain, dysrhythmias, bleeding, hematoma formation, or a dramatic change in peripheral pulses in the affected extremity, contact Rapid Response. Remain with the patient and obtain a 12-lead EKG for patients experiencing chest pain or dysrhythmias. For bleeding or hematoma formation, hold steady, firm pressure, to the access site until Rapid Response arrives. Neurologic changes indicating possible stroke, such as visual disturbances, slurred speech, swallowing difficulties, and extremity weakness, should also be reported immediately. Chapter 34: Nursing Safety Priority QSEN (Care of Patients with Dysrhythmias) 1. For patients with sinus tachycardia, assess for fatigue, weakness, SOB, orthopnea, decreased oxygen saturation, increased pulse rate, and decreased blood pressure. Also assess for restlessness and anxiety from decreased cerebral perfusion and decreased urine output from impaired renal perfusion. The patient may also have anginal pain and palpitations. The ECG pattern may show T-wave inversion or ST-segment elevation or depression in response to MI. 2. Teach patients who have permanent pacemakers: ● Keep handheld cell phones at least 6 in. away from the generator, with the handset ear opposite to the side of the generator ● Avoid sources of strong electromagnetic fields, such as magnets and telecommunication towers/transmitters ● Carry a pacemaker ID card provided by the manufacturer and wear a med alert bracelet at all times 3. Side effects of adenosine include significant bradycardia with pauses, nausea, and vomiting. When administering adenosine, be sure to have emergency medical equipment available! 4. The loss of coordinated atrial contractions in AF can lead to pooling of blood, resulting in clotting. The patient is at high risk for pulmonary embolism! Thrombi may form within the right atrium and then move through the right ventricle to the lungs. If pulmonary embolism is suspected, remain with the patient and monitor for SOB, chest pain, and/or hypotension. Initiate the Rapid Response and notify the provider. ● In addition, the patient is at risk for systemic emboli, particularly an embolic stroke, which may cause severe neurologic impairment or death. Monitor patients carefully for signs of stroke. Initiate Rapid Response Team if stroke is suspected to facilitate timely diagnosis. ● Patients with AF who have valvular disease are particularly at risk for venous thromboembolism. In VTE, the patient may complain of lower extremity pain and swelling. Anticipate ultrasound of vasculature and initiation of systemic anticoagulation. 5. Teach patients taking any type of anticoagulant drug to report bruising, bleeding, nose or gums, and other signs of bleeding to their primary health care provider immediately. 6. For safety before cardioversion, turn oxygen off and away from patient; fire could result. Shout clear before shock delivery for electrical safety. 7. Because other dysrhythmias can cause widened QRS complexes, assess whether the PVCs perfuse to the extremities. Palpate the carotid, brachial, or femoral arteries while observing the monitor for widened complexes or auscultating apical heart sounds. With acute MI, PVCs may be considered as a warning, possibly triggering life-threatening ventricular tachycardia (VT) or ventricular fibrillation (VF). 8. In some patients, VT causes cardiac arrest. Assess the patient’s circulation and airway, breathing, LOC, and oxygenation. For the stable patient with sustained VT, administer oxygen and confirm the rhythm via a 12-lead ECG. Amiodarone (Cordarone), lidocaine, or magnesium sulfate may be given. 9. Early defibrillation is critical in resolving pulseless ventricular tachycardia (VT) or (VF). It must not be delayed for any reason after the equipment and skilled personnel are present. The earlier, the greater chance of survival! Do not defibrillate ventricular asystole. The purpose of defibrillation is disruption of the chaotic rhythm, allowing the SA node signals to restart. In ventricular asystole, no electrical impulses are present to disrupt. ● Before defibrillation, loudly and clearly state clear before shock is delivered. Deliver shock and immediately resume CPR for 5 cycles or about 2 minutes. Reassess rhythm every 2 minutes and if indicated. Charge the defibrillator to deliver an additional shock at the same energy level previously used. During the 2-minute intervals while high-quality CPR is being delivered, the team administers meds and performs interventions to try and restore cardiac rhythm Chapter 35: Nursing Safety Priority QSEN (Care of Patients with Cardiac Problems) 1. Edema is an extremely unreliable sign of HF. Be sure that accurate daily weights are taken to document fluid retention. Assessing weight at the same time of the morning using the same scale is important. Weight is the most reliable indicator of fluid gain and loss! 2. Provide the necessary amount of supplemental oxygen within a range prescribed by the healthcare provider to maintain oxygen saturation at 90% or greater. If the patient has dyspnea, place in high Fowler’s position with pillows under each arm to maximize chest expansion and improve gas exchange. Repositioning and performing cough exercises every 2 hours helps to improve gas exchange and prevent atelectasis. Interprofessional collaboration with the respiratory therapist is important to plan the most effective methods for assisting with ventilation. 3. ACEIs and ARBs are started slowly and cautiously. The first dose may be associated with a rapid drop in BP. Patients at risk for hypotension usually have an initial systolic BP less than 100 mmHg, are older than 75 years of age, have a serum sodium level less than 135, or are volume depleted. Monitor BP every hour for several hours after the initial dose and each time the dose is increased. Immediately report to the HCP and document the systolic BP of less than 90 mmHg. If this problem occurs, place the patient flat and elevate legs to increase cerebral perfusion and promote venous return. 4. When giving Natrecor (human BNP), monitor BP and pulse carefully because significant decreases in BP can occur. Although the patient’s systolic BP may be between 90 and 100 mmHg, he or she is usually asymptomatic. Give Natrecor through a separate infusion line because it is incompatible with heparin and most other parenteral meds. Expect an increase in the serum BNP after drug administration. 5. Increased cardiac automaticity occurs with toxic digoxin levels or in the presence of hypokalemia, resulting in ectopic beats (PVCs). Changes in potassium level, especially a decrease, cause patients to be more sensitive to the drug and cause toxicity. The signs and symptoms of digoxin toxicity are: ● Anorexia ● Fatigue ● Blurred vision ● LOC changes Toxicity may cause nearly any dysrhythmia, but PVCs are most commonly noted. Assess for early signs of toxicity such as bradycardia and loss of P wave on ECG. Carefully monitor the apical pulse rate and heart rhythm of patients receiving digoxin. The HCP determines the desirable heart rate to achieve. Some HCP prefer a rate between 50 and 60. Report the development of either an irregular rhythm in a patient with a previously regular rhythm or a regular rhythm in a patient with a previously irregular rhythm. Monitor serum digoxin and potassium levels to identify toxicity. Older adults are more likely to have this because of decreased renal excretion. Any drug that increases the workload of the heart also increases its oxygen requirement. Be alert for the possibility that the patient may experience angina in response to digoxin. 6. Assess for and report early symptoms, such as crackles in the lung bases, dyspnea at rest, disorientation, and confusion, especially in older patients. Document the precise location of the crackles because the level of fluid progresses from the bases to higher levels in the lungs as HF gets worse. The patient in acute pulmonary edema is typically extremely anxious, tachycardic, and struggling for air. As pulmonary edema becomes more severe, he or she may have a moist cough productive of frothy, blood-tinged sputum; and his or her skin may be cold, clammy, or cyanotic. 7. If the patient is not hypotensive, place in a sitting (high-Fowler’s)position with the legs down to decrease venous return to the heart. The priority nursing action is to administer oxygen therapy at 5 to 12 L/min by simple facemask or at 6 to 10 L/min by non breathing mask with reservoir to promote gas exchange and perfusion. Apply a pulse ox and titrate the oxygen flow to keep the patient’s oxygen sat above 90%. If supplemental oxygen does not resolve the patient’s respiratory distress, collaborate with the respiratory therapist, physician, advanced practice nurse, for more aggressive therapy, such as continuous positive airway pressure (CPAP) or bi-level positive airway pressure (BiPAP) ventilation. Intubation and mechanical ventilation may be needed for some patients. 8. Per the HF Core Measure for discharge instructions, teach the patient and caregiver to immediately report to the HCP the occurrence of ANY of these symptoms, which could indicate worsening or recurrent heart failure: ● Rapid weight gain (3 lb in one week or 1-2 lb overnight) ● Decrease in exercise tolerance lasting 2-3 days ● Cold symptoms (cough) lasting more than 3-5 days ● Excessive awakening at night to urinate ● Development of dyspnea or angina at rest or worsening angina ● Increased swelling in feet, ankles, or hands 9. Teach patients with valve disease the importance of prophylactic antibiotic therapy before any invasive dental or oral procedure. This includes patients with previous history of endocarditis and cardiac transplant or valve recipients. Have patients demonstrate appropriate oral hygiene because oral health is the best intervention to prevent endocarditis. Prophylactic antibiotics are not recommended before GI procedures such as upper GI endoscopy, colonoscopy, or procedures requiring genitourinary instrumentation. 10. After valvuloplasty, observe the patient closely for bleeding from the catheter insertion site and institute post-angiogram precautions. Bleeding is likely because of the large size of the catheter. Assess for signs of a regurgitant valve by closely monitoring heart sounds, cardiac output, and heart rhythm. Because vegetations (thrombi) may have been dislodged from the valve, observe for indications of systemic emboli. 11. Patients with mitral stenosis often have pulmonary hypertension and stiff lungs. Therefore monitor respiratory status closely during weaning from the ventilator. Be specifically alert or bleeding in those with aortic valve replacements because of a higher risk for postoperative hemorrhage. If heart rate or BP decreases, call Rapid Response immediately. 12. Patients must remind HCP (including dentists) of their endocarditis. Guidelines for antibiotic prophylaxis have been revised and are only recommended if the patient with a prosthetic valve, a history of infective endocarditis, or an unrepaired cyanotic congenital heart disease undergoes an invasive dental or oral procedure. Instruct patients to note any indications of recurring endocarditis such as fever. Remind them to monitor and record their temperature daily for up to 6 weeks. Teach them to report fever, chills, malaise, weight loss, increased fatigue, sudden weight gain, or dyspnea to the HCP. 13. After pericardiocentesis, closely monitor the patient for the recurrence of tamponade. Pericardiocentesis alone often does not resolve acute tamponade. Be prepared to provide adequate fluid volumes to increase CO and to prepare the patient for emergency sternotomy if tamponade occurs. 14. After surgery, perform comprehensive cardiovascular and respiratory assessments frequently according to agency or heart transplant surgical protocol. Signs and symptoms of rejection to heart transplant include: ● SOB ● Fatigue ● Fluid gain (edema, increased weight) ● Abdominal bloating ● New bradycardia ● Hypotension ● Atrial fibrillation or flutter ● Decreased activity tolerance ● Decreased ejection fraction (late sign) Report any of these to the HCP immediately! To detect rejection, the surgeon performs right endomyocardial bypass at regularly scheduled intervals and whenever symptoms occur. Chapter 38: Nursing Safety Priority QSEN (Care of Patients with Acute Coronary Symptoms) 1. Before administering Nitroglycerin, ensure that the patient has not taken any meds for erectile dysfunction, such as (Viagra) within the past 24-48 hours. Concomitant use of NTG with these inhibitors can cause profound hypotension. Remind patients not to take these meds within 24-48 hours of one another. Some of those inhibitors are also used in the treatment of pulmonary arterial hypertension. Patients with this cannot stop taking the inhibitors. As a result, NTG is contraindicated. ● Teach the patient to hold the NTG tablet under their tongue and drink 5 mL (1 teaspoon) of water, if necessary, to allow the tablet to dissolve. NTG spray is also available and is more quickly absorbed. Pain relief should begin within 1-2 minutes and should be clearly evident in 3-5 minutes. After 5 minutes, recheck the patient’s BP and pain intensity. If BP is less than 100 mmHg systolic or 25 mmHG lower than the previous reading, lower the head of the bed and notify the HCP. 2. If the patient is experiencing an MI, prepare him or her for transfer to a specialized unit where close monitoring and appropriate management can be provided. If the patient is at home or in the community, call 911 for transfer to the closest ED. 3. Dual antiplatelet therapy is suggested for all patients with Acute Coronary Syndrome, incorporating Aspirin and either Clopidogrel or Brilinta. The major side effect for each is bleeding. Observe for bleeding tendencies, such as nosebleeds, or blood in the stool. Meds will need to be discontinued if evidence of bleeding occurs. Teach patients signs of bleeding and when to contact the HCP. 4. When giving glycoprotein inhibitors, assess the patient closely for bleeding or hypersensitivity reactions. If either occurs, call Rapid Response immediately. Monitor the platelet level 4 hours after starting drug and daily thereafter. Notify the HCP if the patient experiences a significant decrease in platelet count per agency protocol. 5. Do not give beta blockers if the pulse is below 55 or the systolic BP is below 100 mmHg without first checking with the HCP. The beta-blocking agent may lead to persistent bradycardia or further reduction of systolic BP, leading to poor peripheral and coronary perfusion. 6. Monitor for report, and document these signs of inadequate organ perfusion that may result from decreased cardiac output: ● A change in orientation or mental status ● Urine output less than 0.5-1 mL/kg/hr ● Cool, clammy extremities with decreased or absent pulses ● Unusual fatigue ● Recurrent chest pain 7. Use caution when giving positive inotropes because of the potential risk for increasing myocardial oxygen consumption and further decreasing cardiac output. Monitor the patient frequently, paying particular attention to the development of chest pain. 8. Monitor for, report, and document manifestations of cardiogenic shock (necrosis of more than 40% of the left ventricle) immediately: ● Tachycardia ● Hypotension ● Systolic BP less than 90 mmHg or 30 mmHg less than the patient’s baseline ● Urine output less than 0.5-1 mL/kg/hr ● Cold, clammy skin with poor peripheral pulses ● Agitation, restlessness, or confusion ● Pulmonary congestion ● Tachypnea ● Continuing chest discomfort 9. After Percutaneous Coronary Intervention (invasive, but nonsurgical technique that is performed within 90 minutes of an MI to reduce the frequency and severity of discomfort for patients with angina), monitor for potential problems, including acute closure of the vessel (causes chest pain and potential ST elevation on 12-lead ECG), bleeding from the insertion site, and reaction to the contrast medium used in angiography. Also monitor for hypotension, hypokalemia, and dysrhythmias. Document and report any of these findings to the HCP immediately! 10. Bleeding after Coronary Artery Bypass Graft surgery occurs to a limited extent in all patients. Measure mediastinal and pleural chest tube drainage at least hourly. Report drainage amounts over 150 ml/hr to the surgeon. Patients with internal mammary artery grafts may have more chest drainage than those with leg grafts. 11. Assess for, document, and report manifestations of cardiac tamponade immediately: ● Sudden cessation of previously heavy mediastinal drainage ● Beck’s Triad: -JVD, but clear lung sounds -Distant, muffled heart sounds -Hypotension ● Pulsus paradoxus (BP more than 10 mmHg higher on expiration than on inspiration) ● An equalizing of PAWP and right atrial pressure ● Cardiovascular collapse 12. After a CABG surgery, check the patient’s neurologic status every 30-60 minutes until he or she has awakened from anesthesia. Then heck every 2-4 hours per agency policy. 13. Monitor the neurovascular status of the donor arm of patients whose radial artery was used as a graft in CABG surgery. Assess the hand color, temperature, pulse (both ulnar and radial), and cap refill every hour initially. In addition, check the fingertips, hand, and arm for sensation first 24 hours after surgery to promote vasodilation in the donor arm and therefore maintain circulation. 14. The FDA has strengthened the warnings associated with NSAIDs and cardiovascular risk. Use of NSAIDs can increase the chance of an MI or stroke. This risk of heart attack or stroke can occur early in treatment and may increase with length of treatment. Those with CVD have the greatest risk for adverse complications and events. Teach patients that NSAIDs are commonly available OTC, so it is very important to read box labels. Acetaminophen products provide an alternative for pain relief and fever reduction. 15. Use of sublingual or spray NTG deserves special attention. Teach the patient to carry NTG at all times. Keep the tablets in a glass, light-resistant container. The drug should be replaced every 3-5 months before it loses its potency or stops producing a tingling sensation when placed under the tongue. EKG Leads to Detect Cardiac Damage ● Left heart injury: ST elevation in leads (V2, V3, V4), reflecting injury to the anterior wall. Leads (I, aVL, V5, and V6) reflecting injury to the lateral wall ● ST elevation in leads (II, III, and aVF), reflecting injury to the inferior wall ● ST depression in leads (V1, V2, and V3), reflecting posterior wall injury. You should suspect right heart involvement ● Where is the most common site for MI? (R or L ventricle, and why?) [Show More]
Last updated: 1 year ago
Preview 1 out of 36 pages
Instant download
Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Mar 23, 2021
Number of pages
36
Written in
Additional information
This document has been written for:
Uploaded
Mar 23, 2021
Downloads
0
Views
63







Perioperative Nursing Care.png)