*NURSING > TEST BANK > TEST BANK for Advanced Practice Nursing in the Care of Older Adults 2nd Edition by Laurie Malone, (All)
TEST BANK for Advanced Practice Nursing in the Care of Older Adults 2nd Edition by Laurie Malone, Lori Plank, Evelyn Duffy (Chapter 1-19)
Document Content and Description Below
Advanced Practice Nursing in the Care of Older Adults/ Edition2 TESTBANK Chapter 1. Changes with Aging Multiple Choice Identify the choice that best completes the statement or answers the que... stion. 1. The major impact of the physiological changes that occur with aging is: A. Reduced physiological reserve B. Reduced homeostatic mechanisms C. Impaired immunological response D. All of the above 2. The strongest evidence regarding normal physiological aging is available through: A. Randomized controlled clinical trials B. Cross-sectional studies C. Longitudinal studies D. Case control studies 3. All of the following statements are true about laboratory values in older adults except: A. Reference ranges are preferable B. Abnormal findings are often due to physiologicalaging C. Normal ranges may not be applicable for olderadults D. Reference values are not necessarily acceptable values 4. Biochemical individuality is best described as: A. Each individual’s variation is often much greater than that of a larger group B. The unique biochemical profile of a selected population C. The truly “normal” individual—falling within average range D. Each individual’s variation is often much smaller than that of a larger group 5. Polypharmacy is best described as taking: A. More than nine medications per day B. More than five medications per day C. Even a single medication if there is not a clear indication for its use D. When a drug is given to treat the side effect of another drug 6. Pharmacokinetic changes with aging is reflective of: A. What the drug does to the body B. What the body does to the drug C. The effect at the site of action and the time and intensity of the drug D. The side effects commonly associated with the drug 7. All the following statements are false about drug absorption except: A. Antacids increase the bioavailability ofdigitalis B. Gastric acidity decreases withage C. Anticholinergics increase colonicmotility D. Underlying chronic disease has little impact on drugabsorption 8. All of the following statements are true about drug distribution in the elderly except: A. Drugs distributed in water have lowerconcentration B. Drugs distributed in fat have less intense, more prolongedeffect C. Drugs highly protein bound have greater potential to cause an adversedrug reaction D. The fastest way to deliver a drug to the action site is byinhalation 9. Men have faster and more efficient biotransformation of drugs and this is thought to be due to: A. Less obesity rates thanwomen B. Prostateenlargement C. Testosterone D. Less estrogen thanwomen 10. The cytochrome p system involves enzymes that are generally: A. Inhibited bydrugs B. Induced bydrugs C. Inhibited or induced bydrugs D. Associated with decreased liverperfusion 11. A statement not shown to be true about pharmacodynamics changes with aging is: A. Decreased sensitivity to oralanticoagulants B. Enhanced sensitivity to central nervous systemdrugs C. Drug responsiveness can be influenced by patient activitylevel D. There is a decreased sensitivity to betablockers 12. Atypical presentation of disease in the elderly is reflected by all the following except: A. Infection withoutfever B. Depression without dysphoricmood C. Myocardial infarction with chest pain anddiaphoresis D. Cardiac manifestations of thyroid disease 13. Functional abilities are best assessed by: A. Self-report of function B. Observed assessment offunction C. A comprehensive head-to-toeexamination D. Family report offunction Chapter 2. Health Promotion Multiple Choice Identify the choice that best completes the statement or answers the question. 1. The leading cause of death in elderly travelers worldwideis: A. Cardiovasculardisease B. Infections C. Accidents D. Malaria 2. Which of the following should be avoided in countries where food and water precautions are to be observed? A. Hotcoffee B. Bottledwater C. Saladbuffet D. Unpeeledbananas 3. What insect precautions are not necessary to prevent insect-borne diseases in thetropics? A. Using 100% DEET on skin to preventbites B. Treating clothes withpermetherin C. Covering up exposed skin to lessen bitingsurface D. Taking malaria pills as directed for areas at risk formalaria 4. An example of secondary prevention you could recommend/order for older adults would beto: A. Check for fecal occultblood B. Wear seat belts in thecar C. Provide foot care for a diabeticpatient D. Administer a tetanusshot 5. Ali is a 72-year-old man who recently came to the U.S. from Nigeria. He reports having BCG (bacille Calmette-Guerin) vaccination as a child. Which of the following is correct regarding a tuberculin skin test? A. It should not be done atall. B. Itshould be read as smaller than it reallyis. C. Vaccination history is irrelevant; read as usual. D. It should be read as larger than it reallyis. 6. A 72-year-old woman and her husband are on a cross-country driving vacation. After a long day of driving, they stop for dinner. Midway through the meal, the woman becomes very short of breath, with chest pain and a feeling of panic. Which of the following problems is mostlikely? A. Pulmonaryedema B. Heartfailure C. Pulmonaryembolism D. Pneumonia 7. Ivan W. is a 65-year-old man who is new to your practice. He has a history of COPD, CAD, hypertension, and type 2 diabetes mellitus. He has had no immunizations since his discharge from the military at age 25. Childhood diseases included chickenpox, measles, mumps, and “German measles.”Hepresentsforadisease management visit.Whichofthefollowingimmunizationswould you recommend forIvan? A. MMR, influenza, pneumococcal,Zostavax B. Influenza, pneumococcal, PPD, HepatitisB C. Tdap, pneumococcal, influenza,Zostavax D. Hepatitis B, influenza, pneumococcal, HepatitisA 8. Leo L. is a 62-year-old African American male who comes for an initial visit to yourpractice. Personal health history includes smoking 1 pack/day since age 11, consuming a case of beer (24 bottles) every weekend, and working as an assembler (sedentary job) for the past 10 years. Family history in first-degree relatives includes hypertension, high cholesterol, heart attack, and type 2 diabetes mellitus. Leo’s BMI is 32; BP today is 130/86. You order a fasting glucose, lipid profile, and return visit for BP check. This is an example of: A. Primaryprevention B. Secondaryprevention C. Tertiaryprevention D. Healthprofiling 9. A local chapter of a nurse practitioner organization has begun planning a community-based screening for hypertension at a local congregate living facility. This population was selected onthe basisof: A. A predicted decreased incidence of high blood pressurein thispopulation B. A recognized element of high risk within thisgroup C. Readily available treatmentmeasures D. Achieving an administrative goal for the congregate livingfacility 10. Performing range of motion exercises on a client who has had a stroke is an example of which level of prevention? A. Primary prevention B. Tertiary prevention C. Secondary prevention D. Rehabilitation prevention 11. The nurse practitioner demonstrates an understanding of primary prevention of falling among the elderly through which managementplan? A. Evaluate a need for assistive devices for ambulation after the client hasbeen injured from afall. B. Provide resources to correct hazards contributing to falls in the homeenvironment. C. Reinforce the need to use prescribed eyeglasses to prevent further injury from falls. D. Provide information about medications, side effects, andinteractions. 12. An example of an active strategy of health promotion for an individual to accomplish wouldbe: A. Maintaining clean water in the local environment B. Introducing fluoride into thewater C. Beginning a stress managementprogram D. Maintaining a sanitary sewage system 13. You are working with an older male adult with a long history of alcohol abuse and a 30-year history of smoking. In recommending an intervention for this client, your responsibility isto: A. Make the individual abandon his own health practices and follow your recommendations B. 5 tuberculin units intradermal PPD injection and if negative repeat with same dose one weeklater C. Chest x-ray at the same time of PPDtesting D. 5 tuberculin units intradermal PPD injection and if positive repeat same dose in one week Chapter 2: Health Promotion Answer Section Chapter 3. Exercise in Older Adults Multiple Choice Identify the choice that best completes the statement or answers the question. 1. Exercise recommended for older adults should include activitiesthat: A. Conserve energy B. Restrictflexibility C. Strengthenmuscles D. Are anaerobic innature 2. Preferred amount of exercise for older adultsis: A. 10 minutes of physical activity eachmorning B. 30 minutes per day of aerobic activity five times aweek C. Any increase in physical activity over a sedentarylifestyle D. 60 minutes per day that includes 30 minutes of aerobic activity and 30 minutes of weight training five times aweek 3. Which of the following medical conditions is not considered restrictive for engaging in physical activity? A. Unstable angina B. Dehydration C. Depression D. Uncontrolledtachycardia 4. The best recommendation for a patient who states they have no equipment to exercise wouldbe: A. Sign a contract for a year’s membership to a localgym B. Borrow free weights fromgrandchildren C. Have a personal trainer come to the home three times aweek D. Improvise with recommended objects at home that can beused 5. When the nurse practitioner recommends exercise for a sedentary older adult, which of the following pieces of advice should be considered for all types ofexercise? A. Only use equipment recommended by physicaltrainers B. Start low and goslow C. Only group exercise is beneficial to someone who has not been active in a long time D. Focus only on one type of exercise for the first fewmonths Chapter 4. Comprehensive Geriatric Assessment Multiple Choice Identify the choice that best completes the statement or answers the question. 1. The evidence reflects that comprehensive geriatric assessment should beconducted: A. On all individuals 65 andolder B. On all individuals 75 andolder C. By an inter-disciplinary team ofprofessionals D. Targeting the vulnerable and frailelderly 2. Evidence-based geriatric assessment instruments available to theclinician: A. Are largely screening instruments to detect acondition B. Largely do not exist and if they do they have limited clinicalutility C. Include screening, evaluation, and measurement instruments in multipledomains D. Have applicability in the outpatient but not the inpatientsetting 3. When interviewing the older adult with a suspected dementia, it is most importantthat: A. Mental status be evaluated first in order to determine if the patient is a reliable historian B. The examiner use short simple questions and recognize non-verbal signs of discomfort C. Postpone the mental status evaluation for the following visit and establish a rapport first D. The clinician get in contact with a family member to obtain thehistory 4. Which is not considered a dimension ofsymptomatology? A. Onset B. Physicalsigns C. Location D. Absence of associatedsymptoms 5. The best approach to taking the health history isto: A. Start with an open-endedquestion B. Start with the review ofsystems C. Focus on the chiefcomplaint D. Complete the history before conducting the examination 6. A review of the evidence relative to screening of the elderly reveals the highest evidence ratingfor: A. Visionscreening B. Mammographyscreening C. Hearingscreening D. Dementia screening 7. Assessment of vital signs in the elderlyreflect: A. Errors in blood pressure measurement are rare with automated recordingdevices B. Shortness of breath in the elderly is rare in the older, deconditioned, and immobile patient C. Older adults prefer a 0-10 pain ratingscale D. Older adults could be septic with a temperature within normallimits 8. What statement is true about nutrition intake in theelderly? A. Deficiencies in protein intake are common withaging. B. Malnutrition is the most common nutritional disorder among the elderly living in the community. C. Increased caloric consumption is needed as oneages. D. The serum albumin is a good reflection of proteinstores. 9. What is reflective of functional decline in olderadults? A. Functional decline is synonymous with advancedage. B. Some individuals die of “old age” but have maintained an active and healthy lifestyle. C. Instrumental activities of daily living are preserved longer than activities ofdaily living. D. It is always possible to prevent functionaldeterioration. 10. The leading cause of traumatic death in the elderly is dueto: A. Motor vehicleaccidents B. Pedestrianinjuries C. Falls D. Burns 11. Timing of the get-and-go test enhances its sensitivity. The process should take lessthan: A. Thirtyseconds B. Sixteenseconds C. Sixtyseconds D. Tenseconds 12. A validated tool for assessing cognitive function specific to dementiais: A. Mini-cog B. Confusion assessmentmethod C. Yesavage GDSscale D. NuDesc 13. The medical outcome study short form 36 remains the gold standard of quality of life instruments. It measures: A. Mental and socialdomains B. Socialdomain C. Physical, mental, and socialdomains D. Physicaldomain Chapter 5. Symptoms and Syndromes Multiple Choice Identify the choice that best completes the statement or answers the question. 1. The term “geriatric syndrome” is best describedas: A. A condition that has multiple underlying factors and involves multiplesystems B. A condition that has a discreet etiology that is difficult topinpoint C. Significant progress has been made in understanding geriatric syndromes, especially falls anddelirium D. Therapeutic management of a geriatric syndrome can be accomplished once a specific diagnosis ismade 2. The anal wink reflex is used totest: A. Rectalprolapse B. Sensation and pudental nervefunction C. Baseline and squeeze sphinctertone D. Fissures andfistulas 3. Atypical presentation of acute coronary syndrome is: A. Most common in Hispanicfemales B. More common inmen C. Most common in African Americanmen D. More common infemales 4. What disease can mimic and often co-exists with myocardial infarctions in elders with coronary artery disease? A. Hypertension B. Esophagealdisease C. Diabetic gastroparesis D. Vasculardisease 5. Thoracic aortic dissection presents typicallyas: A. Sharp stabbing pain in the midthorax B. Pleuretic chest pain anddyspnea C. Severe retrosternal chest pain that radiates to the back and botharms D. Unilateral pleuretic chest pain anddyspnea 6. Medications known to contribute to constipation include all of the following except: A. Stimulantlaxatives B. Anticholinergic drugs C. Broad-spectrumantibiotics D. Iron 7. Bordetella pertussis is best characterized by: A. Sub-acute cough lasting greater than twoweeks B. Acute cough associated with a coryzalsymptom C. Chronic cough with post-nasaldrip D. Non-productive acutecough 8. The routine testing of tuberculosis should occur in all of the following vulnerable populations except: A. Nursing homeresidents B. Prisoninmates C. Hospitalizedelderly D. Immune-compromisedpatients 9. Which of the following statements about fluid balance in the elderly is false? A. Total body water decreases withage. B. Thirst response decreases as a personages. C. African Americans have higher rates of dehydration than whiteAmericans. D. Assessment of skin turgor at the sternum is a reliable indicator of dehydration in theelderly. 10. Distinguishing delirium from dementia can be problematic since they may co-exist. The primary consideration in the differential is: A. Performance on the Mini Mental StatusExam B. The Confusion Assessment isnegative C. Rapid change and fluctuating course of cognitivefunction D. The presence of behavioral symptoms with cognitiveimpairment 11. Presbystasis is best described as: A. Impairment in vestibular apparatus that causes dizziness B. Age-related disequilibrium of unknown pathology characterized by a gradual onset of difficulty walking C. The loss of high frequency tones with aging that can impair sensation D. A disorder of the inner ear characterized by vertigo 12. If dizziness has a predictable pattern associated with it, the clinician should first consider: A. Hypoglycemia B. Psychogenic etiology C. Cardiovascular cause D. Neurogenic cause 13. All of the following are considered as contributors to dysphagia except: A. Anticholinergics B. Drugs that increase reflux symptoms C. Inadequate intake of fluids with medications and meals D. Smooth muscle relaxants 14. Evidence shows that the most important predictor of a fall is: A. Prior history of a fall B. Cognitiveimpairment C. Gait and balancedisturbance D. Proximal muscle weakness 15. The most cost-effective interventions used to prevent falls are: A. Use of sitters B. Use of alarms (bed, chair, monitors) C. Tai Chi exercises D. Home modifications and vitamin D supplement 16. Chronic fatigue syndrome is best described as A. Fatigue that is constant, lasting more than three months B. Fatigue lasting longer than six months and not relieved by rest C. Fatigue that waxes and wanes over a period of three months D. Total exhaustion with inability to get out of bed 17. Which form of headache is bilateral? A. Cluster B.Tension C. Migraine D. Acute angle closure glaucoma 18. Microscopic hematuria is defined as: A. Twenty or more RBCs on a urine sample B. Three or more RBCs on a urine sample C. Twenty or more RBCs on three or more samples of urine D. Three or more RBCs on three or more samples of urine 19. Risk factors associated with the finding of a malignancy in a patient with hemoptysis include all of the following except: A. Male sex B. Smokinghistory C. Over age 40 D. Childhood asthma 20. Recent weight loss is defined as: A. loss of >10 pounds over the past 3-6 months B. loss of >2 pounds a week C. 5% weight loss in three months D. 10% weight loss in one year 21. The most common cause of disability in the elderly is due to: A. Diabetes B. Arthritis C. Heart disease D. Chronic obstructive pulmonary disease 22. Lipedema is best described as: A. Bilateral accumulation of interstitial fluid B. Bilateral distribution of fat in the lowerextremities C. Fluid retention caused by a compromised lymphaticsystem D. Lipid molecules that break down and cause fluid retention 23. Drug-induced pruritus is distinguished because it: A. Occurs soon after a new drug is taken B. Usually is a generalized rash C. May occur right after the drug is taken or months later D. Usually involves localized circumscribed lesions 24. A form of syncope that is more common in the elderly than younger adults is: A. Vasovagal B. Carotid sinus sensitivity C. Orthostatic hypotension D. Arrhythmias 25. All of the following statements about tremor are true except: A. The most common tremor is the Parkinson tremor B. Most individuals with tremor do not seek medical attention C. Psychogenic tremor is uncommon D. Tremor is more prevalent in whites than blacks 26. Overflow incontinence is usually associated with: A. Loss of urine that occurs with urgency B. Cognitive impairment C. Weak pelvic floor muscles D. Bladder outlet obstruction 27. Wandering is best described as: A. Aimless excessive ambulatory behavior B. Purposeful excessive ambulatorybehavior C. Risk-seeking behavior in the cognitivelyimpaired D. A result of boredom in those withdementia Chapter 6. Skin and Lymphatic Disorders Multiple Choice Identify the choice that best completes the statement or answers the question. 1. Which of the following dermatological conditions results from reactivation of the dormant varicella virus? A. Tinea versicolor B. Seborrheic keratosis C. Verruca D. Herpeszoster 2. An older adult male presents with pain in his right chest wall for the past 48 hours. Upon examination, the nurse practitioner notices a vesicular eruption along the dermatome andidentifies this as herpes zoster. The NP informs the gentlemanthat: A. All symptoms should disappear within threedays B. Oral medications can dramatically reduce the duration and intensity ofhis symptoms C. He has chickenpox and can be contagious to hisgrandchildren D. He has a sexually transmitteddisease 3. A 70-year-old white male comes to the clinic with a slightly raised, scaly, pink, and irregular lesion on his scalp. He is a farmer and works outside all day. You suspect actinic keratosis, but cannot rule out other lesions. What recommendation would you give him? A. Ignore the lesion, as it is associated withaging. B. Instruct him to use a nonprescription hydrocortisone cream to dry up thelesion. C. Perform a biopsy or refer to a dermatologist. D. Advise him to use a dandruff shampoo and return in one month if the lesion has not goneaway. 4. The immunofluorescent antibody (IFA) is a laboratory test used to diagnose which of the following disorders? A. Tinea versicolor B. Herpeszoster C. Squamous cellcarcinoma D. Human papillomavirus 5. A wound with drainage and foul odor should be cleansedwith: A. Normalsaline B. Hydrogenperoxide C. 20% aceticacid D. Betadine 6. A full thickness pressure ulcer is partially covered with eschar and the surrounding tissue is reddened. Which of the following is the most appropriate treatment for thiscondition? A. Apply an occlusivedressing B. Debride mechanically orchemically C. Saline moistened gauzedressings D. Vacuum-assisted woundclosure 7. In examining the skin of your nursing home patient, you note a “stained glass” brownish mark on the face. Which of the following lesions best describes a stained glass brownishmark? A. Actinic keratosis B. Seborrhea keratosis C. Lentigomaligna D. Superficial spreading malignantmelanoma 8. Patients who have an underlying tinea infection to the cellulitis should also be treated with which one of thefollowing? A. An anti-fungalmedication B. Topicalsteroids C. Oralsteroids D. Zinc oxide 9. Identify the type of malignant melanoma that is associated with the Hutchinson’s sign of the cuticle of thefinger. A. Lentigomaligna B. Acrallentiginous C. Nodular D. Superficial spreading malignantmelanoma 10. A smooth round nodule with a pearly gray border and central induration best describes which skin lesion? A. Seborrheic keratosis B. Malignantmelanoma C. Herpeszoster D. Basal cellcarcinoma 11. Cellulitis is a deep skin infection involving the dermis and subcutaneous tissues. The nurse practitioner suspects cellulitis in a 70-year-old Asian diabetic male presenting with reddened edematous skin around his nares. Which statement below will the nurse practitioner use in her decision-making process for the differential diagnosis pertaining to reddened edematousskin? A. Cellulitis is two times more common inwomen B. Facial cellulitis is more common in people>55 C. There is low incidence of cellulitis in patients withdiabetes D. Cellulitis is only a disease of the lower extremities of patients with known arterial insufficiency 12. An 82-year-old female has a “pimple” on his nose that occasionally bleeds and may have increased in size in the past year. The lesion is a 0.7-cm, dome-shaped, umbilicated papule with pearly translucence. There is also a hemorrhagic crust covering the central portion. Which of the following is the most likelydiagnosis? A. Squamous cellcarcinoma B. Basal cellcarcinoma C. Keratocanthoma D. Sebaceoushyperplasia 13. Which of the following is generally not a first-line treatment for post herpeticneuralgia? A. Intrathecalmethylprednisolone B. Gabapentin C. 5% lidocainepatch D. Topicalcapsaicin 14. A nursing home resident with a Stage 4 pressure ulcer that extends to the muscle layer and has significant undermining with heavy exudate should be treatedwith: A. Dry gauzedressings B. Duoderm C. Chemicaldebridement D. Calcium alginatedressings 15. Which of the following descriptions accurately documentscellulitis? A. Cool, erythematous, shiny hairless extremity with decreasedpulse B. Scattered, erythematous ring-like lesions with clearcenters C. Clearly demarcated, raised erythematous area offace D. Diffusely inflamed skin that is warm and tender topalpation 16. Asymmetrical bi-color lesion with irregular border measuring 8 mm is found on the right lower arm of an adult patient. This assessment finding is consistentwith: A. Melanoma B. Basal cellcarcinoma C. Leukoplakia D. Senilelentigines 17. Which of the following descriptions best illustrates assessment findings consistent with tineacapitis? A. Circular erythematous patches with papular, scaly annular borders andclear centers B. Inflamed scaly dry patches with brokenhairs C. Web lesions with erythema and scalingborders D. Scaly pruritic erythematous lesions on inguinalcreases 18. A hyperkeratatotic nodule formed as the result of exposure of the foot to moisture from perspiration iscalled: A. Hardcorn B. Tinea pedis C. Softcorn D. Plantar warts(verrucae) 19. A 64-year-old male presents with an exacerbation of psoriasis. His social history includes 50-year two packs a day of cigarettes and a six-pack a week of beer. He states he had a recent sore throat, which he attributes to minding his young grandson. He reports that until recently the pruritis was only minimal. His BMI is 37. Which of the following factors most likely contributed to the acute presentation ofpsoriasis? A. Alcoholabuse B. Smoking C. Streptococcalinfection D. Obesity 20. Treatment of complicated cellulitis of the lower extremity resulting from an anaerobe requires all of the followingexcept: A. Extended antibiotic medication lasting at least 7-10days B. Topical antifungalmedication C. Inquiry when last tetanus toxoid booster wasgiven D. Elevation of limb and consideration of compressionbandaging Chapter 7. Head, Neck, and Face Disorders Multiple Choice Identify the choice that best completes the statement or answers the question. 1. A 64-year-old male presents with erythema of the sclera, tearing, and bilateral pruritus of the eyes. The symptoms occur intermittently throughout the year and he has associated clear nasal discharge. Which of the following is most likely because of theinflammation? A. Bacterium B. Allergen C. Virus D. Fungi 2. One of the first-line treatments in patients with allergic rhinitis is the use of nasal corticosteroid sprays. What is the anticipated onset of symptom relief with the use of thesemedications? A. Two weeks ormore B. Immediate C. 1 to 2 days D. A minimum of oneweek 3. The nurse practitioner knows that antihistamines work primarily through which of the following mechanisms? A. Vasodilatation B. Blocking leukotrieneeffects C. Inhibiting histamine receptorsites D. Vasoconstriction 4. Cromolyn sodium may also be used in the treatment of allergic rhinitis. What is the mechanism of action of thismedication? A. Mast cellstabilization B. Blocking the effects ofIgE C. Leukotrieneinhibition D. Histamineblockade 5. Patients that have atopic disorders are mediated by the production of IGE will have histamine stimulated as an immediate phase response. This release of histamine results in which of the following? A. Sinus pain, increased vascular permeability, andbronchodilation B. Bronchospasm, vascular permeability, andvasodilatation C. Contraction of smooth muscle, decreased vascular permeability,and vasoconstriction D. Vasodilatation, bronchodilation, and increased vascularpermeability 6. Which of the following maneuvers is used to induce symptoms of benign paroxysmal positional vertigo? A. The Fukuda steppingtest B. The Dix-Hallpikemaneuver C. Forcedhyperventilation D. The head thrust test 7. You have a patient complaining of vertigo and want to know what could be the cause. Knowing there are many causes for vertigo, you question the length of time the sensation lasts. Shetells you several hours to days and is accompanied by tinnitus and hearing loss. You suspect which of the followingconditions? A. Ménière’sdisease B. Benign paroxysmal positionalvertigo C. TIA D. Migraine 8. Sensory impairment (vision and hearing) in the elderly is associatedwith: A. Impaired quality oflife B. Decreasedfunction C. Increasedmortality D. All of theabove 9. Which of the following conditions is the leading cause of blindness in the UnitedStates? A. Maculardegeneration B. Diabetic retinopathy C. Glaucoma D. Cataracts 10. A slightly elevated elastic tissue deposit in the conjunctiva that may extend to the cornea but does not cover it is known as a: A. Pterygium B. Pinguecula C. Xanthelsma D. Limbalnodule 11. A nonmodifiable risk factor for the development of cataracts is: A. Long-term exposure to ultraviolet Bradiation B. High alcoholintake C. Strong familyhistory D. Diabetesmellitus 12. Causes of sensorineural hearing loss include: A. Ototoxicity B. Ménière’sdisease C. Otosclerosis D. Inner earfistula 13. Clinical findings in patients with nonproliferation retinopathy include: A. Cotton woolspots B. Microaneursyms C. Deephemorrhages D. Neovascularization 14. In examining the mouth of an older adult with a history of smoking, the nurse practitioner finds a suspicious oral lesion. The patient has been referred for a biopsy to be sent for pathology. Which is the most common oral precancerous lesion? A. Fictionalkeratosis B. Keratoacanthoma C. Lichenplanus D. Leukoplakia 15. A gross screening for hearing is the whisper tests. Which cranial nerve is being tested when the nurse practitioner conducts this test? A. Cranial nerveV B. Cranial nerveVII C. Cranial nerveVIII D. Cranial nerveIV Chapter 8. Chest Disorders Multiple Choice Identify the choice that best completes the statement or answers the question. 1. In mitral stenosis, p waves maysuggest: A. Left atrialenlargement B. Right atrialenlargement C. Left ventricleenlargement D. Right ventricleenlargement 2. Aortic regurgitation requires medical treatment for early signs of CHFwith: A. Beta blockers B. ACEinhibitors C. Surgery D. Hospitalization 3. A key symptom of ischemic heart disease is chest pain. However, angina equivalents may include exertional dyspnea. Angina equivalents are importantbecause: A. Women with ischemic heart disease many times do not present with chestpain B. Some patients may have no symptoms or atypical symptoms. Diagnosis may only be made at the time of an actual myocardialinfarction C. Elderly patients have the most severesymptoms D. A & Bonly 4. The best evidence rating drugs to consider in a post myocardial infarction patientinclude: A. ASA, ACE/ARB, beta-blocker, aldosteroneblockade B. Ace, ARB, Calcium channel blocker,ASA C. Long-acting nitrates, warfarin, ACE, andARB D. ASA, clopidogrel,nitrates 5. A 55-year-old post-menopausal woman with a history of hypertension complains of jaw pain on heavy exertion. There were no complaints of chest pain. Her ECG indicates normal sinus rhythm without ST segment abnormalities. Your plan mayinclude: A. Echocardiogram B. Exercise stress test C. Cardiac catheterization D. Myocardial perfusionimaging 6. Preceding a stress test, the following lab work mightinclude: A. CBC and differential to differentiate ischemic heart disease fromanemia B. Liver enzymes to rule out underlying gall bladderdisease B. Stresstest C. Chestx-ray D. Echocardiography 12. The aging process causes what normal physiological changes in theheart? A. The heart valve thickens and becomes rigid, secondary to fibrosis andsclerosis B. Cardiology occurs along with prolapse of the mitral valve andregurgitation C. Dilation of the right ventricle occurs with sclerosis of pulmonic andtricuspid valves D. Hypertrophy of the rightventricle 13. An older adult may present with atypical clinical signs of pneumonia. The nurse practitioner needs to be aware that the clustering of all of the following signs and symptoms may be indicative of pneumonia in an older personexcept: A. Bradycardia B. Malaise C. Anorexia D. Confusion 14. Which of the following statements is true concerning anti-arrhythmicdrugs? A. Amiodarone is the only one not associated with increased mortality and it has a very favorable side effectprofile. B. Both long-acting and short-acting calcium channel blockers are associated withan increased risk of cardiovascular morbidity andmortality. Most anti-arrhythmics have a low toxic/therapeutic ratio and some areexceedingly toxic. C. Anti-arrhythmic therapy should be initiated in the hospital for allpatients. 15. Dan G., a 65-year-old man, presents to your primary care office for the evaluation of chest pain and left-sided shoulder pain. Pain begins after strenuous activity, including walking. Pain is characterized as dull, aching; 8/10 during activity, otherwise 0/10. Began a few months ago, intermittent, aggravated by exercise, and relieved by rest. Has occasional nausea. Pain is retrosternal, radiating to left shoulder, definitely affects quality of life by limiting activity. Pain is worse today; did not go away after he stopped walking. BP 120/80. Pulse 72 and regular. Normal heart sounds, S1 and S2, no murmurs. Which of the following differential diagnoses would be mostlikely? A. Musculoskeletal chest wall syndrome withradiation B. Esophageal motor disorder withradiation C. Acute cholecystitis withcholelithiasis D. Coronary artery disease with anginapectoris 16. Jose M. is a 68-year-old man who presents to your primary care practice for a physical. Jose has had type 2 diabetes mellitus for 5 years, diet controlled. His BMI is 32. Smoker, pack per day for 25 years. He denies other medical problems. Family history includes CAD, CABG x4 for father, now deceased; CHF, type 2 diabetes mellitus, HT for mother. According to the AHA/ACC guidelines, what stage isJose? A. StageA B. StageB C. StageC D. StageD 17. Susan P., a 60-year-old woman with a 30 pack year history, presents to your primary care practice for evaluation of a persistent, daily cough with increased sputum production, worse in the morning, occurring over the past three months. She tells you, “I have the same thing, year after year.” Which of the following choices would you consider strongly in your critical thinkingprocess? A. Seasonalallergies B. Acute bronchitis C. Bronchialasthma D. Chronicbronchitis 18. The best way to diagnose structural heart disease/dysfunction non-invasivelyis: A. Chestx-ray B. EKG C. Echocardiogram D. Heartcatheterization 19. A common auscultatory finding in advanced CHFis: A. Systolic ejectionmurmur B. S3 galloprhythm C. Frictionrub D. Bradycardia 20. The organism most commonly responsible for community-acquired pneumonia in older adultsis: A. Pseudomonasaeruginosa B. Staphylococcusaureus C. Proteusmirabilis D. Streptococcuspneumonia 21. A 72-year-old woman and her husband are on a cross-country driving vacation. After a long day of driving, they stop for dinner. Midway through the meal, the woman becomes very short of breath, with chest pain and a feeling of panic. Which of the following problems is mostlikely? A. Pulmonaryedema B. Heartfailure C. Pulmonaryembolism D. Pneumonia Chapter 9. Peripheral Vascular Disorders Chapter 9: Peripheral Vascular Disorders Multiple Choice Identify the choice that best completes the statement or answers the question. 1. The clinician should begin the peripheral vascular examwith: A. Auscultation of the carotidarteries B. Checking for peripheraledema C. Auscultation of theheart D. Palpation of the upper extremityarteries 2. Inspection of the distal nails and nail beds should be evaluated for signs of decreasedperfusion. Signs include: A. Clubbing B. Cyanosis C. Petechiae D. All of theabove 3. A thorough vascular exam includes all of the following except: A. Cardiac exam B. Reproductive organexam C. Peripheral vascularexam D. Cranial nerveexam 4. The majority of abdominal aortic aneurysms are due to: A. Trauma B. Infection C. Inflammation D. Atherosclerosis 5. The best initial screening test for abdominal aortic aneurysm is: A. Angiography B. CT scan with IVcontrast C. Abdominalultrasound D. MRI 6. The initial treatment for symptomatic abdominal aortic aneurysm involves: A. Emergencysurgery B. Aggressive blood pressurecontrol C. Watch-and-waitapproach D. Cardiologyconsult 8. An early symptom of peripheral artery disease is: A. Painful cramping of muscles duringwalking B. Pain is worse when the legs are dependent below the level of theheart C. Pain intensifies after vigorous walking isstopped D. Ulceration or gangrene occurs at the sight of minorinjury 9. The hallmark of venous stasis ulcers include all of the following except: A. Lower extremityedema B. Hyperpigmentation of the lowerextremities C. Ulcers on the medial or lateralmalleolus D. Copious drainingulcers 10. Exercise is an essential element of peripheral arterial disease management primarily because: A. It encourages weight loss, as being overweight is a contributing factor toPAD B. Evidence shows exercise reduces smoking C. Collateral vessels arestrengthened D. It improves aerobic capacity 11. Home exercise programs for peripheral arterial disease focus on: A. Walk until pain develops thenstop B. Walk through the pain thenstop C. Begin at a slow speed with 10 minutes a day and build up to 30minutes D. Walk through the pain, rest until it goes away, then resumewalking 12. When should surgical options for peripheral arterial disease be considered? A. Immediately after the diagnosis since the prognosis without revascularization is poor B. After two weeks of pentoxifylline (Trental)therapy C. Pain is not relieved withrest D. Pain limits the patient’s lifestyle or ulcerationoccurs 13. All of the following are classic signs of venous insufficiency except: A. Pain B. Dependentedema C. Hemosiderosis D. Dermatitis 14. Lower leg edema associated with pain is characteristic of: A. Venousinsufficiency B. Heartfailure C. Deep venousthrombosis D. Diabetes 15. The most common cause of secondary lymphedema is: A. Surgery B. Cancertreatment C. Infection D. Trauma 16. The imaging gold standard for lymphedema is: A. Lymphosonogram B. Lymphoscintigraphy C. Lymphoangiogram D. CTscan 17. Known risk factors for lymphedema include all of the following except: A. Osteoarthritis B. Rheumatoidarthritis C. Obesity D. Venous ulcerdisease 18. Complete decongestive physiotherapy (CDP) works by: A. Stimulating the lymphvessels B. Breaking up subcutaneous fibroustissue C. Redirecting lymphflow D. All of the above Chapter 10. Abdominal Disorders Multiple Choice Identify the choice that best completes the statement or answers the question. 1. Your 70-year-old patient has gastroesophageal reflux disease (GERD). After a trial of lifestyle modifications and antacids, the patient continues to have occasional mild heartburn after occasional meals and at night. The most appropriate next actionis: A. Prokinetic agents B. H2antagonists C. Proton pumpinhibitors D. Surcralfate 2. An older patient reports burning pain after ingestion of many foods and large meals. What assessment would assist the nurse practitioner in making a diagnosis ofGERD? A. Identification of a fluidwave B. Positive Murphy’s sign C. Palpable spleen D. Midepigastric pain that is not reproducible withpalpation 3. The nurse practitioner is examining a 62-year-old female who has been complaining of lower abdominal pain. Upon auscultation, bowel sounds are high pitched and tinkling. Which ofthe following terms describes thisfinding? A. Successionsplash B. Borborygmi C. Tenesmus D. Puddle sign 4. In teaching an older adult female client with end-stage renal disease her medication regimen, the nurse practitioner must include which of the following pieces of information in the treatmentplan? A. Report any changes in the color of herstool B. Take iron supplement and elemental calcium with eachmeal C. Take iron supplement before meals and the calcium aftermeals D. Take calcium with a high phosphorusmeal 5. A 62-year-old client presents with a complaint of fever, pain, and burning on urination. Difficulty urinating with dribbling has been increasing in the past few days. He has a feeling of pressure in his groin. On examination, his prostate is tender, boggy, and warm. A stat urinalysis reveals the presence of leukocytes and bacteria. He is allergic to sulfa drugs. His weight is 70 kg and his last serum creatinine was 1.0. While awaiting the culture and sensitivity, the nurse practitioner begins empiric treatment with which of the following? A. Trimethoprim/sulfamethroxazole DS bid x 2weeks B. Ampicillin 250 mg PO q day for 10days C. Nitrofurantoin 100 mg Q 12 hours for 7days D. Ciprofloxacin 500 mg Q 12 hours for 14days 6. A 62-year-old woman presents with a recurrent urinary tract infection. She now has a fever of 104°F and severe costovertebral tenderness with pyuria. What is the appropriate diagnosis and intervention for this patient? A. Septic arthritis and oral prednisolone isindicated B. Pyelonephritis and hospitalization isrequired C. Recurrent cystitis and 10 days of antibiotics areneeded D. Pelvic inflammatory disease and 7 days of antibiotics areindicated 7. Which of the following drugs would be useful for the nurse practitioner to prescribe for an older adult to prevent gastric ulcers when a nonsteroidal anti-inflammatory drug is used for chronic pain management? A. Misoprostol(Cytotec) B. Cimetidine(Tagamet) C. Metronidazole (Flagyl) D. Bismuth subsalicylate (Peptobismol) 8. A 68-year-old male reports painless rectal bleeding occasionally noted with thin pencil-like stools, but no pain with defection. He has a history of colon polyp removal 10 years ago but was lost to follow-up. The nurse practitioner’s appropriate interventionis: A. Digital rectal exam and send home with 3 hemoccult toreturn B. Immediate referral to gastroenterologist andcolonoscopy C. Order a screeningsigmoidoscopy D. Order a colonoscopy and barium enema and refer based on results 9. Asymptomatic 1+ bacteruria is found in a nursing home resident with an indwelling catheter. The nurse practitioner’s initial intervention includes: A. Assessing resident’s cognitive status and last change of thecatheter/bag B. Prescribing prophylactic Bactrim 1 tablet atbedtime C. Ordering a urine culture and sensitivity and prescribing empiric treatment until resultsobtained D. Ordering an x-ray of the kidney, urine, andbladder 10. When counseling clients regarding the use of antidiarrheal drugs such as Imodium anti-diarrheal and Kaopectate, the nurse practitioner advises patients to: A. Use all themedication B. Do not use for possible infectiousdiarrhea C. Use should exceed one week foreffectiveness D. These drugs provide exactly the same pharmaceuticaleffects 11. When teaching a group of older adults regarding prevention of gastroesophageal reflux disease symptoms, the nurse practitioner will include which of the following instructions? A. Raise the head of the bed with pillows at night and chew peppermints when symptoms of heartburnbegins B. Raise the head of the bed on blocks and take the proton pump inhibitor medication atbedtime C. Sit up for an hour after taking any medication and restrict fluidintake D. Avoid food intolerances, raise head of bed on blocks, and take a protonpump inhibitor before ameal 12. A clinical clue for suspected renal artery stenosis would be: A. Decreased urineoutput B. Development of resistant hypertension in a previously well-controlledpatient C. Retroperitoneal pain on the affectedside D. Rising BUN level with normal creatinine level 13. Helicobacter pylori is implicated as a causative agent in the development of duodenal or gastric ulcers. What teaching should the nurse practitioner plan for a patient who has a positive Helicobacter pylori test? A. It is highly contagious and a mask should be worn athome. B. Treatment regimen is multiple lifetimemedications. C. Treatment regimen is multiple medications taken daily for a fewweeks. D. Treatment regimen is complicated and is not indicated unless the patient is symptomatic. 14. An obese middle-aged client presents with a month of nonproductive irritating cough without fever. He also reports occasional morning hoarseness. What should the differential include? A. Atypicalpneumonia B. Peptic ulcerdisease C. Gastroesophagealreflux D. Mononucleosis(Epstein-Barr) 15. Which of the following findings would indicate a need for another endoscopy in clients with peptic ulcerdisease? A. Cases of dyspepsia withconstipation B. Symptoms persisting after 6-8 weeks oftherapy C. All clients with dyspepsia who smoke and drinkalcohol D. When a therapeutic response to empiric treatment isobtained 16. A careful history of a female client with a chief complaint of intermittent diarrhea reveals that she also experiences bouts of constipation. She has no known allergies and experienced no unintentional weight loss. What is the most likelycondition? A. Inflammatory boweldisease B. Irritable bowelsyndrome C. Giardiasis D. Lactose intolerance 17. The nurse practitioner is discussing lifestyle changes with a patient diagnosed with gastroesophageal reflux. What are the nonpharmacological management interventions that should beincluded? A. Weight reduction and rest 30 minutes after each meal in the supineposition B. Elevation of head of the bed 4-6 inches on blocks and weightreduction C. Encouraged to wear restrictive clothing to add support for diaphragmaticbreathing D. Using oral mints to relieve gastric distress 18. In differentiating a gastric ulcer from a duodenal ulcer, you know that each type of ulcer can present with distinct signs and symptoms. Which of the following pieces of information from the patient’s history is the least useful for you to determine that the patient has a duodenalulcer? A. Pain occurs on an emptystomach B. Diffuse epigastricpain C. Rarely associated with non-steroidaluse D. Occurs in patients under 40 years ofage 19. A 74-year-old obese female presents complaining of persistent right upper quadrant pain. She reports that she has not had any prior abdominal surgeries. Which of the following laboratory studies would be most indicative of acutecholecystitis? A. C-reactive protein level of 3mg B. White blood cell count of11,000 C. Direct serum bilirubin level of 0.3mg/dL D. Serum amylase level of 145U/L 20. Which of the following is not a contributing factor to the development of esophagitis in olderadults? A. Increased gastric emptyingtime B. Regular ingestion ofNSAIDs C. Decreasedsalivation D. Fungal infections such asCandida Chapter 11. Urological and Gynecologic Disorders Multiple Choice Identify the choice that best completes the statement or answers the question. 1. Which ethnic group has the highest incidence of prostatecancer? A. Asians B. Hispanics C. AfricanAmericans D. AmericanIndians 2. Men with an initial PSA level below 2.5 ng/ml can reduce their screening frequency to what intervals? A. Every 6months B. Yearly C. Every 2years D. Every 2 to 4years 3. All of the following may be reasons associated with an elevated PSA besides prostate cancer except: A. Prostatitis B. Urinary tractinfection C. Perinealtrauma D. Digital rectalexam 4. In the diagnosis of acute bacterial prostatitis, a midstream urine culture is of benefit. To be diagnostic, the specimen should reveal how many white blood cells per high-power field? A. Five B. Ten C. Fifteen D. Twenty 5. In chronic bacterial prostatitis, what is the organism most commonly associated with the disease? A. Klebsiella B. Proteus C. Pseudomonas D. Escherichiacoli 6. In acute prostatitis, an exam of the prostate may find the gland to be: A. Nodular B. Cool andpliable C. Swollen andtender D. Asymmetrical 7. All of the following antimicrobials may be indicated in chronic bacterial prostatitis except: A. Ciprofloxacin B. Levofloxacin C. Trimethoprim D. Azithromycin 8. Age-related changes in the bladder, urethra, and ureters include all of the following in older women except: A. Increased estrogen production’s influence on the bladder andureter B. Decline in bladder outletfunction C. Decline in ureteral resistancepressure D. Laxity of the pelvicmuscle 9. Mr. Jones is a 68-year-old retired Air Force pilot that has been diagnosed with prostate cancer in the past week. He has never had a surgical procedure in his life and seeks clarification on the availability of treatments for prostate cancer. He asks the nurse practitioner to tell him the side effects of a radical prostatectomy. Which of the following is NOT a potential side effect of thisprocedure? A. Urinaryincontinence B. Impotence C. Dribblingurine D. Selected low backpain 10. The nurse practitioner is evaluating a patient’s pelvic muscle strength by digital examination. This is performedwhen: A. A male patient complains of nocturia anddribbling B. The nurse practitioner needs to confirm a cystocele or stressincontinence C. The patient reports sudden loss of large amounts of urine or urgeincontinence D. The nurse practitioner suspects overflowincontinence 11. A pelvic mass in a postmenopausalwoman: A. is most commonly due to uterinefibroids. B. is alwayssymptomatic. C. is highly suspicious for ovariancancer. D. should be monitored over a period oftime. 12. A 79-year-old man is being evaluated for frequent urinary dribbling without burning. Physical examination reveals a smooth but slightly enlarged prostate gland. His PSA level is 3.3 ng/mL. The patient undergoes formal urodynamic studies, and findings are as follows: a decreased bladder capacity of 370 mL; a few involuntary detrusor contractions at a low bladder volume of 246 mL; an increased postvoid residual urine volume of 225 mL; and a slightly decreased urinary flowrate. Which of the following is not consistent with a normal age-associated change? A. PSA level of 3.3ng/mL B. Decreased bladdercapacity C. Involuntary detrusorcontradictions D. Increased postvoid residual urinevolume 13. Mrs. Smith, a 65-year-old woman presents to clinic for the first time and complains of urinary incontinence and dyspareunia. She went through menopause 10 years ago without any hormone replacement therapy and had a hysterectomy for a fibroid. Her mother had a hip fracture at 82 years of age. The patient’s most recent mammogram was 5 years ago and no known family history of breast cancer. She is not taking any medications. Her physical examination is unremarkable except for findings consistent with atrophic vaginitis. You decide to begin topical hormonereplacement therapy. Which of the following evaluations would be necessary prior to initiating hormone replacement therapy? A. Mammogram B. Endometrialbiopsy C. Bone mineral densitymeasurement D. Papanicolaousmear 14. Mrs. L. Billings is a 77-year-old Caucasian female who has a history of breast cancer. She has been in remission for 6 years. As her primary care provider, you are seeing her for follow-up of her recent complaintofintermittentabdominalpainofa3-monthdurationandsomegeneralmalaise. Giventhe brief history above, what will you direct your assessment at during physicalexamination? A. Examination of her thyroid to rule out thyroid nodules that may contribute to her feelingfatigued. B. Auscultation of her abdomen for abnormal bowel sounds to rule outperitonitis. C. Thorough abdominal and gynecological exam to rule out masses and identify any tenderness. D. A rectal examination to rule out colon cancer as a secondary site for breastcancer. 15. A 78-year-old female comes to the office because she has pain when she urinates. She has been seen three times for this problem in the last 3 months. Each time she was told she had a UTI and was given antibiotics. She carefully followed the instructions but has had no relief of symptoms. Last UA: WBCs: 2-3/high-power field RBCs: 0-2/high-power field Epithelial cells: Few Nitrite: Negative Leuckocyte esterase: Negative Which of the following should be done next? A. Obtain a clean catch urine for UA and urine forC&S B. Perform a pelvicexamination C. Reassure the patient that she has asymptomatic bacteriuria and does not need antibiotics D. Order a pelvicultrasound Chapter 12. Musculoskeletal Disorders Multiple Choice Identify the choice that best completes the statement or answers the question. 1. Osteoarthritis of the cervical and lumbar spine causes pain that is related to all of the following except: A. Bone spurformation B. Pressure of theligaments C. Reactive musclespasm D. Crystaldeposition 2. In differentiating osteoarthritis from chronic gout, pseudogout, or septic arthritis, the most valuable diagnostic study wouldbe: A. Erythrocyte sedimentation rate(ESR) B. Synovial fluidanalysis C. C-reactive proteinanalysis D. Complete blood cellcount 3. Patients with osteoarthritis of the hip and knee often have a distinguishable gait describedas: A. Ataxic B. Festinating C. Antalgic D. Steppage 4. Which of the following best describes the pain associated with osteoarthritis? A. Constant, burning, and throbbing with an acuteonset? B. Dull and primarily affected by exposure to cold and barometricpressure C. Begins upon arising and after prolonged weight bearing and/or use of thejoint D. Begins in the morning but decreases withactivity 5. Joint effusions typically occur later in the course of OA, especially in the: A. Knee B. Elbow C. DIPjoints D. Hips 6. You have ordered a CBC for your patient you suspect has polymyalgia rheumatica (PMR). Which two clinical findings are common in patients with PMR? A. Neutropenia and hypochromic, normocyticanemia B. Normochromic, normocytic anemia andthrombocytosis C. Microcytic, hypochromic anemia andreticulocytopenia D. Macrocytic, hyperchromic anemia andleukocytopenia 7. You suspect that your patient has polymyalgia rheumatica and now are concerned that the patient may also have Giant Cell Arteritis (GCA). Which of the following two symptoms are most indicative of GCA and PMR? A. Jaw pain and heartmurmur B. Joint swelling and sudden loss of central visionbilaterally C. Hoarseness and the total inability to grasp smallobjects D. Scalp tenderness and aching in shoulder and pelvicgirdle 8. Your 63-year-old Caucasian woman with polymyalgia rheumatica (PMR) will begin treatment with corticosteroids until the condition has resolved. You look over her records and it has been 2 years since her last physical examination and any laboratory or diagnostic tests as she relocated and had not yet identified a health-care provider. In prioritizing your management plan, your first orders should include: A. Recommending she increase her dietary intake of Calcium and VitaminD B. Ordering once a year bisphosphonate and a proton pumpinhibitor C. Participate in a fall preventionprogram D. Dual-energy x-ray (DEXA) scan and updatingimmunizations 9. Which of the following differential diagnosis for patients presenting with polymyalgia rheumatica (PMR) can be ruled out with a muscle biopsy? A. Parkinson’sdisease B. Polymyositis C. Late onset rheumatoidarthritis D. Giant CellArteritis 10. In reviewing laboratory results for patients suspected with polymyalgia rheumatica (PMR), you realize that there is no definitive test to diagnosis PRM, rather clinical response to treatment. Results you would expect to seeinclude: A. Elevated erythrocyte sedimentation rate (ESR) greater than 50mm perhour B. Elevated rheumatoid factor and anti-citrullinated protein antibodies (RFand ACPA) C. Decreased C-reactive protein level(CR-P) D. Elevated thyroid stimulating hormone(TSH) 11. Which of the following is themost appropriate laboratory test for monitoring gout therapy over the long-term? A. Erythrocyte sedimentation rate(ESR) B. Completer blood count(CBC) C. Serum uratelevel D. Serumalbumin 12. In providing health teaching related to dietary restrictions, the nurse practitioner should advise a patient with gout to avoid which of the following dietaryitems: A. Green leafyvegetables B. Beer, sausage, friedseafood C. Sugar D. Gluten and breaditems 13. The best method of verifying a diagnosis of gout in a joint is which of thefollowing: A. Radiographic examination of the joint with twoviews B. Ultrasound C. Palpation D. Joint aspiration and polarized-lightmicroscopy 14. The most appropriate first-line treatment for an acute gout flare is (assuming no kidney disease or elevated bleedingrisk): A. Indomethacin 50 mg TID for 2 days; then 25 mg TID for 3days B. Doxycycline 100 mg BID for 5days C. Prednisolone 35 mg QD for 5days D. Icetherapy 15. The nurse practitioner orders bilateral wrist X-rays on a 69-year-old gentleman complaining of pain in both wrists for the past 6 weeks not related to any known trauma. The nurse practitioner suspects elderly onset rheumatoid arthritis. The initial radiographic finding in a patient with elderly onset rheumatoid arthritis wouldbe: A. Symmetric joint spacenarrowing B. Soft tissueswelling C. Subluxations of thejoints D. Jointerosions 16. The nurse practitioner is examining the hands of a 55-year-old woman with rheumatoid arthritis and notes bilateral spindle shaped deformities on the middle interphalangeal joints. These are knownas: A. Haygarth’snodes B. Heberden’snodes C. Bouchard’snodes D. Benedictionhands 17. A 72-year-old female patient has been diagnosed with gout. She also has a long history of chronic congestive heart failure. The most likely contributing factor to the development of gout in this older femaleis: A. Leadintoxication B. Illegalwhiskey C. Binge-eating D. Thiazide diuretics 18. Which of the following statements about osteoarthritis istrue? A. It affects primarily weight-bearing joints B. It is a systemic inflammatoryillness C. The metacarpal phalangeal joints are commonlyinvolved D. Prolonged morning stiffness iscommon 19. In considering the specificity of laboratory data, the most reliable diagnostic test listed below would be: A. Elevated erythrocyte sedimentation rate (ESR) to rule outinflammation B. CBC to rule outinfection C. Antinuclear Antibody (ANA) test to rule out a collagendisease D. Synovial fluid analysis to differentiate between an infectious versusan inflammatoryinfusion 20. When examining the spine of an older adult you notice a curvature with a sharp angle. This is referred to asa: A. Gibbus B. Scoliosis C. Kyphosis D. Lordosis Chapter13.Central and PeripheralNervous SystemDisorders Chapter 13: Central and Peripheral Nervous System Disorders Multiple Choice Identify the choice that best completes the statement or answers the question. 1. An older adult patient is being evaluated following a stroke, which affected the anterior cerebral circulatory system. Which of the following signs/symptoms would be positive in the assessment of thispatient? A. Bilateral vision disturbance and/ordiplopia B. Dysarthria and speechdifficulties C. Disorders in behavior and incognition D. Motor and sensory problems on both sides of thebody 2. When assessing a patient who complains of a tremor, the nurse practitioner must differentiate essential tremor from the tremor of Parkinson’s disease. Which of the following findings are consistent with essentialtremor? B. Frontallobe C. Temporallobe D. Parietallobe 7. An elderly patient has had a CVA in the anterior cerebral circulatory system (frontal lobe). What symptoms are most likelyexpressed? A. Neglect of body and difficulty organizingspace B. Wernicke’s aphasia (difficulty understandingspeech) C. Disorders of behavior andcognition D. Bilateral motor and sensoryproblem 8. The most common neurological cause of seizures in an older adultis: A. Alzheimer’sdisease B. Multiple sclerosis C. Stroke D. Peripheralneuropathy 9. You are evaluating an elderly patient’s complaint of a new onset of “hand shaking” when he drinks from a cup. The patient is euthyroid and does not drink alcohol. Which of the following signs indicate that this tremoris most likely an essential tremor rather than a Parkinson’stremor? A. It is characteristic of “pill rolling” and occurs atrest B. It is a moderate amplitude tremor that occurs only withmovement/activity C. The tremor is also associated with slowedmovements D. The tremor is accompanied bydyskinesia 10. Mr. Andrews experienced a brief onset of right-sided weakness, slurred speech, and confusion yesterday. The symptoms have resolved. What should the nurse practitionerdo? A. Assure the patient that he will not experience the symptomsagain B. Identify modifiable cardiovascular riskfactors C. Do a thorough medication review and a CTscan D. Order a stat EEG and administer O2 bymask 11. An older male patient is experiencing acute onset of right-sided weakness, slurred speech, and confusion. What should the nurse practitioner dopromptly? A. Administer an aspirin bymouth B. Evaluate for stroke and arrange transport to the hospital right away C. Do a thorough medication review and stat bloodsugar D. Order an EKG and administer O2 by cannulaimmediately 12. An older adult female patient had a stroke. What symptoms are not usually expressed by patients who have had a vertebrobasilarstroke? A. Vertigo B. Ataxia C. Dysarthria D. Monocularblindness 13. When assessing an elderly client who reports a tremor, which assessment findings would be most reliable in identifying Parkinson’sdisease? A. Any presence oftremor B. Symptoms of slowed movement, unstable angina, andtremor C. Resting tremor, slow unsteady gait, and cogwheelresistance D. Cogwheel rigidity, bradykinesia, andamnesia 14. A 78-year-old man with Parkinson’s disease is being cared for in a nursing home. The nurses observe that he coughs at mealtime; he has the ability to still feed himself with adaptive equipment. He has had no aspirations. Oral exam is normal, except during his swallowing assessment you note there is slight delayed elicitation. You assess that he has only mild dysphagia. You recommend which of the following as the next step in hiscare? A. Consult gastroenterologist for g-tubedecision B. Consult speech pathologist for videofluoroscopy C. Provide a trial of foods of differingconsistency D. Require that he is fed all hismeals 15. Which of the following assessment findings is commonly noted in a client with advanced Parkinson’sdisease? A. Macrographia B. Micrographia C. Ataxic gait D. Increased armswing 16. A middle-aged patient has been diagnosed with Parkinson’s disease. What influences the nurse practitioner’s decision to begin pharmacological treatment for thispatient? A. Intentionaltremors B. Gait instability requiring use of acane C. Symptoms interfering with functionalability D. Medications initiated at first sign of unilateralinvolvement 17. An older male presents with incontinence, has a wide-based and irregular gait, and progressive dementia. Which of the following presents with these cardinalsigns? A. Parkinson’sdisease B. Normal pressurehydrocephalus C. Basilar arteryCVA D. Progressive supranuclearpalsy 18. In review of a nursing home patient’s chart, the nurse practitioner discovers that the neurology consult identified that the client has a homonymous hemianopsia. Which of the following statements accurately describes thesefindings? A. Partial loss of visual acuity in the ipsilateral peripheralfields B. Diplopia in the eye contralateral to the cerebral lesion C. Loss of vision in either the right or left halves of the visualfields D. Nystagmus in both eyes with asymmetricalmovement 19. The Mini-Cog is a short screening tool used to assess cognition. Which of the following statements pertaining to the test is a truestatement? A. The patient will be asked to repeat five words immediately following the directions by thepractitioner. B. The patient is asked to draw the hour and minute hands on a picture of an analog clock. C. A score of 0-2 is a positive screen fordementia. D. The patient is asked to recall five images from picture cards following the drawing of the clockhands. Chapter14.Endocrine,Metabolic,andNutritionalDisorders Multiple Choice Identify the choice that best completes the statement or answers the question. 1. An elderly client presents with a new onset of feeling her heart race and fatigue. An EKG reveals atrial fibrillation with rate >110. The patient also has a new fine tremor of both hands. Which of the following would the nurse practitionersuspect? A. Hypothyroidism B. Hyperthyroidism C. Congestive heartfailure D. Type 2 diabetesmellitus 2. A 62-year-old female complains of fatigue and lack of energy. Constipation has increased and the patient has gained ten pounds in the past 3 months. Depression is denied although the patient reports a lack of interest in usual hobbies. Vital signs are within normal limits and the patient’s skin is dry and cool. Which of the following must be included in thedifferential? A. Hyperthyroidism B. Hypothyroidism C. Hyperparathyroidism D. Grave’sdisease 3. Mrs. Black, an 87-year-old patient, has been taking 100 mcg of Synthroid for 10 years. She comes to your office for a routine follow-up, feeling well. Her heart rate is 90. Your first response isto: A. Increase theSynthroid B. OrderTSH C. Start abeta-blocker D. Order thyroid scan 4. Which patient is most likely to haveosteoporosis? A. An 80-year-old underweight male who smokes and has been on steroids for psoriasis B. A 90-year-old female with no family history of osteoporosis who is on hormone replacementtherapy C. A 68-year-old overweight female who drinks 1-2 drinksalcohol/day D. An 82-year-old female with a normal BMI takes calcium and performsweight- bearing exercisedaily 5. When evaluating the expected outcome for a hypothyroid elderly patient placed on levothyroxine, the nurse practitionerwill: A. Assess a weeklyTSH B. Assess the TSH in 4-6weeks C. Ask the patient if the symptoms have subsided and adjust dosageaccordingly D. Decrease the dosage should a cardiac eventoccur 6. A postmenopausal woman with osteoporosis is taking a bisphosphonate daily by mouth. What action information statement would indicate the patient understood the nurse practitioner’s instructions regarding thismedication? A. Takes medication at bedtime with a full glass ofwater B. Takes medication with a full glass of water when up in a.m. 30 minutes priorto other food andmedications C. Takes medication when up in a.m. with a glass of orange juice to increase absorption D. Takes medication sitting up and with a meal to avoid gastrointestinaldistress 7. The primary reason levothyroxine sodium is initiated at a low dose in an elderly patient with hypothyroidism is to prevent which of the following untowardeffects? A. Angina andarrhythmia B. Nausea anddiarrhea C. Confusion anddelirium D. Osteoporosis and muscleweakness 8. Six months ago an elderly patient was diagnosed with subclinical hypothyroidism. Today the patient returns and has a TSH of 11.0 and complains of fatigue. He has taken Synthroid 25 mcg daily as prescribed. What is the best course of action for the nursepractitioner? A. Assess further for a cause offatigue B. Double the dose ofSynthroid C. Discontinue theSynthroid D. Prescribe Liotrix (T3 & T4combination) 9. A fluoroquinolone (Ciprofloxin) is prescribed for a male patient with a UTI. What should the nurse practitioner teach the patient regarding taking thismedication? A. It must be taken on an emptystomach B. Its effectiveness is decreased by antacids, iron, or caffeineingestion C. It may cause a metallicaftertaste D. Its effectiveness is not a concern and it can be taken with anymedications 10. A patient has been prescribed metformin (Glucophage). One week later he returns with lowered blood sugars but complains of some loose stools during the week. How should the nurse practitioner respond? A. Discontinue the medicationimmediately B. Reassure the patient that this is an anticipated sideeffect C. Double the dosage of medication and have patient return in 1week D. Order a chem. 7 to check for lacticacidosis 11. Which of the following signs of hyperthyroidism commonly manifest in younger populations, but is notably lacking in theelderly? A. Weightgain B. Constipation C. Bradycardia D. Exophthalmos 12. A 60-year-old obese male client has type 2 diabetes mellitus and a lipid panel of TC = 250, HDL = 32, LDL = 165. The nurse practitioner teaches the patient about his modifiable cardiac risk factors, which include: A. Advancing age, diabetes, hyperlipidemia, and malegender B. Diabetes, obesity, andhyperlipidemia C. Hyperlipidemia, smoking, and family history of heartdisease D. Male with age > 45, diabetes mellitus, andhyperlipidemia 13. A diabetic patient presents with the complaint of right foot pain but denies any recent known injury. He states it has gotten progressively worse over the past few months. On exam, vibratory sense, as well as sensation tested with a monofilament, was abnormal. The patient’s foot is warm, edematous, and misshapen. The nurse practitioner suspects Charcot foot. What intervention isindicated? A. Warm soaks and return for follow-up in 1week B. Referral to a pain managementclinic C. Referral to anorthopedist D. Referral to a cardiologist for evaluation of peripheral vasculardisease 14. What is a sign of insulin resistance that can present in African Americanpatients? A. AcanthosisNigricans B. PsoriasisNigricans C. Seborrheic Nigricans D. Bullemic Nigricans 15. During a routine physical examination of a 62-year-old female patient, the nurse practitioner identifies xanthelasma around both his eyes. What is the significance of thisfinding? A. High potential for future blindness and requires immediatereferral B. None, normal variant of agingprocess C. Abnormal lipid metabolism requiring medicalmanagement D. Hereditary variant that is of no consequence but requires watchfulwaiting 16. Mr. White is 62 years old and has chronic kidney disease that has been relatively stable. He also has a history of hyperlipidemia, osteoarthritis, and hypertension. He is compliant with his medications, and his BP has been well controlled on a calcium channel blocker. His last lipid panel showed: TC = 201, HDL = 40, TG = 180, LDL = 98. He currently takes Crestor 20 mg daily. In the office today, his BP is 188/90, and his urine dip now shows significant proteinuria. He denies any changes in his dietary habits or medication regimen. What would be the best medication change for Mr. White at this point? A. No change—have him return in 4 weeks for a re-check of his blood pressureand urine B. Increase the dose of the calcium channel blocker for hishypertension C. Change the calcium channel blocker to anACE-I D. Increase the dose of his Crestor and have him return in 3 months for a re-check of hisBP 17. You are working as a nurse practitioner in the Fast Track of the emergency room. A 76-year-old male presents with left upper quadrant abdominal pain. There can be many conditions that present as left upper quadrant pain, but which of the following is least likely to cause pain in the left upper quadrant? A. Splenic abscess Leftpyelonephritis B. Splenicrupture C. Acute pancreatitis 18. Which is a “cardinal feature” of failure tothrive? A. Decline in toiletingability B. Gaitdisturbance C. Poor nutritionalstatus D. Spiritualdistress 19. Feeding gastrostomy tubes at end-of-life Alzheimer’s disease patients have been associatedwith: A. Prolongation oflife B. Aspirationalpneumonia C. Increase in skininfections D. Reversal of any clinical signs of failure tothrive 20. Which of the following nutritional indicators is not an indication of poor nutritional status in an older person? A. Albumin of < 3.5g/dl B. Body mass index of25 C. Total cholesterol < 150mg/dl D. Loss of 10% body weight in 180days Chapter 15. Hematologic and Immune System Disorders Multiple Choice Identify the choice that best completes the statement or answers the question. 1. Iron Deficiency Anemia (IDA) is classified as a microcytic, hypochromic anemia. This classification refers to which of the following laboratorydata? A. Hemoglobin andhematocrit B. Mean Corpuscular Volume (MCV) and Mean Corpuscular Hemoglobin(MCH) C. Serum ferritin and serumiron D. Total iron binding capacity and transferrinsaturation 2. Initial therapy for patients with IDAis: A. Bloodtransfusion B. Increasing dietary intake of green leafyvegetables C. Ferrous sulfate 325 mg orallybid-tid D. Parenteral administration ofVenofer 3. Mrs. G, a 70-year-old patient, presents to you with a hemoglobin of 9.4 and a decreased MCV/MCV. You diagnose her with IDA and start her on ferrous sulfate 325 mg PO tid. The next step in your work-up wouldbe: A. Send Mrs. G for a GIconsult B. Obtain hemoglobin one week after oraltherapy C. Schedule Mrs. G for an upper GIseries D. Obtain stool for occult blood 4. Despite adherence to oral iron therapy of 2 weeks, your elderly patient with IDA demonstrates a drop in his hemoglobin from 8.4 to 7.4. He is complaining of fatigue, dyspnea, and heart racing. You would change his therapy by which of thefollowing: A. Schedule patient for outpatient parenteral ironinfusion B. Switch to a different form of oraltherapy C. Schedule patient for outpatient bloodtransfusion D. Make no changes until evaluated by GIspecialist 5. You are prescribing oral iron therapy for a patient with IDA. In teaching your patient about iron therapy, all of the following instructions should be reviewedexcept: A. Iron is best taken on an empty stomach one hour beforemeals B. Meat, fish, poultry, beans, and green leafy vegetables are good dietary sources of iron C. Adding vitamin D daily enhances absorption ofiron D. Common GI side effects of iron therapy include constipation, nausea, andblack stools 6. When interpreting laboratory data, you would expect to see the following in a patient with Anemia of Chronic Disease(ACD): A. Hemoglobin <12 g/dl, Mean Corpuscular Volume (MCV) decreased, Mean Corpuscular Hemoglobin (MCH)decreased B. Hemoglobin >12 g/dl, Mean Corpuscular Volume (MCV) increased, Mean Corpuscular Hemoglobin (MCH)increased C. Hemoglobin <12 g/dl, Mean Corpuscular Volume (MCV) normal, Mean Corpuscular Hemoglobin (MCH)normal D. Hemoglobin >12 g/dl, Mean Corpuscular Volume (MCV) decreased, Mean Corpuscular Hemoglobin (MCH)increased 7. The pathophysiological hallmark of ACDis: A. Depleted ironstores B. Impaired ability to use ironstores C. Chronic uncorrectablebleeding D. Reduced intestinal absorption ofiron 8. The main focus of treatment of patients with ACDis: A. Replenishing ironstores B. Providing for adequate nutrition high iniron C. Management of the underlyingdisorder D. Administration of monthly vitamin B12injections 9. In addition to the CBC with differential, which of the following laboratory tests is considered to be most useful in diagnosing ACD andIDA? A. Serumiron B. Total iron bindingcapacity C. Transferrinsaturation D. Serumferritin 10. Education of patient and family regarding ACD includes discussion of all of the followingexcept: A. Early prevention of chronic conditions through healthy lifestylemeasures B. Importance of adherence to the treatment plan for management ofchronic conditions C. Explaining the ACD is mainly attributed to the agingprocess D. Importance of regular follow-up to monitor responses totreatments 11. Symptoms in the initial HIV infection include all of the followingexcept: A. Sorethroat B. Fever C. Weightloss D. Headache 12. The primary mode of HIV transmission in the U.S.is: A. Bloodtransfusion B. Men having sex with men C. Heterosexualcontact D. Needle sharing 13. In the older adult, which group comprises the highest rate ofHIV/AIDS? A. African Americanwomen B. African Americanmen C. Hispanic women D. Hispanicmen 14. Contributing factors in HIV development in the older adult include all of the followingexcept: A. Older adults are less likely to betested B. Healthcare providers do not routinely ask older adults about HIV risks C. Older adults are less likely to usecondoms D. Older adults are at low risk to contractHIV 15. Immune system changes that render older adults more susceptible to contracting HIV include all of the followingexcept: A. Hyper-responsive Tcells B. Age-related thymicinvolution C. Depletion of naïve CD4cells D. Decline in B cellfunction Chapter 16. Psychosocial Disorders Multiple Choice Identify the choice that best completes the statement or answers the question. 1. The prevalence of depression in nursing homeresidentsis greater than adults living in the community. A. 1-2times B. 2-3times C. 3-4times D. 5times 2. The majority of depressed older adults remain untreated becauseof: A. Misdiagnosis B. Socialstigma C. Environmentalbarriers D. All of theabove 3. Symptoms of depression distinct to the elderlyinclude: A. Flataffect B. Loss of pleasure in usualactivities C. Appetite and weightdisturbances D. Lack ofemotions 4. The justification for ordering a CBC, TSH, and serum B12 for a patient you suspect may have clinical depressionis: A. To determine the cause ofsadness B. Because of overlapping symptoms with anemia, thyroid dysfunction,and nutritionaldeficiencies 11. In late stages of dementia, a phenomenon called “sun downing” occurs, in which cognitive disturbances tendto: A. Improve as the day goeson B. Become worse toward theevening C. Fluctuate during the course of theday D. Peakmid-day 12. Of the following, which one is the most useful clinical evaluation tool to assist in the diagnosis of dementia? A. Folstein’s Mini-Mental Status Exam(MMSE) B. St. Louis University Mental Status Exam(SLUMS) C. Montreal Cognitive Assessment(MoCA) D. Geriatric Depression Scale(GDS) 13. The cornerstone of pharmacotherapy in treating Alzheimer’s diseaseis: A. Cholinesteraseinhibitors B. NMDA receptorantagonist C. Psychotropicmedications D. Anxiolytics 14. The comorbid psychiatric problem with the highest frequency in dementiais: A. Anxiety B. Depression C. Agitation andaggression D. Psychosis 15. When treating depression associated with dementia, which of the following would be a poor choice and should not beprescribed? A. Fluoxetine B. Desipramine C. Amitriptyline D. Mirtazapine Chapter 17.Polypharmacy MULTIPLE CHOICE 1. The nurse plans to closely monitor an older adult client who is receiving multiple drugs for evidence of adequate excretion of the medications. Which two major organs affecting drug clearance from the body should be monitored when an older adult client is receiving multipledrugs? a. Kidneys andlungs b. Kidneys andpancreas c. Liver andpancreas d. Liver and kidneys ANS:D The older adult client may experience a decrease in hepatic enzyme production, hepatic blood flow, and total liver function. These decreases cause a reduction in drug metabolism. A decrease in renal blood flow and decrease in glomerular filtration rate of 40% to 50% can also occur. 2. The nurse is awarethatincreased may affect the absorption ofmedications. a. gastricmotility b. alkaline gastricsecretion c. intestinal emptyingtime d. peristalsis ANS: B An increase in alkaline gastric secretions may affect the absorption of medications, because gastric motility, gastric emptying time, and peristalsis are all decreased with increased alkaline gastric secretions. 3. The older adult client is prescribed a drug that is excreted through the urine. The nurse anticipates that which laboratory test will be prescribed to evaluate renal function before administration of the medication? a. Blood ureanitrogen b. Serumalbumin c. Serumelectrolytes d. White blood cellcount ANS: A Drug dosages are adjusted according to the older adults weight, adipose tissue, laboratory results (e.g., serum protein, electrolytes, liver enzymes, blood urea nitrogen, creatinine), and current health problems. 4. The nurse recognizes that polypharmacy is more likely to occur in an older adult client because the olderclient: a. has difficulty maintaining a list of currentmedications. b. experiences changes in visualcapability. c. experiences alterations in mentalcapacity. d. may obtain prescribed drugs from variousproviders. ANS: D Polypharmacy is the prescription and administration of many drugs during the same period. This is more likely with the older client, who may see various healthcare providers to manage the health concerns that may accompany aging. 5. The diuretic hydrochlorothiazide (HCTZ; HydroDIURIL) is usually prescribed for the olderadult in a lower dose. The nurse recognizes that this is an attempt to prevent the older adult from experiencinga(n): a. increase in potassiumloss. b. decrease in sodiumloss. c. decrease in blood sugarlevels. d. increase in red and white blood cellcount. ANS: A 6. The nurse notes that Cimetidine has been prescribed for anolder adult client. The nurses highest priority would be tocall: a. the physician. b. the pharmacist. c. the nursingsupervisor. d. PoisonControl. ANS: A Cimetidine is not recommended for the older adult because of its side effects and multiple potential drug interactions. Famotidine, nizatidine, and ranitidine may be prescribed for the geriatric client instead of cimetidine. 7. An older adult client says that he has difficulty removing the cap from his medication bottle. He says, Thats why I dont always take my medication. The nurse should suggest thathe: a. ask a neighbor to help him remove the bottlecap. b. ask the pharmacist to put the drug in a nonchildproofcontainer. c. have a family member visit daily to prepare hismedications. d. ask the healthcare provider not to prescribe drugs that come in childproof bottles. ANS: B Childproof caps may be difficult to remove for older adults with arthritis or decreased strength or motor function. 8. A client is demonstrating signs and symptoms of disorientation. Which question by the nurse would be appropriate, related to the clients medicationuse? a. Are you taking any newmedications? b. Do you take medications with a full glass ofwater? c. Do your medications make youconstipated? d. Have you been diagnosed withdementia? ANS: A A new medication may be associated with changes in sensorium or other behavioral characteristics. This should be evaluated. 9. The nurse is caring for an older adult client and a middle-aged adult client. The nurse anticipates that the medication doses for the older adultwillbe those for the middle-agedadult. a. the sameas b. lessthan c. slightly morethan d. twice as muchas ANS: B Because of changes in metabolism and excretion, doses are generally decreased to avoid accumulation and toxicity. 10. An older adult client is ordered to receive digoxin (Lanoxin). The client has decreased renal function. Which condition could indicate digoxintoxicity? a. Elevated bloodpressure b. Decreased bloodpressure c. Heart rate greater than 100 beats perminute d. Heart rate less than 60 beats perminute ANS: D Digoxin slows and strengthens the heart. Toxicity may be manifested by bradycardia. 11. A client takes ibuprofen to deal with the pain of arthritis. The client complains ofgastrointestinal symptoms. Which is an appropriate strategy for the nurse to teach theclient? a. Take the medication on an emptystomach. b. Do not take the medication if it has sideeffects. c. Try to take an antacid 1 hour before thedose. d. You must take the medicationanyway. ANS: C An antacid may decrease the gastrointestinal side effects of the NSAID. It may also impair absorption, so it must be evaluated for effectiveness. 12. A nurse is administering medication to an older adult client. The nurse is aware that the clients half-life is longer than that of middle-aged adults. What nursing intervention is indicated by this premise? a. Provide higher doses to achieve therapeuticeffects. b. Assess the client for adversereactions. c. Monitor the client for signs ofaccumulation. d. Provide educationto the client on drugreactions. ANS: C Because older adults may have less efficient medication elimination, monitoring for accumulation is an important component of nursing care. 13. The nurse is caring for an older adult client who complains that she has to take multiple medications at various times throughout the day. What is the most appropriate nursing intervention for the nurse to implement with thisclient? a. Encourage family members or friends to monitor drugregimen. b. Explain the purpose, drug action, and importance ofmedication. c. Develop a chart indicating times to takedrugs. d. Provide time for questions; reinforce with writteninformation. ANS: C The nurse should help the client develop a chart indicating times to take drugs. Space should be provided to mark each drug taken. An organizer or calendar can be used to mark days and weeks. 14. The physician is recommending a benzodiazepine medication for an older adult client who has previously been treated with Valium. The nurse recognizes that which medication would be most appropriate for thisclient? a. Librium b. Dalmane c. Ativan d. Equanil ANS: C A short-acting benzodiazepine, such as Ativan, would be preferable to any of the other drugs to avoid prolonged sedation and addiction. 15. Which older adult client is most likely to experience digoxintoxicity? a. 72-year-old man who is also experiencinghyperkalemia b. 74-year-old woman who is also experiencinghypokalemia c. 66-year-old woman who is also experiencinghypercalcemia d. 62-year-old woman who is also experiencinghypocalcemia ANS: B Hypokalemia enhances the effect of digoxin, thus increasing the possibility of toxicity. Chapter18.ChronicIllnessandtheAdvancedPracticeRegisteredNurse (APRN) Multiple Choice Identify the choice that best completes the statement or answers the question. 1. All of the following statements are true about chronic disease/illnessexcept: A. Chronic disease is defined as a condition that requires both modification by the patient along with interaction with theprovider B. The meaning of chronic illness includes the experience of thepatient and family andprovider C. Chronic illness is reversible if diagnosed and treatedearly D. Chronic conditions are those that last a year orlonger 2. The highest number of people with multiple chronic conditions are those that are: A. Over age 85 B. Diagnosed with type 2 diabetes C. African American women over age 65 D. Diagnosed with COPD 3. Long durations of a chronic illness that are most commonly associated in both women and men are: A. Heart disease and obesity B. Diabetes and COPD C. Arthritis and dementia D. Dyslipidemia and eye disease 4. The percentage of non-institutionalized elderly over age 75 with limitations in activity due to a chronic condition is: A.25% B. Nearly 50% C. Over 75% D. Less than 15% 5. Which of the following statements are true? A. Most Medicare participants have a single care provider B. Chronic kidney disease patients have better outcomes due to the dialysis benefit C. Nearly half of Medicare participants have five or more chronic diseases D. Nearly half of Medicare participants have three or more chronic diseases 6. Which statement about chronic mental disorders is false? A. The numbers are projected to increase in the next decade B. Individuals with mental health problems actually have a decreased risk ofmedical problems C. The number of older adults with addiction problems is projected to increase inthe next decade D. Nearly half of individuals with dementia are not diagnosed prior to hospitalization 7. All of the following criteria define frailty except: A. Unintentional weight loss >10 pounds in the past year B. Slow walking speed C. Stooped posture D. Self-reported exhaustion 8. All of the following are health consequences of obesity except: A. Mortality of aging B. Hypertension C. Coronary arterydisease D. Sleep apnea 9. Evidence-based clinical practice guidelines may have limited applicability in the older population because: A. They often are diseasespecific B. They often have complex comorbidconditions C. Both A andB D. None of the above evidence-based clinical practice guidelines are alwaysthe standard 10. Inter-professional care is distinguished from other models of team-based care inthat: A. Independent providers shareinformation B. Expert advice is shared from one provider toanother C. Different disciplines work under oneleader D. Shared leadership and accountability is a primaryfocus 11. All of the following statements about the Chronic Care Model are trueexcept: A. It was developed with Robert Wood Johnson Foundationfunding B. It focuses exclusively on a self-managementmodel C. It is an evidence-based policy response designed to meet the needs of the chronicallyill D. It directs quality improvement and system change for patients with chronicdisease 12. The legislation signed in March 2010 with provisions for addressing chronic diseasewas: A. Accountable Care OrganizationAct B. Independence at HomeAct C. Patient Protection and Affordable CareAct D. Patient Centered Medical HomeAct 13. Reported outcome measures for the Patient Centered Medical Home include all of the following except: A. Emergency roomuse B. Hospitalizations C. Patient/familysatisfaction D. Number of primary carevisits 14. Transitional care is best describedas: A. A set of actions to ensure the coordination and continuity of careacross sites/settings B. The care received in transit from one site of care toanother C. A discharge-planningmodel D. Long-term acute care that provides the transition from hospital to long-term careor home Chapter 19. Palliative Care and End-of-Life Care Multiple Choice Identify the choice that best completes the statement or answers the question. 1. Hospice care differs from palliative care inthat: A. It is not covered byinsurance B. Supports patients and families through both the dying and the bereavement process C. It cannot be provided in the nursinghome D. The majority of those admitted to hospice die within 7days 2. Evidence reflects the primary obstacle to implementing palliative care in the long-term care setting include all of the followingexcept: A. Inadequate communication between decisionmakers B. Failure to recognize futiletreatments C. Lack of advancedirectives D. Lack of sufficientstaff 3. The most prevalent symptom in end-of-life care includes all of the followingexcept: A. Lower extremityweakness B. Pain C. Dyspnea D. Delirium 4. Pain at the end of life is most often due to all of the following except: A. Musculoskeletaldisorders B. Headache C. Cancerpain D. Neuropathic pain 5. The strongest level of evidence reflects the absolute contraindication for NSAID use exists with: A. Chronic kidneydisease B. Peptic ulcerdisease C. Heartdisease D. Liverdisease 6. The drug specific for severe opioid-induced constipation is: A. Lactulose B. Ducolax C. Mineraloil D. Methylnaltrexone 7. Pharmacological interventions for dyspnea include all of the following except: A. Antitussives B. Inhaledanesthetics C. Sedatives D. Anxiolytics 8. Delirium is typically characterized by all of the following except: A. Inattention B. Hyperactive level of psychomotoractivity C. Disorganizedthinking D. Altered level ofconsciousness 9. The first step in treating delirium is to: A. Give low-dose Haldol if the patient haspsychosis B. Identify thecause C. Provide realityorientation D. Use side rails and/or wrist restraints to keep the patientsafe 10. The majority of patients enrolled in hospice care die: A. In a nursinghome B. In thehospital C. In an inpatient hospicefacility D. Athome 11. A drug that can be used to treat two very common symptoms in a dying patient (pain and dyspnea) is: A. Morphine B. Methadone C. Gabapentin D. Lorazepam 12. The tasks of grieving include all of the following except: A. Acknowledge the reality ofdeath B. Work through the pain ofgrief C. Begin todisengage D. Restructure relationships 13. The best description of complicated grief is: A. Chronic, delayed, exaggerated, masked, ordisenfranchised B. Experience of shock during notification of thedeath C. When grief is actually experienced before the death of a lovedone D. A physical illness develops soon after death of a loved one 14. All of the following statements are true about interventions in working with the bereaved except: A. Allow the active expression ofgrief B. There is strong evidence behind recommendedinterventions C. Staff attending memorial services support thefamily D. Provide both emotional and spiritualsupport 15. The highest level of evidence to support interventions at the end of life is with: A. Opioids for paincontrol B. Hyocsyamine for respiratorysecretions C. Stimulant laxatives for treatingconstipation D. Opioids fordyspnea 16. The highest level of evidence with the use of adjuvant analgesics is with: A. Tricyclic antidepressants avoided due to high adverseevents B. Therapeutic trials before discontinuingdrugs C. Patient with fibromyalgia are candidates for adjuvantanalgesics D. Neuropathic pain patients are candidates for adjuvantanalgesia [Show More]
Last updated: 1 month ago
Preview 1 out of 71 pages
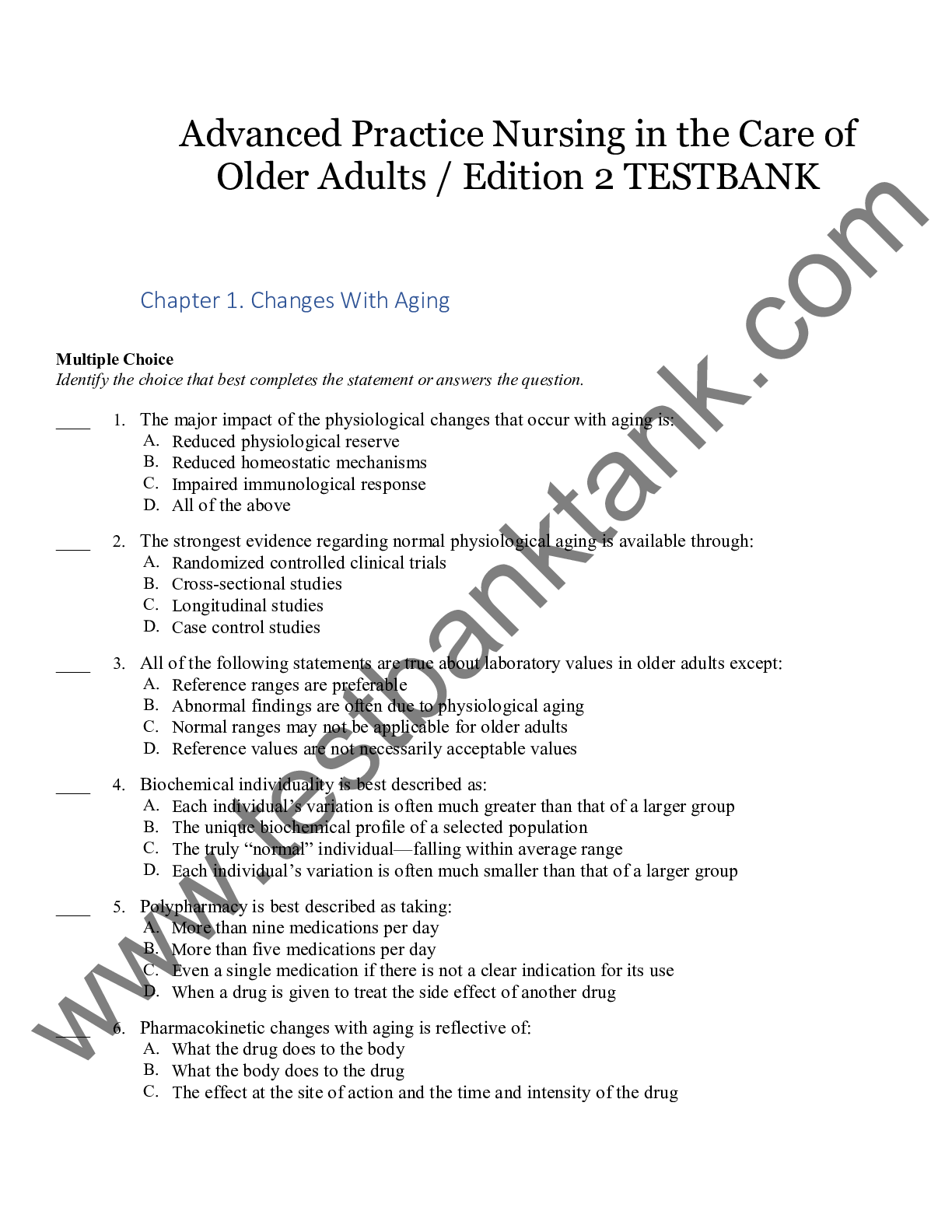
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
May 26, 2020
Number of pages
71
Written in
Additional information
This document has been written for:
Uploaded
May 26, 2020
Downloads
1
Views
91

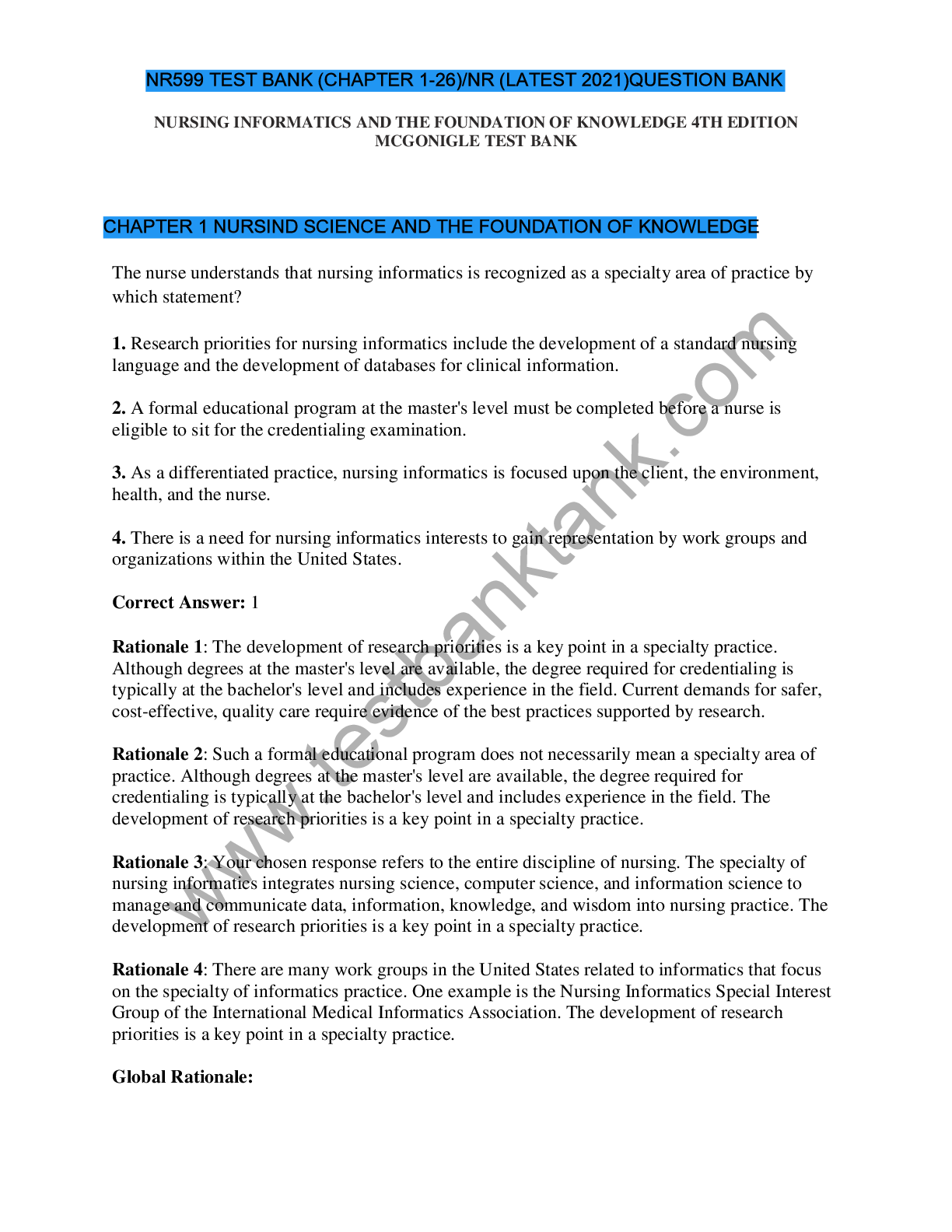
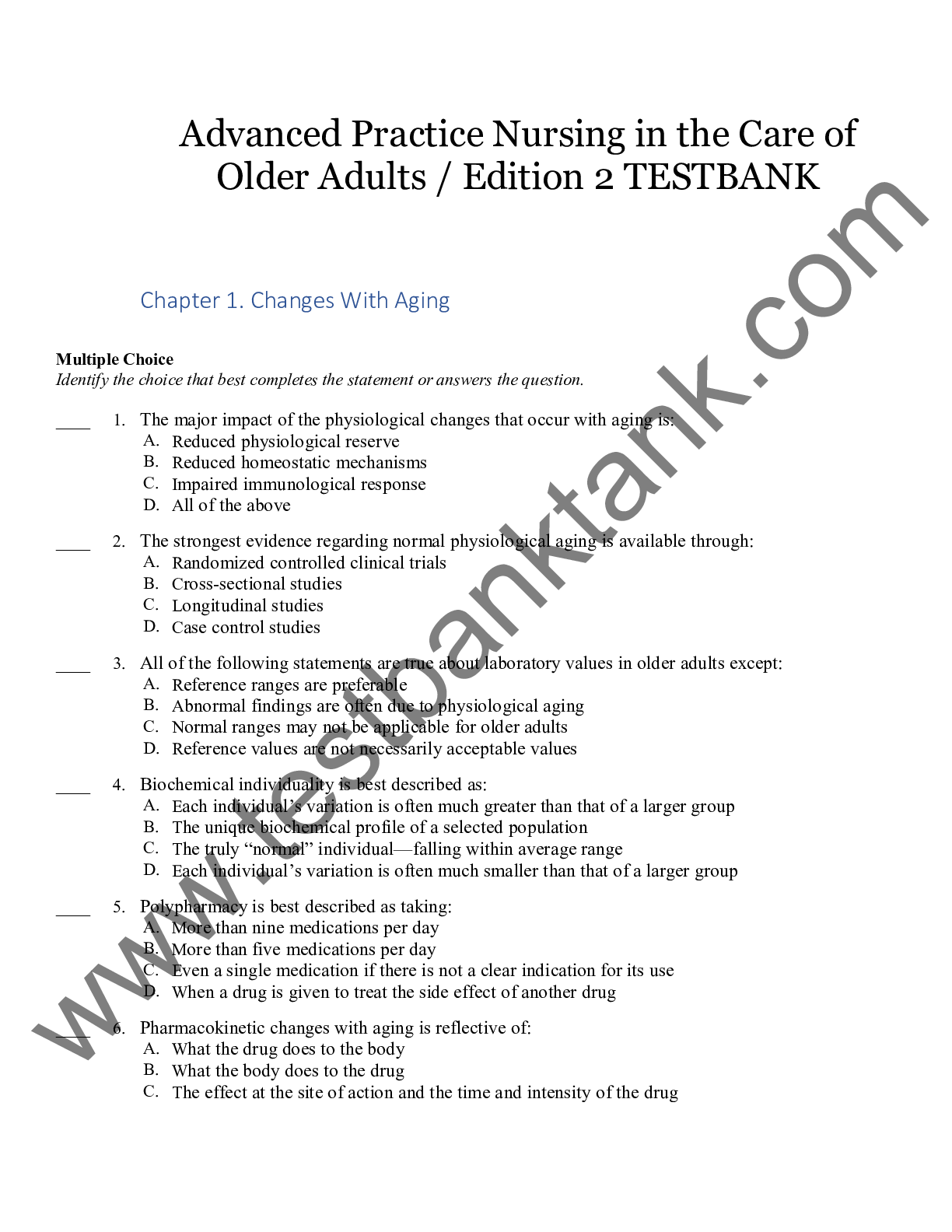
.png)


 Securities Institute of America - Wiley series 63 exam review 2016 + test bank_ the uniform securities state law examination-John Wiley and Sons (2016).png)



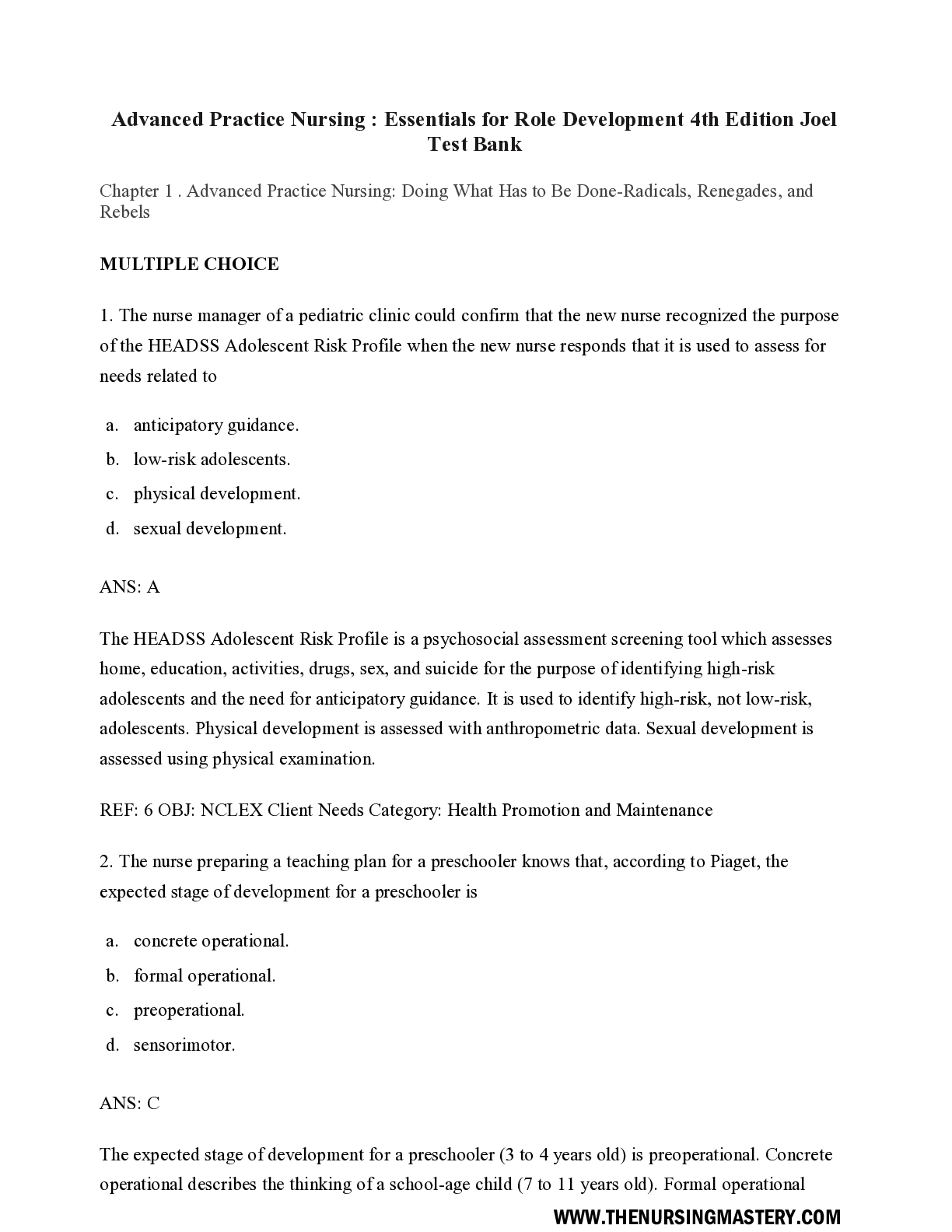
.png)