*NURSING > MED-SURG EXAM > NURS 4325 Med Surg Guide for Exam #3 Perioperative, Seizures, Parkinson’s Disease, Care of the mus (All)
NURS 4325 Med Surg Guide for Exam #3 Perioperative, Seizures, Parkinson’s Disease, Care of the musculoskeletal patient, HIV&AIDS
Document Content and Description Below
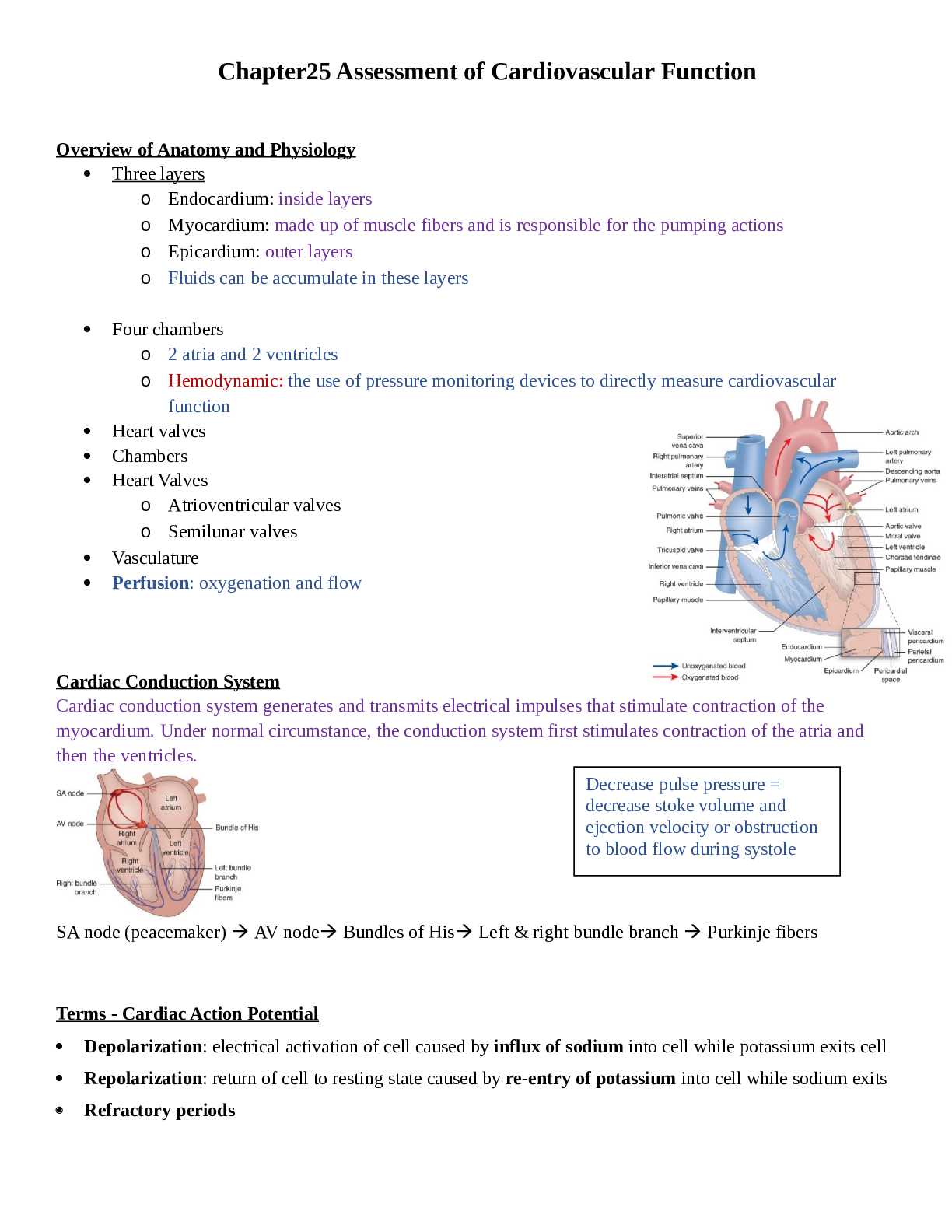
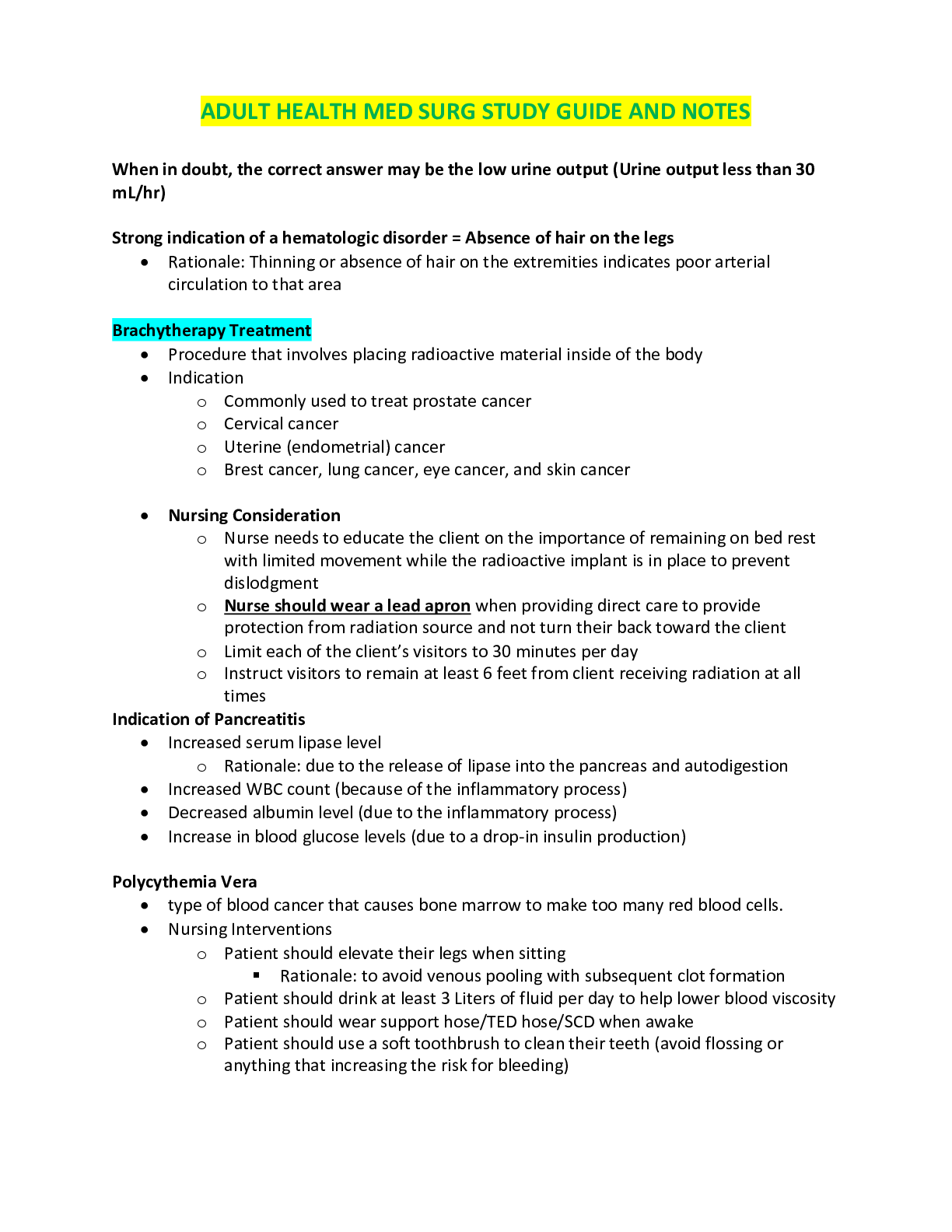
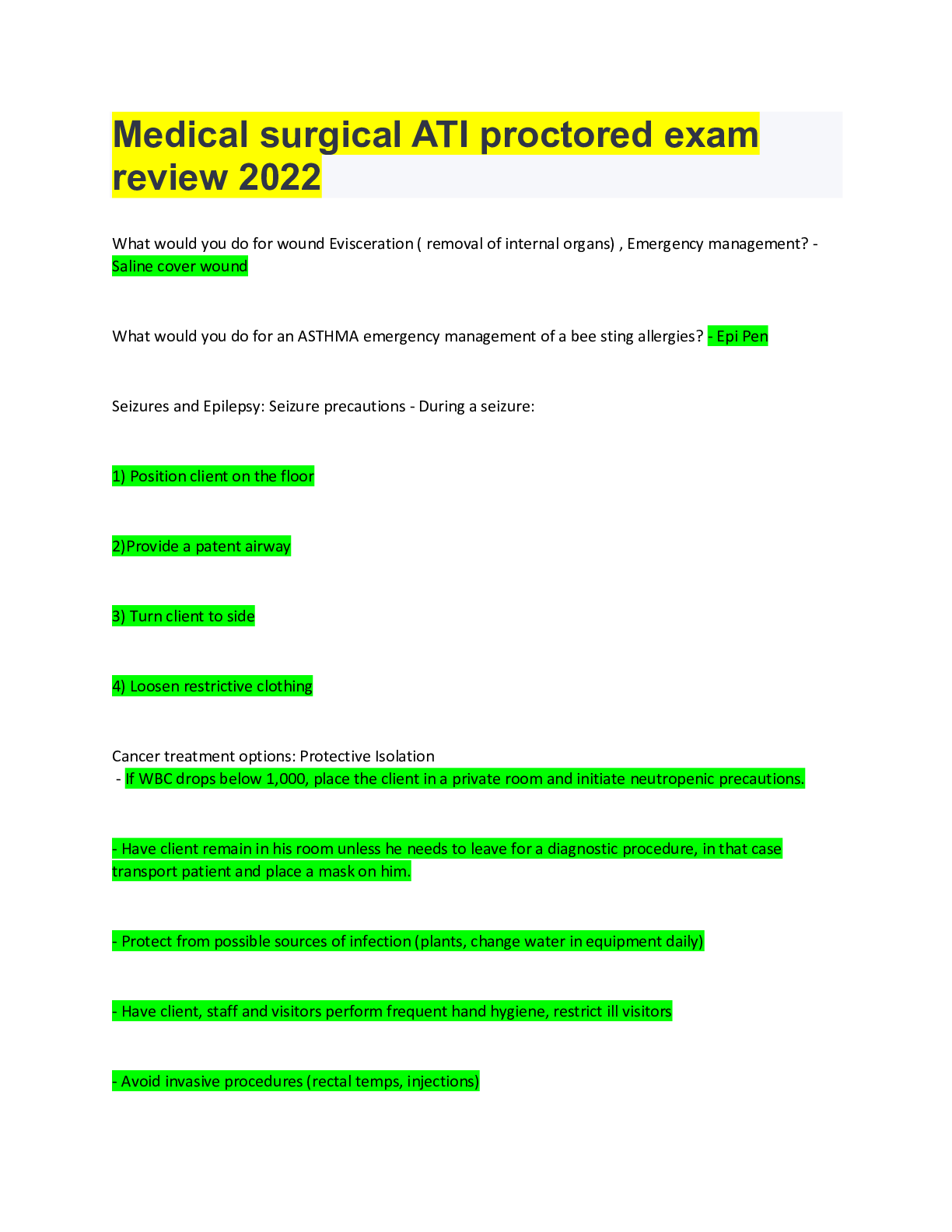
Med Surg Guide for Exam #3 Perioperative Perioperative: concentrate mostly on Pre-op and post-op Pre-op: importance of getting a good history, medication reconciliation, what puts someone at p... ost-op risks (ex: diabetes and obese patient; at risk for poor wound healing/wound issues), what medications may increase bleeding Intra-op: safety focus (not covering any anesthetics) Post-op: post-op care for the orthopedic patient (kind of intertwines with musculoskeletal), prevention of DVT, prevention of pneumonia, getting patient up and moving as quickly as possible, incentive spirometry, cough and deep breathing, remember if they develop fever within the first 24-48 hours it usually is related to a respiratory problem and if they have a wound infection, fever usually occurs at about 72 hours post-op. From lecture notes: Peri-operative nursing care Pre-OP: Goals for pre-op assessment (this assessment can begin a few days prior to when surgery is scheduled and continue the day of surgery. It all depends on the situation): Patient's psychological status- look at coping strategies, how the patient is looking at the surgery, what plan do they have in place, do they need a driver home, do they need rehab, any negative past experiences, etc. Any past history that may increase operative risk factors (weight, PMHx, smoke, allergies, what meds they take (prescription/OTC), make sure they haven't eaten past midnight, etc.) To establish baseline (to compare pre-op to post-ob labs) CBC, type and cross, electrolytes, make sure they are not taking a medicine like Coumadin (increased risk of bleeding) have to stop a week prior to surgery ID and document surgical site and/or procedure Medications- both prescription and OTC (ASA) Identify cultural and ethnic factors (Jehovah Witness) Check level of knowledge of: procedure Why is pre-operative teaching done? To increase patient satisfaction, decrease operative fear, anxiety and stress, decrease development of complications (early ambulation to prevent constipation & control pain before ambulating, coughing and deep breathing), decreased length of stay, decreased recovery time, FOCUS IS ON PATIENT SAFETY, make sure to DOCUMENT all patient teaching. Remember the nurse wants to get a complete history – very detailed – this should include areas like medication history, surgical history- have they had problems with anesthesia before – or problems post op too. Why do you want baseline -labs and vitals – this allows us to compare it to the post op numbers. Ask about allergies. Legal consent: must be informed consent, patient must be of sound mind, it is the physician’s responsibility (the RN can witness the signature and clarify information). It is not the role of the nurse to explain the procedure (RN can clarify points). Make sure the form is accurate – signatures in place. It is important to note that the consent is INFORMED. That means that the patient is of sound mind and knows what it is going on. As a proxy, a family member can give consent for a patient that is not able to consent for themselves (ex: a patient with dementia). It must be proved legally that the person signing the informed consent is a proxy. The physician is responsible for the person who is performing the procedure. The RN can witness and clarify information. If English is second language, must provide a hospital interpreter for the patient (not a family member). Pre-operative checklist: use this the day of surgery, goes through everything that you need to know and make sure of: dentures out, contacts off, nail polish removed, ID band and allergy band are on, client teaching has been completed, consent form signed, NPO, patient is in gown, no jewelry-bands taped, voiding prior to transfer, vitals within 4 hours of surgery of 30 minutes after pre-op, make sure preoperative lab work is on the chart, recognize abnormal lab values (notify physician right away), skin prep, history of aspirin, antidepressant, steroid or NSAID use, pre-op medications given, side rails up after pre-op. Common labs done- CBC, ELECTROLYTES, TYPE AND CROSS MATCH, BUN AND CREAT , PREGNANCY TEST (IF INDICATED), CLOTTING STUDIES – PTT, INR, - remember if they are on anticoagulants they will be discontinued pre-op for a period of time. During pre-op experience, we talk about identifying risk factors, and there are risk factors that patients are going to have questions about (ex: what about infection, anemia, loss of volume-hypovolemia, electrolyte imbalance, DVT), so do teaching involving those pieces. Teach them how to cough and deep breathe and how to use incentive spirometry. Also looking for risk factors that could cause surgical complications (Ex: if a person has chronic respiratory disease, that could potentially cause problems postoperatively, smoking patients, or even patients with heart failure (fluids are given during surgery, so may have to alter diuretics or monitor I&Os very carefully and auscultate breath sounds). Diabetes patients are definitely at risk. They have elevated blood sugars, so the stress of surgery will increase the blood sugar even more and they have increased risk of delayed healing. Obesity patients put more pressure on the incision and are at increased risk for wound evisceration or dehiscence. Older adults have potential for post-operative complications due to their age related changes. Patients should understand that when they are on scheduled medications, they should be aware of the medications that they should take and those that they should not. For example, the BLOOD THINNERS! Reinforce post op teaching- Turn Cough and Deep Breathe – incentive spirometry – post op diet – usual recovery plan- pain control – DVT prevention interventions- demonstrate splinting when coughing. If pre-op teaching occurs prior to surgery ( say a week or two before ) – make sure patient understands what medications they can take( e.g. holding aspirin for a week prior to surgery) , when they should be NPO, refrain from smoking. Intra-OP: SAFETY is the focus!!!!!!! Go through several safety checks to make sure that we have the right patient and the right procedure, etc. Safety includes transferring the patient, positioning on the table, hazards of anesthesia (gasses are flammable)as well as just protecting the patient from general surgery. Prevent complications – proper positioning – making sure the right procedure is being done on the correct patient! Everybody has a role and it is to protect the patient. Intra-op safety time-out- created by the safety organizations to protect patients. Other nursing activities: o Room preparation: ensure privacy, prevention of infection, safety o Transferring patient to the OR suite, safety measures when transferring patient (LOOK IT UP)*** o Take a surgical time out: Before induction of anesthesia ask patient to confirm name, birth date, operative procedure and site and consent. Compare the hospital ID number with the patient's own ID band and chart. During surgery: o Maintain sterile field o Ensure sponge, instrument count is correct (make sure nothing is left inside) o Position patient to ensure correct alignment o Prevent chemical injury o Safety with electrical equipment o Safely administering medications o Monitoring vital signs o Monitoring blood loss and urine output ATI- has great summary of patient centered care, the labs done, and breaks up the responsibilities very well, so it would be a great idea to look this up. Post-op: Will first discuss the PACU- where you provide care for the patient until the patient has recovered from the effects of anesthesia. Purpose is to get the patient awake and see less and less of the effects of anesthesia. Patient has resumption of motor and sensory function, is oriented, has stable VS, shows no evidence of hemorrhage or other complications of surgery. It is vital to perform frequent skilled assessment of patient. What occurs in the PACU: There is a scoring system used to assist the nurse in determining when the patient is ready for transfer, the Aldrete score-monitors the recovery from anesthesia (5 factors-, grades activity, consciousness, respirations, O2 sats and circulation assessment (ACROC)). The patient is typically ready for discharge at about a score of 8-10. Patient will have stable vital signs, able to breathe on own, no evidence of bleeding and return of reflexes (ex: gag). There is minimal to absent nausea and vomiting, wound drainage is minimal to moderate and urine output is also about 30 ml/hr or greater. PACU environment: Beds, other equipment; there are three phases: Phase I, Phase II, and Phase III. The PACU nurse is always assessing the patient; airway, circulation, vitals, positioning, stimulate pt. to wake them up from anesthesia. Assess airway (#1), respirations, cardiovascular function, surgical site, function of CNS, IVs, all tubes and equipment (looking at what is going in and coming out of the patient). Reassess VS, patient status every 15 minutes or more frequently as needed. Assess how the patient is waking up from anesthesia, assess n/v, pain, monitor I&O (how much urine is coming out), assess wound dressing (for drainage) – LOC. Transfer report, to another unit or discharge patient to home. Example interventions: If patient is complaining of nausea, turn the over on side to prevent aspiration. If person is receiving supplemental oxygen (monitoring O2 sats) and when returning to the bedside the patient is sound asleep, NAD, and the O2 sat is 88-89%. Stimulate the patient; make them take a good deep breath and see if the sats return, before upping the oxygen. The primary nursing goal in the immediate postoperative period is maintenance of pulmonary function and prevention of hypoxemia and hypercapnia. Importance of this: positioning (head of bed up), listening to lung sounds, administering oxygen as needed, monitoring O2 sats continuously, looking at circulation, checking mucus membranes, lips and nail beds for any signs of cyanosis, monitoring fluid and electrolyte balances, frequent vital signs at least every 15 minutes, assess for movement, LOC, etc. Discharge from the PACU: Direct discharge (going home directly from recovery room) planning includes written and verbal instructions about medication, wound care, activity restrictions, diet restrictions and complications (when to call the doctor; signs and symptoms of infection, signs of DVT, etc.). They need someone to drive them home and make sure that the caregiver is there to listen to the discharge instructions. If discharged to the unit, the patient should report with stable vital signs, recovered from anesthesia (mostly) and the nurse should have given SBAR report to the receiving unit. When the patient is coming to the unit, what do you do? Get room ready – IV pole and pump, suction equipment, oxygen, emesis basin, tissues, etc. The nurses focus includes ventilation (airway), Hemodynamic stability- check vitals q15m x 1 hr: then q30m x 2h, incisional pain, surgical site, nausea and vomiting, neuro status and thermoregulation – check temp q4h x 24h. When the person comes to the unit, the nursing process is what you follow. -Assessment is critical! Make sure that we start aggressively with the airway management, and that means coughing and deep breathing at least every hour, incentive spirometer every 1-2 hours, sometimes you can have the patient do it more frequently, especially if they are awake (it can’t hurt). – -Turn and position the patient at least every 2 hours and get the patient moving as soon as possible. Pain control is important and you do not want to let the pain get out of control (needs to be controlled so patient will move and do cough and deep breathing, ambulation, etc.). Remember that if they have an abdominal or sternal incision, we have to teach them how to splint the incision, to protect the incision and provide some comfort while performing exercises. -Check I&0’s, check bladder (if they had catheter, is the bladder distended), are they retaining urine? (Bladder scanner if they are voiding small amounts). When was catheter discontinued? – -Assess bowel sounds and maintain NPO if indicated. If NG tube is present, need to assess that as well (make sure functioning and hooked up to correct amount of suction, etc.). Also know when advancing diet, start with clear liquids and assess patient to see if they are tolerating it. -Diet is usually advanced when bowel sounds are present and patient is passing gas. Want to include interventions that prevent DVT (ambulation, SCDs, compression stockings), and watch incisions and drains (drains should be emptied every shift and document the amount and type of drainage). Vitamin C helps with wound healing. How to prevent complications? ATI does a nice job summarizing complications. PREVENTION IS KEY! Complications include: Pulmonary embolism: chest pain, dyspnea, increased resp rate, tachycardia, increased anxiety, diaphoresis, decreased orientation, decreased blood pressure, blood gas changes DVT: patient may be on a low-molecular weight heparin like a Lovenox, avoid pressure behind the knee, or pillow or blanket because it can decrease blood flow and put constriction on blood vessels. Avoid dangling legs for a long period of time and keep the patient well hydrated. Hypovolemic shock: decreased urine, low BP, weak pulse, cool and clammy, restlessness, increased bleeding, increased thirst, decreased CVP Infection: redness, purulent drainage, fever, tachycardia, leukocytosis; respiratory infection occurs about 24-48 hours post op, and wound infection presents about 72 hours post op. Dehiscence: separation of incision Evisceration: evidence of bowel through incision and increase in pain; apply sterile wet dressing on top of it and notifying the doctor stat and the patient will going to the OR. Gastric dilation: nausea and vomiting, abdominal distention (can lead to dehiscence); assess NG tube for patency Paralytic ileus: decreased bowel sounds, no stool or flatus, nausea, vomiting, abdominal distention, abdominal tenderness (prevent with ambulation) Atelectasis: dyspnea, tachypnea, decreased breath sounds, asymmetrical chest movement, tachycardia, increased restlessness Pneumonia: rapid respirations, shallow respirations, fever, wet breath sounds, asymmetrical chest movement, productive cough, hypoxia, tachycardia, leukocytosis, Urinary retention: Unable to void 8-10 hours post op, palpable bladder, frequent small amount (voiding), pain suprapubic area Seizures Seizures: focus on nursing management (what are we going to do for the person who comes in with a seizure?); if a person comes in with a seizure, the most important thing is to protect them, we want to make sure that they are safe. SAFETY!!- -Side lying (to protect airway), loosen anything around the neck, cushion head, remove glasses or anything on face. This is done to prevent injury. Remember as nurses we have to time the seizure, document the movements, and get other information from the patient after the seizure is over, like how long did it take them to wake up, etc. Remember that patients can have a pre-ictal feeling/aura prior to a seizure (this helps understanding triggers). Remember seizures to NEVER PUT ANYTHING IN the patient’s mouth during a seizure (ex: tongue blade, may break off into mouth from biting)! Sometimes the patient may have an oral airway (rarely placed to protect the airway), but this is very different than a tongue blade. Listen to lecture and you will have all of the pieces you need. From lecture notes: Seizures are Abnormal episodes of motor, sensory, autonomic, or psychic activity (or a combination of these) resulting from a sudden, abnormal, uncontrolled electrical discharge from cerebral neurons. Classification: Partial seizures: begin in one part of the brain • Simple partial: consciousness remains intact • Complex partial: impairment of consciousness • Generalized seizure: involve whole brain • Status Epilepticus: Literally a continuous state of seizure • Epilepsy: syndromes of unprovoked, reoccurring seizures • Causes of seizures: • Hypertension • Central nervous system infections • Metabolic and toxic conditions • Brain tumor • Drug and alcohol withdrawal • Cerebrovascular disease • Hypoxemia • Fever (childhood) • Head injury • Allergies • Assessment: Assess verbal response and orientation, alertness, motor responses (follow commands and use of extremities), respiratory status. Also assess eye signs (pupil size), Reflexes, Postures and Glasgow Coma Scale • Glasgow Coma Scale-Three Components (it is objective and standardized) • Eye Opening • Best Verbal Response • Best Motor Response Posturing: Abnormal posturing includes flexor posturing (decorticate=to the Cord), extensor posturing (decerebrate=Lots of E’s) and flaccid (“wet noodle”) Pupils: Really important assessment. Have to assess PERRLA. Do the pupils react slowly or briskly? Dilated pupil (compressed CN III); bilateral dilated, fixed (ominous sign; not a good sign); Pinpoint pupils (pons damage or drugs) Interventions: • A major nursing goal is to compensate for the patient's loss of protective reflexes and to assume responsibility for total patient care. Protection also includes maintaining the patient’s dignity and privacy. • Maintaining an airway o Frequent monitoring of respiratory status, including auscultation of lung sounds o Positioning to promote accumulation of secretions and prevent obstruction of upper airway—head of bed (HOB) elevated 30 degrees; lateral or semi prone position o Suctioning, oral hygiene, and CPT (if aspirated) Stages of seizures/interventions: • Preictal (prior to seizure): 50% of all patients have an aura. • Ictal (when the seizure occurs): epileptic cry (simultaneous contractions of the diaphragm and chest muscles causes cry); loss of consciousness (LOC). o Observe movement of head and eyes, muscle rigidity, progression of seizure, and the duration and LOC, incontinence of stool and urine. o Protect from injury; turn to side and loosen clothes. o DO NOT put anything in mouth • Postictal (after seizure): does not remember seizure, confused, hard to arouse from sleep. o Assess airway, breathing, vital signs, neurologic checks; keep on side and clean up the patient; reorient the patient as the patient awakens. o Collaborative complications include: Respiratory distress or failure, Pneumonia, Aspiration and Pressure ulcer Plan of care for a patient experiencing a seizure: Observation and documentation of patient signs and symptoms before, during, and after seizure (timing & writing details including onset, body part affected, LOC, muscle tone, pupils, cyanosis, altered salivation, incontinence.) Nursing actions during seizure for patient safety and protection (Safety includes maintaining airway, protecting patient from harm, DO NOT restrain, DO NOT place objects inside the mouth and observe and record event.) After seizure care to prevent complications Refer to Chart 66-4 Women’s Health and AEDs (anti-epileptic drugs): Folate supplementation is recommended to women of childbearing age. Reduce risk of birth defects due to AEDs. AEDs can diminish effectiveness of oral contraceptives. AED can triple failure rate of oral contraceptives. Other things to incorporate in teaching: Discuss that the patient should wear a medical alert bracelet. The patient is not allowed to drive. The patient should be aware of the medication that they are on and if they require blood draws. How do they take the medication? Does it interfere with another medication? Parkinson’s Disease Parkinson’s disease: gradual onset disease, usually starts off with minor tremors. The biggest thing with theses populations is safety (shuffling gait problems). As the disease progresses, the patients may have difficulty with swallowing, so we have to monitor them carefully for that. Think about patient safety, supporting them and trying to make them gain or keep their independence as long as possible. Mask like expression makes it hard to assess them sometimes. From lecture notes: Onset of Parkinson’s Disease is usually gradual, after 50 (slowly progressive). Three cardinal symptoms include; -- Tremor – gradual onset usually unilateral but can differ from person to person. Rigidity-stiffness of the arms, legs, face, and posture are common. Early in the disease, the patient may complain of shoulder pain due to rigidity and bradykinesia. Other symptoms include mask-like blank expression, stooped posture and pill-rolling tremors, possible mental deterioration, depression, shuffling & propulsive gait. It rarely occurs in black population. Tremors: commonly in the hands and arm. Pill rolling motion with the fingers. Occurs most often at rest. May involve diaphragm, tongue, lips and jaw. Increases with stress. Muscle Rigidity: Increased resistance to passive movement, Cog wheel, jerky slow movement Bradykinesia: loss of normal arm swing while walking, decreased blinking of the eyelids, loss of ability to swallow, blank expression and difficulty initiating movement. Parkinson’s is associated with decreased levels of dopamine caused by destruction of cells in the substantia nigra in the basal ganglia; this affects the neurotransmission of impulses. Manifestations include tremor, rigidity, bradykinesia, postural instability, depression and other psychiatric changes, dementia, autonomic symptoms, sleep disturbances Simplification of pathophysiology: Too little dopamine o Imbalance of excitatory acetylcholine o Dopamine pathway damage Imbalance of extrapyramidal tracts o Cause muscle movement disturbance o Leads to tremors, rigidity, postural changes, bradykinesia Medical management • Pharmacologic treatment (levodopa/cardopa, etc.) • Surgical procedures (lobectomy, stimulator, etc.) • Other therapies (PT/Speech Therapist/OT, etc.) Assessment of patient with Parkinson’s disease: Focus on the degree of disability and function of the patient including ADLs, IADLS, and cognitive function. Medications and responses to medications. Emotional responses and individual coping. Family processes and coping. Home care and education needs. Fall risk assessment. Manifestations and potential complications related to the specific disorder. Goals may include: improved functional ability • maintaining independence in ADLs • achieving adequate bowel elimination • attaining and maintaining acceptable nutritional status • achieving effective communication • developing positive individual and family coping skills • • Improving mobility in Parkinson’s Disease: • Daily program of exercise • ROM exercises • Postural exercises • Consultation with physical therapy • Walking techniques for safety and balance (may need assistive devices) • Frequent rest periods • Proper shoes • Use of assistive devices Interventions include: • Support of coping • Set achievable, realistic goals • Encourage socialization, recreation, and independence • Planned programs of activity • Support groups and referral to supportive services: counselors, social workers, home care • Enhancing self-care ability • Encourage, educate, and support independence • Environmental modifications (work with OT) • Use of assistive and adaptive devices • Consultation with occupational therapy HIV/AIDS HIV: When it is first diagnosed, of course it is not a good diagnosis, so it is very stressful. There are certain tests that will tell for sure that the patient has HIV (Western Blot). Even if an EIA tests positive, they will always obtain a Western blot for confirmation. !!!Know the symptoms: --most common is flu-like symptoms and fatigue, but others can be present (fever, weight loss, pharyngitis, mouth sores, thrush, esophageal sores, myalgias, liver and spleen enlargement, malaise, headache, neuropathy, lymphadenopathy, skin rash, nausea and vomiting). Starting medications is a big routine for them and education is important for medications as well (not going to ask anything specific about the medications themselves, if there are any questions about medications, it will be more generic about focusing on teaching). From lecture notes: The Treatment has improved steadily since the advent of combination medication therapy. Survival rates have increased dramatically in the past 20 years. 1.2 million people in the United States are living with HIV; one in 7 are unaware they are infected, according to the CDC. There are about 50,000 new infections per year. Number of new HIV infections, globally, declined 18% over the past decade. Gay, bisexual, young African American men are at higher risk. There are 5 body fluids that transmit HIV: blood, seminal fluid, vaginal secretions, amniotic fluid, breast milk. Casual contact does not cause transmission. Breaks in skin or mucosa increase risk. List 3 major risk factors that are associated with HIV infection and AIDS. • Having unprotected sex with infected individuals (both male and female; vaginal anal or oral.) Multiple sex partners. • Infants born to mothers with HIV infection and/or who are breastfed by HIV infected mothers • People who received organ transplants, HIV-infected blood or blood products (especially between 1978 and 1985). Another risk factors associated with HIV/Aids includes sharing infected injection drug equipment. Also older adults (underdiagnosed due to age group) are at risk because some of them may be sexually active and do not believe in using condoms. They also tend to have broken skin more susceptible to fluid exchange can occur. Females going through menopause have vaginal dryness and thinning of the vaginal wall, so it increases susceptibility if they are having sex with infected individuals. Prevention of disease: Standard precautions Safer sex practices and safer behaviors o Abstain from sharing sexual fluids o Reduce the number of sexual partners to one o Always use latex condoms and if allergic to latex, use nonlatex condoms. Do not share drug injection equipment Blood screening and treatment of blood products Maintaining up to date immunizations. Health Care Provider Prevention: Hand hygiene, Personal protective equipment (PPE), Soiled patient care equipment handling, Environmental control, Textiles and laundry, Needles and other sharps and Patient resuscitation. Treatment: Post exposure prophylaxis & Vaccination; go to employee health and get blood drawn (also get consent from other person); you’re screened and then you are followed up. Where does HIV make its viral home in the body, what is seroconversion, and describe the clinical manifestations with initial acute infection? • T lymphocyte and CD 4 cell • After infection – 1-3 week period called acute retroviral syndrome • Seroconversion (when HIV specific antibodies develop): Mononucleosis-like symptoms of fever, swollen lymph glands, sore throat, headache, malaise, nausea, muscle and joint pain, diarrhea or a diffuse rash. Window Period: the time period between infection and development of antibodies. What does the EIA blood test detect and what is the confirmatory test for HIV infection? • Antibodies are detected, resulting in positive results and marking the end of the window period • EIA (enzyme immunoassay) is a variant of a test called, ELISA (enzyme-linked imunosorbent ASSAY which identifies antibodies directed specifically against HIV • WESTERN BLOT is a confirmatory test for a positive EIA • WESTERN BLOT confirms infection [Show More]
Last updated: 1 year ago
Preview 1 out of 49 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Apr 05, 2021
Number of pages
49
Written in
Additional information
This document has been written for:
Uploaded
Apr 05, 2021
Downloads
0
Views
47