Anatomy > MED-SURG EXAM > MED SURG_EXAM ONE STUDY GUIDE |ANATOMY 2086_MED SURG_EXAM ONE STUDY GUIDE (All)
MED SURG_EXAM ONE STUDY GUIDE |ANATOMY 2086_MED SURG_EXAM ONE STUDY GUIDE
Document Content and Description Below
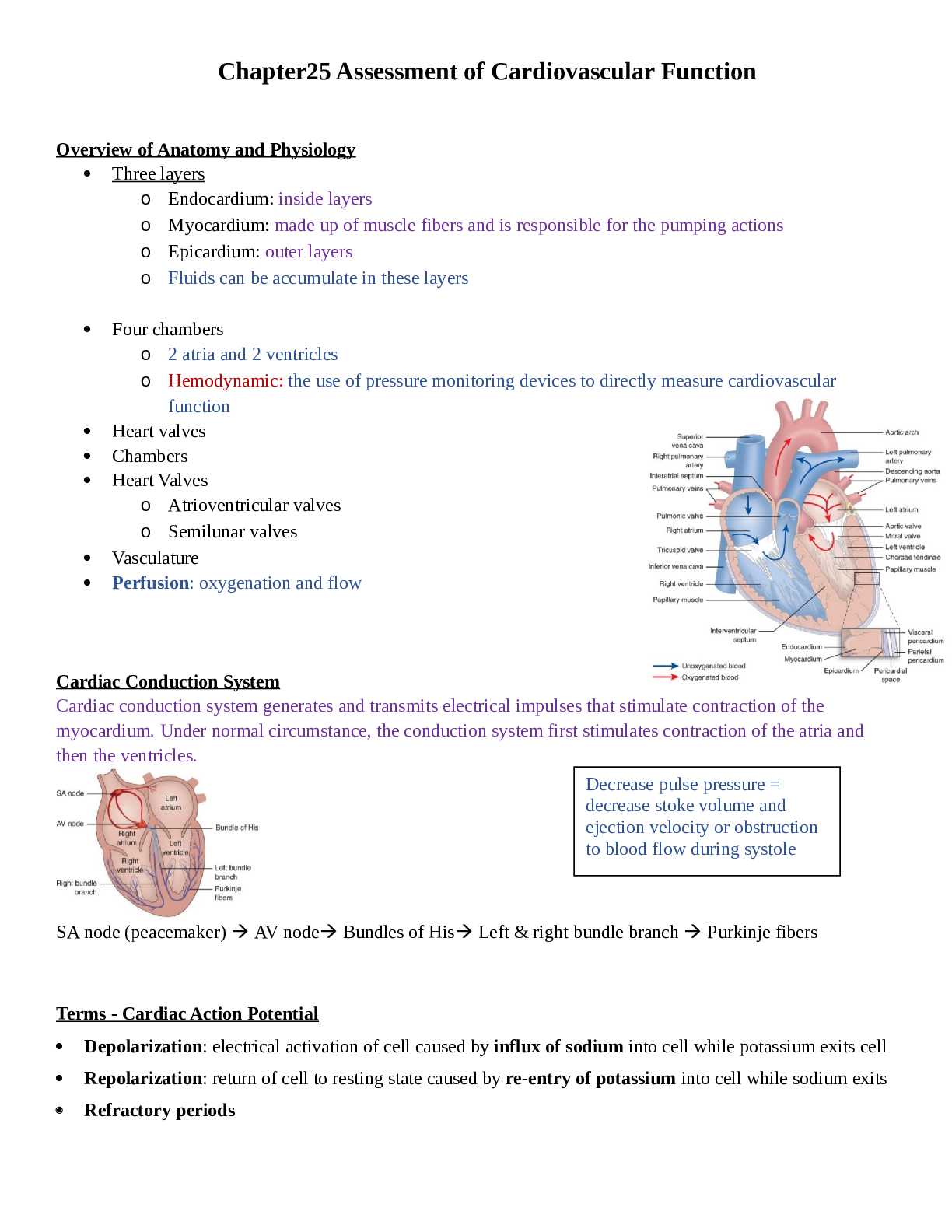
Chapter25 Assessment of Cardiovascular Function Overview of Anatomy and Physiology Three layers o Endocardium: inside layers o Myocardium: made up of muscle fibers and is responsible for the p... umping actions o Epicardium: outer layers o Fluids can be accumulate in these layers Four chambers o 2 atria and 2 ventricles o Hemodynamic: the use of pressure monitoring devices to directly measure cardiovascular function Heart valves Chambers Heart Valves o Atrioventricular valves o Semilunar valves Vasculature Perfusion: oxygenation and flow Cardiac Conduction System Cardiac conduction system generates and transmits electrical impulses that stimulate contraction of the myocardium. Under normal circumstance, the conduction system first stimulates contraction of the atria and then the ventricles. SA node (peacemaker) AV node Bundles of His Left & right bundle branch Purkinje fibers Terms - Cardiac Action Potential Depolarization: electrical activation of cell caused by influx of sodium into cell while potassium exits cell Repolarization: return of cell to resting state caused by re-entry of potassium into cell while sodium exits Refractory periods Decrease pulse pressure = decrease stoke volume and ejection velocity or obstruction to blood flow during systole o Myocardial cells must completely repolarize before they can depolarize again. During the repolarization process. Two phases o Effective refractory period: the cells is completely unresponsive to any electrical stimulus; phase in which cells are incapable of depolarizing Corresponds with the time in phase 0 to the middle of phase 3 of the action potential o Relative refractory period: phase in which cells require stronger-than-normal stimulus to depolarize Corresponds with the short time at the end of phase 3 Cardiac Action Potential 23.4: Cardiac action potential of a fasting-response Purkinje fiber. The arrows indicate the approximate time and direction of movement of each ion influencing membrane potential. Ca++ movement out of the cell is not well defined but is thought to occur during phase 4. Great Vessel and Heart Chamber Pressures 25.2: great vessel and chamber pressures. Pressures are identified in millimeters of mercury (mm Hg) as mean pressure or systolic or systolic over diastolic pressure. Cardiac Hemodynamics CO= HR X SV Hemodynamics Terms - Cardiac Output Stroke volume: amount of blood ejected with each heartbeat o Average resting stoke volume is about 60 to 130 mL Cardiac output: amount of blood pumped by ventricle in liters per minute o In a resting adult is 4 to 6 L/min normally Preload: degree of stretch of cardiac muscle fibers at end of diastole o Preload is referred to as left ventricular o End of diastole is the period when filling volume in the ventricles is the highest and the degree of stretch of the muscle fibers is the greatest o Less blood return to the heart reduced preload o IV fluids will increase preload Contractility: ability of cardiac muscle to shorten in response to electrical impulse o Increased contractility result in increased stroke volume o Contractility is depressed by acidosis, hypoxemia, and certain medication such as beta blockers o Enhanced SNS, such as digoxin, epinephrine increase contractility Afterload: resistance to ejection of blood from ventricle o Arterial vasodilation decrease afterload increase stroke volume o Arterial vasoconstriction increase afterload decrease stoke volume Ejection fraction: percent of end diastolic volume ejected with each heartbeat o Ejection fraction of normal left ventricle is 55% to 65% HR SV Cardiac Output Stro k e Volu m e Preload Afterload Contractility o Used as a measure of myocardial contractility o Measured by echocardiogram *Low heart rate will affect the cardiac output *Stroke volume, if anything is affecting contractility the heart is not contracting, or heart is not stretching/pumping will affect the cardiac output heart is not perfuse b/c CO is low Age-Related Changes of the cardiac System Atria Left ventricles o Myocardial thickening (hypertrophy) stiff and less compliant, and progressive decline cardiac output = fatigue, decrease exercise tolerance, s4 may be present o Left side heart failure- auscultating lungs sounds is cracks. Possible wheeze and gurgles Valves o Thickening or rigidly of the AV valves abnormal blood flow across the valves during cardiac cycle = murmurs may be present Conduction system o Loss function slow heart rate Sympathetic nervous system Aorta and arteries Baroreceptor response Health History Chief complaint History of Present Illness Past medical, surgical history Past family history Past social history Home medications Nutrition Allergies Physical Assessment General appearance o Evaluate the patient’s LOC & mental status o Changes may be attributed to inadequate perfusion of the brain from a compromised cardiac output of thromboembolic event (stroke) o Observe for signs of distress (pain, discomfort, SOB, anxiety) o Measure height and weight Skin and extremities o Skin color, temperature, and texture for problems with arterial or venous circulation Blood pressure Arterial pulses Jugular venous pulsations (JVD) o Right side heart failure fluid overload o What does patient taking to improve fluid overload? Heart inspection and auscultation General assessment Any deviations 偏差 from the normal? o Do you have any change in activity tolerance? o Heart as a pump o Atrial/ventricular filling volumes o Cardiac output o Compensatory mechanisms Did they change their shoes because their legs are swollen? What position are they are laying to sleep? Tripod position: patient falling a sleep on a chair - one sits or stands leaning forward and supporting the upper body with hands on the knees or on another surface. *right sided heart failure= Ascites, hepatojugular reflex, distention Most Common Clinical Manifestations Chest pain Dyspnea Peripheral edema, weight gain, abdominal distention Palpitations Fatigue Dizziness, syncope, changes in level of consciousness o Why would a patient be dizzy? Cardio output and perfusion issues o LOC- due lack of oxygen to the brain Chest Pain Chest pain and chest discomfort are common symptoms that may be caused by a number of cardiac and noncardiac problems summarizes the characteristics and patterns of common of chest pain or discomfort. Identify quantity of pain (0-10 SCALE) Identify location of pain Identify quality of pain Radiation of pain o Chest pain can radiate to left side, jaw, epigastrium, back, shoulder Associated signs/symptoms (diaphoresis or nausea) Duration of pain o Severity or duration of chest pain does not predict the seriousness of its cause. For example, when asked to rate pain using a 0 to 10 scale, patient with esophageal spasm may rate as 10. In contrast, patient with MI, which is a potentially life-threatening event, may report 4 to 6. Assess for other cardiac conditions Assess for other significant conditions (see p. 663-664) o Pneumonia, pulmonary embolism o Hiatal hernia, GERD Doctor will order labs or endoscopy on the patient to rules out GERD instead of heart attack o Costochondritis o Vascular Assessment Medications o Aspirin, a nonprescription medication is an important antithrombotic therapy for secondary prevention in patients recovering from ACS (acute chest syndrome) Nutrition o Dietary modification, exercise, weight loss, and careful monitoring are important strategies for managing three major cardiovascular risk factors: hyperlipidemia, hypertension, and diabetes. o Diet restriction: sodium, fat, cholesterol, or calories. o Height + weight o BMI (assessment for obesity) o Lab result: glucose, glycosylated Hb (diabetes), cholesterol, HDL, LDL, triglycerides o Patient food habits and culture preference Elimination o Typical bowel and bladder habits need to be identified o Nocturia (awakening at night to urinate) is common with HF patient o Vagal maneuvers: try to slow down the fast heart rate by stimulate the vagal nerve increase pressure to the baroreceptor to slow down HR [Show More]
Last updated: 1 year ago
Preview 1 out of 75 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
May 01, 2021
Number of pages
75
Written in
Additional information
This document has been written for:
Uploaded
May 01, 2021
Downloads
0
Views
63