*NURSING > EXAM REVIEW > NUR 611 exam 1 review - Questions and Answers Maryville University (All)
NUR 611 exam 1 review - Questions and Answers Maryville University
Document Content and Description Below
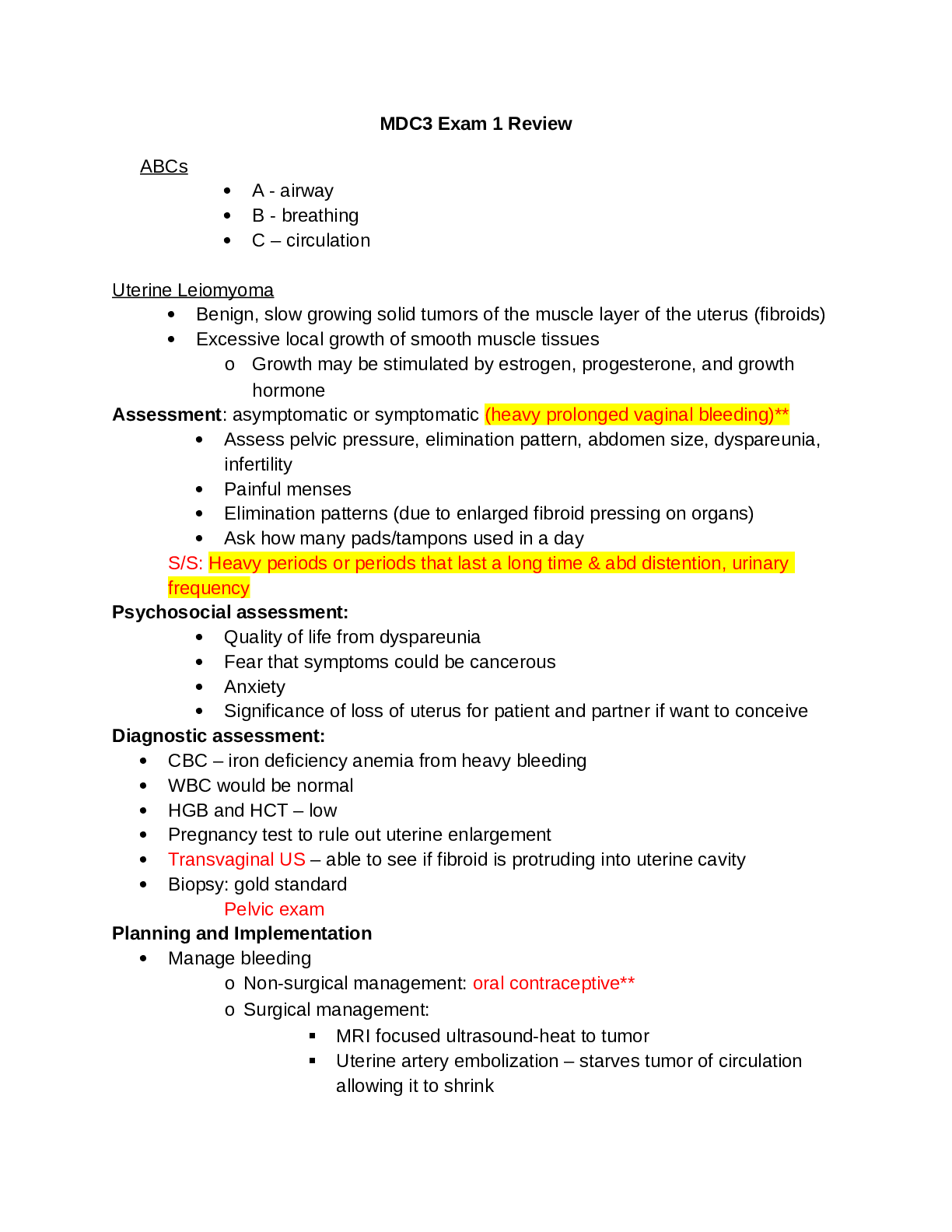
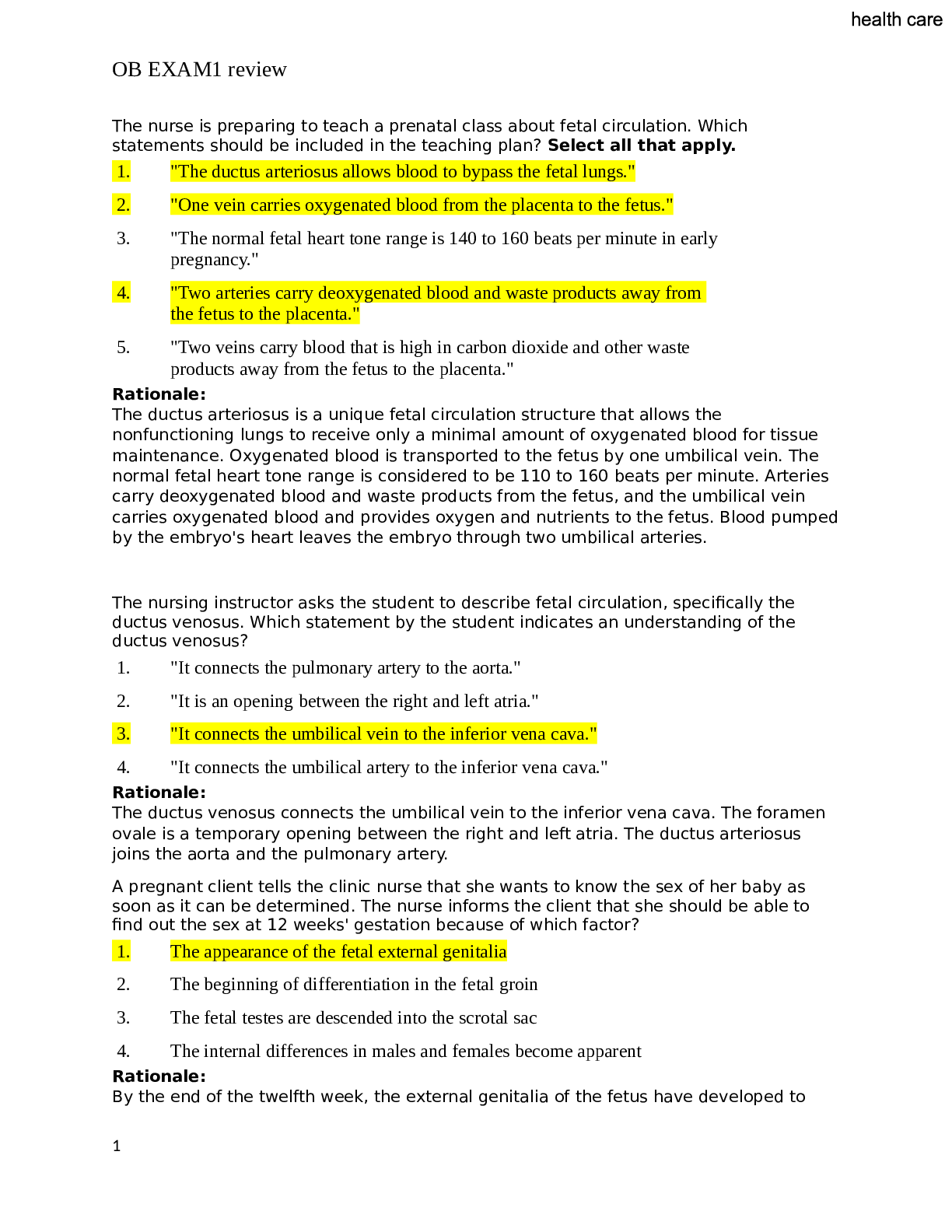
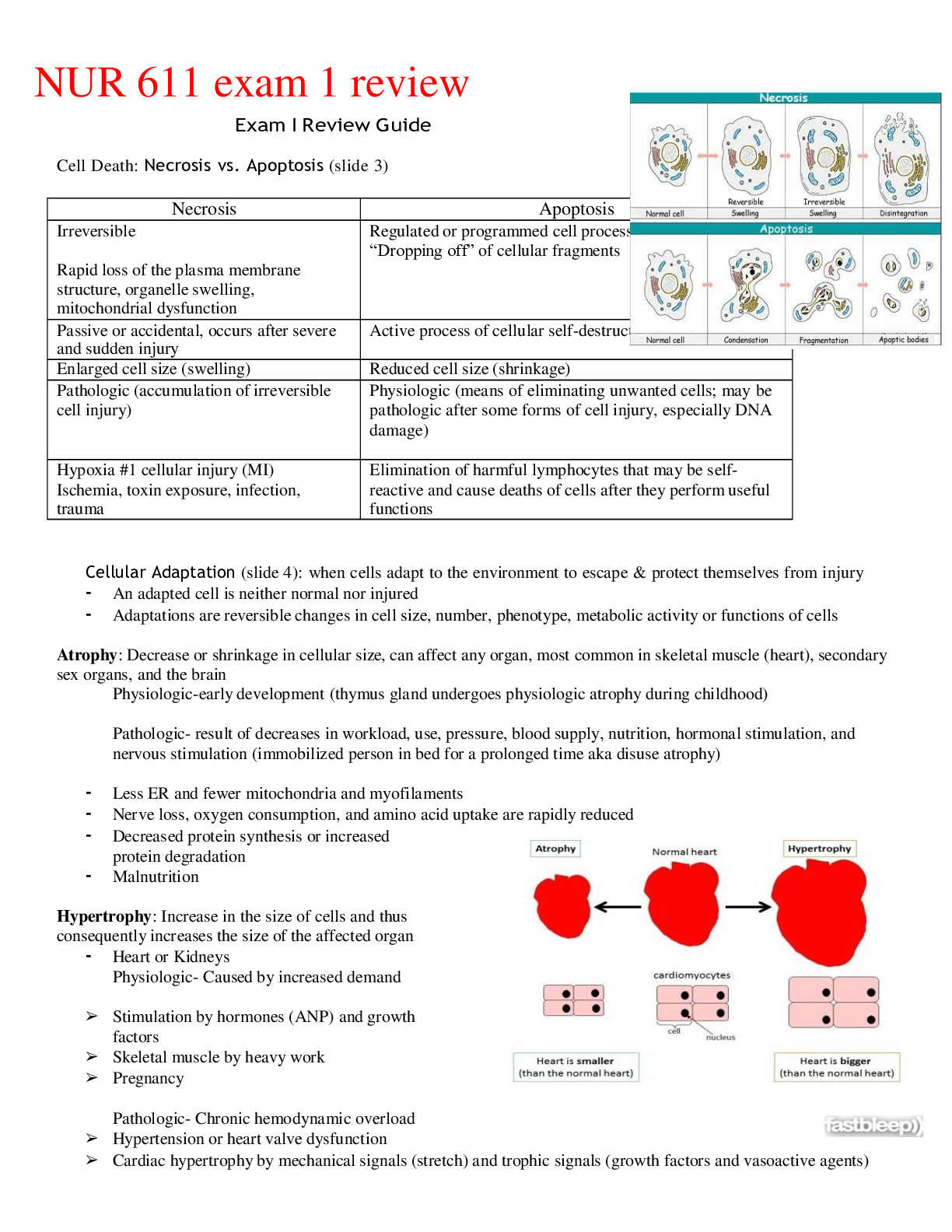
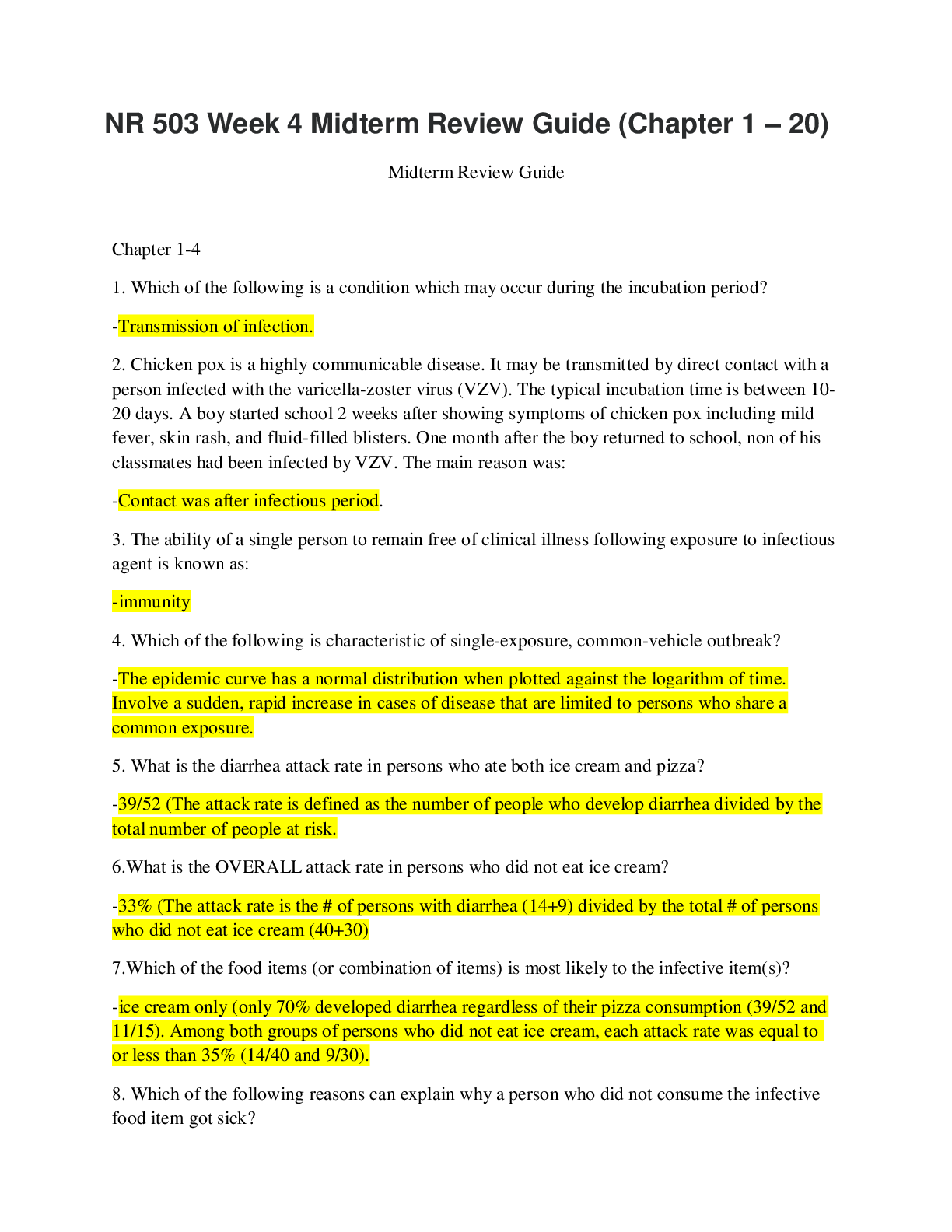
NUR 611 exam 1 review Exam I Review Guide Cell Death: Necrosis vs. Apoptosis (slide 3) Necrosis Apoptosis Irreversible Rapid loss of the plasma membrane structure, organelle swelling, mito... chondrial dysfunction Regulated or programmed cell process “Dropping off” of cellular fragments Passive or accidental, occurs after severe and sudden injury Active process of cellular self-destruction Enlarged cell size (swelling) Reduced cell size (shrinkage) Pathologic (accumulation of irreversible cell injury) Physiologic (means of eliminating unwanted cells; may be pathologic after some forms of cell injury, especially DNA damage) Hypoxia #1 cellular injury (MI) Ischemia, toxin exposure, infection, trauma Elimination of harmful lymphocytes that may be self- reactive and cause deaths of cells after they perform useful functions Cellular Adaptation (slide 4): when cells adapt to the environment to escape & protect themselves from injury • An adapted cell is neither normal nor injured • Adaptations are reversible changes in cell size, number, phenotype, metabolic activity or functions of cells Atrophy: Decrease or shrinkage in cellular size, can affect any organ, most common in skeletal muscle (heart), secondary sex organs, and the brain Physiologic-early development (thymus gland undergoes physiologic atrophy during childhood) Pathologic- result of decreases in workload, use, pressure, blood supply, nutrition, hormonal stimulation, and nervous stimulation (immobilized person in bed for a prolonged time aka disuse atrophy) • Less ER and fewer mitochondria and myofilaments • Nerve loss, oxygen consumption, and amino acid uptake are rapidly reduced • Decreased protein synthesis or increased protein degradation • Malnutrition Hypertrophy: Increase in the size of cells and thus consequently increases the size of the affected organ • Heart or Kidneys Physiologic- Caused by increased demand ➢ Stimulation by hormones (ANP) and growth factors ➢ Skeletal muscle by heavy work ➢ Pregnancy Pathologic- Chronic hemodynamic overload ➢ Hypertension or heart valve dysfunction ➢ Cardiac hypertrophy by mechanical signals (stretch) and trophic signals (growth factors and vasoactive agents) Hyperplasia: Increase in the number of cells in an organ or tissue resulting from an increased rate of cellular division • Response to injury • Main mechanism is the production of growth factors, which stimulate the remaining cells to synthesize new cell components and ultimately to divide • Increased output of new cells from tissue stem cells Compensatory hyperplasia: adaptive mechanism that enables certain organs to regenerate (Liver) Pathologic hyperplasia: abnormal proliferation of normal cells and can occur as a response to excessive hormonal stimulation or the effects of growth factors on target cells (Endometriosis; imbalance of estrogen and progesterone) Metaplasia: Reversible replacement of one mature cell type by another • Found in association with tissue damage, repair, and regeneration • Usually change is not beneficial • Normal columnar ciliated epithelial cells of the bronchial lining have been replaced by stratified squamous epithelial cells • Can be reversed if irritant stopped (smoking) Cellular Metabolism (slide 5): All chemical tasks of maintaining essential cellular function, provides the cell with the energy it needs to synthesize (produce) cellular structures ▪ Energy-using process: Anabolism ▪ Energy-releasing: Catabolism Adenosine Triphosphate (ATP) ▪ “Fuel” inside living cells, needed for biological reactions for cells to function & energy stored in ATP can be used in energy-requiring reactions (anabolism) ▪ The function of ATP is not only to store energy but also to transfer it from one molecule to another ▪ Energy is stored by molecules of carbohydrate, lipid and protein which when catabolized, transfer energy to ATP ▪ Used by cells for muscle contraction and active transport of molecules across cellular membranes ▪ ATP = energy BUT needs Oxygen (Aerobic) Food & Production of Cellular Energy: Catabolism (energy-releasing) of proteins, lipids, and polysaccharides found in food can be divided into 3 phases Phase 1: Digestion ▪ Large molecules broken down into smaller subunits-protein into amino acids, polysaccharides into simple sugars and fats into fatty acids and glycerol ▪ Processes occur outside the cell by the action of enzymes Phase 2: Glycolysis and Oxidation ▪ Small molecules enter the cells and are further broken down in the cytoplasm ▪ Sugars into pyruvate acid ▪ Pyruvate enters mitochondria and converted into acetyl groups of acetyl coenzyme A ▪ Acetyl CoA (like ATP) releases energy when it is hydrolyzed ▪ Glycolysis (lysis) splitting of glucose-produces 2 net molecules of ATP per glucose molecule through oxidation (removal and transfer of a pair of electrons) ▪ Occurs when O2 reserves are depleted Phase 3: Citric Acid Cycle (Krebs cycle) ▪ Most ATP generated in this phase Important Facts to Remember: ▪ A reduction in ATP causes the plasma membrane’s sodium-potassium pump and sodium-calcium exchange to fail ▪ The failure of the Na- K+ pump & Na- Ca+ exchange leads to an intracellular accumulation of sodium and calcium and diffusion of potassium out of the cell ▪ Thus resulting in sodium and water entering the cell freely causing cellular swelling (Edema begins) Free Radicals (slide 6) • Generated by reduction-oxidation reactions in normal metabolic processes (respiration), absorption of extreme energy sources (UV light, radiation), enzymatic metabolism of exogenous chemicals, drugs, and pesticides, process of transition metals (iron and copper) • Any molecular species capable of independent existence that contains a single unpaired electron in an outer orbit • Very unstable due to the one unpaired electron • Molecule wants to be stable: donate the one electron or by accepting an electron • Reactive Oxygen Species (ROS) chemically reactive molecules formed from molecular oxygen formed as natural oxidant species in cells during mitochondrial respiration & energy generation • ROS plays roles in the initiation and progression of CV alterations (HTN, HL, DM, ischemic heart disease, HF, OSA) Cellular Injury (slide 7): Injury to cells and to extracellular matrix (ECM) leads to injury of tissues and organs ultimately determining the structural patterns of disease • Loss of function derives from cell & ECM injury and cell death • When the cells are “stressed” out or unable to maintain homeostasis in the face of injurious stimuli or cell stress (hypoxia, free radicals, infectious agents, physical & mechanical factors, immunologic reactions, genetic factors, nutritional imbalances) cause injuries I. Ethanol: Liver enzymes metabolize ethanol to acetaldehyde causing hepatic cellular dysfunction • Peroxisomes: membrane bound organelles that contain several oxidative enzymes that detoxify compounds & fatty acids • Peroxisomes help detoxify ethanol but when not functioning properly the ethanol is turned into fat in the liver causing Fatty Liver Disease II. Radiation • Targets Deoxyribonucleic Acid (DNA) III. Lysosomes & consequences of lysosome leakage What they are? Membrane-enclosed organelles filled with digestive enzymes (hydrolases) • Enzymatic digestion of cellular organelles, including the nucleus & nucleolus, ensues, halting the synthesis of DNA & RNA Aging of the Cells and Tissues (slide 8) Common Findings Associated with Aging Progressive stiffness (rigidity) • Blood vessels and organs: peripheral vascular resistance (PVR) Stomach • Rate of emptying and secretion of hormones and HCl Immune system Fluid and Electrolytes • Total body K+ concentration • Cellular mass • Sodium/potassium ratio suggests that the cellular mass is accompanied by an extracellular component Muscle mass and strength (Sarcopenia) * Advise patients to get up and move & strengthen for prevention Most at risk for Fluid Volume Deficits Fluid Deficits and Dehydration (slide 10): Causes decreased perfusion Signs & Symptoms • Headache • Thirst • Dry skin & mucous membranes • Weight loss • urine output • Concentrated urine (Urine specific gravity > 1.030) • Skin turgor • Tongue furows prominent • Tachycardia, weak pulses (compensatory) • Postural Hypotension Vulnerable Populations Infants: 75-80% TBW (diarrhea can increase extracellular fluid) Obese: more body fat, less TBW (fat is water repelling) Elderly: increase in age decreases TBW (thirst sensation decreases) Passive Transport: Diffusion, Filtration, and Osmosis Diffusion: movement of a solute molecule from an area of greater solute concentration to an area of lesser solute concentration • Concentration gradient is the difference in concentration • The greater the concentration the higher the diffusion rate • Passive movement of particles “down” a concentration gradient (high to low) • Diffusion rate is influenced by A) Differences of electrical potential across the membrane (pores in the lipid bilayer are often linked to Ca++, other cations (Na+, K+) diffuse slowly because they are repelled by the positive charges in the pores) B) Size and its lipid solubility (smaller the more soluble it is in oil, more hydrophobic or nonpolar the more rapidly it will diffuse across the bilayer) Filtration: movement of water and solutes through a membrane because of a greater pushing pressure (force) on one side of the membrane • Hydrostatic pressure Osmosis: movement of water “down” a concentration gradient, that is, across a semipermeable membrane from a region of higher water concentration to a region of lower water concentration • Membrane must be more permeable to water than to solutes and the concentration of solutes must be greater so that water moves more easily • Directly related to hydrostatic pressure and solute concentration but NOT to particle size or weight • Osmotic pressure is the amount of hydrostatic pressure needed to oppose the osmotic movement of water Hydrostatic Versus Oncotic Pressures (slide 11) Hydrostatic Pressure Oncotic Pressure The pressure exerted by a fluid within a closed system (circulatory system, including capillaries) *Osmotic pressure is the hydrostatic pressure required to stop the flow of water The pressure exerted by plasma proteins, they are unable to pass through a semipermeable membrane themselves *Low plasma albumin causes edema as a result of a reduction in plasma oncotic pressure Pressure that drives fluid OUT of the capillary (filtration), Pushing force Highest at the arteriolar end of the capillary-fluid moves from the intravascular space into the interstitial space bc capillary hydrostatic pressure (influenced by the cardiac system) is higher than the capillary oncotic pressure Lowest at the venous ends (where fluids re-enter the capillary) Pulling force, pulling fluids from the surrounding tissue into the capillaries Increases along the length of the capillary, particularly in capillaries having high net filtration In the capillaries hydrostatic pressure increases filtration by pushing fluid and solute OUT of the capillaries Result of a difference in the concentration of solutes in the fluid inside the capillaries as opposed to outside them In the vascular system, hydrostatic pressure is the blood pressure/pumping of the heart Influenced by type and thickness of the plasma membrane, size of the molecules, concentration of molecules (concentration gradient), solubility of molecules within the membrane Natriuretic Peptides, RAAS, and ADH (slide 12) Natriuretic Peptides: hormones that include atrial natriuretic peptide (ANP) produced by the myocardial atria, brain natriuretic peptide (BNP) produced by myocardial ventricules and Urodilatin within the kidney ➢ Released when there is an increase in transmural arterial pressure caused by increased intraarterial volume (HF) ➢ Increase sodium and water excretion by the kidneys, which lowers blood volume and BP ➢ Natural antagonists to RAAS RAAS: Renin-Angiotensin-Aldosterone System: When circulating blood volume or blood pressure is reduced, renin, an enzyme secreted by the juxtaglomerular cells of the kidney, is released in response to sympathetic nerve stimulation and decreased perfusion of the renal vasculature Antidiuretic Hormone (ADH): Secretion of ADH and the perception of thirst are stimulated by an Increase in plasma osmolality Electrolytes Sodium (Na+): 135-145 mEq/L (slides 14 &15) ▪ 90% of the ECF cations, regulates extracellular osmotic forces (regulates H2O balance and ECF volume) ▪ Regulator of fluids ▪ Maintenance of neuromuscular irritability for conduction of nerve impulses ▪ Regulation for acid-base balance, participation in cellular chemical reactions, transport of substances across the cellular membrane Hypernatremia causes Clinical manifestations Hyponatremia causes Clinical manifestations Inadequate free water intake (elderly, impaired mental state) Confusion Convulsions Cerebral hemorrhage Coma Brain: high sodium in the blood vessels pulls water out of brain cells into the blood vessels, causing brain cells to shrink. Cerebral hemorrhage from stretching/contraction of Pure sodium deficits: Diuretics, vomiting, diarrhea Headache Lethargy Confusion Seizures Coma (cerebral edema) Inappropriate administration of hypertonic saline solution Dilutional hyponatremia: Hypotonic IV solutions (0.45 NS) Over secretion of aldosterone Diseases: kidney failure, HF, liver failure (ascites) veins Potassium: 3.5-5.0 mEq/L (slides 16 & 17) ▪ Major determinant of the resting membrane potential necessary for transmission of nerve impulses ▪ Intracellular electrolyte ▪ Ratio of K+ in the ICF to K+ in the ECF is the major determinant of the resting membrane potential, necessary for the transmission and conduction of nerve impulses, maintenance of cardiac rhythms, and skeletal and smooth muscle contraction Hyperkalemia causes (> 5 mEq/L) Clinical manifestations Hypokalemia causes (< 3.5 mEq/L) Clinical manifestations Renal failure Weakness Feeling of numbness/tingling N/V CP Palpitations or brady- arrhythmias Hyperaldosteronism Neuromuscular excitability is decreased-skeletal muscle weakness, smooth muscle atony Delayed ventricular repolarization Flattened T-waves, AV blocks, bradycardia , paroxysmal tachycardia Addison’s disease (decreased production of aldosterone thus body holds onto K+) Respiratory Alkalosis Massive trauma Diabetic ketoacidosis Insulin deficiency Pernicious anemia Metabolic acidosis *hydrogen ions shift into the cells in exchange for ICF potassium (hyperkalemia & acidosis occur together) GI or renal disorders: diarrhea How is insulin used to treat hyperkalemia? • Insulin transports potassium from the blood to the cell along with glucose • Insulin contributes to the regulation of plasma potassium levels by stimulating the sodium, potassium ATPase pump, thereby promoting the movement of K+ into the liver and muscle cells simultaneously with glucose transport after eating • The intracellular movement of potassium prevents an acute hyperkalemia related to food intake • Insulin can also be used to treat hyperkalemia Movement of electrical impulses: Membrane potentials Body cells are electrically polarized- inside of the cell being more negatively charged • Resting membrane potential is the difference in electrical charge (-70 to -85 milivolts) • Difference in voltage across the plasma membrane is a result of the ionic composition of ICF and ECF • Sodium ions have a greater concentration in the ECF • Potassium ions have a greater concentration in the ICF • Concentration difference is maintained by active transport of Na+ and K+ (sodium-potassium pump), transports sodium outward and potassium inward • The resting plasma membrane is more permeable to K+ which means K+ can diffuse easily from its area of higher concentration in the ICF to its area of lower concentration in the ECF...net result of an excess of anions inside the cell resulting in the resting membrane potential • Nerve & muscle cells are excitable & can change their resting membrane potential in response to electrochemical stimuli • Changes in resting membrane potential convey messages from cell to cell • When a nerve or muscle cell receives a stimulus that exceeds the membrane threshold value, a rapid change in the resting membrane potential known as the action potential • The action potential carries signals along the nerve or muscle cell & conveys information from one cell to another • Resting cell is stimulated (voltage-regulated channels), the cell membranes become more permeable to Na+ • Depolarization is when Na+ moves into the cell, and the membrane potential decreases (moves forward) from a negative value to zero • Depolarized cell is more positively charged and its polarity is neutralized * To generate an action potential and the resulting depolarization, a threshold potential must be reached. When the threshold is reached, the cell will continue to depolarize with no further stimulation. The Na+ gates open and Na+ rushes into the cell, causing the membrane potential to reduce to zero and then become positively charged (depolarization). The rapid reversal in polarity results in an action potential • During repolarization the negative polarity of the resting membrane potential is reestablished. As the Na+ channels close, the voltage-gated K+ channels open (membrane permeability to Na+ decreases and K+ permeability increases) with an outward movement of K+, the membrane potential becomes more negative • The sodium-potassium returns the membrane back to the resting potential by pumping K+ back into the cell and Na+ out of the cell, *During most of the action potential, the plasma membrane cannot respond to other stimuli (absolute refractory period) and is related to changes in permeability to Na+ * During the latter phase of the action potential, when permeability to K+ increases, a stronger than normal stimulus can evoke an action potential (Relative refractory period) • When the membrane potential is more negative than normal, the cell is hyperpolarized (less excitable), a larger than normal stimulus is required to reach the threshold potential and & generate an action potential • When the membrane potential is more positive than normal, the cell is hypopolarized (more excitable) and is demonstrated by Tall-peaked T waves, smaller than normal stimulus is required to reach the threshold potential *Changes in the ECF and ICF concentration of ions or a change in membrane permeability can cause alterations in membrane excitability * Calcium blocking agents for heart disease and migraines developed due to the understanding of ion movement and membrane excitability Calcium: 8.5-10 mg/dL (slide 18) • Bone, teeth, blood clotting and muscle contraction • Ion for fundamental metabolic processes Hypercalcemia causes (>10-12 mg/dL) Clinical manifestations Hypocalcemia causes (< 8.5 mg/dL) Clinical manifestations Hyperparathyroidism--> Associated with thyrotoxicosis Decrease of cell membrane excitability More Ca++ inside cell creates threshold potential more positive (hyperpolarized)& cell membrane becomes refractory to depolarization (decreased excitability) due to greater difference b/t threshold potential & resting membrane potential Fatigue, weakness, lethargy Anorexia Nausea, constipation AMS; confusion Impaired renal function- kidney stones Shortened QT segment, depressed widened T waves Bradycardia AV blocks Inadequate intestinal absorption Increase in neuromuscular excitability Causes partial depolarization of nerves & muscle r/t threshold potential becomes more negative & approaches the resting membrane potential (Hypopolarization)--> smaller stimulus required for initiating action potential Neuromuscular irritability- paresthesias around the mouth & lips and then in digits, carpopedal spasms (hands & feet), hyperreflexia and seizures Convulsions & tetany (continuous severe muscle spasm that can cause laryngospasm & death) Prolonged QT interval (prolonged ventricular depolarization & decreased cardiac contractility) Intestinal cramping, hyperactive bowel sounds Osteoporosis Bone metastases Decrease levels of PTH & vitamin D Vitamin D excess Nutritional deficiencies Malnutrition, Too much phosphorous Tumors r/t PTH production Removal of parathyroid glands (total thyroidectomy) r/t low PTH Sarcoidosis (Growth of tiny collections of inflammatory cells in different parts of the body) Massive blood administration- citrate solution Prolonged immobilization Pancreatitis-release of lipase that bind to Ca++ Acidosis *Decreases serum binding to Ca++ to albumin, Increasing ionized Ca++ levels Alkalosis--> metabolic or respiratory pH change enhances protein binding of ionized Ca++ Hypoalbuminemia-lowers serum Ca++ by decreasing the amount of Ca++ in plasma • Calcium & phosphate regulation is by 3 hormones: PTH, vitamin D, and calcitonin • Parathyroid glands secrete Parathyroid hormone (PTH) in the blood & extracellular fluids—renal regulation of calcium and phosphate balance requires PTH PTH stimulates reabsorption of calcium along the distal tubule of the nephron & inhibits phosphate reabsorption by the proximal tubule, net result is an in serum calcium • Vitamin D (cholecalciferol) fat-soluble steroid ingested in food or synthesized in the skin in the presence of UV light Process of vitamin D activation: starts in the liver, final activation in the kidneys 1) Renal activation occurs when serum Ca++ decreases 2) PTH secreted 3) PTH acts to Ca++ reabsorption & excrete phosphate 4) Activated vitamin D3 (calcitriol) circulates as a hormone in the plasma to increase absorption of Ca++ **Combination of low Ca++ & PTH secretion causes the renal activation of vitamin D * When RF occurs, vitamin D is not activated Calcitonin: produced by C cells of the thyroid gland, decreases Ca++ levels by inhibiting osteoclasic activity in bone • Ca++ increase, PTH secretion suppressed, decreased vitamin D activation, decreased intestinal calcium absorption, increased renal phosphate reabsorption Phosphate: 2.5-4.5 md/dL (slide 19) • Found in bone (85%) • Many metabolic forms: creatine phosphate & adenosine triphosphate (ATP)-muscle contraction • Anion buffer in acid-base balance Hyperphosphatemia (> 4.7mg/dL) Clinical manifestations Hypophosphatemia (< 2.0 mg/dL) Clinical manifestations Acute or chronic RF, loss of GFR *Similar to those of LOW Ca++ levels Calcification of soft tissues in lungs, kidneys, joints Intestinal malabsorption & refeeding syndromes Reduced capacity for O2 transport by RBCs & disturbed energy metabolism Leukocyte & platelet dysfunction- Greater risk for infection & blood clotting impairment, hemorrhage ATP levels become low & diminish release of O2 to the tissues--> Hypoxia with bradycardia & AV blocks Nerve & muscle impairment- muscle weakness causing respiratory failure, cardiomyopathies Irritability, confusion, numbness, coma & convulsions Bone resorption: rickets or osteomalacia Chemotherapy, release in ECF Increased renal excretion- hyperparathyroidism Laxatives or enemas Vitamin D deficiency Hypoparathyroidism Antacids (containing magnesium & aluminum) Respiratory Alkalosis Magnesium: 1.5-3.0 mEq/L (slide 20) • Major intracellular cation, second to potassium • Regulation of metabolism is by small intestine & kidney • Cofactor in intracellular enzymatic reactions, protein synthesis, nucleic acid stability, neuromuscular excitability Hypermagnesemia (> 3.0 mEq/L) Clinical manifestations Hypomagnesemia (< 1.5 mEq/L) Clinical manifestations Renal failure Lethargy Drowsiness Loss of DTR N/V Malnutrition Behavioral changes: irritability Increased reflexes Muscle cramps Adrenal insufficiency Malabsorption Antacids (with Mg++) Alcoholism Urinary loses- renal tubular Muscle weakness dysfunction Ataxia Hypotension Loop diuretics Nystagmus Bradycardia Respiratory distress PPI use Tetany Convulsions Heart block & cardiac arrest Tachycardia Hypotension Genetics (slide 21) Genes are composed of DNA. The most important constituent of DNA, the four types of nitrogenous bases: Adenine, Cytosine, Guanine, and Thymine (Slide 22) Aneuploid cells “those that do not contain a multiple of 23 chromosomes” Trisomic • Three pairs of one chromosome (Trisomy) Ex) Most well-known is Trisomy 21 aka Down Syndrome, characterized by IQs between 25-70, low nasal bridge, protruding tongue and flat, low-set ears Genetic Principles: Penetrance versus Expressivity (slide 23) Penetrance: % of individuals with a specific genotype who also exhibits the phenotype Incomplete penetrance: individual who contains the disease causing allele but may not exhibit the disease phenotype, even though the allele and the associated disease may be transmitted to the next generation • Huntington disease, autosomal dominant condition known as progressive dementia & uncontrollable movements of the limbs • S/S not seen until age 40 (age-dependent penetrance) Expressivity: extent of variation in phenotype associated with a genotype, penetrance is complete but the severity of the disease varies Autosomal recessive & Autosomal dominance (slide 24) Autosomal dominant --> two sexes exhibit the trait proportionately, no skipping of generations, affected heterozygous individuals transmit the trait to approx. half of their children (50%) Ex) BRCA1 and BRCA2 Autosomal recessive --> two copies of abnormal gene must be present (homozygous), carriers are phenotypically normal Ex) Cystic fibrosis How common is a given disease in a population? (slide 25) # of new cases of a disease/ # of individuals in the population = Incidence rate Relative risk= measure of the effect of a specific risk factor, expressed as a ratio Genetic Processes (slide 26) • Epigenetic modifications can cause individuals with the same DNA to have different disease profiles (twins) • As twins age, they demonstrate increasing differences in methylation patterns of their DNA sequences hence phenotypic differences • Environmental factors (diet, exposure to chemicals) • Unlike DNA sequence mutations, cannot be altered, epigenetic modifications can be reversed When Messenger RNA (mRNA) is over-expressed it results in metastasis of an already existing cancer (slide 27) Hypermethylation is seen in miRNA genes that bind to the ends of mRNAs, degrading them & preventing their translation. When miRNA genes are methylated, their mRNA targets are over-expressed, and this over-expression has been associated with metastasis Acid-Base Balance (slide 27) ❖ Acid-base balance & hydrogen ion concentration must be regulated for the body to function normally ❖ Hydrogen ion concentration is necessary to maintain membrane integrity & speed of enzymatic reactions Respiratory Acidosis Respiratory Alkalosis Metabolic Acidosis Metabolic Alkalosis pH pCO2 □ pH pCO2 pH HCO3 □ pH HCO3 COPD Sedative OD Chest wall abnormality PNA Atelectasis Pulmonary edema Respiratory muscle weakness Hyperventilation (hypoxia, anxiety, fear, pain, exercise, fever) Stimulated respiratory center (CVA, meningitis, septicemia, brain injury, salicylate poisoning) Elevated anion gap DKA: Ketoacidosis (DM) Lactic acidosis (shock) Ingestion of ethylene glycol, salicylates Normal anion gap Diarrhea Vomiting NG suctioning Diuretic therapy Hypokalemia Excess NaHCO3 intake Mechanical hypoventilation Liver failure Mechanical hyperventilation Proximal renal tubule acidosis Anion gap = (Na= + K+ ) - (HCO3 + Cl-) = 10-12 mEq/L ABG Interpretation (slide 28) pH (7.35-7.45) pCO2 (35-45) HCO3 (22-26) Acidosis or Alkalosis Respiratory effect Metabolic effect Less than 7.35 (acidic) Greater than 7.45 (alkalotic) Greater than 45 (acidic) Less than 35 (alkalotic) Less than 22 (acidic) Greater than 26 (alkalotic) R =Respiratory O =Opposite M =Metabolic E =Equal ➢ If the disturbance is respiratory in nature, the movement of CO2 will be in the opposite direction to the movement of the pH ➢ If the disturbance is metabolic in nature, the movement of HCO3 will be in the same direction to the movement of the pH ➢ If pH is within the normal range this can indicate compensation [Show More]
Last updated: 1 year ago
Preview 1 out of 13 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Jun 03, 2021
Number of pages
13
Written in
Additional information
This document has been written for:
Uploaded
Jun 03, 2021
Downloads
0
Views
64

.png)
.png)