*NURSING > STUDY GUIDE > MEDSURG NR 324 Exam 1 Study Guide (clinical manifestations) | Chamberlain College of Nursing | 100% (All)
MEDSURG NR 324 Exam 1 Study Guide (clinical manifestations) | Chamberlain College of Nursing | 100% GUARANTEED PASS.
Document Content and Description Below
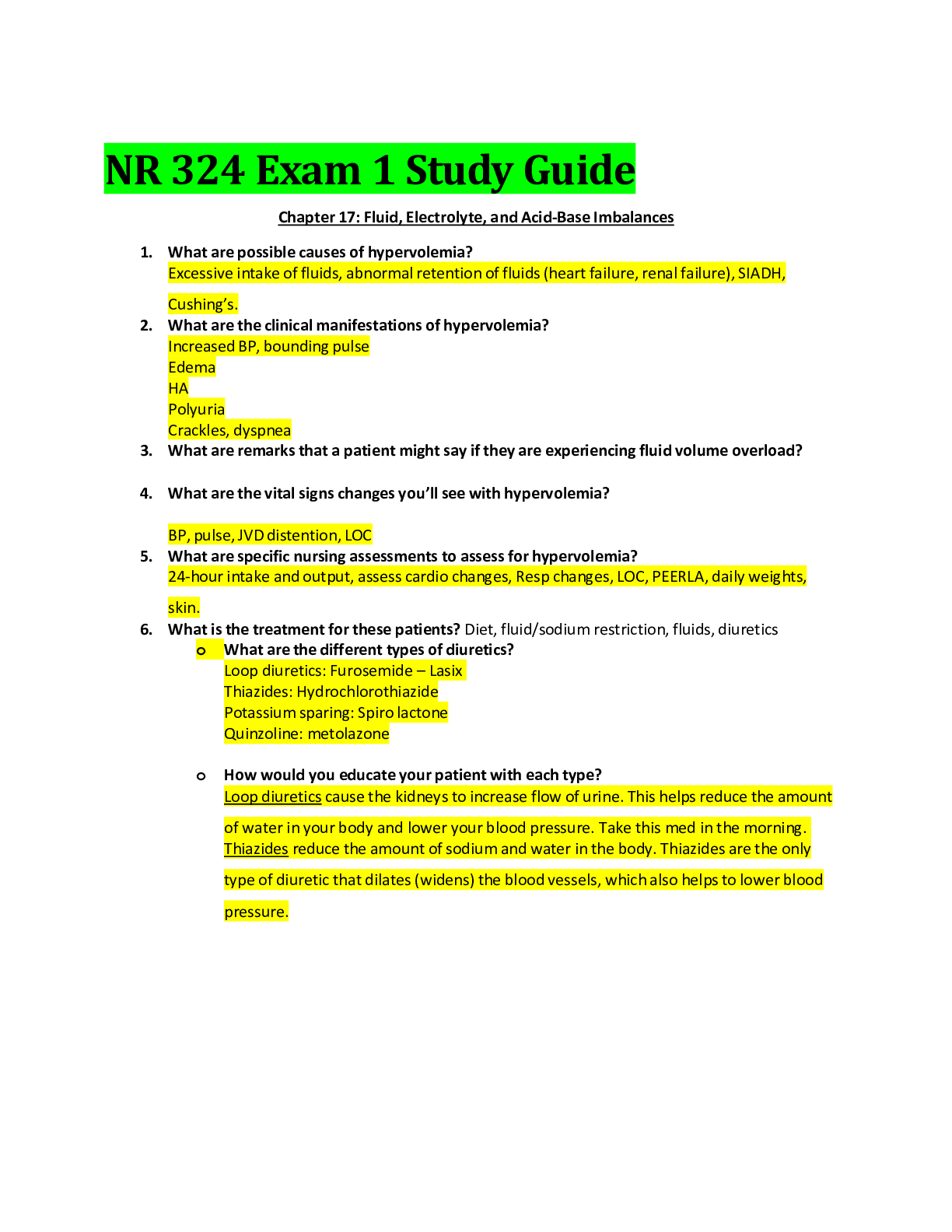
NR 324 Exam 1 Study Guide Chapter 17: Fluid, Electrolyte, and Acid-Base Imbalances 1. What are possible causes of hypervolemia? Excessive intake of fluids, abnormal retention of fluids (heart fai... lure, renal failure), SIADH, Cushing’s. 2. What are the clinical manifestations of hypervolemia? Increased BP, bounding pulse Edema HA Polyuria Crackles, dyspnea 3. What are remarks that a patient might say if they are experiencing fluid volume overload? 4. What are the vital signs changes you’ll see with hypervolemia? BP, pulse, JVD distention, LOC 5. What are specific nursing assessments to assess for hypervolemia? 24-hour intake and output, assess cardio changes, Resp changes, LOC, PEERLA, daily weights, skin. 6. What is the treatment for these patients? Diet, fluid/sodium restriction, fluids, diuretics o What are the different types of diuretics? Loop diuretics: Furosemide – Lasix Thiazides: Hydrochlorothiazide Potassium sparing: Spiro lactone Quinzoline: metolazone o How would you educate your patient with each type? Loop diuretics cause the kidneys to increase flow of urine. This helps reduce the amount of water in your body and lower your blood pressure. Take this med in the morning. Thiazides reduce the amount of sodium and water in the body. Thiazides are the only type of diuretic that dilates (widens) the blood vessels, which also helps to lower blood pressure. Potassium-sparing used to reduce the amount of water in the body. Unlike the other diuretic medicines, these medicines do not cause your body to lose potassium. Do not increase the potassium you eat. 7. What are possible causes of hypovolemia? Fever, heatstroke, Diabetes insipidus, GI losses, Hemorrhage, dehydration 8. What are the clinical manifestations of hypovolemia? Poor skin turgor Lethargy Thirst, dry mucous membranes Decreased urine output, concentrated Increased respiratory rate Orthostatic hypotension 9. What are remarks that a patient might say if they are experiencing dehydration? 10. What are the vital signs changes you’ll see with hypervolemia? Decreased BP, Increased HR, Increased RR, flattened neck veins, thread pulse 11. What are specific nursing assessments to assess for hypovolemia? Skin turgor, skin (dry, breakdown), daily weights, intake and output 12. What is the treatment for these patients? Increase fluids 13. What are way’s to measure fluid volume status? Intake and output, daily weight 14. Which measurement is the best way to measure total body fluid gains/loss? Daily weight 15. What are lab value ranges, action in the body, clinical manifestation and treatments of the following: o Sodium (NA) : 135-145 Maintains the concentration and volume of ECF and influences water distribution. Where water goes sodium follows. Hypernatremia Manifestations: Restlessness, agitation twitching, seizures, coma Treatments: treat underlying cause, hypotonic solution (5% dextrose) Hyponatremia: Manifestation: Lethargy, confusion, decreased reflexes, seizures, and coma Treatments: treat underlying cause, fluid restriction, hypertonic saline in small amounts o Potassium (K): 3.5-5.0 HEART Regulates intracellular osmolality and promotes cellular growth. Neuromuscular and cardiac function are commonly affected. Hyperkalemia (renal failure, rapid TPN) Manifestations: irregular pulse, paresthesia, weakness, irritability Treatments: Kayexalate, IV insulin and glucose (pushes K+ into cells), Hemodialysis Hypokalemia (GI losses, diarrhea, vomiting, NG suction) Manifestations: muscles weakness, irregular pulse, fatigue, hyperglycemia Treatments: treat with oral or IV K+ (needs to be on pump and cannot exceed 10-20 mEq per hour o Magnesium (Mg): 1.5-2.5 Activate enzyme systems required for synthesis of nucleic acids and proteins. Maintains normal calcium and potassium balance. Hypomagnesemia (renal failure, adrenal insuff.) Manifestations: lethargy, drowsiness, nausea and vomiting, potential for respiratory arrest. Treatments: Focus on prevention, especially in renal patients (do not give magnesium controlled drugs) Hypomagnesemia (diarrhea, vomiting, impaired GI absorption, large urine output, alcoholism). Manifestations: confusion, hyperactive deep tendon reflexes, cardiac dysrhythmias Treatments: oral or IV replacement. o Phosphorus (PO): 2.4-4.4 Essential for function of muscle, RBCs, nervous system. Acid-buffer, cellular uptake & use of glucose. Hyperphosphatemia (renal failure, chemo drugs, excessive intake of milk/vit D.) Manifestations: Hypocalcemia, muscle problems, tetany Treatments: Treat underlying cause, promote hydration Hypophosphatemia: (Malabsorption syndrome, respiratory acidosis, phosphate binding antacids) Manifestations: CNS malfunction, muscle weakness, dysrhythmias, severe cases will have many serious complications related to ATP (body needs for energy) not being formed. Treatments: Oral supplementation and monitoring of lab values o Calcium (CA): 8.6-10.2 Structure of bones and teeth. Myocardial contractions, muscle contractions. Hypercalcemia (bone malignancies, hyperparathyroidism) Manifestations: lethargy, weakness, coma, can cause Ventricular arrhythmias Treatments: Promote excretion of calcium with loop diuretic, low calcium diet, encourage fluids to prevent kidney stones, Calcitonin (lowers Ca levels). Hypocalcemia (Chronic Kidney Disease, hypoparathyroidism, Vit D deficiency, Magnesium deficiency) Manifestations: Prolonged QT, hyper excited skeletal muscles Treatments: Watch patients with throat or thyroid surgery for this, treat with aiming at the cause, No Calcium IM because of necrosis risk, IV is given as calcium gluconate. 16. Know how to interpret ABG results and evaluate priority ABG’s (aka terrible ABGs, which ABG result you would assess first) Assess pH since acidosis is the most severe. Alkalosis is the easiest to fix. 17. What type of clinical manifestations and treatments would you expect with each: o Metabolic acidosis: Decreased BP, warm/flush skin, Kussmaul respirations, prolonged diarrhea, lethargy, cardiac dysrhythmias. Increase fluids, IV solution of 0.9% NS. o Metabolic alkalosis: LOC changes, tachycardia, tetany, seizures, HA, N/V, resp. depression. Increase fluids, IV solution 0.9% NS. o Respiratory acidosis: Decreased BP, hypoventilation, tachypnea, absent breath sounds, crackles/dyspnea. o Respiratory alkalosis: Increased work of breathing, fatigue, resp. failure, hyperventilation, lightheadedness, blurred vision, tingling of extremities, palpitations/dysrhythmias. 18. Describe each of the IV fluids (ECF/ICF changes), names of IV fluids in each category (ex. LR, 0.9 NS, 0.45 NS, etc.), when they are used and nursing assessment associated with each: o Hypotonic: solutes are less concentrated than in the cells (swell/burst). D5W (sugar water) - maintance fluid used in diabetes and hypernatremia. 0.45% NACL- maintence fluid used to replace fluid loss. Assess for Fluid overload or hypovolemia. o Hypertonic: Solutes are more concentrated than in the cells (Shrink and die). D10 (dextrose in water), D5 NS (0.9%) treats hyponatremia, D5LR-post surgical, acute blood loss and burns. Monitor lung sounds, swelling, pH increase 7.5, labs, BP. o Isotonic: Same osmolality as the cell interior. Closest to the bloodstream (inflate the cell). DW5, 0.9% NS (NaCl), Lactated ringers. Used when patient has experienced both fluid and sodium losses or as vascular fluid replacement in hypovolemic shock. 19. What are the benefits and risks of a central venous access device? Benefits Immediate access Reduced venipunctures Decreased risk of extravasation (eats tissues) Risks Increased risk of systemic infection and invasive procedure 20. What is the difference between a centrally inserted central line and a peripherally inserted central line? CVADs are inserted in the neck or chest, they administer potential vesicants, blood and blood products and TPN. Multiple port access. PICC lines are placed into a vein in the arm and used for long-term antibiotic or chemo and for patients who need vascular access for 1 week to 6 months but can be in place for longer periods. o Where do these lines end up in the body? CVAD the tip rests in the distal end of the Superior vena cava. PICC the tip ends in the distal one third of the superior vena cava. o What is a sign that the catheter has floated too far into the heart and has gone through the valves? Dysrhythmias (v-tach or v-fib) 21. What are your nursing interventions related to care for these lines? Monitor for infection, systemic or local, vitals, measure at insertion site, flush/blood return MUST have both, pain assessment, listen bilateral lung sounds. Why do we do them? To assess for complications. 22. Be sure to understand which nursing diagnosis are priority over others. (A-B-C) Chapter 26: Nursing Assessment: Respiratory System 23. Describe the sound you would hear, where you would hear it, what could cause this sound, and treatments you would expect to have ordered: o Crackles: popping sounds on inspiration, heard in lungs, causes: HF, pulmonary edema, pneumonia, COPD. Treatments: stop fluids, start diuretics, fluid restriction (severe) and restrict sodium. o Wheezes: Continuous high-pitched squeaking or musical sound. Bronchial wall. Causes: asthma, anaphylaxis, COPD, airway obstruction. Treatments: Steroids (reduce inflammation), bronchodilators (open up). o Rhonchi: Continuous rumbling, snoring or rattling sound in large airways. Causes: COPD, cystic fibrosis, infection, pneumonia, smoker. Treatment: expectorant (mucinex), increase fluids, antibiotics, steroids or bronchodilator. o Pleural rub: coarse grating (sand paper). Inflamed pleural surfaces rubbing together. Causes: pleural effusion, pleurisy, pneumonia. Treatments: chest tube, antibiotic, diuretics and steroids. o Stridor: crowing sound of constant pitch. Partial obstruction of larynx or trachea. Causes: choking, epiglottitis, anaphylaxis. Treatment: epinephrine (Broncho dilates and vasoconstricts), Heimlich, steroids. 24. Explain how to perform the test, the normal findings, abnormal findings, when and why you would feel/hear abnormal findings: o Tactile fremitus: Place the palmar surface of the hands with hyperextended fingers against the patient’s chest. Ask patient to repeat the phrase “99” in a louder and deeper than normal voice. Normal: vibrations are normal. Abnormal: Increased vibrations. Causes: when the lungs become filled with fluid or is denser (pneumonia, lung tumors, thick bronchial secretions). Absent fremitus may be noted with pneumothorax or atelectasis. o Bronchophony: spoken or whispered “99” syllable more distinct than normal on auscultation. Normal: muffled. Abnormal: clear sounds. Causes: pneumonia o Egophony: Spoken “eeee” similar to “aaaa” on auscultation because of altered transmission of voice sounds. Normal: “eeee”. Abnormal: “aaaa”. Causes: pneumonia or pleural effusion. o Whispered pectoriloqy: patients whispers “1, 2, 3”. Normal: muffled. Abnormal: clear sounds. Causes: pneumonia. 25. Identify the following lab results & what specifically you are checking for when you are assessing them: o WBC: 5000-10,000. Infection o Hgb: 12-15. Amount of oxygen in the blood. Anemia or hemorrhage o Hct: 36-45. Amount of RBCs in one blood sample. Shock, hemorrhage, dehydration. o Platelets: 150-450. Thrombocytes in the blood. Promote coagulation. o BUN: 10-25. Evaluate kidney function. When the kidneys can’t get rid of urea. o Creatinine: 1.2-1.5. Evaluate the function of kidneys. 26. Explain nursing interventions you would perform if you have a client that has a high respiratory rate, dyspneic, and desaturation of the SPO2 levels. o How will you know if your patient is getting better after your interventions? Increase in SPO2, decrease RR 27. Explain the nursing management (assessments/interventions) for a patient receiving the following diagnostic tests: o CT scan: Evaluate BUN and creatinine to assess renal function. Assess allergies shellfish or iodine. Patient should be well hydrated before and after to excrete contrast. Warn patient that contrast injection may cause a feeling of being warm and flushed. o MRI: Evaluate BUN and creatinine to assess renal function. Contrast is not iodine based. Assess patient for claustrophobia, provide relaxation or other modes to cope. Patient must remove all metal. Patient with pacemakers and defib cannot have MRI. o Bronchoscopy: Instruct patient to be NPO status for 6-12 hr before the test. Give sedative if ordered. After procedure, keep patient NPO until gag reflex returns. Monitor for recovery for sedation. Blood-tinged mucous is not abnormal. If biopsy was done, monitor for hemorrhage and pneumothorax. o Lung biopsy: Same as bronchoscopy. With TTNA, check breath sounds q4hr for 24 hr and report and resp distress. Check incision site for bleeding. A chest x-ray should be done after TTNA or Tran’s bronchial biopsy to check for pneumothorax. With VATS a chest tube may be in post procedure until lung has reexpanded. Monitor breath sounds to follow chest reexpansion. Encourage deep breathing for lung reinflation. Chapter 27: Nursing Management: Upper Respiratory Problems 28. What is epistaxis? Nosebleeds 29. What are possible causes of epistaxis? Low humidity, allergies, upper resp infection, sinusitis, trauma, foreign bodies, hypertension, chemical irritants, street drugs, overuse nasal sprays. 30. What are the treatments? 1. Keep patient quiet 2. Place patient in a sitting position, leaning slightly forward with head tilted forward 3. Apply direct pressure by pinching the entire soft lower portion of the nose against the nasal septum for 10-15 minutes. o Which one do you do first? #2 o Which treatments are more advanced if simple measures do not work? Applying vasoconstrictive agent, cauterization or anterior packing, silver nitrate. 31. What is allergic rhinitis? Reaction of the nasal mucosa to a specific allergen. 32. What is key in the treatment/prevention of allergic rhinitis? Identifying and avoiding triggers of allergic reactions. 33. What are the 2 different types of flu vaccines? Inactivated and live attenuated. o What types of patients should receive each kind? Inactivated: injection. Over 6 months of age, can be used in people at increased risk (chronic medical conditions, nursing homes, immunocompromised, pregnant women). Live attenuated: nasal spray. Healthy people 2-49. 34. Tracheostomy: a) What is it? Surgically created stoma (opening) in the trachea to establish an airway. b) What is the purpose of it? Used to bypass an upper airway obstruction, facilitate removal of secretion or permit long term mechanical ventilation. c) What are the steps of trach care and suction and why/how they are done? d) What is the purpose of the cuff? Used for risk of aspiration or in mechanical vents. e) How do you accurately measure the pressure in the cuff? Inflate the cuff with the minimum volume of air required to obtain an airway seal. Cuff inflation pressure should not exceed 20 mm Hg or 25 cm H2O in order to prevent tracheal necrosis. MOV and MLT or commonly used methods. f) What are possible complications of a tracheostomy? Airway obstruction, air leak, aspiration, bleeding, infection, tracheal necrosis, tube displacement, fistula formation. g) What are roles of the RN, LPN, and UAP involving trach care? Cleansing inner cannula, cleanse stoma, suctioning, monitor cuff pressure every 8 hours, do not change ties for 24 hours, monitor of resp depression, infection and teach patient self-care. 35. What are common causes of head and neck cancer? Tobacco use, alcohol consumption. 36. What are clinical manifestations of head and neck cancer? Hoarseness that lasts more than 2 weeks, feeling of lump in the throat or change in voice quality. Sore throat, ear pain, swelling or lumps in the neck, coughing up blood, difficulties in chewing, swallowing, moving the tongue or jaw. 37. What is the treatment plan of head and neck cancer? Surgery, radiation therapy, chemotherapy and targeted therapy. Chapter 28: Nursing Management: Lower Respiratory Problems 38. What is the pathophysiology, clinical manifestations, nursing assessments, nursing diagnosis, diagnostic tests, complications and treatments for the following infections: a) Pertussis: highly contagious infection of the respiratory tract caused by gram negative bacillus, Bordetella pertussis. Clinical manifestations occur in stages: 1st-mild upper resp infection with low grade fever or no fever, runny nose, watery eyes and nonproductive cough. 2nd-paroxysms of cough. Inspiration causes the “whooping” sound. Vomiting may also occur. Coughing more frequent at night and last 6-10 weeks. Treatment: antibiotics. ▪ What is the best way to prevent pertussis? The Tdap vaccine against whooping cough. ▪ Who is most susceptible to pertussis? Kids b) Pneumonia: Inflammatory response in the lung. Attraction of neutrophils, release of inflammatory mediators, accumulation of exudates, RBC and bacteria, decreased air exchange. Clinical manifestations: cough, fever/shaking chills, dyspnea, tachypnea, pleuritic chest pain, green/yellow or rust colored sputum. Rhonchi/crackles, egophony, increased fremitus. Tests: chest x-ray, sputum analysis, CBC w/diff, pulse ox or abg, blood cultures, thoracentesis. Assessment: Objective data, objective (fremitus, sputum, changes LOC). Diagnosis: Impaired gas exchange, ineffective breathing pattern, and acute pain. Complications: pleurisy, pleural effusion, atelectasis, bacteremia, empyema, pericarditis, meningitis, sepsis, pneumothorax. Treatment: Vaccine, antibiotic therapy, supportive care, nutritional therapy. ▪ What are the different types of pneumonia? Community acquired (CAP) Medical care-associated acquired (MCAP) Hospital associated (HAP) Ventilator associated (VAP) Health care associated (HCAP) Aspiration pneumonia Opportunistic pneumonia Pneumocystis jiroveci pneumonia (PCP) Cytomegalovirus (CMV) ▪ When is the pneumonia vaccine recommended? Age 65 or older Age 2-64 with long-term health problem or immunosuppression Age 19-64 who smoke or have asthma Live in nursing homes or long term care facility ▪ What is the CURB-65 scale? It’s a test used as a supplement to clinical judgment to determine the severity of pneumonia and if patients need to be hospitalized. ▪ How long are symptoms expected for pneumonia? 2-3 weeks c) Lung Cancer: Arise from mutated epithelial cells, tumor development promoted by epidermal growth factor, Occur primarily in segmental bronchi and upper lobes. Primary lung cancers categorized into 2 sub types: non-small-cell lung cancer (80%) and small- cell lung cancer (20%). ▪ What are the different carcinogens that can cause lung cancer? Pollution Radon/radiation Asbestos Industrial agents Smoking Genetic factors Gender differences ▪ Describe clinical manifestations of lung cancer: Symptoms appear late in disease. May be masked by chronic cough Depend on type of primary lung cancer, location, and metastatic spread Pneumonitis Persistent cough with sputum (most common) Hemoptysis Dyspnea Wheezing Chest pain ▪ Distinguish the different types of lung cancer: ▪ Squamous cell carcinoma Slow growing Early symptoms ▪ Adenocarcinoma Moderate growing Most-common in non-smokers ▪ Large-cell carcinoma Rapid growing Highly metastatic ▪ Describe the TNM staging system: • T: denotes tumor size, location and degree of invasion • N: indicates regional lymph node invasion • M: represents presence/absence of distant metastases d) Tuberculosis: Tuberculosis is an infectious disease caused by mycobacterium tuberculosis involves lungs primarily but any organ can be infected. M. Tuberculosis is gram-positive (acid-fast bacillus). Spreads from person-person via airborne droplets (i.e breathing, talking, singing, sneezing, and coughing). Cannot be spread by touching, sharing food utensils, kissing, or any other types of physical content. Inhalation causes small particles to lodge in the bronchiole & alveolus Local inflammatory reaction occurs Hallmark of TB (ghon focus) developing into a granuloma Granuloma is a defense mechanism (walls of infection and attempts to prevent further spread). M. tuberculosis is aerophilic (oxygen loving) affinity for lungs. Can also spread via lymphatic system. Other organs TB favors for growth can be kidneys, epiphyses of the bone, cerebral cortex, and adrenal glands. Clinical manifestations: LTBI-asymptomatic, Pulmonary TB takes 2-3 weeks to develop symptoms, cough becomes frequent, increased fever, chills, pleuritic pain, productive cough, and adventurous breath sounds. High fever in the afternoon. Complications: military TB, Pleural TB, pneumonia. Tests: TB skin test, chest x-ray, interferon release assays. Treatment: active: 2 phases and is aggressive. Latent: treated for 6-9 months. Diagnosis: ineffective breathing pattern, ineffective airway clearance, noncompliance, ineffective self-health management. Promote health, prevent spread. ▪ What precautions are these patients placed on? Single-occupancy room with 6-12 airflow exchanges/hour, HEPA masks must be worn, airborne isolation. ▪ When can these precautions be removed? Can be considered adequately treated when the therapy regimen has been completed and there is evidence of negative cultures, clinical improvement and improvement on chest x-ray. ▪ How long are the treatments? 6-12 months. e) Pulmonary Embolism: Blockage of one or more pulmonary arteries by a thrombus, fat, air embolus, or tumor tissue, Emboli are mobile clots that generally do not stop moving until they become lodged at a narrow area in the circulatory system, In the lungs the emboli gets lodged in smaller blood vessels and obstructs perfusion of alveoli. ▪ Where is the occlusion located in the body? Pulmonary artery ▪ What are the clinical manifestations of a pulmonary embolism? Variable Dyspnea most common Tachypnea Cough Chest pain Hemoptysis Crackles Wheezing Fever Syncope Change in LOC ▪ What are the treatments? Anticoagulation-low molecular weight heparin, unfractionated IV heparin, warfarin. Fibrinolytic agents – tissue plasminogen activator (tPA), alteplase (activase). ▪ What are possible causes of a pulmonary embolism? DVT in the legs Immobility Surgery Smoking Oral contraceptives ▪ How as nurses do we prevent P.E.’s? Semi-fowlers position IV access Oxygen therapy Frequent labs Emotional support and reassurance Educate the patient 39. What is a pneumothorax? Air entering the pleural cavity 40. What are the clinical manifestations of a pneumothorax? Dyspnea, decreased movement of involved chest wall, diminished or absent breath sounds on the affected side, hyper resonance to percussion. o What clinical manifestation would you see if a patient is developing a tension pneumothorax? Cyanosis, air hunger, tracheal deviation away from affected side, neck distention, violent agitation. o Why is a tension pneumothorax dangerous? Medical emergency, patient can die from inadequate cardiac output or severe hypoxemia. 41. What are possible causes of a pneumothorax? Rupture of small blebs, laceration or puncture of lung, chest trauma, compression of the lung, injury to chest wall. o What is your immediate treatment of a stab wound until a chest tube can be inserted? o What are your priority assessments when you are caring for a patient with a chest wound? Chapter 29: Nursing Management: Obstructive Pulmonary Disease 42. Asthma: a. What is the pathophysiology? Chronic inflammatory disorder of the bronchial mucosa bronchial hyper-responsiveness, airway constriction and airway obstruction. Exposure to antigen initiates innate & adaptive immune response involving dendritic cells, helper T cells, inflammatory cytokines, interleukins, B cells and eosinophils. b. What are possible triggers of asthma? Genetics Allergens Pollution Pollen Dust mites Pet dander Mold, spores Cold air Smoke c. What clinical manifestations do you expect to see? Recurrent episodes of wheezing Chest tightness Cough Shortness of breath Often worse at night or upon waking i. What is an ominous sign that a patient with asthma is decompensating? Oxygen saturation drops d. What types of medications can cause bronchospasms that mimics asthma? Aspirin, NSAIDS, B-adrenergic blockers e. What is a peak flow meter? Device that measures how well air moves out of your lungs. i. When is it used? Daily or as instructed by your provider. ii. How do you instruct a patient to use it? Take a deep breath, filling your lungs completely, place the mouthpiece in your mouth and close your lips around it. Blow as hard and fast as you can in a single blow. iii. How is it helpful? May tell you if there is narrowing of airways hour, days before symptoms occur. iv. What do the green, yellow, and red zones mean? 1. What is the treatment for each area? Green: usually 80-100% of personal best. Remain on medications Yellow: usually 50-80%, indicates caution, something is triggering asthma. May need to change or increase meds. Red: 50% or less, indicates serious problem, definitive action must be taken with health care provider. Call HCP or go to emergency room. f. What are specific types (and names) of and side effects of medications used to treat asthma? Anti-inflammatory drugs: corticosteroids, leukotriene modifiers, monoclonal antibody IgE. Side effects: candidiasis, hoarseness and dry cough. Bronchodilators: B2-adrenergic agonists, methyxanthines, anticholinergics. Side effects: dry mouth, nausea, HA, insomnia. i. When is each type utilized? Corticoid steroids are used for long term to control exacerbations and manage. Leukotriene are used for prophylactic and maintenance therapy. B-adrenergic relieves bronchospasm. Methylxanthines alleviate early phase of attacks. Anticholinergic block the bronchoconstriction effect. Used for quick relief. ii. How do you use an MDI or a DPI? Used for inhalation. 1. What are examples of each? (ex. Advair) MDI: symbicort, spiriva, albuterol DPI: asmanex, twisthaler, diskus 43. COPD: a. What two different disease make up COPD? Chronic bronchitis and emphysema o What is the pathophysiology of each? Chronic bronchitis: Presence of chronic productive cough for 3 months in each of the 2 consecutive years for a patient when other causes of chronic cough have been excluded. Also thought of as an airway obstruction that is caused by mucous hypersecretion Emphysema: Abnormal permanent enlargement of the air spaces distal to the terminal bronchioles accompanied by destruction of their walls and without obvious fibrous. Loss of elastic recoil and airflow obstruction caused by mucus hypersecretion, mucosal edema, bronchospasm that causing the defining feature of not fully reversible airflow limitation during forced exhalation. b. What are possible causes of COPD? Cigarette smoking, occupational chemicals and dust, air pollution, infection, heredity and aging. Alpha antitrypsin testing: autosomal recessive disorder that may affect lungs and liver. Genetic risk factor. c. What are clinical manifestations you would expect? Cough, sputum production, dyspnea, exposure to risk factors, use of accessory muscles, chest tightness, chronic fatigue, wheezes, tripod position, pursed lip breathing. Why do they happen? CO2 retention. Can bring air in but can’t get out. d. What medications are these patients placed on? Bronchodilators, anticholinergic, O2 therapy. o What medication should a COPD patient take before exercising? B-adrenergic agonist 10 minutes before. Why? To open up the lungs e. What type of diet do we place COPD patients on? High calorie/high protein. Why? They are burning up the calories they take in with their breathing. f. What is pursed lip breathing? Prolong exhalation and thereby prevent bronchiolar collapse and air trapping. o How do you do it? Inhale slowly and deeply through nose, exhale slowly through pursed lips, almost as if whistling. o How is it helpful? Gives the patient more control over breathing during exercise or periods of dyspnea. g. What nursing diagnosis are associated with COPD? Ineffective airway clearance, impaired gas exchange, imbalanced nutrition: less than body requirements, risk for infection and insomnia. h. Why is anxiety and depression often associated with COPD patients? Dealing with lifestyle changes that may involve decreased ability to care for themselves, loss or change in job, decreased energy for social activities. o What are nursing interventions we can do to help? Convey a sense of understanding, stress management techniques, therapist, and support groups. i. What is the nursing management of a patient with COPD? Health promotion, activity considerations, sexual activity, ambulatory and home care, sleep, psychosocial considerations. 44. Cystic Fibrosis: a. What is the pathophysiology? Cystic fibrosis is caused by defects in the cystic fibrosis gene, which codes for a protein transmembrane conductance regulator (CFTR) that functions as a chloride channel and is regulated by cyclic adenosine monophosphate (cAMP). b. What are the expected clinical manifestations? Wheezing, cough, frequent pneumonia, failure to thrive, steatorrhea (oily stool). c. What is the nursing management? Acute intervention for the patient with CF includes relief of bronchoconstriction, airway obstruction, and airflow limitation. Interventions include aggressive CPT, antibiotics, and O2therapy in severe disease. Good nutrition is important. Advances in long-term vascular access (e.g., implanted ports) and inhaled antibiotics have made administration of medication much easier. This has also eased the transition for treatment at home. [Show More]
Last updated: 1 year ago
Preview 1 out of 14 pages
Instant download
Instant download
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Aug 12, 2021
Number of pages
14
Written in
Additional information
This document has been written for:
Uploaded
Aug 12, 2021
Downloads
0
Views
30