*NURSING > CASE STUDY > Shadow Health Comprehensive Assessment Tina Jones -Documentation :Electronic Health Record (All)
Shadow Health Comprehensive Assessment Tina Jones -Documentation :Electronic Health Record
Document Content and Description Below
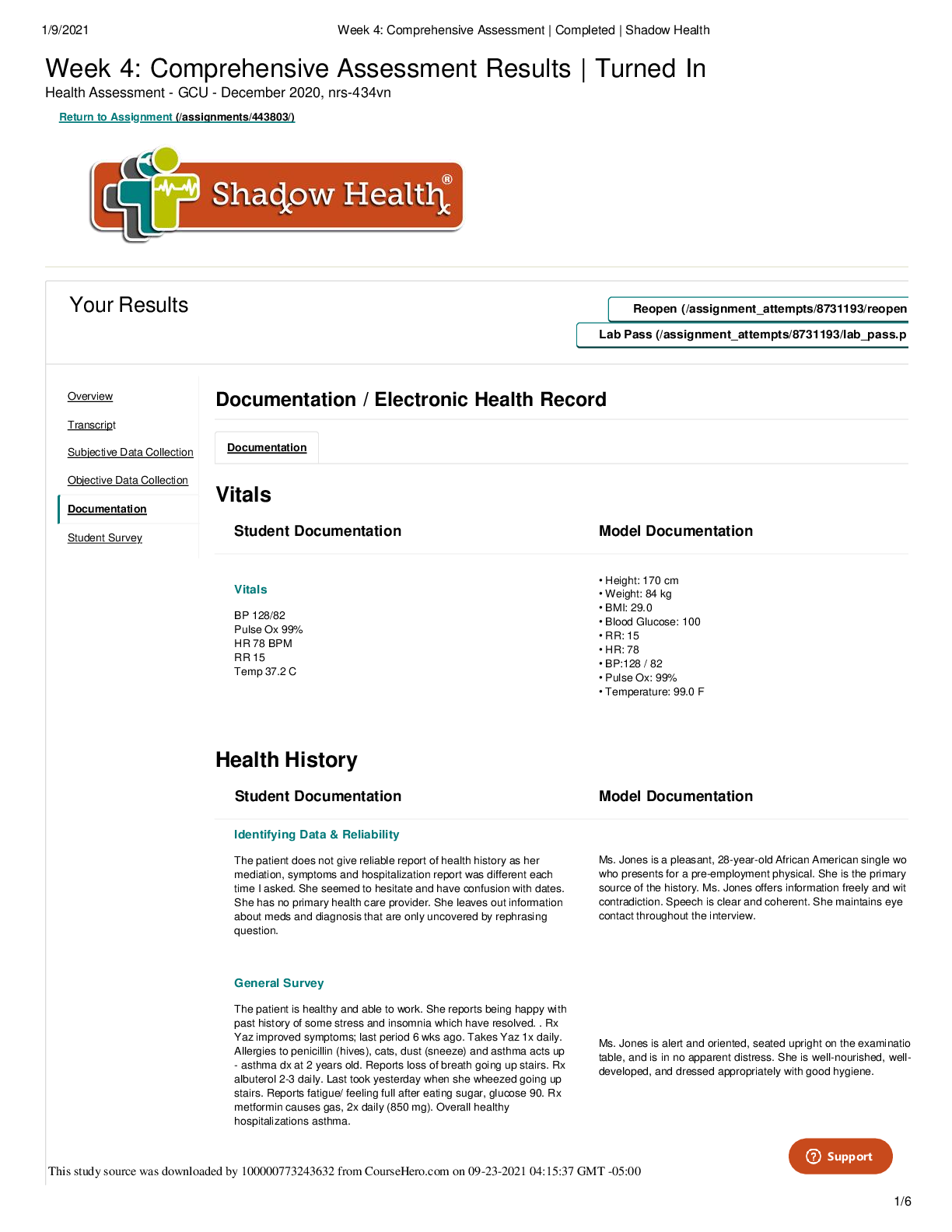
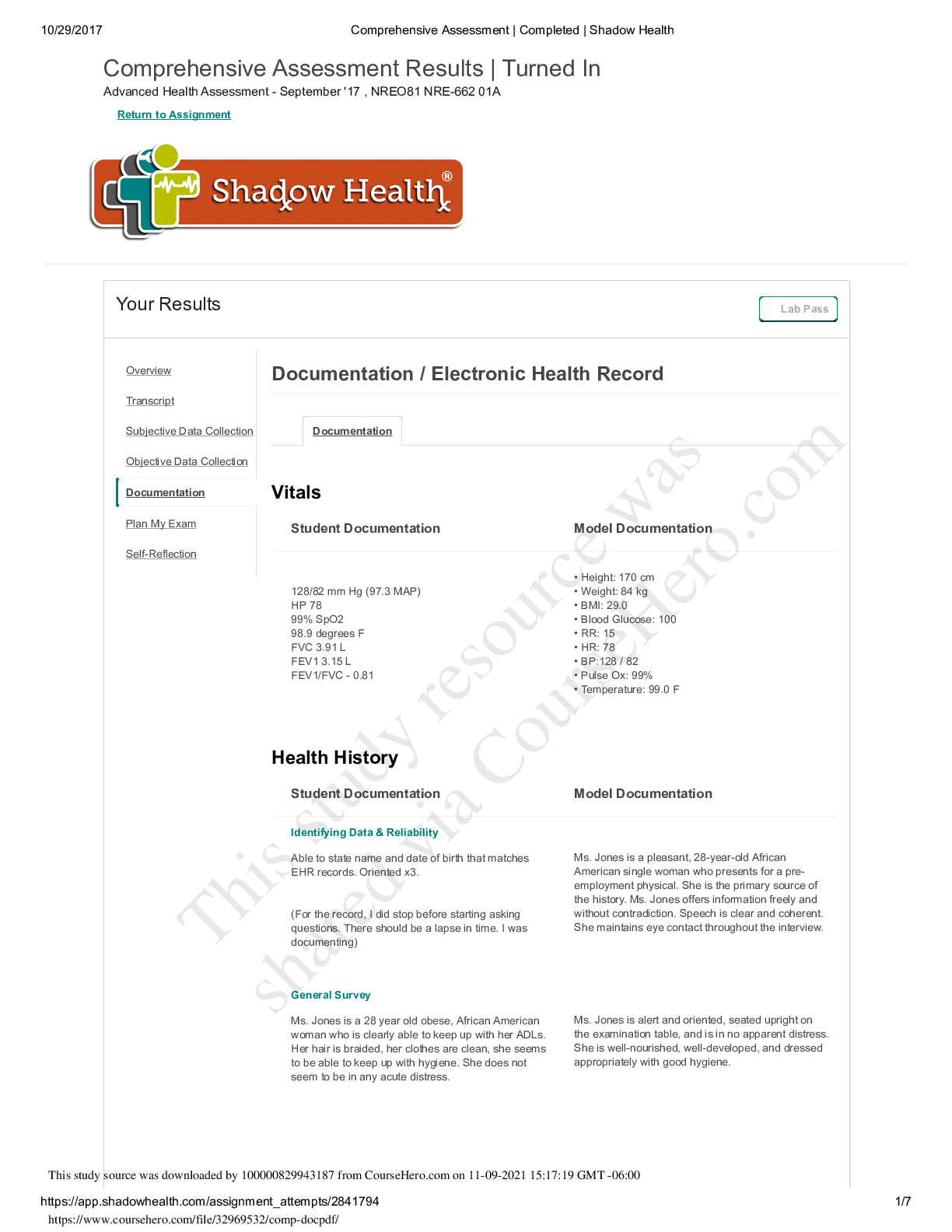
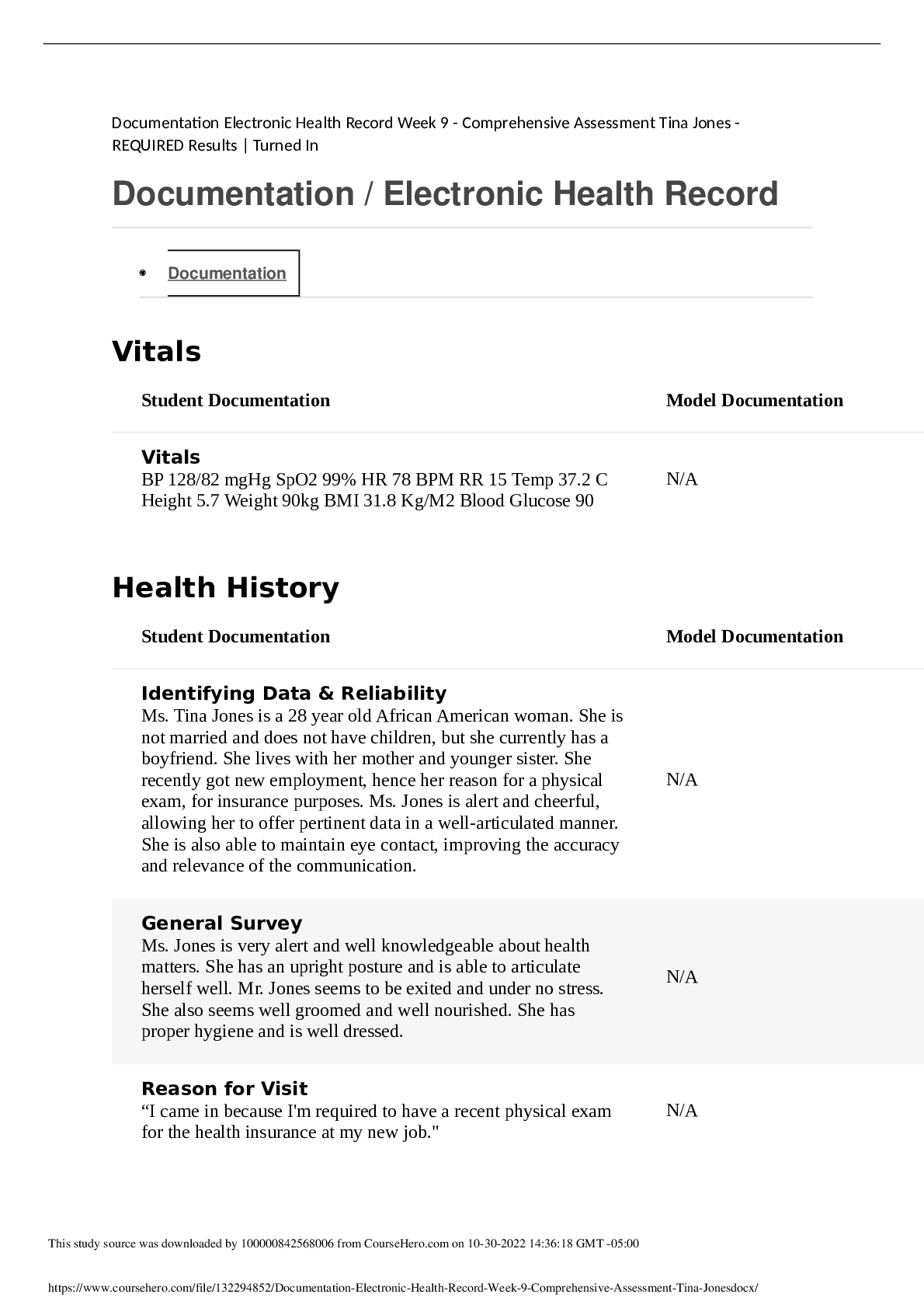
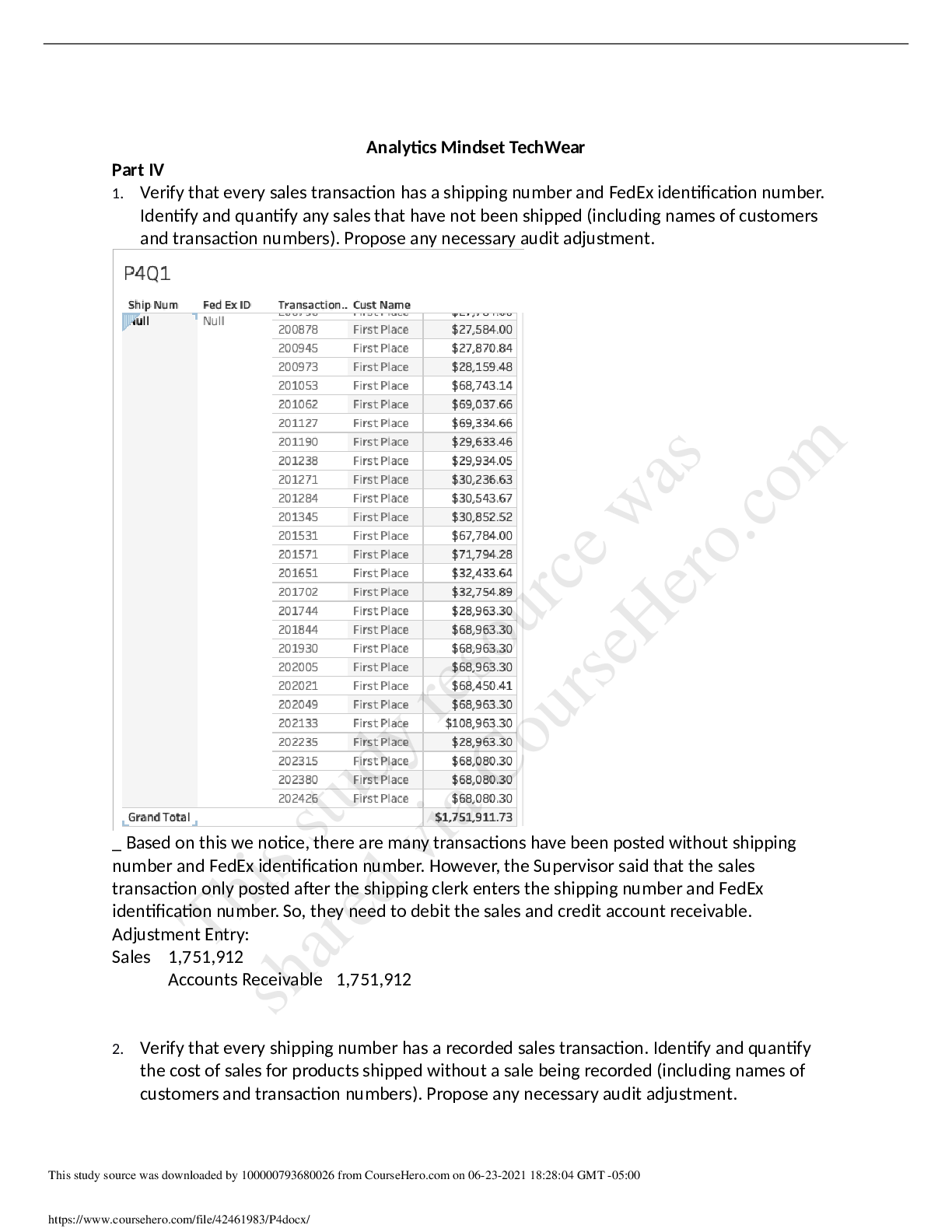
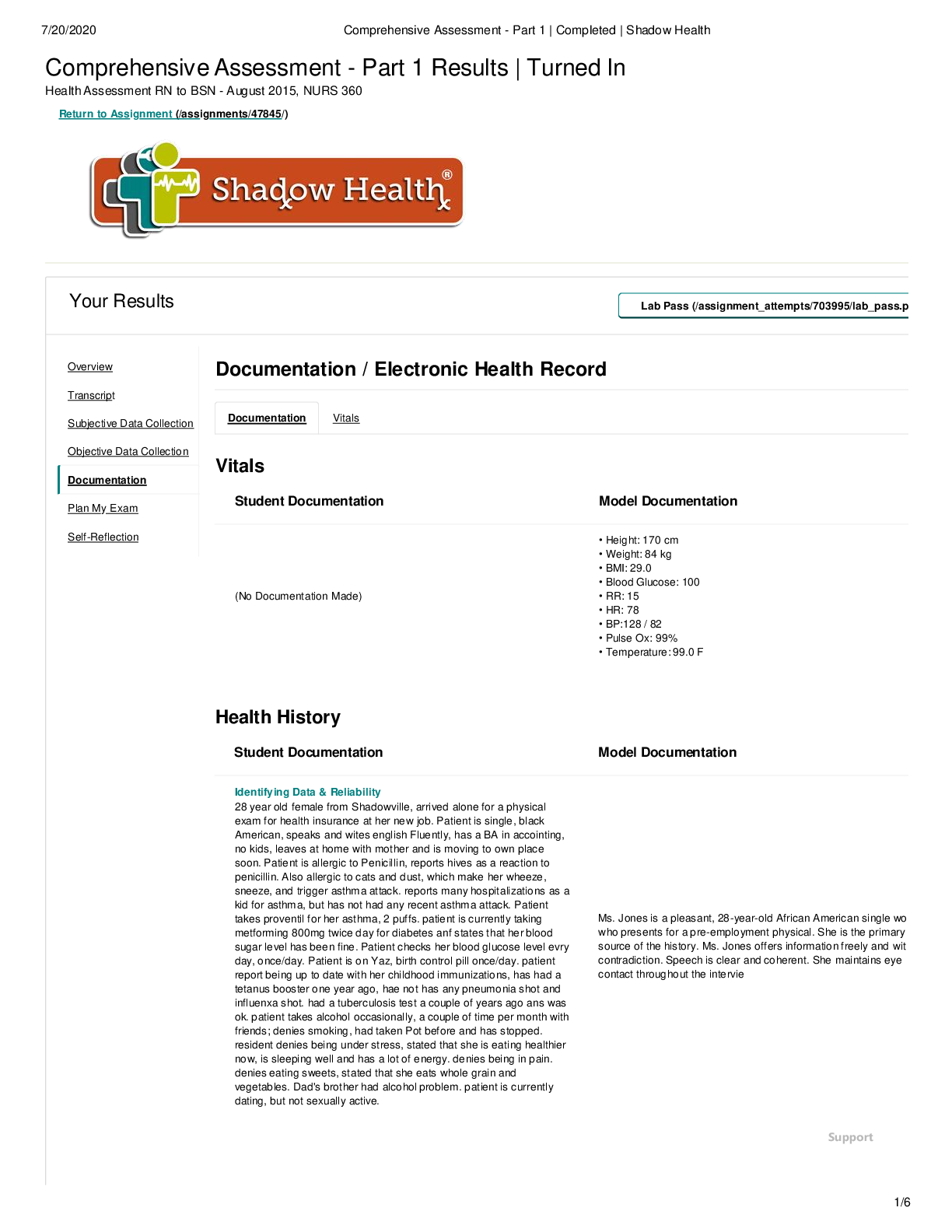
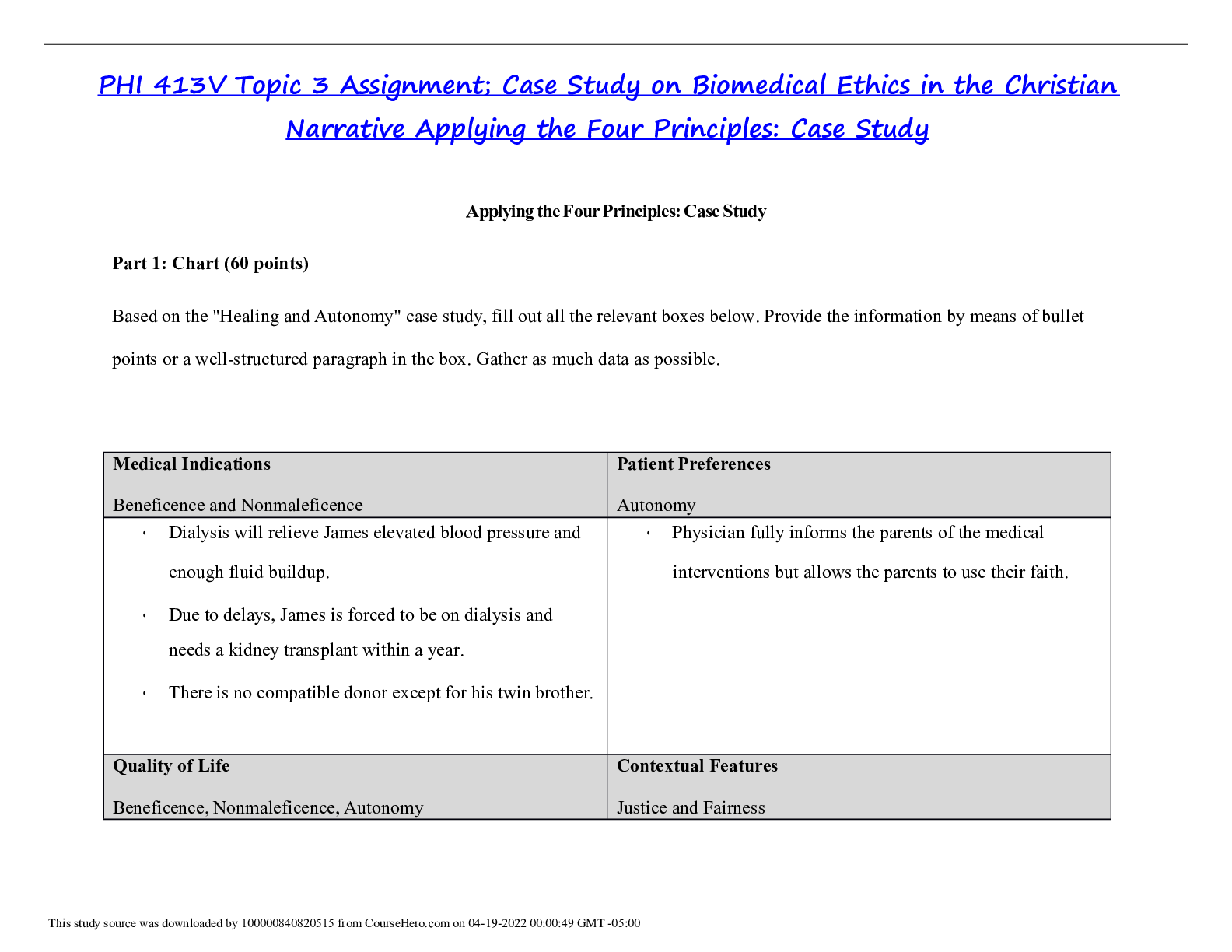
Comprehensive Assessment - Part 1 Results | Turned In Health Assessment RN to BSN - August 2015, NURS 360 Return to Assignment (/assignments/47845/) Your Results Lab Pass (/assignment_attempts/7039... 95/lab_pass.p Overview Transcript Subjective Data Collection Documentation / Electronic Health Record Documentation Vitals Objective Data Collection Documentation Plan My Exam Vitals Student Documentation Model Documentation Self-Reflection (No Documentation Made) • Height: 170 cm • Weight: 84 kg • BMI: 29.0 • Blood Glucose: 100 • RR: 15 • HR: 78 • BP:128 / 82 • Pulse Ox: 99% • Temperature: 99.0 F Health History Student Documentation Model Documentation Identifying Data & Reliability 28 year old female from Shadowville, arrived alone for a physical exam for health insurance at her new job. Patient is single, black American, speaks and wites english Fluently, has a BA in accointing, no kids, leaves at home with mother and is moving to own place soon. Patient is allergic to Penicillin, reports hives as a reaction to penicillin. Also allergic to cats and dust, which make her wheeze, sneeze, and trigger asthma attack. reports many hospitalizations as a kid for asthma, but has not had any recent asthma attack. Patient takes proventil for her asthma, 2 puffs. patient is currently taking metforming 800mg twice day for diabetes anf states that her blood sugar level has been fine. Patient checks her blood glucose level evry day, once/day. Patient is on Yaz, birth control pill once/day. patient report being up to date with her childhood immunizations, has had a tetanus booster one year ago, hae not has any pneumonia shot and influenxa shot. had a tuberculosis test a couple of years ago ans was ok. patient takes alcohol occasionally, a couple of time per month with friends; denies smoking, had taken Pot before and has stopped. resident denies being under stress, stated that she is eating healthier now, is sleeping well and has a lot of energy. denies being in pain. denies eating sweets, stated that she eats whole grain and vegetables. Dad's brother had alcohol problem. patient is currently dating, but not sexually active. Ms. Jones is a pleasant, 28-year-old African American single wo who presents for a pre-employment physical. She is the primary source of the history. Ms. Jones offers information freely and wit contradiction. Speech is clear and coherent. She maintains eye contact throughout the intervie Support 7/20/2020 Comprehensive Assessment - Part 1 | Completed | Shad [Show More]
Last updated: 1 year ago
Preview 1 out of 7 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Sep 13, 2021
Number of pages
7
Written in
Additional information
This document has been written for:
Uploaded
Sep 13, 2021
Downloads
0
Views
290

.png)

.png)