NUR 1211 Cardiovascular 2, Questions and Answers ,100% CORRECT
Document Content and Description Below
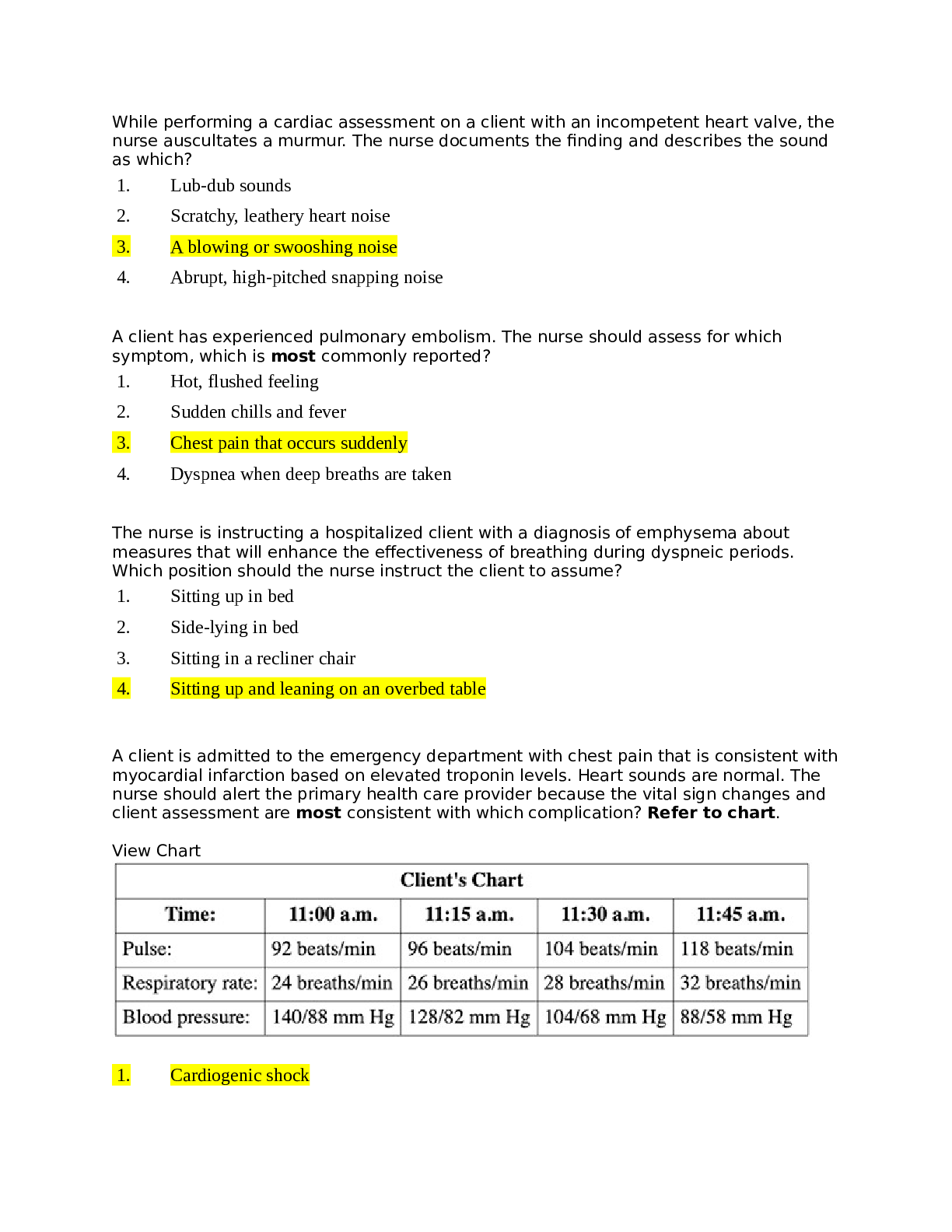
NUR 1211 Cardiovascular 2, Questions and Answers While performing a cardiac assessment on a client with an incompetent heart valve, the nurse auscultates a murmur. The nurse documents the finding an... d describes the sound as which? 1. Lub-dub sounds 2. Scratchy, leathery heart noise 3. A blowing or swooshing noise 4. Abrupt, high-pitched snapping noise A client has experienced pulmonary embolism. The nurse should assess for which symptom, which is most commonly reported? 1. Hot, flushed feeling 2. Sudden chills and fever 3. Chest pain that occurs suddenly 4. Dyspnea when deep breaths are taken The nurse is instructing a hospitalized client with a diagnosis of emphysema about measures that will enhance the effectiveness of breathing during dyspneic periods. Which position should the nurse instruct the client to assume? 1. Sitting up in bed 2. Side-lying in bed 3. Sitting in a recliner chair 4. Sitting up and leaning on an overbed table A client is admitted to the emergency department with chest pain that is consistent with myocardial infarction based on elevated troponin levels. Heart sounds are normal. The nurse should alert the primary health care provider because the vital sign changes and client assessment are most consistent with which complication? Refer to chart. View Chart 1. Cardiogenic shock 2. Cardiac tamponade 3. Pulmonary embolism 4. Dissecting thoracic aortic aneurysm A client in sinus bradycardia, with a heart rate of 45 beats per minute and blood pressure of 82/60 mm Hg, reports dizziness. Which intervention should the nurse anticipate will be prescribed? 1. Administer digoxin. 2. Defibrillate the client. 3. Continue to monitor the client. 4. Prepare for transcutaneous pacing. The nurse in a medical unit is caring for a client with heart failure. The client suddenly develops extreme dyspnea, tachycardia, and lung crackles. The nurse immediately asks another nurse to contact the primary health care provider and prepares to implement which priority interventions? Select all that apply. 1. Administering oxygen 2. Inserting a Foley catheter 3. Administering furosemide 4. Administering morphine sulfate intravenously 5. Transporting the client to the coronary care unit 6. Placing the client in a low-Fowler's side-lying position A client with myocardial infarction suddenly becomes tachycardic, shows signs of air hunger, and begins coughing frothy, pink-tinged sputum. Which finding would the nurse anticipate when auscultating the client's breath sounds? 1. Stridor 2. Crackles 3. Scattered rhonchi 4. Diminished breath sounds A client with myocardial infarction is developing cardiogenic shock. What condition should the nurse carefully assess the client for? 1. Pulsus paradoxus 2. Ventricular dysrhythmias 3. Rising diastolic blood pressure 4. Falling central venous pressure A client who had cardiac surgery 24 hours ago has had a urine output averaging 20 mL/hr for 2 hours. The client received a single bolus of 500 mL of intravenous fluid. Urine output for the subsequent hour was 25 mL. Daily laboratory results indicate that the blood urea nitrogen level is 45 mg/dL (16 mmol/L) and the serum creatinine level is 2.2 mg/dL (194 mcmol/L). On the basis of these findings, the nurse would anticipate that the client is at risk for which problem? 1. Hypovolemia 2. Acute kidney injury 3. Glomerulonephritis 4. Urinary tract infection The nurse is reviewing an electrocardiogram rhythm strip. The P waves and QRS complexes are regular. The PR interval is 0.16 seconds, and QRS complexes measure 0.06 seconds. The overall heart rate is 64 beats per minute. Which action should the nurse take? 1. Check vital signs. 2. Check laboratory test results. 3. Monitor for any rhythm change. 4. Notify the primary health care provider. A client is wearing a continuous cardiac monitor, which begins to sound its alarm. The nurse sees no electrocardiographic complexes on the screen. Which is the priority nursing action? 1. Call a code. 2. Check the client's status. 3. Call the primary health care provider. 4. Document the lack of complexes. The nurse is watching the cardiac monitor and notices that a client's rhythm suddenly changes. There are no P waves, the QRS complexes are wide, and the ventricular rate is regular but more than 140 beats per minute. The nurse determines that the client is experiencing which dysrhythmia? 1. Sinus tachycardia 2. Ventricular fibrillation 3. Ventricular tachycardia 4. Premature ventricular contractions A client has frequent bursts of ventricular tachycardia on the cardiac monitor. What should the nurse be most concerned about with this dysrhythmia? 1. It can develop into ventricular fibrillation at any time. 2. It is almost impossible to convert to a normal rhythm. 3. It is uncomfortable for the client, giving a sense of impending doom. 4. It produces a high cardiac output with cerebral and myocardial ischemia. A client is having frequent premature ventricular contractions. The nurse should place priority on assessment of which item? 1. Causative factors, such as caffeine 2. Sensation of fluttering or palpitations 3. Blood pressure and oxygen saturation 4. Precipitating factors, such as infection he client has developed atrial fibrillation, with a ventricular rate of 150 beats per minute. The nurse should assess the client for which associated signs and/or symptoms? Select all that apply. 1. Syncope 2. Dizziness 3. Palpitations 4. Hypertension 5. Flat neck veins The nurse is watching the cardiac monitor, and a client's rhythm suddenly changes. There are no P waves; instead, there are fibrillatory waves before each QRS complex. How should the nurse interpret the client's heart rhythm? 1. Atrial fibrillation 2. Sinus tachycardia 3. Ventricular fibrillation 4. Ventricular tachycardia The nurse is assisting to defibrillate a client in ventricular fibrillation. After placing the pads on the client's chest and before discharging the device, which intervention is a priority? 1. Ensure that the client has been intubated. 2. Set the defibrillator to the "synchronize" mode. 3. Administer an amiodarone bolus intravenously. 4. Confirm that the rhythm is ventricular fibrillation. The nurse is evaluating a client's response to cardioversion. Which assessment would be the priority? 1. Blood pressure 2. Airway patency 3. Oxygen flow rate 4. Level of consciousness The nurse is evaluating the condition of a client after pericardiocentesis performed to treat cardiac tamponade. Which observation would indicate that the procedure was effective? 1. Muffled heart sounds 2. Client reports dyspnea 3. A rise in blood pressure 4. Jugular venous distention The nurse notes that a client with sinus rhythm has a premature ventricular contraction that falls on the T wave of the preceding beat. The client's rhythm suddenly changes to one with no P waves, no definable QRS complexes, and coarse wavy lines of varying amplitude. How should the nurse interpret this rhythm? 1. Asystole 2. Atrial fibrillation 3. Ventricular fibrillation 4. Ventricular tachycardia A client receiving thrombolytic therapy with a continuous infusion of alteplase suddenly becomes extremely anxious and reports itching. The nurse hears stridor and notes generalized urticaria and hypotension. Which interventions are a priority? Select all that apply. 1. Stop the infusion. 2. Raise the head of the bed. 3. Administer protamine sulfate. 4. Administer diphenhydramine. 5. Call for the Rapid Response Team (RRT). The nurse is caring for a client hospitalized for heart failure exacerbation and suspects the client may be entering a state of shock. The nurse knows that which intervention is the priority for this client? 1. Administration of digoxin 2. Administration of whole blood 3. Administration of intravenous fluids 4. Administration of packed red blood cells Which clinical findings are consistent with sepsis diagnostic criteria? Select all that apply. 1. Urine output 50 mL/hr 2. Hypoactive bowel sounds 3. Temperature of 102° F (38.9° C) 4. Heart rate of 96 beats per minute 5. Mean arterial pressure 65 mm Hg 6. Systolic blood pressure 110 mm Hg The nurse is evaluating the condition of a client after pericardiocentesis performed to treat cardiac tamponade. Which observation would indicate that the procedure was effective? 1. Muffled heart sounds 2. A rise in blood pressure 3. Jugular venous distention 4. Client expressions of dyspnea A client with variant angina is scheduled to receive an oral calcium channel blocker twice daily. Which statement by the client indicates the need for further teaching? 1. "I should notify my doctor if my feet or legs start to swell." 2. "My doctor told me to call his office if my pulse rate decreases below 60." 3. "Avoiding grapefruit juice will definitely be a challenge for me, since I usually drink it every morning with breakfast." 4. "My spouse told me that since I have developed this problem, we are going to stop walking in the mall every morning." he nurse is monitoring a client with acute pericarditis for signs of cardiac tamponade. Which assessment finding indicates the presence of this complication? 1. Flat neck veins 2. A pulse rate of 60 beats/minute 3. Muffled or distant heart sounds 4. Wheezing on auscultation of the lungs The nurse is developing a plan of care for a client with varicose veins in whom skin breakdown occurred over the varicosities as a result of secondary infection. Which is a priority intervention? 1. Keep the legs aligned with the heart. 2. Elevate the legs higher than the heart. 3. Clean the skin with alcohol every hour. 4. Position the client onto the side during every shift. The nurse is caring for a client with cardiac disease who has been placed on a cardiac monitor. The nurse notes that the client has developed atrial fibrillation and has a rapid ventricular rate of 150 beats/minute. The nurse should next assess the client for which finding? 1. Hypotension 2. Flat neck veins 3. Complaints of nausea 4. Complaints of headache The nurse is performing an assessment on a client with a diagnosis of left-sided heart failure. Which assessment component would elicit specific information regarding the client's left-sided heart function? 1. Listening to lung sounds 2. Palpating for organomegaly 3. Assessing for jugular vein distention 4. Assessing for peripheral and sacral edema A home care nurse is visiting a client to provide follow-up evaluation and care of a leg ulcer. On removing the dressing from the leg ulcer, the nurse notes that the ulcer is pale and deep and that the surrounding tissue is cool to the touch. The nurse should document that these findings identify which type of ulcer? 1. A stage 1 ulcer 2. A vascular ulcer 3. An arterial ulcer 4. A venous stasis ulcer The nurse is developing a plan of care for a client who will be admitted to the hospital with a diagnosis of deep vein thrombosis (DVT) of the right leg. The nurse develops the plan, expecting that the primary health care provider (PHCP) will most likely prescribe which option? 1. Maintain activity level as prescribed. 2. Maintain the affected leg in a dependent position. 3. Administer an opioid analgesic every 4 hours around the clock. 4. Apply cool packs to the affected leg for 20 minutes every 4 hours. A client with a diagnosis of angina pectoris is hospitalized for an angioplasty. The client returns to the nursing unit after the procedure, and the nurse provides instructions to the client regarding home care measures. Which statement, if made by the client, indicates an understanding of the instructions? 1. "I need to cut down on cigarette smoking." 2. "I am so relieved that my heart is repaired." 3. "I need to adhere to my dietary restrictions." 4. "I am so relieved that I can eat anything I want to now." The nurse has provided dietary instructions to a client with coronary artery disease. Which statement by the client indicates an understanding of the dietary instructions? 1. "I'll need to become a strict vegetarian." 2. "I should use polyunsaturated oils in my diet." 3. "I need to substitute eggs and whole milk for meat." 4. "I should eliminate all cholesterol and fat from my diet." A client is scheduled for a cardiac catheterization to diagnose the extent of coronary artery disease. The nurse places highest priority on telling the client to report which sensation during the procedure? 1. Chest pain 2. Urge to cough 3. Warm, flushed feeling 4. Pressure at the insertion site A client admitted to the hospital with coronary artery disease complains of dyspnea at rest. The nurse caring for the client uses which item as the best means to monitor respiratory status on an ongoing basis? 1. Apnea monitor 2. Oxygen flowmeter 3. Telemetry cardiac monitor 4. Oxygen saturation monitor The nurse is listening to a lecture about angina. Which statement by the nurse indicates that the teaching has been effective? 1. "Stable angina is chronic." 2. "Variant angina is caused by emotional stress." 3. "Unstable angina is not a life-threatening condition." 4. "Intractable angina rarely limits the client's lifestyle." The nurse has completed an educational course covering first-degree heart block. Which statement by the nurse indicates that teaching has been effective? 1. "Presence of Q waves indicates first-degree heart block." 2. "Tall, peaked T waves indicate first-degree heart block." 3. "Widened QRS complexes indicate first-degree heart block." 4. "Prolonged, equal PR intervals indicate first-degree heart block." The nurse working in a long-term care facility is assessing a client who is experiencing chest pain. The nurse should interpret that the pain is most likely caused by myocardial infarction (MI) on the basis of what assessment finding? 1. The client is not experiencing dyspnea. 2. The client is not experiencing nausea or vomiting. 3. The pain has not been relieved by rest and nitroglycerin tablets. 4. The client says the pain began while she was trying to open a stuck dresser drawer. A hospitalized client has been diagnosed with heart failure as a complication of hypertension. In explaining the disease process to the client, the nurse identifies which chamber of the heart as primarily responsible for the symptoms? 1. Left atrium 2. Right atrium 3. Left ventricle 4. Right ventricle The nurse has just completed education on myocardial infarction (MI) to a group of new nurses. Which statement made by one of the nurses indicates that the teaching has been effective? 1. "Chest pain is caused by tissue hypoxia in the myocardium." 2. "Chest pain is caused by tissue hypoxia in the vessels of the heart." 3. "Chest pain is caused by tissue hypoxia in the parietal pericardium." 4. "Chest pain is caused by tissue hypoxia in the visceral pericardium." The registered nurse (RN) is educating a new nurse on mitral stenosis. Which statement by the new nurse indicates that the teaching has been effective? 1. "Left ventricle to aorta narrowing will impede flow of blood." 2. "Left atrium to left ventricle narrowing will impede flow of blood." 3. "Right atrium to right ventricle narrowing will impede flow of blood." 4. "Right ventricle to pulmonary artery narrowing will impede flow of blood." The registered nurse (RN) is educating a new nurse about aortic regurgitation. Which statement by the new nurse indicates that the teaching has been effective? 1. "Failure of the aortic valve to close completely allows blood to flow retrograde through the aorta to the left ventricle." 2. "Failure of the aortic valve to close completely allows blood to flow retrograde through the left ventricle to the left atrium." 3. "Failure of the aortic valve to close completely allows blood to flow retrograde through the right ventricle to the right atrium." 4. "Failure of the aortic valve to close completely allows blood to flow retrograde through the pulmonary artery to the right ventricle." Which laboratory test results may be associated with peaked or tall, tented T waves on a client's electrocardiogram (ECG)? 1. Chloride level of 98 mEq/L (98 mmol/L) 2. Sodium level of 135 mEq/L (135 mmol/L) 3. Potassium level of 6.8 mEq/L (6.8 mmol/L) 4. Magnesium level of 1.6 mEq/L (0.8 mmol/L) A client's electrocardiogram (ECG) strip shows atrial and ventricular rates of 70 complexes/minute. The PR interval is 0.16 second, the QRS complex measures 0.06 second, and the PP interval is slightly irregular. How should the nurse report this rhythm? 1. Sinus tachycardia 2. Sinus bradycardia 3. Sinus dysrhythmia 4. Normal sinus rhythm The new registered nurse (RN) is reviewing cardiac rhythms with a mentor. Which statement by the new RN indicates that teaching about ventricular fibrillation has been effective? 1. "Ventricular fibrillation appears as irregular beats within a rhythm." 2. "Ventricular fibrillation does not have P waves or QRS complexes." 3. "Ventricular fibrillation is a regular pattern of wide QRS complexes." 4. "Ventricular fibrillation has recognizable P waves, QRS complexes, and T waves." A client with myocardial infarction is experiencing new, multiform premature ventricular contractions and short runs of ventricular tachycardia. The nurse plans to have which medication available for immediate use to treat the ventricular tachycardia? 1. Digoxin 2. Verapamil 3. Acebutolol 4. Amiodarone A client has received antidysrhythmic therapy for the treatment of premature ventricular contractions (PVCs). The nurse evaluates this therapy as most effective if which finding is noted with regard to the PVCs? 1. They occur in pairs. 2. They appear to be multifocal. 3. They fall on the second half of the T wave. 4. They decrease to a frequency of less than 6 per minute. A client with a complete heart block has had a permanent demand ventricular pacemaker inserted. The nurse assesses for proper pacemaker function by examining the electrocardiogram (ECG) strip for the presence of pacemaker spikes at what point? 1. Before each P wave 2. Just after each P wave 3. Just after each T wave 4. Before each QRS complex The nurse is planning care for a client with deep vein thrombosis of the right leg. Which interventions would the nurse plan, based on the primary health care provider's (PHCP's) prescriptions? Select all that apply. 1. Elevation of the right leg 2. Administration of acetaminophen 3. Application of moist heat to the right leg 4. Monitoring for signs of pulmonary embolism 5. Ambulation around the nursing unit every hour A client has been diagnosed with thromboangiitis obliterans (Buerger's disease). The nurse is identifying measures to help the client cope with lifestyle changes needed to control the disease process. The nurse plans to refer the client to which member of the health care team? 1. Dietitian 2. Medical social worker 3. Pain management clinic 4. Smoking cessation program The nurse is planning to teach a client with peripheral arterial disease about measures to limit disease progression. Which items should the nurse include on a list of suggestions for the client? Select all that apply. 1. Soak the feet in hot water daily. 2. Be careful not to injure the legs or feet. 3. Use a heating pad on the legs to aid vasodilation. 4. Walk each day to increase circulation to the legs. 5. Cut down on the amount of fats consumed in the diet. The home health nurse visits a client recovering after an episode of cardiogenic shock secondary to an anterior myocardial infarction (MI) and provides home care instructions to the client. Which statement by the client indicates an understanding of these home care measures? 1. "I exercise every day after breakfast." 2. "I've gained 8 lb (3.6 kg) since discharge." 3. "I take an antacid when I experience epigastric pain." 4. "I have planned periods of rest at 10:00 a.m. and 3:00 p.m. daily." The nurse notes that a client's cardiac rhythm shows absent P waves, no PR interval, and an irregular rhythm. How should the nurse interpret this rhythm? 1. Bradycardia 2. Tachycardia 3. Atrial fibrillation 4. Normal sinus rhythm (NSR) The nurse is assigned the care of a client with a diagnosis of heart failure who is receiving intravenous doses of furosemide. The client is attached to cardiac telemetry, and the nurse is monitoring the client's cardiac status. The nurse notes that the client's cardiac rhythm has changed to this pattern. The nurse determines that the most likely cause of this cardiac rhythm in the client is which problem? Refer to figure. 1. Pacemaker dysfunction 2. The presence of hypokalemia 3.The effectiveness of the furosemide 4.An impending myocardial infarction (MI) A client is attached to a cardiac monitor, and the nurse notes the presence of this cardiac rhythm on the monitor. The nurse quickly assesses the client, knowing that this rhythm is indicative of which rhythm? Refer to figure 1. Atrial fibrillation 2. Ventricular fibrillation (VF) 3. Ventricular tachycardia (VT) 4. Premature ventricular complexes The post–myocardial infarction client is scheduled for a technetium-99m ventriculography (multigated acquisition [MUGA] scan). The nurse ensures that which item is in place before the procedure? 1. A urinary catheter 2. Signed informed consent 3. A central venous pressure (CVP) line 4. Notation of allergies to iodine or shellfish The nurse is teaching a client with cardiomyopathy about home care safety measures. The nurse should address with the client which most important measure to ensure client safety? 1. Assessing pain 2. Administering vasodilators 3. Avoiding over-the-counter (OTC) medications 4. Moving slowly from a sitting to a standing position A client is scheduled for elective cardioversion to treat chronic high-rate atrial fibrillation. Which finding indicates that further preparation is needed for the procedure? 1. The client's digoxin has been withheld for the last 48 hours. 2. The client is wearing a nasal cannula delivering oxygen at 2 L/min. 3. The defibrillator has the synchronizer turned on and is set at 120 joules (J). 4. The client has received an intravenous dose of a conscious sedation medication. The nurse is assisting in the care of a client scheduled for cardioversion. The nurse plans to set the defibrillator to which starting energy range level, depending on the specific emergency health care provider (HCP) prescription? 1. 120 joules 2. 200 joules 3. 250 joules 4. 350 joules A client has developed uncontrolled atrial fibrillation with a ventricular rate of 150 beats/min. What manifestation should the nurse observe for when performing the client's focused assessment? 1. Flat neck veins 2. Nausea and vomiting 3. Hypotension and dizziness 4. Clubbed fingertips and headache The nurse is performing an admission assessment on a client with a diagnosis of Raynaud's disease. How should the nurse assess for this disease? 1. Checking for a rash on the digits 2. Observing for softening of the nails or nail beds 3. Palpating for a rapid or irregular peripheral pulse 4. Palpating for diminished or absent peripheral pulses The primary health care provider prescribes limited activity (bed rest and bathroom only) for a client who developed deep vein thrombosis (DVT) after surgery. What interventions should the nurse plan to include in the client's plan of care? Select all that apply. 1. Encourage coughing with deep breathing. 2. Place in high-Fowler's position for eating. 3. Encourage increased oral intake of water daily. 4. Place thigh-length elastic stockings on the client. 5. Place sequential compression boots on the client. 6. Encourage the intake of dark green, leafy vegetables. Spironolactone is prescribed for a client with heart failure. In providing dietary instructions to the client, the nurse identifies the need to avoid foods that are high in which electrolyte? 1. Calcium 2. Potassium 3. Magnesium 4. Phosphorus The nurse is giving discharge instructions to a client who has just undergone vein ligation and stripping. The nurse evaluates that the client understands activity and positioning limitations if the client states that which action is appropriate to do? 1. Walk for as long as possible each day. 2. Cross the legs at the ankle only, not at the knee. 3. Sit in a chair 3 times a day for 3 hours at a time. 4. Lie down with the legs elevated and avoid sitting. Endovenous laser treatment (EVLT) is done on a client with varicose veins. Which interventions should the nurse include in the postprocedure plan of care? 1. Inform the client that the EVLT procedure ensures closure of the treated vein. 2. Assess color and temperature of the affected limb to determine vascular status. 3. Teach the client the importance of using graduated compression stockings (GCSs) during the day. 4. Inform the client that circulation impairment and nerve damage is expected to occur following the procedure. The nurse is conducting a health history of a client with a primary diagnosis of heart failure. Which conditions reported by the client could play a role in exacerbating the heart failure? Select all that apply. 1 Emotional stress . 2 Atrial fibrillation . 3 Nutritional anemia . 4 Peptic ulcer disease . 5 Recent upper respiratory infection . A client with pulmonary edema has been receiving diuretic therapy. The client has a prescription for additional furosemide in the amount of 40 mg intravenous push. Knowing that the client will also be started on digoxin, which laboratory result should the nurse review as the priority? 1. Sodium level 2. Digoxin level 3. Creatinine level 4. Potassium level A client is at risk for vasovagal attacks that cause bradydysrhythmias. The nurse would tell the client to avoid which actions to prevent this occurrence? Select all that apply. 1. Applying pressure on the eyes 2. Raising the arms above the head 3. Taking stool softeners on a daily basis 4. Bearing down during a bowel movement 5. Simulating a gag reflex when brushing the teeth The nurse employed in a cardiac unit determines that which client is the least likely to have an implanted cardioverter-defibrillator (ICD) inserted? 1. A client with syncopal episodes related to ventricular tachycardia 2. A client with ventricular dysrhythmias despite medication therapy 3. A client with an episode of cardiac arrest related to myocardial infarction 4. A client with 3 episodes of cardiac arrest unrelated to myocardial infarction The nurse is caring for a client immediately after insertion of a permanent demand pacemaker via the right subclavian vein. Which activity will assist with preventing dislodgement of the pacing catheter? 1. Limiting both movement and abduction of the left arm 2. Limiting both movement and abduction of the right arm 3. Assisting the client to get out of bed and ambulate with a walker 4. Having the physical therapist do active range-of-motion exercises to the right arm A client seeks treatment in a vascular surgeon's office for unsightly varicose veins, and radiofrequency ablation (RFA) is recommended. Before leaving the examining room, the client says to the nurse, "Can you tell me again how this is done?" Which statement should the nurse make? 1. "The varicosity is surgically removed." 2. "A heating element is used to occlude the vein." 3. "The vein is tied off at the upper end to prevent stasis from occurring." 4. "The vein is tied off at the lower end to prevent stasis from occurring." A client is scheduled for a cardiac catheterization using an iodine agent. Which assessment is most critical before the procedure? 1. Intake and output 2. Height and weight 3. Baseline peripheral pulse rates 4. Previous allergy to contrast agents The nurse is assessing a client with an abdominal aortic aneurysm. Which assessment finding by the nurse is unrelated to the aneurysm? 1. Pulsatile abdominal mass 2. Hyperactive bowel sounds in the area 3. Systolic bruit over the area of the mass 4. Subjective sensation of "heart beating" in the abdomen The nurse is providing postoperative care for a client who had a percutaneous insertion of an inferior vena cava filter and was on heparin therapy before surgery. The nurse should be most concerned about monitoring for which potential complications? 1. Bleeding and infection 2. Thrombosis and infection 3. Bleeding and wound dehiscence 4. Wound dehiscence and evisceration The nurse is preparing to ambulate a client on the third day after cardiac surgery. What should the nurse plan to do to enable the client to best tolerate the ambulation? 1 Remove telemetry equipment. . 2 Provide the client with a walker. . 3 Premedicate the client with an analgesic. . 4 Encourage the client to cough and breathe deeply. . The nurse is evaluating a client's cardiac rhythm strip to determine if there is proper function of the VVI mode pacemaker. Which denotes proper functioning? 1. Spikes precede all P waves and QRS complexes. 2. There are consistent spikes before each P wave. 3. Spikes occur before QRS complexes when intrinsic ventricular beats do not occur. 4. Spikes occur before all QRS complexes regardless of intrinsic ventricular activity. The nurse determines that a client requires further teaching after permanent pacemaker insertion if which statement is made? 1. "I'll need to call my cardiologist if I feel tired or dizzy." 2. "My pulse rate should be less than what my pacemaker is set at." 3. "I'll have to avoid carrying the grocery bags into the house for the next 6 weeks." 4. "It's safe to use my microwave as long it is properly grounded and well shielded." The nurse is assessing a client newly diagnosed with mild hypertension. Which assessment finding should the nurse expect? 1. Asymptomatic 2. Shortness of breath 3. Visual disturbances 4. Frequent nosebleeds The nurse is caring for a client with heart failure. On assessment, the nurse notes that the client is dyspneic, and crackles are audible on auscultation. What additional manifestations would the nurse expect to note in this client if excess fluid volume is present? 1 Weight loss and dry skin . 2 Flat neck and hand veins and decreased urinary output . 3 An increase in blood pressure and increased respirations . 4 Weakness and decreased central venous pressure (CVP) . The nurse is caring for a client with Crohn's disease who has a calcium level of 8 mg/dL (2 mmol/L). Which patterns would the nurse watch for on the electrocardiogram? Select all that apply. 1. U waves 2. Widened T wave 3. Prominent U wave 4. Prolonged QT interval 5. Prolonged ST segment The nurse manager is teaching the nursing staff about signs and symptoms related to hypercalcemia in a client with metastatic prostate cancer and tells the staff that which is a late sign or symptom of this oncological emergency? 1. Headache 2. Dysphagia 3. Constipation 4. Electrocardiographic changes [Show More]
Last updated: 1 year ago
Preview 1 out of 39 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Sep 30, 2021
Number of pages
39
Written in
Additional information
This document has been written for:
Uploaded
Sep 30, 2021
Downloads
0
Views
16












 (1).png)