NURSING 602 Module 7 Questions for Self-Study,100% CORRECT
Document Content and Description Below
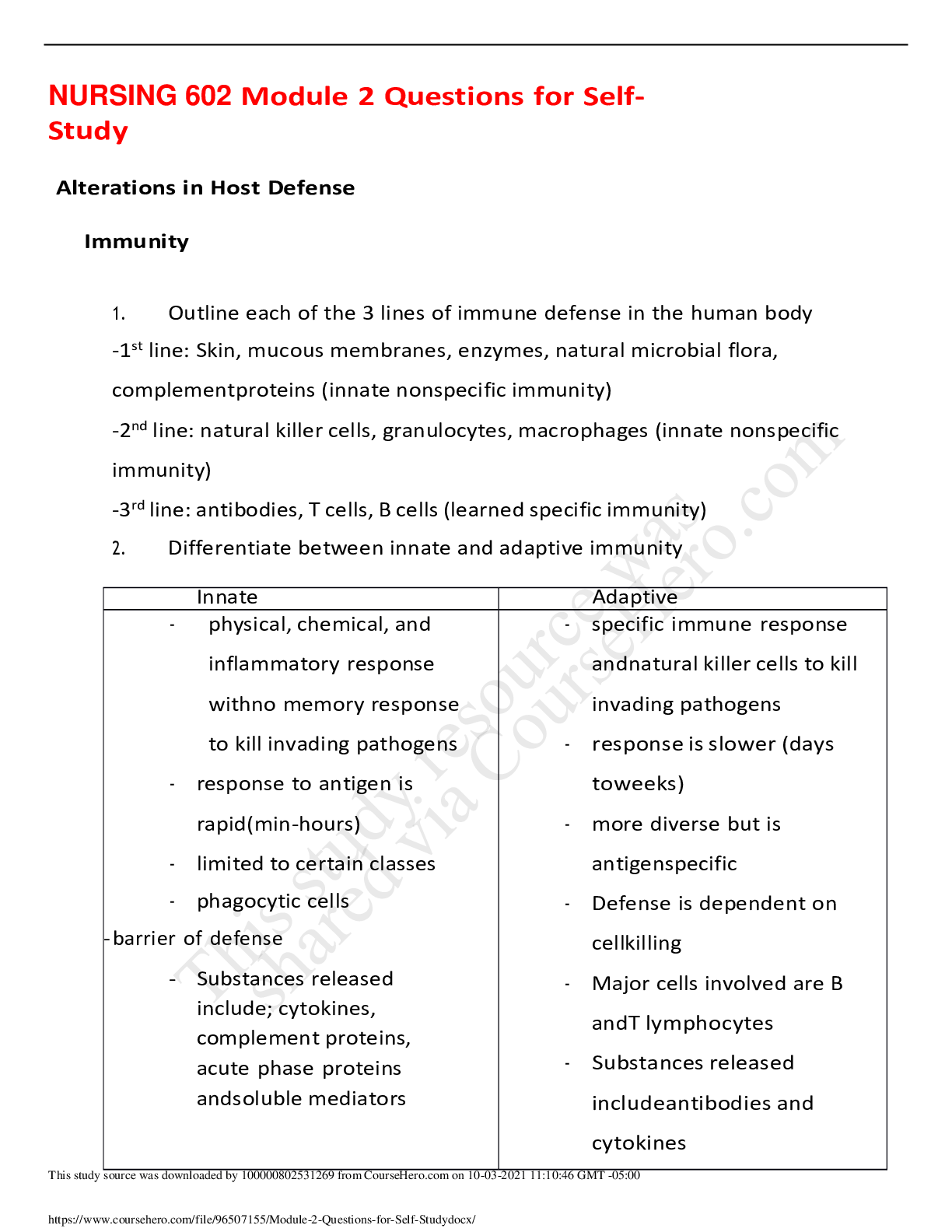
NURSING 602 Module 7 Questions for Self-Study Determinants of Cardiac Output 1. Detail the determinants of cardiac output a. Heart Rate – Beats per minute. Influenced by positive (catacholami... nes) and negative chronotropes. i. Temperature via the Q10 effect (the factor by which the rate of a reaction increases for every 10 degree rise in temperature) will increase heart rate. The temperature effects on heart rate are mediated via increases in metabolic rate. Importantly, a heart rate of greater than 200 beats per minute will reduce cardiac filling time and result in a decrease in cardiac output. Over distention (by increasing preload) of the heart suppresses (inhibits) parasympathetic activity and the heart will increase via the Bainbridge effect. b. Preload – Amount of blood entering ventricles during diastole. Influenced by: venous return, fluid volume and atrial contraction. i. Stretch on cardiac muscle prior to contraction. Determines the degree of cardiac muscle shortening during contraction and is expressed as pressure in the ventricle at the end of diastole. Factors that affect preload include total blood volume, venous tone, ventricular compliance, and body position. Importantly, the Frank-Starling law of the heart states that increased preload increases the efficiency of cross-bridge interaction so that every 2.2 micrometer increase in stretch increases stroke volume. c. Afterload – Ventricles are contracting ejecting blood out of the aorta and into the pulmonary trunk during systole. Resistance to forward flow. Influenced by: HTN, arthrosclerosis and vasoconstriction. i. Equivalent to the tension the heart must develop to produce forward movement of blood. The heart can adapt to higher resistance because the stroke volume is reduced with each contraction (leaving more blood volume in the heart). Consequently, end diastolic volume increases, causing an increased fiber stretch which stimulates a more forceful contraction. However, the price of this adaptation is intensification of the work of the heart and a subsequent increased oxygen demand. d. Contractility – How hard the myocardium must contract for giving preload. Influenced by positive and negative ionotropes. i. Ability of myocardial cells to develop force at a given muscle cell length and is related to the velocity of fiber shortening. Contractility correlates with intracellular calcium concentration and depends on the amount of calcium released from myocardial sarcoplasmic reticulum stores. Circulating catecholamines increase contractility, as does sympathetic nervous system activation, while parasympathetic nervous system decreases contractility. An increased heart rate creates the Bowditch staircase effect (Treppe) that will also augment myocardial contractility. 2. Differentiate between volume work vs. stroke work and the effects on oxygen supply vs. demand a. Volume work is external work and it is the work of moving blood forward during ejection b. Pressure work is internal work and involves increasing wall tension and fluid pressures during isovolumic contraction c. Increasing volume or pressure work of the ventricle increases myocardial oxygen consumption and the demand for ATP. 3. What are the consequences of an imbalance between myocardial oxygen demand and supply? a. Myocardial oxygen consumption is increased by wall stress, heart rate, and contractility. i. Wall stress increases oxygen consumption because it takes more pressure to overcome the resistance to forward flow ii. Heart rate increases the number of times the heart beats so that oxygen requirements are increased iii. Contractility increases “the squeeze” with a resultant increase in myocardial oxygen demand Ischemic Heart Disease Angina and ACS 1. Describe the pathophysiology of coronary artery disease a. Cellular ischemia occurs if there is increased demand for oxygen relative to arterial supply or a reduction in oxygen supply. b. There is a decreased regional blood flow to the myocardium c. Myocardial oxygen and glucose reserves are depleted d. Subsequent switch to anaerobic glycolysis causes diminished ATP synthesis leading to local acidosis and accumulation of lactic acid e. Cell damage triggers release of intracellular enzymes f. Electrolyte disturbances (potassium, calcium, and magnesium) occur g. There can be impulse conduction dysfunction and depression of contractile function h. Eventual cardiac dysfunction may occur 2. What is the major cause of angina and what are the different types of angina (be sure to differentiate between the types of angina)? a. Stable Angina – Most common i. Caused by imbalance between coronary artery perfusion and myocardial oxygen demand. It is predictable. Elicited by physical activity or emotional stress. Transient lasting <5min. Rest relieves/minimizes pain. b. Variant Angina – Episodic Ischemia i. Brought on by arterial vasospasm as with Prinzmetal angina. Unrelated to physical activity, heart rate or blood pressure. c. Unstable Angina – Crescendo Angina i. Increasingly frequent pain. Change in the pattern of what causes pain. Prolonged duration of pain. Precipitated by increasingly lower levels of activity or may occur at rest. Caused by partial plaque disruption with thrombosis formation or even by vasospasm. Early warning sign of imminent acute MI. 3. What causes coronary artery plaques to become vulnerable for disruption? a. Vulnerable intracoronary plaques are areas of active inflammation. They contain a large lipid core covered by a thin cap. The plaques are easily eroded which triggers platelet adhesion at the area of the erosion or at fissures in the plaque. These types of plaques may create severe stenosis leading to high shear stress. They are easily ruptured. b. Formed plaques may be disrupted by: physical exertion, stresses that increase cardiac contractility, tachycardia, stresses that increase blood pressure, vasospasm 4. How long is myocardial tissue viable after an ischemic event? a. By 10 days to 8 weeks post infarction, granulation tissue fills in, collateral vessels circulation develops, collagen deposition occurs, and scar tissue begins to formation. AMI/ Ventricular Remodeling 1. What are common symptoms of an acute coronary event and why do they occur? What are common symptoms of myocardial ischemia in elders and women? a. Men i. Substernal chest discomfort (heaviness, pressure, tightness, squeezing, burning, or crushing) ii. Pain radiating to left shoulder and arm, neck and jaw, back, and right arm iii. Tachycardia, atrial fibrillation or ventricular arrhythmias iv. Lateral displacement of apical pulse, soft S1, palpable S4 or new mitral regurgitation murmur v. Distended neck veins indicating right ventricular failure vi. Dyspnea and shortness of breath vii. Diaphoresis viii. Nausea and vomiting ix. Anxiety x. Lightheadedness b. Women & Elderly i. Palpitations ii. Indigestion iii. Anorexia iv. Fatigue v. Numbness and tingling in arms 2. What are the best biochemical markers used to determine if there is an AMI/ cardiac injury? a. elevations of troponin 1 (4-36 hr. postinjury) b. creatine kinase-MB (4-24 hr. post injury) c. LDH1/LDH2 (12-48 hr. postinjury) d. Creatinine kinase-MB and troponin levels correlate with the extent of damage. 3. What are the pathophysiologic changes in the myocardium after an acute AMI? a. sytolic/diastolic dysfunction b. decreased cardiac output (↓ stroke volume) c. tachycardia d. arrhythmias e. dyspnea f. pulmonary congestion/edema g. ↑ sytemic vascular resistance h. ↑ blood volume i. ↑ systemic edema j. sympathetic activation k. ↑ circulating catecholamines l. ↑ angiotensin II and ↑ aldosterone m. ↑ natriuretic peptides n. ↑ arginine vasopressin (ADH) 4. What are the most common changes in the EKG and of dysthymias after and MI? a. Inverted T waves and S-T segment depression b. Peaked "hyper-acute" T waves (early ischemia) and lead to S-T segment elevation c. Myocardial cell injury reflected by S-T elevations greater than 2 mm in two contiguous leads) d. Areas of infarction reflected by the presence of pathologic Q waves 5. How does sustained hypertension contribute to myocardial infarction? a. Sustained hypertension will causes hypertrophy in cardiac muscle. A 6. What is ventricular remodeling and how does it occur? a. Endothelin and inflammatory cytokines promotes ventricular remodeling. Contractile dysfunction at the site of the myocardium at a site distant from injury and is associated with myocite hypertrophy and dilation. A change in heart geometry or volume or mass occurs. 4. Relate how Beck’s triad causes the clinical manifestations/features of cardiac tamponade a. Anxiety and restlessness, low BP, weakness, chest pain, trouble breathing, rapid breathing, discomfort relieved by leaning forward. Disorders of the Pericardium Pericarditis, Pericardial Effusion, and Tamponade 1. What is pericarditis and what is the mechanism for the complication of cardiac tamponade a. Pericarditis is an inflammatory disease of the pericardium and may be caused by: i. Infection: viral (coxsackie most common) or bacterial (TB, staphylococcus, pneumococcal) ii. Collagen-vascular disease such as SLE, scleroderma or rheumatoid arthritis iii. Neoplastic disease iv. Uremia v. Injuries such as MI, trauma, radiation and after thoracotomy vi. Drug-related (heroin) vii. Idiopathic b. Mechanism i. Acute inflammatory processes produce local vasodilation and increased vascularity 2. How does acute inflammation impact the pathophysiology of pericarditis? a. Increased vascular permeability with extravasation of serum into the pericardium b. Invasion of polymorphonucleated leukocytes (neutrophils and macrophages) into the pericardial tissues c. Fibrin deposition in the pericardium 5. Describe the clinical features/manifestations of pericarditis a. Jugular venous distention, Systemic hypotension, Quiet precordium, Sinus tachycardia, Pulsus paradoxus, Dyspnea and tachypnea, Beck's Triad (if tamponade occurs). 6. Why can restrictive pericarditis lead to elevated venous pressure? a. Impaired diastolic filling of ventricles. Pump Failure Systolic and Diastolic Heart Failure 1. Differentiate between the cardiac dysfunction associated with diastolic and systolic left sided cardiac failure? a. Systolic dysfunction is a progressive disorder of contractile function characterized by: i. Low ejection fraction during ventricular systole ii. Low ejection fraction is thought to be related to myocyte loss, dysregulation of neurohormones (may stimulate apoptosis), beta-receptor downregulation. Increased end systolic volume, Decreased forward flow accompanied by kidney hypoperfusion, Lactic acidosis b. Diastolic dysfunction is the inability of heart chamber to expand and is characterized by i. Low myocardial compliance, Decreased preload, Poor filling during diastole due to failure of relaxation, Increased intraventricular pressure. Relatively normal ejection fraction (> 50 %) despite symptoms of congestive heart failure. ii. Diastolic dysfunction is often associated with: Decreased pumping of calcium from the cytosol which compromises myocardial relaxation. Massive left ventricular hypertrophy related to scar formation or thickening of the ventricular wall. Myocardial fibrosis, Deposition of amyloid proteins, Prolonged constrictive pericarditis. 2. What are the effects of systolic vs. diastolic dysfunction on cardiac ejection fraction? a. Systolic dysfunction is a progressive disorder of contractile function characterized by: i. Low ejection fraction during ventricular systole ii. Low ejection fraction is thought to be related to myocyte loss, dysregulation of neurohormones (may stimulate apoptosis), beta-receptor downregulation. Increased end systolic volume, Decreased forward flow accompanied by kidney hypoperfusion, Lactic acidosis b. Diastolic dysfunction is the inability of heart chamber to expand and is characterized by i. Low myocardial compliance, Decreased preload, Poor filling during diastole due to failure of relaxation, Increased intraventricular pressure. Relatively normal ejection fraction (> 50 %) despite symptoms of congestive heart failure. ii. Diastolic dysfunction is often associated with: Decreased pumping of calcium from the cytosol which compromises myocardial relaxation. Massive left ventricular hypertrophy related to scar formation or thickening of the ventricular wall. Myocardial fibrosis, Deposition of amyloid proteins, Prolonged constrictive pericarditis. Right and Left-Sided Heart Failure 1. In right and left-sided heart failure what are the effects on preload, afterload and contractility? a. Right Sided i. Preload – Less blood goes into left ventricle, which decreases ventricular preload. As left ventricular preload falls, so too does the left ventricular output fall. Leads to decrease in systemic tissue perfusion. ii. Afterload - Increased afterload. iii. Contractility - Decreases b. Left Sided i. Preload – Increases ii. Afterload – Increases right ventricular afterload iii. Contractility – Decreases 2. Differentiate between the clinical manifestations of right vs. left-sided heart failure a. Right i. Shortness of breath in the presence of left sided heart failure ii. Bulging neck veins due to elevated jugular venous pressure iii. Pedal edema iv. Right upper quadrant abdominal pain (liver congestion) v. Anasarca and ascites due to elevated venous pressure vi. Presence of a hepatojugular reflex b. Left i. Shortness of breath and orthopnea ii. Paroxysmal nocturnal dyspnea iii. Nocturia iv. Chest pain v. Rales and pleural effusion vi. Displaced/sustained apical impulse vii. Auscultation of a third and fourth heart sound viii. If the heart failure is severe there may be pale, cold clammy skin due to peripheral vasoconstriction 3. What are the characteristics of the vicious cycle of heart failure? a. Decreased cardiac output (CO) activates production of neurohormones (NE; angiotension II; endothelin-ET) which causes vasoconstriction and increased afterload. This further reduced ejection fraction (EF) and CO, and the cycle repeats. The downward spiral is continued until a new steady state is reached in which CO is lower and afterload is higher than is optimal for normal activity 4. Describe the activation and the consequence of activation of the Renin-Angiotensin-Aldosterone system in heart failure or cardiogenic shock states? a. When contractility is impaired ejection fraction falls, while there is an increase in left ventricular end diastolic volume and this is reflected in an increased preload because the heart muscle must work harder to move more residual blood. Volume work increases to create a greater oxygen demand. RAAS augments afterload. Pressure work at the heart increases, as does o2 demand relative supply, further reducing contractility. Cardiogenic Shock 1. What are the common causes of cardiogenic shock? a. Myocardial infarction that involves the left ventricle (most common), Right ventricular myocardial infarction, End-stage cardiomyopathy, Papillary muscle dysfunction, Myocardial free wall rupture, Congenital heart defects. 2. Why can activation of the renin-angiotensin-aldosterone system worsen cardiac function leading to cardiogenic shock? a. Results in increased blood volume and increase in systemic vascular resistance. This causes increase in preload, stroke volume and heart rate. Systemic edema and pulmonary edema can occur. Decrease in cardiac output, leads to decrease in ejection fraction. Because of this there is htn leading to decrease in tissue perfusion, and this lack of tissue perfusion results in impaired cellular metabolism. 3. Describe the clinical presentation/manifestations of cardiogenic shock a. Decreased systolic BP, but increased diastolic BP b. Narrowing of the pulse pressure c. HR exceeding 100 bpm d. Peripheral vasoconstriction with cool clammy skin e. Coarse crackles in the lung and there may be evidence of pulmonary edema f. An S3 gallop over the left apex of the heart g. Hyperventilation with respiratory alkalosis h. In later stages of pulmonary edema, there may be cyanosis due to hypoxemia Cardiac Valvular Disease Valvular Regurgitation 1. Describe the pathophysiologic consequences of mitral and aortic regurgitation a. Mitral Regurgitation – Forward stroke volume is less than the total output as a result of backward flow through the partially opened valve and decreased flow into the aorta. Left atrial pressure and volume are elevated causing volume-related stress on the left ventricle during diastole. i. The severity is determined by: 1. Size of the mitral orifice 2. Systolic pressure gradient 3. Stroke volume 4. Left atrial compliance 5. Duration of flow regurgitation per systolic contraction b. Aortic regurgitation i. With aortic regurgitation there is backflow of blood into the left ventricle during diastole precipitating an increase in cardiac volume load. Due to the regurgitant flow the heart has blood entering from both left atrium and from the aorta. Consequently, there is an increased blood volume to pump with each contraction. 2. Contrast the effects of acute vs. chronic mitral and acute vs. chronic aortic regurgitation a. Mitral i. Acute: Although left atrial size and compliance are normal during acute mitral regurgitation, there is elevation of left atrial pressure. Consequently, regurgitation with the associated increase in pressure is reflected in high pulmonary vascular pressures. These elevated pressures produce pulmonary congestion. Acute volume overload occurs due to the high left ventricle preload. The rapid increase in left atrial pressure causes pulmonary edema. ii. Chronic: Chronic mitral regurgitation develops slowly, so compensatory mechanisms may reduce the effects. The left atrial and pulmonary venous pressures are more normal, but the left ventricle increases in both size and compliance. Elevated preload and normal afterload (or reduced) facilitates left ventricular ejection. The gradual increase in left atrial size accommodates regurgitated volume at a lower filling pressure. The subsequent increase in volume work is fairly well-tolerated. However, the condition can predispose to atrial fibrillation. b. Aoritc i. Acute: In acute aortic regurgitation a sudden large regurgitant volume remaining in the ventricle leads to a precipitous elevation of left ventricular end diastolic volume and pressure. The increased pressure is transmitted to the left atrium and to the pulmonary veins. Sympathetic stimulation increases heart rate and elevation of pulmonary vascular resistance. This worsens the regurgitation and may trigger pulmonary edema, ventricular arrhythmias, and/or circulatory collapse. ii. Chronic: With chronic aortic regurgitation the left ventricle undergoes compensatory adaptation as evidenced by the left ventricular dilation. Mild hypertrophy develops. The left ventricular compliance increases over time causing the diastolic pressure to drop over time (the systolic pressure also drops). The pulse pressure widens. There is a fall in coronary artery perfusion despite increased wall stress and an increase in myocardial oxygen consumption. Valvular Obstruction/Stenosis 1. Describe the pathophysiologic consequences of mitral and aortic stenosis a. Aortic Valve Stenosis: A fixed outflow obstruction causes left ventricular enlargement. The gradual development of the stenosis gives the left ventricle time to adapt so the ventricular wall hypertrophies. Although ventricular wall thickness increases, the size of the internal heart cavity remains relatively unchanged due to parallel replication of the sarcomeres (concentric hypertrophy). The ventricle becomes dependent on atrial contraction to fill the ventricle due to the “stiff” left ventricle. Left ventricular end diastolic volume increases along with progressive pressure overload. With severe obstruction, the pressure work of the heart may exceed coronary blood flow reserve and signs of systolic and diastolic contractile dysfunction may appear. b. Mitral Valve Stenosis: Impeded left atrial emptying creates an abnormal pressure gradient between the left atrium and ventricle. Chronically elevated pressure in the left atrium occurs along with increased pulmonary venous pressure and pulmonary hypertension. Dilation of the right ventricle develops due to chronic pressure elevation in the pulmonary vasculature. Because the right atrium handles a consistently elevated blood volume there is long standing pulmonary artery. hypertension leading to right ventricular hypertrophy (to overcome increased pressures in pulmonary venous system). Chronic pressure overload leads to disruption of electrical conduction system and may cause atrial fibrillation. 2. Compare the causes and clinical manifestations of aortic and mitral regurgitation and aortic and mitral stenosis a. Aortic valve stenosis i. Causes 1. Congenital malformations which appear before age 30 2. Rheumatic inflammation and fusion of commissures where symptoms develop between 30 and 70 years of age 3. Degenerative changes in the valve leaflets with calcium deposition at the bases where symptoms appear after age 70 ii. Clinical Manifestations 1. Angina pectoris due to supply demand imbalance and compression of small coronary arteries 2. Syncope due to decreased cerebral perfusion secondary to the fixed outflow obstruction or loss of effective atrial “kick” 3. Congestive heart failure due to development of contractile dysfunction 4. Lateral displacement of the apical impulse with a prominent fourth heart sound 5. Mid-systolic crescendo-decrescendo murmur due to narrowed aortic orifice b. Mitral Valve Stenosis i. Causes 1. Rheumatic heart disease 2. Congenital valve lesions 3. Calcium deposition on valve leaflets ii. Clinical Manifestations 1. Shortness of breath, hemoptysis, and orthopnea 2. Atrial arrhythmias (PAT, paroxysmal atrial tach, atrial fibrillation) due to distention of left atrium 3. Reduction of cardiac output because ventricular filling is dependent on atrial contraction 4. Mural thrombi and emboli generation 5. Low-pitched rumbling murmur heard during diastole at the base of the heart due to turbulent flow across the narrowed mitral orifice 6. Accentuation of the 1st heart sound due to increased left atrial pressure c. Cardiac Myopathies 1. Differentiate between the different types of cardiac myopathies? a. Primary Genetic Causes i. Hypertrophic cardiomyopathy (unexplained) ii. Arrhythmogenic right ventricle associated with rhythm disturbances iii. Left ventricular noncompaction-embryonic development b. Primary Mixed Causes i. Dilated cardiomyopathy—most common cause of heart failure ii. Most congenital causes are autosomal dominant iii. Can be associated with an X-linked recessive gene iv. Can be associated with mitochondrial inheritance patterns c. Primary Acquired Causes i. Myocarditis ii. Peripartum iii. Stress (tako-tubo)—transient left ventricular apical ballooning may be due to ischemia or microvascular spasm d. Secondary Heart Muscle Disease in the Presence of a Multisystem Disorder Causes i. Autoimmune (SLE, rheumatic arthritis, scleroderma) ii. Endocrine (acromegaly, diabetes mellitus hyper/hypothyroidism) iii. Familial storage diseases (glycogen storage) iv. Infiltrative diseases (sarcoidosis, radiation-induced fibrosis) v. Neuromuscular diseases (muscular dystrophy, neurofibromatosis) vi. Nutritional deficiencies (thiamine, protein deficiency) vii. Toxins (alcohol, arsenic, Calcium therapeutic agents, hydrocarbons) 2. Describe the pathophysiology of hypertrophic, dilated, and restrictive cardiomyopathy a. Hypertrophic i. 1) Ventricular hypertrophy in any portion of the ventricles 2) Asymmetric hypertrophy of the ventricular septum accounts for 90% of cases 3) Symmetric hypertrophy is less common 4) Short, wide, hypertrophic muscle fibers disorderly organised 5) Myocytes surrounded by fibroblasts and increased extracellular matrix, which manifests as diastolic stiffness and may cause arrhythmias b. Dilated i. 1) Dilatation and impaired systolic function 2) Typically occurs in both ventricles, but may be isolated to only one 3) May result in mitral and tricuspid regurgitation and atrial dilatation, even greater preload which amplifies dysfunction 4) Enlarged atria may give rise to atrial fibrillation c. Restrictive i. 1) Reduced ventricular compliance 2) Elevated holodiastolic pressure in the ventricles 3) Elevated venous pressure (systemic and pulmonary) 4) Symptoms of bilateral heart failure with systemic and pulmonary congestion 5) Reduced ventricular cavity size 6) Decreased stroke volume and decreased CO 3. Compare the clinical features/manifestations of hypertrophic, dilated, and restrictive cardiomyopathy Selected Congenital Heart Disease 1. Compare the defects associated with cyanotic vs. acyanotic congenital heart disease a. Congenital cyanotic heart diseases are birth defects that affect oxygenation of the blood to produce mixing of oxygenated blood with deoxygenated blood. This reduces the amount of oxygen transported to the tissues. Consequently, tissue oxygen requirements may exceed oxygen delivery capabilities. i. Tetralogy of Fallot ii. Transposition of the great vessels iii. Pulmonary atresia iv. Hypoplastic heart b. Congenital acyanotic heart disease is a cardiac structural defect present at birth. It is not associated with inadequate blood oxygenation even though there may be some arterial to venous blood admixture. i. Ventricular septal defects (if small) ii. Atrial septal defects iii. Patent ductus arteriosus iv. Aortic/pulmonary valve stenosis v. Coarctation of the aorta [Show More]
Last updated: 1 year ago
Preview 1 out of 25 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
We Accept:

Reviews( 0 )
$14.00
Document information
Connected school, study & course
About the document
Uploaded On
Sep 30, 2021
Number of pages
25
Written in
Additional information
This document has been written for:
Uploaded
Sep 30, 2021
Downloads
0
Views
14