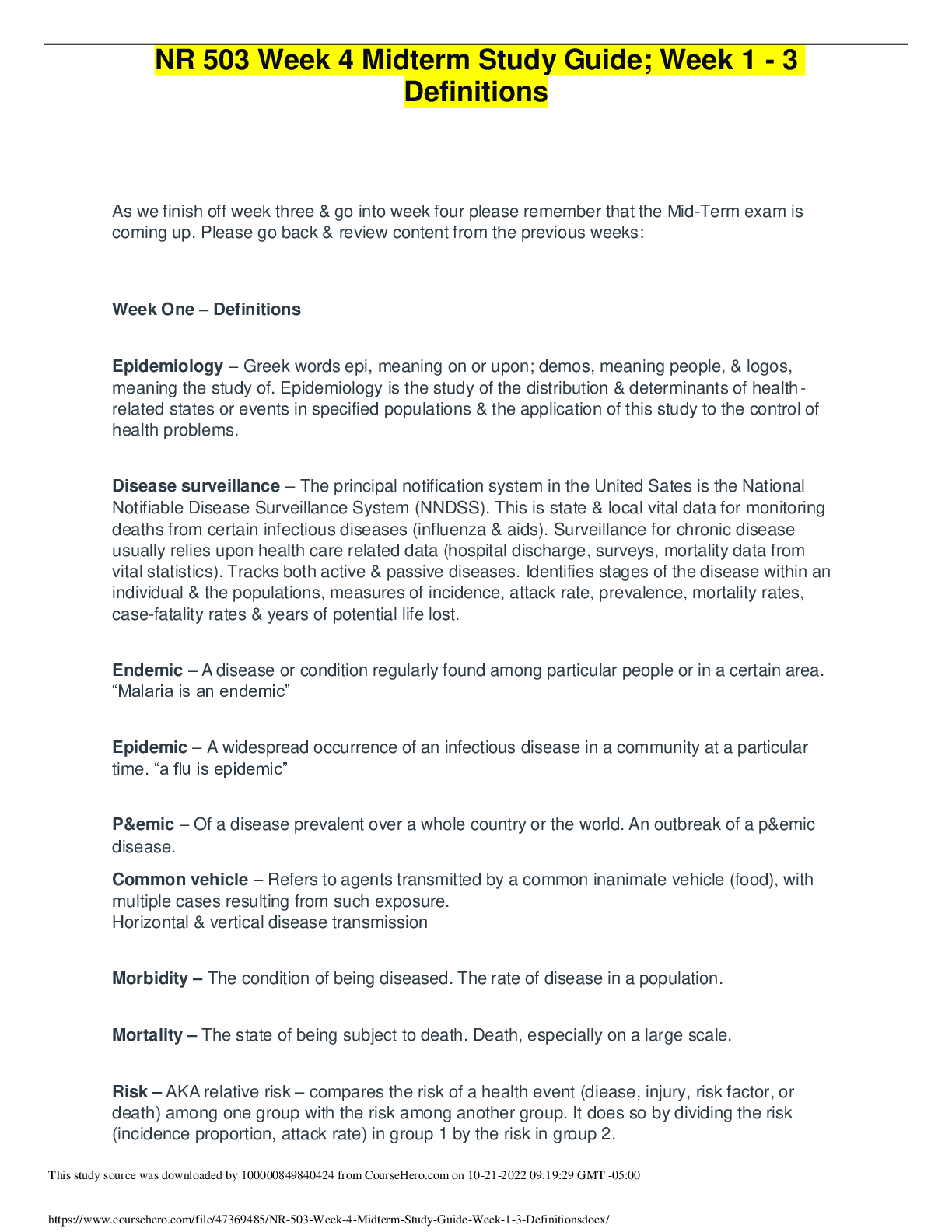
*NURSING > STUDY GUIDE > NURSING NUR 2488 Mental Health Exam 1 Study Guide Complete | Assess Your Knowledge | Download To sco (All)
NURSING NUR 2488 Mental Health Exam 1 Study Guide Complete | Assess Your Knowledge | Download To score An A.
Document Content and Description Below
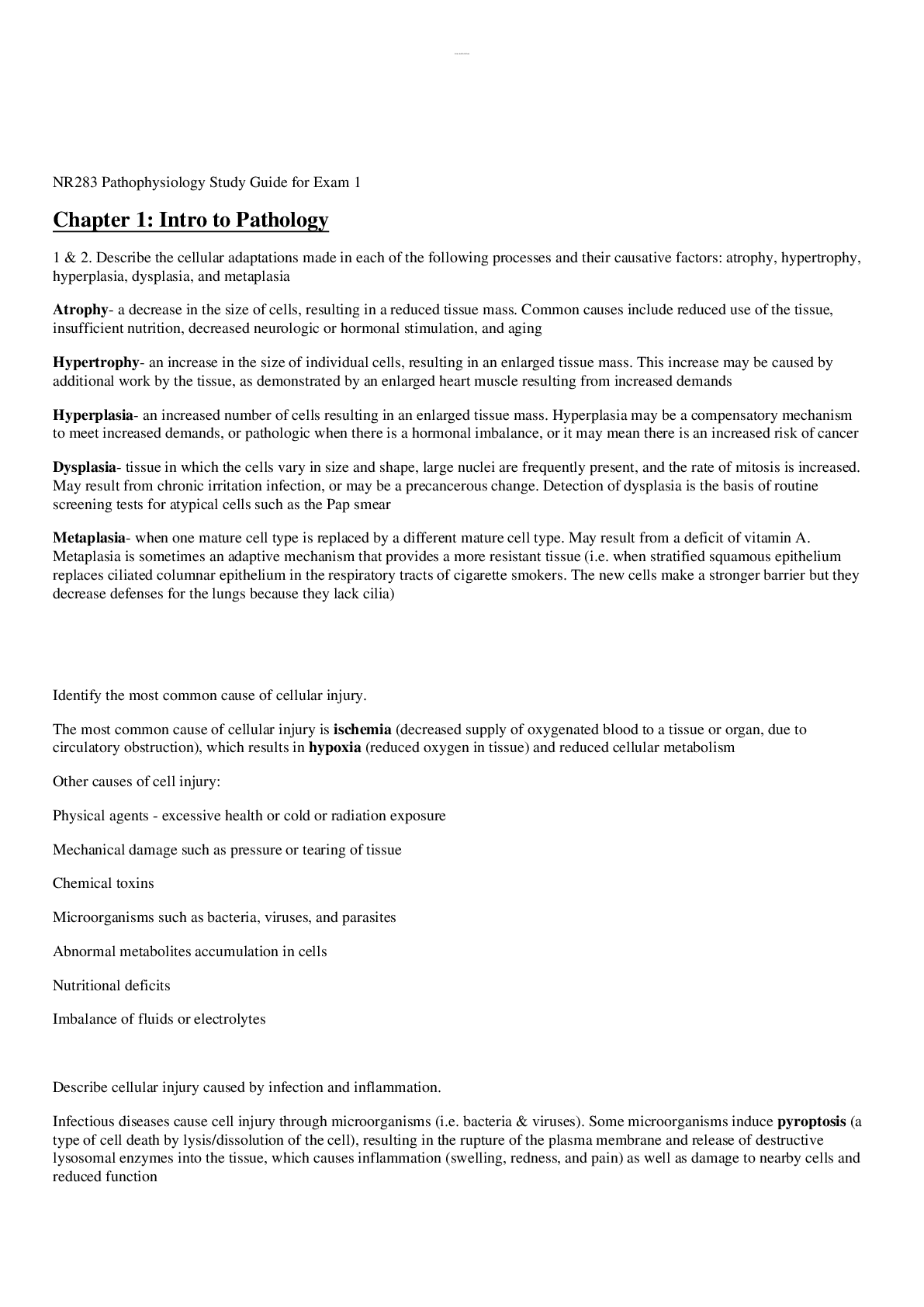
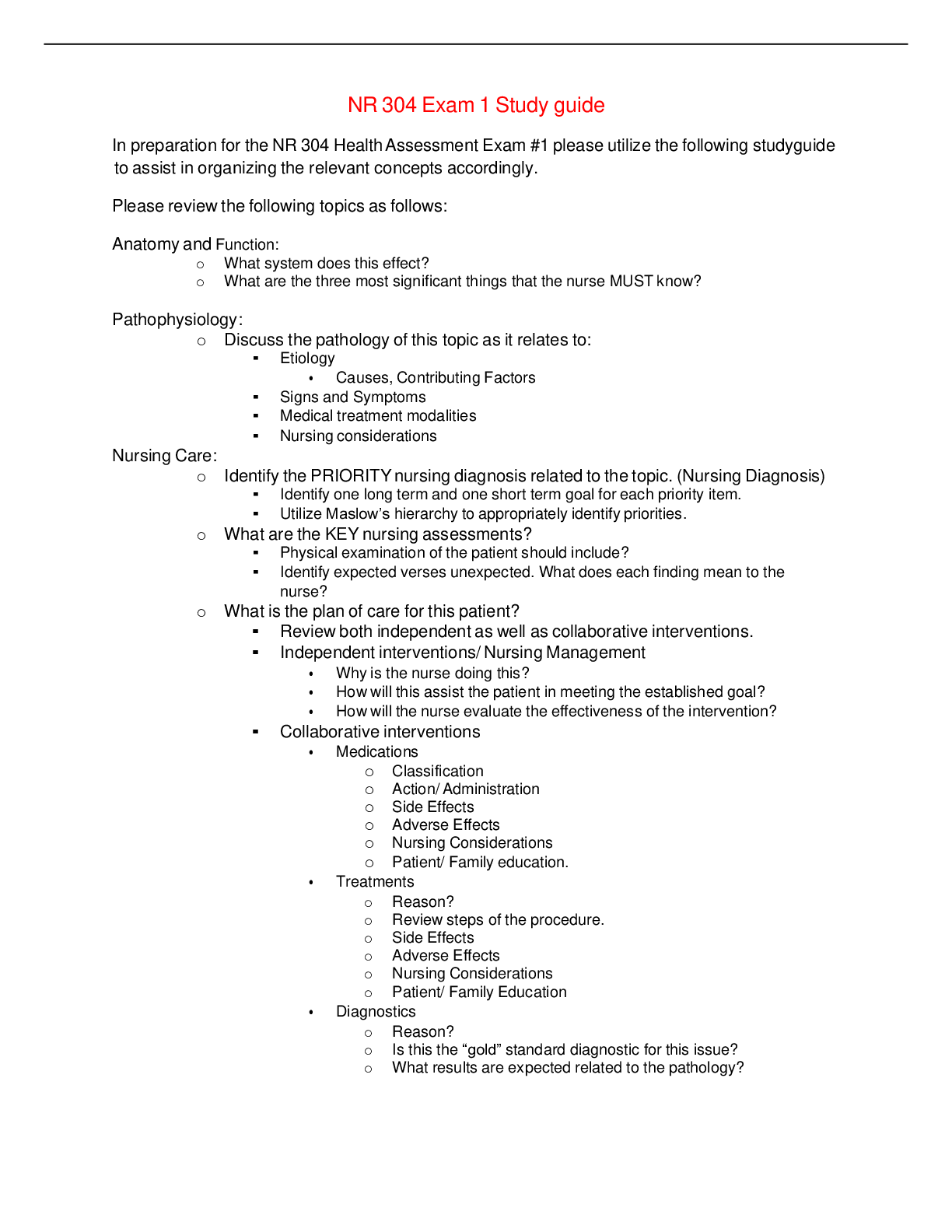
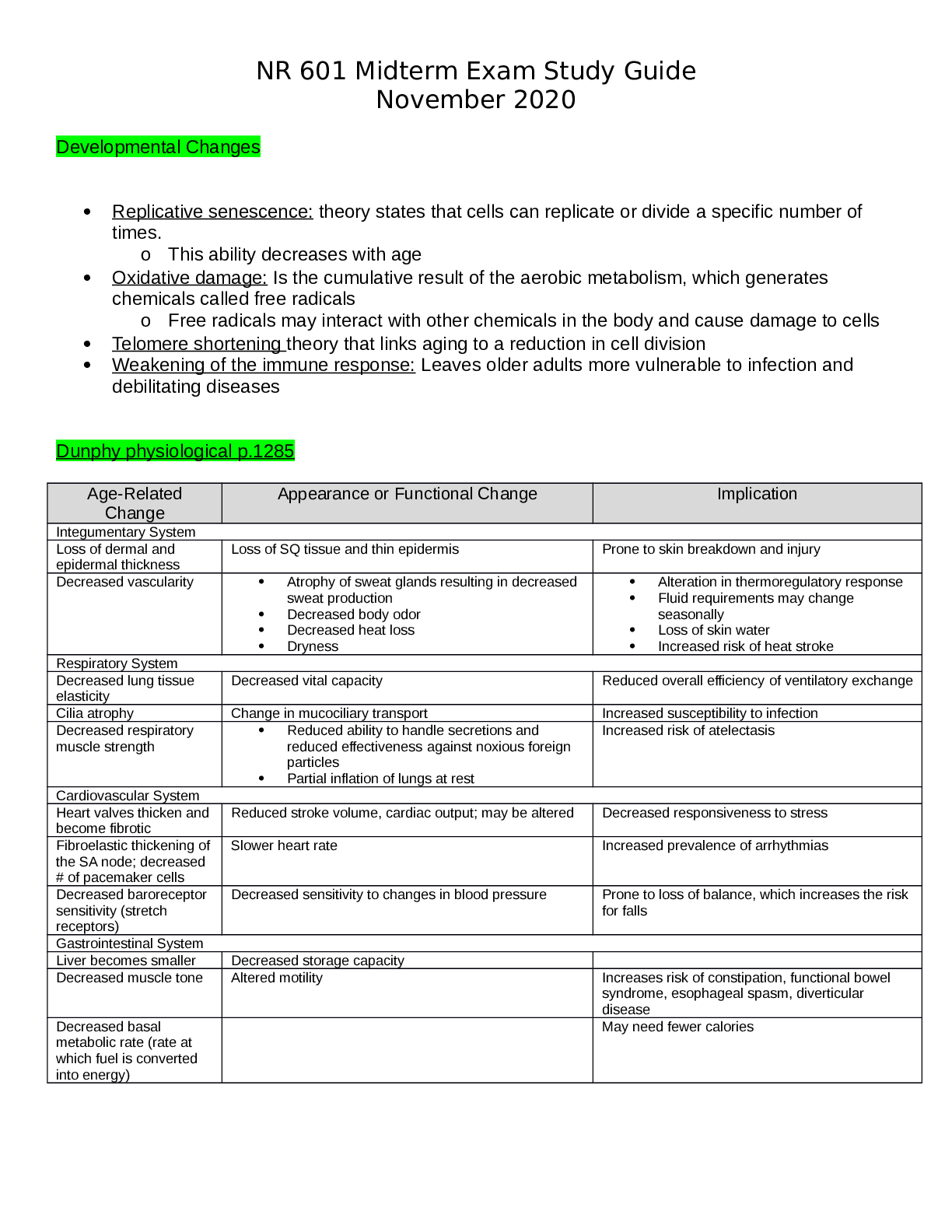
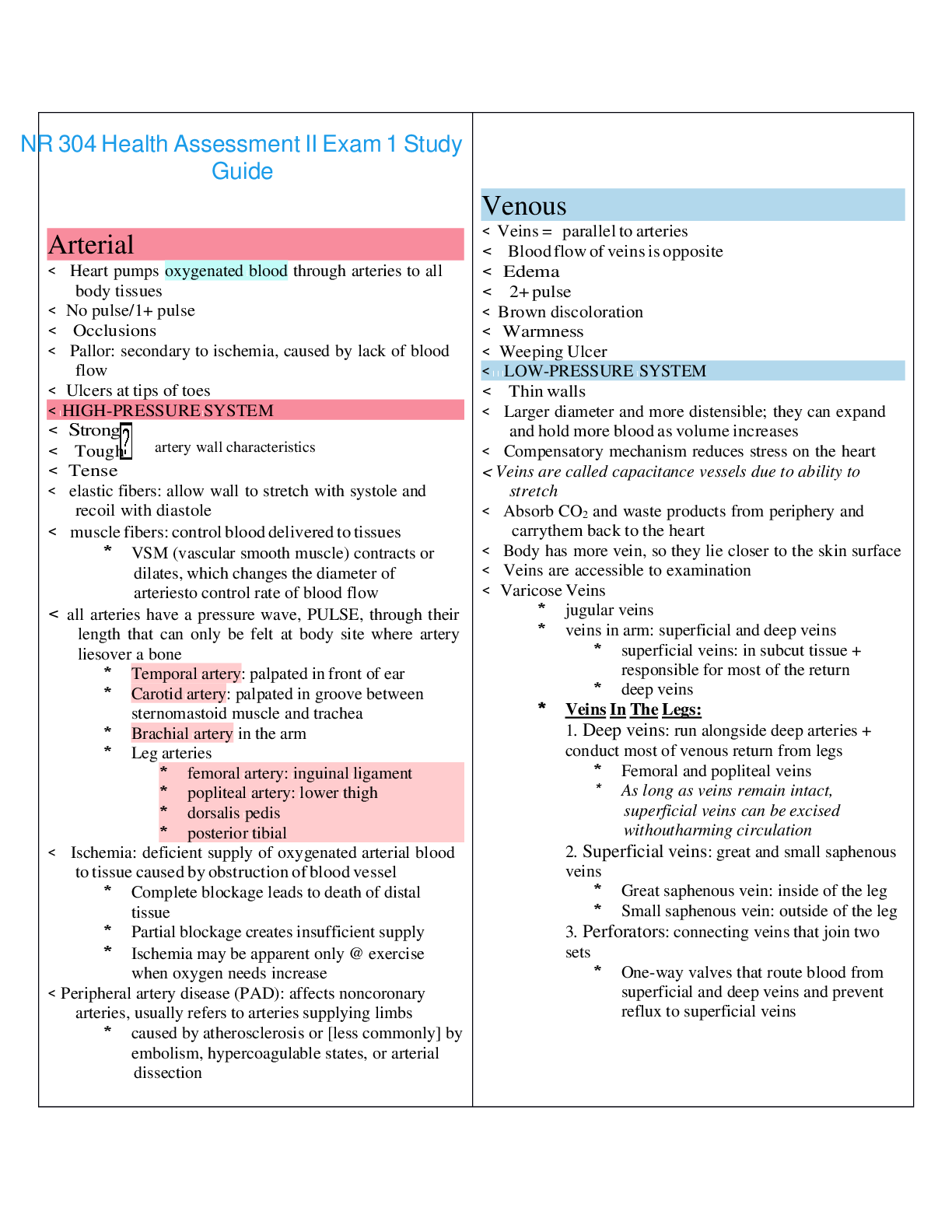
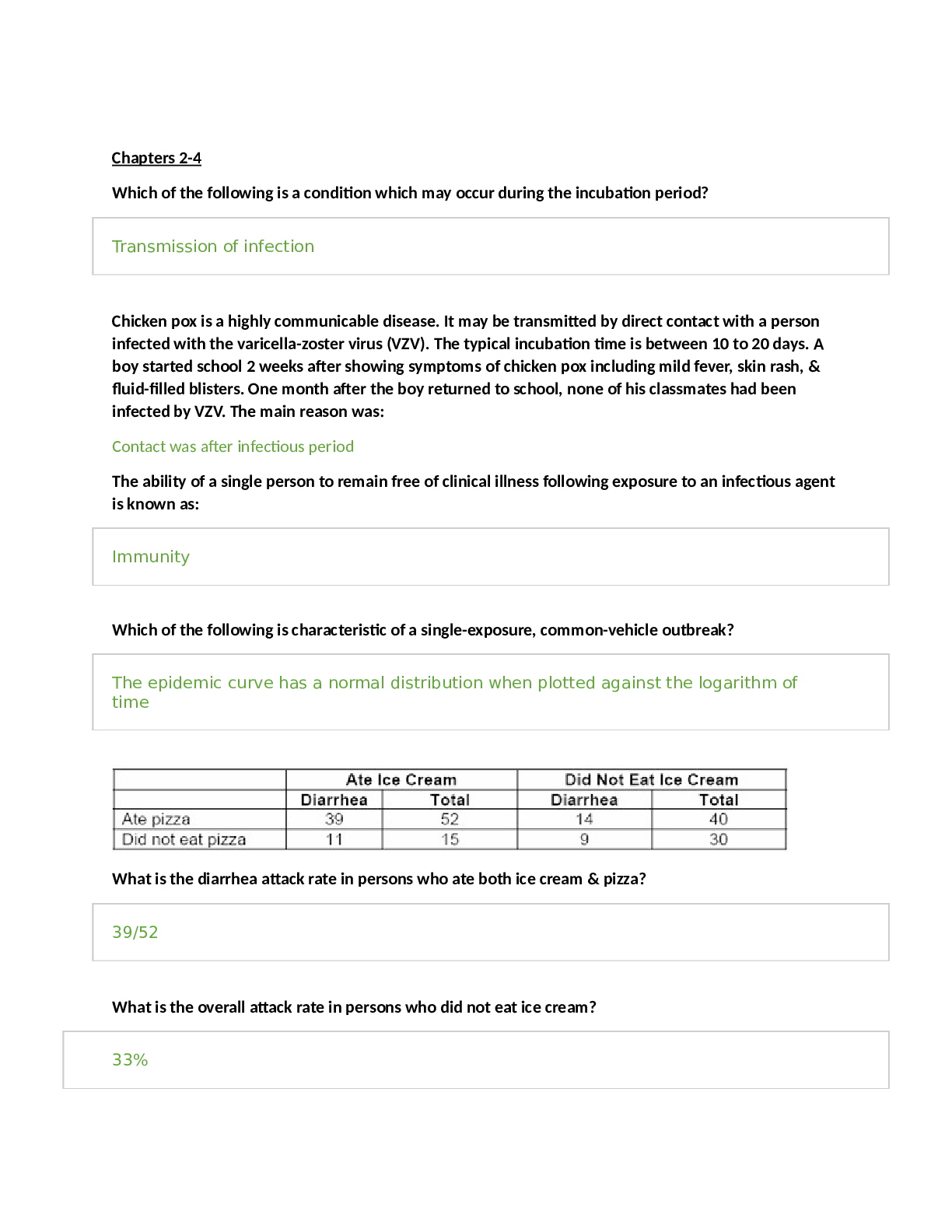
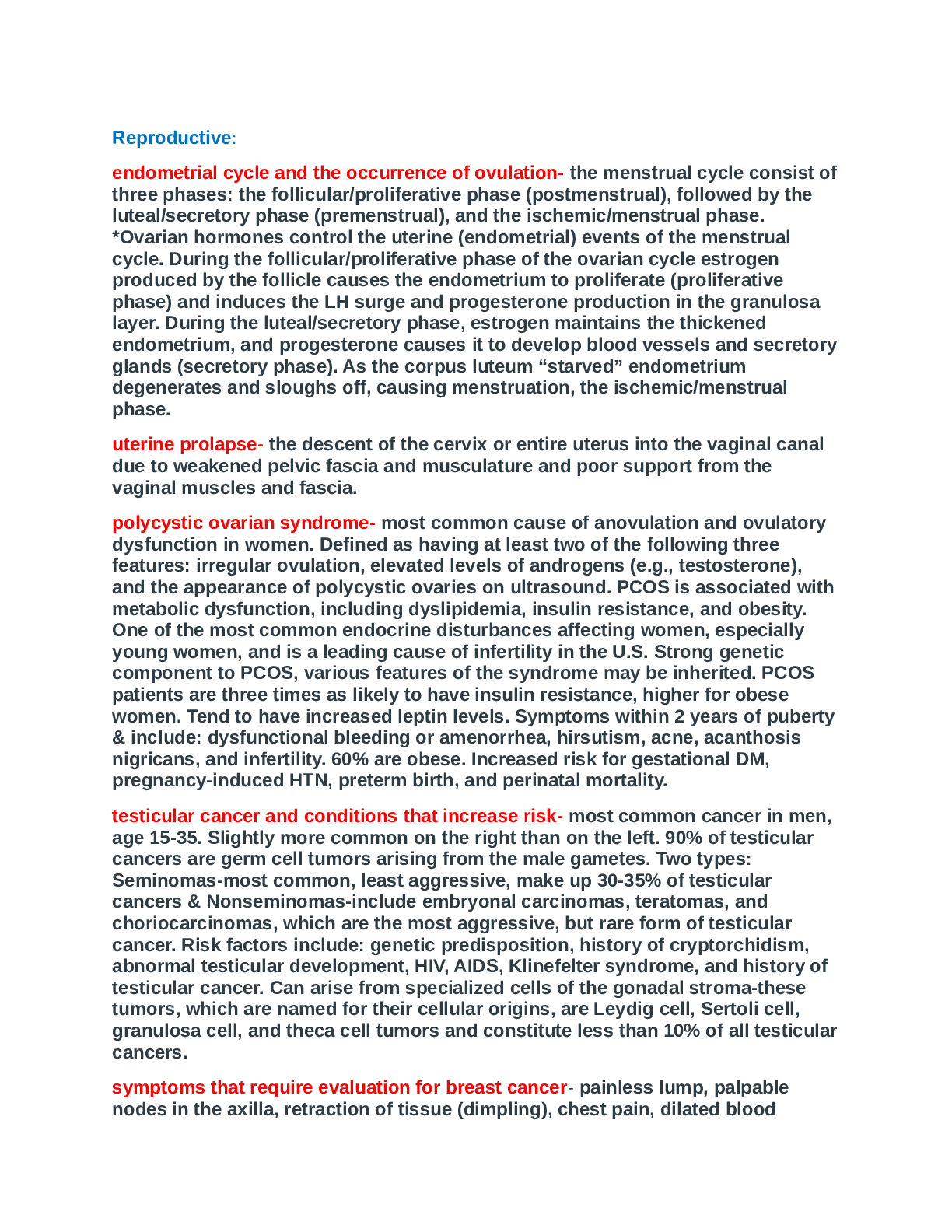
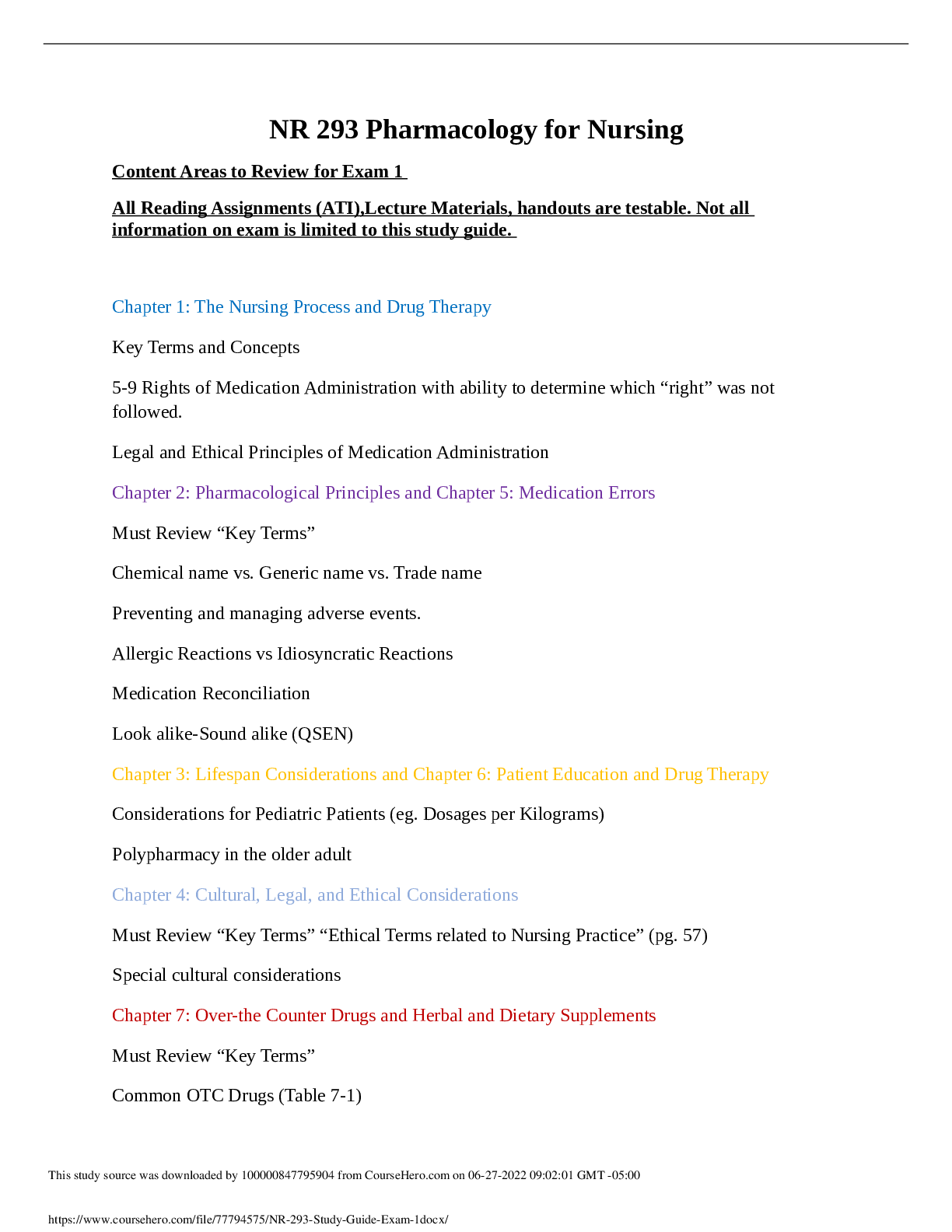
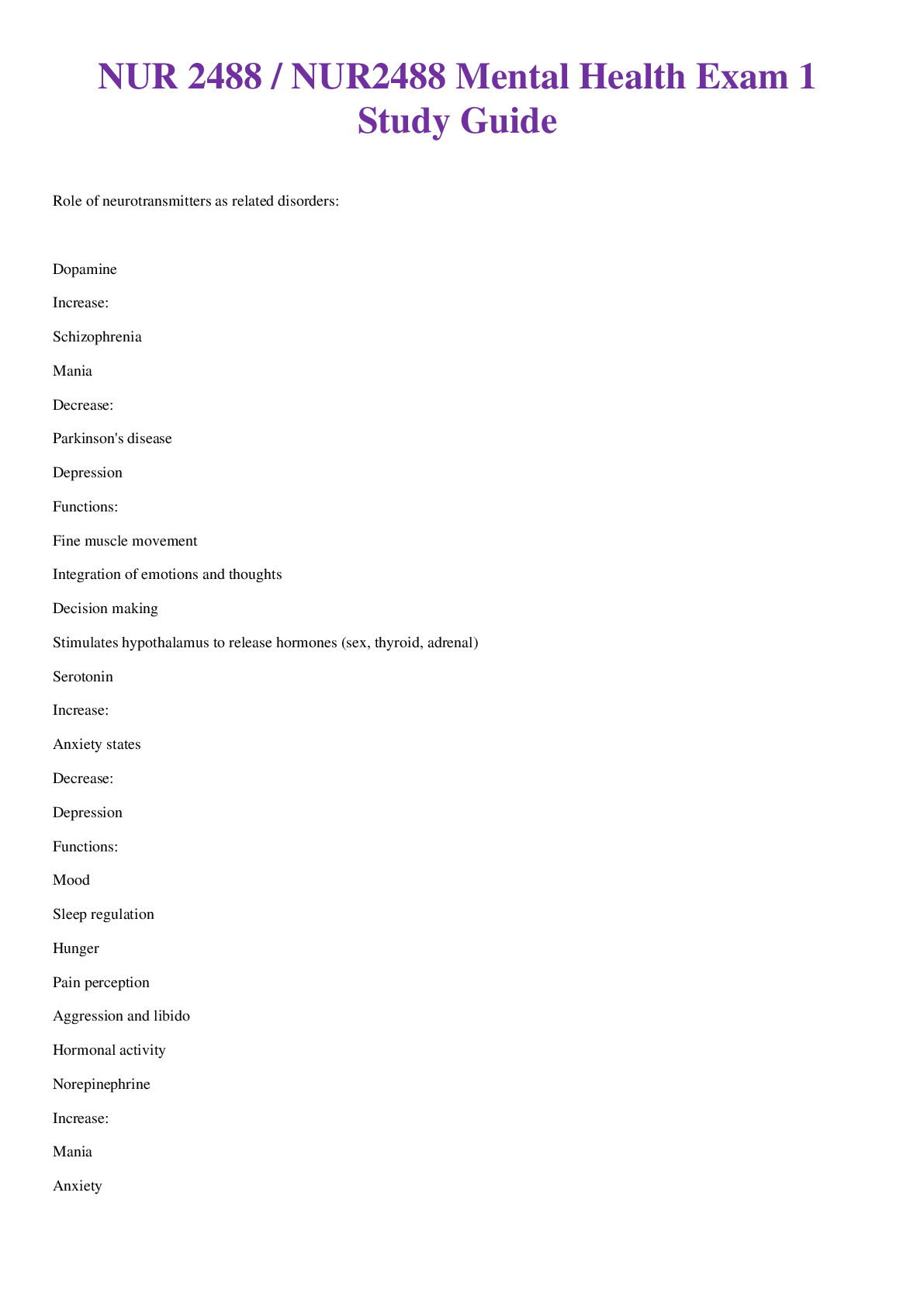
Discuss prominent theories and therapeutic models o Behavioral Therapy: attempts to correct or eliminate maladaptive (bad) behaviors/responses by rewarding & reinforcing adaptive (good) behavior. Use... of Desensitization, Aversion Therapy (becoming not afraid of spiders), Biofeedback and Modeling as well as the below 3 items. ▪ Pavlov, Watson & Skinner • Pavlov: Classical Conditioning (Ex: baby cries and mom has milk “let-down” reflex). • Watson: Personality traits & responses were learned (conscious) behavior. • Skinner: Operant Conditioning. Behaviors are learned through Positive/Negative Reinforcement (Ex: studying hard results in good grades). o Cognitive Behavioral Therapy: combines both behavioral and cognitive theory and seeks to modify negative thoughts that lead to dysfunctional emotions & actions. This is useful for those patients who feel incompetent, abandoned, evil or vulnerable. ▪ It is NOT the stimulus (situation/person/place/thing) that causes the response; it is the person’s evaluation & self- thoughts about the situation that causes the negative feelings/reaction. Therapy aims to remove these negative/repetitive thoughts and replace them with rational interpretations of situations. ▪ Ex: “Matt had a car accident. He now refuses to drive and says, “I shouldn’t be allowed on the road”. (This is distorted thinking and rationalization of his car accident). o Milieu Therapy: Creating a SAFE, structured inpatient/outpatient setting where the mentally ill can test new behaviors and coping mechanisms with others. ▪ Creating a SAFE, structured inpatient/outpatient setting where patients with mental illness can test new behaviors and interactions. ▪ Climate is essential to healing: paint color, relaxed environments are conducive to the healing process. ▪ Florence Nightingale believed that the environment helps heal o Maslow’s Hierarchy of Needs: Basic needs on the bottom of the pyramid have to be met before the top (self-actualization) can be attained. 1. Physiological Needs – most basic needs that a human needs (food, water, O2, sleep, sex, body temperature, elimination, voiding). This level takes priority over all others. 2. Safety Needs – security, protection, and freedom from fear/anxiousness/chaos, law, order and limitations. 3. Belonging & Love Needs – The need for love, affection, intimate relationships and belonging will see to overcome feelings of loneliness and alienation. (Having a Family and a Home is very important). 4. Esteem Needs – If this need is met, we feel confident, valued and valuable. If this need is NOT met, we feel inferior, worthless and helpless. 5. Self-Actualization – What we strive to become as humans. Fulfillment of this need brings inner piece and contentment with ones self. Describe the role of neurotransmitters: dopamine, serotonin, and norepinephrine, GABA • Dopamine: controls emotional responses, the brain’s reward and pleasure centers, stimulates heart and increases blood flow to organs. (Haloperidol = dopamine blocker). Cocaine allows more of dopamine to stay active for longer = increased HR, etc. o EPS is the result of Dopamine blockers (Dopamine needs to get through for proper brain functioning!) o Disorders with HIGH levels: Schizophrenia, Mania o Disorders with LOW levels: Depression, Parkinson’s Disease • Serotonin: Regulates mood, arousal, attention, behavior, and body temperature. Most anti-depressants increase Serotonin production. Muscle Relaxants block serotonin production. Serotonin release by platelets play important role in homeostasis. o High levels of Serotonin S/Sx: causes restlessness, shivering, diarrhea, muscle rigidity, fever and seizures. o Disorders with HIGH levels: Anxiety o Disorders with LOW levels: Depression • Norepinephrine: Regulate mood. A deficiency can cause Depression and excess can cause Mania. o Disorders with HIGH levels: Mania, Anxiety, Schizophrenia o Disorders with LOW levels: Depression • GABA: inhibitory neurotransmitter that regulates excitability and helps treat anxiety by helping you “chill out”. Anti-Anxiety Meds help increase the effectiveness of GABA by making the receptors more responsive. o Disorders with HIGH levels: Reduction of Anxiety o Disorders with LOW levels: Mania, Anxiety, Schizophrenia Describe the phases of the nurse-client relationship, and what occurs during each phase (Hildegard Peplau) 1. Orientation Phase: first time the nurse & patient meet, interact according to their own backgrounds/standards/values/beliefs, roles of the patient and nurse are clarified, confidentiality is discussed and assumed, nurse becomes aware of transferences & countertransference issues, goals are established, termination terms are introduced. 2. Working Phase: exploration of feelings or situations that are causing the problems, re-experiencing of old conflicts can awaken high levels of anxiety, intense emotional states may surface, defense mechanisms, denying, manipulation, evaluation of problems and goals, promote alternative reactions/behaviors to situations, etc. The nurse’s awareness of his or her own personal feelings and reactions to the patient are VITAL for effective interaction with the patient. 3. Termination Phase: summarization of goals, review of what was achieved during communication, discussing new ways to implement new coping strategies, evokes strong feelings in both client & nurse. Describe the client interview- what should be considered and included • What should be Considered: o The interview (content & direction) is lead by the patient. o The nurse uses open communication, positive attending behaviors, and active listening to better understand the patient’s situation. This allows the patient to feel understood, listened to, explore problems, healthy ways to meet emotional needs and have a satisfying interpersonal relationship experience. • What should be Included: o Setting: has a large impact on healing (remember to use Milieu techniques) o Seating: stay between patient and door, avoid sitting behind a desk, sit at an angle with the chairs (not face-to face) o Introductions: who you are, purpose of meeting, length of meeting, confidentiality of meeting, asking patient how they like to be addressed (Blake vs. Mr. Anderson), etc. o Initiating Interview: use open ended questions like “Where should we start”, “Tell me what has been going on when you recently” o Offering Leads: “Go on…” o Making statements of Acceptance: “I follow you…” • Helpful Guidelines o Speak briefly o When you don’t know what to say, don’t say anything o Focus on feelings o Don’t give advice o Avoid relying on questions o Note patient’s non-verbal ques o Keep the focus on the patient Describe the sections of a psychiatric assessment- what should be included? 1. MSE: organizes OBJECTIVE data (physical behavior, mood, perceptions, speech patterns, appearance, nonverbal communication, etc.) 2. Psychosocial Assessment: provides additional information to plan care for the patient. SUBJECTIVE data. • Spirituality/Religious beliefs • Cultural/Social factors • Stressors & Coping methods • Personal background • Quality of ADL’s • Family Psychiatric history • History of violent/suicidal behaviors • Current Meds & Alternative Therapies • Current Drug abuse problems (if any) Discuss the nursing process as it applies to mental health clients • Assess, Diagnosis, Outcome Identification, Planning, Intervention, & Evaluation • Care plan should be: Evidence based, individualized, appropriate, compatible with other therapies, realistic, and safe. • NIC: standardized nursing interventions • NOC: standardized nursing outcomes Describe the role of the psychiatric nurse vs. advanced practice • Nurses (RN) CANNOT: prescribe medications, psychotherapy, or perform consultations. Describe and give examples of therapeutic communication techniques • Therapeutic Communication: goal directed, professional, scientifically based. Goal is to get information so that you can plan care for the patient. • Active Listening o Clarifying: promotes understanding of the patient’s statement o Restating: repeating the same key words the patient has just spoken to echo their feelings. (Ex: If a patient remarks, “My life is empty…it has no meaning,” additional information may be gained by restating, “Your life has no meaning?”) o Reflecting: helps people understand their own thoughts better; summarizes (Ex: For example, to reflect a patient's feelings about his or her life, a good beginning might be, “You sound as if you have had many disappointments.”) o Exploring: use of open-ended questions or statements to allow the patient to express thoughts/feelings. (Ex: “Tell me more…”, “Give me an example of…”) • Communication Technique Examples in Different Scenarios o For Suicidal Patients: “These thoughts are very serious Mr. Adams. I do not want any harm to come to you. Can you tell me what you were feeling and if there were any circumstances that led you to this decision?” o For Patients who start Crying: Stay with your patient and reinforce that it is all right to cry & offer tissues. “You seem upset, what are you thinking right now?” o For Patients who say they “don’t want to talk”: “Its alright. I would like to spend time with you. We don’t have to talk.” Or reapproach at a later time, “Our 5 minutes is up. I will be back at 10am and spend another 5 minutes with you.” o For Patients who ask the nurse to keep a secret: Nurses cannot make such promises, as it may be important to share that information with other staff for safety reasons. “I cannot make that promise Mr. Adams as it might be important for me to share it with the other staff”. Describe and give examples of nontherapeutic communication techniques • Non-Therapeutic Communication: not goal-directed, false reassurances, double messages, giving personal opinions, making assumptions of feelings, asking “Why” questions, showing disapproval, excessive questioning, non-attending behaviors, poor non-verbal communication (eye rolling, staring off into distance, ignoring patient). o Double Bind Messages: intent of the message is to cause confusion o Double Messages: conflicting/mixed messages Describe the types of nonverbal communication- give examples • Tone of voice (tone, pitch, intensity, stuttering, silence, pausing) • Facial expressions (frown, smile, grimaces, raises eyebrows, licks lips) • Posture (slumps over, puts face in hands, taps feet, fidgets with fingers) • Amount of eye contact (angry, suspicious or accusatory looks, wandering) • Sighs • Hand gestures (fidgeting, snapping fingers) • Yawning Cultural Considerations- discusses how these impact the nursing assessment, communication, give examples of cultural differences • Always have a medically trained interpreter for non-English speaking patients. • Communication Styles: some Hispanics/Italians use hand gestures & dramatic body language when describing emotional problems. French/Americans use animated facial expressions and hands during communication. African Americans can be guarded and highly selective in their communication outside of their cultural group. • Eye Contact: Some consider eye contact disrespectful. Hispanics avoid eye contact with authority figures as a sign of respect. Asian cultures believe eye contact is disrespectful (they prefer to shift eye glances towards neck instead of meeting eyes). Haiti – it is customary to hold eye contact with everyone but the poor. • Touch: Hispanics, Italian, & French are accustomed to frequent handholding and touch. Check facility policy on touch (especially with teens and children who could have experienced inappropriate touch in the past) • Cultural Filters: cultural bias; determines what we notice and what we ignore. Bias builds distorted understanding and treat people unfairly. Define Negligence, Autonomy, Justice, Beneficence, Fidelity, and Veracity- Be able to give examples of each: o Negligence –or malpractice is an act or an omission to act that breaches the duty of due care and results in or is responsible for a person’s injuries. The five elements required to prove negligence are: (1) duty, (2) breach of duty, (3) cause in fact, (4) proximate cause, and (5) damages. o Example – A nurse know that a patient’s IV is malfunctioning and the wires are frayed, but decides not to act in a timely manner and leaves the IV on the patient and doesn’t tag it for repair, this results in the patient dying. o Beneficence - This relates to the quality of doing good and can be described as charity. o Example - A nurse helps a newly admitted client who has psychosis feel safe in the environment of the mental health facility. o Autonomy - This refers to the client’s right to make her own decisions. But the client must accept the consequences of those decisions. The client must also respect the decisions of others. o Example - Rather than giving advice to a client who has difficulty making decisions, a nurse helps the client explore all alternatives and arrive at a choice. o Justice - This is defined as fair and equal treatment for all. o Example - During a treatment team meeting, a nurse leads a discussion regarding whether or not two clients who broke the same facility rule were treated equally. o Fidelity - This relates to loyalty and faithfulness to the client and to one’s duty. o Example - A client asks a nurse to be present when he talks to his mother for the first time in a year. The nurse remains with the client during this interaction. o Veracity - This refers to being honest when dealing with a client. o Example - A client states, “You and that other staff member were talking about me, weren’t you?” The nurse truthfully replies, “We were discussing ways to help you relate to the other clients in a more positive way.” Describe the use of seclusion- what it for, when is it appropriate: • Use of seclusion rooms and/or restraints may be warranted and authorized for clients in some cases. In general, seclusion and/or restraint should be ordered for the shortest duration necessary, and only if less restrictive measures are not sufficient. They are for the physical protection of the client and/or the protection of other clients and staff. *A client may voluntarily request temporary seclusion in cases in which the environment is disturbing or seems too stimulating. * *Restraints can be either physical or chemical, such as neuroleptic medication to calm the client. * Seclusion and/or restraint must never be used for: • Convenience of the staff • Punishment of the client • Clients who are extremely physically or mentally unstable • Clients who cannot tolerate the decreased stimulation of a seclusion room When all other less restrictive means have been tried to prevent a client from harming self or others, the following must occur in order for seclusion or restraint to be used: • The primary care provider in writing must order the treatment. • The order must specify the duration of treatment. • The provider must rewrite the order, specifying the type of restraint, every 24 hr. or the frequency of time specified by facility policy. Nursing responsibilities must be identified in the protocol, including how often the client should be: • Assessed (including for safety and physical needs), and the client’s behavior documented • Offered food and fluid • Toileted • Monitored for vital signs Complete documentation includes a description of the following: • Precipitating events and behavior of the client prior to seclusion or restraint • Alternative actions taken to avoid seclusion or restraint • The time treatment began • The client’s current behavior, what foods or fluids were offered and taken, needs provided for, and vital signs • Medication administration • An emergency situation must be present for the charge nurse to use seclusion or restraints without first obtaining a provider’s written order. If this treatment is initiated, the nurse must obtain the written order within a specified period of time (usually 15 to 30 min). Discuss patient rights during an involuntary vs. voluntary admission: Voluntary Commitment – The client or client’s guardian chooses commitment to a mental health facility in order to obtain treatment. A voluntarily committed client has the right to apply for release at any time. This client is considered competent, and so has the right to refuse medication and treatment. Involuntary (civil) Commitment – The client enters the mental health facility against her will for an indefinite period of time. The commitment is based on the client’s need for psychiatric treatment, the risk of harm to self or others, or the inability to provide self-care. The need for commitment could be determined by a judge of the court or by another agency. The number of physicians, which is usually two, required to certify that the client’s condition requires commitment varies from state to state. • Emergency Involuntary Commitment – A type of involuntary commitment in which the client is hospitalized to prevent harm to self or others. Emergency commitment is usually temporary (may be up to 10 days). Primary care providers, mental health providers, or police officers usually impose this type of commitment. • Observational/Temporary Involuntary Commitment – A type of involuntary commitment in which the client is in need of observation, a diagnosis, and a treatment plan. The time for this type of commitment is controlled by state statute and varies greatly between states. A family member, legal guardian, primary care provider, or a mental health provider may impose this. • Long-Term/formal Involuntary Commitment – A type of commitment that is similar to temporary commitment but must be imposed by the courts. Time of commitment varies, but is usually 60 to 180 days. Sometimes, there is no set release date. • Clients admitted under involuntary commitment are still considered competent and have the right to refuse treatment, unless they have gone through a legal competency hearing and have been judged incompetent. The client who has been judged incompetent has a temporary or permanent guardian, usually a family member if possible, appointed by the court. The guardian can sign informed consent for the client. The guardian is expected to consider what the client would want if he were still competent. Describe the impact of Duty to Warn and Tort Law to nursing: • Duty to Warn – The California Supreme Court, 1974, Tarasoff v. Regents of University of California, ruled that a psychotherapist has a duty to warn a patient’s potential victim of potential harm. Duty to warn usually includes the following: o Assessing and predicting the patient’s danger of violence toward another. o Identifying the specific individual(s) being threatened. o Taking appropriate action to protect the identified victim • Tort - Some legal issues regarding health care may be decided in court using a specialized civil category called a tort. A tort is a wrongful act or injury committed by an entity or person against another person or another person’s property. Torts can be used to decide liability issues, as well as intentional issues that may involve criminal penalties, such as abuse of a client. Understand what different classes of medications are used for: Antidepressants - is a substance that prevents/relieves depression. o SSRI (Selective Serotonin Reuptake Inhibitor) – (Associated NT: Serotonin). Anti-Depressant drugs that blocks reuptake of Serotonin. SSRI’s have fewer side effects than TCA’s. (Ex: fluoxetine, citalopram, sertraline). Black Box Warning: increased suicidal thoughts are possible. Takes 2-4 weeks to work. Helps treat Depression, ETOH withdrawal, OCD, ▪ Side Effects: Anxiety, tremors, sexual dysfunction, H/A, agitation, sleeplessness. ▪ S/Sx of Overdose: Serotonin Syndrome (fever, Hyper- Reflexia, sweating, high BP, delirium, hostility). Wait 2 weeks before starting an MAOI or vice-versa. ▪ Contraindications: Those who have attempted suicide don’t use! Pregnancy, Renal/Liver issues o Tricyclic Antidepressant (TCA) – (Associated NT: Norepinephrine & Serotonin). Anti-Depressant drugs that block reuptake of Norepinephrine & Serotonin (so there’s more available). Helps elevate mood. Used for Depression, anorexia, insomnia, ODC, Panic disorder, and neurogenic pain (Mosby’s Pocket Dictionary, 2015). Takes 10-14 days to become effective. Provider will chose this drug if (1) it worked on family member in past and (2) severity of adverse effects. Start with LOW dose and gradually increase if necessary. ▪ Side Effects: Anticholinergic effects (urinary retention, dry mouth, blurred vision, tachycardia, constipation, reflux), Postural Hypotension (increasing falls risk w/this med) ▪ S/Sx of Overdose: tachycardia, MI, heart block, dysrhythmias ▪ Contraindications: Elderly and those with Cardiac Disease ▪ Labs to Watch: o MAOI– (Associated NT: Norepinephrine) Prevents MAO enzyme from breaking down Norepinephrine. Helps treat Depression when other medications fail to work. Irreversible inhabitation of MAO. (ex: Phenelzine) ▪ Side Effects: insomnia, palpitations, H/A, loss of libido, Orthostatic Hypotension ▪ Contraindications: Foods with Tyramine (causes Hypertensive Crisis), Pregnancy ▪ Vitals to Watch: BP and Liver Function Anxiolytics – (Associated NT: GABA). Drug used to depress the CNS; Treats Anxiety, ETOH Withdrawal. o Benzodiazepines – Drug that acts in the Limbic & RAS System to make GABA more effective; depresses CNS to block the S/Sx of Anxiety. ▪ Side Effects: CNS Depression, urinary retention, dry mouth, constipation. ▪ S/Sx of Overdose: ▪ Contraindications: pregnancy, Glaucoma, Renal/Liver issues ▪ Considerations: Patient can build tolerance; monitor Antipsychotics – (Associated NT: Dopamine). Dopamine-receptor blocker that helps people to organize their thoughts, alters perception and behavior. ▪ Side Effects: EPS, CNS Depression, Anticholinergic Effects (dry mouth very common, nasal congestion, constipation), Neuroleptic Malignant Syndrome ▪ Vitals to Monitor: Pulse, BP, Respirations ▪ Contraindications: Beta-Blockers & Alcohol. ▪ Labs to Watch: CBC, LFT’s, Glucose o Typical – Blocks Dopamine receptors. Used for Schizophrenia. (Ex: Chlorpromazine). o Atypical – are newer antipsychotic drugs that block both dopamine and serotonin receptors. Doesn’t have as severe adverse effects as Typical Antipsychotics. If patient has EPS with Typicals, then an Atypical is used. PET Scan/SPECT Scan • Show us evidence of metabolic changes in unmedicated individuals with Depression, Schizophrenia or OCD. Functional MRI • Shows us the effectiveness of psychotropic drugs. Helps us properly dose patients because these tests show us their cognitive function after meds are given. Parts of the Brain & their Function [Show More]
Last updated: 1 year ago
Preview 1 out of 12 pages
 (1).png)
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Oct 27, 2021
Number of pages
12
Written in
Additional information
This document has been written for:
Uploaded
Oct 27, 2021
Downloads
0
Views
29





.png)