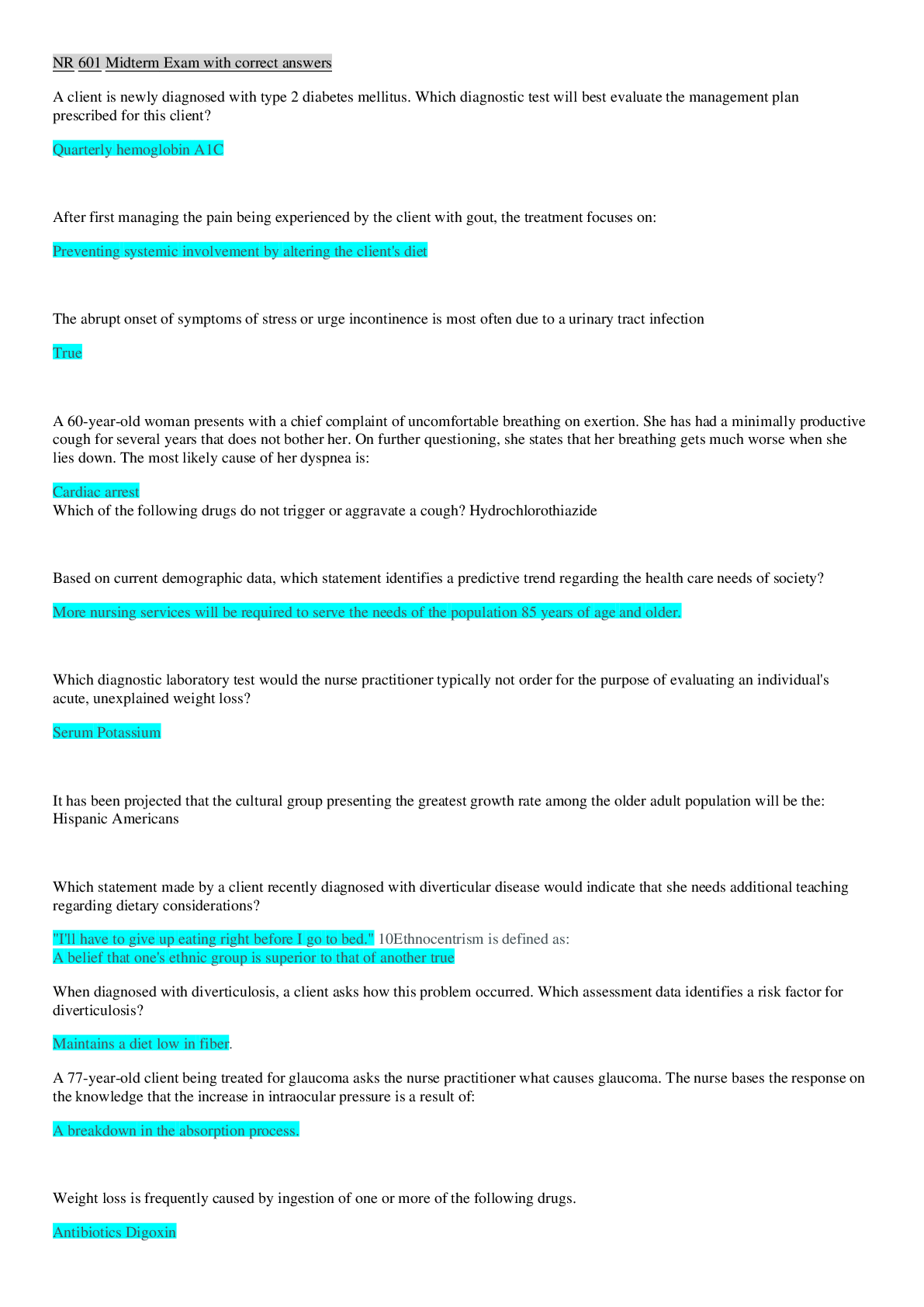
*NURSING > EXAM > Chamberlain College of Nursing - NR 601 Midterm Exam Information: Questions and Answers (All)
Chamberlain College of Nursing - NR 601 Midterm Exam Information: Questions and Answers
Document Content and Description Below
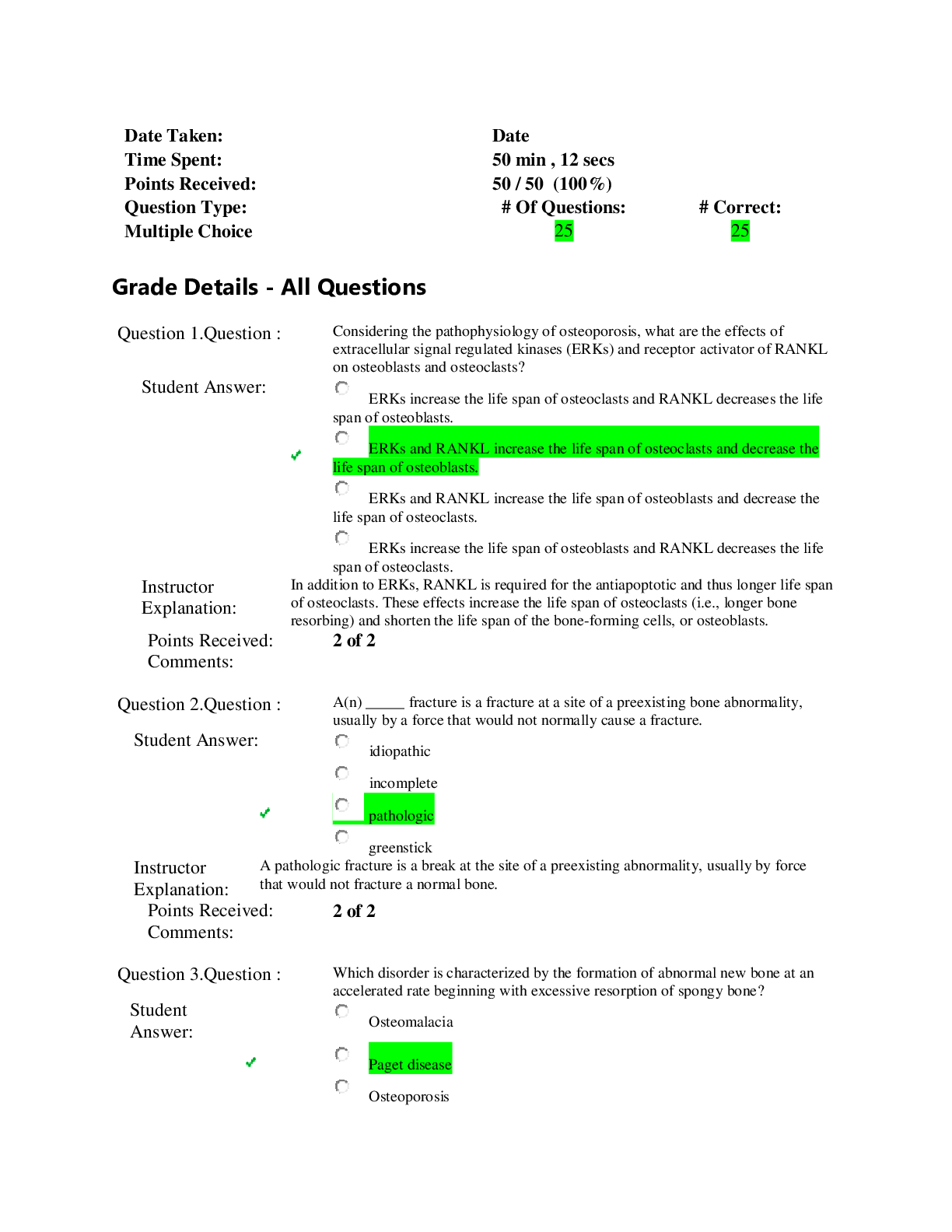
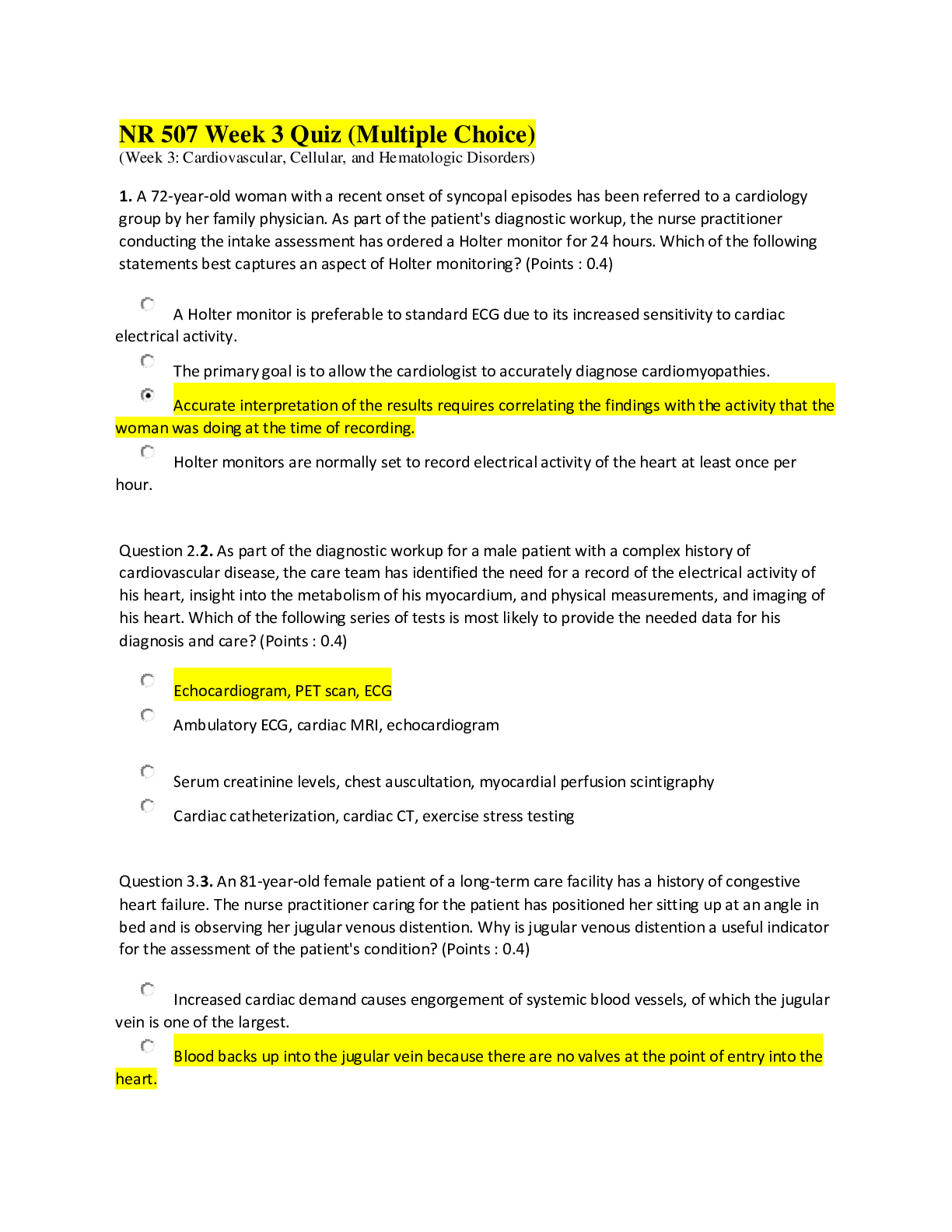
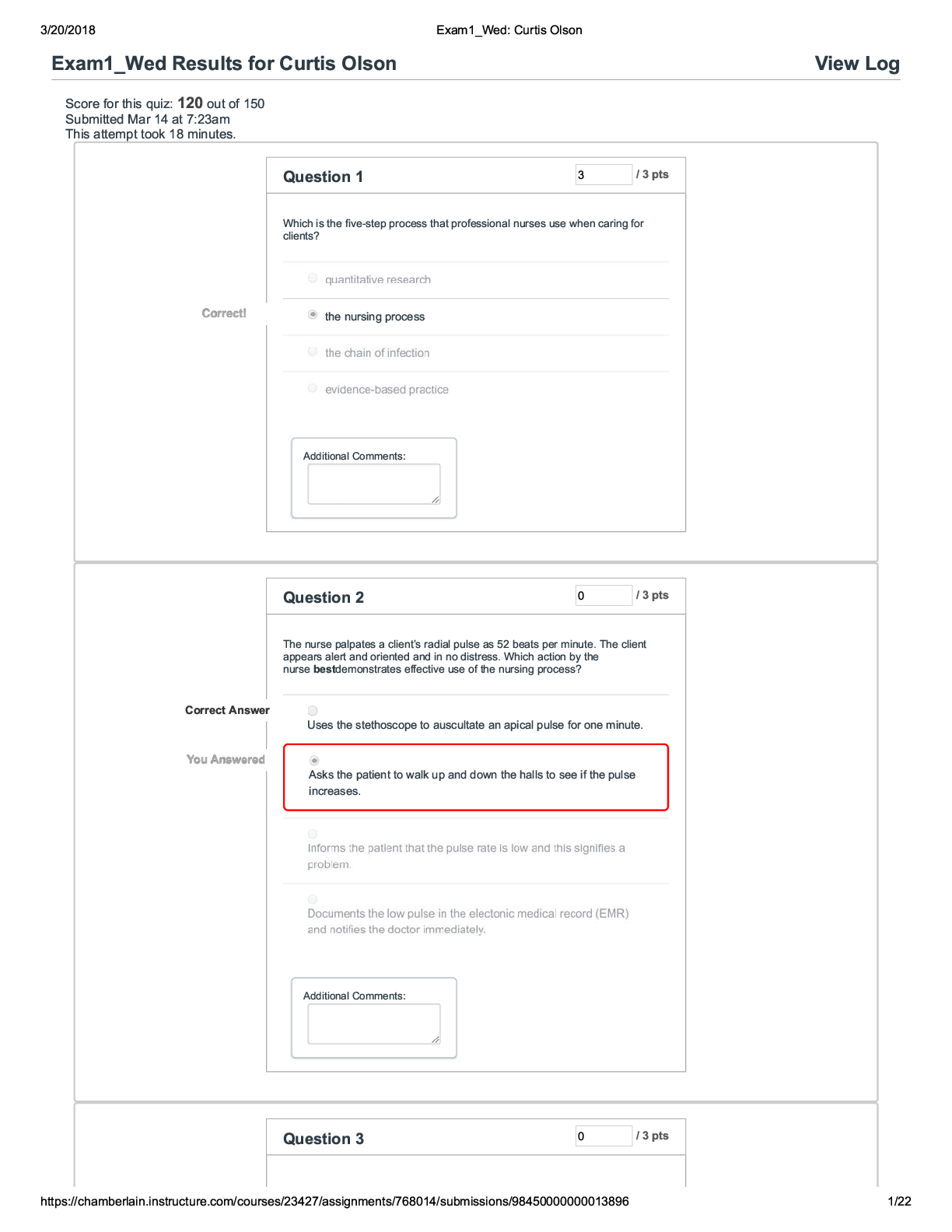
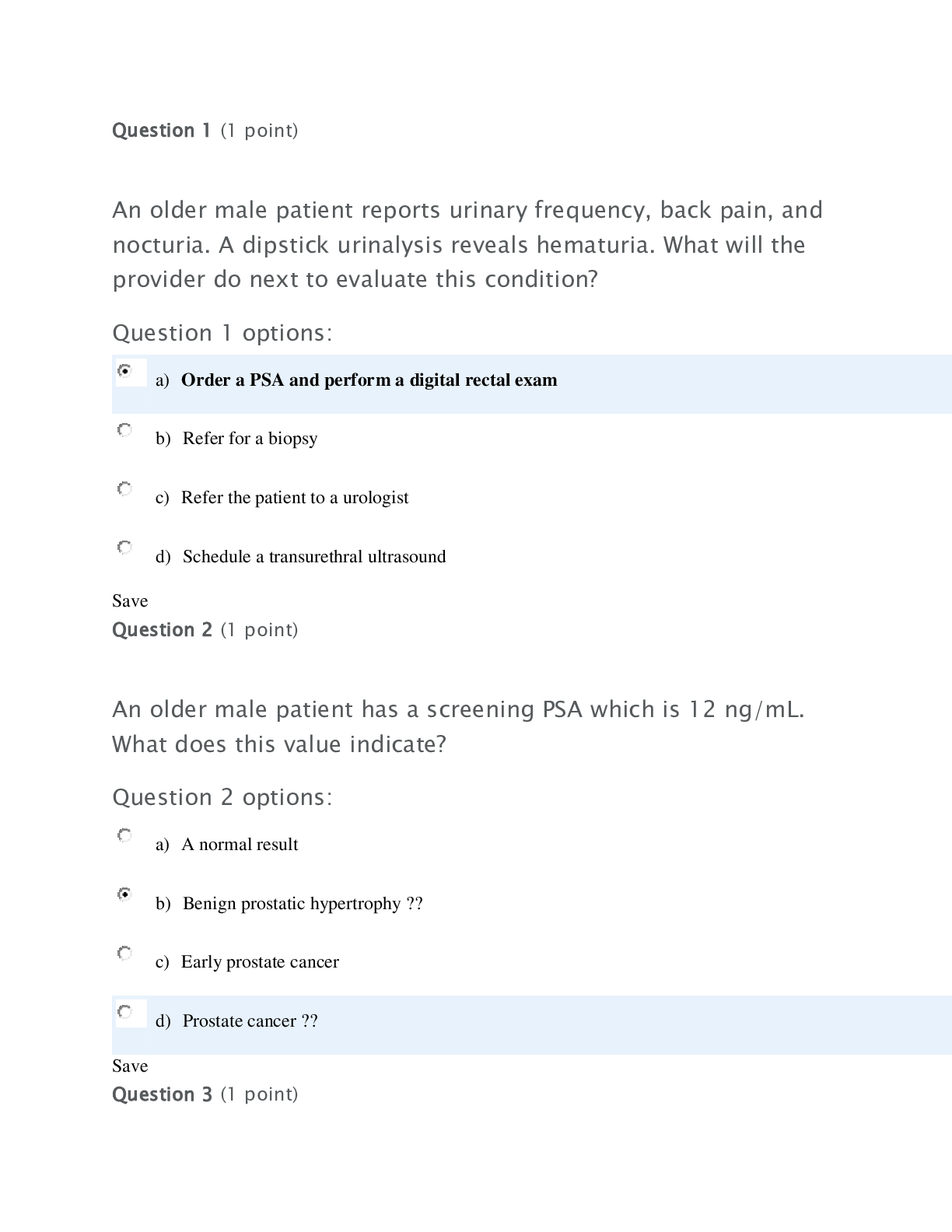
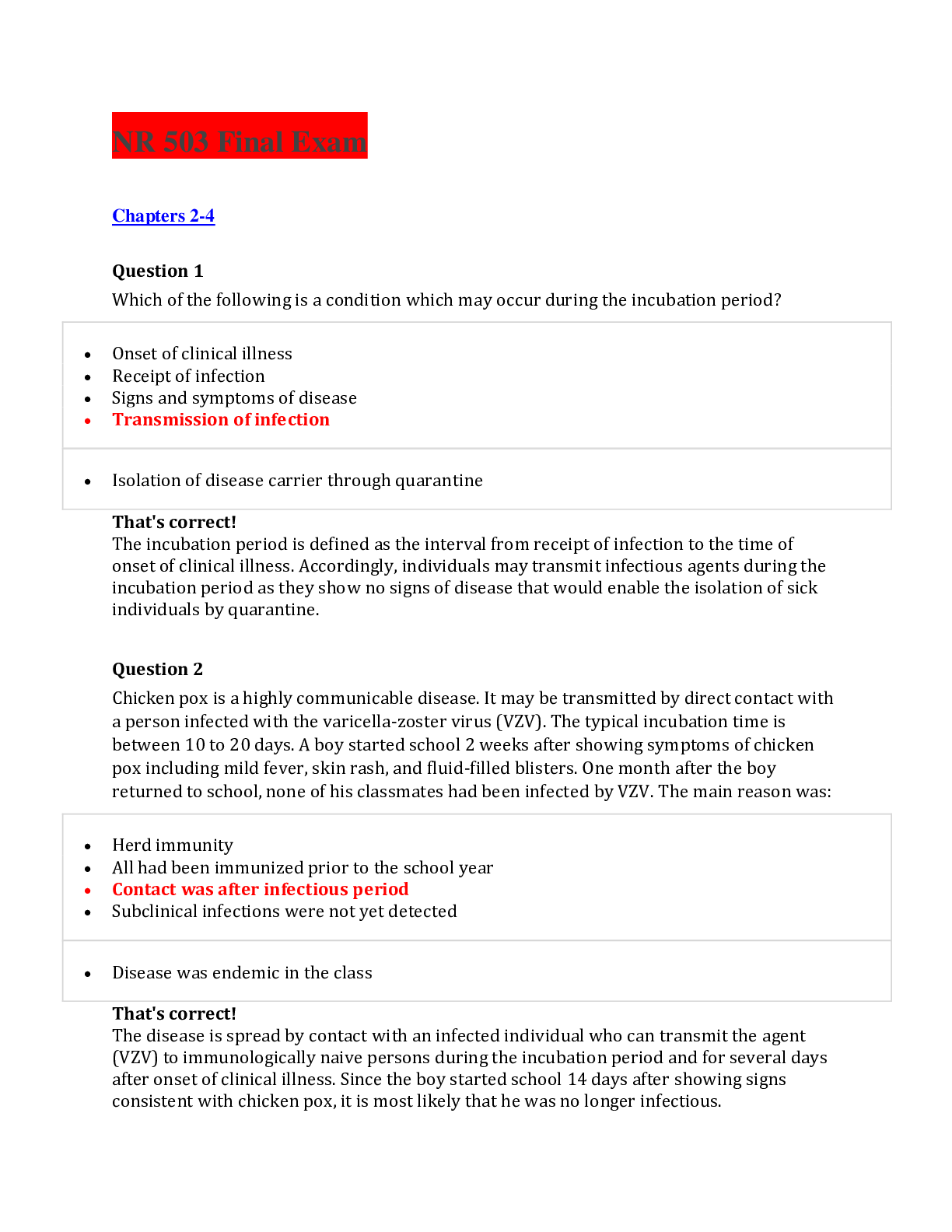
NR 601 Midterm Exam Information: Questions and Answers 1. The percentage of the FVC expired in one second is: a. FEV1/FVC ratio 2. The aging process causes what normal physiological changes in ... the heart? a. The heart valve thickens and becomes rigid, secondary to fibrosis and sclerosis. 3. A 55yo Caucasian male follows up after referral to cardiologist. He thinks his med is causing a cough and sometimes he has difficulty breathing. Which med was most likely prescribed? a. Lisinopril 4. JM is a 68yo man who presents for a physical. He has T2DM x5yrs, smokes 1/2 PPD, BMI is 30. No other previous medical dx, no current complaints. According to the AHA/ACC guidelines, JM is stage A HF. Treatment goals for him include: a. Heart healthy lifestyle 5. MJ presents with h/o structural damage with current s/s of HF. Treatment will be based on his stage of HF, which is: a. Stage C 6. 65yo Caucasian female presents with mitral valve stenosis, physical exam unremarkable. You know her stage of HF is: a. B 7. DG, 65yo man, presents for eval of CP and L-sided shoulder pain, beginning after strenuous activity, including walking. Pain is dull, aching, 8/10 during activity, otherwise 0/10. Began few mo ago, intermittent, aggravated by exercise, relieved by rest. Occasional nausea. Pain is retrosternal, radiating to L shoulder, affects QOL by limiting activity. Pain is worse today, did not go away after stopped walking. BP 120/80, HR 72 and regular. Normal heart sounds, no murmur, S1, S2. Which differential dx would be most likely? a. Coronary artery dz w/angina pectoris 8. The best way to dx structural heart dz/dysfunction non-invasively is: a. Echocardiogram 9. Chronic pain can have major impact on pt's ability to function and have profound impact on overall QOL. Ongoing pain may be linked to: a. Depression, sleep disturbance, decreased socialization 10. The Beers criteria are appropriate for use in evaluating use of certain meds in pts: a. >65yo 11. Pt presents with c/o increasing SOB, cough w/occasional white sputum, fatigue. As part of the plan you order labs. You know the likelihood of HF is low if the BNP is: a. <100 12. All of the following statements are true about lab values in older adults except: a. Normal ranges may not be applicable to older adults b. Abnormal findings are often due to physiological aging c. Reference ranges are preferable d. References values are not necessarily acceptable values a. B 13. According to the 2017 ACC HTN guidelines, the recommended BP goal for a 65yo African American woman w/a h/o HTN and DM and no h/o CKD is: a. <140/80 14. The pathophysiology of HF is due to: a. Inadequate cardiac output to meet the metabolic and O2 demands of the body 15. A 60yo woman w/30 pack yr hx, presents for eval of persistent, daily cough w/increased sputum, worse in the AM, occurring over past 3 months. She tells you, "I have the same thing year after year." Which of the following choices would you consider strongly in your critical thinking process? a. Chronic bronchitis 16. JM is a 68yo man who presents for a physical. He has T2DM x5yrs, diet controlled. His BMI is 32. He has HTN, smoker (10 cigs/day x20yrs). He denies other medical problems. Fam hx includes CAD, CABG x4 for dad, now deceased; CHF, T2DM, HTN for mom. He is asymptomatic today, exam is normal, EKG NSR. According to AHA/ACC guidelines, JM is at risk for what stage of HF? a. Stage A The volume of air a pt is able to exhale for total duration of the test during maximal effort is: b. FVC 17. According to the 2017 ACC HTN guidelines, normal BP is: a. <120/80 18. Functional abilities are best assessed by: a. Observed assessment of function 19. LB is a 77yo pt w/chronic poorly controlled HTN. You know that goals include prevention of target organ damage. During your eval you will assess for evidence of: a. L ventricular hypertrophy 20. Aortic regurgitation requires medical treatment for early signs of HF with: a. ACEi 21. The volume of air in the lungs at max inflation is: a. TLC (total lung capacity) 22. Preferred amount of exercise for older adults is: a. 30min/day of aerobic activity 5 days/wk 23. The total volume of air a pt is able to exhale in the first second during max effort is: a. FEV1 24. You know the following statements regarding the pain of acute coronary syndrome are true except: a. Present atypically more often in men than women 25. Elderly pt presents w/new onset of feeling heart race, fatigue. EKG reveals afib w/rate >100. Pt also has a new tremor in both hands. Which of the following would you suspect? a. Hyperthyroidism 26. 62yo female c/o fatigue, lack of energy. Constipation increased, pt gained 10lbs in past 3mo. Depression is denied although pt reports lack of interest in usual hobbies. VS are WNL, skin is dry/cool. Which of the following must be included in the DD? a. Hypothyroidism 27. Mrs. Black, 87yo, has been taking 100mcg Synthroid x10yrs. She comes for routine follow-up, feeling well. HR is 90. Your first response is to: a. Order TSH 28. Which pt is most likely to have osteoporosis? 29. 80yo underweight male who smokes and has been on steroids for psoriasis 30. When evaluating the expected outcome for hypothyroid elderly pt on levothyroxine, you will: a. Assess TSH in 4-6wks 31. Postmenopausal woman w/osteoporosis is taking bisphosphonate daily PO. What action info statement would indicate she understood your instructions regarding this med? a. Take med w/full glass of water when up in the AM 30min before other food and meds 32. Primary reason levothyroxine sodium is initiated at low dose in elderly pt w/hypothyroidism is to prevent which of the following untoward effects? a. Angina and arrhythmia 33. 6mo ago an elderly pt was dx'd w/subclinical hypothyroidism. Today the pt returns and has TSH of 11 and c/o fatigue. He has taken Synthroid 25mcg daily as prescribed. What is the best course of action? a. Double the dose 34. A fluoroquinolone (Cipro) is prescribed for a male pt w/a UTI. What should you teach him regarding this med? a. Its effectiveness is decreased by antacids, iron, or caffeine 35. Pt has been rx'd metformin (Glucophage). One wk later, he returns w/lowered BGL but c/o loose stools during the week. How should you respond? a. Reassure him that this is an anticipated SE 36. Which of the following s/s of hyperthyroidism commonly manifest in younger populations, but is notably lacking in elderly? a. Exopthalmos 37. 60yo obese male has T2DM and lipid panel of TC = 250, HDL = 32, LDL = 165. You teach him about his modifiable cardiac risk factors, which include: a. DM, obesity, hyperlipidemia 38. Diabetic pt presents w/R foot pain but denies any recent known injury. He states it has gotten progressively worse over past few months. On exam, vibratory sense, as well as sensation tested w/monofilament, was abnormal. Pt's foot is warm, edematous, misshapen. You suspect Charcot foot. What intervention is indicated? a. Referral to orthopedist 39. What is a s/s of insulin resistance that can present in African Americans? a. Acanthosis Nigricans 40. During routine exam of 62yo female, you ID xanthelasma around both eyes. What is the significance of this? a. Abnormal lipid metabolism requiring medical management 41. Mr. White is 62yo, had CKD that has been relatively stable. He also has h/o hyperlipidemia, OA, HTN. He is compliant w/meds, BP has been well controlled on CCB. Last lipids showed: TC = 201, HDL = 40, TG = 180, LDL = 98. He currently takes Crestor 20mg daily. Today his BP is 188/90 and urine dip shows significant proteinuria. He denies changes in dietary habits or med regimen. What would be the best med change at this point? a. Change CCB to ACEi 42. You are working as NP in Fast Track of ER. 76yo male presents w/LUQ pain. There can be many conditions that present as LUQ pain, but which of the following is least likely to cause pain here? a. Acute pancreatitis 43. Which is cardinal feature of failure to thrive? a. Poor nutritional status 44. Feeding gastrostomy tubes at end-of-life Alzheimer's pt's have been associated with: a. Aspiration pna 45. Which of the following nutritional indicators is not an indication of poor nutritional status in elderly? a. BMI 25 46. OA of cervical and lumbar spine causes pain related to all of the following except: a. Crystal deposition 47. In differentiating OA from chronic gout, pseudogout, or septic arthritis, the most valuable diagnostic study would be: a. Synovial fluid analysis 48. Pt's w/OA of hip and knee often have distinguishable gait described as: a. Antalgic 49. Which of the following best describes pain associated w/OA? a. Begins upon arising and after prolonged wt bearing and/or use of the joint 50. Joint effusions typically occur later in the course of OA, especially in the: 51. Knee 52. You ordered CBC for your pt you suspect has polymyalgia rheumatica (PMR). Which 2 clinical findings are common in pt's w/PMR? a. Normochromic, normocytic anemia and thrombocytosis 53. You suspect your pt has PMR and now are concerned that they may have Giant Cell Arteritis (GCA) too. Which of the following 2 symptoms are most indicative of GCA and PMR? a. Scalp tenderness and aching in shoulder and pelvic girdle 54. 63yo Caucasian pt w/PMR will begin Tx w/corticosteroids until the condition has resolved. You look over her records and it has been 2yrs since her last physical exam and any labs or diagnostic tests as she relocated and had not yet ID'd a provider. In prioritizing your management plan, your first orders should include: a. Duel-energy x-ray (DEXA) scan and updating immunizations 55. Which of the following DD for pt's presenting w/PMR can be ruled out w/a muscle biopsy? a. Polymyositis 56. In reviewing lab results for pt's w/suspected PMR, you realize there is no definitive test to dx PMR, rather clinical response to Tx. Results you would expect to see include: a. Elevated erythrocyte sed rate (ESR) >50 57. Which of the following is the most appropriate lab test for monitoring gout therapy over the long-term? a. Serum urate level 58. In providing health teaching related to dietary restrictions, you should advise a pt w/gout to avoid which of the following dietary items: a. Beer, sausage, fried seafood 59. The best method of verifying gout dx in a joint is which of the following: 60. Joint aspiration and polarized-light microscopy 61. The most appropriate first-line Tx for acute gout flare is (assuming no kidney dz or elevated bleeding risk): a. Indomethacin 50mg TID x2 days, then 25mg TID x3 days 62. You order bilat wrist XR on 69yo man c/o pain both wrists x6 wks no related to any known trauma. You suspect early onset RA. The initial XR finding in a pt w/elderly onset RA would be: a. Soft tissue swelling 63. A 72yo female has been dx'd w/gout. She also has h/o chronic HF. The most likely contributing factor to development of gout in this older female is: a. Thiazide diuretics 64. Which of the following statements about OA is true? 65. It affects primarily wt-bearing joints 66. In considering the specificity of lab data, the most reliable diagnostic test listed below would be: a. Synovial fluid analysis to differentiate between infectious versus inflammatory infusion 67. When examining the spine of an older adult you notice a curvature w/a sharp angle. This is referred to as a: a. Gibbus 68. The prevalence of depression in nursing home residents is ___________ greater than adults living in the community. a. 3-4 times 69. The majority of depressed older adults remain untreated because of: a. Misdiagnosis, social stigma, environmental barriers 70. Symptoms of depression distinct to the elderly include: a. Lack of emotions 71. The justification for ordering CBC, TSH, serum B12 for a pt you may suspect have clinical depression is: a. Because of overlapping symptoms w/anemia, thyroid dysfunction, and nutritional deficiencies 72. One major difference that is useful in the DD of dementia versus delirium is that: a. Dementia develops slowly and delirium develops quickly 73. Which of the following is the most appropriate screening tool for delirium? a. Confusion Assessment Method 74. The proposed mechanism by which diphenhydramine causes delirium is: a. Anticholinergic effects 75. The elderly are at high risk for delirium because of: a. Multisensory declines, polypharmacy, multiple medical problems 76. A consistent finding in delirium, regardless of cause, is: a. Reduction in regional cerebral perfusion 77. Older adults w/dementia sometimes suffer from agnosia, which is defined as the inability to: a. Recognize objects 78. In late stages of dementia, a phenomenon called sun downing occurs, in which cognitive disturbances tend to: a. Become worse in the evening 79. Of the following, which one is the most useful clinical eval tool to assist in the dx of dementia? a. St. Louis University Mental Status Exam (SLUMS) 80. The cornerstone of pharmacotherapy in treating Alzheimer's is: a. Cholinesterase inhibitors 81. The comorbid psych problem w/the highest frequency in dementia is: a. Anxiety 82. When treating depression associated w/dementia, which of the following would be a poor choice and should not be prescribed? a. Amitriptyline 83. Which of the following should be avoided in countries where food and water precautions are to be observed? a. Salad buffet 84. What insect precautions are not necessary to prevent insect-borne dz's in the tropics? a. Using 100% DEET on skin to prevent bites 85. An example of secondary prevention you could recommend/order for older adults would be to: a. Check for fecal occult blood 86. Ali is a 72yo man who recently came to US from Nigeria. He reports having BCG (bacille Calmette-Guerin) vax as a child. Which of the following is correct regarding a TB skin test? a. Vax hx is irrelevant; read as usual 87. Leo is a 62yo African American male who comes in for an initial visit. Personal health hx includes smoking 1 PPD since 11yo, consuming a case of beer (24 bottles) every weekend, and working as an assembler (sedentary job) for the past 10yrs. Fam Hx in first-degree relatives includes HTN, high cholesterol, MI, T2DM. Leo's BMI is 32. BP is 130/86. You order fasting glucose, lipid profile, and return visit for BP check. This is an example of: a. Secondary prevention 88. A local chapter of NP organization has begun planning a community-based screening for HTN at a local congregate living facility. This population was selected on the basis of: a. A recognized element of high risk within this group. 89. Performing ROM exercises on a pt who has had a CVA is an example of which level of prevention? a. Tertiary 90. You demonstrate an understanding of primary prevention of falling among the elderly through which management plan? a. Provide info about meds, SE, interactions 91. An example of an active strategy of health promotion for an individual to accomplish would be: a. Beginning stress management program 92. The 4 main domains of clinical preventive services that you will provide are: a. Counseling interventions, screening tests, immunizations, chemoprophylaxis 93. What is the appropriate method for TB screening of an older adult entering a nursing home? a. 5 TBU intradermal PPD injection and if negative, repeat w/same dose one week later 94. Meds known to contribute to constipation include all of the following except: a. Broad-spectrum abx 95. All of the following are considered contributors to dysphagia except: a. Smooth muscle relaxants 96. The term "geriatric syndrome" is best described as: a. Condition that has multiple underlying factors and involves multiple systems 97. The anal wink reflex is used to test: a. Sensation and pudental nerve function 98. Atypical presentation of acute coronary syndrome is: a. More common in females 99. What dz can mimic and often co-exists w/MI in elderly w/CAD? a. Esophageal dz 100. Thoracic aortic dissection presents typically as: a. Severe retrosternal CP that radiates to the back and both arms 101. Bordetella pertussis is best characterized by: a. Sub-acute cough lasting >2wks 102. Routine testing of TB should occur in all of the following vulnerable populations except: a. Hospitalized elderly 103. Which of the following statements about fluid balance in elderly is false? a. Assessment of skin turgor at the sternum is a reliable indicator of dehydration in elderly. 104. Distinguishing delirium from dementia can be problematic since they may co-exist. The primary consideration in the DD is: a. Rapid change and fluctuating course of cognitive function 105. Presbystasis is best described as: a. Age-related disequilibrium of unknown pathology characterized by gradual onset of difficulty walking 106. If dizziness has a predictable pattern associated w/it, you should first consider: a. Hypoglycemia 107. Evidence shows that the most important predictor of a fall is: a. Prior h/o a fall 108. The most cost-effective interventions used to prevent falls are: 109. Home modifications and vit D supplements 110. Chronic fatigue syndrome is best described as: 111. Fatigue lasting longer than 6mo and not relieved by rest 112. Which form of HA is bilat? 113. Tension 114. Microscopic hematuria is defined as: 115. 3 or more RBCs on 3 or mor samples of urine 116. Risk factors associated with the finding of a malignancy in a pt w/hemoptysis include all of the following except: a. Childhood asthma 117. Recent wt loss is defined as: a. Loss of >10lbs over the past 3-6mo 118. The most common cause of disability in elderly is due to: a. Arthritis 119. Lipedema is best described as: a. Bilat distribution of fat in lower extremities 120. Drug-induced pruritis is distinguished because it: a. May occur right after drug is taken or months later 121. A form of syncope that is more common in elderly than in younger adults is: a. Orthostatic hypotension 122. All of the following statements about tremor are true except: a. The most common tremor is the Parkinson tremor 123. Overflow incontinence is usually associated with: a. Bladder outlet obstruction 124. Wandering is best described as: a. Purposeful excessive ambulatory behavior 125. A key symptom of ischemic heart dz is CP. However, angina equivalents may include exertional dyspnea. Angina equivalents are important because: a. Women w/ischemic heart dz many times don't present w/CP. Some pt's may have no symptoms or atypical symptoms so dx may only be made at the time of the actual MI. 126. Which test is clinical standard for assessment of aortic stenosis? a. Echocardiogram 127. Ischemic heart dz is: a. Defined as an imbalance between O2 supply and demand. Frequently manifested as angina. Leading COD in elderly. 128. Preceding a stress test, the following lab work might include: a. CBC w/diff to differentiate ischemic heart dz from anemia. Thyroid studies to rule out hyperthyroidism. 129. On exam, what type of murmur can be auscultated w/aortic regurg? a. Austin flint 130. Which of the following statements is true regarding anti-arrhythmic drugs? a. Most anti-arrhythmics have low toxic/therapeutic ratio and some are exceedingly toxic. 131. In mitral stenosis, p waves may suggest: a. L atrial enlargement 132. Aortic regurg requires medical tx for early signs of CHF with: a. ACEi 133. The best evidence rating drugs in a post-MI pt include: a. ASA, ACEi/ARB, BB, aldosterone blockade 134. 55yo post-menopausal woman with h/o HTN c/o jaw pain on heavy exertion. No c/o CP. EKG is NSR w/out ST segment abnormalities. Your plan may include: a. Exercise stress test 135. What is the most common valvular heart dz in elderly? a. Aortic stenosis 136. Elderly may present with atypical clinical signs of pna. You need to be aware that clustering of all of the following s/s may indicate pna in the elderly except for: a. Bradycardia 137. A common auscultatory finding in CHF is: a. S3 138. The most common organism responsible for CAP in the elderly is: a. Strep pneumoniae 139. 72yo woman and her husband are driving cross-country. After a long day of driving, they stop to eat. Midway through the meal, the woman becomes very SOB w/CP and a sense of panic. Which problem is most likely? a. Pulmonary embolism 140. Exercise recommended for elderly should include activities that: a. Strengthen muscles 141. Preferred amount of exercise for elderly is: a. 30min of aerobic activity a day 5 days a week 142. Which of the following medical conditions is not considered restrictive for engaging in physical activity? a. Depression 143. The best recommendation for a pt who says they have no equipment to exercise is: a. Improvise w/recommended objects at home that can be used 144. When you recommend exercise for elderly, which of the following pieces of advice should be considered for all types of exercise? a. Start low and go slow 145. All of the following statements are true about lab values in the elderly except: a. Abnormal findings are often due to physiological aging 146. Biochemical individuality is best described as: a. Each individual's variation is often much smaller than that of a larger group 147. All the following statements about drug absorption are false except: a. Underlying chronic dz has little impact on drug absorption 148. The cytochrome p system involves enzymes that are generally: a. Inhibited or induced by drugs 149. A statement not shown to be true about pharmacodynamic changes with aging is: a. Decreased sensitivity to oral anticoagulants 150. The major impact of the physiological changes that occur w/aging is: a. Reduced physiological reserve Reduced homeostatic mechanisms Impaired immunolgoical response 151. The strongest evidence regarding normal physiological aging is available through: a. Longitudinal studies 152. Pharmacokinetic changes w/aging is reflective of: a. What the body does to the drug 153. All of the following statements are true about drug distribution in the elderly except: a. Drugs distributed in water have lower concentration 154. Men have faster and more efficient biotransformation of drugs and this is thought to be due to: a. Testosterone 155. Atypical presentation of dz in elderly is reflected by all the following except: a. MI w/CP and diaphoresis 156. Polypharmacy is best described as taking: a. Even a single med if there is not a clear indication for its use What is the major difference between varicose veins and atherosclerosis? Vessels that are affected Pt has had poorly controlled HTN >10yrs. Indicate the most likely position of his PMI. c. 5th ICS left of MCL 43yo hispanic male has audible diastolic murmur best heard at the mitral point. No audible click. He has been monitored for 2yrs. What is the most likely murmur? d. Mitral stenosis What are PFTs? Group of tests that provide quantifiable measurement of lung function, used to dx resp abnormalities or assess progression/resolution of lung dz. What is FEV1? Forced Expiratory Volume in 1 second (80-120%) What is FVC? Forced Vital Capacity (80-120%) What is normal FEV1/FVC ratio? <0.7 (70%) What is GOLD 1 criteria? Mild FEV1 >/= 80% predicted What is GOLD 2 criteria? Moderate FEV1 50-79% predicted What is GOLD 3 criteria? Severe FEV1 30-49% predicted What is GOLD 4 criteria? Very severe FEV1 <30% predicted What are the signal symptoms of COPD? Dyspnea Chronic cough w/sputum Decreased activity tolerance Wheezing What are characteristics of COPD? Common, preventable, treatable. Characterized by persistent airflow limitation. Usually progressive, associated with enhanced chronic inflammatory response in airways and lungs to noxious particles/gases Airway fibrosis, luminal plugs, airway inflammation, increased airway resistance, small airway dz. Decreased elastic recoil of alveoli. What are risk factors for COPD? Smoking (increasing w/number of pack years) Second hand smoke Environmental pollution (endotoxins, coal dust, mineral dust) What is seen on phys exam in COPD? May be normal in early states As severity progresses: lung hyperinflation, decreased breath sounds, wheezes at bases, distant heart tones (b/c of hyperinflation, so S1/S2 sounds off in distance), accessory muscle use, pursed lip breathing, increased expiratory phase, neck vein distention. How is COPD diagnosed? Spirometry is gold standard (pre and post bronchodilator). Irreversible airflow limitation is hallmark. How is COPD treated? Bronchodilators: beta agonists (long/short), anticholinergics (long/short), or combo. What is the MOA of beta agonists? Stimulates beta-2-adrenergic receptors, increasing cyclic AMP, resulting in relaxing airways. What is the MOA of anticholinergics? Block the effect of acetylcholine on muscarinic type 3 receptors, resulting in bronchodilation. Why are long-acting beta agonists prescribed for COPD? They are for moderate airflow limitation. They relieve symptoms, increase exercise tolerance, reduce number of exacerbations, improve QOL. What are some non pulmonary diagnoses that result in COPD-type symptoms? CHF What are some Hyperventilation syndrome Panic attacks Vocal cord dysfunction Obstructive sleep apnea Aspergillosis Chronic fatigue syndrome What are signal symptoms of asthma? Wheezing Shortness of breath Cough (esp at night) Chest tightness What is chronic bronchitis? Daily chronic cough w/increased sputum for at least 3 consecutive months in at least 2 consecutive years. Usually worse on wakening. May or may not be associated with COPD. What is emphysema? Characterized by obstruction to airflow caused by abnormal airspace enlargement distal to terminal bronchioles. Chronic inflammation/remodeling, trapping air, hindering effective O2/CO2 exchange (all due to inflammatory mediators infiltrating airways). What are signal symptoms of ischemic heart dz? Chest pain Chest tightness Chest discomfort What is ischemic heart dz? Imbalance between supply and demand for blood flow to myocardium What are signal symptoms of lung CA? Cough Dyspnea Wt loss Anorexia Hemoptysis What is lung CA? Malignant neoplasm originating in parenchyma of lung/airways What are signal symptoms of MI? Prolonged CP (>20min duration) SOB Confusion Weakness Worsening HF What is an MI? Necrosis of heart tissue caused by lack of blood and O2 supply to the heart What are signal symptoms of pneumonia? Fever Chills Hypothermia New cough w/or w/out sputum Chest discomfort or dyspnea Fatigue HA Some older adults will be asymptomatic but may experience falls/confusion What is community acquired pneumonia? Acute lower resp tract infection of lung parenchyma. Can be bacterial or viral. Bacterial is most common in older adults. What are signal symptoms of a PE? Dyspnea CP on inspiration Anxiety Presentation is variable Symptoms nonspecific Some asymptomatic What is PE description? Occlusion of one or more pulmonary vessels by traveling thrombus originating from distant site. What are signal symptoms of tuberculosis? Initially asymptomatic Later: productive, prolonged cough Fatigue Low-grade fever Night sweats Poor appetite Hemoptysis Wt loss Fever/sweats are less common in elderly Symptoms in elderly are often attributed to other comorbidities What is tuberculosis? Chronic, necrotizing infection caused by slow-growing acid-fast bacillus (Mycobacterium tuberculosis). Most common cause of death related to infectious dz worldwide. What are signal symptoms of valvular heart dz? Asymptomatic in early stages Fatigue Exertional dyspnea What is valvular heart dz? Damage to valve(s) of the heart, causing cardiac dysfunction. Most prevalent types in elderly: calcific and degenerative aortic valve dz What is aortic stenosis? Abnormal narrowing of aortic valve orifice What is aortic regurgitation? Retrograde blood flow through incompetent aortic valve into L ventricle during ventricular diastole What is mitral stenosis? Abnormal narrowing of mitral valve orifice What is mitral regurgitation? Retrograde blood flow during systole from L ventricle into L atrium through incompetent mitral valve What is mitral valve prolapse? Mitral regurgitation associated with bulging of one or both mitral valve leaflets into L atrium during ventricular systole What are most common causes of VHD in elderly? Age-related degenerative calcifications Myxomatous degeneration Papillary muscle dysfunction Infective endocarditis Rheumatic dz What happens in valvular regurgitation? Portion of the ejected blood leaks back into the upstream cardiac chamber What happens in valvular stenosis? Usually results in elevated pressures in the chamber upstream from the stenosis What are signal symptoms of URI? Nasal congestion Rhinorrhea/mucopurulent discharge Sore throat Cough HA Malaise What is a URI? Most frequently called the common cold Usually caused by virus Results in nasal passage inflammation Most are self-limiting, accompanied by minor complaints Included in URI dx: acute laryngitis, acute rhinosinusitis, acute pharyngitis What are signal symptoms of restrictive lung dz? Rapid, shallow respirations Dyspnea Decreased activity tolerance Easily fatigued Nonproductive, irritating cough provoked by deep breathing/exertion What is restrictive lung dz? Heterogenous group of disorders that share common abnormal ventilatory function. Characterized by small tidal volume, rapid rate. Hallmark restrictive pattern is decreased lung volm, esp. total lung capacity and vital capacity. What is the purpose of functional assessment of the elderly? Discovers the ability to care for themselves on a daily bases What can ongoing pain be linked to in the elderly? Depression Decreased socialization Sleep disturbance Impaired cognitive function Is chronic pain a normal sign of aging? No What is polypharmacy? Broad definition, but basically too many medications for what is going on with the patient, the use of multiple pharmacies/providers. What is Stage A of HF? At high risk for heart failure but w/out structural changes/symptoms What is Stage B HF? Structural heart dz but w/out s/s of HF (still "at risk" for HF) What is Stage C HF? Structural heart dz w/prior or current s/s of HF (actually have HF) What is Stage D HF? Refractory heart failure including specialized interventions (actually have HF, need surgery, PM, etc.) What are treatment goals for Stage A HF? Heart-healthy lifestyle Prevent vascular, coronary dz Prevent LV structural abnormalities What are drugs used in Stage A HF? ACEi or ARB in appropriate pt's for vascular dz or DM Statins as appropriate What are treatment goals for Stage B HF? Prevent HF symptoms Prevent further cardiac remodeling What are drugs used in Stage B HF? ACEi or ARB as appropriate Beta blockers as appropriate In selected pt's: ICD Revascularization/valvular surgery as appropriate What are goals of Stage C HFpEF? Control symptoms Improve HRQOL Prevent hospitalization Prevent mortality ID comorbidities What is treatment for Stage C HFpEF? Diuresis to relieve s/s congestion Follow guideline-driven indications for comorbidities (HTN, AF, CAD, DM, etc.) What are treatment goals for Stage C HFrEF? Control symptoms Pt education Prevent hospitalization Prevent mortality What are drugs used in Stage C HFrEF? Diuretics for fluid retention ACEi or ARB BB Aldosterone antagonists Drugs in selected pts: Hydralazine/isosorbide dinitrate ACEi and ARB Digitalis Procedures in selected pts: CRT ICD Revascularization/valvular surgery as appropriate What are treatment goals in Stage D HF? Control symptoms Improve HRQOL Reduce hospital readmissions Establish pt's end-of-life goals What are options for Stage D HF? Advanced care measures Heart transplant Chronic inotropes Temporary or permanent MCS Experimental surgery/drugs Palliative care, hospice ICD deactivation What is the normal BNP level? <100pg/mL (indicates HF is unlikely) What is normal BP? <120/80 What is "elevated" BP? 120-129/<80 What is Stage 1 HTN? 130-139 OR 80-89 What is Stage 2 HTN? >/= 140 or >/= 90 What is recommended BP for DM? <130/80 What is recommended BP for CKD? <130/80 How should HTN be managed? Stage 2 and up should be given consideration for pharm treatment. Others can wait for lifestyle modification. What is first-line meds for non-black HTN population (including those w/DM)? Thiazide, CCB, ACEi, or ARB, either alone or in combo What is the med guideline for ASCVD for those </= 75yo? High-intensity statin (atorvastatin/Lipitor 40-80mg, rosuvastatin/Crestor 20mg) What is the med guideline for ASCVD for those >75yo? Moderate statin (atorvastatin 10mg, rosuvastatin 5mg, simvastatin/Zocor 20-40mg, pravastatin/Pravachol 40mg, lovastatin/Mevacor 40mg, fluvastatin 40mg BID) What is the guideline for meds for LDL >/= 190? High intensity statin (atorvastatin/Lipitor 40-80mg, rosuvastatin/Crestor 20mg) What is the med guideline for ASCVD for 40-75yo w/DM? Their 10yr risk is >7.5%, so high intensity statin (atorvastatin/Lipitor 40-80mg, rosuvastatin/Crestor 20mg) What is the med guideline for LDL 70-189? Their 10yr risk is <7.5%, so moderate intensity statin (atorvastatin/Lipitor 10mg, rosuvastatin/Crestor 5mg, simvastatin/Zocor 20-40mg, pravastatin/Pravachol 40mg, lovastatin/Mevacor 40mg, fluvastatin 40mgBID) What is the ASCVD med guideline for 40-75yo w/out ASCVD or DM? Their 10yr risk is >7.5%, so moderate to high intensity statin The meds listed in Beers Criteria are not absolutely contraindicated in elderly. True The BC recommendations are graded as high, medium, low to assist w/decision making. True The BC list includes dosage adjustments for kidney impairment. True The BC list includes drug to drug interactions to avoid. True Responsible prescribing is an important role of NP and BC can assist in determining the safest meds for geri pts. True What vaccination is recommended for people traveling to countries where dz is common? Hep A How is Hep A vax given? Two doses: initial at least 4wks before departure, second dose 6-12mo later. When is Hep B vax recommended? High-risk people (IV drug users, persons w/multiple partners) How is Hep B vax given? Initial dose 1mo later: 2nd dose 4-6mo after 2nd: 3rd dose When is Zostavax recommended? Anyone over 60yo, given as single dose Can people who have had prior episode of zoster be vaccinated? Yes When is flu vax recommended? Annually for all adults >50yo When should DTaP be given? Once in a lifetime for all adults, then Td booster every 10yrs. When is pneumococcal vax recommended? Once for 65yo and older Younger adults w/severe chronic health conditions What is primary prevention? Activities to prevent occurrence of dz or adverse health condition, including mental health. What is osteoporosis? Skeletal disorder characterized by impaired bone strength that predisposes to increased risk of fracture. Can occur from not only bone loss but also from failure earlier in life to make sufficient bone. Primary: due to aging (increased bone resorption/reduced new bone formation) Secondary: consequence of underlying medical condition/drug What are s/s of osteoporosis? Sometimes not seen until fracture sustained spontaneously or after minimal trauma, usually in thoracic/lumbar vertebrae, hip, wrist, humerus, pelvis. With each fracture, risk of another increases exponentially. Loss of height, kyphosis development. XR: bones appear osteopenic (at least 30% loss in bone mass); spine shows loss of horizontal vertebral trabeculae, accentuating end plates, producing biconcave "codfish" vertebrae; maybe compression fracture. What are diagnostic tests for osteoporosis? XR DEXA (screen all women >65yo, hip/spine; test earlier if major risk factors present; repeat every 3-5yrs depending on degree) What is T-score of -2.5 or lower indicative of? Osteoporosis What is a T-score of -1.0 to -2.5 indicative of? Osteopenia What is a T-score of -1.0 or higher indicative of? Normal bone density What is a Z-score of <-1.5 indicative of? Secondary cause of osteoporosis What are the risk factors for osteoporosis? Previous fracture Advanced age Low body wt/BMI Maternal h/o fracture Current smoking Physical inactivity Excessive exercise resulting in amenorrhea Poor lifetime intake of calcium Endocrine disorders GI dz Chronic systemic illnesses Nutritional deficiencies Meds (steroids, anticonvulsants, thyroid hormone, SSRI, aromatase inhibitors for breast CA) Alcoholism What is the treatment for osteoporosis? Aim to prevent those that are at risk Combine diet, exercise, meds Dietary Ca/vit D Wt-bearing/strength exercises Bisphosphonates Selective estrogen receptor modulators Calcitonin PTH Denosumab Fall prevention How does chronic pain differ from acute pain? [Show More]
Last updated: 1 year ago
Preview 1 out of 22 pages

Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Oct 29, 2020
Number of pages
22
Written in
Additional information
This document has been written for:
Uploaded
Oct 29, 2020
Downloads
0
Views
41