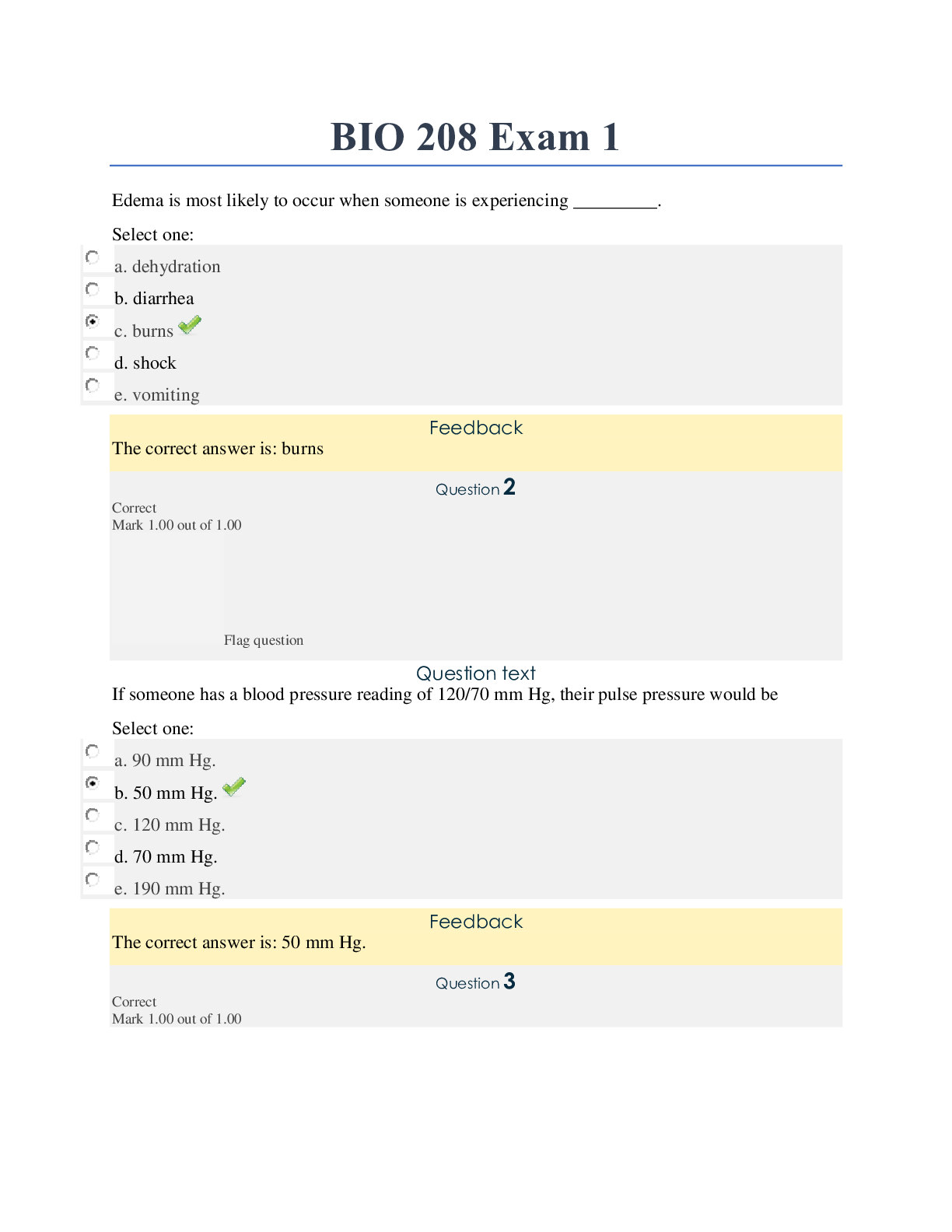
*NURSING > EXAM > Chamberlain College of Nursing - NR 509NR509_SOAP_Note_week2_Respiratory exam. All Filled and Graded (All)
Chamberlain College of Nursing - NR 509NR509_SOAP_Note_week2_Respiratory exam. All Filled and Graded A
Document Content and Description Below
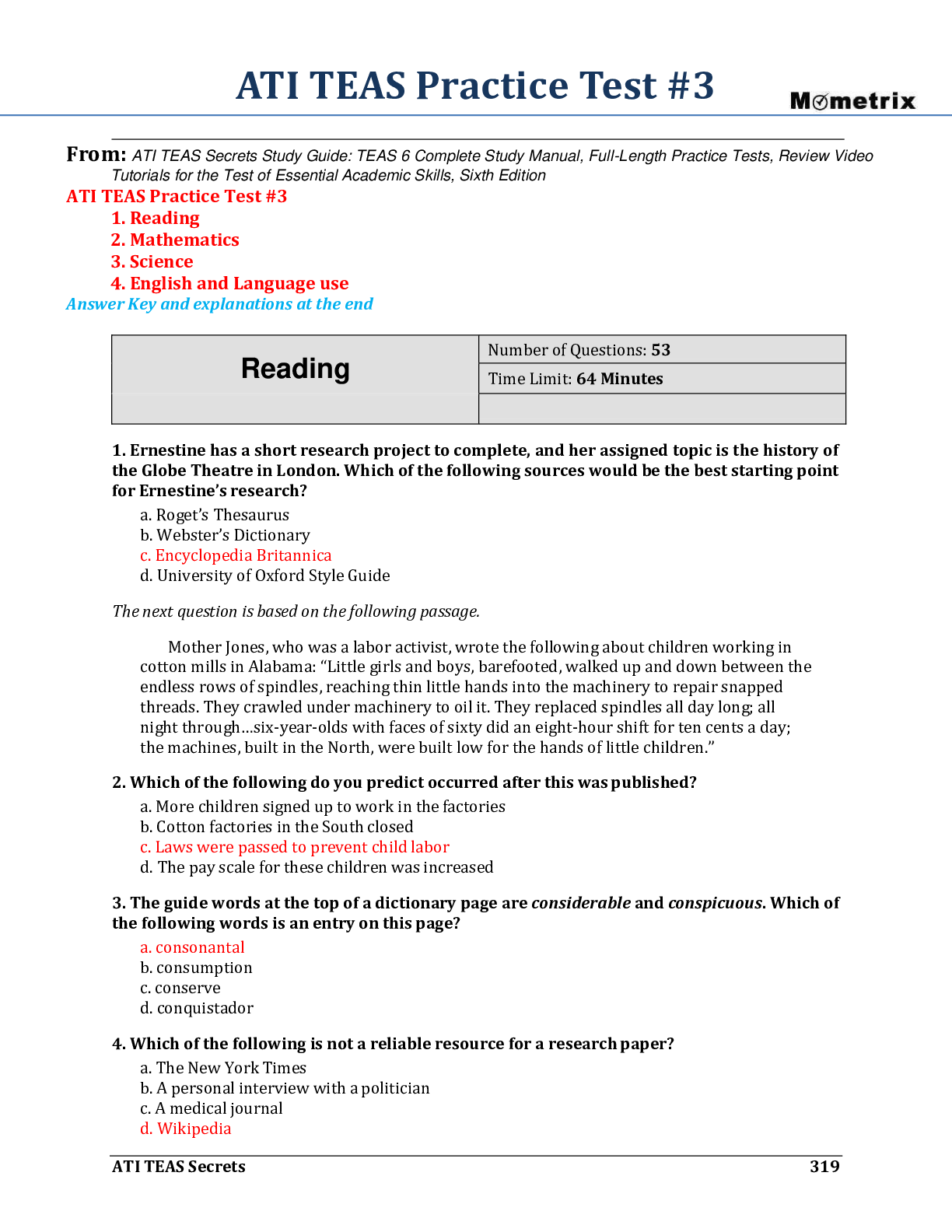
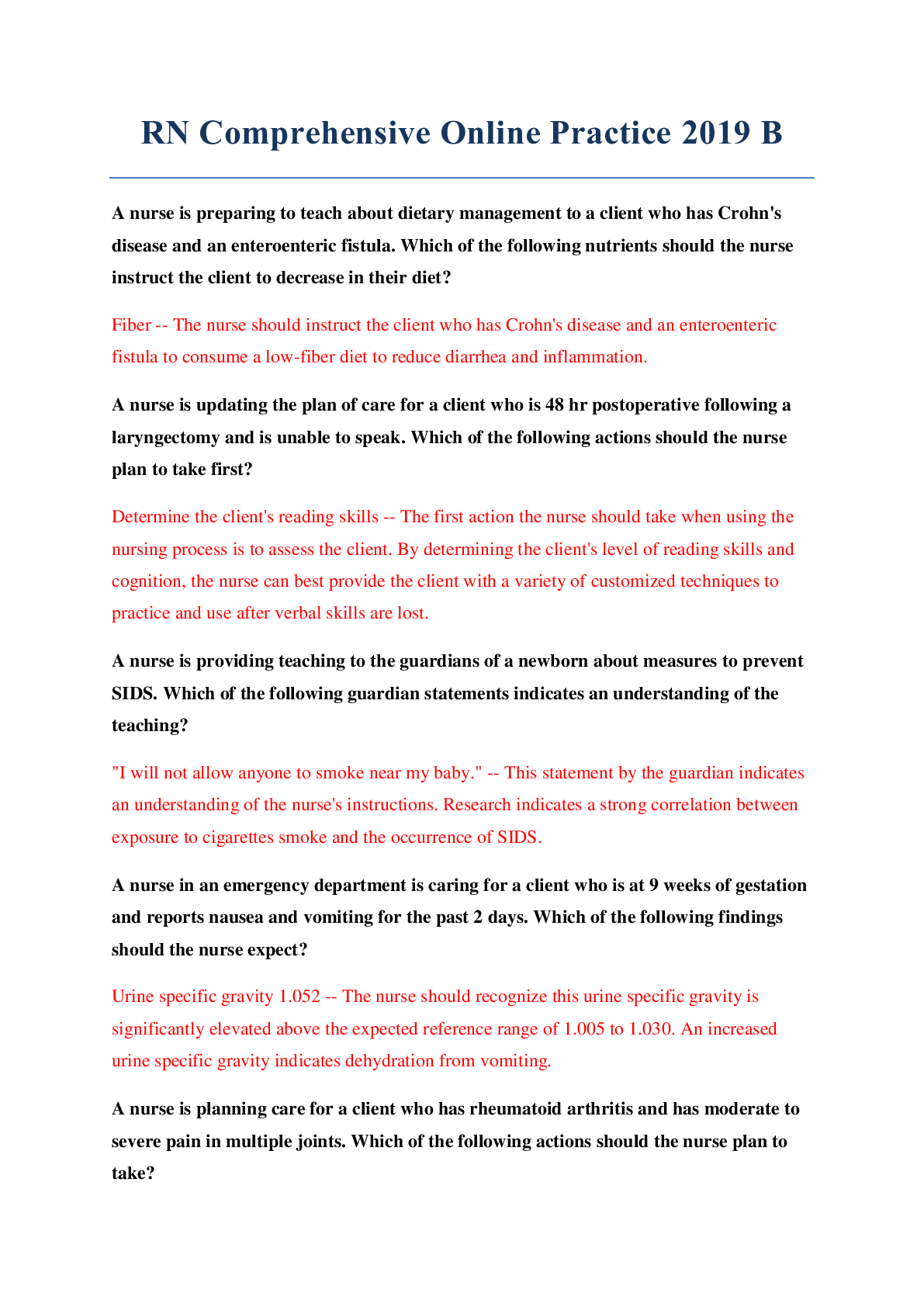
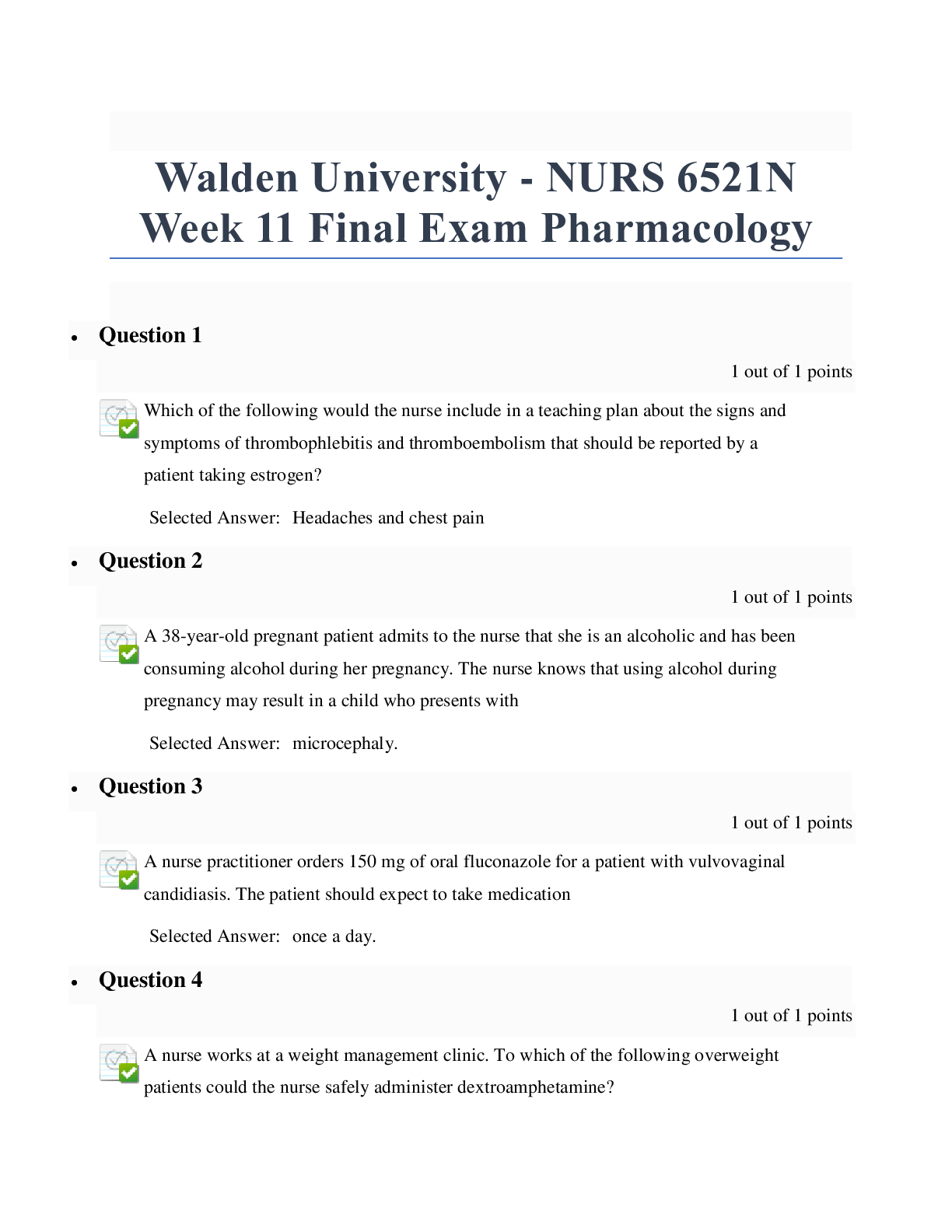
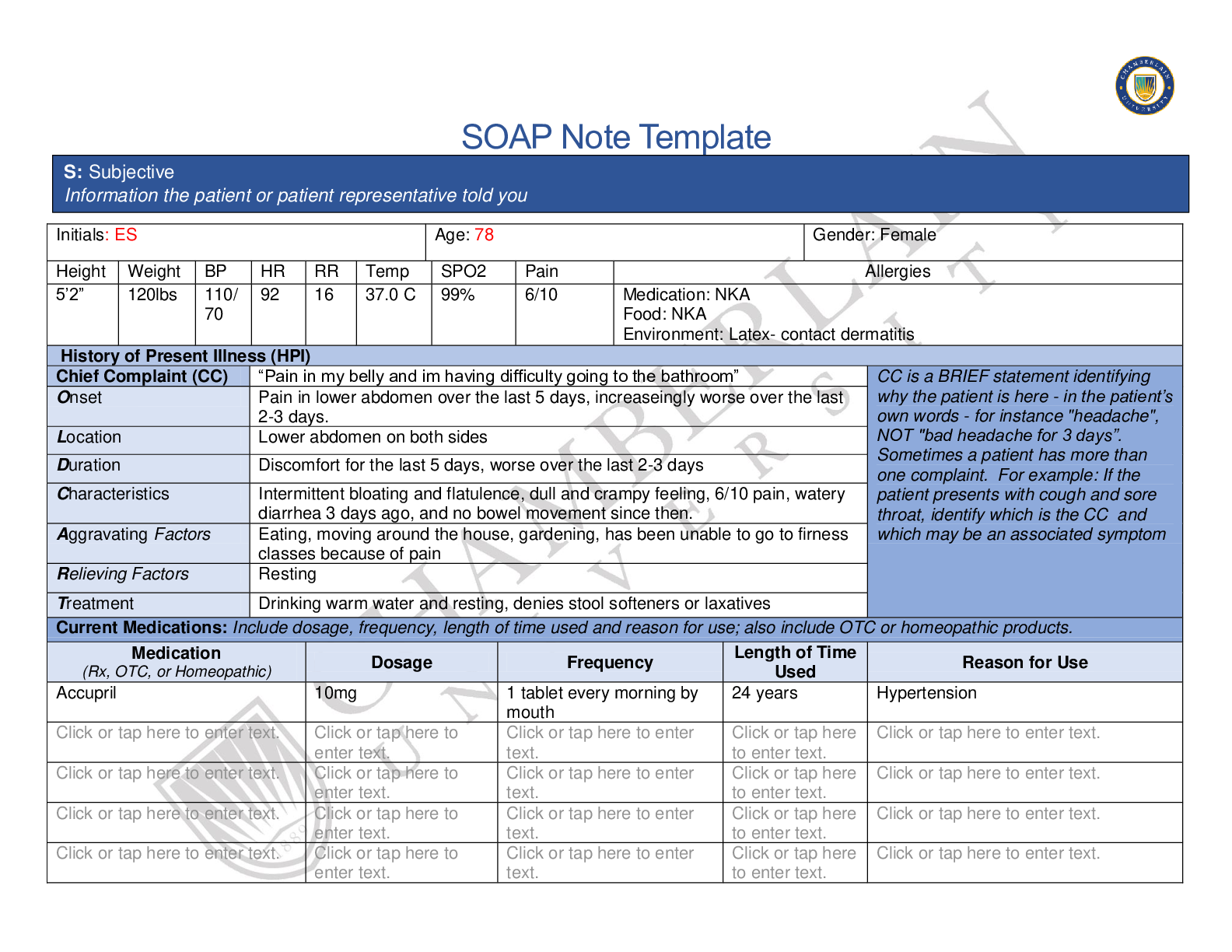
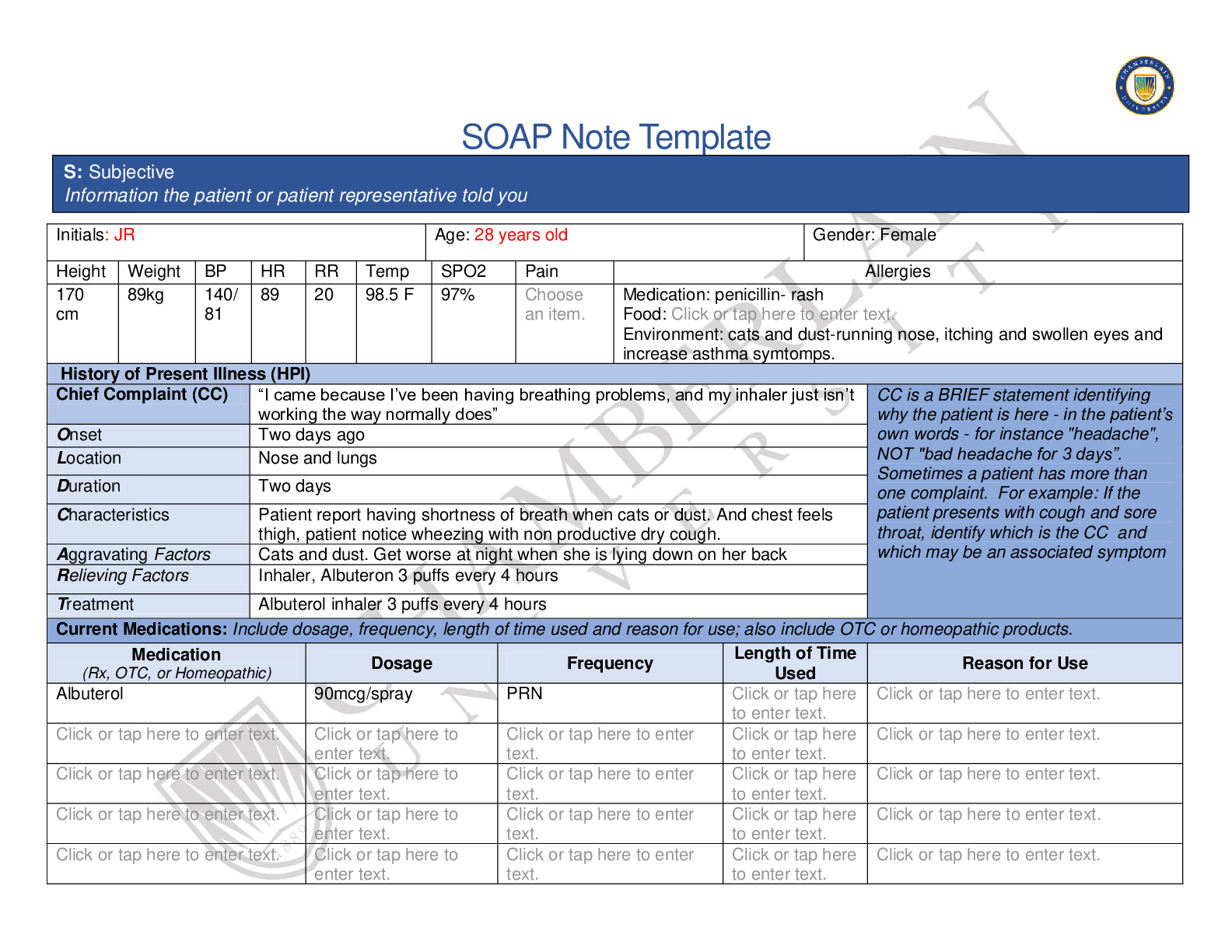
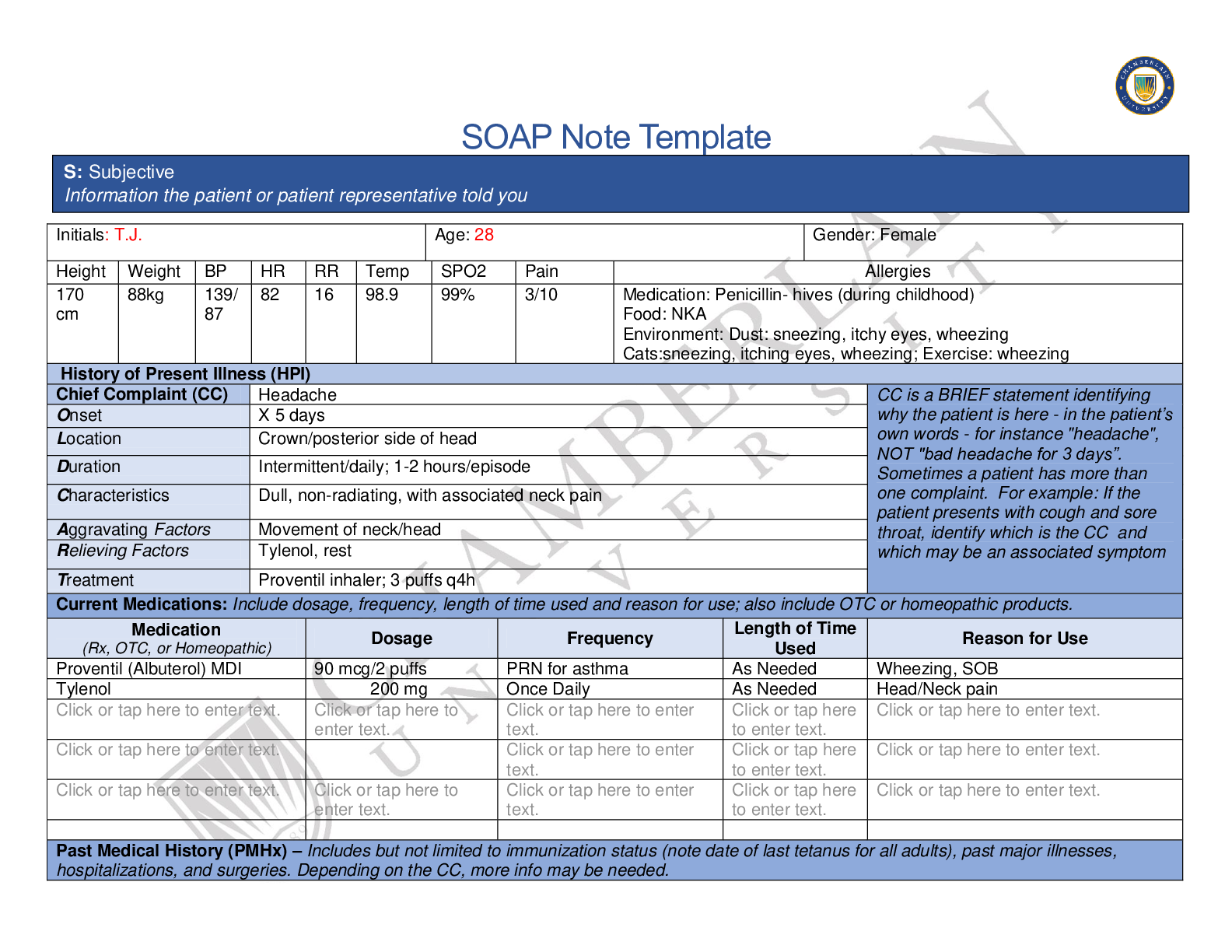
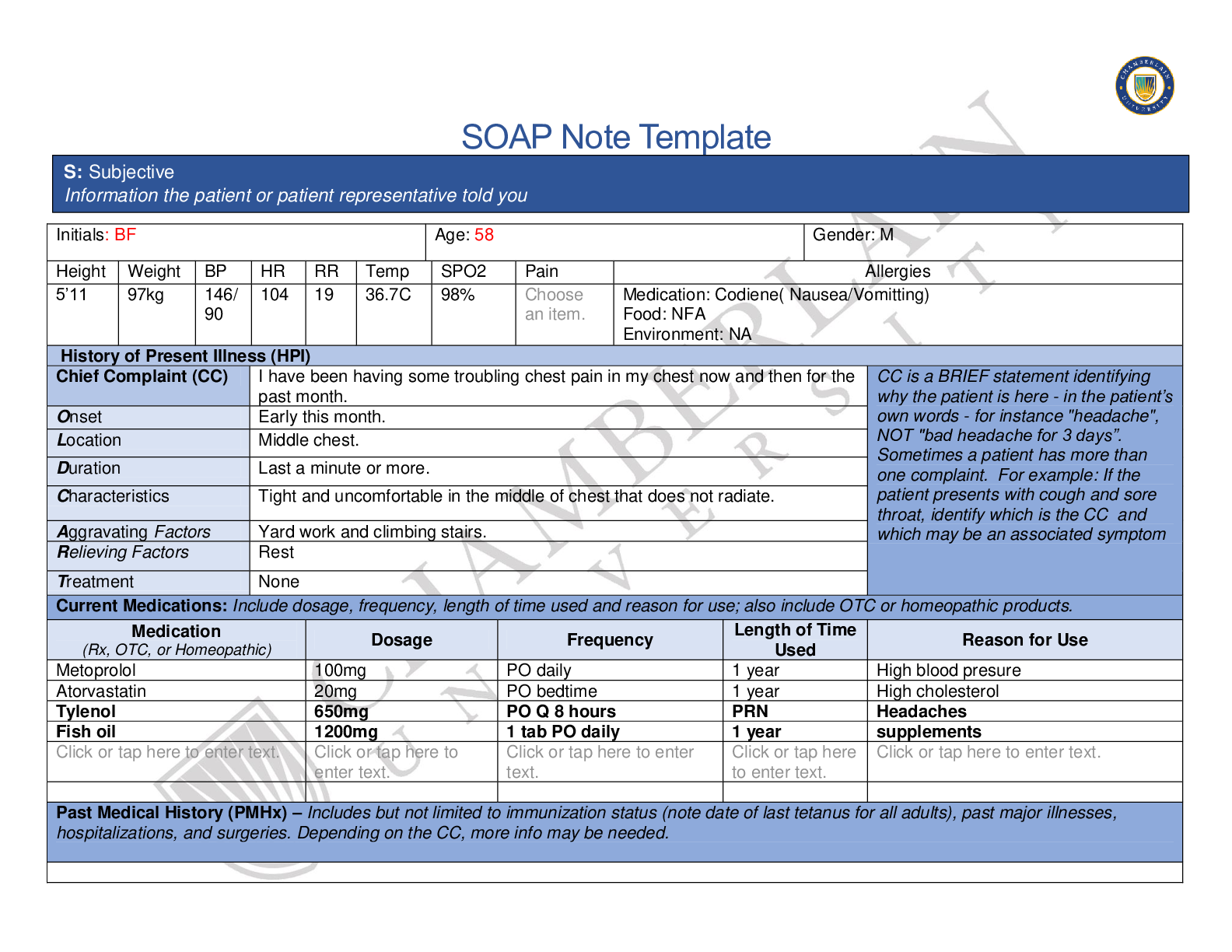
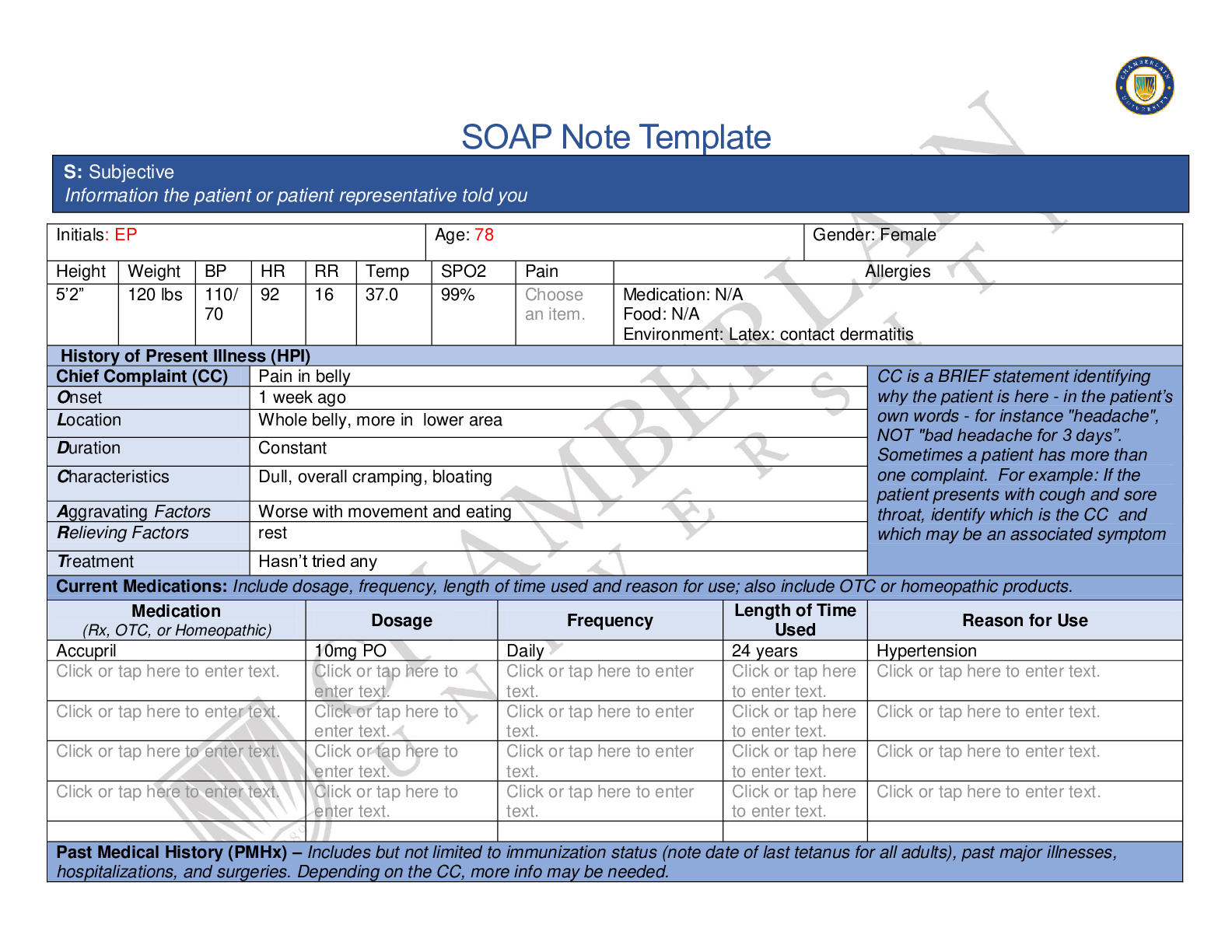
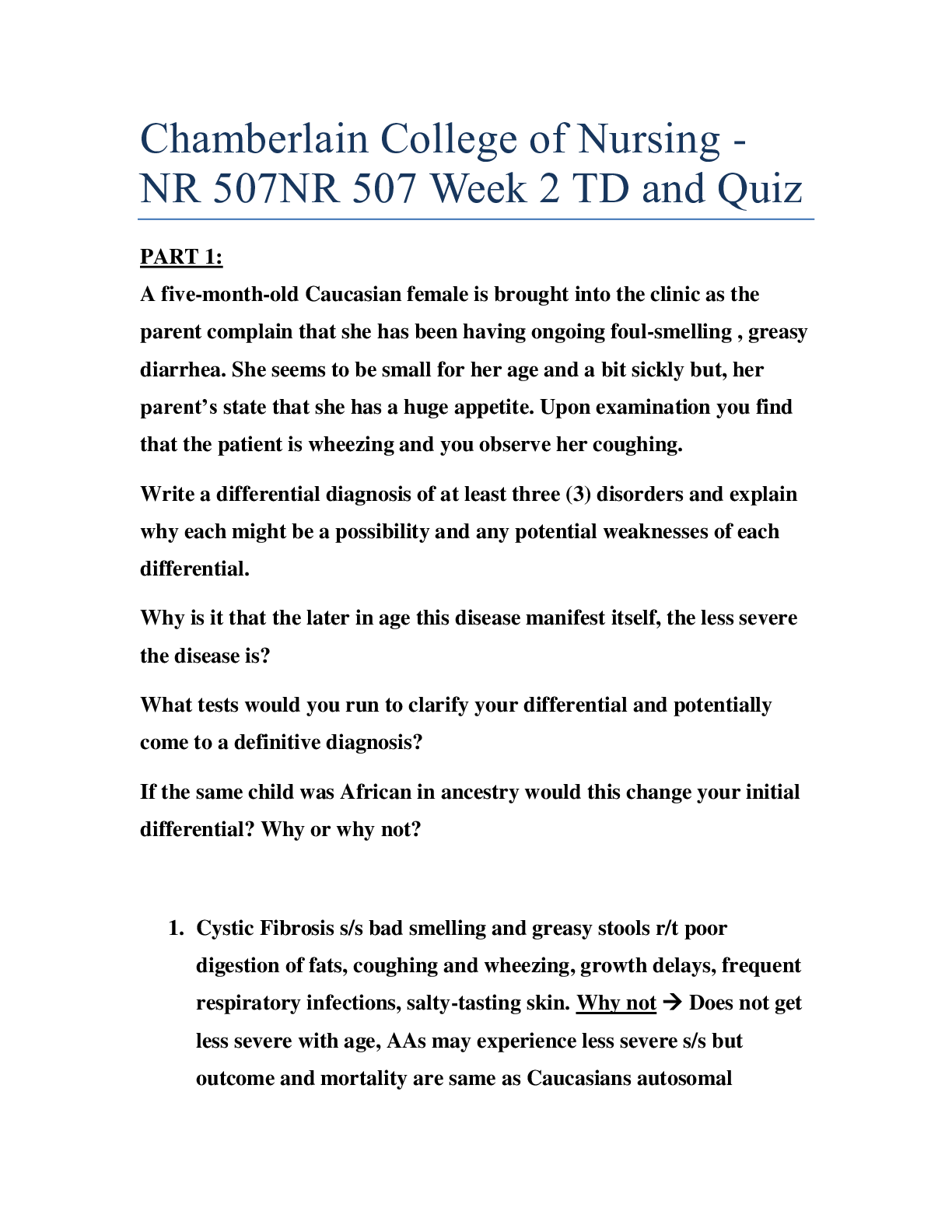
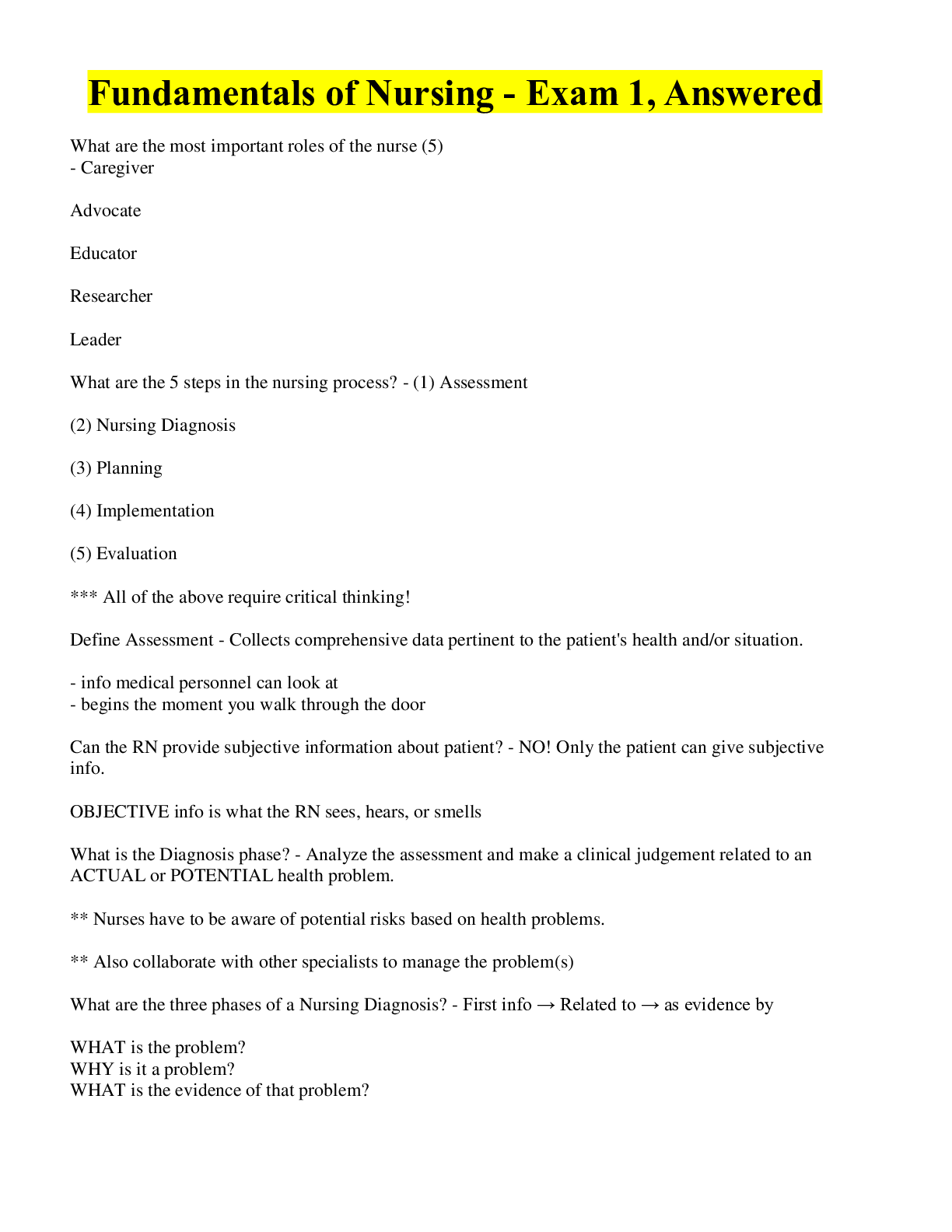
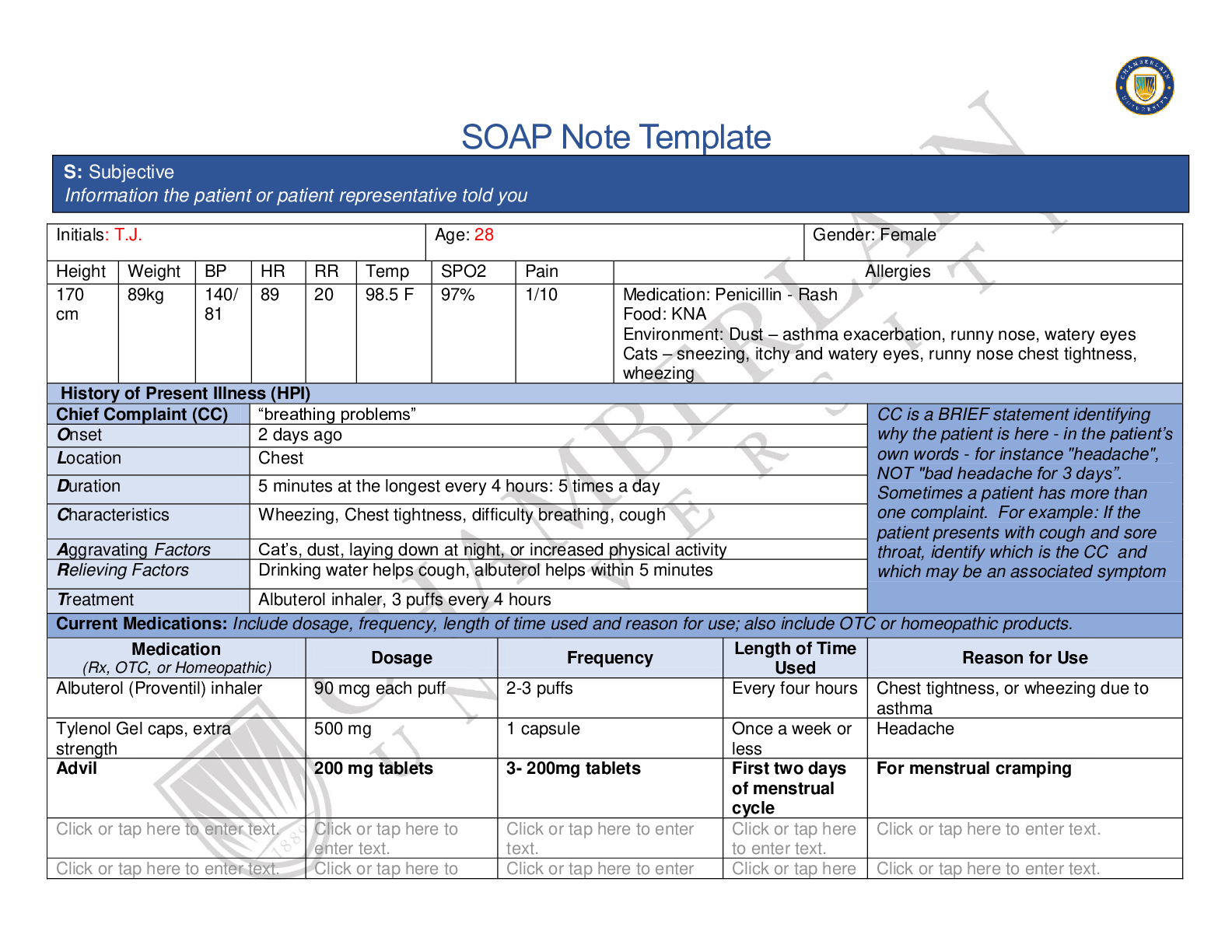
SOAP Note Template Initials: T.J. Age: 28 Gender: Female Height Weight BP HR RR Temp SPO2 Pain Allergies 170 cm 89kg 140/ 81 89 20 98.5 F 97% 1/10 Medication: Penicillin - Rash Food: KNA Envi... ronment: Dust – asthma exacerbation, runny nose, watery eyes Cats – sneezing, itchy and watery eyes, runny nose chest tightness, wheezing History of Present Illness (HPI) Chief Complaint (CC) “breathing problems” CC is a BRIEF statement identifying why the patient is here - in the patient’s own words - for instance "headache", NOT "bad headache for 3 days”. Sometimes a patient has more than one complaint. For example: If the patient presents with cough and sore throat, identify which is the CC and which may be an associated symptom Onset 2 days ago Location Chest Duration 5 minutes at the longest every 4 hours: 5 times a day Characteristics Wheezing, Chest tightness, difficulty breathing, cough Aggravating Factors Cat’s, dust, laying down at night, or increased physical activity Relieving Factors Drinking water helps cough, albuterol helps within 5 minutes Treatment Albuterol inhaler, 3 puffs every 4 hours Current Medications: Include dosage, frequency, length of time used and reason for use; also include OTC or homeopathic products. Medication (Rx, OTC, or Homeopathic) Dosage Frequency Length of Time Used Reason for Use Albuterol (Proventil) inhaler 90 mcg each puff 2-3 puffs Every four hours Chest tightness, or wheezing due to asthma Tylenol Gel caps, extra strength 500 mg 1 capsule Once a week or less Headache Advil 200 mg tablets 3- 200mg tablets First two days of menstrual cycle For menstrual cramping . . enter text. to . . . enter . S: Subjective Information the patient or patient representative told you. text. to . Past Medical History (PMHx) – Includes but not limited to immunization status (note date of last tetanus for all adults), past major illnesses, hospitalizations, and surgeries. Depending on the CC, more info may be needed. Diagnosed with Type 2 Diabetes at the age of 24. Non-compliant with diet Immunizations up to date, Childhood vaccines current. Last Tetanus approximately one year ago. Last Flu vaccine 5-6 years ago. Diagnosed with Asthma at the age of 2 and a half. Hospitalized for Asthma at age 16, Denies surgical history, broken bones, or recent hospitalizations. Heavy Menstrual bleeding, with irregular cycles, mold breast tenderness before cycle. Last PAP smear was four year ago. Normal. No recent dental exam, last dental visit was a few years ago, went twice a week as a child. No recent eye exam. Last exam as a child. Social History (Soc Hx) - Includes but not limited to occupation and major hobbies, family status, tobacco and alcohol use, and any other pertinent data. Include health promotion such as use seat belts all the time or working smoke detectors in the house. Never been married, denies pregnancies. Employed since high school and is a supervisor. Hobbies include reading, attends church, streams TV and documentaries. Denies physical activity outside of work, walks frequently during work hours. Not currently sexually active. Sexual activity began at the age of 18. Straight sexual orientation. Used condoms and the pill for birth control. Lives with mother and sister who are supportive. Has smoke detectors that are working. Uses seat belts. Social alcohol use, 0-4 alcoholic drinks on the weekends. Denies tobacco use, current or past. Is occasionally exposed to second hand smoke through friends. Denies current illicit or recreational drug use. Hx of marijuana use in the past, denies current use, last used at the age of 21. Stopped use due to asthma exacerbation. In college obtain bachelor’s in accounting – 2 semesters left Sleeps about 6-7 hours a night. Family History (Fam Hx) - Includes but not limited to illnesses with possible genetic predisposition, contagious or chronic illnesses. Reason for death of any deceased first degree relatives should be included. Include parents, grandparents, siblings, and children. Include grandchildren if pertinent. Father - HTN, T2DM, Hyperlipidemia – deceased due to car accident 6 months ago Mother –HTN, hyperlipidemia - living Sister – Asthma – living Brother – Obesity - livingPaternal Grandfather- HTN, type 2 diabetes, hyperlipidemia, colon Cancer – deceased due to colon cancer. Paternal Grandmother – HTN - living Maternal Grandmother – HTN, Hyperlipidemia, stroke – deceased from stroke at 73 Maternal Grandfather – HTN, Hyperlipidemia, heart attack – deceased at 80 due to heart attack Paternal Uncle – Alcoholism Denies current family illness or fevers Sister has hay fever that triggers asthma Sister diagnosed with asthma at age 2-3 Review of Systems (ROS): Address all body systems that may help rule in or out a differential diagnosis Check the box next to each positive symptom and provide additional details. Constitutional Skin HEENT ☒Fatigue Feels tired due to lack of sleep ☐Weakness tap . ☐Fever/Chills tap . ☐Weight Gain tap . ☐Weight Loss tap . ☒Trouble Sleeping has been waking up 2 times per night with breathing problems ☐Night Sweats tap . ☐Other: enter text. ☐Itching tap . ☐Rashes tap . ☐Nail Changes Click or tap here to enter text. ☐Skin Color Changes . ☐Other: . ☐Diplopia tap . ☐Eye Pain tap . ☐Eye redness tap . ☐Vision changes tap . ☐Photophobia tap . ☐Eye discharge tap . ☐Earache to . ☐Tinnitus to . ☐Epistaxis tap . ☐Vertigo to . ☐Hearing Changes Click or tap . ☐Hoarseness to . ☐Oral Ulcers to . ☐Sore Throat to . ☐Congestion to . ☐Rhinorrhea to . ☐Other: . Respiratory Neuro Cardiovascular☒Cough Non-productive, small ☐Hemoptysis . ☒Dyspnea Shortness of breath with exertion, but more frequently x2 days ☒Wheezing every four hours for the last 2 days ☐Pain on Inspiration to . ☐Sputum Production . . . ☐Other: enter text. ☐Syncope or Lightheadedness tap . ☐Headache to . ☐Numbness to . ☐Tingling . ☐Sensation Changes . ☐Speech Deficits tap . ☐Other: . ☐Chest pain enter text. ☐SOB . ☐Exercise Intolerance to . ☐Orthopnea enter text. ☐Edema . ☐Murmurs enter text. ☐Palpitations tap . ☐Faintness to . ☐LOC Changes tap . ☐Claudications tap . ☐PND . ☐Other: . MSK GI GU PSYCH ☐Pain enter text. ☐Stiffness . ☐Crepitus . ☐Swelling . ☐Limited ROM . ☐Redness . ☐Misalignment . ☐Other: enter text. ☐Nausea/Vomiting . ☐Dysphasia enter text. ☐Diarrhea enter text. ☐Appetite Change . ☐Heartburn enter text. ☐Blood in Stool . ☐Abdominal Pain . ☐Excessive Flatus . ☐Food Intolerance . ☐Urgency . ☐Dysuria . ☐Burning . ☐Hematuria to . ☐Polyuria . ☐Nocturia . ☐Incontinence tap . ☐Other: . ☐Stress . ☐Anxiety . ☐Depression to . ☐Suicidal/Homicidal Ideation . ☐Memory Deficits tap . ☐Mood Changes tap . ☐Trouble Concentrating Click or tap . ☐Other: .☐Rectal Bleeding . ☐Other: . GYN ☐Rash . ☐Discharge . ☐Itching . ☐Irregular Menses . ☐Dysmenorrhea . ☐Foul Odor . ☐Amenorrhea . ☐LMP: . ☐Contraception . ☐Other:. Body System Positive Findings Negative Findings General . Obesity noted Well nourished, well dressed, well developed. Appropriate affect, alert, and cooperative. Normal speech, judgement and comprehension. Normal mood, no fever. Skin . Acanthosis nigricans noted Skin of chest has no trauma, scares, rashes or lesions noted. HEENT . Respiratory . Wheezing heard in posterior bilateral lower lobes. Accessory muscle use noted. Spirometry results - FVC 3.91L, FEV1 3.15L = 80% percent predicted ratio No asymmetry noted in chest. No deformities noted in chest wall. No rales or rhonchi noted. No retractions noted. O: Objective Information gathered during the physical examination by inspection, palpation, auscultation, and palpation. If a body system, write “”. Document pertinent positive and negative assessment findings.Problem List No dull areas noted during percussion. No absent breath sounds or diminished areas. No bronchophony noted Neuro . Cardiovascular . Musculoskeletal . Gastrointestinal . Genitourinary . Psychiatric . Gynecological . 4 . 9 . 14 . 5 . 10 . 15 . Diagnostics: List tests you will order this visit Test Rationale/Citation Spirometry Performing a full spirometry exam will provide more information on the severity of the patient’s asthma and level of obstruction. A spirometry test can also help rule out differential diagnosis of chronic obstructive pulmonary disease (Domino et al., 2019). Chest x-ray A chest x-ray can rule out other etiologies of cough such as pneumonia (Domino et al., 2019). CBC A CBC can help rule out infectious etiology (David & Esherick, 2019). CMP Kidney function test before steroid administration due to uncontrolled diabetes (David & Esherick, 2019). . . Medications: List medications/treatments including OTC drugs you will order and “continue previous meds” if pertinent. Drug Dosage Length of Treatment Rationale/Citation Prednisolone 1mg/kg (50 mg) once a day in the morning 7 days For mild to moderate asthma exacerbations, 1mg/kg of an oral Diagnosis ICD-10 Code Pertinent Findings Mild persistent asthma, exacerbation J45.51 Expiratory wheezes, shortness of breath, chest tightness, accessory muscle use, worsening cough and chest tightness when lying down (Domino, Baldor, Golding, & Stephens, 2019). COPD J44.9 Cough, prior history of smoking, current exposure to secondhand smoke, shortness of breath (Domino et al., 2019). Gastro esophageal reflux disease K21.9 Nocturnal cough, worsening cough chest tightness when lying down, obesity (Domino et al., 2019). P: Plan Address all 5 parts of the comprehensive treatment plan. If you do not wish to order an intervention for any part of the treatment plan, write “None at this time” but do not leave any heading blank. No intervention is self-evident. Provide a rationale and evidence-based in-text citation for each intervention. A: Assessment Medical Diagnoses. Provide 3 differential diagnoses which may provide an etiology for the CC. The first diagnosis (presumptive diagnosis) is the diagnosis with the highest priority. Provide the ICD-10 code and pertinent findings to support each diagnosis.corticosteroid is standard per clinical guidelines (David & Esherick, 2019). Beclomethasone dipropionate (QVAR) 80 mcg daily 4-6 weeks. To help control her asthma, an inhaled corticosteroid should be added to her SABA to help control her symptoms in the future (Woo & Robinson, 2016). A stepwise approach should be used to taper medications as need, therefore a low dose should be start first (Woo & Robinson, 2016). If symptoms control is not obtained in 4-6 weeks, then a step-up of patient QVAR dose may be needed (Woo & Robinson, 2016). Continue Albuterol 90 mcg every 4 hours prn Indefinitely Continuing Tina’s SABA medication is appropriate due to her symptoms to help prevent severe exacerbations and hospitalization (Woo & Robinson, 2016). . . . . . . . . Referral/Consults: Allergist Pulmonologist Rationale/Citation Referring a patient with allergy induced asthma to an allergist may help predict future exacerbations and help the patient identify other causes of asthma exacerbations (Domino et al., 2019). If the patient’s asthma symptoms do not improve, a referral to pulmonology may be warranted (Woo & Robinson, 2016). . Education:Asthma education Asthma Action plan education Reiterate proper inhaler use Spacer education Strict ED warnings for worsening of symptoms Rationale/Citation Recent research has shown that the initiation of an asthma action plan for adults along with the reiteration of symptoms control and asthma education can decrease symptoms, hospitalization and even death related to asthma exacerbation ( Kouri, Kaplan, Boulet, & Gupta, S. (2019). Along with symptom control, quality of life is also increased due to an increased ability to perform normal activities (Kouri et al., 2019). The patient should also be given very strict ED warnings for worsening of symptoms (Woo & Robinson, 2016). . Follow Up: Indicate when patient should return to clinic and provide detailed instructions indicating if the patient should return sooner than scheduled or seek attention elsewhere. Follow up should be relatively soon, within 2-7 days to assess response to treatment. Pt should also be seen to increase meds if needed if a stepwise process for asthma symptom control is being utilized Patients with an acute exacerbation of asthma have an increased risk of hospitalization if symptom control is not obtained during treatment (David & Esherick, 2019). Therefore, the patient should be educated on the importance of a relatively short follow-up period. . References Include at least one evidence-based peer-reviewed journal article which relates to this case. Use the correct APA 6th edition formatting. David, J. A., & Esherick, J. S. (2019). Current practice guidelines in primary care. New York: Lange Medical Books/McGraw-Hill. Domino, F., Baldor, R., Golding, J., & Stephens, M. (Eds.). (2019). The 5-minute clinical consult 2019 (27th ed., 5-minute consult series) [27th edition.]. Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins Kouri, A., Kaplan, A., Boulet, L.P., & Gupta, S. (2019). New evidence-based tool to guide the creation of asthma action plans for adults. CanadianFamily Physician Medecin De Famille Canadien, 65(2), 103–106. Retrieved from https://search-ebscohostcom.chamberlainuniversity.idm.oclc.org/login.aspx?direct=true&db=mdc&AN=30765356&site=eds-live&scope=site Woo, T. M., & Robinson, M. V. (2016). Pharmacotherapeutics for Advanced Practice Nurse Prescribers(4th ed.). Philadelphia, PA: F.A. Davis Company. . [Show More]
Last updated: 1 year ago
Preview 1 out of 10 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Jun 07, 2020
Number of pages
10
Written in
Additional information
This document has been written for:
Uploaded
Jun 07, 2020
Downloads
0
Views
62