NUR 370 MATERNITY EXAM 2 STUDY GUIDE Latest updated 2021/2022,100% CORRECT
Document Content and Description Below
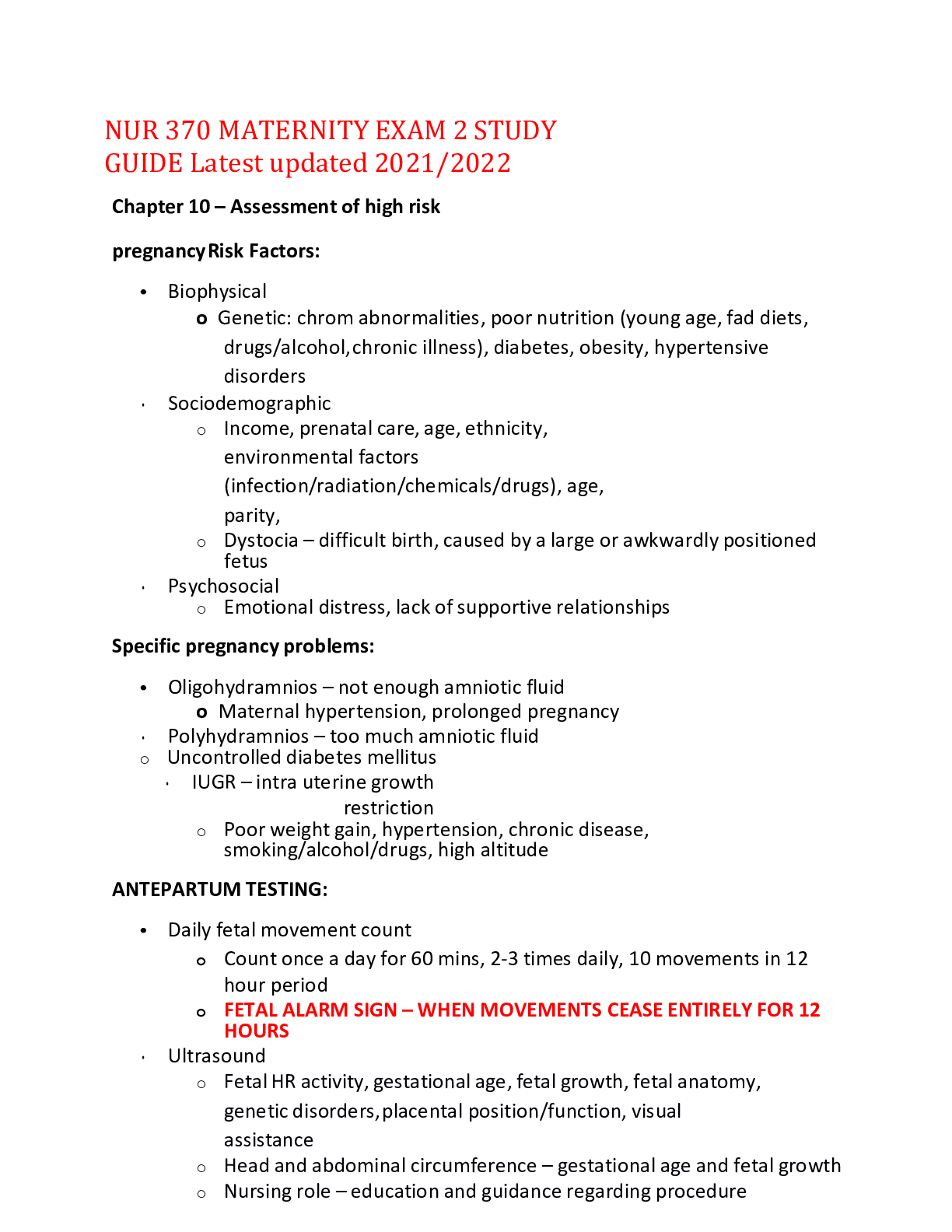
NUR 370 MATERNITY EXAM 2 STUDY GUIDE Latest updated 2021/2022 Chapter 10 – Assessment of high risk pregnancy Risk Factors: • Biophysical o Genetic: chrom abnormalities, poor nutrition (young ag... e, fad diets, drugs/alcohol, chronic illness), diabetes, obesity, hypertensive disorders • Sociodemographic o Income, prenatal care, age, ethnicity, environmental factors (infection/radiation/chemicals/drugs), age, parity, o Dystocia – difficult birth, caused by a large or awkwardly positioned fetus • Psychosocial o Emotional distress, lack of supportive relationships Specific pregnancy problems: • Oligohydramnios – not enough amniotic fluid o Maternal hypertension, prolonged pregnancy • Polyhydramnios – too much amniotic fluid o Uncontrolled diabetes mellitus • IUGR – intra uterine growth restriction o Poor weight gain, hypertension, chronic disease, smoking/alcohol/drugs, high altitude ANTEPARTUM TESTING: • Daily fetal movement count o Count once a day for 60 mins, 2-3 times daily, 10 movements in 12 hour period o FETAL ALARM SIGN – WHEN MOVEMENTS CEASE ENTIRELY FOR 12 HOURS • Ultrasound o Fetal HR activity, gestational age, fetal growth, fetal anatomy, genetic disorders, placental position/function, visual assistance o Head and abdominal circumference – gestational age and fetal growth o Nursing role – education and guidance regarding procedure o Fetal well-being ▪ Doppler blood flow ▪ Amniotic fluid ▪ Biophysical profile • MRI – soft tissues • Biochemical assessment – AMNIOCENTESIS (AFTER 14 WEEKS) o Fetomaternal hemorrhage – fetal blood enters maternal bloodstream – dangerous with Rh o Amniotic fluid embolism – amniotic fluid enters maternal bloodstream – emergency, super dangerous o Used to check for lung maturity • Chronic Villus Sampling – 10-13 weeks gestation o Removal of small tissue specimen from fetal portion of placenta • Percutaneous umbilical blood sampling – replaced in many centers by placental biopsy MATERNAL ASSAYS • Alpha-fetoprotein o Maternal serum screened for neural tube defects (80-85% can be detected early) • Maternal marker screening – 11-14 weeks o Detects chromosomal abnormalities (downs) • Contraction stress test – provides warning of fetal compromise earlier than NST • OLIGOHYDRAMNIOS – associated with fetal renal abnormalities • POLYHYDRAMNIOS – GI, brain/spinal abnormalities CH. 11 – HIGH RISK PRENATAL CARE – PREEXISTING CONDITIONS • Diabetes – strict maternal glucose control • INSULIN NEEDS DURING PREGNANCY ARE DIFFERENT o Lower than normal during weeks 13-20 o Spikes between weeks 26-36 o Drops off after baby is delivered o Non-breastfeeding mother needs more insulin! • Thyroid disorders o Hyperthyroid – Grave's disease – risk for miscarriage and preterm birth o Hypothyroidism – risk for infertility • Maternal phenylketonuria o Baby will have reaction to protein o Prevention – identification of women during childbearing years • Cardiovascular disorders o Heparin – drug that does not cross into the placenta • Anemia o Iron deficiency o Folic acid deficiency o Sickle cell o Thalassemia • Epilepsy – all medications carry risk of congenital abnormalities CHAPTER 12: HIGH RISK: GESTATIONAL CONDITIONS Disorders that did not exist before pregnancy • Most common is hypertension o Preeclampsia – HTN develops after 20 weeks with proteinuria. Can be mild or severe ▪ Disappears after birth ▪ Reduced kidney perfusion ▪ HELLP syndrome – severe preeclampsia – hepatic dysfunction • Hemolysis • Elevated Liver enzymes • Low Platelets ▪ Associated with increased risk for: • Pulmonary edema, renal failure, liver failure, disseminated intravascular coagulation (abnormal clots in blood vessels), placental abruption, acute respiratory distress, sepsis, stroke, fetal and maternal death ▪ IDENTIFYING AND PREVENTING: • Physical exam – dependent/pitting edema, deep tendon reflexes (decrease w magnesium sulfate use), clonus • Lab tests – proteinuria • Magnesium sulfate toxicity – GIVE CALCIUM GLUCONATE OR CALCIUM CHLORIDE o Eclampsia – seizure or coma o Gestational HTN – onset without proteinuria after 20th week o Chronic HTN – present before pregnancy or before 20th week • HEMMORHAGIC DISORDERS – MEDICAL EMERGENCY o Maternal blood loss reduces oxygen-carrying capacity • Recurrent premature dilation of cervix o Prophylactic Cerclage (stitch) is placed in the cervix around 11-15 weeks o Abdominal cerclage 11-13 weeks • Ectopic pregnancy o Patient presents w severe pain, delayed menses and abnormal vaginal bleeding o Treatment: ▪ Medical: methotrexate ▪ Surgical: salpingectomy • Gestational Trophoblastic Disease (molar pregnancy) o Empty o Vaginal bleeding, significantly larger fundus o Most pass spontaneously, or with D&C o *induction of labor not recommended • Late pregnancy bleeding o Placenta previa – placenta implanted in lower uterine segment – covering part of cervix (complete, marginal, low lying) o PAINLESS BLEEDING o Abnormal placental attachment, excessive bleeding, anemia o Diagnose with ultrasound – observation, bed rest, c section o Abruptio placentae – premature separation of placenta (mild, moderate, severe) o HARD, BOARD-LIKE ABDOMEN, VERY PAINFUL BLEEDING • CLOTTING DISORDERS o Disseminated Intravascular Coagulation (DIC) o Major medical emergency o Blood clots excessively • UTI o Triggered by severe preeclampsia, HELLP, gram negative sepsis o Can cause preterm labor!! o Asymptomatic bacteruria – bacteria with no symptoms • Trauma – fetal survival depends on maternal survival CHAPTER 13: LABOR AND BIRTH PROCESS • 5 P’s affecting labor: passenger, passageway, powers, position of mother, psychologic response • Passenger (fetus) o Fetal presentation – part of body coming out first o Fetal lie – spine to spine o Fetal altitude – relation of fetal body parts to one another o Fetal position – presenting part o Back fontanel (soft spot) closes at 6-8 weeks o Front fontanel closes by 18 months • Passageway (pelvis) o Gynecoid – normal female pelvis o Android – male pelvis o Anthropoid o Platypellpoid – flate pelvis • Powers o Effacement – need to be at 100% (lining thinned) o Dilation – need to be at 10 o Ferguson reflex – sensation to bear down • Position o Encourage mother to change position often STAGES OF LABOR: • STAGE 1: o Onset of regular uterine contractions to full dilation • STAGE 2: o Full dilation to birth of baby ▪ LATENT PHASE – fetus descends passively through birth canal and rotates to an anterior position ▪ ACTIVE PUSHING – strong urge to bear down as presenting part of fetus descends and passes on stretch receptors of pelvic floor • STAGE 3: o Birth of baby to birth of placenta • STAGE 4: o 2 hours after the placenta is delivered Signs preceding labor: dropping about 2 weeks prior, mucus plug • Mechanism of labor: occur in vertex presentation o Engagement (asynclitism) - when head passes the pelvic inlet o Descent – the progress of the presenting part – depends on 4 forces: ▪ Pressure from amniotic fluid ▪ Pressure from contractions of fundus on fetus ▪ Force of contraction ▪ Extension and straightening of fetal body o Flexion – when descending head meets resistance from the cervix, pelvic wall or pelvic floor o Internal rotation o Extension o External rotation – after head is born/as shoulders descend and engage o Expulsion (birth) • Fetal adaptations to labor: o Fetal HR ranges from 110-160 bpm o Fetal circulation – affected by position, contraction o Fetal respirations – changes stimulate the fetus to be ready for respirations • Maternal adaptations to labor: o Cardio changes – output peaks at 10-30 mins post-delivery, BP increases during contraction, blood circulation increases during contraction o Increased respiratory rate o Renal – voiding may be difficult, +1 protein may be normal o Stretching of the vaginal introitus o Diaphoresis, fatigue o Euphoric, amnesia o Decreased motility o Decrease in progesterone and blood glucose levels o Increase in estrogen, prostaglandins, oxytocin and metabolism CHAPTER 14 – PAIN MANAGEMENT • First stage of labor – visceral pain (from cervical changes) • Second stage of labor – somatic pain (from stretching or tearing) • Third stage of labor – visceral pain • Nonpharm pain management best for all patients • Anesthesia – watch for decreased resp and BP – have narcan on hand!! • Pharmacological pain management o Local numbing – Lidocaine o Sedatives – relieve anxiety and induce sleep o Analgesia and anesthesia ▪ Anesthesia – abolish pain perception by interrupting nerve impulses to the brain – may be partial or complete ▪ Systemic analgesia – alleviation of sensation of pain or raising threshold of pain perception w/o loss of consiousness • Opiod agonist analgesics – demerol, fetanyl • Opiod agonist-antagonist analgesics – stadol, nubain • Opiod antagonist – narcan --> reverses opiod respiratory distress o Epidural - vaginal delivery, can get if up to 5-6 cm dilated ▪ Immediate relief ▪ Feel pressure, no pain o Spinal block - c-section delivery, subarachnoid space ▪ Immediate relief ▪ Provides numbness higher up (for c-sections) ▪ Can get severe spinal headache ▪ No catheter o Pudendal - vaginal delivery, woman too far along for epidural ▪ 10-20 mins for effects ▪ Blocks lower region pain o General Anesthesia ▪ For emergency c section – rapid birth ▪ Patient is supposed to be NPO prior ***MATERNAL HYPOTENSION IS AN EMERGENCY --> DECREASED PLACENTAL PERFUSION • CONTRAINDICATIONS TO EPIDURAL: o Hemorrhage, maternal hypotension, coagulopathy, infection at injection site, allergy to anesthetic drug, maternal refusal/inability to cooperate, maternal cardiac conditions CHAPTER 15 – FETAL ASSESSMENT DURING LABOR • Fetal monitor – fetal HR is on top, contraction is on bottom • Each box = 10 seconds • One dark line to another = 10 minutes • Measure: frequency of contractions (how many min apart), duration of contractions (how long is 1), strength of contractions, resting tone, relaxation time (between contractions) • Normal FHR pattern: between 110-160, no periodic changes, moderate baseline variability • Internal measurement of FHR – intrauterine pressure transducer (measures uterine contractions), cardiotachometer measures FHR on baby’s head • Absent variability – not good, indicates fetal hypoxemia • Moderate variability is normal (amplitude changes between 6-25 bpm) • High variability – sinusoidal FHR pattern • Tachycardia – FHR >160 for more than 10 mins --> maternal fever • Bradycardia – FHR <110 for more than 10 mins --> cord compression, post term, epidural • REMEMBER VEAL CHOP: o V – VARIABLE DECCELERATION --> C – CORD ISSUE o E – EARLY (DECELERATION SAME TIME AS CONTRACTION) --> H – HEAD COMPRESSED o A – ACCELERATION (HR INCREASE DURING CONTRACTION --> O – OK o L – LATE DECCELERATION --> P – PLACENTAL ABRUPTION *LATE DECCELERATION IS AN EMERGENCY – GET BABY OUT!!! Variable: Early: Late: CHAPTER 16 – NURSING CARE OF THE FAMILY DURING LABOR AND BIRTH • True vs false labor o True labor: ▪ Cervix by vaginal exam shows softening, effacement, and dilation ▪ Presenting part of fetus becomes engaged in pelvis o False labor: ▪ Irregular or temp contractions Stages and phases of labor: • 1st– onset of regular uterine contractions -> full dilation of the cervix- (varies the most in length) o Latent phase: up to 3 cm of dilation (~6 -8 hours) o Active phase: 4 to 7 cm of dilation (~3-6 hours) o Transition phase: 8 to 10 cm of dilation (~20- 40 mins) • 2nd stage cervix is fully dilated -> the birth of the fetus o Latent- the fetus continues to descend passively through the birth canal and rotate to an anterior position as a result of ongoing uterine contractions o Decent Phase- Active pushing- a strong urge to bear down as the presenting part of the fetus descends and presses on the stretch receptors of the pelvic floor • 3rd stage- fetus -> placenta delivered • 4th stage about 2 hours AFTER the placenta is delivered Lepold maneuvers – determine number of fetuses, position, lie, True labor is considered an emergency medical condition Ritgen maneuver – applying upward pressure from the coccyx region CH 17 LABOR AND BIRTH COMPLICATIONS • Low birth weight – only weight, <5.5 lbs • Antenatal glucocorticoids (accelerates fetal lung maturity by stimulating fetal surfactant production. Optimal benefit occurs 24 hours after the 1st injection) • Premature rupture of membranes (PROM) - Rupture of amniotic sac and leakage of amniotic fluid beginning at least 1 hour before onset of labor at any gestational age • ***Chorioamniotis – bacterial infection of amniotic cavity is the most common maternal complication of PPROM • Oxytocin – used to stimulate uterine contractions and induce labor [Show More]
Last updated: 1 year ago
Preview 1 out of 18 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Apr 17, 2022
Number of pages
18
Written in
Additional information
This document has been written for:
Uploaded
Apr 17, 2022
Downloads
0
Views
39