*NURSING > EXAM > NR 511 / NR511: Differential Diagnosis & Primary Care Practicum Week 6 Quiz ( Latest 2020 / 2021 ) C (All)
NR 511 / NR511: Differential Diagnosis & Primary Care Practicum Week 6 Quiz ( Latest 2020 / 2021 ) Chamberlain College of Nursing
Document Content and Description Below
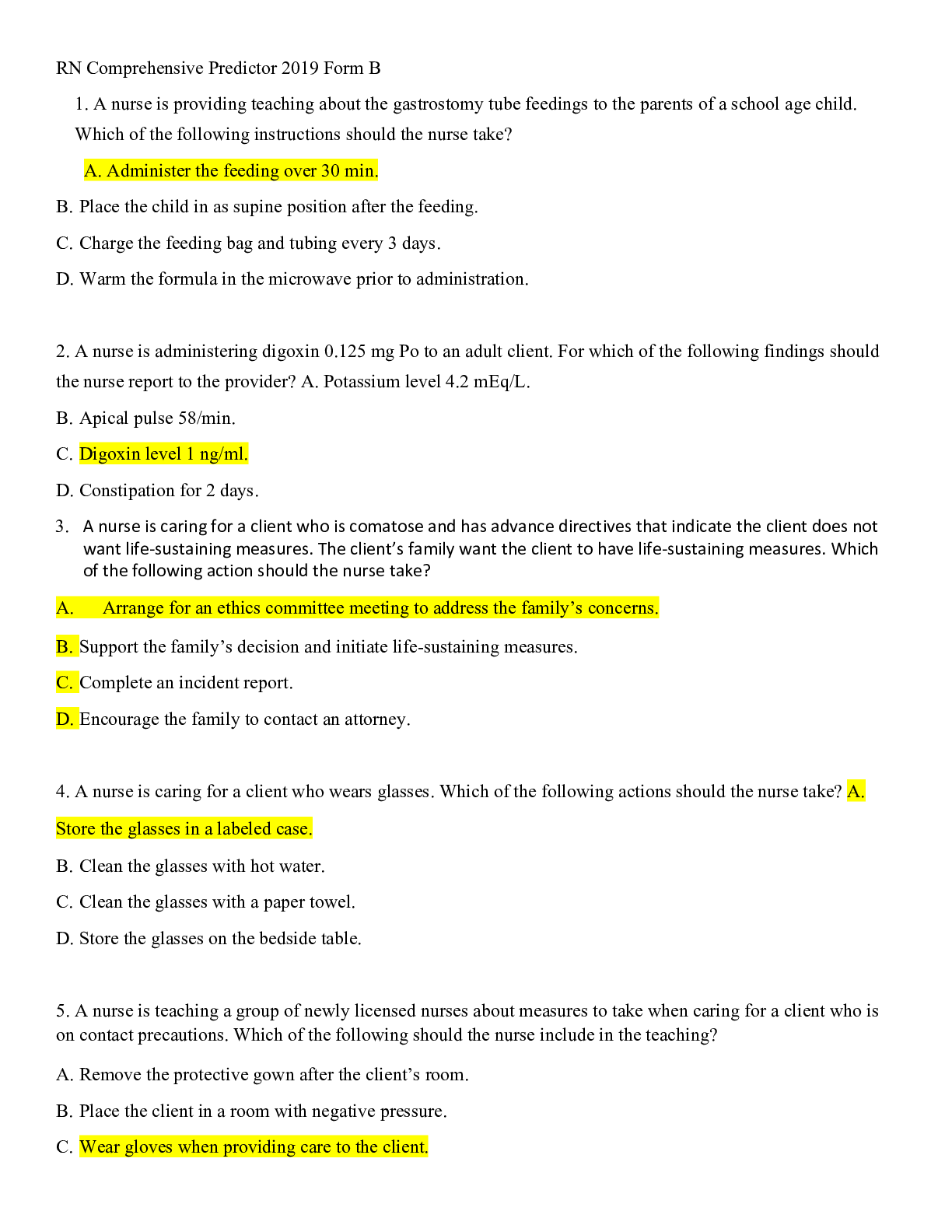
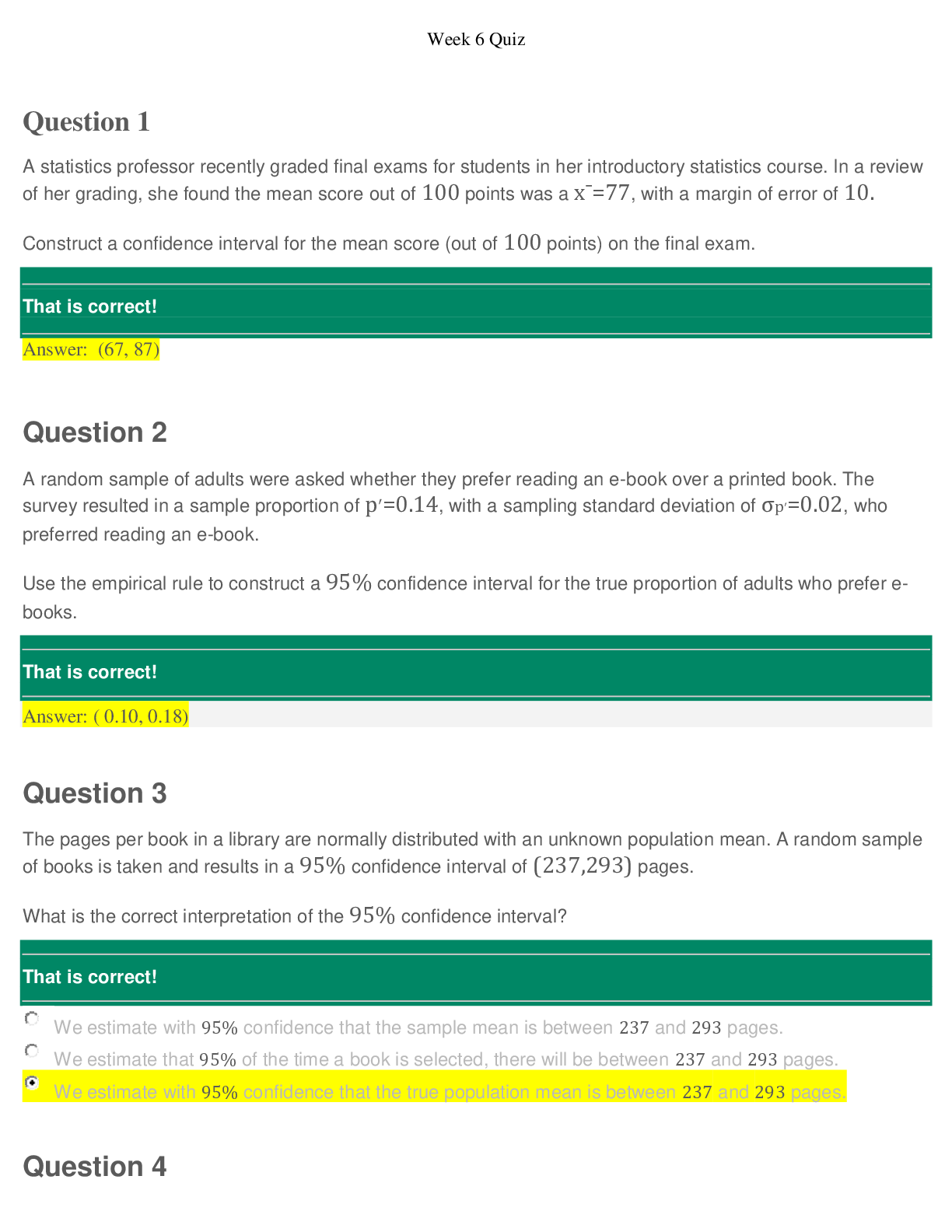
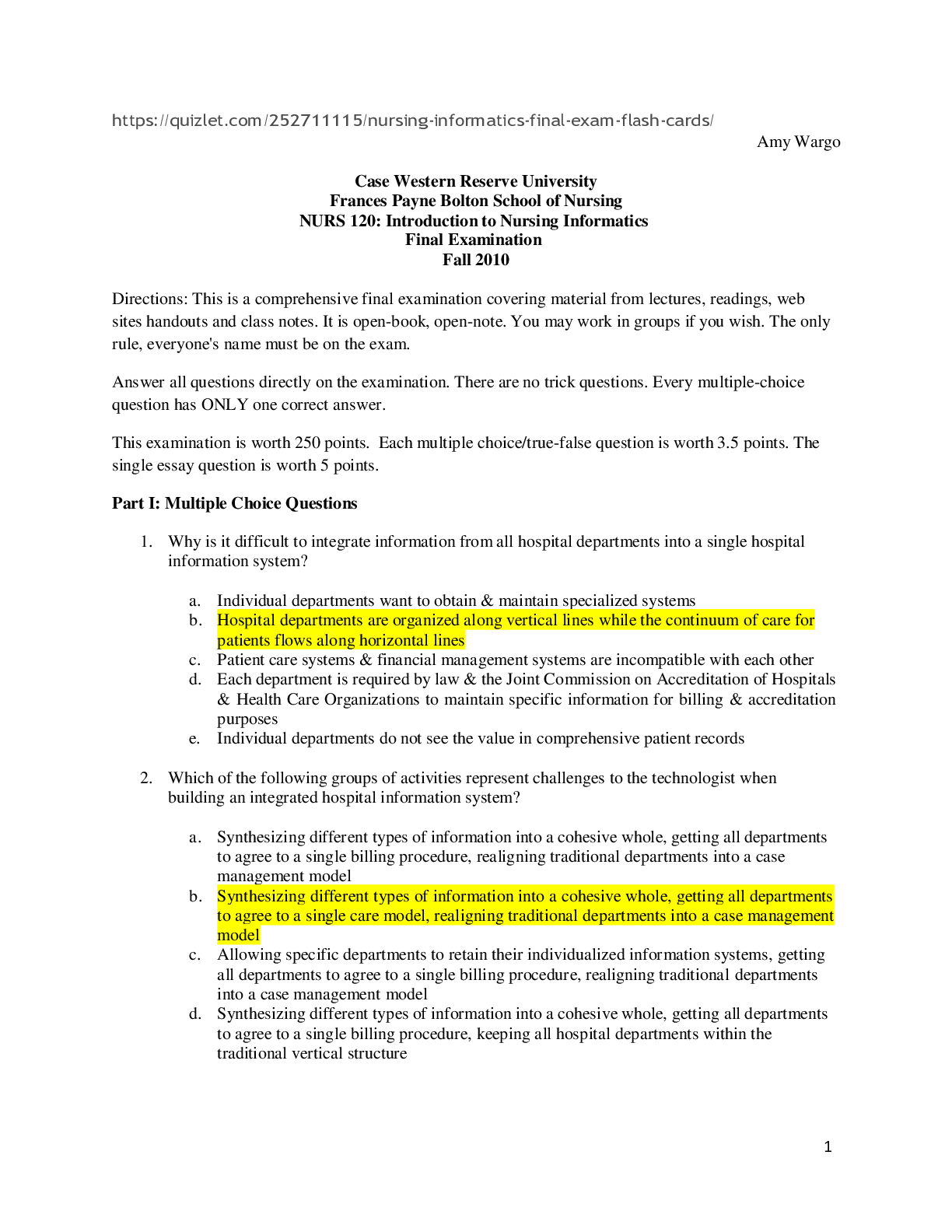
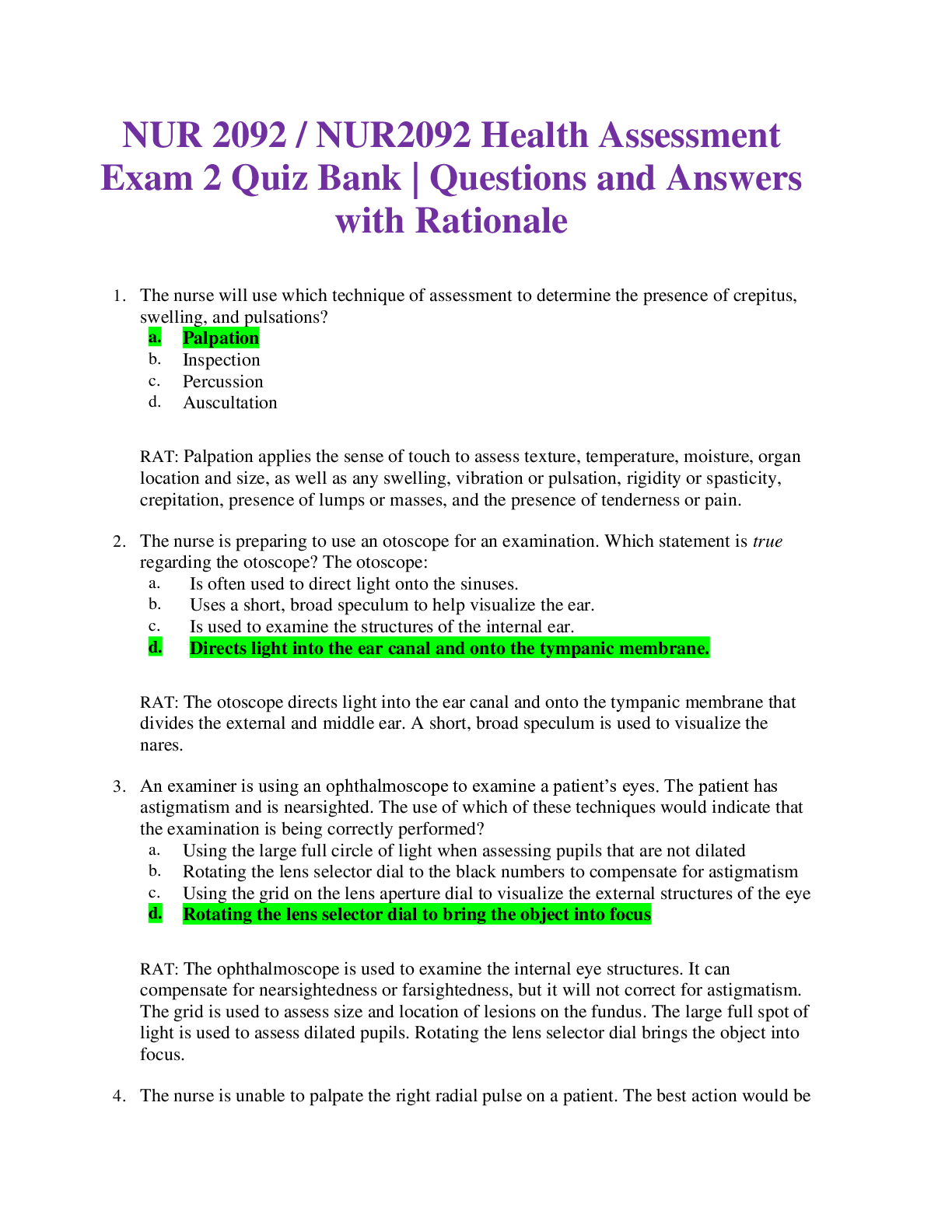
NR-511 Differential Diagnosis & Primary Care Practicum June 2020 Quiz 6 Question 1 1 / 1 pts A client with hyperthyroidism presents with a complaint of a “gritty” feeling in her eyes.... Over the past week, her visual acuity has diminished, and her ability to see colors has changed. She also has a feeling of pressure behind her eyes. The next step for the nurse practitioner is to: Order a total thyroxine (T4). Correct! Refer the client for immediate evaluation by an ophthalmologist. Order a thyroid ultrasound. Prescribe a beta-adrenergic blocker. The practitioner should refer the client for an immediate evaluation by an ophthalmologist. Clinically recognized Graves ophthalmopathy occurs in about 50% of cases of Graves’ disease. A client with Graves orbitopathy with these complaints is at risk of blindness if there is compression of the optic nerve. Additional symptoms include photophobia and diplopia. Autoantibodies present in Graves’ disease can cause increased muscle thickness in the eye, leading to edema and compression of the optic nerve. Fundal exam may reveal disk swelling. This is an emergency situation that may require hospitalization and treatment with prednisone to diminish the inflammation. Artificial tears are also helpful. In 75% of clients, the onset of Graves orbitopathy occurs within a year before or after the diagnosis of thyrotoxicosis but can sometimes precede or follow thyrotoxicosis by several years. Question 2 1 / 1 pts A low thyroid-stimulating hormone (TSH) can lead to: Brittle hair. Correct! Osteoporosis. Weight gain. Bradycardia. Hyperthyroidism presents with a suppressed TSH and elevated free thyroxine (FT4). Manifestations include weight loss, tachycardia, diarrhea, anxiety, and warm, silky skin. The increased metabolic state of hyperthyroidism can cause cardiac dysrhythmias and osteoporosis. The clinical manifestations can also occur when there is excessive thyroid replacement. Question 3 1 / 1 pts Which of the following statements about hypothyroidism is not true? Correct! The rate of hypothyroidism decreases with age. Lithium use is a risk factor for hypothyroidism. The most common cause of autoimmune hypothyroidism is Hashimoto thyroiditis. The most common worldwide cause of hypothyroidism is iodine deficiency. This is not true; hypothyroidism becomes more common as we age. Question 4 1 / 1 pts Alice, age 48, has a benign thyroid nodule. The most common treatment involves: Radioactive iodine therapy. Correct! Watchful waiting with annual follow-up. Administration of levothyroxine therapy. Surgery. Thyroid specialists agree that most benign thyroid nodules require no management beyond watchful waiting and annual follow-up to evaluate their size. Question 5 1 / 1 pts An elderly client presents with atrial fibrillation. Which of the following lab tests is important in forming the diagnosis? Complete blood count (CBC). Correct! Thyroid-stimulating hormone (TSH). C-reactive protein (CRP). Comprehensive metabolic panel (CMP). Atrial fibrillation is a common presentation in elderly clients with hyperthyroidism. If the TSH is suppressed, a free thyroxine (FT4) and triiodothyronine (T3) should be drawn. Question 6 1 / 1 pts A 6-year-old girl was bitten by a friend’s dog. Her mother asks the clinician if the child needs anti-rabies treatment. Which of the following should the clinician advise? “Anti-rabies treatment must be started immediately.” Correct! “If the dog is a domestic pet that has been vaccinated, wound cleansing and irrigation is the only treatment needed.” “Wait until you have observed the animal for 2 weeks to determine if it is rabid.” “Rabies can be contracted only through the bites of wild animals.” If the dog is a domestic pet that has been vaccinated, the wound should be washed thoroughly with soap and water and then treated like any other wound. Question 7 1 / 1 pts The most common cause of hyperthyroidism is: Subacute thyroiditis. A pituitary tumor. A toxic unimodular goiter. Correct! Graves’ disease. The most common cause of hyperthyroidism is an autoimmune condition known as Graves’ disease, which accounts for 90% of hyperthyroid conditions in young adults. Question 8 1 / 1 pts A 24-year-old female is preparing for radioactive iodine therapy to treat Graves’ disease. Which test must she undergo first? Basal metabolism rate. Correct! Beta-human chorionic gonadotropin. Serum calcium. Lithium level. Radioactive iodine therapy is the most commonly used treatment in the United States for Graves disease (hyperthyroidism); however, it is contraindicated during pregnancy. Therefore, for women, a pregnancy test (beta-human chorionic gonadotropin) needs to be performed before initiating therapy. Women of childbearing age should also be told to delay conception for a few months after radioactive iodine therapy. It is also contraindicated in women who are breastfeeding. Older adults or clients at risk of developing cardiac complications may be pretreated with antithyroid drugs (ATDs) before therapy to deplete the thyroid gland of stored hormone, thereby minimizing the risk of exacerbation of hyperthyroidism because of radioactive iodine (131I)–induced thyroiditis. Question 9 1 / 1 pts Which of the following body mass index (BMI) values defines class 1 obesity? 35 25 Correct! 30 40 Class 1 obesity is defined as a BMI of 30 to less than 35. Question 10 1 / 1 pts What is the medication of choice for an initial acute attack of gout? A corticosteroid. Colchicine. Allopurinol (Zyloprim). Correct! A nonsteroidal anti-inflammatory drug (NSAID). The medication of choice for an initial acute attack of gout is an NSAID. Indomethacin (Indocin) is the most commonly prescribed NSAID for this use. An initial dose of 50 to 75 mg is given, followed by 25 to 50 mg every 8 hours for 5 to 10 days. An alternative to indomethacin is naproxen (Naprosyn). The first dose of naproxen is 750 mg, followed by 250 mg every 8 hours for 5 to 10 days. Question 11 1 / 1 pts Which of the following objective findings in a 49-year-old female is a sign of hyperthyroidism? Decreased systolic blood pressure (BP). Slow pulse. Dry, coarse, cool skin. Correct! Exophthalmos. Hyperthyroidism is characterized by exophthalmos, which is a term referring to the forward protrusion of the eyeball. When it is bilateral, it may signify infiltrative ophthalmopathy of Graves’ disease. There may be associated edema and conjunctival injection as well. Question 12 1 / 1 pts A 72-year-old obese male has gout. When teaching him about diet, which of the following should the clinician advise? Correct! “Fluid intake should exceed three thousand milliliters daily to prevent formation of uric acid kidney stones.” “You must go on a restricted, very low-calorie diet to effect immediate change.” "A diet high in red meat will prevent formation of kidney stones." “Keeping your weight stable, even if you are a little overweight, is better than fluctuating.” Fluid intake should exceed 3000 mL daily to prevent formation of uric acid kidney stones. Clients should avoid dehydration because it may precipitate an acute attack. Question 13 0 / 1 pts A 46-year-old male presents with a tender, red and swollen knee. The clinician orders a complete blood count (CBC) with differential, uric acid level and erythrocyte sedimentation rate (ESR). Which of the following results would make the clinician suspect a septic joint rather than gout? Normal Erythrocyte Sedimentation Rate (ESR) and a decreased uric acid level. Correct Answer Elevated white blood cell (WBC) count and an elevated Erythrocyte Sedimentation Rate (ESR). High uric acid level and a decreased Erythrocyte Sedimentation Rate (ESR). You Answered Decreased white blood cell (WBC) count and an elevated uric acid level. To diagnose gout, there should be hyperuricemia and a negative joint culture. Question 14 1 / 1 pts A client presents with clinical manifestations of hyperthyroidism. The differential diagnosis includes Graves disease and subacute thyroiditis. Which of the following findings is consistent with subacute thyroiditis? A 24-hour radioactive iodine uptake (RAIU) demonstrating increased uptake. A fine-needle aspiration is required for diagnosis of subacute thyroiditis. A 24-hour radioactive iodine uptake (RAIU) demonstrating a “cold” nodule. Correct! A 24-hour radioactive iodine uptake (RAIU) demonstrating decreased uptake. A 24-hour radioactive iodine uptake helps establish the functional status of the thyroid gland. In subacute thyroiditis, the radioactive iodine uptake is low. Subacute thyroiditis produces symptoms of thyrotoxicosis via the release of preformed thyroid hormones in response to an inflammatory response after an acute infection. Subacute thyroiditis is usually self-limiting and is treated with nonsteroidal anti-inflammatory drugs (NSAIDs), beta-adrenergic antagonists, and, in severe cases, corticosteroids. Thyroid function should be monitored because a state of hypothyroidism can occur. Question 15 1 / 1 pts A 23-year-old female complains of palpitations that started a few weeks ago; they occur 2 to 4 times a day and last 5 to 10 minutes. She feels nervous and is having trouble sleeping. Her stools have been frequent (1-3 per day) and loose. She is taking levothyroxine 150 µg daily. Her labs indicate free thyroxine (FT4) 2.28 and thyroid-stimulating hormone (TSH) 0.022. She has a history of Graves’ disease and had radioactive iodine (RAI) treatment a few months ago. She has been on thyroid replacement for 2 months. Based on these findings, what should the clinician do next? Keep the dosage the same. Correct! Decrease the levothyroxine dosage. Increase the levothyroxine dosage. Start propranolol every 8 hours. It appears that she may be overcorrected. The usual dosage of thyroid replacement is 1.6 µg/kg/d. She could skip a dose and then resume at a lower dosage of 125 to 137 µg per day. In an older individual, the lower dose would be preferred because overcorrection can lead to atrial fibrillation. She should take the levothyroxine on an empty stomach with a full glass of water and wait 30 minutes before eating for maximum absorption. Quiz Score: 14 out of 15 [Show More]
Last updated: 11 months ago
Preview 1 out of 10 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Nov 14, 2020
Number of pages
10
Written in
Additional information
This document has been written for:
Uploaded
Nov 14, 2020
Downloads
0
Views
47

.png)
 – CHAMBERLAIN COLLEGE OF NURSING.png)
 – Chamberlain College of Nursing.png)