*NURSING > EXAM > Chamberlain College of Nursing - NR 510-Dermatology QBank Questions And Answers (All)
Chamberlain College of Nursing - NR 510-Dermatology QBank Questions And Answers
Document Content and Description Below
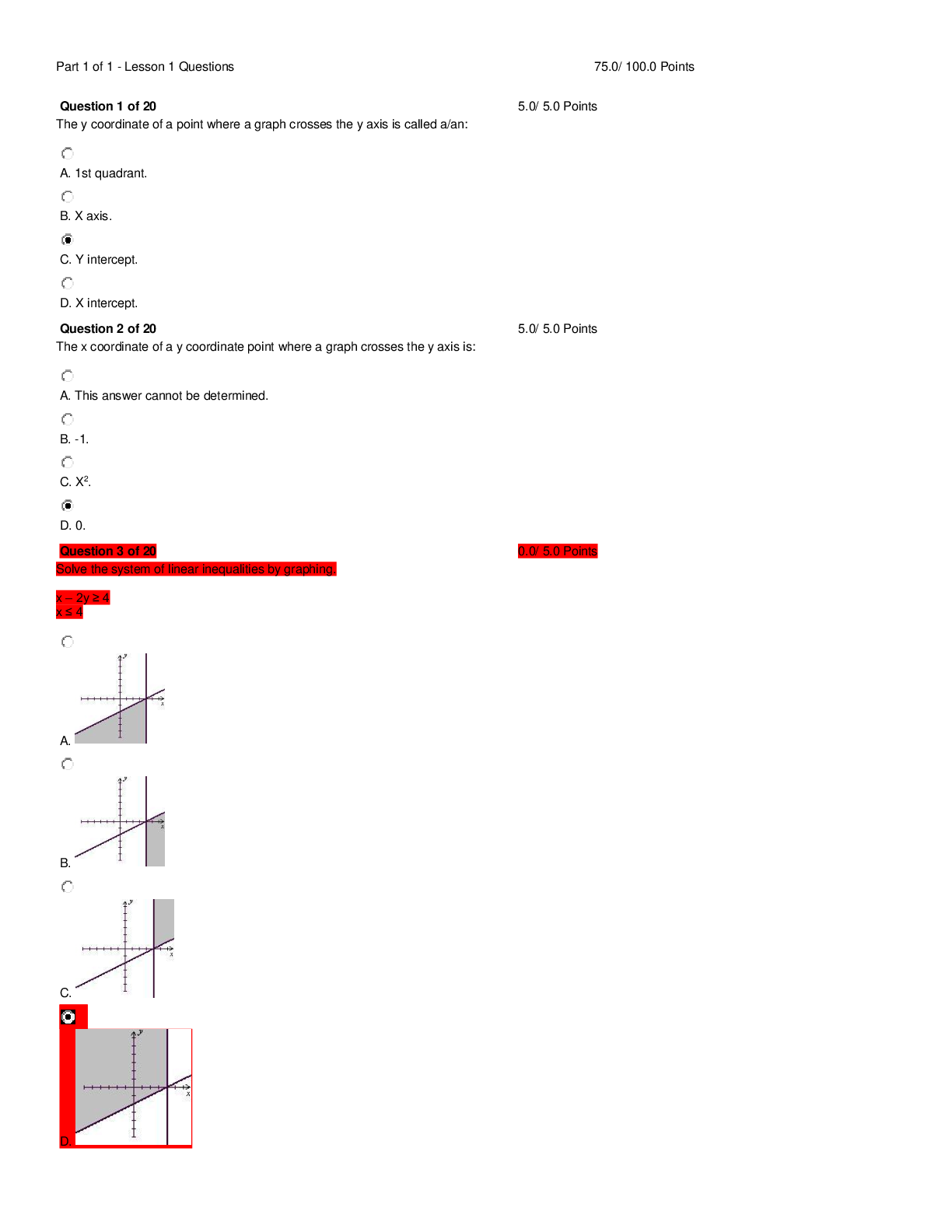
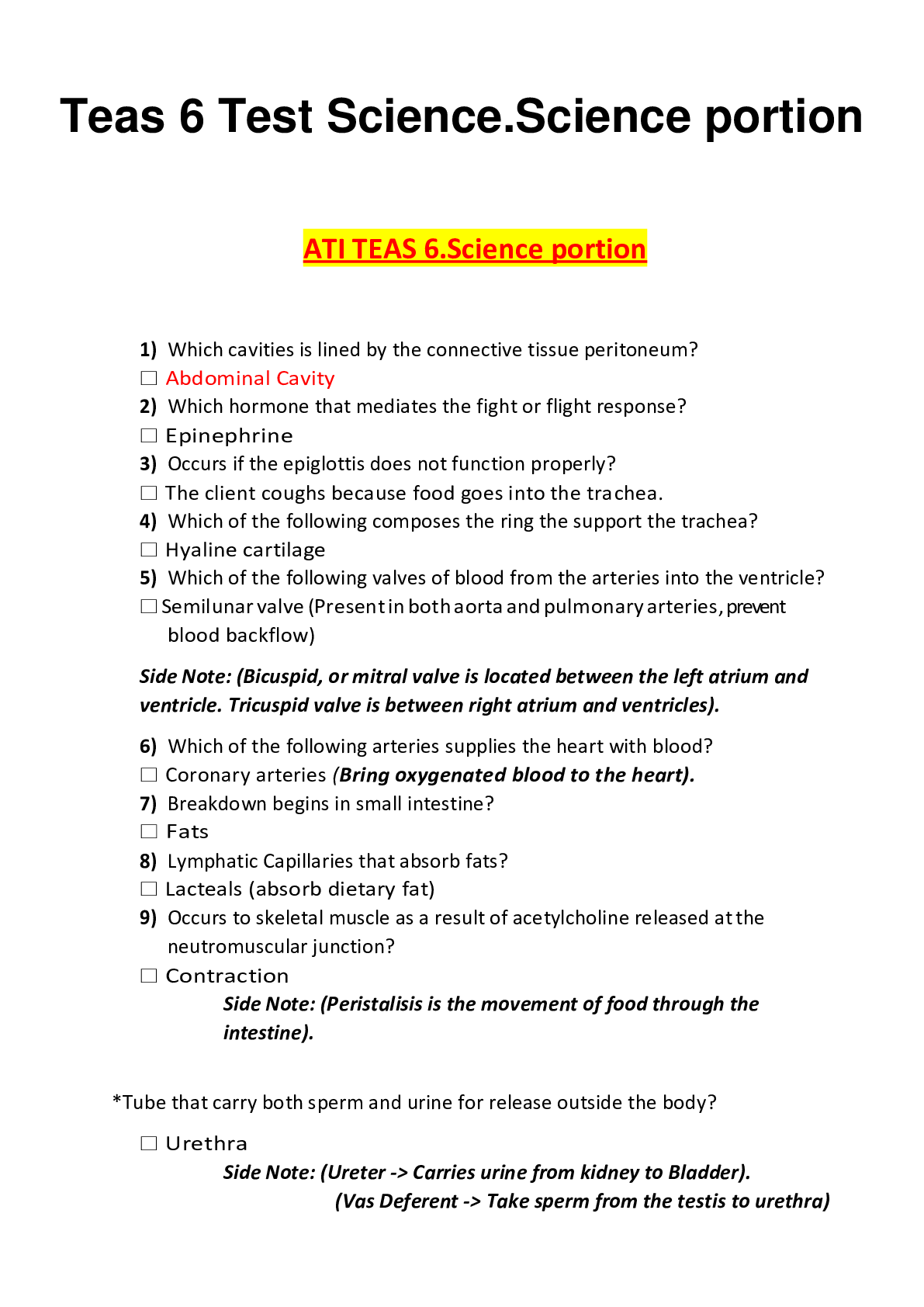
A microscopic examination of the sample taken from a skin lesion indicates hyphae. What type of infection might this indicate? (Fungal) Under microscopic exam, hyphae are long, thin and branching and... indicate dermatophytic infections. Hyphae are typical in tinea pedis, tinea cruris, and tinea corporis. A child with a sandpaper-textured rash probably has: (Strep infection) Streptococcal infections can present as a sandpaper-textured rash that initially is felt on the trunk. Rubeola, measles, produces a blanching erythematous “brick-red” maculopapular rash that begins on the back of the neck and spreads around the trunk and then extremities. Varicella infection produces the classic crops of eruptions on the trunk that spread to the face. The rash is maculopapular initially and then crusts. Roseola produces a generalized maculopapular rash preceded by 3 days of high fever. A 40-year-old female patient presents to the clinic with multiple, painful reddened nodules on the anterior surface of both legs. She is concerned. These are probably associated with her history of: (ulcerative colitis) These nodules describe erythema nodosum. These are most common in women aged 15-40 years old. They are typically found in pretibial locations and can be associated with infectious agents, drugs, or systemic inflammatory disease like ulcerative colitis. They probably occur as a result of a delayed hypersensitivity reaction to antigens. It is not unusual to find polyarthralgia, fever, and/or malaise that precede or accompany the skin nodules. A patient is diagnosed with tinea pedis. A microscopic examination of the sample taken from the infected area would likely demonstrate: (hyphae) Under microscopic exam, hyphae are long, thin and branching, and indicate dermatophytic infections. Hyphae are typical in tinea pedis, tinea cruris, and tinea corporis. Yeasts are usually seen in candidal infections. Cocci and rods are specific to bacterial infections. When can a child with chickenpox return to daycare? (After all lesions have crusted) Chickenpox is highly contagious and can be spread via respiratory secretions from an infected person or by direct contact from the vesicle fluid from lesions on the skin or mucus membranes. The usual incubation period is about 2 weeks but can be as long as 21 days or as short as 10 days. The greatest period of infectivity is 48 hours prior to the onset of the rash and until all the skin lesions have crusted over. A patient with a primary case of scabies was probably infected: (3-4 weeks ago) The incubation period for scabies is about 3-4 weeks after primary infection. Patients with subsequent infections with scabies will develop symptoms in 1-3 days. The classic symptom is itching that is worse at night, coupled with a rash that appears in new areas over time. The nurse practitioner examines a patient who has had poison ivy for 3 days. She asks if she can spread it to her family members. The nurse practitioner replies: (“No, transmission does not occur from the blister’s contents”) The skin reaction seen after exposure to poison ivy (or any other skin irritant), takes place because of contact with the offending substance. In the case of poison ivy, the harmful exposure occurs from contact with oil from the plant. The eruptions seen are NOT able to transmit the reaction to other people unless oil from the plant remains on the skin and someone touches the oil. The fluid found in the blisters is NOT able to transmit poison ivy to anyone; only the oil from the plant can do that. After oil has touched the skin, some time must pass for the reaction to occur. Therefore, reaction times vary depending on skin thickness and quantity of oil contacting the skin. Which chronic skin disorder primarily affects hairy areas of the body? (Seborrheic dermatitis) Seborrheic dermatitis causes flaking of the skin, usually the scalp. In adolescents and adults, when it affects the scalp, it is termed dandruff. When this occurs in young children or infants, it is termed “cradle cap”. The exact cause is unknown; however it has a propensity for hairy areas of the body such as the scalp, face, chest, and legs. It appears greasy and flaky. This may be seen in patients with Parkinson’s disease. A patient with diabetes has right anterior shin edema, erythema, warmth, and tenderness to touch. This developed over the past 3 days. There is no visible pus. What is the most likely diagnosis to consider? (Cellulitis) This description is one of cellulitis. Cellulitis involves an infection of the subcutaneous layers of the skin. It must be treated with an oral antibiotic. In a patient with diabetes, it is particularly important to identify, and aggressively treat cellulitis early, because elevated blood sugar levels will make eradication more difficult. Buerger’s disease involves inflammation of the medium-sized arteries and does not present on the anterior shin only. DVT seldom presents on the anterior shin, so this is not likely. Venous disease does not present acutely, as in this situation. The agent commonly used to treat patients with scabies is permethrin. How often should it be applied to eradicate scabies? (Once) A single whole-body application of permethrin is usually successful in eradicating infection with scabies. It is applied over the entire body from the neck down. The lotion is left on and then showered off 8-12 hours later. All contacts must be treated at the same time and all potential fomites (bed linen, mattresses, cloth furniture, etc.) must be treated as well. Permethrin can be sprayed on cloth fomites, or the fomite can be bagged for several days, washed and dried in a washing machine and dryer. Ironing clothes after washing them is acceptable. Impetigo is characterized by: (honey-colored crusts) Impetigo is a superficial bacterial infection of the skin characterized by honey-colored crusts. Another form of impetigo is characterized by the presence of bullae. These infections are treated with topical antibiotics, good hygiene, and frequent hand washing. It is usually caused by Staphylococcus or Group A Streptococcus. A 60-year-old patient is noted to have rounding of the distal phalanx of the fingers. What might have caused this? (Hepatic cirrhosis) Rounding of the distal phalanx describes clubbing. Clubbing of fingers is most often associated with chronic hypoxia as seen in cigarette smokers and patients with COPD or lung cancer. Other causes are cirrhosis, cystic fibrosis, pulmonary fibrosis and cyanotic heart disease. A patient has suspected scarlet fever. He likely has a sandpaper rash and: (a positive rapid Strep test) A patient with scarlet fever (scarlatina) has a common childhood disease that is characterized by sore throat, fever, and a scarlet “sandpaper” rash. The causative organism is Group A beta hemolytic Streptococcus pyogenes. The patient’s rapid Strep test will likely be positive. Diarrhea with abdominal cramps is not specific to scarlet fever. Petechiae represent an extravasation of blood under the skin and are not present with scarlet fever unless some other disease process is present. Petechiae should be considered to be a serious finding. A patient with a positive history of a tick bite about 2 weeks ago and erythema migrans has a positive ELISA for Borrelia burgdorferi. The Western blot is positive. How should he be managed? (He should receive doxycycline for Lyme disease) The first serologic test for Lyme disease is the ELISA. If this is positive, it should be confirmed. In this case, it was confirmed by a Western blot and it is positive. This patient can be diagnosed with Lyme disease. The appropriate treatment for erythema migrans is doxycycline, amoxicillin, or cefuroxime for 21 days. All three medications were found to be of equal efficacy. A patient will be taking oral terbinafine for fingernail fungus. The NP knows that: (terbinafine is an inhibitor of the CYP 2D6 enzymes) Many oral antifungal agents inhibit the 3A4 or 2D6 enzymes in the cytochrome P450 system. This is why they must be used with extreme caution (or not used) in patients who consume medications that need 3A4 or 2D6 enzymes for metabolism. And, liver enzymes must be monitored in patients who take oral antifungal medications and discontinued if elevations are >2.5 times the upper limits of normal. No oral agent has a 95% cure rate for fingernail fungus (tinea unguium). This can be a difficult infection to clear even if oral antifungal agents are utilized. A topical antifungal agent typically will not clear the infection if the nail matrix is involved. There is anecdotal evidence that menthol ointments or bleach may cause resolution when used topically. Generally, resolution of fingernail fungus occurs more rapidly than toenail fungus because toenails grow at slower rates than fingernails. A skin lesion that is a solid mass is described as a: (papule) A papule is an elevated solid mass up to 1.0 cm. in diameter. A macule is flat and small, like a freckle. A vesicle is filled with a serous fluid and less than 1.0 cm in diameter. A bullae is fluid filled and larger than 1.0 cm in diameter. The nurse practitioner is examining a 3-month-old infant who has normal development. She has identified an alopecic area at the occiput. What should be done? (Encourage the caregiver to change the infant’s head position) In a normally developing infant, an alopecic area at the occipital area generally develops because the infant has been placed in the supine position during sleeping and waking hours. Prolonged pressure on the occipital area can restrict hair growth. This is normal and will resolve when the infant begins to have better head control and movement; and she begins to have less pressure on the occipital area. Sometimes coarse, dry hair can be indicative of hypothyroidism; not necessarily alopecia. The most common form of skin cancer is: (basal cell carcinoma) Skin cancers are divided into two major groups: nonmelanoma and melanoma skin cancer. Basal cell carcinoma is considered nonmelanoma skin cancer and is the most common form of skin cancer in the US. It is most common in 40- to 60-year-olds, but can occur at any age if the skin is regularly exposed to sunlight or ultraviolet radiation. Basal cell carcinoma grows slowly, and if not treated it can spread to surrounding areas of tissue or bone. The nurse practitioner identifies satellite lesions in a 6-month-old infant. These are: (indicative of candidal infection) Satellite lesions are common in the diaper area of infants with a candidal diaper infection. They generally are associated with a beefy red rash. The skin creases are more commonly affected, but satellite lesions can be found anywhere that Candida can be found. A patient who is at high risk for skin cancer should: (examine his skin monthly for changes) Patients should be examined periodically for evidence of skin cancer by a professional examiner (NP, MD or PA). The frequency and type of examination depends on the risk level, and personal and family history of the patient. However, a patient should examine his own skin regularly for changes. Once he has begun to examine his skin, research demonstrates that he will identify early changes and can make his provider aware of them. An example of a premalignant lesion that develops on sun-damaged skin is: (actinic keratosis) Actinic keratoses (AK) are a result of solar damage to the skin. They are most common on the face, bald scalp, and forearms. Patients who present with AK usually have multiple of them. A characteristic that helps identification of AK is an area of erythema that surrounds the lesion. AK is sometimes easier felt than seen. Which of the following areas of the body has the greatest percutaneous absorption? (Genitalia) Genitalia have the highest percutaneous absorption across the entire body. This is important because low-potency creams will act with greater potency in this area. Low-potency creams/lotions should be used initially for treating skin conditions involving the genitalia. The sole of the foot has the lowest percutaneous absorption, followed by the scalp, forehead, and genitalia. Therefore, the sole of the foot will require more potent vehicles to enhance absorption. The main difference between cellulitis and erysipelas is the: (layer of skin involvement) Erysipelas and cellulitis both cause skin erythema, edema, and warmth. However, erysipelas involves the upper dermis and superficial lymphatics; cellulitis involves the deeper dermis and subcutaneous fat. Erysipelas is usually caused by Streptococcus; cellulitis may be caused by Staphylococcus and less commonly by Streptococcus. Most cases of atopic dermatitis exacerbation are treated with: (topical steroids) An exacerbation of atopic dermatitis is termed eczema. Under normal conditions, the skin should be kept well lubricated with emollients. These should be used liberally as often as needed to prevent skin from becoming dry. Dry skin is more prone to exacerbations. When an exacerbation occurs, topical steroids are very effective and are commonly used. The lowest potency steroid that resolves the exacerbation should be used. A 6-year-old patient with sore throat has coryza, hoarseness, and diarrhea. What is the likely etiology? (Viral etiology) This constellation of symptoms is typical of a viral infection. Group A Streptococcus is usually not accompanied by coryza. H. parainfluenzae is not a common cause of pharyngitis. Mycoplasma usually is associated with lower respiratory tract infections. A pregnant mother in her first trimester has a 5-year-old who has Fifth Disease. What implication does this have for the mother? (There is a risk of fetal death if she becomes infected) Pregnant mother should avoid exposure to patients with known Fifth Disease. However, the risk of transmission is very low. She should avoid exposure to aplastic patients who are infected because they are highly contagious. Infection during pregnancy is associated with a 10% risk of fetal death. There is no need for an ultrasound today. This pregnant patient does not have evidence of disease. She should be monitored for a rash which could indicate infection. A 74-year-old woman is diagnosed with shingles. The NP is deciding how to best manage her care. What should be prescribed? (An oral antiviral agent) An oral antiviral agent such as acyclovir, famciclovir or valacyclovir should be prescribed, especially if it can be initiated within 72 hours after the onset of symptoms. The addition of oral corticosteroids to oral antiviral therapy demonstrates only modest benefit. Adverse events to therapy are more commonly reported in patients receiving oral corticosteroids. There is no evidence that corticosteroid therapy decreases the incidence or duration of postherpetic neuralgia or improved quality of life. Corticosteroids should be limited to use in patients with acute neuritis who have not derived benefit from opioid analgesics. An adolescent has acne. The nurse practitioner prescribed a benzoyl peroxide product for him. What important teaching point should be given to this adolescent regarding the benzoyl peroxide? (Photosensitivity of the skin can occur) Benzoyl peroxide can produce sensitivity to the sun, so adolescents should be informed of this. This product can be used twice daily. It can cause peeling of the skin, but this is not a common occurrence. Hypersensitivity can occur with any topical product and is not specific to benzoyl peroxide. A 70-year-old is diagnosed with multiple cherry angiomas. The nurse practitioner knows that: (these may bleed profusely if ruptured) Cherry angiomas are mature capillary proliferations that are more common in middle-aged and older adults. They blanch with pressure and are usually 0.1-0.4 cm in diameter. They are commonly found on the trunk as multiple lesions. Because they are a proliferation of capillaries, they will bleed significantly if they rupture. The bleed is not life threatening, but in older adults who take aspirin, the bleeding will be worse. Pressure should be held over the ruptured area until bleeding stops. These are not precursors of skin malignancies. A patient has seborrheic dermatitis. Which vehicle would be most appropriate to use in the hairline area to treat this? (Foam) Seborrheic dermatitis affects the hairy areas of the body. In hairy areas of the body, foams are specifically used because they spread easily and are transparent. Lotions can be used in hairy areas because they provide a cooling, drying effect and are transparent. Lotions are the weakest of all vehicles. Creams and powders could be used, but patients prefer other vehicles and so adherence is less with these. A patient with eczema asks for a recommendation for a skin preparation to help with xerosis. What should the NP respond? (Use a petroleum-based product) Xerosis is dry skin. It is common in patients who have eczema. Using thick creams or ointments can prevent xerosis. Lotions should be avoided because they have high water content that promotes evaporation of water from the skin. Hypoallergenic refers to the allergenicity of a product. This is not related to the water content of products. A topical treatment for basal cell carcinoma is: (5-fluorouracil) Several treatments exist for basal and squamous cell carcinoma. The majority are simple procedures like cryotherapy, electrodessication, surgical excision, and a topical treatment like 5-fluorouracil (5-FU). The other agents listed are not used to treat basal or squamous cell carcinoma. 5-FU works by inhibiting DNA synthesis. It is effective if used for superficial basal cell carcinomas. It is available in cream and solution and is usually applied twice daily for 3-6 weeks. The most common place for basal cell carcinoma to be found is the: (Face) The most common presentation of basal cell carcinoma (BCC) is on the face. This is probably because BCC occurs secondary to sun damage. The most common sun exposure occurs on the face. In fact, 70% of BCC occurs on the face; 15% occurs on the trunk. An infant is diagnosed with diaper dermatitis. Satellite lesions are visible. This should be treated with a: (topical antifungal agent) The finding of satellite lesions associated with diaper dermatitis indicates a Candidal infection. This patient will be most effectively treated with a topical antifungal agent, allowing the lesions to be exposed to air for periods of time (like during a nap). A moisture barrier like zinc oxide is more beneficial when the diaper dermatitis is due to irritants like prolonged exposure to urine or feces. A low-potency steroid cream should be used with caution in an infant with a fungal infection. A low-potency steroid cream in conjunction with an antifungal can be helpful if there is a great amount of underlying inflammation, but it has the potential to worsen the infection. A 3-year-old female had a fever of 102° F for the last 3 days. Today she woke up from a nap and is afebrile. She has a maculopapular rash. Which statement is true? (The rash will blanch) This describes a patient with roseola or exanthem subitum. This is a common viral exanthem found in young children caused by human herpes virus 6. It is characterized by high fever for 3 days followed by the abrupt cessation of fever and the appearance of a maculopapular rash. This usually resolves in a few days. The child may return to school or daycare when he has been fever-free for 24 hours. A 71-year-old female presents with a vesicular rash that burns and itches. Shingles is diagnosed. An oral antiviral: (should be started within 72 hours of the onset of symptoms) This patient has been diagnosed with shingles. This can produce a painful neuritis. Shingles is treated with an oral antiviral agent, preferably within 72 hours of onset of the symptoms. Treating shingles with an oral antiviral agent shortens the severity and duration of shingles. It may also help decrease the incidence of post-herpetic neuralgia. A skin disorder has a hallmark finding of silvery scales. What word below describes this common condition? (Chronic) “Silvery scales” describes the hallmark finding in psoriasis. This is a chronic condition. It is not infectious, contagious, or acute. There are several variants, but “silvery scales” is the most common form. A child has 8-10 medium brown café au lait spots > 1 cm in diameter. The differential diagnosis should include: (neurofibromatosis) Neurofibromatosis (NF) is a common neurocutaneous disorder. The most common form is von Recklinghausen’s NF. Approximately 85% of patients with NF have this type. The incidence is about 1 in 2,600 people. Children with this disorder may have cognitive deficits, learning disabilities and other neurological related problems. They should be referred to neurology for diagnosis and treatment. A low-potency topical hydrocortisone cream would be most appropriate in a patient who has been diagnosed with: (atopic dermatitis) Low-potency steroid creams are almost never potent enough to treat psoriasis. Psoriasis requires higher-potency steroid preparation or systemic agents. Impetigo is a superficial bacterial infection, and a steroid cream would be contraindicated. Cellulitis is an infection of the subcutaneous layer of the skin and requires an oral or systemic antibiotic. Atopic dermatitis is a chronic inflammatory disorder of the skin that involves a genetic defect in the proteins supporting the epidermal layer. A patient with atopic dermatitis would be the most appropriate (of those listed above) to use a low-potency topical steroid cream. A patient is found to have koilonychia. What laboratory test would be prudent to perform? (Complete blood count) Koilonychia is the term that describes spoon-shaped nails. Spoon-shaped nails may be present in patients who have longstanding iron deficiency anemia. A CBC should be performed to assess for anemia. The most common symptoms of iron deficiency anemia are weakness, headache, irritability, fatigue, and exercise intolerance. A 23-year-old male appears in clinic with the following lesion on his trunk. This lesion is usually associated with: (pityriasis rosea) A herald patch is usually located on the trunk and associated with pityriasis rosea. It precedes the generalized Christmas tree pattern rash. Folliculitis is a superficial infection of the hair follicles. It presents as clusters of small, raised, erythematous lesions, not as a singular lesion as demonstrated in this image. Diabetes may be associated with acanthosis nigricans, a condition characterized by areas of velvety, hyperpigmented skin most commonly on the body folds and skin creases such as the neck and axillae. Hypothyroidism is not associated with this lesion. A 28-year-old has thick, demarcated plaques on her elbows. Which features are suggestive of psoriasis? (Silvery scales that are not pruritic) There are many different presentations of psoriasis. Plaque psoriasis, which is described in this question, is usually found in a symmetrical distribution on the scalp, elbows, knees, and/or back. The size of the lesions ranges from 1-10 cm in diameter. Usually the plaques are asymptomatic, but they may be mildly pruritic. Scaly lesions found on the scalp are not specific to psoriasis and could be seborrheic dermatitis. A scaly border around the plaque could describe the lesions associated with pityriasis rosea. Which of the following skin lesions in an older adult is a premalignant condition? (Actinic keratosis) Actinic keratosis is a premalignant condition of the skin and is considered an evolving carcinoma in situ. It is a precursor of squamous cell carcinoma. The lesions are usually multiple in occurrence and sit on an erythematous base. They appear dry, scaly, and flat and are usually secondary to sun damaged skin. Thus they are found on sun-exposed areas. The most common sites are the face, ears, lateral forearms, and tops of hands. A patient presents with plaques on the extensor surface of the elbows, knees, and back. The plaques are erythematous and thick, silvery scales are present. This is likely: (plaque psoriasis) Plaque psoriasis is seen initially in young adults and is characterized as described above. The thick, silvery scale is pathognomic and is usually asymptomatic, but some patients will complain of pruritus. A clinical finding that will help establish a diagnosis is pitting of fingernails. This occurs in about 50% of patients with psoriasis. The plaques are commonly distributed on the scalp, extensor surface of the elbows, knees, and back. This is a chronic skin disorder. A 15-year-old male has worked this summer as a lifeguard at a local swimming pool. He complains of itching in the groin area. He is diagnosed with tinea cruris. The nurse practitioner is likely to identify: (well marginated half-moon macules on the inner thigh) Tinea cruris, “jock itch” is common during warm months and in humid areas. It is a fungal infection that affects the scrotum and inner thighs, but never affects the penis and is never evidenced by scrotal swelling. He is probably at increased risk because he is working as a lifeguard and may wear damp or wet swim trunks during work. He should be treated with a topical antifungal cream, advised to dry off after swimming, and to put on dry swim trunks. A 68-year-old female adult with pendulous breasts complains of “burning” under her right breast. The nurse practitioner observes a malodorous discharge with mild maceration under both breasts. What is this? (Intertrigo) This is not unusual in adults with pendulous breasts. Intertrigo is common in areas between skin folds, under the breasts, between the scrotum and inner thigh, or between the toes. These are moist lesions that can be easily treated if the skin can be separated from touching the adjoining skin and the area can be kept dry. A topical powder with an antifungal would likely resolve this if used twice daily for 7-14 days. A diagnosis of diabetes should be considered if this is resistant to treatment or if it recurs. An example of a first-generation cephalosporin used to treat a skin infection is: (cephalexin) Two common first-generation cephalosporins used to treat skin and skin structure infections are cephalexin and cefadroxil. These are taken two to four times daily and are generally well tolerated. These antibiotics provide coverage against Staphylococcus and Streptococcus, common skin pathogens. A patient has a “herald patch” and is diagnosed with pityriasis rosea. Where is the “herald patch” most commonly found? (On the chest) The herald patch associated with pityriasis rosea is most commonly found on the trunk. It precedes the generalized Christmas tree pattern rash that is easily noted on the rest of the body. Because it appears round and has a darkened center, it looks like a ringworm. In fact, it is commonly mistaken for ringworm until the Christmas tree pattern rash appears. It would be unusual to identify the herald patch on a body part other than the trunk, but there are case reports of this. A 16-year-old has been diagnosed with Lyme disease. Which drug should be used to treat him? (Doxycycline) Doxycycline is frequently chosen first line to treat Lyme disease. However, numerous studies have demonstrated that amoxicillin and cefuroxime have equal efficacy as doxycycline in treatment of early Lyme disease. These drugs are recommended in patients who exhibit erythema migrans. Doxycycline is not recommended in children younger than 9 years of age. A 9-year-old female has presented to your clinic because of a rash on the left, upper area of her anterior trunk. She is embarrassed and very reticent to lift her blouse because her nipple will be exposed. How should the NP proceed? (Examine all other areas of the trunk, then ask the child to lift her blouse) The NP must visualize the area during exam so that an appropriate diagnosis can be made. Since the child is 9 years old, she should be given the opportunity to remove her blouse before allowing another adult to do this. Allowing the child to do this will put “control” in her hands. Hand-foot-and-mouth disease and herpangina: (are viral infections caused by Coxsackie viruses) These two common viral exanthems are caused by Coxsackie A viruses. Sometimes herpangina is caused by Coxsackie A or B. Ulcerations are produced on the mucous membranes, not pustules. Orchitis can occur in males infected with mumps. Herpangina typically occurs during summer and fall; hand-foot-and-mouth disease (HFM) occurs in late summer and fall. Both produce oral symptoms, but only HFM produces blisters on the palms of the hands and/or soles of the feet. Both are self-limiting viral illnesses A 74-year-old male patient has sustained a laceration to his foot. His last tetanus shot was more than 10 years ago. He has completed the primary series. What should be recommended? (Tetanus, diphtheria, and acellular pertussis (Tdap)) More than 10 years has elapsed since this patient’s last tetanus shot. He needs another one. Tdap is specifically indicated for adolescents, older adults, healthcare providers, and third trimester pregnant patients who have completed a primary series. Tetanus toxoid is indicated in the rare adult or child who is allergic to the aluminum adjuvant in the Td immunization. An adolescent takes isotretinoin for nodulocystic acne. She is on oral contraceptives. Both were prescribed by the dermatologist. The adolescent presents to your clinic with a sinus infection. Her temperature is 99.5° F and her blood pressure is 160/100 mmHg. How should this be managed? (Call the dermatologist to report the elevated BP) The nurse practitioner is responsible for treating the sinus infection but has also become aware of a potentially harmful situation involving the elevated blood pressure and oral contraceptive use. The safest and most professional action is to call the dermatologist to discuss your concerns regarding the elevated BP and concomitant oral contraceptive use since this potentially increases the risk of stroke in this adolescent. Care and professional courtesy should be exercised when discontinuing a medication that another provider has initiated. Professional courtesy is extended to the prescriber by calling them prior to discontinuing a medication they have ordered. Mr. Johnson is a 74-year-old who presents with a pearly-domed, nodular-looking lesion on the back of the neck. It does not hurt or itch. What is a likely etiology? (Basal cell carcinoma) Basal cell’s classic description is “a pearly-domed nodule with a telangiectatic vessel”. It is commonly found on sun-exposed areas like the head or neck. Sending the patient to dermatology (since these represent skin cancer) best treats these lesions. Sometimes these lesions can be treated with a topical agent like 5-fluorouracil if they are superficial; others require surgical removal. A 16-year-old male has nodulocystic acne. What might have the greatest positive impact in managing his acne? (Isotretinoin (Accutane)) Nodulocystic acne is the most severe form of acne vulgaris. Nodules and cysts characterize this disease. They can be palpated and usually seen on the skin, although they actually are under the skin’s surface. They develop when the follicle wall ruptures and leaks pus and cell contents into the dermis. The contaminated material infects adjoining follicles and the nodule develops. Isotretinoin is the only known effective treatment. Which of the following antibiotics may increase the likelihood of photosensitivity? (Ciprofloxacin) Many medications can produce a phototoxic reaction when a patient is exposed to sunlight. Antibiotics are especially notable for this. Common antibiotics associated with photosensitivity are tetracyclines, sulfa drugs, and fluoroquinolones. Ciprofloxacin is a fluoroquinolone. Amoxicillin and cephalexin are beta lactam antibiotics. Azithromycin is a macrolide antibiotic. Other common medications/classes that increase photosensitivity are hydrochlorothiazide, diltiazem, selective serotonin reuptake inhibitors, antihistamines, ibuprofen, and naproxen. Which of the following lesions never blanches when pressure is applied? (Purpura or petechiae) Blanching with pressure over spider angiomas always occurs. Spider veins and cherry angiomas usually blanch with pressure. Purpura and petechiae never blanch with pressure. Purpura and petechiae represent an extravasation of blood under the skin. These will not blanch when pressure is applied. This is usually observed in patients with thrombocytopenia or trauma. An older adult patient has been diagnosed with shingles on the right lateral aspect of her trunk. It initially appeared yesterday. It is very painful. How should she be managed? (An oral antiviral agent and pain medication) The primary goal of antiviral therapy in a patient diagnosed with shingles is to reduce the risk, or severity of postherpetic neuralgia. Since she has been identified within 72 hours of onset of lesions, she can be treated with most benefit with an oral antiviral agent. Studies do not demonstrate that patients have reduction of pain or resolution of symptoms faster if oral steroids are given. They should be avoided in older patients because there is no identified benefit. Shingles can be very painful, so treatment for pain should be priority. A young child has developed a circumferential lesion on her inner forearm. It is slightly raised, red and is pruritic. It is about 2.5 cm in diameter. This is probably related to: (the child’s new cat) This describes ringworm. It is a fungal infection that is common in children. A typical precipitant is a new animal like a cat. Since it appears on the inner forearm, it is likely the child got this from holding the cat. It should be treated with a topical antifungal agent. The primary therapeutic intervention for patients who present with hives is: (antihistamines) The primary cause of pruritus associated with hives is histamine release. Histamine is released from mast cells with other substances of anaphylaxis. Antihistamines are the primary therapeutic intervention. Topical steroid use is not helpful. Calcium channel blockers (nifedipine) are used as a “last resort” for refractory cases of urticaria. Steroids do not inhibit mast cell degradation and so are less helpful than thought. Steroids can be used for persistent attacks of acute urticaria if antihistamines are not helpful. The lesions seen in a patient with folliculitis might be filled with: (pus) Folliculitis is a superficial inflammation of hair follicles usually caused by bacteria. As a superficial infection, it involves only the epidermis. When this occurs, there are usually numerous pustular lesions. The composition of pus is dead white cells and other cellular debris. Which vehicle is least appropriate in a patient who has atopic dermatitis? (Lotions) Patients who have atopic dermatitis need continuous skin hydration. Lotions can worsen xerosis (dry skin) due to evaporation of water on the skin. In contrast to creams and ointments, lotions have a high water content and a low oil content. Creams have a lower water content. Ointments have no water and are excellent agents to use on dry skin as well as to prevent dry skin. A patient has been diagnosed with scabies. What is the medication of choice to treat this? (Permethrin) Scabies is eradicated by using permethrin and good hygiene. All household and personal contacts must be treated simultaneously, and meticulous care must be exercised to prevent transmission by cross contamination. All clothing, stuffed animals, linens, mattresses, and cloth furniture must be treated to prevent further transmission. The American Cancer Society uses an ABCDE mnemonic to help patients develop awareness of suspicious skin lesions. What does the “B” represent? (Border) The mnemonic is helpful when looking at skin lesions, but it is primarily used for patient education. The “A” represents asymmetry (asymmetrical lesions are worrisome), “B” is border (irregular borders), “C” is color (colored lesions have more melanin and may be associated with malignant melanoma), “D” is diameter (larger than a pencil eraser [6 mm] is concerning), and “E” represents enlarging or elevated (lesions that are actively enlarging are growing; elevated lesions are concerning). A “herald patch” is a hallmark finding in which condition? (Pityriasis rosea) Pityriasis rosea (PR) is a self-limiting exanthematous skin disorder characterized by several unique findings. It is more common in young adults. A characteristic finding is the “herald” or “mother” patch found on trunk. This looks like a ringworm and precedes the generalized “Christmas tree” pattern rash. The lesions associated with the rash are salmon-colored and oval in shape. Most cases clear in 4-6 weeks, but the plaques may last for several months. A patient has used a high-potency topical steroid cream for years to treat psoriasis exacerbations when they occur. She presents today and states that this cream “just doesn’t work anymore.” What word describes this? (Tachyphylaxis) Tachyphylaxis is the word used to describe a gradual and progressively poorer clinical response to a treatment or medication. This is particularly true of topical glucocorticoids, bronchodilators, nitroglycerine, and antihistamines when they are overused. The rebound effect describes a condition in which initial clinical improvement occurred, but worsening has occurred. Lichenification refers to a thickening of the skin. Drug-free intervals are important to prevent tachyphylaxis. A patient has been diagnosed with MRSA. She is allergic to sulfa. Which medication could be used to treat her? (Doxycycline) MRSA is methicillin-resistant Staph aureus. This is very common in the community and is typically treated with sulfa medications like TMP/SMX (Bactrim DS and Septra DS). If the patient is allergic to sulfa, this should not be used. A narrow-spectrum antibiotic that can be used is doxycycline or minocycline. It is given twice daily and is generally well tolerated. MRSA is resistant to the antibiotics in the other choices and so they should NOT be used to treat it. Topical 5-fluorouracil (5-FU) is used to treat: (basal cell carcinoma) 5-FU is a topical agent that can be used to treat basal cell carcinoma (BCC). It is most effective on rapidly proliferating cells. This treatment should only be used on superficial BCCs. If it is used on more invasive BCC, the cure rate is significantly lower. Therefore, 5-FU should be used only on superficial BCCs in noncritical locations. It is dosed as a 5% formulation twice daily for 3-6 weeks. A patient was burned with hot water. He has several 2-3 cm fluid-filled lesions. What are these termed? (Bullae) Bullae are fluid-filled lesions that are greater than 6 mm in diameter. These are common in patients who have a superficial partial-thickness burn. Vesicles are also fluid filled, but they are smaller than 5 mm in diameter. A cyst is enclosed in a sac that can contain fluid or gelatinous material. Wheals are erythematous, irregular raised areas on the skin. All of these are termed primary lesions. A child received a burn on his chest from a cup of hot coffee. On examination, the injured area appeared moist, red to ivory white in color, and features blisters. It is painful to touch. This burn would be classified as a: (superficial partial thickness burn) Types of burn injuries are chemical, electric, radiation, or thermal. They are classified by the depth of damaged skin. Symptoms of superficial partial thickness burns include: moist areas that are red to ivory white in color, immediate blister formation and painful to touch (pain receptors are intact). Superficial thickness burns appear erythematous without blisters and usually have local pain. Deep partial thickness burns have a dry, waxy, whitish appearance and resemble full thickness burns. Sometimes grafts are needed. Full thickness burns involve the destruction of all skin elements with coagulation of subdermal plexus, muscle, and or tendons. What finding is most characteristic of shingles? (Single dermatome affected) Shingles is herpes zoster. It characteristically affects a single dermatome. Grouped vesicles on an erythematous base may occur in some patients with shingles, but this is not unique to shingles. In fact, it is typical in many viral infections. Crusting may be seen with shingles, chicken pox, or impetigo. Pain, burning, and itching are symptoms that some patients have with shingles, but not all patients report itching with shingles. A patient reports that he found a tick on himself about 2 weeks ago. He presents today with a red circle and a white center near where he remembers the tick bite. He did not seek treatment at that time. Today he complains of myalgias and arthralgias. Which laboratory test can be used to help diagnose Lyme disease? (ELISA) A detailed history should always precede testing for Lyme disease. The red circle with the white center is likely erythema migrans (EM). EM is the characteristic skin lesion of Lyme disease (and other illnesses) and usually occurs within 1 month following the tick bite. Many learned authorities, including the Infectious Diseases Society of America, conclude that individuals should not be screened/tested for Lyme disease unless they have a high probability of having Lyme disease. In this case, historical features coupled with physical exam support the diagnosis, and thus screening. The most common initial serologic test for screening is an ELISA. If it is positive, it should be confirmed with a Western blot. Unfortunately, there are a large number of false positives and so a confirmation should be performed. The best way to evaluate jaundice associated with liver disease is to observe: (the sclera, skin, and lips) Looking at the sclera allows the examiner to see jaundice most easily and reliably. Jaundice may also appear in the palpebral conjunctiva, lips, hard palate, undersurface of the tongue, tympanic membrane, and skin. Jaundice in adults usually is a result of liver disease, but it can be due to excessive hemolysis of red blood cells. In infants, the usual cause is hemolysis of red blood cells, as is seen in physiologic jaundice. The term caput succedaneum refers to: (scalp edema) Caput succedaneum is a common finding in newborns. It is a result of pressure over the presenting part. This results in some ecchymosis of the scalp. While this may be disturbing to new parents who observe this in their newborn, it will resolve in a few days and is harmless. A 4-year-old has been diagnosed with measles. The nurse practitioner identifies Koplik’s spots. These are: (found on the inside of the cheek and are granular) Koplik’s spots are found in the oral cavity, especially on the buccal mucosa opposite the first and second molars. The spots are white and granular and are circled by an erythematous ring. The spots are pathognomonic for measles. The exanthem associated with measles is typically described as cranial to caudal in progression. The lesions become confluent and last for approximately 4 days before fading begins. A patient calls your office. He states that he just came in from the woods and discovered a tick on his upper arm. He states that he has removed the tick and the area is slightly red. What should he be advised? (No treatment is needed) Many factors must be present for a patient to develop Lyme disease from a tick bite. First, the tick must belong to Ixodes species. The tick must have been attached for at least 48 hours before disease can be spread. Time of year and stage of organism development affect transmission. There is no need for prophylactic treatment in this case because the tick has not been present long enough, though many patients will feel antibiotics are necessary. He could be checked to ensure that the entire tick has been removed. A wound has the following characteristics; partial thickness loss of dermis, a shallow open ulcer with red/pink bed, and no evidence of sloughing. What stage of pressure ulcer does this describe? (Stage II) Stage I is characterized by intact skin and nonblanchable redness of a localized area (usually over a bony prominence). Compared to adjacent tissue, the area may be painful, firm, soft, warmer or cooler. Stage II is characterized by partial-thickness loss of dermis presenting as a shallow open ulcer or a red-pink wound bed, absent sloughing. It may also present as an intact or open/ruptured serum-filled blister. Stage III is characterized by full-thickness tissue loss with or without visible subcutaneous fat; bone, tendon, and muscle are not exposed. Sloughing may be present but does not obscure the depth of tissue loss. The depth varies by anatomical location. Stage IV is characterized by full-thickness tissue loss with exposed bone, tendon, or muscle. Sloughing or eschar may be present on some parts of the wound bed. The depth varies by anatomical location. A patient has been in the sun for the past few weeks and has developed darkened skin and numerous 3-6 mm light-colored, flat lesions on his trunk. What is the likely etiology? (Tinea versicolor) Tinea versicolor is typically visualized during the spring and summer months when a patient has become darkened after sun exposure. The areas that are infected do not tan and so become very noticeable. The chest and back are common areas to observe tinea versicolor. There can be 100 or more in some infections. This can be treated with topical selenium sulfide or an oral antifungal agent. What advice should be given to a parent who has a child with Fifth Disease? (A parent may experience joint aches and pains) Fifth disease, erythema infectiosum, is a common viral exanthem seen in children 5-15 years of age. This produces a maculopapular rash that blanches easily. This rash is not pruritic but may last for several weeks before it completely goes away. Children are allowed to attend school as long as they have been fever free for 24 hours. Discomforts of this illness (fever, body aches, etc.) may be treated with acetaminophen or ibuprofen. Adults who are exposed to children with Fifth Disease may complain of arthralgias and myalgias for several weeks. A 6-year-old has been diagnosed with Lyme disease. Which drug should be used to treat him? (Amoxicillin) Amoxicillin, doxycycline, and cefuroxime have all been shown to have equivalent efficacy for treatment of Lyme disease. However, because this patient is 6 years old, he should not be given doxycycline as a first line treatment unless the other regimens are contraindicated. Macrolides like azithromycin should not be used first line because they are poorly effective at eradicating infection. They may be used in patients who are intolerant of penicillins and cephalosporins and who cannot take doxycycline. First-generation cephalosporins like cephalexin are poorly effective and should not be used. A patient presents with small vesicles on the lateral edges of his fingers and intense itching. On close inspection, there are small vesicles on the palmar surface of the hand. What is this called? (Dyshidrotic dermatitis) This dermatitis is intensely pruritic and involves the palms and soles and lateral aspects of the fingers. Over a couple of weeks, the vesicles desquamate. Recurrences are common. Seborrheic dermatitis affects only hairy areas of the body. The vesicles might raise suspicion of a viral infection, but this is not present in this case. A patient has 10 cm of well demarcated erythema on his lower leg that is raised and warm to touch. He had an abrupt onset of lower leg pain, and fever that began 36 hours ago. What is this? (Erysipelas) Erysipelas is characterized by an acute onset of symptoms as described in this scenario. Fever and chills are common. Patients with cellulitis tend to have a more gradual course, with development of symptoms over several days. The erythema noted in erysipelas is well demarcated and raised above the level of the skin. This elevation reflects that the more superficial dermis is involved. What is the proper technique to safely remove a tick from a human? (Pull it off with tweezers) Use tweezers to pull it off. If tweezers are not available, protected fingers should be used. The person removing the tick should take care NOT to crush the tick because it may contain infectious organisms. After the tick is removed, the skin should be washed well with soap and water. If mouth parts remain after the tick has been removed, they should NOT be removed. They will be expelled on their own and removal of these parts may cause significant skin trauma. The area should be monitored for 30 days for erythema migrans. A skin lesion fluoresces under a Wood’s lamp. What microscopic finding is consistent with this? (Hyphae) A Wood’s lamp emits ultraviolet light when turned on. If an area fluoresces under Wood’s lamp illumination, a fungal (and sometimes bacterial) infection should be suspected. Hyphae are associated with fungal infections. The test is most effectively performed in a darkened room so the fluorescence can be more easily identified. Deodorant, soap, and makeup may also fluoresce. About one-third of hyphae fluoresce. A 23-year-old male appears in clinic with the following nonpruritic lesion on his trunk. He first noticed this about 3 days ago. The lesion is probably: (a herald patch) Pityriasis rosea is a viral rash that is common in older children and young adults. It typically begins with a herald patch, a single round pink or salmon-colored, nonpruritic plaque on the chest, neck, or back. It is often mistaken for ringworm prior to the eruption of the Christmas tree pattern rash. The rash occurs within 1-2 weeks after the appearance of the herald patch. Scabies typically presents as a pruritic eruption characterized by small, erythematous, nondescript papules. Its prominent clinical feature is pruritus. Most cases of eczema initially occur by the age of five years, but can manifest in adults as an area of pruritic, thickened (lichenified), and excoriated skin in the flexural areas. Psoriasis may present as silvery scales or plaques. A patient presents to the minor care area of the emergency department after being bitten by a dog. The patient states that the dog had a tag around his neck and had been seen roaming around the neighborhood for days before the patient was bitten. The dog did not exhibit any odd behavior. How should this be managed? (Report the bite to animal control and administer appropriate medical care) All 50 states require reporting of animal bites to animal control or the state’s appropriate authority for reporting animal bites. It sounds unlikely that the dog could be infected with rabies, but rabies prophylaxis must be considered after all history and information has been gathered. Patients with atopic dermatitis are likely to exhibit: (itching) Atopic dermatitis is diagnosed on clinical presentation and includes evidence of pruritic skin. It is recurrent and often begins in childhood. For decades the "atopic triad" has been used to refer to patients with atopic dermatitis, asthma, and allergic rhinitis. This has recently been called into question. A similar triad, known as Samter’s triad, consists of asthma, aspirin sensitivity, and nasal polyps. Samter’s triad is not the same as the atopic triad. Which test is NOT suitable to diagnose shingles if the clinical presentation is questionable? (Complete blood count (CBC)) Herpes viruses are the causative agents in shingles, chickenpox, genital herpes, and oral fever blisters. Diagnosis is usually made on clinical presentation. However, in questionable cases, lab tests may be employed. A Tzanck preparation is a rapid test used to diagnose infections due to herpes viruses. Cells taken from a blister’s fluid are smeared on a slide and stained with a Wright’s stain, or the fluid can be used for other methods of testing. DFA is the most common test employed for shingles diagnosis because it can be rapidly performed and offers results in about 90 minutes. PCR may be performed on skin scrapings, serum or blood for herpetic diagnosis. CBC may indicate a patient with a viral infection, but it is nonspecific for herpetic infections. A patient exhibits petechiae on both lower legs but has no other complaints. How should the NP proceed? (Order a CBC) The presence of petechiae on the lower legs (or anywhere on the body) should prompt the NP to consider a problem that is related to a low platelet count. A CBC should be checked to assess the platelet count and for any evidence of anemia from blood loss. If the platelet count is found to be low, referral to hematology should be done. Blood cultures are of no value in this patient, who is otherwise asymptomatic. A 9-year-old has been diagnosed with chickenpox. A drug that should be avoided in him is: (aspirin) Aspirin should always avoided in the case of viral infections in children and adolescents. The incidence of Reye syndrome is increased if aspirin is given. This is especially true with varicella and influenza infections. The typical constellation of symptoms occurs during a bout of chickenpox and includes nausea, vomiting, headache, excitability, delirium, and combativeness with progression to coma. Since aspirin use has declined sharply, Reye syndrome has too. [Show More]
Last updated: 1 year ago
Preview 1 out of 17 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Dec 31, 2019
Number of pages
17
Written in
Additional information
This document has been written for:
Uploaded
Dec 31, 2019
Downloads
0
Views
79