*NURSING > QUESTIONS & ANSWERS > NR 328 Pediatric Nursing / NR 328 Final Exam 1 Test Bank (Questions & Answers explained) 2020. (All)
NR 328 Pediatric Nursing / NR 328 Final Exam 1 Test Bank (Questions & Answers explained) 2020.
Document Content and Description Below
NR 328 Final Exam 1 Test Bank (Questions / Answers) Chapter 01: Perspectives of Pediatric Nursing MULTIPLE CHOICE 1. The clinic nurse is reviewing statistics on infant mortality for the United Stat... es versus other countries. Compared with other countries that have a population of at least 25 million, the nurse makes which determination? a. The United States is ranked last among 27 countries. b. The United States is ranked similar to 20 other developed countries. c. The United States is ranked in the middle of 20 other developed countries. d. The United States is ranked highest among 27 other industrialized countries. 2. Which is the leading cause of death in infants younger than 1 year in the United States? a. Congenital anomalies b. Sudden infant death syndrome c. Disorders related to short gestation and low birth weight d. Maternal complications specific to the perinatal period 3. What is the major cause of death for children older than 1 year in the United States? a. Heart disease b. Childhood cancer c. Unintentional injuries d. Congenital anomalies 4. In addition to injuries, what are the leading causes of death in adolescents ages 15 to 19 years? a. Suicide and cancer b. Suicide and homicide c. Drowning and cancer d. Homicide and heart disease 5. The nurse is planning a teaching session to adolescents about deaths by unintentional injuries. Which should the nurse include in the session with regard to deaths caused by injuries? a. More deaths occur in males. b. More deaths occur in females. c. The pattern of deaths does not vary according to age and sex. d. The pattern of deaths does not vary widely among different ethnic groups. 6. What do mortality statistics describe? a. Disease occurring regularly within a geographic location b. The number of individuals who have died over a specific period c. The prevalence of specific illness in the population at a particular time d. Disease occurring in more than the number of expected cases in a community 7. The nurse should assess which age group for suicide ideation since suicide in which age group is the third leading cause of death? a. Preschoolers b. Young school age c. Middle school age d. Late school age and adolescents 8. Parents of a hospitalized toddler ask the nurse, “What is meant by family-centered care?” The nurse should respond with which statement? a. Family-centered care reduces the effect of cultural diversity on the family. b. Family-centered care encourages family dependence on the health care system. c. Family-centered care recognizes that the family is the constant in a child’s life. d. Family-centered care avoids expecting families to be part of the decision-making process. 9. The nurse is describing clinical reasoning to a group of nursing students. Which is most descriptive of clinical reasoning? a. Purposeful and goal directed b. A simple developmental process c. Based on deliberate and irrational thought d. Assists individuals in guessing what is most appropriate 10. Evidence-based practice (EBP), a decision-making model, is best described as which? a. Using information in textbooks to guide care b. Combining knowledge with clinical experience and intuition c. Using a professional code of ethics as a means for decision making d. Gathering all evidence that applies to the child’s health and family situation 11. Which best describes signs and symptoms as part of a nursing diagnosis? a. Description of potential risk factors b. Identification of actual health problems c. Human response to state of illness or health d. Cues and clusters derived from patient assessment 12. The nurse is talking to a group of parents of school-age children at an after-school program about childhood health problems. Which statement should the nurse include in the teaching? a. Childhood obesity is the most common nutritional problem among children. b. Immunization rates are the same among children of different races and ethnicity. c. Dental caries is not a problem commonly seen in children since the introduction of fluoridated water. d. Mental health problems are typically not seen in school-age children but may be diagnosed in adolescents. 13. The nurse is planning care for a hospitalized preschool-aged child. Which should the nurse plan to ensure atraumatic care? a. Limit explanation of procedures because the child is preschool aged. b. Ask that all family members leave the room when performing procedures. c. Allow the child to choose the type of juice to drink with the administration of oral medications. d. Explain that EMLA cream cannot be used for the morning lab draw because there is not time for it to be effective. 14. Which situation denotes a nontherapeutic nurse–patient–family relationship? a. The nurse is planning to read a favorite fairy tale to a patient. b. During shift report, the nurse is criticizing parents for not visiting their child. c. The nurse is discussing with a fellow nurse the emotional draw to a certain patient. d. The nurse is working with a family to find ways to decrease the family’s dependence on health care providers. 15. The nurse is aware that which age group is at risk for childhood injury because of the cognitive characteristic of magical and egocentric thinking? a. Preschool b. Young school age c. Middle school age d. Adolescent 16. The school nurse is assessing children for risk factors related to childhood injuries. Which child has the most risk factors related to childhood injury? a. Female, multiple siblings, stable home life b. Male, high activity level, stressful home life c. Male, even tempered, history of previous injuries d. Female, reacts negatively to new situations, no serious previous injuries 17. The school nurse is evaluating the number of school-age children classified as obese. The nurse recognizes that the percentile of body mass index that classifies a child as obese is greater than which? a. 50th percentile b. 75th percentile c. 80th percentile d. 95th percentile 18. The nurse is teaching parents about the types of behaviors children exhibit when living with chronic violence. Which statement made by the parents indicates further teaching is needed? a. “We should watch for aggressive play.” b. “Our child may show lasting symptoms of stress.” c. “We know that our child will show caring behaviors.” d. “Our child may have difficulty concentrating in school.” 19. The nurse is evaluating research studies according to the GRADE criteria and has determined the quality of evidence on the subject is moderate. Which type of evidence does this determination indicate? a. Strong evidence from unbiased observational studies b. Evidence from randomized clinical trials showed inconsistent results c. Consistent evidence from well-performed randomized clinical trials d. Evidence for at least one critical outcome from randomized clinical trials had serious flaws 20. An adolescent patient wants to make decisions about treatment options, along with his parents. Which moral value is the nurse displaying when supporting the adolescent to make decisions? a. Justice b. Autonomy c. Beneficence d. Nonmaleficence 21. The nurse manager is compiling a report for a hospital committee on the quality of nursing-sensitive indicators for a nursing unit. Which does the nurse manager include in the report? a. The average age of the nurses on the unit b. The salary ranges for the nurses on the unit c. The education and certification of the nurses on the unit d. The number of nurses who have applied but were not hired for the unit MULTIPLE RESPONSE 1. Which responsibilities are included in the pediatric nurse’s promotion of the health and well-being of children? (Select all that apply.) a. Promoting disease prevention b. Providing financial assistance c. Providing support and counseling d. Establishing lifelong friendships e. Establishing a therapeutic relationship f. Participating in ethical decision making 2. The nurse is conducting a teaching session for parents on nutrition. Which characteristics of families should the nurse consider that can cause families to struggle in providing adequate nutrition? (Select all that apply.) a. Homelessness b. Lower income c. Migrant status d. Working parents e. Single parent status 3. The nurse is preparing to complete documentation on a patient’s chart. Which should be included in documentation of nursing care? (Select all that apply.) a. Reassessments b. Incident reports c. Initial assessments d. Nursing care provided e. Patient’s response of care provided 4. Which actions by the nurse demonstrate overinvolvement with patients and their families? (Select all that apply.) a. Buying clothes for the patients b. Showing favoritism toward a patient c. Focusing on technical aspects of care d. Spending off-duty time with patients and families e. Asking questions if families are not participating in care 5. Which are included in the evaluation step of the nursing process? (Select all that apply.) a. Determination if the outcome has been met b. Ascertaining if the plan requires modification c. Establish priorities and selecting expected patient goals d. Selecting alternative interventions if the outcome has not been met e. Determining if a risk or actual dysfunctional health problem exists 6. Which should the nurse teach to parents regarding oral health of children? (Select all that apply.) a. Fluoridated water should be used. b. Early childhood caries is a preventable disease. c. Dental caries is a rare chronic disease of childhood. d. Dental hygiene should begin with the first tooth eruption. e. Childhood caries does not happen until after 2 years of age. 7. The school nurse is explaining to older school children that obesity increases the risk for which disorders? (Select all that apply.) a. Asthma b. Hypertension c. Dyslipidemia d. Irritable bowel disease e. Altered glucose metabolism 8. The nurse is reviewing the Healthy People 2020 leading health indicators for a child health promotion program. Which are included in the leading health indicators? (Select all that apply.) a. Decrease tobacco use. b. Improve immunization rates. c. Reduce incidences of cancer. d. Increase access to health care. e. Decrease the number of eating disorders. 9. Which actions by the nurse demonstrate clinical reasoning? (Select all that apply.) a. Basing decisions on intuition b. Considering alternative action c. Using formal and informal thinking to gather data d. Giving deliberate thought to a patient’s problem e. Developing an outcome focused on optimum patient care . COMPLETION 1. The nurse is determining if a newborn is classified in the low birth weight (LBW) category of less than 2500 g. The newborn’s weight is 5 lb, 4 oz. What is the newborn’s weight in grams? Record your answer in a whole number. __________________ MATCHING The nursing process is a method of problem identification and problem solving that describes what the nurse actually does. Match each step of the nursing process with its definition. a. Assessment b. Diagnosis c. Outcomes identification d. Planning e. Implementation f. Evaluation Ethical dilemmas arise when competing moral considerations underlie various alternatives. Match each competing moral value with its definition. a. Autonomy b. Nonmaleficence c. Beneficence d. Justice Chapter 02: Social, Cultural, Religious, and Family Influences on Child Health Promotion MULTIPLE CHOICE 1. Children are taught the values of their culture through observation and feedback relative to their own behavior. In teaching a class on cultural competence, the nurse should be aware that which factor may be culturally determined? a. Ethnicity b. Racial variation c. Status d. Geographic boundaries 2. The nurse is aware that if patients’ different cultures are implied to be inferior, the emotional attitude the nurse is displaying is what? a. Acculturation b. Ethnocentrism c. Cultural shock d. Cultural sensitivity 3. Which term best describes the sharing of common characteristics that differentiates one group from other groups in a society? a. Race b. Culture c. Ethnicity d. Superiority 4. After the family, which has the greatest influence on providing continuity between generations? a. Race b. School c. Social class d. Government 5. The nurse is planning care for a patient with a different ethnic background. Which should be an appropriate goal? a. Adapt, as necessary, ethnic practices to health needs. b. Attempt, in a nonjudgmental way, to change ethnic beliefs. c. Encourage continuation of ethnic practices in the hospital setting. d. Strive to keep ethnic background from influencing health needs. 6. The nurse discovers welts on the back of a Vietnamese child during a home health visit. The child’s mother says she has rubbed the edge of a coin on her child’s oiled skin. The nurse should recognize this as what? a. Child abuse b. Cultural practice to rid the body of disease c. Cultural practice to treat enuresis or temper tantrums d. Child discipline measure common in the Vietnamese culture 7. A Hispanic toddler has pneumonia. The nurse notices that the parent consistently feeds the child only the broth that comes on the clear liquid tray. Food items, such as Jell-O, Popsicles, and juices, are left. Which statement best explains this? a. The parent is trying to feed the child only what the child likes most. b. Hispanics believe the “evil eye” enters when a person gets cold. c. The parent is trying to restore normal balance through appropriate “hot” remedies. d. Hispanics believe an innate energy called chi is strengthened by eating soup. 8. How is family systems theory best described? a. The family is viewed as the sum of individual members. b. A change in one family member cannot create a change in other members. c. Individual family members are readily identified as the source of a problem. d. When the family system is disrupted, change can occur at any point in the system. 9. Which family theory is described as a series of tasks for the family throughout its life span? a. Exchange theory b. Developmental theory c. Structural-functional theory d. Symbolic interactional theory . 10. Which family theory explains how families react to stressful events and suggests factors that promote adaptation to these events? a. Interactional theory b. Family stress theory c. Erikson’s psychosocial theory d. Developmental systems theory 11. Which type of family should the nurse recognize when the paternal grandmother, the parents, and two minor children live together? a. Blended b. Nuclear c. Extended d. Binuclear 12. Which type of family should the nurse recognize when a mother, her children, and a stepfather live together? a. Traditional nuclear b. Blended c. Extended d. Binuclear 13. Which is an accurate description of homosexual (or gay-lesbian) families? a. A nurturing environment is lacking. b. The children become homosexual like their parents. c. The stability needed to raise healthy children is lacking. d. The quality of parenting is equivalent to that of nongay parents. 14. The nurse is teaching a group of new nursing graduates about identifiable qualities of strong families that help them function effectively. Which quality should be included in the teaching? a. Lack of congruence among family members b. Clear set of family values, rules, and beliefs c. Adoption of one coping strategy that always promotes positive functioning in dealing with life events d. Sense of commitment toward growth of individual family members as opposed to that of the family unit 15. When assessing a family, the nurse determines that the parents exert little or no control over their children. This style of parenting is called which? a. Permissive b. Dictatorial c. Democratic d. Authoritarian 16. When discussing discipline with the mother of a 4-year-old child, which should the nurse include? a. Parental control should be consistent. b. Withdrawal of love and approval is effective at this age. c. Children as young as 4 years rarely need to be disciplined. d. One should expect rules to be followed rigidly and unquestioningly. 17. Which is a consequence of the physical punishment of children, such as spanking? a. The psychologic impact is usually minimal. b. The child’s development of reasoning increases. c. Children rarely become accustomed to spanking. d. Misbehavior is likely to occur when parents are not present. 18. The parents of a young child ask the nurse for suggestions about discipline. When discussing the use of time-outs, which should the nurse include? a. Send the child to his or her room if the child has one. b. A general rule for length of time is 1 hour per year of age. c. Select an area that is safe and nonstimulating, such as a hallway. d. If the child cries, refuses, or is more disruptive, try another approach. . 19. A 3-year-old child was adopted immediately after birth. The parents have just asked the nurse how they should tell the child that she is adopted. Which guideline concerning adoption should the nurse use in planning a response? a. It is best to wait until the child asks about it. b. The best time to tell the child is between the ages of 7 and 10 years. c. It is not necessary to tell a child who was adopted so young. d. Telling the child is an important aspect of their parental responsibilities. 20. Children may believe that they are responsible for their parents’ divorce and interpret the separation as punishment. At which age is this most likely to occur? a. 1 year b. 4 years c. 8 years d. 13 years 21. A parent of a school-age child tells the school nurse that the parents are going through a divorce. The child has not been doing well in school and sometimes has trouble sleeping. The nurse should recognize this as what? a. Indicative of maladjustment b. A common reaction to divorce c. Suggestive of a lack of adequate parenting d. An unusual response that indicates a need for referral 22. A mother brings 6-month-old Eric to the clinic for a well-baby checkup. She comments, “I want to go back to work, but I don’t want Eric to suffer because I’ll have less time with him.” Which is the nurse’s most appropriate answer? a. “I’m sure he’ll be fine if you get a good babysitter.” b. “You will need to stay home until Eric starts school.” c. “Let’s talk about the child care options that will be best for Eric.” d. “You should go back to work so Eric will get used to being with others.” 23. A foster parent is talking to the nurse about the health care needs for the child who has been placed in the parent’s care. Which statement best describes the health care needs of foster children? a. Foster children always come from abusive households and are emotionally fragile. b. Foster children tend to have a higher than normal incidence of acute and chronic health problems. c. Foster children are usually born prematurely and require technologically advanced health care. d. Foster children will not stay in the home for an extended period, so health care needs are not as important as emotional fulfillment. 24. The nurse is planning to counsel family members as a group to assess the family’s group dynamics. Which theoretic family model is the nurse using as a framework? a. Feminist theory b. Family stress theory c. Family systems theory d. Developmental theory 25. The nurse is reviewing the importance of role learning for children. The nurse understands that children’s roles are primarily shaped by which members? a. Peers b. Parents c. Siblings d. Grandparents 26. The nurse is caring for an adolescent hospitalized for asthma. The adolescent belongs to a large family. The nurse recognizes that the adolescent is likely to relate to which group? a. Peers b. Parents c. Siblings d. Teachers 27. The nurse is explaining different parenting styles to a group of parents. The nurse explains that an authoritative parenting style can lead to which child behavior? a. Shyness b. Self-reliance c. Submissiveness d. Self-consciousness 28. Parents of a preschool child ask the nurse, “Should we set rules for our child as part of a discipline plan?” Which is an accurate response by the nurse? a. “It is best to delay the punishment if a rule is broken.” b. “The child is too young for rules. At this age, unrestricted freedom is best.” c. “It is best to set the rules and reason with the child when the rules are broken.” d. “Set clear and reasonable rules and expect the same behavior regardless of the circumstances.” 29. The nurse is discussing issues that are important with parents considering a cross-racial adoption. Which statement made by the parents indicates further teaching is needed? a. “We will try to preserve the adopted child’s racial heritage.” b. “We are glad we will be getting full medical information when we adopt our child.” c. “We will make sure to have everyone realize this is our child and a member of the family.” d. “We understand strangers may make thoughtless comments about our child being different from us.” 30. The school nurse understands that children are impacted by divorce. Which has the most impact on the positive outcome of a divorce? a. Age of the child b. Gender of the child c. Family characteristics d. Ongoing family conflict 31. The nurse is discussing parenting in reconstituted families with a new stepparent. The nurse is aware that the new stepparent understands the teaching when which statement is made? a. “I am glad there will be no disruption in my lifestyle.” b. “I don’t think children really want to live in a two-parent home.” c. “I realize there may be power conflicts bringing two households together.” d. “I understand contact between grandparents should be kept to a minimum.” MULTIPLE RESPONSE 1. The nurse is presenting a staff development program about understanding culture in the health care encounter. Which components should the nurse include in the program? (Select all that apply.) a. Cultural humility b. Cultural research c. Cultural sensitivity d. Cultural competency 2. The parents of a 5-year-old child ask the nurse how they can minimize misbehavior. Which responses should the nurse give? (Select all that apply.) a. Set clear and reasonable goals. b. Praise your child for desirable behavior. c. Don’t call attention to unacceptable behavior. d. Teach desirable behavior through your own example. e. Don’t provide an opportunity for your child to have any control. 3. Which describe the feelings and behaviors of early preschool children related to divorce? (Select all that apply.) a. Regressive behavior b. Fear of abandonment c. Fear regarding the future d. Blame themselves for the divorce e. Intense desire for reconciliation of parents 4. Which describe the feelings and behaviors of adolescents related to divorce? (Select all that apply.) a. Disturbed concept of sexuality b. May withdraw from family and friends c. Worry about themselves, parents, or siblings d. Expression of anger, sadness, shame, or embarrassment e. Engage in fantasy to seek understanding of the divorce 5. The nurse is teaching parents about the effects of media on childhood obesity. The nurse realizes the parents understand the teaching if they make which statements? (Select all that apply.) a. “Advertising of unhealthy food can increase snacking.” b. “Increased screen time may be related to unhealthy sleep.” c. “There is a link between the amount of screen time and obesity.” d. “Increased screen time can lead to better knowledge of nutrition.” e. “Physical activity increases when children increase the amount of screen time.” MATCHING Culture characterizes a particular group with its values, beliefs, norms, patterns, and practices that are learned, shared, and transmitted from one generation to another. Match the terms used to describe groups with shared values, beliefs, norms, patterns, and practices. a. Race b. Gender c. Ethnicity d. Social class e. Socialization Chapter 04: Communication, Physical, and Developmental Assessment MULTIPLE CHOICE 1. The nurse is seeing an adolescent and the parents in the clinic for the first time. Which should the nurse do first? a. Introduce him- or herself. b. Make the family comfortable. c. Give assurance of privacy. d. Explain the purpose of the interview. 2. Which is considered a block to effective communication? a. Using silence b. Using clichés c. Directing the focus d. Defining the problem 3. Which is the single most important factor to consider when communicating with children? a. Presence of the child’s parent b. Child’s physical condition c. Child’s developmental level d. Child’s nonverbal behaviors 4. Because children younger than 5 years are egocentric, the nurse should do which when communicating with them? a. Focus communication on the child. b. Use easy analogies when possible. c. Explain experiences of others to the child. d. Assure the child that communication is private. 5. The nurse’s approach when introducing hospital equipment to a preschooler who seems afraid should be based on which principle? a. The child may think the equipment is alive. b. Explaining the equipment will only increase the child’s fear. c. One brief explanation will be enough to reduce the child’s fear. d. The child is too young to understand what the equipment does. 6. When the nurse interviews an adolescent, which is especially important? a. Focus the discussion on the peer group. b. Allow an opportunity to express feelings. c. Use the same type of language as the adolescent. d. Emphasize that confidentiality will always be maintained. 7. The nurse is preparing to assess a 10-month-old infant. He is sitting on his father’s lap and appears to be afraid of the nurse and of what might happen next. Which initial actions by the nurse should be most appropriate? a. Initiate a game of peek-a-boo. b. Ask the infant’s father to place the infant on the examination table. c. Talk softly to the infant while taking him from his father. d. Undress the infant while he is still sitting on his father’s lap. 8. An 8-year-old girl asks the nurse how the blood pressure apparatus works. The most appropriate nursing action is which? a. Ask her why she wants to know. b. Determine why she is so anxious. c. Explain in simple terms how it works. d. Tell her she will see how it works as it is used. 9. The nurse is having difficulty communicating with a hospitalized 6-year-old child. Which technique should be most helpful? a. Recommend that the child keep a diary. b. Provide supplies for the child to draw a picture. c. Suggest that the parent read fairy tales to the child. d. Ask the parent if the child is always uncommunicative. 10. Which data should be included in a health history? a. Review of systems b. Physical assessment c. Growth measurements d. Record of vital signs 11. The nurse is taking a health history of an adolescent. Which best describes how the chief complaint should be determined? a. Request a detailed listing of symptoms. b. Ask the adolescent, “Why did you come here today?” c. Interview the parent away from the adolescent to determine the chief complaint. d. Use what the adolescent says to determine, in correct medical terminology, what the problem is. 12. The nurse is interviewing the mother of an infant. The mother reports, “I had a difficult delivery, and my baby was born prematurely.” This information should be recorded under which heading? a. History b. Present illness c. Chief complaint d. Review of systems 13. Where in the health history does a record of immunizations belong? a. History b. Present illness c. Review of systems d. Physical assessment 14. The nurse is taking a sexual history on an adolescent girl. Which is the best way to determine whether she is sexually active? a. Ask her, “Are you sexually active?” b. Ask her, “Are you having sex with anyone?” c. Ask her, “Are you having sex with a boyfriend?” d. Ask both the girl and her parent if she is sexually active. 15. When doing a nutritional assessment on a Hispanic family, the nurse learns that their diet consists mainly of vegetables, legumes, and starches. The nurse should recognize that this diet is which? a. Lacking in protein b. Indicating they live in poverty c. Providing sufficient amino acids d. Needing enrichment with meat and milk . 16. Which parameter correlates best with measurements of total muscle mass? a. Height b. Weight c. Skinfold thickness d. Upper arm circumference 17. The nurse is preparing to perform a physical assessment on a 10-year-old girl. The nurse gives her the option of her mother staying in the room or leaving. This action should be considered which? a. Appropriate because of child’s age b. Appropriate, but the mother may be uncomfortable c. Inappropriate because of child’s age d. Inappropriate because child is same sex as mother 18. With the National Center for Health Statistics criteria, which body mass index (BMI)–for-age percentiles should indicate the patient is at risk for being overweight? a. 10th percentile b. 75th percentile c. 85th percentile d. 95th percentile 19. Rectal temperatures are indicated in which situation? a. In the newborn period b. Whenever accuracy is essential c. Rectal temperatures are never indicated d. When rapid temperature changes are occurring 20. What is the earliest age at which a satisfactory radial pulse can be taken in children? a. 1 year b. 2 years c. 3 years d. 6 years 21. The nurse needs to take the blood pressure of a small child. Of the cuffs available, one is too large and one is too small. The best nursing action is which? a. Use the small cuff. b. Use the large cuff. c. Use either cuff using the palpation method. d. Wait to take the blood pressure until a proper cuff can be located. 22. Where is the best place to observe for the presence of petechiae in dark-skinned individuals? a. Face b. Buttocks c. Oral mucosa d. Palms and soles 23. During a routine health assessment, the nurse notes that an 8-month-old infant has a significant head lag. Which is the most appropriate action? a. Recheck head control at next visit. b. Teach the parents appropriate exercises. c. Schedule the child for further evaluation. d. Refer the child for further evaluation if the anterior fontanel is still open. 24. The nurse has just started assessing a young child who is febrile and appears ill. There is hyperextension of the child’s head (opisthotonos) with pain on flexion. Which is the most appropriate action? a. Ask the parent when the neck was injured. b. Refer for immediate medical evaluation. c. Continue assessment to determine the cause of the neck pain. d. Record “head lag” on the assessment record and continue the assessment of the child. 25. During a funduscopic examination of a school-age child, the nurse notes a brilliant, uniform red reflex in both eyes. The nurse should recognize that this is which? a. A normal finding b. A sign of a possible visual defect and a need for vision screening c. An abnormal finding requiring referral to an ophthalmologist d. A sign of small hemorrhages, which usually resolve spontaneously 26. Which explains the importance of detecting strabismus in young children? a. Color vision deficit may result. b. Amblyopia, a type of blindness, may result. c. Epicanthal folds may develop in the affected eye. d. Corneal light reflexes may fall symmetrically within each pupil. 27. Which is the most frequently used test for measuring visual acuity? a. Snellen letter chart b. Ishihara vision test c. Allen picture card test d. Denver eye screening test 28. The nurse is testing an infant’s visual acuity. By which age should the infant be able to fix on and follow a target? a. 1 month b. 1 to 2 months c. 3 to 4 months d. 6 months 29. During an otoscopic examination on an infant, in which direction is the pinna pulled? a. Up and back b. Up and forward c. Down and back d. Down and forward 30. What is an appropriate screening test for hearing that the nurse can administer to a 5-year-old child? a. Rinne test b. Weber test c. Pure tone audiometry d. Eliciting the startle reflex 31. What is the appropriate placement of a tongue blade for assessment of the mouth and throat? a. On the lower jaw b. Side of the tongue c. Against the soft palate d. Center back area of the tongue 32. When assessing a preschooler’s chest, what should the nurse expect? a. Respiratory movements to be chiefly thoracic b. Anteroposterior diameter to be equal to the transverse diameter c. Retraction of the muscles between the ribs on respiratory movement d. Movement of the chest wall to be symmetric bilaterally and coordinated with breathing 33. When auscultating an infant’s lungs, the nurse detects diminished breath sounds. What should the nurse interpret this as? a. Suggestive of chronic pulmonary disease b. Suggestive of impending respiratory failure c. An abnormal finding warranting investigation d. A normal finding in infants younger than 1 year of age 34. Which type of breath sound is normally heard over the entire surface of the lungs except for the upper intrascapular area and the area beneath the manubrium? a. Vesicular b. Bronchial c. Adventitious d. Bronchovesicular 35. The nurse is assessing a child’s capillary refill time. This can be accomplished by doing what? a. Inspect the chest. b. Auscultate the heart. c. Palpate the apical pulse. d. Palpate the nail bed with pressure to produce a slight blanching. 36. Which heart sound is produced by vibrations within the heart chambers or in the major arteries from the back-and-forth flow of blood? a. S1 and S2 b. S3 and S4 c. Murmur d. Physiologic splitting 37. Examination of the abdomen is performed correctly by the nurse in which order? a. Inspection, palpation, percussion, and auscultation b. Inspection, percussion, auscultation, and palpation c. Palpation, percussion, auscultation, and inspection d. Inspection, auscultation, percussion, and palpation 38. Superficial palpation of the abdomen is often perceived by the child as tickling. Which measure by the nurse is most likely to minimize this sensation and promote relaxation? a. Palpate another area simultaneously. b. Ask the child not to laugh or move if it tickles. c. Begin with deeper palpation and gradually progress to superficial palpation. d. Have the child “help” with palpation by placing his or her hand over the palpating hand. 39. During examination of a toddler’s extremities, the nurse notes that the child is bowlegged. The nurse should recognize that this finding is which? a. Abnormal and requires further investigation b. Abnormal unless it occurs in conjunction with knock-knee c. Normal if the condition is unilateral or asymmetric d. Normal because the lower back and leg muscles are not yet well developed 40. The nurse is caring for a non–English-speaking child and family. Which should the nurse consider when using an interpreter? a. Pose several questions at a time. b. Use medical jargon when possible. c. Communicate directly with family members when asking questions. d. Carry on some communication in English with the interpreter about the family’s needs. 1. Which action should the nurse implement when taking an axillary temperature? a. Take the temperature through one layer of clothing. b. Add a degree to the result when recording the temperature. c. Place the tip of the thermometer under the arm in the center of the axilla. d. Hold the child’s arm away from the body while taking the temperature. 42. The nurse is aware that skin turgor best estimates what? a. Perfusion b. Adequate hydration c. Amount of body fat d. Amount of anemia 43. The Asian parent of a child being seen in the clinic avoids eye contact with the nurse. What is the best explanation for this considering cultural differences? a. The parent feels inferior to the nurse. b. The parent is showing respect for the nurse. c. The parent is embarrassed to seek health care. d. The parent feels responsible for her child’s illness. MULTIPLE RESPONSE 1. The nurse is performing an otoscopic examination on a child. Which are normal findings the nurse should expect? (Select all that apply.) a. Ashen gray areas b. A well-defined light reflex c. A small, round, concave spot near the center of the drum d. The tympanic membrane is a nontransparent grayish color e. A whitish line extending from the umbo upward to the margin of the membrane 2. The nurse is assessing breath sounds on a child. Which are expected auscultated breath sounds? (Select all that apply.) a. Wheezes b. Crackles c. Vesicular d. Bronchial e. Bronchovesicular 3. The nurse is performing an oral examination on a preschool child. Which strategies should the nurse use to encourage the child to open the mouth for the examination? (Select all that apply.) a. Lightly brush the palate with a cotton swab. b. Perform the examination in front of a mirror. c. Let the child examine someone else’s mouth first. d. Have the child breathe deeply and hold his or her breath. e. Use a tongue blade to help the child open his or her mouth. 4. Which are effective auscultation techniques? (Select all that apply.) a. Ask the child to breathe shallowly. b. Apply light pressure on the chest piece. c. Use a symmetric and orderly approach. d. Place the stethoscope over one layer of clothing. e. Warm the stethoscope before placing it on the skin. 5. The nurse is assessing heart sounds on a school-age child. Which should the nurse document as abnormal findings if found on the assessment? (Select all that apply.) a. S4 heart sound b. S3 heart sound c. Grade II murmur d. S1 louder at the apex of the heart e. S2 louder than S1 in the aortic area 6. The nurse understands that blocks to therapeutic communication include what? (Select all that apply.) a. Socializing b. Use of silence c. Using clichés d. Defending a situation e. Using open-ended questions Chapter 05: Pain Assessment and Management in Children MULTIPLE CHOICE 1. Which is the most consistent and commonly used data for assessment of pain in infants? a. Self-report b. Behavioral c. Physiologic d. Parental report 2. Children as young as age 3 years can use facial scales for discrimination. What are some suggested anchor words for the preschool age group? a. “No hurt.” b. “Red pain.” c. “Zero hurt.” d. “Least pain.” 3. What is an important consideration when using the FACES pain rating scale with children? a. Children color the face with the color they choose to best describe their pain. b. The scale can be used with most children as young as 3 years. c. The scale is not appropriate for use with adolescents. d. The FACES scale is useful in pain assessment but is not as accurate as physiologic responses. 4. What describes nonpharmacologic techniques for pain management? a. They may reduce pain perception. b. They usually take too long to implement. c. They make pharmacologic strategies unnecessary. d. They trick children into believing they do not have pain. 5. Which nonpharmacologic intervention appears to be effective in decreasing neonatal procedural pain? a. Tactile stimulation b. Commercial warm packs c. Doing procedure during infant sleep d. Oral sucrose and nonnutritive sucking 6. A 6-year-old child has patient-controlled analgesia (PCA) for pain management after orthopedic surgery. The parents are worried that their child will be in pain. What should your explanation to the parents include? a. The child will continue to sleep and be pain free. b. Parents cannot administer additional medication with the button. c. The pump can deliver baseline and bolus dosages. d. There is a high risk of overdose, so monitoring is done every 15 minutes. 7. Which drug is usually the best choice for patient-controlled analgesia (PCA) for a child in the immediate postoperative period? a. Codeine sulfate (Codeine) b. Morphine (Roxanol) c. Methadone (Dolophine) d. Meperidine (Demerol) 8. A child is in the intensive care unit after a motor vehicle collision. The child has numerous fractures and is in pain that is rated 9 or 10 on a 10-point scale. In planning care, the nurse recognizes that the indicated action is which? a. Give only an opioid analgesic at this time. b. Increase dosage of analgesic until the child is adequately sedated. c. Plan a preventive schedule of pain medication around the clock. d. Give the child a clock and explain when she or he can have pain medications. 9. The parents of a preterm infant in a neonatal intensive care unit are concerned about their infant experiencing pain from so many procedures. The nurse’s response should be based on which characteristic about preterm infants’ pain? a. They may react to painful stimuli but are unable to remember the pain experience. b. They perceive and react to pain in much the same manner as children and adults. c. They do not have the cortical and subcortical centers that are needed for pain perception. d. They lack neurochemical systems associated with pain transmission and modulation. 10. A preterm infant has just been admitted to the neonatal intensive care unit. The infant’s parents ask the nurse about anesthesia and analgesia when painful procedures are necessary. What should the nurse’s explanation be? a. Nerve pathways of neonates are not sufficiently myelinated to transmit painful stimuli. b. The risks accompanying anesthesia and analgesia are too great to justify any possible benefit of pain relief. c. Neonates do not possess sufficiently integrated cortical function to interpret or recall pain experiences. d. Pain pathways and neurochemical systems associated with pain transmission are intact and functional in neonates. 11. A bone marrow aspiration and biopsy are needed on a school-age child. The most appropriate action to provide analgesia during the procedure is which? a. Administer TAC (tetracaine, adrenalin, and cocaine) 15 minutes before the procedure. b. Use a combination of fentanyl and midazolam for conscious sedation. c. Apply EMLA (eutectic mixture of local anesthetics) 1 hour before the procedure. d. Apply a transdermal fentanyl (Duragesic) “patch” immediately before the procedure. 12. What is a significant common side effect that occurs with opioid administration? a. Euphoria b. Diuresis c. Constipation d. Allergic reactions 13. The nurse is caring for a child receiving a continuous intravenous (IV) low-dose infusion of morphine for severe postoperative pain. The nurse observes a slower respiratory rate, and the child cannot be aroused. The most appropriate management of this child is for the nurse to do which first? a. Administer naloxone (Narcan). b. Discontinue the IV infusion. c. Discontinue morphine until the child is fully awake. d. Stimulate the child by calling his or her name, shaking gently, and asking the child to breathe deeply. 14. The nurse is teaching a staff development program about levels of sedation in the pediatric population. Which statement by one of the participants should indicate a correct understanding of the teaching? a. “With minimal sedation, the patient’s respiratory efforts are affected, and cognitive function is not impaired.” b. “With general anesthesia, the patient’s airway cannot be maintained, but cardiovascular function is maintained.” c. “During deep sedation, the patient can be easily aroused by loud verbal commands and tactile stimulation.” d. “During moderate sedation, the patient responds to verbal commands but may not respond to light tactile stimulation.” 15. The nurse is planning to administer a nonopioid for pain relief to a child. Which timing should the nurse plan so the nonopioid takes effect? a. 15 minutes until maximum effect b. 30 minutes until maximum effect c. 1 hour until maximum effect d. 1 1/2 hours until maximum effect 16. The nurse is planning pain control for a child. Which is the advantage of administering pain medication by the intravenous (IV) bolus route? a. Less expensive than oral medications b. Produces a first-pass effect through the liver c. Does not need to be administered frequently d. Provides most rapid onset of effect, usually in about 5 minutes 17. The nurse is teaching the parents of a child with recurrent headaches methods to modify behavior patterns that increase the risk of headache. Which statement by the parents indicates understanding the teaching? a. “We will allow the child to miss school if a headache occurs.” b. “We will respond matter-of-factly to requests for special attention.” c. “We will be sure to give much attention to our child when a headache occurs.” d. “We will be sure our child doesn’t have to perform at a band concert if a headache occurs.” 18. Which is a complication that can occur after abdominal surgery if pain is not managed? a. Atelectasis b. Hypoglycemia c. Decrease in heart rate d. Increase in cardiac output 19. A burn patient is experiencing anxiety over dressing changes. Which prescription should the nurse expect to be ordered to control anxiety? a. Lorazepam (Ativan) b. Oxycodone (OxyContin) c. Fentanyl (Sublimaze) d. Morphine Sulfate (Morphine) 20. A cancer patient is experiencing neuropathic cancer pain. Which prescription should the nurse expect to be ordered to control anxiety? a. Lorazepam (Ativan) b. Gabapentin (Neurontin) c. Hydromorphone (Dilaudid) d. Morphine sulfate (MS Contin) MULTIPLE RESPONSE 1. Which are components of the FLACC scale? (Select all that apply.) a. Color b. Capillary refill time c. Leg position d. Facial expression e. Activity Facial expression, consolability, cry, activity, and leg position are components of the FLACC scale. Color is a component of the Apgar scoring system. Capillary refill time is a physiologic measure that is not a component of the FLACC scale. 2. The nurse is using the CRIES pain assessment tool on a preterm infant in the neonatal intensive care unit. Which are the components of this tool? (Select all that apply.) a. Color b. Moro reflex c. Oxygen saturation d. Posture of arms and legs e. Sleeplessness f. Facial expression Need for increased oxygen, crying, increased vital signs, expression, and sleeplessness are components of the CRIES pain assessment tool used with neonates. Color, Moro reflex, and posture of arms and legs are not components of the CRIES scale. 3. Which coanalgesics should the nurse expect to be prescribed for pruritus? (Select all that apply.) a. Naloxone (Narcan) b. Inapsine (Droperidol) c. Hydroxyzine (Atarax) d. Promethazine (Phenergan) e. Diphenhydramine (Benadryl) The coanalgesics prescribed for pruritus include naloxone, hydroxyzine, and diphenhydramine. Inapsine and promethazine are administered as antiemetics. 4. A child receiving chemotherapy is experiencing mucositis. Which prescriptions should the nurse plan to administer for initial treatment? (Select all that apply.) a. Scope mouth rinse b. Listerine antiseptic mouth rinse c. Carafate suspension (Sucralfate) d. Nystatin oral suspension (Nystatin) e. Lidocaine viscous (Lidocaine hydrochloride solution) Initial treatment of stomatitis includes single agents (sucralfate suspension, nystatin, and viscous lidocaine). Scope and Listerine are plaque and gingivitis control mouth rinses that would have a drying effect and are not used with mucositis. COMPLETION 1. A health care provider prescribes promethazine (Phenergan), 9 mg IV every 6 to 8 hours as needed for pruritus. The medication label states: “Promethazine 25 mg/1 mL.” The nurse prepares to administer one dose. How many milliliters will the nurse prepare to administer one dose? Fill in the blank. Record your answer using two decimal places. ________________ 2. A health care provider prescribes diphenhydramine (Benadryl), 1 mg/kg PO every 4 to 6 hours as needed for pruritus. The child weighs 10 kg. The medication label states: “Diphenhydramine 12.5 mg/5 mL.” The nurse prepares to administer one dose. How many milliliters will the nurse prepare to administer one dose? Fill in the blank. Record your answer in a whole number. ________________ 12.5 mg 3. A health care provider prescribes hydroxyzine (Atarax), 0.6 mg/kg PO every 4 to 6 hours as needed for pruritus. The medication label states: “Hydroxyzine 10 mg/5 mL.” The child weighs 20 kg. The nurse prepares to administer one dose. How many milliliters will the nurse prepare to administer one dose? Fill in the blank. Record your answer in a whole number. ________________ Follow the formula for dosage calculation. 4. A child receiving morphine sulfate (Morphine) is experiencing respiratory depression. A health care provider prescribes naloxone (Narcan), 0.5 mcg/kg IV in 2-minute increments until breathing improves. The medication label states: “Naloxone 400 mcg/1 mL.” The child weighs 40 kg. The nurse prepares to administer one dose. How many milliliters will the nurse prepare to administer one dose? Fill in the blank. Record your answer using two decimal places. ________________ 5. A health care provider prescribes haloperidol (Haldol), 0.15 mg/kg IV every 4 to 6 hours as needed for confusion. The medication label states: “Haloperidol 2 mg/1 mL.” The child weighs 30 kg. The nurse prepares to administer one dose. How many milliliters will the nurse prepare to administer one dose? Fill in the blank. Record your answer rounding to one decimal place. ________________ 6. A health care provider prescribes Kytril (granisetron), 10 mcg/kg IV every 4 to 6 hours as needed for nausea. The medication label states: “Kytril 100 mcg/1 mL.” The child weighs 15 kg. The nurse prepares to administer one dose. How many milliliters will the nurse prepare to administer one dose? Fill in the blank. Record your answer to one decimal place. _______________ 7. A health care provider prescribes OxyContin (oxycodone), 3 mg PO every 4 to 6 hours as needed for pain. The medication label states: “OxyContin 5 mg/1 mL.” The nurse prepares to administer one dose. How many milliliters will the nurse prepare to administer one dose? Fill in the blank. Record your answer using one decimal place. ________________ 8. A health care provider prescribes acetaminophen (Tylenol) gtt, 10 mg/kg/dose PO every 4 to 6 hours as needed for pain. The infant weighs 8 kg. The medication label states: “Acetaminophen 80 mg/0.8 mL.” The nurse prepares to administer one dose. How many milliliters will the nurse prepare to administer one dose? Fill in the blank. Record your answer to one decimal place. ________________ 9. A health care provider prescribes naproxen (Naprosyn), 7 mg/kg PO every 12 hours for pain. The child weighs 25 kg. The medication label states: “Naproxen 125 mg/5 mL.” The nurse prepares to administer one dose. How many milliliters will the nurse prepare to administer one dose? Fill in the blank. Record your answer in a whole number. ________________ 10. A health care provider prescribes choline magnesium trisalicylate (Trilisate), 15 mg/kg PO every 8 to 12 hours as needed for pain. The child weighs 10 kg. The medication label states: “Choline magnesium trisalicylate 500 mg/5 mL.” The nurse prepares to administer one dose. How many milliliters will the nurse prepare to administer one dose? Fill in the blank. Record your answer to one decimal place. ________________ 11. A health care provider prescribes ibuprofen (Motrin), 5 mg/kg PO every 6 to 8 hours as needed for pain. The child weighs 8 kg. The medication label states: “Ibuprofen 100 mg/5 mL.” The nurse prepares to administer one dose. How many milliliters will the nurse prepare to administer one dose? Fill in the blank. Record your answer in a whole number. ________________ MATCHING Complementary and alternative medicine therapies are grouped into five classes. Match the complementary or alternative therapy to its classification. a. Vitamins b. Massage c. Reiki d. Hypnosis e. Homeopathy Chapter 06: Childhood Communicable and Infectious Diseases MULTIPLE CHOICE 1. Pertussis vaccination should begin at which age? a. Birth b. 2 months c. 6 months d. 12 months 2. A mother tells the nurse that she does not want her infant immunized because of the discomfort associated with injections. What should the nurse explain? a. This cannot be prevented. b. Infants do not feel pain as adults do. c. This is not a good reason for refusing immunizations. d. A topical anesthetic can be applied before injections are given. 3. A 4-month-old infant comes to the clinic for a well-infant checkup. Immunizations she should receive are DTaP (diphtheria, tetanus, acellular pertussis) and IPV (inactivated poliovirus vaccine). She is recovering from a cold but is otherwise healthy and afebrile. Her older sister has cancer and is receiving chemotherapy. Nursing considerations should include which? a. DTaP and IPV can be safely given. b. DTaP and IPV are contraindicated because she has a cold. c. IPV is contraindicated because her sister is immunocompromised. d. DTaP and IPV are contraindicated because her sister is immunocompromised. 4. Which serious reaction should the nurse be alert for when administering vaccines? a. Fever b. Skin irritation c. Allergic reaction d. Pain at injection site 5. Which muscle is contraindicated for the administration of immunizations in infants and young children? a. Deltoid b. Dorsogluteal c. Ventrogluteal d. Anterolateral thigh 6. Which is described as an elevated, circumscribed skin lesion that is less than 1 cm in diameter and filled with serous fluid? a. Cyst b. Papule c. Pustule d. Vesicle 7. Which vitamin supplementation has been found to reduce both morbidity and mortality in measles? a. A b. B1 c. C d. Zinc 8. What does impetigo ordinarily results in? a. No scarring b. Pigmented spots c. Atrophic white scars d. Slightly depressed scars 9. What often causes cellulitis? a. Herpes zoster b. Candida albicans c. Human papillomavirus d. Streptococci or staphylococci 10. Lymphangitis (streaking) is frequently seen in what? a. Cellulitis b. Folliculitis c. Impetigo contagiosa d. Staphylococcal scalded skin 11. What is most important in the management of cellulitis? a. Burow solution compresses b. Oral or parenteral antibiotics c. Topical application of an antibiotic d. Incision and drainage of severe lesions 12. What causes warts? a. A virus b. A fungus c. A parasite d. Bacteria 13. What is the primary treatment for warts? a. Vaccination b. Local destruction c. Corticosteroids d. Specific antibiotic therapy 14. Herpes zoster is caused by the varicella virus and has an affinity for which? a. Sympathetic nerve fibers b. Parasympathetic nerve fibers c. Lateral and dorsal columns of the spinal cord d. Posterior root ganglia and posterior horn of the spinal cord 15. Treatment for herpes simplex virus (type 1 or 2) includes which? a. Corticosteroids b. Oral griseofulvin c. Oral antiviral agent d. Topical or systemic antibiotic 16. What should the nurse explain about ringworm? a. It is not contagious. b. It is a sign of uncleanliness. c. It is expected to resolve spontaneously. d. It is spread by both direct and indirect contact. 17. When giving instructions to a parent whose child has scabies, what should the nurse include? a. Treat all family members if symptoms develop. b. Be prepared for symptoms to last 2 to 3 weeks. c. Carefully treat only areas where there is a rash. d. Notify practitioner so an antibiotic can be prescribed. 18. Which is usually the only symptom of pediculosis capitis (head lice)? a. Itching b. Vesicles c. Scalp rash d. Localized inflammatory response 19. The school reviewed the pediculosis capitis (head lice) policy and removed the “no nit” requirement. The nurse explains that now, when a child is found to have nits, the parents must do which before the child can return to school? a. No treatment is necessary with the policy change. b. Shampoo and then trim the child’s hair to prevent reinfestation. c. The child can remain in school with treatment done at home. d. Treat the child with a shampoo to treat lice and comb with a fine-tooth comb every day until nits are eliminated. 20. The nurse should know what about Lyme disease? a. Very difficult to prevent b. Easily treated with oral antibiotics in stages 1, 2, and 3 c. Caused by a spirochete that enters the skin through a tick bite d. Common in geographic areas where the soil contains the mycotic spores that cause the disease 21. The nurse is teaching a nursing student about standard precautions. Which statement made by the student indicates a need for further teaching? a. “I will use precautions when I give an infant oral care.” b. “I will use precautions when I change an infant’s diaper.” c. “I will use precautions when I come in contact with blood and body fluids.” d. “I will use precautions when administering oral medications to a school-age child.” 22. The nurse is preparing an airborne infection isolation room for a patient. Which communicable disease does the patient likely have? a. Varicella b. Pertussis c. Influenza d. Scarlet fever 23. An infant with respiratory syncytial virus (RSV) is being admitted to the hospital. The nurse should plan to place the infant on which precaution? a. Enteric b. Airborne c. Droplet d. Contact 24. The nurse is administering the first hepatitis A vaccine to an 18-month-old child. When should the child return to the clinic for the second dose of hepatitis A vaccination? a. After 2 months b. After 3 months c. After 4 months d. After 6 months 25. The nurse is preparing to administer a measles, mumps, rubella, and varicella (MMRV) vaccine. Which is a contraindication associated with administering this vaccine? a. The child has recently been exposed to an infectious disease. b. The child has symptoms of a cold but no fever. c. The child is having intermittent episodes of diarrhea. d. The child has a disorder that causes a deficient immune system. 26. An immunocompromised child has been exposed to chickenpox. What should the nurse anticipate to be prescribed to the exposed child? a. Acyclovir (Zovirax) b. Valacyclovir (Valtrex) c. Amantadine (Symmetrel) d. Varicella-zoster immune globulin 27. The clinic nurse is instructing parents about caring for a toddler with ascariasis (common roundworm). Which statement made by the parents indicates a need for further teaching? a. “We will wash our hands often, especially after diaper changes.” b. “We know that roundworm can be transmitted from person to person.” c. “We will be sure to continue the nitazoxanide (Alinia) orally for 3 days.” d. “We will bring a stool sample to the clinic for examination in 2 weeks.” 28. The nurse is assessing a child suspected of having pinworms. Which is the most common symptom the nurse expects to assess? a. Restlessness b. Distractibility c. Rectal discharge d. Intense perianal itching 29. A child has been diagnosed with giardiasis. Which prescribed medication should the nurse expect to administer? a. Acyclovir (Zovirax) b. Metronidazole (Flagyl) c. Erythromycin (Pediazole) d. Azithromycin (Zithromax) 30. A child has been diagnosed with scabies. Which statement by the parent indicates understanding of the nurse’s teaching about scabies? a. “The itching will stop after the cream is applied.” b. “We will complete extensive aggressive housecleaning.” c. “We will apply the cream to only the affected areas as directed.” d. “Everyone who has been in close contact with my child will need to be treated.” 31. An 18-month-old child has been diagnosed with pediculosis capitis (head lice). Which prescription should the nurse question if ordered for the child? a. Malathion (Ovide) b. Permethrin 1% (Nix) c. Benzyl alcohol 5% lotion d. Pyrethrin with piperonyl butoxide (RID) 32. A child has been diagnosed with cat scratch disease. The nurse explains which characteristics about this disease? a. “The disease is usually a benign, self-limiting illness.” b. “The animal that transmitted the disease will also be ill.” c. “The disease is treated with a 5-day course of oral azithromycin.” d. “Symptoms include pruritus, especially at the site of inoculation.” MULTIPLE RESPONSE 1. The nurse is planning care for a child with chickenpox (varicella). Which prescribed supportive measures should the nurse plan to implement? (Select all that apply.) a. Administration of acyclovir (Zovirax) b. Administration of azithromycin (Zithromax) c. Administration of Vitamin A supplementation d. Administration of acetaminophen (Tylenol) for fever e. Administration of diphenhydramine (Benadryl) for itching 2. The nurse is planning care for an infant with candidiasis (moniliasis) diaper dermatitis. Which topical ointments may be prescribed for the patient? (Select all that apply.) a. Nystatin b. Bactroban c. Neosporin d. Miconazole e. Clotrimazole 3. The nurse is conducting discharge teaching to an adolescent with a methicillin-resistant staphylococcus aureus (MRSA) infection. What should the nurse include in the instructions? (Select all that apply.) a. Avoid sharing of towels and washcloths. b. Launder clothes and bedding in cold water. c. Use bleach when laundering towels and washcloths. d. Take a daily bath or shower with an antibacterial soap. e. Apply mupirocin (Bactroban) to the nares twice a day for 2 to 4 weeks. 4. The clinic nurse is reviewing the immunization guidelines for hepatitis B. Which are true of the guidelines for this vaccine? (Select all that apply.) a. The hepatitis B vaccination series should be begun at birth. b. The adolescent not vaccinated at birth does not have a need to be vaccinated. c. Any child not vaccinated at birth should receive two doses at least 4 months apart. d. An unimmunized 10-year-old child should receive three doses administered 4 weeks apart. 5. The nurse is planning to administer immunizations to a 6-month-old infant. Which interventions should the nurse implement to minimize local reactions from the vaccines? (Select all that apply.) a. Select a needle length of 1 inch. b. Administer in the deltoid muscle. c. Inject the vaccine into the vastus lateralis. d. Draw the vaccine up from a vial with a filter needle. e. Change the needle on the syringe after drawing up the vaccine and before injecting. 6. The nurse is preparing to admit a 5-year-old child who developed lesions of varicella (chickenpox) 3 days ago. Which clinical manifestations of varicella should the nurse expect to observe? (Select all that apply.) a. Nonpruritic rash b. Elevated temperature c. Discrete rose pink rash d. Vesicles surrounded by an erythematous base e. Centripetal rash in all three stages (papule, vesicle, and crust) 7. The nurse is preparing to admit a 1-year-old child with pertussis (whooping cough). Which clinical manifestations of pertussis should the nurse expect to observe? (Select all that apply.) a. Earache b. Coryza c. Conjunctivitis d. Low-grade fever e. Dry hacking cough 8. The nurse is preparing to admit a 2-year-old child with rubella (German measles). Which clinical manifestations of rubella should the nurse expect to observe? (Select all that apply.) a. Sore throat b. Conjunctivitis c. Koplik spots d. Lymphadenopathy e. Discrete, pinkish red maculopapular exanthema 9. The clinic nurse is assessing a child with bacterial conjunctivitis (pink eye). Which assessment findings should the nurse expect? (Select all that apply.) a. Itching b. Swollen eyelids c. Inflamed conjunctiva d. Purulent eye drainage e. Crusting of eyelids in the morning 10. The clinic nurse is assessing a child with a heavy ascariasis lumbricoides (common roundworm) infection. Which assessment findings should the nurse expect? (Select all that apply.) a. Anemia b. Anorexia c. Irritability d. Intestinal colic e. Enlarged abdomen MATCHING Match the key immunization terms to their meanings. a. Natural immunity b. Acquired immunity c. Active immunity d. Passive immunity e. Herd immunity Chapter 23: Pediatric Nursing Interventions and Skills MULTIPLE CHOICE 1. A 16-year-old girl comes to the pediatric clinic for information on birth control. The nurse knows that before this young woman can be examined, consent must be obtained from which source? a. Herself b. Her mother c. Court order d. Legal guardian 2. The nurse needs to take the blood pressure of a preschool boy for the first time. What action would be best in gaining his cooperation? a. Tell him that this procedure will help him get well faster. b. Take his blood pressure when a parent is there to comfort him. c. Explain to him how the blood flows through the arm and why the blood pressure is important. d. Permit him to handle the equipment and see the cuff inflate and deflate before putting the cuff in place. 3. A 4-year-old girl is admitted to outpatient surgery for removal of a cyst on her back. Her mother puts the hospital gown on her, but the child is crying because she wants to leave on her underpants. What is the most appropriate nursing action at this time?? a. Allow her to wear her underpants. b. Discuss with her mother why this is important to the child. c. Ask her mother to explain to her why she cannot wear them. d. Explain in a kind, matter-of-fact manner that this is hospital policy. 4. Using knowledge of child development, what approach is best when preparing a toddler for a procedure? a. Avoid asking the child to make choices. b. Plan for a teaching session to last about 20 minutes. c. Demonstrate on a doll how the procedure will be done. d. Show the necessary equipment without allowing child to handle it. 5. The nurse is preparing a 9-year-old boy before obtaining a blood specimen by venipuncture. The child tells the nurse he does not want to lose his blood. What approach is best by the nurse? a. Explain that it will not be painful. b. Suggest to him that he not worry about losing just a little bit of blood. c. Discuss with him how his body is always in the process of making blood. d. Tell the child that he will not even need a Band-Aid afterward because it is a simple procedure. 6. A bone marrow biopsy will be performed on a 7-year-old girl. She wants her mother to hold her during the procedure. How should the nurse respond? a. Holding your child is unsafe. b. Holding may help your child relax. c. Hospital policy prohibits this interaction. d. Holding your child is unnecessary given the child’s age. 7. A 6-year-old child needs to drink 1 L of GoLYTELY in preparation for a computed tomography scan of the abdomen. To encourage the child to drink, what should the nurse do? a. Give him a large cup with ice so it tastes better. b. Restrict him to his room until he drinks the GoLYTELY. c. Use little cups and make a game to reward him for each cup he drinks. d. Tell him that if he does not finish drinking by a set time, the practitioner will be angry. 8. A toddler is being sent to the operating room for surgery at 9 AM. As the nurse prepares the child, what is the priority intervention? a. Administering preoperative antibiotic b. Verifying that the child and procedure are correct c. Ensuring that the toddler has been NPO since midnight d. Informing the parents where they can wait during the procedure 9. A 5-year-old child returns from the pediatric intensive care unit after abdominal surgery. The orders state to monitor vital signs every 2 hours. On assessment, the nurse observes that the child’s heart rate is 20 beats/min less than it was preoperatively. What should be the nurse’s next action? a. Follow the orders and check in 2 hours. b. Ask the parents if this is the child’s usual heart rate. c. Recheck the pulse and blood pressure in 15 minutes. d. Notify the surgeon that the child is probably going into shock. 10. A 10-year-old child requires daily medications for a chronic illness. Her mother tells the nurse that the child continually forgets to take the medicine unless reminded. What nursing action is most appropriate to promote adherence to the medication regimen? a. Establish a contract with her, including rewards. b. Suggest time-outs when she forgets her medicine. c. Discuss with her mother the damaging effects of her rescuing the child. d. Ask the child to bring her medicine containers to each appointment so they can be counted. 11. A 7-year-old is identified as being at risk for skin breakdown. What intervention should the nursing care plan include? a. Massaging reddened bony prominences b. Teaching the parents to turn the child every 4 hours c. Ensuring that nutritional intake meets requirements d. Minimizing use of extra linens, which can irritate the child’s skin 12. A 6-year-old boy is hospitalized for intravenous antibiotic therapy. He eats very little on his “regular diet” trays. He tells the nurse that all he wants to eat is pizza, tacos, and ice cream. What nursing action is the most appropriate? a. Request these favorite foods for him. b. Identify healthier food choices that he likes. c. Explain that he needs fruits and vegetables. d. Reward him with ice cream at the end of every meal that he eats. 13. A 14-year-old adolescent is hospitalized with cystic fibrosis. What nursing note entry represents best documentation of his breakfast meal? a. Tolerated breakfast well b. Finished all of breakfast ordered c. One pancake, eggs, and 240 ml OJ d. No documentation is needed for this age child. 14. A child, age 7 years, has a fever associated with a viral illness. She is being cared for at home. What is the principal reason for treating fever in this child? a. Relief of discomfort b. Reassurance that illness is temporary c. Prevention of secondary bacterial infection d. Avoidance of life-threatening complications 15. A critically ill child has hyperthermia. The parents ask the nurse to give an antipyretic such as acetaminophen. How should the nurse respond to the parents? a. Febrile seizures can result. b. Antipyretics may cause malignant hyperthermia. c. Antipyretics are of no value in treating hyperthermia. d. Liver damage may occur in critically ill children. 16. The nurse gives an injection in a patient’s room. How should the nurse dispose of the needle? a. Remove the needle from the syringe and dispose of it in a proper container. b. Dispose of the syringe and needle in a rigid, puncture-resistant container in the patient’s room. c. Close the safety cover on the needle and return it to the medication preparation area for proper disposal. d. Place the syringe and needle in a rigid, puncture-resistant container in an area outside of the patient’s room. 17. A child who has cystic fibrosis is admitted to the pediatric unit with methicillin-resistant Staphylococcus aureus (MRSA) infection. The nurse recognizes that in addition to a private room, the child is placed on what precautions? a. Droplet b. Contact c. Airborne d. Standard 18. An 11-month-old hospitalized boy is restrained because he is receiving intravenous (IV) fluids. His grandmother has come to stay with him for the afternoon and asks the nurse if the restraints can be removed. What nurse’s response is best? a. “Restraints need to be kept on all the time.” b. “That is fine as long as you are with him.” c. “That is fine if we have his parents’ consent.” d. “The restraints can be off only when the nursing staff is present.” 19. A nurse must do a venipuncture on a 6-year-old child. What consideration is important in providing atraumatic care? a. Use an 18-gauge needle if possible. b. Show the child the equipment to be used before the procedure. c. If not successful after four attempts, have another nurse try. d. Restrain the child completely. 20. A 2-year-old child is being admitted to the hospital for possible bacterial meningitis. When preparing for a lumbar puncture, what should the nurse do? a. Set up a tray with equipment the same size as for adults. b. Apply EMLA to the puncture site 15 minutes before the procedure. c. Prepare the child for conscious sedation being used for the procedure. d. Reassure the parents that the test is simple, painless, and risk free. 21. Frequent urine tests for specific gravity are required on a 6-month-old infant. What method is the most appropriate way to collect small amounts of urine for these tests? a. Apply a urine collection bag to the perineal area. b. Tape a small medicine cup inside of the diaper. c. Aspirate urine from cotton balls inside the diaper with a syringe without a needle. d. Use a syringe without a needle to aspirate urine from a superabsorbent disposable diaper. 22. A child has a central venous access device for intravenous (IV) fluid administration. A blood sample is needed for a complete blood count, hemogram, and electrolytes. What is the appropriate procedure to implement for this blood sample? a. Perform a new venipuncture to obtain the blood sample. b. Interrupt the IV fluid and withdraw the blood sample needed. c. Withdraw a blood sample equal to the amount of fluid in the device, discard, and then withdraw the sample needed. d. Flush the line and central venous device with saline and then aspirate the required amount of blood for the sample. 23. The nurse has just collected blood by venipuncture in the antecubital fossa. What should the nurse do next? a. Keep the child’s arm extended while applying a Band-Aid to the site. b. Keep the child’s arm extended and apply pressure to the site for a few minutes. c. Apply a Band-Aid to the site and keep the arm flexed for 10 minutes. d. Apply a gauze pad or cotton ball to the site and keep the arm flexed for several minutes. 24. An appropriate method for administering oral medications that are bitter to an infant or small child should be to mix them with which? a. Bottle of formula or milk b. Any food the child is going to eat c. One teaspoon of something sweet-tasting such as jam d. Carbonated beverage, which is then poured over crushed ice 25. The practitioner has ordered a liquid oral antibiotic for a toddler with otitis media. The prescription reads 1 1/2 tsp four times per day. What should the nurse consider in teaching the mother how to give the medicine? a. A measuring spoon should be used, and the medication must be given every 6 hours. b. The mother is not able to handle this regimen. Long-acting intramuscular antibiotics should be administered. c. A hollow-handled medication spoon is advisable, and the medication should be equally spaced while the child is awake. d. A household teaspoon should be used and the medicine given when the child wakes up, around lunch time, at dinner time, and before bed. 26. Guidelines for intramuscular administration of medication in school-age children include what standard? a. Inject medication as rapidly as possible. b. Insert needle quickly, using a dartlike motion. c. Have the child stand if at all possible and if the child is cooperative. d. Penetrate the skin immediately after cleansing the site while the skin is moist. 27. What is an advantage of the ventrogluteal muscle as an injection site in young children? a. Easily accessible from many directions b. Free of significant nerves and vascular structures c. Can be used until child reaches a weight of 9 kg (20 lb) d. Increased subcutaneous fat, which provides sustained drug absorption 28. When teaching a mother how to administer eye drops, where should the nurse tell her to place them? a. At the lacrimal duct b. On the sclera while the child looks to the outside c. In the conjunctival sac when the lower eyelid is pulled down d. Carefully under the eyelid while it is gently pulled upward 29. What is the best method to verify the placement of a nasogastric tube before each use? a. Radiologic confirmation b. Auscultation of injected air c. Aspiration of stomach contents d. Verification of tape placement on tube 30. Parents are being taught how to feed their infant using a newly placed gastrostomy tube (G-tube). What is essential information for the parents to receive? a. Verify placement before each feeding. b. Use a syringe with a plunger to give the infant bolus feedings. c. Position the infant on the right side during and after the feeding. d. Beefy red tissue around the G-tube site must be reported to the practitioner. . 31. What is a priority intervention for an infant with a temporary colostomy for Hirschsprung disease? a. Teaching how to irrigate the colostomy b. Protecting the skin around the colostomy c. Discussing the implications of a colostomy during puberty d. Using simple, straightforward language to prepare the child 32. A 1-month-old infant is admitted to the hospital. The infant’s mother is 17 years old and single and lives with her parents. Who signs the informed consent for the 1-month-old infant? a. The infant’s mother b. The maternal grandparents of the infant c. The paternal grandparents of the infant d. Both the infant’s mother and the maternal grandparents 33. A preschool child needs a dressing change. To prepare the child, what strategy should the nurse implement? a. Explain the procedure using medical terminology. b. Plan a 30-minute teaching session. c. Give choices when possible but avoid delay. d. Allow time after the procedure for questions and discussion. 34. The nurse on a pediatric unit is writing guidelines for age-specific preparation of children for procedures based on developmental characteristics. What guideline is accurate? a. Inform toddlers about an upcoming procedure 2 hours before the procedure is to be performed. b. Inform school-age children about an upcoming procedure immediately before the procedure is scheduled to occur. c. Discourage parent presence during procedures on infants and toddlers. d. Use simple diagrams of anatomy and physiology to explain a procedure to a school-age child. 35. A laboratory technician is performing a blood draw on a toddler. The toddler is holding still but crying loudly. The nurse should take which action? a. Have the lab technician stop the procedure until the child stops crying. b. Do nothing. It’s Okay for a child to cry during a painful procedure. c. Tell the child to stop crying; it’s only a small prick. d. Tell the child to stop crying because the procedure is almost over. 36. At which age should a nurse keep teaching time short (5 minutes)? a. Infant b. Toddler c. Preschool d. School age 37. The nurse is preparing to give acetaminophen (Tylenol) to a child who has a fever. What nursing action is appropriate? a. Retake the temperature in 15 minutes after giving the Tylenol. b. Place a warm blanket on the child so chilling does not occur. c. Check to be sure the Tylenol dose does not exceed 15 mg/kg. d. Use cold compresses instead of Tylenol to control the fever. 38. The nurse is administering an IM injection into a vastus lateralis muscle of a 6-month-old infant. What should the length of the needle and amount to be given be? a. 5/8 to 1 inch; 0.5 to 1.0 ml b. 1 inch to 1 1/2 inch; 1.0 to 2.0 ml c. 1 inch to 1 1/2 inch; 0.5 to 1.0 ml d. 5/8 to 1 inch; 0.75 to 2 ml 39. The nurse needs to start an intravenous (IV) line on an 8-year-old child to begin administering intravenous antibiotics. The child starts to cry and tells the nurse, “Do it later, okay?” What action should the nurse take? a. Postpone starting the IV until the next shift. b. Start the IV line and then allow for expression of feelings. c. Change the route of the antibiotics to PO. d. Postpone starting the IV line until the child is ready. 40. The nurse is preparing to administer a liquid medication by a nasogastric feeding tube. What is the first thing the nurse should do? a. Check placement of the tube. b. Check the pH of the gastric aspirate. c. Flush the tube with a small amount of water. d. Give the medication and then flush with a small amount of water. 41. To facilitate the administration of an oral medication to a preschool-age child, what action should the nurse take? a. Dilute the medication in a large amount of favorite liquid and allow the child to hold the cup. b. Set limits about the need to take medication and offer praise immediately after the task is accomplished. c. Mix the medication in a moderate amount of the child’s favorite food. d. Explain the purpose of the medication and allow the child time to express resistance before giving the medication. 42. A 2-year-old child has to receive Rocephin IM injections every 12 hours. What nursing intervention should be implemented for the child? a. Hold the child while rocking in a chair after each injection. b. Prepare the child several hours before the injection is given. c. Allow the child to watch a younger child receive an injection. d. Encourage the child to draw a picture of the pain experienced when an injection is given. 43. When checking the intravenous (IV) site on a child, the nurse should take which action? a. Look at the site. b. Ask the child if the site “hurts.” c. Look at the site while palpating the area. d. Take all the tape off, assess the site, and redress. MULTIPLE RESPONSE 1. The nurse is caring for a 12-year-old child who is on fall precautions secondary to seizures. What interventions should be included in the child’s care plan? (Select all that apply.) a. Place a call light and desired items within reach. b. Keep the bed in the highest position with the two side rails up. c. Turn off the lights and television at night. d. Keep personal belongings and clutter contained in one area of the floor. e. Have the child wear an appropriate-size gown and nonskid footwear. 2. What methods should the nurse use to measure compliance to a treatment plan? (Select all that apply.) a. Pill counts b. Chemical assays c. Direct observation d. Third-party reporting e. Monitoring therapeutic response 3. What interventions should the nurse implement to prevent a pressure ulcer in a critically ill child? (Select all that apply.) a. Nutrition consults b. Using skin moisturizers c. Turning the child every 2 hours d. Using plastic disposable underpads e. Using draw sheets to minimize shear 4. The nurse is preparing to obtain a nasal washing from a child. What equipment should the nurse gather for the procedure? (Select all that apply.) a. Sterile water b. A sterile swab c. Syringe with tubing d. Sterile normal saline e. Tracheal suction catheter 5. The clinic nurse is teaching parents about when to call the office immediately for a child with a fever. What should the nurse include in the teaching session? (Select all that apply.) a. The child has a stiff neck. b. The fever is over 40.6° C (105° F). c. The child is younger than 2 months. d. The fever has lasted for more than 3 days. e. The fever went away for more than 24 hours and then returned. 6. What strategies should the nurse implement to assist in feeding a sick child? (Select all that apply.) a. Serve large portions. b. Make mealtimes pleasant. c. Avoid foods that are highly seasoned. d. Provide finger foods for young children. e. Ensure a variety of foods, textures, and colors. 7. What disease processes require contact isolation? (Select all that apply.) a. Rotavirus b. Hepatitis A c. Streptococcal pharyngitis d. Mycoplasmal pneumonia e. Respiratory syncytial virus 8. What disease processes require airborne precautions? (Select all that apply.) a. Measles b. Varicella c. Pertussis d. Meningitis e. Tuberculosis 9. What are the advantages of an implanted port (Port-a-Cath)? (Select all that apply.) a. Reduced risk of infection b. Reduced cost for the family c. Placed completely under the skin d. Easy to use for self-administered infusions e. Removal does not require a surgical procedure 10. What play activities should the nurse implement to encourage fluid intake for a child? (Select all that apply.) a. Have a tea party. b. Use a crazy straw. c. Cut gelatin into fun shapes. d. Place liquid in large Styrofoam cups. e. Make ice pops using the child’s favorite juice. Chapter 27: Overview of Oxygen and Carbon Dioxide Exchange MULTIPLE CHOICE 1. What respiratory condition or disease results in both increased compliance and increased resistance? a. Asthma b. Atelectasis c. Surfactant deficiency d. Bronchopulmonary dysplasia 2. How much oxygen is contained in ambient air (room air)? a. 15% b. 21% c. 30% d. 42% 3. During a respiratory assessment, the nurse notes a sinking in of soft tissues relative to the cartilaginous and bony thorax. What is the term for this finding? a. Grunting b. Tachypnea c. Retractions d. Nasal flaring . 4. What test measures the amount of air inhaled and exhaled during any respiratory cycle? a. Tidal volume b. Vital capacity c. Dynamic compliance d. Pulmonary resistance 5. What is the best explanation for using pulse oximetry on young children to determine oxygen saturation? a. Pulse oximetry is noninvasive. b. Pulse oximetry is better than capnography. c. Pulse oximetry is more accurate than arterial blood gases. d. Pulse oximetry provides intermittent measurements of oxygen. 6. It is important to make certain that sensory connectors and oximeters are compatible because incompatible wiring can cause which condition? a. Hyperthermia b. Electrocution c. Pressure necrosis d. Burns under sensors 7. What test should the nurse do as a precautionary measure before doing an arterial puncture to obtain an arterial blood sample? a. Allen test b. Smith test c. Venipuncture d. Cold compress 8. Arterial blood gases have just been drawn on a child. What should the nurse do next? a. Take the sample to the laboratory immediately. b. Pack the sample in ice and take it to the laboratory immediately. c. Place the sample in a brown bag until it can be taken to laboratory. d. Refrigerate the sample until it can be taken to the laboratory. 9. The continuous administration of mist, or aerosolized water, for the treatment of inflammatory conditions of the airways is a common practice that functions in which manner? a. Has no proven benefit b. Decreases the viscosity of mucus c. Decreases bronchoconstriction d. Reduces the inflammation of the lower airways 10. When is bronchial (postural) drainage generally performed? a. Before meals and at bedtime b. Right before all aerosol therapy c. Immediately on arising and at bedtime d. Thirty minutes after meals and at bedtime 11. What nursing consideration is most important in the care of a child on a mechanical ventilator? a. Humidification is not necessary. b. Respiratory assessment is done by the ventilator. c. Positioning the child for comfort and optimum ventilation is necessary. d. Support and reassurance are not as important because the child is unconscious. 12. What intervention is necessary when weaning a child from the ventilator? a. Light sedation before scheduled extubation b. No suctioning before scheduled extubation c. Cool mist begun immediately after extubation d. Vigorous chest physiotherapy and suctioning performed immediately after extubation 13. The nurse must suction a 6-month-old infant with a tracheostomy. What intervention should be included? a. Encourage the child to cough to raise the secretions before suctioning. b. Perform each pass of the suction catheter for no longer than 5 seconds. c. Allow the child to rest after every five times the suction catheter is passed. d. Select a catheter with a diameter three quarters of the diameter of the tracheostomy tube. 14. A 3-year-old child with a tracheostomy will soon be discharged. What recommendation should the nurse share with the family? a. Tub baths cannot be given. b. The child cannot be allowed to play outdoors. c. Avoid exposure to noxious fumes such as paint or varnish. d. Cover the tracheostomy with a plastic bib when exposed to cold air. 15. The nurse is planning home care for a 2-year-old child with a tracheostomy. What recommendation should be included? a. Sterile technique is essential in home care of the tracheostomy. b. Parents are able to change the tracheostomy tube when needed. c. Play activities must be sedentary such as listening to music and working on puzzles. d. The child must wear a plastic bib when eating or drinking to prevent aspiration into the stoma. 16. Respiratory failure can result from many causes. What condition is a specific primary cause of inefficient gas transfer? a. Anemia b. Pneumothorax c. Cystic fibrosis d. Laryngospasm 17. The nurse is caring for a child with a tracheostomy. What clinical manifestation should the nurse recognize as an early sign of impending respiratory distress or failure? a. Cyanosis b. Restlessness c. Audible stridor d. Crowing respirations 18. Cardiopulmonary resuscitation is begun on a toddler. What pulse is usually palpated because it is the most central and accessible? a. Radial b. Carotid c. Femoral d. Brachial 19. What medication is considered to be the most useful in treating cardiac arrest? a. Bretylium tosylate (Bretylium) b. Xylocaine (lidocaine) c. Adrenaline (epinephrine) d. Naloxone (Narcan) 20. Effective cardiopulmonary resuscitation (CPR) on a 5-year-old child should include what technique? a. Provide one breath to every five chest compressions. b. Provide two breaths to every 30 chest compressions. c. Reassess the child every 10 minutes while CPR continues. d. Evaluate the child after 50 cycles of compression and ventilation. 21. A series of subdiaphragmatic abdominal thrusts (the Heimlich maneuver) is recommended for airway obstruction in children older than which age? a. 1 year b. 4 years c. 8 years d. 12 years 22. The mother of a toddler yells to the nurse, “Help! He is choking to death on his food!” The nurse determines that lifesaving measures are necessary based on which finding? a. Gagging b. Coughing c. Pulse over 100 beats/min d. Inability to speak 23. The nurse is caring for a 4-year-old child who is receiving 2 L of oxygen per nasal cannula. What disadvantage should the nurse consider when planning care for the child? a. The child may need to have high humidity administered with the oxygen. b. The child may not be able to eat and drink comfortably. c. A nasal cannula may cause an accumulation of moisture on the face. d. A nasal cannula may cause abdominal distention. 24. A 5-month-old infant is in respiratory distress. What should the nurse expect to find? a. Nasal flaring b. Bradycardia c. Abdominal breathing d. Capillary refill of 2 seconds 25. A child is in uncompensated respiratory acidosis. What should the nurse expect the arterial blood gas to be? a. O2, 95; CO2, 45; pH, 7.40 b. O2, 88; CO2, 55; pH, 7.30 c. O2, 88; CO2, 35; pH, 7.28 d. O2, 92; CO2, 54; pH, 7.35 26. A child is in uncompensated respiratory alkalosis. What should the nurse expect the arterial blood gas to be? a. CO2, 30; pH, 7.50 b. CO2, 55; pH, 7.30 c. CO2, 35; pH, 7.28 d. CO2, 54; pH, 7.35 27. A child is in uncompensated metabolic alkalosis. What should the nurse expect the arterial blood gas to be? a. HCO3, 24; pH, 7.35 b. HCO3, 28; pH, 7.50 c. HCO3, 20; pH, –7.30 d. HCO3, 26; pH, 7.40 28. A child is in uncompensated metabolic acidosis. What should the nurse expect the arterial blood gas to be? a. HCO3, 24; pH, 7.35 b. HCO3, 28; pH, 7.50 c. HCO3, 20; pH, 7.30 d. HCO3, 26; pH, 7.40 29. A nurse is calculating the correlation of Pao2 with Sao2 according to the oxyhemoglobin dissociation curve. What parameter should indicate that the Pao2 is less than 50 to 60 mm Hg? a. Coarse lung sounds b. Temperature of 100° F c. Respiratory rate of 58 d. Pulse oximetry reading of 90% or less 30. The nurse is reviewing factors that affect lung development. What factor delays surfactant production and maturation of alveolar cells? a. Thyroxine b. Prolactin c. Glucocorticosteroids d. Excess of endogenous insulin 31. The nurse is caring for a child in respiratory distress. What is an early but less obvious sign of respiratory failure? a. Stupor b. Headache c. Bradycardia d. Somnolence 32. The nurse is caring for a child on oxygen being delivered by a nasal cannula. What is the advantage of delivering oxygen in this manner? a. It can deliver mist if desired. b. It is less likely to cause abdominal distention. c. The child is able to eat and talk while getting oxygen. d. This method can deliver a higher concentration of oxygen. 33. The nurse is evaluating arterial blood gas results. What condition can cause an increase in PCO2? a. Hypoxia b. Hyperventilation c. Pulmonary embolism d. Obstructive lung disease 34. The nurse is evaluating arterial blood gas results. What condition can cause an increase in HCO3? a. Renal failure b. Lactic acidosis c. Diabetic ketoacidosis d. Fluid loss from upper gastrointestinal tract 35. The nurse is analyzing an arterial blood gas of pH, 7.30; PCO2, 50; and HCO3, 29. What result should the nurse document for this blood gas? a. Fully compensated respiratory acidosis b. Partially compensated respiratory acidosis c. Fully compensated metabolic acidosis d. Partially compensated metabolic acidosis 36. The nurse is analyzing an arterial blood gas of pH, 7.50; PCO2, 50; and HCO3, 29. What result should the nurse document for this blood gas? a. Fully compensated metabolic alkalosis b. Partially compensated metabolic alkalosis c. Fully compensated respiratory alkalosis d. Partially compensated respiratory alkalosis 37. The nurse is analyzing an arterial blood gas of pH, 7.29; PCO2, 30; and HCO3, 20. What result should the nurse document for this blood gas? a. Fully compensated respiratory acidosis b. Partially compensated respiratory acidosis c. Fully compensated metabolic acidosis d. Partially compensated metabolic acidosis 38. The nurse is analyzing an arterial blood gas of pH, 7.50; PCO2, 30; and HCO3, 20. What result should the nurse document for this blood gas? a. Fully compensated metabolic alkalosis b. Partially compensated metabolic alkalosis c. Fully compensated respiratory alkalosis d. Partially compensated respiratory alkalosis MULTIPLE RESPONSE 1. What conditions can produce hyperventilation? (Select all that apply.) a. Hysteria b. Narcotics c. Atelectasis d. Salicylate intoxication e. Mechanical ventilation 2. What condition or disease decreases lung compliance? (Select all that apply.) a. Asthma b. Atelectasis c. Pneumothorax d. Pulmonary edema e. Lobar emphysema 3. The nurse is caring for an intubated child on mechanical ventilation. What interventions should the nurse implement to prevent ventilator-assisted pneumonia (VAP)? (Select all that apply.) a. Routine oral hygiene b. Appropriate hand hygiene c. Limit oropharyngeal suctioning of secretions d. Elevating the head of the bed 30 to 45 degrees e. Wearing gloves to handle respiratory secretions 4. The nurse recognizes that oxygen mist tents are rarely used for a child with respiratory distress. What are reasons for not using an oxygen mist tent? (Select all that apply.) a. Poor access to the child b. Cool and wet tent environment c. Oxygen levels fall when tent is entered d. Child may not tolerate it around the crib/bed e. Lower oxygen concentrations cannot be achieved COMPLETION 1. The nurse is participating in a code blue on a 12-year-old child in a full respiratory arrest. The child weighs 110 lb. The health care provider has ordered an initial dose of epinephrine hydrochloride (1:10,000) given intravenously. Calculate the correct initial dose of epinephrine in mg. Record your answer using one decimal place. _____________ 2. The nurse is calculating the amount of expected urinary output for a 24-hour period on an intubated young child who weighs 22 lb. The nurse recognizes the formula to be used is 2 ml/kg/hr. What is the expected 24-hour urinary output for this child in milliliters? Record your answer below in a whole number. _____________ 3. The nurse is calculating the amount of expected urinary output for a 24-hour period on an intubated young child who weighs 33 lb. The nurse recognizes the formula to be used is 2 ml/kg/hr. What is the expected 24-hour urinary output for this child in milliliters? Record your answer below in a whole number. _____________ Chapter 28: The Child with Respiratory Dysfunction MULTIPLE CHOICE 1. Why are cool-mist vaporizers rather than steam vaporizers recommended in the home treatment of respiratory infections? a. They are safer. b. They are less expensive. c. Respiratory secretions are dried by steam vaporizers. d. A more comfortable environment is produced. 2. Decongestant nose drops are recommended for a 10-month-old infant with an upper respiratory tract infection. Instructions for nose drops should include which information? a. Do not use for more than 3 days. b. Keep drops to use again for nasal congestion. c. Administer drops after feedings and at bedtime. d. Give two drops every 5 minutes until nasal congestion subsides. 3. The parent of an infant with nasopharyngitis should be instructed to notify the health professional if the infant shows signs or symptoms of which condition? a. Has a cough b. Becomes fussy c. Shows signs of an earache d. Has a fever higher than 37.5° C (99° F) 4. It is important that a child with acute streptococcal pharyngitis be treated with antibiotics to prevent which condition? a. Otitis media b. Diabetes insipidus (DI) c. Nephrotic syndrome d. Acute rheumatic fever 5. When caring for a child after a tonsillectomy, what intervention should the nurse do? a. Watch for continuous swallowing. b. Encourage gargling to reduce discomfort. c. Apply warm compresses to the throat. d. Position the child on the back for sleeping. 6. What statement best represents infectious mononucleosis? a. Herpes simplex type 2 is the principal cause. b. A complete blood count shows a characteristic leukopenia. c. A short course of ampicillin is used when pharyngitis is present. d. Clinical signs and symptoms and blood tests are both needed to establish the diagnosis. 7. Parents bring their 15-month-old infant to the emergency department at 3:00 AM because the toddler has a temperature of 39° C (102.2° F), is crying inconsolably, and is tugging at the ears. A diagnosis of otitis media (OM) is made. In addition to antibiotic therapy, the nurse practitioner should instruct the parents to use what medication? a. Decongestants to ease stuffy nose b. Antihistamines to help the child sleep c. Aspirin for pain and fever management d. Benzocaine ear drops for topical pain relief 8. An 18-month-old child is seen in the clinic with otitis media (OM). Oral amoxicillin is prescribed. What instructions should be given to the parent? a. Administer all of the prescribed medication. b. Continue medication until all symptoms subside. c. Immediately stop giving medication if hearing loss develops. d. Stop giving medication and come to the clinic if fever is still present in 24 hours. 9. An infant’s parents ask the nurse about preventing otitis media (OM). What information should be provided? a. Avoid tobacco smoke. b. Use nasal decongestants. c. Avoid children with OM. d. Bottle- or breastfeed in a supine position. 10. Chronic otitis media with effusion (OME) differs from acute otitis media (AOM) because it is usually characterized by which signs or symptoms? a. Severe pain in the ear b. Anorexia and vomiting c. A feeling of fullness in the ear d. Fever as high as 40° C (104° F) 11. A 4-year-old girl is brought to the emergency department. She has a “froglike” croaking sound on inspiration, is agitated, and is drooling. She insists on sitting upright. The nurse should intervene in which manner? a. Make her lie down and rest quietly. b. Examine her oral pharynx and report to the physician. c. Auscultate her lungs and prepare for placement in a mist tent. d. Notify the physician immediately and be prepared to assist with a tracheostomy or intubation. 12. The nurse is assessing a child with croup in the emergency department. The child has a sore throat and is drooling. Examining the child’s throat using a tongue depressor might precipitate what condition? a. Sore throat b. Inspiratory stridor c. Complete obstruction d. Respiratory tract infection 13. The mother of a 20-month-old boy tells the nurse that he has a barking cough at night. His temperature is 37° C (98.6° F). The nurse suspects mild croup and should recommend which intervention? a. Admit to the hospital and observe for impending epiglottitis. b. Provide fluids that the child likes and use comfort measures. c. Control fever with acetaminophen and call if cough gets worse tonight. d. Try over-the-counter cough medicine and come to the clinic tomorrow if no improvement. 14. The nurse encourages the mother of a toddler with acute laryngotracheobronchitis to stay at the bedside as much as possible. What is the primary rationale for this action? a. Mothers of hospitalized toddlers often experience guilt. b. The mother’s presence will reduce anxiety and ease the child’s respiratory efforts. c. Separation from the mother is a major developmental threat at this age. d. The mother can provide constant observations of the child’s respiratory efforts. 15. An infant with bronchiolitis is hospitalized. The causative organism is respiratory syncytial virus (RSV). The nurse knows that a child infected with this virus requires what type of isolation? a. Reverse isolation b. Airborne isolation c. Contact Precautions d. Standard Precautions 16. An infant has been diagnosed with staphylococcal pneumonia. Nursing care of the child with pneumonia includes which intervention? a. Administration of antibiotics b. Frequent complete assessment of the infant c. Round-the-clock administration of antitussive agents d. Strict monitoring of intake and output to avoid congestive heart failure 17. What consideration is most important in managing tuberculosis (TB) in children? a. Skin testing b. Chemotherapy c. Adequate rest d. Adequate hydration 18. A toddler has a unilateral foul-smelling nasal discharge and frequent sneezing. The nurse should suspect what condition? a. Allergies b. Acute pharyngitis c. Foreign body in the nose d. Acute nasopharyngitis 19. The nurse is caring for a child with acute respiratory distress syndrome (ARDS) associated with sepsis. What nursing action should be included in the care of the child? a. Force fluids. b. Monitor pulse oximetry. c. Institute seizure precautions. d. Encourage a high-protein diet. 20. The nurse is caring for a child with carbon monoxide (CO) poisoning associated with smoke inhalation. What intervention is essential in this child’s care? a. Monitor pulse oximetry. b. Monitor arterial blood gases. c. Administer oxygen if respiratory distress develops. d. Administer oxygen if child’s lips become bright, cherry-red in color. 21. What diagnostic test for allergies involves the injection of specific allergens? a. Phadiatop b. Skin testing c. Radioallergosorbent tests (RAST) d. Blood examination for total immunoglobulin E (IgE) 22. What statement is the most descriptive of asthma? a. It is inherited. b. There is heightened airway reactivity. c. There is decreased resistance in the airway. d. The single cause of asthma is an allergic hypersensitivity. 23. What condition is the leading cause of chronic illness in children? a. Asthma b. Pertussis c. Tuberculosis d. Cystic fibrosis 24. A child has a chronic cough and diffuse wheezing during the expiratory phase of respiration. This suggests what condition? a. Asthma b. Pneumonia c. Bronchiolitis d. Foreign body in trachea 25. A child with asthma is having pulmonary function tests. What rationale explains the purpose of the peak expiratory flow rate? a. To assess severity of asthma b. To determine cause of asthma c. To identify “triggers” of asthma d. To confirm diagnosis of asthma 26. Children who are taking long-term inhaled steroids should be assessed frequently for what potential complication? a. Cough b. Osteoporosis c. Slowed growth d. Cushing syndrome 27. One of the goals for children with asthma is to maintain the child’s normal functioning. What principle of treatment helps to accomplish this goal? a. Limit participation in sports. b. Reduce underlying inflammation. c. Minimize use of pharmacologic agents. d. Have yearly evaluations by a health care provider. 28. What drug is usually given first in the emergency treatment of an acute, severe asthma episode in a young child? a. Ephedrine b. Theophylline c. Aminophylline d. Short-acting 2-agonists 29. Cystic fibrosis (CF) may affect single or multiple systems of the body. What is the primary factor responsible for possible multiple clinical manifestations in CF? a. Hyperactivity of sweat glands b. Hypoactivity of autonomic nervous system c. Atrophic changes in mucosal wall of intestines d. Mechanical obstruction caused by increased viscosity of mucous gland secretions 30. What is the earliest recognizable clinical manifestation(s) of cystic fibrosis (CF)? a. Meconium ileus b. History of poor intestinal absorption c. Foul-smelling, frothy, greasy stools d. Recurrent pneumonia and lung infections 31. What tests aid in the diagnosis of cystic fibrosis (CF)? a. Sweat test, stool for fat, chest radiography b. Sweat test, bronchoscopy, duodenal fluid analysis c. Sweat test, stool for trypsin, biopsy of intestinal mucosa d. Stool for fat, gastric contents for hydrochloride, radiography . 32. A child with cystic fibrosis (CF) receives aerosolized bronchodilator medication. When should this medication be administered? a. After chest physiotherapy (CPT) b. Before chest physiotherapy (CPT) c. After receiving 100% oxygen d. Before receiving 100% oxygen 33. A child with cystic fibrosis is receiving recombinant human deoxyribonuclease (DNase). What statement about DNase is true? a. Given subcutaneously b. May cause voice alterations c. May cause mucus to thicken d. Not indicated for children younger than age 12 years 34. The parent of a child with cystic fibrosis (CF) calls the clinic nurse to report that the child has developed tachypnea, tachycardia, dyspnea, pallor, and cyanosis. The nurse should tell the parent to bring the child to the clinic because these signs and symptoms are suggestive of what condition? a. Pneumothorax b. Bronchodilation c. Carbon dioxide retention d. Increased viscosity of sputum 35. Pancreatic enzymes are administered to the child with cystic fibrosis. What nursing consideration should be included in the plan of care? a. Give pancreatic enzymes between meals if at all possible. b. Do not administer pancreatic enzymes if the child is receiving antibiotics. c. Decrease the dose of pancreatic enzymes if the child is having frequent, bulky stools. d. Pancreatic enzymes can be swallowed whole or sprinkled on a small amount of food taken at the beginning of a meal. 36. The nurse is giving discharge instructions to the parents of a 5-year-old child who had a tonsillectomy 4 hours ago. What statement by the parent indicates a correct understanding of the teaching? a. “I can use an ice collar on my child for pain control along with analgesics.” b. “My child should clear the throat frequently to clear the secretions.” c. “I should allow my child to be as active as tolerated.” d. “My child should gargle and brush teeth at least three times per day.” 37. A child is admitted with acute laryngotracheobronchitis (LTB). The child will most likely be treated with which? a. Racemic epinephrine and corticosteroids b. Nebulizer treatments and oxygen c. Antibiotics and albuterol d. Chest physiotherapy and humidity 38. A 6-year-old child has had a tonsillectomy. The child is spitting up small amounts of dark brown blood in the immediate postoperative period. The nurse should take what action? a. Notify the health care provider. b. Continue to assess for bleeding. c. Give the child a red flavored ice pop. d. Position the child in a Trendelenburg position. 39. A 3-year-old child is experiencing pain after a tonsillectomy. The child has not taken in any fluids and does not want to drink anything, saying, “My tummy hurts.” The following health care prescriptions are available: acetaminophen (Tylenol) PO (orally) or PR (rectally) PRN, ice chips, clear liquids. What should the nurse implement to relieve the child’s pain? a. Ice chips b. Tylenol PO c. Tylenol PR d. Popsicle 40. A 1-year-old child has acute otitis media (AOM) and is being treated with oral antibiotics. What should the nurse include in the discharge teaching to the infant’s parents? a. A follow-up visit should be done after all medicine has been given. b. After an episode of acute otitis media, hearing loss usually occurs. c. Tylenol should not be given because it may mask symptoms. d. The infant will probably need a myringotomy procedure and tubes. 41. What do the initial signs of respiratory syncytial virus (RSV) infection in an infant include? a. Rhinorrhea, wheezing, and fever b. Tachypnea, cyanosis, and apnea c. Retractions, fever, and listlessness d. Poor breath sounds and air hunger 42. The nurse is caring for a 1-month-old infant with respiratory syncytial virus (RSV) who is receiving 23% oxygen via a plastic hood. The child’s SaO2 saturation is 88%, respiratory rate is 45 breaths/min, and pulse is 140 beats/min. Based on these assessments, what action should the nurse take? a. Withhold feedings. b. Notify the health care provider. c. Put the infant in an infant seat. d. Keep the infant in the plastic hood. 43. A 5-year-old child is admitted with bacterial pneumonia. What signs and symptoms should the nurse expect to assess with this disease process? a. Fever, cough, and chest pain b. Stridor, wheezing, and ear infection c. Nasal discharge, headache, and cough d. Pharyngitis, intermittent fever, and eye infection 44. An infant with a congenital heart defect is to receive a dose of palivizumab (Synagis). What is the purpose of this? a. Prevent RSV infection. b. Prevent secondary bacterial infection. c. Decrease toxicity of antiviral agents. d. Make isolation of infant with RSV unnecessary. 45. A 3-year-old is brought to the emergency department with symptoms of stridor, fever, restlessness, and drooling. No coughing is observed. Based on these findings, the nurse should be prepared to assist with what action? a. Throat culture b. Nasal pharynx washing c. Administration of corticosteroids d. Emergency intubation 46. A 3-year-old child woke up in the middle of the night with a croupy cough and inspiratory stridor. The parents bring the child to the emergency department, but by the time they arrive, the cough is gone, and the stridor has resolved. What can the nurse teach the parents with regard to this type of croup? a. A bath in tepid water can help resolve this type of croup. b. Tylenol can help to relieve the cough and stridor. c. A cool mist vaporizer at the bedside can help prevent this type of croup. d. Antibiotics need to be given to reduce the inflammation. 47. A 3-month-old infant is admitted to the pediatric unit for treatment of bronchiolitis. The infant’s vital signs are T, 101.6° F; P, 106 beats/min apical; and R, 70 breaths/min. The infant is irritable and fussy and coughs frequently. IV fluids are given via a peripheral venipuncture. Fluids by mouth were initially contraindicated for what reason? a. Tachypnea b. Paroxysmal cough c. Irritability d. Fever 48. A child is in the hospital for cystic fibrosis. What health care provider’s prescription should the nurse clarify before implementing? a. Dornase alfa (Pulmozyme) nebulizer treatment bid b. Pancreatic enzymes every 6 hours c. Vitamin A, D, E, and K supplements daily d. Proventil (albuterol) nebulizer treatments tid 49. A 6-year-old child is in the hospital for status asthmaticus. Nursing care during this acute period includes which prescribed interventions? a. Prednisolone (Pediapred) PO every day, IV fluids, cromolyn (Intal) inhaler bid b. Salmeterol (Serevent) PO bid, vital signs every 4 hours, spot check pulse oximetry c. Triamcinolone (Azmacort) inhaler bid, continuous pulse oximetry, vital signs once a shift d. Methylprednisolone (Solumedrol) IV every 12 hours, continuous pulse oximetry, albuterol nebulizer treatments every 4 hours and prn 50. In providing nourishment for a child with cystic fibrosis (CF), what factors should the nurse keep in mind? a. Fats and proteins must be greatly curtailed. b. Most fruits and vegetables are not well tolerated. c. Diet should be high in calories, proteins, and unrestricted fats. d. Diet should be low fat but high in calories and proteins. 51. A quantitative sweat chloride test has been done on an 8-month-old child. What value should be indicative of cystic fibrosis (CF)? a. Less than 18 mEq/L b. 18 to 40 mEq/L c. 40 to 60 mEq/L d. Greater than 60 mEq/L 52. A preschool child has asthma, and a goal is to extend expiratory time and increase expiratory effectiveness. What action should the nurse implement to meet this goal? a. Encourage increased fluid intake. b. Recommend increased use of a budesonide (Pulmicort) inhaler. c. Administer an antitussive to suppress coughing. d. Encourage the child to blow a pinwheel every 6 hours while awake. 53. A school-age child has asthma. The nurse should teach the child that if a peak expiratory flow rate is in the yellow zone, this means that the asthma control is what? a. 80% of a personal best, and the routine treatment plan can be followed. b. 50% to 79% of a personal best and needs an increase in the usual therapy. c. 50 % of a personal best and needs immediate emergency bronchodilators. d. Less than 50% of a personal best and needs immediate hospitalization. . 54. A family requires home care teaching with regard to preventative measures to use at home to avoid an asthmatic episode. What strategy should the nurse teach? a. Use a humidifier in the child’s room. b. Launder bedding daily in cold water. c. Replace wood flooring with carpet. d. Use an indoor air purifier with HEPA filter. 55. A school-age child with cystic fibrosis takes four enzyme capsules with meals. The child is having four or five bowel movements per day. The nurse’s action in regard to the pancreatic enzymes is based on the knowledge that the dosage is what? a. Adequate b. Adequate but should be taken between meals c. Needs to be increased to increase the number of bowel movements per day d. Needs to be increased to decrease the number of bowel movements per day 56. A term infant is delivered, and before delivery, the medical team was notified that a congenital diaphragmatic hernia (CDH) was diagnosed on ultrasonography. What should be done immediately at birth if respiratory distress is noted? a. Give oxygen. b. Suction the infant. c. Intubate the infant. d. Ventilate the infant with a bag and mask. 57. A child has a streptococcal throat infection and is being treated with antibiotics. What should the nurse teach the parents to prevent infection of others? a. The child can return to school immediately. b. The organism cannot be transmitted through contact. c. The child can return to school after taking antibiotics for 24 hours. d. The organism can only be transmitted if someone uses a personal item of the sick child. 58. What medication is contraindicated in children post tonsillectomy and adenoidectomy? a. Codeine b. Ondansetron (Zofran) b. Amoxil (amoxicillin) c. Acetaminophen (Tylenol) MULTIPLE RESPONSE 1. The nurse is preparing a staff education program about pediatric asthma. What concepts should the nurse include when discussing the asthma severity classification system? (Select all that apply.) a. Children with mild persistent asthma have nighttime signs or symptoms less than two times a month. b. Children with moderate persistent asthma use a short-acting -agonist more than two times per week. c. Children with severe persistent asthma have a peak expiratory flow (PEF) of 60% to 80% of predicted value. d. Children with mild persistent asthma have signs or symptoms more than two times per week. e. Children with moderate persistent asthma have some limitations with normal activity. f. Children with severe persistent asthma have frequent nighttime signs or symptoms. 2. The nurse is caring for a newborn with suspected congenital diaphragmatic hernia. What of the following findings would the nurse expect to observe? (Select all that apply.) a. Loud, harsh murmur b. Scaphoid abdomen c. Poor peripheral pulses d. Mediastinal shift e. Inguinal swelling f. Moderate respiratory distress 3. What interventions can the nurse teach parents to do to ease respiratory efforts for a child with a mild respiratory tract infection? (Select all that apply.) a. Cool mist b. Warm mist c. Steam vaporizer d. Keep child in a flat, quiet position e. Run a shower of hot water to produce steam 4. A tonsillectomy or adenoidectomy is contraindicated in what conditions? (Select all that apply.) a. Cleft palate b. Seizure disorders c. Blood dyscrasias d. Sickle cell disease e. Acute infection at the time of surgery 5. The clinic nurse is administering influenza vaccinations. Which children should not receive the live attenuated influenza vaccine (LAIV)? (Select all that apply.) a. A child with asthma b. A child with diabetes c. A child with hemophilia A d. A child with cancer receiving chemotherapy e. A child with gastroesophageal reflux disease 6. The nurse is preparing to admit a 7-year-old child with acute laryngotracheobronchitis (LTB). What clinical manifestations should the nurse expect to observe? (Select all that apply.) a. Dysphagia b. Brassy cough c. Low-grade fever d. Toxic appearance e. Slowly progressive 7. The nurse is preparing to admit a 3-year-old child with acute spasmodic laryngitis. What clinical features of hepatitis B should the nurse recognize? (Select all that apply.) a. High fever b. Croupy cough c. Tendency to recur d. Purulent secretions e. Occurs sudden, often at night 8. A child is diagnosed with active pulmonary tuberculosis. What medications does the nurse anticipate to be prescribed for the first 2 months? (Select all that apply.) a. Isoniazid (INH) b. Cefuroxime (Ceftin) c. Rifampin (Rifadin) d. Pyrazinamide (PZA) e. Ethambutol (Myambutol) 9. The nurse is interpreting a tuberculin skin test. If the nurse finds a result of an induration 5 mm or larger, in which child should the nurse document this finding as positive? (Select all that apply.) a. A child with diabetes mellitus b. A child younger than 4 years of age c. A child receiving immunosuppressive therapy d. A child with a human immunodeficiency virus (HIV) infection e. A child living in close contact with a known contagious case of tuberculosis 10. The nurse is preparing to admit a 7-year-old child with pulmonary edema. What clinical manifestations should the nurse expect to observe? (Select all that apply.) a. Fever b. Bradycardia c. Diaphoresis d. Pink frothy sputum e. Respiratory crackles COMPLETION 1. The nurse is calculating the amount of expected urinary output for a 24-hour period on a child with bacterial pneumonia who weighs 22 lb. The nurse recognizes the formula to be used is 1 ml/kg/hr. What is the expected 24-hour urinary output for this child in milliliters? Record your answer below in a whole number. _____________ 2. The nurse is calculating the amount of expected urinary output for a 24-hour period on a child with laryngotracheobronchitis who weighs 33 lb. The nurse recognizes the formula to be used is 1 ml/kg/hr. What is the expected 24-hour urinary output for this child in milliliters? Record your answer below in a whole number. _____________ 3. The health care provider prescribes ceftazidime (Fortaz) 75 mg per intravenous piggy back (IVPB) every 8 hours for a child with cystic fibrosis. The pharmacy sends the medication to the unit in a 100-ml bag with directions to run the medication over 30 minutes. What milliliters per hour will the nurse set the intravenous pump to run the medication over 30 minutes? Fill in the blank and record your answer in a whole number. _____________ 4. The health care provider prescribes vancomycin 200 mg per intravenous piggy back (IVPB) every 6 hours for a child with cystic fibrosis. The pharmacy sends the medication to the unit in a 150-ml bag with directions to run the medication over 120 minutes. What milliliters per hour will the nurse set the intravenous pump to run the medication over 120 minutes? Fill in the blank and record your answer in a whole number. _____________ [Show More]
Last updated: 1 year ago
Preview 1 out of 141 pages
Instant download
Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Apr 11, 2020
Number of pages
141
Written in
Additional information
This document has been written for:
Uploaded
Apr 11, 2020
Downloads
0
Views
79

.png)
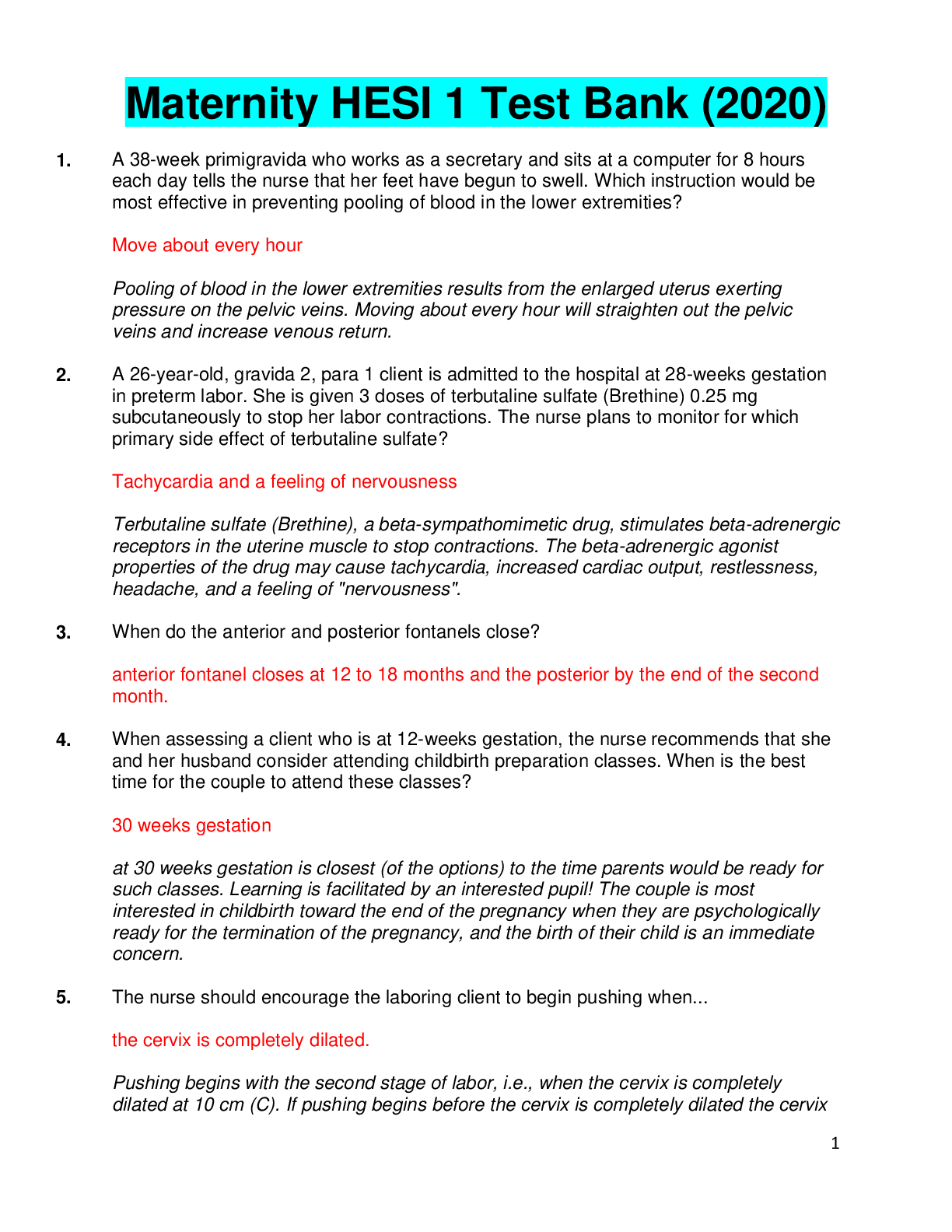
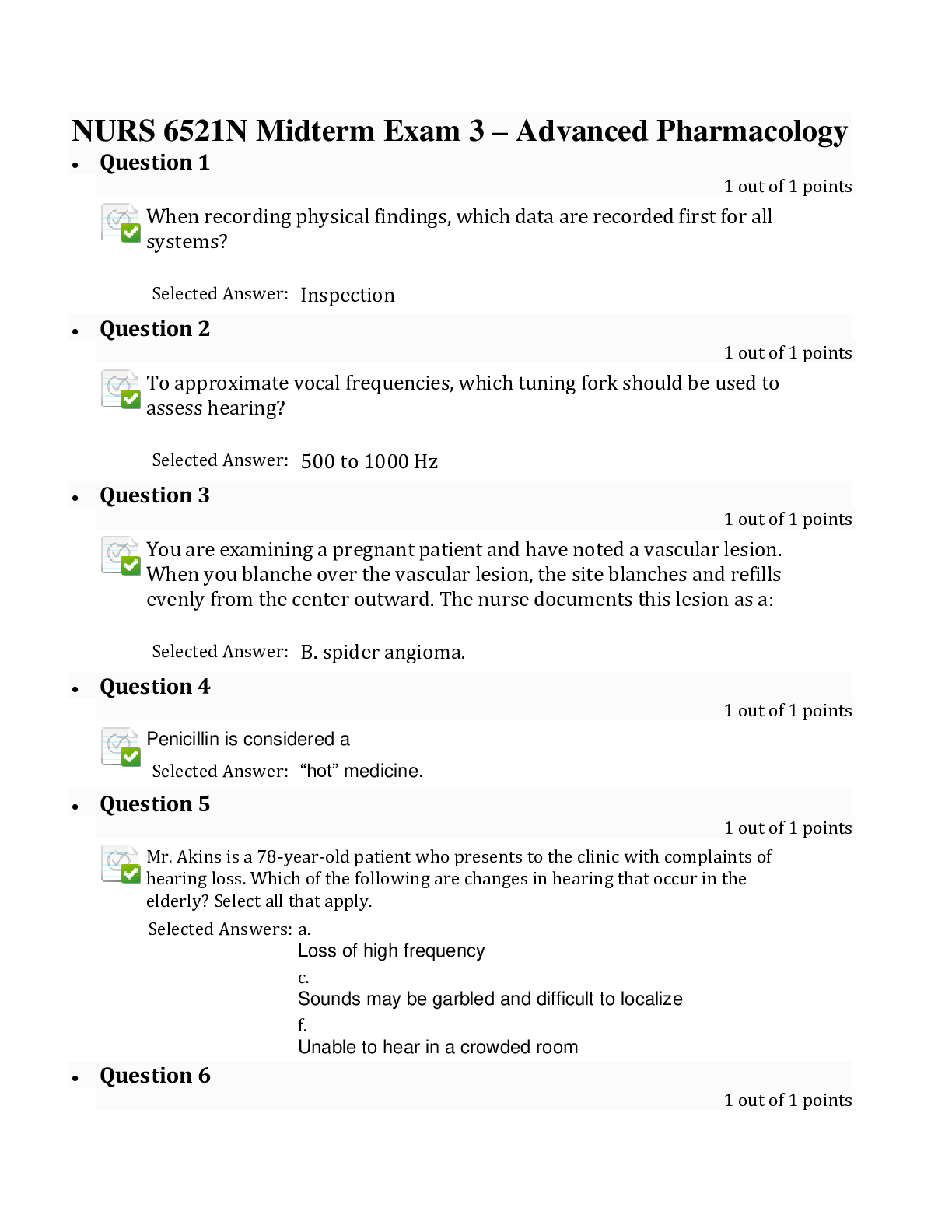
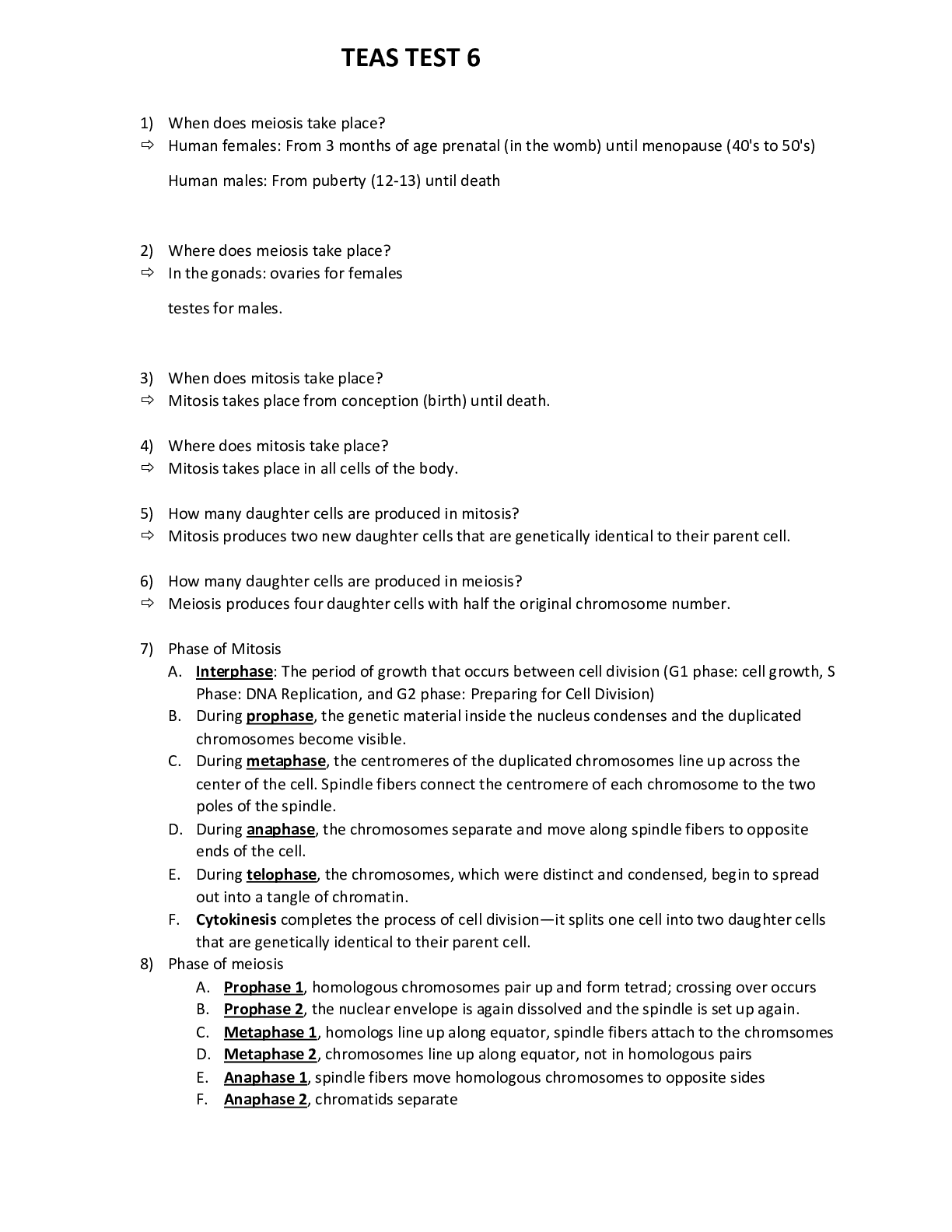
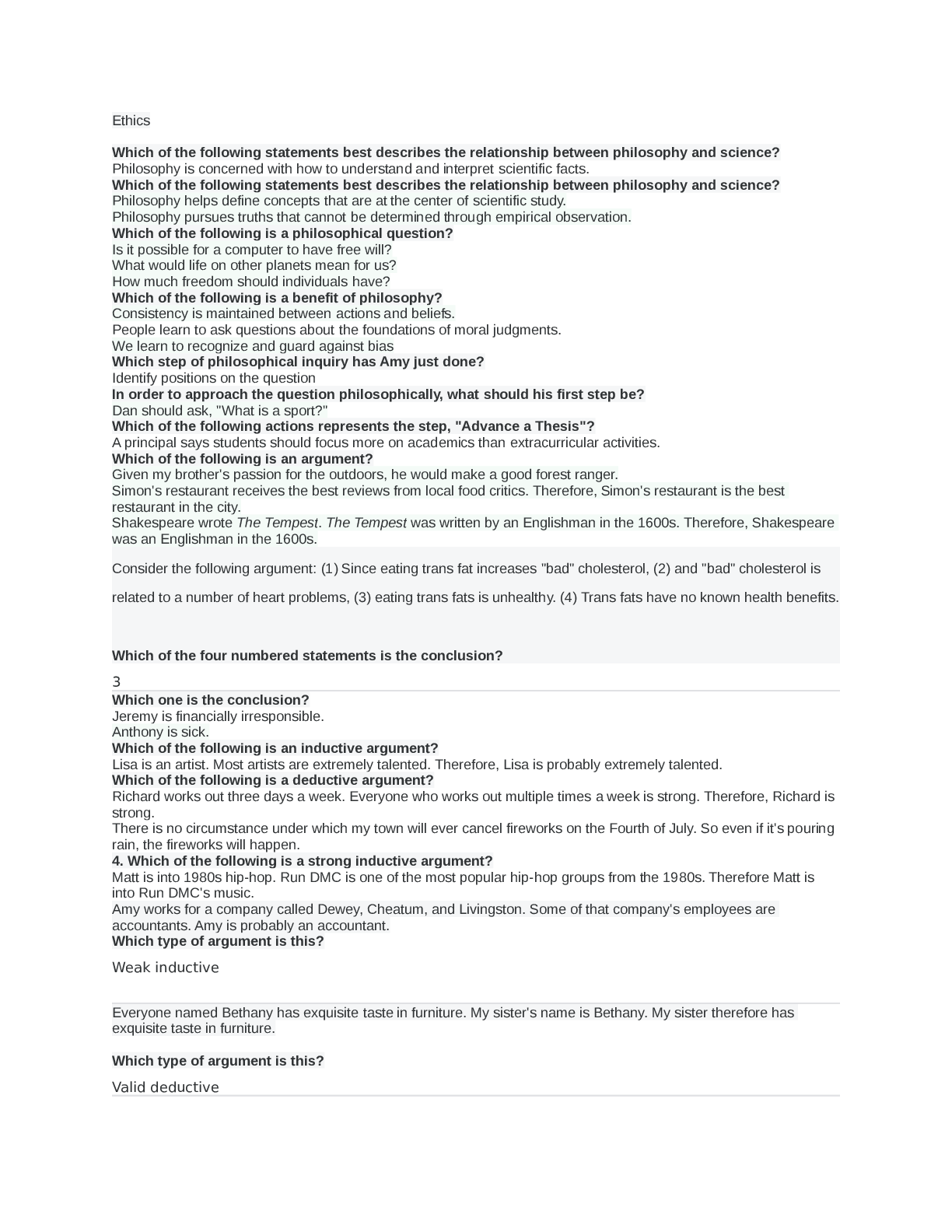

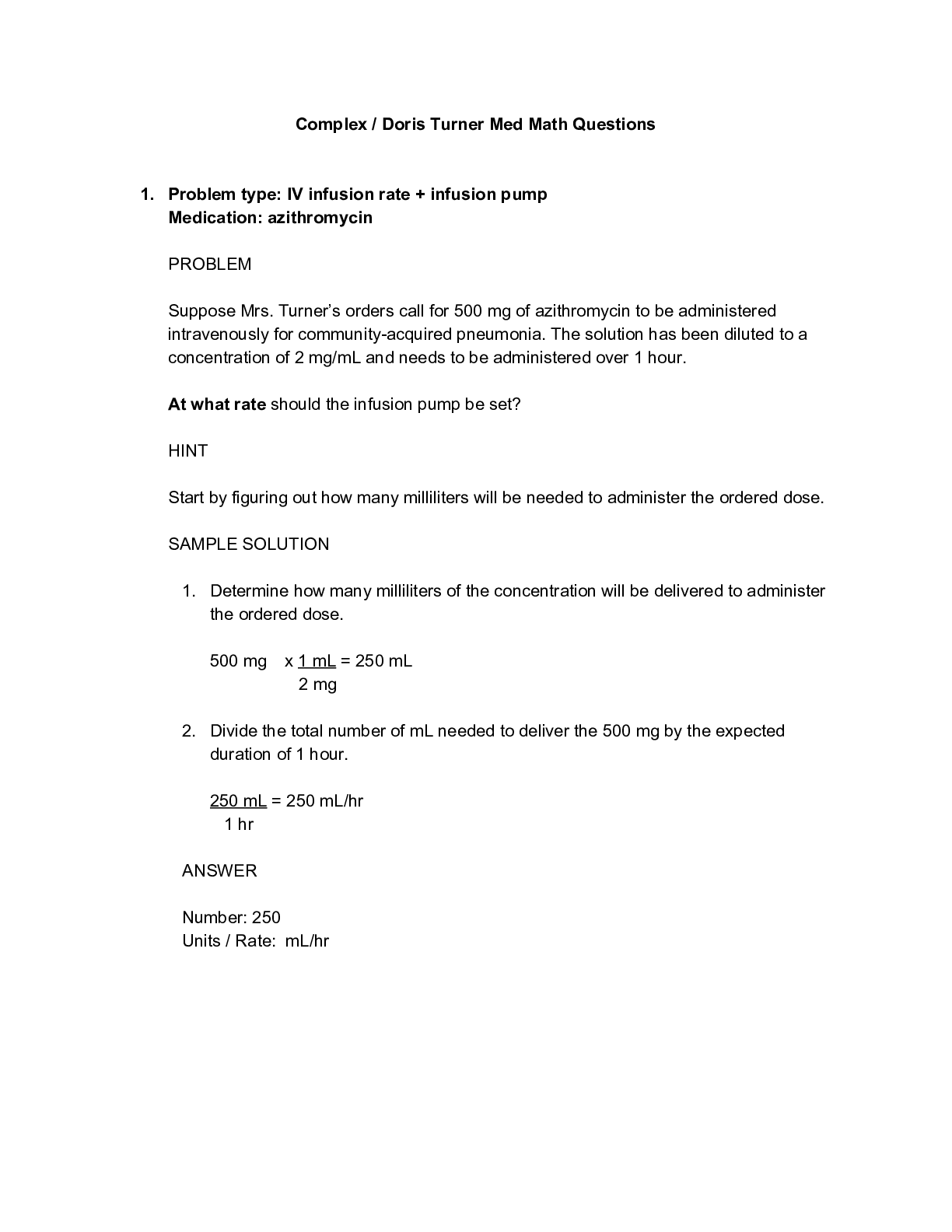
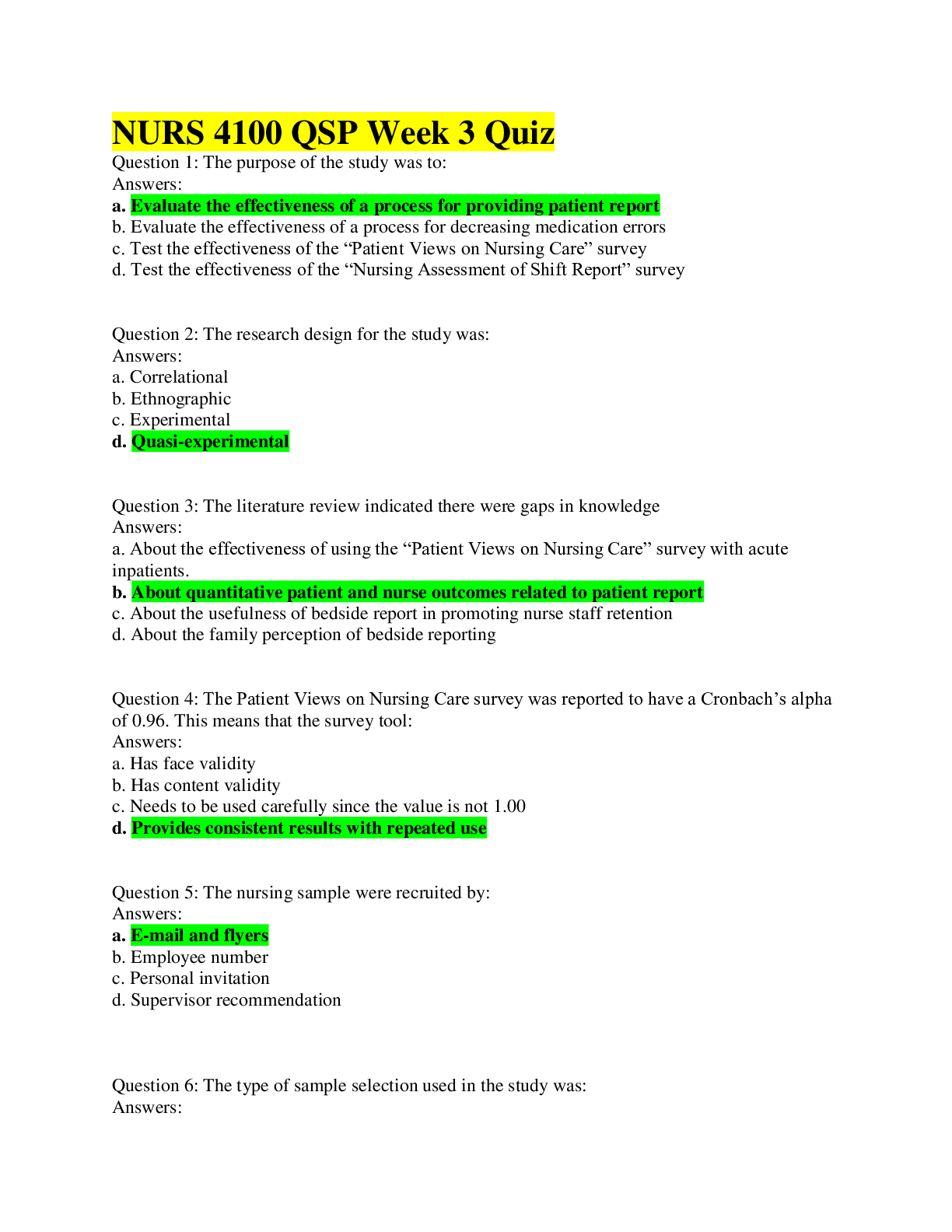
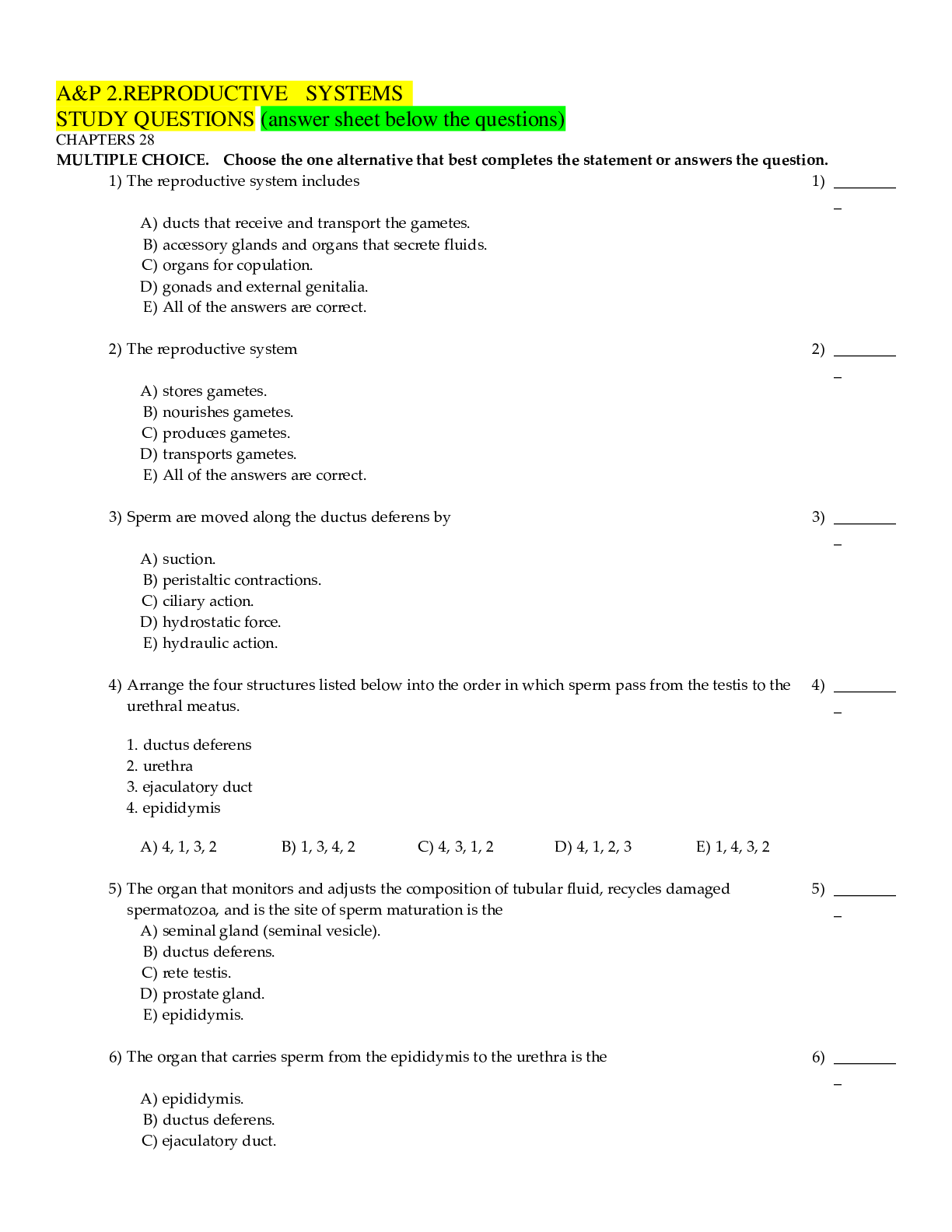
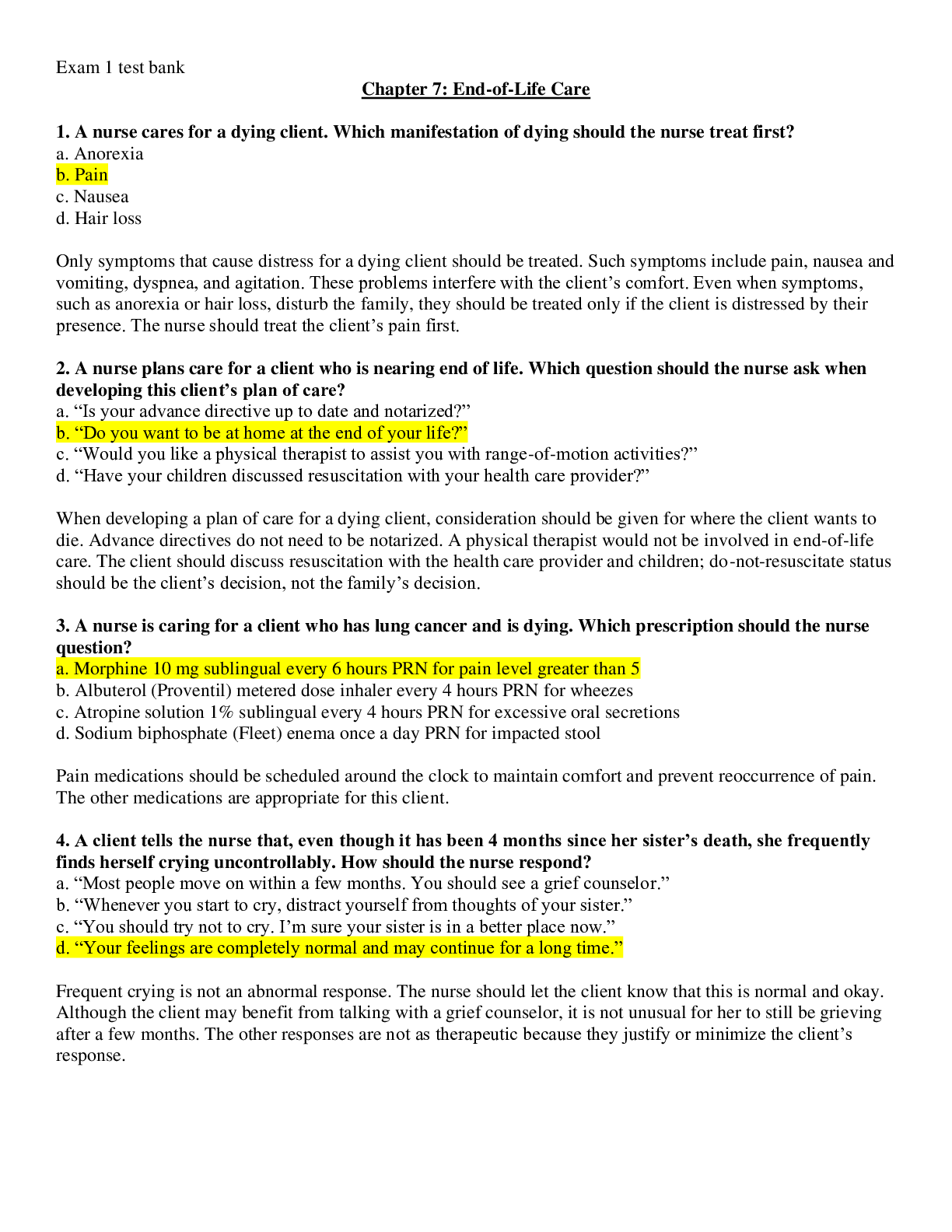
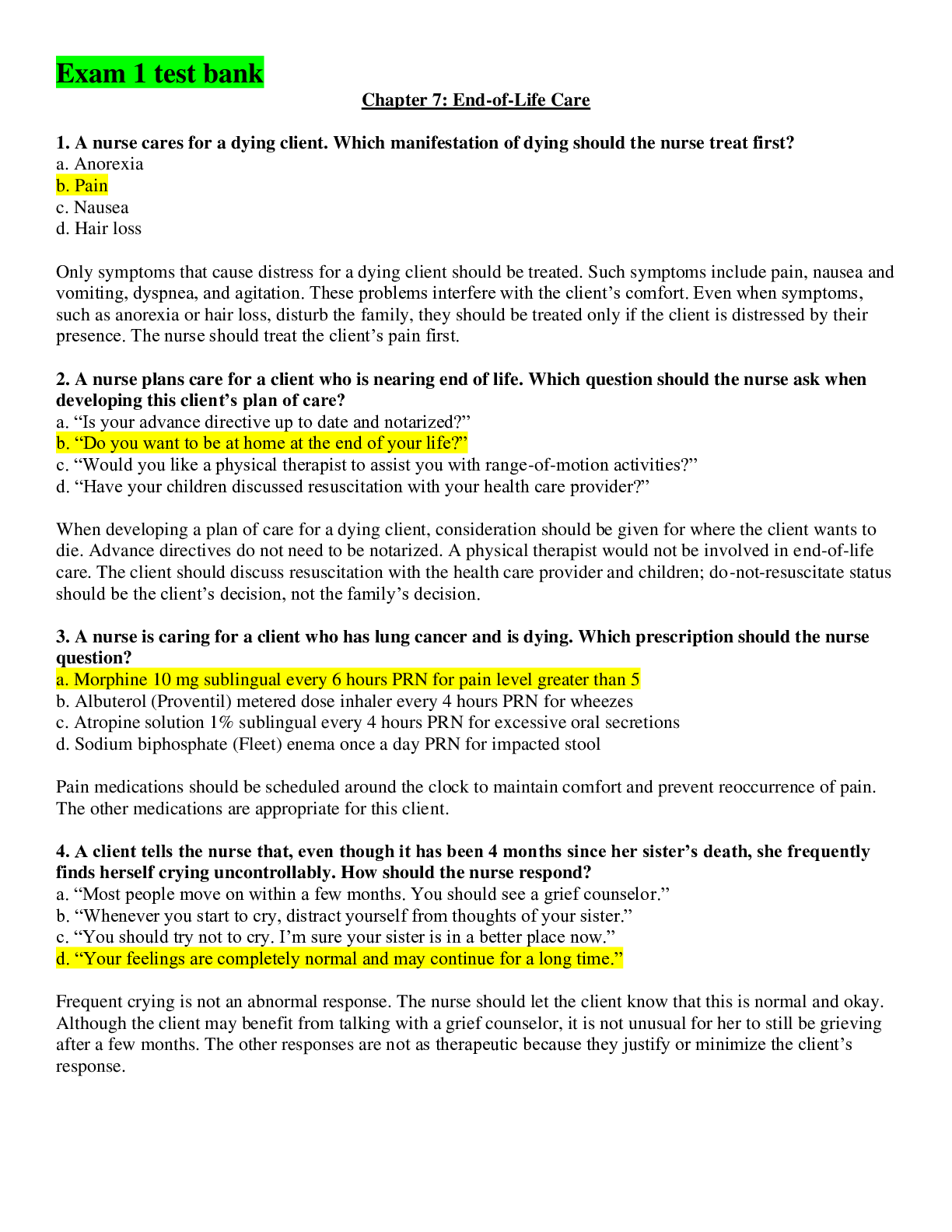
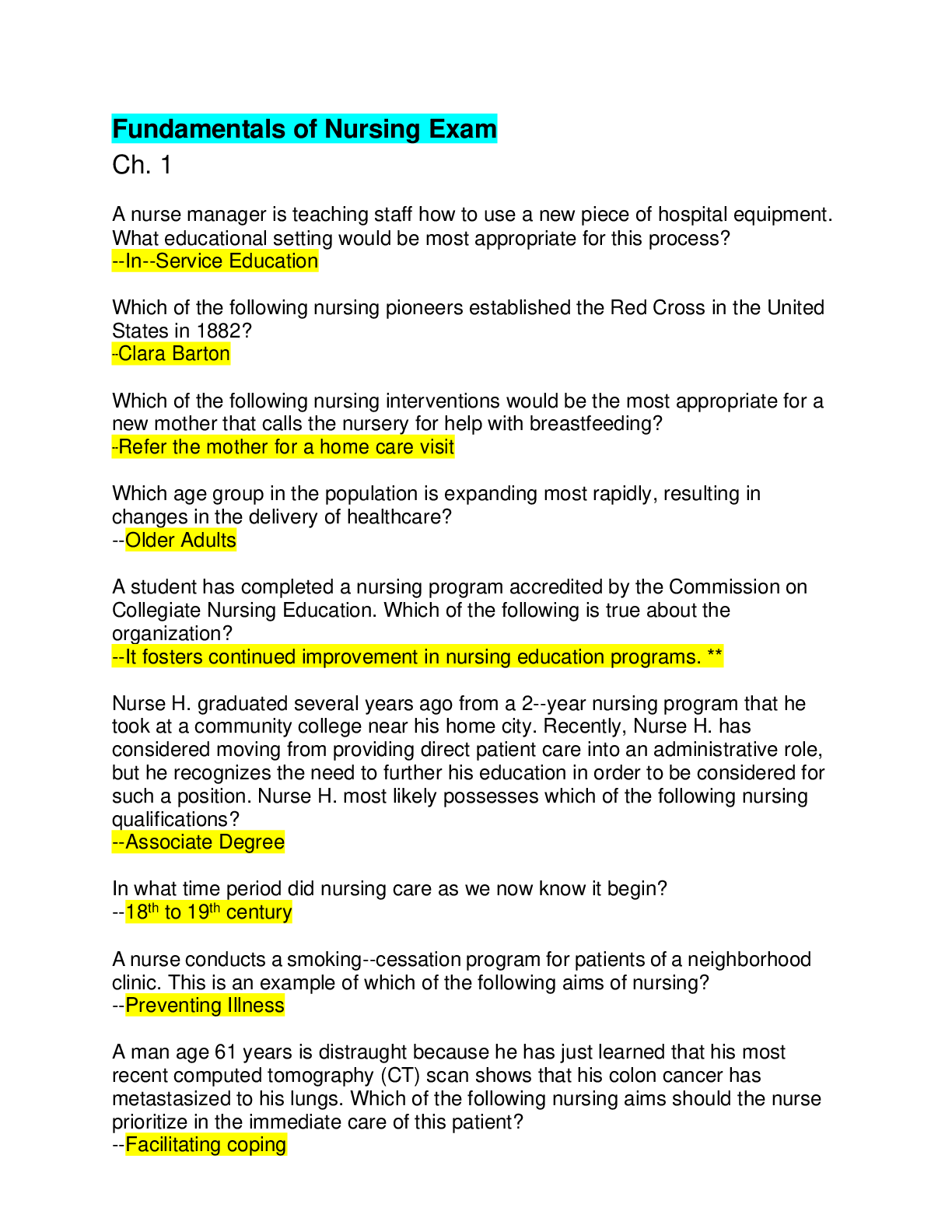
 Questions and Answers (latest Update), 100% Correct, Download to Score A.png)
.png)
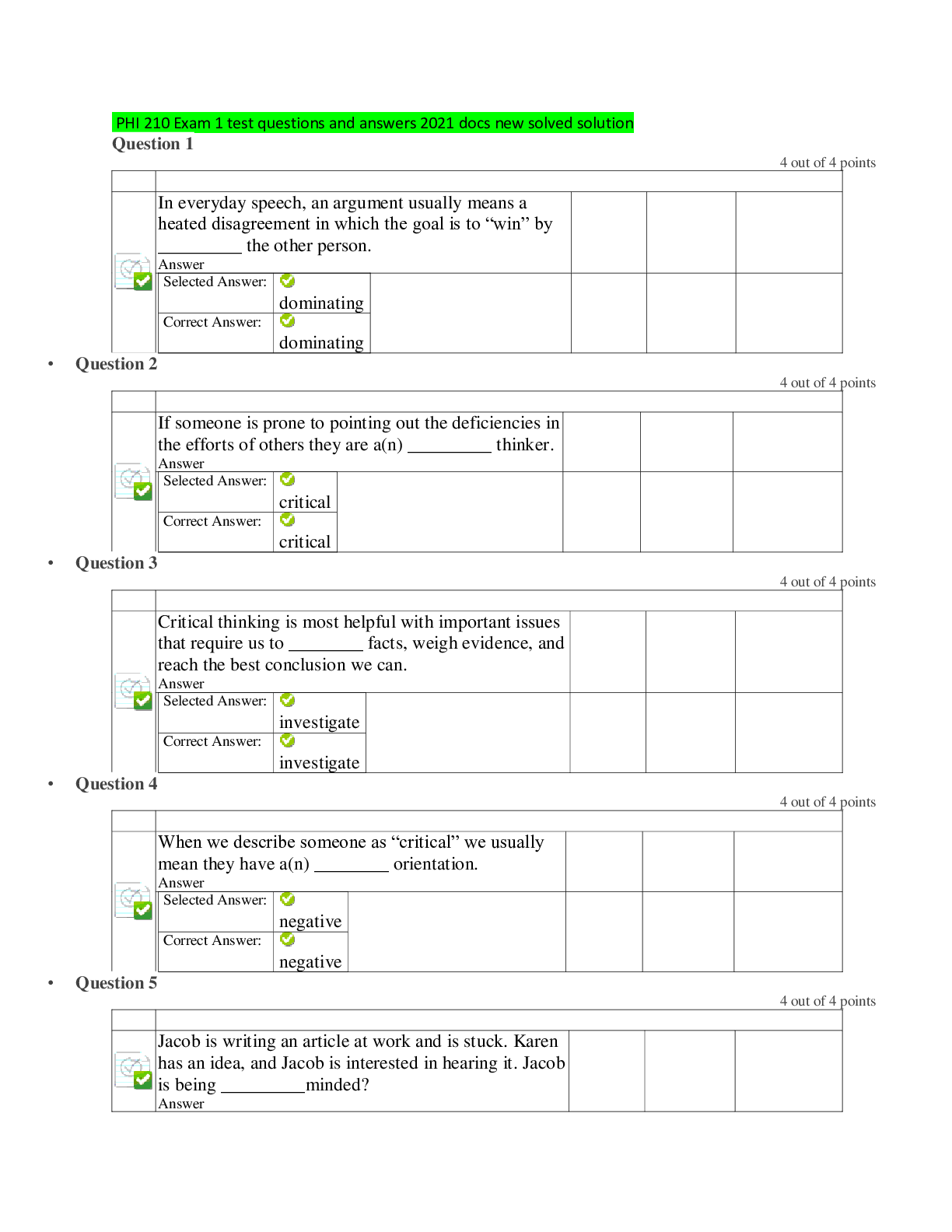

 Questions and Answers (latest Update) Download to Score A.png)
 Questions and Answers (latest Update), All Correct, Download to Score A.png)
 Study Guide.png)

