*NURSING > QUESTIONS & ANSWERS > NR 328 Pediatric Nursing; Final Exam Test Bank 3, Latest 2019/2020. (All)
NR 328 Pediatric Nursing; Final Exam Test Bank 3, Latest 2019/2020.
Document Content and Description Below
NR 328 Pediatric Nursing; Final Exam Test Bank 3, Latest 2019/2020. Chapter 21: The Child with Cognitive, Sensory, or Communication Impairment MULTIPLE CHOICE 1. The American Association on Intelle... ctual and Developmental Disabilities (AAIDD), formerly the American Association on Cognitive Impairment, classifies cognitive impairment based on what parameter? a. Age of onset b. Subaverage intelligence c. Adaptive skill domains d. Causative factors for cognitive impairment The AAIDD has categorized cognitive impairment into adaptive skill domains. The child must demonstrate functional impairment in at least two of the following adaptive skill domains: communication, self-care, home living, social skills, use of community resources, self-direction, health and safety, functional academics, leisure, and work. Age of onset before 18 years is part of the former criteria. Low intelligence quotient (IQ) alone is not the sole criterion for cognitive impairment. Etiology is not part of the classification. DIF: Cognitive Level: Understanding REF: p. 824 TOP: Nursing Process: Assessment MSC: Client Needs: Psychosocial Integrity 2. Secondary prevention for cognitive impairment includes what activity? a. Genetic counseling b. Avoidance of prenatal rubella infection c. Preschool education and counseling services d. Newborn screening for treatable inborn errors of metabolism Secondary prevention involves activities that are designed to identify the condition early and initiate treatment to avert cerebral damage. Inborn errors of metabolism such as hypothyroidism, phenylketonuria, and galactosemia can cause cognitive impairment. Genetic counseling and avoidance of prenatal rubella infections are examples of primary prevention strategies to preclude the occurrence of disorders that can cause cognitive impairment. Preschool education and counseling services are examples of tertiary prevention. These are designed to include early identification of conditions and provision of appropriate therapies and rehabilitation services. DIF: Cognitive Level: Understanding REF: p. 826 TOP: Nursing Process: Implementation MSC: Client Needs: Health Promotion and Maintenance 3. What is a primary goal in caring for a child with cognitive impairment? a. Developing vocational skills b. Promoting optimum development c. Finding appropriate out-of-home care d. Helping child and family adjust to future care The goal for children with cognitive impairment is the promotion of optimum social, physical, cognitive, and adaptive development as individuals within a family and community. Vocational skills are only one part of that goal. The focus must also be on the family and other aspects of development. Out-of-home care is considered part of the child’s development. Optimum development includes adjustment for both the family and child. DIF: Cognitive Level: Understanding REF: p. 828 TOP: Nursing Process: Planning MSC: Client Needs: Psychosocial Integrity 4. One of the techniques that has been especially useful for learners having cognitive impairment is called fading. What description best explains this technique? a. Positive reinforcement when tasks or behaviors are mastered b. Repeated verbal explanations until tasks are faded into the child’s development c. Negative reinforcement for specific tasks or behaviors that need to be faded out d. Gradually reduces the assistance given to the child so the child becomes more independent Fading is physically taking the child through each sequence of the desired activity and gradually fading out the physical assistance so the child becomes more independent. Positive reinforcement when tasks or behaviors are mastered is part of behavior modification. An essential component is ignoring undesirable behaviors. Verbal explanations are not as effective as demonstration and physical guidance. Consistent negative reinforcement is helpful, but positive reinforcement that focuses on skill attainment should be incorporated. DIF: Cognitive Level: Analyzing REF: p. 827 TOP: Nursing Process: Evaluation MSC: Client Needs: Health Promotion and Maintenance 5. The parents of a child with cognitive impairment ask the nurse for guidance with discipline. What should the nurse’s recommendation be based on? a. Discipline is ineffective with cognitively impaired children. b. Cognitively impaired children do not require discipline. c. Behavior modification is an excellent form of discipline. d. Physical punishment is the most appropriate form of discipline. Discipline must begin early. Limit-setting measures must be clear, simple, consistent, and appropriate for the child’s mental age. Behavior modification, especially reinforcement of desired behavior and use of time-out procedures, is an appropriate form of behavior control. Aversive strategies should be avoided in disciplining the child. DIF: Cognitive Level: Applying REF: p. 827 TOP: Nursing Process: Implementation MSC: Client Needs: Health Promotion and Maintenance 6. What intervention is most appropriate to facilitate social development of a child with a cognitive impairment? a. Provide age-appropriate toys and play activities. b. Avoid exposure to strangers who may not understand cognitive development. c. Provide peer experiences, such as infant stimulation and preschool programs. d. Emphasize mastery of physical skills because they are delayed more often than verbal skills. The acquisition of social skills is a complex task. Initially, an infant stimulation program should be used. Children of all ages need peer relationships. Parents should enroll the child in preschool. When older, they should have peer experiences similar to those of other children such as group outings, Boy and Girl Scouts, and Special Olympics. Providing age-appropriate toys and play activities is important, but peer interactions facilitate social development. Parents should expose the child to individuals who do not know the child. This enables the child to practice social skills. Verbal skills are delayed more often than physical skills. DIF: Cognitive Level: Applying REF: p. 835 TOP: Nursing Process: Implementation MSC: Client Needs: Health Promotion and Maintenance 7. The nurse is discussing sexuality with the parents of an adolescent girl who has a moderate cognitive impairment. What factor should the nurse consider when dealing with this issue? a. Sterilization is recommended for any adolescent with cognitive impairment. b. Sexual drive and interest are very limited in individuals with cognitive impairment. c. Individuals with cognitive impairment need a well-defined, concrete code of sexual conduct. d. Sexual intercourse rarely occurs unless the individual with cognitive impairment is sexually abused. Adolescents with moderate cognitive impairment may be easily persuaded and lack judgment. A well-defined, concrete code of conduct with specific instructions for handling certain situations should be defined for the adolescent. Permanent contraception by sterilization presents moral and ethical issues and may have psychologic effects on the adolescent. It may be prohibited in some states. The adolescent needs to have practical sexual information regarding physical development and contraception. Cognitively impaired individuals may desire to marry and have families. The adolescent needs to be protected from individuals who may make intimate advances. DIF: Cognitive Level: Applying REF: p. 829 TOP: Integrated Process: Teaching/Learning MSC: Client Needs: Health Promotion and Maintenance 8. The mother of a young child with cognitive impairment asks for suggestions about how to teach her child to use a spoon for eating. The nurse should make which recommendation? a. Do a task analysis first. b. Do not expect this task to be learned. c. Continue to spoon feed the child until the child tries to do it alone. d. Offer only finger foods so spoon feeding is unnecessary. Successful teaching begins with a task analysis. The endpoint (self-feeding, toilet training, and so on) is broken down into the component steps. The child is then guided to master the individual steps in sequence. Depending on the child’s functional level, using a spoon for eating should be an achievable goal. The child requires demonstration and then guided training for each component of the self-feeding. Feeding finger foods so spoon feeding is unnecessary eliminates some of the intermediate steps that are necessary to using a fork and spoon. For socialization purposes, it is desirable that a child use feeding implements. DIF: Cognitive Level: Understanding REF: p. 827 TOP: Nursing Process: Implementation MSC: Client Needs: Health Promotion and Maintenance 9. A newborn assessment shows a separated sagittal suture, oblique palpebral fissures, a depressed nasal bridge, a protruding tongue, and transverse palmar creases. These findings are most suggestive of which condition? a. Microcephaly b. Cerebral palsy c. Down syndrome d. Fragile X syndrome These are characteristics associated with Down syndrome. An infant with microcephaly has a small head. Cerebral palsy is a diagnosis not usually made at birth; no characteristic physical signs are present. The infant with fragile X syndrome has increased head circumference; long, wide, or protruding ears; a long, narrow face with a prominent jaw; hypotonia; and a high-arched palate. DIF: Cognitive Level: Understanding REF: p. 834 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 10. A 2-week-old infant with Down syndrome is being seen in the clinic. His mother tells the nurse that he is difficult to hold, that “he’s like a rag doll. He doesn’t cuddle up to me like my other babies did.” What is the nurse’s best interpretation of this lack of clinging or molding? a. Sign of detachment and rejection b. Indicative of maternal deprivation c. A physical characteristic of Down syndrome d. Suggestive of autism associated with Down syndrome Infants with Down syndrome have hypotonicity of muscles and hyperextensibility of joints, which complicate positioning. The limp, flaccid extremities resemble the posture of a rag doll. Holding the infant is difficult and cumbersome, and parents may feel that they are inadequate. A lack of clinging or molding is characteristic of Down syndrome, not detachment. There is no evidence of maternal deprivation. Autism is not associated with Down syndrome, and it would not be evident at 2 weeks of age. DIF: Cognitive Level: Analyzing REF: p. 836 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 11. Many of the clinical features of Down syndrome present challenges to caregivers. Based on these features, what intervention should be included in the child’s care? a. Delay feeding solid foods until the tongue thrust has stopped. b. Modify the diet as necessary to minimize the diarrhea that often occurs. c. Provide calories appropriate to the child’s mental age. d. Use a cool-mist vaporizer to keep the mucous membranes moist and secretions liquefied. The constant stuffy nose forces the child to breathe by mouth, drying the mucous membranes and increasing the susceptibility to upper respiratory tract infections. A cool-mist vaporizer will keep the mucous membranes moist and liquefy secretions. Respiratory tract infections combined with cardiac anomalies are the primary cause of death in the first years. The child has a protruding tongue, which makes feeding difficult. The parents must persist with feeding while the child continues the physiologic response of the tongue thrust. The child is predisposed to constipation. Calories should be appropriate to the child’s weight and growth needs, not mental age. DIF: Cognitive Level: Applying REF: p. 837 TOP: Nursing Process: Planning MSC: Client Needs: Physiological Integrity 12. What description applies to fragile X syndrome? a. Chromosomal defect affecting only females b. Second most common genetic cause of cognitive impairment c. Most common cause of uninherited cognitive impairment d. Chromosomal defect that follows the pattern of X-linked recessive disorders Fragile X syndrome is the most common inherited cause of cognitive impairment and the second most common genetic cause of cognitive impairment after Down syndrome. Fragile X primarily affects males and follows the pattern of X-linked dominant inheritance with reduced penetrance. DIF: Cognitive Level: Understanding REF: p. 837 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 13. The nurse should suspect a hearing impairment in an infant who fails to demonstrate which behavior? a. Babbling by age 12 months b. Eye contact when being spoken to c. Startle or blink reflex to sound d. Gesturing to indicate wants after age 15 months The absence of babbling or inflections in voice by at least age 7 months is an indication of hearing difficulties. Lack of eye contact is not indicative of a hearing loss. An infant with a hearing impairment might react to a loud noise but not respond to the spoken word. The child with hearing impairment uses gestures rather than vocalizations to express desires at this age. DIF: Cognitive Level: Understanding REF: p. 854 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 14. The nurse is talking with a 10-year-old boy who wears bilateral hearing aids. The left hearing aid is making an annoying whistling sound that the child cannot hear. What intervention is the most appropriate nursing action? a. Ignore the sound. b. Suggest he reinsert the hearing aid. c. Ask him to reverse the hearing aids in his ears. d. Suggest he raise the volume of the hearing aid. The whistling sound is acoustic feedback. The nurse should have the child remove the hearing aid and reinsert it, making sure no hair is caught between the ear mold and the ear canal. Ignoring the sound or suggesting he raise the volume of the hearing aid would be annoying to others. The hearing aids are molded specifically for each ear. DIF: Cognitive Level: Applying REF: p. 842 TOP: Nursing Process: Implementation MSC: Client Needs: Physiological Integrity 15. What technique facilitates lip reading by a hearing-impaired child? a. Speak at an even rate. b. Avoid using facial expressions. c. Exaggerate pronunciation of words. d. Repeat in exactly the same way if child does not understand. Help the child learn and understand how to read lips by speaking at an even rate. Avoiding using facial expressions, exaggerating pronunciation of words, and repeating in exactly the same way if the child does not understand interfere with the child’s understanding of the spoken word. DIF: Cognitive Level: Applying REF: p. 843 TOP: Nursing Process: Implementation MSC: Client Needs: Psychosocial Integrity 16. What condition is defined as reduced visual acuity in one eye despite appropriate optical correction? a. Myopia b. Hyperopia c. Amblyopia d. Astigmatism Amblyopia, or lazy eye, is reduced visual acuity in one eye. Amblyopia is usually caused by one eye not receiving sufficient stimulation. The resulting poor vision in the affected eye can be avoided with the treatment of the primary visual defect such as strabismus. Myopia, or nearsightedness, refers to the ability to see objects clearly at close range but not a distance. Hyperopia, or farsightedness, is the ability to see objects at a distance but not at close range. Astigmatism is unequal curvatures in refractive apparatus. DIF: Cognitive Level: Understanding REF: p. 844 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 17. The school nurse is caring for a child with a penetrating eye injury. Emergency treatment includes what intervention? a. Place a cool compress on eye during transport to the emergency department. b. Irrigate the eye copiously with a sterile saline solution. c. Remove the object with a lightly moistened gauze pad. d. Apply a Fox shield to the affected eye and any type of patch to the other eye. The nurse’s role in a penetrating eye injury is to prevent further injury to the eye. A Fox shield (if available) should be applied to the injured eye and a regular eye patch to the other eye to prevent bilateral movement. Placing cool compress on the eye during transport to emergency department, irrigating eye copiously with a sterile saline solution, or removing object with a lightly moistened gauze pad may cause more damage to the eye. DIF: Cognitive Level: Applying REF: p. 847 TOP: Nursing Process: Implementation MSC: Client Needs: Physiological Integrity 18. A father calls the emergency department nurse saying that his daughter’s eyes burn after getting some dishwasher detergent in them. The nurse recommends that the child be seen in the emergency department or by an ophthalmologist. The nurse also should recommend which action before the child is transported? a. Keep the eyes closed. b. Apply cold compresses. c. Irrigate the eyes copiously with tap water for 20 minutes. d. Prepare a normal saline solution (salt and water) and irrigate the eyes for 20 minutes. The first action is to flush the eyes with clean tap water. This will rinse the detergent from the eyes. Keeping the eyes closed and applying cold compresses may allow the detergent to do further harm to the eyes during transport. Normal saline is not necessary. The delay can allow the detergent to cause continued injury to the eyes. DIF: Cognitive Level: Applying REF: p. 847 TOP: Nursing Process: Implementation MSC: Client Needs: Physiological Integrity 19. A 5-year-old child has bilateral eye patches in place after surgery yesterday morning. Today he can be out of bed. What nursing intervention is most important at this time? a. Speak to him when entering the room. b. Allow him to assist in feeding himself. c. Orient him to his immediate surroundings. d. Reassure him and allow his parents to stay with him. Safety is the priority concern. Because he can now be out of bed, it is imperative that he knows about his physical surroundings. Speaking to the child is a component of nursing care that is expected with all clients unless contraindicated. Unless additional impairments are present, his meal tray should be set up, and he should be able to feed himself. Reassuring him and allowing his parents to stay with him are essential parts of nursing care for all children. DIF: Cognitive Level: Applying REF: p. 849 TOP: Nursing Process: Implementation MSC: Client Needs: Physiological Integrity 20. Autism is a complex developmental disorder. The diagnostic criteria for autism include delayed or abnormal functioning in which area with onset before age 3 years? a. Parallel play b. Gross motor development c. Ability to maintain eye contact d. Growth below the fifth percentile One hallmark of autism spectrum disorders is the child’s inability to maintain eye contact with another person. Parallel play is play typical of toddlers and is usually not affected. Social, not gross motor, development is affected by autism. Physical growth and development are not usually affected. DIF: Cognitive Level: Understanding REF: p. 845 TOP: Nursing Process: Assessment MSC: Client Needs: Health Promotion and Maintenance 21. What intervention should be included in the nursing care of a child with autism spectrum disorder (ASD)? a. Assign multiple staff to care for the child. b. Communicate with the child at his or her developmental level. c. Provide a wide variety of foods for the child to try. d. Place the child in a semiprivate room with a roommate of a similar age. Children with ASD require individualized care. The nurse needs to communicate with the child at the child’s developmental level. Consistent caregivers are essential for children with ASD. The same staff members should care for the child as much as possible. Children with ASD do not adapt to changing situations. The same foods should be provided to allow the child to adjust. A private room is desirable for children with ASD. Stimulation is minimized. DIF: Cognitive Level: Applying REF: p. 857 TOP: Nursing Process: Implementation MSC: Client Needs: Physiological Integrity 22. What suggestion by the nurse for parents regarding stuttering in children is most helpful? a. Offer rewards for proper speech. b. Encourage the child to take it easy and go slow when stuttering. c. Help the child by supplying words when he or she is experiencing a block. d. Give the child plenty of time and the impression that you are not in a hurry. Hesitancy and dysfluency should be considered a normal part of speech development. An important approach is to allow the child plenty of time to speak. Promising rewards for proper speech places additional pressure on the child. Encouraging the child to take it easy and go slow when stuttering draws attention to the dysfluency. The child needs to complete a sentence and thought without being interrupted. DIF: Cognitive Level: Understanding REF: p. 858 TOP: Integrated Process: Teaching/Learning MSC: Client Needs: Health Promotion and Maintenance 23. What observation in a child should indicate the need for a referral to a specialist regarding a communication impairment? a. At 2 years of age, the child fails to respond consistently to sounds. b. At 3 years of age, the child fails to use sentences of more than five words. c. At 4 years of age, the child has impaired sentence structure. d. At 5 years of age, the child has poor voice quality. If a 2-year-old child fails to respond consistently to sounds, it is an indication for referral to a specialist regarding communication impairment. At age 3 years, the child failing to use sentences of three words would be an indication for referral; impaired sentence structure would be seen in a 5-year-old child and poor voice quality in an older child who has a communication impairment. DIF: Cognitive Level: Applying REF: p. 859 TOP: Nursing Process: Assessment MSC: Client Needs: Health Promotion and Maintenance 24. The nurse is performing a physical assessment on a 3-year-old child. The parents state that the child excessively rubs the eyes and often tilts the head to one side. What visual impairment should the nurse suspect? a. Strabismus b. Astigmatism c. Hyperopia, or farsightedness d. Myopia, or nearsightedness Clinical manifestations of myopia include excessive eye rubbing, head tilting, difficulty reading, headaches, and dizziness. Strabismus, astigmatism, and hyperopia have other clinical manifestations. DIF: Cognitive Level: Applying REF: p. 845 TOP: Nursing Process: Assessment MSC: Client Needs: Health Promotion and Maintenance 25. The community nurse is planning prevention measures designed to avoid conditions that can cause cognitive impairment. Taking folic acid supplements during pregnancy to prevent neural tube defects is which type of prevention strategy? a. Primary b. Secondary c. Tertiary d. Rehabilitative Primary prevention strategies are those designed to avoid conditions that cause cognitive impairment. Use of folic acid supplements during pregnancy to prevent neural tube defects is a primary prevention strategy. Secondary prevention activities are those designed to identify the condition early and initiate treatment to avert cerebral damage. Tertiary prevention strategies are those concerned with treatment to minimize long-term consequences. Rehabilitation services is an example of tertiary prevention. DIF: Cognitive Level: Analyzing REF: p. 825 TOP: Nursing Process: Assessment MSC: Client Needs: Health Promotion and Maintenance 26. The nurse is teaching a preschool child with a cognitive impairment how to throw a ball overhand. What teaching strategy should the nurse use for this child? a. Demonstrate how to throw a ball overhand. b. Explain the reason for throwing a ball overhand. c. Show pictures of children throwing balls overhand. d. Explain to the child how to throw the ball overhand. Children with cognitive impairment have a deficit in discrimination, which means that concrete ideas are much easier to learn effectively than abstract ideas. Therefore, demonstration is preferable to verbal explanation, and the nurse should direct learning toward mastering a skill rather than understanding the scientific principles underlying a procedure. Demonstrating how to throw the ball is the best teaching strategy. DIF: Cognitive Level: Applying REF: p. 827 TOP: Integrated Process: Teaching/Learning MSC: Client Needs: Health Promotion and Maintenance 27. The camp nurse is choosing a toy for a child with cognitive impairment to play with during swimming time. What toy should the nurse choose to encourage improvement of developmental skills? a. Dive rings b. An inner tube c. Floating ducks d. A large beach ball Toys are selected for their recreational and educational value. For example, a large inflatable beach ball is a good water toy; encourages interactive play; and can be used to learn motor skills such as balance, rocking, kicking, and throwing. Dive rings, an inner tube, and floating ducks are not interactive toys. DIF: Cognitive Level: Applying REF: p. 829 TOP: Nursing Process: Implementation MSC: Client Needs: Health Promotion and Maintenance 28. The nurse is teaching feeding strategies to a parent of a 12-month-old infant with Down syndrome. What statement made by the parent indicates a need for further teaching? a. “If the food is thrust out, I will reefed it.” b. “I will use a small, long, straight-handled spoon.” c. “I will place the food on the top of the tongue.” d. “I know the tongue thrust doesn’t indicate a refusal of the food.” Parents of a child with Down syndrome need to know that the tongue thrust does not indicate refusal to feed but is a physiologic response. Parents are advised to use a small but long, straight-handled spoon to push the food toward the back and side of the mouth. If food is thrust out, it should be refed. If the parent indicates placing the food on the tongue, further teaching is needed. DIF: Cognitive Level: Applying REF: p. 837 TOP: Integrated Process: Teaching/Learning MSC: Client Needs: Health Promotion and Maintenance 29. The nurse is counseling a pregnant 35-year-old woman about estimated risk of Down syndrome. What is the estimated risk for a woman who is 35 years of age? a. One in 1200 b. One in 900 c. One in 350 d. One in 100 The estimated risk of Down syndrome for a 35-year-old woman is one in 350. One in 1200 is the risk for a 25-year-old woman, one in 900 is the risk for a 30-year–old woman, and one in 100 is the risk for a 40-year-old woman. DIF: Cognitive Level: Applying REF: p. 833 TOP: Integrated Process: Teaching/Learning MSC: Client Needs: Health Promotion and Maintenance 30. The nurse is teaching parents of a child with cataracts about the upcoming treatment. The nurse should give the parents what information about the treatment of cataracts? a. “The treatment may require more than one surgery.” b. “It is corrected with biconcave lenses that focus rays on the retina.” c. “Cataracts require surgery to remove the cloudy lens and replace it.” d. “Treatment is with a corrective lenses; no surgery is necessary.” Treatment for cataracts requires surgery to remove the cloudy lens and replace it (with an intraocular lens implant, removable contact lens, or prescription glasses). Treatment for glaucoma may require more than one surgery. Anisometropia is treated with corrective lenses. Myopia is corrected with biconcave lenses that focus rays on the retina. DIF: Cognitive Level: Applying REF: p. 846 TOP: Integrated Process: Teaching/Learning MSC: Client Needs: Physiological Integrity 31. What action should the school nurse take for a child who has a hematoma (black eye) with no hemorrhage into the anterior chamber? a. Apply a warm moist pack. b. Have the child keep the eyes open. c. Apply ice for the first 24 hours. d. Refer to an ophthalmologist immediately. The care for a hematoma eye injury with no hemorrhage into the anterior chamber is to apply ice for the first 24 hours. A warm moist pack should not be applied, and the child should keep the eyes closed. Referral to an ophthalmologist is recommended if hyphema (hemorrhage into the anterior chamber) is present. DIF: Cognitive Level: Applying REF: p. 847 TOP: Nursing Process: Implementation MSC: Client Needs: Safe and Effective Care Environment MULTIPLE RESPONSE 1. The nurse is preparing an education program on hearing impairment for a group of new staff nurses. What concepts should be included? (Select all that apply.) a. A child with a slight hearing loss is usually unaware of a hearing difficulty. b. A clinical manifestation of a hearing impairment in children is avoidance of social interaction. c. A child with a severe hearing loss may hear a loud voice if nearby. d. Children with sensorineural hearing loss can benefit from the use of a hearing aid. e. A clinical manifestation of hearing impairment in an infant is lack of the startle reflex. f. Identification of a hearing loss after the first year is essential to facilitate language development in children. , B, C, E When discussing hearing impairment in children, the nurse should include information about differences in hearing losses, such as with a slight hearing loss, the child is usually unaware of a hearing difficulty, and with a severe loss, the child may hear a loud noise if it is nearby. An infant with a hearing loss may lack the startle response, and a hearing impaired child may avoid social interaction. Children with a sensorineural hearing loss would not benefit from a hearing aid. Identification of a hearing loss is imperative in the first 3 to 6 months to facilitate language and educational development for children. DIF: Cognitive Level: Analyzing REF: p. 842 TOP: Integrated Process: Teaching/Learning MSC: Client Needs: Health Promotion and Maintenance 2. The nurse understands that which gestational disorders can cause a cognitive impairment in the newborn? (Select all that apply.) a. Prematurity b. Postmaturity c. Low birth weight d. Physiological jaundice e. Large for gestational age , B, C Prematurity, postmaturity, and low birth weight can be causes of cognitive impairment in newborns. Physiological jaundice and large for gestational age are not associated causes of cognitive impairment in newborns. DIF: Cognitive Level: Understanding REF: p. 825 TOP: Nursing Process: Assessment MSC: Client Needs: Health Promotion and Maintenance 3. The clinic nurse is assessing an infant. What are early signs of cognitive impairment the nurse should discuss with the health care provider? (Select all that apply.) a. Head lag at 11 months of age b. No pincer grasp at 4 months of age c. Colicky incidents at 3 months of age d. Unable to speak two to three words at 24 months of age e. Unresponsiveness to the environment at 12 months of age , D, E Early signs of cognitive impairment include gross motor delay (head lag should be established by 6 months, and head lag still present at 11 months is a delay), language delay (normal language development is speaking two to three words by age 12 months; if unable to speak two to three words at 24 months, that is a delay), and unresponsiveness to the environment at 12 months. No pincer grasp at 4 months of age is normal (palmar grasp is the expected finding), and colicky incidents at 3 months of age is a normal finding. DIF: Cognitive Level: Analyzing REF: p. 826 TOP: Nursing Process: Assessment MSC: Client Needs: Health Promotion and Maintenance 4. The nurse is teaching parents of a child with a cognitive impairment signs that indicate the child is developmentally ready for dressing training. What signs should the nurse include that indicate the child is developmentally ready for dressing training? (Select all that apply.) a. Can follow verbal commands b. Can sit quietly for 1 to 2 minutes c. Can master every task of dressing d. Can follow physical gestures or cues e. Can relate clothing to the appropriate body part , D, E Children are considered developmentally ready for dressing training if they can sit quietly for 3 to 5 minutes (not 1 to 2) while working on a task; can follow physical gestures or cues; can follow verbal commands; and can relate clothing to the appropriate body part, such as socks to feet. As with other self-help skills, the child may not be able to master every task but should be evaluated for evidence of willingness to participate at his or her level of readiness. DIF: Cognitive Level: Applying REF: p. 832 TOP: Integrated Process: Teaching/Learning MSC: Client Needs: Health Promotion and Maintenance 5. The nurse is assessing a child with Down syndrome. The nurse recognizes that which are possible comorbidities that can occur with Down syndrome? (Select all that apply.) a. Diabetes mellitus b. Hodgkin’s disease c. Congenital heart defects d. Respiratory tract infections e. Acute megakaryoblastic leukemia , D, E Children with Down syndrome often have multiple comorbidities, contributing to numerous other conditions. Respiratory tract infections are prevalent; when combined with cardiac anomalies, they are the chief cause of death, particularly during the first year. The incidence of leukemia is several times more frequent than expected in the general population, and in about half of the cases, the type is acute megakaryoblastic leukemia. DIF: Cognitive Level: Analyzing REF: p. 835 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 6. A child has a slight (26–40 dB) degree of hearing loss. The nurse recognizes this amount of hearing loss can have what effect? (Select all that apply.) a. No speech defects b. Difficulty hearing faint speech c. Usually is unaware of the hearing difficulty d. Can distinguish vowels but not consonants e. Unable to understand conversational speech , B, C A child with a slight degree of hearing loss has no speech defects, may have difficulty hearing faint speech, and is usually unaware of the hearing difficulty. The ability to distinguish vowels but not consonants is an effect of severe hearing loss and being unable to understand conversational speech is an effect of moderately severe hearing loss. DIF: Cognitive Level: Analyzing REF: p. 840 TOP: Nursing Process: Assessment MSC: Client Needs: Health Promotion and Maintenance 7. What risk factors can cause a sensorineural hearing impairment in an infant? (Select all that apply.) a. Cat scratch disease b. Bacterial meningitis c. Childhood case of measles d. Childhood case of chicken pox e. Administration of aminoglycosides for more than 5 days , C, E Risk criteria for sensorineural hearing impairment in infants include bacterial meningitis; a case of measles; and administration of ototoxic medications (e.g., gentamicin, tobramycin, kanamycin, streptomycin), including but not limited to the aminoglycosides, for more than 5 days. Cat scratch disease and a childhood case of chicken pox are not risk factors that can cause a sensorineural hearing impairment. DIF: Cognitive Level: Understanding REF: p. 841 TOP: Nursing Process: Assessment MSC: Client Needs: Health Promotion and Maintenance 8. The nurse is teaching parents the signs of a hearing impairment in infants. What should the nurse include as signs? (Select all that apply.) a. Lack of a fencing reflex b. Lack of a startle reflex to a loud sound c. Awakened by loud environmental noises d. Failure to localize a sound by 6 months of age e. Response to loud noises as opposed to the voice , D, E The fencing reflex is elicited when the infant is placed on his or her back; it does not indicate a hearing impairment. Awakening by a loud environmental noise is a normal response. DIF: Cognitive Level: Applying REF: p. 842 TOP: Integrated Process: Teaching/Learning MSC: Client Needs: Health Promotion and Maintenance 9. The nurse is teaching parents the signs of a hearing impairment in a child. What should the nurse include as signs? (Select all that apply.) a. Outgoing behavior b. Yelling to express pleasure c. Asking to have statements repeated d. Foot stamping for vibratory sensation e. Failure to develop intelligible speech by age 24 months , C, D, E Signs of a hearing impairment in a child include yelling to express pleasure, asking to have statements repeated, foot stamping for vibratory sensation, and failure to develop intelligible speech by age 24 months. The child’s behavior is shy, not outgoing. DIF: Cognitive Level: Applying REF: p. 842 TOP: Integrated Process: Teaching/Learning MSC: Client Needs: Health Promotion and Maintenance 10. The nurse should plan which actions to assist the stuttering child? (Select all that apply.) a. Ask the child to stop and start over. b. Promise a reward for proper speech. c. Set a good example by speaking clearly. d. Give the child plenty of time to finish sentences. e. Look directly at the child while he or she is speaking. , D, E Actions to be encouraged to help the stuttering child include setting a good example by speaking clearly, giving the child plenty of time to finish sentences, and looking directly at the child while he or she is speaking. Asking the child to stop and start over and promising a reward for proper speech are actions to be avoided with stuttering children. DIF: Cognitive Level: Applying REF: p. 858 TOP: Nursing Process: Planning MSC: Client Needs: Health Promotion and Maintenance 11. The nurse should plan which actions to facilitate lipreading for a child with a hearing impairment? (Select all that apply.) a. Face the child directly. b. Speak at eye level. c. Keep sentences short. d. Speak at a fast, even-paced rate. e. Establish eye contact and show interest. , B, C, E To facilitate lipreading, the nurse should plan to face the child directly, speak at eye level, keep sentences short, and establish eye contact and show interest. The nurse should plan to speak at a slow rate, not a fast one. DIF: Cognitive Level: Applying REF: p. 843 TOP: Nursing Process: Planning MSC: Client Needs: Health Promotion and Maintenance 12. What are indications for a referral regarding a communication impairment in a school-age child? (Select all that apply.) a. Barely audible voice quality b. Vocal pitch inappropriate for age c. Intonation noted during speaking d. Maintains a rhythm while speaking e. Distortion of sounds after age 7 years , B, E Barely audible voice quality, vocal pitch inappropriate for age, and distortion of sounds after age 7 years are indications for a referral regarding a communication impairment. Intonation noted while speaking and maintaining a rhythm while speaking are normal characteristics of speech. DIF: Cognitive Level: Understanding REF: p. 859 TOP: Nursing Process: Assessment MSC: Client Needs: Health Promotion and Maintenance MATCHING Match the type of visual impairment to its definition. a. Myopia b. Hyperopia c. Astigmatism d. Anisometropia e. Amblyopia 1. Different refractive strength in each eye 2. Ability to see objects clearly at close range but not at a distance 3. Reduced visual acuity in one eye 4. Unequal curvatures in refractive apparatus 5. Ability to see objects at a distance but not at a close range 1. DIF: Cognitive Level: Understanding REF: p. 846 TOP: Nursing Process: Implementation MSC: Client Needs: Health Promotion and Maintenance 2. DIF: Cognitive Level: Understanding REF: p. 845 TOP: Nursing Process: Implementation MSC: Client Needs: Health Promotion and Maintenance 3. ANS: E DIF: Cognitive Level: Understanding REF: p. 845 TOP: Nursing Process: Implementation MSC: Client Needs: Health Promotion and Maintenance 4. DIF: Cognitive Level: Understanding REF: p. 845 TOP: Nursing Process: Implementation MSC: Client Needs: Health Promotion and Maintenance 5. DIF: Cognitive Level: Understanding REF: p. 846 TOP: Nursing Process: Implementation MSC: Client Needs: Health Promotion and Maintenance Chapter 31: The Child with Cancer MULTIPLE CHOICE 1. What childhood cancer may demonstrate patterns of inheritance that suggest a familial basis? a. Leukemia b. Retinoblastoma c. Rhabdomyosarcoma d. Osteogenic sarcoma Retinoblastoma is an example of a pediatric cancer that demonstrates inheritance. The absence of the retinoblastoma gene allows for abnormal cell growth and the development of retinoblastoma. Chromosome abnormalities are present in many malignancies. They do not indicate a familial pattern of inheritance. The Philadelphia chromosome is observed in almost all individuals with chronic myelogenous leukemia. There is no evidence of a familial pattern of inheritance for rhabdomyosarcoma or osteogenic sarcoma cancers. DIF: Cognitive Level: Understanding REF: p. 1379 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 2. As part of the diagnostic evaluation of a child with cancer, biopsies are important for staging. What statement explains what staging means? a. Extent of the disease at the time of diagnosis b. Rate normal cells are being replaced by cancer cells c. Biologic characteristics of the tumor or lymph nodes d. Abnormal, unrestricted growth of cancer cells producing organ damage Staging is a description of the extent of the disease at the time of diagnosis. Staging criteria exist for most tumors. The stage usually relates directly to the prognosis; the higher the stage, the poorer the prognosis. The rate that normal cells are being replaced by cancer cells is not a definition of staging. Classification of the tumor refers to the biologic characteristics of the tumor or lymph nodes. Abnormal, unrestricted growth of cancer cells producing organ damage describes how cancer cells grow and can cause damage to an organ. DIF: Cognitive Level: Understanding REF: p. 1400 TOP: Nursing Process: Planning MSC: Client Needs: Physiological Integrity 3. What statement related to clinical trials developed for pediatric cancers is most accurate? a. Are accessible only in major pediatric centers b. Do not require consent for standard therapy c. Provide the best available therapy compared with an expected improvement d. Are standardized to provide the same treatment to all children with the disease Most clinical trials have a control group in which the patients receive the best available therapy currently known. The experimental group(s) receives treatment that is thought to be even better. The protocol outlines the therapy plan. Protocols are developed for many pediatric cancers. They can be accessed by pediatric oncologists throughout the United States. Consent is always required in treatment of children, especially for research protocols. The protocol is designed to optimize therapy for children based on disease type and stage. DIF: Cognitive Level: Understanding REF: p. 1382 TOP: Nursing Process: Evaluation MSC: Client Needs: Physiological Integrity 4. Chemotherapeutic agents are classified according to what feature? a. Side effects b. Effectiveness c. Mechanism of action d. Route of administration Chemotherapeutic agents are classified according to mechanism of action. For example, antimetabolites resemble essential metabolic elements needed for growth but are different enough to block further deoxyribonucleic acid (DNA) synthesis. Although the side effect profiles may be similar for drugs within a classification, they are not the basis for classification. Most chemotherapeutic regimens contain combinations of drugs. The effectiveness of any one drug is relative to the cancer type, combination therapy, and protocol for administration. The route of administration is determined by the pharmacodynamics and pharmacokinetics of each drug. DIF: Cognitive Level: Understanding REF: p. 1383 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 5. What type of chemotherapeutic agent alters the function of cells by replacing a hydrogen atom of a molecule? a. Plant alkaloids b. Antimetabolites c. Alkylating agents d. Antitumor antibiotics Alkylating agents replace a hydrogen atom with an alkyl group. The irreversible combination of alkyl groups with nucleotide chains, particularly deoxyribonucleic acid (DNA), causes unbalanced growth of unaffected cell constituents so that the cell eventually dies. Plant alkaloids arrest the cell in metaphase by binding to proteins needed for spindle formation. Antimetabolites resemble essential metabolic elements needed for growth but are different enough to block further DNA synthesis. Antitumor antibiotics are natural substances that interfere with cell division by reacting with DNA in such a way as to prevent further replication of DNA and transcription of ribonucleic acid (RNA). DIF: Cognitive Level: Understanding REF: p. 1383 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 6. What side effect commonly occurs with corticosteroid (prednisone) therapy? a. Alopecia b. Anorexia c. Nausea and vomiting d. Susceptibility to infection Corticosteroids have immunosuppressive effects. Children who are taking prednisone are susceptible to infections. Hair loss is not a side effect of corticosteroid therapy. Children taking corticosteroids have increased appetites. Gastric irritation, not nausea and vomiting, is a potential side effect. The medicine should be given with food. DIF: Cognitive Level: Understanding REF: p. 1404 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 7. What chemotherapeutic agent is classified as an antitumor antibiotic? a. Cisplatin (Platinol AQ) b. Vincristine (Oncovin) c. Methotrexate (Texall) d. Daunorubicin (Cerubidine) Daunorubicin is an antitumor antibiotic. Cisplatin is classified as an alkylating agent. Vincristine is a plant alkaloid. Methotrexate is an antimetabolite. DIF: Cognitive Level: Understanding REF: p. 1383 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 8. The nurse is administering an intravenous chemotherapeutic agent to a child with leukemia. The child suddenly begins to wheeze and have severe urticaria. What nursing action is most appropriate to initiate? a. Recheck the rate of drug infusion. b. Stop the drug infusion immediately. c. Observe the child closely for next 10 minutes. d. Explain to the child that this is an expected side effect. When an allergic reaction is suspected, the drug is immediately discontinued. Any drug in the line should be withdrawn, and a normal saline infusion begun to keep the line open. The intravenous infusion is stopped to minimize the amount of drug that infuses. The infusion rate can be confirmed at a later time. Observation of the child for 10 minutes is essential, but it is done after the infusion is stopped. These signs are indicative of an allergic reaction, not an expected response. DIF: Cognitive Level: Applying REF: p. 1384 TOP: Nursing Process: Implementation MSC: Client Needs: Physiological Integrity 9. Total-body irradiation is indicated for what reason? a. Palliative care b. Lymphoma therapy c. Definitive therapy for leukemia d. Preparation for bone marrow transplant Total-body irradiation is used as part of the destruction of the child’s immune system necessary for a bone marrow transplant. The child is at great risk for complications because there is no supportive therapy until engraftment of the donor marrow takes place. Irradiation for palliative care is done selectively. The area that is causing pain or potential obstruction is irradiated. Lymphoma and leukemia are treated through a combination of modalities. Total-body irradiation is not indicated. DIF: Cognitive Level: Understanding REF: p. 1384 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 10. The parents of a child with cancer tell the nurse that a bone marrow transplant (BMT) may be necessary. What information should the nurse recognize as important when discussing this with the family? a. BMT should be done at the time of diagnosis. b. Parents and siblings of the child have a 25% chance of being a suitable donor. c. If BMT fails, chemotherapy or radiotherapy will need to be continued. d. Finding a suitable donor involves matching antigens from the human leukocyte antigen (HLA) system. The most successful BMTs come from suitable HLA-matched donors. The timing of a BMT depends on the disease process involved. It usually follows intensive high-dose chemotherapy or radiotherapy. Usually, parents only share approximately 50% of the genetic material with their children. A one in four chance exists that two siblings will have two identical haplotypes and will be identically matched at the HLA loci. The decision to continue chemotherapy or radiotherapy if BMT fails is not appropriate to discuss with the parents when planning the BMT. That decision will be made later. DIF: Cognitive Level: Applying REF: p. 1385 TOP: Integrated Process: Teaching/Learning MSC: Client Needs: Physiological Integrity 11. An adolescent will receive a bone marrow transplant (BMT). The nurse should explain that the bone marrow will be administered by which method? a. Bone grafting b. Intravenous infusion c. Bone marrow injection d. Intraabdominal infusion Bone marrow from a donor is infused intravenously, and the transfused stem cells migrate to the recipient’s marrow and repopulate it. DIF: Cognitive Level: Applying REF: p. 1386 TOP: Integrated Process: Teaching/Learning MSC: Client Needs: Physiological Integrity 12. After chemotherapy is begun for a child with acute leukemia, prophylaxis to prevent acute tumor lysis syndrome includes which therapeutic intervention? a. Hydration b. Oxygenation c. Corticosteroids d. Pain management Acute tumor lysis syndrome results from the release of intracellular metabolites during the initial treatment of leukemia. Hyperuricemia, hypocalcemia, hyperphosphatemia, and hyperkalemia can result. Hydration is used to reduce the metabolic consequences of the tumor lysis. Oxygenation is not helpful in preventing acute tumor lysis syndrome. Allopurinol, not corticosteroids, is indicated for pharmacologic management. Pain management may be indicated for supportive therapy of the child, but it does not prevent acute tumor lysis syndrome. DIF: Cognitive Level: Analyzing REF: p. 1387 TOP: Nursing Process: Planning MSC: Client Needs: Physiological Integrity 13. Nursing care of the child with myelosuppression from leukemia or chemotherapeutic agents should include which therapeutic intervention? a. Restrict oral fluids. b. Institute strict isolation. c. Use good hand-washing technique. d. Give immunizations appropriate for age. Good hand washing minimizes the exposure to infectious organisms and decreases the chance of infection spread. Oral fluids are encouraged if the child is able to drink. If possible, the intravenous route is not used because of the increased risk of infection from parenteral fluid administration. Strict isolation is not indicated. When the child is immunocompromised, the vaccines are not effective. If necessary, the appropriate immunoglobulin is administered. DIF: Cognitive Level: Applying REF: p. 1393 TOP: Nursing Process: Implementation MSC: Client Needs: Physiological Integrity 14. In teaching parents how to minimize or prevent bleeding episodes when the child is myelosuppressed, the nurse includes what information? a. Meticulous mouth care is essential to avoid mucositis. b. Rectal temperatures are necessary to monitor for infection. c. Intramuscular injections are preferred to intravenous ones. d. Platelet transfusions are given to maintain a count greater than 50,000/mm3. The decrease in blood platelets secondary to the myelosuppression of chemotherapy can cause an increase in bleeding. The child and family are taught how to perform good oral hygiene to minimize gingival bleeding and mucositis. Rectal temperatures are avoided to minimize the risk of ulceration. Hygiene is also emphasized. Intramuscular injections are avoided because of the risk of bleeding into the muscle and of infection. Platelet transfusions are usually not given unless there is active bleeding or the platelet count is less than 10,000/mm3. The use of platelets when not necessary can contribute to antibody formation and increased destruction of platelets when transfused. DIF: Cognitive Level: Applying REF: p. 1392 TOP: Nursing Process: Planning MSC: Client Needs: Physiological Integrity 15. A school-age child with leukemia experienced severe nausea and vomiting when receiving chemotherapy for the first time. What is the most appropriate nursing action to prevent or minimize these reactions with subsequent treatments? a. Administer the chemotherapy between meals. b. Give an antiemetic before chemotherapy begins. c. Have the child bring favorite foods for snacks. d. Keep the child NPO (nothing by mouth) until nausea and vomiting subside. The most beneficial regimen to minimize nausea and vomiting associated with chemotherapy is to administer a 5-hydroxytryptamine-3 receptor antagonist (e.g., ondansetron) before the chemotherapy is begun. The goal is to prevent anticipatory signs and symptoms. The child will experience nausea with chemotherapy whether or not food is present in the stomach. Because some children develop aversions to foods eaten during chemotherapy, refraining from offering favorite foods is advised. Keeping the child NPO until nausea and vomiting subside will help with this episode, but the child will have discomfort and be at risk for dehydration. DIF: Cognitive Level: Applying REF: p. 1393 TOP: Nursing Process: Implementation MSC: Client Needs: Physiological Integrity 16. A young child with leukemia has anorexia and severe stomatitis. What approach should the nurse suggest that the parents try? a. Relax any eating pressures. b. Firmly insist that the child eat normally. c. Serve foods that are either hot or cold. d. Provide only liquids because chewing is painful. A multifaceted approach is necessary for children with severe stomatitis and anorexia. First, the parents should relax eating pressures. The nurse should suggest that the parents try soft, bland foods; normal saline or bicarbonate mouthwashes; and local anesthetics. Insisting that the child eat normally is not suggested. For some children, not eating may be a way to maintain some control. This can set the child and caregiver in opposition to each other. Hot and cold foods can be painful on ulcerated mucosal membranes. Substitution of high-calorie foods that the child likes and can eat should be used. DIF: Cognitive Level: Applying REF: p. 1394 TOP: Integrated Process: Teaching/Learning MSC: Client Needs: Physiological Integrity 17. The nurse is preparing a child for possible alopecia from chemotherapy. What information should the nurse include? a. Wearing hats or scarves is preferable to a wig. b. Expose head to sunlight to stimulate hair regrowth. c. Hair may have a slightly different color or texture when it regrows. d. Regrowth of hair usually begins 12 months after chemotherapy ends. Alopecia is a side effect of certain chemotherapeutic agents and cranial irradiation. When the hair regrows, it may be of a different color or texture. Children should choose the head covering they prefer. A wig should be selected similar to the child’s own hairstyle and color before the hair loss. The head should be protected from sunlight to avoid sunburn. The hair usually grows back within 3 to 6 months after the cessation of treatment. DIF: Cognitive Level: Applying REF: p. 1395 TOP: Integrated Process: Teaching/Learning MSC: Client Needs: Psychosocial Integrity 18. What pain management approach is most effective for a child who is having a bone marrow test? a. Relaxation techniques b. Administration of an opioid c. EMLA cream applied over site d. Conscious or unconscious sedation Children need explanations before each procedure that is being done to them. Effective pharmacologic and nonpharmacologic measures should be used to minimize pain associated with procedures. For bone marrow aspiration, conscious or unconscious sedation should be used. Relaxation, opioids, and EMLA can be used to augment the sedation. DIF: Cognitive Level: Applying REF: p. 1396 TOP: Nursing Process: Planning MSC: Client Needs: Physiological Integrity 19. The nurse is caring for a child receiving chemotherapy for leukemia. The child’s granulocyte count is 600/mm3 and platelet count is 45,000/mm3. What oral care should the nurse recommend for this child? a. Rinsing mouth with water b. Daily toothbrushing and flossing c. Lemon glycerin swabs for cleansing d. Wiping teeth with moistened gauze or Toothettes Oral care is essential for children receiving chemotherapy to prevent infections and other complications. When the child’s granulocyte count is above 500/mm3 and platelet count is above 40,000/mm3, daily brushing and flossing are recommended. Rinsing the mouth with water is not effective for oral hygiene. Lemon glycerin swabs are avoided because they have a drying effect on the mucous membranes, and the lemon may irritate eroded tissue and decay the child’s teeth. Wiping teeth with moistened gauze or Toothettes is recommended when the child’s granulocyte count is below 500/mm3 and platelet count is below 40,000/mm3. DIF: Cognitive Level: Applying REF: p. 1397 TOP: Nursing Process: Planning MSC: Client Needs: Physiological Integrity 20. What immunization should not be given to a child receiving chemotherapy for cancer? a. Tetanus vaccine b. Inactivated poliovirus vaccine c. Diphtheria, pertussis, tetanus (DPT) d. Measles, mumps, rubella (MMR) The vaccine used for MMR is a live virus and can cause serious disease in immunocompromised children. The tetanus vaccine, inactivated poliovirus vaccine, and DPT are not live vaccines and can be given to immunosuppressed children. The immune response is likely to be suboptimum, so delaying vaccination is usually recommended. DIF: Cognitive Level: Analyzing REF: p. 1397 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 21. What description identifies the pathophysiology of leukemia? a. Increased blood viscosity b. Abnormal stimulation of the first stage of coagulation process c. Unrestricted proliferation of immature white blood cells (WBCs) d. Thrombocytopenia from an excessive destruction of platelets Leukemia is a group of malignant disorders of the bone marrow and lymphatic system. It is defined as an unrestricted proliferation of immature WBCs in the blood-forming tissues of the body. Increased blood viscosity may result secondary to the increased number of WBCs. The coagulation process is unaffected by leukemia. Thrombocytopenia may occur secondary to the overproduction of WBCs in the bone marrow. DIF: Cognitive Level: Understanding REF: p. 1399 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 22. A child with leukemia is receiving intrathecal chemotherapy to prevent which condition? a. Infection b. Brain tumor c. Central nervous system (CNS) disease d. Drug side effects Children with leukemia are at risk for invasion of the CNS with leukemic cells. CNS prophylactic therapy is indicated. Intrathecal chemotherapy does not prevent infection or drug side effects. A brain tumor in a child with leukemia would be a second tumor, and additional appropriate therapy would be indicated. DIF: Cognitive Level: Applying REF: p. 1401 TOP: Nursing Process: Planning MSC: Client Needs: Physiological Integrity 23. A parent tells the nurse that 80% of children with the same type of leukemia as his son’s have a 5-year survival. He believes that because another child on the same protocol as his son has just died, his son now has a better chance of success. What is the best response by the nurse? a. “It is sad for the other family but good news for your child.” b. “Each child has an 80% likelihood of 5-year survival.” c. “The data suggest that 20% of the children in the clinic will die. There are still many hurdles for your son.” d. “You should avoid the grieving family because you will be benefiting from their loss.” This is a common misconception for parents. The success data are based on numerous factors, including the effectiveness of the protocol and the child’s response. These are aggregate data that apply to each child and do not depend on the success or failure in other children. The failure of one child in a protocol does not improve the success rate for other children. Although the son does face more hurdles, these are aggregate data, not specific to the clinic. It may be difficult for this family to be supportive given their concerns about their child. Families usually form support groups in pediatric oncology settings, and support during bereavement is common. DIF: Cognitive Level: Applying REF: p. 1421 TOP: Integrated Process: Teaching/Learning MSC: Client Needs: Psychosocial Integrity 24. What is a common clinical manifestation of Hodgkin disease? a. Petechiae b. Bone and joint pain c. Painful, enlarged lymph nodes d. Nontender enlargement of lymph nodes Asymptomatic, enlarged cervical or supraclavicular lymphadenopathy is the most common presentation of Hodgkin disease. Petechiae are usually associated with leukemia. Bone and joint pain are not likely in Hodgkin disease. The enlarged nodes are rarely painful. DIF: Cognitive Level: Understanding REF: p. 1403 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 25. What are the most common clinical manifestations of brain tumors in children? a. Headaches and vomiting b. Blurred vision and ataxia c. Hydrocephalus and clumsy gait d. Fever and poor fine motor control Headaches, especially on awakening, and vomiting that is not related to feeding are the most common clinical manifestations of brain tumors in children. Diplopia (double vision), not blurred vision, can be a presenting sign of brainstem glioma. Ataxia is a clinical manifestation of brain tumors, but headaches and vomiting are the most common. Hydrocephalus can be a presenting sign in infants when the sutures have not closed. Children at this age are usually not walking steadily. Poor fine motor coordination may be a presenting sign of astrocytoma, but headaches and vomiting are the most common presenting signs of brain tumors. DIF: Cognitive Level: Understanding REF: p. 1406 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 26. A 5-year-old child is being prepared for surgery to remove a brain tumor. Preparation for surgery should be based on which information? a. Removal of the tumor will stop the various signs and symptoms. b. Usually the postoperative dressing covers the entire scalp. c. He is not old enough to be concerned about his head being shaved. d. He is not old enough to understand the significance of the brain. The child should be told what he will look and feel like after surgery. This includes the anticipated size of the dressing. The nurse can demonstrate on a doll the expected size and shape of the dressing. Some of the symptoms may be alleviated by removal of the tumor, but postsurgical headaches and cerebellar symptoms such as ataxia may be aggravated. Children should be prepared for the loss of their hair, and it should be removed in a sensitive, positive manner if the child is awake. Children at this age have poorly defined body boundaries and little knowledge of internal organs. Intrusive experiences are frightening, especially those that disrupt the integrity of the skin. DIF: Cognitive Level: Applying REF: p. 1409 TOP: Integrated Process: Teaching/Learning MSC: Client Needs: Psychosocial Integrity 27. Essential postoperative nursing management of a child after removal of a brain tumor includes which nursing care? a. Turning and positioning every 2 hours b. Measuring all fluid intake and output c. Changing the dressing when it becomes soiled d. Using maximum lighting to ensure accurate observations After brain surgery, cerebral edema is a risk. Careful monitoring is essential. All fluids, including intravenous antibiotics, are included in the intake. Turning and positioning depend on the surgical procedure. When large tumors are removed, the child is usually not positioned on the operative side. The dressing is not changed. It is reinforced with gauze after the amount of drainage is marked and estimated. A quiet, dimly lit environment is optimum to decrease stimulation and relieve discomfort such as headaches. DIF: Cognitive Level: Applying REF: p. 1410 TOP: Nursing Process: Planning MSC: Client Needs: Physiological Integrity 28. An adolescent is scheduled for a leg amputation in 2 days for treatment of osteosarcoma. What approach should the nurse implement? a. Answer questions with straightforward honesty. b. Avoid discussing the seriousness of the condition. c. Explain that although the amputation is difficult, it will cure the cancer. d. Help the adolescent accept the amputation as better than a long course of chemotherapy. Honesty is essential to gain the child’s cooperation and trust. The diagnosis of cancer should not be disguised with falsehoods. The adolescent should be prepared for the surgery so there is time for reflection about the diagnosis and subsequent treatment. This allows questions to be answered. To accept the need for radical surgery, the child must be aware of the lack of alternatives for treatment. Amputation is necessary, but it will not guarantee a cure. Chemotherapy is an integral part of the therapy with surgery. The child should be informed of the need for chemotherapy and its side effects before surgery. DIF: Cognitive Level: Analyzing REF: p. 1413 TOP: Integrated Process: Teaching/Learning MSC: Client Needs: Psychosocial Integrity 29. What is an important priority in dealing with the child suspected of having Wilms tumor? a. Intervening to minimize bleeding b. Monitoring temperature for infection c. Ensuring the abdomen is protected from palpation d. Teaching parents how to manage the parenteral nutrition Wilms tumor, or nephroblastoma, is the most common malignant renal and intraabdominal tumor of childhood. The abdomen is protected, and palpation is avoided. Careful handling and bathing are essential to prevent trauma to the tumor site. Before chemotherapy, the child is not myelosuppressed. Bleeding is not usually a risk. Infection is a concern after surgery and during chemotherapy, not before surgery. Parenteral therapy is not indicated before surgery. DIF: Cognitive Level: Understanding REF: p. 1415 TOP: Nursing Process: Planning MSC: Client Needs: Physiological Integrity 30. The mother of an infant tells the nurse that sometimes there is a whitish “glow” in the pupil of his eye. The nurse should suspect which condition? a. Brain tumor b. Retinoblastoma c. Neuroblastoma d. Rhabdomyosarcoma When the nurse examines the eye, the light will reflect off of the tumor, giving the eye a whitish appearance. This is called a cat’s eye reflex. Brain tumors are not usually visible. Neuroblastoma usually arises from the adrenal medulla and sympathetic nervous system. The most common presentation sites are in the abdomen, head, neck, or pelvis. Supraorbital ecchymosis may be present with distant metastasis. Rhabdomyosarcoma is a soft tissue tumor that derives from skeletal muscle undifferentiated cells. DIF: Cognitive Level: Understanding REF: p. 1418 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 31. The nurse is caring for a 6-year-old child with acute lymphoblastic leukemia (ALL). The parent states, “My child has a low platelet count, and we are being discharged this afternoon. What do I need to do at home?” What statement is most appropriate for the nurse to make? a. “You should give your child aspirin instead of acetaminophen for fever or pain.” b. “Your child should avoid contact sports or activities that could cause bleeding.” c. “You should feed your child a bland, soft, moist diet for the next week.” d. “Your child should avoid large groups of people for the next week.” A child with a low platelet count needs to avoid activities that could cause bleeding such as playing contact sports, climbing trees, using playground equipment, or bike riding. The child should be given acetaminophen, not aspirin, for fever or pain; the child does not need to be on a soft, bland diet or avoid large groups of people because of the low platelet count. DIF: Cognitive Level: Applying REF: p. 1392 TOP: Nursing Process: Planning MSC: Client Needs: Physiological Integrity 32. One pediatric oncologic emergency is acute tumor lysis syndrome. Symptoms that this may be occurring include what? a. Muscle cramps and tetany b. Respiratory distress and cyanosis c. Thrombocytopenia and sepsis d. Upper extremity edema and neck vein distension Risk factors for development of tumor lysis syndrome include a high white blood cell count at diagnosis, large tumor burden, sensitivity to chemotherapy, and high proliferative rate. In addition to the described metabolic abnormalities, children may develop a spectrum of clinical symptoms, including flank pain, lethargy, nausea and vomiting, muscle cramps, pruritus, tetany, and seizures. Respiratory distress and cyanosis occur with hyperleukocytosis. Thrombocytopenia and sepsis occur with disseminated intravascular coagulation. Upper extremity edema and neck vein distention occur with superior vena cava syndrome. DIF: Cognitive Level: Analyzing REF: p. 1386 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 33. A child has an absolute neutrophil count (ANC) of 500/mm3. The nurse should expect to be administering which prescribed treatment? a. Platelets b. Packed red blood cells c. Zofran (ondansetron) d. G-CSF (Neupogen) daily G-CSF (filgrastim [Neupogen], pegfilgrastim [Neulasta]) directs granulocyte development and can decrease the duration of neutropenia following immunosuppressive therapy. G-CSF is discontinued when the ANC surpasses 10,000/mm3. DIF: Cognitive Level: Applying REF: p. 1391 TOP: Nursing Process: Planning MSC: Client Needs: Physiological Integrity 34. What specific gravity of the urine is desired so that hemorrhagic cystitis is prevented? a. 1.035 b. 1.030 c. 1.025 d. 1.005 Sterile hemorrhagic cystitis is a side effect of chemical irritation to the bladder from chemotherapy or radiotherapy. It can be prevented by a liberal oral or parenteral fluid intake (at least one and a half times the recommended daily fluid requirement). The urine should be dilute so 1.005 is the expected specific gravity. DIF: Cognitive Level: Analyzing REF: p. 1395 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 35. A child, age 10 years, has a neuroblastoma and is in the hospital for additional chemotherapy treatments. What laboratory values are most likely this child’s? a. White blood cell count, 17,000/mm3; hemoglobin, 15 g/dl b. White blood cell count, 3,000/mm3; hemoglobin, 11.5 g/dl c. Platelets, 450,000/mm3; hemoglobin, 12 g/dl d. White blood cell count, 10,000/mm3; platelets, 175,000/mm3 Chemotherapy is the mainstay of therapy for extensive local or disseminated neuroblastoma. The drugs of choice are vincristine, doxorubicin, cyclophosphamide, cisplatin, etoposide, ifosfamide, and carboplatin. These cause immunosuppression, so the laboratory values will indicate a low white blood cell count and hemoglobin. DIF: Cognitive Level: Analyzing REF: p. 1411 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 36. Calculate the absolute neutrophil count (ANC) for the following: WBC count of 5000 mm3; neutrophils (segs) of 10%; and nonsegmented neutrophils (bands) of 12%. a. 110/mm3 b. 500/mm3 c. 1100/mm3 d. 5000/mm3 Determine the total percentage of neutrophils (“polys,” or “segs,” and “bands”). Multiply white blood cell (WBC) count by percentage of neutrophils. WBC = 1000/mm3, neutrophils = 7%, and nonsegmented neutrophils (bands) = 7% Step 1: 10% + 12% = 22% Step 2: 0.22 5000 = 1100/mm3 ANC DIF: Cognitive Level: Applying REF: p. 1391 TOP: Nursing Process: Evaluation MSC: Client Needs: Physiological Integrity 37. A child has been diagnosed with a Wilms tumor. What should preoperative nursing care include? a. Careful bathing and handling b. Monitoring of behavioral status c. Maintenance of strict isolation d. Administration of packed red blood cells Careful bathing and handling are important in preventing trauma to the Wilms tumor site. DIF: Cognitive Level: Applying REF: p. 1416 TOP: Nursing Process: Implementation MSC: Client Needs: Safe and Effective Care Environment 38. What is appropriate mouth care for a toddler with mucosal ulceration related to chemotherapy? a. Mouthwashes with plain saline b. Lemon glycerin swabs for cleansing c. Mouthwashes with hydrogen peroxide d. Swish and swallow with viscous lidocaine Administering mouth care is particularly difficult in infants and toddlers. A satisfactory method of cleaning the gums is to wrap a piece of gauze around a finger; soak it in saline or plain water; and swab the gums, palate, and inner cheek surfaces with the finger. Mouth rinses are best accomplished with plain water or saline because the child cannot gargle or spit out excess fluid. Avoid agents such as lemon glycerin swabs and hydrogen peroxide because of the drying effects on the mucosa. Lidocaine should be avoided in young children. DIF: Cognitive Level: Applying REF: p. 1385 TOP: Nursing Process: Implementation MSC: Client Needs: Physiological Integrity 39. The nurse should expect to care for which age of child if the admitting diagnosis is retinoblastoma? a. Infant or toddler b. Preschool- or school-age child c. School-age or adolescent child d. Adolescent The average age of the child at the time of diagnosis is 2 years, and bilateral and hereditary disease is diagnosed earlier than unilateral and nonhereditary disease. DIF: Cognitive Level: Understanding REF: p. 1418 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 40. Postoperative positioning for a child who has had a medulloblastoma brain tumor (infratentorial) removed should be which? a. Trendelenburg b. Head of bed elevated above heart level c. Flat on operative side with pillows behind the head d. Flat, on either side with pillows behind the back The child with an infratentorial procedure is usually positioned flat and on either side. Pillows should be placed against the child’s back, not head, to maintain the desired position. The Trendelenburg position is contraindicated in both infratentorial and supratentorial surgeries because it increases intracranial pressure and the risk of hemorrhage. DIF: Cognitive Level: Applying REF: p. 1410 TOP: Nursing Process: Implementation MSC: Client Needs: Physiological Integrity 41. A child is receiving vincristine (Oncovin). The nurse should monitor for which side effect of this medication? a. Diarrhea b. Photosensitivity c. Constipation d. Ototoxicity Vincristine, and to a lesser extent vinblastine, can cause various neurotoxic effects. One of the more common neurotoxic effects is severe constipation caused from decreased bowel innervation. DIF: Cognitive Level: Applying REF: p. 1412 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 42. What chemotherapeutic agent can cause an anaphylactic reaction? a. Prednisone (Deltasone) b. Vincristine (Oncovin) c. L-Asparaginase (Elspar) d. Methotrexate (Trexall) A potentially fatal complication is anaphylaxis, especially from L-asparaginase, bleomycin, cisplatin, and etoposide (VP-16). DIF: Cognitive Level: Understanding REF: p. 1383 TOP: Nursing Process: Assessment MSC: Client Needs: Safe and Effective Care Environment 43. A child with cancer being treated with chemotherapy is receiving a platelet transfusion. The nurse understands that the transfused platelets should survive the body for how many days? a. 1 to 3 days b. 4 to 6 days c. 7 to 9 days d. 10 to 12 days Transfused platelets generally survive in the body for 1 to 3 days. The peak effect is reached in about 1 hour and decreased by half in 24 hours. DIF: Cognitive Level: Understanding REF: p. 1392 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 44. Daily toothbrushing and flossing can be encouraged for the child on chemotherapy when the platelet count is above which? a. 10,000/mm3 b. 20,000/mm3 c. 30,000/mm3 d. 40,000/mm3 Daily toothbrushing and flossing are encouraged in children with platelet counts above 40,000/mm3. DIF: Cognitive Level: Analyzing REF: p. 1397 TOP: Nursing Process: Evaluation MSC: Client Needs: Physiological Integrity 45. A parent of a hospitalized child on chemotherapy asks the nurse if a sibling of the hospitalized child should receive the varicella vaccination. The nurse should give which response? a. The sibling can get a varicella vaccination. b. The sibling should not get a varicella vaccination. c. The sibling should wait until the child is finished with chemotherapy. d. The sibling should get varicella-zoster immune globulin if exposed to chickenpox. Siblings and other family members can receive the live measles, mumps, and rubella vaccine and the varicella vaccine without risk to the child who is immunosuppressed. DIF: Cognitive Level: Applying REF: p. 1397 TOP: Integrated Process: Teaching/Learning MSC: Client Needs: Health Promotion and Maintenance 46. The nurse is collecting a 24-hour urine sample on a child with suspected diagnosis of neuroblastoma. What finding in the urine is expected with neuroblastomas? a. Ketones b. Catecholamines c. Red blood cells d. Excessive white blood cells Neuroblastomas, particularly those arising on the adrenal glands or from a sympathetic chain, excrete the catecholamines epinephrine and norepinephrine. Urinary excretion of catecholamines is detected in approximately 95% of children with adrenal or sympathetic tumors. DIF: Cognitive Level: Analyzing REF: p. 1412 TOP: Nursing Process: Evaluation MSC: Client Needs: Physiological Integrity 47. A child with osteosarcoma is experiencing phantom limb pain after an amputation. What prescribed medication is effective for short-term phantom pain relief? a. Phenytoin (Dilantin) b. Gabapentin (Neurontin) c. Valproic Acid (Depakote) d. Phenobarbital (Phenobarbital) A recent Cochrane review reported that various medications have been used for phantom limb pain but complete pain relief has been unsuccessful. Morphine, gabapentin, and ketamine are effective for short-term pain relief. DIF: Cognitive Level: Applying REF: p. 1414 TOP: Nursing Process: Implementation MSC: Client Needs: Physiological Integrity MULTIPLE RESPONSE 1. The nurse is precepting a new graduate nurse at an ambulatory pediatric hematology and oncology clinic. What cardinal signs of cancer in children should the nurse make the new nurse aware of? (Select all that apply.) a. Sudden tendency to bruise easily b. Transitory, generalized pain c. Frequent headaches d. Excessive, rapid weight gain e. Gradual, steady fever f. Unexplained loss of energy , C, F The cardinal signs of cancer in children include a sudden tendency to bruise easily; frequent headaches, often with vomiting; and an unexplained loss of energy. Other cardinal signs include persistent, localized pain; excessive, rapid weight loss; and a prolonged, unexplained fever. DIF: Cognitive Level: Applying REF: p. 1381 TOP: Integrated Process: Teaching/Learning MSC: Client Needs: Physiological Integrity 2. A child on chemotherapy has developed rectal ulcers. What interventions should the nurse teach to the child and parents to relieve the discomfort of rectal ulcers? (Select all that apply.) a. Warm sitz baths b. Use of stool softeners c. Record bowel movements d. Use of an opioid for discomfort e. Occlusive ointment applied to the area , B, C, E If rectal ulcers develop, meticulous toilet hygiene, warm sitz baths after each bowel movement, and an occlusive ointment applied to the ulcerated area promote healing; the use of stool softeners is necessary to prevent further discomfort. Parents should record bowel movements because the child may voluntarily avoid defecation to prevent discomfort. Opioids would cause increased constipation. DIF: Cognitive Level: Applying REF: p. 1394 TOP: Integrated Process: Teaching/Learning MSC: Client Needs: Physiological Integrity 3. What are favorable prognostic criteria for acute lymphoblastic leukemia? (Select all that apply.) a. Male gender b. CALLA positive c. Early pre–B cell d. 2 to 10 years of age e. Leukocyte count ?7?50,000/mm3 , C, D Favorable prognostic criteria for acute lymphoblastic leukemia include CALLA positive, early pre–B cell, and age 2 to 10 years. Leukocyte count less, not greater, than 50,000/mm3 and female, not male, gender are favorable prognostic criteria. DIF: Cognitive Level: Analyzing REF: p. 1400 TOP: Nursing Process: Evaluation MSC: Client Needs: Physiological Integrity 4. The nurse should teach the family that which residual disabilities can occur for a child being treated for a brain tumor? (Select all that apply.) a. Ataxia b. Anorexia c. Dysphagia d. Sensory deficits e. Crania nerve palsies , C, D, E Even with children who are long-term survivors after treatment for a brain tumor, residual disabilities, such as short stature, cranial nerve palsies, sensory defects, motor abnormalities (especially ataxia), intellectual deficits, dysphagia, dysgraphia, and behavioral problems, may occur. Anorexia is not a residual disability. DIF: Cognitive Level: Applying REF: p. 1411 TOP: Integrated Process: Teaching/Learning MSC: Client Needs: Health Promotion and Maintenance 5. The nurse is caring for a child with retinoblastoma that was treated with an enucleation. What interventions should the nurse plan for care of an eye socket after enucleation? (Select all that apply.) a. Clean the prosthesis. b. Change the eye pad daily. c. Keep the opposite eye covered initially. d. Irrigate the socket daily with a prescribed solution. e. Apply a prescribed antibiotic ointment after irrigation. , D, E Care of the socket is minimal and easily accomplished. The wound itself is clean and has little or no drainage. If an antibiotic ointment is prescribed, it is applied in a thin line on the surface of the tissues of the socket. To cleanse the site, an irrigating solution may be ordered and is instilled daily or more frequently if necessary before application of the antibiotic ointment. The dressing consists of an eye pad changed daily. The prosthesis is not placed until the socket has healed. The opposite eye is not covered. DIF: Cognitive Level: Applying REF: p. 1420 TOP: Nursing Process: Implementation MSC: Client Needs: Physiological Integrity 6. What guidelines should the nurse follow when handling chemotherapeutic agents? (Select all that apply.) a. Use clean technique. b. Prepare medications in a safety cabinet. c. Wear gloves designed for handling chemotherapy. d. Wear face and eye protection when splashing is possible. e. Discard gloves and protective clothing in a special container. , C, D, E Safe handling of chemotherapeutic agents includes preparing medications in a safety cabinet, wearing gloves designed for handling chemotherapy, wearing face and eye protection when splashing is possible, and discarding gloves and protective clothing in a special container. Aseptic, not clean, technique should be used. DIF: Cognitive Level: Applying REF: p. 1384 TOP: Nursing Process: Implementation MSC: Client Needs: Safe and Effective Care Environment 7. What strategies should the nurse implement to increase nutritional intake for the child receiving chemotherapy? (Select all that apply.) a. Allow the child any food tolerated. b. Fortify foods with nutritious supplements. c. Allow the child to be involved in food selection. d. Encourage the parents to place pressure on the importance of eating. e. Encourage the child to eat favorite foods during infusion of chemotherapy medications. , B, C To increase nutritional intake for the child receiving chemotherapy, the nurse should allow the child any food tolerated, fortify foods with nutritious supplements, and allow the child to be involved in food selection. The parents should be encouraged to reduce pressure placed on eating. Some children develop aversions to certain foods if they are eaten during chemotherapy. It is best to refrain from offering the child’s favorite foods while the child is receiving chemotherapy. DIF: Cognitive Level: Applying REF: p. 1389 TOP: Nursing Process: Implementation MSC: Client Needs: Physiological Integrity COMPLETION 1. A health care provider prescribes ondansetron (Zofran) 0.15 mg/kg intravenously (IV) 30 minutes before chemotherapy for a child with acute lymphoblastic leukemia. The child weighs 22 kg. The medication label states: “Ondansetron (Zofran) 2 mg/1 ml.” The nurse prepares to administer the dose. How many milliliters will the nurse prepare to administer the dose? Fill in the blank. Round your answer to one decimal place. ________________ ANS: 1.7 Follow the formula for dosage calculation. 22 0.15 = 3.3 mg as the dose Desired ———– Volume = ml per dose Available 3.3 mg ———– 1 ml = 1.65 ml round to 1.7 ml 2 mg DIF: Cognitive Level: Applying REF: p. 1393 TOP: Nursing Process: Implementation MSC: Client Needs: Physiological Integrity 2. The health care provider prescribes ceftazidime (Fortaz) 75 mg per intravenous piggyback (IVPB) every 8 hours for a child with cancer admitted with fever and neutropenia. The pharmacy sends the medication to the unit in a 50-ml bag with directions to run the medication over 30 minutes. What milliliters per hour will the nurse set the intravenous pump to run the medication over 30 minutes? Fill in the blank and record your answer in a whole number. _____________ ANS: 100 Perform the calculation. 50 ml ________ 60 minutes = 100 ml/hr 30 minutes DIF: Cognitive Level: Applying REF: p. 1390 TOP: Nursing Process: Implementation MSC: Client Needs: Physiological Integrity 3. The health care provider prescribes vancomycin 200 mg per intravenous piggyback (IVPB) every 6 hours for a child with cancer admitted to the hospital for fever and neutropenia. The pharmacy sends the medication to the unit in a 240-ml bag with directions to run the medication over 120 minutes. What milliliters per hour will the nurse set the intravenous pump to run the medication over 120 minutes? Fill in the blank and record your answer in a whole number. _____________ ANS: 120 Perform the calculation. Convert the minutes to hours = 120/60 = 2 hours 240 ml ________ = 120 ml/hr 2 hours DIF: Cognitive Level: Applying REF: p. 1390 TOP: Nursing Process: Implementation MSC: Client Needs: Physiological Integrity 4. A health care provider prescribes Osmitrol (mannitol) 0.25 g/kg intravenously (IV) every 6 hours for a child after a brain tumor removal. The child weighs 20 kg. The medication label states: “Osmitrol (Mannitol) 250 mg/1 ml.” The nurse prepares to administer the dose. How many milliliters will the nurse prepare to administer the dose? Fill in the blank. Record your answer in a whole number. ________________ ANS: 20 Calculate the dose. 0.25 g 20 = 5 g convert to mg = 5000 mg Follow the formula for dosage calculation. Desired ———– Volume = ml per dose Available 5000 mg ———– 1 ml = 20 ml 250 mg DIF: Cognitive Level: Applying REF: p. 1410 TOP: Nursing Process: Implementation MSC: Client Needs: Safe and Effective Care Environment 5. Calculate the absolute neutrophil count for a child with a WBC = 3000/mm3, neutrophils = 10%, and nonsegmented neutrophils (bands) = 10%. Record your answer below in a whole number. _____________ ANS: 600 Perform the calculation Determine the total percentage of neutrophils (“polys,” or “segs,” and “bands”). Multiply white blood cell (WBC) count by percentage of neutrophils. WBC = 3000/mm3, neutrophils = 10%, and nonsegmented neutrophils (bands) = 10% Step 1: 10% + 10% = 20% Step 2: 0.2 3000 = 600/mm3 ANC DIF: Cognitive Level: Applying REF: p. 1391 TOP: Nursing Process: Evaluation MSC: Client Needs: Physiological Integrity 6. Calculate the absolute neutrophil count for a child with a WBC = 6000/mm3, neutrophils = 18%, and nonsegmented neutrophils (bands) = 20%. Record your answer below in a whole number. ____________ ANS: 2280 Perform the calculation Determine the total percentage of neutrophils (“polys,” or “segs,” and “bands”). Multiply white blood cell (WBC) count by percentage of neutrophils. WBC = 6000/mm3, neutrophils = 18%, nonsegmented neutrophils (bands) = 20% Step 1: 18% + 20% = 38% Step 2: 0.38 6000 = 2280/mm3 ANC DIF: Cognitive Level: Applying REF: p. 1391 TOP: Nursing Process: Evaluation MSC: Client Needs: Physiological Integrity 7. Calculate the absolute neutrophil count for a child with a WBC = 10,000/mm3, neutrophils = 25%, and nonsegmented neutrophils (bands) = 22%. Record your answer in a whole number. _____________ ANS: 4700 Perform the calculation Determine the total percentage of neutrophils (“polys,” or “segs,” and “bands”). Multiply white blood cell (WBC) count by percentage of neutrophils. WBC = 10,000/mm3, neutrophils = 25%, and nonsegmented neutrophils (bands) = 22% Step 1: 25% + 22% = 47% Step 2: 0.47 10,000 = 4700/mm3 ANC DIF: Cognitive Level: Applying REF: p. 1391 TOP: Nursing Process: Evaluation MSC: Client Needs: Physiological Integrity 8. Calculate the absolute neutrophil count for a child with a WBC = 15,000/mm3, neutrophils = 29%, and nonsegmented neutrophils (bands) = 29%. Record your answer in a whole number. _____________ ANS: 8700 Perform the calculation Determine the total percentage of neutrophils (“polys,” or “segs,” and “bands”). Multiply white blood cell (WBC) count by percentage of neutrophils. WBC = 3000/mm3, neutrophils = 10%, and nonsegmented neutrophils (bands) = 10% Step 1: 29% + 29% = 58% Step 2: 0.58 15,000 = 8700/mm3 ANC DIF: Cognitive Level: Applying REF: p. 1391 TOP: Nursing Process: Evaluation MSC: Client Needs: Physiological Integrity Chapter 32: The Child with Cerebral Dysfunction MULTIPLE CHOICE 1. An injury to which part of the brain will cause a coma? a. Brainstem b. Cerebrum c. Cerebellum d. Occipital lobe Injury to the brainstem results in stupor and coma. Signs of damage to the cerebrum are specific to the involved area. Individuals with frontal lobe injury may have impaired memory, personality changes, or altered intellectual functioning. Individuals with damage to the cerebellum have difficulties with coordination of muscle movements, including ataxia and nystagmus. Impaired vision and functional blindness result from injury to the occipital lobe. DIF: Cognitive Level: Understanding REF: p. 1425 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 2. What finding is a clinical manifestation of increased intracranial pressure (ICP) in children? a. Low-pitched cry b. Sunken fontanel c. Diplopia, blurred vision d. Increased blood pressure Diplopia and blurred vision are signs of increased ICP in children. A high-pitched cry and a tense or bulging fontanel are characteristic of increased ICP. Increased blood pressure, common in adults, is rarely seen in children. DIF: Cognitive Level: Analyzing REF: p. 1428 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 3. What are quick, jerky, grossly uncoordinated, irregular movements that may disappear on relaxation called? a. Twitching b. Spasticity c. Choreiform movements d. Associated movements Quick, jerky, grossly uncoordinated, irregular movements that may disappear on relaxation are called choreiform movements. Twitching is defined as spasmodic movements of short duration. Spasticity is the prolonged and steady contraction of a muscle characterized by clonus (alternating relaxation and contraction of the muscle) and exaggerated reflexes. Associated movements are the voluntary movement of one muscle accompanied by the involuntary movement of another muscle. DIF: Cognitive Level: Understanding REF: p. 1430 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 4. What term is used when a patient remains in a deep sleep, responsive only to vigorous and repeated stimulation? a. Coma b. Stupor c. Obtundation d. Persistent vegetative state Stupor exists when the child remains in a deep sleep, responsive only to vigorous and repeated stimulation. Coma is the state in which no motor or verbal response occurs to noxious (painful) stimuli. Obtundation describes a level of consciousness in which the child is arousable with stimulation. Persistent vegetative state describes the permanent loss of function of the cerebral cortex. DIF: Cognitive Level: Understanding REF: p. 1431 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 5. What term is used to describe a child’s level of consciousness when the child is arousable with stimulation? a. Stupor b. Confusion c. Obtundation d. Disorientation Obtundation describes a level of consciousness in which the child is arousable with stimulation. Stupor is a state in which the child remains in a deep sleep, responsive only to vigorous and repeated stimulation. Confusion is impaired decision making. Disorientation is confusion regarding time and place. DIF: Cognitive Level: Understanding REF: p. 1431 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 6. The nurse is closely monitoring a child who is unconscious after a fall and notices that the child suddenly has a fixed and dilated pupil. How should the nurse interpret this? a. Eye trauma b. Brain death c. Severe brainstem damage d. Neurosurgical emergency The sudden appearance of a fixed and dilated pupil(s) is a neurosurgical emergency. The nurse should immediately report this finding. Although a dilated pupil may be associated with eye trauma, this child has experienced a neurologic insult. One fixed and dilated pupil is not suggestive of brain death. Pinpoint pupils or fixed, bilateral pupils for more than 5 minutes are indicative of brainstem damage. The unilateral fixed and dilated pupil is suggestive of damage on the same side of the brain. DIF: Cognitive Level: Analyzing REF: p. 1433 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 7. The nurse is caring for a child with severe head trauma after a car accident. What is an ominous sign that often precedes death? a. Delirium b. Papilledema c. Flexion posturing d. Periodic or irregular breathing Periodic or irregular breathing is an ominous sign of brainstem (especially medullary) dysfunction that often precedes complete apnea. Delirium is a state of mental confusion and excitement marked by disorientation for time and place. Papilledema is edema and inflammation of the optic nerve. It is commonly a sign of increased intracranial pressure. Flexion posturing is seen with severe dysfunction of the cerebral cortex or of the corticospinal tracts above the brainstem. DIF: Cognitive Level: Applying REF: p. 1429 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 8. What test is never performed on a child who is awake? a. Doll’s head maneuver b. Oculovestibular response c. Assessment of pyramidal tract lesions d. Funduscopic examination for papilledema The oculovestibular response (caloric test) involves the instillation of ice water into the ear of a comatose child. The caloric test is painful and is never performed on an awake child or one who has a ruptured tympanic membrane. The doll’s head maneuver, assessment of pyramidal tract lesions, and funduscopic examination for papilledema are not considered painful and can be performed on awake children. DIF: Cognitive Level: Analyzing REF: p. 1433 TOP: Nursing Process: Planning MSC: Client Needs: Physiological Integrity 9. The nurse is doing a neurologic assessment on a 2-month-old infant after a car accident. Moro, tonic neck, and withdrawal reflexes are present. How should the nurse interpret these findings? a. Neurologic health b. Severe brain damage c. Decorticate posturing d. Decerebrate posturing Moro, tonic neck, and withdrawal reflexes are three reflexes that are present in a healthy 2-month-old infant and are expected in this age group. DIF: Cognitive Level: Applying REF: p. 1434 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 10. The nurse is preparing a school-age child for computed tomography (CT) scan to assess cerebral function. The nurse should include what statement in preparing the child? a. “The scan will not hurt.” b. “Pain medication will be given.” c. “You will be able to move once the equipment is in place.” d. “Unfortunately no one can remain in the room with you during the test.” For CT scans, the child must be immobilized. It is important to emphasize to the child that at no time is the procedure painful. Pain medication is not required; however, sedation is sometimes necessary. The child will not be allowed to move and will be immobilized. Someone is able to remain with the child during the procedure. DIF: Cognitive Level: Applying REF: p. 1435 TOP: Integrated Process: Teaching/Learning MSC: Client Needs: Physiological Integrity 11. What is a nursing intervention to reduce the risk of increasing intracranial pressure (ICP) in an unconscious child? a. Suction the child frequently. b. Turn the child’s head side to side every hour. c. Provide environmental stimulation. d. Avoid activities that cause pain or crying. Unrelieved pain, crying, and emotional stress all contribute to increasing the ICP. Disturbing procedures should be carried out at the same time as therapies that reduce ICP, such as sedation. Suctioning is poorly tolerated by children. When necessary, it is preceded by hyperventilation with 100% oxygen. Turning the head side to side is contraindicated for fear of compressing the jugular vein. This would block the flow of blood from the brain, raising ICP. Nontherapeutic touch and environmental stimulation increase ICP. Minimizing both touch and environmental stimuli noise reduces ICP. DIF: Cognitive Level: Applying REF: p. 1439 TOP: Nursing Process: Implementation MSC: Client Needs: Physiological Integrity 12. What nursing intervention is appropriate when caring for an unconscious child? a. Avoid using narcotics or sedatives to provide comfort and pain relief. b. Change the child’s position infrequently to minimize the chance of increased intracranial pressure (ICP). c. Monitor fluid intake and output carefully to avoid fluid overload and cerebral edema. d. Give tepid sponge baths to reduce fevers above 38.3° C (101° F) because antipyretics are contraindicated. Often comatose patients cannot cope with the quantity of fluids that they normally tolerate. Overhydration must be avoided to prevent fatal cerebral edema. Narcotics and sedatives should be used as necessary to reduce pain and anxiety, which can increase ICP. The child’s position should be changed frequently to avoid complications such as pneumonia and skin breakdown. Antipyretics are the method of choice for fever reduction. DIF: Cognitive Level: Applying REF: p. 1439 TOP: Nursing Process: Implementation MSC: Client Needs: Physiological Integrity 13. What statement is descriptive of a concussion? a. Petechial hemorrhages cause amnesia. b. Visible bruising and tearing of cerebral tissue occur. c. It is a transient and reversible neuronal dysfunction. d. It is a slight lesion that develops remote from the site of trauma. A concussion is a transient, reversible neuronal dysfunction with instantaneous loss of awareness and responsiveness resulting from trauma to the head. Petechial hemorrhages on the superficial aspects of the brain along the point of impact are a type of contusion but are not necessarily associated with amnesia. A contusion is visible bruising and tearing of cerebral tissue. Contrecoup is a lesion that develops remote from the site of trauma as a result of an acceleration–deceleration injury. DIF: Cognitive Level: Understanding REF: p. 1444 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 14. What statement best describes a subdural hematoma? a. Bleeding occurs between the dura and the skull. b. Bleeding occurs between the dura and the cerebrum. c. Bleeding is generally arterial, and brain compression occurs rapidly. d. The hematoma commonly occurs in the parietotemporal region. A subdural hematoma is bleeding that occurs between the dura and the cerebrum as a result of a rupture of cortical veins that bridge the subdural space. An epidural hemorrhage occurs between the dura and the skull, is usually arterial with rapid brain concussion, and occurs most often in the parietotemporal region. DIF: Cognitive Level: Understanding REF: p. 1446 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 15. A 10-year-old boy on a bicycle has been hit by a car in front of a school. The school nurse immediately assesses airway, breathing, and circulation. What should be the next nursing action? a. Place the child on his side. b. Take the child’s blood pressure. c. Stabilize the child’s neck and spine. d. Check the child’s scalp and back for bleeding. After determining that the child is breathing and has adequate circulation, the next action is to stabilize the neck and spine to prevent any additional trauma. The child’s position should not be changed until the neck and spine are stabilized. Blood pressure is a later assessment. A less urgent but important assessment is inspection of the scalp for bleeding. DIF: Cognitive Level: Applying REF: p. 1448 TOP: Nursing Process: Implementation MSC: Client Needs: Physiological Integrity 16. A school-age child has sustained a head injury and multiple fractures after being thrown from a horse. The child’s level of consciousness is variable. The parents tell the nurse that they think their child is in pain because of periodic crying and restlessness. What is the most appropriate nursing action? a. Explain that analgesia is contraindicated with a head injury. b. Have the parents describe the child’s previous experiences with pain. c. Consult with a practitioner about what analgesia can be safely administered. d. Teach the parents that analgesia is unnecessary when the child is not fully awake and alert. A key nursing role is to provide sedation and analgesia for the child. Consultation with the appropriate practitioner is necessary to avoid conflict between the necessity to monitor the child’s neurologic status and to promote comfort and relieve anxiety. Analgesia can be safely used in individuals who have sustained head injuries. The child’s previous experiences with pain should be obtained as part of the assessment, but because of the severity of the injury, analgesia should be provided as soon as possible. Analgesia can decrease anxiety and resultant increased intracranial pressure. DIF: Cognitive Level: Applying REF: p. 1450 TOP: Integrated Process: Teaching/Learning MSC: Client Needs: Physiological Integrity 17. The nurse is assessing a child who was just admitted to the hospital for observation after a head injury. What clinical manifestation is the most essential part of the nursing assessment to detect early signs of a worsening condition? a. Posturing b. Vital signs c. Focal neurologic signs d. Level of consciousness The most important nursing observation is assessment of the child’s level of consciousness. Alterations in consciousness appear earlier in the progression of an injury than do alterations of vital signs or focal neurologic signs. Neurologic posturing is indicative of neurologic damage. DIF: Cognitive Level: Analyzing REF: p. 1451 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 18. A 5-year-old girl sustained a concussion when she fell out of a tree. In preparation for discharge, the nurse is discussing home care with her mother. What sign or symptom is considered a manifestation of postconcussion syndrome and does not necessitate medical attention? a. Vomiting b. Blurred vision c. Behavioral changes d. Temporary loss of consciousness The parents are advised of probable posttraumatic symptoms that may be expected. These include behavioral changes, sleep disturbances, emotional lability, and alterations in school performance. If the child is vomiting, has blurred vision, or has temporary loss of consciousness, she should be seen for evaluation. DIF: Cognitive Level: Understanding REF: p. 1451 TOP: Integrated Process: Teaching/Learning MSC: Client Needs: Physiological Integrity 19. An 18-month-old child is brought to the emergency department after being found unconscious in the family pool. What does the nurse identify as the primary problem in drowning incidents? a. Hypoxia b. Aspiration c. Hypothermia d. Electrolyte imbalance Hypoxia is the primary problem because it results in global cell damage, with different cells tolerating variable lengths of anoxia. Neurons sustain irreversible damage after 4 to 6 minutes of submersion. Severe neurologic damage occurs from hypoxia in 3 to 6 minutes. Aspiration of fluid does occur, resulting in pulmonary edema, atelectasis, airway spasm, and pneumonitis, which complicate the anoxia. Hypothermia occurs rapidly, except in hot tubs. Electrolyte imbalances do result, but they are not a major cause of morbidity and mortality. DIF: Cognitive Level: Understanding REF: p. 1453 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 20. The mother of a 1-month-old infant tells the nurse she worries that her baby will get meningitis like the child’s younger brother had when he was an infant. The nurse should base a response on which information? a. Meningitis rarely occurs during infancy. b. Often a genetic predisposition to meningitis is found. c. Vaccination to prevent all types of meningitis is now available. d. Vaccinations to prevent pneumococcal and Haemophilus influenzae type B meningitis are available. H. influenzae type B meningitis has been virtually eradicated in areas of the world where the vaccine is administered routinely. Bacterial meningitis remains a serious illness in children. It is significant because of the residual damage caused by undiagnosed and untreated or inadequately treated cases. The leading causes of neonatal meningitis are the group B streptococci and Escherichia coli organisms. Meningitis is an extension of a variety of bacterial infections. No genetic predisposition exists. Vaccinations are not available for all of the potential causative organisms. DIF: Cognitive Level: Applying REF: p. 1454 TOP: Integrated Process: Teaching/Learning MSC: Client Needs: Physiological Integrity 21. A toddler is admitted to the pediatric unit with presumptive bacterial meningitis. The initial orders include isolation, intravenous access, cultures, and antimicrobial agents. The nurse knows that antibiotic therapy will begin when? a. After the diagnosis is confirmed b. When the medication is received from the pharmacy c. After the child’s fluid and electrolyte balance is stabilized d. As soon as the practitioner is notified of the culture results Antimicrobial therapy is begun as soon as a presumptive diagnosis is made. The choice of drug is based on the most likely infective agent. Drug choice may be adjusted when the culture results are obtained. Waiting for culture results to begin therapy increases the risk of neurologic damage. Although fluid and electrolyte balance is important, there is no indication that this child is unstable. Antibiotic therapy would be a priority intervention. DIF: Cognitive Level: Analyzing REF: p. 1454 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 22. The nurse is planning care for a school-age child with bacterial meningitis. What intervention should be included? a. Keep environmental stimuli to a minimum. b. Have the child move her head from side to side at least every 2 hours. c. Avoid giving pain medications that could dull sensorium. d. Measure head circumference to assess developing complications. The room is kept as quiet as possible and environmental stimuli are kept to a minimum. Most children with meningitis are sensitive to noise, bright lights, and other external stimuli. The nuchal rigidity associated with meningitis would make moving the head from side to side a painful intervention. If pain is present, the child should be treated appropriately. Failure to treat can cause increased intracranial pressure. In this age group, the head circumference does not change. Signs of increased intracranial pressure would need to be assessed. DIF: Cognitive Level: Applying REF: p. 1458 TOP: Nursing Process: Planning MSC: Client Needs: Physiological Integrity 23. A young child’s parents call the nurse after their child is bitten by a raccoon in the woods. The nurse’s recommendation should be based on what knowledge? a. Antirabies prophylaxis must be initiated immediately. b. The child should be hospitalized for close observation. c. No treatment is necessary if thorough wound cleaning is done. d. Antirabies prophylaxis must be initiated as soon as clinical manifestations appear. Current therapy for a rabid animal bite consists of a thorough cleansing of the wound and passive immunization with human rabies immunoglobulin (HRIG) as soon as possible. Hospitalization is not necessary. The wound cleansing, passive immunization, and immunoglobulin administration can be done as an outpatient. The child needs to receive both HRIG and rabies vaccine. DIF: Cognitive Level: Applying REF: p. 1462 TOP: Integrated Process: Teaching/Learning MSC: Client Needs: Physiological Integrity 24. What intervention should be beneficial in reducing the risk of Reye syndrome? a. Immunization against the disease b. Medical attention for all head injuries c. Prompt treatment of bacterial meningitis d. Avoidance of aspirin for children with varicella or those suspected of having influenza Although the etiology of Reye syndrome is obscure, most cases follow a common viral illness, either varicella or influenza. A potential association exists between aspirin therapy and the development of Reye syndrome, so use of aspirin is avoided. No immunization currently exists for Reye syndrome. Reye syndrome is not correlated with head injuries or bacterial meningitis. DIF: Cognitive Level: Understanding REF: p. 1463 TOP: Nursing Process: Planning MSC: Client Needs: Physiological Integrity 25. What term refers to seizures that involve both hemispheres of the brain? a. Absence b. Acquired c. Generalized d. Complex partial Clinical observations of generalized seizures indicate that the initial involvement is from both hemispheres. Absence seizures have a sudden onset and are characterized by a brief loss of consciousness, a blank stare, and automatisms. Acquired seizure disorder is a result of a brain injury from a variety of factors; it is not a term that labels the type of seizure. Complex partial seizures are the most common seizures. They may begin with an aura and be manifested as repetitive involuntary activities without purpose, carried out in a dreamy state. DIF: Cognitive Level: Understanding REF: p. 1465 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 26. What is the initial clinical manifestation of generalized seizures? a. Confusion b. Feeling frightened c. Loss of consciousness d. Seeing flashing lights Loss of consciousness is a frequent occurrence in generalized seizures and is the initial clinical manifestation. Being confused, feeling frightened, and seeing flashing lights are clinical manifestations of a complex partial seizure. DIF: Cognitive Level: Understanding REF: p. 1466 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 27. What type of seizure may be difficult to detect? a. Absence b. Generalized c. Simple partial d. Complex partial Absence seizures may go unrecognized because little change occurs in the child’s behavior during the seizure. Generalized, simple partial, and complex partial all have clinical manifestations that are observable. DIF: Cognitive Level: Understanding REF: p. 1468 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 28. What is important to incorporate in the plan of care for a child who is experiencing a seizure? a. Describe and record the seizure activity observed. b. Suction the child during a seizure to prevent aspiration. c. Place a tongue blade between the teeth if they become clenched. d. Restrain the child when seizures occur to prevent bodily harm. When a child is having a seizure, the priority nursing care is observation of the child and seizure. The nurse then describes and records the seizure activity. The child is not suctioned during the seizure. If possible, the child should be placed on the side, facilitating drainage to prevent aspiration. DIF: Cognitive Level: Applying REF: p. 1437 TOP: Nursing Process: Implementation MSC: Client Needs: Physiological Integrity 29. A 10-year-old child, without a history of previous seizures, experiences a tonic-clonic seizure at school that lasts more than 5 minutes. Breathing is not impaired. Some postictal confusion occurs. What is the most appropriate initial action by the school nurse? a. Stay with child and have someone else call emergency medical services (EMS). b. Notify the parent and regular practitioner. c. Notify the parent that the child should go home. d. Stay with the child, offering calm reassurance. Because this is the child’s first seizure and it lasted more than 5 minutes, EMS should be called to transport the child, and evaluation should be performed as soon as possible. The nurse should stay with the recovering child while someone else notifies EMS. DIF: Cognitive Level: Applying REF: p. 1478 TOP: Nursing Process: Implementation MSC: Client Needs: Physiological Integrity 30. A child has been seizure free for 2 years. A father asks the nurse how much longer the child will need to take the antiseizure medications. How should the nurse respond? a. Medications can be discontinued at this time. b. The child will need to take the drugs for 5 years after the last seizure. c. A step-wise approach will be used to reduce the dosage gradually. d. Seizure disorders are a lifelong problem. Medications cannot be discontinued. A predesigned protocol is used to wean a child gradually off antiseizure medications, usually when the child is seizure free for 2 years. Medications must be gradually reduced to minimize the recurrence of seizures. The risk of recurrence is greatest within 6 months after discontinuation. DIF: Cognitive Level: Applying REF: p. 1478 TOP: Nursing Process: Teaching/Learning MSC: Client Needs: Physiological Integrity 31. A young adolescent experiences infrequent migraine episodes. What pharmacologic intervention is most likely to be prescribed? a. Opioid b. Lorazepam c. Ergotamine d. Sumatriptan Sumatriptan is a serotonin agonist at specific vascular serotonin receptor sites and causes vasoconstriction in large intracranial arteries. Opioids are used infrequently because they rarely work on the mechanism of pain. Lorazepam is a benzodiazepine that acts as an anxiolytic and sedative. It is not indicated for treatment of migraine episodes. Ergotamine, an -adrenergic blocker, is used for adult vascular headaches, but it is not used in adolescents because of the side effects. DIF: Cognitive Level: Understanding REF: p. 1483 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 32. The nurse is teaching the parents of a 3-year-old child who has been diagnosed with tonic-clonic seizures. What statement by the parent should indicate a correct understanding of the teaching? a. “I should attempt to restrain my child during a seizure.” b. “My child will need to avoid contact sports until adulthood.” c. “I should place a pillow under my child’s head during a seizure.” d. “My child will need to be taken to the emergency department [ED] after each seizure.” Parents should try to place a pillow or folded blanket under the child’s head for protection. The parent should not try to restrain the child during the seizure. The child does not need to go to the ED with each seizures; the nurse can teach parents certain criteria for when their child would need to be seen. Discussing what will happen in adulthood is not appropriate at this time. DIF: Cognitive Level: Analyzing REF: p. 1468 TOP: Integrated Process: Teaching/Learning MSC: Client Needs: Physiological Integrity 33. The nurse is caring for a 10-year-old child who has an acute head injury, has a pediatric Glasgow Coma Scale score of 9, and is unconscious. What intervention should the nurse include in the child’s care plan? a. Elevate the head of the bed 15 to 30 degrees with the head maintained in midline. b. Maintain an active, stimulating environment. c. Perform chest percussion and suctioning every 1 to 2 hours. d. Perform active range of motion and nontherapeutic touch every 8 hours. Nursing activities for children with head trauma and increased intracranial pressure (ICP) include elevating the head of the bed 15 to 30 degrees and maintaining the head in a midline position. The nurse should try to maintain a quiet, nonstimulating environment for a child with increased ICP. Chest percussion and suctioning should be performed judiciously because they can elevate ICP. Range of motion should be passive and nontherapeutic touch should be avoided because both of these activities can increase ICP. DIF: Cognitive Level: Applying REF: p. 1439 TOP: Nursing Process: Implementation MSC: Client Needs: Physiological Integrity 34. What clinical manifestations suggest hydrocephalus in an infant? a. Closed fontanel and high-pitched cry b. Bulging fontanel and dilated scalp veins c. Constant low-pitched cry and restlessness d. Depressed fontanel and decreased blood pressure Bulging fontanels, dilated scalp veins, and separated sutures are clinical manifestations of hydrocephalus in neonates. A closed fontanel, high-pitched cry, constant low-pitched cry, restlessness, a depressed fontanel, and decreased blood pressure are not clinical manifestations of hydrocephalus, but all should be referred for evaluation. DIF: Cognitive Level: Understanding REF: p. 1482 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 35. A pregnant woman asks about prenatal diagnosis of hydrocephalus. The nurse’s response should be based on which knowledge? a. It can be diagnosed only after birth. b. It can be diagnosed by chromosome studies. c. It can be diagnosed with fetal ultrasonography. d. It can be diagnosed by measuring the lecithin-to-sphingomyelin ratio. Hydrocephalus can be diagnosed by fetal ultrasonography as early as 14 weeks of gestation. Most incidents of hydrocephalus are not chromosomal in origin. The lecithin-to-sphingomyelin ratio can be used to determine fetal lung maturity. DIF: Cognitive Level: Analyzing REF: p. 1486 TOP: Integrated Process: Teaching/Learning MSC: Client Needs: Physiological Integrity 36. A child is admitted for revision of a ventriculoperitoneal shunt for noncommunicating hydrocephalus. What is a common reason for elective revision of this shunt? a. Meningitis b. Gastrointestinal upset c. Hydrocephalus resolution d. Growth of the child since the initial shunting An elective revision of a ventriculoperitoneal shunt would most likely be done to accommodate the child’s growth. Meningitis would require an emergent replacement or revision of the shunt. Gastrointestinal upset alone would not indicate the need for shunt revision. Noncommunicating hydrocephalus will not resolve without surgical intervention. DIF: Cognitive Level: Understanding REF: p. 1487 TOP: Nursing Process: Planning MSC: Client Needs: Physiological Integrity 37. What is a priority of care when a child has an external ventricular drain (EVD)? a. Irrigation of drain to maintain flow b. As-needed dressing changes if dressing becomes wet c. Frequent assessment of amount and color of drainage d. Maintaining the EVD below the level of the child’s head The EVD is inserted into the child’s ventricle. Frequent assessment is necessary to determine amount of drainage and whether an infection is present. The EVD is a closed system and is not opened for irrigation. Antibiotics may be administered through the drain, but this is usually done by the neuropractitioner. The dressing is not changed. If it becomes wet, then the practitioner should be notified that cerebrospinal fluid (CSF) may be leaking. Unless ordered, maintaining the EVD below the level of the child’s head position will create too much pressure and potentially drain too much CSF. DIF: Cognitive Level: Understanding REF: p. 1438 TOP: Nursing Process: Planning MSC: Client Needs: Physiological Integrity 38. The nurse is discussing long-term care with the parents of a child who has a ventriculoperitoneal shunt. What issues should be addressed? a. Most childhood activities must be restricted. b. Cognitive impairment is to be expected with hydrocephalus. c. Wearing head protection is essential until the child reaches adulthood. d. Shunt malfunction or infection requires immediate treatment. Because of the potentially severe sequelae, symptoms of shunt malfunction or infection must be assessed and treated immediately. Limits should be appropriate to the child’s developmental age. Except for contact sports, the child will have few restrictions. Cognitive impairment depends on the extent of damage before the shunt was placed. DIF: Cognitive Level: Applying REF: p. 1487 TOP: Integrated Process: Teaching/Learning MSC: Client Needs: Physiological Integrity 39. A 6-year-old child is admitted for revision of a ventriculoperitoneal shunt for noncommunicating hydrocephalus. What sign or symptom does the child have that indicates a revision is necessary? a. Tachycardia b. Gastrointestinal upset c. Hypotension d. Alteration in level of consciousness In older children, who are usually admitted to the hospital for elective or emergency shunt revision, the most valuable indicators of increasing intracranial pressure are an alteration in the child’s level of consciousness, complaint of headache, and changes in interaction with the environment. DIF: Cognitive Level: Analyzing REF: p. 1489 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 40. After a tonic-clonic seizure, what symptoms should the nurse expect the child to experience? a. Diarrhea and abdominal discomfort b. Irritability and hunger c. Lethargy and confusion d. Nervousness and excitability In the postictal phase, after a tonic-clonic seizure, the child may remain semiconscious and difficult to arouse. The average duration of the postictal phase is usually 30 minutes. The child may remain confused or sleep for several hours. He or she may have mild impairment of fine motor movements. The child may have visual and speech difficulties and may vomit or complain of headache. DIF: Cognitive Level: Analyzing REF: p. 1467 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 41. What is the antiepileptic medication that requires monitoring of vitamin D and folic acid? a. Topiramate (Topamax) b. Valproic acid (Depakene) c. Gabapentin (Neurontin) d. Phenobarbital (Luminal) Children taking phenobarbital or phenytoin should receive adequate vitamin D and folic acid because deficiencies of both have been associated with these drugs. DIF: Cognitive Level: Analyzing REF: p. 1479 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 42. A 2-year-old child starts to have a tonic-clonic seizure. The child’s jaws are clamped. What is the most important nursing action at this time? a. Place a padded tongue blade between the child’s jaws. b. Stay with the child and observe his respiratory status. c. Prepare the suction equipment. d. Restrain the child to prevent injury. It is impossible to halt a seizure once it has begun, and no attempt should be made to do so. The nurse must remain calm, stay with the child, and prevent the child from sustaining any harm during the seizure. The nurse should not move or forcefully restrain the child during a tonic-clonic seizure and should not place a solid object between the teeth. Suctioning may be needed but not until the seizure has ended. DIF: Cognitive Level: Applying REF: p. 1478 TOP: Nursing Process: Implementation MSC: Client Needs: Physiological Integrity 43. A child has been admitted with status epilepticus. An emergency medication has been ordered. What medication should the nurse expect to be prescribed? a. Lorazepam (Ativan) b. Phenytoin (Dilantin) c. Topiramate (Topamax) d. Ethosuximide (Zarontin) For in-hospital management of status epilepticus, intravenous diazepam or lorazepam (Ativan) is the first-line drug of choice. Lorazepam is the preferred agent because of its rapid onset (2–5 minutes) and long half-life (12–24 hours) with few side effects. DIF: Cognitive Level: Analyzing REF: p. 1473 TOP: Nursing Process: Planning MSC: Client Needs: Physiological Integrity 44. A child is on phenytoin (Dilantin). What should the nurse encourage? a. Fluid restriction b. Good dental hygiene c. A decrease in vitamin D intake d. Taking the medication with milk Chronic treatment with phenytoin may cause gum hypertrophy. Children taking phenobarbital or phenytoin should receive adequate vitamin D and folic acid because deficiencies of both have been associated with these drugs. The medication should not be taken with milk, and fluids should be encouraged, not restricted. DIF: Cognitive Level: Applying REF: p. 1472 TOP: Nursing Process: Implementation MSC: Client Needs: Physiological Integrity 45. A child has a seizure disorder. What test should be done to gather the most specific information about the type of seizure the child is having? a. Sleep study b. Skull radiography c. Serum electrolytes d. Electroencephalogram (EEG) An EEG is obtained for all children with seizures and is the most useful tool for evaluating a seizure disorder. The EEG confirms the presence of abnormal electrical discharges and provides information on the seizure type and the focus. The EEG is carried out under varying conditions—with the child asleep, awake, awake with provocative stimulation (flashing lights, noise), and hyperventilating. Stimulation may elicit abnormal electrical activity, which is recorded on the EEG. Various seizure types produce characteristic EEG patterns: high-voltage spike discharges are seen in tonic-clonic seizures, with abnormal patterns in the intervals between seizures; a three-per-second spike and wave pattern is observed in an absence seizure; and absence of electrical activity in an area suggests a large lesion, such as an abscess or subdural collection of fluid. DIF: Cognitive Level: Analyzing REF: p. 1470 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 46. A child develops syndrome of inappropriate antidiuretic hormone secretion (SIADH) as a complication to meningitis. What action should be verified before implementing? a. Forcing fluids b. Daily weights with strict input and output (I and O) c. Strict monitoring of urine volume and specific gravity d. Close observation for signs of increasing cerebral edema The treatment of SIADH consists of fluid restriction until serum electrolytes and osmolality return to normal levels. SIADH often occurs in children who have meningitis. Monitoring weights, keeping I and O and specific gravity of urine, and observing for signs of increasing cerebral edema are all part of the nursing care for a child with SIADH. DIF: Cognitive Level: Applying REF: p. 1440 TOP: Nursing Process: Implementation MSC: Client Needs: Physiological Integrity 47. When taking the history of a child hospitalized with Reye syndrome, the nurse should not be surprised if a week ago the child had recovered from what? a. Measles b. Influenza c. Meningitis d. Hepatitis The etiology of Reye syndrome is not well understood, but most cases follow a common viral illness, typically influenza or varicella. DIF: Cognitive Level: Analyzing REF: p. 1462 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 48. If an intramuscular (IM) injection is administered to a child who has Reye syndrome, the nurse should monitor for what? a. Bleeding b. Infection c. Poor absorption d. Itching at the injection site The nurse should watch for bleeding from the site. Because of related liver dysfunction with Reye syndrome, laboratory studies, such as prolonged bleeding time, should be monitored to determine impaired coagulation. DIF: Cognitive Level: Applying REF: p. 1463 TOP: Nursing Process: Implementation MSC: Client Needs: Physiological Integrity 49. A 23-month-old child is admitted to the hospital with a diagnosis of meningitis. She is lethargic and very irritable with a temperature of 102° F. What should the nurse’s care plan include? a. Observing the child’s voluntary movement b. Checking the Babinski reflex every 4 hours c. Checking the Brudzinski reflex every 1 hour d. Assessing the level of consciousness (LOC) and vital signs every 2 hours Observation of vital signs, neurologic signs, LOC, urinary output, and other pertinent data is carried out at frequent intervals on a child with meningitis. The nurse should avoid actions that cause pain or increase discomfort, such as lifting the child’s head, so the Brudzinski reflex should not be checked hourly. Checking the Babinski reflex or child’s voluntary movements will not help with assessing the child’s status. DIF: Cognitive Level: Applying REF: p. 1459 TOP: Nursing Process: Implementation MSC: Client Needs: Physiological Integrity 50. A lumbar puncture (LP) is being done on an infant with suspected meningitis. The nurse expects which results for the cerebrospinal fluid that can confirm the diagnosis of meningitis? a. WBCs; glucose b. RBCs; normal WBCs c. glucose; normal RBCs d. Normal RBCs; normal glucose A lumbar puncture is the definitive diagnostic test. The fluid pressure is measured and samples are obtained for culture, Gram stain, blood cell count, and determination of glucose and protein content. The findings are usually diagnostic. The patient generally has an elevated white blood cell count, often predominantly polymorphonuclear leukocytes. The glucose level is reduced, generally in proportion to the duration and severity of the infection. DIF: Cognitive Level: Analyzing REF: p. 1457 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity MULTIPLE RESPONSE 1. The nurse is preparing to admit a 6-month-old infant with increased intracranial pressure (ICP). What clinical manifestations should the nurse expect to observe in this infant? (Select all that apply.) a. High-pitched cry b. Poor feeding c. Setting-sun sign d. Sunken fontanel e. Distended scalp veins f. Decreased head circumference , B, C, E Clinical manifestations of increased ICP in an infant include a high-pitched cry, poor feeding, setting-sun sign, and distended scalp veins. The infant would have a tense, bulging fontanel and an increased head circumference. DIF: Cognitive Level: Applying REF: p. 1428 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 2. The nurse is caring for a child with increased intracranial pressure (ICP). What interventions should the nurse plan for this child? (Select all that apply.) a. Avoid jarring the bed. b. Keep the room brightly lit. c. Keep the bed in a flat position. d. Administer prescribed stool softeners. e. Administer a prescribed antiemetic for nausea. , D, E Other measures to relieve discomfort for a child with ICP include providing a quiet, dimly lit environment; limiting visitors; preventing any sudden, jarring movement, such as banging into the bed; and preventing an increase in ICP. The latter is most effectively achieved by proper positioning and prevention of straining, such as during coughing, vomiting, or defecating. An antiemetic should be administered to prevent vomiting, and stool softeners should be prescribed to prevent straining with bowel movements. The head of the bed should be elevated 15 to 30 degrees. DIF: Cognitive Level: Applying REF: p. 1438 TOP: Nursing Process: Planning MSC: Client Needs: Physiological Integrity 3. The nurse is preparing to admit a 5-year-old with an epidural hemorrhage. What clinical manifestations should the nurse expect to observe? (Select all that apply.) a. Headache b. Vomiting c. Irritability d. Cephalhematoma e. Pallor with anemia , B, C The classic clinical picture of an epidural hemorrhage is a lucid interval (momentary unconsciousness) followed by a normal period for several hours, and then lethargy or coma due to blood accumulation in the epidural space and compression of the brain. The child may be seen with varying degrees of impaired consciousness depending on the severity of the traumatic injury. Common symptoms in a child with no neurologic deficit are irritability, headache, and vomiting. In infants younger than 1 year of age, the most common symptoms are irritability, pallor with anemia, and cephalhematoma. DIF: Cognitive Level: Applying REF: p. 1446 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 4. The nurse is caring for a child with a subdural hematoma. The nurse should assess for what signs that can indicate brainstem compression? (Select all that apply.) a. Coma b. Lethargy c. Hemiplegia d. Hemiparesis e. Unequal pupils , D, E Hemiparesis, hemiplegia, and anisocoria (unequal pupils) are signs of brainstem compression and require emergency treatment targeted at decreasing increased intracranial pressure. Coma and lethargy are seen with a subdural hematoma but do not indicate a brainstem compression. DIF: Cognitive Level: Analyzing REF: p. 1447 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 5. The nurse is preparing to admit a neonate with bacterial meningitis. What clinical manifestations should the nurse expect to observe? (Select all that apply.) a. Jaundice b. Cyanosis c. Poor tone d. Nuchal rigidity e. Poor sucking ability , B, C, E Clinical manifestations of bacterial meningitis in a neonate include jaundice, cyanosis, poor tone, and poor sucking ability. The neck is usually supple in neonates with meningitis, and there is no nuchal rigidity. DIF: Cognitive Level: Applying REF: p. 1456 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 6. The nurse is preparing to admit an adolescent with bacterial meningitis. What clinical manifestations should the nurse expect to observe? (Select all that apply.) a. Fever b. Chills c. Headache d. Poor tone e. Drowsiness , B, C, E Clinical manifestations of bacterial meningitis in an adolescent include, fever, chills, headache, and drowsiness. Hyperactivity is present, not poor tone. DIF: Cognitive Level: Applying REF: p. 1456 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 7. The nurse is caring for a child with meningitis. What acute complications of meningitis should the nurse continuously assess the child for? (Select all that apply.) a. Seizures b. Cerebral palsy c. Cerebral edema d. Hydrocephalus e. Cognitive impairments , C, E Acute complications of meningitis include syndrome of inappropriate antidiuretic hormone (SIADH), subdural effusions, seizures, cerebral edema and herniation, and hydrocephalus. Long-term complications include cerebral palsy, cognitive impairments, learning disorder, attention deficit hyperactivity disorder, and seizures. DIF: Cognitive Level: Applying REF: p. 1440 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 8. What cerebrospinal fluid (CSF) analysis should the nurse expect with viral meningitis? (Select all that apply.) a. Color is turbid. b. Protein count is normal. c. Glucose is decreased. d. Gram stain findings are negative. e. White blood cell (WBC) count is slightly elevated. , D, E The CSF analysis in viral meningitis shows a normal or slightly elevated protein count, negative Gram stain, and a slightly elevated WBC. The color is clear or slightly cloudy, and the glucose level is normal. DIF: Cognitive Level: Applying REF: p. 1460 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 9. The nurse is preparing to admit an adolescent with encephalitis. What clinical manifestations should the nurse expect to observe? (Select all that apply.) a. Malaise b. Apathy c. Lethargy d. Hypoactivity e. Hypothermia , B, D The clinical manifestations of encephalitis include malaise, apathy, and lethargy. There is hyperactivity, not hypoactivity, and hyperthermia, not hypothermia. DIF: Cognitive Level: Applying REF: p. 1461 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 10. The nurse is preparing to admit a 7-year-old child with complex partial seizures. What clinical features of complex partial seizures should the nurse recognize? (Select all that apply.) a. They last less than 10 seconds. b. There is usually no aura. c. Mental disorientation is common. d. There is frequently a postictal state. e. There is usually an impaired consciousness. , D, E Clinical features of complex partial seizures include the following: it is common to have mental disorientation, there is frequently a postictal state, and there is usually an impaired consciousness. These seizures last longer than 10 seconds (usually longer than 60 seconds), and there is usually an aura. DIF: Cognitive Level: Analyzing REF: p. 1466 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 11. What effects of an altered pituitary secretion in a child with meningitis indicates syndrome of inappropriate antidiuretic hormone (SIADH)? (Select all that apply.) a. Hypotension b. Serum sodium is decreased c. Urinary output is decreased d. Evidence of overhydration e. Urine specific gravity is increased , C, D, E The serum sodium is decreased, urinary output is decreased, evidence of overhydration is present, and urine specific gravity is increased in SIADH. Hypertension, not hypotension, occurs. DIF: Cognitive Level: Analyzing REF: p. 1440 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 12. The nurse is caring for a child with an epidural hematoma. The nurse should assess for what signs that can indicate Cushing triad? (Select all that apply.) a. Fever b. Flushing c. Bradycardia d. Systemic hypertension e. Respiratory depression , D, E Cushing triad (systemic hypertension, bradycardia, and respiratory depression) is a late sign of impending brainstem herniation. Fever or flushing does not occur with Cushing triad. DIF: Cognitive Level: Applying REF: p. 1446 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 13. The nurse is preparing to admit a 10-year-old child with absence seizures. What clinical features of absence seizures should the nurse recognize? (Select all that apply.) a. There is no aura. b. There is a postictal state. c. They usually last longer than 30 seconds. d. There is a brief loss of consciousness. e. There is an occasional clonic movement. , D, E Clinical features of absence seizures include no auras, a brief loss of consciousness, and an occasional clonic movement. There is no postictal state, and the seizures rarely last longer than 30 seconds. DIF: Cognitive Level: Understanding REF: p. 1466 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 14. The nurse is teaching the parents of a child with a seizure disorder about the triggers that can cause a seizure. What should the nurse include in the teaching session? (Select all that apply.) a. Cold b. Sugared drinks c. Emotional stress d. Flickering lights e. Hyperventilation , D, E The most common factors that may trigger seizures in children include emotional stress, sleep deprivation, fatigue, fever, and physical exercise. Other precipitating factors include sleep, flickering lights, menstrual cycle, alcohol, heat, hyperventilation, and fasting. Cold and sugared drinks are not triggers for seizures. DIF: Cognitive Level: Applying REF: p. 1480 TOP: Integrated Process: Teaching/Learning MSC: Client Needs: Physiological Integrity COMPLETION 1. The health care provider has prescribed fosphenytoin (Cerebyx) 4 mg/kg/day divided every 12 hours for a child with a seizure disorder. The child weighs 55 lb. The nurse is preparing to administer the 1200 dose. Calculate the dose the nurse should administer in milligrams. Record your answer below in a whole number. ______________ ANS: 50 The correct calculation is: 55 lb/2.2 kg = 25 kg divided every 12 hours Dose of Cerebyx is 4 mg/kg 4 25 = 100 mg/2 = 50 mg DIF: Cognitive Level: Applying REF: p. 1438 TOP: Nursing Process: Implementation MSC: Client Needs: Physiological Integrity 2. The health care provider has prescribed gabapentin (Neurontin) 30 mg/kg/day divided q 8 hours for a child with a seizure disorder. The child weighs 110 lb. The nurse is preparing to administer the 1200 dose. Calculate the dose the nurse should administer in milligrams. Record your answer below in a whole number. _________ ANS: 500 The correct calculation is: 110 lb/2.2 kg = 50 kg Dose of Neurontin is 30 mg/kg/day divided every 8 hours 30 mg 50 = 1500 mg/day 1500 mg/3 = 500 mg for one dose DIF: Cognitive Level: Applying REF: p. 1469 TOP: Nursing Process: Implementation MSC: Client Needs: Physiological Integrity 3. The health care provider has prescribed valproic acid (Depakene) 30 mg/kg/day divided bid for a child with a seizure disorder. The child weighs 77 lb. The nurse is preparing to administer the 0900 dose. Calculate the dose the nurse should administer in milligrams. Record your answer below in a whole number. __________ ANS: 525 The correct calculation is: 77 lb/2.2 kg = 35 kg Dose of Depakene is 30 mg/kg/day divided bid 30 mg 35 = 1050 mg 1050 mg/2 = 525 mg for one dose DIF: Cognitive Level: Applying REF: p. 1471 TOP: Nursing Process: Implementation MSC: Client Needs: Physiological Integrity 4. The health care provider has prescribed carbamazepine (Tegretol) 20 mg/kg/day divided bid for a child with a seizure disorder. The child weighs 33 lb. The nurse is preparing to administer the 0900 dose. Calculate the dose the nurse should administer in milligrams. Record your answer below in a whole number. __________ ANS: 150 The correct calculation is: 33 lb/2.2 kg = 15 kg Dose of Tegretol is 20 mg/kg/day divided bid 20 mg 15 = 30 mg 300 mg/2 = 150 mg DIF: Cognitive Level: Applying REF: p. 1471 TOP: Nursing Process: Implementation MSC: Client Needs: Physiological Integrity MATCHING Match the level of consciousness to its description. a. Confusion b. Disorientation c. Obtundation d. Stupor e. Coma 1. Arousable with stimulation 2. Remaining in a deep sleep, responsive only to repeated stimulation 3. Impaired decision making 4. Confusion regarding time and place 5. No motor or verbal response to noxious stimuli 1. DIF: Cognitive Level: Understanding REF: p. 1431 TOP: Nursing Process: Evaluation MSC: Client Needs: Physiological Integrity 2. DIF: Cognitive Level: Understanding REF: p. 1431 TOP: Nursing Process: Evaluation MSC: Client Needs: Physiological Integrity 3. DIF: Cognitive Level: Understanding REF: p. 1431 TOP: Nursing Process: Evaluation MSC: Client Needs: Physiological Integrity 4. DIF: Cognitive Level: Understanding REF: p. 1431 TOP: Nursing Process: Evaluation MSC: Client Needs: Physiological Integrity 5. ANS: E DIF: Cognitive Level: Understanding REF: p. 1431 TOP: Nursing Process: Evaluation MSC: Client Needs: Physiological Integrity Chapter 33: The Child with Endocrine Dysfunction MULTIPLE CHOICE 1. Homeostasis in the body is maintained by what is collectively known as the neuroendocrine system. What is the name of the nervous system that is involved? a. Central b. Skeletal c. Peripheral d. Autonomic The autonomic nervous system (composed of the sympathetic and parasympathetic systems) controls involuntary functions. In combination with the endocrine system, it maintains homeostasis. The central, skeletal, and peripheral subdivisions of the nervous system are not part of the neuroendocrine system. DIF: Cognitive Level: Understanding REF: p. 1494 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 2. A child with hypopituitarism is being started on growth hormone (GH) therapy. Nursing considerations should be based on which knowledge? a. Therapy is most successful if it is started during adolescence. b. Replacement therapy requires daily subcutaneous injections. c. Hormonal supplementation will be required throughout child’s lifetime. d. Treatment is considered successful if children attain full stature by adolescence. Additional support is required for children who require hormone replacement therapy, such as preparation for daily subcutaneous injections and education for self-management during the school-age years. Young children, obese children, and those who are severely GH deficient have the best response to therapy. Replacement therapy is not needed after attaining final height. The children are no longer GH deficient. When therapy is successful, children can attain their actual or near-final adult height at a slower rate than their peers. DIF: Cognitive Level: Analyzing REF: p. 1499 TOP: Nursing Process: Planning MSC: Client Needs: Physiological Integrity 3. A child with growth hormone (GH) deficiency is receiving GH therapy. When is the best time for the GH to be administered? a. At bedtime b. After meals c. Before meals d. After arising in morning Injections are best given at bedtime to more closely approximate the physiologic release of GH. After meals, before meals, and after arising in the morning do not parallel the physiologic release of the hormone. DIF: Cognitive Level: Applying REF: p. 1499 TOP: Nursing Process: Implementation MSC: Client Needs: Physiological Integrity 4. What is a condition that can result if hypersecretion of growth hormone (GH) occurs after epiphyseal closure? a. Cretinism b. Dwarfism c. Gigantism d. Acromegaly Excess GH after closure of the epiphyseal plates results in acromegaly. Cretinism is associated with hypothyroidism. Dwarfism is the condition of being abnormally small. Gigantism occurs when there is hypersecretion of GH before the closure of the epiphyseal plates. DIF: Cognitive Level: Understanding REF: p. 1501 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 5. Peripheral precocious puberty (PPP) differs from central precocious puberty (CPP) in which manner? a. PPP results from a central nervous system (CNS) insult. b. PPP occurs more frequently in girls. c. PPP may be viewed as a variation in sexual development. d. PPP results from hormonal stimulation of the hypothalamic gonadotropin-releasing hormone (Gn-RH). PPP may be viewed as a variation in sexual development. PPP results from hormone stimulation other than the hypothalamic Gn-RH. Isolated manifestations of secondary sexual development occur. PPP can be missed if these changes are viewed as variations in pubertal onset. CPP results from CNS insult, occurs more frequently in girls, and results from hormonal stimulation of the hypothalamic Gn-RH. DIF: Cognitive Level: Understanding REF: p. 1502 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 6. A child will start treatment for central precocious puberty. What synthetic hormone will be injected? a. Thyrotropin b. Gonadotropins c. Somatotropic hormone d. Luteinizing hormone–releasing hormone Precocious puberty of central origin is treated with monthly subcutaneous injections of luteinizing hormone–releasing hormone, which regulates pituitary secretions. Thyrotropin, gonadotropins, and somatotropic hormone are not the appropriate therapies for precocious puberty. DIF: Cognitive Level: Understanding REF: p. 1502 TOP: Nursing Process: Implementation MSC: Client Needs: Physiological Integrity 7. The nurse is planning care for a child recently diagnosed with diabetes insipidus (DI). What intervention should be included? a. Encourage the child to wear medical identification. b. Discuss with the child and family ways to limit fluid intake. c. Teach the child and family how to do required urine testing. d. Reassure the child and family that this is usually not a chronic or life-threatening illness. DI is a potentially life-threatening disorder if the voluntary demand for fluid is suppressed or the child does not have access to fluids. Medical alert identification should be worn. Fluid intake is not restricted in children with DI. The child is unable to concentrate urine and can rapidly become dehydrated. Fluid intake may be limited during diagnosis, when the lack of intake will result in decreased urinary output and dehydration. Urine testing is not required in DI. Changes in body weight provide information about approximate fluid balance. This is a lifelong disorder that requires supplemental vasopressin throughout life. DIF: Cognitive Level: Applying REF: p. 1502 TOP: Nursing Process: Planning MSC: Client Needs: Physiological Integrity 8. Intranasal administration of desmopressin acetate (DDAVP) is used to treat which condition? a. Hypopituitarism b. Diabetes insipidus (DI) c. Syndrome of inappropriate antidiuretic hormone (SIADH) d. Acute adrenocortical insufficiency DDAVP is the treatment of choice for DI. It is administered intranasally through a flexible tube. The child’s response pattern is variable, with effectiveness lasting from 6 to 24 hours. DIF: Cognitive Level: Understanding REF: p. 1503 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 9. What nursing care should be included for a child diagnosed with syndrome of inappropriate antidiuretic hormone (SIADH)? a. Maintain the child NPO (nothing by mouth). b. Turn the child frequently. c. Restrict fluids. d. Encourage fluids. Increased secretion of ADH causes the kidney to reabsorb water, which increases fluid volume and decreases serum osmolarity with a progressive reduction in sodium concentration. The immediate management of the child is to restrict fluids but not food. Frequently turning the child is not necessary unless the child is unresponsive. Encouraging fluids will worsen the child’s condition. DIF: Cognitive Level: Analyzing REF: p. 1504 TOP: Nursing Process: Planning MSC: Client Needs: Physiological Integrity 10. What is a common clinical manifestation of juvenile hypothyroidism? a. Insomnia b. Diarrhea c. Dry skin d. Rapid growth Dry skin, mental decline, and myxedematous skin changes are associated with juvenile hypothyroidism. Children with hypothyroidism often have sleepiness, constipation, and decelerated growth. DIF: Cognitive Level: Understanding REF: p. 1505 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 11. A goiter is an enlargement or hypertrophy of which gland? a. Thyroid b. Adrenal c. Anterior pituitary d. Posterior pituitary A goiter is an enlargement or hypertrophy of the thyroid gland. Goiter is not associated with the adrenal, anterior pituitary, or posterior pituitary secretory organs. DIF: Cognitive Level: Understanding REF: p. 1505 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 12. Exophthalmos (protruding eyeballs) may occur in children with which condition? a. Hypothyroidism b. Hyperthyroidism c. Hypoparathyroidism d. Hyperparathyroidism Exophthalmos is associated with hyperthyroidism. Hypothyroidism, hypoparathyroidism, and hyperparathyroidism are not associated with exophthalmos. DIF: Cognitive Level: Understanding REF: p. 1507 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 13. A child is receiving propylthiouracil for the treatment of hyperthyroidism (Graves disease). The parents and child should be taught to recognize and report which sign or symptom immediately? a. Fatigue b. Weight loss c. Fever, sore throat d. Upper respiratory tract infection Children being treated with propylthiouracil must be carefully monitored for the side effects of the drug. Parents must be alerted that sore throat and fever accompany the grave complication of leukopenia. These symptoms should be immediately reported. Fatigue and weight loss are manifestations of hyperthyroidism. Their presence may indicate that the drug is not effective but does not require immediate evaluation. Upper respiratory tract infections are most likely viral in origin and not a sign of leukopenia. DIF: Cognitive Level: Applying REF: p. 1507 TOP: Integrated Process: Teaching/Learning MSC: Client Needs: Physiological Integrity 14. The school nurse practitioner is consulted by a fifth-grade teacher about a student who has become increasingly inattentive and hyperactive in the classroom. The nurse notes that the child’s weight has changed from the 50th percentile to the 30th percentile. The nurse is concerned about possible hyperthyroidism. What additional sign or symptom should the nurse anticipate? a. Skin that is cool and dry b. Blurred vision and loss of acuity c. Running and being active during recess d. Decreased appetite and food intake Visual disturbances such as loss of visual acuity and blurred vision are associated with hyperthyroidism. They may occur before the actual onset of other symptoms. The child’s skin is usually warm, flushed, and moist. Although the signs of hyperthyroidism include excessive motion, irritability, hyperactivity, short attention span, and emotional lability, these children are easily fatigued and require frequent rest periods. Children with hyperthyroidism have increased food intake. Even with voracious appetites, weight loss occurs. DIF: Cognitive Level: Applying REF: p. 1507 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 15. A child with hypoparathyroidism is receiving vitamin D therapy. The parents should be advised to watch for which signs or symptoms of vitamin D toxicity? a. Headache and seizures b. Weakness and lassitude c. Anorexia and insomnia d. Physical restlessness, voracious appetite without weight gain Vitamin D toxicity can be a serious consequence of therapy. Parents are advised to watch for weakness, fatigue, lassitude, headache, nausea, vomiting, and diarrhea. Renal impairment is manifested through polyuria, polydipsia, and nocturia. Headaches may be a sign of vitamin D toxicity, but seizures are not. Anorexia and insomnia are not characteristic of vitamin D toxicity. Physical restlessness and a voracious appetite with weight loss are manifestations of hyperthyroidism. DIF: Cognitive Level: Applying REF: p. 1509 TOP: Integrated Process: Teaching/Learning MSC: Client Needs: Physiological Integrity 16. Glucocorticoids, mineralocorticoids, and sex steroids are secreted by which gland? a. Thyroid gland b. Adrenal cortex c. Anterior pituitary d. Parathyroid glands The glucocorticoids, mineralocorticoids, and sex steroids are secreted by the adrenal cortex. The thyroid gland produces thyroid hormone and thyrocalcitonin. The anterior pituitary produces hormones such as growth hormone, thyroid-stimulating hormone, adrenocorticotropic hormone, gonadotropin, prolactin, and melanocyte-stimulating hormone. The parathyroid glands produce parathyroid hormone. DIF: Cognitive Level: Understanding REF: p. 1510 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 17. Congenital adrenal hyperplasia (CAH) is suspected in a newborn because of ambiguous genitalia. The parents are appropriately upset and concerned about their child’s gender. In teaching the parents about CAH, what should the nurse explain? a. Reconstructive surgery as a female is preferred. b. Sexual assignment should wait until genetic sex is determined. c. Prenatal masculinization will strongly influence the child’s development. d. The child should be raised as a boy because of the presence of a penis and scrotum. It is preferable to raise the child according to genetic sex. With hormone replacement and surgical intervention if needed, genetically female children achieve satisfactory results in reversing virilism and achieving normal puberty and ability to conceive. Reconstructive surgery as a female is only preferred for infants who are genetically female. Infants who are genetically male should be given hormonal supplementation. Sex assignment and rearing depend on psychosocial influences, not on genetic sex hormone influences during fetal life. It is not advised to raise the child as a boy because of the presence of a penis and scrotum unless the child is genetically male. If a genetic female, the child will be sterile and may never be able to function satisfactorily in a heterosexual relationship. DIF: Cognitive Level: Applying REF: p. 1517 TOP: Integrated Process: Teaching/Learning MSC: Client Needs: Psychosocial Integrity 18. What form of diabetes is characterized by destruction of pancreatic beta cells, resulting in insulin deficiency? a. Type 1 diabetes b. Type 2 diabetes c. Gestational diabetes d. Maturity-onset diabetes of the young (MODY) Type 1 diabetes is characterized by the destruction of the pancreatic beta cells, which leads to absolute insulin deficiency. Type 2 diabetes results usually from insulin resistance. The pancreatic beta cells are not destroyed in gestational diabetes. MODY is an autosomal dominant monogenetic defect in beta cell function that is characterized by impaired insulin secretion with minimum or no defects in insulin action. DIF: Cognitive Level: Understanding REF: p. 1519 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 19. What statement is characteristic of type 1 diabetes mellitus? a. Onset is usually gradual. b. Ketoacidosis is infrequent. c. Peak age incidence is 10 to 15 years. d. Oral agents are available for treatment. Type 1 diabetes mellitus typically usually has its onset before the age of 20 years, with a peak incidence between ages 10 and 15 years. Type 1 has an abrupt onset, in contrast to type 2, which has a more gradual appearance. Ketoacidosis occurs when insulin is unavailable and the body uses sources other than glucose for cellular metabolism. Ketoacidosis is more common in type 1 diabetes than in type 2. At this time, oral agents are available only for type 2 diabetes. DIF: Cognitive Level: Analyzing REF: p. 1520 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 20. What clinical manifestation is considered a cardinal sign of diabetes mellitus? a. Nausea b. Seizures c. Impaired vision d. Frequent urination Hallmarks of diabetes mellitus are glycosuria, polyuria, and polydipsia. Nausea and seizures are not clinical manifestations of diabetes mellitus. Impaired vision is a long-term complication of the disease. DIF: Cognitive Level: Understanding REF: p. 1523 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 21. What blood glucose measurement is most likely associated with diabetic ketoacidosis? a. 185 mg/dl b. 220 mg/dl c. 280 mg/dl d. 330 mg/dl Diabetic ketoacidosis is a state of relative insulin insufficiency and may include the presence of hyperglycemia, a blood glucose level greater than or equal to 330 mg/dl; 185, 220, and 280 mg/dl are values that are too low for the definition of ketoacidosis. DIF: Cognitive Level: Understanding REF: p. 1530 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 22. The parents of a child who has just been diagnosed with type 1 diabetes ask about exercise. What effect does exercise have on a type 1 diabetic? a. Exercise increases blood glucose. b. Extra insulin is required during exercise. c. Additional snacks are needed before exercise. d. Excessive physical activity should be restricted. Exercise lowers blood glucose levels, decreasing the need for insulin. Extra snacks are provided to maintain the blood glucose levels. Exercise is encouraged and not restricted unless indicated by other health conditions. DIF: Cognitive Level: Applying REF: p. 1527 TOP: Integrated Process: Teaching/Learning MSC: Client Needs: Physiological Integrity 23. A child eats some sugar cubes after experiencing symptoms of hypoglycemia. This rapid-releasing sugar should be followed by which dietary intervention? a. Sports drink and fruit b. Glucose tabs and protein c. Glass of water and crackers d. Milk and peanut butter on bread Symptoms of hypoglycemia are treated with a rapid-releasing sugar source followed by a complex carbohydrate and protein. Milk supplies lactose and a more prolonged action from the protein. The bread is a complex carbohydrate, which with the peanut butter provides a sustained action. The sports drink contains primarily simple carbohydrates. The fruit contains additional carbohydrates. A protein source is needed for sustained action. The glucose tabs are simple carbohydrates. Complex carbohydrates are needed with the protein. Crackers are a complex carbohydrate, but protein is needed to stabilize the blood sugar. DIF: Cognitive Level: Applying REF: p. 1528 TOP: Nursing Process: Planning MSC: Client Needs: Physiological Integrity 24. A 20-kg (44-lb) child in ketoacidosis is admitted to the pediatric intensive care unit. What order should the nurse not implement until clarified with the physician? a. Weigh on admission and daily. b. Replace fluid volume deficit over 48 hours. c. Begin intravenous line with D5 0.45% normal saline with 20 mEq of potassium chloride. d. Give intravenous regular insulin 2 units/kg/hr after initial rehydration bolus. The initial hydrating solution is 0.9% normal saline. Potassium is not given until the child is voiding 25 ml/hr, demonstrating adequate renal function. After initial rehydration and insulin administration, then potassium is given. Dextrose is not given until blood glucose levels are between 250 and 300 mg/dl. An accurate, current weight is essential for determination of the amount of fluid loss and as a basis for medication dosage. Replacing fluid volume deficit over 48 hours is the current recommendation in diabetic ketoacidosis in children. Cerebral edema is a risk of more rapid administration. Intravenous regular insulin 2 units/kg/hr after initial rehydration bolus is the recommended insulin administration for a child of this weight. Only regular insulin can be given intravenously, and it is given after initial fluid volume expansion. DIF: Cognitive Level: Applying REF: p. 1530 TOP: Nursing Process: Implementation MSC: Client Needs: Physiological Integrity 25. What clinical manifestation occurs with hypoglycemia? a. Lethargy b. Confusion c. Nausea and vomiting d. Weakness and dizziness Some of the clinical manifestations of hypoglycemia include weakness; dizziness; difficulty concentrating, speaking, focusing, and coordinating; sweating; and pallor. Lethargy, confusion, and nausea and vomiting are manifestations of hyperglycemia. DIF: Cognitive Level: Understanding REF: p. 1537 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 26. A 12-year-old girl is newly diagnosed with diabetes when she develops ketoacidosis. How should the nurse structure a successful education program? a. Essential information is presented initially. b. Teaching should take place in the child’s semiprivate room. c. Education is focused toward the parents because the child is too young. d. All information needed for self-management of diabetes is taught at once. Diagnosis of type 1 diabetes can be traumatic for the child and family. Most families are not psychologically ready for the complex teaching that is needed for self-management. Most structured diabetes education programs begin with essential or survival information followed by the complex background material when the family is better able to learn. Teaching can take place either as an outpatient or as an inpatient. The actual teaching area should be free from distractions that would interfere with learning. A semiprivate room would have many individuals entering and leaving the room, causing distraction. A 12-year-old child who is cognitively age appropriate needs to be included in the educational process. Most children older than the age of 8 years can be involved in blood glucose monitoring and insulin administration. Teaching all information needed for self-management of diabetes at once would be too overwhelming for a family in crisis. DIF: Cognitive Level: Applying REF: p. 1524 TOP: Integrated Process: Teaching/Learning MSC: Client Needs: Physiological Integrity 27. The nurse is discussing with a child and family the various sites used for insulin injections. What site usually has the fastest rate of absorption? a. Arm b. Leg c. Buttock d. Abdomen The abdomen has the fastest rate of absorption but the shortest duration. The arm has a fast rate of absorption but a short duration. The leg has a slow rate of absorption but a long duration. The buttock has the slowest rate of absorption and the longest duration. DIF: Cognitive Level: Applying REF: p. 1525 TOP: Nursing Process: Implementation MSC: Client Needs: Physiological Integrity 28. The nurse is teaching an adolescent about giving insulin injections. The adolescent asks if the disposable needles and syringes can be used more than once. The nurse’s response should be based on which knowledge? a. It is unsafe. b. It is acceptable for up to 24 hours. c. It is acceptable for families with very limited resources. d. It is suitable for up to 3 days if stored in the refrigerator. Bacterial counts are unaffected if insulin syringes are handled in an aseptic manner and stored in the refrigerator between use. The syringes can be used up to 3 days and result in a considerable cost savings. Bacterial counts remain low for up to 72 hours with proper technique. The family’s resources are not an issue; if a practice is unsafe, the family should not be encouraged to endanger the child by reusing equipment. DIF: Cognitive Level: Applying REF: p. 1526 TOP: Nursing Process: Implementation MSC: Client Needs: Physiological Integrity 29. A preadolescent has maintained good glycemic control of his type 1 diabetes through the school year. During summer vacation, he has had repeated episodes of hypoglycemia. What additional teaching is needed? a. Carbohydrates in the diet need to be replaced with protein. b. Additional snacks are needed to compensate for increased activity. c. The child needs to decrease his activity level to minimize episodes of hypoglycemia. d. Insulin dosage should be increased to compensate for a change in activity level. Most children have a different schedule during summer vacation. The increased activity and exercise reduce insulin resistance and increase glucose utilization. Additional snacks should be eaten before physical activity to increase carbohydrates and protein and compensate for increased activity. Physical activity should always be encouraged if the child is capable. The benefits include improved glucose utilization and decreased insulin requirements. In consultation with the practitioner, insulin dosage may need to be decreased because of improved glucose utilization. DIF: Cognitive Level: Applying REF: p. 1526 TOP: Integrated Process: Teaching/Learning MSC: Client Needs: Physiological Integrity 30. To help an adolescent deal with diabetes, the nurse needs to consider which characteristic of adolescence? a. Desire to be unique b. Preoccupation with the future c. Need to be perfect and similar to peers d. Awareness of peers that diabetes is a severe disease Adolescence is a time when the individual has a need to be perfect and similar to peers. Having diabetes makes adolescents different from their peers. Adolescents do not wish to be unique; they desire to fit in with the peer group. An adolescent is usually not future oriented. Awareness of peers that diabetes is a severe disease would further alienate the adolescent with diabetes. The peer group would focus on the differences. DIF: Cognitive Level: Analyzing REF: p. 1538 TOP: Integrated Process: Teaching/Learning MSC: Client Needs: Psychosocial Integrity 31. An adolescent diabetic is admitted to the emergency department for treatment of hyperglycemia and pneumonia. What are characteristics of diabetic hyperglycemia? a. Cold, clammy skin and lethargy b. Hunger and hypertension c. Thirst, being flushed, and fruity breath d. Disorientation and pallor The signs of hyperglycemia are thirst, being flushed, and fruity breath. The skin is not cold or clammy, and there is not hunger and hypertension. Disorientation and pallor are signs of hypoglycemia. DIF: Cognitive Level: Understanding REF: p. 1528 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 32. A school-age child with diabetes gets 30 units of NPH insulin at 0800. According to when this insulin peaks, the child should be at greatest risk for a hypoglycemic episode between when? a. Lunch and dinner b. Breakfast and lunch c. 0830 to his midmorning snack d. Bedtime and breakfast the next morning Intermediate-acting (NPH and Lente) insulins reach the blood 2 to 6 hours after injection. The insulins peak 4 to 14 hours later and stay in the blood for about 14 to 20 hours. DIF: Cognitive Level: Analyzing REF: p. 1525 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 33. The nurse is teaching the parent of a preschool child how to administer the child’s insulin injection. The child will be receiving 2 units of regular insulin and 12 units of NPH insulin every morning. What should the parent be taught? a. Draw the insulin in separate syringes. b. Draw the regular insulin first and then the NPH into the same syringe. c. Draw the NPH insulin first and then the regular into the same syringe. d. Check blood sugar first, and if below 120, hold the regular insulin and give the NPH. To obtain maximum benefit from mixing insulins, the recommended practice is to (1) inject the measured amount of air (equivalent to the dosage) into the long-acting insulin; (2) inject the measured amount of air into the rapid-acting (clear) insulin and, without removing the needle; (3) withdraw the clear insulin; and (4) insert the needle (already containing the clear insulin) into the long-acting (cloudy) insulin and then withdraw the desired amount. The blood sugar may be checked before giving the insulin, but the prescribed dose should not be withheld if the blood sugar is 120. DIF: Cognitive Level: Applying REF: p. 1535 TOP: Integrated Process: Teaching/Learning MSC: Client Needs: Physiological Integrity 34. What statement applies to the current focus of the dietary management of children with diabetes? a. Measurement of all servings of food is vital for control. b. Daily calculate specific amounts of carbohydrates, fats, and proteins. c. The number of calories for carbohydrates remains constant on a daily basis; protein and fat calories are liberal. d. The intake ensures day-to-day consistency in total calories, protein, carbohydrates, and moderate fat while allowing for a wide variety of foods. Essentially the nutritional needs of children with diabetes are no different from those of healthy children. Children with diabetes need no special foods or supplements. They need sufficient calories to balance daily expenditure for energy and to satisfy the requirement for growth and development. DIF: Cognitive Level: Analyzing REF: p. 1526 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 35. During the summer many children are more physically active. What changes in the management of the child with diabetes should be expected as a result of more exercise? a. food intake b. food intake c. risk of hyperglycemia d. risk of insulin reaction Exercise is encouraged and never restricted unless indicated by other health conditions. Exercise lowers blood glucose levels, depending on the intensity and duration of the activity. Consequently, exercise should be included as part of diabetes management, and the type and amount of exercise should be planned around the child’s interests and capabilities. However, in most instances, children’s activities are unplanned, and the resulting decrease in blood glucose can be compensated for by providing extra snacks before (and, if the exercise is prolonged, during) the activity. In addition to a feeling of well-being, regular exercise aids in utilization of food and often results in a reduction of insulin requirements. DIF: Cognitive Level: Analyzing REF: p. 1527 TOP: Nursing Process: Implementation MSC: Client Needs: Physiological Integrity 36. Prolonged steroid therapy has caused a child to have Cushing syndrome. To lessen the cushingoid effects, the steroid should be administered at which time? a. In the PM b. After lunch c. QD in the AM d. QOD in the AM When cushingoid features are caused by steroid therapy, the effects may be lessened with administration of the drug early in the morning and on an alternate-day basis. Giving the drug early in the day maintains the normal diurnal pattern of cortisol secretion. If given during the evening, it is more likely to produce symptoms because endogenous cortisol levels are normally low and the additional supply exerts more pronounced effects. An alternate-day schedule allows the anterior pituitary an opportunity to maintain more normal hypothalamic–pituitary–adrenal control mechanisms. DIF: Cognitive Level: Applying REF: p. 1515 TOP: Nursing Process: Implementation MSC: Client Needs: Physiological Integrity 37. The thyroid-stimulating hormone (TSH) increases secretion in response to which hormone? a. Low levels of circulating thyroid hormone b. High levels of circulating thyroid hormone c. Low levels of circulating adrenocorticotropic hormone d. High levels of circulating adrenocorticotropic hormone As blood concentrations of the target hormones reach normal levels, a negative message is sent to the anterior pituitary to inhibit release of the tropic hormone. For example, TSH responds to low levels of circulating TH. As blood levels of TH reach normal concentrations, a negative feedback message is sent to the anterior pituitary, resulting in diminished release of TSH. Adrenocorticotropic stimulates the adrenals to secrete glucocorticoids. DIF: Cognitive Level: Understanding REF: p. 1494 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 38. The nurse is caring for an adolescent with anorexia nervosa. What pituitary dysfunction should the nurse assess for in the adolescent? a. Hypopituitarism b. Pituitary hyperfunction c. Hyperplasia of the pituitary cells d. Overproduction of the anterior pituitary hormones Anorexia nervosa can cause hypopituitarism. It does not cause the hyperfunction of the pituitary, hyperplasia of the pituitary cells, or overproduction of the anterior pituitary hormones. DIF: Cognitive Level: Understanding REF: p. 1496 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 39. The clinic nurse is assessing a child with hypopituitarism. Hypopituitarism can lead to which disorder? a. Gigantism b. Hyperthyroidism c. Cushing syndrome d. Growth hormone deficiency Hypopituitarism can lead to a growth hormone deficiency. An overproduction of the anterior pituitary hormones can result in gigantism (caused by excess growth hormone production during childhood), hyperthyroidism, or hypercortisolism (Cushing syndrome). DIF: Cognitive Level: Understanding REF: p. 1500 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 40. The nurse is assisting with a growth hormone stimulation test for a child with short stature. What should the nurse monitor closely on this child during the test? a. Hypotension b. Tachycardia c. Hypoglycemia d. Nausea and vomiting Patients receiving clonidine (Catapres) for a growth hormone stimulation test require close blood pressure monitoring for hypotension. Tachycardia, hypoglycemia, and nausea and vomiting do not occur with Catapres administered for a growth hormone stimulation test. DIF: Cognitive Level: Applying REF: p. 1500 TOP: Nursing Process: Assessment MSC: Client Needs: Safe and Effective Care Environment 41. The nurse is preparing to administer a prescribed dose of desmopressin acetate (DDAVP) intramuscularly (IM) to a child with diabetes insipidus. What action should the nurse take before drawing the medication into a syringe? a. Mix the medication with sterile water. b. Mix the medication with sterile normal saline. c. Have another nurse double-check the medication dose. d. Hold the medication under warm water for 10 to 15 minutes and then shake vigorously. To be effective, vasopressin must be thoroughly mixed in the oil by being held under warm running water for 10 to 15 minutes and shaken vigorously before being drawn into the syringe. If this is not done, the oil may be injected minus the antidiuretic hormone. Small brown particles, which indicate drug dispersion, must be seen in the suspension. DIF: Cognitive Level: Applying REF: p. 1503 TOP: Nursing Process: Implementation MSC: Client Needs: Safe and Effective Care Environment 42. The nurse is taking care of a child who had a thyroidectomy. The nurse recognizes what as a positive Chvostek sign? a. Paresthesia occurring in feet and toes b. Frequent sharp flexion of wrist and ankle joints c. Carpal spasm elicited by pressure applied to the nerves of the upper arm d. Facial muscle spasm elicited by tapping the facial nerve in the region of the parotid gland A positive Chvostek sign is a facial muscle spasm that is elicited by tapping the facial nerve in the region of the parotid gland. Paresthesia occurring in the feet and toes and frequent sharp flexion of the wrist and ankle joints can be signs of hypoparathyroidism but are not part of a positive Chvostek sign. Carpal spasm elicited by pressure applied to nerves of the upper arm is called a positive Trousseau sign. DIF: Cognitive Level: Analyzing REF: p. 1508 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 43. A child is having tests done to determine parathyroid function. The clinic nurse knows that the parathyroid hormone (PTH) regulates the homeostasis of what in the serum? a. Sodium b. Calcium c. Potassium d. Magnesium The parathyroid glands secrete PTH. Along with vitamin D and calcitonin, PTH regulates the homeostasis of serum calcium concentrations. DIF: Cognitive Level: Understanding REF: p. 1508 TOP: Nursing Process: Assessment MSC: Client Needs: Health Promotion and Maintenance 44. The nurse is caring for a child after a parathyroidectomy. What medication should the nurse have available if hypocalcemia occurs? a. Insulin b. Calcium gluconate c. Propylthiouracil (PTU) d. Cortisone (hydrocortisone) Because hypocalcemia is a potential complication after a parathyroidectomy, observing for signs of tetany, instituting seizure precautions, and having calcium gluconate available for emergency use are part of the nursing care. DIF: Cognitive Level: Applying REF: p. 1510 TOP: Nursing Process: Assessment MSC: Client Needs: Safe and Effective Care Environment MULTIPLE RESPONSE 1. The nurse is preparing a community outreach program for adolescents about the characteristic differences between type 1 and type 2 diabetes mellitus (DM). What concepts should the nurse include? (Select all that apply.) a. Type 1 DM has an abrupt onset. b. Type 1 DM is often controlled with oral glucose agents. c. Type 1 DM occurs primarily in whites. d. Type 2 DM always requires insulin therapy. e. Type 2 DM frequently has a familial history. f. Type 2 DM occurs in people who are overweight. , C, E, F Characteristics of type 1 DM include having an abrupt onset, primarily occurring in whites, and not being controlled with oral glucose agents (insulin is required for therapy). Type 2 DM frequently has a familial history, occurs in people who are overweight, and does not always require insulin therapy (it is used in 20% to 30% of patients). DIF: Cognitive Level: Analyzing REF: p. 1520 TOP: Integrated Process: Teaching/Learning MSC: Client Needs: Physiological Integrity 2. The nurse is preparing to admit a 9-year-old child with syndrome of inappropriate antidiuretic hormone (SIADH). What interventions should the nurse include in the child’s care plan? (Select all that apply.) a. Provide a low-sodium, low-fat diet. b. Initiate seizure precautions. c. Weigh daily at the same time each day. d. Encourage intake of 1 l of fluid per day. e. Measure intake and output hourly. , C, E Nursing care of the child with SIADH includes placing the child on seizure precautions, obtaining a daily weight at the same time each day, and accurately measuring the child’s intake and output. The nurse does not need to provide a low-sodium, low-fat diet because there are no diet restrictions. The child would be on fluid precautions to avoid fluid overload, so 1 l of fluid would not be encouraged. DIF: Cognitive Level: Applying REF: p. 1505 TOP: Nursing Process: Implementation MSC: Client Needs: Physiological Integrity 3. The nurse is planning to admit a 14-year-old adolescent with Cushing syndrome. What clinical manifestations should the nurse expect to observe in this child? (Select all that apply.) a. Truncal obesity b. Decreased pubic hair c. Petechial hemorrhage d. Hyperpigmentation of elbows e. Facial plethora f. Headache and weakness , C, E Clinical manifestations of Cushing syndrome include truncal obesity, petechial hemorrhage, and facial plethora. Decreased pubic and axillary hair; hyperpigmentation of elbows, knees, and wrists; and headache and weakness are clinical manifestations of adrenocortical insufficiency. DIF: Cognitive Level: Applying REF: p. 1514 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 4. The nurse is teaching the family of a child with type 1 diabetes about insulin. What should the nurse include in the teaching session? (Select all that apply.) a. Unopened vials are good for 60 days. b. Diabetic supplies should not be left in a hot environment. c. Insulin can be placed in the freezer if not used every day. d. After it has been opened, insulin is good for up to 28 to 30 days. e. Insulin bottles that have been opened should be stored at room temperature or refrigerated. , D, E Insulin bottles that have been “opened” (i.e., the stopper has been punctured) should be stored at room temperature or refrigerated for up to 28 to 30 days. After 1 month, these vials should be discarded. Unopened vials should be refrigerated and are good until the expiration date on the label. Diabetic supplies should not be left in a hot environment. Insulin need not be refrigerated but should be maintained at a temperature between 15° and 29.5° C (59° and 85° F). Freezing renders insulin inactive. DIF: Cognitive Level: Applying REF: p. 1534 TOP: Integrated Process: Teaching/Learning MSC: Client Needs: Health Promotion and Maintenance 5. The nurse is caring for a child with an anterior pituitary tumor. What hormones are secreted by the anterior pituitary? (Select all that apply.) a. Oxytocin b. Luteinizing hormone c. Antidiuretic hormone d. Thyroid-stimulating hormone e. Adrenocorticotrophic hormone , D, E The anterior pituitary is responsible for secreting the following hormones: growth hormone, thyroid-stimulating hormone, adrenocorticotrophic hormone, follicle-stimulating hormone, luteinizing hormone, and prolactin. The posterior pituitary secretes antidiuretic hormone and oxytocin. DIF: Cognitive Level: Analyzing REF: p. 1495 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 6. The nurse is preparing to assist with a growth hormone provocative test for a child with short stature. The nurse recognizes that which pharmacologics should be used to provoke the release of growth hormone (GH)? (Select all that apply.) a. Larodopa (levodopa) b. Clonidine (Catapres) c. Propranolol (Inderal) d. Cortisone (hydrocortisone) e. Biosynthetic growth hormone , B, C GH stimulation, or provocative testing, involves the use of pharmacologics to provoke the release of GH either directly or indirectly. Provocative testing involves the use of neuromodulators such as levodopa or agents such as clonidine, arginine, insulin, propranolol, or glucagon followed by the measurement GH blood levels. Cortisone is given to replace hormone deficiencies that can occur with GH deficiency. Biosynthetic GH is used to treat GH deficiency. DIF: Cognitive Level: Applying REF: p. 1499 TOP: Nursing Process: Planning MSC: Client Needs: Physiological Integrity 7. The clinic nurse is assessing a child with central precocious puberty. What conditions can cause central precocious puberty? (Select all that apply.) a. Trauma b. Neoplasms c. Radiotherapy d. Exogenous sex hormones e. Primary hypothyroidism , B, C Trauma, neoplasms, and radiotherapy can be the cause of central precocious puberty. Exogenous sex hormones and primary hypothyroidism can cause peripheral precocious puberty. DIF: Cognitive Level: Understanding REF: p. 1502 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 8. The nurse is planning to admit a 10-year-old child with syndrome of inappropriate antidiuretic hormone (SIADH). What clinical manifestations should the nurse expect to observe in this child? (Select all that apply.) Clinical manifestations of hypoparathyroidism include muscle cramps, positive Chvostek sign, and laryngeal spasms. Emotional lability and short attention span are signs of Graves disease. DIF: Cognitive Level: Applying REF: p. 1509 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 11. What are characteristics of diabetic ketoacidosis? (Select all that apply.) a. Pallor b. Acidosis c. Bradypnea d. Dehydration e. Electrolyte imbalance , D, E Characteristics of diabetic ketoacidosis include acidosis, dehydration, and electrolyte imbalance. Respirations are rapid (Kussmaul respirations), not slow, and flushing, not pallor, would occur. DIF: Cognitive Level: Understanding REF: p. 1523 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 12. The nurse is preparing to admit a 7-year-old child with type 2 diabetes. What clinical features of type 2 diabetes should the nurse recognize? (Select all that apply.) a. Oral agents are effective. b. Insulin is usually needed. c. Ketoacidosis is infrequent. d. Diet only is often effective. e. Chronic complications frequently occur. , C, D The clinical features of type 2 diabetes include the following: oral agents are effective, ketoacidosis is infrequent, and diet only is often effective. Insulin is only needed in 20% to 30% of cases and chronic complications occur infrequently. DIF: Cognitive Level: Understanding REF: p. 1520 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 13. The nurse is planning to admit a 14-year-old adolescent with hyperparathyroidism. What clinical manifestations should the nurse expect to observe in this patient? (Select all that apply.) a. Polyuria b. Diarrhea c. Hypotension d. Vague bone pain e. Paresthesia in extremities , D, E Clinical manifesta 1 The correct calculation is: 88 lb/2.2 kg = 40 kg Dose of DDAVP is 0.05 mg/kg/day divided bid 0.05 mg 40 = 2 mg/day 2 mg/2 = 1 mg for one dose DIF: Cognitive Level: Applying REF: p. 1503 TOP: Nursing Process: Implementation MSC: Client Needs: Physiological Integrity 3. The health care provider has prescribed levothyroxine (Synthroid) 4 mcg/kg/day PO for a child with hypothyroidism. The child weighs 77 lb. The nurse is preparing to administer the daily dose. Calculate the dose the nurse should administer in micrograms. Record your answer below in a whole number. ________ ANS: 140 The correct calculation is: 77 lb/2.2 kg = 35 kg Dose of Synthroid is 4 mcg/kg/day 4 mcg 35 = 140 mcg for the daily dose DIF: Cognitive Level: Applying REF: p. 1505 TOP: Nursing Process: Implementation MSC: Client Needs: Physiological Integrity 4. The health care provider has prescribed propylthiouracil (PTU) 7 mg/kg/day PO divided every 12 hours for a child with Graves disease. The child weighs 66 lb. The nurse is preparing to administer the 0800 dose. Calculate the dose the nurse should administer in milligrams. Record your answer below in a whole number. _________ ANS: 105 The correct calculation is: 66 lb/2.2 kg = 30 kg Dose of PTU is 7 mg/kg/day divided every 12 hours 7 mg 30 = 210 mg 210 mg/2 = 105 mg DIF: Cognitive Level: Applying REF: p. 1507 TOP: Nursing Process: Implementation MSC: Client Needs: Physiological Integrity 5. A health care provider prescribes hydrocortisone (Solu-Cortef) 200 mg IV STAT for a child with acute adrenocortical insufficiency. The medication label states Solu-Cortef 100 mg/2 ml. The nurse prepares to administer one dose. How many milliliters will the nurse prepare to administer one dose? Fill in the blank. Record your answer below in a whole number. ________________ ANS: 4 Follow the formula for dosage calculation. TOP: Nursing Process: Implementation MSC: Client Needs: Physiological Integrity 2. The nurse stops to assist an adolescent who has experienced severe trauma when hit by a motorcycle. The emergency medical system (EMS) has been activated. The first person who provided assistance applied a tourniquet to the child’s leg because of arterial bleeding. What should the nurse do related to the tourniquet? a. Loosen the tourniquet. b. Leave the tourniquet in place. c. Remove the tourniquet and apply direct pressure if bleeding is still present. d. Remove the tourniquet every 5 minutes, leaving it off for 30 seconds each time. A tourniquet is applied only as a last resort, and then it is left in place and not loosened until definitive treatment is available. After the tourniquet is applied, skin and tissue necrosis occur below the site. Loosening or removing the tourniquet allows toxins from the tissue necrosis to be released into the circulation. This can induce systemic, deadly tourniquet shock. DIF: Cognitive Level: Analyzing REF: p. 1545 TOP: Nursing Process: Implementation MSC: Client Needs: Physiological Integrity 3. What is a physiologic effect of immobilization on children? a. Metabolic rate increases. b. Venous return improves because the child is in the supine position. c. Circulatory stasis can lead to thrombus and embolus formation. d. Bone calcium increases, releasing excess calcium into the body (hypercalcemia). The physiologic effects of immobilization, as a result of decreased muscle contraction, include venous stasis. This can lead to pulmonary emboli or thrombi. The metabolic rate decreases with immobilization. With the loss of muscle contraction, there is a decreased venous return to the heart. Calcium leaves the bone during immobilization, leading to bone demineralization and increasing the calcium ion concentration in the blood. DIF: Cognitive Level: Understanding REF: p. 1549 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 4. What condition can result from the bone demineralization associated with immobility? a. Osteoporosis b. Pooling of blood c. Urinary retention d. Susceptibility to infection Bone demineralization leads to a negative calcium balance, osteoporosis, pathologic fractures, extraosseous bone formation, and renal calculi. Pooling of blood is a result of the cardiovascular effects of immobilization. Urinary retention is secondary to the effect of immobilization on the urinary tract. Susceptibility to infection can result from the effects of immobilization on the respiratory and renal systems. DIF: Cognitive Level: Understanding REF: p. 1554 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 5. What measure is important in managing hypercalcemia in a child who is immobilized? a. Provide adequate hydration. b. Change position frequently. c. Encourage a diet high in calcium. d. Provide a diet high in calories for healing. Vigorous hydration is indicated to prevent problems with hypercalcemia. Suggested intake for an adolescent is 3000 to 4000 ml/day of fluids. Diuretics are used to promote the removal of calcium. Changing position is important for skin and respiratory concerns. Calcium in the diet is restricted when possible. A high-protein diet served as frequent snacks with favored foods is recommended. A high-calorie diet without adequate protein will not promote healing. DIF: Cognitive Level: Understanding REF: p. 1554 TOP: Nursing Process: Implementation MSC: Client Needs: Physiological Integrity 6. The nurse is caring for an immobilized preschool child. What intervention is helpful during this period of immobilization? a. Encourage wearing pajamas. b. Let the child have few behavioral limitations. c. Keep the child away from other immobilized children if possible. d. Take the child for a “walk” by wagon outside the room. Transporting the child outside of the room by stretcher, wheelchair, or wagon increases environmental stimuli and provides social contact. Street clothes are preferred for hospitalized children. This decreases the sense of illness and disability. The child needs appropriate limits for both adherence to the medical regimen and developmental concerns. It is not necessary to keep the child away from other immobilized children. DIF: Cognitive Level: Analyzing REF: p. 1563 TOP: Integrated Process: Teaching/Learning MSC: Client Needs: Psychosocial Integrity 7. The nurse is teaching parents the proper use of a hip–knee–ankle–foot orthosis (HKAFO) for their 4-year-old child. The parents demonstrate basic essential knowledge by making what statement? a. “Alcohol will be used twice a day to clean the skin around the brace.” b. “Weekly visits to the orthotist are scheduled to check screws for tightness.” c. “Initially, a burning sensation is expected and the brace should remain in place.” d. “Condition of the skin in contact with the brace should be checked every 4 hours.” This type of brace has several contact points with the child’s skin. To minimize the risk of skin breakdown and facilitate use of the brace, vigilant skin monitoring is necessary. Alcohol should not be used on the skin. It is drying. Parents are capable of checking and tightening the screws when necessary. If a burning sensation occurs, the brace should be removed. If several complaints of burning occur, the orthotist should be contacted. DIF: Cognitive Level: Applying REF: p. 1565 TOP: Integrated Process: Teaching/Learning MSC: Client Needs: Physiological Integrity 8. Immobilization causes what effect on metabolism? a. Hypocalcemia b. Decreased metabolic rate c. Positive nitrogen balance d. Increased levels of stress hormones Immobilization causes a decreased metabolic rate with slowing of all systems and a decreased food intake. Immobilization leads to hypercalcemia and a negative nitrogen balance secondary to muscle atrophy. Decreased production of stress hormones occurs with decreased physical and emotional coping capacity. DIF: Cognitive Level: Understanding REF: p. 1554 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 9. What finding is characteristic of fractures in children? a. Fractures rarely occur at the growth plate site because it absorbs shock well. b. Rapidity of healing is inversely related to the child’s age. c. Pliable bones of growing children are less porous than those of adults. d. The periosteum of a child’s bone is thinner, is weaker, and has less osteogenic potential compared to that of an adult. Healing is more rapid in children. The younger the child, the more rapid the healing process. Nonunion of bone fragments is uncommon except in severe injuries. The epiphyseal plate is the weakest point of long bones and a frequent site of injury during trauma. Children’s bones are more pliable and porous than those of adults. This allows them to bend, buckle, and break. The greater porosity increases the flexibility of the bone and dissipates and absorbs a significant amount of the force on impact. The adult periosteum is thinner, is weaker, and has less osteogenic potential than that of a child. DIF: Cognitive Level: Understanding REF: p. 1568 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 10. A 14-year-old is admitted to the emergency department with a fracture of the right humerus epiphyseal plate through the joint surface. What information does the nurse know regarding this type of fracture? a. It will create difficulty because the child is left handed. b. It will heal slowly because this is the weakest part of the bone. c. This type of fracture requires different management to prevent bone growth complications. d. This type of fracture necessitates complete immobilization of the shoulder for 4 to 6 weeks. This type of fracture (Salter type III) can cause problems with growth in the affected limb. Early and complete assessment is essential to prevent angular deformities and longitudinal growth problems. The difficulty for the child does not depend on the locati The injured extremity should be kept elevated while resting and in a sling when upright. This will increase venous return. The child should not engage in strenuous activity for the first few days. Rest with elevation of the extremity is encouraged. Joints above and below the cast on the affected extremity should be moved. Swelling of the fingers may indicate neurovascular damage and should be reported immediately. Permanent damage can occur within 6 to 8 hours. DIF: Cognitive Level: Applying REF: p. 1566 TOP: Integrated Process: Teaching/Learning MSC: Client Needs: Physiological Integrity 13. The nurse uses the five Ps to assess ischemia in a child with a fracture. What finding is considered a late and ominous sign? a. Petaling b. Posturing c. Paresthesia d. Positioning Paresthesia distal to the injury or cast is an ominous sign that requires immediate notification of the practitioner. Permanent muscle and tissue damage can occur within 6 hours. The other signs of ischemia that need to be reported are pain, pallor, pulselessness, and paralysis. Petaling is a method of placing protective or smooth edges on a cast. Posturing is not a sign of peripheral ischemia. Finding a position of comfort can be difficult with a fracture. It would not be an ominous sign unless pain was increasing or uncontrollable. DIF: Cognitive Level: Applying REF: p. 1573 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 14. A child is upset because, when the cast is removed from her leg, the skin surface is caked with desquamated skin and sebaceous secretions. What technique should the nurse suggest to remove this material? a. Soak in a bathtub. b. Vigorously scrub the leg. c. Carefully pick material off the leg. d. Apply powder to absorb the material. Simply soaking in the bathtub is usually sufficient for removal of the desquamated skin and sebaceous secretions. Several days may be required to eliminate the accumulation completely. The parents and child should be advised not to scrub the leg vigorously or forcibly remove this material because it may cause excoriation and bleeding. Oil or lotion, but not powder, may provide comfort for the child. DIF: Cognitive Level: Applying REF: p. 1557 TOP: Nursing Process: Implementation MSC: Client Needs: Physiological Integrity 15. A child with a hip spica cast is being prepared for discharge. Recognizing that caring for a child at home is complex, the nurse should include what instructions for the parents’ discharge teaching? a. Turn every 8 hours. b. Specially designed car restraints are necessary. c. Diapers should be avoided to reduce soiling of the cast. d. Use an abduction bar between the legs to aid in turning. Standard seat belts and car seats may not be readily adapted for use by children in some casts. Specially designed car seats and restraints meet safety requirements. The child must have position changes much more frequently than every 8 hours. During feeding and play activities, the child should be moved for both physiologic and psychosocial benefit. Diapers and other strategies are necessary to maintain cleanliness. The abduction bar is never used as an aid for turning. Putting pressure on the bar may damage the integrity of the cast. DIF: Cognitive Level: Applying REF: p. 1559 TOP: Integrated Process: Teaching/Learning MSC: Client Needs: Physiological Integrity 16. What is an appropriate nursing intervention when caring for a child in traction? a. Removing adhesive traction straps daily to prevent skin breakdown b. Assessing for tightness, weakness, or contractures in uninvolved joints and muscles c. Providing active range of motion exercises to affected extremity three times a day d. Keeping child prone to maintain good alignment Traction places stress on the affected bone, joint, and muscles. The nurse must assess for tightness, weakness, or contractures developing in the uninvolved joints and muscles. The adhesive straps should be released or replaced only when absolutely necessary. Active, passive, or active with resistance exercises should be carried out for the unaffected extremity only. Movement is expected with children. Each time the child moves, the nurse should check to ensure that proper alignment is maintained. DIF: Cognitive Level: Applying REF: p. 1562 TOP: Nursing Process: Implementation MSC: Client Needs: Physiological Integrity 17. The nurse is caring for a hospitalized adolescent whose femur was fractured 18 hours ago. The adolescent suddenly develops chest pain and dyspnea. The nurse should suspect what complication? a. Sepsis b. Osteomyelitis c. Pulmonary embolism d. Acute respiratory tract infection Fat emboli are of greatest concern in individuals with fractures of the long bones. Fat droplets from the marrow are transferred to the generursing Process: Planning MSC: Client Needs: Health Promotion and Maintenance 19. The middle school nurse is speaking to parents about prevention of injuries as a goal of the physical education program. How should the goal be achieved? a. Use of protective equipment at the family’s discretion b. Education of adults to recognize signs that indicate a risk for injury c. Sports medicine program to help student athletes work through overuse injuries d. Arrangements for multiple sports to use same athletic fields to accommodate more children Adults close to sports activities need to be aware of the early warning signs of fatigue, dehydration, and risk for injury. School policy should require mandatory use of protective equipment. Proper sports medicine therapy does not support “working through” overuse injuries. Too many students involved in different activities create distractions, which contribute to the child losing focus. This is a contributing factor to injury. DIF: Cognitive Level: Applying REF: p. 1584 TOP: Nursing Process: Planning MSC: Client Needs: Health Promotion and Maintenance 20. A young girl has just injured her ankle at school. In addition to notifying the child’s parents, what is the most appropriate, immediate action by the school nurse? a. Apply ice. b. Observe for edema and discoloration. c. Encourage child to assume a position of comfort. d. Obtain parental permission for administration of acetaminophen or aspirin. Soft tissue injuries should be iced immediately. In addition to ice, the extremity should be rested, be elevated, and have compression applied. The nurse observes for the edema while placing a cold pack. The applying of ice can reduce the severity of the injury. Maintaining the ankle at a position elevated above the heart is important. The nurse helps the child be comfortable with this requirement. The nurse obtains parental permission for administration of acetaminophen or aspirin after ice and rest are assured. DIF: Cognitive Level: Applying REF: p. 1601 TOP: Nursing Process: Implementation MSC: Client Needs: Physiological Integrity 21. A student athlete was injured during a basketball game. The nurse observes significant swelling. The player states he thought he “heard a pop,” that the pain is “pretty bad,” and that the ankle feels “as if it is coming apart.” Based on this description, the nurse suspects what injury? a. Sprain b. Fracture c. Dislocation d. Stress fracture Sprains account for approximately 75% of all ankle injuries in children. A sprain results when the trauma is so severe that a ligament is either stretched or partially or completely torn by the force created as a joint is twisted or wrenched. Joint laxity is the mo Heatstroke is a failure of normal thermoregulatory mechanisms. The onset is rapid with initial symptoms of headache, weakness, and disorientation. Immediate care is relocation to a cool environment, removal of clothing, and applying of cool water (wet towels or immersion). Antipyretics are not used because they are metabolized by the liver, which is already not functioning. Salt tablets are not indicated and may be harmful by increasing dehydration. Rubbing alcohol is not used. DIF: Cognitive Level: Applying REF: p. 1580 TOP: Nursing Process: Implementation MSC: Client Needs: Physiological Integrity 24. What is the recommended drink for athletes during practice and competition? a. Sports drinks to replace carbohydrates b. Cold water for gastrointestinal tract rapid absorption c. Carbonated beverages to help with acid–base balance d. Enhanced performance carbohydrate–electrolyte drinks Water is recommended for most athletes, who should drink 4 to 8 oz every 15 to 20 minutes. Cold water facilitates rapid gastric emptying and intestinal absorption. Most carbohydrate sports drinks have 6% to 8% carbohydrate, which can cause gastrointestinal upset. Carbonated beverages are discouraged. There is no evidence that these drinks enhance function. DIF: Cognitive Level: Analyzing REF: p. 1580 TOP: Nursing Process: Implementation MSC: Client Needs: Physiological Integrity 25. The nurse is teaching the girls’ varsity sports teams about the “female athlete triad.” What is essential information to include? a. They should take low to moderate calcium to avoid hypercalcemia. b. They have strong bones because of the athletic training. c. Pregnancy can occur in the absence of menstruation. d. A diet high in carbohydrates accommodates increased training. Sexually active teenagers, regardless of menstrual status, need to consider contraceptive precautions. Increased calcium (1500 mg) is recommended for amenorrheic athletes. The decreased estrogen in girls with the female athlete triad, coupled with potentially inadequate diet, leads to osteoporosis. Diets high in protein and calories are necessary to avoid potentially long-term consequences of intensive, prolonged exercise programs in pubertal girls. DIF: Cognitive Level: Applying REF: p. 1604 TOP: Integrated Process: Teaching/Learning MSC: Client Needs: Physiological Integrity 26. Parents are considering treatment options for their 5-year-old child with Legg-Calvé-Perthes disease. Both surgical and conservative therapies are appropriate. They are able to verbalize the differences between the therapies when they make what statement? a. “All therapies require extended periods of bed rest.” b. “Conservative therapy will be required until puberty.” c. “Our child cannot attend school during the treatment phase.” d. “Surgical correction requires a 3- to 4-month recovery period.” Surgical correction involves additional risks of anesthesia, infection, and possibly blood transfusion. The recovery period is only 3 to 4 months rather than the 2 to 4 years of conservative therapies. The use of non–weight-bearing appliances and surgical intervention does not require prolonged bed rest. Conservative therapy is indicated for 2 to 4 years. The child is encouraged to attend school and engage in activities that can be adapted to therapeutic appliances. DIF: Cognitive Level: Applying REF: p. 1588 TOP: Integrated Process: Teaching/Learning MSC: Client Needs: Physiological Integrity 27. A 4-year-old child is placed in Buck extension traction for Legg-Calvé-Perthes disease. He is crying with pain as the nurse assesses the skin of his right foot and sees that it is pale with an absence of pulse. What should the nurse do first? a. Reposition the child and notify the practitioner. b. Notify the practitioner of the changes noted. c. Give the child medication to relieve the pain. d. Chart the observations and check the extremity again in 15 minutes. The absence of a pulse and change in color of the foot must be reported immediately for evaluation by the practitioner. This is b. “Most preadolescents use the brace for 6 months.” c. “Until your vertebral column has reached skeletal maturity.” d. “It will be necessary to wear the brace for the rest of your life.” Bracing can halt or slow the progress of most curvatures. They must be used continuously until the child reaches skeletal maturity. Telling the child “for as long as you have been told” does not answer the child’s question and does not promote involvement in care. Six months is unrealistic because skeletal maturity is not reached until adolescence. When skeletal growth is complete, bracing is no longer effective. DIF: Cognitive Level: Applying REF: p. 1587 TOP: Integrated Process: Teaching/Learning MSC: Client Needs: Physiological Integrity 31. A 17-year-old patient is returning to the surgical unit after Luque instrumentation for scoliosis repair. In addition to the usual postoperative care, what additional intervention will be needed? a. Position changes are made by log rolling. b. Assistance is needed to use the bathroom. c. The head of the bed is elevated to minimize spinal headache. d. Passive range of motion is instituted to prevent neurologic injury. After scoliosis repair using a Luque procedure, the adolescent is turned by log rolling to prevent damage to the fusion and instrumentation. The patient is kept flat in bed for the first 12 hours and is not ambulatory until the second or third postoperative day. A urinary catheter is placed. The head of the bed is not elevated until the second postoperative day. Range of motion exercises are begun on the second postoperative day. DIF: Cognitive Level: Understanding REF: p. 1589 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 32. What is the primary method of treating osteomyelitis? a. Joint replacement b. Bracing and casting c. Intravenous antibiotic therapy d. Long-term corticosteroid therapy Osteomyelitis is an infection of the bone, most commonly caused by Staphylococcus aureus infection. The treatment of choice is antibiotics. Joint replacement, bracing and casting, and long-term corticosteroid therapy are not indicated for infectious processes. DIF: Cognitive Level: Understanding REF: p. 1597 TOP: Nursing Process: Implementation MSC: Client Needs: Physiological Integrity 33. What nursing intervention is most appropriate when caring for the child with osteomyelitis? a. Encourage frequent ambulation. b. Administer antibiotics with meals. c. Move and turn the child carefully and gently to minimize pain. tiinflammatory drug (NSAID). What nursing consideration should be included? a. Monitor heart rate. b. Administer NSAIDs between meals. c. Check for abdominal pain and bloody stools. d. Expect inflammation to be gone in 3 or 4 days. NSAIDs are the first-line drugs used in JIA. Potential side effects include gastrointestinal (GI), renal, and hepatic side effects. The child is at risk for GI bleeding and elevated blood pressure. The heart rate is not affected by this drug class. NSAIDs should be given with meals to minimize gastrointestinal problems. The antiinflammatory response usually takes 3 weeks before effectiveness can be evaluated. DIF: Cognitive Level: Applying REF: p. 1605 TOP: Nursing Process: Implementation MSC: Client Needs: Physiological Integrity 37. What is an important nursing consideration when caring for a child with juvenile idiopathic arthritis (JIA)? a. Apply ice packs to relieve acute swelling and pain. b. Administer acetaminophen to reduce inflammation. c. Teach the child and family correct administration of medications. d. Encourage range of motion exercises during periods of inflammation. The management of JIA is primarily pharmacologic. The family should be instructed regarding administration of medications and the value of a regular schedule of administration to maintain a satisfactory blood level in the body. They need to know that nonsteroidal antiinflammatory drugs should not be given on an empty stomach and to be alert for signs of toxicity. Warm, moist heat is best for relieving stiffness and pain. Acetaminophen does not have antiinflammatory effects. Range of motion exercises should not be done during periods of inflammation. DIF: Cognitive Level: Applying REF: p. 1605 TOP: Integrated Process: Teaching/Learning MSC: Client Needs: Physiological Integrity 38. What needs to be included as essential teaching for adolescents with systemic lupus erythematosus (SLE)? a. High calorie diet because of increased metabolic needs b. Home schooling to decrease the risk of infections c. Protection from sun and fluorescent lights to minimize rash d. Intensive exercise regimen to build up muscle strength and endurance The photosensitive rash is a major concern for individuals with SLE. Adolescents who spend time outdoors need to use sunscreens with a high SPF, hats, and clothing. Uncovered fluorescent lights can also cause a photosensitivity reaction. The diet should be sufficient in calories and nutrients for growth and development. The use of steroids can cause increased hunger, resulting in weight gain. This can present additional emotional issues for the adolescent. Normal functions should be maximized. The individual with SLE is encouraged to attend school and participate in peer activities. A balance of rest and exercise is important; excessive exercise is avoided. DIF: Cognitive Level: Applying REF: p. 1609 TOP: Integrated Process: Teaching/Learning MSC: Client Needs: Physiological Integrity 39. The nurse is teaching the parent of a 4-year-old child with a cast on the arm about care at home. What statement by the parent indicates a correct understanding of the teaching? a. “I should have the affected limb hang in a dependent position.” b. “I will use an ice pack to relieve the itching.” c. “I should avoid keeping the injured arm elevated.” d. “I will expect the fingers to be swollen for the next 3 days.” Teaching the parent to use an ice pack to relieve the itching is an important aspect when planning discharge for a child with a cast. The affected limb should not be allowed to hang in a dependent position for more than 30 minutes. The affected arm should be kept elevated as much as possible. If there is swelling or redness of the fingers, the parent should notify the health care provider. DIF: Cognitive Level: Applying REF: p. 1559 TOP: Integrated Process: Teaching/Learning MSC: Client Needs: Physiological Integrity 40. The nurse is teaching the parents of a 1-month-old infant with developmental dysplasia of the hip about preventing skin breakdown under the Pavlik harness. What statement by the parent would indicate a correct understanding of the teaching? a. “I should gently massage the skin under the straps once a day to stimulate circulation.” b. “I will apply a lotion for sensitive skin under the straps after my baby has been given a bath to prevent skin irritation.” c. “I should remove the harness several times a day to prevent contractures.” d. “I will place the diaper over the harness, preferably using a superabsorbent disposable diaper that is relatively thin.” To prevent skin breakdown with an infant who has developmental dysplasia of the hip and is in a Pavlik harness, the parent should gently massage the skin under the straps once a day to stimulate circulation. The parent should not apply lotions or powder because this could irritate the skin. The parent should not remove the harness, except during a bath, and should place the diaper under the straps. DIF: Cognitive Level: Applying REF: p. 1591 TOP: Integrated Process: Teaching/Learning MSC: Client Needs: Physiological Integrity 41. A neonate is bor a. As soon as possible after birth b. When the infant is developmentally ready to stand up c. At about ages 12 to 15 months, when most children are walking d. At about 4 years, when the healthy limb is not growing so rapidly An infant should be fitted with a functional prosthetic leg when the infant is developmentally ready to pull to a standing position. When the infant begins limb exploration, a soft prosthesis can be used. The child should begin using the prosthesis as part of his or her normal development. This will match the infant’s motor readiness. DIF: Cognitive Level: Analyzing REF: p. 1552 TOP: Nursing Process: Implementation MSC: Client Needs: Physiological Integrity 43. The nurse knows that parents need further teaching with regard to the treatment of congenital clubfoot when they state what? a. “We’ll keep the cast dry.” b. “We’re happy this is the only cast our baby will need.” c. “We’ll watch for any swelling of the foot while the cast is on.” d. “We’re getting a special car seat to accommodate the cast.” The common approach to clubfoot management and treatment is the Ponseti method. Serial casting is begun shortly after birth. Weekly gentle manipulation and stretching of the foot along with placement of serial long-leg casts allow for gradual repositioning of the foot. The extremity or extremities are casted until maximum correction is achieved, usually within 6 to 10 weeks. If parents state that this is the only cast the infant will need, they need further teaching. DIF: Cognitive Level: Applying REF: p. 1597 TOP: Integrated Process: Teaching/Learning MSC: Client Needs: Physiological Integrity 44. A child has just returned from surgery for repair of a fractured femur. The child has a long-leg cast on. The toes on the leg with the cast are edematous, but they have color, sensitivity, and movement. What action should the nurse take? a. Call the health care provider to report the edema. b. Elevate the foot and leg on pillows. c. Apply a warm moist pack to the foot. d. Encourage movement of toes. During the first few hours after a cast is applied, the chief concern is that the extremity may continue to swell to the extent that For a child who is immobilized, circulatory stasis and DVT development are prevented by instructing patients to change positions frequently, dorsiflex their feet and rotate the ankles, sit in a bedside chair periodically, or ambulate several times daily. Elevating the legs or placing a foot cradle on the bed will not prevent DVTs. A pillow under the knee would impair circulation, not improve it. DIF: Cognitive Level: Applying REF: p. 1551 TOP: Nursing Process: Implementation MSC: Client Needs: Physiological Integrity 47. The nurse is teaching a child with a cast about cast removal. What should the nurse teach the child about cast removal? a. “The cast cutter will be a quiet machine.” b. “You will feel cold as the cast is removed.” c. “You will feel a tickly sensation as the cast is removed.” d. “The cast cutter cuts through the cast like a circular saw.” Cutting the cast to remove it or to relieve tightness is frequently a frightening experience for children. They fear the sound of the cast cutter and are terrified that their flesh, as well as the cast, will be cut. Because it works by vibration, a cast cutter cuts only the hard surface of the cast. The oscillating blade vibrates back and forth very rapidly and will not cut when placed lightly on the skin. Children have described it as producing a “tickly” sensation. DIF: Cognitive Level: Applying REF: p. 1557 TOP: Integrated Process: Teaching/Learning MSC: Client Needs: Physiological Integrity 48. A 3-year-old child has a femoral shaft fracture. The nurse recognizes that the approximate healing time for this child is how long? a. 2 weeks b. 4 weeks c. 6 weeks d. 8 weeks The approximate healing times for a femoral shaft fracture are as follows: neonatal period, 2 to 3 weeks; early childhood, 4 weeks; later childhood, 6 to 8 weeks; and adolescence, 8 to 12 weeks. DIF: Cognitive Level: Understanding REF: p. 1570 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 49. The nurse is teaching infant care to parents with an infant who has been diagnosed with osteogenesis imperfecta (OI). What should the nurse include in the teaching session? a. “Bisphosphonate therapy is not beneficial for OI.” b. “Physical therapy should be avoided as it may cause damage to bones.” c. “Lift the infant by the buttocks, not the ankles, when changing diapers.” d. “The infant should meet expected gross motor development without assistive devices.” Infants and children with this disorder require careful handling to prevent fractures. They must be supported when they are being turned, positioned, moved, and held. Even changing a diaper may cause a fracture in severely affected infants. These children should never be held by the ankles when being diapered but should be gently lifted by the buttocks or supported with pillows. Bisphosphonate and physical therapy are beneficial for OI. Lightweight braces will be used when the child starts to ambulate. DIF: Cognitive Level: Applying REF: p. 1601 TOP: Integrated Process: Teaching/Learning MSC: Client Needs: Physiological Integrity MULTIPLE RESPONSE 1. In teach , D, E To prevent renal calculi in a child who is immobilized, a nurse should monitor output; ensure adequate fluids; and encourage cranberry juice, which acidifies urine. Apple juice and milk alkalize the urine, so they should not be encouraged. DIF: Cognitive Level: Applying REF: p. 1561 TOP: Nursing Process: Implementation MSC: Client Needs: Physiological Integrity 3. The nurse is assisting with application of a synthetic cast on a child with a fractured humerus. What are the advantages of a synthetic cast over a plaster of Paris cast? (Select all that apply.) a. Less bulky b. Drying time is faster c. Molds readily to body part d. Permits regular clothing to be worn e. Can be cleaned with small amount of soap and water , B, D, E The advantages of synthetic casts over plaster of Paris casts are that they are less bulky, dry faster, permit regular clothes to be worn, and can be cleaned. Plaster of Paris casts mold readily to a body part, but synthetic casts do not mold easily to body parts. DIF: Cognitive Level: Analyzing REF: p. 1558 TOP: Nursing Process: Evaluation MSC: Client Needs: Physiological Integrity 4. A child has had a short-arm synthetic cast applied. What should the nurse teach to the child and parents about cast care? (Select all that apply.) a. Relieve itching with heat. b. Elevate the arm when resting. c. Observe the fingers for any evidence of discoloration. d. Do not allow the child to put anything inside the cast. e. Examine the skin at the cast edges for any breakdown. , C, D, E Cast care involves elevating the arm, observing the fingers for evidence of discoloration, not allowing the child to put anything inside the cast, and examining the skin at the edges of the cast for any breakdown. Ice, not heat, should be applied to relieve itching. DIF: Cognitive Level: Applying REF: p. 1559 TOP: Integrated Process: Teaching/Learning MSC: Client Needs: Physiological Integrity 5. The nurse is conducting preoperative teaching to parents and their child about an external fixation device. What should the nurse include in the teaching session? (Select all that apply.) a. Pin care b. Crutch walking c. Modifications in activity d. Observing pin sites for infection e. Full weight bearing will be allowed after 24 hours , B, C, D The device is attached surgically by securing a series of external full or half rings to the bone with wires. Children and parents should be instructed in pin care, including observation for infection and loosening of pins. Partial weight bearing is allowed, and the child needs to learn to walk with crutches. Alterations in activity include modifications at school and in physical education. Full weight bearing is not allowed until the distraction is completed and bone consolidation has occurred. DIF: Cognitive Level: Applying REF: p. 1562 TOP: Integrated Process: Teaching/Learning MSC: Client Needs: Physiological Integrity 6. The nurse is caring for a 14-year-old child with systemic lupus erythematous (SLE). What clinical manifestations should the nurse expect to observe? (Select all that apply.) a. Arthralgia b. Weight gain c. Polycythemia d. Abdominal pain e. Glomerulonephritis , D, E Clinical manifestations of SLE include arthralgia, abdominal pain, and glomerulonephritis. Weight loss, not gain, and anemia, not polycythemia, are manifestations of SLE. DIF: Cognitive Level: Analyzing REF: p. 1608 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 7. The nurse is caring for a 14-year-old child with juvenile idiopathic arthritis (JIA). What clinical manifestations should the nurse expect to observe? (Select all that apply.) a. Erythema over joints b. Soft tissue contractures c. Swelling in multiple joints d. Morning stiffness of the joints e. Loss of motion in the affected joints , C, D, E Whether single or multiple joints are involved, stiffness, swelling, and loss of motion develop in the affected joints in JIA. The swelling results from soft tissue edema, joint effusion, and synovial thickening. The affected joints may be warm and tender to the touch, but it is not uncommon for pain not to be reported. The limited motion early in the disease is a result of muscle spasm and joint inflammation; later it is caused by ankylosis or soft tissue contracture. Morning stiffness of the joint(s) is characteristic and present on arising in the morning or after inactivity. Erythema is not typical, and a warm, painful, red joint is always suspect for infection. DIF: Cognitive Level: Analyzing REF: p. 1602 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity The correct calculation is: 55 lb/2.2 kg = 25 kg Dose of Azulfidine is 5 mg/kg 5 mg 25 = 125 mg DIF: Cognitive Level: Applying REF: p. 1604 TOP: Nursing Process: Implementation MSC: Client Needs: Physiological Integrity 2. The health care provider has prescribed cyclosporin (Sandimmune) 5 mg/kg/day PO divided twice daily for a child with juvenile arthritis. The child weighs 110 lb. The nurse is preparing to administer the 0900 dose. Calculate the dose the nurse should administer in milligrams. Record your answer in a whole number. _________ ANS: 125 The correct calculation is: 110 lb/2.2 kg = 50 kg Dose of Sandimmune is 5 mg/kg/day divided bid 5 mg 50 = 250 mg/day 250 mg/2 = 125 mg for one dose DIF: Cognitive Level: Applying REF: p. 1602 TOP: Nursing Process: Implementation MSC: Client Needs: Physiological Integrity 3. The health care provider has prescribed azathioprine (Imuran) 1 mg/kg/day PO for a child with juvenile arthritis. The child weighs 77 lb. The nurse is preparing to administer the daily dose. Calculate the dose the nurse should administer in milligrams. Record your answer below in a whole number. _______ ANS: 35 The correct calculation is: 77 lb/2.2 kg = 35 kg Dose of Imuran is 1 mg/kg/day 1 mg 35 = 35 mg for the daily dose DIF: Cognitive Level: Applying REF: p. 1609 TOP: Nursing Process: Implementation MSC: Client Needs: Physiological Integrity 4. The health care provider has prescribed hydroxychloroquine (Plaquenil) 5 mg/kg/day PO divided bid for a child with systemic lupus erythematosus. The child weighs 66 lb. The nurse is preparing to administer the 0900 dose. Calculate the dose the nurse should administer in milligrams. Record your answer below in a whole number. _________ ANS: 75 The correct calculation is: 66 lb/2.2 kg = 30 kg Dose of Plaquenil is 5 mg/kg/day divided bid 5 mg 30 = 150 mg 150 mg/2 = 75 mg DIF: Cognitive Level: Applying REF: p. 1609 TOP: Nursing Process: Implementation MSC: Client Needs: Physiological Integrity MATCHING Match the type of fracture to its definition. a. Transverse b. Oblique c. Spiral d. Comminuted 1. Slanting and circular, twisting around the bone shaft 2. Small fragments of bone are broken from the fractured shaft and lie in the surrounding tissue 3. Crosswise at right angles to the long axis of the bone 4. Slanting but straight between a horizontal and a perpendicular direction 1. DIF: Cognitive Level: Understanding REF: p. 1569 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 2. DIF: Cognitive Level: Understanding REF: p. 1569 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 3. DIF: Cognitive Level: Understanding REF: p. 1569 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 4. DIF: Cognitive Level: Understanding REF: p. 1569 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integri Chapter 35: The Child with Neuromuscular or Muscular Dysfunction MULTIPLE CHOICE 1. What is the most common cause of cerebral palsy (CP)? a. Central nervous system (CNS) diseases b. Birth asphyxia c. Cerebral trauma d. Neonatal encephalopathy Approximately 80% of CP is caused by unknown prenatal causes. Neonatal encephalopathy in term and preterm infants is believed to play a significant role in the development of CP. CNS diseases such as meningitis or encephalitis can result in CP. Birth asphyxia does contribute to some cases of CP. Cerebral trauma, including shaken baby syndrome, can result in CP. DIF: Cognitive Level: Understanding REF: p. 1632 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 2. Spastic cerebral palsy (CP) is characterized by which clinical manifestations? a. Athet TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 4. The parents of an infant with cerebral palsy (CP) ask the nurse if their child will have cognitive impairment. The nurse’s response should be based on which knowledge? a. Affected children have some degree of cognitive impairment. b. Around 20% of affected children have normal intelligence. c. About 45% of affected children have normal intelligence. d. Cognitive impairment is expected if motor and sensory deficits are severe. Children with CP have a wide range of intelligence, and 40% to 50% are within normal limits. A large percentage of children with CP do not have mental impairment. Many individuals who have severely limiting physical impairment have the least amount of intellectual compromise. DIF: Cognitive Level: Applying REF: p. 1620 TOP: Integrated Process: Teaching/Learning MSC: Client Needs: Physiological Integrity 5. Gingivitis is a common problem in children with cerebral palsy (CP). What preventive measure should be included in the plan of care? a. High-carbohydrate diet b. Meticulous dental hygiene c. Minimum use of fluoride d. Avoidance of medications that contribute to gingivitis Meticulous oral hygiene is essential. Many children with CP have congenital enamel defects, high-carbohydrate diets, poor nutritional intake, and difficulty closing their mouths. These, coupled with the child’s spasticity or clonic movements, make oral hygiene difficult. Children with CP have high carbohydrate intake and retention, which contribute to dental caries. Use of fluoride should be encouraged through fluoridated water or supplements and toothpaste. Certain medications such as phenytoin do contribute to gingival hyperplasia. If that is the drug of choice, then meticulous oral hygiene must be used. DIF: Cognitive Level: Applying REF: p. 1621 TOP: Nursing Process: Implementation MSC: Client Needs: Physiological Integrity 6. What is a major goal of therapy for children with cerebral palsy (CP)? a. Cure the underlying defect causing the disorder. b. Reverse the degenerative processes that have occurred. c. Prevent the spread to individuals in close contact with the child. d. Recognize the disorder early and promote optimum development. The goals of therapy include early recognition and promotion of an optimum developmental course to enable affected children to attain their potential within the limits of their dysfunction. The disorder is permanent, and therapy is chiefly symptomatic and preventive. It is not possible at this time to reverse the degenerative processes. CP is not contagious. DIF: Cognitive Level: Understanding REF: p. 1621 TOP: Nursing Process: Implementation MSC: Client Needs: Physiological Integrity 7. The parents of a child with spastic cerebral palsy (CP) state that their child seems to have significant pain. In addition to systemic pharmacologic management, the nurse includes which teaching? a. Patterning b. Positions to reduce spasticity c. Stretching exercises after meals d. Topical analgesics for muscle spasms Parents and childr nurse’s response should be based on which knowledge? a. Most activities such as Girl Scouts cannot be adapted for children with CP. b. After-school activities usually result in extreme fatigue for children with CP. c. Trying to participate in activities such as Girl Scouts leads to lowered self-esteem in children with CP. d. Recreational activities often provide children with CP with opportunities for socialization and recreation. After-school and recreational activities serve to stimulate children’s interest and curiosity. They help the children adjust to their disability, improve their functional ability, and build self-esteem. Increasing numbers of programs are adapted for children with physical limitations. Almost all activities can be adapted. The child should participate to her level of energy. Self-esteem increases as a result of the positive feedback the child receives from participation. DIF: Cognitive Level: Applying REF: p. 1626 TOP: Integrated Process: Teaching/Learning MSC: Client Needs: Psychosocial Integrity 10. A 4-month-old with significant head lag meets the criteria for floppy infant syndrome. A diagnosis of progressive infantile spinal muscular atrophy (Werdnig-Hoffmann disease) is made. What should be included in the nursing care for this child? a. Infant stimulation program b. Stretching exercises to decrease contractures c. Limited physical contact to minimize seizures d. Encouraging parents to have additional children Werdnig-Hoffmann disease (spinal muscular atrophy type 1) is the most common paralytic form of floppy infant syndrome (congenital hypotonia). An infant stimulation program is essential. Frequent position changes, including changes in environment, provide the child with more physical contacts. Verbal, tactile, and auditory stimulation are also included. Contractures do not occur because of muscular atrophy. Sensation is normal in children with this disorder. Frequent touch is necessary as part of the stimulation. Werdnig-Hoffmann disease is inherited as an autosomal recessive trait. Parents should be referred for genetic counseling. DIF: Cognitive Level: Applying REF: p. 1641 TOP: Nursing Process: Planning MSC: Client Needs: Physiological Integrity 11. An 8-year-old child is hospitalized with infectious polyneuritis (Guillain-Barré syndrome [GBS]). When explaining this disease process to the parents, what should the nurse consider? a. Paralysis is progressive with little hope for recovery. b. Disease is inherited as an autosomal, sex-linked, recessive gene. c. Disease results from an apparently toxic reaction to certain medications. d. Muscle strength slowly returns, and most children recover. Recovery usually begins within 2 to 3 weeks, and most patients regain full muscle strength. The paralysis is progressive with proximal muscle weakness occurring before distal weakness. The recovery of muscle strength occurs in the reverse order of onset of paralysis. Most individuals regain full muscle strength. Better outcomes are associated with younger ages. GBS is an immune-mediated disease often associated with a number of viral or bacterial infections or the administration of vaccines. DIF: Cognitive Level: Applying REF: p. 1644 TOP: Integrated Process: Teaching/Learning MSC: Client Needs: Physiological Integrity 12. A 12-year-old child with Guillain-Barré syndrome (GBS) is admitted to the pediatric intensive care unit. She tells you that yesterday her legs were weak and that this morning she was unable to walk. After the nurse determines the current level of paralysis, which should the next priority assessment be? a. Swallowing ability b. Parental involvement c. Level of consciousness d. Antecedent viral infections Assessment of swallowing is essential. Both pharyngeal involvement and respiratory function are usually involved at the same time. The child may require ventilatory support. The inability to swallow also contributes to aspiration pneumonia. Parental involvement is important after the physiologic assessment is complete. The child is answering questions and describing the onset of the illness, which demonstrates she is alert and oriented. Information regarding antecedent viral infections can be obtained after the child is assessed and stabilized. DIF: Cognitive Level: Applying REF: p. 1644 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 13. What statement is most accurate in describing tetanus? a. Inflammatory disease that causes extreme, localized muscle spasm. b. Disease affecting the salivary gland with resultant stiffness of the jaw. c. Acute infectious disease caused by an exotoxin produced by an anaerobic spore-forming, gram-positive bacillus. d. Acute infection that causes meningeal inflammation resulting in symptoms of generalized muscle spasm. Tetanus results from an infection by the anaerobic spore-forming, gram-positive bacillus Clostridium tetani. The organism forms two exotoxins that affect the central nervous system to produce the clinical manifestations of the disease. Tetanus is not an inflammatory process. The toxin acts at the neuromuscular junction to produce muscular stiffness and to lower the threshold for reflex excitability. It is usonstipated, is less active than usual, and has a weak-sounding cry. The nurse suspects botulism and questions the mother about the child’s diet. What factor should support this diagnosis? a. Breastfeeding b. Commercial formula c. Infant cereal with honey d. Improperly sterilized bottles Ingestion of honey is a risk factor for infant botulism in the United States. Honey should not be given to children younger than the age of 1 year. Botulism is not found with the use of commercial infant cereals. Although there is a slight increase in botulism in breastfed infants when compared with formula-fed infants, there is not sufficient evidence to support formula feeding as prevention. Thoroughly cleaning bottles used for formula feeding is sufficient for botulism prevention. Inadequate sterilization of home-canned foods can contribute to botulism. DIF: Cognitive Level: Analyzing REF: p. 1647 TOP: Integrated Process: Assessment MSC: Client Needs: Physiological Integrity 16. An adolescent has just been brought to the emergency department with a spinal cord injury and paralysis from a diving accident. The parents keep asking the nurse, “How bad is it?” The nurse’s response should be based on which knowledge? a. Families adjust better to life-threatening injuries when information is given over time. b. Immediate loss of function is indicative of the long-term consequences of the injury. c. Extent and severity of damage cannot be determined for several weeks or even months. d. Numerous diagnostic tests will be done immediately to determine extent and severity of damage. The extent and severity of damage cannot be determined initially. The immediate loss of function is caused by anatomic and impaired physiologic function, and improvement may not be evident for weeks or months. It is essential to provide information about the adolescent’s status to the parents. Immediate treatment information should be provided. Long-term rehabilitation and prognosis can be addressed after the child is stabilized. During the immediate postinjury period, physiologic responses to the injury make an accurate assessment of damage difficult. DIF: Cognitive Level: Applying REF: p. 1654 TOP: Integrated Process: Teaching/Learning MSC: Client Needs: Psychosocial Integrity 17. A 14-year-old girl is in the intensive care unit after a spinal cord injury 2 days ago. What nursing intervention is a priority for this chito achieve a significant level of independence. Some assistance is needed with transfers and lower extremity dressing. Patients are able to roll over in bed and to sit and eat independently. Patients with injuries at C3 or higher have complete respiratory paralysis. Those with injuries at C4 or higher do not have voluntary function of higher extremities. Injuries at C5 or higher prevent rolling over or sitting. DIF: Cognitive Level: Analyzing REF: p. 1651 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 19. An adolescent with a spinal cord injury is admitted to a rehabilitation center. Her parents describe her as being angry, hostile, and uncooperative. The nurse should recognize that this is suggestive of which psychosocial state? a. Normal phase of adolescent development b. Severe depression that will require long-term counseling c. Normal response to her situation that can be redirected in a healthy way d. Denial response to her situation that makes rehabilitative efforts more difficult During the rehabilitation phase, it is desirable for adolescents to begin to express negative feelings toward the situation. The rehabilitation team can redirect the negative energy toward learning a new way of life. The injury has interrupted the normal adolescent process of achieving independence, triggering these negative behaviors. Severe depression can occur, but it indicates that the child is no longer in denial. Long-term therapy is not indicated. Being angry, hostile, and uncooperative are behaviors that are indications that the adolescent understands the severity of the injury and need for rehabilitation. DIF: Cognitive Level: Applying REF: p. 1661 TOP: Integrated Process: Teaching/Learning MSC: Client Needs: Psychosocial Integrity 20. What statement best describes Duchenne (pseudohypertrophic) muscular dystrophy (DMD)? a. It has an autosomal dominant inheritance pattern. b. Onset occurs in later childhood and adolescence. c. It is characterized by presence of Gower sign, a waddling gait, and lordosis. d. Disease stabilizes during adolescence, allowing for life expectancy to approximately age 40 years. DMD is characterized by a waddling gait and lordosis. Gower sign is a characteristic way of rising from a squatting or sitting position on the floor. DMD is inherited as an X-linked recessive gene. Genetic counseling is recommended for parents, female siblings, maternal aunts, and their female offspring. Onset occurs usually between ages 3 and 5 years. DMD has a progressive and relentless loss of muscle function until death by respiratory or cardiac failure. DIF: Cognitive Level: Understanding REF: p. 1664 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 21. The nurse is preparing a staff education in-service session for a group of new graduate nurses who will be working in a long-term care facility for children; many of the children have cerebral palsy (CP). What statement should the nurse include in the training? a. Children with dyskinetic CP have a wide-based gait and repetitive movements. b. Children with spastic pyramidal CP have a positive Babinski sign and ankle clonus. c. 23. The nurse is caring for a 4-year-old child with cerebral palsy (CP). The child, developmentally, is at an infant stage. Appropriate developmental stimulation for this child should be what? a. Playing “pat-a-cake” with the child b. None so the child does not become overstimulated c. Putting a colorful mobile with music on the bed d. Giving the child a coloring book and crayons Incorporating play into the therapeutic program for a child with CP often requires great ingenuity and inventiveness from those involved in the child’s care. Objects and toys are chosen for the child’s developmental stage to provide needed sensory input using a variety of shapes, forms, and textures. Nurses can help parents integrate therapy into play activities in natural ways. DIF: Cognitive Level: Applying REF: p. 1622 TOP: Nursing Process: Implementation MSC: Client Needs: Health Promotion and Maintenance 24. A recommendation to prevent neural tube defects (NTDs) is the supplementation of what? a. Vitamin A throughout pregnancy b. Folic acid for all women of childbearing age c. Folic acid during the first and second trimesters of pregnancy d. Multivitamin preparations as soon as pregnancy is suspected The widespread use of folic acid among women of childbearing age has decreased the incidence NTDs. In the United States, the rates of NTDs have declined from 1.3 per 1000 births in 1990 to 0.3 per 1000 after the introduction of mandatory folic acid supplementation in food in 1998. Vitamin A is not related to the prevention of NTDs. Folic acid supplementation is recommended for the preconceptual period, as well as during the pregnancy. The NTD is a failure of neural tube closure during early development, the first 3 to 5 weeks. DIF: Cognitive Level: Understanding REF: p. 1628 TOP: Nursing Process: Implementation MSC: Client Needs: Physiological Integrity 25. The nurse is caring for a family whose infant was just born with anencephaly. What is the most important nursing intervention? a. Implement measures to facilitate the attachment process. b. Help the family cope with the birth of an infant with a fatal defect. c. Prepare the family for extensive surgical procedures that will be needed. d. Provide emotional support so the family can adjust to the birth of an infant with problems. Anencephaly is the most serious neural tube defect. The infants have an intact brainstem and, if born alive, may be able to maintain vital functions for a few hours to several weeks. The family requires emotional support and counseling to cope with the birth of an infant with a fatal defect. The parents should be encouraged to hold their infant and provide comfort measures. This facilitates the grieving process because the infant has a limited life expectancy. Infants with anencephaly do not have cerebral hemispheres. There is no surgical correction available for this defect. Emotional support is needed as the family adjusts to the birth of a child who has a fatal defect. DIF: Cognitive Level: Applying REF: p. 1631 TOP: Nursing Process: Implementation MSC: Client Needs: Psychosocial Integrity 26. What refers to a hernial protrusion of a saclike cyst of meninges, spinal fluid, and a portion of the spinal cord with its nerves through a defect in the vertebral column? a. Rachischisis b. Meningocele c. Encephalocele d. Myelomeningocele A myelomeningocele has a visible defect with an external saclike protrusion, containing meninges, spinal fluid, and nerves. Rachischisis is a fissure in the spinal column that leaves the meninges and the spinal cord exposed. Meningocele is a hernial protrusion of a saclike cyst of meninges with spinal fluid but no neural elements. Encephalocele is a herniation of brain and meninges through a defect in the skull, producing a fluid-filled sac. DIF: Cognitive Level: Understanding REF: p. 1631 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 27. A woman who is 6 weeks pregnant tells the nurse that she is worried that, even though she is taking folic acid supplements, the baby might have spina bifida because of a family history. The nurse’s response should be based on what? a. Prenatal detection is not possible yet. b. There is no genetic basis for the defect. c. Chromosome studies done on amniotic fluid can diagnose the defect prenatally. d. Open neural tube defects (NTDs) result in elevated concentrations of -fetoprotein in amniotic fluid. Ultrasound scanning and measurement of -fetoprotein may indicate the presence of anencephaly or myelomeningocele. The optimum time for performing this analyzing is between 16 and 18 weeks. Prenatal diagnosis is possible through amniocentesis. A multifactorial origin is suspected, including drugs, radiation, maternal malnutrition, chemicals, and possibly a genetic mutation. Chromosome abnormalities are not present in NTDs. DIF: Cognitive Level: Applying REF: p. 1631 TOP: Integrated Process: Teaching/Learning MSC: Client Needs: Physiological Integrity 28. The most important nursing intervention when caring for an infant with myelomeningocele in the preoperative stage is which? a. Take vital signs every hour. b. Place the infant on the side to decrease pressure on the spinal sac. c. Watch for signs that might indicate developing hydrocephalus. d. Apply a heat lamp to facilitate drying and toughening of the sac. The spinal sac is protected from damage until surgery is performed. Early surgical closure is recommended to prevent local trauma and infection. Monitoring vital signs and watching for signs that might indicate developing hydrocephalus are important interventions, but preventing trauma to the sac is a priority. The sac is kept moist until surgical intervention is done. DIF: Cognitive Level: Applying REF: p. 1638 TOP: Nursing Process: Planning MSC: Client Needs: Physiological Integrity 29. Neuropathic bladder disorders are common among children with which disorder? a. Plagiocephaly b. Meningocele c. Craniosynostosis d. Myelomeningocele Myelomeningocele is one of the most common causes of neuropathic bladder dysfunction among children. Plagiocephaly is the flattening of a side of the child’s head. This is not associated with neuropathic bladder. Children with meningocele usually do not have neuropathic bladder. Craniosynostosis is the premature closure of one or more cranial sutures. It is not associated with neuropathic bladder. DIF: Cognitive Level: Understanding REF: p. 1635 TOP: Nursing Process: Planning MSC: Client Needs: Physiological Integrity 30. What most accurately describes bowel function in children born with a myelomeningocele? a. Incontinence cannot be prevented. b. Enemas and laxatives are contraindicated. c. Some degree of fecal continence can usually be achieved. d. Colostomy is usually required by the time the child reaches adolescence. With a combination of dietary modification, regular toilet habits, and prevention of constipation and impaction, some degree of fecal continence can usually be achieved. Incontinence can be minimized with the development of a regular bowel training program. A surgical intervention can assist with continence. Enemas and laxatives are part of a bowel training program. Colostomies are not indicated in children with myelomeningocele. DIF: Cognitive Level: Understanding REF: p. 1637 TOP: Nursing Process: Planning MSC: Client Needs: Physiological Integrity 31. The nurse is caring for a neonate born with a myelomeningocele. Surgery to repair the defect is scheduled the next day. What is the most appropriate way to position and feed this neonate? a. Prone with the head turned to the side b. On the side c. Supine in an infant carrier d. Supine, with defect supported with rolled blankets The prone position with the head turned to the side for feeding is the optimum position for the infant. It protects the spinal sac and allows the infant to be fed without trauma. The side-lying position is avoided preoperatively. It can place tension on the sac and affect hip dysplasia if present. The infant should not be placed in a supine position. DIF: Cognitive Level: Applying REF: p. 1638 TOP: Nursing Process: Planning MSC: Client Needs: Physiological Integrity 32. A goal for children with spina bifida is to reduce the chance of allergy development. What is a priority nursing intervention? a. Recommend allergy testing. b. Provide a latex-free environment. c. Use only powder-free latex gloves. d. Limit use of latex products as much as possible. A latex-free environment is the goal. This includes eliminating the use of latex gloves and other medical devices containing latex. Allergy testing would provide information about whether the allergy has developed. It will not reduce the chances of developing the allergy. Although powder-free latex gloves are less allergenic, latex should not be used. Limiting the use of latex products is one component of providing a latex-free environment, but latex products should not be used. DIF: Cognitive Level: Applying REF: p. 1640 TOP: Nursing Process: Planning MSC: Client Needs: Physiological Integrity 33. When a child develops latex allergy, which food may also cause an allergic reaction? a. Yeast b. Wheat c. Peanuts d. Bananas There are cross-reactions between allergies to latex and to a number of foods such as bananas, avocados, kiwi, and chestnuts. Although yeast, wheat, and peanuts are potential allergens, currently they are not known to cross-react with latex allergy. DIF: Cognitive Level: Analyzing REF: p. 1640 TOP: Nursing Process: Planning MSC: Client Needs: Physiological Integrity 34. The clinic nurse is assessing infant reflexes. What assessment indicates a persistence of primitive reflexes? a. Tonic neck reflex at 8 months of age b. Palmar grasp at 4 months of age c. Plantar grasp at 9 months of age d. Rooting reflex at 3 months of age Persistence of primitive reflexes is one of the earliest clues to CP (e.g., obligatory tonic neck reflex at any age or nonobligatory persistence beyond 6 months of age and the persistence or even hyperactivity of the Moro, plantar, and palmar grasp reflexes). The palmar grasp disappears by 6 months, the plantar grasp disappears by 12 months, and the rooting reflex disappears at 4 months, so these are normal findings. DIF: Cognitive Level: Analyzing REF: p. 1620 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 35. A toddler with spastic cerebral palsy needs to be transported to the radiology department. What transportation method should the nurse use to take the toddler to the radiology department? a. A stretcher b. A wheelchair c. A wagon with pillows d. Carried in the nurse’s arms A wagon with pillows would support the child with spastic cerebral palsy better than a stretcher or wheelchair. A wagon would give the child a “wheelchair” experience, so the nurse should not carry the child. DIF: Cognitive Level: Applying REF: p. 1643 TOP: Nursing Process: Implementation MSC: Client Needs: Physiological Integrity 36. What is the rationale for orthopedic surgery for a child with cerebral palsy? a. To cure spasticity b. To improve function c. For cosmetic purposes d. T TOP: Integrated Process: Teaching/Learning MSC: Client Needs: Health Promotion and Maintenance 38. The nurse is teaching the family of an infant with cerebral palsy how to administer a diazepam (Valium) pill by gastrostomy tube. What should the nurse include in the teaching session? a. The pill should be crushed and mixed with a small amount of water. b. The pill should be crushed and mixed with the infant’s formula. c. After administering the medication, flush the tube with air. d. Before administering the medication, check the placement of the tube. Pills may be crushed and mixed with small amounts of water but not other liquids, such as formula or elixir medications, because these may act together to form a sludge that can interfere with gastrostomy tube function. When crushed pills or tablets are administered, flush the feeding tube with more water after instilling the dissolved pill in water. The tube should not be flushed with air, and placement does not need to be checked because it is directly into the stomach. DIF: Cognitive Level: Applying REF: p. 1627 TOP: Integrated Process: Teaching/Learning MSC: Client Needs: Health Promotion and Maintenance 39. The nurse is caring for a child with tetanus during the acute phase. What should the nurse plan in the care for this child? a. Playing music on a radio b. Giving frequent back rubs c. Providing bright lighting in the room d. Clustering nursing care to limit distractions In caring for a child with tetanus during the acute phase, every effort should be made to control or eliminate stimulation from sound, light, and touch. Although a darkened room is ideal, sufficient light is essential so that the child can be carefully observed; light appears to be less irritating than vibratory or auditory stimuli. The infant or child is handled as little as possible, and extra effort is expended to avoid any sudden or loud noise to prevent seizures. DIF: Cognitive Level: Applying REF: p. 1647 TOP: Nursing Process: Implementation MSC: Client Needs: Physiological Integrity 40. A mother tells the clinic nurse that she often puts honey on her infant’s pacifier to soothe the infant. What response should the nurse make to the mother? a. “That is a good way to soothe your baby.” b. “Honey does not have any soothing effects.” c. “There is still a risk for infant botulism from honey.” d. “Honey is OK, but it should not be put on the pacifier.” Although the precise source of Clostridium botulinum spores has not been identified as originating from honey in many cases of infant botulism in the United States, it is still recommended that honey not be given to infants younger than 12 months because the spores have been found in honey. DIF: Cognitive Level: Applying REF: p. 1648 TOP: Integrated Process: Teaching/Learning MSC: Client Needs: Health Promotion and Maintenance 41. The nurse is caring for a child with myasthenia gravis (MG). What health care prescription should the nurse verify before administering? a. Ceftizoxime (Cefizox) b. Cefotaxime (Claforan) c. Ceftriaxone (Rocephin) d. Garamycin (gentamicin) Avoid aminoglycoside antibiotics such as gentamicin because they potentiate MG symptoms. Cefizox, Claforan, and Rocephin are cephalosporin antibiotics. DIF: Cognitive Level: Applying REF: p. 1649 TOP: Nursing Process: Implementation MSC: Client Needs: Safe and Effective Care Environment MULTIPLE RESPONSE 1. What findings should the nurse expect to observe in a 7-month-old infant with Werdnig-Hoffman disease? (Select all that apply.) a. Noticeable scoliosis b. Absent deep tendon reflexes c. Abnormal tongue movements d. Failure to thrive e. Prominent pectus excavatum f. Significant leg involvement , C, D Clinical manifestations of Werdnig-Hoffman disease in an infant include absent deep tendon reflexes, abnormal tongue movements, and failure to thrive. Scoliosis, prominent pectus excavatum, and significant leg involvement are findings observed in a child with intermediate spinal muscular atrophy. DIF: Cognitive Level: Understanding REF: p. 1641 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 2. The nurse is teaching the family with a child with cerebral palsy (CP) strategies to prevent constipation. What should the nurse include in the teaching session? (Select all that apply.) a. Increase fluid intake. b.ntrols is a functional goal for a T1 to T10 spinal cord injury. Ambulation with bilateral long braces using four-point or swing-through crutch gait is a functional goal for a T10 to L2 injury. DIF: Cognitive Level: Understanding REF: p. 1651 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 4. What functional goal should the nurse expect for a child who has a T1 to T10 spinal cord injury? (Select all that apply.) a. May be braced for standing b. Able to drive automobile with hand controls c. Can manage adapted public transportation d. Some able to use regular public transportation e. Ambulates well, often with short leg braces with or without cane , B, C A child with a T1 to T10 spinal cord injury may be braced for standing, is able to drive an automobile with hand controls, and can manage adapted public transportation. The ability to use regular public transportation and ambulation with bilateral long braces using four-point or swing-through crutch gait are functional goals for individuals with a T10 to L2 injury. DIF: Cognitive Level: Understanding REF: p. 1651 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 5. The nurse is preparing to admit a 7-year-old child with ataxic cerebral palsy. What clinical manifestations of ataxic cerebral palsy should the nurse expect to observe? (Select all that apply.) a. Wide-based gait b. Rapid, repetitive movements performed poorly c. Slow, twisting movements of the trunk or extremities d. Hypertonicity with poor control of posture, balance, and coordinated motion e. Disintegration of movements of the upper extremities when the child reaches for objects , B, E Clinical manifestations of ataxic cerebral palsy include a wide-based gait; rapid, repetitive movements performed poorly; and disintegration of movements of the upper extremities when the child reaches for objects. Slow, twisting movements of the trunk are seen with dyskinetic cerebral palsy, and hypertonicity with poor control of posture, balance, and coordinated motion are seen with spastic cerebral palsy. DIF: Cognitive Level: Applying REF: p. 1619 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 6. What are some of the associated disabilities seen with cerebral palsy? (Select all that apply.) a. Visual impairment b. Hearing impairment c. Speech difficulties d. Intellectual impairment e. Associated heart defects , B, C, D Some of the disabilities associated with CP are visual impairment, hearing impairment, behavioral problems, communication and speech difficulties, seizures, and intellectual impairment. Additional sensory deficits such as hypersensitivity, hyposensitivity, and balance difficulties may occur in children with CP. DIF: Cognitive Level: Understanding REF: p. 1620 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 7. The nurse is preparing to admit a 5-year-old with spina bifida cystica that was below the second lumbar vertebra. What clinical manifestations of spina bifida cystica below the second lumbar vertebra should the nurse expect to observe? (Select all that apply.) a. No motor impairment b. Lack of bowel control c. Soft, subcutaneous lipomas d. Flaccid, partial paralysis of lower extremities e. Overflow incontinence with constant dribbling of urine , D, E The clinical manifestations of spina bifida cystica below the second lumbar vertebra include lack of bowel control, flaccid, partial paralysis of lower extremities, and overflow incontinence with constant dribbling of urine. No motor impairment occurs with spina bifida cystica that was below the third lumbar vertebra, and soft, subcutaneous lipomas occur with spina bifida occulta. DIF: Cognitive Level: Applying REF: p. 1633 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 8. The nurse is preparing to admit a 2-year-old child with spina bifida occulta. What clinical manifestations of spina bifida occulta should the nurse expect to observe? (Select all that apply.) a. Dark tufts of hair b. Skin depression or dimple c. Port-wine angiomatous nevi d. Soft, subcutaneous lipomas e. Bladder and sphincter paralysis , B, C, D Clinical manifestations of spina bifida occulta include dark tufts of hair; skin depression or dimple; port-wine angiomatous nevi; and soft, subcutaneous lipomas. Bladder and sphincter paralysis are present with spina bifida cystica but not occulta. DIF: Cognitive Level: Applying REF: p. 1633 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 9. The nurse is preparing to admit a 5-year-old child with a lower motor neuron syndrome. What clinical manifestations of a lower motor neuron syndrome should the nurse expect to observe? (Select all that apply.) a. Loss of hair b. Babinski reflex present c. Skin and tissue changes d. Marked atrophy of atonic muscle e. Hyperreflexia with tendon reflexes exaggerated , C, D Clinical manifestations of a lower motor neuron syndrome include loss of hair, skin and tissue changes, and marked atrophy of atonic m , C, E Clinical manifestations of an upper motor neuron syndrome include Babinski reflex present, no wasting of muscle mass, and hyperreflexia with tendon reflexes exaggerated. No flexor spasms and marked atrophy of atonic muscle are manifestations of a lower motor neuron syndrome. DIF: Cognitive Level: Applying REF: p. 1652 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity 11. The nurse is preparing to admit a 10-year-old child with Duchenne muscular dystrophy. What clinical features of Duchenne muscular dystrophy should the nurse recognize? (Select all that apply.) a. Calf muscle hypertrophy b. Late onset, usually between 6 and 8 years of age c. Progressive muscular weakness, wasting, and contractures d. Loss of independent ambulation by 9 to 12 years of age e. Slowly progressive, generalized weakness during adolescence , C, D, E Clinical features of Duchenne muscular dystrophy include calf muscle hypertrophy; progressive muscular weakness; wasting and contractures; loss of independent ambulation by 9 to 12 years of age; and slowly progressive, generalized weakness during adolescence. The onset is early, not late, usually between 3 and 5 years of age. DIF: Cognitive Level: Understanding REF: p. 1665 TOP: Nursing Process: Assessment MSC: Client Needs: Physiological Integrity COMPLETION 1. The health care provider has prescribed dantrolene sodium (Dantrium) 0.5 mg/kg PO once a day for a child with cerebral palsy. The child weighs 55 lb. Calculate the dose the nurse should administer in milligrams. Record your answer below using one decimal place. ________ ANS: 12.5 The correct calculation is: 55 lb/2.2 kg = 25 kg Dose of Dantrium is 0.5 mg/kg given once a day 0.5 mg 25 = 12.5 mg DIF: Cognitive Level: Applying REF: p. 1623 TOP: Nursing Process: Implementation MSC: Client Needs: Physiological Integrity 2. The health care provider has prescribed diazepam (Valium) 0.8 mg/kg/day PO divided q 6 hours for a child with cerebral palsy. The child weighs 110 lb. The nurse is preparing to administer the 1200 dose. Calculate the dose the nurse should administer in milligrams. Record your answer below in a whole number. _______ ANS: 10 The correct calculation is: 110 lb/2.2 kg = 50 kg Dose of Valium is 30 mg/kg/day divided q 6 hours 0.8 mg 50 = 40 mg/day 40 mg/4 = 10 mg for one dose DIF: Cognitive Level: Applying REF: p. 1623 TOP: Nursing Process: Implementation MSC: Client Needs: Physiological Integrity 3. The health care provider has prescribed neostigmine (Prostigmin) 0.04 mg/kg/per dose SC q 4 to 6 hrs PRN for a child with myasthenia gravis. The child weighs 77 lb. The nurse is preparing to administer a dose. Calculate the dose the nurse should administer in milligrams. Record your answer below using one decimal place. ________ ANS: 1.4 The correct calculation is: 77 lb/2.2 kg = 35 kg Dose of Prostigmin is 0.04 mg/kg/dose 0.04 mg 35 = 1.4 mg DIF: Cognitive Level: Applying REF: p. 1648 TOP: Nursing Process: Implementation MSC: Client Needs: Physiological Integrity 4. The health care provider has prescribed oxybutynin (Ditropan) 0.2 mg/kg/day divided bid for a child with myelomeningocele. The child weighs 33 lb. The nurse is preparing to administer the 0900 dose. Calculate the dose the nurse should administer in milligrams. Record your answer below using one decimal place. _______ ANS: 1.5 The correct calculation is: 33 lb/2.2 kg = 15 kg Dose of Ditropan is 0.2 mg/kg/day divided bid 0.2 mg 15 = 3 mg 3 mg/2 = 1.5 mg DIF: Cognitive Level: Applying REF: p. 1636 TOP: Nursing Process: Implementation MSC: Client Needs: Physiological Integrity 5. The h The correct calculation is: 22 lb/2.2 kg = 11 kg Dose of Depakene is 30 mg/kg/day divided bid 30 mg 11 = 330 mg 330 mg/2 = 165 mg for one dose DIF: Cognitive Level: Applying REF: p. 1623 TOP: Nursing Process: Implementation MSC: Client Needs: Physiological Integrity 7. The health care provider has prescribed carbamazepine (Tegretol) 20 mg/kg/day divided bid for a child with cerebral palsy having seizures. The child weighs 44 lb. The nurse is preparing to administer the 0900 dose. Calculate the dose the nurse should administer in milligrams. Record your answer below in a whole number. _________ ANS: 200 The correct calculation is: 44 lb/2.2 kg = 20 kg Dose of Tegretol is 20 mg/kg/day divided bid 20 mg 20 = 400 mg 400 mg/2 = 200 mg DIF: Cognitive Level: Applying REF: p. 1623 TOP: Nursing Process: Implementation MSC: Client Needs: Physiological Integrity [Show More]
Last updated: 1 year ago
Preview 1 out of 252 pages
Instant download
Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Apr 11, 2020
Number of pages
252
Written in
Additional information
This document has been written for:
Uploaded
Apr 11, 2020
Downloads
0
Views
58

.png)
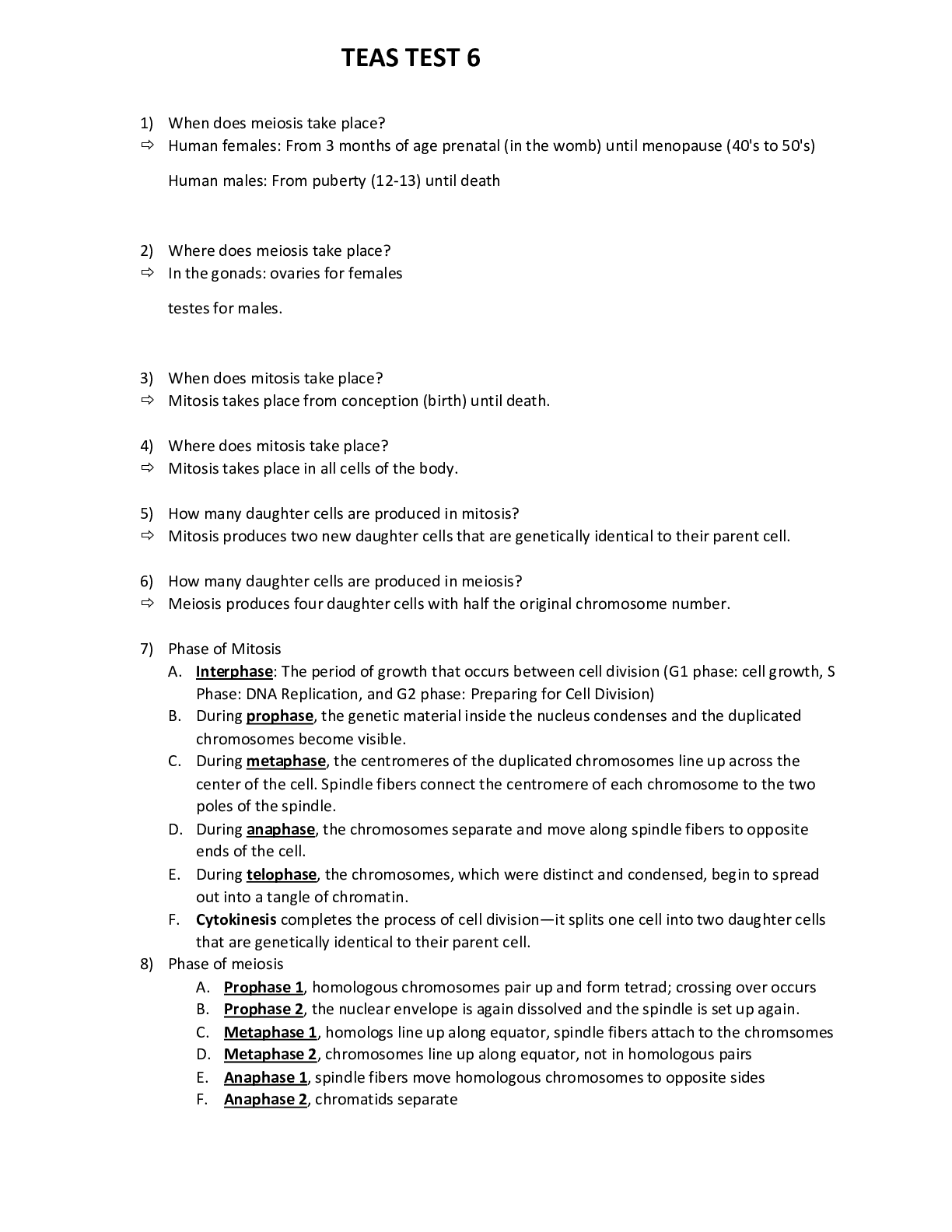

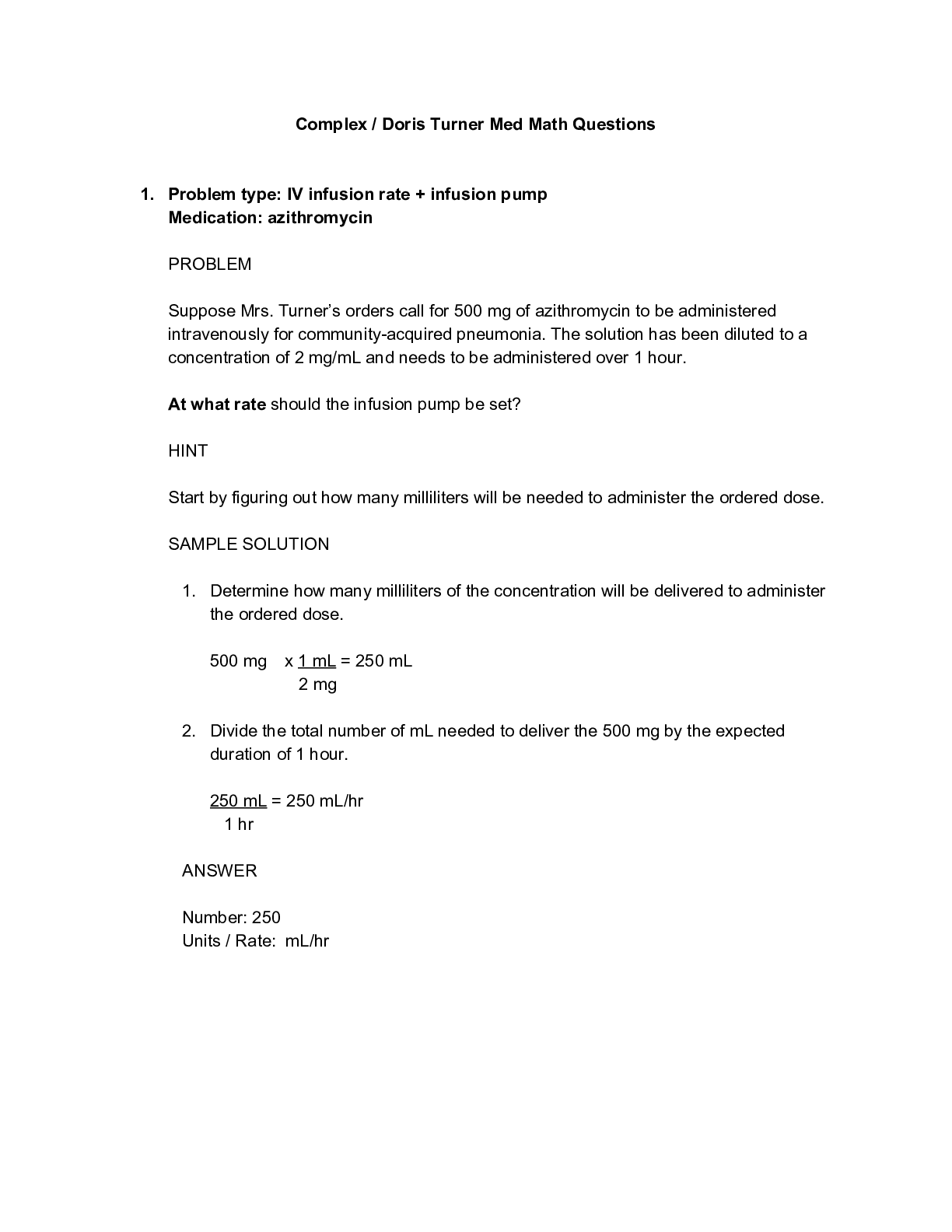
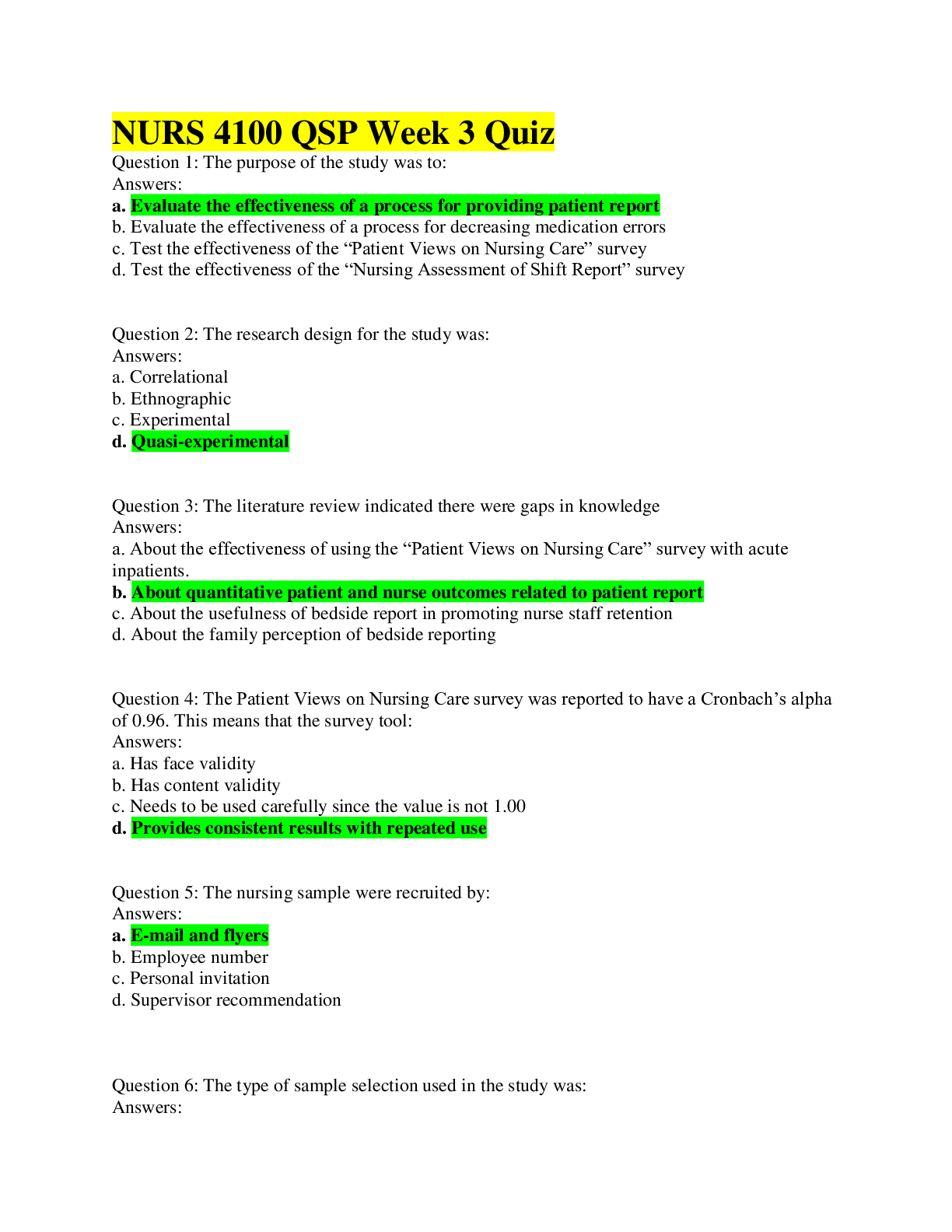
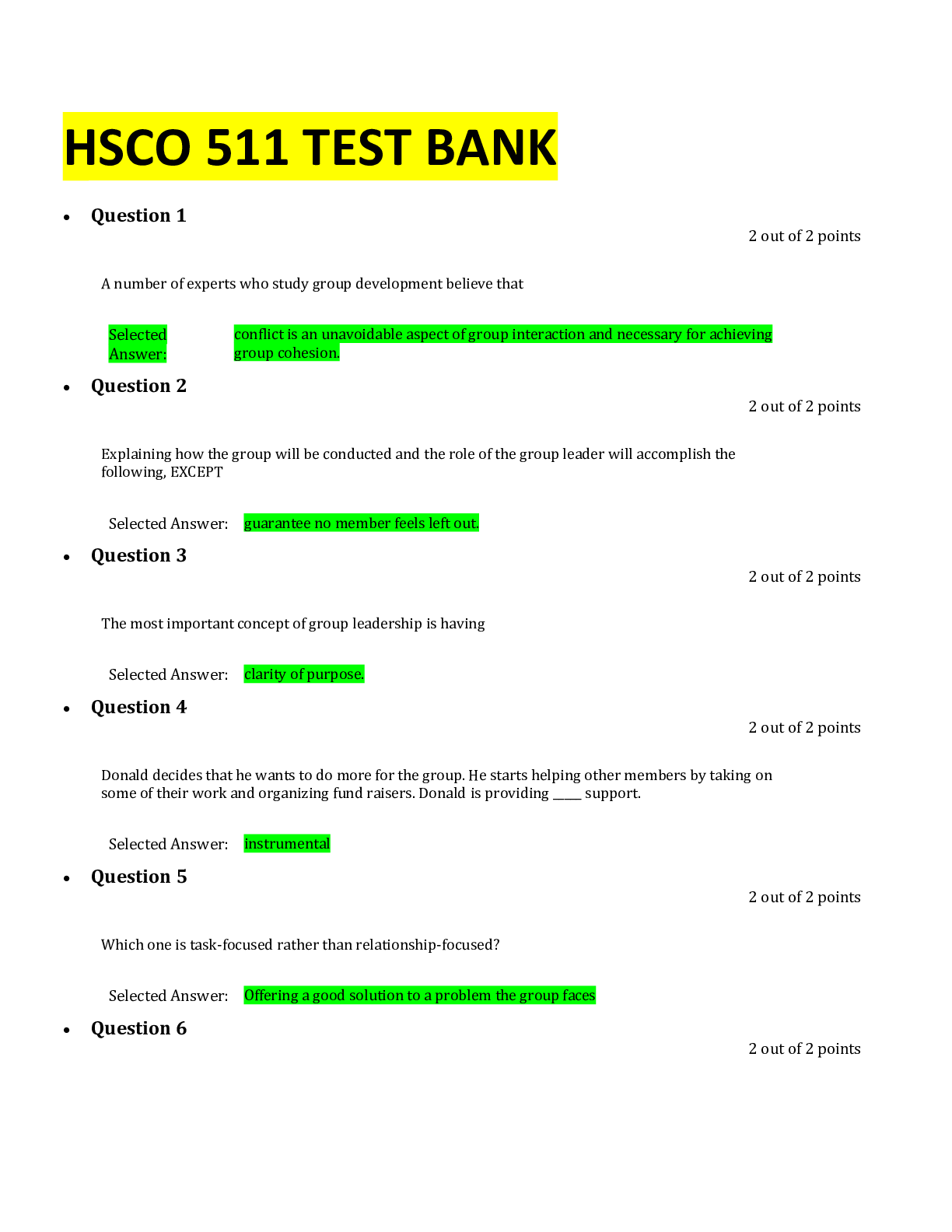
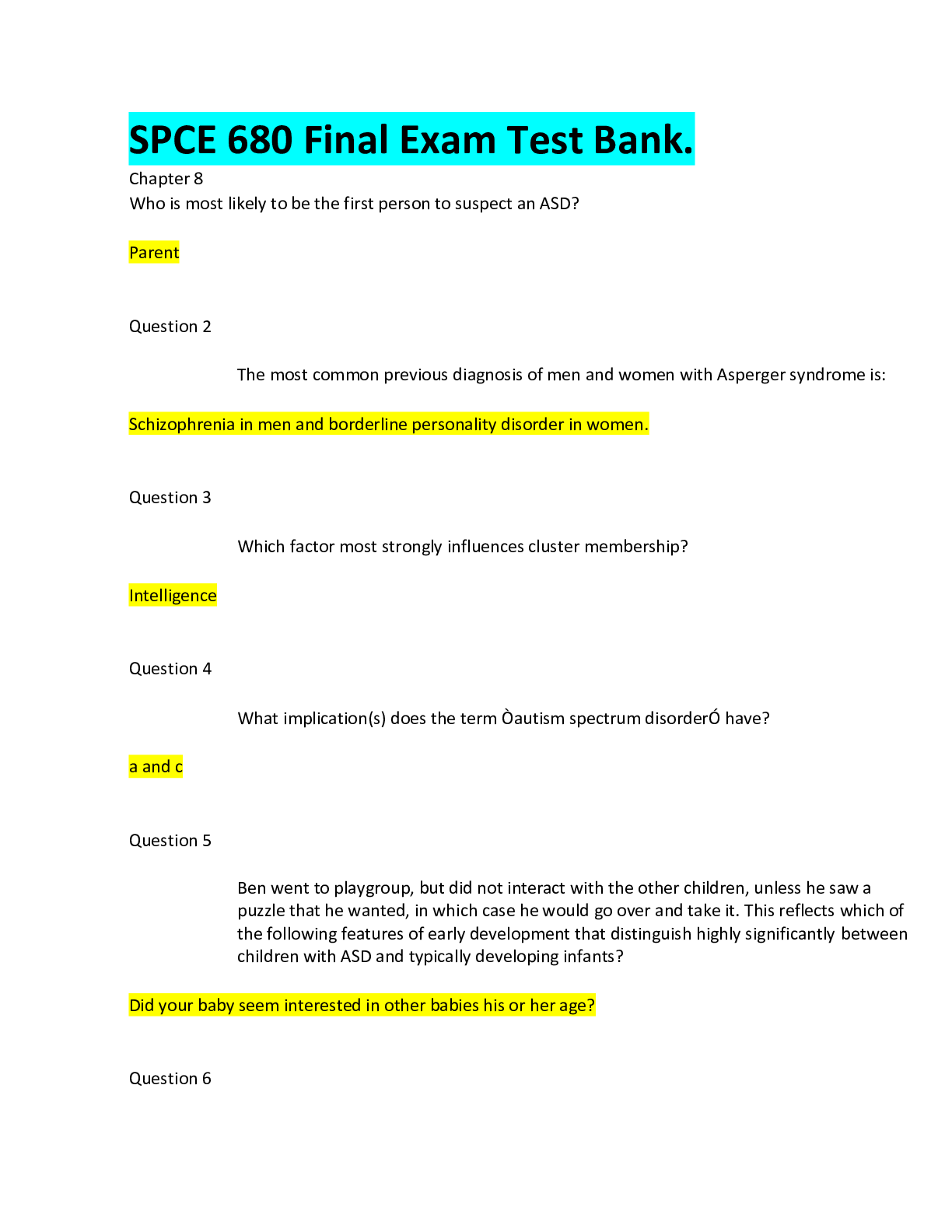
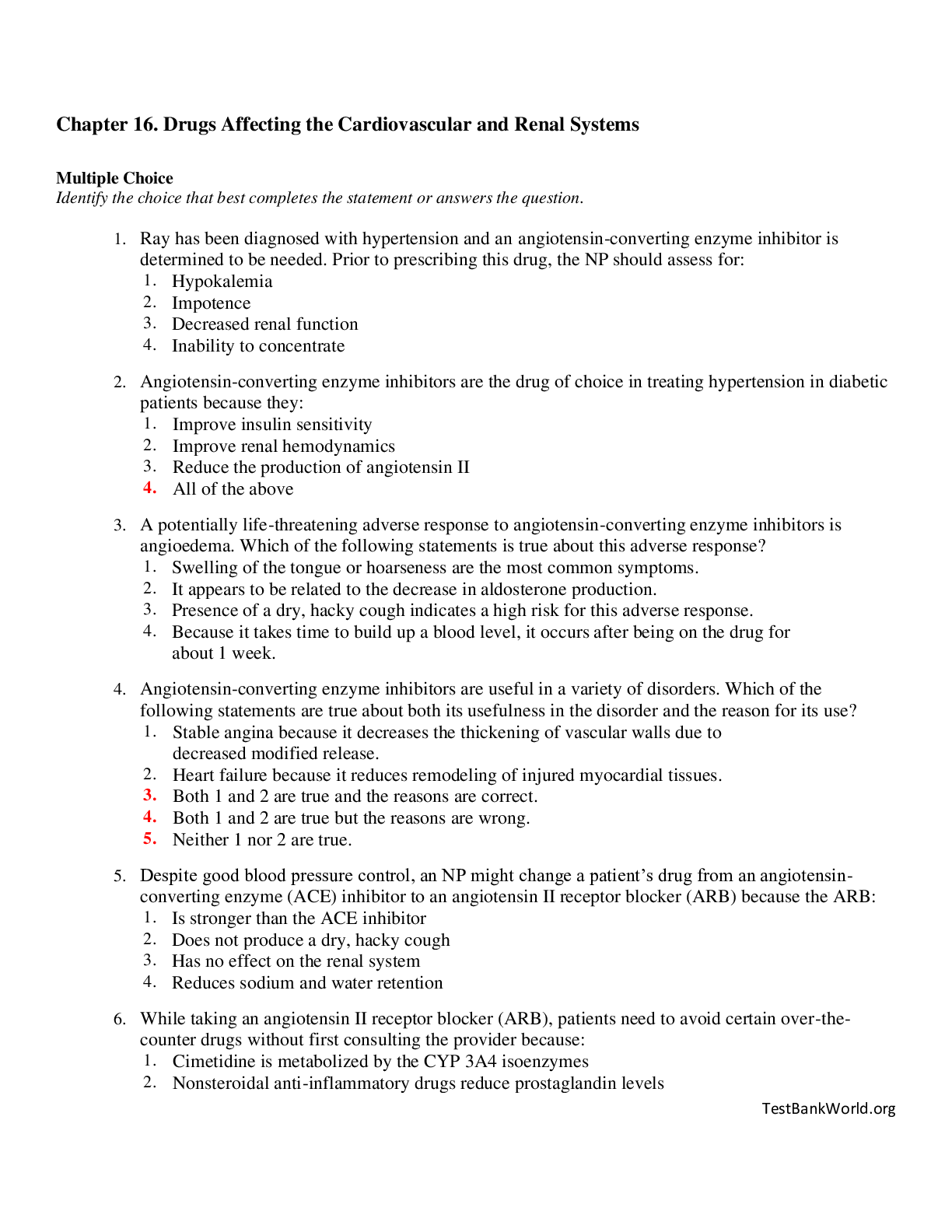

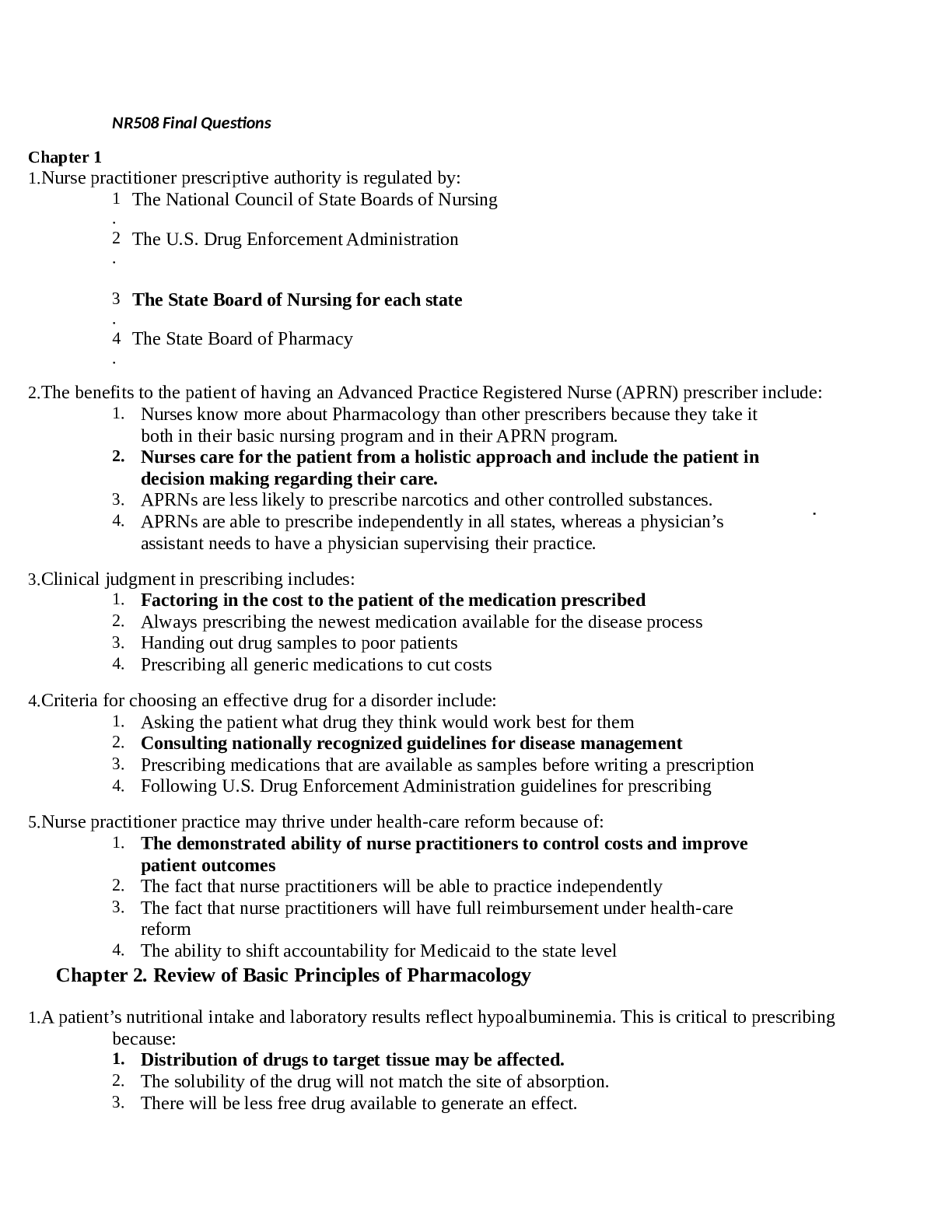
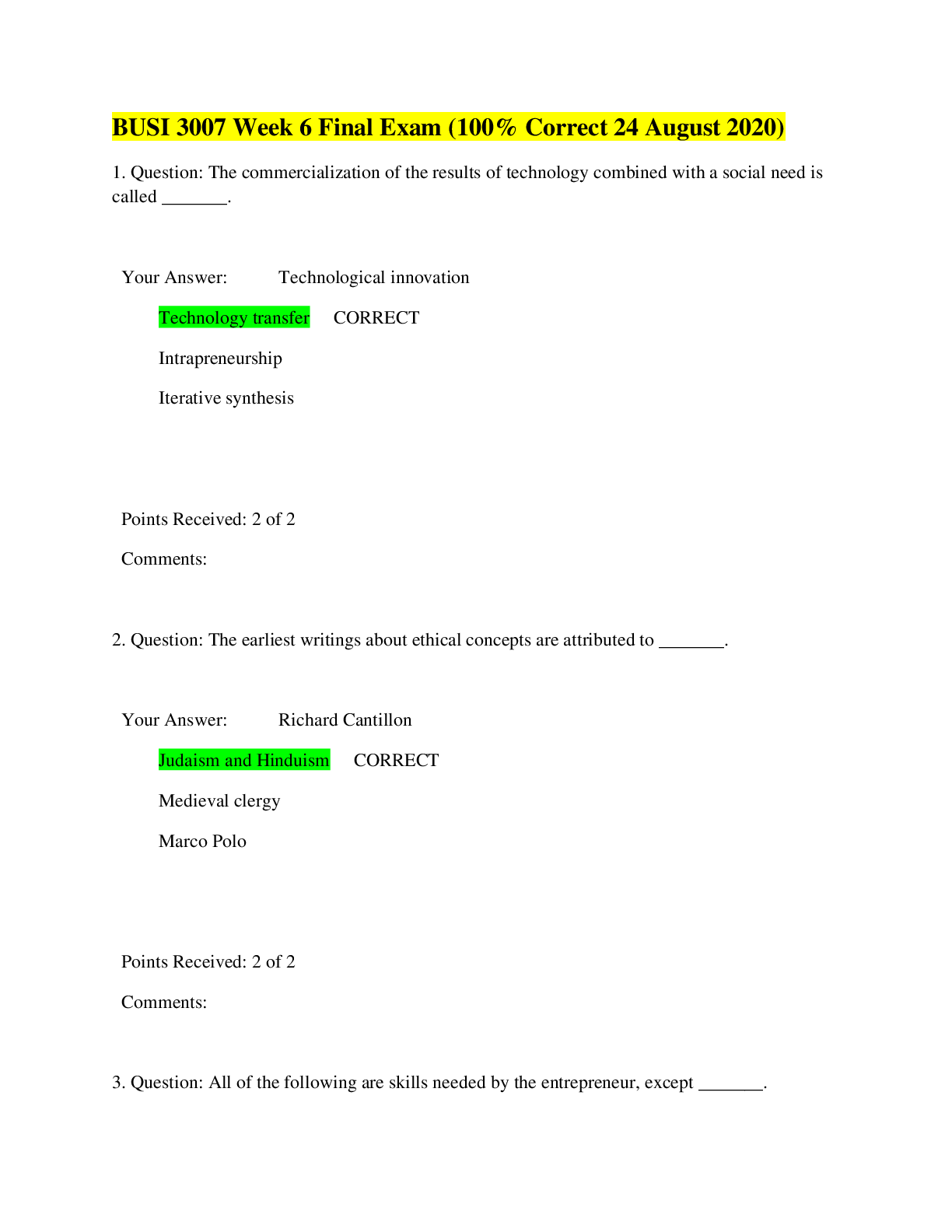
, 100% Correct, Download to Score A.png)