*NURSING > QUESTIONS & ANSWERS > Gastrointestinal - exam 1 Questions, Answers and Rationale Professional Nursing 2 (Rasmussen College (All)
Gastrointestinal - exam 1 Questions, Answers and Rationale Professional Nursing 2 (Rasmussen College) GASTROINTESTINAL
Document Content and Description Below
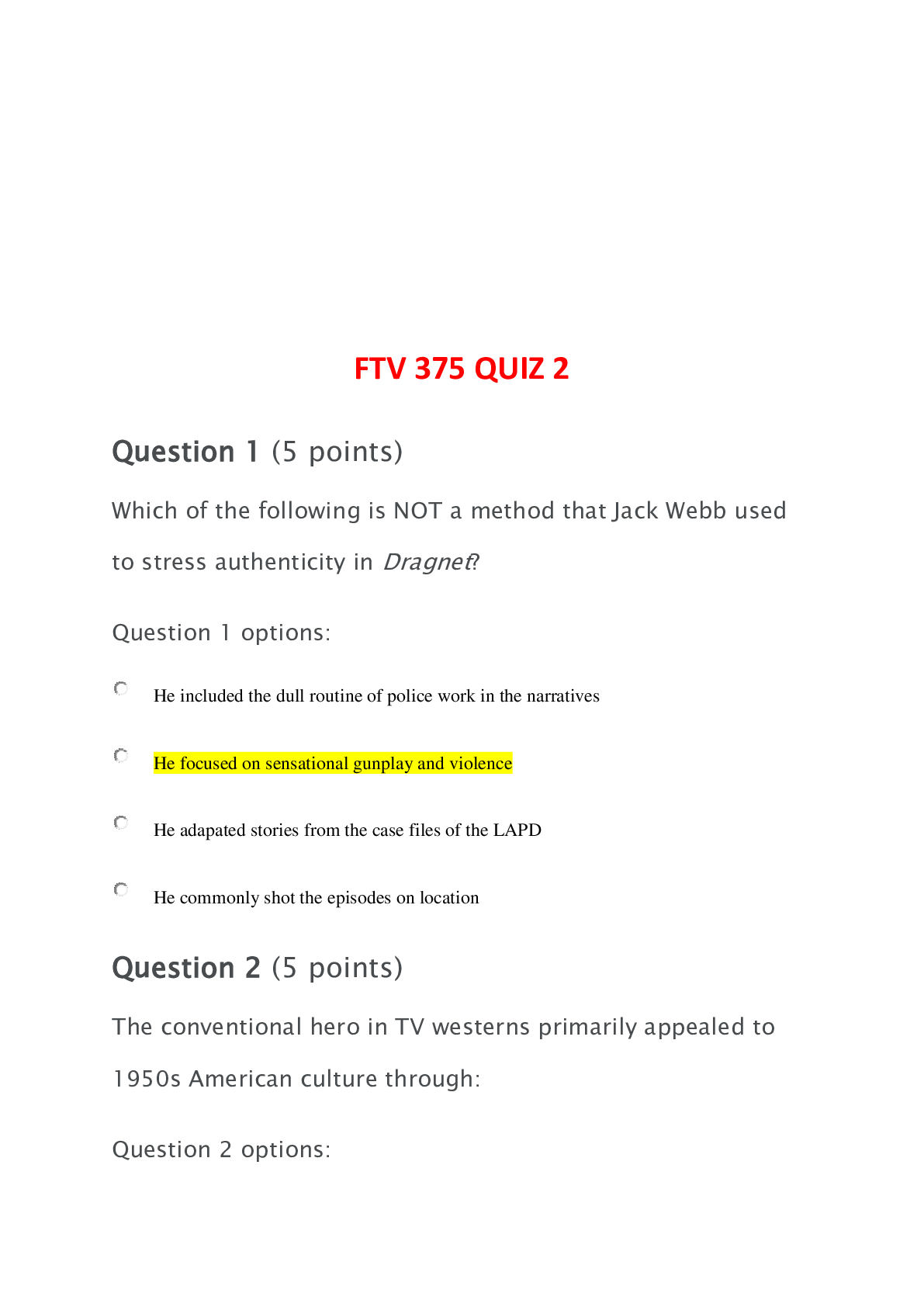
T-Tube NCLEX Questions for Nursing Care 1. A patient had a cholecystectomy and has a t-tube in place. You’re helping the nursing student understand how to care for the t-tube. The nursing student... asks you where the t-tube is located in the body. Your response is the: A. Cystic duct B. Hepatic duct C. Bile duct D. Pancreatic duct 2. The nurse helps the patient with a t-tube get up from the bed and sit in the bedside chair. Where will the nurse make it priority to position the tubing and drainage bag of the t-tube? A. Slightly elevated above the t-tube insertion site B. At heart level C. Midline with the t-tube insertion site D. At or below the waist 3. Which position is best for a patient with a t-tube? A. Supine B. Semi-Fowler’s C. Right lateral recumbent D. Left lateral recumbent 4. A patient is post-op day 4 from a t-tube placement. Which finding below requires you to notify the physician? A. Drainage from the t-tube is yellowish green. B. Drainage from the t-tube within the past 24 hours is approximately 925 cc. C. Blood tinged drainage from the t-tube has decreased. D. Patient reports a decrease in nausea. 5. The physician orders a patient’s t-tube to be clamped 1 hour before and 1 hour after meals. You clamp the t-tube as prescribed. While the tube is clamped which finding requires immediate nursing intervention? A. The t-tube is not draining. B. The t-tube tubing is below the patient’s waist. C. The patient reports nausea and abdominal pain. D. The patient’s stool is brown and formed. 6. You’re assessing a patient’s t-tube and note that it is not draining bile. The patient is reporting nausea. The nurse will first? A. Notify the physician B. Assess if the tubing from the t-tube is kinked or clamped. C. Flush the tubing. D. Administer an antiemetic medication per physician order. Cholecystits NCLEX Questions 1. The gallbladder is found on the side of the body and is located under the . It stores . A. right; pancreas; bilirubin B. left; liver; bile C. right; thymus’ bilirubin D. right; liver; bile 2. Which statements below are CORRECT regarding the role of bile? Select all that apply: A. Bile is created and stored in the gallbladder. B. Bile aids in digestion of fat soluble vitamins, such as A, D, E, and K. C. Bile is released from the gallbladder into the duodenum. D. Bile contains bilirubin. 3. You’re providing a community in-service about gastrointestinal disorders. During your teaching about cholecystitis, you discuss how cholelithiasis can lead to this condition. What are the risk factors for cholelithiasis that you will include in your teaching to the participants? Select all that apply: A. Being male B. Underweight C. Being female D. Older age E. Native American F. Caucasian G. Pregnant H. Family History I. Obesity 4. A patient is being transferred to your unit with acute cholecystitis. In report the transferring nurse tells you that the patient has a positive Murphy’s Sign. You know that this means: A. The patient stops breathing in when the examiner palpates under the ribs on the right upper side of the abdomen at the midclavicular line. B. The patient stops breathing out when the examiner palpates under the ribs on the right upper side of the abdomen at the midclavicular line. C. The patient verbalizes pain when the lower right quadrant is palpated. D. The patient reports pain when pressure is applied to the right lower quadrant but then reports an increase in pain intensity when the pressure is released. 5. Your patient is post-op day 3 from a cholecystectomy due to cholecystitis and has a T- Tube. Which finding during your assessment of the T-Tube requires immediate nursing intervention? A. The drainage from the T-Tube is yellowish/green in color. B. There is approximately 750 cc of drainage within the past 24 hours. C. The drainage bag and tubing is at the patient’s waist. D. The patient is in the Semi-Fowler’s position. 6. The physician orders a patient’s T-Tube to be clamped 1 hour before and 1 hour after meals. You clamp the T-Tube as prescribed. While the tube is clamped which finding requires you to notify the physician? A. The T-Tube is not draining. B. The T-Tube tubing is below the patient’s waist. C. The patient reports nausea and abdominal pain. D. The patient’s stool is brown and formed. 7. Your recent admission has acute cholecystitis. The patient is awaiting a cholecystostomy. What signs and symptoms are associated with this condition? Select all that apply: A. Right lower quadrant pain with rebound tenderness B. Negative Murphy’s Sign C. Epigastric pain that radiates to the right scapula D. Pain and fullness that increases after a greasy or spicy meal E. Fever GASTROINTESTINAL F. Tachycardia G. Nausea 8. A patient in the emergency room has signs and symptoms associated with cholecystitis. What testing do you anticipate the physician will order to help diagnose cholecystitis? Select all that apply: A. Lower GI series B. Abdominal ultrasound C. HIDA Scan (Hepatobiliary Iminodiacetic AciD scan) D. Colonoscopy 9. You’re precepting a nursing student who is helping you provide T-Tube drain care. You explain to the nursing student that the t-shaped part of the drain is located in what part of the biliary tract? A. Cystic duct B. Common hepatic duct GASTROINTESTINAL C. Common bile duct D. Pancreatic duct 10. Your patient is unable to have a cholecystectomy for the treatment of cholecystitis. Therefore, a cholecystostomy tube is placed to help treat the condition. Which statement about a cholecystostomy (C-Tube) is TRUE? A. The C-Tube is placed in the cystic duct of the gallbladder and helps drain infected bile from the gallbladder. B. Gallstones regularly drain out of the C-Tube, therefore, the nurse should flush the tube regularly to ensure patency. C. The C-Tube is placed through the abdominal wall and directly into the gallbladder where it will drain infected bile from the gallbladder. D. The tubing and drainage bag of the C-Tube should always be level with the insertion site to ensure the tube is draining properly. 11. A patient, who has recovered from cholecystitis, is being discharged home. What meal options below are best for this patient? A. Baked chicken with steamed carrots and rice B. Broccoli and cheese casserole with gravy and mashed potatoes C. Cheeseburger with fries D. Fried chicken with a baked potato 12. Your patient is diagnosed with acute cholecystitis. The patient is extremely nauseous. A nasogastric tube is inserted with GI decompression. The patient reports a pain rating of 9 on 1- 10 scale and states the pain radiates to the shoulder blade. Select all the appropriate nursing interventions for the patient: A. Encourage the patient to consume clear liquids. B. Administered IV fluids per MD order. C. Provide mouth care routinely. D. Keep the patient NPO. E. Administer analgesic as ordered. F. Maintain low intermittent suction to NG tube. As a nurse providing care to a patient with hepatitis, it is important to know the signs and symp 1. The liver receives blood from two sources. The is responsible for pumping blood rich in nutrients to the liver. A. hepatic artery B. hepatic portal vein C. mesenteric artery D. hepatic iliac vein 2. Which statements are INCORRECT regarding the anatomy and physiology of the liver? Select all that apply: A. The liver has 3 lobes and 8 segments. B. The liver produces bile which is released into the small intestine to help digest fats. C. The liver turns urea, a by-product of protein breakdown, into ammonia. D. The liver plays an important role in the coagulation process. 3. You’re providing an in-service on viral hepatitis to a group of healthcare workers. You are teaching them about the types of viral hepatitis that can turn into chronic infections. Which types are known to cause ACUTE infections ONLY? Select all that apply: A. Hepatitis A B. Hepatitis B C. Hepatitis C D. Hepatitis D E. Hepatitis E 4. Which patients below are at risk for developing complications related to a chronic hepatitis infection, such as cirrhosis, liver cancer, and liver failure? Select all that apply: A. A 55-year-old male with Hepatitis A. B. An infant who contracted Hepatitis B at birth. C. A 32-year-old female with Hepatitis C who reports using IV drugs. D. A 50-year-old male with alcoholism and Hepatitis D. E. A 30-year-old who contracted Hepatitis E. 5. A patient is diagnosed with Hepatitis A. The patient asks how a person can become infected with this condition. You know the most common route of transmission is? A. Blood B. Percutaneous C. Mucosal D. Fecal-oral The answer is D. Hepatitis A is most commonly transmitted via the fecal-oral route. 6. Which of the following is NOT a common source of transmission for Hepatitis A? Select all that apply: A. Water B. Food C. Semen D. Blood 7. A 36-year-old patient’s lab work show anti-HAV and IgG present in the blood. As the nurse you would interpret this blood work as? A. The patient has an active infection of Hepatitis A. B. The patient has recovered from a previous Hepatitis A infection and is now immune to it. C. The patient is in the preicetric phase of viral Hepatitis. D. The patient is in the icteric phase of viral Hepatitis. 8. TRUE or FALSE: A patient with Hepatitis A is contagious about 2 weeks before signs and symptoms appear and 1-3 weeks after the symptoms appear. 9. A 25-year-old patient was exposed to the Hepatitis A virus at a local restaurant one week ago. What education is important to provide to this patient? A. Inform the patient to notify the physician when signs and symptoms of viral Hepatitis start to appear. B. Reassure the patient the chance of acquiring the virus is very low. C. Inform the patient it is very important to obtain the Hepatitis A vaccine immediately to prevent infection. D. Inform the patient to promptly go to the local health department to receive immune globulin. 10. Select all the ways a person can become infected with Hepatitis B: A. Contaminated food/water B. During the birth process C. IV drug use D. Undercooked pork or wild game E. Hemodialysis F. Sexual intercourse 11. A patient has completed the Hepatitis B vaccine series. What blood result below would demonstrate the vaccine series was successful at providing immunity to Hepatitis B? A. Positive IgG B. Positive HBsAg C. Positive IgM D. Positive anti-HBs 12. A patient has lab work drawn and it shows a positive HBsAg. What education will you provide to the patient? A. Avoid sexual intercourse or intimacy such as kissing until blood work is negative. B. The patient is now recovered from a previous Hepatitis B infection and is now immune. C. The patient is not a candidate from antiviral or interferon medications. D. The patient is less likely to develop a chronic infection. 13. A patient with Hepatitis A asks you about the treatment options for this condition. Your response is? A. Antiviral medications B. Interferon C. Supportive care D. Hepatitis A vaccine 14. A patient was exposed to Hepatitis B recently. Postexposure precautions include vaccination and administration of HBIg (Hepatitis B Immune globulin). HBIg needs to be given as soon as possible, preferably after exposure to be effective. A. 2 weeks B. 24 hours C. 1 month D. 7 days 15. You’re providing education to a patient with an active Hepatitis B infection. What will you include in their discharge instructions? Select all that apply: A. “Take acetaminophen as needed for pain.” B. “Eat large meals that are spread out through the day.” C. “Follow a diet low in fat and high in carbs.” D. “Do not share toothbrushes, razors, utensils, drinking cups, or any other type of personal hygiene product.” E. “Perform aerobic exercises daily to maintain strength.” 16. What is the MOST common transmission route of Hepatitis C? A. Blood transfusion B. Sharps injury C. Long-term dialysis D. IV drug use 17. A patient is diagnosed with Hepatitis D. What statement is true about this type of viral Hepatitis? Select all that apply: A. The patient will also have the Hepatitis B virus. B. Hepatitis D is most common in Southern and Eastern Europe, Mediterranean, and Middle East. C. Prevention of Hepatitis D includes handwashing and the Hepatitis D vaccine. D. Hepatitis D is most commonly transmitted via the fecal-oral route. 18. Select all the signs and symptoms associated with Hepatitis? A. Arthralgia B. Bilirubin 1 mg/dL C. Ammonia 15 mcg/dL D. Dark urine E. Vision changes F. Yellowing of the sclera G. Fever H. Loss of appetite 19. A patient with Hepatitis has a bilirubin of 6 mg/dL. What findings would correlate with this lab result? Select all that apply: A. None because this bilirubin level is normal B. Yellowing of the skin and sclera C. Clay-colored stools D. Bluish discoloration on the flanks of the abdomen E. Dark urine F. Mental status changes 20. A patient with Hepatitis is extremely confused. The patient is diagnosed with Hepatic Encephalopathy. What lab result would correlate with this mental status change? A. Ammonia 100 mcg/dL B. Bilirubin 7 mg/dL C. ALT 56 U/L D. AST 10 U/L 21. The physician writes an order for the administration of Lactulose. What lab result indicates this medication was successful? A. Bilirubin <1 mg/dL B. ALT 8 U/L C. Ammonia 16 mcg/dL D. AST 10 U/L 22. How is Hepatitis E transmitted? A. Fecal-oral B. Percutaneous C. Mucosal D. Body fluids The answer is A. 23. Which patient below is at MOST risk for developing a complication related to a Hepatitis E infection? A. A 45-year-old male with diabetes. B. A 26-year-old female in the 3rd trimester of pregnancy. C. A 12-year-old female with a ventricle septal defect. D. A 63-year-old male with cardiovascular disease. 24. What is the BEST preventive measure to take to help prevent ALL types of viral Hepatitis? A. Vaccination B. Proper disposal of needles C. Hand hygiene D. Blood and organ donation screening 25. Select all the types of viral Hepatitis that have preventive vaccines available in the United States? A. Hepatitis A B. Hepatitis B C. Hepatitis C D. Hepatitis D E. Hepatitis E The answers are A and B. Currently there is only a vaccine for Hepatitis A and B in the U.S. 26. A patient is prescribed Peginterferon alfa-2a. The nurse will prepare to administer this medication what route? A. Oral B. Intramuscular C. Subcutaneous D. Intravenous The answer is C. This medication is administered subq. 27. A patient with viral Hepatitis states their flu-like symptoms have subsided. However, they now have yellowing of the skin and sclera along with dark urine. Based on this finding, this is what phase of Hepatitis? A. Icteric B. Posticteric C. Preicteric D. Convalescent 28. During the posticteric phase of Hepatitis the nurse would expect to find? Select all that apply: A. Increased ALT and AST levels along with an increased bilirubin level B. Decreased liver enzymes and bilirubin level C. Flu-like symptoms D. Resolved jaundice and dark urine Cirrhosis NCLEX Questions 1. Which condition is NOT a known cause of cirrhosis? A. Obesity B. Alcohol consumption C. Blockage of the bile duct D. Hepatitis C E. All are known causes of Cirrhosis The answer is E. All of these conditions can cause cirrhosis. 2. The liver receives it blood supply from two sources. One of these sources is called the , which is a vessel network that delivers blood in nutrients but in oxygen. A. hepatic artery, low, high B. hepatic portal vein, high, low C. hepatic lobule, high, low D. hepatic vein, low, high 3. A patient with late-stage cirrhosis develops portal hypertension. Which of the following options below are complications that can develop from this condition? Select all that apply: A. Increase albumin levels B. Ascites C. Splenomegaly D. Fluid volume deficient E. Esophageal varices 4. Your patient with cirrhosis has severe splenomegaly. As the nurse you will make it priority to monitor the patient for signs and symptoms of? Select all that apply: A. Thrombocytopenia B. Vision changes C. Increased PT/INR D. Leukopenia 5. A patient is admitted with hepatic encephalopathy secondary to cirrhosis. Which meal option selection below should be avoided with this patient? A. Beef tips and broccoli rabe B. Pasta noodles and bread C. Cucumber sandwich with a side of grapes D. Fresh salad with chopped water chestnuts 6. During your morning assessment of a patient with cirrhosis, you note the patient is disoriented to person and place. In addition while assessing the upper extremities, the patient’s hands demonstrate a flapping motion. What lab result would explain these abnormal assessment findings? A. Decreased magnesium level B. Increased calcium level C. Increased ammonia level D. Increased creatinine level 7. You are receiving shift report on a patient with cirrhosis. The nurse tells you the patient’s bilirubin levels are very high. Based on this, what assessment findings may you expect to find during your head-to-toe assessment? Select all that apply: A. Frothy light-colored urine B. Dark brown urine C. Yellowing of the sclera D. Dark brown stool E. Jaundice of the skin F. Bluish mucous membranes 8. A 45 year old male has cirrhosis. The patient reports concern about the development of enlarged breast tissue. You explain to the patient that this is happening because? A. The liver cells are removing too much estrogen from the body which causes the testicles to produce excessive amounts of estrogen, and this leads to gynecomastia. B. The liver is producing too much estrogen due to the damage to the liver cells, which causes the level to increase in the body, and this leads to gynecomastia. C. The liver cells are failing to recycle estrogen into testosterone, which leads to gynecomastia. D. The liver cells are failing to remove the hormone estrogen properly from the body, which causes the level to increase in the body, and this leads to gynecomastia. 9. You’re providing an in-service to new nurse graduates about esophageal varices in patients with cirrhosis. You ask the graduates to list activities that should be avoided by a patient with this condition. Which activities listed are correct: Select all that apply A. Excessive coughing B. Sleeping on the back C. Drinking juice D. Alcohol consumption E. Straining during a bowel movement F. Vomiting 10. While providing mouth care to a patient with late-stage cirrhosis, you note a pungent, sweet, musty smell to the breath. This is known as: A. Metallic Hepatico B. Fetor Hepaticus C. Hepaticoacidosis D. Asterixis 11. The physician orders Lactulose 30 mL by mouth per day for a patient with cirrhosis. What findings below demonstrates the medication is working effectively? Select all that apply: A. Decrease albumin levels B. Decrease in Fetor Hepaticus C. Patient is stuporous. D. Decreased ammonia blood level E. Presence of asterixis The answer is B and D. A patient with cirrhosis may experience a complication called hepatic encephalopathy. This will cause the patient to become confused (they may enter into a coma), GASTROINTESTINAL 12. reside in the liver and help remove bacteria, debris, and old red blood cells. A. Hepatocytes B. Langerhan cells C. Enterocytes D. Kupffer cells 13. Which of the following is NOT a role of the liver? A. Removing hormones from the body B. Producing bile C. Absorbing water D. Producing albumin GASTROINTESTINAL Pancreatitis NCLEX Questions 1. Inside the pancreas are special cells that secrete digestive enzymes and hormones. The cells that secrete digestive enzymes are known as cells. A. Islet of Langerhans B. Protease C. Acinar D. Amylase 2. From the pancreas and gallbladder, the common bile duct and pancreatic duct open into the where digestive enzymes and bile flow through the duodenum via the major duodenal papilla which is surrounded by a muscular valve that controls the release of digestive enzymes known as the . A. ampulla of vater, sphincter of Oddi B. papilla of vater, sphincter of Oddi C. minor duodenal papilla, ampulla of vater D. jejunum, sphincter of pylori 3. Select-ALL-that-apply: In the pancreas, the acinar cells release: A. Amylase B. Somatostatin C. Lipase GASTROINTESTINAL D. Protease 4. You’re caring for a 45 year old patient who is admitted with suspected acute pancreatitis. The patient reports having extreme mid-epigastric pain that radiates to the back. The patient states the pain started last night after eating fast food. As the nurse, you know the two most common causes of acute pancreatitis are: A. High cholesterol and alcohol abuse B. History of diabetes and smoking C. Pancreatic cancer and obesity D. Gallstones and alcohol abuse 5. Which patient below is at MOST risk for CHRONIC pancreatitis? A. A 25 year old female with a family history of gallstones. B. A 35 year old male who reports social drinking of alcohol. C. A 15 year old female with cystic fibrosis. D. A 66 year old female with stomach cancer. 6. Your patient with acute pancreatitis is scheduled for a test that will use a scope to assess the pancreas, bile ducts, and gallbladder. The patient asks you, “What is the name of the test I’m going for later today?” You tell the patient it is called: A. MRCP B. ERCP GASTROINTESTINAL C. CT scan of the abdomen D. EGD 7. A patient is admitted to the ER with the following signs and symptoms: very painful mid- epigastric pain felt in the back, elevated glucose, fever, and vomiting. During the head-to-toe assessment, you notice bluish discoloration around the belly button. As the nurse, you know this is called? A. Grey-Turner’s Sign B. McBurney’s Sign C. Homan’s Sign D. Cullen’s Sign 8. While assisting a patient with chronic pancreatitis to the bathroom, you note the patient’s stool to be oily/greasy in appearance. In your documentation you note this as: A. Steatorrhea B. Melena C. Currant D. Hematochezia 9. A patient with acute pancreatitis is reporting excessive thirst, excessive voiding, and blurred vision. As the nurse, it is priority you? A. Reassure the patient this is normal with pancreatitis GASTROINTESTINAL B. Check the patient’s blood glucose C. Assist the patient with drinking a simple sugar drink like orange juice D. Provide a dark and calm environment 10. A patient who received treatment for pancreatitis is being discharged home. You’re providing diet teaching to the patient. Which statement by the patient requires immediate re- education about the diet restrictions? A. “It will be hard but I will eat a diet low in fat and avoid greasy foods.” B. “It is very important I limit my alcohol intake to no more than 2-3 glasses of wine a week.” C. “I will concentrate on eating complex carbohydrates rather than refined carbohydrates.” D. “I will purchase foods that are high in protein.” 11. The physician orders a patient with pancreatitis to take a pancreatic enzyme. What assessment finding demonstrates the pancreatic enzymes are working properly? A. Abdominal girth is decreased B. Skin turgor is less than 2 seconds C. Blood glucose is 250 D. Stools appear formed and solid 12. During a home health visit, you are assessing how a patient takes the prescribed pancreatic enzyme. The patient is unable to swallow the capsule whole, so they open the capsule and mix the beads inside the capsule with food/drink. Which food or drink is safe for the patient to mix the beads with? GASTROINTESTINAL A. Pudding B. Ice cream C. Milk D. Applesauce Celiac Disease NCLEX Questions 1. You’re educating a group of nursing students about the pathophysiology of Celiac Disease. You ask the group to identify the specific protein that plays a role in the immune reaction experienced in Celiac Disease. Which answer is correct? A. Zein B. Globulins C. Gliadins D. Glutamate 2. A patient is suspected to be suffering from Celiac Disease. The physician orders an endoscopy. If the patient has Celiac Disease, what finding will be discovered with the endoscopy? A. Over exaggerated intestinal villi B. Ulcerations in the small intestine, specifically the Jejunum C. Flat intestinal villi GASTROINTESTINAL D. Cobble-stone appearance throughout the small intestine 3. Which of the following is not an anti-body blood test ordered by a physician to diagnose Celiac Disease? A. Antinuclear antibody (ANA) B. Tissue Transglutaminase Antibodies (tTG-IgA) C. IgA Endomysial antibody (EMA) D. IgA serum 4. A patient, who was recently diagnosed with Celiac Disease, has blister type bumps on the elbow and knees. The patient reports it is extremely itchy. As the nurse, you know this is as known as: A. Seborrheic Dermatitis B. Psoriasis C. Dyshidrotic Eczema D. Dermatitis Herpetiformis 5. During an outpatient clinic visit, a female patient reports feeling abdominal bloating/pain, and diarrhea when eating foods that contain wheat or rye. The patient states her mother was diagnosed with Celiac Disease 5 years ago. What other symptoms will you assess the patient for that can be present in Celiac Disease? SELECT-ALL-THAT-APPLY: A. Unexplained Weight loss B. Jelly-like stools GASTROINTESTINAL C. Mouth ulcers D. Menstrual irregularities E. Pain at McBurney’s Point F. Ribbon-like stools G. Inability to tolerate dairy products H. Enamel changes 6. Your patient was admitted 3 days ago for treatment of severe malnourishment secondary to Celiac Disease. The patient is doing well and will be discharged tomorrow. When you arrive to the patient’s room, the patient’s friends and family are visiting and have brought dinner for the patient. Which food item below should the patient avoid consuming? A. Pork barbeque sandwich B. Steak and steamed broccoli C. Braised chicken with carrots D. Vegetables and rice 7. Gliadin is a wheat prolamin, which is a plant storage protein that is high in the amino acids particularly and . A. lysine and proline B. glutamine and cysteine C. gliadin and gluten GASTROINTESTINAL D. proline and glutamine 8. You’re helping a mother, whose child was recently diagnosed with Celiac Disease, read food labels. Which items below, if listed as the ingredients, should the mother avoid feeding her child? A. Millet B. Wheat C. Malt D. Corn E. Buckwheat F. Rye GASTROINTESTINAL GERD NCLEX Questions 1. A patient reports frequent heartburn twice a week for the past 4 months. What other symptoms reported by the patient may indicate the patient has GERD? SELECT-ALL-THAT-APPLY: A. Bitter taste in mouth B. Dry cough C. Melena D. Difficulty swallowing E. Smooth, red tongue F. Murphy’s Sign 2. Your patient, who is presenting with signs and symptoms of GERD, is scheduled to have a test that assesses the function of the esophagus’ ability to squeeze food down into the stomach and the closer of the lower esophageal sphincter. The patient asks you, “What is the name of the test I’m having later today?” You tell the patient the name of the test is: A. Lower Esophageal Gastrointestinal Series B. Transesophageal echocardiogram C. Esophageal manometry D. Esophageal pH monitoring 3. After dinner time, during hourly rounding, a patient awakes to report they feel like “food is coming up” in the back of their throat and that there is a bitter taste in their mouth. What nursing intervention will you perform next? A. Perform deep suctioning B. Assist the patient into the Semi-Fowler’s position C. Keep the patient NPO D. Instruct the patient to avoid milk products 4. During a home health visit, you are helping a patient develop a list of foods they should avoid due to GERD. Which items in the patient’s pantry should be avoided? SELECT-ALL-THAT- APPLY: A. Hot and Spicy Pork Rinds B. Peppermint patties C. Green Beans D. Tomato Soup E. Chocolate Fondue F. Almonds G. Oranges 5. After providing education to a patient with GERD. You ask the patient to list 4 things they can do to prevent or alleviate signs and symptoms of GERD. Which statement is INCORRECT? A. “It is best to try to consume small meals throughout the day than eat 3 large ones.” B. “I’m disappointed that I will have to limit my intake of peppermint and spearmint because I love eating those types of hard candies.” C. “It is important I avoid eating right before bedtime.” D. “I will try to lie down after eating a meal to help decrease pressure on the lower esophageal sphincter.” 6. You’re collecting a patient’s medication history that has GERD. Which medication below is NOT typically used to treat GERD? A. Colesevelam “Welchol” B. Omeprazole “Prilosec” C. Metoclopramide “Reglan” D. Ranitidine HCL “Zantac” 7. A patient is taking Bethanechol “Urecholine” for treatment of GERD. This is known as what type of drug? A. Proton-pump inhibitor B. Histamine receptor blocker C. Prokinetic D. Mucosal Healing Agent 8. Which of the following does NOT play a role in the development of GERD? A. Pregnancy B. Hiatal hernia C. Usage of antihistamines or calcium channel blockers D. All the above play a role in GERD Peptic Ulcer Disease NCLEX Questions 1. In the stomach lining, the parietal cells release and the chief cells release which both play a role in peptic ulcer disease. A. pepsin, hydrochloric acid B. pepsinogen, pepsin C. pepsinogen, gastric acid D. hydrochloric acid, and pepsinogen 2. A patient has developed a duodenal ulcer. As the nurse, you know that which of the following plays a role in peptic ulcer formation. Select ALL that apply: A. Spicy foods B. Helicobacter pylori C. NSAIDs D. Milk E. Zollinger-Ellison Syndrome 3. You’re educating a group of patients at an outpatient clinic about peptic ulcer formation. Which statement is correct about how peptic ulcers form? A. “An increase in gastric acid is the sole cause of peptic ulcer formation.” B. “Peptic ulcers can form when acid penetrates unprotected stomach mucosa. This causes histamine to be released which signals to the parietal cells to release more hydrochloric acid which erodes the stomach lining further.” C. “Peptic ulcers form when acid penetrates unprotected stomach mucosa. This causes pepsin to be released which signals to the parietal cells to release more pepsinogen which erodes the stomach lining further.” D. “The release of prostaglandins cause the stomach lining to breakdown which allows ulcers to form.” 4. Your patient is diagnosed with peptic ulcer disease due to h.pylori. This bacterium has a unique shape which allows it to penetrate the stomach mucosa. You know this bacterium is: A. Rod shaped B. Spherical shaped C. Spiral shaped D. Filamentous shaped 5. Helicobacter pylori can live in the stomach’s acidic conditions because it secretes which neutralizes the acid. A. ammonia B. urease C. carbon dioxide D. bicarbonate 6. The physician orders a patient with a duodenal ulcer to take a UREA breath test. Which lab value will the test measure to determine if h. pylori is present? A. Ammonia B. Urea C. Hydrochloric acid D. Carbon dioxide 7. A patient arrives to the clinic for evaluation of epigastric pain. The patient describes the pain to be relieved by food intake. In addition, the patient reports awaking in the middle of the night with a gnawing pain in the stomach. Based on the patient’s description this appears to be what type of peptic ulcer? A. Duodenal B. Gastric C. Esophageal D. Refractory 8. A patient with chronic peptic ulcer disease underwent a gastric resection 1 month ago and is reporting nausea, bloating, and diarrhea 30 minutes after eating. What condition is this patient most likely experiencing? A. Gastroparesis B. Fascia dehiscence C. Dumping Syndrome D. Somogyi effect 9. Thinking back to the patient in question 8, select ALL the correct statements on how to educate this patient about decreasing their symptoms: A. “It is best to eat 3 large meals a day rather than small frequent meals.” B. “After eating a meal lie down for 30 minutes.” C. “Eat a diet high in protein, fiber, and low in carbs.” D. “Be sure to drink at least 16 oz. of milk with meals.” 10. A patient is recovering from discomfort from a peptic ulcer. The doctor has ordered to advance the patient’s diet to solid foods. The patient’s lunch tray arrives. Which food should the patient avoid eating? A. Orange B. Milk C. White rice D. Banana 11. Which statement is INCORRECT about Histamine-receptor blockers? A. “H2 blockers block histamine which causes the chief cells to decrease the secretion of hydrochloric acid.” B. “Ranitidine and Famotidine are two types of histamine-receptor blocker medications.” C. “Antacids and H2 blockers should not be given together.” D. All the statements are CORRECT. 12. You are providing discharge teaching to a patient taking Sucralfate (Carafate). Which statement by the patient demonstrates they understand how to take this medication? A. “I will take this medication at the same time I take Ranitidine.” B. “I will always take this medication on an empty stomach.” C. “It is best to take this medication with antacids.” D. “I will take this medication once a week.” 13. Select all the medications a physician may order to treat a H. Pylori infection that is causing a peptic ulcer? A. Proton-Pump Inhibitors B. Antacids C. Anticholinergics D. 5-Aminosalicylates E. Antibiotics F. H2 Blockers G. Bismuth Subsalicylates 14. A physician prescribes a Proton-Pump Inhibitor to a patient with a gastric ulcer. Which medication is considered a PPI? A. Pantoprazole B. Famotidine C. Magnesium Hydroxide D. Metronidazole 15. A patient with a peptic ulcer is suddenly vomiting dark coffee ground emesis. On assessment of the abdomen you find bloating and an epigastric mass in the abdomen. Which complication may this patient be experiencing? A. Obstruction of pylorus GASTROINTESTINAL B. Upper gastrointestinal bleeding C. Perforation 1. B Diverticulosis and Diverticulitis NCLEX Questions 1. Most patients with diverticulosis are most likely to have diverticula located in the? A. Transverse colon GASTROINTESTINAL B. Sigmoid Colon C. Rectum D. Ascending Colon 2. You’re providing nursing education to a group of nursing students about diverticulosis versus diverticulitis. Which statement by the nursing students demonstrate they understand the education provided? A. “Most patients with diverticulitis are asymptomatic.” B. “Diverticulosis tends to occur in young women with a family history of diverticulosis.” C. “Diverticulitis, if not treated, can lead to abscess formation and peritonitis.” D. “Patients with diverticulosis should at all times avoid eating seeds and nuts.” 3. A patient with a history of diverticulosis is admitted with abdominal pain. The physician suspects diverticulitis. What other findings would correlate with diverticulitis? SELECT-ALL- THAT-APPLY: A. Abdominal pain that is mainly present in the upper right quadrant B. Unrelenting cramping type pain C. Pain found at McBurney’s Point D. Blood in stool E. Fever F. Reports of constipation GASTROINTESTINAL G. Abdominal bloating H. Positive Cullen’s Sign 4. A patient asks what type of testing is performed to assess for diverticulosis. As the nurse, you know that which test below is used to assess for diverticulosis? A. Colonoscopy B. Fleets enema C. Bronchoscopy D. Cystoscopy 5. A patient is experiencing an acute episode of diverticulitis. The patient is having abdominal pain, temperature 102.6 ‘F, and elevated WBCs. As the nurse, you know it is important to: A. Encourage intake of high-fiber foods B. Monitor the patient for peritonitis C. Apply a heating pad to the patient’s abdomen to help alleviate pain D. Encourage intake of full liquids 6. In regards to question 5, this patient signs and symptoms are starting to subside. Which of the following food items would be best for the patient to consume? A. Oatmeal and bran B. Orange juice and eggs C. Chicken broth and Jello GASTROINTESTINAL D. Salad with chicken 7. You’re providing discharge teaching to a patient who was hospitalized with diverticulitis. Which statement by the patient requires you to re-educate the patient? A. “It is important I consume a diet high in fiber and keep hydrated to keep my stool soft.” B. “The physician prescribed me to take Psyllium every day which will help prevent constipation.” C. “I will be sure to always cook and skin my fruits and vegetables rather than eating them fresh.” D. “I will notify my physician if I develop abdominal pain and fever.” 8. True or False: Most patients with chronic diverticulitis require surgery at some point, such as a bowel resection. If the healthy bowel cannot be reconnected right away, a permanent colostomy will be created until it can be reconnected. GASTROINTESTINAL Crohn’s Disease vs Ulcerative Colitis NCLEX Practice Questions 1. True or False: Crohn’s Disease and ulcerative colitis are two forms of IBS (irritable bowel syndrome). 2. Select ALL the options below that are similarities between ulcerative colitis and Crohn’s Disease: A. Each cause inflammation B. Both affect the serosa layer C. Each are found from the mouth to anus D. They both increase colon cancer risk E. The cause of both is unknown D. The cure for both diseases includes total colectomy 3. Which medications are used in the treatment of Crohn’s Disease and ulcerative colitis? SELECT-ALL-THAT-APPLY: A. Guanylate Cyclase-C agonists B. Anticholinergics C. 5-Aminosalicylates D. Antacids E. Corticosteroids F. Immune suppressors GASTROINTESTINAL 4. is most commonly found in the terminal ileum and beginning of the colon. Ulcerative Colitis Crohn’s Disease 5. affects the inner layer of the intestinal lining. Ulcerative Colitis Crohn’s Disease 6. Which bowel disease starts in the rectum and migrates in a continuous fashion throughout the colon? Ulcerative Colitis Crohn’s Disease 7. Which of the following is NOT a potential complication associated with ulcerative colitis? A. Toxic megacolon B. Anemia C. Stricture D. Peritonitis 8. A patient has the following symptoms: urgent and frequent bowel movements of diarrhea that contains blood with pus and mucous, low hemoglobin/hematocrit, potassium level of 2.0. Based on the patient’s signs and symptoms, which disease does this describe? Ulcerative Colitis GASTROINTESTINAL Crohn’s Disease 9. A patient had a colonoscopy which showed a “cobble-stone” appearance of the GI lining. This is found in: Ulcerative Colitis Crohn’s Disease 10. A patient with severe ulcerative colitis had a barium enema. Which finding is associated with this disease? A. Cobble-stone appearance of the colon B. Cullen’s Sign C. Lead-Pipe Sign D. McBurney’s Sign 11. Which type of bowel disease is most likely to cause severe malnourishment? Ulcerative Colitis Crohn’s Disease 12. Select-ALL-the complications associated with Crohn’s Disease: A. Loss of form to the haustra B. Fistulas C. Strictures D. Hemorrhoids GASTROINTESTINAL E. Anal Fissure 13. A patient has the following signs and symptoms: abdominal cramping which is mainly located in the right lower side, ulcers in the mouth, bleeding anal fissure, and diarrhea. Based on the patient’s signs and symptoms, which disease does this describe? Ulcerative Colitis Crohn’s Disease Crohn’s Disease NCLEX Questions 1. True or False: A patient with Crohn’s Disease can experience inflammation in the large intestine that affects mainly the mucosa (inner layer) of the bowel. 2. A patient with Crohn’s Disease is most likely to have the disease is what part of the GI tract? A. Rectum B. Duodenum of the small intestine C. Terminal Ileum D. Descending colon 3. You’re providing teaching to a patient who has been newly diagnosed with Crohn’s Disease. Which statement by the patient’s spouse requires re-education? A. “Crohn’s Disease can be scattered throughout the GI tract in patches with some areas appearing healthy while others are diseased.” B. “There is no cure for Crohn’s Disease.” C. “Strictures are a common complication with Crohn’s Disease.” D. “Crohn’s Disease can cause the haustra of the large intestine to lose its form.” 4. A physician is explaining to a patient that the patient has a type of Crohn’s Disease that is found in both the ileum and colon. As the nurse, you know this type of Crohn’s Disease is called? A. Gastroduodenal Crohn’s Disease B. Granulomatous Colitis C. Ileitis D. Ileocolitis 5. Select ALL of the following that are complications associated with Crohn’s Disease: A. Cobble-stone appearance of GI lining B. Lead-pipe sign C. Toxic megacolon D. Fistula E. Abscess F. Anal Fissure 6. Your patient with Crohn’s Disease is admitted with an opening that has formed between the bowel and bladder. As the nurse, you know this is what type of complication associated with this disease? A. Enterovesical Fistula B. Rectovaginal Stricture C. Enteroenteric Fistula D. Perianal Fissure 7. A patient experiencing a flare-up with Crohn’s Disease is ordered complete bowel rest by the physician. You are administering TPN (total parental nutrition) per physician order. When developing the patient’s nursing plan of care, which nursing diagnosis is MOST important to include in the care plan? A. Risk for allergy response B. Risk for unstable blood glucose level C. Risk for imbalance nutrition: more than body requirements D. Risk for imbalanced nutrition: less than body requirements 8. A patient is receiving treatment for Crohn’s Disease. Which food found on the patient’s food tray should the patient avoid? A. Fresh Salad B. White rice C. Baked chicken D. Cooked skinless apples 9. A physician has prescribed a patient with a severe case of Crohn’s Disease to take a drug that works by suppressing the immune system. This medication achieves this by blocking a protein that plays a role the inflammatory process. Which drug does this describe? A. Azathioprine B. Sulfasalazine C. Infliximab D. Prednisone 10. A patient with Crohn’s Disease is taking corticosteroids. The patient is complaining of extreme thirst, polyuria, and blurred vision. What is your next nursing action? A. Check the patient’s blood glucose B. Give the patient a food containing sugar (ex: orange juice) C. Administer oxygen via nasal cannula D. Assess bowel sounds Ulcerative Colitis NCLEX Questions 1. True or False: Ulcerative colitis is a type of inflammatory bowel disease that causes inflammation and ulcer formation in the inner lining of the small intestine, specifically the terminal ileum. 2. A patient is admitted with ulcerative colitis. In the physician’s notes, it is stated that the patient’s barium enema results showed the patient has colitis that starts in the rectum and extends into the sigmoid and descending colon. As the nurse, you know that this is what type of ulcerative colitis? A. Right-sided colitis B. Proctosigmoiditis C. Ulcerative procotitis D. Left-sided colitis 3. You’re educating a group of outpatients about signs and symptoms of ulcerative colitis. Which of the following are NOT typical signs and symptoms of ulcerative colitis? SELECT-ALL- THAT-APPLY: A. Rectal Bleeding B. Abdominal mass C. Bloody diarrhea D. Fistulae E. Extreme Hungry F. Anemia 4. A patient diagnosed with pancolitis is experiencing extreme abdominal distension, pain 10 on 1-10 scale in the abdomen, temperature of 103.6 ‘F, HR 120, and profuse diarrhea. What complication due you suspect the pain is experiencing? A. Fistulae B. Stricture C. Bowel obstruction D. Toxic megacolon 5. A patient is newly diagnosed with mild ulcerative colitis. What type of anti-inflammatory medication is typically prescribed as first line treatment for this condition? A. 5-Aminosalicylates (Sulfasalazine) B. Immunomodulators (Adalimumab) C. Corticosteroids (Prednisone) D. Immunosupressors (Azathioprine) 6. You’re providing education to a patient with severe ulcerative colitis about Adalimumab. Which statement by the patient is CORRECT? A. “This medication is used as first-line treatment for ulcerative colitis.” B. “My physician will order a TB skin test before I start taking this medication.” C. “This medication works by increasing the tumor necrosis factor protein which helps decrease inflammation.” D. “This medication is a corticosteroid. Therefore, I need to monitor my blood glucose levels regularly.” 7. A patient is receiving treatment for ulcerative colitis by taking Azathioprine. Which physician’s order would the nurse question if received? A. Ambulate the patient twice day B. Low-fiber and high-protein diet C. Administer varicella vaccine intramuscularly D. Administer calcium carbonate by mouth daily 8. A patient with ulcerative colitis is scheduled for ileoanal anastomosis (J-Pouch) surgery. You know that this procedure: A. Removes the colon and rectum which allows a pouch to be created that will attach to the ileum. This will allow stool to pass from the small intestine to the anus. B. Removes the colon and rectum and creates a permanent ileostomy. C. Removes the colon and creates a temporary colostomy. D. Removes the rectum which allows a pouch to be created from the colon. This will allow stool to pass from the colon to the anus. 9. True or False: NSAIDs are used as first-line treatment for pain relief with patients with ulcerative colitis. 10. You’re providing diet teaching to a patient with ulcerative colitis about what types of foods to avoid during a “flare-up”. Which foods below should the patient avoid? SELECT-ALL- THAT-APPLY: A. Ice cream B. White Rice C. Fresh apples and pears D. Popcorn E. Cooked carrots Appendicitis NCLEX Questions 1. True or False: The appendix is found on the left lower side of the abdomen and is connected to the cecum of the large intestine. 2. Select all the following options that are NOT causes of appendicitis: A. Fecalith B. Routine usage of NSAIDs C. Infection due to Helicobacter pylori D. Lymph node enlargement due to viral or bacterial infection E. Diet low in fiber 3. A 23 year old patient is admitted with suspected appendicitis. The patient states he is having pain around the umbilicus that extends into the lower part of his abdomen. In addition, he says that the pain is worst on the right lower quadrant. The patient points to his abdomen at a location which is about a one-third distance between the anterior superior iliac spine and umbilicus. This area is known as what? A. Rovsing’s Point B. Hamman’s Point C. McBurney’s Point D. Murphy’s Point 4. Thinking back to the scenario in question 3, what other signs and symptoms are associated with appendicitis. SELECT-ALL-THAT-APPLY: A. Increased red blood Cells B. Patient has the desire to be positioned in the prone position to relieve pain C. Umbilical pain that extends in the right lower quadrant D. Abdominal rebound tenderness E. Abdominal Flaccidity 5. An 18 year old patient is admitted with appendicitis. Which statement by the patient requires immediate nursing intervention? A. “The pain hurts so much it is making me nauseous.” B. “I have no appetite.” C. “The pain seems to be gone now.” D. “If I position myself on my right side, it makes the pain less intense.” 6. You’re providing education to a group of nursing students about the care of a patient with appendicitis. Which statement by a nursing student requires re-education about your teaching? A. “After an appendectomy the patient may have a nasogastric tube to remove stomach fluids and swallowed air.” B. “Non-pharmacological techniques for a patient with appendicitis include application of heat to the abdomen and the side-lying position.” C. “The nurse should monitor the patient for signs and symptoms of peritonitis which includes increased heart rate, respirations, temperature, abdominal distention, and intense abdominal pain.” D. “It is normal for some patients to have shoulder pain after a laparoscopic appendectomy.” 7. Your patient is 4 days post-opt from an appendectomy. Which assessment finding requires further evaluation? A. The patient reports their last bowel movement was the day before surgery. B. The patient reports incisional pain. C. The patient coughs and deep breathes while splinting the abdominal incision. D. Options A and C 8. A patient is recovering after having an appendectomy. The patient is 48 hours post-opt from surgery and is tolerating full liquids. The physician orders for the patient to try solid foods. What types of foods should the patient incorporate in their diet? A. Foods high in fiber B. Foods low in fiber C. Foods high in carbohydrates D. Foods low in protein 9. A patient is scheduled for appendectomy at noon. While performing your morning assessment, you note that the patient has a fever of 103.8 ‘F and rates abdominal pain 9 on 1-10. In addition, the abdomen is distended and the patient states, “I was feeling better last night but it seems the pain has become worst.” The patient is having tachycardia and tachypnea. Based on the scenario, what do you suspect the patient is experiencing? Colostomy and Ileostomy NCLEX Practice Questions 1. On assessment of a patient with a colostomy, you note the stoma is located on the right lower quadrant. Due to its location, this is known as what type of colostomy? A. Descending Colostomy B. Transverse C. Ileostomy D. Ascending Colostomy 2. Thinking back to the patient in Question 1, what type of stool would you expect the stoma to be excreting? A. Liquid stool B. Lose to partly formed stool C. Similar to normal stool D. Semi-solid stool 3. True or False: An ileostomy is a surgical opening created to bring the large intestine to the surface of the abdomen. 4. Describe, in order, how food travels from the stomach to the rectum: A. It exits the stomach into: the cecum, jejunum to the ileum, then into the duodenum, descending colon, transverse colon, ascending colon, sigmoid colon, and rectum. B. It exits the stomach into: the duodenum, ileum to the jejunum, then into the cecum, ascending colon, sigmoid colon, descending colon, transverse colon, and rectum. C. It exits the stomach into: the ileum, jejunum to the duodenum, then into the cecum, sigmoid colon, transverse colon, descending colon, ascending colon, and rectum. D. It exits stomach into: the duodenum, jejunum to the ileum, then into the cecum, ascending colon, transverse colon, descending colon, sigmoid colon, and rectum. 5. A patient has a double-barrel colostomy of the transverse colon. You note on assessment two stomas, a proximal and distal stoma. What type of stool do you expect to drain from the proximal and distal stomas? A. Proximal: lose to partly formed stool; Distal: mucous B. Proximal: liquid stool; Distal: mucous C. Proximal: mucous; Distal: lose to partly formed stool D. Proximal & Distal: lose to partly formed stool 6. A patient is 8 hours post-opt from a colostomy placement. Which finding requires immediate nursing action? A. The stoma is swollen and large. B. The stoma is black. C. The stoma is not draining any stool. D. The patient states the site is tender. 7. A patient, who had a colostomy placed yesterday, calls on the call light to say their surgical dressing “fell off”. You will re-apply what type of dressing over the stoma? A. Wet to dressing B. No dressing is needed. You will keep it open to air. C. Petroleum gauze dressing D. Telfa gauze 8. You’re providing teaching to a patient with an ileostomy on how to change their pouch drainage system. Which statement is INCORRECT about how to change a pouching system for an ostomy? A. Empty the pouch when it is 1/3 to 1/2 full. B. Change the pouching system every 3-5 days. C. When measuring the stoma for skin barrier placement, be sure the opening of the skin barrier is a 2/3 inch larger than the stoma. D. Keep the skin around the stoma clean and dry at all times. 9. You receive a doctor’s order for a patient to take Aspirin EC by mouth daily. The patient has the following medication history: diabetes type 2, peripheral vascular disease, and a permanent ileostomy. What is your next nursing action? A. Administer the medication as ordered. B. Crush the medication and mix it in applesauce. C. Hold the medication and notify the doctor the patient has an ileostomy. D. Crush the medication and mix it in pudding. 10. You’re providing diet teaching to a patient with an ileostomy. Which foods should the patient consume in very small amounts or completely avoid? A. Peanut butter, bananas, rice B. Corn, popcorn, nut and seeds C. Grape juice, bread, and pasta D. Vinegar, soft drinks, and cured meats 11. A patient, who has a colostomy, asks what type of foods they should avoid to decrease odorous gas. You would tell the patient to avoid: A. Onions, alcoholic beverages, eggs, and cabbage B. Beef, fried foods, lettuce, and rice C. Apple, pears, nuts, and wheat D. Potatoes, peas, carrots, and chicken 12. A patient is 2 days post-opt from an ileostomy placement. Which finding requires immediate nursing action? A. The stoma is excreting liquid stool. B. The patient’s potassium level is 2.0 C. The stoma is bright red and moist. D. The patient reports mucoid drainage from the anus. 13. Which type of colostomy can allow a patient to have bowel continence? A. Descending or Sigmoid Colostomy B. Ascending or Transverse Colostomy C. Transverse or Descending Colostomy D. Ascending or Descending Colostomy 14. True or False: Patients with an ileostomy are at greater risk for dehydration and an electrolyte imbalance. Colostomy and Ileostomy NCLEX Practice Questions 1. On assessment of a patient with a colostomy, you note the stoma is located on the right lower quadrant. Due to its location, this is known as what type of colostomy? A. Descending Colostomy B. Transverse C. Ileostomy D. Ascending Colostomy 2. Thinking back to the patient in Question 1, what type of stool would you expect the stoma to be excreting? A. Liquid stool B. Lose to partly formed stool C. Similar to normal stool D. Semi-solid stool 3. True or False: An ileostomy is a surgical opening created to bring the large intestine to the surface of the abdomen. 4. Describe, in order, how food travels from the stomach to the rectum: A. It exits the stomach into: the cecum, jejunum to the ileum, then into the duodenum, descending colon, transverse colon, ascending colon, sigmoid colon, and rectum. B. It exits the stomach into: the duodenum, ileum to the jejunum, then into the cecum, ascending colon, sigmoid colon, descending colon, transverse colon, and rectum. C. It exits the stomach into: the ileum, jejunum to the duodenum, then into the cecum, sigmoid colon, transverse colon, descending colon, ascending colon, and rectum. D. It exits stomach into: the duodenum, jejunum to the ileum, then into the cecum, ascending colon, transverse colon, descending colon, sigmoid colon, and rectum. 5. A patient has a double-barrel colostomy of the transverse colon. You note on assessment two stomas, a proximal and distal stoma. What type of stool do you expect to drain from the proximal and distal stomas? A. Proximal: lose to partly formed stool; Distal: mucous B. Proximal: liquid stool; Distal: mucous C. Proximal: mucous; Distal: lose to partly formed stool D. Proximal & Distal: lose to partly formed stool 6. A patient is 8 hours post-opt from a colostomy placement. Which finding requires immediate nursing action? A. The stoma is swollen and large. B. The stoma is black. C. The stoma is not draining any stool. D. The patient states the site is tender. 7. A patient, who had a colostomy placed yesterday, calls on the call light to say their surgical dressing “fell off”. You will re-apply what type of dressing over the stoma? A. Wet to dressing B. No dressing is needed. You will keep it open to air. C. Petroleum gauze dressing D. Telfa gauze 8. You’re providing teaching to a patient with an ileostomy on how to change their pouch drainage system. Which statement is INCORRECT about how to change a pouching system for an ostomy? A. Empty the pouch when it is 1/3 to 1/2 full. B. Change the pouching system every 3-5 days. C. When measuring the stoma for skin barrier placement, be sure the opening of the skin barrier is a 2/3 inch larger than the stoma. D. Keep the skin around the stoma clean and dry at all times. 9. You receive a doctor’s order for a patient to take Aspirin EC by mouth daily. The patient has the following medication history: diabetes type 2, peripheral vascular disease, and a permanent ileostomy. What is your next nursing action? A. Administer the medication as ordered. B. Crush the medication and mix it in applesauce. C. Hold the medication and notify the doctor the patient has an ileostomy. D. Crush the medication and mix it in pudding. 10. You’re providing diet teaching to a patient with an ileostomy. Which foods should the patient consume in very small amounts or completely avoid? A. Peanut butter, bananas, rice B. Corn, popcorn, nut and seeds C. Grape juice, bread, and pasta D. Vinegar, soft drinks, and cured meats 11. A patient, who has a colostomy, asks what type of foods they should avoid to decrease odorous gas. You would tell the patient to avoid: A. Onions, alcoholic beverages, eggs, and cabbage B. Beef, fried foods, lettuce, and rice C. Apple, pears, nuts, and wheat D. Potatoes, peas, carrots, and chicken 12. A patient is 2 days post-opt from an ileostomy placement. Which finding requires immediate nursing action? A. The stoma is excreting liquid stool. B. The patient’s potassium level is 2.0 C. The stoma is bright red and moist. D. The patient reports mucoid drainage from the anus. 13. Which type of colostomy can allow a patient to have bowel continence? A. Descending or Sigmoid Colostomy B. Ascending or Transverse Colostomy C. Transverse or Descending Colostomy D. Ascending or Descending Colostomy 14. True or False: Patients with an ileostomy are at greater risk for dehydration and an electrolyte imbalance. [Show More]
Last updated: 1 year ago
Preview 1 out of 74 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Apr 30, 2020
Number of pages
74
Written in
Additional information
This document has been written for:
Uploaded
Apr 30, 2020
Downloads
0
Views
173

.png)
.png)

 (2021 Update) WITH ANSWERS AND RATIONALE.png)