*NURSING > EXAM REVIEW > NUR 2356 / NUR2356 Multidimensional Care I Exam 2 / MDC 1 Exam 2 Final Review | Highly Rated| Comple (All)
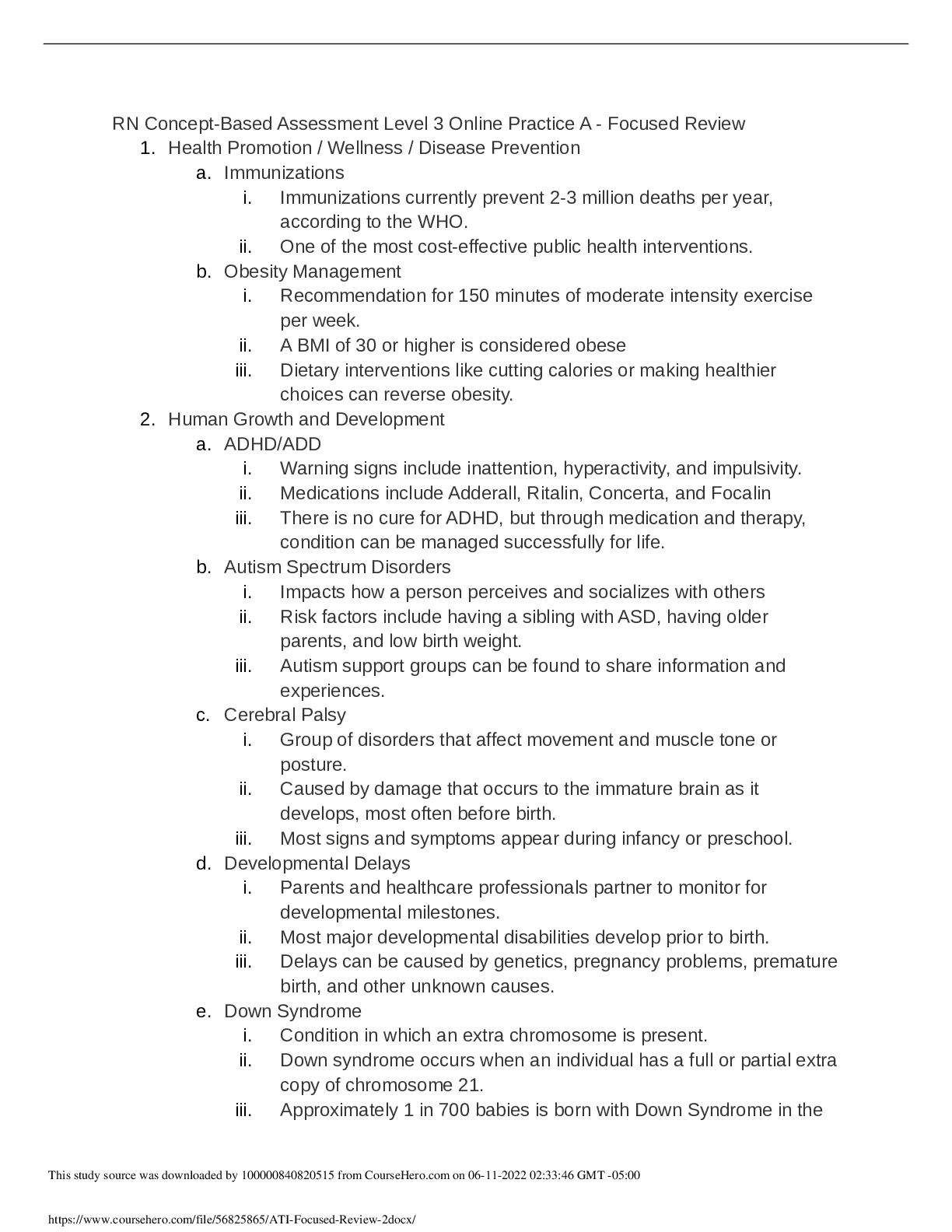
NUR 2356 / NUR2356 Multidimensional Care I Exam 2 / MDC 1 Exam 2 Final Review | Highly Rated| Complete Guide | Latest FALL | Rasmussen College
Document Content and Description Below
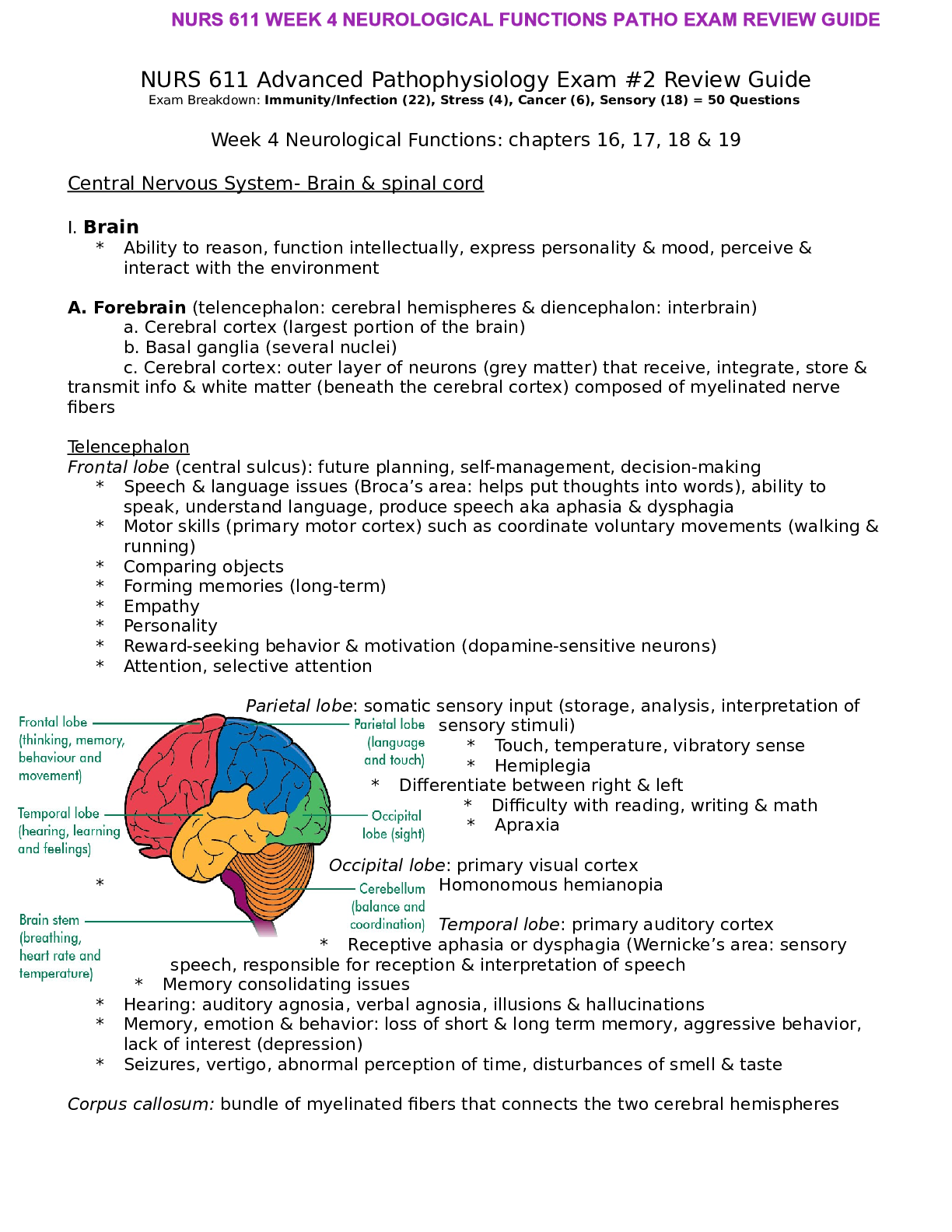
MDC EXAM 2 REVIEW 1. The effects of Immobility a) Interventions that improve flexibility • P.R.E.P.(Perform passive ROM, Reposition Q2HR, Encourage independent activity as much as possible even i... n bedrest, Provide assistive devices) • Know examples of exercises for flexibility b) Assessment/ Findings of a patient with DVT • Assessment (1) Compare distal pulses for pulse quality, observe the color and temp. of extremities, evaluate sensation and motion, and determine speed of capillary refill. Compare calf circumferences. • Findings (1) Redness, warmth, tenderness, swelling (Thrombus formation), Peripheral and sacral edema. c) Identify patients at risk for skin breakdown • Older adults, immobile, cognitive impairments, incontinence, poor nutrition/ malnutrition. Medications may also cause vasoconstriction and result in poor tissue perfusion. 2. Benefits of Exercise a) Rationale for weight bearing exercise • Promotes bone reformation and growth (Makes bones stronger) • At least 3-5 times a week Identify benefits of exercise • Bone reformation and growth • Cardiovascular health promotion • Promotes balance and stability • Reduce stress and increase energy levels b) Identify benefits of exercise • Bone reformation and growth • Cardiovascular health promotion • Promotes balance and stability • Reduce stress and increase energy levels • Improves pulmonary circulation, skeletal development, skin tone • Reduces systemic inflammation c) Identify negative effects of immobility on musculoskeletal system • Osteoarthritis • Rheumatoid Arthritis • Loss of muscle strength • Impaired balance • Altered join mobility • Decreased stability • Osteoporosis • Depression, isolation, anxiety, and mood change • Can cause decreased peristalsis d) Explain ways to maintain proper posture for a client • Place the spine in a neutral position(Resting) • This allows the bones to be aligned, reduce stress and fatigue & muscle joints, and ligament can work efficiently • Avoid standing in 1 position for a long period of time • Do not lock your knees when standing • Keep core tight and don’t bend at the waist or neck • No slumping when sitting • Sit close to your work and use back support • Sit with feet flat on floor • Sleep on firm mattress • Do not wear high heels for a prolonged time, do not slump, and use a chair that supports your back. e) Identify interventions in minimizing contractures (which is a negative effect of immobility) • Gently straighten out contracted extremity, fingers. Etc • Mobility-encouraging interventions such as passive ROM, and rotation. Flexion and extension exercises • These interventions should be performed about every 2hrs and as needed if the contractures are present 3. Identify bed positions • Semi-fowlers: Patient is on their back with the head raised between 15 and 45 degrees. • High-fowlers: Patient is on their back with the head of the bed raised between 60 and 90 degrees. • Prone: Lying on the abdomen with the head turned to one side • Supine: Lying on the back • Sims: Patient lies on their side with the left thigh slightly flexed and the right thigh acutely flexed on the abdomen. • Trendelenburg's Position: Patient is on their back whose lower section is inclined 15-30 degrees so that the head is lower than the body. • Reverse Trendelenburg's Position: Patient is in the supine position with the feet facing downward and head is inclined 15-30 degrees. • Lateral Position: Side lying position, and a pillow is often placed between the legs for patient comfort 4. Identify proper body mechanics for moving the patients in bed • Transfer board • Mechanical lift • Transfer belt • What are the proper ways to move patients in bed? 5. Explain how to use walkers to the elderly • Push or lift your walker 6-12 inches forward • Make sure all 4 tips or wheels of your walker are touching the ground before taking a step • Step forward with your weak leg first • Then step forward with your other leg placing it in front of the weaker leg 6. Be able to assess client with diabetic neuropathy • Monofilament test: touch foot at the same time and have patient which time they were touched • Vibration perception: use a 128 hz tuning fork and ask the patient if they are able to feel vibrations • Look for ulceration or inspection of the feet 7. Assessment of pain and questions to ask • P: What causes the pain or when did it start? What makes it better and what makes it worse? • Q: How does the pain feel? • R: Where is the pain? Does it spread from one area to another? • S: How does the pain rate on a scale of 1-10, with ten being the worst pain? • T: When did the pain start? Is it sudden or gradual? Intermittent or constant 8. Teaching plan for patients with bunionectomy and healing • Allow them to walk with foot shoe or boot • Healing time is 6 to 12 weeks (healing time is slow due to less blood flow) • Use assistive devices for ambulatory until full weight bearing and allowed after surgery which is several weeks postop. • When educating patients and they do not follow recommendations, ask them to tell about their experiences. 9. Osteomy elitis a) Interventions in prevention and risk of osteomyelitis • Proper dental care • Maintaining clean & intact skin • Proper hand hygiene • Not leaving catheters in long tern • Understanding who is at risk • Using proper standard and contact precautions • Reduce caffeine and stop smoking b) Explain why clients would have chronic osteomyelitis • A chronic infection or disease • If it is difficult to treat the underlying cause or inadequate treatment of acute osteomyelitis • Misdiagnosis c) Care for patients with kyphosis • ROM & mobility issues • Turn patient every 2 hours • Passive and active ROM exercises • Prevention of skin breakdown • Consider breathing issues & a plan of care that includes this ( auscultate lungs) d) Teaching plan for care of osteomyelitis • Use of contact precautions to prevent spread of the infection • Hand Hygiene • Complete antibiotic regimen e) Identify various ROM exercises and when they would be utilized • Passive ROM – is movement of the joints through their ROM by another person, moving the leg inward, toward the body’s midline. • Active ROM – are often performed as a rehabilitation procedure; also improves respiratory and cardiac function • Both types improve joint mobility, increase circulation to the area exercised, and help maintain function • Types of Passive ROM for each body part; understand what flexion, extension, etc are (Funds book vol 2 pg 643-647) • What are proper body mechanics for moving a patient in bed 10. Bone Diseases/ Immobility a) Identify goals for a patient with osteoarthritis • Osteoarthritis – progressive deterioration & loss of cartilage & bone in one or more joints (crepitus). • Goals i) Maintain proper nutrition to prevent obesity ii) Take care to avoid injuries, especially those that can occur from professional or amateur sports iii) Take adequate work breaks to rest joints in jobs where repetitive motion is common iv) Stay active & maintain a healthy lifestyle (low impact sports, maintain nutrition) v) Manage chronic pain vi) Increase activity tolerance vii) Participation in ADLs and increase range of motion b) Explain why patients with osteoporosis are prone to fractures • Bone resorption (osteoclastic) is greater than bone building (osteoblastic). This results in decreased bone mineral density (BMD). BMD is what determines bone strength. Due to the loss of strength spongy bone & compact bone can be lost or pourous. This results in fragile bine tissue at more risk for fractures c) Identify assessment of a client with rheumatoid arthritis • Physical assessment i) Early signs and symptoms – Inflammation; low-grade fever, fatigue, weakness, anorexia, paresthesia ii) Late signs – deformities, moderate to severe pain & morning stiffness; osteoporosis, severe fatigue, anemia, weight loss, subcutaneous nodules, peripheral neuropathy, vasculitis, pericarditis, fibrotic lung disease, Sjogren’s syndrome, kidney disease, Felty’s syndrome, chronic pain, redness and swelling of affected joints. Symptoms are bilateral and symmetric • Psychosocial Assessment • Diagnostic i) X-Ray, CT ii) Arthrocentisis • Laboratory Assessment i) Rheumatoid Factor ii) ANA iii) Serum Complement iv) Erythrocyte Sedimentation Rate v) SPEP (1) Albumin (2) Globulin (3) Alpha1 Globulin (4) Alpha2 Globulin (5) Beta Globulin (6) Gamma Globulin (7) HLA Testing • What non-pharmalogical interventions would help for a patient with rheumatoid arthritis? d) Explain complications of patients on prolonged bedrest • Pressure ulcers • Loss of muscle mass • Increased risk of kidney stones • Constipation • Altered ventilation/ perfusion • Weakness & tightness of the diaphragm • Decreased carbohydrate tolerance • Postural hypotension • DVT/ pulmonary embolus • Neurological changes 11. Falls a) Identify priority assessment after a patient has fallen • The nurse should assist the patient in ensuring that they are safe • Do not leave the patient alone • Ensure the patient has not suffered major injuries • Ensure the patient is breathing • Assess neurological status b) Identify interventions to prevent falls • Hand rails in bathrooms • Ramps instead of stairs • Wear rubber sole shoes • Avoid scatter rugs • Prevent clutter • Avoid slippery floors • Offer frequent toileting (Maslow’s hierarchy of needs) 12. CAST care a) Care of a patient with a cast and interventions for poor circulation • Handle with the palms of your hands • Have the patient report painful “hot spots” under the cast which might indicate area of pressure necrosis. • Encourage the patient/family to smell the area for mustiness or unpleasant odor. (if ignored the patient may develop a fever) • Instruct the patient to never put anything down into the cast (like a pencil or hanger) • If the cast or patient is immobilized for a long period of time, the patient may suffer from complications of immobility. b) Care of a patient in traction, purpose, and proper use. • Skin traction (Buck’s): a boot attached to 5-10 pound weight used to relieve muscle spasm pain from a hip or proximal femur fracture • Skeletal traction: screws directly into the bone which allows for heavier weights 15-30 pounds. Client is immobile so will need to be monitored for all the complications associated with immobility • Equipment ropes, pulleys and weights need to be checked every shift • If the patient reports severe pain and realignment and repositioning of the patient does not relieve the discomfort, the weight may be too heavy and the PCP will need to be notified. • Monitor neurovascular checks of affected limb • Monitor pin sites for infection c) Post-op hip fracture surgery care, identity possible complications • Pneumonia • UTI • Loss of muscle mass (fall risk) • Take pedal pulses (prevent necrosis) • Take capillary refill (prevent necrosis) • Bed sore/pressure ulcer d) Explain compartment syndrome- know signs and symptoms- numbness and tingling are not always compartment syndrome • A condition in which increased tissue pressure in a confined anatomic space causes decreased perfusion (peripheral blood flow to the area). The decreased circulation to the area leads to hypoxia and pain in the area. • Alert the primary health care provider promptly if the patient exhibits any signs of decreased circulation to the limb such as coolness, swelling, mottling, or discoloration. • Without improvement in perfusion to the limb, the patient could ultimately require amputation of the limb. e) Identify stages of bone healing • In stage one, within 24 to 72 hours after the injury, a hematoma forms at the site of the fracture because bone is extremely vascular. • Stage two occurs in 3 days to 2 weeks when granulation tissue begins to invade the hematoma. This then prompts the formation of fibrocartilage, providing the foundation for bone healing. • Stage three of bone healing occurs as a result of vascular and cellular proliferation. The fracture site is surrounded by new vascular tissue known as a callus (within 3 to 6 weeks). Callus formation is the beginning of a non- bony union. • As healing continues in stage four, the callus is gradually resorbed and transformed into bone. This stage usually takes 3 to 8 weeks. • During the fifth and final stage of healing, consolidation and remodeling of bone continue to meet mechanical demands. This process may start as early as 4 to 6 weeks after fracture and can continue for up to 1 year, depending on the severity of the injury and the age and health of the patient. 13. Fractures, Traction and Bone Healing a) Identify care for pincare (p.1042) • Pay particular attention to the pin sites for signs of inflammation or infection. In the first 48 to 72 hours, clear fluid drainage or weeping is expected. • Although no standardized method or evidence-based protocol for pin-site care has been established, recommendations have been made based on the evidence available regarding pin-site care. • Because the pins go through the skin and into bone, the risk for infection is high. Monitor the pin sites at least every 8 to 12 hours for drainage, color, odor, and severe redness, which indicate inflammation and possible infection. • Follow agency policy for how to clean the pin-site areas. b) Complications of surgery for fractures (p.1042) • Patients with open-reduction with external fixation are at greater risk for infection related to the pin sites. Proper hand hygiene and strict infection control practices are used to prevent infections or osteomyelitis. Educate patients on antibiotic medication adherence. • When infected, what actions are taken? • Pulmonary embolism c) Identify the difference between compartment syndrome and poor circulation (p.1033) • Acute compartment syndrome (ACS) is a serious, limb-threatening condition in which increased pressure within one or more compartments reduces circulation to the area. The most common sites for this problem in patients with musculoskeletal trauma are the compartments in the lower leg (tibial fractures) and forearm • Related to the muscle, blood vessels and nerves are caught within the fascia leading to the increase in the venous pressure and the resulting edema. • The edema leads to increasing pain which is unrelieved by pain medication. • The edema continues to increase and leads to tissue necrosis and possible tissue infection. • If unrelieved could lead to amputation distal to the compartment syndrome. • May appear 6 – 8 hours following an injury or can take up to 2 days to appear. • Monitor for the 6 P’s (pain, pressure, paralysis, paresthesia, pallor, pulselessness) d) Stages of bone healing (p.1032) • 1st stage: Hematoma Formation i. First 24-72 hours a hematoma forms at the site of the fracture • 2nd stage: Hematoma to Granulation Tissue i. 3 days- 2 weeks when granulation tissue begins to invade the hematoma ii. This prompts the formation of fibrocartilage providing the foundation for bone healing • 3rd stage: Callus Formation i. Occurs as a result of vascular and cellular proliferation ii. Within 3-6 weeks the fracture site is surrounded by new vascular tissue (callus is the beginning of a nonbony union) • 4th stage: Osteoblastic Proliferation i. In 3-8 weeks, the callus is gradually resorbed and transformed into bone (osteoblastic proliferation) • 5th stage: Bone Remodeling à Bone Healing Completed i. Consolidation and remodeling of bone continue to meet mechanical demands ii. This process may start as early as 4-6 weeks after fracture and can continue for up to 1 year iii. Depends on the severity of the injury and the age and health of the patient e) Discharge instructions for cast care (p.1039) • Handle with the palms of your hands • Have patient report painful “hot spots” under the cast which might indicate area of pressure necrosis. • Instruct the patient to never put anything down into the cast i.e. pencil. • Encourage the patient/family to smell the area for mustiness or unpleasant odor. If ignored the patient may develop a fever. • If the cast or patient is immobilized for a log period of time, may suffer from complications of immobility f) Reasons for traction (p.1040) • Traction is the application of a pulling force to a part of the body to provide reduction, alignment, and rest. It is also used as a last resort to decrease muscle spasm (thus relieving pain) and prevent or correct deformity and tissue damage • Skin Traction (Buck’s)- Boot attached to 5 – 10-pound weight used to relieve muscle spasm pain from a hip or proximal femur fracture. • Skeletal Traction i. Screws directly into the bone which allows for heavier weights 15 – 30 pounds. ii. Client is immobile so will need to be monitored for all the complications associated with immobility. iii. The equipment ropes, pulleys and weights need to be checked every shift- where should the weights be placed? iv. If patient reports severe pain and realignment and repositioning of the patient does not relieve the discomfort the weight may be to heavy and the PCP will need to be notified v. Monitor Neurovascular checks of affected limb vi. Monitor pin sites for infection 14. Sensory-Vision a) Care for patients who are blind (p.982) • Teach the patient techniques to perform ADLs and self-care independently • Refer the patient to local services, resources, and support groups for the blind and those with low vision. • Speaking with patient in normal voice and natural tone • Promote safety: • Teach family members who have good vision to make appropriate adaptations in the patient’s home to increase his or her safety and independence • Ask the patient whether describing the space layout would help • Use clock or compass direction for room orientation b) Test to diagnose glaucoma (p. 972) • Ophthalmoscopic exam shows cupping and atrophy of optic disc. Optic disc turns white or gray • Loss of peripheral visual fields with a gradual increase in the loss of the fields test by perimetry • Tonometry: measures intraocular pressure. Intraocular pressure varies throughout the day. Increase IOP (22 and 32 mmHg). Normal IOP is 10 to 21 mmHg. • Gonioscopy: is used when elevation intraocular pressure is diagnosed to determine if the glaucoma is open-angle or closed-angle. It allows the visualization of the angle where the iris meets the cornea. Determine whether the angle is open or closed. • Ultrasonic imagining of the retina and optic nerve: creates a three-dimensional view of the back of the eye. Used for clients with ocular hypertension or at risk for glaucoma from other problems. Used to evaluated the thickness, contour of the optic nerve fiber layers and retina for changes indicating damage from high intraocular pressure. c) Symptoms of cataracts (p.968) • Blurred vision • Decreased color perception • May think that glasses are smudged, prescription changes for eyeglasses • Double vision • Problems with ADL’s • Without surgical intervention blindness follows • Affects reading and driving • Halos, difficulty with night vision d) Special care patients taking Timolol eye drops • Timolol is a beta-blocker eye drop used to treat glaucoma. Timolol lower the pressure in the eye by decreasing the amount of fluid within the eye. This drug induces hypoglycemia and also mask the hypoglycemic symptoms. Therefore, special care may include monitoring patient’s glucose level. Take vital signs. • Other side effects of Timolol are slow heart rate, hives, difficult breathing, swelling of face, lips, tongue, or throat. Therefore, when caring for patient taking Timolol eye drops, assess breathing, swelling of face, lips, tongue, and throat. In addition, asses skin for hives. e) Clients with decreased vision may require additional care at home-what are these considerations? • Assistance with ADLs and self-care • Safety concerns/fall risk: Teach family members who have good vision to make appropriate adaptations in the patient’s home to increase his or her safety and independence f) Difference between Glaucoma and Cataracts. • Glaucoma is increase intraocular pressure in the hollow organ. When the intraocular pressure increase it leads to compression of the retinal blood vessels and photoreceptors and their nerve fibers resulting in hypoxemia and death of the tissue and loss of vision • Cataracts is opacity of the lens of the eye that lies just behind the iris. Most are related to age. Causes for cataract may be due to blunt injury to eye or head, lens water loss, radiation exposure, diabetes, glaucoma & retinal detachment. 15. Sensory-Hearing a) Teaching for clients with Meniere’s Disease • teach patients to move head slowly to prevent worsening of the vertigo, reduce sodium intake, and reduce or stop smoking, continue medications. P. 995 b) Definition of Ringing in the ears(Tinnitus) • Tinnitus, a continuous ringing or noise perception in the ears. P. 995 c) What is considered emergent at the Urgent Care- Which patients should be seen first? • ABC’s (airway, breathing, circulation) • This is related to vision. d) What assessment uses a tuning fork? • “Weber and Rinne” distinguishes between conductive and sensorineural hearing. P. 989 [Show More]
Last updated: 1 year ago
Preview 1 out of 10 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
May 16, 2021
Number of pages
10
Written in
Additional information
This document has been written for:
Uploaded
May 16, 2021
Downloads
0
Views
53

.png)
.png)



.png)