*NURSING > CASE STUDY > NUR 6104: Florence Blackman (66 y/o female) – Chest Pain. Case Study. {100% EXPLAINED} (All)
NUR 6104: Florence Blackman (66 y/o female) – Chest Pain. Case Study. {100% EXPLAINED}
Document Content and Description Below
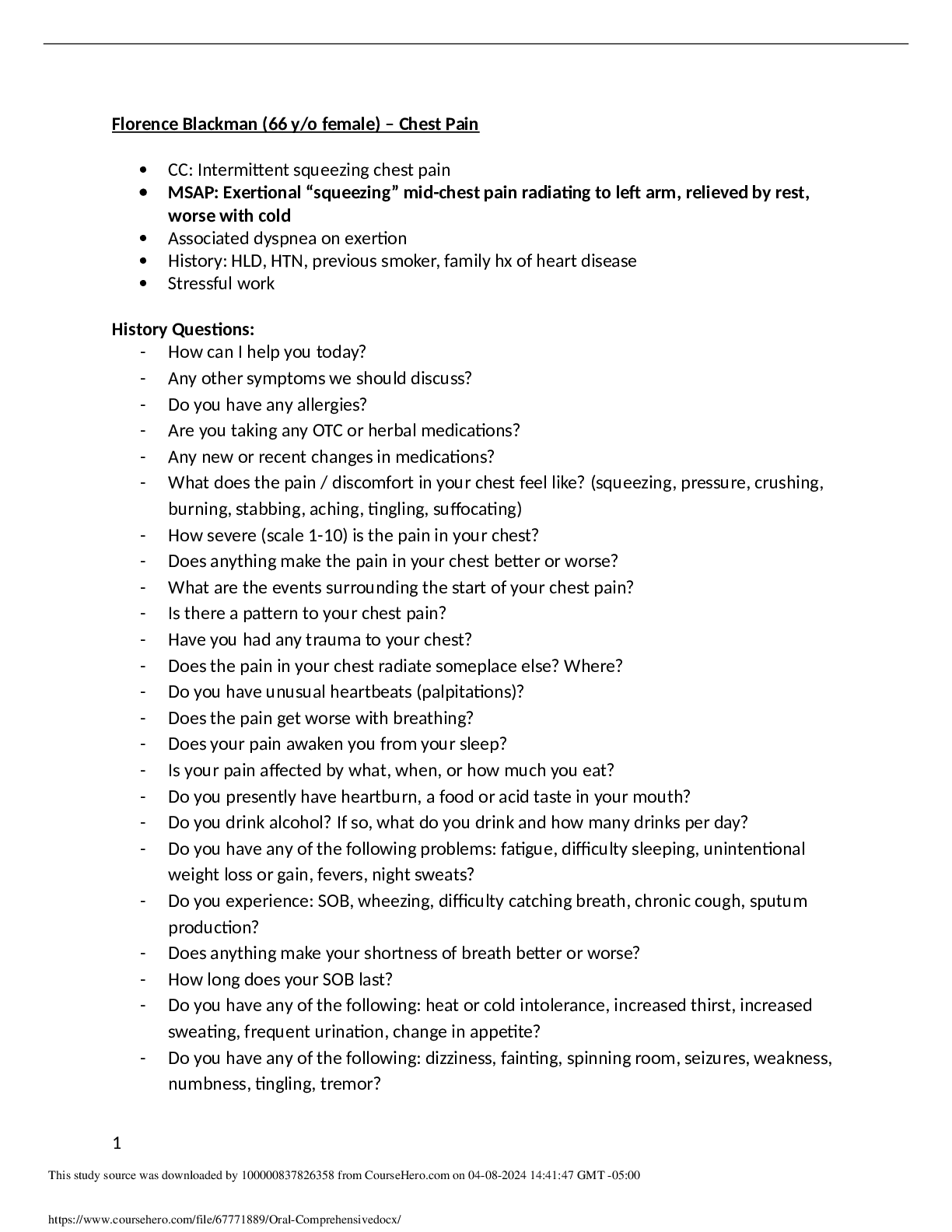
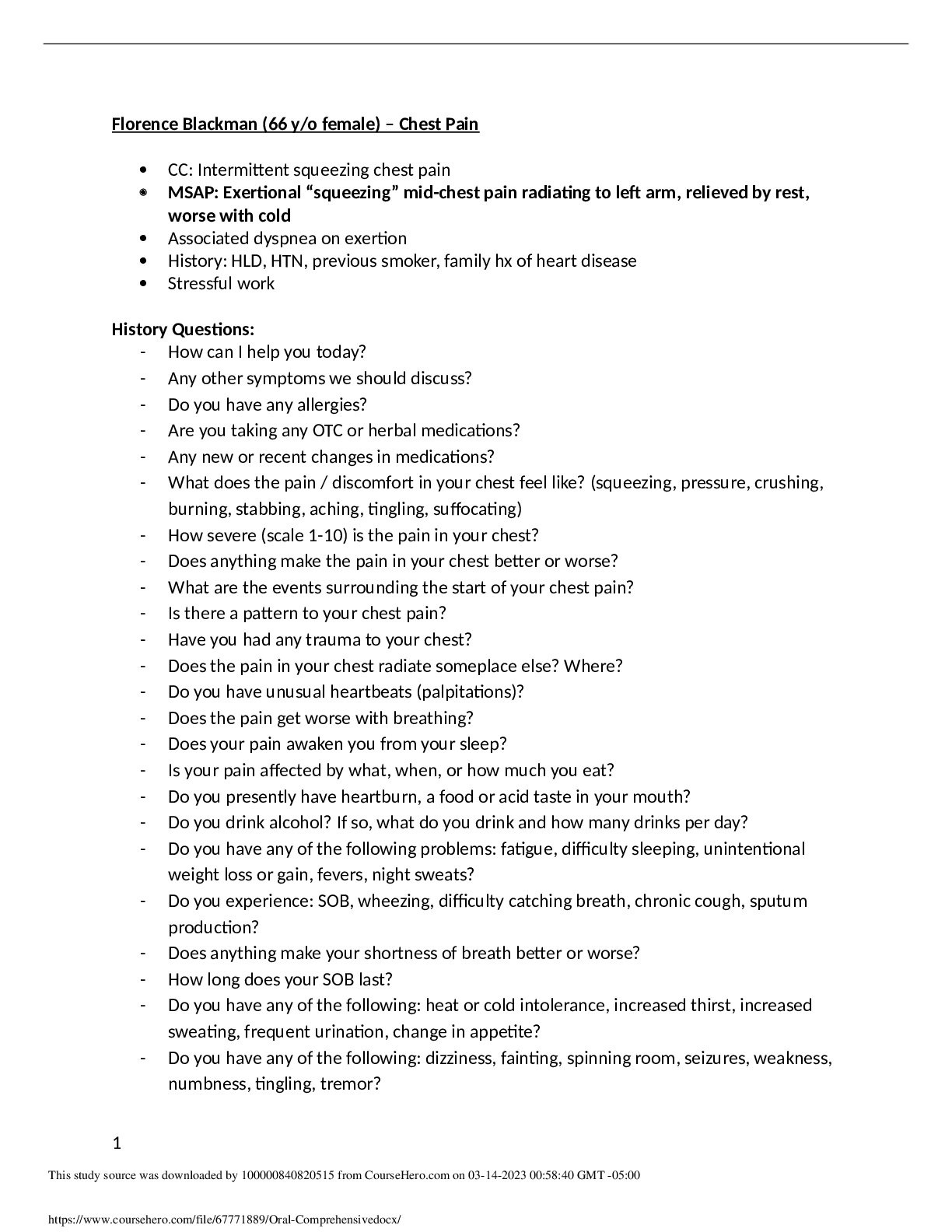
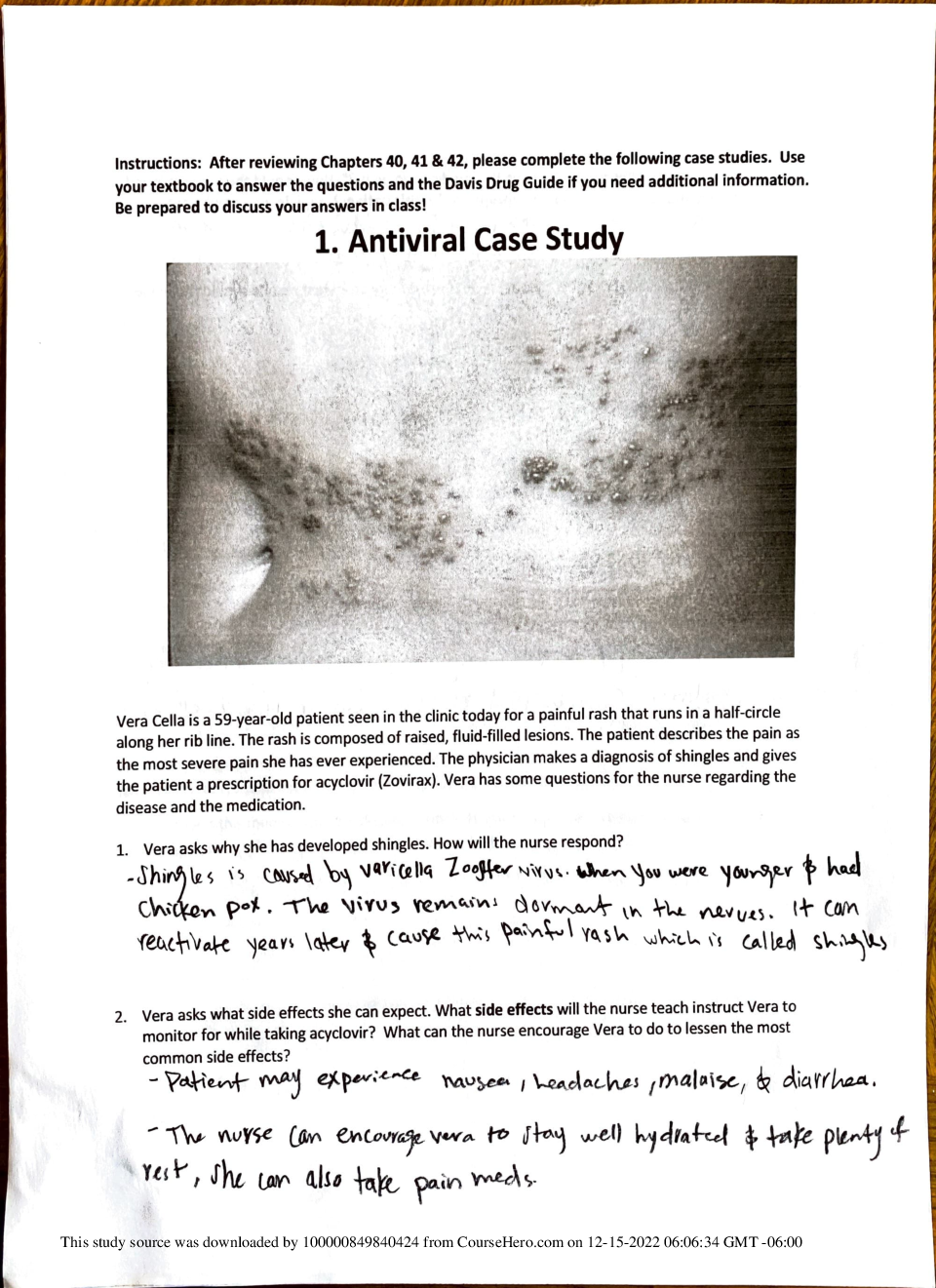
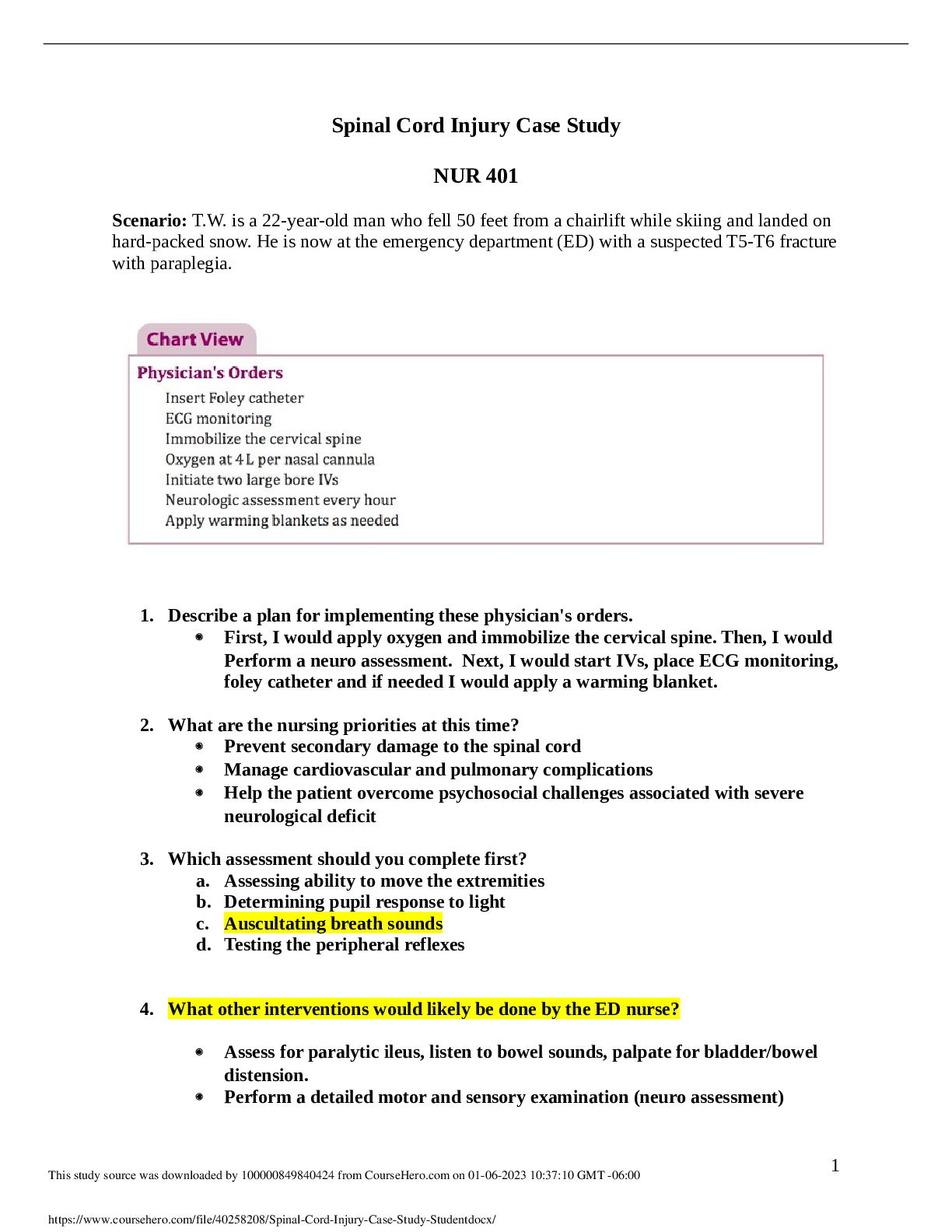
NUR 6104: Florence Blackman (66 y/o female) – Chest Pain. Case Study. Florence Blackman (66 y/o female) – Chest Pain • CC: Intermittent squeezing chest pain • MSAP: Exertional “sque... ezing” mid-chest pain radiating to left arm, relieved by rest, worse with cold • Associated dyspnea on exertion • History: HLD, HTN, previous smoker, family hx of heart disease • Stressful work History Questions: - How can I help you today? - Any other symptoms we should discuss? - Do you have any allergies? - Are you taking any OTC or herbal medications? - Any new or recent changes in medications? - What does the pain / discomfort in your chest feel like? (squeezing, pressure, crushing, burning, stabbing, aching, tingling, suffocating) - How severe (scale 1-10) is the pain in your chest? - Does anything make the pain in your chest better or worse? - What are the events surrounding the start of your chest pain? - Is there a pattern to your chest pain? - Have you had any trauma to your chest? - Does the pain in your chest radiate someplace else? Where? - Do you have unusual heartbeats (palpitations)? - Does the pain get worse with breathing? - Does your pain awaken you from your sleep? - Is your pain affected by what, when, or how much you eat? - Do you presently have heartburn, a food or acid taste in your mouth? - Do you drink alcohol? If so, what do you drink and how many drinks per day? - Do you have any of the following problems: fatigue, difficulty sleeping, unintentional weight loss or gain, fevers, night sweats? - Do you experience: SOB, wheezing, difficulty catching breath, chronic cough, sputum production? - Does anything make your shortness of breath better or worse? - How long does your SOB last? - Do you have any of the following: heat or cold intolerance, increased thirst, increased sweating, frequent urination, change in appetite? - Do you have any of the following: dizziness, fainting, spinning room, seizures, weakness, numbness, tingling, tremor? - Do you have problems with: N/V, constipation, diarrhea, coffee grounds in your vomit, dark tarry stool, bright red blood in your BM, early satiety, bloating? - How is your overall health? - Tell me about your work. - Tell me about daily exercise or sports that you play. Physical Exam: - Vitals: pulse, BP, respirations - Examine skin - Neck: measure JVP (jugular venous pressure) - Neck: auscultate carotid arteries - Chest wall & lungs: o Visual inspection of anterior & posterior chest o Palpate anterior & posterior chest o Auscultate lungs - Heart: o Palpate for PMI (Point of Maximal Impact) o Auscultate heart - Abdomen: o Auscultate abdominal/femoral arteries o Palpate abdomen - Extremities: Visual inspection of extremities Assessment note: - F.B. is a 66 y/o Caucasian female presenting with 2-week h/o new onset, intermittent, stable chest pain which radiates to the L arm, occurs with SOB, is worse with cold temperatures and exertion, and improved by rest. On physical exam she is pain free with stable vital signs. PMH risk factors include: distant history of smoking (5 pack/years), a history of HTN, and high cholesterol, and a family history of coronary vascular disease. - Stress test: 2-mm ST segment depression in inferior leads, 2, 3, and aVF and V3-6 Diagnosis: Coronary artery disease: stable angina Plan: - Determine need for coronary angiography based on stress test results and ECHO. Her Duke score of 10.5 is slightly above moderate risk, and arguments could be made for both a trial at medication intervention since the pt needs improvement on both HTN and HLD o Augment management of preexisting HTN and HLD with a BB (metoprolol 25 mg XR daily); a statin (atorvastatin 40 mg daily); and ASA 81 mg daily - Continue use of HCTZ 25 mg daily - Encourage lifestyle modification: o Decrease intensity of aerobic workouts for next 3 months o D/c alcohol for next 2 months as starts a statin - f/u in 3-4 weeks Ben Kapinsky (18 y/o male) – Fever • CC: Fatigue, SOB, productive cough with yellow/green sputum • MSAP: Hypoxia • Tachypnea, dyspnea • Fever and chills • Fatigue and myalgia • Right-sided chest wall pain aggravated by coughing • Productive cough • Right middle and lower lung crackles • Bilateral cervical lymphadenopathy • Tachycardia • Previous hx of the flu 2 weeks ago, but got better • Childhood asthma per history History Questions: - How can I help you today? - Any other symptoms or concerns we should discuss? - Do you have any allergies? - Are you taking any prescription medications? - Are you taking any OTC or herbal medications? - How high is your fever? - When did your cough start? – 4 days ago - Is there a pattern to your cough? – no - Does anything make your cough better or worse? - Are you coughing up any sputum? – yellowish green stuff - What are the events surrounding the start of your cough? – symptoms started without much warning, thought maybe just got tired going to the party, but got worse over time - What treatments have you had for your cough? – cough syrup, doesn’t help - Do you awaken at night coughing? – yes, can’t sleep - Have you had a cough like this before? – no - Do you have any pain in your chest? – yes, here on the right side when I cough or take a deep breath (points to right thorax, 6-8th intercostal space at midaxillary line) - How severe (1-10 scale) is the pain in your chest? – 7-8 when cough or deep breathe - Have you had any contact with other sick people? – no - Tell me about any current or past medical problems? – none besides mild asthma - Any previous medical, surgical, or dental procedures? – none besides fillings in teeth - Have you ever been hospitalized? – no - Do you have any of the following problems: fatigue, difficulty sleeping, unintentional weight loss or gain, fevers, night sweats? – “some of that stuff for sure” - Do you have any problems with: headaches that don’t go away with ASA or Tylenol, double or blurred vision, difficulty with night vision, problems hearing, ear pain, sinus problems, chronic sore throats, difficulty swallowing? - Do you experience: chest pain discomfort or pressure; pain/pressure/dizziness with exertion or getting angry; palpitations; decreased exercise tolerance; blue/cold fingers or toes? - Do you have problems with: N/V, constipation, diarrhea, coffee grounds in your vomit, dark tarry stool, bright red blood in your BM, early satiety, bloating? - When you urinate, have you noticed: pain, burning, blood, difficulty starting or stopping, dribbling, incontinence, urgency during day or night or any changes in frequency? - Do you have problems with: muscle or joint pain, redness, swelling, muscle cramps, joint stiffness, joint swelling or redness, back pain, neck or shoulder pain, hip pain? - Have you noticed: any bruising, bleeding gums, nose bleeds, or other sites of increased bleeding? - Do you have any of the following: heat or cold intolerance, increased thirst, increased sweating, frequent urination, change in appetite? - Do you have any of the following: dizziness, fainting, spinning room, seizures, weakness, numbness, tingling, tremor? - Do you have any problems with nervousness, depression, lack of interest, sadness, memory loss, or mood changes, or even hear voices or see things that you know are not there? - Do you drink alcohol? If so, what do you drink and how many drinks per day? – occasional beer or wine after studying - Do you use any recreational drugs? – no - Do you now or have you ever smoked or chewed tobacco? – no, athletic - Are you sexually active? – no - Do you have HIV? Physical Exam: - Vitals: Temp, pulse, BP, orthostatic BP, respirations - Skin, hair, nails: inspect skin overall – tenting of dorsal hand skin (dehydration) - HEENT: inspect mouth/pharynx - Neck: palpate neck - Lymphatic: palpate all lymph nodes – tender cervical lymph nodes on neck - Chest wall & lungs: auscultate lungs - Heart: auscultate heart - Abdomen: o Visual inspection o Palpate - Extremities: visual inspection - Genitourinary: male exam - Musculoskeletal: o inspect for muscle bulk and tone o test strength - Neurological: o cranial nerves o reflexes – deep tendon Assessment note: - Ben Kapinsky is a 18 y/o college student who presents with a hx of the flu which resolved and then was followed by a 4-day history of sudden onset fevers, chills, SOB, fatigue, pleuritic chest pain, and a productive cough without wheezing. Physical exam is significant for a fever of 103.2 F (oral), tachypnea (24 breath/min), hypoxia, and R middle and lower lobe coarse crackles, and tender anterior cervical lymphadenopathy. He denies known sick contacts and has a childhood hx of asthma, now off therapy without recent attacks. Diagnosis: Community acquired bacterial pneumonia Plan: - Admit to the student health center inpatient service - Oxygen PRN - IV fluids - IV antibiotics - Respiratory therapy as needed if he develops an asthma exacerbation Ramona Frankel (6 y/o female) – Red Right Eye • CC: came in with mother complaining of red right eye for past 3 days • MSAP: right eye redness • Right eye discharge • Other children at school with similar symptoms • Congestion History Questions: - How can I help you today? – mom - Any other symptoms or concerns we should discuss? – mom - Does she have any allergies? – mom - Is she taking any prescription medications? – mom - Is she taking any OTC or herbal meds? – mom - What treatments has she had for her eye problem? – mom - Are there any other people she has had contact with who have a similar eye problem? – mom - Has she had any trauma to her eyes? – mom - Does she have any pain in her eyes? – mom - Has she noticed any blurred vision? – mom - Does she have a runny nose/nasal congestion? – mom - Does she have a cough? – mom - Tell me about any current or past medical problems? – mom - Any previous medical, surgical, or dental procedures? - mom - Are her immunizations up to date? – mom Physical Exam: - Vitals: temp, pulse, BP, respiration - HEENT: o inspect eyes o test visual acuity o examine pupils o look in ears with otoscope o inspect mouth/pharynx o look up nostrils - Chest wall & lungs: auscultate - Heart: auscultate Assessment note: - Ramona is a 6 year old female with right eye redness and purulent drainage for the last 3 days. She was sent home from school today along with other children who had similar symptoms. She has also had some nasal congestion for the last few days. She has not had any fevers or trauma to the eye. Physical exam is significant for right conjunctival redness and purulent discharge. Mother is requesting a clearance to return to school. Diagnosis: Bacterial conjunctivitis (pink eye) Plan: - 7-10 days of antibiotic eye drops - Instruct patient/parent about handwashing, and educate to not rub eyes to prevent spread of infection - Children can return to school 24 hrs after starting treatment - If symptoms worsen or if child has eye pain or blurry vision, return to clinic or ER [Show More]
Last updated: 1 year ago
Preview 1 out of 8 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
May 16, 2021
Number of pages
8
Written in
Additional information
This document has been written for:
Uploaded
May 16, 2021
Downloads
2
Views
45



 – Chest Pain Complete Latest Solutions.png)