*NURSING > QUESTIONS & ANSWERS > South University, Savannah - NSG 6005Nsg 6005 midterm. 100%. 487 Questions and Answers. (All)
South University, Savannah - NSG 6005Nsg 6005 midterm. 100%. 487 Questions and Answers.
Document Content and Description Below
1. The first-line treatment for cough related to a upper respiratory infection in a five-year-old is: A. Fluids and symptomatic care B. Dextromethorphan and guaifenesin syrup (Robitussin DM for kids... ) C. Guaifenesin and codeine syrup (Tussin AC) D. Chlorpheniramine and dextromethorphan syrup (NyQuil for kids) 2. Pregnant patients with asthma may safely use ____ throughout their pregnancies. A. oral terbutaline B. prednisone C. inhaled corticosteroids (budesonide) D. montelukast (Singulair) 3. A stepwise approach to the pharmacologic management of asthma: A. Begins with determining the severity of the asthma and assessing asthma control B. Is used when the asthma is severe and requires daily steroids C. Allows for each provider to determine his or her personal approach to the care of asthmatic patients D. Provides a framework for the management of severe asthmatics but is not as helpful when patients have intermittent asthma 4. Infants with reflux are initially treated with: A. Histamine 2 receptor antagonist (ranitidine) B. A PPI (omeprazole) C. Antireflux maneuvers (elevate the head of the bed) D. Prokinetic (metoclopramide) 5. Many patients self-medicate with antacids. Which patients should be counseled to not take calcium carbonate antacids without discussing with their providers or a pharmacist first? A. Patients with kidney stones B. Pregnant patients C. Patients with heartburn D. Postmenopausal women 6. Second-generation antihistamines such as loratadine (Claritin) are prescribed for seasonal allergies because they: A. Are more effective than first-generation antihistamines B. Are less sedating than first-generation antihistamines C. Are prescription products and, therefore, are covered by insurance D. Can be taken with CNS sedatives, such as alcohol 7. Decongestants such as pseudoephedrine (Sudafed): A. Are Schedule III drugs in all states B. Should not be prescribed or recommended for children under four years of age C. Are effective in treating the congestion children experience with the common cold D. May cause drowsiness in patients of all ages 8. Patients with pheochromocytoma should avoid which of the following classes of drugs due to the possibility of developing hypertensive crisis? A. Expectorants B. Beta 2 agonists C. Antitussives D. Antihistamines 9. Education of patients with COPD who use inhaled corticosteroids includes the following: A. They should double the dose at the first sign of a upper respiratory infection. B. They should use the inhaled corticosteroid first and then the bronchodilator. C. They should rinse their mouths after use. D. They should not smoke for at least thirty minutes after use. 10. Monitoring a patient with persistent asthma includes: A. Monitoring how frequently the patient has a upper respiratory infection during treatment B. Monthly in-office spirometry testing C. Determining whether the patient has increased use of his or her long-acting beta 2 agonists due to exacerbations D. Evaluating the patient every one to six months to determine whether the patient needs to step up or down in his or her therapy 11. Harold, a forty-two-year-old African American, has moderate persistent asthma. Which of the following asthma medications should he use cautiously, if at all? A. Betamethasone, an inhaled corticosteroid B. Salmeterol, an inhaled long-acting beta-agonist C. Albuterol, a short-acting beta-agonist D. Montelukast, a leukotriene modifier 12. When prescribing montelukast (Singulair) for asthma, patients or parents of patients should be instructed as follows: A. Montelukast twice a day is started when there is an asthma exacerbation. B. Patients may experience weight gain on montelukast. C. Aggression, anxiety, depression, and/or suicidal thoughts may occur when taking montelukast. D. Lethargy and hypersomnia may occur when taking montelukast. 13. Lifestyle changes are the first step in the treatment of GERD. Foods that may aggravate GERD include: A. Eggs B. White bread C. Chocolate D. Chicken 14. Christy has exercise and mild persistent asthma and is prescribed two puffs of albuterol fifteen minutes before exercise and as needed for wheezing. One puff per day of beclomethasone (Qvar) is also prescribed. Teaching regarding her inhalers includes which one of the following? A. She should use one to two puffs of albuterol per day to prevent an attack, with no more than eight puffs per day. B. Beclomethasone needs to be used every day to treat her asthma. C. She should report any systemic side effects she is experiencing, such as weight gain. D. She should use the albuterol MDI immediately after her corticosteroid MDI to facilitate bronchodilation. 15. One goal of asthma therapy outlined by the NHLBI Expert Panel 3 guidelines is: A. Use albuterol daily to control symptoms B. Minimize exacerbations to once a month C. Keep nighttime symptoms at a maximum of twice a week D. Require infrequent use of beta 2 agonists (albuterol) for relief of symptoms 16. Treatment failure in patients with PUD associated with H. pylori may be due to: A. Antimicrobial resistance B. Ineffective antacid C. Overuse of PPIs D. All of the above 17. When using the "step-up" approach in caring for a patient with GERD, the "step up" from OTC antacid use is: A. Prokinetic (metoclopramide) for four to eight weeks B. A PPI (omeprazole) for twelve weeks C. Histamine 2 receptor antagonist (ranitidine) for four to eight weeks D. Cytoprotective drug (misoprostol) for two weeks 18. Long-term use of PPIs may lead to: A. Hip fractures in at-risk persons B. Vitamin B6 deficiency C. Liver cancer D. All of the above 19. Art is a fifty five year old smoker who has been diagnosed with angina and placed on nitrates. He complains of headaches after using his nitrate. An appropriate reply might be: A. "This is a parasympathetic response to the vasodilating effects of the drug." B. "Headaches are common side effects with these drugs. How severe are they?" C. "This is associated with your smoking. Let's work on having you stop smoking." D. "This is not related to your medication. Are you under a lot of stress?" 20. . In teaching about the use of sublingual nitroglycerine, the patient should be instructed: A. To swallow the tablet with a full glass of water B. To place one tablet under the tongue if chest pain occurs and allow it to dissolve C. To take one tablet every five minutes until the chest pain goes away D. That it should "burn" when placed under the tongue or it is no longer effective 21. A potentially life-threatening adverse response to ACE inhibitors is angioedema. Which of the following statements is true about this adverse response? A. Swelling of the tongue and hoarseness are the most common symptoms. B. It appears to be related to a decrease in aldosterone production. C. The presence of a dry, hacky cough indicates a high risk for this adverse response. D. Because it takes time to build up a blood level, it occurs after being on the drug for about one week. 22. Patients who are being treated for folate deficiency require monitoring of: A. Complete blood count every four weeks B. Hematocrit and hemoglobin at one week and then at eight weeks C. Reticulocyte count at one week D. Folate levels every four weeks until the hemoglobin stabilizes 23. Treatments for heart failure, including drug therapy, are based on the stages developed by the American Heart Association and the American College of Cardiology. Stage A patients are: A. Treated with drugs for hypertension and hyperlipidemia, if they exist B. Taught lifestyle management, including diet, exercise, and smoking cessation only C. Treated with ACE inhibitors to directly affect the heart failure only D. Not given any drugs in this early stage 24. Furosemide is added to a treatment regimen for heart failure, which includes digoxin. Monitoring for this combination includes: A. Hemoglobin B. Serum potassium C. Blood urea nitrogen D. Serum glucose 25. Isosorbide dinitrate is a long-acting nitrate given twice daily (BID). The schedule for administration is 7 a.m. and 2 p.m. because: A. Long-acting forms have a higher risk for toxicity. B. Orthostatic hypotension is a common adverse effect. C. It must be taken with milk or food. D. Nitrate tolerance can develop. 26. The New York Heart Association and the Canadian Cardiovascular Society have described grading criteria for levels of angina. Angina that occurs with unusually strenuous activity or on walking or climbing stair after meals is: A. Class I B. Class II C. Class III D. Class IV 27. Kyle has Crohn's disease and has a documented folate deficiency. Drug therapy for folate deficiency anemia is: A. Oral folic acid 1 to 2 mg/day B. Oral folic acid 1 gm/day C. IM folate weekly for at least six months D. Oral folic acid 400 mcg daily 28. The American Heart Association and the American College of Cardiology have devised a classification system for heart failure that can be used to direct treatment. Patients with symptoms and underlying disease are classified as: A. Stage A B. Stage B C. Stage C D. Stage D 29. Disease states in addition to hypertension in which beta blockade is a compelling indication for the use of beta blockers include: A. Heart failure B. Angina C. MI D. Dyslipidemia 30. Which of the following classes of drugs is contraindicated in heart failure? A. Nitrates B. Long-acting dihydropyridines C. Calcium channel blockers D. Alpha-beta blockers 31. Which of the following is true about procainamide and its dosing schedule? A. It produces bradycardia and should be used cautiously in patients with cardiac conditions that a slower heart rate might worsen. B. GI adverse effects are common, so the drug should be taken with food. C. Adherence can be improved by using a sustained-release formulation that can be given once daily. D. Doses of this drug should be taken evenly spaced around the clock to keep an even blood level. 32. At which stage/classification of hypertension should drug therapy be instituted according to the JNC-7 Report? A. Prehypertension B. Stage 1 C. Stage 2 D. Any stage where the blood pressure is greater than 120/80 mm Hg 33. Jose is a twelve-year-old overweight child with a total cholesterol level of 180 mg/dL and LDL of 125 mg/dL. Along with diet education and recommending increased physical activity, a treatment plan for Jose would include ____ with a reevaluation in six months. A. statins B. niacin C. sterols D. bile acid-binding resins 34. Patients who have angina, regardless of class, who are also diabetic should be on: A. Nitrates B. Beta blockers C. ACE inhibitors D. Calcium channel blockers 35. If not chosen as the first drug in hypertension treatment, which drug class should be added as the second step because it will enhance the effects of most other agents? A. ACE inhibitors B. Beta blockers C. Calcium channel blockers D. Diuretics 36. Donald has been diagnosed with hyperlipidemia. On the basis of his lipid profile, atorvastatin is prescribed. Rhabdomyolysis is a rare but serious adverse response to this drug. Donald should be told to: A. Become a vegetarian since this disorder is associated with eating red meat B. Stop taking the drug if abdominal cramps and diarrhea develop C. Report muscle weakness or tenderness and dark urine to his provider immediately D. Expect "hot flash" sensations during the first two weeks of therapy 37. 1.2ND LINE TX FOR GERD: quadruple therapy - 2nd line therapy for those who fail treatment initially is the PPI twice a day plus metronidazole plus tetracycline plus bismuth subsalicylate for 14 days 38. 2.39. How will you choose a diuretic in the treatment of hypertension?: - Check kidney function, thiazide diuretic need to have a GFR higher than the mid 40 mL/min range... so you would want to check a BUN and creatinine in these patients 39. 3.After H. pylori treatment is completed, the next step in peptic ulcer disease therapy is:: 1. Testing for H. pylori eradication with a serum ELISA test 2. Endoscopy by a specialist 3. A proton pump inhibitor for 8 to 12 weeks until healing is complete *All of the above* 40. .Angela is a 5-year-old patient who presents to the clinic with a 48-hour history of nausea, vomiting, and some diarrhea. She is unable to keep fluids down and her weight is 4 pounds less than her last recorded weight. Besides IV fluids, her exam warrants the use of an antinausea medication. Which of the following would be the appropriate drug to order for Angela?: - Ondansetron (Zofran) 41. 5.Antacid's - S/E: constipation and diarrhea 42. 6.Decongestants such as pseudoephedrine (Sudafed):: - Should not be prescribed or recommended for children under 4 years of age 43. .Flovent: - is an inhaled steroid 44. .How are upper respiratory infections treated?: - - Supportive care ...fluids, resting 45. Phenylephrine can be useful for patients with symptomatic relief in adults without - HTN 46. If a patient with H. pylori-positive peptic ulcer disease fails first-line therapy, the second-line treatment is:: - Proton pump inhibitor bid plus metronidazole plus tetracycline plus bismuth subsalicylate for 14 days(P-M-T+BSx14) 47. .If a patient with symptoms of gastroesophageal reflux disease states that he has been self-treating at home with OTC ranitidine daily, the appropriate treatment would be:: - Proton pump inhibitor (omeprazole) for 12 weeks 48. 12.Jaide will be traveling to Mexico with her church group over spring break to build houses. She is concerned she may develop traveler's diarrhea. Advice includes following normal food and water precautions as well as taking:: - Bismuth subsalicylate with each meal and at bedtime 49. 13.Mech of action for muscarinic antagonist: - tiotropium bromide is a muscarinic receptor antagonist often referred to as an antimuscarinic or anticholinergic agent.... acts mainly on the M3 muscarinic receptors located on smooth muscle cells and submucosal glands this leads to a reduction in smooth muscle contraction and mucus secretion and thus produces a bronchodilatory effect 50. 14.Metoclopramide improves gastroesophageal reflux disease symptoms by:: - Increasing lower esophageal tone 51. 15.Michelle is a 72-year-old patient who takes omeprazole for her chronic GERD. Chronic long-term omeprazole use places her at increased risk for:: - Megaloblastic anemia 52. 16.Misoprostol should not be given to: - Pregnant women 53. 17.Patients on digioxin and albuterol should have what checked?: - Potassium level 54. 18.Patients who are on chronic long-term proton pump inhibitor therapy require monitoring for:: - Iron deficiency anemia, vitamin B12 and calcium deficiency 55. 19.Reglan (metoclopramide): - LOWERS esophageal tone- The antiemetic action of metoclopramide is due to its antagonist activity at the D2 receptors and the chemoreceptor trigger zone in the CNS....this action prevents nausea and vomiting triggered by most stimuli...at higher doses the 5HT3 antagonists activity may also contribute to the antiemetic effect- Remember that the D2 receptor is a dopamine receptor and at the higher the dose the 5HT3 which is the serotonin receptor antagonist activity...so it works both on dopamine receptors and serotonin receptors but more so on the dopamine receptors 56. 20.Richard is a 10-year-old patient who presents with uncomfortable constipation. Along with diet changes, a laxative is ordered to provide more rapid relief of constipation. An appropriate choice of medication for a 10-year-old child would be:: - Bisacodyl (Dulcolax) suppository 57. 22.Stan, a 42-year-old African American, has moderate persistent asthma. Which of the following asthma medications should be used cautiously, if at all?: - Salmeterol, an inhaled long-acting beta-agonist 58. 23.Tiotropium bromide (Spiriva) is an inhaled anticholinergic:: - Used for the treatment of chronic obstructive pulmonary disease (COPD) 59. 24.Treatment failure in patients with peptic ulcer disease associated with H. pylori may be because of:: - Antimicrobial resistance 60. 26.What are the disadvantages of using stimulant laxatives for prolonged periods of time?: - - Long term use of stimulant laxatives can lead to dependence 61. 27.What conditions should cause a patient to avoid the use of antihistamines?: - Not recommended for patients over the age of 60 or under the age of - Patient with BPH should avoid what medications - Antihistamines such as diphenhydramine can also slow urine flow in some men with BPH 62. .What do H2 blockers do?: - block the action of histamine on parietal cells specifically the histamine H2 receptors in the stomach ....this decreases the production of aci 63. What do PPI's do?: - - Act by irreversibly blocking the hydrogen potassium, adenosine triphosphates enzyme system or the ATPA or more commonly the gastric proton pump of the gastric parietal cells 64. 30.What ethnic background should not be prescribed long-acting beta agonists?: - African Americans 65. 31.What is the first line therapy for peptic ulcer disease with a positive H. pylori?: - - Triple therapy with a PPI twice a day, amoxicillin 1gm twice daily and clarithromycin 500mg twice daily for 7-14 days 66. 32.What is the mechanism of action of codeine in the suppression of cough?: - It is likely that both central & peripheral effects may play a role.It works as a CNS depressant. Works on the cough center of the brain in themedulla oblongata 67. 33.What is the mechanism of action of docusate sodium?: - - It's a laxative of the stool softener type and works by allowing more water to be absorbed by the feces ...it typically comes in the form a sodium, calcium or potassium salt 68. 34.What is the mechanism of action of ondansetron?: - - Highly specific selective serotonin receptor antagonist, with a low affinity for dopamine receptors - may stimulate vagal afferents via the serotonin receptors to initiate the vomiting reflex 69. 35.What is the mechanism of action of the phenothiazine antiemetics?: - - Prochlorperazine or Promethazine ....both of these agents antagonize dopaminergic D2 receptors in various pathways to the CNS...the D2 or dopamine blockade results in antipsychotic and antiemetic and other effects 70. 36.What is the Step Down Approach with GERD?: - PPI daily for 8 weeks, if the symptoms have not resolved then the dose of the PPI is doubled for another 4-8 weeks ....after 4 weeks a lower dose of PPI is tried ...if no relief after 8 weeks of twice daily PPI then referral to a GI doctor is warranted 71. 37.What is the Step Up Approach with GERD?: - - Begins with lifestyle modifications and OTC antacids followed by H2RA blockers and PPI's - If symptoms are refractory after 4-8 weeks of treatment or if endoscopy shows evidence of erosive disease then PPI's become central management ...first once daily and if symptoms continue then twice daily 72. Asthma exacerbations at home are managed by the patient by: CORRECT Increasing the frequency of beta 2 agonists and contacting his or her provider Doubling inhaled corticosteroid dose Increasing the frequency of beta 2 agonists Starting montelukast (Singulair) 73. Howard is a seventy-two-year-old male who occasionally takes diphenhydramine for his seasonal allergies. Monitoring for this patient taking diphenhydramine would include assessing for: CORRECT Urinary retention Cardiac output Peripheral edema Skin for rash 74. A patient with a COPD exacerbation may require Doubling of inhaled corticosteroid dose CORRECT Systemic corticosteroid burst Continuous inhaled beta 2 agonists Leukotriene therapy ... 75. Decongestants such as pseudoephedrine (Sudafed): Are Schedule III drugs in all states CORRECT Should not be prescribed or recommended for children under four years of age Are effective in treating the congestion children experience with the common cold May cause drowsiness in patients of all ages 76. An acceptable first-line treatment for PUD disease with positive H. pylori test is: Histamine 2 receptor antagonists for four to eight weeks A PPI twice daily (BID) for twelve weeks until healing is complete CORRECT A PPI BID plus clarithromycin plus amoxicillin for fourteen days A PPI BID and levofloxacin for fourteen days 77. In five- to eleven-year-old children, mild-persistent asthma is diagnosed when asthma symptoms occur: At nighttime one to two times a month CORRECT At nighttime three to four times a month Less than twice a week Daily 78. When treating a patient using the "step-down" approach, the patient with GERD is started on ____ first antacids histamine 2 receptor antagonists prokinetics CORRECT PPIs 79. Monitoring a patient with persistent asthma includes: Monitoring how frequently the patient has a upper respiratory infection during treatment Monthly in-office spirometry testing Determining whether the patient has increased use of his or her long-acting beta 2 agonists due to exacerbations CORRECT Evaluating the patient every one to six months to determine whether the patient needs to step up or down in his or her therapy 80. Patients with pheochromocytoma should avoid which of the following classes of drugs due to the possibility of developing hypertensive crisis? Expectorants CORRECT Beta 2 agonists Antitussives Antihistamines 81. Metoclopramide improves GERD symptoms by: Reducing acid secretion Increasing gastric pH CORRECT Increasing lower esophageal tone Decreasing lower esophageal tone 82. Patients who are on chronic long-term PPI therapy require monitoring for: CORRECT Iron deficiency anemia, vitamin B12, and calcium deficiency Folate and magnesium deficiency Elevated uric acid levels leading to gout Hypokalemia and hypocalcemia 83. Digoxin levels need to be monitored closely when the following medication is started: - Albuterol 84. Patients with pheochromocytoma should avoid which of the following classes of drugs because of the possibility of developing hypertensive crisis? - Beta 2-agonists 85. Stan, a 42-year-old African American, has moderate persistent asthma. Which of the following asthma medications should be used cautiously, if at all? - Salmeterol, an inhaled long-acting beta-agonist 86. Long-acting beta-agonists (LTBAs) received a Black Box Warning from the U.S. Food and Drug Administration due to the: - Increased risk of asthma-related deaths when LTBAs are used 87. The bronchodilator of choice for patients taking propranolol is: - Ipratropium 88. Mathew is a 52-year-old overweight smoker taking theophylline for his persistent asthma. He tells his provider he is going to start the Atkin's diet for weight loss. The appropriate response would be: - Recommend smoking cessation 89. Marty takes theophylline for his persistent asthma and calls the office with a complaint of nausea, vomiting, and headache. The best advice for him would be to: - Schedule him for an appointment in 2 to 3 days, which he can cancel if he is better 90. Tiotropium bromide (Spiriva) is an inhaled anticholinergic: - Used for the treatment of chronic obstructive pulmonary disease (COPD) 91. Angela has exercise-induced and mild persistent asthma and is prescribed two puffs of albuterol 15 minutes before exercise and as needed for wheezing. One puff per day of beclomethasone (QVAR) is also prescribed. Teaching regarding her inhalers includes: - Beclomethasone needs to be used every day to treat her asthma 92. When educating patients who are starting on inhaled corticosteroids, the provider should tell them that: - Patients should rinse their mouths out after using the inhaled corticosteroid to prevent thrush. 93. Patients with allergic rhinitis may benefit from a prescription of: - Fluticasone (Flonase) Cetirizine (Zyrtec) OTC cromolyn nasal spray (Nasalcrom) * Any of the above * 94. William is a 72-year-old male who occasionally takes diphenhydramine for his seasonal allergies. Monitoring for this patient taking diphenhydramine would include assessing for: - Urinary retention 95. When recommending dimenhydrinate (Dramamine) to treat motion sickness, patients should be instructed to: - Take the dimenhydrinate 15 minutes before it is needed 96. Cough and cold medications that contain a sympathomimetic decongestant such as phenylephrine should be used cautiously in what population: - Older adults Hypertensive patients Infants * All of the above * 97. George is a 60-year-old patient with hypertension. The first-line decongestant to prescribe would be: - Nasal oxymetazoline 98. Prior to developing a plan for the treatment of asthma, the patient's asthma should be classified according to the NHLBI Expert Panel 3 guidelines. In adults, mild-persistent asthma is classified as asthma symptoms that occur: - More than twice a week and less than once a day 99. In children age 5 to 11 years mild-persistent asthma is diagnosed when asthma symptoms occur: - At nighttime three to four times a month 100. One goal of asthma therapy outlined by the NHLBI Expert Panel 3 guidelines is: - Require infrequent use of beta 2 agonists (albuterol) for relief of symptoms 101. Treatment for mild intermittent asthma is: - Short-acting beta-2-agonists (albuterol) as needed 102. The first-line therapy for mild-persistent asthma is: - Low-dose inhaled corticosteroids 103. Monitoring a patient with persistent asthma includes: - Evaluating the patient every 1 to 6 months to determine if the patient needs to step up or down in their therapy 104. Asthma exacerbations at home are managed by the patient by: - Increasing frequency of beta-2-agonists and contacting their provider 105. Patients who are at risk of a One of the three types of heart failure involves systolic dysfunction. Potential causes of this most common form of heart failure include: A. Myocardial ischemia and injury secondary to myocardial infarction B. Inadequate relaxation and loss of muscle fiber secondary to valvular dysfunction C. Increased demands of the heart beyond its ability to adapt secondary to anemia D. Slower filling rate and elevated systolic pressures secondary to uncontrolled hypertension 106. One goal of asthma management in children is: - Participation in school and sports activities 107. Medications used in the management of patients with chronic obstructive pulmonary disease (COPD) include: - Inhaled beta-2-agonists Inhaled anticholinergics (ipratropium) Inhaled corticosteroids * All of the above * 108. Patients with a COPD exacerbation may require: - May require a systemic corticosteroid burst 109. Patients with COPD require monitoring of: - Beta-2-agonist use 110. Education for patients who use an inhaled beta-agonist and an inhaled corticosteroid includes: - Use the inhaled beta-agonist first, followed by the inhaled corticosteroid. 111. The most common bacterial pathogen in community-acquired pneumonia is - Streptococcus pneumoniae 112. The first-line drug choice for a previously healthy adult patient diagnosed with community-acquired pneumonia would be: - Azithromycin 113. The first-line antibiotic choice for a patient with comorbidities or who is immunosuppressed who has pneumonia and can be treated as an outpatient would be - Levofloxacin 114. If an adult patient with comorbidities cannot reliably take oral antibiotics to treat pneumonia, an appropriate initial treatment option would be: - IV or IM ceftriaxone 115. Jennifer is 34 weeks pregnant and has been diagnosed with pneumonia. She is stable enough to be treated as an outpatient. What would be an appropriate antibiotic to prescribe? - Azithromycin 116. Adults with pneumonia who are responding to antimicrobial therapy should show improvement in their clinical status in: - 48 to 72 hours 117. Along with prescribing antibiotics, adults with pneumonia should be instructed on lifestyle modifications to improve outcomes, including: - Adequate fluid intake 118. Liam is a 4-week-old infant who has been diagnosed with chlamydial pneumonia. An appropriate treatment for his pneumonia would be: - Erythromycin 119. Charlie is a 4-year-old patient who has suspected bacterial pneumonia. He has a temperature of 102°F, oxygen saturation level of 95%, and is taking fluids adequately. What would be appropriate initial treatment for his pneumonia? - Ceftriaxone 120. Bailey is a 14-year-old patient who presents to the clinic with symptoms consistent with mycoplasma pneumonia. What is the treatment for suspected mycoplasma pneumonia in an adolescent? - Azithromycin 121. Drug resistant tuberculosis (TB) is defined as TB that is resistant to: - Rifampin and isoniazid 122. Goals when treating tuberculosis include: - Completion of recommended therapy 123. The principles of drug therapy for the treatment of tuberculosis include: - Drugs need to be taken on a regular basis for a sufficient amount of time to be effective. 124. Lilliana has confirmed tuberculosis and is placed on a 6-month treatment regimen. The 6-month regimen consists of: - Two months of four-drug therapy (INH, rifampin, pyrazinamide, and ethambutol) followed by Four months of INH and rifampin 125. Jordan has extensively resistant tuberculosis (TB). Treatment for extensively resistant TB would include: - Treatment with at least two drugs to which the TB is susceptible 126. Sunny is 24 weeks pregnant and has been diagnosed with tuberculosis (TB). Treatment regimens for a pregnant patient with TB would include: - Pyridoxine 127. Lola is a 5-year-old patient who has been diagnosed with tuberculosis. His treatment would include: - Pyridoxine 128. Frankie is a 9-year-old patient who lives in a household with a family member newly diagnosed with tuberculosis (TB). To prevent Ezekiel from developing TB he should be treated with: - 9 months of INH 129. Cidney is completing a 6-month regimen to treat tuberculosis (TB). Monitoring of a patient on TB therapy includes: - Monthly sputum cultures 130. Compliance with directly observed therapy can be increased by: - Convenient clinic times Incentives such as food, clothing, and transportation costs Offering gifts for compliance *All of the above* 131. Patients taking antacids should be educated regarding these drugs, including letting them know that: - They may cause constipation or diarrhea Many are high in sodium They should separate antacids from other medications by 1 hour *All of the above* 132. Charlotte has diarrhea and is wondering if she can take loperamide (Imodium) for the diarrhea. Loperamide: - Slows gastric motility and reduces fluid and electrolyte loss from diarrhea 133. Bismuth subsalicylate (Pepto Bismol) is a common OTC remedy for gastrointestinal complaints. Bismuth subsalicylate: - May lead to toxicity if taken with aspirin Is contraindicated in children with flu-like illness Has antimicrobial effects against bacterial and viral enteropathogens *All of the above* 134. Joe presents with complaints of "heartburn" that is minimally relieved with Tums (calcium carbonate) and is diagnosed with gastroesophageal reflux disease (GERD). An appropriate first-step therapy would be: - Ranitidine (Zantac) twice a day 135. Patients who are on chronic long-term proton pump inhibitor therapy require monitoring for: - Iron deficiency anemia, vitamin B12 and calcium deficiency 136. Michelle is a 72-year-old patient who takes omeprazole for her chronic GERD. Chronic long-term omeprazole use places her at increased risk for: - Megaloblastic anemia 137. Richard is a 10-year-old patient who presents with uncomfortable constipation. Along with diet changes, a laxative is ordered to provide more rapid relief of constipation. An appropriate choice of medication for a 10-year-old child would be: - Bisacodyl (Dulcolax) suppository 138. Methylnaltrexone is used to treat constipation in: - Opioid-associated constipation 139. An elderly person has been prescribed lactulose for treatment of chronic constipation. Monitoring with long-term treatment would include: - Electrolytes, including potassium and chloride 140. Gastroesophageal reflux disease may be aggravated by the following medication that affects lower esophageal sphincter (LES) tone: - Estrogen 141. Lifestyle changes are the first step in treatment of gastroesophageal reflux disease (GERD). Food or drink that may aggravate GERD include: - Caffeine 142. Metoclopramide improves gastroesophageal reflux disease symptoms by: - Increasing lower esophageal tone 143. Antacids treat gastroesophageal reflux disease by: - Increasing gastric pH 144. When treating patients using the "Step-Down" approach the patient with gastroesophageal reflux disease is started on _______ first. - Proton pump inhibitors 145. If a patient with symptoms of gastroesophageal reflux disease states that he has been self-treating at home with OTC ranitidine daily, the appropriate treatment would be: - Proton pump inhibitor (omeprazole) for 12 weeks 146. If a patient with gastroesophageal reflux disease who is taking a proton pump inhibitor daily is not improving, the plan of care would be: - Proton pump inhibitor (omeprazole) twice a day for 4 to 8 weeks 147. The next step in treatment when a patient has been on proton pump inhibitors twice daily for 12 weeks and not improving is: - Referral for endoscopy 148. Long-term use of proton pump inhibitors may lead to: - Hip fractures in at-risk persons 149. An acceptable first-line treatment for peptic ulcer disease with positive H. pylori test is: - Proton pump inhibitor bid plus clarithromycin plus amoxicillin for 14 days 150. Treatment failure in patients with peptic ulcer disease associated with H. pylori may be because of: - Antimicrobial resistance 151. If a patient with H. pylori-positive peptic ulcer disease fails first-line therapy, the second-line treatment is: - Proton pump inhibitor bid plus metronidazole plus tetracycline plus bismuth subsalicylate for 14 days 152. After H. pylori treatment is completed, the next step in peptic ulcer disease therapy is: - A proton pump inhibitor for 8 to 12 weeks until healing is complete 153. The treatment goals when treating urinary tract infection (UTI) include: - Eradication of infecting organism Relief of symptoms Prevention of recurrence of the UTI *All of the above* 154. Janis is a 16-year-old female with a urinary tract infection. She is healthy, afebrile, with no use of antibiotics in the previous 6 months and no drug allergies. An appropriate first-line antibiotic choice for her would be: - Trimethoprim/sulfamethoxazole 155. Laurel is a 24-year-old female with a urinary tract infection. She is healthy, afebrile, and her only drug allergy is sulfa, which gives her a rash. An appropriate first-line antibiotic choice for her would be: - Ciprofloxacin 156. Karina is a 28-year-old pregnant woman at 38 weeks' gestation who is diagnosed with a lower urinary tract infection (UTI). She is healthy with no drug allergies. Appropriate first-line therapy for her UTI would be: - Amoxicillin 157. Which of the following patients may be treated with a 3-day course of therapy for their urinary tract infection? - Laurel, a 24-year-old female 158. Carmin is a 4-year-old female with a febrile urinary tract infection (UTI). She is generally healthy and has no drug allergies. Appropriate initial therapy for her UTI would be: - Ceftriaxone 159. Monitoring for a healthy, non-pregnant adult patient being treated for a urinary tract infection is: - Symptom resolution in 48 hours 160. Monitoring for a child who has had a urinary tract infection is: - Follow-up urine culture at completion of therapy 161. Monitoring for a pregnant woman who has had a urinary tract infection is: - Follow-up urine culture every 2 weeks until delivery 162. Along with an antibiotic prescription, lifestyle education for a non-pregnant adult female who has had a urinary tract infection includes: - Voiding 10 to 15 minutes after intercourse 163. Cheryl a is a healthy non-pregnant adult woman who recently had a urinary tract infection (UTI). She is asking about drinking cranberry juice to prevent a recurrence of the UTI. The correct answer to give her would be: - 100% cranberry juice or cranberry juice extract may decrease UTIs in some patients. 164. Furosemide is added to a treatment regimen for heart failure that includes digoxin. Monitoring for this combination includes: - Serum potassium 165. What assessments should be made before prescribing any antihypertensive agent? BP, RF, and head to toe assessment. Assess diet, sodium intake, electrolytes, and potassium levels. Prior to prescribing any antihypertensives, creatinine and BUN levels should be evaluated. Confirmation of elevated BP at 3 different times. Children over 3 years old should be assessed at least once at every visit-preferred method for children is by auscultation, the correct measurement requires using a cuff that is appropriate to the child's upper arm. 12 lead EKG. UA, albumin, albumin/creatinine ratio. Diabetics or those with renal disease should have the albumin/creatinine ratio annually. The presence of albuminuria, micro albuminuria even in the setting of normal GFR is associated with increased cardiovascular risk. Blood sugar, hct, serum calcium, and lipid profile. 166. Why are ACE inhibitors the drug of choice in diabetic patients with hypertension? - ACE-Is will improve insulin sensitivity, as well as reduce the effects of DM on the kidneys. Protect the kidneys, watch for renal function, any creatinine >2.5 requires dose reduction. Prevents diabetic nephropathy or slow its progression. Reduce albuminuria and BP. ACEIs and ARBs should be used to treat the HTN. Renal protection, reduces the conversion of AT II and improve the insulin sensitivity. 167. What is the drug of choice to improve symptoms for patients taking propranolol? - Ipratropium 168. What is the most common adverse effect of an ACE inhibitor? - Dry, hacking cough in some patients. Can switch to an angiotensin blocker which won't cause cough. Reduce dose with either of these if Cr >2.5. Most are associated with hypotension, dizziness, HA, fatigue, orthostatic hypotension, tachyphylaxis. 169. What is the action of an ACE inhibitor? - Decreases angiotensin II and aldosterone. Vasodilatation on the venous and arterial sides of the heart. Blocks the RAAS system leads to rennin acts on angiotensinogen to angiotensin I to angiotensin II through ACE. Angiotensin II stimulates aldosterone causing sodium and water while losing potassium via the kidney. ACE is also involved in the inactivation of bradykinin a vasodilator. Bradykin is what causes the cough (irritating the lungs). 170. What is the action of an Angiotensin Receptor Blocker? - Blocks the angiotensin II receptor to leading to increasing vascular tone and stimulating vascular smooth muscle contraction. One of the greatest advantages: doesn't produce the dry, hacking cough that ACE-Is do. Similar to ACE-I except to bradykinin activity (no cough), lowers BP, decreases vascular resistance, decreases pulmonary cap wedge pressure, decreases HR, increases cardiac index. 171. What ethnic background should not be prescribed long-acting beta-agonists? - African Americans, increased incidence of death in this population 172. What is tiotropium used to treat? - COPD, after patient stops smoking, this medication slow the progression of COPD. 173. What is the action of a Calcium Channel Blocker? - Decrease the amount of calcium inside the cell to control blood pressure. Dihydropyridine CCB: inhibits transmembrane influx of extracellular calcium ions across myocardial and vascular smooth muscle cell membranes without changing serum calcium concentrations. This results in inhibition of cardiac and vascular smooth muscle contraction, thereby dilating main coronary and systemic arteries. Vasodilatation with decreased peripheral resistance and increased heart rate. Nondihydropyridine CCB: inhibits extracellular calcium ion influx across membranes of myocardial cells and vascular smooth muscle cells. Resulting in inhibition of cardiac and vascular smooth muscle contraction and thereby dilating main coronary and systemic arteries. No effect on serum calcium contractions. Substantial inhibitory effects on cardiac conduction system, acting principally at AV node, with some effects at sinus node. 174. What are the adverse effects of a dihydropyridine-type calcium channel blocker? - Causes edema of the feet and hands, especially feet. Amlodipine and nifedipine. Type 2 (dihydropyridine=vessel loving) = peripheral edema. Type 1 (non-dihydropyridine=heart loving)=bradycardia, dizziness, hypotension. 175. A 70-year-old patient is admitted with peripheral edema. He is taking a calcium channel blocker and metformin. What is the cause of his peripheral edema? - The edema is not related to metformin. Type 1 CCB more commonly exhibit peripheral edema. Pts report swelling of the hands, feet, ankles, and decreased urine output. 176. What special populations should not be prescribed pseudoephedrine? - Children under the age of 4, first line treatment for coughs and colds is increased fluids and symptomatic management. Schedule III- addictive personalities, HTN, CAD. Children under 4= Infants cause sudden death, not recommended for children under 4. Anytime thinking of cough and cold medications you should always think of the elderly, very young and HTN. 177. How is amlodipine metabolized? - All CCBs are metabolized by the liver in the CYP 3A4. Avoid, don't administer CCB with grapefruit juice, it will increase amlodipine level. Has a half life of 30-50 hours (56hr in hepatic impairment), eliminated via urine. 178. A patient is prescribed amlodipine. She develops reflex tachycardia. What is the reason for the development of bradycardia? - It increases the myocardial oxygen delivery in patients with angina. Sub-peripheral vasodilatation causes such a dramatic drop in BP that baroreceptor reflex is triggered. The baroreceptors are in the aortic arch. The baroreceptor causes sympathetic stimulation of the heart. It increases pulse, it increases contractile force. Peripheral or facial edema can result. Hypotension is a common adverse effect of CCB. A beta blocker can be administered to prevent the reflex tachycardia. When prescribing CCB you always start low and progress slow. Older patients should be started at half the regular dose. Decrease in SA and AV node conduction velocity occurs. 179. What drug should be prescribed for a patient with nasal congestion with hypertension? - Nasal oxymetazoline or nasal azelastine. Cromolyn sodium, ipratropium bromide, or corticosteroids by inhalation can be used safely for nasal congestion by patients with HTN. 180. What patient teaching will you provide when prescribing amiodarone? - Take the drug as prescribed. Take the next day's dose if a dose is missed. Change position slowly d/t hypotension. Avoid taking hot showers or baths, they will cause hypotension. COPD patients. For doses taken more than once daily, evenly space the doses. An abrupt withdrawal may result in life threatening arrhythmia, HTN or myocardial ischemia. Keep enough medication on vacations, holidays, and weekends. If a dose is missed at its usual time, take the next day. 181. What are the drug interactions with digoxin? - Quinidine, amiodarone, verapamil, diltiazam, and propafenone increase serum cardiac glycoside levels and lead to toxicity. Drugs that cause bradycardia will increase the risk of bradycardia. Albuterol and digoxin will decrease digoxin levels. Levels go down especially with increased albuterol use. Phenobarbital, phenytoin, rifampin = decrease effect of digoxin. Thiazide and loop diuretics, mezlocillin, piperacillin, ticarcillin, amphotericin B, glucocorticoids=may cause hypokalemia, increase risk of digoxin toxicity. Calcium preparations = facilitates toxicity by accelerating overloading of intracellular calcium stores. Spironolactone=increases digoxin half life. Beta adrenergic blockers, quinidine, disopyramide + additive bradycardia. Antacids, colestipol, kaolinpectin, cholestyramine=decreases absorption of CG if given concurrently. Thyroid hormones=may decrease therapeutic effects and cause arrhythmias. Reductase inhibitors=increase digoxin levels. Albuterol=decreases digoxin levels. 182. What is the purpose of a thyroid panel with amiodarone what is nitrate tolerance? - Amiodorone can inhibit the thyroid gland, resulting in inflammation of the gland, causing hyperthyroidism. It is also a known cause of hypothyroidism, interferes with thyroid hormone (TH). Can cause hypothyroidism in normal thyroid patients. 183. What are the adverse effects of statins. - Rhabdomyolysis is a severe reaction. #1 weakness and pain (Severe) in the muscles, hepatotoxicity, HA, urine will get dark, CPK checks for muscle breakdown. Monitor liver function and initially and then every 1-3 months. S/s unusual or increased muscle weakness, dark urine. 184. What is nitrate tolerance? - Administration of nitrates too frequently leads to nitrate tolerance. Dosing should be 7am and 2 pm (helps prevent intolerance). This is due attenuation of the vascular effects of nitrates. If the doses are too close together then the patient will develop nitrate tolerance. In regards to adverse effects, assess the severity of the HA (is expected). Patient teaching for sublingual use: if swallowed there will be decrease in effect, under tongue to dissolve. Tachyphylaxis: once start using nitrates and you continue using the medication you are going to get to a level where increasing the dose isn't going to necessarily help. It's a ceiling effect. Only after nitrates have been absent from the body for 10-12 hours does the effectiveness return. 185. What are the adverse effects of antihistamines? - Drowsiness, urinary retention, HTN, dizziness, HA, fatigue, cardio vascular collapse, insomnia, confusion, dry mouth. In the elderly pt 1st generation antihistamines shouldn't be prescribed. The risk of urinary retention is extremely large. 186. What patient education will you provide for a client in which you have prescribed a statin - The patient should report any unexplained or unusual muscle pain or weakness, dark urine (rhabdo). Don't take if you are pregnant or planning to become pregnant. Administer the medication at night (works best at HS, the bodies cholesterol time). Best taken at night. Don't take with grapefruit juice because it is an inhibitor of P450. Call practitioner with weakness or muscle pain because it's a sign of rhabdomyolysis. Limit fats in the diet, exercise and weight control. 187. How will you choose a diuretic in the treatment of hypertension? - Lasix is really hard on K, need to monitor. Start on HTZ. Initial therapy is with thiazide diuretics with an (estimated GFR higher than mid 40) this is key, if less choose an alternative. Furosemide (lasix) and HTZ are not K sparing. CrCl <25, race, amount of dieresis you are going to go with things like thiazide diuretics, sironolactone. Extensive dieresis you will use furosemide. Depends on K. If renal disease usually use angiotensin receptor blockers or ACE-I along with diuretics. Look at the level of kidney function and GFR that is in the mid 40s range. Want to know that kidneys are functioning, as long as looking in direction of renal functions. You have a question you have a 57 year old HTN patient that you want to start furosemide or any diuretic. What is one of the first things you would check or monitor if you want to lean toward renal function. 188. What are the central nervous system adverse effects with montelukast (Singular)? - It's a leukotriene modifier. Leukotrienes are substances that induce numerous effects that contribute to the inflammatory process. They include smooth muscle contractility, neutrophil aggregation, degranulation and chemotaxis which is vascular permeability. Montelukast (Singular) is rapidly absorbed following oral administration. Its peak concentration is reached in 3-4 hours. Adverse effects: agitation, aggression, anxiety, dream abnormalities, hallucinations, depression, irritability, insomnia, restlessness, suicidal thinking, and tremor. Be sure that you are assessing these pts for suicidal ideation. Instruct the patient and families about the adverse effects. Can be prescribed to pts 2 years and older, but it has to be with persistent asthma, not for sudden onset. Zafirlukast & Lukast is indicated in the treatment of pts with chronic asthma 5 years and older. The FDA recommends that patients be informed of the potential for neuropsychiatric events with these medications and discontinue if neuropsychiatric problems arise. Sleep disorders were most frequent. 189. Ray has been diagnosed with hypertension and an ACE inhibitor is determined to be needed. Prior to prescribing this drug, the NP should assess for: A. Hypokalemia B. Impotence C. Decreased renal function D. Inability to concentrate 190. ACE inhibitors are the drug of choice in treating hypertension in diabetic patients because they: A. Improve insulin sensitivity B. Improve renal hemodynamics C. Reduce the production of angiotensin II D. All of the above 191. ACE inhibitors are useful in a variety of disorders. Which of the following statements are true about both its usefulness in the disorder and the reason for its use? A. Stable angina because it decreases the thickening of vascular walls to decreased MOD. B. Heart failure because it reduces remodeling of injured myocardial tissues. C. Both A and B are true and the reasons are correct D. Both A and B are true but the reasons are wrong E. Neither A nor B are true 192. Despite good blood pressure control, a NP might change a patient's drug from an ACEI to an angiotensin II receptor blocker (ARB) because the ARB: A. Is stronger than the ACEI B. Does not produce a dry, hacky cough C. Has no effect on the renal system D. Reduces sodium and water retention 193. While taken an ARB, patients need to avoid certain over-the-counter drugs without first consulting the provider because: A. Cimetidine is metabolized by the CYP 3A4 isoenzymes B. Nonsteroidal anti-inflammatory drugs reduce prostaglandin levels C. Both A and B D. Neither A nor B 194. Laboratory monitoring for patients on ACEIs or ARBs should include: A. White blood cells counts with the drug dose increased for elevations above 10,000 B. Liver function tests with the drug dose stopped for ALT values 2 normal C. Serum creatinine levels with the drug dose reduced for values above 2.5 mg/dL D. Serum glucose levels with the drug dose increased for levels above 120 mg/dL 195. Jacob has hypertension for which a calcium channel blocker has been prescribed. This drug helps control blood pressure because it: A. Decreases the amount of calcium inside the cell B. Reduces stroke volume C. Increases the activity of the Na+/K+/ATPase pump indirectly D. Decreases heart rate 196. Which of the following adverse effects may occur due to a dihydropyridine-type calcium channel blocker? A. Bradycardia B. Hepatic impairment C. Increased contractility D. Edema of the hands and feet 197. Patient teaching related to amlodipine includes: A. Increase calcium intake to prevent osteoporosis from calcium blockade. B. Do not crush the tablet; it must be given in liquid form if the patient has trouble swallowing it. C. Avoid grapefruit juice as it affects the metabolism of this drug. D. Rise slowly from a supine position to reduce orthostatic hypotension. 198. Vera, age 70, has isolated systolic hypertension. Calcium channel blocker doses for her should be: A. Started at about half the usual dose B. Not raised above the usual dose for an adult C. Given once daily due to memory issues in the older adult D. Withheld if she experiences gastroesophageal reflux 199. Larry has heart failure which is being treated with digoxin because it exhibits: A. Negative inotropism B. Positive chronotropism C. Both A and B D. Neither A nor B 200. Furosemide is added to a treatment regimen for heart failure which includes digoxin. Monitoring for this combination includes: A. Hemoglobin B. Serum potassium C. Blood urea nitrogen D. Serum glucose 201. Which of the following create higher risk for digoxin toxicity? Both the cause and the reason for it must be correct. A. Older adults due to reduced renal function B. Administration of aldosterone antagonist diuretics due to decreased potassium levels C. Taking an antacid for GERD because it increases the absorption of digoxin D. Doses between 0.25 and 0.5 mg/day 202. Serum digoxin levels are monitored for potential toxicity. Monitoring should occur: A. Within 6 hours of the last dose B. Because a reference point is needed in adjusting a dose C. After three half-lives from the starting of the drug D. When a patient has stable renal function 203. Rodrigo has been prescribed procainamide after a myocardial infarction. He is monitored for dyspnea, jugular venous distention, and peripheral edema because they may indicate: A. Widening of the area of infarction B. Onset of congestive heart failure C. An electrolyte imbalance involving potassium D. Renal dysfunction 204. Amiodarone has been prescribed in a patient with a supraventricular dysrhythmia. Patient teaching should include all of the following EXCEPT: A. Notify your health-care provider immediately if you have visual change B. Monitor your own blood pressure and pulse daily C. Take a hot shower or bath if you feel dizzy D. Use a sunscreen on exposed body surfaces 205. The NP orders a thyroid panel for a patient on amiodarone. The patient tells the NP that he does not have thyroid disease and wants to know why the test is ordered. Which is a correct response? A. "Amiodarone inhibits an enzyme that is important in making thyroid hormone and can cause hypothyroidism." B. "Amiodarone damages the thyroid gland and can result in inflammation of that gland causing hyperthyroidism." C. "Amiodarone is a broad spectrum drug with many adverse effects. Many different tests need to be done before it is given." D. "Amiodarone can cause corneal deposits in up to 25% of patients." 206. Art is a 55-year-old smoker who has been diagnosed with angina and placed on nitrates. He complains of headaches after using his nitrate. An appropriate reply might be: A. "This is a parasympathetic response to the vasodilating effects of the drug." B. "Headaches are common side effects with these drugs. How severe are they?" C. "This is associated with your smoking. Let's work on having you stop smoking." D. "This is not related to your medication. Are you under a lot of stress?" 207. Which of the following diagnostic studies would NOT indicate a problem related to a reductase inhibitor? A. Elevated serum transaminase B. Increased serum creatinine C. Elevated creatinine kinase D. Increased white blood cells counts 208. Because of the pattern of cholesterol synthesis, reductase inhibitors are given: A. In the evening in a single daily dose B. Twice daily in the morning and the evening C. With each meal and at bedtime D. In the morning before eating 209. Janice has elevated LDL, VLDL, and triglyceride levels. Niaspan, an extended-release form of niacin, is chosen to treat her hyperlipidemia. Due to its metabolism and excretion, which of the following labs should be monitored? A. Serum alanine aminotransferase B. Serum amylase C. Serum creatinine D. Phenylketonuria 210. Niaspan is less likely to cause which side effect that is common to niacin? A. Gastrointestinal irritation B. Cutaneous flushing C. Dehydration D. Headaches 211. Which of the following statements is true? A. Niacin is a B-complex vitamin and taking double the dose of the over-the-counter vitamin will lower LDL and save money. B. Niacin has been shown to reduce all-cause mortality for patients with CAD if taken in prescription strength. C. Niacin should be given on an empty stomach to avoid GI irritation. D. All of the above 212. Dulcea has type 2 diabetes and a high triglyceride level. She has gemfibrozil prescribed to treat her hypertriglyceridemia. A history of which of the following might contraindicate the use of this drug? A. Reactive airway disease/asthma B. Inflammatory bowel disease C. Allergy to aspirin D. Gallbladder disease 213. Many patients with hyperlipidemia are treated with more than one drug. Combining a fibric acid derivative such as gemfibrozil with which of the following is not recommended? The drug and the reason must both be correct for the answer to be correct. A. Reductase inhibitors, due to an increased risk for rhabdomyolysis B. Bile-acid sequestering resins, due to interference with folic acid absorption C. Grapefruit juice, due to interference with metabolism D. Niacin, due to decreased gemfibrozil activity 214. Felicity has been prescribed colestipol to treat her hyperlipidemia. Unlike other anti-lipidemics, this drug: A. Blocks synthesis of cholesterol in the liver B. Exchanges chloride ions for negatively charged acids in the bowel C. Increases HDL levels the most among the classes D. Blocks the lipoprotein lipase pathway 215. Because of their site of action, bile acid sequestering resins: A. Should be administered separated from other drugs by at least 4 hours B. May increase the risk for bleeding C. Both A and B D. Neither A nor B 216. Colestipol comes in a powdered form. The patient is taught to: A. Take the powder dry and follow it with at least 8 ounces of water B. Take it with a meal to enhance its action on fatty food C. Mix the powder with 4 to 6 ounces of milk or fruit juice D. Take after the evening meal to coincide with cholesterol synthesis 217. The choice of diuretic to use in treating hypertension is based on: A. Presence of diabetes with loop diuretics being used for these patients B. Level of kidney function with a thiazide diuretic being used for an estimated glomerular filtration rate higher than the mid-40 mL/min range C. Ethnicity with aldosterone antagonists best for African Americans and older adults D. Presence of hyperlipidemia with higher doses needed for patients with LDL above 130 mg/dL 218. Digoxin levels need to be monitored closely when the following medication is started: A. Loratadine B. Diphenhydramine C. Ipratropium D. Albuterol 219. Patients with pheochromocytoma should avoid which of the following classes of drugs due to the possibility of developing hypertensive crisis? A. Expectorants B. Beta-2-agonists C. Antitussives D. Antihistamines 220. Harold, a 42-year-old African American, has moderate persistent asthma. Which of the following asthma medications should be used cautiously, if at all? A. Betamethasone, an inhaled corticosteroid B. Salmeterol, an inhaled long-acting beta-agonist C. Albuterol, a short-acting beta-agonist D. Montelukast, a leukotriene modifier 221. Long-acting beta-agonists (LTBAs) received a Black Box warning from the U.S. Food and Drug Administration due to the: A. Risk of life-threatening dermatological reactions B. Increased incidence of cardiac events when LTBAs are used C. Increased risk of asthma-related deaths when LTBAs are used D. Risk for life-threatening alterations in electrolytes 222. The bronchodilator of choice for patients taking propranolol is: A. Albuterol B. Pirbuterol C. Formoterol D. Ipratropium 223. James is a 52-year-old overweight smoker taking theophylline for his persistent asthma. He tells his provider he is going to start the Atkin's diet for weight loss. The appropriate response would be: A. Congratulate him on making a positive change in his life B. Recommend he try stopping smoking instead of the Atkin's diet C. Schedule him for regular serum theophylline levels during his diet due to increased excretion of theophylline D. Decrease his theophylline dose because a high-protein diet may lead to elevated theophylline levels 224. Li takes theophylline for his persistent asthma and calls the office with a complaint of nausea, vomiting, and headache. The best advice for him would be to: A. Reassure him this is probably a viral infection and should be better soon B. Have him seen the same day for an assessment and theophylline level C. Schedule him for an appointment in 2 to 3 days, which he can cancel if he is better D. Order a theophylline level at the lab for him 225. Tiotropium bromide (Spiriva) is an inhaled anticholinergic: A. Used for the treatment of COPD B. Used in the treatment of asthma C. Combined with albuterol for treatment of asthma exacerbations D. Combined with fluticasone for the treatment of persistent asthma 226. Montelukast (Singulair) may be prescribed for: A. A 6 year old with exercise-induced asthma B. A 2 year old with moderate persistent asthma C. An 18 month old with seasonal allergic rhinitis D. None of the above; montelukast is not approved for use in children 227. the known drug interactions with the inhaled corticosteroid beclomethasone (QVAR) include: A. Albuterol B. MMR vaccine C. Insulin D. None of the above 228. When educating patients who are starting on inhaled corticosteroids, the provider should include: A. They need to get any live vaccines before starting the medication. B. Inhaled corticosteroids need to be used daily during asthma exacerbations to be effective. C. Patients should rinse their mouths out after using the inhaled corticosteroid to prevent thrush. D. They can triple the dose number of inhalations of medication during colds to prevent needing systemic steroids. 229. Patients with allergic rhinitis may benefit from a prescription of: A. Fluticasone (Flonase) B. Cetirizine (Zyrtec) C. OTC cromolyn nasal spray (Nasalcrom) D. Any of the above 230. Howard is a 72-year-old male who occasionally takes diphenhydramine for his seasonal allergies. Monitoring for this patient taking diphenhydramine would include assessing for: A. Urinary retention B. Cardiac output C. Peripheral edema D. Skin for rash 231. Martin is a 60 year old with hypertension. The first-line decongestant to prescribe would be: A. Oral pseudoephedrine B. Oral phenylephrine C. Nasal oxymetazoline D. Nasal azelastine 232. Angina is produced by an imbalance between oxygen supply (MOS) and demand (MOD) in the myocardium. Which of the following drugs help to correct this imbalance by increasing MOS? A. Calcium channel blockers B. Beta blockers C. ACE inhibitors D. Aspirin 233. Not all chest pain is caused by myocardial ischemia. Non-cardiac causes of chest pain include: A. Pulmonary embolism B. Pneumonia C. Gastroesophageal reflux D. All of the above 234. Patients at high risk for developing significant coronary heart disease are those with: A. LDL values between 100 and 130 B. Systolic blood pressure between 120 and 130 C. Class III angina D. Obesity 235. To reduce mortality, all patients with angina, regardless of Class, should be on: A. Aspirin 81 to 325 mg/d B. Nitroglycerin sublingually for chest pain C. ACE inhibitors or ARBs D. Digoxin 236. Patients who have angina, regardless of Class, who are also diabetic, should be on: A. Nitrates B. Beta blockers C. ACE inhibitors D. Calcium channel blockers 237. Management of all types and grades of angina includes the use of lifestyle modification to reduce risk factors. Which of these modifications are appropriate for which reason? Both the modification and the reason for it must be true for the answer to be correct. A. Lose at least 10 pounds of body weight. Excessive weight increases cardiac workload. B. Reduce sodium intake to no more than 2,400 mg of sodium. Sodium increases blood volume and cardiac workload. C. Increase potassium intake to at least 100 mEq/d. The heart needs higher levels of potassium to improve contractility and oxygen supply. D. Intake a moderate amount of alcohol. Moderate intake has been shown by research to improve cardiac function. 238. The American Heart Association and the American College of Cardiology have devised a classification system for heart failure that can be used to direct treatment. Patients with symptoms and underlying disease are classified as: A. Stage A B. Stage B C. Stage C D. Stage D 239. Diagnosis of heart failure cannot be made by symptoms alone since many disorders share the same symptoms. The most specific and sensitive diagnostic test for heart failure is: A. Chest x-rays that show cephalization and measure heart size B. Two-dimensional echocardiograms that identify structural anomalies and cardiac dysfunction C. Complete blood count, BUN, and serum electrolytes that facilitate staging for end-organ damage D. Measurement of brain natriuretic peptide to distinguish between systolic and diastolic dysfunction 240. treatments for heart failure, including drug therapy, are based on the stages developed by the ACC/AHA. Stage A patients are treated with: A. Drugs for hypertension and hyperlipidemia, if they exist B. Lifestyle management including diet, exercise, and smoking cessation only C. ACE inhibitors to directly affect the heart failure only D. No drugs are used in this early stage 241. Class I recommendations for Stage A heart failure include: A. Aerobic exercise within tolerance levels to prevent the development of heart failure B. Reduction of sodium intake to less than 2,000 mg/day to prevent fluid retention C. Beta blockers for all patients regardless of cardiac history D. Treatment of thyroid disorders, especially if they are associated with tachyarrhythmias 242. Stage B patients should have beta blockers added to their heart failure treatment regimen when: A. They have an ejection fraction less than 40% B. They have had a recent MI C. Both A and B D. Neither A nor B 243. Increased life expectancy for patients with heart failure has been associated with the use of: A. ACE inhibitors, especially when started early in the disease process B. All beta blockers regardless of selectivity C. Thiazide and Loop diuretics D. Cardiac glycosides 244. Stage C patients usually require a combination of three to four drugs to manage their heart failure. In addition to ACE inhibitors and beta blockers, diuretics may be added. Which of the following statements about diuretics is NOT true? A. Diuretics reduce preload associated with fluid retention. B. Diuretics can be used earlier than Stage C when the goal is control of hypertension. C. Diuretics may produce problems with electrolyte imbalances and abnormal glucose and lipid metabolism. D. Diuretics from the potassium-sparing class should be used when using an ARB. 245. Digoxin has a very limited role in treatment of heart failure. It is used mainly for patients with: A. Ejection fractions above 40% B. An audible S3 C. Mitral stenosis as a primary cause for heart failure D. Renal insufficiency 246. Which of the following classes of drugs is contraindicated in heart failure? A. Nitrates B. Long-acting dihydropyridines C. Calcium channel blockers D. Alpha-beta blockers 247. Heart failure is a leading cause of death and hospitalization in older adults (greater than 65 years old). The drug of choice for this population is: A. Aldosterone antagonists B. Eplerenone C. ACE inhibitors D. ARBs 248. Nitrates are especially helpful for patients with angina who also have: A. Heart failure B. Hypertension C. Both A and B D. Neither A nor B 249. Beta blockers are especially helpful for patients with exertional angina who also have: A. Arrhythmias B. Hypothyroidism C. Hyperlipidemia D. Atherosclerosis 250. Rapid-acting nitrates are important for all angina patients. Which of the following are true statements about their use? A. These drugs are useful for immediate symptom relief when the patient is certain it is angina. B. The dose is one sublingual tablet or spray every 5 minutes until the chest pain goes away. C. Take one nitroglycerine tablet or spray at the first sign of angina; repeat every 5 minutes for no more than three doses. If chest pain is still not relieved, go to the hospital. D. All of the above 251. Combinations of a long-acting nitrate and a beta blocker are especially effective in treating angina because: A. Nitrates increase MOS and beta blockers increase MOD B. Their additive affects permit lower doses of both drugs and their adverse reactions cancel each other out. C. They address the pathology of patients with exertional angina who have fixed atherosclerotic coronary heart disease D. All of the above 252. Although they are often described as helpful in the lay media, which of the following therapies have not been shown to be helpful based on clinical evidence? A. Vitamins C and E B. Co-enzyme Q10 C. Folic acid D. All of the above 253. Drug choices to treat angina in older adults differ from those of younger adults only in: A. Consideration of risk factors for diseases associated with and increased in aging B. The placement of drug therapy as a treatment choice before lifestyle changes are tried C. The need for at least three drugs in the treatment regimen because of the complexity of angina in the older adult D. Those with higher risk for silent myocardial infarction (MI) 254. Which of the following drugs has been associated with increased risk for myocardial infarction (MI) in women? A. Aspirin B. Beta blockers C. Estrogen replacement D. Lipid-lowering agents 255. Cost of antianginal drug therapy should be considered in drug selection because of all of the following EXCEPT: A. Patients often require multiple drugs B. A large number of angina patients are older adults on fixed incomes C. Generic formulations may be cheaper but are rarely bioequivalent D. Lack of drug selectivity may result in increased adverse reactions 256. Five questions should be asked during the follow up of any angina patient. They include: A. Have there been any changes in lab data since the last visit? B. Has the level of physical activity associated with the angina changed since the last visit? C. Have new risk factors come to light in producing the angina? D. Is the patient filling prescriptions and taking the drugs as prescribed? 257. Situations that suggest referral to a specialist is appropriate include: A. When chronic stable angina becomes unpredictable in its characteristics and precipitating factors B. When a post-MI patient develops new-onset angina C. When standard therapy is not successful in improving exercise tolerance or reducing the incidence of angina D. All of the above 258. Prior to developing a plan for the treatment of asthma, the patient's asthma should be classified according to the NHLBI Expert Panel 3 guidelines. In adults mild-persistent asthma is classified as asthma symptoms that occur: A. Daily B. Daily and limit physical activity C. Less than twice a week D. More than twice a week and less than once a day 259. ACE inhibitors are contraindicated in pregnancy. While treatment of heart failure during pregnancy is best done by a specialist, which of the following drug classes are considered to be safe, at least in the later parts of pregnancy? A. Diuretics B. ARBs C. Beta blockers D. Nitrates 260. Heart failure is a chronic condition that can be adequately managed in primary care. However, consultation with or referral to a cardiologist is appropriate when: A. Symptoms markedly worsen or the patient becomes hypotensive and has syncope B. There is evidence of progressive renal insufficiency or failure C. The patient remains symptomatic on optimal doses of an ACE inhibitor, a beta blocker, and a diuretic D. Any of the above 261. Nurse practitioner prescriptive authority is regulated by: 1. The National Council of State Boards of Nursing 2. The U.S. Drug Enforcement Administration 3. The State Board of Nursing for each state 4. The State Board of Pharmacy 262. The benefits to the patient of having an Advanced Practice Registered Nurse (APRN) prescriber include: 1. Nurses know more about Pharmacology than other prescribers because they take it both in their basic nursing program and in their APRN program. 2. Nurses care for the patient from a holistic approach and include the patient in decision making regarding their care. 3. APRNs are less likely to prescribe narcotics and other controlled substances. 4. APRNs are able to prescribe independently in all states, whereas a physician's assistant needs to have a physician supervising their practice. 263. Clinical judgment in prescribing includes: 1. Factoring in the cost to the patient of the medication prescribed 2. Always prescribing the newest medication available for the disease process 3. Handing out drug samples to poor patients 4. Prescribing all generic medications to cut costs 264. Criteria for choosing an effective drug for a disorder include: 1. Asking the patient what drug they think would work best for them 2. Consulting nationally recognized guidelines for disease management 3. Prescribing medications that are available as samples before writing a prescription 4. Following U.S. Drug Enforcement Administration guidelines for prescribing 265. Nurse practitioner practice may thrive under health-care reform because of: 1. The demonstrated ability of nurse practitioners to control costs and improve patient outcomes 2. The fact that nurse practitioners will be able to practice independently 3. The fact that nurse practitioners will have full reimbursement under health-care reform 4. The ability to shift accountability for Medicaid to the state level 266. A patient's nutritional intake and laboratory results reflect hypoalbuminemia. This is critical to prescribing because: 1. Distribution of drugs to target tissue may be affected. 2. The solubility of the drug will not match the site of absorption. 3. There will be less free drug available to generate an effect. 4. Drugs bound to albumin are readily excreted by the kidneys. 267. Drugs that have a significant first-pass effect: 1. Must be given by the enteral (oral) route only 2. Bypass the hepatic circulation 3. Are rapidly metabolized by the liver and may have little if any desired action 4. Are converted by the liver to more active and fat-soluble forms 268. The route of excretion of a volatile drug will likely be the: 1. Kidneys 2. Lungs 3. Bile and feces 4. Skin 269. Medroxyprogesterone (Depo Provera) is prescribed intramuscularly (IM) to create a storage reservoir of the drug. Storage reservoirs: 1. Assure that the drug will reach its intended target tissue 2. Are the reason for giving loading doses 3. Increase the length of time a drug is available and active 4. Are most common in collagen tissues 270. The NP chooses to give cephalexin every 8 hours based on knowledge of the drug's: 1. Propensity to go to the target receptor 2. Biological half-life 3. Pharmacodynamics 4. Safety and side effects 271. Azithromycin dosing requires that the first day's dosage be twice those of the other 4 days of the prescription. This is considered a loading dose. A loading dose: 1. Rapidly achieves drug levels in the therapeutic range 2. Requires four- to five-half-lives to attain 3. Is influenced by renal function 4. Is directly related to the drug circulating to the target tissues 272. The point in time on the drug concentration curve that indicates the first sign of a therapeutic effect is the: 1. Minimum adverse effect level 2. Peak of action 3. Onset of action 4. Therapeutic range 273. Phenytoin requires that a trough level be drawn. Peak and trough levels are done: 1. When the drug has a wide therapeutic range 2. When the drug will be administered for a short time only 3. When there is a high correlation between the dose and saturation of receptor sites 4. To determine if a drug is in the therapeutic range 274. A laboratory result indicates that the peak level for a drug is above the minimum toxic concentration. This means that the: 1. Concentration will produce therapeutic effects 2. Concentration will produce an adverse response 3. Time between doses must be shortened 4. Duration of action of the drug is too long 275. Drugs that are receptor agonists may demonstrate what property? 1. Irreversible binding to the drug receptor site 2. Upregulation with chronic use 3. Desensitization or downregulation with continuous use 4. Inverse relationship between drug concentration and drug action 276. Drugs that are receptor antagonists, such as beta blockers, may cause: 1. Downregulation of the drug receptor 2. An exaggerated response if abruptly discontinued 3. Partial blockade of the effects of agonist drugs 4. An exaggerated response to competitive drug agonists 277. Factors that affect gastric drug absorption include: 1. Liver enzyme activity 2. Protein-binding properties of the drug molecule 3. Lipid solubility of the drug 4. Ability to chew and swallow 278. Drugs administered via IV: 1. Need to be lipid soluble in order to be easily absorbed 2. Begin distribution into the body immediately 3. Are easily absorbed if they are nonionized 4. May use pinocytosis to be absorbed 279. When a medication is added to a regimen for a synergistic effect, the combined effect of the drugs is: 1. The sum of the effects of each drug individually 2. Greater than the sum of the effects of each drug individually 3. Less than the effect of each drug individually 4. Not predictable, as it varies with each individual 280. Which of the following statements about bioavailability is true? 1. Bioavailability issues are especially important for drugs with narrow therapeutic ranges or sustained-release mechanisms. 2. All brands of a drug have the same bioavailability. 3. Drugs that are administered more than once a day have greater bioavailability than drugs given once daily. 4. Combining an active drug with an inert substance does not affect bioavailability. 281. Which of the following statements about the major distribution barriers (blood- brain or fetal-placental) is true? 1. Water soluble and ionized drugs cross these barriers rapidly. 2. The blood-brain barrier slows the entry of many drugs into and from brain cells. 3. The fetal-placental barrier protects the fetus from drugs taken by the mother. 4. Lipid-soluble drugs do not pass these barriers and are safe for pregnant women. 282. Drugs are metabolized mainly by the liver via phase I or phase II reactions. The purpose of both of these types of reactions is to: 1. Inactivate prodrugs before they can be activated by target tissues 2. Change the drugs so they can cross plasma membranes 3. Change drug molecules to a form that an excretory organ can excrete 4. Make these drugs more ionized and polar to facilitate excretion 283. Once they have been metabolized by the liver, the metabolites may be: 1. More active than the parent drug 2. Less active than the parent drug 3. Totally "deactivated" so they are excreted without any effect 4. All of the above 284. All drugs continue to act in the body until they are changed or excreted. The ability of the body to excrete drugs via the renal system would be increased by: 1. Reduced circulation and perfusion of the kidney 2. Chronic renal disease 3. Competition for a transport site by another drug 4. Unbinding a nonvolatile drug from plasma proteins 285. Steady state is: 1. The point on the drug concentration curve when absorption exceeds excretion 2. When the amount of drug in the body remains constant 3. When the amount of drug in the body stays below the minimum toxic concentration 4. All of the above 286. Two different pain medications are given together for pain relief. The drug—drug interaction is: 1. Synergistic 2. Antagonistic 3. Potentiative 4. Additive 287. Actions taken to reduce drug—drug interaction problems include all of the following EXCEPT: 1. Reducing the dosage of one of the drugs 2. Scheduling their administration at different times 3. Prescribing a third drug to counteract the adverse reaction of the combination 4. Reducing the dosage of both drugs 288. Phase I oxidative-reductive processes of drug metabolism require certain nutritional elements. Which of the following would reduce or inhibit this process? 1. Protein malnutrition 2. Iron-deficiency anemia 3. Both 1 and 2 4. Neither 1 nor 2 289. The time required for the amount of drug in the body to decrease by 50% is called: 1. Steady state 2. Half-life 3. Phase II metabolism 4. Reduced bioavailability time 290. An agonist activates a receptor and stimulates a response. When given frequently over time, the body may: 1. Upregulate the total number of receptors 2. Block the receptor with a partial agonist 3. Alter the drug's metabolism 4. Downregulate the numbers of that specific receptor 291. Drug antagonism is best defined as an effect of a drug that: 1. Leads to major physiological and psychological dependence 2. Is modified by the concurrent administration of another drug 3. Cannot be metabolized before another dose is administered 4. Leads to a decreased physiological response when combined with another drug 292. Instructions to a client regarding self-administration of oral enteric-coated tablets should include which of the following statements? 1. "Avoid any other oral medicines while taking this drug." 2. "If swallowing this tablet is difficult, dissolve it in 3 ounces of orange juice." 3. "The tablet may be crushed if you have any difficulty taking it." 4. "To achieve best effect, take the tablet with at least 8 ounces of fluid." 293. The major reason for not crushing a sustained-release capsule is that, if crushed, the coated beads of the drugs could possibly result in: 1. Disintegration 2. Toxicity 3. Malabsorption 4. Deterioration 294. Which of the following substances is the most likely to be absorbed in the intestines rather than in the stomach? 1. Sodium bicarbonate 2. Ascorbic acid 3. Salicylic acid 4. Glucose 295. Which of the following variables is a factor in drug absorption? 1. The smaller the surface area for absorption, the more rapidly the drug is absorbed. 2. A rich blood supply to the area of absorption leads to better absorption. 3. The less soluble the drug, the more easily it is absorbed. 4. Ionized drugs are easily absorbed across the cell membrane. 296. An advantage of prescribing a sublingual medication is that the medication is: 1. Absorbed rapidly 2. Excreted rapidly 3. Metabolized minimally 4. Distributed equally 297. Drugs that use CYP 3A4 isoenzymes for metabolism may: 1. Induce the metabolism of another drug 2. Inhibit the metabolism of another drug 3. Both 1 and 2 4. Neither 1 nor 2 298. Therapeutic drug levels are drawn when a drug reaches steady state. Drugs reach steady state: 1. After the second dose 2. After four to five half-lives 3. When the patient feels the full effect of the drug 4. One hour after IV administration 299. Upregulation or hypersensitization may lead to: 1. Increased response to a drug 2. Decreased response to a drug 3. An exaggerated response if the drug is withdrawn 4. Refractoriness or complete lack of response 300. An NP would prescribe the liquid form of ibuprofen for a 6-year-old child because: 1. Drugs given in liquid form are less irritating to the stomach. 2. A 6-year-old child may have problems swallowing a pill. 3. Liquid forms of medication eliminate the concern for first-pass effect. 4. Liquid ibuprofen does not have to be dosed as often as the tablet form. 301. In deciding which of multiple drugs used to use to treat a condition, the NP chooses Drug A because it: 1. Has serious side effects and it is not being used for a life-threatening condition 2. Will be taken twice daily and will be taken at home 3. Is expensive, but covered by health insurance 4. None of these are important in choosing a drug 302. A client asks the NP about the differences in drug effects between men and women. What is known about the differences between the pharmacokinetics of men and women? 1. Body temperature varies between men and women. 2. Muscle mass is greater in women. 3. Percentage of fat differs between genders. 4. Proven subjective factors exist between the genders. 303. The first step in the prescribing process according to the World Health Organization is: 1. Choosing the treatment 2. Educating the patient about the medication 3. Diagnosing the patient's problem 4. Starting the treatment 304. Treatment goals in prescribing should: 1. Always be curative 2. Be patient-centered 3. Be convenient for the provider 4. Focus on the cost of therapy 305. The therapeutic goals when prescribing include(s): 1. Curative 2. Palliative 3. Preventive 4. All of the above 306. When determining drug treatment the NP prescriber should: 1. Always use evidence-based guidelines 2. Individualize the drug choice for the specific patient 3. Rely on his or her experience when prescribing for complex patients 4. Use the newest drug on the market for the condition being treated 307. Patient education regarding prescribed medication includes: 1. Instructions written at the high school reading level 2. Discussion of expected adverse drug reactions 3. How to store leftover medication such as antibiotics 4. Verbal instructions always in English 308. Passive monitoring of drug effectiveness includes: 1. Therapeutic drug levels 2. Adding or subtracting medications from the treatment regimen 3. Ongoing provider visits 4. Instructing the patient to report if the drug is not effective 309. Pharmacokinetic factors that affect prescribing include: 1. Therapeutic index 2. Minimum effective concentration 3. Bioavailability 4. Ease of titration 310. Pharmaceutical promotion may affect prescribing. To address the impact of pharmaceutical promotion, the following recommendations have been made by the Institute of Medicine: 1. Conflicts of interest and financial relationships should be disclosed by those providing education. 2. Providers should ban all pharmaceutical representatives from their office setting. 3. Drug samples should be used for patients who have the insurance to pay for them, to ensure the patient can afford the medication. 4. Providers should only accept low-value gifts, such as pens and pads of paper, from the pharmaceutical representative. 311. Under new U.S. Food and Drug Administration labeling, Pregnancy Categories will be: 1. Strengthened with a new coding such as C+ or C- to discern when a drug is more or less toxic to the fetus 2. Changed to incorporate a pregnancy risk summary and clinical considerations on the drug label 3. Eliminated, and replaced with a link to the National Library of Medicine TOXNET Web site for in-depth information regarding pregnancy concerns 4. Clarified to include information such as safe dosages in each trimester of pregnancy 312. A comprehensive assessment of a patient should be holistic when trying to determine competence in drug administration. Which of the following factors would the NP omit from this type of assessment? 1. Financial status 2. Mobility 3. Social support 4. Sexual practices 313. Rod, age 68, has hearing difficulty. Which of the following would NOT be helpful in assuring that he understands teaching about his drug? 1. Stand facing him and speak slowly and clearly. 2. Speak in low tones or find a provider who has a lower voice. 3. Write down the instructions as well as speaking them. 4. If he reads lips, exaggerate lips movements when pronouncing the vowel sounds. 314. Which of the following factors may adversely affect a patient's adherence to a therapeutic drug regimen? 1. Complexity of the drug regimen 2. Patient perception of the potential adverse effects of the drugs 3. Both 1 and 2 4. Neither 1 nor 2 315. The health-care delivery system itself can create barriers to adherence to a treatment regimen. Which of the following system variables creates such a barrier? 1. Increasing copayments for care 2. Unrestricted formularies for drugs, including brand names 3. Increasing the number of people who have access to care 4. Treating a wider range of disorders 316. Ralph's blood pressure remains elevated despite increased doses of his drug. The NP is concerned that he might not be adhering to his treatment regimen. Which of the following events would suggest that he might not be adherent? 1. Ralph states that he always takes the drug "when I feel my pressure is going up." 2. Ralph contacts his NP to discuss the need to increase the dosage. 3. Ralph consistently keeps his follow-up appointments to check his blood pressure. 4. All of the above show that he is adherent to the drug regimen. 317. Nonadherence is especially common in drugs that treat asymptomatic conditions, such as hypertension. One way to reduce the likelihood of nonadherence to these drugs is to prescribe a drug that: 1. Has a short half-life so that missing one dose has limited effect 2. Requires several dosage titrations so that missed doses can be replaced with lower doses to keep costs down 3.Has a tolerability profile with fewer of the adverse effects that are considered "irritating," such as nausea and dizziness 4. Must be taken no more than twice a day 318. Factors in chronic conditions that contribute to nonadherence include: 1. The complexity of the treatment regimen 2. The length of time over which it must be taken 3. Breaks in the usual daily routine, such as vacations and weekends 4. All of the above 319. While patient education about their drugs is important, information alone does not necessarily lead to adherence to a drug regimen. Patients report greater adherence when: 1. The provider spent a lot of time discussing the drugs with them 2. Their concerns and specific area of knowledge deficit were addressed 3. They were given written material, such as pamphlets, about the drugs 4. The provider used appropriate medical and pharmacological terms 320. Patients with psychiatric illnesses have adherence rates to their drug regimen between 35% and 60%. To improve adherence in this population, prescribe drugs: 1. With a longer half-life so that missed doses produce a longer taper on the drug curve 2. In oral formulations that are more easily taken 3. That do not require frequent monitoring 4. Combined with patient education about the need to adhere even when symptoms are 321. Many disorders require multiple drugs to treat them. The more complex the drug regimen, the less likely the patient will adhere to it. Which of the following interventions will NOT improve adherence? 1. Have the patient purchase a pill container with compartments for daily or multiple times-per-day dosing. 2. Match the clinic appointment to the next time the drug is to be refilled. 3. Write prescriptions for new drugs with shorter times between refills. 4. Give the patient a clear drug schedule that the provider devises to fit the characteristic of the drug. 322. Pharmacologic interventions are costly. Patients for whom the cost/benefit variable is especially important include: 1. Older adults and those on fixed incomes 2. Patients with chronic illnesses 3. Patients with copayments for drugs on their insurance 4. Patients on public assistance 323. Providers have a responsibility for determining the best plan of care, but patients also have responsibilities. Patients the provider can be assured will carry through on these responsibilities include those who: 1. Are well-educated and affluent 2. Have chronic conditions 3. Self-monitor drug effects on their symptoms 4. None of the above guarantee adherence 324. Monitoring adherence can take several forms, including: 1. Patient reports from data in a drug diary 2. Pill counts 3. Laboratory reports and other diagnostic markers 4. All of the above 325. Factors that explain and predict medication adherence include: 1. Social 2. Financial 3. Health system 4. All of the above 326. Cultural factors that must be taken into account when prescribing include(s): 1. Who the decision maker is in the family regarding health-care decisions 2. The patient's view of health and illness 3. Attitudes regarding the use of drugs to treat illness 4. All of the above 327. Ethnic differences have been found in drug: 1. Absorption 2. Hepatic metabolism 3. Filtration at the glomerulus 4. Passive tubular reabsorption 328. The National Standards of Culturally and Linguistically Appropriate Services are required to be implemented in all: 1. Hospitals 2. Clinics that serve the poor 3. Organizations that receive federal funds 4. Clinics that serve ethnic minorities 329. According to the National Standards of Culturally and Linguistically Appropriate Services, an interpreter for health care: 1. May be a bilingual family member 2. May be a bilingual nurse or other health-care provider 3. Must be a professionally trained medical interpreter 4. Must be an employee of the organization 330. According to the U.S. Office of Minority Health, poor health outcomes among African Americans are attributed to: 1. The belief among African Americans that prayer is more powerful than drugs 2. Poor compliance on the part of the African American patient 3. The genetic predisposition for illness found among African Americans 4. Discrimination, cultural barriers, and lack of access to health care 331. The racial difference in drug pharmacokinetics seen in American Indian or Alaskan Natives are: 1. Increased CYP 2D6 activity, leading to rapid metabolism of some drugs 2. Largely unknown due to lack of studies of this population 3. Rapid metabolism of alcohol, leading to increased tolerance 4. Decreased elimination of opioids, leading to increased risk for addiction 332. Pharmacokinetics among Asians are universal to all the Asian ethnic groups. 1. True . False 333. Alterations in drug metabolism among Asians may lead to: 1. Slower metabolism of antidepressants, requiring lower doses 2. Faster metabolism of neuroleptics, requiring higher doses 3. Altered metabolism of omeprazole, requiring higher doses 4. Slower metabolism of alcohol, requiring higher doses 334. Asians from Eastern Asia are known to be fast acetylators. Fast acetylators: 1. Require acetylization in order to metabolize drugs 2. Are unable to tolerate higher doses of some drugs that require acetylization 3. May have a toxic reaction to drugs that require acetylization 4. Require higher doses of drugs metabolized by acetylization to achieve efficacy 335. Hispanic native healers (curanderas): 1. Are not heavily utilized by Hispanics who immigrate to the United States 2. Use herbs and teas in their treatment of illness 3. Provide unsafe advice to Hispanics and should not be trusted 4. Need to be licensed in their home country in order to practice in the United States 336. Michael asks you about why some drugs are over-the-counter and some are prescription. You explain that in order for a drug to be approved for over-the-counter use the drug must: 1. Be safe and labeled for appropriate use 2. Have a low potential for abuse or misuse 3. Be taken for a condition the patient can reliably self-diagnose 4. All of the above 337. In the United States, over-the-counter drugs are regulated by: 1. No one. There is no oversight for over-the-counter medications. 2. The U.S. Food and Drug Administration Center for Drug Evaluation and Research 3. The U.S. Drug Enforcement Administration 4. MedWatch 338. As drugs near the end of their patent, pharmaceutical companies may apply for the drug to change to over-the-counter status in order to: 1. Get a new patent for the over-the-counter form of the drug 2. Lower the costs because most prescription benefit plans do not cover generics 3. Market the drug to a whole new population, as they are able to market to patients instead of just providers 4. Continue to make large profits from their blockbuster brand-name drug 339. New over-the-counter drug ingredients must undergo the U.S. Food and Drug Administration New Drug Application process, just as prescription drugs do. 1. True 2. False 340. The ailment that generates the greatest over-the-counter annual drug sales is: 1. Constipation 2. Cough and colds 3. Heartburn 4. Acute and chronic pain 341. Common over-the-counter pain relievers such as acetaminophen or ibuprofen: 1. Are always safer for the patient than prescription pain medication 2. Are harmful if taken in higher than recommended amounts 3. Have minimal interaction with prescription medications 4. Should never be given to children unless recommended by their provider 342. When obtaining a drug history from Harold, he gives you a complete list of his prescription medications. He denies taking any other drugs, but you find that he occasionally takes aspirin for his arthritis flare ups. This is an example of: 1. His appropriately only telling you about his regularly prescribed medications 2. His hiding information regarding his inappropriate use of aspirin from you 3. A common misconception that intermittently taken over-the counter medications are not an important part of his drug history 4. A common misuse of over-the-counter aspirin 343. The Combat Methamphetamine Epidemic Act, which is part of the 2006 U.S. Patriot Act: 1. Requires all providers to screen their patients for methamphetamine use 2. Restricts the prescribing of amphetamines to U.S. citizens 3. Requires a prescription be written for all methamphetamine precursors in all states 4. Restricts the sales of drugs that contain methamphetamine precursors, including a daily and 30-day limit on sales 344. When prescribing a tetracycline or quinolone antibiotic it is critical to instruct the patient: 1. Not to take their regularly prescribed medications while on these antibiotics 2. Regarding the need for lots of acidic foods and juices, such as orange juice, to enhance absorption 3. Not to take antacids while on these medications, as the antacid decreases absorption 4. That there are no drug interactions with these antibiotics 345. Factors that place a patient at risk of developing an antimicrobial-resistant organism include: 1. Age over 50 years 2. School attendance 3. Travel within the U.S. 4. Inappropriate use of antimicrobials 346. 4. Inappropriate use of antimicrobials 347. Infants and young children are at higher risk of developing antibiotic-resistant infections due to: 1. Developmental differences in pharmacokinetics of the antibiotics in children 2. The fact that children this age are more likely to be in daycare and exposed to pathogens from other children 3. Parents of young children insisting on preventive antibiotics so they don't miss work when their child is sick 4. Immunosuppression from the multiple vaccines they receive in the first 2 years of life 348. Providers should use an antibiogram when prescribing. An antibiogram is: 1. The other name for the Centers for Disease Control guidelines for prescribing antibiotics 2. An algorithm used for prescribing antibiotics for certain infections 3. The reference also known as the Pink Book, published by the Centers for Disease Control 4. A chart of the local resistance patterns to antibiotics developed by laboratories 349. There is often cross-sensitivity and cross-resistance between penicillins and cephalosporins because: 1. Renal excretion is similar in both classes of drugs. 2. When these drug classes are metabolized in the liver they both produce resistant enzymes. 3. Both drug classes contain a beta-lactam ring that is vulnerable to beta-lactamase-producing organisms. 4. There is not an issue with cross-resistance between the penicillins and cephalosporins. 350. Jonathan has been diagnosed with strep throat and needs a prescription for an antibiotic. He says the last time he had penicillin he developed a red, blotchy rash. An appropriate antibiotic to prescribe would be: 1. Penicillin VK, because his rash does not sound like a serious rash 2. Amoxicillin 3. Cefadroxil (Duricef) 4. Azithromycin 351. Sarah is a 25-year-old female who is 8 weeks pregnant and has a urinary tract infection. What would be the appropriate antibiotic to prescribe for her? 1. Ciprofloxacin (Cipro) 2. Amoxicillin (Trimox) 3. Doxycycline 4. Trimethoprim-sulfamethoxazole (Septra) 352. Pong-tai is a 12-month-old child who is being treated with amoxicillin for acute otitis media. His parents call the clinic and say he has developed diarrhea. The appropriate action would be to: 1. Advise the parents that some diarrhea is normal with amoxicillin and recommend probiotics daily. 2. Change the antibiotic to one that is less of a gastrointestinal irritant. 3. Order stool cultures for suspected viral pathogens not treated by the amoxicillin. 4. Recommend increased fluids and fiber in his diet. 353. Lauren is a 13-year-old child who comes to clinic with a 4-day history of cough, low-grade fever, and rhinorrhea. When she blows her nose or coughs the mucous is greenish-yellow. The appropriate antibiotic to prescribe would be: 1. Amoxicillin 2. Amoxicillin/clavulanate 3. TMP/SMZ (Septra) 4. None 354. Joanna had a small ventricle septal defect (VSD) repaired when she was 3 years old and has no residual cardiac problems. She is now 28 and is requesting prophylactic antibiotics for an upcoming dental visit. The appropriate antibiotic to prescribe according to current American College of Cardiology and American Heart Association guidelines is: 1. None, no antibiotic is required for dental procedures 2. Amoxicillin 2 grams 1 hour before the procedure 3. Ampicillin 2 grams IM or IV 30 minutes before the procedure 4. Azithromycin 1 gram 1 hour before the procedure 355. To prevent further development of antibacterial resistance it is recommended that fluoroquinolones be reserved for treatment of: 1. Urinary tract infections in young women 2. Upper respiratory infections in adults 3. Skin and soft tissue infections in adults 4. Community-acquired pneumonia in patients with comorbidities 356. Fluoroquinolones have a Black Box Warning regarding ________ even months after treatment. 1. Renal dysfunction 2. Hepatic toxicity 3. Tendon rupture 4. Development of glaucoma 357. Janet was recently treated with clindamycin for an infection. She calls the advice nurse because she is having frequent diarrhea that she thinks may have blood in it. What would be the appropriate care for her? 1. Encourage increased fluids and fiber. 2. Assess her for pseudomembranous colitis. 3. Advise her to eat yogurt daily to help restore her gut bacteria. 4. Start her on an antidiarrheal medication. 358. Keng has chronic hepatitis that has led to mildly impaired liver function. He has an infection that would be best treated by a macrolide. Which would be the best choice for a patient with liver dysfunction? 1. Azithromycin (Zithromax) 2. Clarithromycin (Biaxin) 3. Erythromycin (E-mycin) . None of the above 359. Jamie has glucose-6-phosphate dehydrogenase deficiency (G6PD) and requires an antibiotic. Which class of antibiotics should be avoided in this patient? 1. Penicillins 2. Macrolides 3. Cephalosporins 4. Sulfonamides 360. If a patient is allergic to sulfonamide antibiotics, he or she will most likely have cross-sensitivity to: 1. Loop diuretics 2. Sulfonylureas 3. Thiazide diuretics 4. All of the above 361. Tetracyclines such as minocycline are safe to use in: 1. Pregnant women 2. Adolescents 3. Patients with renal dysfunction 4. Patients with hepatic dysfunction 362. Tetracyclines should not be prescribed to children younger than 8 years due to: 1. Risk of developing cartilage problems 2. Development of significant diarrhea 3. Risk of kernicterus 4. Adverse effects on bone growth 363. Nicole is a 16-year-old female who is taking minocycline for acne. She comes to the clinic complaining of a headache. What would be the plan of care? 1. Advise acetaminophen or ibuprofen as needed for headaches. 2. Prescribe sumatriptan (Imitrex) to be taken at the onset of the headache. 3. Evaluate her for pseudotremor cerebri. 4. Assess her caffeine intake and sleep patterns. 364. Patricia has been prescribed doxycycline for a chlamydia infection. She is healthy and her only medication is an oral combined contraceptive. Patricia's education would include: 1. Use a back-up method of birth control (condom) until her next menses. 2. Doxycycline may cause tendonitis and she should report any joint pain. 3. Her partner will need treatment if her infection doesn't clear with the doxycycline. 4. Doxycycline is used for one-dose treatment of STIs; take the whole prescription at once. 365. To prevent the development of peripheral neuropathy in patients taking isoniazid for tuberculosis the patient is also prescribed: 1. Niacin (vitamin B3) 2. Pyridoxine (vitamin B6) 3. Riboflavin (vitamin B2) 4. Thiamine (vitamin B1) 366. Sadie is an 82-year-old patient who has herpes zoster (shingles) and would benefit from an antiviral such as valacyclovir. Prior to prescribing valacyclovir she will need an assessment of: 1. Complete blood count to rule out anemia 2. Liver function 3. Renal function 4. Immunocompetence 367. When prescribing acyclovir, patients should be educated regarding the: 1. High risk of developing diarrhea 2. Need to drink lots of fluids during treatment 3. Risk for life-threatening rash such as Stevens-Johnson 4. Eccentric dosing schedule 368. Nicholas has been diagnosed with type A influenza. Appropriate prescribing of oseltamivir (Tamiflu) would include: 1. Starting oseltamivir within the first 48 hours of influenza symptoms 2. Advising the patient he can stop the oseltamivir when his symptoms resolve 3. Educating the patient that oseltamivir will cure influenza 4. Prophylactic treatment of all family members 369. Monitoring for patients who are on long-term antifungal therapy with ketoconazole includes: 1. Platelet count 2. BUN and creatinine 3. White blood cell count 4. AST, ALT, alkaline phosphatase, and bilirubin 370. When prescribing metronidazole (Flagyl) to treat bacterial vaginosis, patient education would include: 1. Metronidazole is safe in the first trimester of pregnancy. 2. Consuming alcohol in any form may cause a severe reaction. 3. Sexual partners need concurrent therapy. 4. Headaches are a sign of a serious adverse reaction and need immediate evaluation. 371. Every antibiotic drug class has resistant organisms that influence prescribing decisions. 1. True 2. False 372. The goals of treatment when prescribing antiretroviral medication to patients with HIV include: 1. Prevent vertical HIV transmission 2. Improve quality of life 3. Prolong survival 4. All of the above 373. A challenge faced with antiretroviral therapy (ART) is: 1. Patients abusing ART 2. Drug-resistant mutations of HIV 3. Reduction of transmissibility of HIV 4. Lack of efficacy data 374. Predictors for successful treatment with antiretroviral therapy (ART) in HIV- positive patients include: 1. They respond to a low-potency treatment regimen 2. They have demonstrated resistance in the past and should respond to newer ART drugs 3. The patient is strictly adherent to the ART treatment regimen 4. Lower baseline CD4 T-cell count at baseline 375. The goal of antiretroviral therapy in HIV-positive patients is: 1. Maximum suppression of HIV replication 2. Eradication of HIV virus from the body 3. Determining a treatment regimen that is free of adverse effects 4. Suppression of CD4 T-cell count 376. Pregnant women who are HIV positive: 1. Are treated with AZT alone to prevent birth defects 2. Are treated with a combination antiretroviral therapy (ART) regimen 3. Should not be treated with ART due to teratogenicity of the drugs 4. Are at high risk of developing resistance to ART drugs 377. Antiretroviral therapy is recommended for HIV-positive patients with: 1. A history of AIDS-defining illness 2. Pregnant women 3. Hepatitis B co-infection 4. All of the above 378. If considering starting a patient on the nucleoside reverse transcriptase inhibitor abacavir, the following testing is recommended prior to prescribing: 1. Renal function 2. HLA B*5701 testing 3. Pancreatic enzyme levels 4. CYP 450 enzyme activity 379. Suzanne is pregnant and has tested HIV positive. Which antiretroviral drug should be avoided in women who are pregnant? 1. Lopinavir/r 2. Zidovudine 3. Ritonavir 4. Lopinavir/ritonavir 380. The cost of HIV treatment can be prohibitive for any patient. Patients can receive assistance from the: 1. Best Pharmaceuticals for HIV/AIDS Patient Act 2. Ryan White HIV/AIDS Treatment Modernization Act 3. National Institute of Health HIV/AIDS Assistance Fund 4. Centers for Disease Control HIV/AIDS Treatment Fund 381. Resistance to antiretroviral therapy (ART) is measured by: 1. Measuring the DNA viral load in the serum 2. Determining plasma viral RNA on two successive measurements 3. Phenotype assays of the combination of ART the patient is on 4. Elevation of T4 counts 382. Phenotype assays are used to measure _______ of antiretroviral therapy. 1. Effectiveness 2. Genotype 3. Sensitivity 4. Hypersensitivity susceptibility 383. Patient factors that contribute to antiretroviral therapy (ART) failure include: 1. Being a male who has sex with males 2. HIV diagnosis in pregnancy 3. Good compliance with the ART treatment regimen 4. ART adverse effects 384. Patients who are taking antiretroviral therapy need to have the following monitored: 1. Lipid levels 2. Sexual functioning 3. Platelet count 4. All of the above 385. Successful antiretroviral therapy (ART) in an HIV-positive patient is determined by: 1. Being able to stop ART therapy due to HIV virus eradication 2. Lowering HIV viral load to unmeasurable amounts 3. Individual measures of success based on their personal situation 4. Normal blood hematologic factors 386. Drug resistant tuberculosis (TB) is defined as TB that is resistant to: 1. Fluoroquinolones 2. Rifampin and isoniazid 3. Amoxicillin 4. Ceftriaxone 387. Goals when treating tuberculosis include: 1. Completion of recommended therapy 2. Negative purified protein derivative at the end of therapy 3. Completely normal chest x-ray 4. All of the above 388. The principles of drug therapy for the treatment of tuberculosis include: 1. Patients are treated with a drug to which M. tuberculosis is sensitive. 2. Drugs need to be taken on a regular basis for a sufficient amount of time. 3. Treatment continues until the patient's purified protein derivative is negative. 4. All of the above 389. Isabella has confirmed tuberculosis and is placed on a 6-month treatment regimen. The 6-month regimen consists of: 1. Two months of four-drug therapy (INH, rifampin, pyrazinamide, and ethambutol) followed by Four months of INH and rifampin 2. Six months of INH with daily pyridoxine throughout therapy 3. Six months of INH, rifampin, pyrazinamide, and ethambutol 4. Any of the above 390. Kaleb has extensively resistant tuberculosis (TB). Treatment for extensively resistant TB would include: 1. INH, rifampin, pyrazinamide, and ethambutol for at least 12 months 2. INH, ethambutol, kanamycin, and rifampin 3. Treatment with at least two drugs to which the TB is susceptible 4. Levofloxacin 391. Lila is 24 weeks pregnant and has been diagnosed with tuberculosis (TB). Treatment regimens for a pregnant patient with TB would include: 1. Streptomycin 2. Levofloxacin 3. Kanamycin 4. Pyridoxine 392. Bilal is a 5-year-old patient who has been diagnosed with tuberculosis. His treatment would include: 1. Pyridoxine 2. Ethambutol 3. Levofloxacin 4. Rifabutin 393. Ezekiel is a 9-year-old patient who lives in a household with a family member newly diagnosed with tuberculosis (TB). To prevent Ezekiel from developing TB he should be treated with: 1. 6 months of Isoniazid (INH) and rifampin 2. 2 months of INH, rifampin, pyrazinamide, and ethambutol, followed by 4 months of INH 3. 9 months of INH 4. 12 months of INH 394. Leonard is completing a 6-month regimen to treat tuberculosis (TB). Monitoring of a patient on TB therapy includes: 1. Monthly sputum cultures 2. Monthly chest x-ray 3. Bronchoscopy every 3 months 4. All of the above 395. Compliance with directly observed therapy can be increased by: 1. Convenient clinic times 2. Incentives such as food, clothing, and transportation costs 3. Offering gifts for compliance 4. All of the above 396. Which of the following patients would be at higher risk of experiencing adverse drug reactions (ADRs): 1. A 32-year-old male 2. A 22-year-old female 3. A 3-month-old female 4. A 48-year-old male 397. Infants and young children are at higher risk of ADRs due to: 1. Immature renal function in school-age children 2. Lack of safety and efficacy studies in the pediatric population 3. Children's skin being thicker than adults, requiring higher dosages of topical medication 4. Infant boys having a higher proportion of muscle mass, leading to a higher volume of distribution 398. The elderly are at high risk of ADRs due to: 1. Having greater muscle mass than younger adults, leading to higher volume of distribution 2. The extensive studies that have been conducted on drug safety in this age group 3. The blood-brain barrier being less permeable, requiring higher doses to achieve therapeutic effect 4. Age-related decrease in renal function 399. The type of adverse drug reaction that is idiosyncratic when a drug given in the usual therapeutic doses is type: 1. A 2. B 3. C 4. D 400. Digoxin may cause a type A adverse drug reaction due to: 1. Idiosyncratic effects 2. Its narrow therapeutic index 3. Being a teratogen 4. Being a carcinogen 401. Sarah developed a rash after using a topical medication. This is a type __ allergic drug reaction. 1. I 2. II 3. III 4. IV 402. A patient may develop neutropenia from using topical Silvadene for burns. Neutropenia is a(n): 1. Cytotoxic hypersensitivity reaction 2. Immune complex hypersensitivity 3. Immediate hypersensitivity reaction 4. Delayed hypersensitivity reaction 403. Anaphylactic shock is a: 1. Type I reaction, called immediate hypersensitivity reaction 2. Type II reaction, called cytotoxic hypersensitivity reaction 3. Type III allergic reaction, called immune complex hypersensitivity 4. Type IV allergic reaction, called delayed hypersensitivity reaction 404. James has hypothalamic-pituitary-adrenal axis suppression from chronic prednisone (a corticosteroid) use. He is at risk for what type of adverse drug reaction? 1. Type B 2. Type C 3. Type E 4. Type F 405. Immunomodulators such as azathioprine may cause a delayed adverse drug reaction known as a type D reaction because they are known: 1. Teratogens 2. Carcinogens 3. To cause hypersensitivity reactions 4. Hypothalamus-pituitary-adrenal axis suppressants 406. A 24-year-old male received multiple fractures in a motor vehicle accident that required significant amounts of opioid medication to treat his pain. He is at risk for a _____ adverse drug reaction when he no longer requires the opioids. 1. Rapid 2. First-dose 3. Late 4. Delayed 407. An example of a first-dose reaction that may occur includes: 1. Orthostatic hypotension that does not occur with repeated doses 2. Purple glove syndrome with phenytoin use 3. Hemolytic anemia from ceftriaxone use 4. Contact dermatitis from neomycin use 408. Drugs that are prone to cause adverse drug effects include: 1. Diuretics 2. Inhaled anticholinergics 3. Insulins 4. Stimulants 409. The U.S. Food and Drug Administration MedWatch system is activated when: 1. There is an adverse event to a vaccine. 2. The patient has a severe reaction that is noted in the "Severe Reaction" section in the medication label. 3. A lactating woman takes a medication that is potentially toxic to the breastfeeding infant. 4. An adverse event or serious problem occurs with a medication that is not already identified on the label. 410. The Vaccine Adverse Events Reporting System is: 1. A mandatory reporting system for all health-care providers when they encounter an adverse vaccine event 2. A voluntary reporting system that health-care providers or consumers may use to report vaccine adverse events 3. Utilized to send out safety alerts regarding emerging vaccine safety issues 4. Activated when a vaccine has been proven to cause significant adverse effects 411. Charlie is a 65-year-old male who has been diagnosed with hypertension and benign prostatic hyperplasia. Doxazosin has been chosen to treat his hypertension because it: 1. Increases peripheral vasoconstriction 2. Decreases detrusor muscle contractility 3. Lowers supine blood pressure more than standing pressure 4. Relaxes smooth muscle in the bladder neck 412. To reduce potential adverse effects, patients taking a peripherally acting alpha1 antagonist should do all of the following EXCEPT: 1. Take the dose at bedtime 2. Sit up slowly and dangle their feet before standing 3. Monitor their blood pressure and skip a dose if the pressure is less than 120/80 4. Weigh daily and report weight gain of greater than 2 pounds in one day 413. John has clonidine, a centrally acting adrenergic blocker, prescribed for his hypertension. He should: 1. Not miss a dose or stop taking the drug because of potential rebound hypertension 2. Increase fiber in the diet to treat any diarrhea that may occur 3. Reduce fluid intake to less than 2 liters per day to prevent fluid retention 4. Avoid sitting for long periods, as this can lead to deep vein thrombosis 414. Clonidine has several off-label uses, including: 1. Alcohol and nicotine withdrawal 2. Post-herpetic neuralgia 3. Both 1 and 2 4. Neither 1 nor 2 415. Jim is being treated for hypertension. Because he has a history of heart attack, the drug chosen is atenolol. Beta blockers treat hypertension by: 1. Increasing heart rate to improve cardiac output 2. Reducing vascular smooth muscle tone 3. Increasing aldosterone-mediated volume activity 4. Reducing aqueous humor production 416. Which of the following adverse effects are less likely in a beta1-selective blocker? 1. Dysrhythmias 2. Impaired insulin release 3. Reflex orthostatic changes 4. Decreased triglycerides and cholesterol 417. Richard is 70 years old and has a history of cardiac dysrhythmias. He has been prescribed nadolol. You do his annual laboratory work and find a CrCl of 25 ml/min. What action should you take related to his nadolol? 1. Extend the dosage interval. 2. Decrease the dose by 75%. 3. Take no action because this value is expected in the older adult. 4. Schedule a serum creatinine level to validate the CrCl value. 418. Beta blockers are the drugs of choice for exertional angina because they: 1. Improve myocardial oxygen supply by vasodilating the coronary arteries 2. Decrease myocardial oxygen demand by decreasing heart rate and vascular resistance 3. Both 1 and 2 4. Neither 1 nor 2 419. Adherence to beta blocker therapy may be affected by their: 1. Short half-lives requiring twice daily dosing . Tendency to elevate lipid levels 3. Effects on the male genitalia, which may produce impotence 4. None of the above 420. Beta blockers have favorable effects on survival and disease progression in heart failure. Treatment should be initiated when the: 1. Symptoms are severe 2. Patient has not responded to other therapies 3. Patient has concurrent hypertension 4. Left ventricular dysfunction is diagnosed 421. Abrupt withdrawal of beta blockers can be life threatening. Patients at highest risk for serious consequences of rapid withdrawal are those with: 1. Angina 2. Coronary artery disease 3. Both 1 and 2 4. Neither 1 nor 2 422. To prevent life-threatening events from rapid withdrawal of a beta blocker: 1. The dosage interval should be increased by 1 hour each day. 2. An alpha blocker should be added to the treatment regimen before withdrawal. 3. The dosage should be tapered over a period of weeks. 4. The dosage should be decreased by one-half every 4 days. 423. Beta blockers are prescribed for diabetics with caution because of their ability to produce hypoglycemia and block the common symptoms of it. Which of the following symptoms of hypoglycemia is not blocked by these drugs and so can be used to warn diabetics of possible decreased blood glucose? 1. Dizziness 2. Increased heart rate 3. Nervousness and shakiness 4. Diaphoresis 424. Combined alpha-beta antagonists are used to reduce the progression of heart failure because they: 1. Vasodilate the peripheral vasculature 2. Decrease cardiac output 3. Increase renal vascular resistance 4. Reduce atherosclerosis secondary to elevated serum lipoproteins 425. Carvedilol is heavily metabolized by CYP2D6 and 2C9, resulting in drug interactions with which of the following drug classes? 1. Histamine 2 blockers 2. Quinolones 3. Serotonin re-uptake inhibitors 4. All of the above 426. Alpha-beta blockers are especially effective to treat hypertension for which ethnic group? 1. White 2. Asian 3. African American 4. Native American 427. Bethanechol: 1. Increases detrusor muscle tone to empty the bladder 2. Decreases gastric acid secretion to treat peptic ulcer disease 3. Stimulates voluntary muscle tone to improve strength 4. Reduces bronchial airway constriction to treat asthma 428. Clinical dosing of Bethanechol: 1. Begins at the highest effective dose to obtain a rapid response 2. Starts at 5 mg to 10 mg PO and is repeated every hour until a satisfactory clinical response is achieved 3. Requires dosing only once daily 4. Is the same for both the oral and parenteral route 429. Patients who need to remain alert are taught to avoid which drug due to its antimuscarinic effects? 1. Levothyroxine 2. Prilosec 3. Dulcolax 4. Diphenhydramine 430. Anticholinesterase inhibitors are used to treat: 1. Peptic ulcer disease 2. Myasthenia gravis 3. Both 1 and 2 4. Neither 1 nor 2 431. Which of the following drugs used to treat Alzheimer's disease is not an anticholinergic? 1. Donepezil 2. Memantine 3. Rivastigmine 4. Galantamine 432. Taking which drug with food maximizes it bioavailability? 1. Donepezil 2. Galantamine 3. Rivastigmine 4. Memantine 433. Which of the following drugs should be used only when clearly needed in pregnant and breastfeeding women? 1. Memantine 2. Pyridostigmine 3. Galantamine 4. Rivastigmine 434. There is a narrow margin between first appearance of adverse reaction to AChE inhibitors and serious toxic effects. Adverse reactions that require immediate action include: 1. Dizziness and headache 2. Nausea 3. Decreased salivation 4. Fasciculations of voluntary muscles 435. Adherence is improved when a drug can be given once daily. Which of the following drugs can be given once daily? 1. Tacrine 2. Donepezil 3. Memantine 4. Pyridostigmine 436. Nicotine has a variety of effects on nicotinic receptors throughout the body. Which of the following is NOT an effect of nicotine? 1. Vasodilation and decreased heart rate 2. Increased secretion of gastric acid and motility of the GI smooth muscle 3. Release of dopamine at the pleasure center 4. Stimulation of the locus coeruleus 437. Nicotine gum products are: 1. Chewed to release the nicotine and then swallowed for a systemic effect 2. "Parked" in the buccal area of the mouth to produce a constant amount of nicotine release 3. Bound to exchange resins so the nicotine is only released during chewing 4. Approximately the same in nicotine content as smoking two cigarettes 438. Nicotine replacement therapy (NRT): 1. Is widely distributed in the body only when the gum products are used 2. Does not cross the placenta and so is safe for pregnant women 3. Delays healing of esophagitis and peptic ulcers 4. Has no drug interactions when a transdermal patch is used 439. Success rates for smoking cessation using NRT: 1. Are about the same regardless of the method chosen 2. Vary from 40% to 50% at 12 months 3. Both 1 and 2 4. Neither 1 nor 2 440. Cholinergic blockers are used to: 1. Counteract the extrapyramidal symptoms (EPS) effects of phenothiazines 2. Control tremors and relax smooth muscle in Parkinson's disease 3. Inhibit the muscarinic action of ACh on bladder muscle 4. All of the above 441. Several classes of drugs have interactions with cholinergic blockers. Which of the following is true about these interactions? 1. Drugs with a narrow therapeutic range given orally may not stay in the GI tract long enough to produce an action. 2. Additive antimuscarinic effects may occur with antihistamines. 3. Cholinergic blockers may decrease the sedative effects of hypnotics. 4. Cholinergic blockers are contraindicated with antipsychotics. 442. Scopolamine can be used to prevent the nausea and vomiting associated with motion sickness. The patient is taught to: 1. Apply the transdermal disk at least 4 hours before the antiemetic effect is desired. 2. Swallow the tablet 1 hour before traveling where motion sickness is possible. 3. Place the tablet under the tongue and allow it to dissolve. 4. Change the transdermal disk daily for maximal effect. 443. You are managing the care of a patient recently diagnosed with benign prostatic hyperplasia (BPH). He is taking tamsulosin but reports dizziness when standing abruptly. The best option for this patient is: 1. Continue the tamsulosin because the side effect will resolve with continued treatment. 2. Discontinue the tamsulosin and start doxazosin. 3. Have him double his fluid intake and stand more slowly. 4. Prescribe meclizine as needed for the dizziness. 444. You are treating a patient with a diagnosis of Alzheimer's disease. The patient's wife mentions difficulty with transportation to the clinic. Which medication is the best choice? 1. Donepezil 2. Tacrine 3. Doxazosin 4. Verapamil 445. A patient presents with a complaint of dark stools and epigastric pain described as gnawing and burning. Which of the medications is the most likely cause? 1. Acetaminophen 2. Estradiol 3. Donepezil 4. Bethanechol 446. Your patient calls for an appointment before going on vacation. Which medication should you ensure he has an adequate supply of before leaving to avoid life-threatening complications? 1. Carvedilol 2. Donepezil 3. Bethanechol 4. Tacrine 447. Activation of central alpha2 receptors results in inhibition of cardioacceleration and ______________ centers in the brain. 1. Vasodilation 2. Vasoconstriction 3. Cardiovascular 4. Respiratory 448. Digoxin levels need to be monitored closely when the following medication is started: 1. Loratadine 2. Diphenhydramine 3. Ipratropium 4. Albuterol 449. Patients with pheochromocytoma should avoid which of the following classes of drugs because of the possibility of developing hypertensive crisis? 1. Expectorants 2. Beta-2-agonists 3. Antitussives 4. Antihistamines 450. Harold, a 42-year-old African American, has moderate persistent asthma. Which of the following asthma medications should be used cautiously, if at all? 1. Betamethasone, an inhaled corticosteroid 2. Salmeterol, an inhaled long-acting beta-agonist 3. Albuterol, a short-acting beta-agonist 4. Montelukast, a leukotriene modifier 451. Long-acting beta-agonists (LTBAs) received a Black Box Warning from the U.S. Food and Drug Administration due to the: 1. Risk of life-threatening dermatological reactions 2. Increased incidence of cardiac events when LTBAs are used 3. Increased risk of asthma-related deaths when LTBAs are used 4. Risk for life-threatening alterations in electrolytes 452. The bronchodilator of choice for patients taking propranolol is: 1. Albuterol 2. Pirbuterol 3. Formoterol 4. Ipratropium 453. James is a 52-year-old overweight smoker taking theophylline for his persistent asthma. He tells his provider he is going to start the Atkin's diet for weight loss. The appropriate response would be: 1. Congratulate him on making a positive change in his life. 2. Recommend he try stopping smoking instead of the Atkin's diet. 3. Schedule him for regular testing of serum theophylline levels during his diet due to increased excretion of theophylline. 4. Decrease his theophylline dose because a high-protein diet may lead to elevated theophylline levels. 454. Li takes theophylline for his persistent asthma and calls the office with a complaint of nausea, vomiting, and headache. The best advice for him would be to: 1. Reassure him this is probably a viral infection and should be better soon 2. Have him seen the same day for an assessment and theophylline level 3. Schedule him for an appointment in 2 to 3 days, which he can cancel if he is better 4. Order a theophylline level at the laboratory for him 455. Tiotropium bromide (Spiriva) is an inhaled anticholinergic: 1. Used for the treatment of chronic obstructive pulmonary disease (COPD) 2. Used in the treatment of asthma 3. Combined with albuterol for treatment of asthma exacerbations 4. Combined with fluticasone for the treatment of persistent asthma 456. Christy has exercise-induced and mild persistent asthma and is prescribed two puffs of albuterol 15 minutes before exercise and as needed for wheezing. One puff per day of beclomethasone (QVAR) is also prescribed. Teaching regarding her inhalers includes: 1. Use one to two puffs of albuterol per day to prevent an attack with no more than eight puffs per day 2. Beclomethasone needs to be used every day to treat her asthma 3. Report any systemic side effects she is experiencing, such as weight gain 4. Use the albuterol metered-dose inhaler (MDI) immediately after her corticosteroid MDI to facilitate bronchodilation 457. Conjunctivitis in a child that is accompanied by acute otitis media is treated with: 1. Sulfacetamide 10% ophthalmic solution (Bleph-10) 2. Bacitracin/polymyxin B (Polysporin) ophthalmic drops 3. Ciprofloxacin (Ciloxan) ophthalmic drops 4. High-dose oral amoxicillin 458. Twenty-year-old Annie comes to the clinic complaining of copious yellow-green eye discharge. Gram stain indicates she most likely has gonococcal conjunctivitis. While awaiting the culture results, the plan of care should be: 1. None, wait for the culture results to determine the course of treatment 2. Ciprofloxacin (Ciloxan) ophthalmic drops 3. IM ceftriaxone 4. High-dose oral amoxicillin 459. Sadie was prescribed betaxolol ophthalmic drops by her ophthalmologist to treat her glaucoma. Oral beta blockers should be avoided in patients who use ophthalmic beta blockers because: 1. There may be an antagonistic reaction between the two. 2. The additive effects may include bradycardia. 3. They may potentiate each other and cause respiratory depression. 4. The additive effects may cause metabolic acidosis. 460. David presents to the clinic with symptoms of allergic conjunctivitis. He is prescribed cromolyn sodium (Opticrom) eye drops. The education regarding using cromolyn eye drops includes: 1. He should not wear his soft contacts while using the cromolyn eye drops. 2. Cromolyn drops are instilled once a day to prevent allergy symptoms. 3. Long-term use may cause glaucoma. 4. He may experience bradycardia as an adverse effect. 461. Ciprofloxacin otic drops are contraindicated in: 1. Children 2. Patients with acute otitis externa 3. Patients with a perforated tympanic membrane 4. Swimmer's ear 462. __________ is / are prescribed to prevent swimmer's ear. 1. Ciprofloxacin otic drops (Ciloxan) 2. Isopropyl ear drops (EarSol) 3. Colistin (Coly-Mycin S Otic) 4. Gentamicin otic drops 463. Patient education regarding the use of ciprofloxacin-hydrocortisone (Cipro HC otic) ear drops includes: 1. Fill the canal with the drops with each dose. 2. Some redness and itching around the ear canal is normal. 3. Warm the bottle of ear drops in his or her hand before administering. 4. Cipro HC otic may cause ototoxicity. 464. Janie presents to the clinic with hard ear wax in both ear canals. Instructions regarding home removal of hard cerumen include: 1. Moisten a cotton swab (Q-tip) and swab the ear canal twice daily. 2. Instill tap water in both ears while bathing. 3. Squirt hydrogen peroxide into ears with each bath. 4. Instill carbamide peroxide (Debrox) twice daily until canals are clear. 465. Prior to developing a plan for the treatment of asthma, the patient's asthma should be classified according to the NHLBI Expert Panel 3 guidelines. In adults mild-persistent asthma is classified as asthma symptoms that occur: 1. Daily 2. Daily and limit physical activity 3. Less than twice a week 4. More than twice a week and less than once a day 466. In children age 5 to 11 years mild-persistent asthma is diagnosed when asthma symptoms occur: 1. At nighttime one to two times a month 2. At nighttime three to four times a month 3. Less than twice a week 4. Daily 467. The first-line drug choice for a previously healthy adult patient diagnosed with community-acquired pneumonia would be: 1. Ciprofloxacin 2. Azithromycin 3. Amoxicillin 4. Doxycycline 468. The first-line antibiotic choice for a patient with comorbidities or who is immunosuppressed who has pneumonia and can be treated as an outpatient would be: 1. Levofloxacin 2. Amoxicillin 3. Ciprofloxacin 4. Cephalexin 469. If an adult patient with comorbidities cannot reliably take oral antibiotics to treat pneumonia, an appropriate initial treatment option would be: 1. IV or IM gentamicin 2. IV or IM ceftriaxone 3. IV amoxicillin 4. IV ciprofloxacin 470. Samantha is 34 weeks pregnant and has been diagnosed with pneumonia. She is stable enough to be treated as an outpatient. What would be an appropriate antibiotic to prescribe? 1. Levofloxacin 2. Azithromycin 3. Amoxicillin 4. Doxycycline 471. Adults with pneumonia who are responding to antimicrobial therapy should show improvement in their clinical status in: 1. 12 to 24 hours 2. 24 to 36 hours 3. 48 to 72 hours 4. 4 or 5 days 472. Along with prescribing antibiotics, adults with pneumonia should be instructed on lifestyle modifications to improve outcomes, including: 1. Adequate fluid intake 2. Increased fiber intake 3. Bedrest for the first 24 hours 4. All of the above 473. John is a 4-week-old infant who has been diagnosed with chlamydial pneumonia. An appropriate treatment for his pneumonia would be: 1. Levofloxacin 2. Amoxicillin 3. Erythromycin 4. Cephalexin 474. Wing-Sing is a 4-year-old patient who has suspected bacterial pneumonia. He has a temperature of 102°F, oxygen saturation level of 95%, and is taking fluids adequately. What would be appropriate initial treatment for his pneumonia? 1. Ceftriaxone 2. Azithromycin 3. Cephalexin 4. Levofloxacin 475. Giselle is a 14-year-old patient who presents to the clinic with symptoms consistent with mycoplasma pneumonia. What is the treatment for suspected mycoplasma pneumonia in an adolescent? 1. Ceftriaxone 2. Azithromycin 3. Ciprofloxacin 4. Levofloxacin 476. Caleb is an adult with an upper respiratory infection (URI). Treatment for his URI would include: 1. Amoxicillin 2. Diphenhydramine 3. Phenylpropanolamine 4. Topical oxymetazoline 477. Rose is a 3-year-old patient with an upper respiratory infection (URI). Treatment for her URI would include: 1. Amoxicillin 2. Diphenhydramine 3. Pseudoephedrine 4. Nasal saline spray 478. Patients who should be cautious about using decongestants for an upper respiratory infection (URI) include: 1. School-age children 2. Patients with asthma 3. Patients with cardiac disease 4. Patients with allergies 479. Jaheem is a 10-year-old low-risk patient with sinusitis. Treatment for a child with sinusitis is: 1. Amoxicillin 2. Azithromycin 3. Cephalexin 4. Levofloxacin 480. Jacob has been diagnosed with sinusitis. He is the parent of a child in daycare. Treatment for sinusitis in an adult who has a child in daycare is: 1. Azithromycin 500 mg q day for 5 days 2. Amoxicillin-clavulanate 500 mg bid for 7 days 3. Ciprofloxacin 500 mg bid for 5 days 4. Cephalexin 500 mg qid for 5 days 481. The length of treatment for sinusitis in a low-risk patient should be: 1. 5-7 days 2. 7-10 days 3. 14-21 days 4. 7 days beyond when symptoms cease 482. Patient education for a patient who is prescribed antibiotics for sinusitis includes: 1. Use of nasal saline washes 2. Use of inhaled corticosteroids 3. Avoiding the use of ibuprofen while ill 4. Use of laxatives to treat constipation 483. Myles is a 2-year-old patient who has been diagnosed with acute otitis media. He is afebrile and has not been treated with antibiotics recently. First-line treatment for his otitis media would include: 1. Azithromycin 2. Amoxicillin 3. Ceftriaxone 4. Trimethoprim/sulfamethoxazole 484. Alyssa is a 15-month-old patient who has been on amoxicillin for 2 days for acute otitis media. She is still febrile and there is no change in her tympanic membrane examination. What would be the plan of care for her? 1. Continue the amoxicillin for the full 10 days. 2. Change the antibiotic to azithromycin. 3. Change the antibiotic to amoxicillin/clavulanate. 4. Change the antibiotic to trimethoprim/sulfamethoxazole. 485. A child that may warrant "watchful waiting" instead of prescribing an antibiotic for acute otitis media includes patients who: 1. Are low risk with temperature of less than 39oC or 102.2oF 2. Have reliable parents with transportation 3. Are older than age 2 years 4. All of the above 486. Whether prescribing an antibiotic for a child with acute otitis media or not, the parents should be educated about: 1. Using decongestants to provide faster symptom relief 2. Providing adequate pain relief for at least the first 24 hours 3. Using complementary treatments for acute otitis media, such as garlic oil 4. Administering an antihistamine/decongestant combination (Dimetapp) so the child can sleep better 487. First-line therapy for a patient with acute otitis externa (swimmer's ear) and an intact tympanic membrane includes: 1. Swim-Ear drops 2. Ciprofloxacin and hydrocortisone drops 3. Amoxicillin 4. Gentamicin ophthalmic drops [Show More]
Last updated: 1 year ago
Preview 1 out of 77 pages
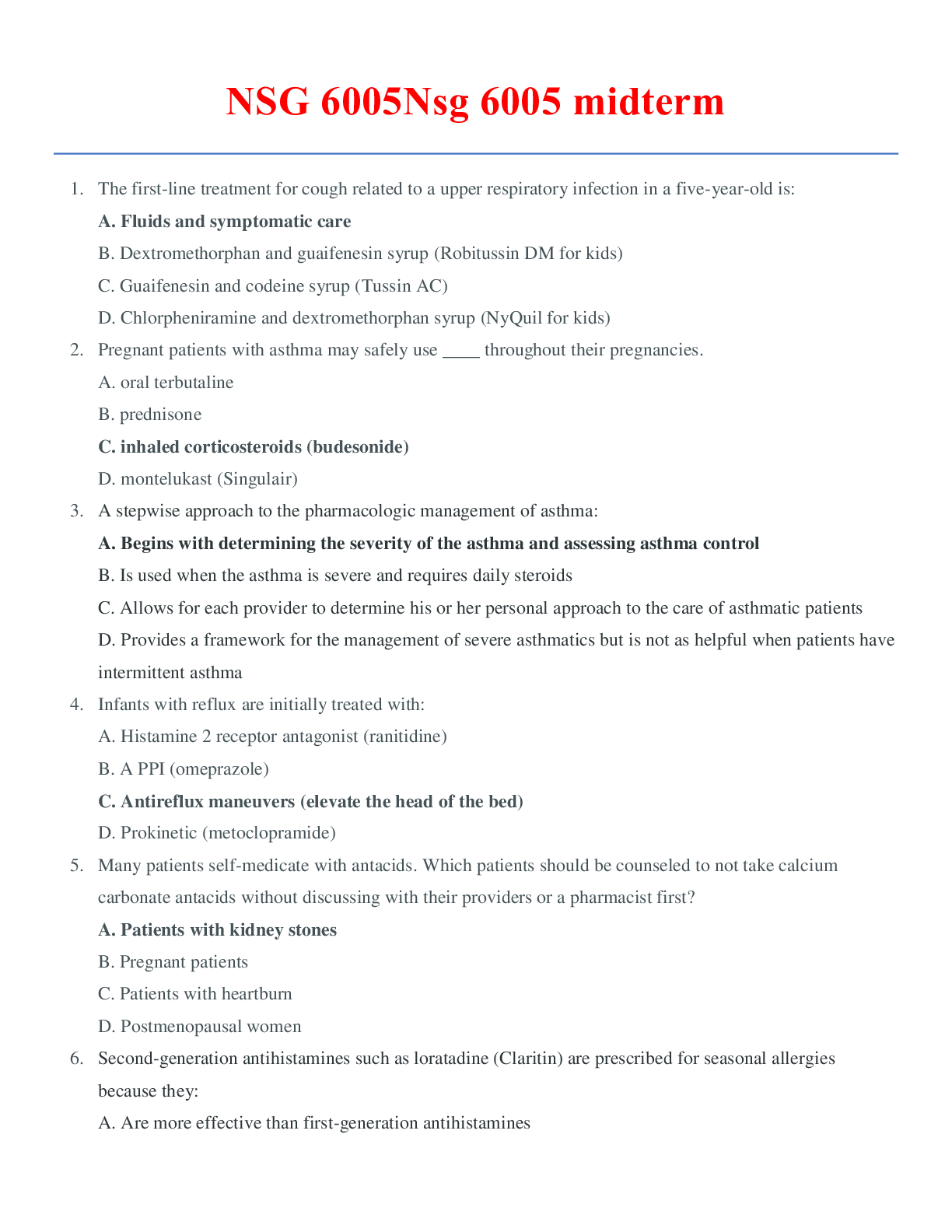
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Jul 13, 2020
Number of pages
77
Written in
Additional information
This document has been written for:
Uploaded
Jul 13, 2020
Downloads
0
Views
44