*NURSING > EXAM REVIEW > NURSING FN NURS 6670N- Midterm exam with answers marked (All)
NURSING FN NURS 6670N- Midterm exam with answers marked
Document Content and Description Below
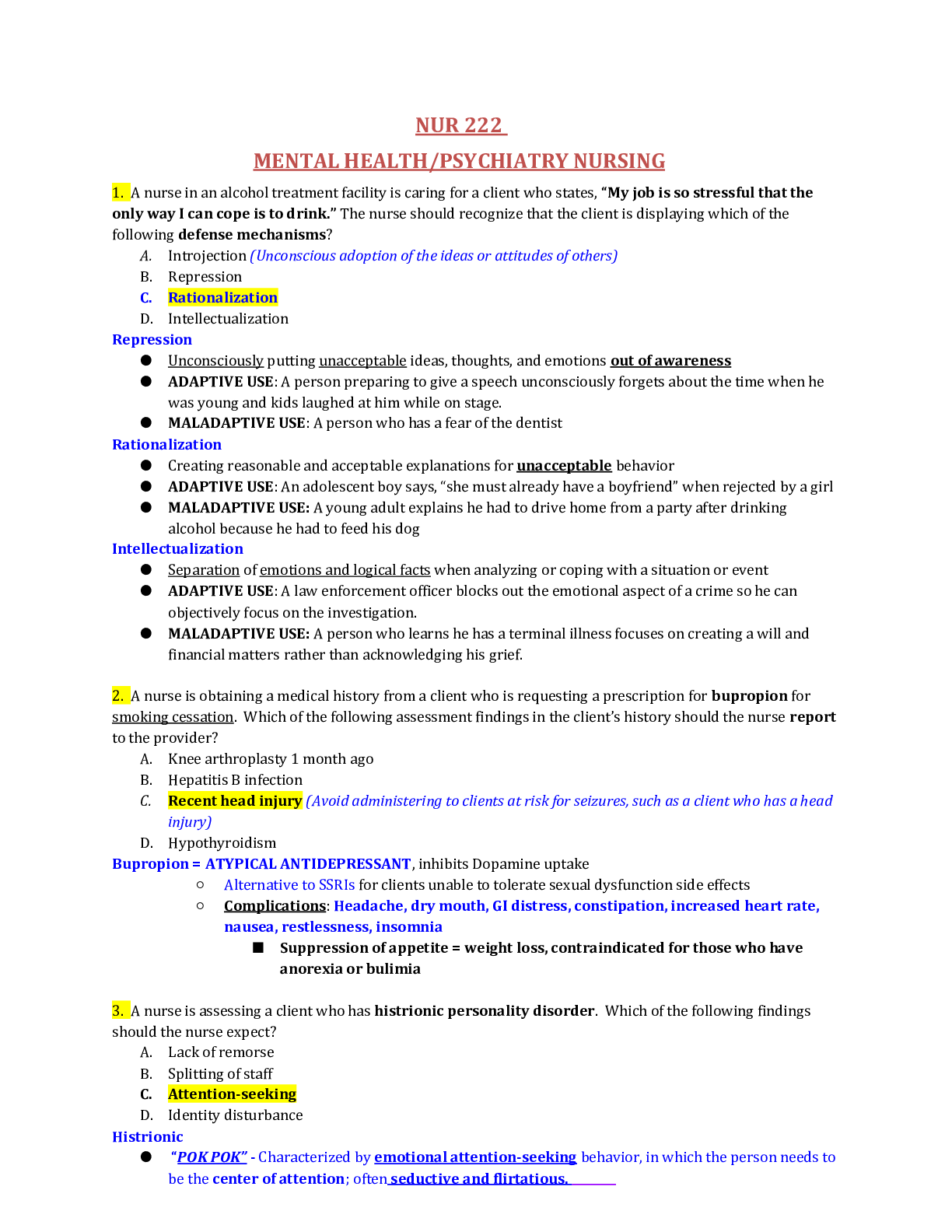
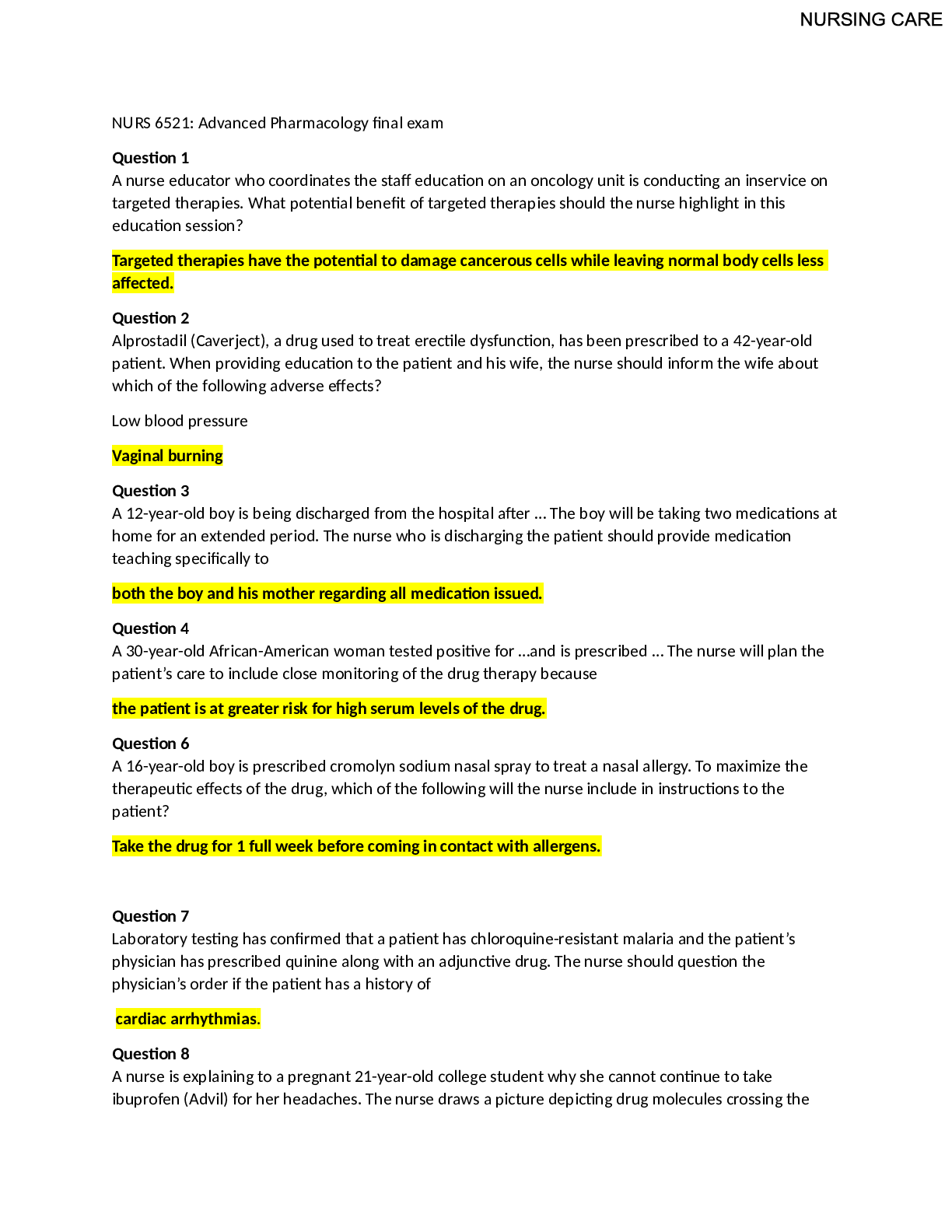
1 www.OnlineNursingPapers.com Correct answers marked yellow. Question 1 Alexa is a 27-year-old female who has come to group therapy while she is in the city jail. She was arrested for vagrancy bec... ause she was sleeping in her car in a parking lot at a local shopping center. She could not post bail, so she is sentenced to 14 days in jail. During group, she contributes that none of this is her fault. Her mother is totally evil because she would not let Alexa stay in the family home. She has some other family. but they are all jerks because they won’t help her. Alexa’s friend Melanie is the absolute best person in the world, but she can’t help because her boss fired her for no reason. Alexa has a history of arrests for buying illegal drugs and prostitution. The last time she was in jail, her sentence was extended for 30 days because she got into a fight with another inmate and beat her up so badly she had to be admitted to the hospital for 6 days. The PMHNP considers which of the following personality disorders? Histrionic Narcissistic Borderline Schizoid Question 2 Anne is a 32-year-old female who presented to care after a random drug screening at work was positive for cocaine. She was initially resistant to therapy, maintaining that her use is not a problem and she could stop at any time. Upon further discussion in session, it appears that she uses cocaine every day at work, sometimes 2–3 times, other days more. She also uses it occasionally at home and most weekends. During her third session, she admitted that it is a financial burden, and she basically cannot afford any other form of recreation. She understands that if she uses again she will lose her job, and she admits that she loves her job and that cocaine is not worth losing it. When counseling her about cessation strategies, the PMHNP advises all the following except: The physiologic symptoms of withdrawal may require a short-term hospitalization Unlike other substances of abuse, there are no medications to help reduce the intensity of withdrawal She will need to be monitored for depression Overcoming the intense craving for cocaine is the biggest issue Question 3 Clare’s history of personal relationships is characterized by complete intolerance of being alone. Whether it is an2 www.OnlineNursingPapers.com intimate-partner relationship or a close friend, Clare appears to always need someone in her life. She had a livein boyfriend of 3 years, and while they were together, he took care of everything. The PMHNP expects all of the following to be additional features of Clare’s history except: Has disproportionate anger toward an abusive spouse Question 4 The PMHNP is conducting an initial interview with a patient whose history is consistent with avoidant personality disorder. The PMHNP understands that one of the most striking features of this interview is likely to be centered upon the patient’s: Clothing Speech pattern Anger Anxiety Question 5 A PMHNP student is reviewing his notes from his clinical experience over the past week to prepare his first required case presentation on a patient suffering a major depressive episode. Which of the following patients best represents the DSM-5 criteria for major depressive episode? A 27-year-old female with a 1-month history of social withdrawal, anorexia, hypersomnia, unprovoked outbursts of anger, and a strong family history of endogenous depression A 41-year-old male with a history of childhood sexual abuse, loss of interest in both his professional and personal life, an unplanned 10 lb. weight loss in the last 3 months, and perceptual disturbances A 65-year-old male whose wife died 2 months ago and he reports a 3-week history of generally depressed mood, guilt about his wife’s death, insomnia, difficulty focusing on daily tasks, with increasing thoughts of dying A 72-year-old female who just relocated across country to live with her adult son and daughter-in-law who is despondent about leaving her home and reports forgetfulness, loss of appetite, new onset bowel problems, and extreme loss of energy3 www.OnlineNursingPapers.com Question 6 A variety of pharmacologic agents have demonstrated effectiveness in the treatment of post-traumatic stress disorder. Which of the following does not have any evidenced-based support in the literature? SSRIs TCAs Antiadrenergics Antipsychotics Question 7 The PMHNP is on call at the local county correctional facility. He is asked to evaluate M.S., a 21-year-old male who was just arrested following an altercation at a local bar. M.S. has never been incarcerated before and apparently has no psychiatric or medical history available. His toxicology screen was negative for alcohol or any drugs of abuse. His mother says that he has in the past had some occasions when he got kind of agitated, but this is the first time it’s been a problem. Reportedly some people from his office were at the bar celebrating a birthday, and before anyone knew what happened an argument escalated into M.S. getting very loud, yelling, and acting ―crazy‖ before he punched a coworker and started breaking bottles. When considering a manic or hypomanic episode, the PMHNP expects that his speech would most likely be: Stuttered Increased Childlike Confused Question 8 Fletcher is a 29-year-old male referred for court-ordered counseling. He has a long history of repeated offenses including DUI, domestic violence, battery, and other violent acts that fortunately have not yet caused any serious injury or death to the recipients. An interview with his wife reveals that he has lied about almost everything for the4 www.OnlineNursingPapers.com last few years; he is able to get hired for jobs because he is very engaging and likeable, and then invariably he gets fired because he misses work and doesn’t do his job properly when he is there. According to the wife, they have known each other since high school, where Fletcher was very happy and well-adjusted. He was on the soccer team, liked by teachers, and never demonstrated the tendencies he does now. Apparently in college he got involved with a fraternity that was notorious for alcohol and drug abuse, and he started drinking heavily; it was ―all downhill from there.‖ The PMHNP considers that: History and symptoms are most consistent with antisocial personality disorder Fletcher needs a neurological workup to include an EEG and assessment for neurological soft signs Consistent with his symptoms, Fletcher will likely respond well to a stress interview It is likely that substance abuse is the underlying cause of symptoms and should be explored further Question 9 Which among the following neurotransmitters is decreased in depression and increased in mania? Dopamine Norepinephrine Serotonin Glutamate Question 10 Among the various types of therapeutic intervention for patients with borderline personality disorder, which of the following is characterized as polymodal, including group skills training, individual therapy, telephone consultation, and a consultation team with a goal of improving interpersonal skills and decreasing self-destructive behavior? Mentalization-based treatment (MBT) Transference-focused psychotherapy (TFP)5 www.OnlineNursingPapers.com Countertransference-focused psychotherapy (CTFP) Dialectical behavioral therapy (DBT) Question 11 Mr. Kendall is a 47-year old male who is presented to care by his younger sister, Megan. Mr. Kendall has spent his entire adult life living in an apartment that was attached to his parents’ home. His mother died a few weeks ago, and the property is listed for sale. Mr. Kendall will have to move, and while discussing this with him, Megan became very concerned. He has apparently been considered odd all his life, has never married or even dated as far as Megan knows, but she had no idea how odd he was. When his mother died, he seemed disconnected from reality and had episodes of talking to people who weren’t present. Megan says that sometimes she does not even understand what he is talking about. He seems to think he has psychic powers, and that he doesn’t need to move because he knows the house will not be sold. When considering a diagnosis of schizotypal disorder, the PMHNP expects which of the following to be present in the history? A history of schizophrenia of a first-degree relative Sustained psychosis predating his mother’s death Comorbid Asperger’s syndrome Apparent frank thought disorder Question 12 Which of the following is a true statement with respect to the treatment of narcissistic personality disorder?6 www.OnlineNursingPapers.com Psychoanalytic psychotherapy has strong empiric support Both serotonergic drugs and lithium are useful Group therapy is rarely helpful Immobilized patients (hospitalized or incarcerated) have the best outcomes Question 13 While preparing a class on personality disorders for a class of PMHNP students, the instructor is presenting case studies of patients with cluster A personalities. One of these cases is Clark M., a 41-year-old man who is described as a life-long ―loner.‖ In high school and college, he kept to himself, excelling in his studies in the sciences. Currently described as a brilliant computer programmer, he clearly prefers solitary pursuits and the company of his cat over people. He knows he is socially isolated, but he is just more comfortable this way. This description is most consistent with: Schizoid personality disorder Schizotypal personality disorder Paranoid personality disorder Delusional disorder Question 14 Darius is a 26-year-old male who presents for care as part of couple therapy with his wife, who is being seen for dependency issues. Darius himself seems very anxious to ―do the right thing‖ and appears to want to please the therapist. During the evaluation, Darius is impeccably dressed, very formal in his presentation and interaction, and is watchful of time because he has an appointment after the interview and states several times that he cannot be late. The PMHNP considers that Darius may have obsessive compulsive personality disorder (OCPD). In differentiating this from obsessive compulsive disorder (OCD), she explores his history further for: A history of racing thoughts Difficulty interacting with others Extremely high expectations of self Significant impairment at work7 www.OnlineNursingPapers.com Question 15 Hugo is a 39-year-old male who has encouraged his wife to come to counseling because he is worried about her wine drinking. Hugo says that he and his wife have shared a bottle of wine with dinner most nights for the last couple of years, but in the last few months he has become worried that she drinks too much. They both agree that she never really becomes intoxicated, but he does not like the fact that evening wine has become the most important part of her meal. If he wants to go out, she will only go to a place that has a wine she likes. Last month they went on a week-long vacation, and she insisted on packing enough of her wine to last the whole time. If they go to a restaurant that does not have a wine she likes, she will take her own in a disposable coffee cup. It seems like for the last few months, she has been drinking more and more, occasionally finishing the bottle alone when he doesn’t want any. Both partners agree that there is no interference with work or any activities or responsibilities, but it is causing some tension in their marriage. When considering a diagnosis of substance use disorder, the PMHNP considers that: Hugo’s wife meets diagnostic criteria for this disorder A trial period with no wine ingestion is necessary to assess for withdrawal symptoms The family history should be assessed for genetic tendency Hugo may have unreasonable expectations Question 16 When developing a pharmacologic treatment plan for the management of major depressive disorder, the PMHNP counsels the patient that the medication will be titrated up to the appropriate dose and then continued for a minimum of 3 months; medication must not be stopped abruptly or without provider supervision. This is because the physiologic consequence of abrupt cessation is likely to result in: Antidepressant discontinuation syndrome Rebound depressive symptoms A manic or hypomanic episode Unresponsiveness to medication with future episodes8 www.OnlineNursingPapers.com Question 17 Which of the following is a true statement with regard to the etiology of substance abuse? Neurotransmitters or receptors have been identified with most substances of abuse except for alcohol Twin and sibling studies do not support a genetic component with respect to the etiology of substance abuse Substances of abuse decrease activity in the amygdala and anterior cingulate The WHO schematic of drug use and dependence identifies immediate antecedents as the central element of abuse Question 18 Assessment of the manic state in a patient with bipolar disorder is likely to include all the following except: Mood-congruent delusions of grandeur Suicidal or homicidal ideation Impaired judgment with no insight Unrestrained flow of ideas Question 19 When performing a psychiatric assessment of an elderly patient with Alzheimer’s dementia, the PMHNP recognizes that: An important part of the history will come from the caregiver The patient must also be interviewed alone to preserve privacy of the relationship A sexual history is not necessary in patients who are not sexually active All of the above.9 www.OnlineNursingPapers.com Question 20 Jeffrey T. is a 27-year-old man who has presented for care after being required to do so by the county court. He was involved in a car accident, and while he was not at fault for the accident, routine blood alcohol screening revealed that he was driving while intoxicated. He is a bit resentful at being required to attend therapy; he is very vocal that his driving was not impaired and that he is able to function normally even after drinking what others might consider excess amounts of alcohol. His wife confirms this; they both admit that what began as one or two beers after work a few years ago has evolved to where he now drinks at least a 12 pack of beer nightly. Regardless, they both confirm that he never ―seems drunk,‖ and this does not interfere with his job or fulfilling his family functions. Jeffrey’s ability to function normally despite high blood alcohol is likely a result of: Dependence Abuse Adaptation Addiction Question 21 Danielle is a 31-year-old female who is having a psychiatric evaluation at the insistence of her husband. They have been married for 4 years, and her husband has finally become so frustrated by her jealous behavior that he threatened to leave her if she didn’t ―get help.‖ Her husband insists that he has never been unfaithful, but Danielle repeatedly accuses him of having an affair. If he is even a few minutes late getting home from work, she demands an explanation and then does not believe anything he says. She does not have any real friends—her sister is her closest social contact, but Danielle has been angry with her for several weeks and won’t answer phone calls. Reportedly she does this often, and according to her husband can ―hold a grudge forever.‖ During the interview, Danielle is calm, responsive, but distant. She says she really doesn’t understand why she is there—there is not a problem. The PMHNP considers the most likely diagnosis and discusses with Danielle that the treatment of choice is: Diazepam Pimozide Psychotherapy Group therapy10 www.OnlineNursingPapers.com Question 22 Margo is a 47-year-old female who admits to a history of fairly heavy alcohol use over many years. She admits that she has had periods in the past where she stopped drinking for a brief time, but she has always gone back to it. At this point she says she has been drinking a fifth of bourbon every 2–3 days for over a year. She has a new boyfriend and really wants to stop drinking, but she is afraid she will ―go into the DTs.‖ She has been reading about it on the Internet, and she knows it can be fatal. Other than her drinking, Margo is amazingly healthy. She had a complete physical exam with blood work through her primary doctor, and he says that her drinking does not appear to have affected her physical health at all. While counseling Margo about alcohol withdrawal delirium (delirium tremens), the PMHNP advises Margo that: She should be admitted for inpatient detoxification People in good physical health rarely have DTs A beta adrenergic antagonist medication can minimize her risk of DTs Women rarely experience DTs Question 23 Anthony is a 41-year-old male patient who presents for evaluation. His wife made the appointment because she is worried about him and he would not seek care on his own. Anthony has become progressively withdrawn over the last few months and is in danger of losing his job because he misses so many days. He has been evaluated by his primary care provider and has no apparent medical conditions. His wife reports that he has been diagnosed with depression in the past, and has even taken medication that seemed to help. This time he just refused to pursue care. After a comprehensive assessment, the PMHNP diagnoses the patient with major depressive episode with psychotic features. Consistent with the Texas Algorithm Medication Project (TAMP), the appropriate choice of initial medication therapy would be: Venlafaxine and clozapine Fluoxetine and olanzapine Amitriptyline and haloperidol Paroxetine and buspirone Question 2411 www.OnlineNursingPapers.com Marlene is a 35-year-old female who is in therapy primarily to develop coping mechanisms for living with her husband, who has narcissistic personality disorder. She is committed to the marriage and loves her husband, but finds his inflated sense of self-importance and complete lack of empathy to be especially difficult. She believes he has a good side, but most of her friends have only ever seen extreme arrogance, and she is embarrassed by that. While counseling Marlene, the PMHNP advises her that patients with narcissistic personality disorder have extremely fragile: Sense of self-importance Defense mechanisms Self-esteem Interpersonal relationships Question 25 Marie is a 30-year-old woman who presents for follow-up after starting treatment for bipolar disorder. She had been treated on and off for depression for years and had a history of alcohol abuse. After her marriage, she decided to stop drinking and was successful in eliminating alcohol from her life; unfortunately, she then went on to have a manic episode and was finally started on a mood stabilizer 1 month ago. She tolerated medication very well, and within 2 weeks symptoms were much improved. Now, 4 weeks later, she feels much better and wants to come off medication. The PMHNP tells her that: Discontinuing medication presents a marked risk of return to alcohol A program of psychotherapy should be started before stopping medication She needs to continue medication for a minimum of 3 months Cessation of mood stabilizers prematurely increases risk for a depressive episode Question 26 Validated and reliable instruments are an important part of assessment for both clinical practice and research in psychiatrics. Which of the following tools is currently considered the standard for assessing clinical outcomes in treatment studies of schizophrenia? SCID BPRS PANSS12 www.OnlineNursingPapers.com HAM-D Question 27 Among the various psychotherapeutic techniques available for treating post-traumatic stress disorder, which mechanism achieves its effect by having patients work through the traumatic event while in a deep state of relaxation? Eye movement desensitization and reprocessing therapy Implosive therapy Systematic desensitization Relaxation and cognitive techniques Question 28 A 22-year-old male patient is started on sertraline 50 mg p.o. daily after presenting with a major depressive episode. After tolerating without difficulty for 2 weeks, his dose is increased to 100 mg p.o. daily. Approximately 4 weeks later he reports an unusual set of new symptoms for the last week and a half. He says he feels ―amped up‖ and just very generally agitated and nervous. He was short-tempered at work and home and was snapping at people for no good reason. He also reports difficulty concentrating at work. Last week he expressed disproportionate anger at his work and his boss told him that he was bipolar and should be put on medication. The PMHNP discusses with the patient that: When symptoms are preceded by antidepressant therapy, a diagnosis of bipolar does not apply His symptoms may be consistent with bipolar disorder if they persist for at least 2 weeks A formal assessment of the social and occupational implications of his symptoms should be performed The symptoms are most likely a physiologic adaptation to the sertraline and most often normalize13 www.OnlineNursingPapers.com Question 29 The PMHNP is seeing a patient who has been referred by primary care. The patient was diagnosed with major depressive disorder and trialed on both an SSRI and SNRI by the primary care provider. The patient appears refractory to therapy and has not had any appreciable clinical response. A more detailed psychiatric history is significant for indicators of bipolar disease, as well as a family history of bipolar disease in both the patient’s father and paternal aunt. This patient will most likely benefit from: Lamotrigine Valproic acid Lithium Amitriptyline Question 30 Mariel is a middle-aged woman who is referred by her primary care provider for management of agoraphobia. Mariel has had this fear as long as she can remember, but now that her children have moved away from home she will need to be more independent and is very committed to trying to manage her fear. The PMHNP counsels Mariel that the most successful therapy for phobic disorders is: Insight-oriented psychotherapy Behavior therapy Virtual therapy Pharmacotherapy Question 31 Cannabis intoxication delirium is characterized by all of the following except: Impaired memory Perception14 www.OnlineNursingPapers.com Psychosis Motor coordination Question 32 Tim is a 20-year-old male who has been referred for care by his college counselor. The counselor has noted that Tim engages in virtually no social activities in college, and for that matter avoids day-to-day activities that require social interaction. By his own admission, Tim never participates in class discussions, even in online discussion boards. Tim is so afraid of rejection that he confines himself to his room and his studies. When differentiating schizoid personality from avoidant personality, the PMHNP knows that a primary difference is that: Avoidant personalities have a strong desire for personal relationships Avoidant personalities may have an active fantasy life Schizoid personalities are perceived as distant and aloof Schizoid personalities may be very attached to animals Question 33 Cory J. is a 23-year-old male being seen by the PMHNP today for an initial evaluation. He says that he does not think anything is wrong, but his family, including his mother, grandmother, and aunt, have all told him that he must be ―mentally ill.‖ He has been unable to hold a job and has worked as a cook at more than five chain restaurants in the last 6 months. He has no real friends—he says his ―friends‖ only call him when they need something but never help him. He is currently staying with his grandmother but reportedly will soon be homeless ―unless things change.‖ While he is telling his story, the PMHNP appreciates that Cory repeatedly includes details that make it hard to understand his point. When asked why he thinks he will be homeless, he responds by talking about how many hours he has worked and how everything was going well but then his car broke down and he couldn’t afford to fix it because his tax return was held by the IRS. The PMHNP recognizes that this represents an abnormal: Affect Cognition Thought process Abstract reasoning15 www.OnlineNursingPapers.com Question 34 Cory is a 23-year-old male recently incarcerated in the county correction facility for a 9-month sentence following his third conviction for battery. As part of an early release program, he is required to participate in the therapy program. During his initial interview, he is very pleasant and engaged, expressing no anxiety or distress with his current circumstances. His psychiatric history is significant for numerous adolescent episodes of running away, truancy, and substance abuse. As a young adult, he reportedly has not held a steady job but rather is constantly coming up with money-making schemes. According to family reports is a personality disorder are very likely to: Have a family history of the same disorder Respond well to dialectical behavioral therapy Have impaired emotional defense mechanisms Come from smaller nuclear families Question 35 Mrs. Maxwell is a 75-year-old patient with moderate Alzheimer’s dementia. She lives with her son and his wife and generally does very well with her day to day activities. The family understands the importance of routine and Mrs. Maxwell maintains a regular schedule of activities including her meals, timed toileting, and recreational activities. Which of the following behaviors should prompt and immediate depression screening for Mrs. Maxwell? An acute change in mental status Angry verbal outbursts that seem unwarranted Death of her best friend An unplanned weight loss despite consistent oral intake Question 3616 www.OnlineNursingPapers.com The psychological sciences have contributed theoretical foundations to the etiology and management of anxiety disorders from both conceptual and practical perspectives. The concept that anxiety develops in persons who feel as though they are living in a world devoid of meaning is an example of which theoretical foundation? Psychoanalytic Behavioral Existential Cognitive Question 37 Mrs. Bowen is a 33-year-old female who presents as a new patient requesting medication for depression. She reports a long history of mood disorders on and off going back to adolescence. She is very articulate in describing her history and reports that neither sertraline nor fluoxetine ―worked for her.‖ She was unable to remember the dose or how long she took the medication. With respect to considering Mrs. Bowen’s medication history, the PMHNP knows that: An SNRI will likely be the most appropriate choice if pharmacotherapy is indicated for this episode This may be an inaccurate characterization, as depressed patients tend to overemphasize negatives In some circumstances patients will purposefully mischaracterize the efficacy of medications they feel were ineffective Some forms of recurrent depression are best managed with nonpharmacologic strategies Question 38 Dependence is a common feature of many psychiatric disorders. One of the primary distinguishing features that differentiates dependent personality disorder from histrionic and borderline personalities is that: The treatment of dependent personality is rarely successful Occupational dysfunction is rarely impaired Dependent personalities tend to have long-term relationships with one person17 www.OnlineNursingPapers.com This disorder tends to be more common in men Question 39 M.T. is a 39-year-old female being seen by the PMHNP for a major depressive episode. She is being managed with SNRI therapy in combination with cognitive behavioral therapy. She is having difficulty achieving remission, and her husband comes with her to this office visit because he is becoming very frustrated. He wants to be supportive, but he is finding it very difficult to understand why she is so depressed. M.T. had an episode of depression approximately 2 years ago, but that was when her sister died in an accident. After 6 months of treatment, she seemed to return to normal. This time, her husband points out that she ―has nothing to be depressed about,‖ but she has become so depressed that she has essentially withdrawn from the family. In trying to help M.T.’s husband understand the disease process, the PMHNP discusses with him that: The physiologic stress accompanying her first episode of depression may have produced changes in brain biology that makes her susceptible to subsequent episodes without an external trigger The pharmacotherapy required to achieve remission with her first episode resulted in neuroplastic changes that increased her likelihood of experiencing additional depressive episodes The scientific literature suggests that the loss of a sibling is the life event most closely associated with recurrent episodes of major depressive disorder throughout adulthood Response to pharmacotherapy often takes a minimum of 8 weeks and that M.T. is much more likely to achieve remission if he can continue to provide the necessary support throughout her remission period. Question 40 Becci is a 31-year-old female who presents to the PMHNP for evaluation after being referred by her friend who is a patient of the practice. She describes a relatively acute, recent onset of panic attacks. Becci says that ―out of the blue‖ her heart starts to race, her mouth gets dry, she gets shaky, and feels like she cannot get her breath. She is afraid because her friend has panic disorder and Becci knows that before her friend got treatment, she basically would not leave the house in case an attack happened. The PMHNP recognizes that the immediate priority in assessment for Becci is: A thorough physical examination A family history of mental health disease A urine drug screen18 www.OnlineNursingPapers.com An assessment for phobic disorder Question 41 The difference between a manic and hypomanic episode is best characterized by all the following except: The duration of symptoms is shorter for hypomanic episodes Hypomanic episodes do not cause marked impairment in function There are no psychotic features with hypomanic episodes Hypomanic episodes may occur as a response to antidepressants Question 42 Janel is a 37-year-old woman who is being interviewed as part of a family assessment. Her 10-year-old son is having some behavioral issues in school and has been referred for evaluation. While interviewing Janel, the PMHNP appreciates that she appears very emotional. She expresses extreme distress at her son’s behavior and says she will do anything to help him; they are ―best friends.‖ She is very demonstrative during the assessment and seems unhappy when she is not the center of attention during the evaluation process. She repeatedly talks about her own medical problems, such as recurrent headache and abdominal pain, which her doctors cannot diagnose. Her appearance is very flamboyant, and her dress is more appropriate to a nightclub than a family assessment. In addition to managing her son’s needs, Janel would likely benefit from: Pharmacotherapy Psychoanalytic psychotherapy Transference-focused psychotherapy A stress interview Question 4319 www.OnlineNursingPapers.com The PMHNP is asked to evaluate the parent of one of her existing patients, a 49-year-old woman named Sheri. Sheri reports that her father, a 78-year-old man who lives alone, has always been in good health. However, when Sheri went to have breakfast with him this past Sunday, she found her father overtly confused and he did not even seem to recognize her at first. Sheri is concerned that he has Alzheimer’s disease, and she is amazed because two days prior he was ―completely fine.‖ The PMHNP knows that the most likely cause of this presentation is: Urinary tract infection Mild cognitive impairment Normal pressure hydrocephalus Depression Question 44 In documenting a mental status exam (MSE) for Janet, a 54-year-old female, the PMHNP notes that she is bradykinesic, has poverty of speech, is depressed, and appears flat. This includes all the following elements of physical examination except: Appearance Motor activity Mood Affect Question 45 Jen is a 31-year-old female who presents for care complaining of depressed mood. During the interview, it becomes apparent that she has a long history of depressive symptoms, as well as a long history of being socially isolated and feeling generally inadequate. When considering a diagnosis of dysthymia, the PMHNP considers that the core concept of dysthymia refers to sub-affective or subclinical depressive disorder with all of the following except:20 www.OnlineNursingPapers.com Low-grade chronicity for at least 2 years Insidious onset, usually in childhood or adolescence Strong family history of depression and bipolar disorder Long asymptomatic periods between episodes Question 46 Which of the following personality disorders is associated with females with fragile X syndrome? Borderline Narcissistic Dependent Schizotypal Question 47 The PMHNP is evaluating Jared, a 47-year-old male who is brought to care by his wife because ―he’s not the man I married 20 years ago.‖ According to his wife, she and Jared have been married for 20 years, have two children, and have lived a ―normal‖ life. Jared owns a local construction company and their marriage has been a solid one, characterized by the typical day-to-day issues that occur in most marriages, but otherwise happy. For the last 2–3 months, she says Jared has completely changed. He will get angry for no apparent reason and even broke a lamp once. He tells stupid and offensive jokes that no one else thinks are funny, and even had someone call the police when he continued to make inappropriate remarks to a woman in a restaurant. Jared seems unsure what to say, but his wife is adamant that this is a totally different man from the one she has known. The PMHNP knows that Jared should be evaluated for: Borderline personality disorder Structural brain damage Substance abuse disorder Cognitive impairment21 www.OnlineNursingPapers.com Question 48 Trudy L. is a 29-year-old female patient who initiated care because she feels like she has no energy. She just had her annual wellness exam and her primary care provider told her that she is in excellent health. Because she complained about this excessive fatigue, her PCP performed a CBC, CMP, UA and thyroid function tests and was told, along with her physical examination, that everything looks normal. Further discussion reveals that Trudy is having some relationship challenges with her boyfriend of 2 years and this seems to be ―spilling over‖ at work, where she is having persistent conflict with her supervisor. Ultimately the PMHNP diagnoses Trudy with major depressive disorder, mild, single episode. The PMHNP and Trudy discuss treatment options, and Trudy would really like to try nonpharmacologic interventions. Which of the following represents the best approach for Trudy? Family therapy Behavior therapy Psychoanalytic therapy Interpersonal therapy Question 49 Maurice is a 22-year-old male who is being treated for major depressive episode. He presents today for a follow up visit. He was started on sertraline 50 mg daily 4 weeks ago, and 2 weeks ago, his dose was increased to 150 mg daily. Today he is concerned because he doesn’t really feel much symptom improvement, and he thinks he needs something else. The best response to Maurice is to tell him that: He needs to be increased to 200 mg today and follow up in 4 weeks He should maintain this dose for 4 weeks and reassess He should change his therapy to an SNRI Addition of cognitive behavioral therapy would likely improve response22 www.OnlineNursingPapers.com Question 50 Depressive personality disorder exists along the spectrum of dysthymia and major depressive disorder, but it is different from these two in that: Pharmacologic treatment is not indicated The etiology is different Perfectionism is common Physical symptoms are lacking Question 51 Karen is a 19-year-old female who has been referred to care after being seen in the emergency department following a violent sexual assault. She was working late one evening at the shopping mall and walked alone to her car after dark. She was assaulted, beaten, and thankfully a passerby saw her lying in some bushes and called 911. Initially she was resistant to mental health care, but now, 2 months later, she feels as though she needs help because she is experiencing a collection of symptoms including flashbacks, dreams of the assault, palpitations, anxiety, and a sense that she is watching the assault happen to her This sense of watching the assault as if she was an observer is characteristic of which diagnostic domain of PTSD? Intrusion symptoms Avoiding stimuli Autonomic arousal Clinical significance23 www.OnlineNursingPapers.com Question 52 Melissa is a family nurse practitioner who is enrolled in a PMHNP program and is beginning her first clinical rotation. After being oriented to the practice processes and procedures, she is preparing for her first solo interview of a patient who is presenting to the practice to establish care. Melissa knows that, unlike her experience as a primary care nurse practitioner, the first office visit with a psychiatric patient should be: At least 90 minutes Person-centered Comprehensive Insight-oriented Question 53 The International Study of Expert Judgment on Therapeutic Use of Benzodiazepines and Other Psychotherapeutic Medications was designed to gather systematic data on the opinions of leading clinicians concerning the benefits and risks of benzodiazepines and alternative anxiety treatments. Which of the following best characterizes the majority opinion of this group? Patients who require long-term benzodiazepine management should be maintained on long-acting agents The use of benzodiazepines long term for anxiety does not pose a high risk of dependence and abuse The panel supports increased federal and/or state restrictions on benzodiazepine prescribing When detoxifying from therapeutic dosages, daily intake should be decreased by 10–25% Question 54 Differentiating post-traumatic stress disorder (PTSD) from panic disorder and generalized anxiety disorder can be challenging. Which of the following provides the strongest support for PTSD vs the other two differential diagnoses? The time course of symptoms Presence of physiologic arousal Reexperiencing the event24 www.OnlineNursingPapers.com Response to pharmacotherapy Question 55 John is a 41-year-old male who presents for management of heroin addiction. He has a long history of opiate abuse spanning decades and has had several unsuccessful attempts at recovery. Because of his lifestyle, he has developed a variety of chronic health problems, including cardiomyopathy and stage 2 chronic kidney disease. He currently takes several psychiatric medications for mood disorder. When considering methadone maintenance as a mechanism of treating his opiate addiction, the PMHNP knows that if he requires more than 100 mg of methadone at the start of therapy he should have a baseline: Urine drug screen Hepatic function test Pulmonary function test 12-lead ECG Question 56 During the interview of Kevin, a 42-year-old male who presents for treatment because of marital problems, the PMHNP responds to his tears by gently moving a box of tissues toward him. This is a facilitating intervention of interview known as: Reinforcement Reassurance Encouragement Acknowledgement25 www.OnlineNursingPapers.com Question 57 When evaluating the laboratory assessment of a patient with alcohol use disorder, the PMHNP may reasonably expect to find all of the following abnormalities due to chronic alcohol use except: Macrocytosis Transaminitis Uremia Hypertriglyceridemia Question 58 Mr. Henderson is a 69-year-old man who presents for evaluation and care for depression. His wife died 6 months ago following a difficult 2 years with breast cancer. His primary complaint is that he just does not look forward to anything anymore. He cannot get interested in his children and grandchildren, he no longer enjoys any of his hobbies because he and his wife used to do them together. He does not sleep well, and wakes up frequently during the night. He also admits to thinking more and more about dying himself, although he expressly denies suicidal ideation. His medical history is significant for coronary artery disease, osteoarthritis, hypothyroidism, hypertension, and dyslipidemia. He also has atrial fibrillation and is on warfarin for emboli prophylaxis, but he does not remember the names of all of his other medications. When considering pharmacotherapy for Mr. Henderson, the PMHNP considers that which of the following SSRIs is safest with respect for potential drug interactions? Fluoxetine Paroxetine Escitalopram Sertraline Question 59 The PMHNP is called to the acute care unit to evaluate a patient who is admitted after being brought in by his friends. They were at a party where there were numerous drugs of abuse as well as alcohol. The patient cannot provide a history, and his friends are unclear as to which drugs he used. Physical examination reveals a patient who is diaphoretic, tremulous, has a pulse of 130 bpm, dilated pupils, and cannot perform fine motor tasks. These physical findings are most consistent with which type of intoxication?26 www.OnlineNursingPapers.com Alcohol Cannabis Opiate Hallucinogen Question 60 Kevin is a 24-year-old male who seeks treatment for anxiety. He thinks he has an anxiety disorder because he has a lot of the same symptoms that his mother does, and she takes medications for anxiety. He reports being ―constantly wired,‖ irritable, and not sleeping well. Kevin says he always has energy, but it’s not a good kind of energy. He does not have isolated panic attacks; he is always just ―amped up.‖ He denies any substance abuse, and he does not smoke cigarettes. When considering organic causes of his symptoms, the PMHNP must evaluate his: Caffeine intake Use of dietary supplements Testosterone level Liver function tests Question 61 From a biological perspective, all of the following neurotransmitters are implicit in the anxiety response except: Gamma-aminobutyric acid Norepinephrine27 www.OnlineNursingPapers.com Serotonin Dopamine Question 62 Laura T. is a 27-year-old female who has been referred for psychiatric evaluation. She has no significant psychiatric or medical history and denies any history of substance abuse, but she is here because she is persistently having olfactory hallucinations. For the last 3 months, she has been having this progressive sense of smelling particularly foul odors—feces, rotting food, trash— with no obvious cause. She made the appointment because she had an uncle who had schizophrenia and he used to have hallucinations too, although he was mostly hearing voices. The PMHNP knows that a priority of assessment includes a: BPRS Toxicology screen Head imaging Family history Question 63 Marcus is an 18-year-old male presented for care by his parents. It is time for Marcus to begin exploring colleges and he flat out refuses to do so. Both Marcus and his parents admit that he has had a rather solitary lifestyle. He has been home-schooled since the eighth grade. According to his parents, he is extremely intelligent and in junior high it became very difficult for him to be in school. He was very uncomfortable in the school setting and it was counterproductive to learning, so the parents were amenable to home schooling. However, now they want him to go to college, but he will not discuss it. When considering differential diagnosis, the PMHNP considers all of the following except: Schizophrenia Social anxiety Schizoid personality Agoraphobia28 www.OnlineNursingPapers.com Question 64 Chantel is a 19-year-old female who presents for care because she thinks she is bipolar. During her initial interview, she admits that she has a long history of feeling like she was the person in the family of whom there were always high expectations, and she was never able to express concerns or feelings of inadequacy. When asked why she thinks she is bipolar, she says she gets very moody. She was at the grocery store last week and slipped and fell. While waiting for help, she could not control her anger and reached up to swipe all the food off of the shelves. She has been fired from jobs because of her uncontrollable temper; she sometimes ―just can’t be around certain people.‖ Chantel also reports that at times she will go two full days and nights being unable to sleep, and that her mind keeps racing and she can’t ―shut it down.‖ When this happens, she just gets up and does things around the house. Finally, Chantel reports that she cannot hold onto money at all. Whenever she gets a paycheck, she immediately spends it on things that she acknowledges she doesn’t even need. When considering a diagnosis of bipolar disorder, the PMHNP specifically assesses for: Any history of suicidal attempts or serious ideation History and current patterns of substance abuse Concomitant psychotic features such as hallucination or delusion Manic symptoms that are sustained most of the day for at least 2 weeks Question 65 Joe W. is a 28-year-old male who is currently having an acute manic episode. He has not slept for 3 days, is extremely irritable, and is prone to violent outbursts of anger. He reports what is clearly a sustained episode of racing thoughts and has experienced psychotic episodes. According to his history, Joe has been on mood stabilizing medication in the past, but he is very unreliable when it comes to follow-up. When considering medication therapy for Joe, the PMHNP knows that: Lithium carbonate is the drug of choice for Joe Joe would be best managed with injectable antipsychotics Risperidone is an appropriate choice when mania is characterized by anger and violence Symbyax (olanzapine/fluoxetine) is the safest choice for Joe given his psychosis29 www.OnlineNursingPapers.com Question 66 The professional relationship between therapist and patient with schizoid personality disorder is a challenge because these patients do not typically seek care independently. However, once a trusting relationship develops, this type of patient may: Reveal a very strong desire for an intimate relationship Become very engaged in group therapy Describe an active fantasy life with imaginary friends Demonstrate psychotic or delusional features Question 67 Patients on lithium carbonate for management of bipolar disorder should be subject to routine assessment of: CBC and BMP TSH and serum Na+ CMP and ECG LFTs and EEG30 www.OnlineNursingPapers.com Question 68 The PMHNP is preparing a presentation for a primary care conference on geriatric health care. The topic is geriatric depression, and this presentation is designed to increase recognition of community-dwelling elders at risk. An important talking point in this presentation will include all of the following about geriatric depression except: Depression presents with more somatic symptoms as compared to younger age groups Ageism may cause primary care clinicians to accept depressive symptoms in the elderly as normal Risk factors include loss of spouse, physical illness, and social isolation Incidence of geriatric depression is estimated at 60–75% of the population Question 69 When differentiating a major depressive episode from dysthymic disorder, the PMHNP considers that: The cognitive theory of depression does not apply to dysthymia Hospitalization is typically indicated early in the course of dysthymia Dysthymia is more subjective in its presentation than depression Insight-oriented therapy is the most effective treatment for dysthymia Question 70 Sarah is a 23-year-old patient who presents for a follow-up of her major depressive episode. She was titrated up to maximal dose fluoxetine 6 weeks ago after demonstrating tolerance without side effects at lower doses. Today in follow-up, she reports that she still has no sides effects but no therapeutic effect either. There does not appear to be any measurable improvement of her initial presenting symptoms. The PMHNP knows that the most appropriate approach at this point is to: Reconsider the diagnosis of major depressive episode Add bupropion to her medication regimen31 www.OnlineNursingPapers.com Increase the dose of fluoxetine Change to another antidepressant medication Question 71 The PMHNP is working on a graduate program in which he is hoping to develop a new personality assessment tool. After an exhaustive review of the literature and many months of work, he developed a tool to use in a research study and needs to establish its psychometric properties. He distributes the tool to four different professionals in the field and asks that they assess whether the questions appear to measure what they are purported to measure. This is an assessment of: Internal consistency reliability Parallel form reliability Construct validity Face validity Question 72 The PMHNP is considering a diagnosis of paranoid personality disorder in a new patient. When reviewing the history and physical examination, which of the following findings would be most consistent with this diagnosis? The presence of fixed delusional thought Disdain for weak or sickly people A history of antisocial behavior Extreme ―drama‖ in most personal relationships32 www.OnlineNursingPapers.com Question 73 The major defensive mechanisms employed by patients with histrionic personality disorder include: Repression and dissociation Projective identification Fantasy and isolation Splitting Question 74 The PMHNP is considering pharmacotherapeutic options for Ana, a 28-year-old female with generalized anxiety disorder. Ana is very concerned about becoming ―addicted‖ to medication, but she is open to pharmacotherapy because there are a lot of things going on in her life and she worries all the time. Her husband is deployed overseas, she has just started a new job, and her only child has just started kindergarten. Ana denies any panic-type symptoms; her primary concern is that she is worried about everything and it is making it hard to sleep and concentrate on learning the skills for her new job. Ana may best benefit from: Lorazepam Venlafaxine Propranolol Buspirone Question 75 Sally is a 54-year-old female who presents for care at the urging of her employer. She says that she doesn’t think she needs to be there, but the manager of her division at work strongly suggested that she make an appointment. She is the evening shift manager in the accounting department of a major online sales organization. Her role requires meticulous accountability of a complex system of production statistics, and she has done this exceedingly well for years. She has been a valued employee, and her work is above reproach. A few months ago, the company adopted a new software program that required a complete revamping of Sally’s department. She has not adapted well, and her resulting anxiety is almost prohibitive of functioning in her role. During her interview, Sally is very somber and serious, and is clearly having difficulty with this change. She is distraught over the potential of not being able to do33 www.OnlineNursingPapers.com her job well and meet her immediate supervisor’s expectations. Recognizing the likely diagnosis, the PMHNP knows that Sally is likely to respond best to: Pharmacotherapy with clonazepam Free-association, nondirective therapy Interpersonal therapy Serotonergic agents [Show More]
Last updated: 1 year ago
Preview 1 out of 33 pages

Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Aug 21, 2020
Number of pages
33
Written in
Additional information
This document has been written for:
Uploaded
Aug 21, 2020
Downloads
2
Views
152






 101 Correct Q & A s_6531_Final_Exam.png)