*NURSING > EXAM REVIEW > ATI FINAL MATERNAL HEALTH EXAM 3 latest (All)
ATI FINAL MATERNAL HEALTH EXAM 3 latest
Document Content and Description Below
EXAM 3 1 ATI FINAL MATERNAL HEALTH EXAM 3 Postpartum Hemorrhage (PPH) From delivery up to 6wks postpartum SVD Spontaneous vaginal delivery: greater than 500ml (considered PPH) o Estimate... d blood loss o Quantitative blood loss (weighing everything) CS C-Section: greater than 1000ml Two main reasons for PPH Full bladder Retained placenta What you will assess when you walk into a patient’s room for PPH 1. Assess Fundus -should always be right at umbilicus If it feels like your cheek: boggy; (massage it) Don’t stop unless it firms up 2. Call for help 3. Call Dr. 4. Meds 5. VS and O2 stat 6. Weigh under pads (add this amount of blood loss to what she lost at delivery 7. Change under pads 8. Empty bladder (foley) 9. Start 2nd IV; may need to give patient blood o Once you start to feel the fundus firm up you can stop massaging o Only thing that can misplace the fundus is a full bladder The uterus has to contract to stop bleeding Meds (all usually standing orders) Pitocin: usually IV sometimes IM every patient after they deliver will get this drug (immediately) o If there is a fetus in the uterus; has to be on pump and is piggybacked o If not given wide open Methergine: given IM; if patient has HTN CANNOT be given this drug Hemabate: given IM; CANNOT give if patient has asthma (can cause explosive diarrhea) Cytotec: rectally; given 800-1000 mcg *Methergine and Hemabate: work within 2-3 minutes If all of this doesn’t work then back to the OR Should be dark brown Firm w/ Bright red blood- lacerationEXAM 3 2 After delivery check every 15 minutes x 4 Every 30 minutes x 4 Oxygen 8-10L Non-rebreather mask Never nasal cannula Menstrual cycle 28, 32, or 36-day cycle 36-day cycle, go back 14 days, she will ovulate on day 22 (can get pregnant on this day) Have sex on the 17th and the 27th Ovulation: go back 14 days from very last day of cycle Sperm lives 3-5 days (200,000,000-800,000,000 per ejaculation) Ova can only be penetrated for the first 24 hrs If you want to get pregnant start intercourse 5 days before or 5 days after ovulation Should have sex every 6 hrs during that time period Progesterone levels decrease signals hypothalamus to anterior pituitary gland to stimulate the follicle stimulating hormone and luteinizing hormone; which increase estrogen and progesterone (~36 hours) Corpus luteum: hole where egg left. increases/produces progesterone; you need increase in progesterone to carry a pregnancy Progesterone levels have to go up in order to hold a pregnancy Placenta takes over hormone level regulation after 6 - 7 weeks * Naegele’s Rule (estimated due date) 1st day of last period (minus) 3 months (plus) 7 days -3 months + 7 days 30 days has September, April, June & November 1st Trimester Conception – 13 6/7 weeks (13 weeks & 6 days) 2nd trimester 14 weeks -26 6/7 weeks (26 weeks & 6 days) 3rd Trimester 27 weeks-40 6/7 weeks (40 weeks & 6 days) Term: 37 weeks or greater 20 weeks gestation when the organs are done being formedEXAM 3 3 G- # of pregnancies T- # of term deliveries P- # of preterm deliveries (20- 36 6/7 weeks) A- # of abortions (less than 20 weeks) L- # of living children Fetus cannot survive before 20 weeks Antepartum o fetus in uterus Prenatal Visit (1st things that need to be checked) Vital signs Estimated Date of Confinement (Estimated Due Date) Medical hx CBC Hep B HIV VDRL- STI Blood type- Rh factor Rubella titters; drawn at prenatal visit (if nonimmune she needs Rubella titters w/in 72hrs after delivery) TB skin test Pap smear Weight UA- urinalysis Fetal heart tones (can be heard at 6 weeks) If mother is Rh-(negative), she needs Rhogam (26-28wks), she needs that because negative antigens may try to fight off pregnancy If mom is negative and baby blood positive; mom needs Rhogam within 72hrs after delivery to protect next pregnancy *Only run babies cord blood to find out blood type if moms blood type is negative Next visits VS Weight UA Fetal heart tones Measure abdomen Office Visits- doctor for normal pregnancies 1 week (conception) - 28 6/7 weeks:EXAM 3 4 o Mom will visit Dr. every 4 weeks 29 weeks- 36 6/7 weeks: o Mom will visit Dr. every 2 weeks 37 weeks and greater: o Mom will visit Dr. every week Changes in Body Systems: Reproductive Uterus o F Cervix o Chadwick signs: bluesish/purplish o Goodell’s sign: cervix softening o Mucus plug: keeps the uterus safe from any germs getting into uterus; can cause some spotting as separating from cervix wall o Hrg’s sign: softening of lower segment of the uterus Vagina and vulva o Increased vascularity o Vaginal mucosa thickens o Vaginal rugae becomes prominent o Increased roiduction Breast o Grow larger o Areola gets darker o Colostrum- thick yellow discharge; body getting ready for breast home Heart Blood o Blood volume increase o Plasma volume increases: o Cardiac output increase Relaxin: o body releases during pregnancy; smooth muscle relaxer; keeps BP normal - Has clotting factors in it Oxygen needs increase o RR will go up about 20% Appetite o increase after 1st trimesterEXAM 3 5 Mouth o gums may bleed, can get gingivitis, ptyalism Esophagus o acid reflux; heart burn Large and small intestines o everything slows down; constipation (moms need to increase fluid intake and fiber) Liver and gallbladder o gall stones Bladder o 1st and 3rd trimester: frequent urination o 2nd trimester: slows down Kidneys and ears o formed at the same time: around 16 weeks; if ear is deformed they will look further at the kidney function of the baby Increase in nutrients in urine o can increase the risk of UTI in mom Hair and nails o grow rapid and thicker Ear o cornea becomes thicker o diminished hearing; increased wax Autoimmune conditions o decrease during pregnancy o after pregnancy condition becomes worst Pituitary gland o Prolactin o Oxytocin: after 36 weeks oxytocin levels go up progesterone starts to go down *Normal for pregnant women to have a trace of glucose in urine o Moms become insulin resistant to make more glucose for baby Conformation of pregnancy: Presumptive (subjective) o AmenorrheaEXAM 3 6 o N/V o Fatigue o Urinary frequency o Breast changes o Vaginal & cervical color changes o Quickening (fetal movement)- flutter of gas Probable (objective) o Abdominal enlargement o Goodell’s sign softening of the lower part of the cervix-soft like your cheek. o Hagar’s sign (softening of the lower uterine segment) o Ballottement- Dr. does a dig vag exam & can push up on cervix. Fetus will go up & come back down o Braxton Hicks pre-contractions ATI o Palpation of fetal outline- Enlarged abdomen o Positive pregnancy test o Chadwick sign-- bluish purple color of the cervix Positive o Fetal heart sounds o Fetal movement detected by provider o Visualization of the embryo or fetus First Trimester Uncertainty Second Trimester Physical evidence of pregnancy Fetus as the primary Narcissism and introversion Body image Changes in sexuality; changes in sex drive Third Trimester Vulnerability Increasing dependence Preparation for birth o Nesting behavior (happen later on; just before labor) Maternal Role Transition Three stages of attachmentEXAM 3 7 o Accepts pregnancy o Baby becomes real; she loves it o Increasing love and vulnerability; mom will do anything she has to do Couvade: where the father goes through the same symptoms as the mom Things to know: o Mom needs 600mcg/day of folic acid o Mom: needs extra calcium o hCG: levels go up when pregnant o Moms should gain 25-35lbs: normal weight gain o Should drink 6-8liters/day o DO NOT ovulate during pregnancy o Never lie a pregnant women supine/flat on back; always needs to have a pillow wedged behind her back Week 2 Notes Effects of the birth process: Maternal Response Variability- (goes up & down) when we look at a fetal monitor strip. We’re always going to look for variability It’s the babies hear beat from beat to beat Absent- 0 BPM Minimal 0-5 BPM Moderate 5-25 BPM—Always want Marked >25 BPM Characteristics of contractions: Coordinated o Frequency Beginning of one uterine contraction to the beginning of the next Range in minutes; how often (ex. 1.5- 2 minutes) Don’t want a frequeny to be any more than 2 min’s lasting about 60-90 sec’s o Duration Beginning of a uterine contraction to the end of the same contraction when it comes back to baseline Range in seconds; how long is last (ex. 60-90 sec’s) Involuntary Intermittent- relaxation of the contraction (we must have this relaxation period, because if not. That means the uterus is not contracting & it’s where the fetus is getting most nutrients & oxygen. During that resting tone)EXAM 3 8 Contraction Cycle o Increment Period of increasing strength o Acme Period during which the contraction is most intense o Decrement Period of decreasing intensity as the uterus relaxes *In-between contractions is where baby gets it oxygen and blood supply that is being sent through the umbilical cord. Want contractions to be about 2 mins apart lasting 60- 90 secs Skinniest to fattest.. shortest to longest.. contraction Fetal Heart Tones Baseline o Where the baby’s heart rate hits the most Accelerations Decelerations o Variable o Early- head compression- close to delivery- they mirror the contractions o Late Variability: BPM (beats per minute)- V Shape or W shape 0-5: absent -minimal 5-25: moderate (what we want) >25: marked 3 Ss (reasons for absent to moderate variability will vary) o Sleeping o Sedated- mom may have been given fentanyl or stadol or any narcotic o Sick (neonates temp will drop) If baby is not any of these- notify HCP Fetal Heart strip Baby heart tone always at top Mom contractions at the bottom Variable (type of deceleration) Cord Compression -Sudden drop with a quick return to baseline -Reposition mom w/in 30 seconds. V or W appearance Early (starts right w/contraction) Head Compression (usually est. 8cm) -mirrors mom contraction -Sterile vaginal exam (find out dilation)EXAM 3 9 - reposition mom Acceleration (above baseline)-lack of baseline Oxygenated -Baby is saying he is ok Late (declaration and contraction don’t match) Placental insufficiency -Baby suffering -Not getting enough oxygen & nutrients Characteristics of late- beginning, middle, & end are off LATE deceleration (what to do) 1. Reposition mom 2. Shut off Pitocin (causes contractions) 3. Increase IV fluids 4. o2 via nonrebreather mask (8-10/L) 5. Sterile vaginal exam- 6. Call provider *Anything goes below baseline; deceleration *Want to see lots & lots of acceleration (when baby moves HR should go up) *NEVER nasal cannula in L&D Accelerated Increase in fetal heart rate 15 beats by 15 beats above baseline (32+weeks) 10 beats by 10 beats above baseline (under 32 weeks) Fetus well oxygenated Uterine body Upper two thirds of the uterus contracts actively to push fetus down Lower one third remains less active Cervical changes Effacement (thinning and shortening: cervix) Dilation (opening) Effacement and dilation occur concurrently during labor bur at different rates *the only soft tissue that can hold a baby up from delivering is a full bladder Placental circulationEXAM 3 10 Most placenta exchange occurs during the interval b/w contractions Components of the Birth Process Five major factors that interact Powers o Contractions o Maternal pushing Passage o Pelvis Passenger o Baby o Placenta o Membranes Baby can’t come out if it’s extended or hyperextended Psyche (how mom feels about pushing) o Anxiety o Culture and expectation o Birth as an experience o Support o Impact of technology Position o Fetal head position o Want baby to be in an anterior position (occipital) OA o OT- occipital transverse Presentation Fetal part that first enters the pelvis Cephalic o Vertex, military, brow, face Breech o Frank, full, footling Shoulder Cephalic Presentation The cephalic presentation is more favorable than others for the following reasons: • The fetal head is the largest single fetal part, although the breech (buttocks), with the legs and feet flexed on the abdomen, is collectively larger than the head. After the head is born, the smaller parts follow easily as the extremities unfold. • During labor, the fetal head can gradually change shape, molding to adapt to the size and shape of the maternal pelvis. • The fetal head is smooth, round, and hard, making it a more effective part to dilate the cervix, which is also round. Cephalic presentation has the following four variations (Fig. 12.8): • Vertex—This is the most common type of cephalic presentation, in which the fetal head is fully flexed. It is called a vertex or occiput presentation and is the most favorable for normal progress of labor because the smallest suboccipitobregmatic diameter is presenting. • Military—The head is in a neutral position, neither flexed nor extended. The longer occipitofrontal diameter is presenting.EXAM 3 11 • Brow—The fetal head is partly extended. The brow presentation is unstable, usually converting to a vertex presentation if the head flexes or to a face presentation if it extends. The longest supraoccipitomental diameter is presenting. C-section • Face—The head is extended, and the fetal occiput is near the fetal spine. The submentobregmatic diameter is presenting. C-section Breech Presentation A breech presentation occurs when the fetal buttocks or legs enter the pelvis first, which happens in approximately 3% to 4% of births. Breech presentation is more common in preterm births, hydrocephaly (enlargement of the head with fluid), multiple gestations, abnormalities of the maternal uterus and pelvis, and with placenta previa (placenta in the lower uterus) (Cunningham et al., 2014). Breech presentations are associated with the following disadvantages: • The buttocks are not smooth and firm like the head and are less effective at dilating the cervix. • The fetal head is the last part to be born. By the time the fetal head is deep in the pelvis, the umbilical cord is outside the mother’s body and is subject to compression between the fetal head and the maternal pelvis. • Because the umbilical cord can be compressed after the fetal chest is born, the head should be delivered quickly to allow the infant to breathe. This does not permit gradual molding of the fetal head as it passes through the pelvis. The breech presentation has the following three variations, depending on the relationship of the legs to the body (Fig. 12.9): • Frank breech—This is the most common variation, occurring when the fetal legs are extended across the abdomen toward the shoulders. • Complete breech—This is a reversal of the usual cephalic presentation. The head, knees, and hips are flexed, but the buttocks are presenting. Full breach- tucked in & flexed but upside down • Footling breech—This occurs when one or both feet are presenting. Shoulder Presentation The shoulder presentation is a transverse lie and accounts for only 0.3% of births (Cunningham et al., 2014). It occurs more often with preterm birth, high parity, prematurely ruptured membranes, hydramnios, and placenta previa. A cesarean birth is necessary when the fetus is viable (one of a gestational age that might survive).EXAM 3 12 Fetal lie Orientation of the long axis of the fetus to the long axis of the woman (baby’s spinal cord to mom’s spinal cord) In more than 99% of pregnancies, the lie is longitudinal and parallel to the long axis of the woman There are 3 lies: vertex, oblique, and transverse. Transverse lie is immediate c-section-horizontal Normal Labor:EXAM 3 13 Premonitory Signs Braxton Hicks contractions Lightening Increased vaginal mucus secretion Cervical changes o Softening o Possible dilation o Bloody show- associated w/ cervical dilation & effacement expected finding Brownish vaginal discharge True Labor Contractions w/cervical change Increased contractions Increased discomfort Cervical change: progressive effacement and dilation most important False labor Contractions inconsistent Discomfort is more annoying than truly painful Cervix does not change Cervix has not shortened Membranes still intact Labor Mechanism- cardinal movements Descent o Movement of fetus through the birth canal Engagement- fetal positioning o Fetal presenting part reaches 0 station o Baby’s head has to be at ischial spine to be considered 0 station o Station- where is babies head according to mom’s pelvis Flexion Internal rotation Extension External rotation Expulsion Stages of Labor 1st stage: 3 phases o Latent phase: 0-3 cm (putting on make-up, doing hair) o Active phase: 4-7 cm (starting to ask for pain meds) o Transition phase: 8-10 cm (no epidural; wants to be left alone, epidural: feeling ok) 2nd stage o 10 cm: delivery of baby 3rd stage o Delivery of placenta (usually happens 20-30mins after)EXAM 3 14 4th stage o First 1-4hrs post delivery The cervix usually hangs down 2cm from the uterus this is 0% effaced. When we can no longer feel the cervix(paper thin) this is 100%. Don’t push until completely dilated and 100% effaced. During labor dilation and effacement occur at different rate Ex. 90% and 5cm A preceptor will have a new nurse close her eyes and put fingers into a plactic mold. The contraction starts at the top of the uterus or fundus- only the top 2/3 of the uterus is active. The lower1/3 is passive. Push ball through the sock to show how the cervix opens. Blood flow to the placenta decreases during a contraction. The muscle fibers of the uterus constrict around the maternal spiral arteries, which supply the placenta. There is a relative increase in the woman’s blood volume. This temporary change increases her blood pressure slightly and slows her pulse rate. • Vital signs are best assessed during the interval between contractions. Supine hypotension (aortocaval depression) may occur during labor if the woman lies on her back. The woman should be encouraged to rest in positions other than supine to promote blood return to her heart. Supine hypotensive syndrome is characterized by severe supine symptoms and hypotension in late pregnancy, which compel the unconstrained subject to change position. Rarely, it may manifest even from the fifth month of pregnancy or postpartum, as well as in the pelvic tilt or sitting positions. Inferior vena cava compression, influenced primarily by the size of the uterus and exact maternal and fetal position, is the major determinant in its development Aortocaval compression is thought to be the cause of supine hypotensive syndrome. Supine hypotensive syndrome is characterized by pallor, tachycardia, sweating, nausea, hypotension and dizziness, and occurs when a pregnant woman lies on her back and resolves when she is turned on her side Maternal resp system Increase depth and rate of respirations (deeper and faster) Hyperventilation It may occur with rapid and deep breathing. Respiratory alkalosis occurs as she exhales too much carbon dioxide. She may feel tingling of her hands and feet, numbness, and dizziness. The nurse should help her slow her breathing and breathe into a paper bag or her cupped hands to restore normal blood levels of carbon dioxide and relieve these symptoms.EXAM 3 15 Umbilical Cord 2 arteries 1 vein Characteristics First Stage Second Stage Third Stage Fourth Stage Work accomplis hed Effacement and dilation of cervix Expulsion of fetus Separation of placenta Physical recovery and bonding with newborn Forces Uterine contractions Uterine contractions and voluntary bearingdown efforts Uterine contraction s Uterine contraction to control bleeding from placental site Cervical dilation Latent phase∗ : 0-3cm Active phase∗ : 4-7 cm Transition phase: 8-10 cm 10cm (complete dilation) Not applicable Not applicable Uterine contractio ns Latent phase: Initially mild and infrequent; progress to moderate strength, every 5min with a regular pattern; duration increases to 30-40sec by end of latent phase Active phase: Increase in frequency, duration, and intensity until every 2-3 min, 40-60 sec, and moderate to strong intensity Transition phase: Strong, every 1½-2 min, 60-90 sec Strong, every 2-3min, lasting 40-60sec; may be slightly less intense than during transition phase of first stage; may pause briefly as second stage begins Firmly contracted Firmly contractedEXAM 3 16 Characteristics First Stage Second Stage Third Stage Fourth Stage Discomfort† Often begins with a low backache and sensations similar to those of menstrual cramps; back discomfort gradually sweeps to lower abdomen in a girdle-like fashion; discomfort intensifies as labor progresses Urge to push or bear down with contractions, which becomes stronger as fetus descends; distention of vagina and vulva may cause a stretching or splitting sensation Little discomfort; sometimes slight cramp is felt as placenta is passed Discomfort varies; some women have afterpains, more common in multigravidas or those who have had a large baby; as anesthesia wears off, perineal discomfort may become noticeable Maternal behaviors† Sociable, excited, and somewhat anxious during early labor; becomes more inwardly focused as labor intensifies; may lose control during transition Intense concentration on pushing with contractions; often oblivious to surroundings and appears to doze between contractions Excited and relieved after baby’s birth; usually very tired; often cries Tired, but may find it difficult to rest because of excitement; eager to become acquainted with her newborn Nursing Care During Labor and Birth Issues for New Nurses Pain associated with birth Inexperience and negative experiences Unpredictability Intimacy Cyclic pain: only hurts with contraction May have experienced negative things Labor follws it’s own course # of labor patients change from one minute to minute Admission to Birth Facility: Number & duration of previous labors Distance from the hospital Available transportation Childcare needs Risk status FIRST PRIORITY IS FETAL WELL BEING!!EXAM 3 17 Nursing Responsibility During Admission Make family feel welcome Determine family expectations Convey confidence Assign a primary nurse Use touch for comfort Respect cultural values Ultrasound transducer for FHT- goes over the fetal back Toco transducer for contractions- goes over the fundus Focus assessment Fetal heart rate o FHR 110-160 o Regular rhythm: presence of acceleration; absence of deceleration Maternal vital signs o Identify signs of HTN and infection o Impending birth o Grunting sounds- tell her to pant- breathe o Bearing down- we don’t want her to push because the doctor is not there o Urgency to push Fern- test that shows if mom has truly ruptured Admission Procedure o Notify the birth attendant Give report Obtain orders o Consent forms- vaginal, c-section, & epidural o Lab tests- CBC & T&S o IV access- for Pitocin after delivery Nursing Responsibility After Admission: Fetal Assessment FHR Amniotic fluid: spontaneous rupture of membranes (SROM) or artificial rupture of membranes (AROM)-looks like a crochet hook Maternal Assessment Vital signs Contractions Labor progress Intake & OutputEXAM 3 18 Response to labor Support person’s response- check on them & see if they’re pale or freezing (give blanket) Nursing Care During the Late Intrapartum Period: Responsibilities during birth o Preparation of a delivery table with sterile gowns, gloves, drapes, solutions, and instruments o Perineal cleansing preparation o Supporting the woman and partner with final pushing efforts o Initial care and assessment of the newborn o Administration of medications (usually oxytocin) to contract the uterus and to control blood loss Responsibilities after birth o Care of the infant Maintaining cardiopulmonary function (Apgar) Support thermoregulation Identify infant o Care of the mother Observe for hemorrhage Promote comfort o Promote early family attachment *Patients water breaks spontaneously: very first thing to do is check fetal heart rate Then we’ll look at the time, color & consistency. We do not want to meconium *Once patients’ water is broken: temp taken q2hr Postpartum Physiologic Adaptations Postpartum Assessment: Initial assessments Vital signs Skin color Location and firmness of fundus Amount and color of lochia Perineum o Edema o Episiotomy o Lacerations o Hematoma Presence, degree, and location of pain Intravenous (IV) infusions o Type of fluid o Rate of administrationEXAM 3 19 o Type and amount of added medications o Patency of IV line o Redness, pain, edema of the site Urinary Output o Time and amount o Presence of a catheter o Color and character of urine Status of abdominal incision and dressing Level of feeling and ability to move if regional anesthesia was administered *Pudendal block: numbing of vaginal area; only numbs one area; doesn’t last look Moms at risk for PPH one that has a macrosomia baby; weighs 8.8lbs or more very quick delivery; precipitous labor *Breastfeeding delays return of ovulation and menstruation Focused Assessments After Vaginal Birth Every 15mins first hr. Every 30mins for the sec hr. Every 4 hrs. for the 24hrs Every 8-12 hrs. thereafter Know BUBBLE HE Breast Uterus Bowel Bladder Lochia Episiotomy Homan’s Sign Emotions Fundus Usually at umbilicus day of birth Should go down 1 fingerbreadth a day Involution going from a pregnant state (uterus) back down to non-pregnant state; uterus should be size of women’s fist (3 finger breaths below the umbilicus) *If mom wants epidural: gets bolus of LR first (1000ml)EXAM 3 20 *Mom needs to void at least 150ml for it to be counted as a void; count (measure) the first three voids *If moms not voiding, will need bladder scan Straight Cath if: She is unable to void The amount voided is less than 150 mL, and the bladder can be palpated The fundus is elevated or displaced from the midline Changes in color Lochia rubra: first 3 days (ruby red like period blood) Lochia serosa: days 4 -10 (pinkish color) Lochia alba: after day 10 (clearish, creamy) *Bright red blood means laceration somewhere-obtain H&H Episiotomy where doc cuts (makes incision) to allow more room for baby to deliver Episiotomy Healing evaluation (Perineum) R-redness E-edema E-ecchymosis D-discharge, drainage A-approximation * lacerations in skin; from tears Care in immediate postpartum: providing comfort measure Ice packs Used to soothe lacerations or episiotomy o can only be on perineum: 15-20 mins; off for 1 full hr. o cold pack can be left on: up to 4 hrs. o put on right after delivery Sitz bath Cool water for 1st 24hrs Warm water after 24hrs Perineal care Topical medications Sitting measures Analgesics Discomfort Assessment Analysis Provide choices to enhance client control Determine whether anxiety is contributing to discomfortEXAM 3 21 Planning Pain relief is NOT a realistic goal Goal is for positive birth experience Interventions Comfort measures Lighting Temperature Cleanliness Mouth care Bladder Positioning *Every pt gets ibuprofen q6hrs around the clock; unless allergic *Encourage to drink 2500ml per day Examine for signs/symptoms of thrombophlebitis Palpate pedal pulses Assess Homan sign Assess for edema Assess deep tendon reflexes Preventing Thrombophlebitis Early ambulation Frequent trips to the bathroom Nursing Care Following Cesarean Birth Assessment Pain relief Respirations Abdomen I&O Interventions: The First 24 hours Pain relief o Offer pain medication if not in PCA o Assess respiratory status if epidural Overcoming effects of immobility Provide Comfort Interventions: After 24 hours Resume normal activities Assist mother with infant feeding Prevent abdominal distention Teaching for dischargeEXAM 3 22 Postpartum Psychosocial Adaptations Process of Maternal Adaptation: Puerperal Phases Taking-in phase Focused on own need for fluid, food, and sleep Allows other to make decisions Mother is integrating her birth experience into reality Taking-hold phase Mother becomes more independent Assumes responsibility for own self-care Begins to shift attention to infant Welcomes information about newborn behavior Letting-go phase Couple relinquishes role as a childless couple Gives up idealized expectations of birth experience Relinquishes infant of their fantasy; accepts real infant Postpartum blues 50-85% mothers in 1st 2 weeks postpartum Symptoms: Irritability, anxiety, fluctuating mood, & increased emotional reactivity Mild & spontaneous remits, not considered psychiatric disorder Mom irritable, anxious Can care for baby, self She functions well, just kind of down and out Should go away around 6 wks. Postpartum depression Hits about 13% of mothers in first yr. Symptoms Excessive guilt. Anxious, depressed mood, anhedonia, insomnia/hypersomnia, suicidal ideation, & fatigue Doesn’t know the last time she fed baby, she ate, or slept Moderate to severe symptoms, prolonged course Postpartum psychosis 0.01% mothers in 1st 3 months postpartum Symptoms: Mixed or rapid cycling, agitation, delusions, hallucinations, disorganized behavior, cognitive impairment, & low insight. Severe, considered psychiatric emergency often necessitates hospitalization Diseases that went away while pregnant: schizo, bipolar Diseases come back w/a vengeanceEXAM 3 23 Augmentation- Pitocin Action- rupture the membranes Normal Newborn: Processes of Adaptation Neonate 0-28 days Neonates when sick: Low temp- (priority) if you can’t get the babies temp up, check the glucose because it’s probably low. Babies with low temp- feed them w/ breast milk or formula. 30 after he eats, you’ll do another BS Low glucose Increase 02 consumption Bilirubin same If baby temp low, can’t get it up check glucose, its prob low, resp increase, HR not infected When mom is going through later stage 1 & 2: also painful for baby When baby is in utero left lung: hypertensive Ductus arteriosa: must close after delivery; if not will hear a heart murmur Neurologic Adaptation: Thermoregulation Methods of heat loss o Evaporation o Conduction o Convection Don’t put baby near fan or any type of air condition o radiation When baby comes out of womb, DRY so, they don’t lose heat from evaporation-thermoregulation to stimulate babies to cry to expand the lungs Sites of brown fat around heart and kidneys IntraUGR and premature babies don’t have brown fatEXAM 3 24 We do not want our babies to use up their brown fat. Place a hat, socks, & blanket for the 1st 24hrs. We want to keep them nice & warm. Heat is transferred through the blood Hematologic Adaptation Newborn o 60-70% for hematocrit Vitamin K is given- because GI tract is sterile To help with blood clotting Prevent intracranial hemorrhage Given in the vastus lateralis GI system: Stomach- digestive tract is sterile- need bacteria & need early feeding Stomach will start to stretch as baby grows o Capacity expands within first few days of life First feeding:15-20ml Q3-4hrs (bottle feeding) Rapid peristalsis Gastrocolic reflux o colic can be caused by overfeeding GI system: Intestines Bowel sounds are present within the first hour. The digestive tract is sterile until feeding begins Infants are more prone to rapid water loss with diarrhea. GI system: Digestive Enzymes Breast milk more easily digested Saliva production limited until third month of life GI system: Stools Meconium is the first stool excreted o Greenish black with a thick, sticky, tarlike consistency o First stool is usually passed within 12 hours o Consists of particles from amniotic fluid Transitional stool is the second type Breastfed infant- poop more often than bottle fed o Stools are seedy and mustard colored. o Stools are more frequent than with formula. o Stools have a sweet-sour smell. Formula-fed infant o Stools are pale yellow to light brown.EXAM 3 25 o Stools are firmer in consistency-never should have a formed stool o Stools have the characteristic odor of stools. o Stools smell like formula RBCs- live in newborn 100 days, premie- 80 dyas Iron Bilirubin other stuff Conjugation of Bilirubin Unconjugated bilirubin: albumin picks up unconjugated and takes to liver (enzyme in liver conjugates it) Then, transported to GI and baby poops it out; early feeds are important If baby isn’t fed enough an enzyme in the GI track will unconjugate and put back into blood stream Physiologic jaundice becomes visible when the serum bilirubin reaches 5 to 7 mg/dL, which occurs when the baby is approximately 3 days old. This finding is within normal limits for the newborn. Pathologic jaundice occurs during the first 24 hours of life. Pathologic jaundice is caused by blood incompatibilities, causing excessive destruction of erythrocytes, and must be investigated. Breast milk jaundice occurs in one third of breastfed infants at 2 weeks and is caused by an insufficient intake of fluids.EXAM 3 26 Hepatic System: Hyperbilirubinemia- crosses the BBB can cause brain damage Physiologic jaundice o Caused by transient hyperbilirubinemia o Never present during first 24 hours of life o Jaundice is visible when bilirubin level is greater than 5 mg/dL o Rate of rise and fall of bilirubin level is important o EARLY frequent FEEDS so we can introduce good bacteria. o Breastfeed 1st then bottle feed for phototherapy Babies with jaundice need frequent feeds start to feed them within an hour How to get rid of bilirubin: Frequent feeds Breastfeed: feed q2-3hrs Formula babies: fed q3-4 hours phototherapy Urinary system If ear deformed or hole outside ear o kidney looked at Immune System Less effective at fighting off infection Immunoglobulin G (IgG) o Crosses placenta and provides temporary immunity Immunoglobulin M (IgM) o First immunoglobulin produced when exposed to infection Immunoglobulin A (IgA) o Receive some from colostrum and breast milk o Must be produced by the infant Psychosocial Adaptation Periods of reactivityo First period of reactivity o Period of sleep o Second period of reactivity Behavioral states o Quiet sleep state o Active sleep state o Drowsy state o Quiet alert state o Active alert state o Crying stateEXAM 3 27 Assessment of the Normal Newborn Early Focused Assessment Do VS before you assess the baby o while their sleep HR and RR (40-60): listen full minute First things we check: Fontanels Early Focused Assessment: Assessment of Cardiorespiratory Status Airway o Respiratory rate o Breath sounds o Signs of respiratory distress o Choanal atresia Color Heart sounds Brachial and femoral pulses Blood pressure Capillary refill Early Focused Assessment: Thermoregulation Take temperature soon after birth. Set warmer controls to regulate the amount of heat produced. Reassess every 30 minutes until stable. Early Focused Assessment: Hepatic System Blood glucose o At-risk newborns o Signs o Screening Bilirubin o At-risk newborns o Jaundice o Phototherapy-babies eyes are covered Assessment of Gestational Age: Ballard Score Scoring Gestational age and infant size o Small for gestational age o Large for gestational age o Appropriate for gestational age Monitor for complications common to age and size of infant.EXAM 3 28 Care of the Normal Newborn Vitamin K – to prevent intracranial problems o Administer within 1 hour of birth o Give intramuscularly- we do not aspirate o One dose prevents bleeding problems Eye treatment- given to every newborn o Erythromycin ophthalmic ointment (given to all babies)- given once in the eyes- start from cornea to the outside corner of the eye o Administer within 1 hour of birth Thermoregulation Assessment o Temperature shortly after birth o Assess every 30 min. until stable o More frequent if abnormal temperature Blood Glucose Assessment o Risk factors Really big babies Diabetic mother: GD, type 1 or 2 Interventions o Maintain safe glucose levels o Repeating glucose tests (after 30 mins of eating) levels below 40 o Provide other care Bilirubin Assessment o Assess for jaundice Interventions o Identify infants at risk for hyperbilirubinemia o Explain importance of adequate feedings o Explain significance of skin color changes o Continue to monitor during home or clinic visits Ongoing Assessments and Care Assess every 8 hours Provide skin care Bathing once while in the hospital Cord care Cleansing the diaper area Feedings Positioning- babies sleep on their backs Protecting the infant- ID bands & baby by the window BathingEXAM 3 29 Cord care o make sure it is dry; but do nothing to it Cleansing the diaper area o use baby wipe w/q diaper change Feedings Positioning Protecting the infant Cord Takes 7-10 days to fall off Do not immerse baby in water until it falls off Circumcision Babies given Tylenol Consideration: o Less likely to develop HPV o Women who have regular intercourse with an uncircumcised man Higher risk of developing cervical cancer Take 4x4 gauze with vaseline and put directly over penis Yellowy crusty discharge will appear around head of penis (Gomco & Mogen only) normal, leave alone 1 week- 10 days to heal NEVER wipe (it’s the healing process) 3 methods of circumcision: Mogen clamp- must put Vaseline over penis- put diaper loose Plastibell device- no vaseline Gomco clamp- must put Vaseline over penis- put diaper loose Bathing- DO not submerge baby in water until have to wait 7-10 before bathing for circumcision healed if baby wasn’t circumcised, will have to wait till the cord falls off NEVER USE LOTION (can clog baby pores) OR TALCUM POWDER ON BABIES If mom is Hep B positive: Cannot refuse baby getting Hep B vaccine Baby will get Hep B vacine and Hep B immune globulin o Give globulin within 12hrs of birth Hepatitis B Included with routine childhood vaccinations Newborn Screening Tests Hearing o any loss?; doing for early treatmentEXAM 3 30 Phenylketonuria (PKU) o checks for 60+ diseases; done after 24hrs of life; must have PKU drawn on NB before d/c. Make sure the physician information is correct because they’re the only person that will be notified Hypothyroidism Galactosemia Hemoglobinopathies Congenital adrenal hyperplasia Discharge and Newborn Follow-Up Care: Early discharge o Appropriate for gestational age o Vital signs within normal limits o Feeding successfully o Making transition from fetal to neonatal life o Passed urine and stool o Mother able to care for infant Follow-up care o Professional follow-up care recommended with early discharge o Can be provided in a number of ways Nutritional Needs of Newborn: Calories o Breastfed 85 to 100 kcal/kg daily o Formula fed 100 to 110 kcal/kg daily o May lose less than 10% of birth weight Breast Milk: Nutrients Protein Carbohydrates Fat Vitamins Minerals Enzymes (can have 1cp of caffeine (chocolate has caffeine in it) Colostrum Thick yellow (rich in everything baby needs); o First form of milk produced from the breast o Colostrum until milks comes in Maternal Diet Increase calories 500/dayEXAM 3 31 Premature Babies Need high caloric diet Prolactin Produces milk Oxytocin Stimulate the release of milk through the nipple Start back feeding where you left off Alternate breast Engorgement- do not skip feedings to prevent Happens 1 time before milk comes in; gets hard as a rock (baby may slip off) Have the mom hand express her milk (massage the breast to make softer) Pump milk to relieve pain so it can soften up so baby can latch on to it Cold compress If mom is NOT breastfeeding, tell mom to put cabbage leaves on breast, then their bra on, & it will dry up & they will have to keep changing cabbage leaves. Breast milk can be frozen up to 6 months Newborn Assessment Axillary temp HR taken for 1 full minute. VS when sleeping Blood pressure & VS will be taken on all 4 extremities on a newborn if heart murmur is heard. Are there bleeding coming form the cord? 2 arteries & 1 veins at delivery, but once the cord starts to dry up, you won’t be able to see those anymore because it will turn into scab. Any discharge Apgar Score∗ Points Assessment 0 1 2EXAM 3 32 Points Assessment 0 1 2 Heart rate Absent Below 100 beats per minute (bpm) 100 bpm or higher Respiratory effort No spontaneous respiration s Slow respirations or weak cry Below 40 Spontaneous respirations with strong, lusty cry. Vigorously cry. RR 40-60 Muscle tone Limp Minimal flexion of extremities; sluggish movement Flexed body posture; spontaneous and vigorous movement Reflex respon se No response to suction or gentle slap on soles Minimal response (grimace) to suction or gentle slap on soles Responds promptly to suction or gentle slap to sole with cry or active movement Color Pallor or cyanosis Whole body blue Bluish hands and feet only (acrocyanosis) Pink (light skinned) or absence of cyanosis (dark skinned); pink mucous membranes 0 1 2 3 4 5 6 7 8 9 10 Infant needs resuscitation.† Gently stimulate by rubbing infant’s back while administering oxygen. Determine whether mother received narcotics, which may have depressed infant’s respirations. Provide no action other than support of infant’s spontaneous efforts andEXAM 3 33 Points Assessment 0 1 2 continued observation. ∗ The Apgar score is a method for rapid evaluation of the infant’s cardiorespiratory adaptation after birth. The nurse scores the infant at 1 minute and 5 minutes in each of five areas. The assessments are arranged from most important (heart rate) to least important (color). The infant is assigned a score of 0 to 2 in each of the five areas, and the scores are totaled. Resuscitation should not be delayed until the 1-minute score is obtained. However, general guidelines for the infant’s care are based on three ranges of 1- minute scores: 0 to 2, 3 to 6, 7 to 10. † Note: Neonatal resuscitation measures, if needed, do not await 1-minute Apgar scoring but are instituted at once. Skin-to-skin contact with a parent also maintains the infant’s temperature and promotes bonding between the infant and parent. Delaying the first bath for several hours allows the temperature to stabilize. Avoid positioning yourself between the infant and the radiant heat source in the warmer. The infant should be wrapped in dry, warm blankets when not in the warmer or making skin-to-skin contact. Remove wet linens, replacing them with warm and dry ones. A stockinette cap further reduces heat loss if it is placed on the baby’s dry head. A cap is not worn while the infant is in the radiant warmer because the cap slows transfer of heat to the baby. Assessing for Anomalies Head Fontanels- anterior fontanelle is diamond shape, posterior triangular shape There are little lines that come from these fontanels that are called sutures. The sutures are what allows the baby’s head to squish down & mold to come through the birth canal. Caput succedaneum- is what’s delivered 1st. It’s swelling and maybe some clear fluid build up between the skull and the scalp. It’s from being in the birth canal too long. It will go away in 1-2 days. Caput cross those sutures lines (cone head) Cephalohematoma- caused by trauma, it does not cross those suture lines. It’s in one area of the scalp. Buildup of blood & takes 3-4 weeks for that blood to be absorbed into the baby’s peripheral system. Low set ears- sign of down syndrome Neural Defect Spina Bifida o Sacral Dimple- spread those cheeks o If you see a hole, notify HCP Observe for hip click Check for anal patency Assessing Neurologic System Reflexes Sensory assessmentEXAM 3 34 Other neurologic signs Jitteriness (tremors) signs of hypoglycemia Seizures- baby straightening out extremities w/ tiny shakes (rigid) Irritability Facial bruising is probably from a quick delivery Baby may have a lot of petechia or facial bruising If the baby was covered up to his neck, you would think the baby was blue 1st action- uncover him Then see if his mucous membranes are pink. Oral Cavity Take your gloved finger & make sure his pallet is closed Gonna see if he can suck on his finger. Check his neck & abdomen & make sure it’s not distended & that it’s soft Baby should have bowel sounds 3 hours after birth Umbilical hernia- baby will have to have surgery Babies that are stretched out are more premature Flexed babies are termed Feet Creases in feet are termed babies Smooth feet are premature Legs Creases on back of legs should be equal They should go straight across. 1 leg creases should be equal w/ the other leg creases. If not equal, there may be a little hip displacement Little girls The more term the baby is, the labia majora is going to cover everything The more preterm, the clitoris is going to be more prominent than anything else. Little boys Look at genitals Check scrotum to make sure both testes are down in the scrotum They’ll feel like tiny peas. You have to check each side. Hypospadias- if you notice part of his skin is gone & he did not have a circumcision. This baby was born this way. He doesn’t have all of the foreskin. We do not do a circumcision on them. They need to see a urologist. Because maybe the meatus is not atEXAM 3 35 the tip of the penis. It might be at the side. May need some of the foreskin to do reconstructive surgery. So do not do circumcisions. Newborn Pearl- White spot at end of penis. Nothing to worry about. Floppy Tone Baby is not flexed Pick up baby arm & falls back down Full term baby, you could pull up arm & he will pull it back -Jittery- sign of low BS- heel stick on outer part of foot. -Rigid- could be sign of seizure -Absence of startle reflex Take babies wrist. Pull him up by his arms & his body off the bed & let go & he should startle & if he doesn’t then we’re worried. This floppy tone is not normal Reflex Moro or startle reflex Take babies wrist. Pull him up by his arms & his body off the bed & let go & he should startle & if he doesn’t then we’re worried. Palmer grass reflex- putting your finger in the baby’s palm. He should grab your finger The plantar reflex- Put your finger at the base of the baby’s toes & it should flex, it should grab your finger. The Babinski reflexes is elicited by stroking the lateral sole of the infant’s foot from the heel forward & across the ball of the foot. This causes the toes to flare outward & the big toe to dorsiflex. Sucking reflex You put your finger in the baby’s mouth & he starts sucking on your finger Integumentary System Color Lanugo-hair on the baby (peach fuzz) Milia-little white dots on the baby’s nose. Leave them alone. Don’t touch them Marks from delivery- if the baby is forceps or vacuum baby. Check for trauma Breast, hair & nails- just document. Expected findings Mongolian spots dark area on buttocks they do get lighter with age. (not a bruise) Stork bites eyelids. appears when baby gets really upset. They get real dark. They will fade w/ time. Port wine stain- these babies that are born w/ this does not go away. Permanent birth mark on face. Face is asymmetricalEXAM 3 36 EXAM 1 Need to know the stages of labor Apgar 5p’s Prenatal visits Nageals rule Frequency, labor & contractions Involution Why do we feed babies with hyperbillirubin Make priority when babies come into the hospital Remember different stations Fundal height, fundal measurements Signs of pregnancy Different ways to prevent heat loss How do we pt’s truly in labor GTPAL How much folate acid How to care for circumcision PPH BUBBLE HE Be familiar with generic & Psychosis, blues, etc. Cephalohematoma & caput Labs during prenatal visit Prenatal Care and Expected Findings in Pregnancy Prenatal care is a vital component of a healthy pregnancy. Adequate, routine care will increase the likelihood of a safe birth for mother and child. To ensure adequate care, the pregnant woman must select from a variety of prenatal healthcare providers toEXAM 3 37 manage her pregnancy. The individualized needs of the woman, her family, and the unborn baby will determine the best source of healthcare during the pregnancy. After selecting a prenatal care provider, prenatal care visits will begin as soon as possible, if not prior to conception. During the initial visits, a health history and physical will be conducted, gestational age of the fetus will be determined, and laboratory and diagnostic tests will be evaluated. Below is a table illustrating many of these common laboratory values explored during prenatal visits. Laboratory and Diagnostic Tests and Pregnancy Findings Laboratory or Diagnostic Test Normal Value Blood Typing A, B, A B, O Rh Factor Positive or negative Hemoglobin (Hgb) > 11.5 mg/dL Hematocrit (Hct) > 33% Platelets 150,000–400,000 mm WBC 5,000–12,000 mm3 RPR Negative HIV Negative Hepatitis B Antigen Negative Rubella Titer 1:8 immune Chlamydia/Gonorrhea Culture Negative Pap Smear Normal cytologyEXAM 3 38 Preterm Labor: (< 37 weeks) Lower backache, increased vaginal discharge, bloody show, leaking amniotic fluid, contractions, pelvic pressure Term Labor: (> 37 weeks) Gross rupture of membranes, progressive cervical change, contractions continuing to get closer and stronger regardless of maternal activity Report to provider Decreased fetal movement Pelvic pressure Bleeding Contractions that are regular and coming closer together (more than 6 noted in an hour) Rupture of membranes Obstetrical Procedures Stages of Labor Stage One Phase Dilation Contractions Duration Latent 0–3 cm Frequency 5–10 minutes 30–45 seconds Active 4–7 cm Frequency 2–5 minutes 40–60 seconds Transition 8–10 cm Frequency 1.5–3 minutes 45–90 seconds Stage Two Phase Dilation Contractions Duration Expulsion (birth of baby) 10 cm Frequency 2–3 minutes 60–90 seconds Stage Three Phase Contractions Duration Delivery of Placenta Strong 5 minutes to 20 minutes Stage Four Phase Vaginal Cesarean Section Recovery 2 hours minimum 4 hours minimum General Adjunct IV sedation Adjunct IV sedation is often applied via a nurse anesthetist or anesthesia provider to complement the patient's relaxation of the prior provided anesthesia. Epidural SpinalEXAM 3 39 Spinal anesthesia is frequently utilized for scheduled C/S. Antepartum Fetal Assessment Indications for Fetal Diagnostic Testing To detect congenital anomalies To evaluate the condition of the fetus The woman has the right to refuse antepartum Nurses must respect the woman’s personal decisions Ultrasound- positive pregnancy signs (1st diagnostic test) It is directed through tissues of the abdomen or vagina to provide two-dimensional images High-frequency sound waves are aimed at body tissues The amount of energy returned as an echo depends on the properties of the tissues. It is deflected by tissues in their path & returned as echoes. Three-dimensional ultrasound images have greater detail o They provide more accurate identification of the extent and size of abnormalities Real-time scanning o Shows movement as it happens o Allows the observer to see fetal heart motion, fetal breathing activity, and fetal body movement o Can distinguish between moving tissues of the fetus and maternal tissues *By the 5th week of gestation, the U.S. tech can see the baby’s heartbeat Ultrasound: Emotional Response Some parents are excited Some parents report anxiety Many couples expect to know the gender of the fetus Others do not want to know the gender Sonographers often give a still image *Mom may exhibit postpartum blues if wrong gender was given & was prepared to have the other gender. Postpartum blues • Hits mom in first couple weeks • Mom irritable, anxious • Can care for baby, self • She functions well, just kind of down and out Should go away around 6 wks ATI EXPECTED FINDINGS of postpartum blues: Feelings of sadness Lack of appetite Sleep pattern disturbances Feeling of inadequacies\ Crying easily for no apparent reasonEXAM 3 40 Restlessness, insomnia, fatigue Headache Anxiety, anger, sadness Nursing Care for postpartum blues monitor interactions between client & baby. Encourage bonding activities Monitor for mood & effect Reinforce that feeling down in the postpartum period is expected & self-limiting. Encourage client to notify HCP if feeling persist Reinforce the importance of compliance w/ any prescribed medications regimen Contact a community resource to schedule a follow up visit after discharge for clients who are high risk for postpartum depression Ask client if she has thoughts of self-harm, suicide, or harming the infant. Provide for the safety of the infant as the priority care. Levels of Obstetric Ultrasound Standard (basic) o General survey Example: anatomy scan Specialized (comprehensive) o Specific Example: looking for abnormalities to diagnose what the screening test said Limited o Address a specific question Example: fetal presentation (scanned by symphysis pubis to see if there’s a head down there) usually a breech if you don’t feel the head Ultrasound: First Trimester Purpose o Confirm pregnancy (checking how many baby’s); o Verify the location of the pregnancy (checking to see where embryo implanted) o Detect multifetal gestations o Determine gestational age o Identify markers o Determine the locations of the uterus, cervix, and placenta for procedures such as chorionic villus sampling (CVS) Procedure o Transvaginal for 1st trimester An invasive procedure in which a probe is inserted vaginally to allow for more accurate evaluation Ultrasound: Second and Third Trimester Purpose o Confirm viability searching for FHT (ex. Mom maybe 29wks hasn’t felt her baby in days) worse o Evaluate fetal anatomyEXAM 3 41 o Determine gestational age- crown to rump- is 1 twin growing faster than the other. Is 1 getting all of the nourishment o Assess serial fetal growth o Compare growth of fetuses in multifetal gestations o Evaluate four of five markers in a biophysical profile o Locate the placenta when placenta previa is suspected o Determine fetal presentation o Guide needle for amniocentesis or percutaneous umbilical cord sampling (PUBS) Specialized ultrasound for abnormal findings o Hydramnios (excessive amniotic fluid) o Oligohydramnios (insufficient amniotic fluid) o Abnormal levels of maternal serum alpha-fetoprotein (MSAFP) or other tests in multiple-marker testing o Neural tube defects (NTDs) (failure of the bony encasement of spinal cord or skull to close) Procedure o Transabdominal for 2nd & 3rd trimester Doppler Ultrasound Blood Flow Assessment Purpose o Identify abnormalities in the diastolic flow o Enhances detail about the degree of resistance to normal blood flow in the growthrestricted fetus Alpha-Fetoprotein Screening MSAFP (Maternal Serum Alpha-Fetoprotein) blood draw Alpha-fetoprotein (AFP) is the predominant protein in fetal plasma. AFP crosses placental membranes into the maternal circulation AFP can be measured in maternal serum (MSAFP) and amniotic fluid (AFAFP) *All we do is draw some blood from mom Purpose Abnormal concentrations of AFP are associated with serious fetal anomalies Low levels of MSAFP suggest chromosomal abnormalities such as trisomy 21 ATI: down syndrome Elevated MSAFP levels are associated with open NTDs (neural tube defects) and body wall defects. ATI: open abdominal defect o Anencephaly o Spina bifida *every single pregnant woman gets a MSAFP drawn Procedure Initial screening (every pregnant woman gets this) is offered at 16 and 18 weeks of gestation- (can have an abortion up to 20 weeks gestation) RISK FACTORS: Gestational age, maternal weight, multifetal pregnancy, race, maternal diabetes, and ethnicity must be considered when evaluating the levels The mother is informed that MSAFP is a screening test rather than a diagnostic testEXAM 3 42 Multiple-Marker Screening (everybody gets it)-consent does not need to be obtained MSAFP (1st test for screening if AFP is abnormal) o Elevated levels used to detect open body wall defect o Low levels linked to chromosome defects Triple-screen (done if MSAFP is abnormal) o Unconjugated estriol and hCG have been added to routine MSAFP evaluation. Quad-screen (if additional screening is needed if triple screen still show abnormalities) o A fourth marker, the placental hormone inhibin A (protein produced by the ovaries & placenta), improves the accuracy of the triple-screen. o If all these screening come back abnormal then we can do a specialized ultrasound to diagnose what the MSAFP was alluding to Chorionic Villus Sampling (only if you have a history if chromosomal abnormalities in family) Diagnostic test (2nd) o Checks for fetal chromosomal, metabolic, or DNA abnormalities Procedure o Use Ultrasound to guide, go in with needle right into placenta & withdraw it, as needle comes out collects sample. IFMOM IS RH NEGATIVE: Rhogam given if mom is negative &/or indication of blood mixing when after needle was withdrawn & blood may have been mixed o Usually performed between 10 and 12 weeks sooner than MSAFP-advantage: done earlier to allow parents to see what they want to do o Transcervical or the transabdominal approach- mom supine o Genetic counseling o Counseling about the procedure Advantages o Results are known earlier than early amniocentesis o CVS offers prenatal diagnosis to women who find later procedures unacceptable Risks o Rate of pregnancy loss after CVS is similar to that of amniocentesis o More than two attempts or bleeding during the week before the procedure increases the risk for fetal loss. o Reports of limb reduction defects Amniocentesis- (3rd diagnostic test) which will be done to confirm chromosome abnormalities. HCP wants to avoid hitting any other products of conception (no fetus, no cord, no placenta) The aspiration using a long needle to draw amniotic fluid from the amniotic sac or examination. Also done by a guided ultrasound Purpose: Mid-trimester to determine MSAFP o Examine fetal cells present in amniotic fluid to identify chromosome abnormalities o Evaluate the fetal condition when the woman is sensitized to Rh-positive blood o Diagnose intrauterine infections o Investigate amniotic fluid AFP when the multiple-marker test done on maternal serum is not normalEXAM 3 43 Purpose: Third Trimester-Because MSAFP is not done until 16-18 wks o Tests to determine fetal lung maturity Lecithin/sphingomyelin (L/S)ratio-takes 20mls to analyze the fluid o Test for fetal hemolytic disease Determine fetal bilirubin concentration (Rh sensitized) Monitored after amniocentesis procedure o Baby: 1 hour after- make sure fetus is good Monitor fetal HR o Mom: 1 hour after-because we wanna make sure mom doesn’t contract Disadvantage o Must wait until 16 weeks after MSAFP is drawn o Gives little time for decisions about additional tests or whether to terminate pregnancy before 20wks ATI: Indications Potential diagnoses from amniocentesis Previous birth w/ a chromosomal anomaly A parent who is a carrier of a chromosomal anomaly Family history of neural tube defects Prenatal diagnosis of a genetic disorder or congenital anomaly of the fetus AFP level for fetal abnormalities Lung maturity assessment Fetal hemolytic disease Meconium in the amniotic fluid Percutaneous umbilical blood sampling- very dangerous test Aspiration of fetal blood from the umbilical cord for prenatal diagnosis or therapy Procedure o High-resolution ultrasound is used to locate the fetus, placenta, and umbilical cord and guide needle insertion o Needle is inserted into the umbilical cord near the site at which the cord meets the placenta o Rho(D) immune globulin (RhoGAM) is given to Rh-negative women because of guided ultrasound Fetal Nonstress test-looking for acceleration (NST) eval for fetal well being (what does the HR do with fetal movement.) Nursing action ATI & instructor: Make sure mom voids Have her nice & comfy sitting up in bed place in high or semi-fowler’s position or left lateral position or seat client in a reclining chair next to the bed. Place toco & transducers. Toco (monitor uterine contractions) doppler transducer (monitor FHR) Give mom a button-each time mom feels baby moving, she will push button Have something to drink sitting next to her Put her on a fetal monitorEXAM 3 44 Checking fetal wellbeing; not causing baby any stress-just placing mom on monitor Observes the fetal heart rate response to fetal movement MUST be on the monitor for minimum of 40 minutes-looking fetal well-being o Looking for minimum 2 accelerations a 15*15 in a 20min block (ATI: 20-30min’s to complete) To be considered an acceleration 32 weeks or greater: (2-15x15 accelerarions) in a 20 min’s period under 32 weeks: (2x10x10) acceleration 2-15x15: called reactive and reassuring min go up 15 beats from baseline and last a min 15 seconds ex. Baby hr 130 then goes up 15 & last for 15 sec’s that’s good to be considered an acceleration Test is good for 1 week Nonreactive and non-reassuring: Fetal movement but no increase in HR Not routine must have Dr. order Procedure o Women should void, baseline BS should be taken o Women may be seated in a reclining chair or have her head elevated at least 45° *Babies heart rate should go up with fetal movement Get mom something to eat & something cold (something that’s going to wake the baby up just in case he’s sleep). If still no movement, move on to vibroacoustic stimulation on if mom is not contracting o (ATI you might be asked to drink orange juice for stimulation) Advantage of NST Noninvasive Painless Believed to be w/o risk to mother or fetus Easily administered Results immediately available Disadvantage of NST High false-positive rate (ATI: fetal movement response blunted by sleep cycles of the fetus, fetal immaturity, maternal medications, and nicotine use disorder) Additional testing related to a nonreactive NST Vibroacoustic Stimulation Test (used for if we have nonreactive & non-reassuring) find where the fetus head is located & zap Uses sound stimulation to elicit fetal movemento Stimulate fetal movement that results in a reactive NST o Confirm nonreactive NST 3 seconds, 3 minutes in a row, only 3 times Risks Appears to be safe for the fetus in terms of hearing at 33 wks Call physician if all has failedEXAM 3 45 Contraction Stress test - we’re causing stress to the babies by inducing contractions. We’re looking for decelerations. Want to see if baby can handle stress during vaginal labor. If baby has decelerations, baby can’t handle stress of labor. Negative CST: reassuring Positive CST: non-reassuring-if baby has decelerations Making mom contract o we don’t want baby to have HR accelerations o we need 3 contractions in 10 minutes. Once we get mom to get 3 contractions in 10 minutes, we’re looking for decelerations. If there is no decelerations, it is NEGATIVE (means no) which is reassuring for CST *we get our mothers to contract by either nipple stimulation or Pitocin Start Pitocin to have mom contract (Pitocin is time consuming) Test is good for 1 week If mom doesn’t have decelerations. It is negative for decelerations & it’s reassuring. If mom has decelerations. It is positive for decelerations (late) & non reassuring because the baby will not be able to handle that pregnancy & will need a C-section when it’s time for mom to deliver baby Stimulate baby & feed mom if there’s no acceleration (stimulate ATI: nipple stimulation in order to receive uterine contraction) Procedure EFM-transducer applied to abdomen to monitor FHR patterns during labor & birth Oxytocin/nipple stimulation 3 contractions in 10 minutes Interpretation Negative (reassuring) Positive (non-reassuring) Biophysical Profile (BPP)- (good for 1wk) if the HCP doesn’t order CST, he will order BPP Done by US Assesses 5 different parameters of fetal status o FHR Reactive=2 nonreactive=0 o Fetal breathing movements At least 1 episode >30sec’s=2, Absent or <30sec’s duration=0 o Gross fetal movements At least 3 body or limb extensions w/ return to flexion=2, <3 limb=0 o Fetal muscle tone At least 1 episode of slow extension w/ return to flexion=2 Slow extension & flexion. Lack of flexion, or absent movement=0 o Amniotic fluid volume At least 1 pocket of fluid that measures at least 2cm in 2 perpendicular planes=2 Pockets absent or less than 2cm=0 Baby will either get 0 (No HR) or 2 (HR) Normal is 8/10 or 10/10EXAM 3 46 Baby that has a 2/10 needs to be delivered immediately- mom can be induced (doesn’t have to be delivered C-section)- baby is not doing well in utero (doesn’t mean baby will die) 4/10 or 6/10 will be up to the physician if the baby needs to delivered ATI: total scores 8-10 normal 4-6 abnormal-suspect chronic fetal asphyxia Less than 4 abnormal-strongly suggest chronic fetal asphyxia Asphyxia-(deficient supply of oxygen to the body that arises from abnormal breathing) chokingcausing generalized hypoxia. Maternal Assessment of Fetal Movement (ex. Mom says baby hasn’t been moving much) Kick counts Baby should move/kick at least 8-10 times an hr. Procedure o Women lies on her side, gets something cold to drink for stimulation, places her hands on the largest part of her abdomen and concentrates (not while on phone nor watching tv) on fetal movements 1hr 3x’s a day Advantages o May identify fetal problems early in the client who has no known pregnancy risk factors o Noninvasive Disadvantage-phone rings, someone comes in & interrupts her What if a mom comes in for an induction during 20 wks? Pregnancy termination You can’t have judgement. But you do have the right to refuse the pt until someone can take over the pt. CHPT 16 Amniotomy Artificial rupture of membrane (AROM)- amniotic hook Indications Induce labor- pt not in labor Augment labor- pt in labor but not going quick enough. We’ll break her water to help her along. We’ll augment her if she falls off the Friedman’s labor curve. Allow internal fetal monitoring (internal scalp electrode) - water has be broke in order to put this on. In order to get a true heart rate from the baby. Risks for artificial rupture of membrane Prolapse cord- if that fetus is above the ischial spine (too high) & dr breaks amniotic sac, the cord can come down before the baby. Then mom will have to have an emergency C-section. You will see a deceleration Infection- if HCP does an amniotomy & her water has been broken for hours. Theres a chance the doctor may have introduced an infection.EXAM 3 47 Abruptio placenta (not very common) it’s like a balloon, once you break a ballon, it shrivels down. Once you rupture membranes that uterus can get smaller & if the placenta was attached, it can get smaller & detach. She can have abruptio placenta Technique Done by physician or nurse-midwife Amnio hook snags membrane (sterile) Nursing considerations Obtain baseline information (assess FHT 1st) because if that cord is the vagina & you can’t see it, baby’s gonna choke baby will tell you something’s blocking me & I can’t get my oxygen & blood supply) o (FHR) 20 to 30 minutes before procedure Assist with procedure o Place absorbent pads o Equipment Provide care after procedure o Identify complications o Promote comfort *Very first thing you assess with provider breaks water for amniotomy Fetal heart tone Color, consistency, amount Contraindication- for amniotomy PT who is GBS & hasn’t gotten their ABX PT who had a previous C-Section Pt who had a macrocosmic baby Artificial methods to stimulate uterine contractionsIf the baby is in the bag of water, the head is not hitting the surface. Once you rupture the membrane now when the mom is having contractions, the head is pushing on the cervix & should help it to dilate which will help w/ labor. Induction and Augmentation of Labor: Indications Hostile intrauterine environment Spontaneous rupture of the membranes (SROM)-we need to get her into labor (induce her) because the longer she’s ruptured is the higher chance of getting an intrauterine infection Post-term pregnancy 40+ weeks- we will induce her because she’s not in labor) Chorioamnionitis (inflammation of the amniotic sac) she has an infection & needs to be induced Hypertension-needs to be delivered Abruptio placentae Maternal medical conditions that worsen with continuation of the pregnancy Fetal death- fetal demise (baby died in utero) need to be delivered vaginally Before we start inductionEXAM 3 48 Need to check cervix 1st (need to know if it’s midline) Do Bishop score (5pt’s before we induce) The higher the # the readier the cervix is to go into labor 25mcg vaginally tablet; Cytotec to soften cervix (admin vaginal for cervical ripening put between fingers outside cervical aus & stays there) (admin rectally for PPH 800- 1000mcg). Bad thing about Cytotec is, if we start having hypertonic contractions, we can’t scoop it back out so we have to start giving her medications like terbutaline & fluids Cervidil; helps to soften cervix; prepare it for labor. *Do not induce anybody under 38 wks. Induction and Augmentation of Labor: Contraindications (will never induce) Placenta previa Vasa previa Umbilical cord prolapse (emergency c section) Abnormal fetal presentation-transverse lie, military, breech Fetal presenting part above the pelvic inlet- if pelvis is large enough for baby to come through, we would never indue mom Previous surgery in the upper uterus Induction and Augmentation of Labor: Risks Hypertonic uterine activity, too many contractions late decelerations (placetal insufficiency) more than 2.5min’s apart (we don’t want her to contract more than that because we can cause stress on the baby or we can rupture her uterus) Cervidil for hypertonic contractions benefits & we can pull the string/wafer out. Terbutaline can slow down her contractions Uterine rupture Maternal water intoxication-hypotension, crackles (when a pt comes in we put them on Pitocin, IF we’re going to induce w/ pitocin. Pitocin is always SECONDARY & always piggybacked into a main line. LR is constantly running. If mom wants to have an epidural. We have to give 1000ml LR prior to her epidural because it causes HYPOTENSION. Anytime during labor, we can give a pt up to 3000ml of fluid so we can cause water intoxication so we can hear crackles. Greater risk for chorioamnionitis-if she’s ruptured (same as below) Greater risk for cesarean birth- if she’s induced or augmented & things don’t happen in a timely manner Induction and Augmentation of Labor: Techniques Determining whether induction is indicated o Gestational age- will not be induced unless their 38wks or greater o Cervical assessment (Bishop score) Cervical ripening- uterus not ready o Medical methods- by giving a prostaglandin gel (cervedil or Cytotec to soften or ripen the cervix) cervidil can put mom into labor, it’s left in for 12 hours. The cervix is re-assessed & if it has softened or ripen, then we’ll start her Pitocin.EXAM 3 49 o Mechanical methods- balloon Induction and Augmentation of Labor: Techniques Oxytocin administration o Dilute in an isotonic solution o Secondary (piggyback) infusion into the lowest port possible If she’s pregnant, she must be piggy backed on a pump into main line o Insert oxytocin into the primary intravenous line o Start slowly, increase gradually Start out with 1mu PITOCIN=1ml of fluid or always increase slowly usually 2mu/hr. Then we’ll Increase q20-30mins by 2mu on the Pitocin Max they can get is 20mu/hr. (ex. then go to 4 in 30 min’s, then increase another 2mu every 30min’s until we reach the max of 20mu/hr. if mom still not contracting, CALL HCP (order needed) to see if we can go higher. The highest he’ll let you go is 40mu/hr o Monitor uterine activity, FHR, and fetal heart patterns frequently Must chart q30mins while mom is on Pitocin: - Monitoring & assessing uterine activity every 30 mins - Monitoring FHR every 15 min’s - 30 units to 500 per each bag - 1 mu = 1mL Serial induction of labor- need to soften the cervix 1st & then you’ll do Pitocin. Usually for a pt over 40wks Induction and Augmentation of Labor: Nursing Considerations Observe fetal response/reaction to the Pitocin for contraction pattern o Hypertonic contractions reduce intra uteroplacental blood flow.-causes placental insufficiency (late decelerations) o Assess FHR pattern o Reduce or stop infusion for non-reassuring FHR. o Side lying position o Oxygen by facemask via non re-breather Induction and Augmentation of Labor: Nursing Considerations Observe maternal response o Assess uterine activity o Assess blood pressure and pulse- always take VS between contractions o Be aware of pain management techniques- pitocin contractions very o Record intake and output- anyone w/ IV has be on I&O’s o Observe for signs of water intoxication o Assess for uterine atony (boggy fundus) in postpartum period- if she’s on Pitocin during labor.EXAM 3 50 *Mom will not get out of bed once Pitocin/oxytocin has been started *If mom is on oxytocin mom cannot be on oxygen Never give 2 O’s at the same time Oxytocin What the body makes Pitocin Man-made oxytocin 30units Pitocin in 500 ml 1mu Pitocin = 1ml of solution Augmentation -if she in labor already; going to help her; doing something to stimulate contractions Version: Indications External version o Doctor will change the fetal position from a breech, shoulder (transverse lie), or oblique presentation to cephalic w/ an US to see where the baby’s head is so they can externally turn the baby o NST done 1st Monitor mom 1 hr. after procedure Watch to make sure baby is not having any declarations Make sure that mom is not having any contractions Can’t be done until pt. is 37 weeks Only I fetus May be given terbutaline so she doesn’t contract. If baby is stressed, we’ll have to deliver baby Internal version o Change the position of a second twin in a vaginal birth. Can be done w/ 1 baby This is done only when there are twins in utero & 1 twin was delivered & the other twin did a flip. Dr will go in & internally remove the baby. Only RNs can give rhogam Version: Contraindications (we would nerver do) Uterine malformations Previous cesarean, could rupture uterus Fetal size ≥4000 g macrocosmic baby o 8.8lbs or greater Cephalopelvic disproportion Multifetal gestation-never do an external version unless there’s 1 baby Oligohydramnios o Not enough amniotic fluid Ruptured membranes Cord around the fetal body or neck (nuchal cord)EXAM 3 51 Uteroplacental insufficiency (late decels) Engagement of the fetal head Placenta previa- she would need a C-section/ cesarean o When the placenta covers the opening in the mother’s cervix Version: Risks Few risks to the woman are present. Few serious fetal risks exist. Fetus may become entangled in the umbilical cord. Abruptio placentae may occur. Mixing of fetal and maternal blood Version: Techniques External version o Nonstress test (NST) to evaluate fetal well-being o Determine gestational age beyond 37 weeks o Administer tocolytic drug to relax uterus o Use ultrasound to guide manipulations o Rho(D) immune globulin (RhoGAM) given if indicated Operative Vaginal Birth: Indications Forceps or Vacuum to get the baby out Shortened second stage of labor Maternal indications o Mom exhausted Fetal indications o Fetal distress Operative Vaginal Birth: Contraindications Cesarean birth preferable o Severe fetal compromise o Acute maternal conditions o High fetal station Only do this when baby is +2 station o Cephalopelvic disproportion Pelvic not big enough to deliver baby Operative Vaginal Birth: Risk Trauma to maternal and fetal tissues o If Dr. did forceps delivery and mom has bright red bleeding after Trauma somewhere Operative Vaginal Birth: Technique Preparation of woman o Empty bladder (action)EXAM 3 52 o Cervix completely dilated, and membrane ruptured o Adequate anesthesia o Regional block, pudendal block (perineum, vulva, rectal areas)- injection of lidocaine in the vagina so mom doesn’t feel vacuum or forceps. o Epidural Classification of techniques o Outlet: fetal head on perineum o Low: leading edge of fetal skull at station +2 o Mid: leading edge of fetal skull between 0 and +2 station Operative Vaginal Birth: Nursing Considerations Observe mother for trauma after birth. o Bright red bleeding with firm fundus call DR. immediately!!! Observe neonate for trauma after birth. o Facial asymmetry *Forceps birth- facial bruising & facial symmetry (temple, cheeks, & face) trauma to the face expected finding *Vacuum: suction cup only allowed to come off 3 times; after mom must have c-section - not on fontanel *Caput: crosses suture line If baby has cephalohematoma more prone To develop jaundice Episiotomy: Indications (it’s where they take the scissors & cut the area between the vagina & rectum to allow for a bigger area for the fetus to come out) Shoulder dystocia Vacuum or forceps-assisted births Face presentation Preterm fetus o Don’t want to cause trauma to the fetus The tear from the vagina to the rectum is called 3rd degree laceration 4th degree is a torn sphincter Episiotomy: Risks Infection Perineal pain Cesarean Birth: Indications Dystocia- dr has 5-7 minutes to get the baby out o Baby stuck Cephalopelvic (fetopelvic) disproportion o Unborn child’s head too large to enter or pass through the birth canal Severe hypertensionEXAM 3 53 Maternal diseases, dwarfism, MS Active genital herpes Some previous uterine surgical procedures o Classic cesarean incision (vertical incision) o Removal of fibroid tumors Persistent non-reassuring FHR patterns Prolapsed umbilical cord Fetal malpresentations Hemorrhagic conditions Cesarean Birth: Contraindications Fetal death Immature fetus Maternal coagulation defects Cesarean Birth: Maternal Risks Infection Hemorrhage Urinary tract trauma or infection Thrombophlebitis, thromboembolism Paralytic ileus Atelectasis Anesthesia complications Cesarean Birth: Fetal Risks Lung immaturity is the greatest risk if the fetus is delivered preterm. Inadvertent preterm birth Transient tachypnea Persistent pulmonary hypertension of the newborn Traumatic injury Cesarean Birth: Technique Preparation o Anesthesia o Medication Given protonic prior to c-sec - Zantac & Bicitra or Reglan: to neutralize acids in the stomach o Laboratory studies o Prophylactic antibiotics everybody gets it before baby is born Ancef If allergic to Ancef, give ampicillin Everybody get’s their abdomen clipped/shaved o Skin prep o Foley catheter IncisionEXAM 3 54 o Low transverse o Low vertical- (can get a no doctor will take the chance to do a vaginal delivery o Classical o Shave mom to symhis pubis Cesarean Birth: Nursing Considerations Provide emotional support Teach Promote safety Provide postoperative care Different degrees of lacerations 1° involves the outermost layer of the vagina itself but no muscles 2° deeper tear, into the muscle underneath 3° tear in vaginal tissue, perineal skin, perineal muscles that extends into the anal sphincter 4° goes through anal sphincter and the tissue underneath it Moms must have Week 5 Notes- CHPT 10 Complications of PregnancyEXAM 3 55 Hemorrhagic Conditions of Early Pregnancy All abortions 20 weeks or below- 1st trimester Spontaneous o Congenital/chromosomal abnormalities incompatible with life) when the body Threatened o Patient came to ED and is bleeding (18wks)..expect threated abortion- pad count Inevitable o It’s going to happen…pt is dilating (cervix is changing nothing can be done about it) Incomplete abortion o Some products of conception still inside o D&C or D&E (dilate & evacuate-using a vacuum) Action: we’ll do a cerclage Complete o All products of conception have been expelled Missed o Fetus has died inside uterus (everything has remained inside) o o Amenorrhea o N/V o Fatigue o Urinary frequency o Breast changes o Vaginal & cervical color changes o Quickening (fetal movement) o Recurrent spontaneous o Patient has had 3 or more abortions (can be from abnormally shaped uterus, incompetent cervix (starts to dilate doesn’t stayed closed, chromosomal abnormalities) o We need enough progesterone in our bodies to maintain the pregnancy o Incompetent cervix (pt gets to so many weeks & the cervix start to open up/ dilate) *We need to know the s/s Incompetent cervix: Done around 16wks Patient is put to sleep for procedure to be done Cerclage (dr. will remove around 36 or 37wks)- 1 stich that holds the uterus closed. If it’s not taken out, the mom & baby can create a tear if it tries to dilate. (THE 1 STITCH MUST COME OUT). If cesarean, they’ll take stich out before c-section We watch mom for 24 hours Monitor her contractions & the fetus We’re going give her betamethasone (lung maturity) once she’s 24wks Complication of cerclage is her water can breakEXAM 3 56 Disseminated intravascular coagulation (DIC)- life threatening complication of abruptio placentae in which procoagulation factors are simultaneously activated Tiny, tiny clots in the bloodstream Drug of choice: heparin Ectopic pregnancy-1st trimester Implantation of a fertilized ovum outside of uterus Where the ovum is implanted in the fallopian tube Fertilized ova not in the uterus (can be caused by recurrent pelvic infections) s/s lower abdominal pain that’s on either side, radiates up to the shoulder of affected side. (ex. If mom has a problem w/ left fallopian tube, it will radiate to the left shoulder) Patient will have s/s Positive preg test Missed period Spotting Severe pain-abdominal pain TX: Methotrexate (stops cell division) o Hopefully to shrink it, so pt. can pass it- dissolve it o Assess for hypovolemic shock o If that doesn’t work: surgery mom will need some psych help because of ectopic pregnancy if ectopic pregnancy ruptures, it can rupture the whole tube: ampular, fimbrial, isthmic Gestational trophoblastic disease: form of cancer (detected in 1st trimester) hydatidform Positive pregnancy test HCG levels rise very quickly Uterus enlarges very quickly No heart beat No fetus Can have up to 69 chromones Severe am sickness (usually) Excessive/Severe N/V Brownish discharge *THERE IS NO BABY IN HERE TX: Dr. need to evacuate (D&E) the pregnancy (the mole) hydatidiform Dr. will then run an MRI or CT of chest- want to see if it’s traveled to the lungsEXAM 3 57 Teach: DO not get pregnant for 1 full year. hCG levels will be drawn 6 wks postpartum & then drawn q month for 6 months postpartum. Have a CT on lungs just in case. It’s a form of cancer & the next place it metastases is their lungs Next 6 months draw every other month Watching hCg levels for 1 full year; tell/teach patient cannot get pregnant for 1 year (12 full months) If she gets pregnant again, we don’t know if it’s the pregnancy of hydatidiform Can be a form of cancer Hemorrhagic Conditions of Late Pregnancy Placenta Previa- usually occurs in 2/3rd trimester Vaginal (external)bright red bleeding no pain; NEVER DO VAG EXAM (because you can hit that dirty Duncan side of the placenta & it can cause major bleeding)- must have a C-section- Fetal well being is our main assessment. Can break off part of the placenta or cause hemorrhage. IT’S NOT BECAUSE WE WANT TO RUPTURE MEMBRANES Low transverse C-section & placenta will come out 1st Marginal Patient can deliver vaginally (placenta implanted in lower uterus, but its lower border is >3cm from internal cervical os) doesn’t cover any part of the uterus & the placental edge just reaches the internal os Partial- already diagnosed at 16wks Cannot deliver vaginally (lower border of placenta is w/in 3cm of internal cervical os but does not fully cover Total- already diagnosed at 16wks Cannot deliver vaginally (placenta completely covers internal cervical os) MUST HAVE CESAREAN- fetus will die if delivered vaginally Very first thing you do First time (placenta previa) o Monitor Fetal heart tones- (make sure baby is still alive) right away. Will be on strict bedrest. & they’ll do an U.S to see where it is. It should stop Second time o Bedrest Third time they come in: (only allowed to have 3 bleeding episodes) o Must have C-Section/ *all this bleeding (bright red) but NO pain for placenta previa- 1st thing to do is find those FHT to make sure baby is still alive. Type & cross is ready in case they have to transfuse her. Assessment- fetal well bleedingEXAM 3 58 Abruptio placenta- abprution- usually in 2/3rd trimester w/wo external bleeding, internal bleed but PAIN where placenta has detached from the uterine wall. Determining cervical dilation and effacement Partial Part of placenta (can see a small hole) came detached from uterine wall (usually will form a blood clot’ bleeding will stop; done through U/S Marginal Half of placenta has detached (will see late deceleration) mom may have external bleeding may not- placental insufficiency Complete Entire placenta has detached from uterine wall (baby will die w/i a matter of minutes) caused by drug use: cocaine Uterine bleeding where abruption occurred Abdomen hard/firm/rigid board-like- concealed hemorrhage (when the edges of the placenta do not separate) because that’s where the blood is filling up the uterus Causes of abruption placenta (manifestations) #1: HTN (hypertension)- per ATI cause vasoconstriction Cocaine Trauma Smoking Short cord Ruptured membrane- water breaks diabetes *assessment: Fetal well being *Call U/S find out what’s going on Hyperemesis Gravidarum Cause unknown Some women can’t keep anything Give mom something to calm her stomach Brought into hospital Give iv therapy Start her off on small clear liquid feedings COMPLICATIONS: dehydration & starvation Watch for signs of dehydration Needs to be hospitalized, given IV, & give TPN if she can’t keep down nutrients. Emotional support is essential to the care of this client: she needs to express Therapeutic management Promethazine (Phenergan) suppository Diphenhydramine (Benadryl) Histamine-receptor antagonistsEXAM 3 59 Gastric acid inhibitors Metoclopramide (Reglan) Ondansetron (Zofran) sublingual Hypertensive Disorders of Pregnancy-Gestational, Preeclampsia, Eclampsia, & Chronic HTN Gestational hypertension Fetus causing the HTN- Develops after 20 weeks gestation Goes away after she delivers baby which is the cure Criteria o Develops after 20 weeks of gestation o PROTEINURIA ABSENT o BP return to normal by 6wks postpartum- is the cure (delivery of the baby) Morbidity is directly r/t the degree of HTN Eclampsia: seizure; pt has seized Occurs after 20wks Chronic HTN Already had HTN Diagnosed under 20wks gestation (develops before 20) convulsion *Elevated BP in L & D Considered greater than or equal to 140/90 Chronic HTN diagnosed before 24 weeks gestations, BP >140/90 Came into that 1st prenatal visit w/ bp >140-180systolic & >90 Watch diet Increase exercise Decrease NA intake More proteins and carbs More frequent prenatal visits Relieve some stress in life *Drug of choice: Aldomet (methyldopa), can give: calcium channel blockers or beta blocker *Never give pregnant women: ACE inhibitor or diuretics Preeclampsia: pre-seizure (BP is so high, she can sz); can happen while pregnant or Postpartum Develops after 20 weeks Spilling protein in urine (should not have any protein in pregnant women’s urine)EXAM 3 60 Gestational HTN can turn in preeclampsia s/s gen swelling, spots before eyes (visual disturbances), headaches, protein in the urine, epigastric pain (if severe, will be hospitalized & be on modified bedrest & watch her diet if it’s more severe, she can have pain under ribs (HELLP) (Ex. Bp 210/100 as soon as we get the give IV in. 1st give hydralazine (antihypertensive med given during pregnancy) or labetalol IV push.) WE DO NOT WANT PT TO HAVE A SEIZURE SO WE NEED TO BRING THE BP DOWN AS FAST AS WE CAN. Next give magnesium sulfate MGSO4 (it’s a smooth muscle relaxer & ANTICONVULSIVE) can SIDE EFFECt: LOWERS BP. bolus dose 1st usually a concentrated amount of MGSO4 usual a bolus of 4g/50ml solution NS fast ran in 20 or 30 minutes. Maintenance dose 2gms/hr. 1gmMgSO4=25ml’s (ex. 20min’s set pump 2/1hr=3 3x50ml=150mL) after this is done 2gms/hr.: maintenance dose Standard 1gm MGSO4=25mL Ex. 25mL x 2gms=50mL MGSO4- (normal/expected finding) TEACH feel like you’re burning up inside out, nauseated, hot flash, Hot flush, blurred vision, N/V, makes you feel like crap, sleepy Action: bring fan in room, cold compress, bring big basin (emesis) or garbage can because she’s going to feel real bad after getting the bolus that’s being ran in quickly. Fluid restriction 125mL EX. Pt on 100ml & now the pt will need Pitocin because pt BP is too high & baby needs to be induced. As we increase Pitocin, we will need to decreased LR. Pt is at risk for POSTPARTUM HEMORRHAGE when on MGSO4 & PITOCIN at the same time if given during labor. MONITOR FOR PPH While pt is on MGSO4 which makes more sleepy. We’re going to expect our pt’s variability to be decreased. Fetus may be depressed may need to resuscitate before apgar & skin to skin. Preeclampsia Early prenatal visit Check urine q week Can take low dose aspirin q day (81mg) Magnesium sulfate Anticonvulsant medication (don’t want pt. to seizure) Smooth muscle relaxer Preterm labor *Mom coming into hospital: BP 226/156 Start this ASAP: Hydralazine (IV push) STAT o Hang bag off LR o give 4g Mag Sul (bolus) in 50mL solution run over 20 minsEXAM 3 61 o 2gms/hr.: maintenance dose Warn mom about- EXPECTED FINDING (EXPECTED ADVERSE EFFECT) o N/V o Flushed skin o sweating o Very hot from inside out o Give emesis bag o Fan *Dr. will limit amount of IV fluids this pt. can have (125ml/hr.) Don’t want to give pt. pulmonary edema *Mag Sul: ALWAYs piggybacked into another IV so mom doesn’t go into respiratory distress. on a pump by itself, tubing is labeled, bluish in color, has NO PORTS, cant put anything into this, lowest port 1gm=25mL Ran at 2gms/hr Monitor Intrapartum If you go up on Pitocin, go down on the LR All have open pump by it’s self- bluish in color, labeled, can’t put anything into this, must be piggybacked into the pt’s mainline. Lowest port (hand) LR Mag Sulfate M Pitocin What we want to check for, for a pt. on Magnesium sulfate (q 1hour, if on Pit q 30mins for24 hours) HR RR <12=stop MGSO4 call HCP B/P Output <30ml stop MGSO4 call doctor Deep tendon reflex (brisk reflexes before medication) (while on MGSO4 will have diminished DTR’S) if DTR’S are gone=STOP MGSO4 CALL HCP (hyporeflexia) LOC-cant wake pt w/o falling asleep= STOP MGSO4 CALL HCP O2 stat (continuous; leave pulse ox on finger) LOW O2=STOP MGSO4 CALL HCP FHR fetal(if she’s pregnant) if not we’re checking FUNDUS When baby is delivered will need to monitor for RR q1hr check check fundus after postpartumEXAM 3 62 edema- quantified by daily weights) needs to be on bedrest- use bedpan Calcium gluconate: antidote for Magnesium Sulfate (mag toxicity)- for any of the above decline standing order- 10mg IV push If mom is on Magnesium sulfate during labor must stay on 24hrs after labor, after 24 hours shut off Leave running b/c of preeclampsia mom has. Magnesium sulfate Also used for preterm labor (to stop contractions) c Pt with preeclampsia Will have generalized edema Mom will get weighed daily Lab findings Urine dipstick for protein 24hour urine CBC CMP LIVER ENZYMES URIC ACID FETAL KICK COUNTS NST BPP AMNIOCENTESIS FOR FETAL LUNG MATURITY-if she need to delivered early & will be given betamethasone STEROIDS IF PREMATURE DELIVERY ANTICIPATED CERIVAL RIPENESS ASSESSMENT Vs-document maternal position Pulse ox reading LOC Headache Visual changes Lung sounds- if she on bedrest & fluids Epigastric pain Edema ReflexesEXAM 3 63 Clonus-when grabbing moms foot and it doesn’t go back immediately, you would count beats of clonus till it goes back Weight gain urine output HELLP syndrome: life threatening (sickest she can get) severe preeclampsia Hemolysis Elevated Liver enzymes up AST 5-40 ALT 7-56 Low Platelets (below 100,000) Symptoms Upper right quad tenderness (pain under ribs) Don’t palpate around liver (or abdomen) N/V *Get patient delivered ASAP Adolescent Pregnancy Socioeconomic status has the highest on fetal well-being Assessment Determine the degree of participation by the father Amount of family support Delayed Pregnancy Disadvantages o High risk of abnormalities o Down syndrome Substance Abuse Tobacco- higher risk for abruptio placentae o These babies are born addicted to nicotine o Childhood obesity o Colic o asthma Alcohol o Can cause spontaneous abortions o Abruptions o Neuro developmental disorders o Alcohol related birth defects o CNS impairment o Intellectual disabilities o Poor short-term memory CocaineEXAM 3 64 o Can cause abruptions o Neonatal abstinence syndrome o CNS depressant o Fetal growth restrictions o Stillbirth o Low birth weight o Higher incidence of SIDS Heroin o Preterm labor o Precipitous delivery Adoption Process Therapeutic communication Teaching infant care to adoptive parents Rhogam injections Betamethasone cause a reduction in respiratory distress in a newborn. It’s given to stimulate fetal lung maturity & prevent respiratory distress between 24-36 wks Lung maturity must be checked before a cesarean Edema +1- edema of lower extremities +2- marked edema of lower extremities +3- extremities, face, & sacral +4 includes accumulation of the fluid in the peritoneal cavity Week 6 Notes Concurrent Disorders During Pregnancy DM Type 1, II, GD Cannot metabolize carbohydrates Caused by a partial or complete lack of insulin secretion by the beta cells of the pancreas Without insulin, glucose accumulates in the blood (hyperglycemia) Classic symptoms of diabetes Polyuria Polydipsia PolyphagiaEXAM 3 65 Effect of pregnancy on fuel metabolism Early pregnancy 1-20 wks. 1st trimester Small change in maternal metabolic need Insulin release in response to serum glucose levels accelerates. May experience hypoglycemia-vomiting may cause it or she doesn’t eat during 1st trimester Late pregnancy 20-40 wks. 2nd trimester Fetal growth accelerates Rise in placental hormone levels Hormones create resistance to insulin- so we can give that baby all the glucose that he needs Birth Baby can develop hypoglycemia after birth if mom has a pre-existing diabetes Postpartum Never give pregnant women oral diabetes medicine o Will get insulin The need for additional insulin falls after pregnancy Breastfeeding is encouraged. The added calorie intake by the mother helps lower the amount of insulin needed in women with types 1 and 2 diabetes mellitus. The woman with gestational diabetes mellitus (GDM) usually needs NO insulin after birth o B/c it was due to pregnancy Classification Type 1 Insulin deficient Type 2 Insulin resistant GDM The onset of glucose intolerance due to pregnancy Diabetes Mellitus: Preexisting Maternal effects During first trimester o Hypoglycemia, hyperglycemia, ketosis o Increased incidence of spontaneous abortion or major fetal malformations HTN hypertension, Preeclampsia is two to three times more likely to develop in a woman has pre-existing diabetes Premature rupture of the membranes (PROM)EXAM 3 66 Macrosomia (greater than 4000g or 8.8lbs)-increased risk for GDM Hydramnios- too much amniotic fluid At risk for shoulder dystocia Difficult labors Higher chance of c-section Higher chance of injury to birth canal or baby Fetal effects Congenital malformation o Most common is neuro tube defects Variations in fetal size o Small for gestational age (SGA) o Intrauterine growth restriction (IUGR) o Large for gestational age (LGA) Neonatal effects Hypoglycemia Hypocalcemia Hyperbilirubinemia Respiratory distress syndrome (cortisol production reduced; less amount of surfactant) o Babies born to DM mom have a higher chance of having lungs that aren’t mature. o Give betamethasone *anybody with DM: considered high risk pregnancy *factor important in diminishing maternal, fetal, & neonatal complications in pregnant client w/ diabetes- degree of glycemic control before & during pregnancy Maternal Assessment History Onset and management of diabetic condition May need insulin to control (no oral agent) Physical exam Baseline electrocardiogram (ECG) Ophthalmology referral Height, weight, and blood pressure (BP) Laboratory tests 24-hour urine (drawn for creatine clearance, glucose) Hemoglobin A1c (HbA1c) Fetal Surveillance Surveillance should begin early for women with preexisting diabetes. Testing for anomalies Frequent ultrasoundEXAM 3 67 Fetal echocardiogram Fetal kick count More frequent office visits Therapeutic Management Maintain normal blood glucose levels. Facilitate the birth of a healthy baby. Avoid accelerated impairment of blood vessels and other major organs. Preconception care Diet (eat three meals/day, with three snacks Self-monitoring of glucose Insulin therapy Risk factors Overweight Maternal age older than 25 years Previous birth outcome often associated with GDM GDM in previous pregnancy (large baby) History of abnormal glucose tolerance Family history of diabetes Member of a high-risk ethnic group Gestational Diabetes Mellitus: Screening Ran b/w 24-28 wks. gestation Glucose challenge test doesn’t need to fast o 1-hour test, 50g of oral glucose solution; after 1-hour if greater than 140: (fails) will need to come in another day for the 3hr o If abnormal: 3-hour oral glucose tolerance test (OGTT) 100g of glucose solution Fasting before she comes in Will drink 100g of oral glucose Will do blood sugar 1hr, 2hr, 3hr If has 2 or more will be deemed Gestational Diabetic Oral glucose challenge test (OGT) does not need to fast Fasting, greater than 95 mg/dL 1 hour, greater than 180 mg/dL- failed 2 hours, greater than 155 mg/dL-failed 3 hours, greater than 140 mg/dL- failed Therapeutic Management- after failing glucose test- we’ll have her meet w/ a dietician Diet o Registered dietitian, registered dietary technician, or diabetes educator o Nonobese pre-pregnancy weight, an average of 30 kcal/kg/day is recommended o Obese: 25 kcal/kg/dayEXAM 3 68 (what do you like to eat? When do you eat it? What are the cravings you have?) Exercise Blood glucose monitoring Fetal surveillance- kick counts Nursing Considerations Increase effective communication. Provide opportunities for control. Provide normal pregnancy care. Cardiac Disease: Incidence Acquired from The two major categories of heart disease are rheumatic heart disease and congenital heart disease. Classification Rheumatic heart disease o Sometimes follows a streptococcal pharyngitis o May cause scarring (from rheumatic fever) of the heart valves o The mitral valve is the most common site of stenosis. o May lead to pulmonary hypertension, pulmonary edema, or congestive heart failure Four classes of heart disease Class I-Beginning (small malformation in structure of the heart)- benign Can perform ADL ok Can tolerate pregnancy Class II-stenosis of mitral valve (from rheumatoid fever or strep) prolaspse (undiagnosed) Could be benign & asymptomatic (according to quizlet) Very common Can perform ADL’s ok Can tolerate pregnancy Class III (some type of cyanotic heart lesion Severe stenosis- severe prolapse mitral valve ADL’s very difficult to do-need to rest in between activities Can’t exercise High risk of morbidity & mortality Class IV (severe stenosis of mitral valve) stenosis from that mitral valve from strep they acquired Need help with everything Take shower, need to sit for 30 min Want them to deliver vaginally Slow induction Slow pushingEXAM 3 69 High risk of morbidity & mortality Class III & IV High morbidity and mortality (told not to get pregnant-dangerous for mom) Stage 4 is the hardest on the heart. Because the placenta is holding 500mL of blood in all times. Once that cord is cut before that placenta is delivered. It pushes all that 500 amounts of blood back into the peripheral system. So it’s cardiac overload. Harder stress on mom heart. we rather them deliver vaginally Class III Prob told not to get pregnant Class IV Told NOT to get pregnant (sent to ICU after delivery) hardest part on the heart. We want them to deliver vaginally, we can induce them, we can take their labor slowly, induce them slowly. We do not want them to do much pushing, but they can push a baby out. Unless there’s something wrong w/ the baby we don’t push w/ every contraction. Every other contraction, every 2 contractions but we rather them deliver vaginally. & will always go to ICU after Drug therapy Heparin Anticoagulants Antidysrhythmic Anti-infective (bacterial endocarditis) Drugs for heart failure Diagnosis and classification Assessment for specific signs and symptoms of heart disease is part of every initial prenatal visit. Signs and symptoms of postpartum pt o Dyspnea, syncope (stand up & faint) with exertion o Hemoptysis o Paroxysmal nocturnal dyspnea o Chest pain with exertion (elephant sitting on chest) o Additional signs (hemorrhage, DVT, signs of infection) The severity of the disease is determined by ability to endure physical activity Intrapartum Management 300 to 500 mL of blood is shifted from the uterus and placenta into the central circulation. o Extra fluid causes a sharp rise in cardiac workload. Vaginal delivery is recommended for a woman with heart disease unless there are specific indications for cesarean birth. Minimize maternal pushing and use of the Valsalva maneuver. Limit prolonged labor.EXAM 3 70 **Do not have to push with every contraction Postpartum Management Although no evidence of distress during pregnancy, labor, and childbirth, women may have cardiac decompensation during the postpartum period o Blood from the placenta and uterus increases the workload on the heart. Close observation for signs of infection, hemorrhage, and thromboembolism o Conditions can act together to precipitate postpartum heart failure. Signs and symptoms of congestive heart failure include: o Cough (frequent, productive, hemoptysis) o Progressive dyspnea with exertion o Orthopnea o Pitting edema of legs and feet or generalized edema of face, hands, or sacral area (weigh pt daily) o Heart palpitations o Progressive fatigue or syncope with exertion o Moist rales in lower lobes, indicating pulmonary edema Intervention Teach about increased cardiac workload Excessive weight gain Exertion Exposure Emotional stress Help the family accept restrictions on activity. Provide postpartum care Application of the Nursing Process: Pregnant Woman with Heart Disease Assessment o Vital signs o Fatigue o Signs of congestive heart failure o Weight o Mother’s knowledge base Anemias Iron-deficiency anemia 1000mg daily (shes pale, lethargic, complaints of headache caused by - pica (chew on chalk, ice, dirt, clay, paint chips, baking soda, not really eating) should be eating organ meat & green leafy vegetables Folic acid deficiency anemia (megaloblastic) 600mcg- can have NTD neural- Sickle cell disease- decrease o2 concentration causes sickle cell w/ acidosis & dehydration Thalassemia Infections During Pregnancy: ViralEXAM 3 71 Cytomegalovirus-herpes impetigo (passed through daycares) Rubella- (German measles) rubella titers for 1st prenatal visit- we need to know what her titers are so we can give after her, her vaccine after she delivers. Varicella-zoster Herpes simplex- HSV positive can deliver vaginally. If they have any active lesions during delivery. They will have to be delivered via cesarean 36wks gestation start them on acyclovir prophoactin to hopefully not have any lesions Parvovirus B19 Hepatitis B- give baby Hep B vaccine & HB Human immunodeficiency virus (HIV) give zidovudine (ZDV) & via IV in labor & will give baby when born Nonviral Toxoplasmosis (from changing cat litter; preg. women should not go near cat litter, from eating undercooked meat, should not play in sandbox) Group B streptococci (GBS) (vaginal swab & rectum at 36 wks. gestation) o If pos. when she goes into deliver will get penicillin 5m units; will need to have 4 hours before she delivers to protect the baby. If it’s not given during the 4 hours, baby will need to have blood work drawn to see if baby is septic or any signs of. If mom delivers after 4 hour period & received her 2nd dose, baby does not need to have labs drawn. MOM MUST HAVE THE ANTIBIOTIC IN HER SYSTEM AT LEAST 4 HOURS BEFORE SHE DELIVERS. To work & protect the baby. Usually w/I 4 hours we’ll know if that baby is sick or not Tuberculosis Intrapartum complications Dysfunctional Labor- anything wrong w/ the 5 p’s will give a dysfunctional labor Problems of the powers o Ineffective contractions o Ineffective maternal pushing Fatigue (forceps & vacuum (operative vaginal delivery) baby down low & at +1or +2 station. Forceps baby-assess for symmetry & bruising. Vacuum babyassess head for cephalohematoma Afraid to push/ she’ll tear really bad- mom needs to push Problems with the passenger o Fetal size (macrocosmic baby) o Abnormal fetal presentation or position (baby should be vertex, cephalic) o Multifetal pregnancy o Fetal anomalies (hydrocephalic head)EXAM 3 72 Problems of the passage o Pelvis o Soft tissue obstructions Problems of the psyche o Stress o Pain Abnormal labor duration o Prolonged (come off Friedman’s curve) o Precipitate (L&D; everything happen within 3hrs) dangerous for both mom and baby Placenta abruption Uterine rupture Baby: respiratory distress syndrome, intracranial hemorrhage, petechiae Causes: cocaine, **Babies that come out with petechiae higher risk of jaundice** o Hypertonic Uncoordinated dysfunction contractions Decreases uterine blood flow o Hypotonic Dysfunctional o Arrest of dilation Mom’s dilation has stopped; not having any more dilation o Arrest of decent Baby not coming down anymore; has stopped descending through pelvis A women having 1st baby should dilate 1-2 cm q hr. 2nd baby: should dilate ½ cm q hr. McRoberts’s maneuver Used for shoulder dystocia 5-7 mins to get baby out 1st call for help Mom is going to grab behind her knees & pull her legs back as far as she can. 2 nurses are going to assist her w/ pulling her legs as far as she can. Helps flatten out the sacrum. It should give the baby more room to come through. If it doesn’t work, along w/ Mcroberts is suprapubic pressure. Doctor will tell us what angle to do the pressure. We’re going to go behind the symphysis pubis & put pressure as hard as we need it, if that doesn’t work. He’ll do a corkscrew maneuver & try & turn the baby. If that doesn’t work dr. will try to deliver the posterior shoulder. Its’been almost 6 minutes, he’ll do a Zavanelli manuever by pushing the baby back in & do an emergency cesarean. If McRoberts’s don’t work- we’ll do suprapubic pressureEXAM 3 73 Shoulder dystocia (emergency situation)- turtle sign (heads deliver, shoulder stuck) 5-7 minutes to get the baby out alive Check baby for cracked clavicle- when using suprapubic pressure Check for movement of the arm (palsy) RN: get a step stool (look at the clock & note: head delivered at) doctor has 5-7min’s to get the rest of the baby out. Get the pt do a McRobert’s maneuver. So the doctor is going to tell mom to bear down & push & he will tell us to push to the left or right while we supra pubic pressure. NEVER do fundal pressure If suprapubic worked, we Intrauterine infection from: Catheters Too many vaginal exams Once moms water breaks, to keep from getting intrauterine infection Wash hands Wipe from front to back Limit vaginal exams Change pads often *Temp is checked q two hours *Temp suggest infection; anything greater than 100.4 *If mom has fever, babies HR will go up *Will do cultures on baby after delivery Maternal exhaustion Allow mom to rest (she doesn’t have to push with q contraction, unless baby is compromised) Dim lights Music Premature rupture of the membranes Prior to 37 wks. Causes: Chorioamnionitis (infections of membranes) Tear in amniotic sac Weak amniotic sac Previous preterm ROM Incompetent cervix How to know water has broken (amniotic sac ruptured) Cotton swab, sample of secretion put under scope; if it looks like a fern she has rupturedEXAM 3 74 Under 24 wks. water broke Vaginal rest at home Check temp q 2-4 hr. Restricted activity Avoid nipple stimulation Any odor coming from vagina: call DR Once 24 wks. will bring into hospital **Mom ruptures at 34 wks.: most dangerous Preterm labor Contractions w/cervical changes, cramps UTI Shortened cervix Socioeconomical status Fetal issues TX: try to stop with Tocolytics ( 3 shots within 20 mins) Terbutaline (asses HR first Mag Sulfate for 24 hrs., weaned off and monitored 24 hrs. Prolonged Pregnancy: Post Date patients Anything greater than 42 wks. Placenta can calcify Great ppl for serial inductions (using diff methods of induction at one time) o Break water o Pitocin o Ripening cervix *Doing BPP, NST Intrapartum Emergencies Placental abnormalities Prolapsed umbilical cord (late decelerations) o Emergency situation- we may not see it coming it through the vagina o RN you will put your 2 fingers in the vagina & put pressure & lift up on the presenting part of the fetus to get pressure off of the cord Uterine rupture Uterine inversion o Too much tugging on the cord. Pulled the uterus out & it’s lying between her legs. Turned the uterus inside out. Anaphylactoid syndrome TraumaEXAM 3 75 Postpartum Maternal Complication Assessing: One hand is cupped to massage and gently compress the fundus toward the lower uterine segment The other hand remains cupped against the uterus at the level of the symphysis pubis to support the uterus **Postpartum hemorrhage is the leading cause of maternal death worldwide. Bright red blood Uterine laceration Cervical laceration Vaginal laceration Postpartum Hemorrhage Early postpartum hemorrhage o Uterine atony (dark brick red; old blood) Boggy (feels like cheek); weak o Trauma (bright red blood) Late postpartum hemorrhage o Subinvolution Uterus not going back down to normal size fast enough o Retained placental fragments Vaginal hematoma after birth Dr. will take pt back to OR, lance it and drain it out Hypovolemic Shock Early signs: o Increased BP, pulse, anxiety, respirations (deep), cool, clammy (moist) o First thing you should do: o Get an IV started or 2nd IV started o Increase IV fluids, 2nd IV; if she needs blood o Do ABCs o O2 non-rebreather mask: 8-10L* Do this FIRST o Set monitor to take vitals q 10mins o One of the main things to do: find the source of the bleeding and stop it Late signs: o BP u,EXAM 3 76 o Pulse increased, but weak o Pale o Com, o Respirations shallow Woman with Excessive Bleeding (not quite hemorrhaging) Assessment o Uterine atony or trauma Intervention o Check the uterus (fundus) o Check the bladder o Check the skin o Weigh pads o VS q 15 mins Subinvolution of the Uterus (uterus should return 1 fingerbreadth a day) Definition o Slower-than-expected return of the uterus to its nonpregnant size Causes o Retained placental fragments o Pelvic infection Therapeutic management o Oral methergine (10mg) o Pelvic infection Methergine and oral antibiotic *Hemabate: causes explosive diarrhea Thromboembolic Disorders Superficial Venous Thrombosis Clinical signs and symptoms o Swelling o Tenderness o Redness (lil) o Warm o Bilateral Therapeutic management o Warm pack o Analgesics (Tylenol, ibuprofen) o Rest o Elastic stockings o Elevation of lower extremities Do not give anticoagulant or anti-inflammatoryEXAM 3 77 Deep Venous Thrombosis Signs and symptoms o Swelling o Erythema o Hot o Positive Homan’s sign o Tender o Unilateral Diagnosis o Doppler o Magnetic resonance imaging (MRI) Therapeutic management o Prevention of thrombus formation With early ambulation In hospital will have on SCD TX: o Pt. will be on bedrest o Given anticoagulant (Warfarin) o Still pregnant and develop DVT: Lovenox *Very important to check pedal pulses Pulmonary Embolism Clinical signs and symptoms o Dyspnea, chest pain, tachycardia, and tachypnea o Pulmonary rales, moist cough o Hemoptysis (expectoration of blood or bloody sputum) o Abdominal pain o Low-grade fever Therapeutic management o First thing you do elevate HOB o O2 o Stat ABG o Give heparin o Lay on left side Puerperal Infection Bacterial infection women get after birth o From: breast engorgement, pyelonephritis, respiratory complication after c-sec TX: Antibiotics Rest Lots of fluids Endometritis Infection of lining of uterusEXAM 3 78 Clinical signs and symptoms Chills, Malaise, Abd. pain Cramping, Anorexia TX: IV antibiotics Pain meds Wound infection C-section, Episiotomy, Laceration TX IV antibiotics *When ask pt to roll to side looking for: Infection, blood, approximated UTI Frequent urination Burning Cloudy urine TX: Increase fluids Oral antibiotics (drug of choice: Bactrim; unless allergic to sulfur) Suggest drinking pure cranberry juice Mastitis Infection in the breast Cracked nipples: more chance of developing mastitis; cracked nipple: rub colostrum on nipple Flu like symptoms: fever, chills Usually only 1 breast (unilateral) Continue breast feeding; unless blood then: Pump and Dump (DO NOT SKIP FEEDINGS) breast feed on both sides & empty the breast. Women who doesn’t wash hands: Most at risk TX: Warm compress Analgesic Septic Pelvic Thrombophlebitis Infection of the ovarian veins Clinical signs and symptomsEXAM 3 79 Groin pain Abd. pain Flank pain: radiates Fever Tachycardia Vomiting Distress Decrease bowel sounds TX: Anticoagulant Analgesic Assessing for Anomalies Head Fontanels- anterior fontanelle is diamond shape, posterior triangular shape There are little lines that come from these fontanels that are called sutures. The sutures are what allows the baby’s head to squish down & mold to come through the birth canal. Caput succedaneum- is what’s delivered 1st. It’s swelling and maybe some clear fluid build up between the skull and the scalp. It’s from being in the birth canal too long. It will go away in 1-2 days. Caput cross those sutures lines Cephalohematoma- caused by trauma, it does not cross those suture lines. It’s in one area of the scalp. Buildup of blood & takes 3-4 weeks for that blood to be absorbed into the baby’s peripheral system. Low set ears- sign of down syndrome Neural Defect Spina Bifida o Sacral Dimple- spread those cheeks o If you see a hole, notify HCP Observe for hip click Check for anal patency Assessing Neurologic System Reflexes Sensory assessment Other neurologic signs Jitteriness (tremors) signs of hypoglycemia Seizures- baby straightening out extremities w/ tiny shakes (rigid) Irritability Facial bruising is probably from a quick delivery Baby may have a lot of petechia or facial bruising If the baby was covered up to his neck, you would think the baby was blueEXAM 3 80 1st action- uncover him Then see if his mucous membranes are pink. Oral Cavity Take your gloved finger & make sure his pallet is closed Gonna see if he can suck on his finger. Check his neck & abdomen & make sure it’s not distended & that it’s soft Baby should have bowel sounds 3 hours after birth Umbilical hernia- baby will have to have surgery Babies that are stretched out are more premature Flexed babies are termed Feet Creases in feet are termed babies Smooth feet are premature Legs Creases on back of legs should be equal They should go straight across. 1 leg creases should be equal w/ the other leg creases. If not equal, there may be a little hip displacement Little girls The more term the baby is, the labia majora is going to cover everything The more preterm, the clitoris is going to be more prominent than anything else. Little boys Look at genitals Check scrotum to make sure both testes are down in the scrotum They’ll feel like tiny peas. You have to check each side. Hypospadias- if you notice part of his skin is gone & he did not have a circumcision. This baby was born this way. He doesn’t have all of the foreskin. We do not do a circumcision on them. They need to see a urologist. Because maybe the meatus is not at the tip of the penis. It might be at the side. May need some of the foreskin to do reconstructive surgery. So do not do circumcisions. Newborn Pearl- White spot at end of penis. Nothing to worry about. Floppy Tone Baby is not flexed Pick up baby arm & falls back down Full term baby, you could pull up arm & he will pull it back -Jittery- sign of low BS- heel stick on outer part of foot. -Rigid- could be sign of seizureEXAM 3 81 -Absence of startle reflex Take babies wrist. Pull him up by his arms & his body off the bed & let go & he should startle & if he doesn’t then we’re worried. This floppy tone is not normal Reflex Moro or startle reflex Take babies wrist. Pull him up by his arms & his body off the bed & let go & he should startle & if he doesn’t then we’re worried. Palmer grass reflex- putting your finger in the baby’s palm. He should grab your finger The plantar reflex- Put your finger at the base of the baby’s toes & it should flex, it should grab your finger. The Babinski reflexes is elicited by stroking the lateral sole of the infant’s foot from the heel forward & across the ball of the foot. This causes the toes to flare outward & the big toe to dorsiflex. Sucking reflex You put your finger in the baby’s mouth & he starts sucking on your finger Integumentary System Color Lanugo-hair on the baby (peach fuzz) Milia-little white dots on the baby’s nose. Leave them alone. Don’t touch them Marks from delivery- if the baby is forceps or vacuum baby. Check for trauma Breast, hair & nails- just document. Expected findings Mongolian spots dark area on buttocks they do get lighter with age. (not a bruise) Stork bites eyelids. appears when baby gets really upset. They get real dark. They will fade w/ time. Port wine stain- these babies that are born w/ this does not go away. Permanent birth mark on face. Face is asymmetrical Newborn Assessment Axillary temp HR taken for 1 full minute. VS when sleeping Blood pressure & VS will be taken on all 4 extremities on a newborn if heart murmur is heard.EXAM 3 82 Are there bleeding coming form the cord? 2 arteries & 1 veins at delivery, but once the cord starts to dry up, you won’t be able to see those anymore because it will turn into scab. Any discharge Apgar Score∗ Points Assessment 0 1 2 Heart rate Absent Below 100 beats per minute (bpm) 100 bpm or higher Respiratory effort No spontaneous respiration s Slow respirations or weak cry Spontaneous respirations with strong, lusty cry Muscle tone Limp Minimal flexion of extremities; sluggish movement Flexed body posture; spontaneous and vigorous movement Reflex respon se No response to suction or gentle slap on soles Minimal response (grimace) to suction or gentle slap on soles Responds promptly to suction or gentle slap to sole with cry or active movement Color Pallor or cyanosis Bluish hands and feet only (acrocyanosis) Pink (light skinned) or absence of cyanosis (dark skinned); pink mucous membranes 0 1 2 3 4 5 6 7 8 9 10 Infant needs resuscitation.† Gently stimulate by rubbing infant’s back while administering oxygen. Determine whether mother received narcotics, which may Provide no action other than support ofEXAM 3 83 Points Assessment 0 1 2 have depressed infant’s respirations. infant’s spontaneous efforts and continued observation. ∗ The Apgar score is a method for rapid evaluation of the infant’s cardiorespiratory adaptation after birth. The nurse scores the infant at 1 minute and 5 minutes in each of five areas. The assessments are arranged from most important (heart rate) to least important (color). The infant is assigned a score of 0 to 2 in each of the five areas, and the scores are totaled. Resuscitation should not be delayed until the 1-minute score is obtained. However, general guidelines for the infant’s care are based on three ranges of 1- minute scores: 0 to 2, 3 to 6, 7 to 10. † Note: Neonatal resuscitation measures, if needed, do not await 1-minute Apgar scoring but are instituted at once. Skin-to-skin contact with a parent also maintains the infant’s temperature and promotes bonding between the infant and parent. Delaying the first bath for several hours allows the temperature to stabilize. Avoid positioning yourself between the infant and the radiant heat source in the warmer. The infant should be wrapped in dry, warm blankets when not in the warmer or making skin-to-skin contact. Remove wet linens, replacing them with warm and dry ones. A stockinette cap further reduces heat loss if it is placed on the baby’s dry head. A cap is not worn while the infant is in the radiant warmer because the cap slows transfer of heat to the baby. Term: 37 weeks or greater 20 weeks gestation when the organs are done being formed G- # of pregnancies T- # of term deliveries (37-41 6/7 weeks) P- # of preterm deliveries (20- 36 6/7 weeks) A- # of abortions (less than 20 weeks) 19 6/7 weeks L- # of living children Fetus cannot survive before 20 weeks Components of the Birth Process Five major factors that interact Powers o Contractions o Maternal pushing Passage o Pelvis Passenger o Baby o Placenta o MembranesEXAM 3 84 Baby can’t come out if it’s extended or hyperextended Psyche (how mom feels about pushing) o Anxiety o Culture and expectation o Birth as an experience o Support o Impact of technology Position o Fetal head position o Want baby to be in an anterior position (occipital) OA o OT- occipital transverse Presentation Fetal part that first enters the pelvis Cephalic o Vertex, military, brow, face Breech o Frank, full, footling Shoulder Cephalic Presentation The cephalic presentation is more favorable than others for the following reasons: • The fetal head is the largest single fetal part, although the breech (buttocks), with the legs and feet flexed on the abdomen, is collectively larger than the head. After the head is born, the smaller parts follow easily as the extremities unfold. • During labor, the fetal head can gradually change shape, molding to adapt to the size and shape of the maternal pelvis. • The fetal head is smooth, round, and hard, making it a more effective part to dilate the cervix, which is also round. Cephalic presentation has the following four variations (Fig. 12.8): • Vertex—This is the most common type of cephalic presentation, in which the fetal head is fully flexed. It is called a vertex or occiput presentation and is the most favorable for normal progress of labor because the smallest suboccipitobregmatic diameter is presenting. • Military—The head is in a neutral position, neither flexed nor extended. The longer occipitofrontal diameter is presenting. • Brow—The fetal head is partly extended. The brow presentation is unstable, usually converting to a vertex presentation if the head flexes or to a face presentation if it extends. The longest supraoccipitomental diameter is presenting. C-section • Face—The head is extended, and the fetal occiput is near the fetal spine. The submentobregmatic diameter is presenting. C-section Breech Presentation A breech presentation occurs when the fetal buttocks or legs enter the pelvis first, which happens in approximately 3% to 4% of births. Breech presentation is more common in preterm births, hydrocephaly (enlargement of the head with fluid), multiple gestations, abnormalities of the maternal uterus and pelvis, and with placenta previa (placenta in the lower uterus) (Cunningham et al., 2014). Breech presentations are associated with the following disadvantages: • The buttocks are not smooth and firm like the head and are less effective at dilating the cervix. • The fetal head is the last part to be born. By the time the fetal head is deep in the pelvis, the umbilical cord is outside the mother’s body and is subject to compression between the fetal head and the maternal pelvis. • Because the umbilical cord can be compressed after the fetal chest is born, the head should be delivered quickly to allow the infant to breathe. This does not permit gradual molding of the fetal head as it passes through the pelvis.EXAM 3 85 The breech presentation has the following three variations, depending on the relationship of the legs to the body (Fig. 12.9): • Frank breech—This is the most common variation, occurring when the fetal legs are extended across the abdomen toward the shoulders. • Complete breech—This is a reversal of the usual cephalic presentation. The head, knees, and hips are flexed, but the buttocks are presenting. Full breach- tucked in & flexed but upside down • Footling breech—This occurs when one or both feet are presenting. Shoulder Presentation The shoulder presentation is a transverse lie and accounts for only 0.3% of births (Cunningham et al., 2014). It occurs more often with preterm birth, high parity, prematurely ruptured membranes, hydramnios, and placenta previa. A cesarean birth is necessary when the fetus is viable (one of a gestational age that might survive). Fetal lie Orientation of the long axis of the fetus to the long axis of the woman (baby’s spinal cord to mom’s spinal cord) In more than 99% of pregnancies, the lie is longitudinal and parallel to the long axis of the woman There are 3 lies: vertex, oblique, and transverse.EXAM 3 86 Transverse lie is immediate c-section-horizontal Normal Labor: Premonitory Signs Braxton Hicks contractions Lightening Increased vaginal mucus secretion Cervical changes o Softening o Possible dilation o Bloody show- associated w/ cervical dilation & effacement expected finding Brownish vaginal discharge True Labor Contractions w/cervical change Increased contractions Increased discomfort Cervical change: progressive effacement and dilation most important False labor Contractions inconsistent Discomfort is more annoying than truly painful Cervix does not changeEXAM 3 87 Cervix has not shortened Membranes still intact Labor Mechanism- cardinal movements Descent o Movement of fetus through the birth canal Engagement- fetal positioning o Fetal presenting part reaches 0 station o Baby’s head has to be at ischial spine to be considered 0 station o Station- where is babies head according to mom’s pelvis Flexion Internal rotation Extension External rotation Expulsion Stages of Labor 1st stage: 3 phases o Latent phase: 0-3 cm (putting on make-up, doing hair) o Active phase: 4-7 cm (starting to ask for pain meds) o Transition phase: 8-10 cm (no epidural; wants to be left alone, epidural: feeling ok) 2nd stage o 10 cm: delivery of baby o Pushing stage 3rd stage o Delivery of placenta (usually happens 20-30mins after) 4th stage o First 1-4hrs post delivery The cervix usually hangs down 2cm from the uterus this is 0% effaced. When we can no longer feel the cervix(paper thin) this is 100%. Don’t push until completely dilated and 100% effaced. During labor dilation and effacement occur at different rate Ex. 90% and 5cm A preceptor will have a new nurse close her eyes and put fingers into a plactic mold. The contraction starts at the top of the uterus or fundus- only the top 2/3 of the uterus is active. The lower1/3 is passive. Push ball through the sock to show how the cervix opens. Blood flow to the placenta decreases during a contraction.EXAM 3 88 The muscle fibers of the uterus constrict around the maternal spiral arteries, which supply the placenta. There is a relative increase in the woman’s blood volume. This temporary change increases her blood pressure slightly and slows her pulse rate. • Vital signs are best assessed during the interval between contractions. Supine hypotension (aortocaval depression) may occur during labor if the woman lies on her back. The woman should be encouraged to rest in positions other than supine to promote blood return to her heart. Determine gestational age Ultrasound sound-measure fetus from crown to rump or butt to head Fundal height 20wks is at umbilicus Neagel’s rule Interventions: Provide comfort (non-pharmacological and pharmacology). Nonpharmacological: changing positions, warm shower or bath, massages between contractions, breathing techniques, ice or fluids for dry mouth. Pharmacological: epidural etc. Encourage frequent urination to keep bladder empty (full bladder prevents uterus from contracting properly and can slow down labor), monitor vitals of mother and fetal heart rate Chapter 18 – Postpartum Maternal Complications Assessing the fundus One hand is cupped to massage & gently compress the fundus toward the lower uterine segment. The other hand remains cupped against the uterus at the level of the symphysis pubis to support the uterus *PPH is the leading cause of maternal death worlwide Early PPH postpartum hemorrhage risk o Uterine atony – uterus remains inadequately contracted (bladder (full) distention, retained placenta fragments) Multi-fetus (multigravida) Macrosomia Having another baby within a year of the last Magnesium sulfate & oxytocin o Trauma (bright red blood)- precipitous delivery(fast delivery <3 hr) ClotsEXAM 3 89 (1st thing you do is assess the fundus to find it’s firm & midline) Don’t massage because it’s already firm (no uterine atony). Action: call doctor, may be a laceration. No massage or medication is going to help her. HCP needs to come in & find the source Bright red blood Uterine laceration Cervical laceration Vaginal laceration Late PPH o Retained placental fragment (stuff left inside) o Subinvolution (uterus stay distended longer than should) (NOTE: involution- is when the uterus turns back to it’s normal size after delivery) Delayed return of the uterus back to “normal” state *EDUCATE PT: when the LOCHIA changes from RUBRA, SEROUSA & THEN ALBA. Make sure s/o is in the room during d/c instructions Hematoma – throbbing pain, doctor has to go to OR and lance, drain & suture the hematoma Hypovolemic shock o Early S/S BP could be normal RR increases (increase in rate/depth) HR increases (tachycardia) Color could be normal Anxious Cool/moist skin o Delayed S/S BP decreases (systolic decreases) HR increased, but weak and thready RR increased, but shallow Cold skin Pale Coma o Interventions Raise the head of bed Start second IV (don’t use second line) FIRST Start IV fluids 16-18g( b/c if we don’t those veins will collapse & we will never get another IV in O2 via nonrebreather mask 8-10L Foley catheter-done by HCP Could have standing order for uterine catheter and compresses sides of the uterus to decrease bleeding Call doctor immediately to find bleeding Monitor VS and O2 q15minEXAM 3 90 Remain calm so patient remains calm Dopamine can be given to raise BP for hypovolemic shock Medications – Pitocin, Methergine, Hemabate, Cytotec if ordered (not for laceration) What is bleeding? Find the source Usually PPH **On mother baby, you do not need an order to start O2 Woman with Excessive Bleeding o Assessment Uterine atony or trauma o Interventions Check uterus – (fundus) massage Check bladder Check skin (color, cool/moist?) Check under the woman (bleeding) Weigh pads VS q15min Subinvolution (uterus should return 1 fingerbreadth a day) o Slower than expected return of the uterus to its nonpregnant size o Causes Retained placental fragments Pelvic infection o Medications Methergine 10mg IM now & then 10mg PO – so mom can take with her at home- if she had retained placenta fragments Can be given, IM, IV, PO Antibiotics if infection *Hemabate causes explosive diarrhea Thromboembolic Disorders o Superficial venous thrombosis Varicose veins Normally bilateral on calves S/S Swelling Warmth Redness Tenderness Bilaterally Do not give anticoagulants/anti-inflammatories Analgesics, rest, elevate legs, stockings, warm packs o Deep Venous Thrombosis (DVT) S/S Swelling Redness Warm TenderEXAM 3 91 Pain in calf Unilateral Do not do Homan’s sign – but patient has positive Homan’s sign-b/c it can loosen the clot & it can go to the lungs Check pedal pulses (in the infected leg) If no pulse CALL DR IMMEDIATELY Diagnosis (HCP WILL OR ORDER) Doppler MRI Therapeutic management Prevention (main thing)- o Early ambulation o Sequential hose (SCD) C-section pt will get these while there in the OR & will keep this on until the foley cath is removed for prevention of DVT If have DVT o Warm Moist heat o Bedrest o Gradual ambulation w/ medication o Anticoagulant (Warfarin or Coumadin to help break cots. If pregnant, give lovenox.) Medications Postpartum – Warfarin or coumadin If still pregnant – Lovenox Pulmonary Embolism o Clot that has invaded the lungs o S/S Chest pain Tachycardia Tachypnea Dyspnea Pulmonary rales, cough Hemoptysis (expectoration of blood or bloody sputum) Abdominal pain Low grade fever o Interventions Elevate HOB-1st thing O2 lay on left side if you can’t raise HOB STAT ABGs Heparin (drug of choice Puerperal Infection o Any bacterial infections of the female reproductive tract following childbirth or miscarriage.EXAM 3 92 o Bacterial infection after birth, infection of genital track o Temperature of 38C (100.4 F) or higher after the first 24 hours and occurring on at-least 2 of the first 10 days following childbirth o Examples: mastitis and endometritis o RF: Woman who doesn’t wash their hands after the bathroom (UTI) Respiratory complications after C/S o Intervention Antibiotics Rest Fluids Endometritis o Infection of inner lining of uterus o Treatment: IV antibiotics o S/S Chills Cramping Abdominal pain Malaise Decreased appetite Anorexia Foul smelling lochia Subinvolution (if it’s an infection) Treatment: Give something for the fever Antibiotics If it’s causing subinvolution, we’ll give methergine to help the uterus to contract Salpingitis o Infection of Fallopian Tube o IV antibiotics, fluid & rest Peritonitis o Infection spreads through the lymphatic to peritoneum o IV antibiotics, fluid & rest Could get a pelvic abscess Wound Infection o C/S, laceration, episiotomy o IV antibiotic, fluid & rest o Hard time walking, sitting, bowel movement Urinary Tract Infections o S/S Frequency Burning Cloudy, bloody urine o Interventions Antipyretics (numbs urinal tract) Antibiotics (Bactrim) Increase fluidsEXAM 3 93 Cranberry juice (creates an alkaline ash environment in urine) Mastitis o Infection of the breasts, usually unilateral (normally side that breastfeeding) o Flu-like symptoms, temperature o Continue breast feeding, unless bleeding from nipple o Cool compresses, warm compresses o Different from engorgement Cracked nipples Not washing hands Septic Pelvic Thrombophlebitis o 2-4 days post-partum o Infection spreads across pelvic venous system o Least common o Groin pain, flank pain, abdominal pain Moves to shoulder pain o S/S Fever, tachycardia Vomiting Decreased bowel sounds Bloating o Treat same as DVT Anticoagulant therapy IV heparin Antibiotics Chapter 23 & 24 – The High-Risk Neonate Small for gestational age o 10th percentile Large for gestational age o 90th percentile Appropriate gestational age o Between 10th and 90th percentile Low birth weight o 2500 grams o 5lbs 8oz Very low birth weight o 1500 grams o 3lbs 5oz Extremely low birth weight o 1000 grams o 2lbs 3oz Ultra-low birth weight o 550 grams Dubowitz/Ballard o Neuromuscular maturityEXAM 3 94 3 conditions a baby can be born with 1) TTN 2) GBS 3) RDS All three present with the following: TRIAD s/s o Grunting o Retracting o Nasal flaring Starting treatment (before IDing what illness is) o O2EXAM 3 95 o Blood drawn o IV fluids Transient Tachypnea for the Newborn (TTN)-O2 o Resolves within 24-48 hours o Usually due to delay in uptake of pulmonary fluids. Baby hasn’t completely cleared lungs Precipitous delivery o Respiratory rate above 60 (Normal RR: 40-60) o C-section babies are at risk Nurse action for TTN: Do percussion to loosen up the secretions so they can come up **Never feed a baby orally with RR higher than 60 Priority: check for RR Group Beta Streptococcus (GBS) KNOW MOM GBS status-ABX o IV antibiotics (ampicillin and gentamycin) w/i 1st hr of life (mom was GPS+, didn’t get their antibiotics during labor w/I for 4 hours) Respiratory Distress Syndrome (RDS)-surfactant o Cause Lack of surfactant (produced within 24-25 weeks and 34-36 weeks) Surfactant stabilizes/lubricates the alveoli-because it collapsed High risks: Premature babies Babies born to diabetic moms o Other signs Increased RR- above 66 (normal RR: higher than 60) Head bobbing o Treatment Will receive artificial surfactant, Betamethasone makes alveoli slimy so they do not stick Given through their Endotracheal (ET) tube only O2 through nasal canula CPAP – baby is breathing on their own, but forcing more O2. Keeps alveoli open Mechanical Ventilation – baby is not breathing on their own at all, pressure & volume IV antibiotics Oxy hoods o Complications (from oxygen) Bronchopulmonary Dysplasia (BDP)EXAM 3 96 Barotrauma – building hardened area on alveoli from where oxygen has hit the alveoli for so long. Basically COPD. Permanent damage. Respiratory infections & asthma maybe later Retinopathy of Prematurity Arteries behind the eyes are not mature enough, and too much oxygen can damage those arteries. On term babies, these arteries are mature – so this doesn’t not affect term babies Intraventricular Hemorrhage Causes the ventricles in the brain to rupture o Hydrocephaly o Nerve damage o Brain bleeds (grade 1-4, grade 4 is the worst) Other Breathing Issues of the Preterm Infant o Periodic breathing 5-10 seconds without breathing (normal must take VS 1 minute) o Apneic 20 seconds or less without changes Give caffeine IV – stimulates CNS o Meconium Aspiration Syndrome post- over 40 weeks gestation Babies that pooped in utero have a higher chance of developing this When babies have this, we do NOT want them to cry Pulmonary HTN can be a cause Treatment Oscillator o Vibrates 250-260 times a minute ECMO o Bypass the heart & the lungs o Can only be on this for 10 days o Baby has to be at least 37 weeks or greater o 98% mortality rate Nutrition o Total Parenteral Nutrition (TPN) – aspiration precautions Hyper el (yellow bag. Hung q24h) and Lipids (hung q8h) Can cause a heart attack for the newborns, so have to monitor cholesterol levels- triglycerides o Enteral Feeding NG/OG J – bypasses the stomach Continuous Intermittent Have to have a pacifier – needs to learn how to suck Babies don’t know how to suck/swallow until 34 weeks gestationEXAM 3 97 **Have to make sure this baby gets the right amount of formula. So, if don’t get enough from bottle, have to give the rest through NG/OG or J tube Necrotizing Enterocolitis o Part of GI dies Abdomen distended No bowel sounds o Only diagnosed through an x-ray o Will remove the dead/necrotic part of intestines o Newborn can have a temporary colostomy to let the GI rest o High percentage death rate. Normally only with premature babies, not term Stress o No noise, keep extremely stress free Chapter 25 – Family Planning Information about contraception o Common sources: social settings o Roles for nurses: Help pick right contraceptive for them specifically o Considerations when choosing a method: Safety Protection from STI – abstinence Convenience of some contraceptives Expensive o Age considerations Adolescent knowledge Misinformation Perimenopausal women (can’t have a period for 12 months until you’re into menopause, until then, you still can get pregnant) Fertility decreases between ages 35-40 Cannot take if have HTN, blood clots, smokers Sterilization – PERMANENT (99% effective) o Female sterilization Tubal ligation No other contraceptives are needed after Avoid intercourse for 1 week Avoid heavy lifting or strenuous exercise for 1 week Mild analgesics (soreness & gas pains are common complaints) Sterile immediately Esure device – permanent Insert a coil in each fallopian tube via vagina, cervix, and uterus o Done in a doctor’s officeEXAM 3 98 o Male sterilization Vasectomy Rest Ice packs on scrotum (on and off) for 24 hours Scrotal support for 24 hours Mild analgesics No bathing for 24 hours No strenuous exercise for 1 week Avoid intercourse for 1 week Not sterile immediately until have a sperm count of 0, MUST use a back-up contraceptive until sperm count 0 in order to be sterile o Hormonal Contraceptives Hormone implants – Nexplanon Lasts for 3 years Into the arm Hormone injections - Depo 15 weeks – 3 months Should be reinjected every 13 weeks Side effect – weight gain Oral contraceptives Combination – estrogen and progesterone Or progestin only – thickens uterine lining so ova cannot implant Suppress LH Cannot take if HTN, gallstones, smokers, thrombophlebitis, cardiovascular disease, estrogen dependent cancer, migraines ATI: Someone over 35 Start taking pills the Sunday after period, or the day after period Can clear acne, helps with menstrual cramps, regulates periods, increase bone density 3 weeks of colored pills, 7 days of white pills (helps patient have period – iron filled) Take missed pill as soon as you remember. If you miss 2, take when remember but use another contraceptive for a week. If you miss 3 pills, you have to throw that pack away. Antibiotics can affect St. John’s Warts can affect Anti-convulsive can affect Postpartum and lactation – wait till doctor says you can use Murphy’s rule: Emergency contraceptives Plan B – within 72 hours, but the sooner the better Do not use as birth control Transdermal contraceptive patchEXAM 3 99 Estrogen or progesterone, or both Change every 28 days Contraceptive vagina rings NuvaRing In for 21 days, taken out for 7 day, then a new one Intrauterine devices o Copper-T Stiff, copper In place for 10-15 years No hormones Keeps from fertilizing in the uterus Cramping, bleeding, s/s infection, & pregnancy o Mirena Soft, plastic In place for 5 years Hormones – progesterone Thickens lining and mucus so sperm cannot make it through Painful period If you cannot feel the string, then need to call the doctor o Cannot be pregnant o Cannot not have any inflammatory pelvic disease o Causes inflammatory responses that does not allow ova to implant o Done in doctor’s office, dilate cervix, then insert. Physician has to remove o Side effects: cramping, bleeding o Watch for S/S of pregnancy or infection Barrier methods o Male condom o Sponge Over the counter Spermicide in sponge Absorbs the sperm that keeps the sperm from entering the cervix Leave in for a few hours after intercourse o Diaphragm Diaphragm over the cervix and prevents sperm from going into uterus Fitted by provider, if you gain or lose 10 pounds, it must be refitted You put it inside yourself Has to be left in for 6 hours after intercourse, cannot be left in longer than 24 hours total Reusable No sooner than 6 weeks post-partum Must use spermicide with diaphragm Can get TSS o Cervical CapEXAM 3 100 Fits snugly over the cervix Can leave in place for 48 hours Over the counter o Female condom Natural Family Planning Method o Calendar – avoid five days before ovulation and 5 days after. Only works if you have regular period o Standard days method o Basal body temperature- if trying to get pregnant Temperature in the morning before getting out of bed If ovulating, your temperature is up Infection, stress, etc. – can affect temperature = not as accurate o Cervical mucus Thicker mucus – cannot get pregnant Thicker before ovulation Thinner mucus – ovulating o 2-day method o Symptothermal methods o Abstinence Least Reliable Method o Breastfeeding o Coitus interruptus – pull out method Application of Nursing Process: Choosing a contraceptive method o Best intervention = teaching o Expected outcome – client not pregnant or have STI Chapter 26 – Infertility *Unable to get pregnant or to continue to hold a pregnancy to term *Secondary infertility- unable to get pregnant after already having one child Factors in the Man o Abnormalities of sperm Average sperm in ejaculation: 25 million - 200 million Anything below 20 million is sterile Tight underwear, drug use, smoking, alcohol can all influence the amount or type of sperm a man has o Abnormal erection Cannot achieve or maintain o Abnormal ejaculation Hypospadias Retrograde ejaculation- goes back up instead of out o Abnormalities of seminal fluids Prostaglandins can kill sperm High vaginal PH can kill spermEXAM 3 101 Thick & traps sperm inside Supposed to be alkaline Can cause low sperm count- GI infections, smokers, alcoholics, drug users, cancer meds (toxins), tight underwear (gets too hot) Low sperm count Factors in the Woman o Disorders of ovulation- doesn’t ovulate or isn’t regular o Abnormalities of the fallopian tubes- blockage, or one is very narrow o Abnormalities of the cervix Repeated pregnancy lost o 80% – fetal chromosomal abnormalities o Abnormalities of cervix or uterus Single horn – unicornuate- less chance of pregnancy Single uterus with a midline septum- uterus divided in ½ Uterus having two horns – bicornuate- indent @ the top, harder to carry pregnancy Double uterus with one vagina Double uterus and double vagina o Endocrine abnormalities – not enough progesterone o Immunologic factors – different antigen than mom o Environmental agents- toxins, radiation, cancer therapy, or environment o Infections Evaluation of Infertility o Preconception counseling o History and physical exam o Diagnostic tests Blood work Sperm count Post-coital test – have intercourse, 8-12 hours after intercourse go to doctor, scrape vagina and tests Ph level o Therapies to facilitate pregnancy o Medications Ovulation induction – Clomid injections- stimulates pituitary gland o Surgical procedures- pelvic adhesions, variceal o Therapeutic insemination- IUI (wash all prostaglandin off and inject sperm into uterus) o Egg donation o Surrogate parenting Whoever delivers the baby legally is the mother of the child. So, the surrogate mother (the biological mother-surrogate) can change their mind. The surrogate mother has to sign off the right for the other parents to adopt the baby o Assisted reproductive technology In vitro fertilization (IVF) very expensive (30k-60k per)EXAM 3 102 Preimplantation genetic testing **2nd leading cause to divorce infertility Response to Infertility o Assumption of fertility blaming the significant other o Growing awareness of a problem o Seeking help for infertility o Reactions during evaluation and treatment Influences on decision making Psychosocial reactions Guilt Isolation Depression Stress on the relationship Outcomes After Infertility Therapy o Pregnancy loss after infertility therapy o Parenthood after infertility therapy o Choosing to adopt Mother who gives babies up have 6 months after baby is born to choose to keep (take back) the baby Chapter 27 – Preventive Care for Women Healthy People 2020 Health Maintenance: Health history o RF for variety conditions o Focus on age o Family history o Psychosocial assessment o Vitals o Height, weight o Auscultation o Extremities examined o Abdomen palpated o STIs Health Maintenance: Screening Procedures o Prevention is better than a cure o Early diagnosis Early treatment o Breast self-awareness / breast self-examination Use finger pads Every month In the shower, standing o Clinical breast examination o Mammography once you reach the age of 40 unless cancer in the family, after 60 not needed o Vulvar self-examination o Pelvic examination o Cervical cytology or Pap test o Rectal examinationEXAM 3 103 o Screening o Immunization Chapter 34 – Women’s Health Problems Breast Disorders: Diagnostic Evaluation o Ultrasound o Fine needle aspiration biopsy o Core needle biopsy o Open or surgical biopsy Benign Disorders o Fibrocystic breast changes Before menopause Fill up with fluid Painful Dense breast tissue As long as they remain in the same spot and the same size- okay Usually benign Malignant tumors o 1 in 8 women in the US o 1 in 1000 men o Higher for white women over 25 o Higher for Black women over 35 o Risk factors Mutation of the BRCA1 and BRCA 2 genes Mutation of CHEK-2 gene in men and women Insurance will pay for these tests if your mother had breast cancer o Pathophysiology o Staging- 1-4 o Management Surgical Radiation- destroys cancer cells Chemotherapy- kills cancer cells Hormonal therapy- reduce production of estrogen (Tamoxifen estrogen blocking drug) Immunotherapy o Breast reconstruction Timing Method o Psychosocial consequences of breast cancer o Nursing consideration Emotional support Preoperative and discharge teaching Printed informationEXAM 3 104 Cardiovascular Disease o Risk Factors Fixed, or unmodifiable Factors that can be changed o Prevention HTN Smoking cessation Diet and glucose Increased activity Aspirin Menstrual Cycle Disorder o Menopause – 12 months without a period Normal age – 51.5 S/S Hot flashes Irritable, mood swings Weight gain Vaginal secretions dry use water soluble lubricants- if someone is having painful intercourse after intercourse Decreased bone density Painful intercourse Can have hormone replacement, but does increase risk of ovarian cancer o Amenorrhea (absence of menses) Primary Secondary o Abnormal uterine bleeding Anything abnormal after menopause needs to be checked Breast cancer o Early period o Late menopause o No children o Prolonged or early use of oral contraceptives o Overweight o Lack of exercise o Excessive alcohol use Cyclic Pelvic Pain o Painful menstruation Endometriosis o Overgrowth of endometrial tissue o All over, not just the uterus o Causes of cancer- obesity, never had a child, abnormal bleeding after menopause o Once have a baby it should help o Abnormal bleeding o Heavy bleeding o Painful bleeding OsteoporosisEXAM 3 105 o After menopause higher risk for osteoporosis o Prevention Drug therapy Calcium and Vitamin D 3 Exercise Diet o Bone density scan is suggested Pelvic Floor Dysfunction o Cystocele- weakening of uterine wall can no longer support bladder o Enterocele- wall b/w vagina & rectum, loop in bowel, uterine prolapse o Rectocele- posterior vaginal wall becomes weak & thin, tries to have BM & pushes vaginal wall, rectum will protrude into vagina o Uterus is falling o First – Third Degree (third degree is the worst, further the uterus has fallen) Fibroids o If you have fibroids while pregnant, they will never remove the fibroids during a C-section o Caffeine makes it hurt more o Fill with fluid prior to period Cervical polyps o Small tumors o Proliferation of cervical mucosa Uterine leiomyomas (fibroids) o Develop from uterine smooth muscle cells o Estrogen dependent o Normally will not remove during C-section Ovarian cysts o Follicular or luteal o Can rupture Sexually Transmitted Diseases o Cannot be cured: HIV Herpes – genital warts Cannot have vaginal delivery if have herpes lesions Valtrex @ 36 weeks gestation HAS to BE A C-section HPV- warts Can have vaginal delivery with genital warts Can be lasered off Painful o Sexually transmitted infections (can be cured) Trichomoniasis Bacterial vaginosisEXAM 3 106 Yeast infection Gonorrhea/chlamydia Pelvic Inflammatory Disease o Fishy smell Toxic Shock Syndrome o Tampon use – in too long o Diaphragm and cervical cap – in too long Cardiovascular disease o #1 cause of female death in the country o High stress jobs o More smokers o Alcohol o Takes more women’s lives than all cancers Risk factors o Obesity o Diet o Diabetes o HTN o Decreased physical activity o Can quit smokingEXAM 3 107 Take an aspirin a day Termination of pregnancy Drugs Surgical o Over 7 weeks Medical methods o Used in the second trimester Review PPH Preeclampsia GTPAL 5 Ps Hyperbilirubinemia – least risk is a baby fed in 1st hour Only soft tissue that can hold baby – uterus Infertility Ballard/Dubowitz – why it’s done, normal range Nonstress test – checking for fetal well-being Caput – CROSSES the suture line Iron Deficient Anemia – organ meats Hypovolemic shock Placenta previa Abruption – number one cause is HTN Ectopic pregnancy More old stuff than new** Triads How long does a sperm live? 3-5 days Ova can be penetrated up to 24 hours Most reliable form of contraceptive? IUD Magnesium Sulfate MSAFP, CVS Crisis situation – shoulder dystocia, prolapse cord Decelerations – causes and interventions Babies cannot shiver when cold. They can jitter d/t hypoglycemia. Stiff & fine movements is a seizure. Low fever – cover head and recheck in 30 minutes Low BG – feed, and recheck in 30 minutes Inversions Molar pregnancy (cancer) Dry baby – to stimulate to cry and keep warm so does not lose heatEXAM 3 108 Mom will know if baby is getting enough breast milk by the amount of diaper change which is 6-8 wet diapers. 1st thing checked on baby when born are respirations RR Remove w/ finger & push down on baby Post dates- overgrown fingernails, cracked & leather like skin Erythromycin & Vitamin K (prevent intracranial hemorrhage) *Dilation/ effacement/station strip Late decelerations [Show More]
Last updated: 1 year ago
Preview 1 out of 108 pages
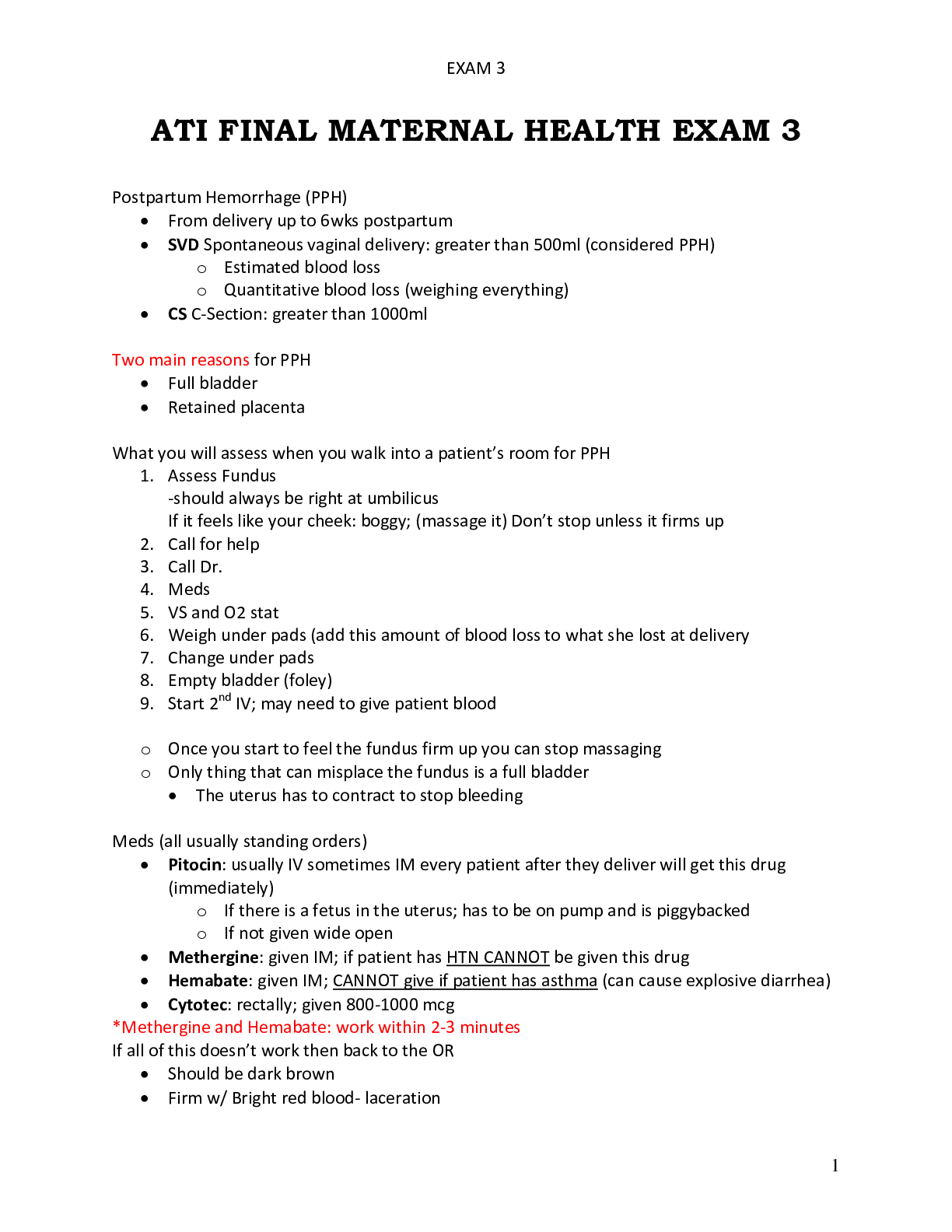
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Aug 01, 2021
Number of pages
108
Written in
Additional information
This document has been written for:
Uploaded
Aug 01, 2021
Downloads
0
Views
28