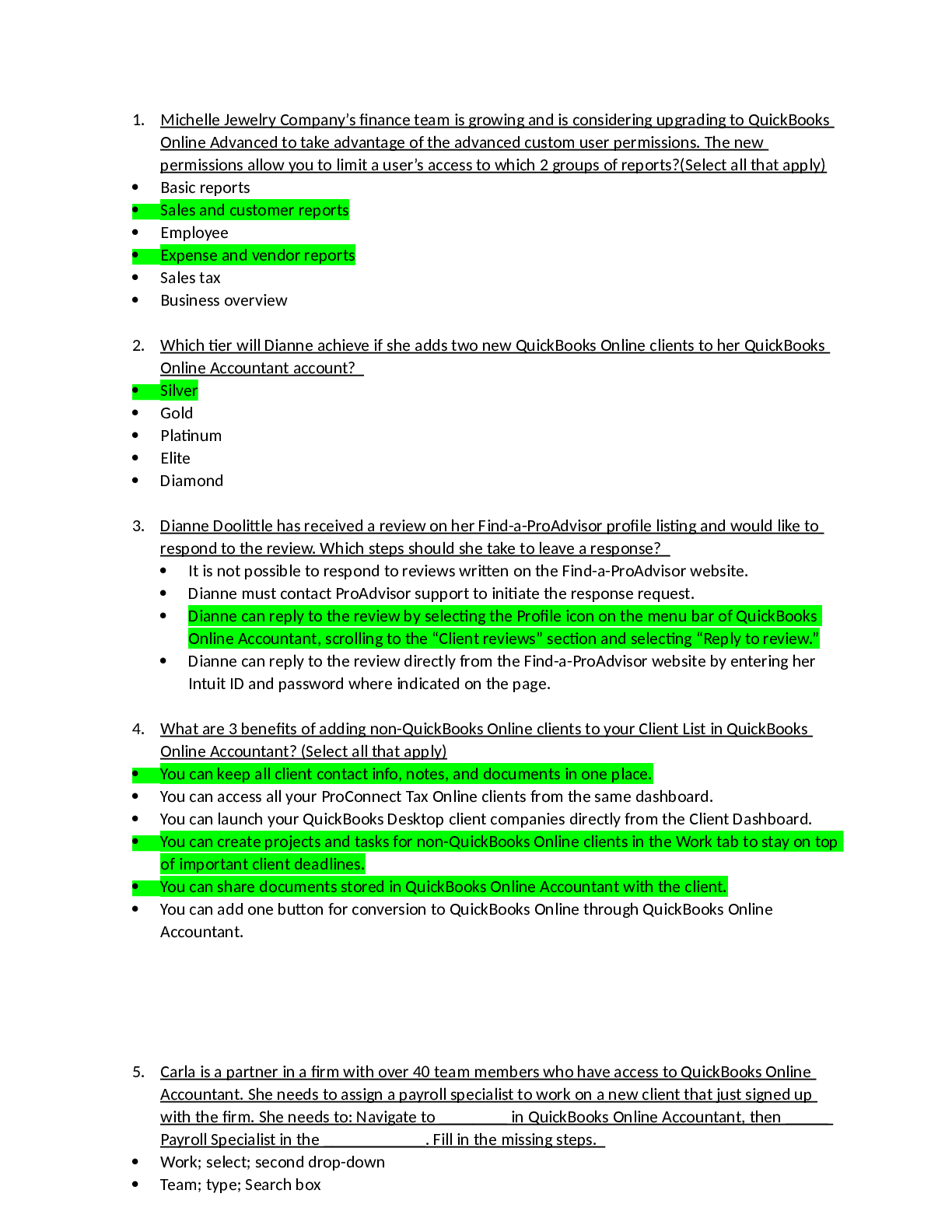
*NURSING > QUESTIONS & ANSWERS > FNDH 620 Exam 3 – 2022 (COMPLETE SOLUTIONS). 100% Pass Rate (All)
FNDH 620 Exam 3 – 2022 (COMPLETE SOLUTIONS). 100% Pass Rate
Document Content and Description Below
FNDH 620 Exam 3 – 2022 (COMPLETE SOLUTIONS) When water soluble vitamins are consumed in excess of body needs, generally the excess is: A. excreted in the feces; B. stored in liver, bone, and adi... pose tissue; C. excreted in the urine; D. not absorbed; E. none of these. - ✔✔excreted in the urine Vitamin C acts as a coenzyme by maintaining iron in a reduced state in: A. collagen synthesis B. methylation of homocysteine C. release of energy from nutrients D. heme synthesis - ✔✔collagen synthesis As little as 10 mgs/day of vitamin C may be enough to prevent scurvy. A. True B. False - ✔✔true A major role for thiamin is: A. energy transformation; B. blood coagulation; C. collage formation; D. erythrocyte synthesis; E. none of above. - ✔✔energy transformationWhy may alcoholics cause thiamin deficiency ? A. alcohol prevents thiamin uptake; B. alcohol prevents thiamin utilization; C. alcohol destroys thiamin activity; D. Both A and B; E. None of above. - ✔✔Both A and B alcohol prevents thiamin uptake; alcohol prevents thiamin utilization Riboflavin is required for: A. formation of active folate; B. conversion of tryptophan to niacin; C. function of B6; D. all of A, B & C; E. none of these - ✔✔all of A B and C formation of active folate; conversion of tryptophan to niacin; function of B6; Nicotinamide, but not nicotinic acid, is the form required for the synthesis of nicotinamide adenine dinucleotide. A. True B. False - ✔✔false How are the recommended intakes of niacin expressed (units)? A. grams B. niacin equivalents (mgs)C. in micrograms D. in milliliters - ✔✔niacin equivalents (mgs) List four water soluble vitamins that are required by pyruvate dehydrogenase complex. - ✔✔B1, B2, B3, pantothenic acid (B5) Bioavailability of biotin is near 0% from wheat. A. True B. False - ✔✔True (but it is near 100% from corn) Intake of raw egg white may cause deficiency of A. pantothenic acid B. thiamin; C. riboflavin; D. biotin; E. niacin - ✔✔Biotin Which of the following is one of the main functions of vitamin B6? A. coagulation B. depigmentation C. transamination D. antioxidation - ✔✔transamination Methionine cycle requires: A. B6; B. B12; C. folate; D. Niacin; E. All of above. - ✔✔all of the aboveB6; B12; folate; Niacin Which anemia is related to folate deficiency? A. Pernicious anemia B. Megaloblastic anemia C. Hypochromic microcytic anemia D. Hemodilution anemia - ✔✔megaloblastic anemia To protect against birth defects, a higher RDA of folic acid has been suggested for pregnant women A. True B. False - ✔✔True Vitamin B12 is only available from ___products. A. grain B. fruit C. animal D. vegetable - ✔✔animal Why the RDA of vitamin B12 is so low? A. In the liver, free cobalamin can be stored for years B. Little B12 in the body is degraded C. Whole body turnover is about 0.1% daily D. All of A, B, & C E. None of above - ✔✔all of a b and c In the liver, free cobalamin can be stored for years Little B12 in the body is degraded Whole body turnover is about 0.1% dailyHigh dietary folate may cure megaloblastic anemia caused by: A. folate deficiency; B. B12 deficiency; C. less methionine; D. both A & B; E. all of A, B & C. - ✔✔Both A & B folate deficiency; B12 deficiency; Formation of retinol from beta-carotene requires the presence of what B vitamin? A. ascorbic acid B. folic acid C. niacin D. pyridoxal phosphate E. None of above - ✔✔Niacin Dietary fat is not very important regarding the digestion and absorption of pre- and provitamin A forms A. True B. False - ✔✔False Within the nucleus, retinoic acid binds to ______ A. retinoic acid nuclear receptors B. Transcription factors C. Retinoid X receptors D. Retinoic acid response elements E. Both A and C - ✔✔Retinoid X receptorsWhat % of vitamin D3 from diet is absorbed? A. 20 B. 30 C. 40 D. 50 E. 100 - ✔✔50% What form of vitamin D is the major circulating form? A. calcidiol B. calcitriol C. cholecalciferol D. ergocalciferol E. None of above - ✔✔Calcidiol The vitamin D receptor is a member of the super family of nuclear receptors that regulates gene expression. A. True B. False - ✔✔True What is the principal transport vehicle for vitamin E in the blood? A. the blood plasma B. lipoproteins C. cytochrome P450 system D. alpha tocopherol - ✔✔lipoproteins Which mechanism has been proposed but not proved as vitamin E's principal function against chronic disease prevention? A. Immune functionB. Cell cycle arrest C. Anti-proliferation D. DNA repair E. Anti-oxidation - ✔✔anti-oxidation For which vitamin is the tolerable upper limit set because of increased tendency for bleeding? A. Vitamin A B. Vitamin D C. Vitamin E D. Vitamin K - ✔✔vitamin E What is the chemical name for vitamin K in green plants? A. menaquinone B. menadione C. phylloquinone D. Beta carotene - ✔✔phylloquinone As coenzyme, vitamin K is required in the carboxylation of Gla proteins by converting glutamate residues to gamma-carboxyglutamate residues. A. True B. False - ✔✔True Vitamin K deficiency is most often observed in: A. old people B. adolescents C. children D. newborns - ✔✔newborns Which food group contributes the most calcium to our diet?A. meat B. dairy C. fruits/vegetables D. breads/cereals - ✔✔dairy The primary function of parathyroid hormone (PTH) is: A. to reduce blood calcium levelsb. B. to inactivate calcitoninc. C. to stimulate calcitriol synthesis in the kidney and then enhance bone calcium levels D. to enhance blood calcium levels by taking calcium from bone - ✔✔to enhance blood calcium levels by taking calcium from bone Which two minerals are part of the bone crystal, hydroxyapatite: A. Sodium, chloride B. Sulphur, magnesium C. Calcium, phosphorus D. Calcium, potassium - ✔✔Calcium, phosphorus Which of the following amounts comes closest to the level of sodium typically in our daily diets? A. 0.5 g/day B. 1-2 g/day C. 2-3 g/day D. 3-5 g/day E. 5-8 g/day - ✔✔2-3 g/day All of the following are true about potassium except: A. It increases blood pressure B. Is found inside cells C. Helps regulate water balance and osmotic pressureD. Essential for muscle contractility - ✔✔It increases blood pressure Oral supplements of ferrous iron are available in complexes with sulfate, succinate, citrate, lactate, tartate, fumarate or gluconate. The absorption of these nonheme iron supplements could be ______ when ingested with vitamin C or other antioxidants. A. increased B. decreased C. not affected - ✔✔increased Iron deficiency is second only to ______as the most prevalent nutrition problem in the USA. A. high cholesterol B. malnutrition C. obesity D. low blood pressure - ✔✔obesity Among the trace minerals, which mineral participates as cofactors in the most enzyme systems? A. zinc B. iron C. selenium D. copper - ✔✔zinc What two minerals can cause oxidative damage to cells when in their free ion forms? A. zinc and copper B. iron and zinc C. copper and iron D. None of above - ✔✔copper and iron Which mineral is an essential cofactor in the action of glutathione peroxidase (GPX) in the reduction of organic peroxides and hydrogen peroxide?A. zinc B. iron C. copper D. selenium - ✔✔selenium Excess dietary iron can decrease copper absorption. A. True B. False - ✔✔true Keshan disease is associated with ______deficiency. A. zinc B. copper C. selenium D. iron - ✔✔selenium Water Soluble Vitamins - ✔✔B vitamins and vitamin C B Vitamins - ✔✔Thiamin (B1), Riboflavin (B2), Niacin (B3), Biotin (B7), Pantothenic Acid (B5), Vitamin B6, Folic Acid, Vitamin B12 Fat Soluble Vitamins - ✔✔Vitamins A, D, E, K Vitamins are.. - ✔✔Organic compounds that are required in the diet in only small amounts to maintain fundamental functions of the body (growth, metabolism, cellular integrity, etc.). Small Amounts of Vitamins - ✔✔distinguish from macronutrients because vitamins don't provide energy and don't use for structure Organic - ✔✔distinguishes from minerals that are required in small amounts but inorganic natureThe activity of a vitamin is often found in several closely related compounds known as.. - ✔✔vitamers Some of vitamins are not Strictly Dietary Essentials - ✔✔Niacin (from tryptophan) and Vitamin D (from 7-dehydrocholesterol upon sunlight) can be made in the human body Biotin and Vitamin K can be made, at least in part, by bacteria in the large intestine Multivitamin-mineral Use as Dietary Supplements - ✔✔About one half of US population and 70% of adults ≥71 y use dietary supplements (33% are multivitamins & multiminerals): - >$21 billion spent annually reported in 2006 - ~4% increase yearly since 2000 - Early use by children and adolescents for sport performance Do we really need supplements? - ✔✔No overall benefits from taking multivitamin/mineral on mortality and incidence of chronic diseases such as cancer or heart disease Some studies showed increased risk of cancers Characteristics of Water Soluble Vitamins - ✔✔Apart from their solubility characteristics, the water soluble vitamins have little in common from the chemical point of view Because of their water solubility: - excesses of these vitamins are excreted in urine - rarely accumulate in toxic concentrations - their storage is limited (except for cobalamin) and must be provided regularly Function of Water Soluble Vitamins - ✔✔The function of vitamins are varied, but the most common function for Vitamin Bs, C, and reduced K is required as coenzymes or components of coenzymes.Coenzymes are defined as small, organic molecules that are required by an enzyme and that participate in the chemistry of catalysis. - e.g.: Ascorbic acid, biotin, NAD, NADP, FAD, FMN, thiamin pyrophosphate, folate coenzymes, methylB12, Co-A, etc Vitamin C - ✔✔also called ascorbic acid (AA) Ascorbic acid can be synthesized from glucose Humans & primates, guinea pigs etc. are unable to synthesize AA due to genetic mutation Sources: fruits and vegetables (~80-90% AA & 10-20% DHAA) 2 Digestion, Absorption, and Transfer of Vitamin C - ✔✔- AA is absorbed via sodium-dependent active transport in the small intestine - DHAA is absorbed via passive diffusion or glucose transporters - AA exits the enterocyte to the liver via portal vein, then to extrahepatic tissues Bioavailability of Vitamin C - ✔✔Bioavailability is defined as the proportion of the compound administered intravenously that appears in plasma over time when compared with the compound administrated orally. Bioavailability represents the proportion of the compound that is absorbed from GI tract. Vitamin C bioavailability is nearly 100% for dose between 15-200 mg, which declines for higher doses (~50% for 1250 mg)Metabolism and Excretion of Vitamin C - ✔✔Kidneys can reabsorb AA or DHAA that depends on plasma AA concentrations AA metabolites (DHAA, diketogulonate, oxalic acid etc.) and excess AA are excreted in urine if plasma level is higher than renal threshold. Renal threshold: plasma level at 0.8-1.4 mg/dL or body pool at 1,500 mg or dietary 100 mg daily RDA for Vitamin C - ✔✔Males --> 90 Females --> 75 Pregnancy --> 100 Lactation -->120 Smokers --> Additional +35 Dietary Reference Intake (DRI) - ✔✔In the US, DRIs are usually set up by US Food and Nutrition Board (FNB): Dietary Reference Intakes Subcommittee In addition, the Institute of Medicine (National Academy of Sciences, USA) installed a Standing Committee on the Scientific Evaluation of Dietary Reference Intakes Recommended dietary allowance (RDA) • Adequate intake (AI) • Tolerable upper intake level (UL) • Estimated average requirement (EAR) Recommended Dietary Allowance (RDA) - ✔✔DRA or AI is adequate to meet the known nutrient needs of practically all healthy persons. The determination of adequacy is difficult dependent on the functional outcome chosen: • multiple functions of each nutrient• bioavailability, distribution, metabolism, excretion • variation of requirements (children, elderly, gender, race, etc) • Interaction with other nutrients or factors Tolerable Upper Intake Level (UL) - ✔✔UL is the concept of Safety versus Risk Traditional models are animal models to setup an acceptable daily intake (ADI) and then extrapolate noobserved-adverse-effect-level from animal to human Collagen Synthesis (Vitamin C) - ✔✔- AA is utilized for hydroxylation of proline and lysine residues of achains of procollagen - AA functions as a reduced agent for the reduction of iron from Fe3+ to Fe2+. - Hydroxyproline plays a role in the formation of the triple helix of collagen, which is utilized for connective tissues in bone, cartilage and blood vessel, etc. Neurotransmitter Synthesis (Vitamin C) - ✔✔AA is utilized in the synthesis of norepinephrine from dopamine AA is also utilized for the synthesis of serotonin from tryptophan Bile Acid Synthesis (Vitamin C) - ✔✔AA is required for the hydroxylation of cholesterol via 7-ahydroxylase, a ratelimiting step of bile acid synthesis Carnitine Synthesis (Vitamin C) - ✔✔AA is involved in two reactions required for the synthesis of carnitine Sufficient production of carnitine is of significance in fat metabolismNonenzymatic Reductive Function (Vitamin C) - ✔✔aka - antioxidant As an electron donor to reduce free radicals AA may defense against oxidant damage Oxidative damage in DNA has been postulated to cause gene mutation and then attribute to aging and cancer, etc. Oxidative damage in LDL (lipid peroxidation) has been postulated to accelerate atherosclerosis --> Coronary heart disease (CHD) Oxidative damage in proteins has been linked to develop cataract Vitamin C and Coronary Heart Disease - ✔✔AA has been shown to inhibit metal-catalyzed LDL oxidation in vitro, but the effect in vivo is unknown. Several large prospective cohort studies (the Nurses' Health Study, the Health Professionals Follow-up Study, and the Iowa Women's Health Study) have not found a link between high AA intake and reduced risk of heart disease Vitamin C and Cancer - ✔✔Lab tests in animals have shown AA inhibits tumor growth and reduces genetic damage caused by carcinogens. Studies on eating habits of large groups of people show that a high intake of AA-rich foods may reduce the risk of cancers at mouth, stomach, lung & pancreas. The mechanisms of anticancer by antioxidant in vivo are not clear. Vitamin C and Eye Health - ✔✔A 1997 study of women in Harvard's Nurses' Health Study found that AA supplements for over 10 years greatly reduced the risk of cataracts Long term use of AA supplements was associated with a reduced risk of age-related lens damageVitamin C and Colds - ✔✔In 1970s, Nobel prize-winning chemist Dr. Pauling proposed that a very high intake of AA could protect against cold However, 18 studies published have shown that AA supplements had no effect on cold incidence Scurvy - ✔✔Intake < 10 mg daily may result in scurvy Most notable symptoms include bleeding gums, skin discolorations, impaired wound and fracture healing, joint pain, loose and decaying teeth, etc. Scurvy is rare in the U.S., but poor diets with alcoholism or drug abuse may cause deficient Vitamin C Toxicity - ✔✔Relatively nontoxic Intake above 1 g per day may cause nausea and diarrhea High dose > 1 g/day may induce renal stones (oxalic acid) Thiamin (B1) - ✔✔1st recognized in 1896, determined as vital amine in 1912 and discovered the structure in 1936 Biologically active form is Thiamin diphosphate (TDP) or thiamin pyrophosphate (TPP) Pyrimidine Thiazole ring thiaminase Food Sources of Thiamin - ✔✔enriched grain products meats, especially pork nutsDigestion, Absorption, Transport & Storage of Thiamin - ✔✔TDP is digested into free form before absorption Low concentrations of thiamin is absorbed into enterocyte via Na+-K+-pump, but high conc. is via passive diffusion Within liver, ATP donates phosphate to thiamin --> TDP --> extrahepatic tissues 50% of thiamin in body is contained in muscle tissue Metabolism and Excretion of Thiamin - ✔✔At least 50 metabolites have been reported to occur in the urine Major metabolites are thiamin acetic acid, 2- methyl-4-amino-5- formylaminomethylpyrimidine, etc Thiamin Functions - ✔✔Coenzyme for several decarboxylation reactions in carbohydrate catabolism. Important in ATP synthesis and acetyl CoA production (--> synthesis of fatty acids, ketone bodies and cholesterol) Coenzyme for transketolase in pentose phosphate pathway that - a means of generating NADPH for fatty acid synthesis - essential for synthesis of ribose (nucleic acid) Thiamin Deficiency - ✔✔Beriberi (can't can't) - Dry beriberi: characterized by muscle weakness - Wet beriberi: characterized by heart failure Thiamin deficiency is rare in the U.S. since grains are supplemented with thiaminDeficiency may occur due to alcoholics - Alcohol prevents thiamin uptake and utilization Riboflavin (B2) - ✔✔Riboflavin = ribose + flavus (Latin for yellow) Synthesized in all plants and microorganisms, but not in humans & higher organisms Food Sources of Riboflavin - ✔✔milk and dairy products meats, especially organ meats, and eggs broccoli, spinach, mushrooms fortified, ready to eat breakfast cereals Digestion, Absorption, Transport & Storage of Riboflavin - ✔✔Riboflavin attached to proteins is freed by stomach HCl and gastric/intestinal enzymatic hydrolysis FAD and FMN are further digested to free riboflavin prior to absorption Free riboflavin is absorbed in enterocyte via a sodium-dependent carrier Riboflavin can be circulated to the liver via portal vein In liver, some riboflavin is phosphorylated into FMN and FAD Free riboflavin can be circulated from liver to extrahepatic tissues via blood binding proteins such as albumin, immunoglobulins, etc. Free riboflavin passes most cell membranes by a carrier-mediated process Brain cells uptake FAD through a high-affinity transport system, so that FAD in brain does not decline even during riboflavin deficiencyWithin cells, riboflavin is converted to FMN and FAD that prevent diffusion out of tissue Metabolism and Excretion of Riboflavin - ✔✔Free riboflavin is a primary metabolite found in urine (60- 70%) Urinary excretion of riboflavin may be noticeable a couple of hours following oral ingestion Urinary excretion of flavins reflects dietary intake (biomarker for intervention studies) Riboflavin Functions - ✔✔FAD & FMN are donors or acceptors of hydrogen and electrons in many oxidationreduction reactions • Krebs cycle • B-oxidation of fatty acids Into electron transport chain to produce 2ATP FMN is a component of the electron transport chain FADH2 is used in the formation of the active form of folate FAD is required for conversion of tryptophan to niacin FMN is important in B6 function Riboflavin Deficiency and Toxicity - ✔✔Riboflavin deficiency can be severe -Growth is stunted & skin lesions appear - Clinical features: • Cheilosis: cracks on the outside of the lips• Glossitis: inflammation of the tongue • Hyperemia: redness of the oral cavity No incidences have been reported of toxicity Niacin (B3) - ✔✔aka - nicotinic acid The word niacin sometimes is used as the generic name for both Nicotinic acid & Nicotinamide Active niacin is Nicotinamide Adenine Dinucleotide (NAD+) and Nicotinamide Adenine Dinucleotide Phosphate (NADP+) Nicotinic acid is the form required for the synthesis of NAD + and NADP +, therefore, any dietary nicotinamide must 1st undergo deamination to nicotinic acid Tryptophan also may serve as a precursor for synthesis of NAD + and NADP + (60 1, required FAD and PLP) Niacin equivalent (NE) = 1 mg niacin or 60 mg tryptophan Food Sources of Niacin - ✔✔meat, poultry, fish peanuts enriched grain products Niacin in Foods - ✔✔Widely distributed in plant & animal origin Niacin in some plant foods (corn, wheat & sorghum etc.) is bound to carbohydrates or peptides that are not readily bioavailable (<10-30%) Corn-based diets have also low tryptophan content, which may cause niacin deficiencySorghum diets also contain high levels of leucine that may inhibit niacin synthesis from tryptophan Digestion, Absorption, Transport & Storage of Niacin - ✔✔Glycohydrolase converts NAD + or NADP + into nicotinamide before absorption Absorption into enterocyte is via active sodium dependent pump for low concentrations, but passive diffusion for high concentrations Niacin can be utilized in enterocyte or transported to liver Converted to NAD + or NADP + in liver or circulated to extrahepatic tissues Metabolism and Excretion of Niacin - ✔✔Little loss of niacin into urine when intake is modest, because both nicotinic acid & nicotinamide may be reabsorbed Primary metabolites are N'- methynicotinamide or N'-methynicotinic acid Niacin Functions - ✔✔NAD+ or NADP+ is donors or acceptors of hydrogen and electrons NAD+ or NADP+ is required by about 200 enzymes (most are dehydrogenases) Most of the NADH is used to transfer electrons to the electron transport chain --> 3ATP Most of the NADPH is used in synthesis of cholesterol, fatty acids, deoxynucleotides & steroid hormones NADPH is also used to reduce DHAA to AA Niacin Deficiency - ✔✔Deficiency results in a syndrome called Pellagra [Italian pelle (skin) + agra (rough)] 4Ds: dermatitis, diarrhea, dementia & deathNiacin Toxicity - ✔✔Nicotinic acid is prescribed in gram as a drug to lower blood cholesterol in hypercholesterolemia or hypertriglyceridemia Pharmacological doses may cause heart abnormalities, GI problem, hot flashes, skin irritations & liver damage UL = 35 mg/day Pantothenic Acid (B5) - ✔✔Pantothenic acid (vitamin B5)or pantothenate (Greek: pantos means everywhere) Widely distributed in all plant and animal foods ( deficiency is unlikely) Pantothenic acid is typically used to synthesize CoA & acyl carrier protein (ACP) Food Sources of Pantothenic Acid - ✔✔meat, fish, poultry milk and yogurt legumes and whole grain cereals Digestion, Absorption, Transport & Storage of Pantothenic Acid - ✔✔CoA is hydrolyzed to pantothenic acid before absorption by enterocyte Low conc. are absorbed by a sodium-dependent active process, high conc. are via passive diffusion Most of the pantothenic acid in blood is found in red blood cells Heart, muscle & liver cells take up by Na+- dependent active transport, but nervous, adipose & renal uptake is via passive diffusionMetabolism and Excretion of Pantothenic Acid - ✔✔CoA is dephosphorylated and through a series of subsequent reactions --> pantothenic acid Pantothenic acid is excreted as such primarily in urine Urinary excretion is thought to reflect dietary intake AI for Pantothenic Acid - ✔✔5 mg/day AI is used instead of RDA when there are insufficient data available to establish RDA Constituent of Coenzyme A (Pantothenic Acid) - ✔✔Pyruvate dehydrogenase complex Reacts with oxaloacetate to form citrate in Krebs Makes ketone bodies in liver Makes fatty acids & cholesterol Binds with fatty acids to start B-oxidation Constituent of Coenzyme ACP - ✔✔Acyl carrier in the synthesis of fatty acids Pantothenic Acid Functions - ✔✔Both oxidation and synthesis of fats utilize acetylCoA. However, the acetyl-CoA in fat synthesis exists in cytosol that is bound to the enzyme complex with malonyl-CoA. The enzyme, acetyl-CoA carboxylase (ACC), is the major site of regulation of fatty acid synthesis.ACC requires a biotin co-factor Pantothenic Acid Deficiency - ✔✔Very rare and only in cases of severe malnutrition. Symptoms of a pantothenic acid deficiency include burning feet syndrome (a feeling of tingling and tenderness in the feet), headache, fatigue, and a sensation of weakness. No reports of pantothenic acid toxicity Biotin (B7) - ✔✔Biotin was once referred to as vitamin H Within many foods, biotin is bound to protein as biocytin or biotinyllysine Active form is as biocytin occurred in four carboxylases The protein avidin in raw egg white binds biotin and prevents intestinal absorption --> deficiency Intestinal flora produces a small amount of biotin Biotin Food Sources - ✔✔Widely distributed in foods such as liver, soybeans, egg yolk, cereals & nuts, etc Digestion, Absorption, Transport & Storage of Biotin - ✔✔Proteins that contain biotin --> biocytin --> free biotin for absorption by enterocyte via Na + - dependent process High dose of biotin is absorbed via passive diffusion - 80% of biotin is free in the blood, but some are bound by proteins Bioavailability of biotin is variable from 100% in corn to near 0% in wheatBiotin appears to be stored, at least to a minor degree, in muscle, brain & liver Metabolism and Excretion of Biotin - ✔✔Biotin metabolites in urine include free biotin, bisnorbiotin, biotin sulfone & biotin sulfoxide, etc Biotin Deficiency - ✔✔Raw egg white (avidin) --> binding biotin & preventing absorption Inflammatory bowel disease --> inhibiting bacterium growth --> inhibiting biotin synthesis AI of Biotin - ✔✔30 ug/day AI is used instead of RDA when there are insufficient data available to establish RDA Vitamin B6 - ✔✔Vitamin B6 appears in the body in six chemical forms that are interchangeable Active form is Pyridoxal phosphate (PLP) Pyridoxine (PN) or pyridoxine phosphate (PNP) is found [Show More]
Last updated: 1 year ago
Preview 1 out of 69 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
We Accept:

Reviews( 0 )
$8.00
Document information
Connected school, study & course
About the document
Uploaded On
Sep 04, 2022
Number of pages
69
Written in
Additional information
This document has been written for:
Uploaded
Sep 04, 2022
Downloads
0
Views
76



.png)



.png)