*NURSING > QUESTIONS & ANSWERS > NCCT Practice Test 2 Billing and Coding Questions and Answers Latest Updated with Complete Solutions (All)
NCCT Practice Test 2 Billing and Coding Questions and Answers Latest Updated with Complete Solutions
Document Content and Description Below
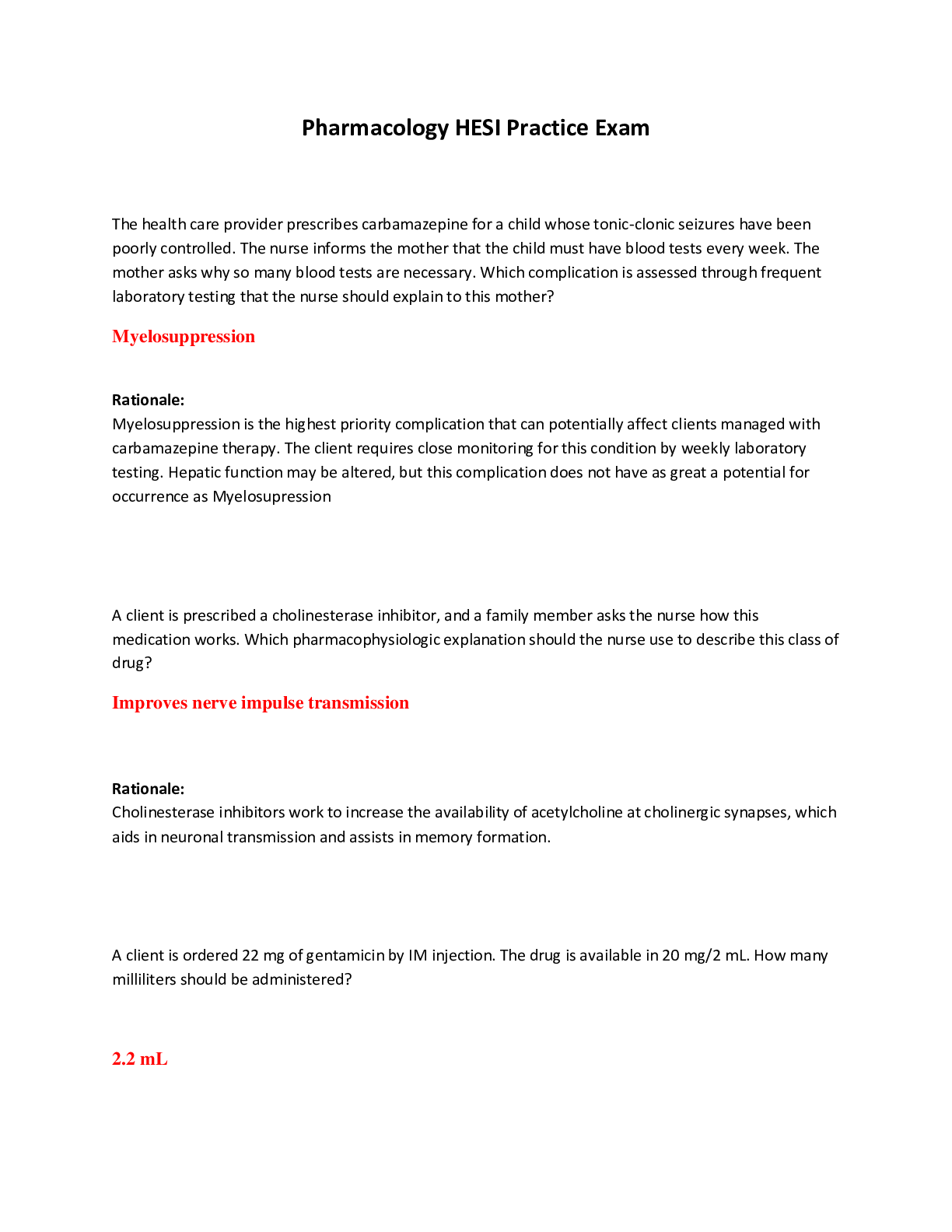
NCCT Practice Test 2 Billing and Coding Questions and Answers Latest Updated with Complete Solutions CPT codes are Correct Answer-5 digits An organization which provides a wide range of services f... or a specified group at a fixed periodic payment is termed an Correct Answer-HMO TBSA refers to: Correct Answer-Total body surface area There are two types of CPT codes, stand alone and: Correct Answer-Indented Codes Services in which opinions of specialists are requested, are called: Correct Answer-Consultations Examples of HCPCS Level II codes are: Correct Answer-Supplies, orthotics, prosthetics, DME, equipment, and ambulance services Everything that you see, hear, or read about a patients condition must remain: Correct AnswerConfidential Because of the new Medicare regulations insurance companies are predominantly using what type of claims? Correct Answer-Electronic A "combining form" meaning joint is: Correct Answer-Arthro/o If an error is made in a patients chart, what should be done before adding the correct information nearby? Correct Answer-Draw a single line through the error When sequencing codes for multiple burns, list: Correct Answer-Third degree firstAnother name for a release of information form is a: Correct Answer-Consent Which of the following is not a type of wound? Correct Answer-Excision The opposite of ventral is: Correct Answer-Dorsal In a Medicare billing dispute, the amount of controversy must be at least: Correct Answer-$100 A suffix indicating the surgical creation of an opening is: Correct Answer-Ostomy The usual abbreviation for complete blood count is: Correct Answer-CBC Which of the following abbreviations might charted if a patient has a bladder infection: Correct AnswerUTI All of the following are included in the Medicare EPSDT program for welfare children except: Correct Answer-Remedial Education Intentional misrepresentation of facts in order to deceive or mislead others is: Correct Answer-Fraud Self-Employed insurance billing specialists can deduct all but which one of the following expenses from income taxes: Correct Answer-Theatre Tickets The medical term for high blood pressure: Correct Answer-Hypertension An individual who promises to pay the medical bill by signing an agreement to pay form is the: Correct Answer-Guarantor A report mentioning such words as cranium, maxilla, and mandible would be referring to: Correct AnswerHeadThe following subsections of Evaluation and Management services except: Correct Answer-Concurrent Care In the Medicare program a clean claim means that: Correct Answer-D. The claim has no deficiencies, does not further investigation, and that it passes all electronic edits HCT is the medical abbreviation for: Correct Answer-Hematocrit The subsequent injury fund was established for problems that arise when a: Correct Answer-Previously injured person is injured at work again Tricare offers 3 types of plans: Correct Answer-Standard, Extra & Prime Workers Compensation can be found in: Correct Answer-All US States A 66 year old retired school teacher presenting for a first visit at a medical office would most likely be covered by: Correct Answer-Medicare When a claim is returned for incorrect or missing information, the correct action for a medical biller to take would be to: A. Add or correct the information & resubmit the claim B. Send an appeal letter C. Schedule a hearing before an administrative law judge D. Resend duplicate claim Correct Answer-Add or correct the information & resubmit the claim One insurance plan jointly sponsored by federal & state government is: A. Medicare B. Medicaid C. Tricare D. Blue Cross/Blue Shield Correct Answer-MedicaidIf a person is enlisted in the military service and killed in the line of duty, future medical benefits for his/her family would be covered under: A. Tricare B. Social Security C. ChampVA D. Workers' Compensation Correct Answer-CHAMPVA A patients medical record should be faxed only if: A. It is convenient for both the sender & the recipient B. The patient asks for it to be delivered via fax C. There is an emergent need for the information stated by the physician D. The medical assistant or insurance clerk chooses to do so Correct Answer-There is an emergent need for the information stated by the physician To keep insurance in force, a person must pay a monthly, quarterly, or annual fee known as the: A. Premium B. Deductible C. Co-Insurance D. Co-Payment Correct Answer-Premium Seven days after major surgery, the surgical wound dressing change would be: A. Coded 15852 B. Included in the surgical package & not billed C. Coded 15850 D. Coded using modifier - 24 Correct Answer-Included in the surgical package & not billed If a patient had an operative procedure on his/her thumb on the right hand, a coder would: A. Use the appropriate CPT procedure code only B. Add modifier RT to the appropriate procedure code C. Add modifier F5 to the appropriate procedure code D. Add modifier FA to the appropriate procedure code Correct Answer-Add Modifier F5 to the appropriate procedure codeThe anesthesia physical status code modifier for a patient with severe systemic disease is: A. 99116 B. P1 C. P2 D. P3 Correct Answer-P3 Lou Gehrigs disease is also known as: A. Amytrophic Lateral Sclerosis B. Gehrig-Hoffman disease C. Louis Barr syndrome D. Epstein-Barr Infection Correct Answer-Amytrophic Lateral Sclerosis For the insurance check to go directly to the physician, the patient must sign an: A. Consent to release medical information B. Assignment of Benefits form C. Financial responsibility form D. A guarantor Signature Correct Answer-Assignment of Benefits When making arrangements in the physician's office to collect payment in more than 4 installments (excluding the down payment) a specific written disclosure agreement needs to be signed according: A. Equal credit opportunity act B. Fair credit billing act C. Truth in lending act D. Statute of limitation Correct Answer-Truth in Lending Act Physician office coding systems are used for diagnosis and: A. Symptoms B. Services and Procedures C. Computer directories D. Appointments Correct Answer-Services and ProceduresIn order to work competently as a medical claims specialist in a physicians office, one needs: A. To learn to do medical transcription B. To know procedural & diagnostic coding C. To take the hippocratic oath D. Certification as a medical assistant Correct Answer-to know procedural & diagnostic coding In addition to medical data, the medical record may include: A. Personal Data B. Financial Data C. Social Data D. All answers are correct Correct Answer-D. All Answers are correct : Personal data, financial data & social data Medical ethics will typically address standards of: A. Law B. Courtesy C. Safety D. Conduct Correct Answer-Conduct Everything that a medical claims specialist learns about a patients condition must remain: A. Accurate B. Confidential C. Historical D. Inclusive Correct Answer-Confidential Which of the following skills would not be required for accurate filing of claims: A. Computer Programming B. Medical Terminology C. Basic Mathematics D. Keyboarding Correct Answer-Computer Programming Which of the following is not typical knowledge expected of an insurance billing specialist:A. How to prevent fraudulent claims B. Constitutes abuse when processing insurance claims C. How to respond to a subpoena D. How to repair a fax machine Correct Answer-How to repair a fax machine A legally enforceable document composed by an insurance company describing an agreement is a: A. Application B. Policy C. Health Plan D. Eligibility Verification Correct Answer-Policy Who should interpret reports and laboratory test to the patient: A. The Physician B. The medical billing specialist C. The medical assistant D. The Nurse Correct Answer-The Physician An insurance and billing specialist should be able to do all but which of the following: A. Define common insurance terms B. Advise patients which insurance companies offer the best insurance C. Handle insurance claims to to minimize rejection by carriers D. Ask appropriate question to complete a patient record Correct Answer-Advise patients which insurance companies offer the best insurance Which of the following is not an area of expected expertise for the medical billing specialist: A. ICD- 9 B. CPT Coding C. Counseling D. Claims processing Correct Answer-Counseling The following should be considered when selecting and setting up a computer system except: A. Electrical ModificationsB. Cost C. Decor D. Storage capacity Correct Answer-Decor Medical ethics has to do with: A. Consideration for others B. Customs in the medical profession C. Conduct, Courtesy , & manners D. Making right and wrong decisions Correct Answer-making right and wrong decisions Computer data regarding patient medical records is considered: A. Confidential B. Efficient C. Transient D. Accurate Correct Answer-Confidential A destructive computer program that attaches itself to other programs is called a: A. Revision B. Update C. Malignancy D. Virus Correct Answer-Virus Backing-Up refers to: A. Saving Data B. Working Cautiously C. Ergonomic furniture D. Extra stuff Correct Answer-Saving Data A list of items displayed on a computer screen from which the operator can choose a function is termed a: A. Window B. MenuC. Directory D. Hard Drive Correct Answer-Menu Billing for services not provided is an example of: A. Incentives B. Pre-planning C. Fraud D. Abuse Correct Answer-Fraud Claims for services deemed not medically necessary by insurance plans or programs are examples of: A. Abuse B. Hardship waivers C. Improper delegation D. Fraud Correct Answer-Abuse A form sent to the insurance company to find out the maximum dollar amount that will be paid for a procedure is called insurance: A. Certification Form B. Preauthorization Form C. Pre certification Form D. Pre determination Correct Answer-Predetermination form A government program that provides medical services for dependents of active military personnel: A. Medicare B. Medicaid C. Tricare D. ChampVA Correct Answer-Tricare A program that insures a person against on the job injury or illness is called: A. State disability B. Workers' compensation C. Workmens' insuranceD. Prepaid health Correct Answer-Workers' Compensation Third party payers require all the following information except: A. Triplicate copies of invoices B. Diagnosis using ICD-9 CM codes C. DOS D. POS Correct Answer-triplicate copies of invoices Careful and thorough recording of information at the time of the initial office visit: A. Takes too long B. Is always done by the insurance specialist C. Enables one to handle insurance claims promptly D. Is done only when the patient is scheduled for durgery Correct Answer-Enables one to handle insurance claims promptly If a claim is filed after the submission time limit for the carrier, payment is usually: A. Processed B. Guaranteed C. Denied D. Suspended Correct Answer-Denied Incorrect payments form an insurance company should be: A. Appealed B. Accepted C. Forwarded to the patient D. Deposited Correct Answer-Appealed A physician who will accept assignment under blue cross blue shield is called a: A. Member Physician B. Group practice C. Non-member provider D. Nonparticipating provider Correct Answer-Member PhysicianThe amount that a physician normally or usually charges the majority of his or her patients is the: A. Customary Fee B. RUV C. RBRVS D. UCR Correct Answer-Customary fee Random audits of medical records by insurance carriers are used to: A. Catch errors by insurance companies B. Monitor coding accuracy C. Assess physician dictation timeliness D. Revise CPT codes Correct Answer-Monitor coding accuracy A correctly completed claim submitted within the policy time limit is termed a: A. Paper Claim B. Paid Claim C. Legal Claim D. Clean Claim Correct Answer-Clean claim An EOB document may include all of the following except: A. Deductible B. Patient Name C. Allowed Amounts D. Coding Updates Correct Answer-Coding updates Claims paid with no errors are considered: A. Closed B. Pending C. Filed D. Suspended Correct Answer-Closed A third party entity that receives, separates, and transmits claims to the appropriate payer is called:A. Carrier B. Insurance Specialist C. Clearinghouse D. National Network Correct Answer-Clearinghouse Large medical practices generally submit electronic claims: A. Daily B. Hourly C. Weekly D. Monthly Correct Answer-Hourly [Show More]
Last updated: 1 year ago
Preview 1 out of 27 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
We Accept:

Reviews( 0 )
$8.00
Document information
Connected school, study & course
About the document
Uploaded On
Sep 09, 2022
Number of pages
27
Written in
Additional information
This document has been written for:
Uploaded
Sep 09, 2022
Downloads
0
Views
68