*NURSING > EXAM > NR 507 Advanced Pathophysiology Week 2 Quiz . Chamberlain College of Nursing | NR507 Week 2 Q&A (All)
NR 507 Advanced Pathophysiology Week 2 Quiz . Chamberlain College of Nursing | NR507 Week 2 Q&A
Document Content and Description Below
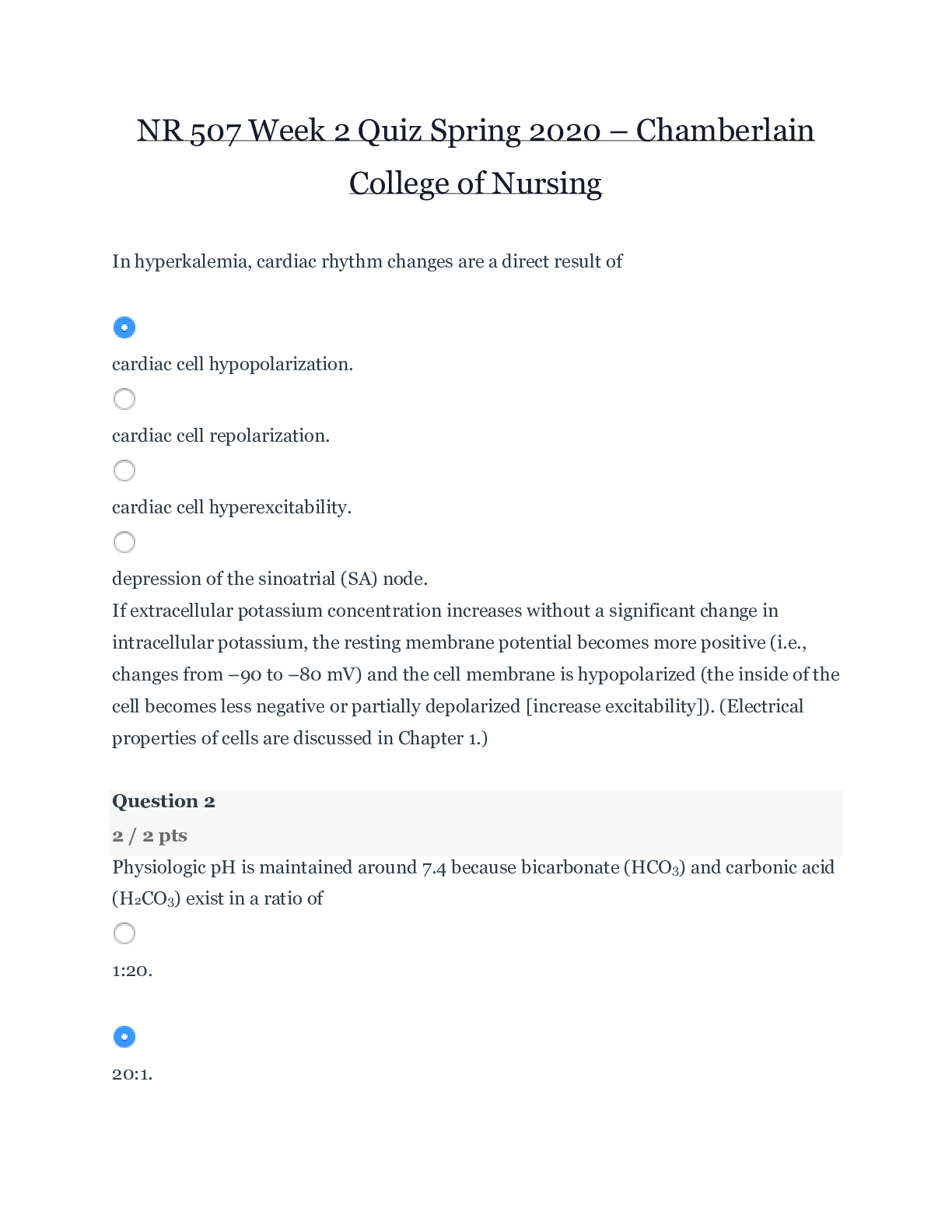
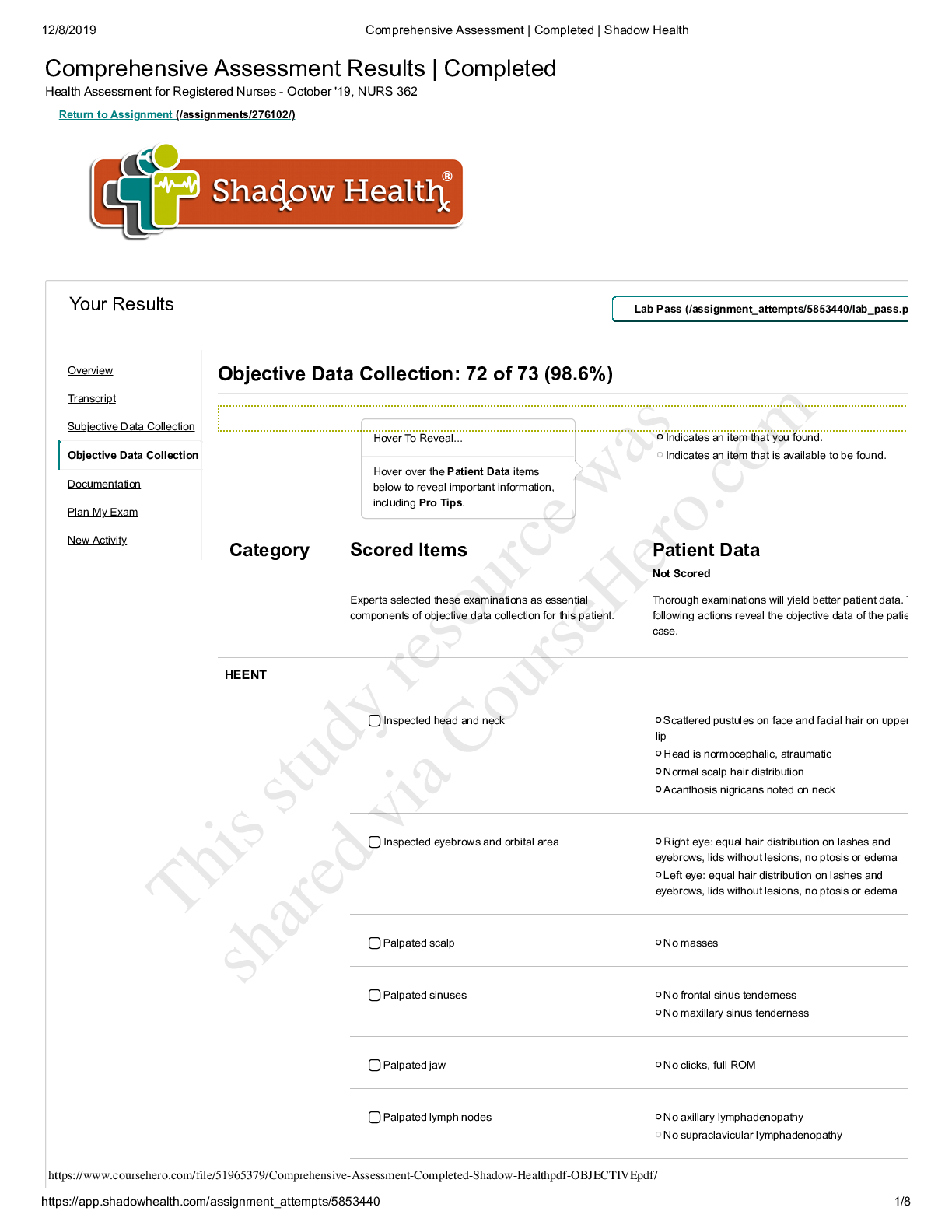
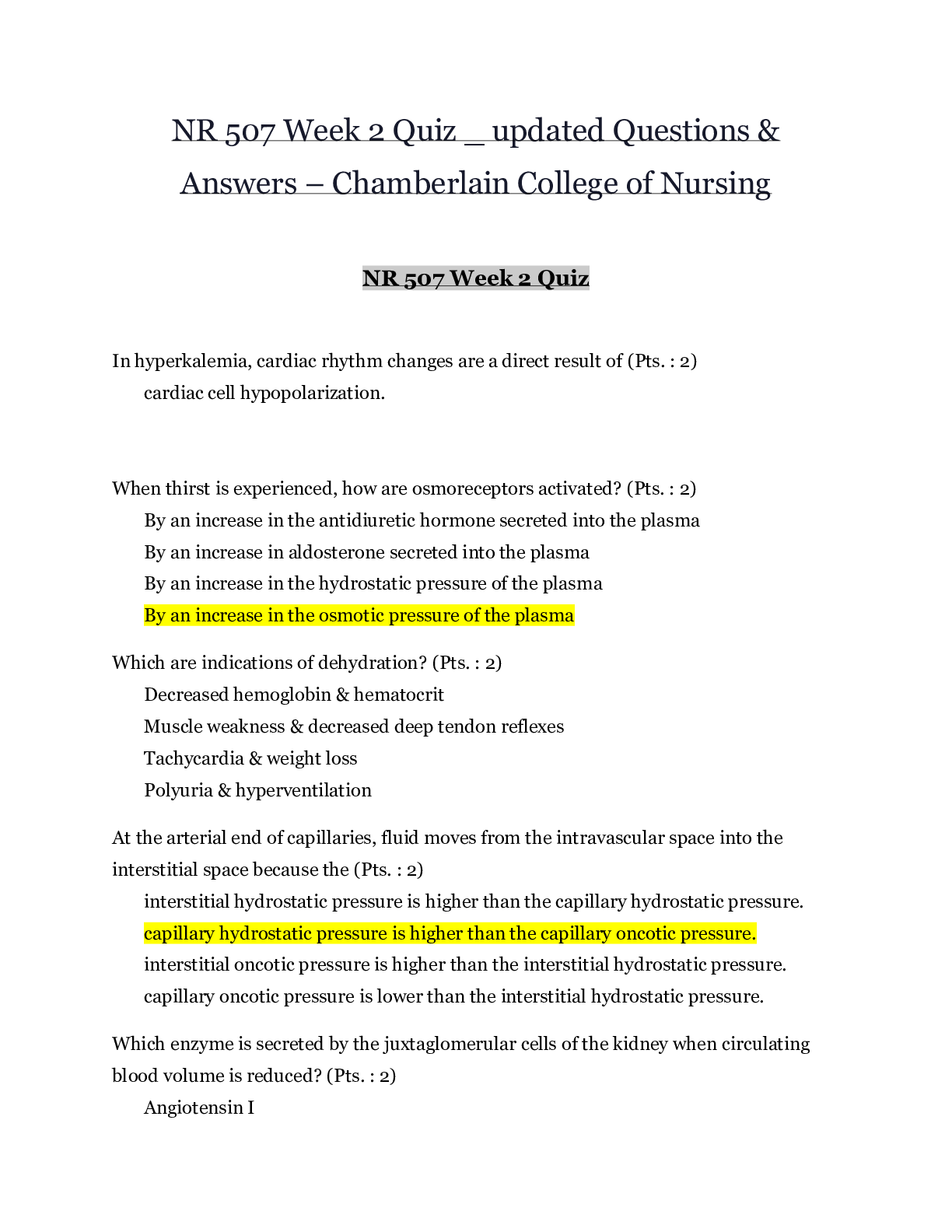
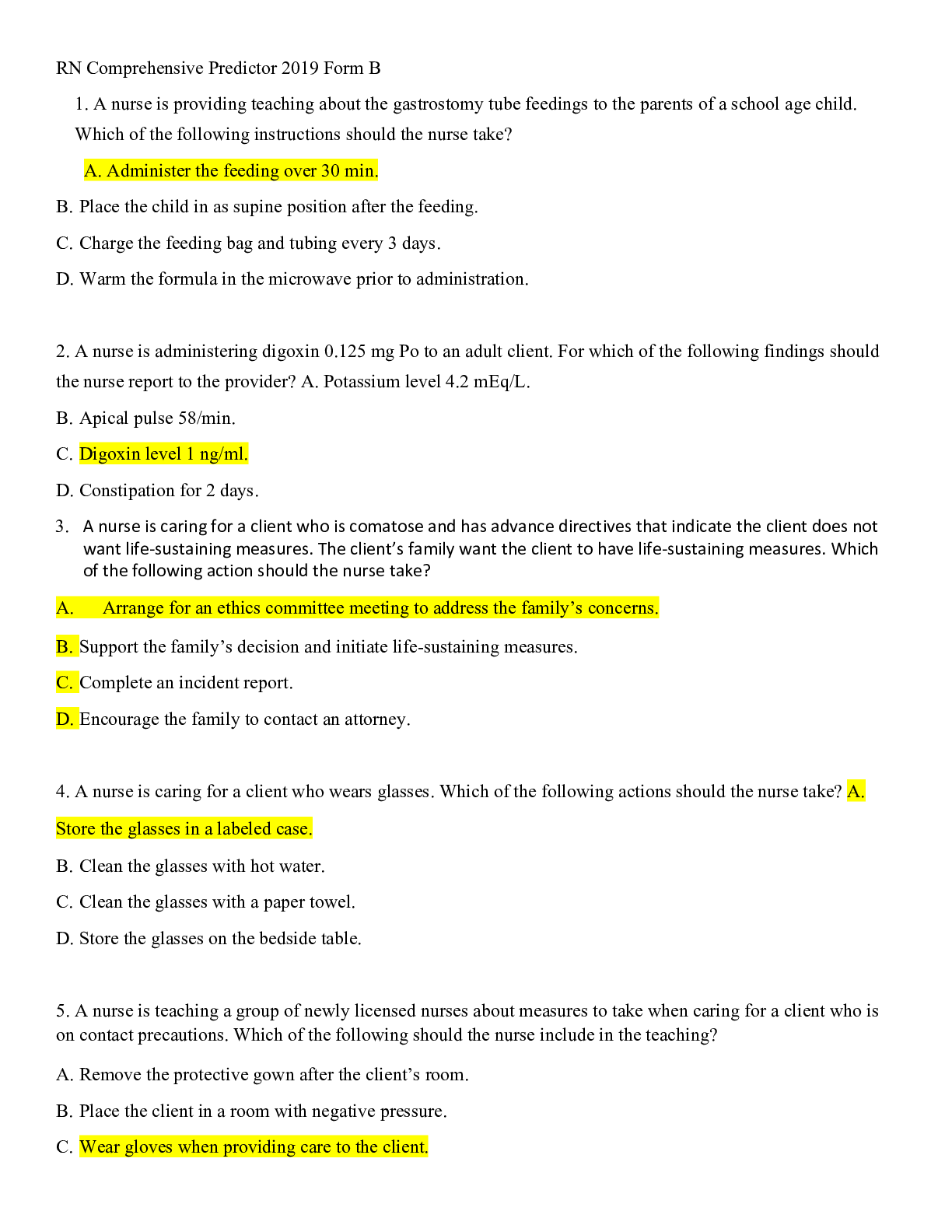
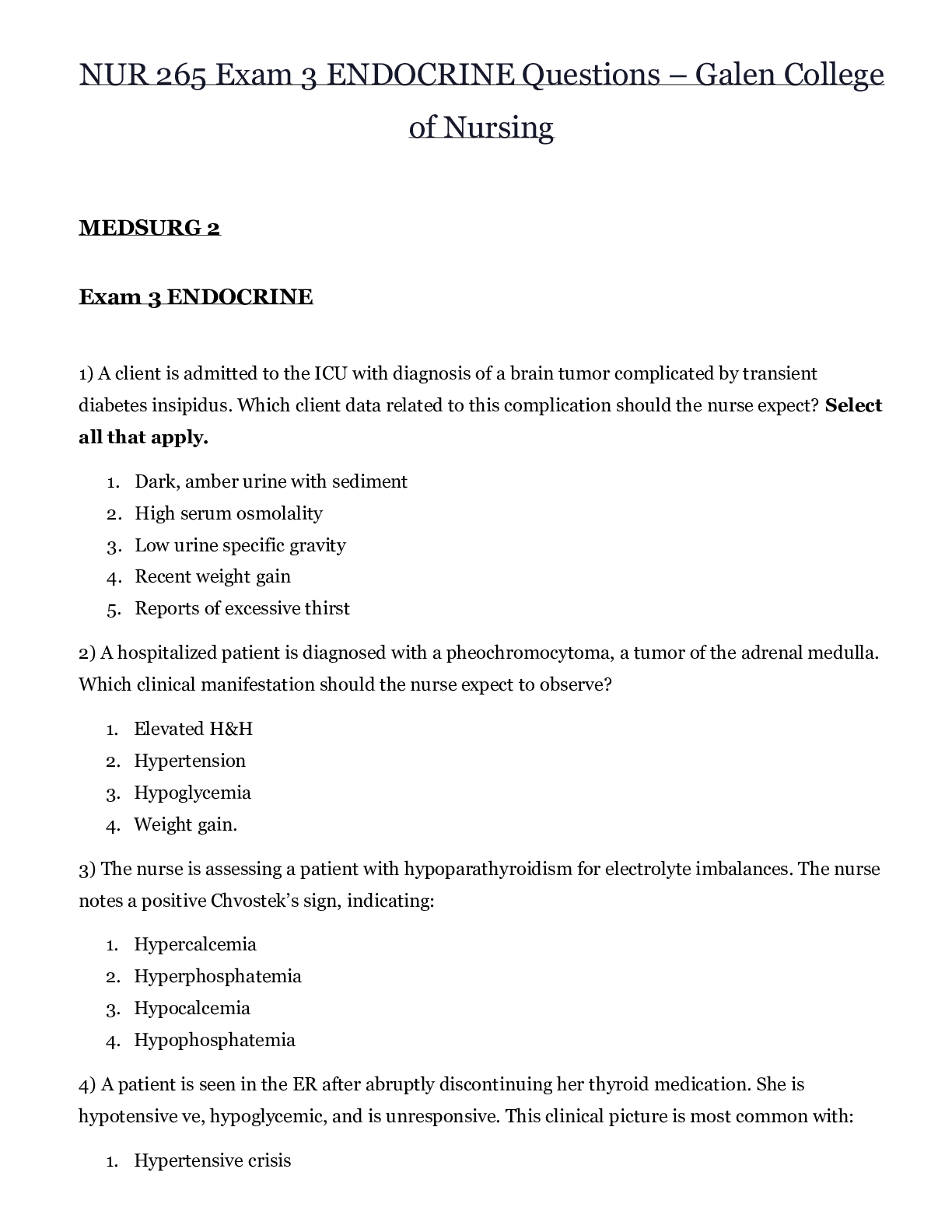
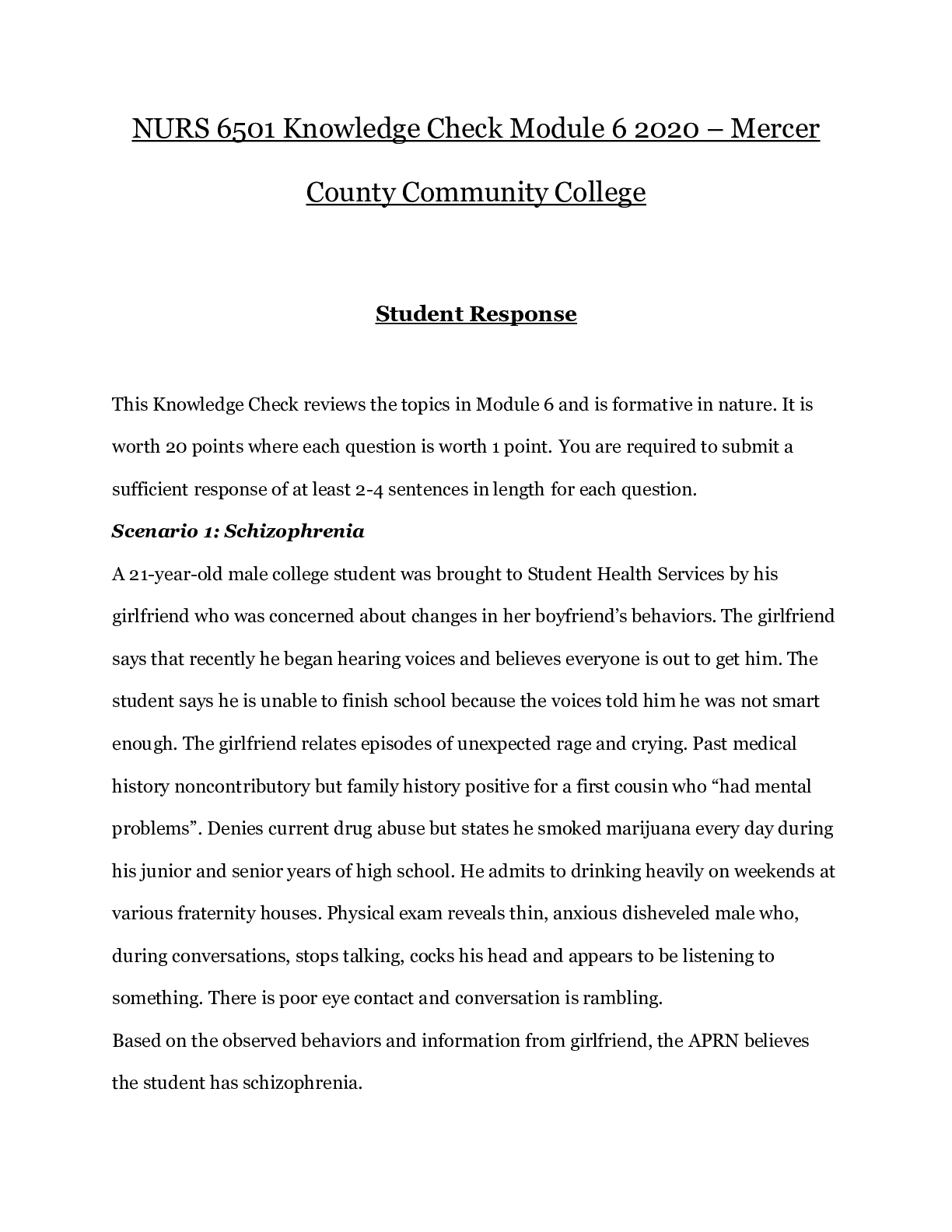
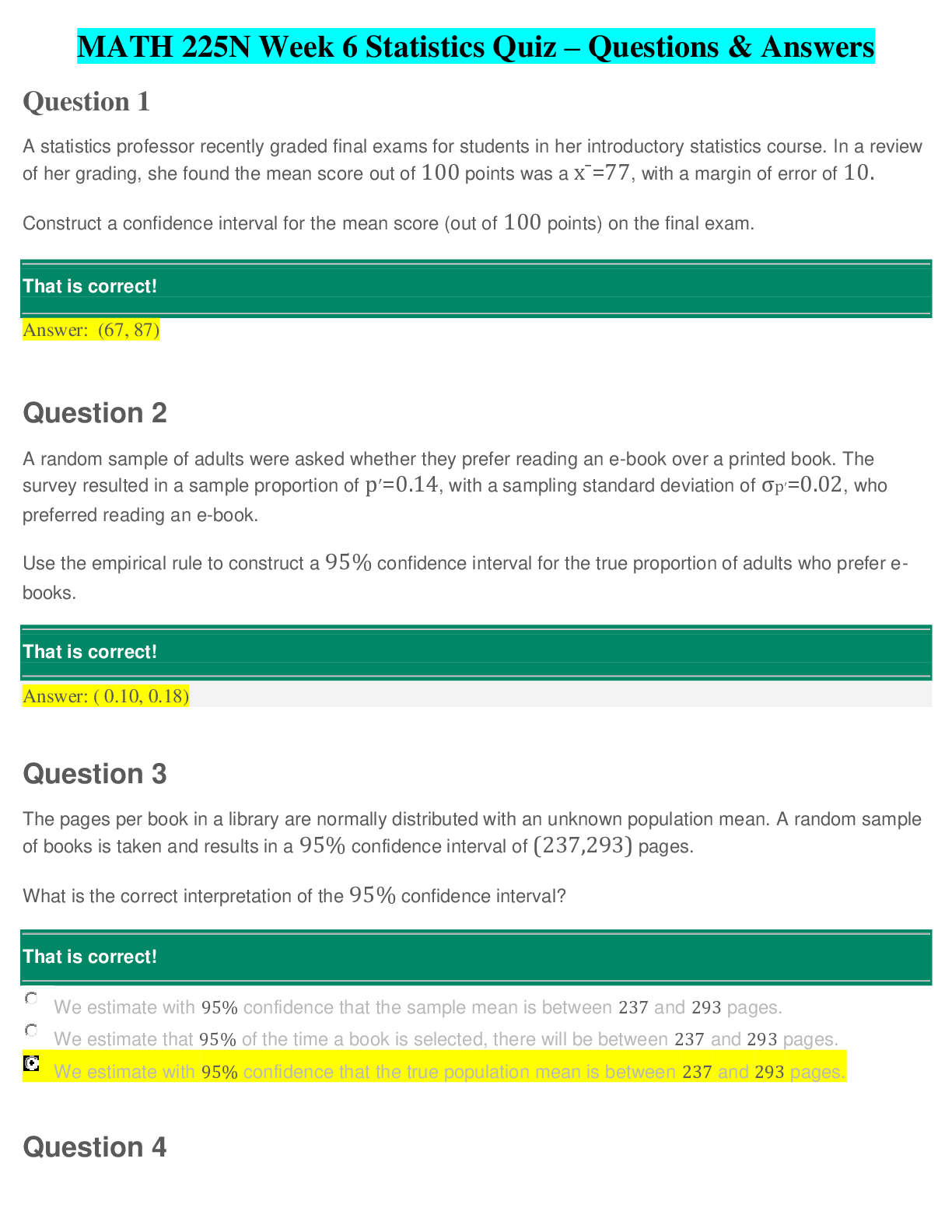
NR 507 Week 2 Quiz – Chamberlain College of Nursing In hyperkalemia, cardiac rhythm changes are a direct result of Correct! cardiac cell hypopolarization. cardiac cell repolariz... ation. cardiac cell hyperexcitability. depression of the sinoatrial (SA) node. If extracellular potassium concentration increases without a significant change in intracellular potassium, the resting membrane potential becomes more positive (i.e., changes from –90 to –80 mV) and the cell membrane is hypopolarized (the inside of the cell becomes less negative or partially depolarized [increase excitability]). (Electrical properties of cells are discussed in Chapter 1.) Question 2 2 / 2 pts Physiologic pH is maintained around 7.4 because bicarbonate (HCO3) and carbonic acid (H2CO3) exist in a ratio of 1:20. Correct! 20:1. 10:2. 10:5. The relationship between bicarbonate and carbonic acid is usually expressed as a ratio. When the pH is 7.40, this ratio is 20:1 (bicarbonate/carbonic acid). Question 3 2 / 2 pts Chvostek sign and Trousseau sign indicate hypokalemia. hyperkalemia. Correct! hypocalcemia. hypercalcemia. Two clinical signs are Chvostek sign and Trousseau sign. Question 4 2 / 2 pts Which are indications of dehydration? Polyuria and hyperventilation Muscle weakness and decreased deep tendon reflexes Decreased hemoglobin and hematocrit Correct! Tachycardia and weight loss Marked water deficit is manifested by symptoms of dehydration: headache, thirst, dry skin and mucous membranes, elevated temperature, weight loss, and decreased or concentrated urine (with the exception of diabetes insipidus). Skin turgor may be normal or decreased. Symptoms of hypovolemia, including tachycardia, weak pulses, and postural hypotension, may be present. Question 5 2 / 2 pts How does the loss of chloride during vomiting cause metabolic alkalosis? Loss of chloride causes hydrogen to move into the cell and exchange with potassium to maintain cation balance. Loss of chloride stimulates the release of aldosterone, which causes the retained sodium to bind with the chloride. Correct! Loss of chloride causes retention of bicarbonate to maintain the anion balance. Loss of chloride causes hypoventilation to compensate for the metabolic alkalosis. When acid loss is caused by vomiting with depletion of ECF and chloride (hypochloremic metabolic alkalosis), renal compensation is not very effective because the volume depletion and loss of electrolytes (Na+, K+, H+, Cl-) stimulate a paradoxical response by the kidneys. The kidneys increase sodium and bicarbonate reabsorption with excretion of hydrogen. Bicarbonate is reabsorbed to maintain an anionic balance because the ECF chloride concentration is decreased. Question 6 0 / 2 pts Water movement between the intracellular fluid compartment and the extracellular compartment is primarily a function of You Answered antidiuretic hormone. hydrostatic forces. plasma oncotic pressure. Correct Answer osmotic forces. The movement of water between ICF and ECF compartments is primarily a function of osmotic forces. (Osmosis and other mechanisms of passive transport are discussed in Chapter 1.) Question 7 0 / 2 pts At the arterial end of capillaries, fluid moves from the intravascular space into the interstitial space because the Correct Answer capillary hydrostatic pressure is higher than the capillary oncotic pressure. interstitial hydrostatic pressure is higher than the capillary hydrostatic pressure. You Answered capillary oncotic pressure is lower than the interstitial hydrostatic pressure. interstitial oncotic pressure is higher than the interstitial hydrostatic pressure. At the arterial end of capillaries, fluid moves from the intravascular space into the interstitial, because capillary hydrostatic pressure is higher than the capillary oncotic pressure. Question 8 0 / 2 pts In ARDS, alveoli and respiratory bronchioles fill with fluid as a result of the increased capillary hydrostatic pressure that forces fluid into the alveoli and respiratory bronchioles. Correct Answer inactivation of surfactant and the impairment of type II alveolar cells. You Answered increased capillary permeability, which causes alveoli and respiratory bronchioles to fill with fluid. compression on the pores of Kohn, thus preventing collateral ventilation. Lung inflammation and injury damages the alveolar epithelium and the vascular endothelium. Surfactant is inactivated, and its production by type II alveolar cells is impaired as alveoli and respiratory bronchioles fill with fluid or collapse. Question 9 2 / 2 pts _____ is a fulminant form of respiratory failure characterized by acute lung inflammation and diffuse alveolocapillary injury. Pulmonary emboli Correct! Acute respiratory distress syndrome (ARDS) Acute pulmonary edema Pneumonia ARDS is a fulminant form of respiratory failure characterized by acute lung inflammation and diffuse alveolocapillary injury. Question 10 2 / 2 pts Clinical manifestations that include unexplained weight loss, dyspnea on exertion, use of accessory muscles, and tachypnea with prolonged expiration are indicative of chronic bronchitis. pneumonia. Correct! emphysema. asthma. Individuals with emphysema usually have dyspnea on exertion that later progresses to marked dyspnea, even at rest (Table 33-3). Little coughing and very little sputum are produced. The individual often is thin, has tachypnea with prolonged expiration, and must use accessory muscles for ventilation. The anteroposterior diameter of the chest is increased (barrel chest), and the chest has a hyperresonant sound with percussion. Question 11 2 / 2 pts Pulmonary edema usually begins at a pulmonary capillary wedge pressure or left atrial pressure of _____ mm Hg. 10 30 40 Correct! 20 Pulmonary edema usually begins to develop at a pulmonary capillary wedge pressure or left atrial pressure of 20 mm Hg. Question 12 2 / 2 pts Kussmaul respirations may be characterized as a respiratory pattern with alternating periods of deep and shallow breathing. commonly observed in pulmonary fibrosis. commonly observed in chronic obstructive pulmonary disease. Correct! with a slightly increased ventilatory rate, large tidal volumes, and no expiratory pause. Kussmaul respirations are characterized by a slightly increased ventilatory rate, very large tidal volume, and no expiratory pause. Question 13 2 / 2 pts Which inflammatory mediators are produced in asthma? Lymphokines, serotonin, and prostaglandins Bradykinin, serotonin, and neutrophil proteases Neutrophil proteases, bradykinin, and histamine Correct! Histamine, prostaglandins, and leukotrienes A large number of inflammatory mediators, such as histamine, prostaglandins, and leukotrienes are produced by asthma. Question 14 2 / 2 pts Which pleural abnormality involves a site of pleural rupture that act as a one-way valve, permitting air to enter on inspiration but preventing its escape by closing during expiration? Secondary pneumothorax Spontaneous pneumothorax Correct! Tension pneumothorax Open pneumothorax In tension pneumothorax, the site of pleural rupture acts as a one-way valve, permitting air to enter on inspiration but preventing its escape by closing up during expiration. As more and more air enters the pleural space, air pressure in the pneumothorax begins to exceed barometric pressure. Question 15 2 / 2 pts In tuberculosis, the body walls off the bacilli in a tubercle by stimulating phagocytosis by neutrophils and eosinophils. formation of immunoglobulin G to initiate the complement cascade. Correct! apoptotic infected macrophages that activate cytotoxic T cells. macrophages that release TNF-α. In defense, macrophages and lymphocytes release interferon, which inhibits the replication of the microorganism and stimulates more macrophages to attack the bacterium. Apoptotic infected macrophages also can activate cytotoxic T cells (CD8). Question 16 0 / 2 pts Dyspnea is not a result of fatigue of the intercostal muscles and diaphragm. You Answered decreased pH, increased PaCO2, and decreased PaO2. Correct Answer decreased blood flow to the medulla oblongata. stimulation of stretch or J-receptors. There are no data to support the role of decreased blood flow to the medulla oblongata as being a cause of dyspnea. Question 17 2 / 2 pts Clinical manifestations of pulmonary hypertension include dyspnea on exertion and paroxysmal nocturnal dyspnea. Correct! peripheral edema and jugular venous distention. productive cough and rhonchi bilaterally. systemic blood pressure greater than 130/90. Symptoms of fatigue, chest discomfort, tachypnea, and dyspnea on exertion, palpitations, and cough are common. Examination may reveal peripheral edema, jugular venous distention, a precordial heave, and accentuation of the pulmonary compartment of the second heart sound. Question 18 2 / 2 pts High altitudes may produce hypoxemia through diffusion abnormalities. hypoventilation. shunting. Correct! decreased inspired oxygen. The first factor is the presence of adequate oxygen content of the inspired air. Oxygen content is lessened at high altitudes. Question 19 0 / 2 pts The release of fibroblast growth factors affects ARDS by causing You Answered disruption of alveolocapillary membrane. Correct Answer pulmonary fibrosis. atelectasis and decreased lung compliance. pulmonary hypertension. In the fibroproliferative phase, type II alveolar cells proliferate, and there is alveolar septal thickening and collagen deposition. Interstitial fibrosis can be evident as early as 10 days after the initial insult. Similarly, vascular changes may occur, including obliteration of the microcirculation and thickening of the walls of pulmonary arterioles and arteries, which can lead to chronic pulmonary hypertension in survivors. Question 20 0 / 2 pts Which of the following statements about the advances in the treatment of RDS of the newborn is incorrect? You Answered Administering glucocorticoids to women in preterm labor accelerates the maturation of the fetus’s lungs. Treatment includes the instillation of exogenous surfactant down an endotracheal tube of infants weighing less than 1,000 g. Supporting the infant’s respiratory function by using continuous positive airway pressure (CPAP). An infant’s respiratory function is supported by using continuous pressure (CPAP). Correct Answer Administering oxygen to mothers during preterm labor increases their arterial oxygen before birth of the fetus. Administration of oxygen to the mother is not a valid treatment of RDS. Question 21 2 / 2 pts Chest wall compliance in infants is _____ in adults. Correct! higher than lower than the same as unlike that Chest wall compliance is high in infants, particularly premature infants. Question 22 2 / 2 pts Cystic fibrosis (CF) is caused by a(n) malignancy. infection. autosomal dominant inheritance. Correct! autosomal recessive inheritance. Cystic fibrosis is an autosomal recessive inherited disorder that is associated with defective epithelial ion transport. Question 23 2 / 2 pts Which immunoglobulin is present in childhood asthma? Correct! IgE IgA IgG IgM Included in the long list of asthma-associated genes are those that code for increased levels of immune and inflammatory mediators (e.g., IL-4, IgE, and leukotrienes), nitric oxide, and transmembrane proteins in the endoplasmic reticulum. Question 24 2 / 2 pts Which of the following types of croup is most common? Fungal Autoimmune Correct! Viral Bacterial In 85% of cases, croup is caused by a virus, most commonly parainfluenza; however, other viruses such as influenza A or RSV also can cause croup. Question 25 2 / 2 pts An accurate description of childhood asthma is that it is a(n) Correct! obstructive airway disease characterized by reversible airflow obstruction, bronchial hyperreactivity, and inflammation. pulmonary disease characterized by severe hypoxemia, decreased pulmonary compliance, and diffuse densities on chest x-ray. pulmonary disorder involving an abnormal expression of a protein producing viscous mucus that lines the airways, pancreas, sweat ducts, and vas deferens. obstructive airway disease characterized by atelectasis and increased pulmonary resistance as a result of a surfactant deficiency. Asthma is an obstructive airway disease characterized by reversible airflow obstruction, bronchial hyperreactivity, and inflammation. PreviousNext Last Attempt Details: Time: 38 minutes Current Score: 38 out of 50 Kept Score: 38 out of 50 Unlimited Attempts Take the Quiz Again (Will keep the highest of all your scores) [Show More]
Last updated: 9 months ago
Preview 1 out of 15 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Sep 06, 2020
Number of pages
15
Written in
Additional information
This document has been written for:
Uploaded
Sep 06, 2020
Downloads
1
Views
95




 – CHAMBERLAIN COLLEGE OF NURSING.png)

 – Chamberlain College of Nursing.png)