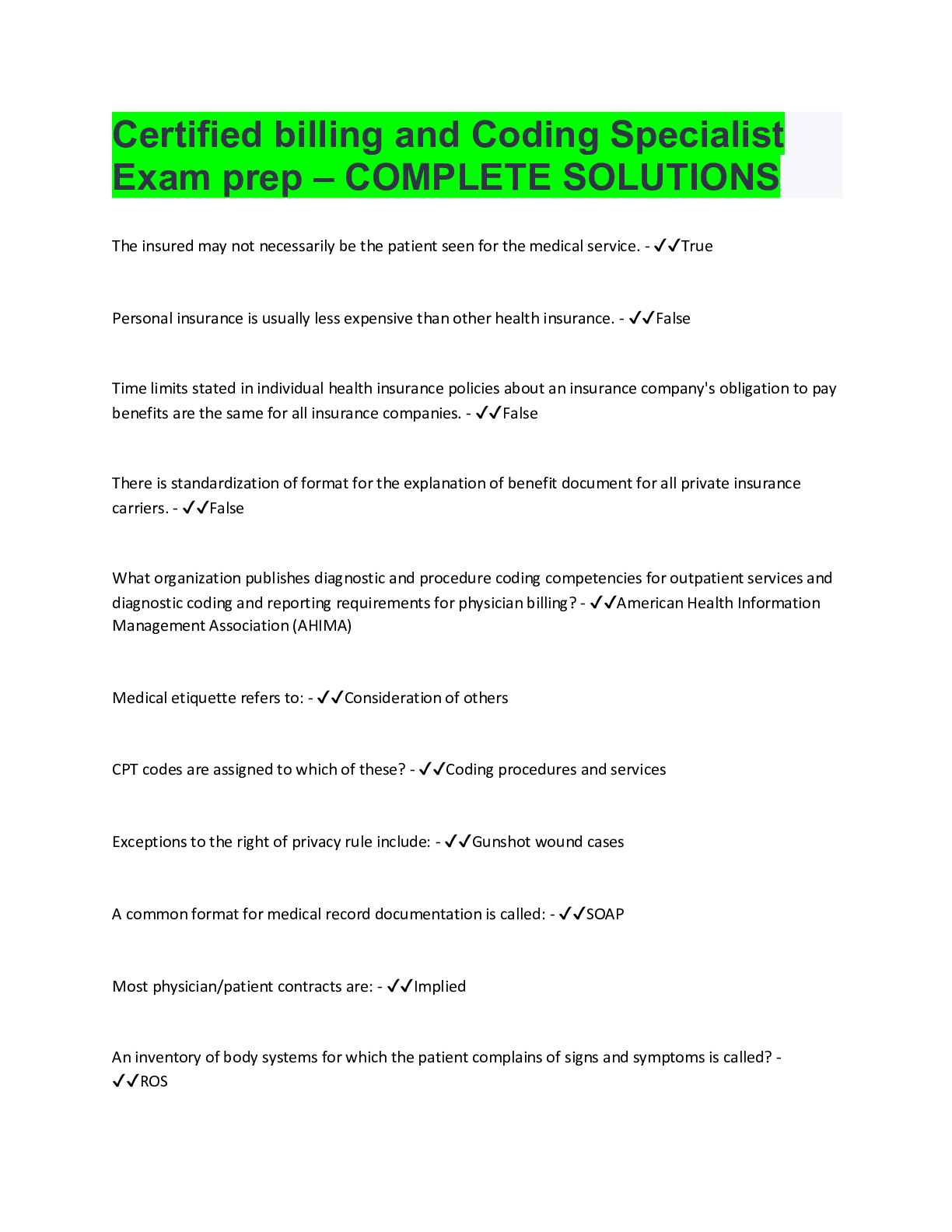
Computer Science > QUESTIONS & ANSWERS > NHA - Certified Billing and Coding Specialist (CBCS) Study Guide (All)
NHA - Certified Billing and Coding Specialist (CBCS) Study Guide
Document Content and Description Below
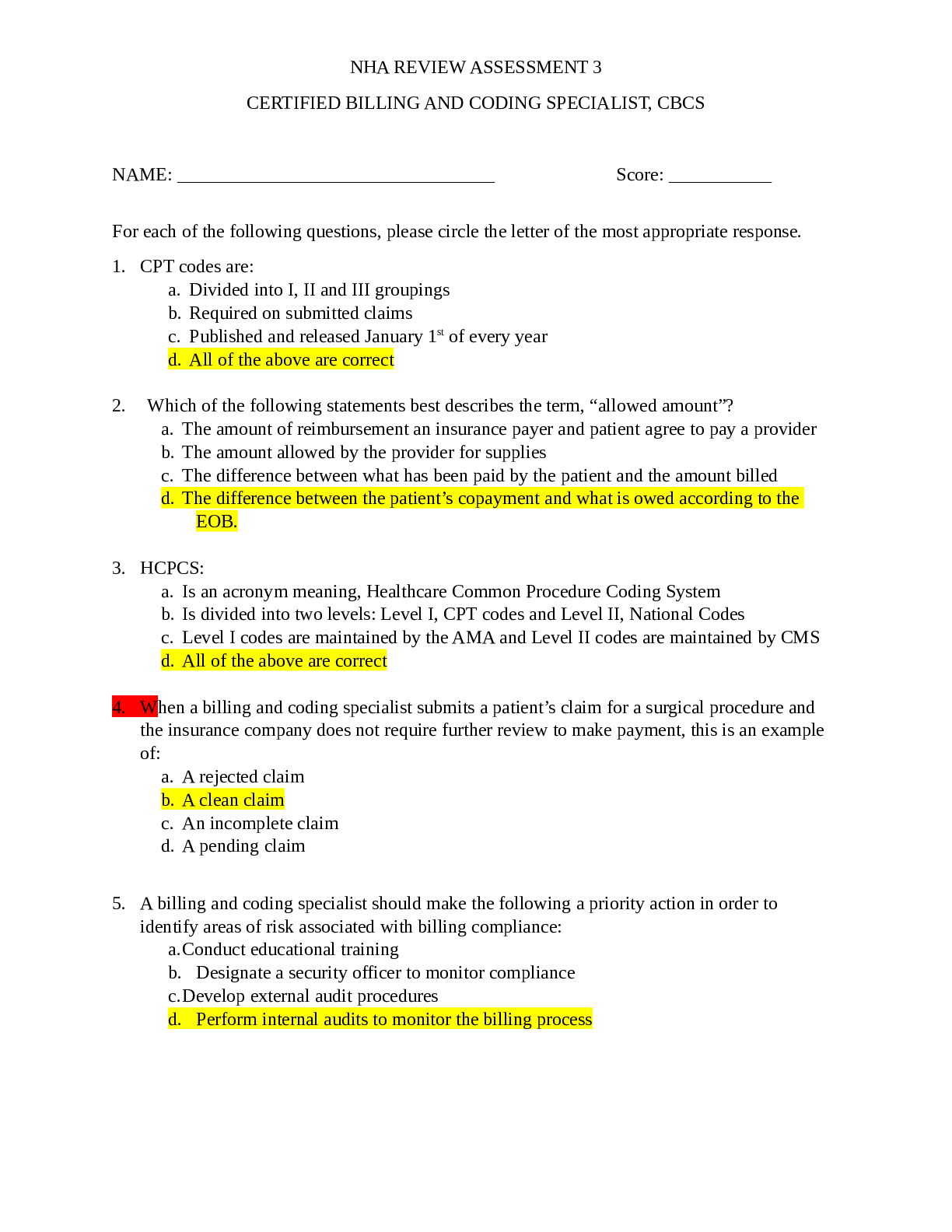
The symbol "O" in the Current Procedural Terminology reference is used to indicate what? - Ans-Reinstated or recycled code In the anesthesia section of the CPT manual, what are considered qualifyin... g circumstances? - Ans-Add-on codes As of April 1, 2014 what is the maximum number of diagnoses that can be reported on the CMS-1500 claim form before a further claim is required? - Ans-12 What is considered proper supportive documentation for reporting CPT and ICD codes for surgical procedures? - Ans-Operative report What action should be taken first when reviewing a delinquent claim? - Ans-Verify the age of the account A claim can be denied or rejected for which of the following reasons? - Ans-Block 24D contains the diagnosis code A coroner's autopsy is comprised of what examinations? - Ans-Gross Examination Medigap coverage is offered to Medicare beneficiaries by whom? - Ans-Private third-party payers What part of Medicare covers prescriptions? - Ans-Part C What plane divides the body into left and right? - Ans-Sagittal Where can unlisted codes be found in the CPT manual? - Ans-Guidelines prior to each section Ambulatory surgery centers, home health care, and hospice organizations use which form to submit claims? - Ans-UB-04 Claim Form What color format is acceptable on the CMS-1500 claim form? - Ans-Red Who is responsible to pay the deductible? - Ans-Patient A patient's health plan is referred to as the "payer of last resort." What is the name of that health plan? - Ans-Medicaid Informed Consent - Ans-Providers explain medical or diagnostic procedures, surgical interventions, and the benefits and risks involved, giving patients an opportunity to ask questions before medical intervention is provided. Implied Consent - Ans-A patient presents for treatment, such as extending an arm to allow a venipuncture to be performed. Clearinghouse - Ans-Agency that converts claims into standardized electronic format, looks for errors, and formats them according to HIPAA and insurance standards. Individually Identifiable - Ans-Documents that identify the person or provide enough information so that the person can be identified. De-identified Information - Ans-Information that does not identify an individual because unique and personal characteristics have been removed. Consent - Ans-A patient's permission evidenced by signature. Authorizations - Ans-Permission granted by the patient or the patient's representative to release information for reasons other than treatment, payment, or health care operations. Reimbursement - Ans-Payment for services rendered from a third-party payer. Auditing - Ans-Review of claims for accuracy and completeness. Fraud - Ans-Making false statements of representations of material facts to obtain some benefit or payment for which no entitlement would otherwise exist. Upcoding - Ans-Assigning a diagnosis or procedure code at a higher level than the documentation supports, such as coding bronchitis as pneumonia. Unbundling - Ans-Using multiple codes that describe different components of a treatment instead of using a single code that describes all steps of the procedure. Abuse - Ans-Practices that directly or indirectly result in unnecessary costs to the Medicare program. Business Associate (BA) - Ans-Individuals, groups, or organizations who are not members of a covered entity's workforce that perform functions or activities on behalf of or for a covered entity. What is the main job of the Office of the Inspector General (OIG)? - Ans-The OIG protects Medicare and other HHS programs from fraud and abuse by conducting audits, investigations , and inspections. Medicare - Ans-Federally funded health insurance provided to people age 65 or older, and people 65 and younger with certain disabilities. Medicaid - Ans-A government-based health insurance option that pays for medical assistance for individuals who have low incomes and limited financial resources. Timely Filing Requirements - Ans-Within 1 calendar year of a claim's date of service. Electronic Data Interchange (EDI) - Ans-The transfer of electronic information in a standard form. Coordination of Benefits Rules - Ans-Determines which insurance plan is primary and which is secondary. Conditional Payment - Ans-Medicare payment that is recovered after primary insurance pays. Crossover Claim - Ans-Claim submitted by people covered by a primary and secondary insurance plan. Assignment of Benefits - Ans-Contract in which the provider directly bills the payer and accepts the allowable charge. Allowable Charge - Ans-The amount an insurer will accept as full payment, minus applicable cost sharing. Clean Claim - Ans-Claim that is accurate and complete. They have all the information needed for processing, which is done in a timely fashion. Dirty Claim - Ans-Claim that is inaccurate, incomplete, or contains other errors. Medicare Administrative Contractor (MAC) - Ans-Processes Medicare Parts A and B claims from hospitals, physicians, and other providers. Remittance Advice (RA) - Ans-The report sent from the third-party payer to the provider that reflects any changes made to the original billing. Explanation of Benefits (EOB) - Ans-Describes the services rendered, payment covered, and benefit limits and denials. National Provider Identifier (NPI) - Ans-Unique 10-digit code fro providers required by HIPAA. Heath Maintenance Organization (HMO) - Ans-Plan that allows patients to only go to physicians, other health care professionals, or hospitals on a list of approved providers, except in an emergency. Modifier - Ans-Additional information about types of services, and part of valid CPT or HCPCS codes. By signing block 12 of CMS-1500 form, a patient is doing what? - Ans-Authorizes the release of medical information. Claim - Ans-Complete record of the services provided by the health care professional, along with appropriate insurance information. Where does the NPI number go on the CMS-1500 form? - Ans-17b What are two pieces of information that need to be collected from patients? - Ans-Full name and date of birth. Deductible - Ans-The amount [Show More]
Last updated: 1 year ago
Preview 1 out of 14 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
We Accept:

Also available in bundle (1)
NHA CBCS BUNDLE QUESTIONS AND ANSWERS,
All you need to pass the NHA CBCS exams, Rated A+
By bundleHub Solution guider 1 year ago
$24
5
Reviews( 0 )
$10.00
Document information
Connected school, study & course
About the document
Uploaded On
Jun 11, 2022
Number of pages
14
Written in
Additional information
This document has been written for:
Uploaded
Jun 11, 2022
Downloads
0
Views
63




.png)
.png)
 Study Guide.png)

