Pharmacology > QUESTIONS & ANSWERS > Pharm Exam 1 questions with answers and explanations, 100% Mastery, Graded A+ (All)
Pharm Exam 1 questions with answers and explanations, 100% Mastery, Graded A+
Document Content and Description Below
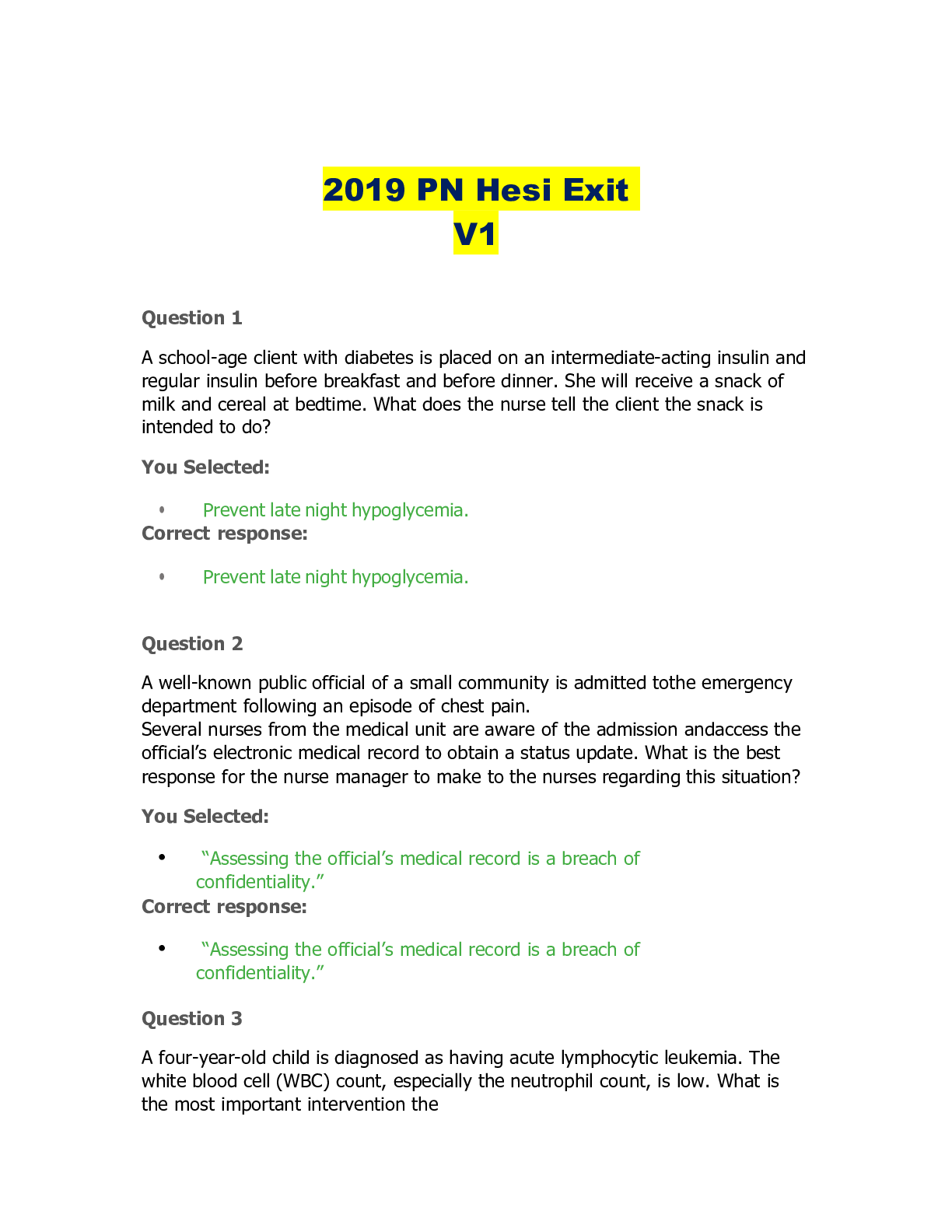
Pharm Exam 1 questions with answers and explanations, 100% Mastery, Graded A+ A patient who has HIV and is taking the nucleoside/nucleotide reverse transcriptase inhibitor (NRTI) zidovudine (Re... trovir) reports vomiting, abdominal pain, fatigue, and hyperventilation. Which laboratory result is the priority for the nurse to evaluate? A) Megakaryocytes B) Red blood cell (RBC) counts C) CD4 T-lymphocyte counts D) Arterial blood lactate - ☑☑D Potentially fatal lactic acidosis and hepatic steatosis (fatty liver) can occur with all NRTIs. Measuring arterial blood lactate is a priority for the diagnosis of lactic acidosis. Associated symptoms of nausea, vomiting, abdominal pain, fever, and hyperventilation may occur. Megakaryocytes, RBC counts, and CD4 T-lymphocyte counts also may be measured with NRTI therapy, but alterations in these values are not associated with the complication of lactic acidosis. A nurse should recognize that a patient who is infected with HIV is at the highest risk to develop opportunistic infections during which clinical phase of HIV? A) Late B) Intermediate C) Initial D) Prodromal - ☑☑A During the late phase of HIV infection, CD4 T lymphocytes (CD4 T cells) are reduced below a critical level (200 cells/mL). This significantly increases the risk for opportunistic infections. During the initial phase of HIV infection, patients experience flulike symptoms of fever, pharyngitis, and myalgias. In the intermediate or middle phase of HIV infection, blood levels of HIV remain low and most patients are asymptomatic. There are no prodromal or premonitory clinical signs that indicate the onset of HIV infection. A patient has been prescribed efavirenz (Sustiva). The nurse should instruct the patient to use which administration approach to minimize central nervous system (CNS) adverse effects? A) The drug should be taken in divided doses throughout the day. B) Bedtime dosing is most effective. C) The drug should be mixed only with an acidic beverage. D) A steroid medication should be used concurrently. - ☑☑B Efavirenz frequently causes CNS symptoms of dizziness, impaired consciousness, drowsiness, vivid dreams, and nightmares. Bedtime dosing can minimize CNS effects, which typically resolve in 2 to 4 weeks. Mixing with an acidic beverage, using a steroid medication concurrently, and taking efavirenz in divided doses throughout the day are not effective means of minimizing CNS effects. The antiretroviral medication raltegravir (Isentress) achieves therapeutic effectiveness through which action when administered to a patient infected with HIV? A) It blocks the entry of HIV into CD4 T cells. B) It increases protease enzyme activity. C) It inhibits the enzyme integrase. D) It destroys reverse transcriptase. - ☑☑C Raltegravir is the first and only member of a new class of antiretroviral medications, the HIV integrase inhibitors. Integrase is one of three viral enzymes needed for HIV-derived DNA insertion into DNA of CD4 T cells. Raltegravir effectively blocks HIV replication. It does not increase protease enzyme activity or destroy reverse transcriptase. Blocking HIV entry into CD4 T cells is an action of other antiretroviral medications, not raltegravir. Which administration instruction should the nurse give a patient scheduled to start receiving the HIV fusion inhibitor enfuvirtide (Fuzeon)? A) "Rotate injection sites in the arm, thigh, and abdomen." B) "Take only when you consume low-fat meals." C) "Dosing is optimal 30 minutes before meals." D) "Injection-site reactions are usually uncommon." - ☑☑A The primary action of enfuvirtide is to block the entry of HIV into CD4 T cells. It is administered through subcutaneous injection, and the injections should be rotated in the upper arm, thigh, and abdominal areas of the body. Injection-site reactions of pain, tenderness, erythema, and induration occur in almost every patient. Enfuvirtide is not an oral medication; dosing before meals or with low-fat meals is not a relevant instruction. A nurse should recognize that which laboratory result is used as a major factor in deciding when antiretroviral therapy is indicated for a patient infected with HIV? A) Plasma HIV RNA assay B) CD4 T-lymphocyte count C) Western blot assay D) OralQuick Rapid HIV-1 Antibody Test - ☑☑B The CD4 T-cell count is the principal indicator of how much immunocompetence remains when a patient is infected with HIV. It is used as a guide in the initiation, discontinuation, and resumption of medications for opportunistic infections. A plasma HIV RNA assay is a measure of viral load that indicates HIV replication and magnitude and accordingly is used to predict clinical outcomes. The Western blot assay and OralQuick Rapid HIV-1 Antibody Test, respectively, are used for initial screening and follow-up confirmation of HIV infection. A nurse should teach a patient who has Pneumocystis pneumonia (PCP) about the dosing and therapeutic effects of which medication? A) Trimethoprim/sulfamethoxazole (Bactrim) B) Azithromycin (Zithromax) C) Acyclovir (Zovirax) D) Ganciclovir (Cytovene) - ☑☑A PCP is a potentially fatal infection caused by Pneumocystis jiroveci. Among people with advanced HIV infection, it is the most common opportunistic infection. The preferred regimen for treatment and prophylaxis of PCP is trimethoprim/sulfamethoxazole. Azithromycin is used in the treatment of Mycobacterium avium infection. Cytomegalovirus (CMV) retinitis is treated with ganciclovir. Acyclovir is the preferred treatment of varicella-zoster virus, which causes chickenpox and herpes zoster. The human immunodeficiency virus (HIV) uses which enzymes to replicate and infect a host cell? (Select all that apply.) A) Integrase B) Dihydrofolate reductase C) Reverse transcriptase D) Carbonic anhydrase E) Protease - ☑☑A,C,E HIV is a retrovirus that replicates itself in a host cell by transcribing RNA into DNA. The enzyme used for this process is viral RNA-dependent DNA polymerase, commonly known as reverse transcriptase. HIV DNA becomes integrated into the host's DNA under the influence of a viral enzyme called integrase. Final maturation of HIV depends on protease, which breaks large HIV polyproteins into smaller, functional forms. Dihydrofolate reductase and carbonic anhydrase are other enzymes used to catalyze chemical cellular reactions, but they are not participants in HIV replication. A patient is receiving the protease inhibitor (PI) amprenavir (Agenerase). Which laboratory results would the nurse evaluate as indicators of adverse effects of this medication? (Select all that apply.) A) Plasma cholesterol level B) Serum transaminases C) Cardiac enzymes D) Blood glucose level E) Creatinine level - ☑☑A,B,D All PIs cause hyperglycemia and diabetes, and patients should be instructed to report symptoms of polydipsia, polyphagia, and polyuria. In addition, PIs can increase serum levels of transaminases and should be used with caution in patients with chronic liver disease. Cholesterol should be measured for elevation caused by the use of PIs that results in a risk of cardiovascular events. Altered cardiac enzymes and serum creatinine levels are not associated with adverse effects of PIs. A nurse develops a plan of care for a patient who has an outbreak of recurrent genital herpes and is taking oral acyclovir (Zovirax). Which outcome should be included? A) Minimal scarring from lesions B) Less frequent eruption of lesions C) Prevention of transmission to contacts D) Complete eradication of the virus - ☑☑B Acyclovir is used to treat herpes simplex infections caused by type 2 herpes simplex virus (HSV-2). For patients with recurrent herpes genitalis, oral therapy reduces the frequency with which lesions appear. It does not eradicate the virus or produce cure. Acyclovir does not prevent transmission of the virus to sexual contacts. It does not affect scarring from lesions. Which approach should a nurse take to administer intravenous (IV) acyclovir (Zovirax) to an immunocompromised patient? A) Infuse IV fluids during administration of the dose and for 2 hours afterward. B) Administer IV acyclovir diluted in 20 mL normal saline (NS) over 10 minutes. C) Only infuse the drug if the white blood cell (WBC) count is above 2500/mm3. D) Ask the provider to change the route to subcutaneous (subQ) injection. - ☑☑A Acyclovir can cause renal damage, and hydration of the patient during the infusion and for 2 hours afterward minimizes this risk. Acyclovir is not given by IV bolus or by intramuscular (IM) or subQ injection. It is used to treat infections in immunocompromised patients, but the dose is not changed or affected by the WBC count. A nurse is preparing to administer ganciclovir (Cytovene) to a patient for treatment of Cytomegalovirus (CMV) pneumonitis. Which laboratory result should the nurse recognize as a contraindication to use of this drug? A) Neutrophil count below 500/mm3 B) Platelet count of 350,000/mm3 C) Serum calcium level of 9.5 mg/dL D) Reduced forced vital capacity (FVC) - ☑☑A Ganciclovir is used to treat and prevent CMV infection in immunocompromised patients. Bone marrow suppression is a dose-limiting toxicity of ganciclovir; therefore, the drug is contraindicated in patients with neutrophil counts below 500/mm3 or platelet counts below 25,000/mm3. It does not affect the serum calcium level or FVC, a measure of lung function in patients who have airflow-restrictive disorders. A patient is receiving weekly subcutaneous injections of peg-interferon-alfa-2a (Pegasys) for chronic hepatitis C. A nurse teaches the patient that which adverse effect will diminish with continued therapy? A) Black, sticky, tarry stools B) Lower leg muscle weakness C) Dyspnea and wheezing D) Flulike symptoms - ☑☑D The most common adverse side effect of peg-interferon-alfa-2a, a long-acting interferon used to treat chronic hepatitis C, is flulike symptoms characterized by fever, fatigue, myalgia, headache, and chills. Symptoms are likely to diminish with continued therapy over time. Black, tarry stools; lower leg muscle weakness; dyspnea; and wheezing are not adverse effects of peg-interferon-alfa-2a. What is the priority instruction a nurse gives to a male patient who is scheduled to receive ribavirin (Rebetol) combined with peg-interferon-alfa-2a for treatment of hepatitis C? A) "Combining these two medications will greatly increase response rates." B) "An antidepressant can be prescribed to alleviate symptoms of depression." C) "If you are sexually active, use two reliable forms of birth control to prevent pregnancy." D) "It is very important that you have blood counts checked every 2 weeks." - ☑☑C Because ribavirin is embryolethal when taken by female patients and causes sperm abnormalities when taken by males, it is a priority that pregnancy be avoided during its use. Pregnancy must be avoided both by female patients and by female partners of men taking ribavirin. Couples should use two reliable forms of birth control during treatment and for 6 months afterward. It is less important that the patient know that ribavirin is not effective against hepatitis C unless it is combined with interferon alfa. Less important information to provide than avoiding pregnancy includes: hemolytic anemia is an adverse effect; frequent blood checks are advised; and depression is an adverse effect of peg-interferon-alfa-2a for which antidepressants can be prescribed. A nurse should recognize that for maximum therapeutic effects against the influenza virus, oseltamivir (Tamiflu) should be taken when? A) Two days or more after symptom onset B) When lung crackles are present C) Within 12 hours of symptom onset D) Only when fever is above 102°F - ☑☑C Oseltamivir is a neuraminidase inhibitor that is effective against the influenza A and influenza B viruses. Its benefits decline greatly when treatment is delayed. Dosing must begin early—no later than 2 days after symptom onset. If treatment is started within 12 hours of symptom onset, symptom duration is reduced by more than 3 days. Specific symptoms, such as lung crackles and fever above 102°F, are not criteria for receiving oseltamivir. A nurse is providing teaching to a group of patients regarding flu season in the United States. Which statement should the nurse include in the teaching? A) In the United States, flu season usually peaks in October or November. B) To insure full protection, the best time to vaccinate is September. C) For people who missed the best time, vaccinating as late as April may be of help. D) The influenza vaccine may not be administered at the same time as the pneumococcal vaccine. - ☑☑C Peak flu season in the United States is usually January or February. To ensure full protection, the best time to vaccinate is October or November. For people who missed the best time, vaccinating as late as April may be helpful. Influenza vaccine may be given at the same time as other vaccines, including pneumococcal vaccine. The nurse identifies which medication as the drug of choice for most infections caused by herpes simplex viruses and varicella-zoster virus? A) Ganiciclovir B) Amantadine C) Acyclovir D) Oseltamivir - ☑☑C Acyclovir is the drug of choice for most infections caused by herpes simplex viruses and varicella-zoster virus. Ganiciclovir is the drug of choice for prophylaxis and treatment of CMV infection in immunocompromised patients, including those with AIDS. Amantadine and Oseltamivir are drugs of choice for the treatment and prophylaxis of influenza. A nurse administering flu vaccines at an annual clinic should recognize that which individuals should be vaccinated, as recommended by the Advisory Committee on Immunization Practices (ACIP)? (Select all that apply.) A) Women who will be pregnant during flu season B) All children 6 months and older and older adults C) Those who report severe allergy to chicken eggs D) Those who have a history of Guillain-Barré syndrome E) Those 6 months to 18 years old receiving aspirin therapy - ☑☑A,B,E The ACIP recommends flu vaccination for all children 6 months and older and for older adults. Individuals at high risk of complications from the flu who also should be vaccinated include women who will be pregnant during flu season and children receiving long-term therapy with aspirin (to prevent Reye's syndrome). Influenza vaccines are produced from viruses grown in eggs and should be avoided in persons with allergies to chicken eggs. Influenza vaccine may carry a small risk of Guillain-Barré syndrome, a paralyzing neuromuscular disorder, and should be avoided in those who have experienced it. A patient has been diagnosed with respiratory syncytial virus. The nurse anticipatates administration of which drug(s)? (Select all that apply._ A) Ganciclovir B) Oseltamivir C) Ribavirin (inhaled) D) Palivizumab E) Entecavir - ☑☑C,D Ribavirin (inhaled) and Palivizumab are used for the treatment of RSV. Ganiciclovir is useful in the treatment of cytomegalovirus. Oseltamivir is used for the treatment of Influenza A and B. Entacavir is a nucleoside analog used in the treatment of HBV. When teaching a patient about therapy with Famciclovir, which statement(s) does the nurse include? (Select all that apply.) A) Famciclovir is generally well tolerated. B) Famciclovir is safe to use during pregnancy. C) Famciclovir is administered intravenously. D) Famiciclovir is used in the treatment of acute herpes zoster. E) Famiciclovir is contraindicated in the treatment of herpes simplex genitalis. - ☑☑A,D Famiciclovir is generally well tolerated and is used in the treatment of acute herpes zoster as well as herpes simplex genitalis. The safety of Famiciclovir during pregnancy and breat-feeding and in children younger than 18 years has not been established. Famiciclovir is supplied in tablets for oral dosing. The nurse is assessing a patient who is receiving a sulfonamide for treatment of a urinary tract infection. To monitor the patient for the most severe response to sulfonamide therapy, the nurse will assess for what? A) Diarrhea B) Skin rash and lesions C) Hypertension D) Bleeding - ☑☑B The nurse's priority is to monitor for hypersensitivity reactions. The most serious response to sulfonamide therapy is Stevens-Johnson syndrome, which manifests as symptoms of the skin and mucous membranes, lesions, fever, and malaise. In rare cases, hematologic effects occur, requiring periodic blood studies. A patient is receiving local applications of mafenide (Sulfamylon) to burn areas. Before application, it is most important for the nurse to do what? A) Administer a pain medication. B) Obtain a set of vital signs. C) Auscultate the lung fields. D) Obtain a signed consent form. - ☑☑A The sulfonamide mafenide (Sulfamylon) is used to suppress bacterial colonization in patients with burns. Local application frequently is painful. It is important to administer a pain medication before applying mafenide (Sulfamylon). Obtaining vital signs and a signed informed consent form and auscultating lung fields are not essential actions for mafenide application. A nurse should recognize that which sulfonamide, applied topically, has the greatest therapeutic benefit for burns? A) Sulfadiazine B) Trimethoprim (Trimpex) C) Sulfacetamide (Isopto Cetamide) D) Silver sulfadiazine (Silvadene) - ☑☑D Silver sulfadiazine is a topical anti-infective agent used to treat and prevent infection in second- and third-degree burns. Its effects are due primarily to the release of free silver and not to the sulfonamide portion of the molecule. Sulfadiazine and trimethoprim are sulfonamides used systemically, not topically. Sulfacetamide is used for superficial infections of the eye. A patient taking a sulfonamide is breast-feeding an infant. Which complication in the infant would the nurse associate with kernicterus? A) Hemolytic anemia B) Neurologic deficits C) Hepatocellular failure D) Ophthalmic infection - ☑☑B Kernicterus is a disorder in newborns caused by deposition of bilirubin in the brain, which leads to severe neurologic deficits and death. Sulfonamides promote kernicterus by displacing protein-bound bilirubin from the proteins, leaving newly freed bilirubin access to brain sites. Sulfonamides are not administered to infants under 2 years old, nor are they given to pregnant patients near term or nursing mothers. Hemolytic anemia, hepatocellular failure, and ophthalmic infection are not associated sulfonamide effects in infants. When providing patient teaching for oral sulfonamide therapy, the nurse should instruct the patient to take the sulfonamide in what way? A) At mealtime, when food is available B) With soy or nonmilk products C) Between meals with a full cup of water D) On awakening before breakfast - ☑☑C Oral sulfonamides should be taken on an empty stomach and with a full glass of water. To minimize the risk of renal damage, adults should maintain a daily urine output of 1200 mL. Sulfonamides should not be taken with soy or nonmilk products or food or before breakfast without liquids. Before administering trimethoprim, it is most important for the nurse to assess the patient for a history of what? A) Heart failure B) Alcoholism C) Diabetes D) Emphysema - ☑☑B Trimethoprim inhibits bacterial synthesis of folic acid. It is avoided in patients when folate deficiency is likely, such as in alcoholism, because bone marrow suppression may occur. Heart failure, diabetes, and emphysema are unrelated to adverse effects with trimethoprim. A patient who has acquired immunodeficiency syndrome (AIDS) is receiving trimethoprim/sulfamethoxazole (Bactrim). Which response should a nurse expect if the medication is achieving the desired effect? A) Increase in CD4 T cells B) Increased appetite and weight gain C) Resolution of pneumonia D) Decrease in joint pain - ☑☑C Trimethoprim/sulfamethoxazole is the treatment of choice for Pneumocystis pneumonia (PCP), an infection caused by Pneumocystis jiroveci (formerly thought to be Pneumocystis carinii). PCP is an opportunistic pneumonia caused by a fungus that thrives in immunocompromised hosts. It does not increase the number of CD4 T cells, the targeted cells of the human immunodeficiency virus (HIV), nor does it affect joint pain. Increased appetite and weight gain are not therapeutic actions of trimethoprim/sulfamethoxazole. When caring for a patient receiving mafenide (Sulfamylon) for treatment of a severe burn, it is most important for the nurse to monitor which laboratory value? A) Blood glucose level B) Acid-base status C) Sodium level D) Peak mafenide level - ☑☑B Mafenide (Sulfamylon) therapy is associated with the development of acidosis. Peak mafenide levels are not obtained. The blood glucose and sodium levels are not affected by mafenide. The nurse identifies which statements about Stevens-Johnson syndrome as true? (Select all that apply.) A) Patients with Stevens-Johnson syndrome have a mortality rate of about 25%. B) Toxemia is associated with Stevens-Johnson syndrome. C) Short-acting sulfonamides do not induce Stevens-Johnson syndrome. D) Patients with Stevens-Johnson syndrome usually are hypothermic. E) Lesions of the mucous membranes are a characteristic of Stevens-Johnson syndrome. - ☑☑A,B,E Short-acting sulfonamides do induce Stevens-Johnson syndrome on rare occasions, and patients with Stevens-Johnson syndrome usually are hyperthermic. The other three statements are true. Which manifestations does the nurse associate with the development of hemolytic anemia? (Select all that apply.) A) Urticaria B) Fever C) Pallor D) Jaundice E) Diarrhea - ☑☑B,C,D Urticaria and diarrhea are not associated with the development of hemolytic anemia. Fever, pallor, and jaundice are associated with the development of hemolytic anemia. A nurse is administering a daily dose of tobramycin (Nebcin) at 1000. At which time should the nurse obtain the patient's blood sample to determine the trough level? A) 0800 B) 0900 C) 1130 D) 1200 - ☑☑B Trough levels determine the lowest level between doses. Blood is drawn just before the next dose is administered when a divided dose is used or 1 hour before the next dose if a single daily dose is used. A patient who is receiving an aminoglycoside (gentamicin) has a urinalysis result with all of these findings. Which finding should a nurse associate most clearly with an adverse effect of gentamicin? A) White blood cells (WBCs) B) Glucose C) Ketones D) Protein - ☑☑D Aminoglycoside-induced nephrotoxicity usually presents as acute tubular necrosis. Symptoms of concern are protein in the urine, dilute urine, and elevation of the serum creatinine and blood urea nitrogen (BUN) levels. WBCs, glucose, and ketones are not specifically related to gentamicin use. A patient is receiving an aminoglycoside (tobramycin) antibiotic. A nurse asks the patient to choose daily meal selections, to which the patient responds, "Oh, dear, I don't want another IV." The nurse makes which assessment about the patient's response? A) Some hearing loss may have occurred. B) The confusion is due to the hospital stay. C) A nutrition consult most likely is needed. D) The patient has a family history of dementia. - ☑☑A The patient's comment suggests that the person did not hear the instructions. Aminoglycoside antibiotics can cause ototoxicity. The first sign may be tinnitus (ringing in the ears), progressing to loss of high-frequency sounds. Audiometric testing is needed to detect it. Nutrition, confusion, and a family history of dementia do not address the problem of possible hearing loss associated with aminoglycosides. A nurse monitors a patient who is receiving an aminoglycoside (gentamicin) for symptoms of vestibular damage. Which finding should the nurse expect the patient to have first? A) Unsteadiness B) Vertigo C) Headache D) Dizziness - ☑☑C Gentamicin causes irreversible ototoxicity, which results in both impaired hearing and disruption of balance. Headache is the first sign of impending vestibular damage (balance) and may last 1 to 2 days. Unsteadiness, vertigo, and dizziness appear after headache. The nurse knows that there is an increased risk of ototoxicity in a patient receiving an aminoglycoside if which level is high? A) Concentration B) Trough C) Peak D) Dose - ☑☑B When trough levels remain elevated, aminoglycosides are unable to diffuse out of inner ear cells, thus exposing the cells to the medication for an extended time. Prolonged exposure (i.e., high trough levels), rather than brief exposure to high levels, underlies cellular injury. When administering an aminoglycoside to a patient with myasthenia gravis, it is most important for the nurse to assess what? A) Deep tendon reflexes B) Breath sounds C) Eyelid movement D) Muscle strength - ☑☑B Aminoglycosides can inhibit neuromuscular transmission, causing potentially fatal respiratory depression. Patients with myasthenia gravis (MG) are at an increased risk. Deep tendon reflexes, eyelid movement, and muscle strength are important assessments for a patient who has MG, but they are not as important as airway and breathing ability. A patient who is receiving an aminoglycoside develops flaccid paralysis and impaired breathing. Which medication does the nurse anticipate administering? A) Magnesium sulfate (Epsom salt) B) Potassium chloride (K-Dur) C) Sodium bicarbonate (Citrocarbonate) D) Calcium gluconate (Kalcinate) - ☑☑D Flaccid paralysis and impaired breathing are signs of impaired neuromuscular transmission, which may occur with aminoglycosides, especially if they are administered concurrently with a neuromuscular blocking agent. Impaired transmission can be reversed with intravenous infusion of a calcium salt (calcium gluconate). Magnesium sulfate, potassium chloride, and sodium bicarbonate do not reverse impaired neuromuscular transmission caused by aminoglycosides. Which enteral aminoglycoside would the nurse expect to be ordered preoperatively for a patient having intestinal surgery? A) Gentamicin B) Tobramycin C) Amikacin D) Neomycin - ☑☑D In general, aminoglycosides are poorly absorbed in the gastrointestinal (GI) tract. Neomycin is given orally to suppress bowel flora before surgery of the intestine and is not used parenterally because of its high nephrotoxicity and ototoxicity. Gentamicin, tobramycin, and amikacin are administered parenterally only. Before administering an aminoglycoside, it is most important for the nurse to assess the patient for a history of what? A) Myasthenia gravis B) Asthma C) Hypertension D) Diabetes mellitus - ☑☑A Aminoglycosides can inhibit neuromuscular transmission, causing flaccid paralysis and potentially fatal respiratory depression. These drugs should be used with extreme caution in patients with myasthenia gravis. Which statements about ototoxicity and aminoglycosides does the nurse identify as true? (Select all that apply.) A) The risk of ototoxicity is related primarily to excessive peak levels. B) The first sign of impending cochlear damage is headache. C) The first sign of impending vestibular damage is tinnitus . D) Ototoxicity is largely irreversible. E) Use of aminoglycosides for less than 10 days is recommended to avoid ototoxicity. - ☑☑D,E The risk of ototoxicity with aminoglycoside use is related primarily to excessive trough levels. The first sign of impending vestibular damage is headache. The first sign of cochlear damage is tinnitus. The other two statements are true. Which statements about serum drug levels does the nurse identify as true? (Select all that apply.) A) With once-daily dosing, only trough levels need to be drawn. B) Peak levels for intramuscular (IM) injections should be drawn 30 minutes after administration of the medication. C) The trough level ideally should be close to zero. D) For patients receiving once-daily doses, the sample should be drawn 2 hours before the next dose. E) For patients receiving divided doses, trough levels should be drawn 1 hour before the next dose. - ☑☑A,B,C For patients receiving once-daily doses, the sample should be drawn 1 hour before the next dose. For patients receiving divided doses, trough levels should be drawn immediately before the next dose. The other three statements are true. Which instruction should a nurse include in the discharge teaching for a patient who is to start taking tetracycline (Sumycin)? A) "You may stop taking the pills when you begin to feel better." B) "Use sunscreen and protective clothing when outdoors." C) "You'll have to come back to the clinic for weekly blood work." D) "Take the medication with yogurt or milk so you won't have nausea." - ☑☑B Tetracyclines are bacteriostatic antibiotics; photosensitivity and severe sunburn are common adverse effects. A full course of antibiotics must always be taken. Blood studies are not necessary for therapeutic levels. Absorption decreases after ingestion of chelates, such as calcium and magnesium, so doses should be given 2 hours before or 2 hours after ingestion of milk products. A nurse assessing a patient who is 12 years old should associate which complication with the patient's receiving tetracycline (Sumycin) as a younger child? A) Delay in long bone growth B) Early onset of puberty C) Severe face and body acne D) Discoloration of the teeth - ☑☑D Tetracycline is contraindicated in children younger than 8 years of age, because it binds to calcium in developing teeth, resulting in permanent discoloration of the teeth. Delay in long bone growth, early onset of puberty, and severe face and body acne are not adverse effects associated with tetracyclines. Which laboratory result should a nurse monitor more frequently when a patient is receiving clarithromycin (Biaxin) and warfarin (Coumadin)? A) Activated partial thromboplastin time (aPTT) B) Platelet count C) Erythrocyte sedimentation rate (ESR) D) International normalized ratio (INR) - ☑☑D Clarithromycin is a macrolide similar to erythromycin and can inhibit hepatic metabolism of medications such as warfarin and theophylline. The INR is the blood test used to evaluate warfarin ranges. The aPTT is the blood test used in monitoring heparin. The platelet count and ESR are not affected by clarithromycin. A patient who has a vancomycin-resistant enterococci (VRE) infection is receiving linezolid (Zyvox). Which laboratory result indicates that the patient is having an adverse effect? A) White blood cell (WBC) count of 1200 units/L B) Hemoglobin (Hgb) level of 18 g/dL C) Potassium level of 3.0 mEq/dL D) Glucose level of 200 mg/dL - ☑☑A Linezolid can cause reversible myelosuppression, manifesting as anemia, leukopenia, or even pancytopenia. The potassium and blood glucose levels are not affected by linezolid. Which cardiovascular finding does the nurse identify as a possible adverse effect of erythromycin (Ery-Tab) therapy? A) Heart rate of 52 beats per minute B) Prolonged QT interval C) Jugular vein distention D) Grade III diastolic murmur - ☑☑B When present in high levels, erythromycin can prolong the QT interval, causing a potentially fatal ventricular dysrhythmia. It should be avoided by patients taking class IA or class III antidysrhythmic medications or others that inhibit metabolism. What does the nurse identify as an adverse effect of clindamycin (Cleocin) therapy? A) Cyanosis and gray discoloration of the skin B) Frequent loose, watery stools with mucus and blood C) Reduction in all blood cells produced in the bone marrow D) Elevated bilirubin, with dark urine and jaundice - ☑☑B Clostridium difficile-associated diarrhea (CDAD) is the most severe toxicity associated with clindamycin and is characterized by profuse, watery stools. The cause is superinfection of the bowel with Clostridium difficile, an anaerobic gram-positive bacillus. Gray syndrome, which usually occurs in infants and those with aplastic anemia, is an adverse effect of chloramphenicol (Chloromycetin). Hepatotoxicity is associated most closely with telithromycin (Ketek). The nurse identifies tigecycline (Tygacil) as a derivative of what? A) Penicillins B) Cephalosporins C) Tetracyclines D) Macrolides - ☑☑C Tigecycline is the first representative of a new class of antibiotics, the glycyclines. It is a tetracycline derivative made to overcome drug resistance and is active against many drug-resistant strains. It has adverse effects similar to those of the tetracyclines. The nurse identifies which drug as a short-acting tetracycline? A) Sumycin B) Declomycin C) Vibramycin D) Minocin - ☑☑A Sumycin is a short-acting tetracycline. Declomycin is an intermediate-acting tetracycline, and Vibramycin and Minocin are long-acting tetracyclines. Which statements about CDAD associated with clindamycin therapy does the nurse identify as true? (Select all that apply.) A) Leukopenia commonly occurs. B) It is a potentially fatal condition. C) Patients usually experience abdominal pain. D) Anticholinergics are effective in treating the diarrhea. E) Clindamycin therapy should be discontinued and vancomycin started. - ☑☑B,C,E CDAD is a potentially fatal condition in which patients experience abdominal pain. If CDAD develops, clindamycin therapy should be stopped and vancomycin or metronidazole therapy started. Leukocytosis, not leukopenia, develops. Anticholinergics can make the diarrhea worse and therefore should be avoided. The nurse should include which instructions when teaching a patient about tigecycline therapy? (Select all that apply.) A) "Use sunscreen when you are outside." B) "If you have diarrhea more than five times a day, notify your healthcare provider." C) "Avoid using this drug if you are pregnant." D) "Stop taking the drug if you experience nausea." E) "Stop taking the drug if you experience vomiting." - ☑☑A,B,C Nausea and vomiting may occur. The patient should not stop taking the medication; rather, the healthcare provider should be notified so that an alternative plan can be discussed. The other three instructions should be included in the patient teaching. A nurse observes a red streak and palpates the vein as hard and cordlike at the intravenous (IV) site of a patient receiving cefepime (Maxipime). Which assessment should the nurse make about the IV site? A) An allergic reaction has developed to the drug solution. B) The drug has infiltrated the extravascular tissues. C) Phlebitis of the vein used for the antibiotic has developed. D) Local infection from bacterial contamination has occurred. - ☑☑C IV cephalosporins may cause thrombophlebitis. To minimize this, the injection site should be rotated and a dilute solution should be administered slowly. An allergic response would be shown as itching, redness, and swelling. Infiltration would show as a pale, cool, and puffy IV site. Infection would show as pus, tenderness, and redness. A patient develops flushing, rash, and pruritus during an IV infusion of vancomycin (Vancocin). Which action should a nurse take? A) Reduce the infusion rate. B) Administer diphenhydramine (Benadryl). C) Change the IV tubing. D) Check the patency of the IV. - ☑☑A When vancomycin is infused too rapidly, histamine release may cause the patient to develop hypotension accompanied by flushing and warmth of the neck and face; this phenomenon is called red man syndrome. Diphenhydramine is not necessary if the infusion is administered slowly over at least 60 minutes. Changing the IV tubing would not help the symptoms. The patency of the IV needs to be checked before the administration is started. A patient who is receiving vancomycin (Vancocin) IV for a methicillin-resistant Staphylococcus aureus (MRSA) infection asks a nurse, "Why can't I take this medicine in a pill?" Which response should the nurse make? A) "The prescription could be changed, because vancomycin comes in two forms." B) "You're allergic to penicillin, and this is the only way this medication can be given." C) "It will cause too much loss of appetite and nausea if given in the oral form." D) "It is more effective by IV, because the pill form will stay in the digestive tract." - ☑☑D Because of its chemical size and weight, vancomycin is absorbed poorly in the gastrointestinal (GI) tract and is given parenterally for most infections. It is used for serious infections caused by organisms such as MRSA and in patients with susceptible organisms allergic to penicillins. Oral administration is used only for infections of the intestine. It is not associated with loss of appetite or nausea. A patient who is receiving cefotetan (Cefotan) has all of these medications ordered. The nurse monitors the patient for an adverse effect related to an interaction with which medication? A) Regular insulin B) Ampicillin (Polycillin) C) Naproxen (Naprosyn) D) Bisacodyl (Dulcolax) - ☑☑C Three cephalosporins—cefmetazole (Zefazone), cefoperazone (Cefobid), and cefotetan (Cefotan)—cause bleeding tendencies. Caution should be used during concurrent use of anticoagulants and other nonsteroidal medications. Regular insulin, ampicillin, and bisacodyl are unrelated to adverse effects with cefotetan. [Show More]
Last updated: 1 year ago
Preview 1 out of 75 pages
Instant download
Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Aug 20, 2022
Number of pages
75
Written in
Additional information
This document has been written for:
Uploaded
Aug 20, 2022
Downloads
0
Views
119



 (1).png)
.png)
.png)
.png)
.png)

