*NURSING > QUESTIONS & ANSWERS > PANCE Practice Exam 2 Questions and answers, 2022. Rated A+. Question bank (All)
PANCE Practice Exam 2 Questions and answers, 2022. Rated A+. Question bank
Document Content and Description Below
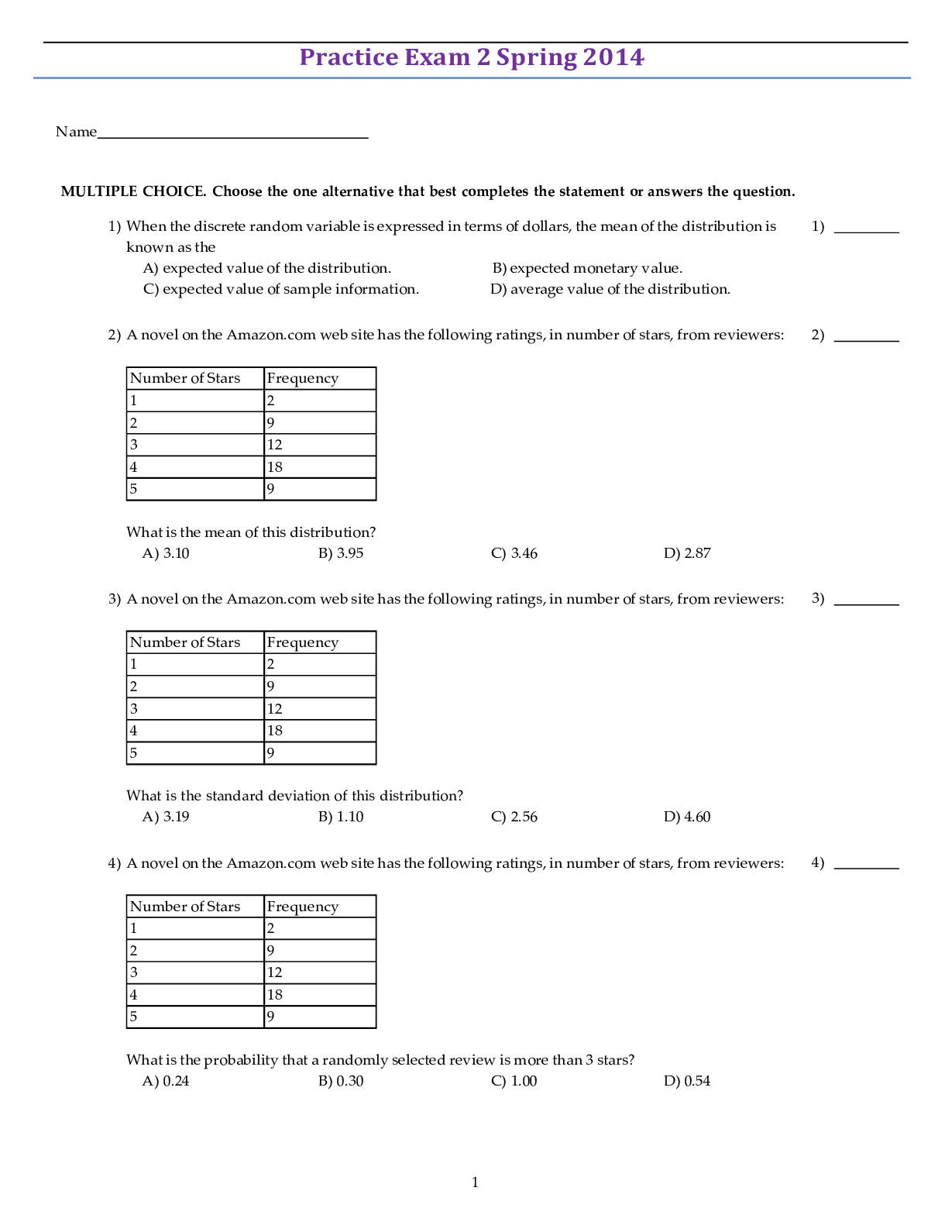
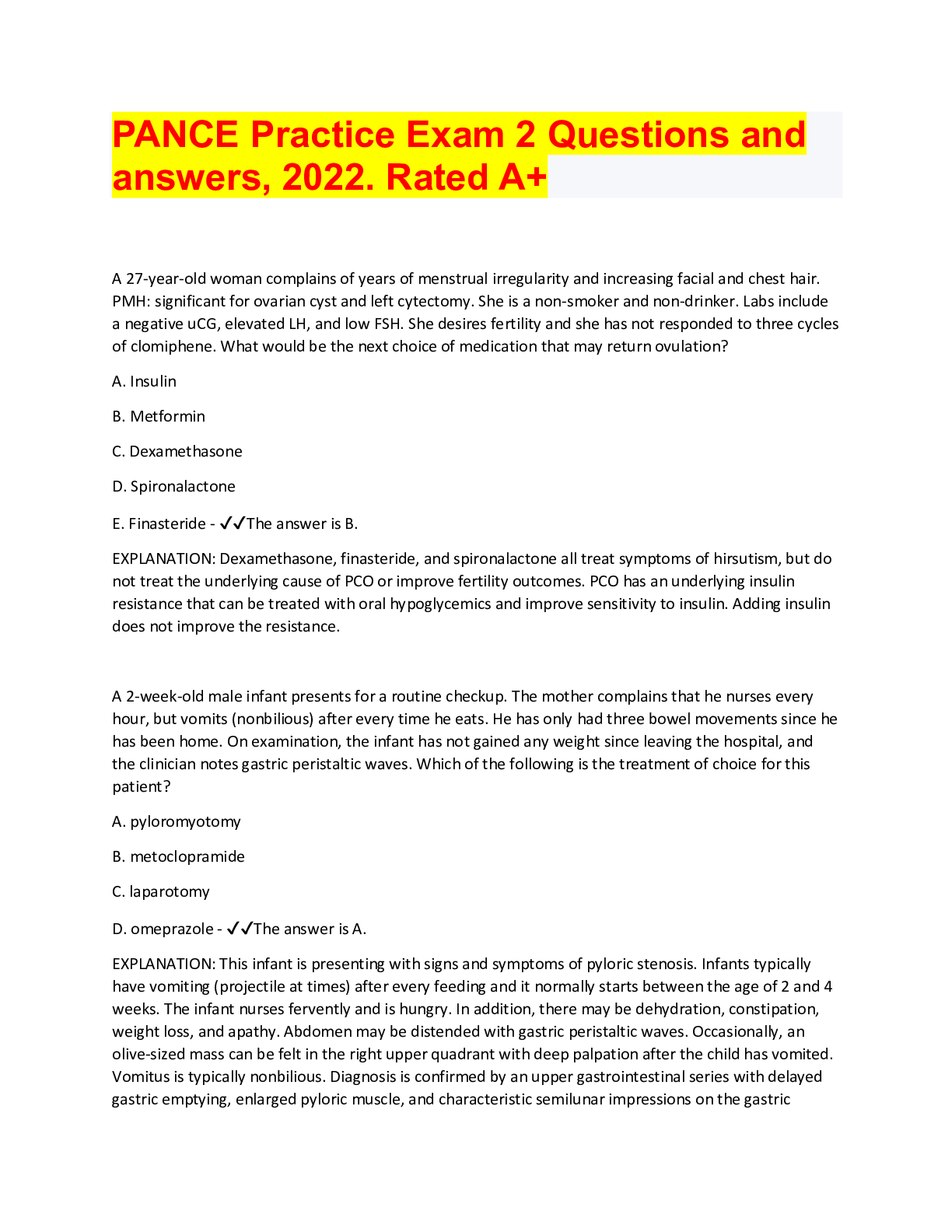
PANCE Practice Exam 2 Questions and answers, 2022. Rated A+ A 27-year-old woman complains of years of menstrual irregularity and increasing facial and chest hair. PMH: significant for ovarian cys... t and left cytectomy. She is a non-smoker and non-drinker. Labs include a negative uCG, elevated LH, and low FSH. She desires fertility and she has not responded to three cycles of clomiphene. What would be the next choice of medication that may return ovulation? A. Insulin B. Metformin C. Dexamethasone D. Spironalactone E. Finasteride - ✔✔The answer is B. EXPLANATION: Dexamethasone, finasteride, and spironalactone all treat symptoms of hirsutism, but do not treat the underlying cause of PCO or improve fertility outcomes. PCO has an underlying insulin resistance that can be treated with oral hypoglycemics and improve sensitivity to insulin. Adding insulin does not improve the resistance. A 2-week-old male infant presents for a routine checkup. The mother complains that he nurses every hour, but vomits (nonbilious) after every time he eats. He has only had three bowel movements since he has been home. On examination, the infant has not gained any weight since leaving the hospital, and the clinician notes gastric peristaltic waves. Which of the following is the treatment of choice for this patient? A. pyloromyotomy B. metoclopramide C. laparotomy D. omeprazole - ✔✔The answer is A. EXPLANATION: This infant is presenting with signs and symptoms of pyloric stenosis. Infants typically have vomiting (projectile at times) after every feeding and it normally starts between the age of 2 and 4 weeks. The infant nurses fervently and is hungry. In addition, there may be dehydration, constipation, weight loss, and apathy. Abdomen may be distended with gastric peristaltic waves. Occasionally, an olive-sized mass can be felt in the right upper quadrant with deep palpation after the child has vomited. Vomitus is typically nonbilious. Diagnosis is confirmed by an upper gastrointestinal series with delayed gastric emptying, enlarged pyloric muscle, and characteristic semilunar impressions on the gastric antrum. In addition, an ultrasound is needed to verify the hypertrophic muscle. The treatment of choice for these patients is pyloromyotomy, which can be done laparoscopically. These patients make full recoveries and have an excellent prognosis. Upon performing a newborn examination, the clinician notes a widened pulse pressure, paradoxical splitting of S2, and a "machine"-like murmur heard best at the second intercostal space, left sternal border, and inferior to the clavicle. Which of the following is the most likely diagnosis? A. tetralogy of Fallot B. ventricular septal defect C. atrial septal defect D. patent ductus arteriosus - ✔✔The answer is D. EXPLANATION: Patent ductus arteriosus (PDA) is an isolated abnormality that occurs in infants. The ductus arteriosus is a normal fetal vessel that joins the aorta and the pulmonary artery and spontaneously closes after 3 to 5 days. Lack of closure results in the audible murmur that is "machine-like" and maximal at the second intercostal space (ICS), at the left sternal border (LSB), and inferior to the clavicle. It is typically a pansystolic murmur with bounding pulses and a widened pulse pressure. There is also a paradoxical splitting of S1 and S2. Echocardiography confirms the PDA, the direction and degree of shunting, and the presence of lesions for which the PDA is needed to keep. If there are no other cardiac malformations requiring the PDA, then if the PDA is large, surgery should be completed before 1 year of age. Symptomatic PDAs that are relatively small may be closed with indomethacin in preterm infants. an ejection type, systolic murmur heard best at the LSB, second ICS with a wide, fixed S2 and normal pulses. - ✔✔atrial septal defect (ASD) a harsh, pansystolic murmur heard best at the third and fourth ICS. With increasing size, heaves, thrills, and lifts are present along with radiation throughout the chest. - ✔✔Ventricular septal defect (VSD) a rough ejection, systolic murmur heard best at the LSB and the third ICS with radiation to the back. - ✔✔Tetralogy of Fallot A 42-year-old woman, with a history of struvite renal calculus, calls the office with a complaint of a urinary tract infection. As part of the interview, she reports intermittent, mild right flank pain for 4 days. Her urine dipstick is positive for microscopic hematuria, and the urine pH is 7.5. The KUB film is positive with two visible stones in the right kidney. Which of the following organisms is most likely to be cultured from the urine specimen? A. Escherichia coli B. Klebsiella C. Proteus D. Chlamydia trachomatis - ✔✔The answer is C. EXPLANATION: This patient has struvite stones. They are frequently associated with recurrent urinary tract infections, visible stones, and high urine pH. These stones are formed by urease-producing organisms including Proteus and Pseudomonas while being caused less commonly by Klebsiella. Struvite stones are not typically caused by E. coli and C. trachomatis. A 33-year-old woman treated with trifluoperazine for the past 3 months is seen in the emergency department because of recent-onset fever, stiffness and tremor, as reported by her accompanying sister. The patient also appears to be mildly confused when asked about location, day, and time. Her temperature is 104.5°F, and her serum creatine kinase (CK) level is markedly elevated. Which of the following has most likely occurred? A. a delayed allergic reaction has occurred with trifluoperazine B. tardive dyskinesia has begun to develop in the patient C. the patient has developed neuroleptic malignant syndrome D. the patient has developed serotonin syndrome E. the patient has overdosed on trifluoperazine - ✔✔The answer is C. EXPLANATION: Neuroleptic malignant syndrome is an uncommon but serious complication with therapeutic doses of antipsychotic drug therapy, particularly the first-generation (typical) class. Cardinal signs and symptoms include a body temperature above 100.4°F, altered state of consciousness, autonomic dysfunction, and rigidity. A 48-year-old man presents to the clinic for a routine employment physical. The patient is asymptomatic. A pre-employment CBC reveals hemoglobin of 13.2g/dl, hematocrit of 39.5%, and MCV of 60.6 fL. Subsequent iron studies, hemoglobin electrophoresis, and sickle cell screening are "normal." After the labs are reviewed, the patient states "they are always normal." Which of the following is the most appropriate management for this patient? A. Bone marrow aspirate B. Ferrous sulfate daily C. Folic acid supplements D. Reassurance E. Refer to an oncologist - ✔✔The answer is D. EXPLANATION: The patient has a mild anemia with pronounced microcytosis consistent with alpha thalassemia minor and requires reassurance. Alpha thalassemia minor hemoglobin electrophoresis reveals normal results. Patients with alpha thalassemia are often inappropriately advised to take iron supplements (B) and don't require iron, folic acid (C) or vitamin B12 supplements unless a coexisting deficiency is confirmed. Referral to an oncologist (E) and a bone marrow aspirate (A) aren't necessary for this patient. white blood cell count (WBC) reveals 14,800 mcL with more than 10% atypical lymphocytes. On physical examination you find significant yellowish-grey pharyngeal exudate, cervical lymphadenopathy as well as an enlarged spleen. Her rapid strep is negative. What should be your treatment of this patient? A. Begin treatment with cephalexin. B. Send out a back-up throat culture and begin treatment with cephalexin pending those results .C. Send out a back-up throat culture and hold treatment pending those results. D. Draw a Monospot test and treat the patient supportively pending the results, insuring that they avoid contact sports until a definitive diagnosis has been made. E. Draw an Epstein-Barr virus (EBV) IgG level and treat the patient supportively if positive. - ✔✔The answer is D. EXPLANATION: With this patient's presentation and a negative rapid strep test, other etiologies beyond group A beta-hemolytic strep should be seriously considered. In light of her symptoms including fatigue, her WBC, and that her significant other is having similar symptoms, infectious mononucleosis is highest on the differential diagnosis. A Monospot test would rule this possibility in or out. She should refrain from contact sports until her infection and any associated splenomegaly has resolved. barking" cough and a low-grade fever. She has some runny nose and her voice is somewhat raspy and hoarse. mild inspiratory stridor. What is the most likely etiology of this child's illness? A. Adenovirus B. Coxsackievirus C. Cytomegalovirus D. Parainfluenza virus E. Respiratory syncytial virus - ✔✔The answer is D. EXPLANATION: This child has the classic presentation for croup. Sixty-five percent of croup is caused by a parinfluenza virus infection. Adenoviruses tend to cause severe pharyngitis/tonsillitis with tender, enlarged cervical nodes (A), while Coxsackievirus is commonly associated with hand-foot-and-mouth disease. (B) Cytomegalovirus causes an infectious-mononucleosis-like picture. (C) RSV is more typically associated with bronchiolitis. (E) Glucose challenge testing to rule out gestational diabetes should be done when? A. Between 12 and 16 weeks gestation B. Between 16 and 20 weeks gestation C. Between 20 and 24 weeks gestation D. Between 24 and 28 weeks gestation E. Between 28 and 32 weeks gestation - ✔✔The answer is D. EXPLANATION: Routine surveillance for gestational diabetes of a pregnant women is between 24 and 28 weeks; it is not modified due to obesity or other risk factors for diabetes. Gestational diabetes is a hormone-mediated intolerance. Surveillance is modified in the presence of pre-existing diabetes A 45-year-old patient came in to see his health care provider today, to discuss the results of his last annual assessment. He was told that he had developed type 2 diabetes mellitus. One of the recommendations from the physician assistant included a visit to an ophthalmologist. The physician assistant was concerned after seeing new capillaries, macular edema, and fibrous tissue within the retina during his funduscopic exam. What type of ocular complication does this patient most likely have at this time? A. Background retinopathy B. Closed angle glaucoma C. Macular degeneration D. Diabetic cataracts E. Proliferative retinopathy - ✔✔The answer is E. The correct choice is E, proliferative retinopathy. The distinguishing factor in the patient's presentation, which signals this disorder, is the development of newly formed vessels. Proliferative retinopathy is the leading cause of blindness in the United States. Up to 20% of patients with type 2 diabetes have retinopathy at the time of diagnosis. Choice A, background retinopathy, or simple retinopathy includes retinal microaneurysms, hemorrhages, exudates, and edema, without new vessel formation. Choice B, closed angle glaucoma, is relatively uncommon in patients with diabetes, except after cataract extraction. Choice C, macular degeneration, is not associated with diabetes mellitus specifically. Choice D, diabetic cataracts, tends to occur in patients with diabetes earlier than the general population, and may correlate with the severity of the disease. A 32-year-old male presents to your office with the complaint of low back pain for 7 months. The patient states he was initially injured on the job while trying to lift a 50-pound barrel off a truck. He denies any paresthesias or bowel/bladder problems associated with the low back pain. The patient states that he had been given NSAIDs and a muscle relaxer, followed by physical therapy treatments. X-rays that were taken 5 months ago were reported as normal. He was placed on light duty at that time. The patient has seen many practitioners who have "not helped him." Another person who works with this patient was at the clinic and stated the patient has had problems with one of his other coworkers. You consider trying the patient on an antidepressant first and then possibly sending him to a pain clinic if there is no success. What is the most likely diagnosis? A. conversion disorder B. hypochondriasis C. drug addiction D. somatoform pain disorder E. schizophreniform - ✔✔The answer is D. EXPLANATION: Somatoform pain disorder is a focus on pain for greater than 6 months. The subjective findings outweigh the objective findings. Pain in the neck, pelvic, or low back areas are frequent sites, as well as headaches. The disorder may be precipitated by an injury. The patient will have a history of seeing multiple providers and possibly many medical and surgical treatments. The patient is unresponsive to treatment. Stressors can aggravate or precipitate the pain. There may be an expectation of secondary gains. Age of onset is around 30s and 40s. Treatment consists of placing the patient on an antidepressant and sending the patient to a pain clinic. A patient presents with a cerumen impaction. Which of the following is true when performing the Rinne- Weber test? A. Weber lateralizes to the affected ear B. Weber is equal in both ears C. Weber lateralizes to the unaffected ear D. Air conduction > Bone conduction in the affected ear E. Air conduction = Bone conduction in the affected ear - ✔✔The answer is A. EXPLANATION: For conductive hearing loss, the Weber will lateralize to the affected ear and bone conduction will be greater than air conduction. Conductive hear loss prevents sound from entering the inner ear due to obstruction in the external auditor canal and middle ear. Examples would be cerumen impaction and otitis media. Sensory neural hearing loss affects the inner ear and cranial nerve VIII. Weber will lateralize to the unaffected ear (normal ear) and Rinne will reveal Air conduction > Bone conduction. Which of the following findings is consistent with a lower motor neuron deficit? A. aphasia B. dysdiadochokinesia C. sensory loss D. weakness E. hyperreflexia - ✔✔The answer is D. EXPLANATION: Weakness is one potential finding of a lower motor neuron process. Aphasia results from injury to the speech pathways within the brain. Sensory loss arises from many causes, but it is not a motor issue. Dysdiadochokinesia is consistent with cerebellar pathology. Hyperreflexia is typically a signal of upper motor neuron disease. A 54 year-old female returns for pathology results after being diagnosed with ovarian cancer. Which of the following is the most likely cause of ovarian epithelial malignancy? A. Serous tumors B. Endometrioid tumors C. Mucinous tumors D. Clear cell tumors E. Transitional cell tumors - ✔✔The answer is A. EXPLANATION: The most common of the ovarian epithelial malignancies are serous tumors (50%); tumors of mucinous (25%) (C), endometrioid (15%) (B), clear cell (5%) (D), and transitional cell (E) histology or Brenner tumors (1%) represent smaller proportions of epithelial ovarian tumors. Over half of all epithelial ovarian cancers have serous histology. The second most common histologic type of epithelial ovarian cancers are endometrioid adenocarcinomas. A 25-year-old woman is seen today in your office for vague abdominal pain, nausea, anorexia, weight loss, anxiety, and dizziness. Her past medical history is significant for type 1 diabetes mellitus, and her family history is significant for hypothyroidism in several family members. A review of systems reveal a history of amenorrhea. Upon exam, you note hyperpigmentation of her skin and areas of vitiligo, but no mucocutaneous candidiasis. You are not surprised to find that her serum ACTH level is elevated and her serum cotisol is low. Which of the following syndromes should be investigated in this patient? A. Type 1 polyglandular autoimmune syndrome type 1 B. Type 2 polyglandular autoimmune syndrome type 2 C. Multiple endocrine neoplasia type 2A D. Multiple endocrine neoplasia type 1 E. Metabolic syndrome - ✔✔The answer is B. The correct choice is B, type 2 polyglandular autoimmune syndrome. This patient is presenting with signs and symptoms of adrenal insufficiency including abdominal pain, nausea, anorexia, vomiting, weight loss, anxiety, and hyperpigmentation. Type 2 polyglandular autoimmune syndrome presents most commonly in young women between 20 and 40 years old, with evidence of adrenal insufficiency, type 1 diabetes mellitus, and autoimmune thyroid disease. Because of the strong family history of thyroid disease, it would be prudent to conduct an investigation into this disorder, starting with a serum TSH level. Primary ovarian failure and vitiligo may be symptoms of the autoimmune polyglandular syndrome as well. Choice A, type 1 autoimmune polyglandular syndrome, presents more commonly in childhood with adrenal insufficiency, hypoparathyroidism, and mucocutaneous candidiasis. Choices C and D are inherited disorders, characterized by the development of several different types of endocrine organ neoplasias. Choice E, metabolic syndrome, includes a constellation of several metabolic disorders that increase the risk of cardiovascular disease and diabetes mellitus in the patient. A 24-year-old male with thalassemia major who has received adequate transfusions, chelation therapy, and regular health checkups is in to establish care. He is 5'4" with a BMI of 17. He eats a balanced healthy diet and gets regular exercise. You know that there are complications of this disease. What is the best next step for this patient? A. Increase threshold for blood transfusions B. Maintain sustained reduction of body iron C. Obtain a Dexa scan for osteoporosis D. Obtain an ECHO to evaluate for cardiac siderosis E. Obtain regular testosterone levels and treat - ✔✔The answer is B. Maintaining sustained reductions in body iron has demonstrated increased overall survival rates through reductions in cardiac disease specifically due to siderosis. While these patients are at increased risk for osteoporosis and cardiac siderosis, the next best step in this patient is to maintain reduced iron levels. There is no place for increased blood transfusion or obtaining regular testosterone levels. which is the test of choice for confirming a diagnosis of pertussis? - ✔✔A special medium culture plate (such as a Bordet-Gengou agar) is required for the nasopharyngeal swab for the diagnosis of pertussis. A 76-year-old male has a history of hypertension, diabetes mellitus, and prior history of stroke six years ago without neurological deficits. He presents with a new finding of atrial fibrillation. He is independent, drives his own car, and tends to his daily activities without assistance. He is currently having no symptoms, and his heart rate is 90, with a blood pressure of 146/76. Given this clinical scenario, what is the best pharmacologic anticoagulation treatment for this patient? A. No anticoagulation B. Aspirin C. Warfarin D. Aspirin and warfarin E. Clopidogrel - ✔✔The answer is D. EXPLANATION: This patient is a high risk for stroke related to atrial fibrillation given his CHADS2 score of 5 (HTN, age, diabetes, stroke). His activity level and daily life appear to be stable, and he is an appropriate candidate for aspirin and warfarin combination therapy (D) to prevent stroke. Aspirin or warfarin alone (B and C) would not adequately anticoagulate (A) this patient, and the use of single drug therapy of clopidogrel (E) is not indicated for atrial fibrillation. A 43-year-old male presents to the Emergency Department complaining of right eye pain after treating his yard with fertilizer and lime. He attempted to flush his eye at home without relief of pain. Which of the following is the most appropriate initial step in managing this patient's symptoms? A. Double evert his eyelids to look for remaining foreign bodies B. Fluorescein stain his eye C. Instill proparacaine 0.5% ophthalmic solution D. Irrigate his eye until the pH is between 6.8 and 7.4 E. Refer to ophthalomogist - ✔✔The answer is C. EXPLANATION: The patient requires all of the above steps and should be given pain relief (C) prior to thoroughly flushing the eye (D), removing foreign bodies (A), assessing for corneal injuries (B), and referring to ophthalmology (E). Which of the following is the most likely explanation for the increase in the patient's INR? A. decreased warfarin absorption in the small intestine B. decreased warfarin metabolism by the liver C. increased plasma protein binding of warfarin D. increased warfarin absorption in the small intestine E. increased warfarin metabolism by the liver - ✔✔The answer is B. EXPLANATION: There are several clinically important warfarin drug interactions, with most of them causing an increase in the drug's anticoagulant effect (ie, increasing the INR). Warfarin metabolism occurs via hepatic cytochrome P450 enzymes that can be inhibited by a large number of drugs, including the fluoroquinolones. When this inhibition occurs, plasma levels of warfarin rise, thereby enhancing the anticoagulant effect. Of the following, which of the following is the most appropriate test to order at this stage to confirm the suspected diagnosis of syphilis? A. Darkfield microscopic examination B. IgG enzyme immunoassay (EIA) C. Polymerase chain reaction (PCR) D. Rapid Plasma Reagin (RPR) test E. Venereal Disease Research Laboratory (VDRL) test - ✔✔The answer is B. EXPLANATION: The EIA or CIA (chemoluminescence assay) is faster and less expensive than traditional syphilis testing, so current algorithms suggest beginning with one of these tests. The darkfield examination of fresh exudate from a lesion is usually only available in specialized laboratories as it requires expertise in obtaining and examining specimens. (A) PCR testing is increasingly used, but not widely commercially available in the U.S. (C) The RPR and VDRL tests (D, E) do not become positive until 1-3 weeks following the appearance of a chancre. A 29-year-old woman comes to the emergency department with abrupt onset of left lower quadrant pain approximately 1.5 hours ago after she and her roommate moved multiple heavy pieces of furniture into their new apartment. The pain is now excruciating and she rates it "100 out of 10." She vomits on admission to the department. She is not currently sexually active and has no other significant past medical history. On exam she is found to have fullness and extreme tenderness in the left adnexa. Of the following, what is the most likely diagnosis? A. Diverticulitis B. Pelvic inflammatory disease C. Renal calculus D. Ruptured ovarian cyst E. Torsion of the left ovary - ✔✔The answer is E. EXPLANATION: Ovarian torsion is often extremely painful and is often accompanied by vomiting, with sudden onset and may be associated with episodes of heavy exertion. Diverticulitis (A) typically causes LLQ pain, but would be unusual in a 26-year-old woman because it occurs more often in older adults. The symptoms of PID (B) do not begin abruptly and vomiting is not typical. The pain of renal calculi (C) is colicky and calculi are not associated with a palpable adnexal mass. The pain of a ruptured ovarian cyst (D) would be sudden in onset; however, rupture would not be associated with a palpable mass. At what stage of hospitalization can active tuberculosis patients be placed in a non-negative pressure room? - ✔✔When there is a clear sputum gram stain LP was positive for gram-negative bacilli, decreased glucose, increased protein, and increased neutrophils. Which of the following is the most likely etiologic agent? - ✔✔Salmonella ototoxic medications - ✔✔furosemide, gentamycin, aspirin, and cisplatin. acute vertigo treatment - ✔✔is more effective using a combination of vestibular suppressants (benzodiazepines), anti-emetics (prochlorperazine), and anticholinergics (diphenhydramine or scopolamine). A 57-year-old male is being monitored for Binet Stage A CLL. He is emergently seen in the clinic with rapid lymph node enlargement, fever, weight loss, and hepatosplenomegaly. On laboratory examination, he is found to have an elevated serum lactate dehydrogenase and a monoclonal gammopathy on serum protein electrophoresis. A retroperitoneal ultrasound reveals bulky adenopathy. What is the most likely diagnosis? A. Acute lymphadenitis secondary to HSV B. Epstein-Barr viral infection C. Hodgkin lymphoma D. Rapidly advancing CLL E. Richter transformation - ✔✔The answer is E. EXPLANATION: All findings are classic for Richter transformation of CLL to an aggressive large B-cell, high-grade lymphoma. While HSV cannot be totally ruled out without a node biopsy, given the patient history and findings the most likely diagnosis is Richter transformation. Rapidly advancing CLL does not usually develop retroperitoneal adenopathy. Occasionally, Richter syndrome with Hodgkin lymphoma features is seen, but accounts for less than one-fifth of all cases of Richter transformation. EBV may play a role in this later syndrome. pharmacologic agents have phototoxicity as a side effect - ✔✔Doxycycline, hydrochlorothiazide, and naproxen A 29-year-old female who is only taking oral contraceptives presents to the emergency department with a 1-day history of worsening shortness of breath. On examination, the patient is afebrile, her pulse rate is 105, respiratory rate is 24, and blood pressure is 122/78. She has wheezing to all lung fields and appears to be in mild to moderate distress. There is no swelling or edema to the lower extremities. Based on these findings, what is the best test to order to determine the diagnosis in this patient? A. CT chest B. Chest x-ray C. Ventilation to perfusion scan D. Pulmonary arteriography E. MRI chest - ✔✔The answer is D. EXPLANATION: This patient presents with a history and physical exam that is consistent with an acute pulmonary embolus (PE). The prognosis for this type of illness can be serious, and in some cases death can result. The test that is still the gold standard for determination of a PE is the pulmonary arteriogram. CT of the chest with contrast tends to be the more utilized testing modality, but the arteriogram remains the test of choice. Which of the following factors would be a contraindication to prescribing him bupropion? A. Allergy to sulfa B. Depression C. Decreased libido D. Seizure disorder - ✔✔The answer is D. EXPLANATION: Bupropion is contraindicated in situations where patients are at risk of seizures (D). Bupropion is indicated for the treatment of depression (B) and doesn't typically cause libido concerns (C). Bupropion is commonly prescribed with nicotine replacement therapy (E) during tobacco cessation efforts. 42-year-old female complains of weight gain (especially in her abdomen) over the past 8 months. She also has noted that her skin bruises easily. Her husband has noted she seems to be very moody lately and she is worried about their relationship. Furthermore, her hair seems to be getting thinner and she is now getting acne like she had in her teenage years. She wonders if this is due to menopause since her periods have stopped suddenly about a year ago. On physical examination her BP = 170/50, P = 82, T = 98.2°F. You note the following findings on examination (see picture) purple straiae). What diagnostic test is indicated initially to confirm your suspected diagnosis? A. cosyntropin stimulation test B. MRI pituitary C. dexamethasone suppression test D. 24-hour urine for protein E. serum protein electrophoresis - ✔✔The answer is C. EXPLANATION: The correct answer is (C). The patient's symptoms are consistent with a diagnosis of Cushing's syndrome (or disease). Her physical examination findings of hypertension and abdominal obesity with the classic purple striae also support the diagnosis. The initial diagnostic test of choice would be the dexamethasone suppression test. If the test is positive, further confirmatory testing is done which would also help to identify the cause. An MRI of the pituitary is appropriate if further testing suggests the possibility of a pituitary adenoma as the cause of the Cushing's syndrome, but is not used as an initial diagnostic test for Cushing's disease. A cosyntropin stimulation test, choice (A), is indicated for the diagnosis of Addison's disease. A 12-year-old boy presents to the clinic for follow-up regarding his recently diagnosed partial seizures. He reports no seizures or side effects since starting carbamazepine (Tegretol) 1 month ago. What study should be ordered to monitor this patient's treatment? A. blood glucose B. complete blood cell count C. electroencephalogram D. vitamin B12E. urinalysis - ✔✔The answer is B. EXPLANATION: Carbamazepine is an anti-epileptic drug that potentially causes blood dyscrasias and requires CBC monitoring. Disorders of carbohydrate metabolism, vitamin B12 deficiency, or renal toxicity are not commonly reported. EEG is used to help establish a diagnosis of a seizure disorder. A combination of which of the following medications may increase the risk of muscle and liver disease more than either drug used alone? A. Ezetimibe and HMG-CoA reductase inhibitor B. Low dose niacin and HMG-CoA reductase inhibitor C. Colestipol and gemfibrozil D. Niacin and cholestyramine E. Gemfibrozil and HMG-CoA reductase inhibitor - ✔✔The answer is E. The correct choice is E, gemfibrozil and HMG-CoA reductase inhibitor. In combination, these can potentiate the risk of developing hepatic disease or myopathy. Choice A, Ezetimibe and HMG-CoA reductase inhibitor, is a synergistic treatment plan for patients with primary hypercholesterolemia. Choice B, low dose niacin and HMG-CoA reductase inhibitor, is a practical and effective treatment plan for patients with familial combined hyperproteinemia. Choice C, colestipol and gemfibrozil, is sometimes useful in patients with familial combined hyperlipidemia who are intolerant of niacin or HMG-CoA reductase inhibitors. Unfortunately, this combination may increase the risk of cholelithiasis. Choice D, niacin and cholestyramine, is useful in disorders with elevated VLDL and LDL, and useful in treating heterozygous familial hypercholesterolemia. A 48-year-old female presents with a gradual progression of fatigue, pallor, and dyspnea on exertion over the last few months. Initial CBC results show a hemoglobin of 10.2 mg/dL, hematocrit of 31%, an MCV of 74 fL, and a reticulocyte count of 0.1%. After treatment for her anemia begins, which of the following diagnostic studies can be ordered first (earliest) to demonstrate a response to therapy? A. Bone marrow aspirate B. Ferritin C. Hemoglobin/hematocrit D. Iron binding capacity E. Reticulocyte count - ✔✔The answer is E. EXPLANATION: The patient most likely has an underlying iron deficiency anemia (IDA) which requires confirmation and then evaluation for sources of chronic blood loss. IDA is treated with iron replacement (e.g., ferrous sulfate) and response to therapy can be assessed in 7-10 days via a reticulocyte count. The elevation of the reticulocyte count (after initial reticulocyte count was relatively low) at this time demonstrates the return of normal hemoglobin production (E). Bone marrow aspirate (A) would be an inappropriately invasive test to perform in this scenario. The patient's hemoglobin, hematocrit (C), MCV, and iron studies (B and D) will take a couple to a few months to return to normal "apple core" lesion - ✔✔Colorectal carcinoma string sign - ✔✔Crohn's disease is typically associated with the string sign, which is an area of stricture or stenosis that shows up as a narrow line of contrast, giving the appearance of a string associated with the stricture. A 9-year-old male child presents with a painful rash of his upper extremity. His mom states it started 4 days ago and seems like it is spreading. Physical examination demonstrates a vesicular rash across the right upper arm and chest but does not cross the midline. Which of the following prescriptions would be most appropriate for this patient at today's visit? A. hydration B. nonsteroidal anti-inflammatory drugs (NSAIDs) C. Varicella-Zoster immunoglobulin (VZIG) D. oral acyclovir - ✔✔The answer is D. EXPLANATION: As this patient is presenting with signs and symptoms of herpes zoster within the appropriate time frame for antiviral treatment, the treatment for this patient would be oral acyclovir. NSAIDs may help with the pain associated from zoster but will not hasten the length of the course of the virus as acyclovir will. Varicella-Zoster immunoglobulin (VZIG) is indicated for prophylaxis in exposed individuals who are immunocompromised. Which of the following is a result of untreated or partially treated otitis media, which presents with fever, ear pain, otorrhea, tenderness behind the ear, fluid collection, and destruction of air cells seen on head CT? A. Suppurative otitis media B. Peritonsillar abcess C. Mastoiditis D. Meningitis E. Ethmoid sinusitis - ✔✔The answer is C. EXPLANATION: Untreated or partially otitis media can result in mastoiditis. Tenderness, redness, and fluctuance over the mastoid bone is characteristic. Peritonsillar abcess symptoms include severe sore throat, drooling, dysphonia, and outpouching of the tonsillar pillar on the affected side and trismus. Ethmoid sinusitis presents with nasal congestion, discharge, and headache. Suppurative otits media is contained in the middle ear, without spreading to adjacent structures. A 72-year-old male presents to you for a routine physical exam. He complains of increasing abdominal distention, weight loss, and night sweats over the past 2 months. He admits to having a blood transfusion as a young adult. His labs include +anti-HCV and HCV RNA. Which of the following is the most likely explanation for his history and laboratory findings? A. acute hepatitis B B. alcoholic hepatitis C. chronic hepatitis A D. Gilbert's syndrome E. hepatocellular carcinoma - ✔✔The answer is E. EXPLANATION: The correct answer is (E). The patient's symptoms are consistent with a possible malignancy. Labs indicate chronic hepatitis C, likely longstanding with liver cirrhosis, which is associated with an increased risk of hepatocellular carcinoma. Chronic hepatitis B is also associated with an increased risk of hepatocellular carcinoma, but not acute hepatitis B, choice (A). Choices (B), (C), and (D) are not consistent with the laboratory results and do not increase the patient's risk of hepatocellular carcinoma. A 42-year-old woman comes in with a "lump in her neck." When she was a teenager, she underwent radiation treatment for "some kind of tumor" in her neck. Ultrasound reveals a 1.5 cm lesion in the left lobe of the thyroid; biopsy confirms papillary carcinoma. Thorough evaluation reveals no evidence of metastasis. Which of the following is the initial treatment of choice for her? A. chemotherapy B. lobectomy with isthmectomy C. radiation therapy D. radioactive iodine therapy E. total thyroidectomy - ✔✔The answer is E. EXPLANATION: Total or near-total thyroidectomy is indicated for this woman. No chemotherapy (A) is available for thyroid cancer. Lobectomy with isthmectomy is reserved for papillary carcinoma that is less than 1 cm in size in persons with no history of radiation exposure and no evidence of metastasis. Radiation therapy (C) is used to treat bone metastasis and anaplastic carcinoma. Radioactive iodine therapy (D) may be used following thyroidectomy to ablate any remnant of the gland and to treat cancer that has metastasized or is otherwise high risk. A 33-year-old woman presents with a 3-year history of a persistent, unfluctuating depressed mood. She also notes persistent insomnia, poor concentration, and very little appetite. She denies previous similar symptoms, substance abuse, current prescriptive drug use, and has had no change in her overall life circumstances. She remains functional at work and in most relationships. On the basis of the information presented, what is the most likely diagnosis? A. dysthymic disorder B. premenstrual dysphoric disorder C. major depressive disorder D. cyclothymic disorder - ✔✔The answer is D. EXPLANATION: The main historical component that points to this diagnosis is the long-term (equal to or greater than 2 years), unfluctuating symptoms without mention of manic or hypomanic symptoms that would be typical of cyclothymic disorders. No variances with menstrual cycles are mentioned. Major depressive disorder is generally associated with more intense symptoms, including suicidal ideation, and only requires a 2-week duration of symptoms to diagnose. An endoscopy is ordered and the results show several large, deep ulcerations. Initial treatment consists of which of the following medications? - ✔✔The correct answer is ganciclovir. This patient has cytomegalovirus esophagitis, and the initial treatment is ganciclovir 5 mg/kg IV every 12 hours for 3 to 6 weeks. Nystatin suspension is used to treat oropharyngeal candidiasis. Acyclovir and famciclovir are used to treat herpetic esophagitis. Fluconazole is used to treat candidal esophagitis. A 58-year-old man with a 20-year history of gastroesophageal reflux disease (GERD) presents with progressive dysphagia for 5 months associated with a 20-lb weight loss. Results from a barium swallow are pictured below (Figure 18-1) apple cores esophageus. Which of the following is the most likely diagnosis? a. Achalasia B. Esophageal leiomyoma C. Uncomplicated reflux esophagitis D. Esophageal carcinoma - ✔✔he answer is D. EXPLANATION: Dysphagia on a background of GERD is an alarm signal for cancer, since GERD is related to increased risk for esophageal adenocarcinoma. Esophageal cancer is associated with a progressive course of dysphagia, first to bulky foods, then softer foods, and then liquids as the tumor invades the esophagus; significant weight loss is almost universal at the time of presentation. Barium swallow demonstrates narrowing at the tumor site with normal appearance of the remainder of the esophagus. Achalasia is a motor disorder characterized by dysphagia to both liquids and solids as well as regurgitation of food. Patients with achalasia typically drink large amounts of liquids to force their food down and have problems with aspiration pneumonia. Barium swallow in achalasia typically shows a dilated esophagus with a narrowing at the lower esophageal sphincter (bird's beak). Leiomyomas are generally asymptomatic. Patients with reflux esophagitis will complain of epigastric or substernal pain that is worse when supine or leaning forward Fluoroquinolones are contraindicated in which pts? - ✔✔pediatric patients. The risk-benefit assessment indicates that levaquin is only appropriate in pediatric patients at least 6 months of age, for treatment of inhalational anthrax (post-exposure). There are other medications, both oral and injectable, with better safety profiles that are available. Which of the following medications is approved for the prevention of NSAID-induced gastric and duodenal ulcers, and should be recommended to this patient? A. Ranitidine B. Ondansetron C. Omeprazole D. Sucralfate E. Dicyclomine - ✔✔The answer is C. EXPLANATION: Omeprazole is a proton pump inhibitor, and is the only medication listed that is indicated for the prevention of NSAID induced ulcers. Ranitidine is an H2 antagonist and is indicated for active duodenal or benign gastric ulcers and GERD. Ondansetron is a 5-HT3 receptor antagonist and is indicated in the prevention of nausea and vomiting. Sucralfate is approved for treatment of an active duodenal ulcer and maintaining healed ulcers. Dicyclomine is an anticholinergic, and is indicated for the treatment of irritable bowel syndrome. A 64-year-old male presents with right knee pain and stiffness while walking and going up and down stairs for the past six months. He states the pain persists all day long and is relieved with rest. There is no history of trauma and his past medical history is unremarkable. An x-ray of the right knee is performed and the following is observed: joint space narrowing A. Bursitis B. Osteoarthritis C. Torn posterior cruciate ligament - ✔✔The answer is B. EXPLANATION: Osteoarthritis (OA) is the most common cause of chronic knee pain over 45 years of age and commonly seen in weight-bearing joints when walking or climbing stairs. As disease progresses, it becomes continuous and present at night. OA in the x-ray shows a narrowed joint space (white arrow) on the medial side of the knee A 28-year-old female presents complaining of progressive vision loss and mild eye pain in the right eye. She states that her vision is most impacted centrally. She denies any injury, chemical exposure, contact lens use, recent illness, or history of similar symptoms. She has had some diplopia and dysequilibrium for the past two weeks. Her visual acuity reveals 20/50 in her right eye, 20/20 in her left eye, and 20/30 together. She has no conjunctival, scleral, or fundoscopic changes. Her intraocular pressure is 14 bilaterally. What is the most likely diagnosis? A. Conjunctivitis B. Glaucoma C. Keratitis D. Macular degeneration E. Optic neuritis - ✔✔The answer is E. EXPLANATION: This patient presents with classic symptoms for optic neuritis. Symptoms may include sudden or progressive unilateral vision loss, often with central field defect (scotoma). Pain may be present with eye movement. Vision changes will vary in severity, based on the level of inflammation. The majority of optic neuritis cases are retrobulbar, resulting in a normal fundoscopic exam. There is often a loss of color differentiation, and the affected eye may have decreased papillary light reactivity. The patient also exhibits additional symptoms that are suggestive of possible demyelinating disease (such as Multiple Sclerosis), which are strongly associated with optic neuritis. Conjunctivitis would have associated conjunctival injection, a clear cornea, no visual acuity changes, and would likely be associated with allergic, viral, or bacterial symptomology. Acute glaucoma would likely be associated with marked vision loss, headache, a fixed pupil, corneal cloudiness, and conjunctival injection. In addition, the intraocular pressure would be increased. Keratitis often presents with vision loss, pain, photophobia, conjunctival injection, stromal infiltrate, and corneal disruption. Macular degeneration develops gradually with increasing age, causing bilateral central visual loss. Which of the following types of thyroid cancer involve the parafollicular cells (or C cells) of the thyroid? - ✔✔medullary thyroid carcinoma. Unlike papillary (choice B) and follicular (choice C) thyroid cancers, which arise from thyroid epithelial cells, medullary thyroid cancer arises from the parafollicular cells of the thyroid. Anaplastic thyroid cancer, choice E, arises from undifferentiated cells. Thyroid lymphoma, choice D, is most commonly of B cell follicle center cell origin. A 21-year-old male with benign essential tremor asks to be placed on medication, to decrease his tremor for upcoming graduate school interviews. You discuss the potential benefits and side effects of medication and he is agreeable. Which of the following is the first-line agent of choice? A. Alprazolam B. Botulinum toxin C. Primidone D. Propanolol E. Topiramate - ✔✔The answer is D. EXPLANATION: Benign essential tremor is often worse during times of increased stress and decreased sleep. Management should include addressing these situations and providing nonpharmacologic therapy information. In specific cases such as this patient, beta-blocker therapy has been shown to effectively reduce tremor activity, with intermittent therapy being acceptable. Other medications, such as the others listed in the answer choices, may be used as alternatives to beta blockers, with each having individual risks and side effect profiles. An avulsion fracture at the base of the fifth metatarsal is commonly called which of the following? A. Bennett fracture B. Boxer's fracture C. Chauffer's fracture D. Jones fracture E. Lisfranc fracture - ✔✔The answer is D. EXPLANATION: An avulsion fracture at the base of the fifth metatarsal, usually secondary to plantar flexion and inversion is called a Jones fracture. Also called a ballet or dancer's fracture, it is the most common metatarsal fracture. The fracture occurs at the proximal diaphysis. A Bennett fracture is an oblique fracture of the first metacarpal near the carpometacarpal joint. A boxer's fracture is a fracture of the fifth metacarpal. This is the most common fracture of the hand. A chauffer's fracture is an oblique fracture through the base of the radial styloid in the forearm. A Lisfranc fracture is actually a fracture and dislocation involving the tarsometatarsal joints A 28-year-old male is concerned because he has a friend who was diagnosed with chronic hepatitis C and wants to know if he is at risk for this disease as well. Which of the following answers elicited in your history would make you the most suspicious? A. previous intravenous drug use B. blood transfusion last year C. monogamous relationship D. recent negative HIV test E. previous history of hepatitis - ✔✔The answer is A. EXPLANATION: Intravenous drug abuse accounts for over 50% of hepatitis C cases. Recent blood transfusions are unlikely to cause hepatitis C. Hepatitis C is more likely to be contracted in patients with multiple sexual partners, although the incidence of transmission via sexual intercourse is considered low. Hepatitis A is transmitted via the fecal-oral route and does not increase the chances of hepatitis C. Which of the following drugs is indicated for the treatment of anemia associated with chronic renal failure? A. deferoxamine B. warfarin C. protamine sulfate D. erythropoietin E. argatroban - ✔✔The answer is D. EXPLANATION: Erythropoietin (EPO) is a naturally occurring hormone synthesized and secreted by the kidneys. Synthetic forms of EPO include Epogen and Procrit. EPO works at the red bone marrow to stimulate erythropoiesis. In patients with chronic renal failure, EPO production is usually impaired, and this EPO deficiency leads to anemia. Deferoxamine is an iron-chelating compound that can be given systemically in situations of iron overdose. Warfarin and argatroban are both anticoagulants and do not typically affect red cell count. Protamine sulfate is a heparin-chelating compound that can be given in cases of heparin overdose. You are examining n 42-year-old male with the following physical examination findings (see picture below). What symptoms would most likely correspond to his diagnosis? Pic-acanthcosis nigrans A. anxiety B. palpitations C. excessive snoring D. polyuria and polydipsia E. weight gain - ✔✔The answer is D. EXPLANATION: The correct answer is (D). The patient's physical examination findings suggest acanthosis nigricans, a condition associated with diabetes mellitus. This patient would most likely present with polydipsia and polyuria at diagnosis. He may have weight loss and fatigue. Anxiety and palpitaions are not as likely to present symptoms of diabetes. De Quervain tenosynovitis affects which tendons - ✔✔De Quervain tenosynovitis is a common condition that occurs in patients who have experienced excessive use of the thumb or wrist. This is a tenosynovitis of the extensor pollicis brevis and abductor pollicis tendons (A), where the tendons lie in the groove of the radial styloid. The diagnosis of De Quervain tenosynovitis is supported by a history of pain in this location along with a painful range of motion of the thumb and further confirmation may be provided by a positive Finkelstein test. carpal tunnel syndrome affects which tendons - ✔✔The flexor pollicis longus and flexor digitorum profundus Which ligament is injured in Gamekeeper's thumb. - ✔✔The ulnar collateral ligament is injured in Gamekeeper's thumb. Treatment of complete heart block - ✔✔Permanent pacemaker insertion A patient is found with a microcytic anemia. Further laboratory findings include a serum iron value of 26 mcg/dl (50 to 175 mcg/dl), a total iron binding capacity of 376 mcg/dl (250 to 370 mcg/dl), a lactic dehydrogenas of 143 U/L (100 to 190 U/L) and a creatinine level of 0.8 mg/dl (0.1 to 1.5 mg/dl). Which of the following is the best recommendation for therapy? A. Ascorbic acid 250 mg po daily B. Ferrous sulfate 325 mg po three times daily C. Glucophage 500 mg po twice daily D. Sodium ferric gluconate 1.5 GMs IM monthly E. Vitamin B12 1000 mcg po daily - ✔✔The answer is B. EXPLANATION: Based on laboratory values, this patient has iron deficiency anemia. The most important part of treatment is identifying the cause of the blood loss. Therapy consists of replacement of iron through the use of ferrous sulfate. If the patient is unable to tolerate oral iron dosing, IM sodium ferric gluconate may be used, but only after intolerance of po dosing is demonstrated. Glucophage is used for diabetes. Vitamin B12 is used in vitamin B12 anemia (a macrocytic anemia). Ascorbic acid (vitamin C) is used to increase iron absorption if needed. A 12 year-old African-American male with a history of sickle cell disease presents to the clinic for routine follow up. A peripheral smear is performed. Which of the following best describes the cause of the abnormality pictured in the patient's peripheral smear? (note photo taken from figure 29-12 in Harrison's)--> howell jolley bodies A. Absent or non-functioning spleen B. Failure of nuclear maturation C. Intravascular hemolysis D. Lead intoxication E. Presence of uremia - ✔✔The answer is A. EXPLANATION: Howell-Jolly bodies are noted in the peripheral smear and result from the lack of removal of nuclear material due to an absent or non-functioning spleen. Failure of nuclear maturation (B) produces macrocytosis, intravascular hemolysis (C) leads to the creation of schizocytes, lead intoxication (D) and thalassemia cause basophilic stippling, and uremia (E) is associated with Burr cells. radioactive iodine (RAI) therapy contraindication to receiving this treatment? - ✔✔Pregnancy In a 73-year-old male, laboratory and radiologic findings that demonstrate marrow plasmacytosis with >30% plasma cells, a monoclonal globulin spike present, and lytic bone lesions is most consistent with which of the following? A. Acute myelogenous leukemia B. Chronic myelogenous leukemia C. Hodgkin lymphoma D. Multiple myeloma E. Non-Hodgkin lymphoma - ✔✔The answer is D. EXPLANATION: The diagnosis of plasma cell myeloma is confirmed when at least one major and one minor criterion, or three minor criteria, are documented in a patient. This patient has one major and two minor criteria. AML and CML are not associated with lytic lesions. Hodgkin and Non-Hodgkin lymphoma typically do not have lytic lesions or monoclonal globulin spikes. An 84-year-old male is admitted to the hospital for the chief complaint of syncope. The history provided states that the patient was in his normal state of health and feeling well when he had fallen, with an apparent loss of consciousness for 25-30 seconds. He has a history of hypertension and arthritis, and is well managed on medications that include lisinopril and acetaminophen. During his time on the telemetry unit it's noted that the patient has periods of sinus bradycardia in the 30s, followed by normal sinus rhythms that fluctuate in the 60 to 120 range. During several of the bradycardia episodes the patient becomes symptomatic with shortness of breath, lightheadedness, and dizziness. His blood pressure during these episodes is measured at 88/56. Given this clinical scenario, what is the most likely diagnosis for this patient? A. Ventricular tachycardia B. Sick sinus syndrome C. First-degree AV block D. Wolff-Parkinson-White syndrome E. Premature atrial contractions - ✔✔The answer is B. EXPLANATION: This patient is exhibiting signs and symptoms related to sick sinus syndrome (B). There is no evidence in the clinical scenario to suggest any ventricular ectopy (A), and the patient's age and characteristics of the arrhythmia are not consistent with Wolff-Parkinson-White syndrome (D), or other skipped beat abnormalities (C and E). [Show More]
Last updated: 1 year ago
Preview 1 out of 92 pages
Instant download
Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
Also available in bundle (1)

PANCE EXAM BUNDLE,
ALL YOU NEED TO PASS THE PANCE EXAM, DOWNLOAD TO SCORE HIGH
By bundleHub Solution guider 1 year ago
$38
11
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Aug 20, 2022
Number of pages
92
Written in
Additional information
This document has been written for:
Uploaded
Aug 20, 2022
Downloads
0
Views
46


.png)
, All Correct, Download to Score A.png)
, All Correct, Download to Score A.png)
, All Correct, Download to Score A.png)
, Correct, Download to Score A.png)
, Correct, Download to Score A.png)