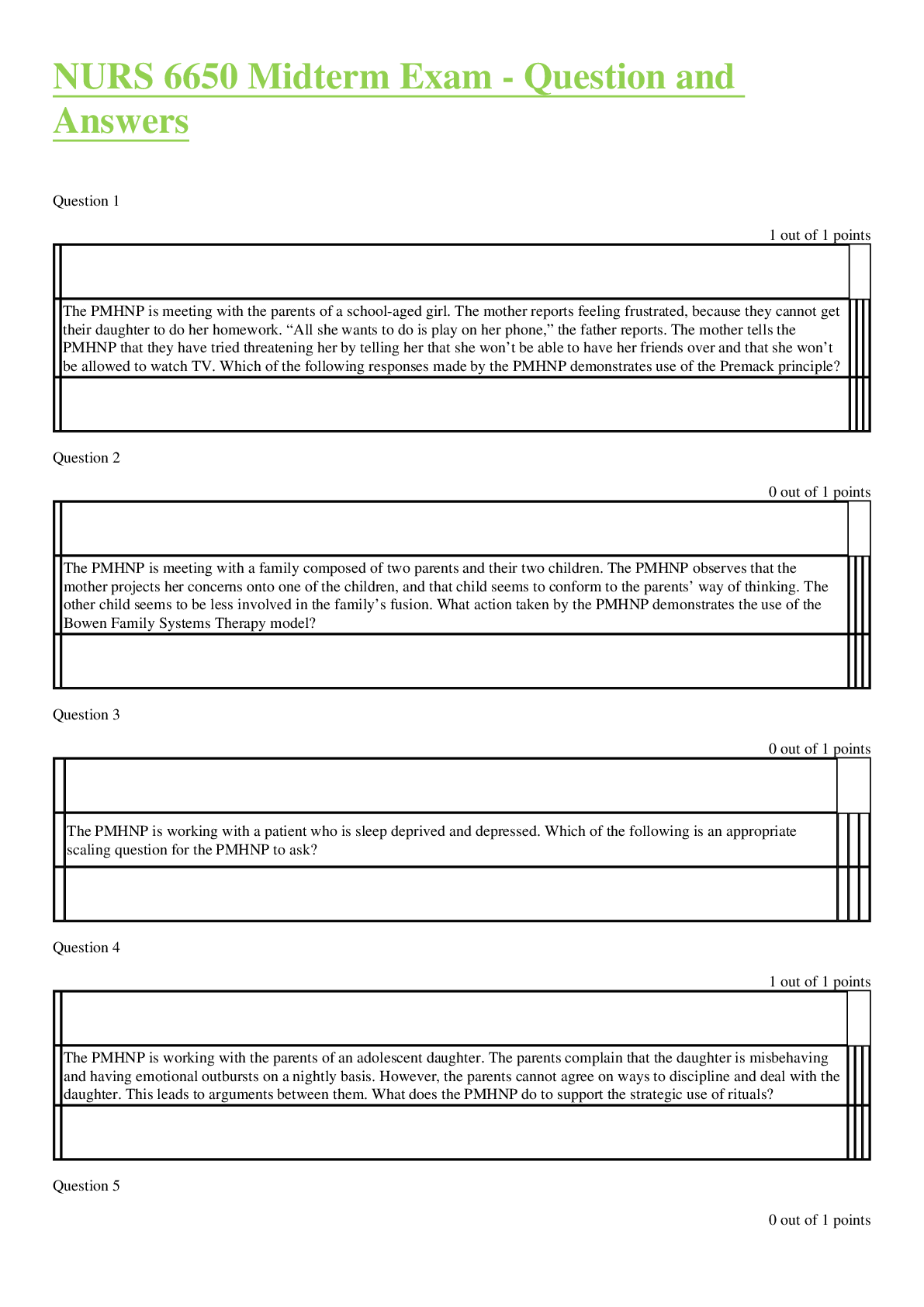
Health Care > QUESTIONS & ANSWERS > Accident and Health Insurance Agent/Broker Practice Exam Questions with 100% Correct Answers. Rated (All)
Accident and Health Insurance Agent/Broker Practice Exam Questions with 100% Correct Answers. Rated A+
Document Content and Description Below
Accident and Health Insurance Agent/Broker Practice Exam Questions with 100% Correct Answers Sally is considering her Medicare options. She understands that to enroll in Medicare Part B, she will h... ave to pay a monthly premium. Since she is healthy, she is considering delaying her enrollment until later. Will she be able to enroll at a later date? 1.Yes, she can enroll at anytime in the future 2.Yes, however; she would have a permanent premium penalty when she does enroll 3.No, this is a take or leave it situation 4.Yes, but she would have to show evidence of good health. - Yes, however; she would have a permanent premium penalty when she does enroll Under Medicare Part A, a spell of illness begins again and is subject to a new deductible for another admission when: 1.The patient has been discharged from a prior stay and 45 days have elapsed 2.The patient has been discharged from a prior stay and 30 days have elapsed 3.The patient has been discharged from a prior stay and 60 days have elapsed 4.The patient has been discharged from a prior stay and 90 days have elapsed - The patient has been discharged from a prior stay and 60 days have elapsed What type of insurer retains risk? 1.Government insurance. 2.Reinsurers. 3.Self insurers. 4.Assessment insurers. - Self insurers. A variety of types of care are provided under a long-term care policy. All of the following are types of care generally provided EXCEPT: 1.Home health care 2.Intensive care 3.Custodial care 4.Skilled care - Intensive care Melvin has a long-term care policy with a 30-day elimination period. The policy has a daily benefit of $100/day. The policy has a 3-year benefit period. If Melvin is confined to a nursing home for 9 months, how much in benefits will his policy pay? 1.$27,000 2.$18,000 3.$24,000 4.$17,000 - $24,000Martin and his friends were at a local tavern celebrating his birthday. Martin left the bar to drive home, but unfortunately, he was involved in a fatal accident, killing himself and two other individuals. An autopsy reveals that Martin was well above the legal limit on his blood alcohol test. Martin's family will receive the following from his Accidental Death and Dismemberment policy: 1.His family will receive reduced benefits since other deaths were involved. 2.His family will receive the principal sum since this was death 3.His family will receive no benefits, since he was in the act of committing a felony 4.His family will receive no benefits since there was no dismemberment involved. - His family will receive no benefits, since he was in the act of committing a felony An exclusion that always appears in a health policy is: 1.No coverage for drug or alcohol related illness 2.Hernia from an accident 3.Travel outside of the USA 4.Injury in the act of committing a felony - Injury in the act of committing a felony Bruce owns a plan that pays $100 daily benefit for a hospital stay with no deductible. This kind of policy is known as a (an): 1.Major medical plan 2.Basic plan 3.Indemnity plan 4.Reimbursement plan - Indemnity plan Under what conditions is the death benefit (principal sum) payable under an Accidental Death and Dismemberment (AD&D) policy? 1.The insured dies from a grave illness 2.The insured dies from natural causes 3.The insured dies from an accident 4.All of the above - The insured dies from an accident An insurance agent told a member of his church who had recently experienced several personal and financial losses that he could see that she got a more favorable rate on her insurance policies than her health and general circumstances would warrant. The woman had been his kindergarten teacher and was a pillar in the community's life. He wanted to help her. Which of the following is FALSE? 1.The agent was breaking the law. 2.The agent is compassionate. 3.The agent was engaging in unfair discrimination. 4.The agent was engaging in twisting. - The agent was engaging in twisting.Which of the following is NOT considered to be an unfair claims settlement practice? 1.Knowingly misrepresenting policy provisions. 2.Replacing one insurance policy with another. 3.Failing to promptly acknowledge pertinent communications. 4.Refusing to pay claimants without conducting a reasonable investigation. - Replacing one insurance policy with another. The practice of using misrepresentation to induce a policyholder to replace a policy issued by the insurer the producer represents is called: 1.twisting. 2.churning. 3.intimidation. 4.misrepresentation. - churning. All of the following acts are considered unfair trade practices EXCEPT: 1.replacement. 2.misrepresentation 3.coercion. 4.rebating. - replacement. What gives the insurance company the right to assume rights of the insured in order to sue a responsible third party when damages are inflicted on the insured? 1.Warranties 2.Subrogation 3.Concealment 4.Utmost good faith - Subrogation Insurance contracts sometimes contain ambiguities. Which of the following has not been taken to court for further interpretation? 1.Reasonable expectations 2.Subrogation 3.Ambiguities in a contract of adhesion 4.Utmost good faith - Subrogation There are various optional provision for health policies. Which of the following is not an optional provision? 1.Intoxicants and narcotics 2.Conformity with state statutes 3.Reinstatement 4.Illegal occupation - ReinstatementTony (the insured) cancelled his health policy by submitting a written notice to the insurer. How are unearned premiums handled? 1.Returned to the insured using a pro-rata basis 2.They are returned to the agent 3.The insurer gets to keep them 4.Returned to the insured using a short-rate basis - Returned to the insured using a short-rate basis The Patient Protection and Affordable Care Act allows states to combine their SHOP exchange with - 1.Commercial insurance companies 2.Their Medicaid recipients 3.Their exchange for individual consumers 4.All of the above - Their exchange for individual consumers o elect continuation of coverage, the insured must request continuation during the election period (45 days after the date of the _____). Employers must provide the proper forms for election within 14 days of receipt of request of election. 1.Arraignment, annulment, or release on bond 2.Indictment, cancellation, or invalidation 3. incarceration, or arraignment 4.Death, divorce, or termination - Death, divorce, or termination Insurers must maintain an advertising file of all material printed, published, or distributed advertisements of policies for _____, subject to examination by the Commissioner. 1.No more than five years 2.No less than four years 3.No more than two years 4.No less than three years - No less than three years For dependents that were not previously eligible for enrollment in the Maryland Health Connection, how much time must they be given to enroll after being sent a notice that they are now eligible? 1.30 days 2.45 days 3.60 days 4.90 days - 30 dayaIndividuals covered under a Medicare Supplement policy may suspend benefits and premiums for up to _____ months if the individual applies and is determined to be eligible for Social Security disability benefits. 40 24 10 52 - 24 Home health care services are long-term care benefits: 1.For medical and non-medical services 2.Provided to the ill, injured, or disabled individuals in their home 3.That includes those of a homemaker, and assistance with activities of daily living 4.All of the Above - All of the Above What provides hospital or medical policies or plans, nonprofit health service policies or plans, and health maintenance organizations? Health benefit plans Wellness cooperative plans "Cafeteria" wellness plans Annuitized wellness cooperatives - Health benefit plans No policy may be advertised, solicited, or issued as a Medicare supplement policy if the policy or certificate contains limitations or exclusions on coverage that are more restrictive than: Those of Medicare Those agreed to by the insured Those allowed by the Commissioner Those permitted under Medigap Part B - Those of Medicare Continuation of coverage for group medical plans shall continue for up to __ months after the date of death, divorce, or termination, subject to payment of premiums. 9 1 8 15 4 - 18 What provides affordable and accessible health insurance to support public and private initiatives for individuals without health insurance and promotes a health care system that meets the needs of all of the residents of its jurisdiction? Wellness maintenance associationsPrepaid health service alliances Nonprofit health service plans Prepaid wellness cooperatives - Nonprofit health service plans To act as an insurer in the state of Maryland, an insurer must hold _____ issued by the Commissioner. A compelling warrant of remuneration An applicable diploma of indemnity A valid certificate of authority A legitimate record of credibility - A valid certificate of authority Which type of care is a system of cost containment methods used by insurers or their agents to control cost and access to health care services, where insurers and providers review and preauthorize treatment plans? Non-critical Managed Free Supplemental - Managed Long-term care insurers may require a physical examination of any applicant: Age 70 or older Age 65 or older Age 75 or older Age 80 or older - Age 80 or older Which type of care is a system of cost containment methods used by insurers or their agents to control cost and access to health care services, where insurers and providers review and preauthorize treatment plans? Free Non-critical Managed Supplemental - Managed An insurer is anyone who acts as a/an __________in the business of entering into insurance contracts. Surety Indemnity Contractor All of the Above - All of the Abovevery Medicare supplement insurer must establish marketing procedures that any comparison of policies is fair and accurate, and _____ is not sold or issued. An unwarranted annuity Excessive insurance Prepaid insurance A disproportionate annuity - Excessive insurance Some policies require that the insured be confined to his/her home and be under a doctor's care. This type of policy is called a: Recurrent disability Nonoccupational Residual disability Medically defined disability - Medically defined disability Insurance companies use which of the following to limit claims from pre-existing disabilities or to control adverse selection? Recurrent disability clauses Reduced benefits Elimination periods Probationary periods - Probationary periods An example of presumptive disability might be any of the following EXCEPT: Severance of a hand Complete loss of hearing Amputation of a leg at the hip Total Blindness - Severance of a hand The government is one of three primary types of insurers. Government insurance provides protections against fundamental risks. Which of the following is an example of a government insurance program? Social Security Blue Cross Lloyd's Associations All of the above - Social Security Medicaid is a needs tested program. It provides medical benefits for the poor and indigent. It is funded as follows: 1.Employer taxes based on payroll 3.Payroll taxes from the employed 4.Part of Medicare5.Jointly funded by individual states and the federal government - Jointly funded by individual states and the federal government A Medicare Supplement policy is issued with a "Free Look" period. This is usually a minimum of: 10 days 45 days 30 days 20 days - 30 days All long-term care policies are guaranteed renewable. Some long-term policies are called noncancellable. Which of the following is true about a noncancellable policy. 1.Policy cannot be cancelled as long as premiums are paid 2.Provisions of the policy can be changed 3.The insurer can decline to renew 4.The insurer can change the policy premium - Policy cannot be cancelled as long as premiums are paid Both private and government insurance are available in every state in the United States. Which of the following is one of the major differences between private and government insurance. 1.Government insurance can be either Federal or state 2.Both private and government have disability coverage 3.Government insurance is more efficient to run. 4.Private insurance can deny coverage to individuals - Private insurance can deny coverage to individuals In all of the following scenarios, the statements regarding loss are false EXCEPT: 1.Betty submits a claim for $300 to her insurance company. The amount of Betty's loss is $300. 2.Andrew gets in a fender bender, causing $3,000 in property damage to his car. He submits the claim to his insurance company, and the insurance company pays for the repairs. Andrew did not experience a loss. 3.Susie Q purchases a life insurance policy that will pay $100,000 to a beneficiary upon her death. The amount of loss upon Susie Q's death is $1,000,000. 4.Jim Bo has a renter's insurance policy that pays him $2,000 for loss of property caused by theft even though the actual cash value of his loss is $3,000. The amount of Jim Bo's loss is $2,000. - Betty submits a claim for $300 to her insurance company. The amount of Betty's loss is $300Once an insurance agent or company advertises their services, they must maintain a complete file of all material available for periodic inspection as to the content, modes of distribution and frequency. These advertising files must be maintained for: A period of not less than 1 year A period of not less than 3 years A period of not less than 2 years A period of not less than 5 years - A period of not less than 3 years Mark is a producer and has authority to sell life and health insurance, but is not associated with ACME Insurance company, but they can accept applications from him if: 1.The insurer can issue the insurance, but it must contain a rider which clearly states the relationship between the insurer and producer 2.The insurer cannot accept applications from producers not associated with the company until after they have been appointed 3.The insurer can issue the insurance and appoint the producer immediately if his license was issued in the state of Maryland 4.If the insurer appoints him as a producer and updates the register within 30 days of the application date - If the insurer appoints him as a producer and updates the register within 30 days of the application date Under which of the following circumstances will the Commissioner not waive the license application requirements for an applicant who is not a resident of Maryland? 1.The applicant has a valid license in his/her home state 2.The applicant pays applicable nonresident license fees 3.The applicant's home state does not award nonresident licenses 4.The applicant submits the home state application - The applicant's home state does not award nonresident licenses Joey would try and lure prospective clients to purchase a policy from him by manipulation. He would subtly suggest or offer to recommend the client for membership to a selective country club if the person purchases a particular policy from Joey. This type of practice is called: 1.Intimidation 2.Bait and switch 3.Discrimination 4.Coercion - Coercion In addition to any greater penalty provided under the law, violation of Maryland insurance laws and regulations is a ________offense, subject to a fine up to $100,000. 1.Federal2.Felony 3.Misdemeanor 4.None of the Above - Misdemeanor The Commissioner is given broad powers to establish insurance rules, hold hearings and issue orders, take disciplinary action, and assess penalties and fines. He may examine and investigate individuals or entities as deemed necessary, but must conduct examinations at least every ¬¬¬¬____________: 18 months 2 years 5 years 48 months - 5 years As a disciplinary action, the Commissioner may assess penalties of ________. $400 to $800 $200 to $600 $100 to $500 $1000 to $5000 - $100 to $500 Martha is issued her license on October 17, 2012. When will she need to renew her license? On or before October 17, 2015 By midnight on December 31, 2014 On or before October 17, 2014 By midnight on December 31, 2015 - On or before October 17, 2014 The Commissioner may require up to __ hours of continuing education per renewal period for producer licensed for less than 25 consecutive years. 8 4 32 16 - 16 Insurers must report _________of a producer and update the producer register with the Commissioner within 30 days of the effective date. Termination Resignation Appointment Hiring - Termination [Show More]
Last updated: 1 year ago
Preview 1 out of 32 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
We Accept:

Reviews( 0 )
$10.00
Document information
Connected school, study & course
About the document
Uploaded On
Sep 20, 2022
Number of pages
32
Written in
Additional information
This document has been written for:
Uploaded
Sep 20, 2022
Downloads
0
Views
70


.png)

.png)
.png)
 answers.png)
 answers.png)

