*NURSING > STUDY GUIDE > NR507 FINAL EXAM STUDY GUIDE, Latest 2021, A guide - Chamberlain College Of Nursing. (All)
NR507 FINAL EXAM STUDY GUIDE, Latest 2021, A guide - Chamberlain College Of Nursing.
Document Content and Description Below
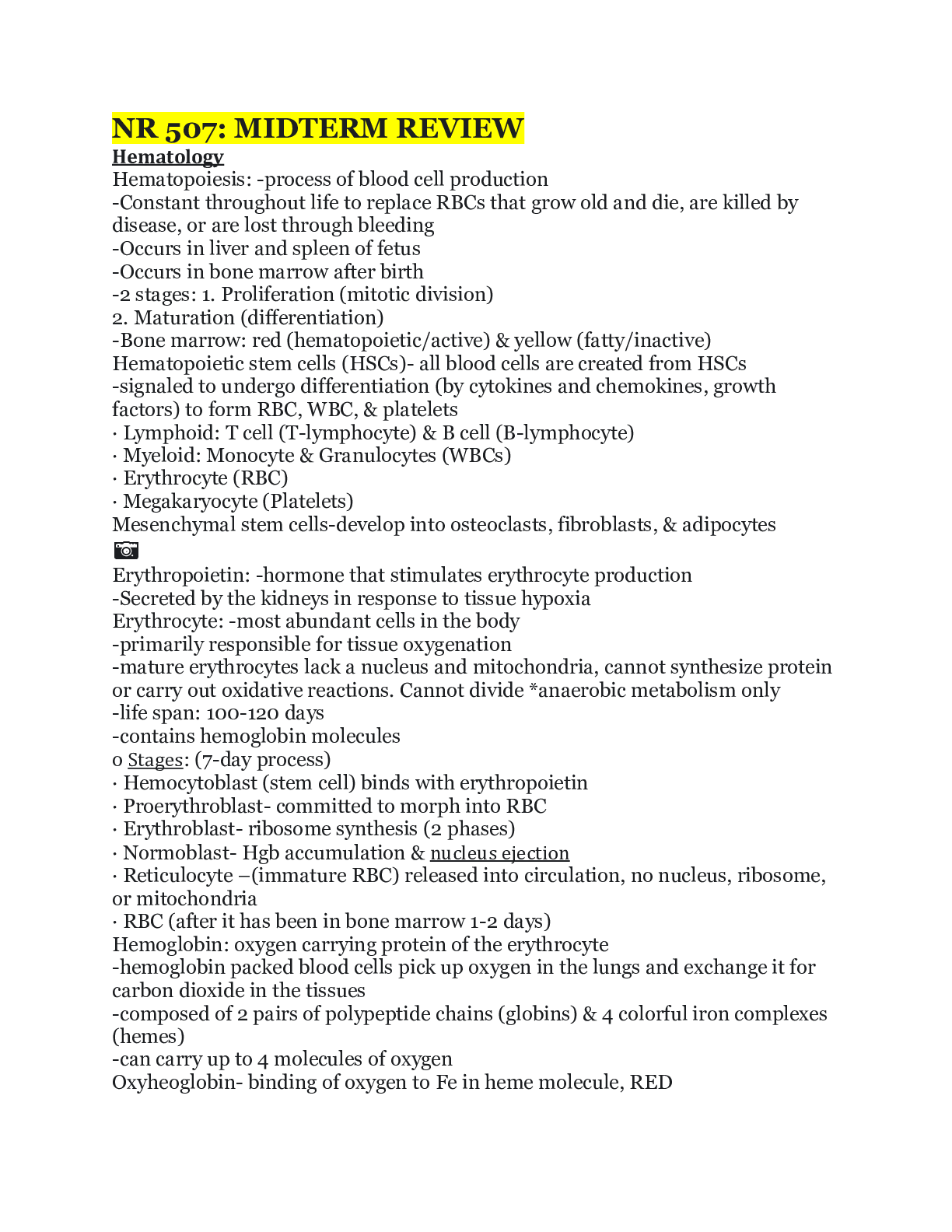
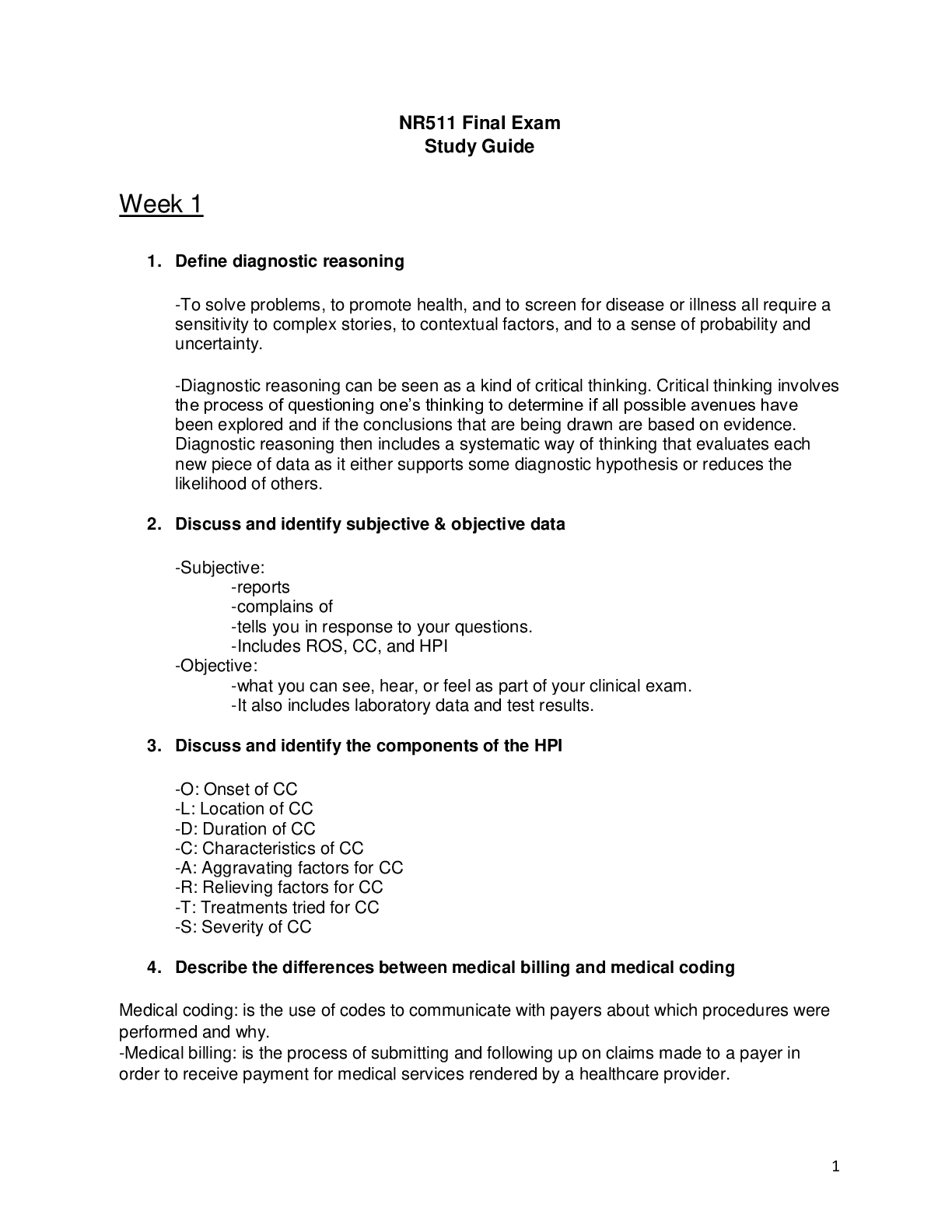
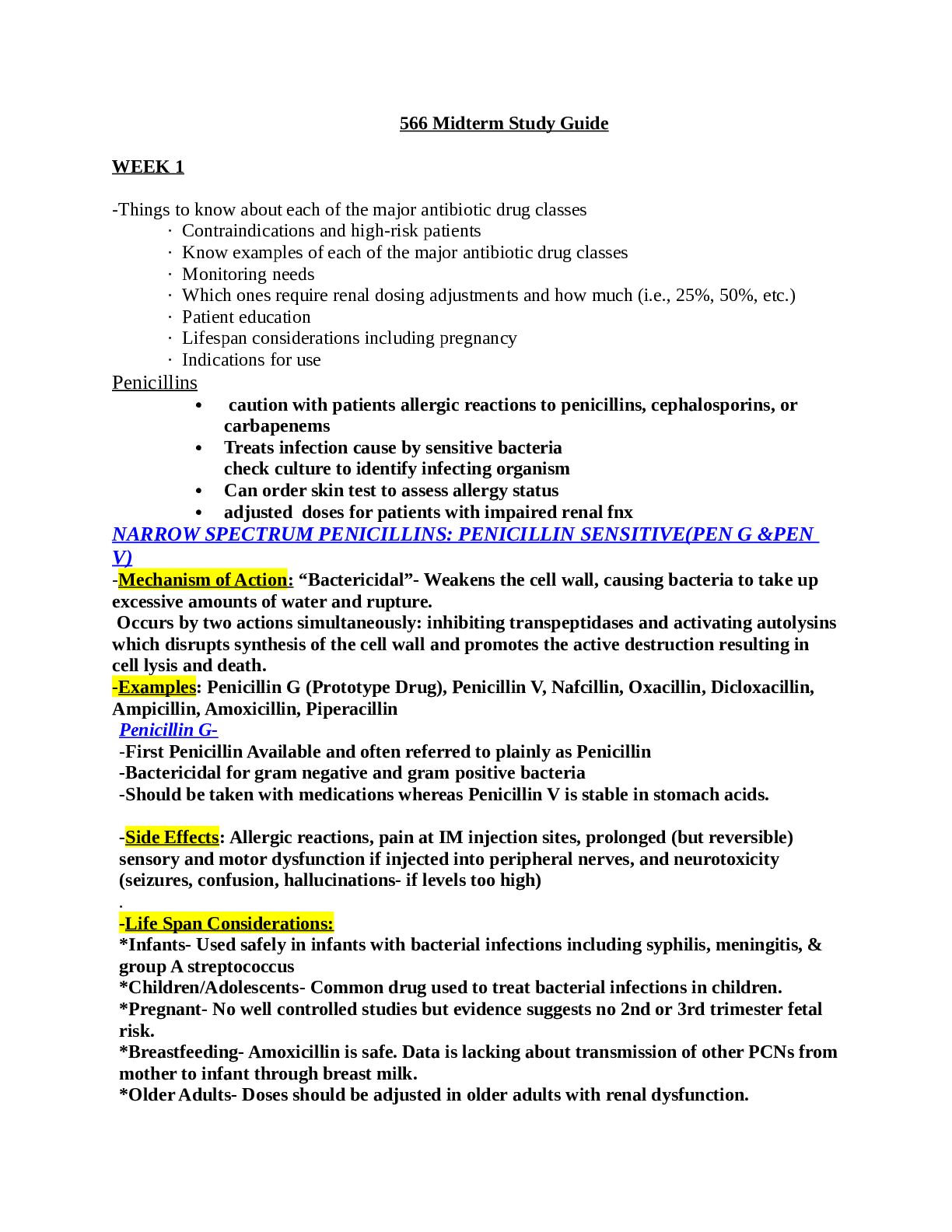
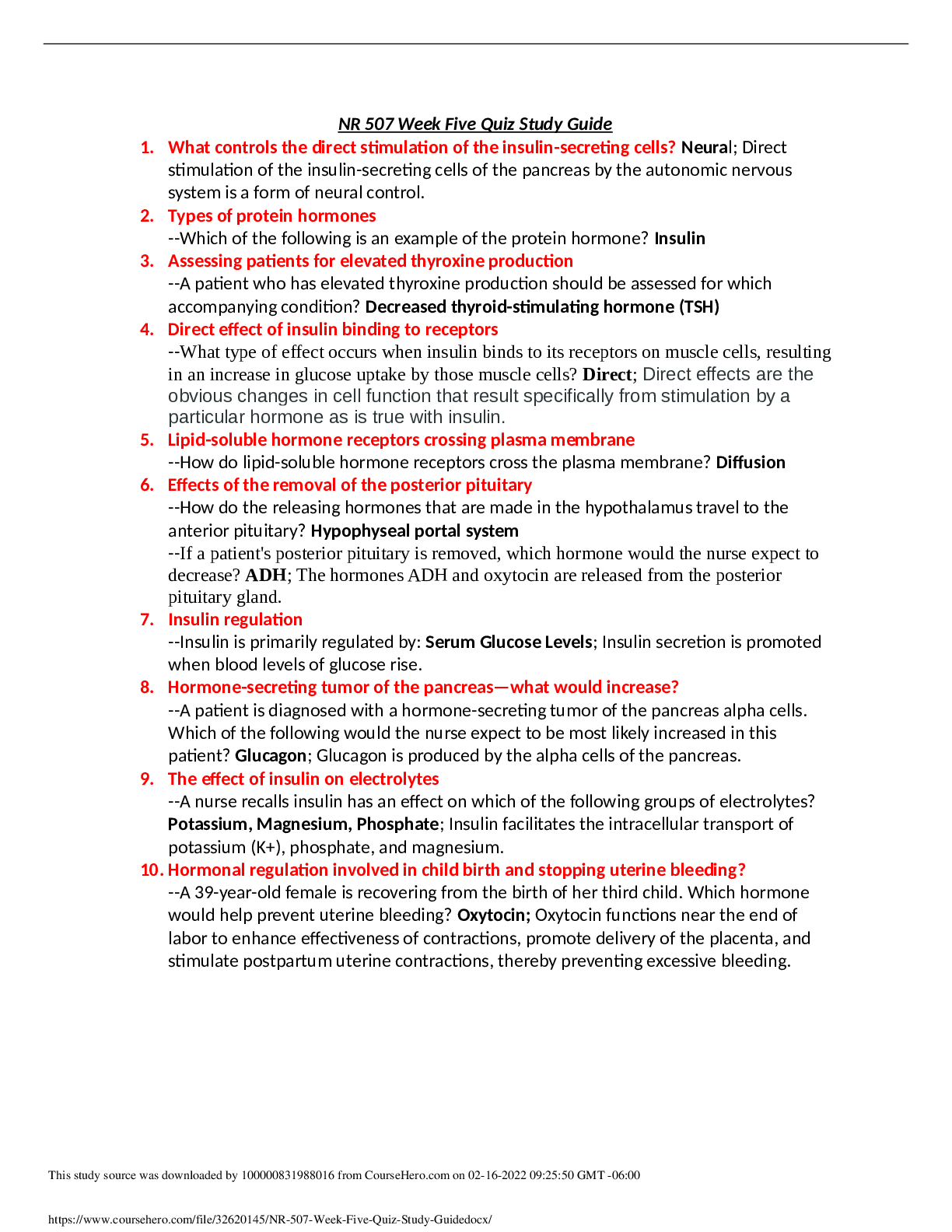
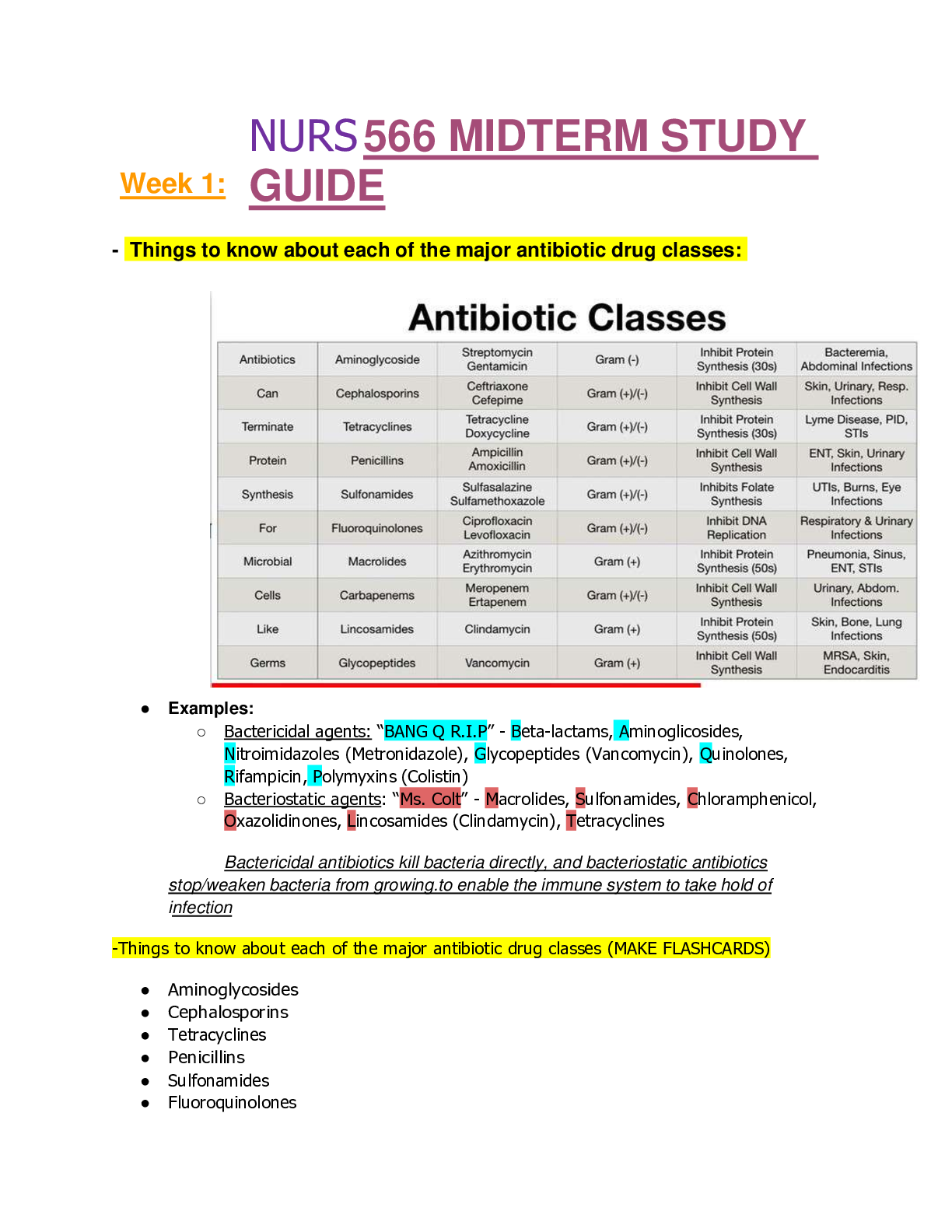
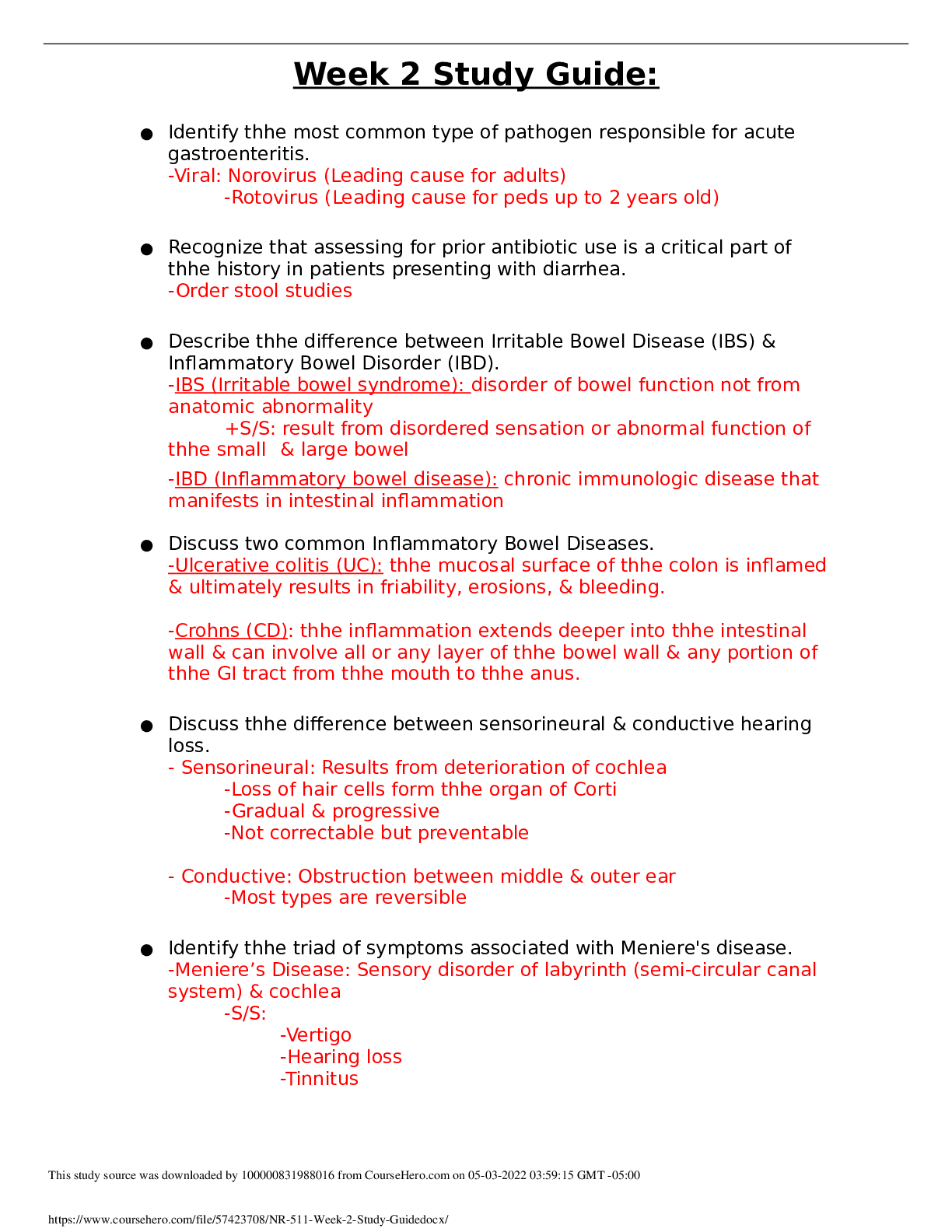
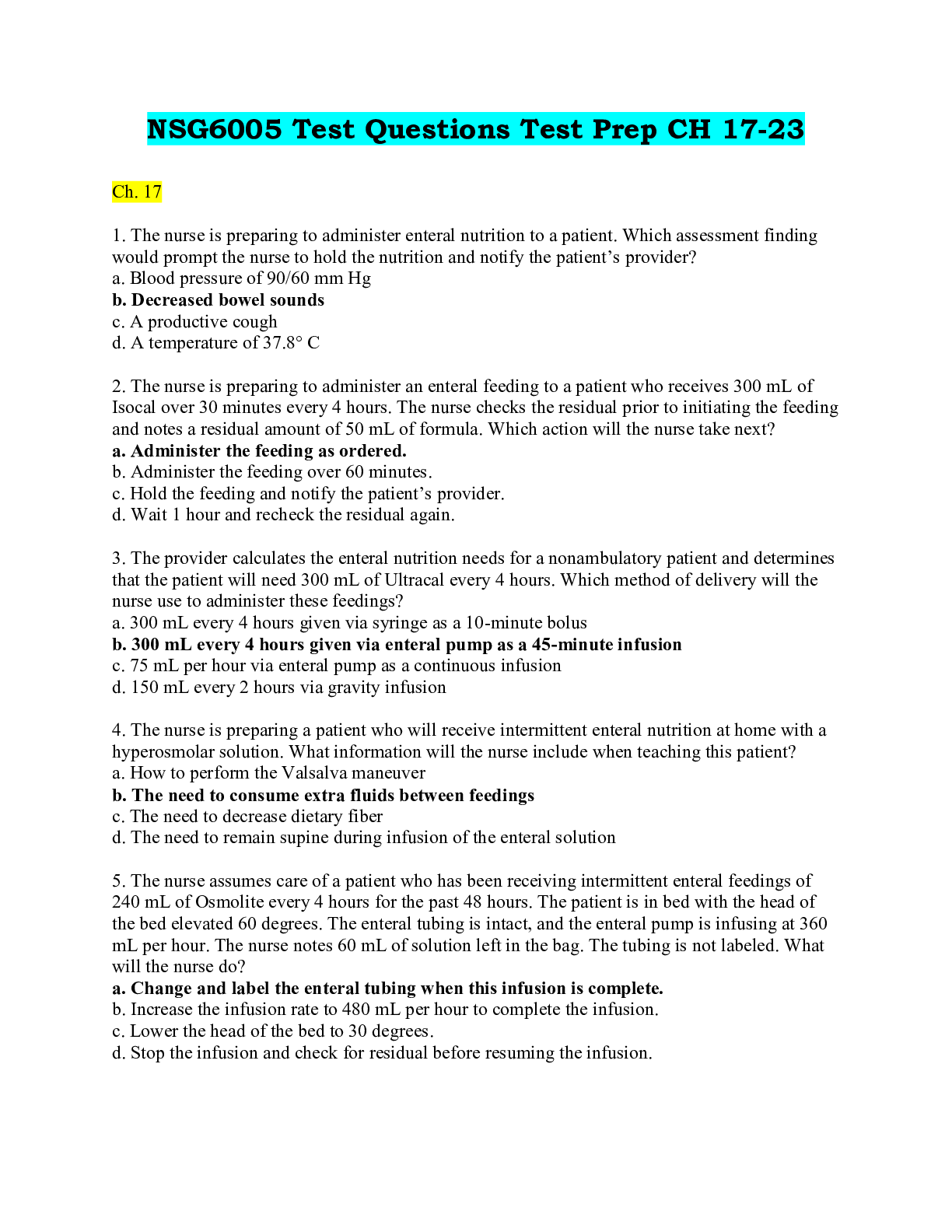
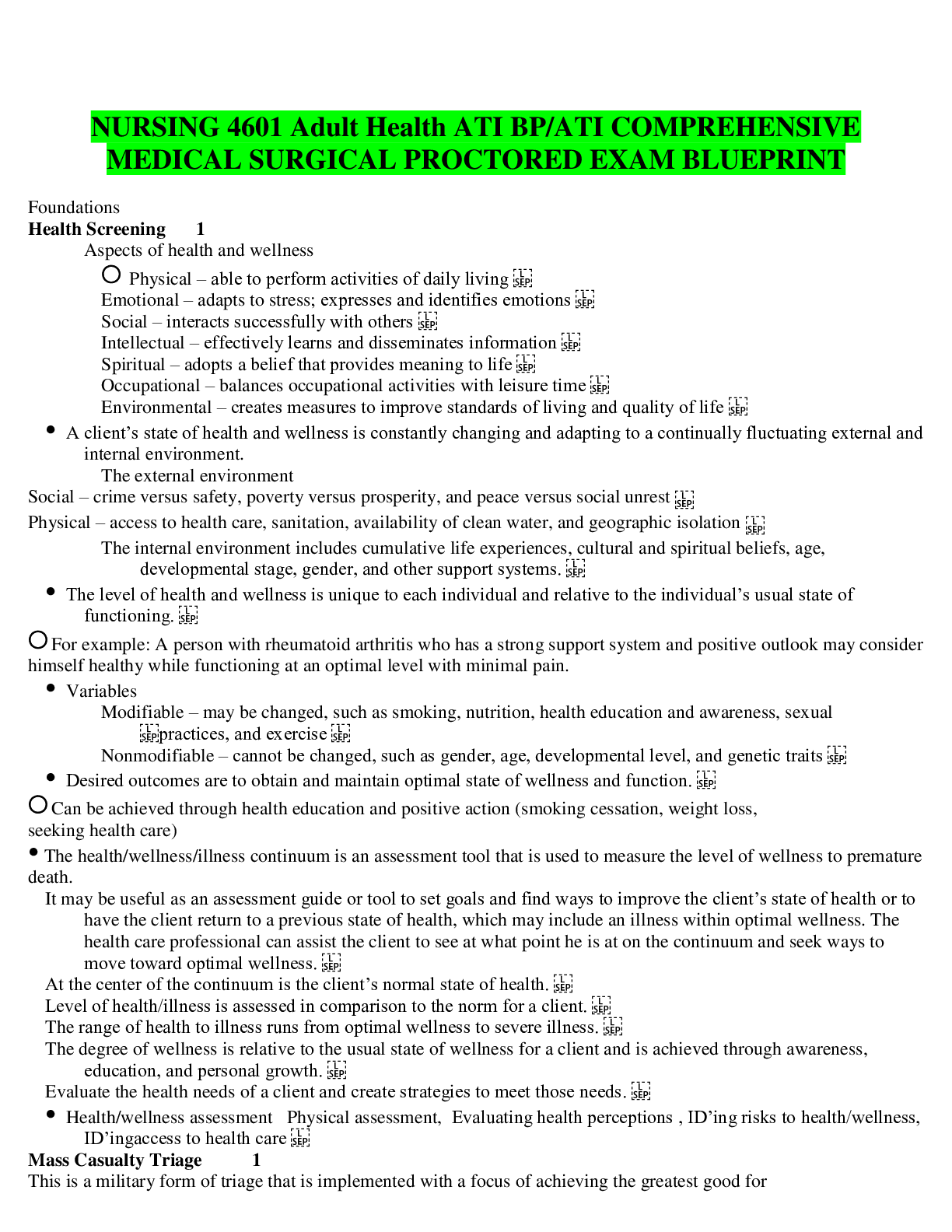
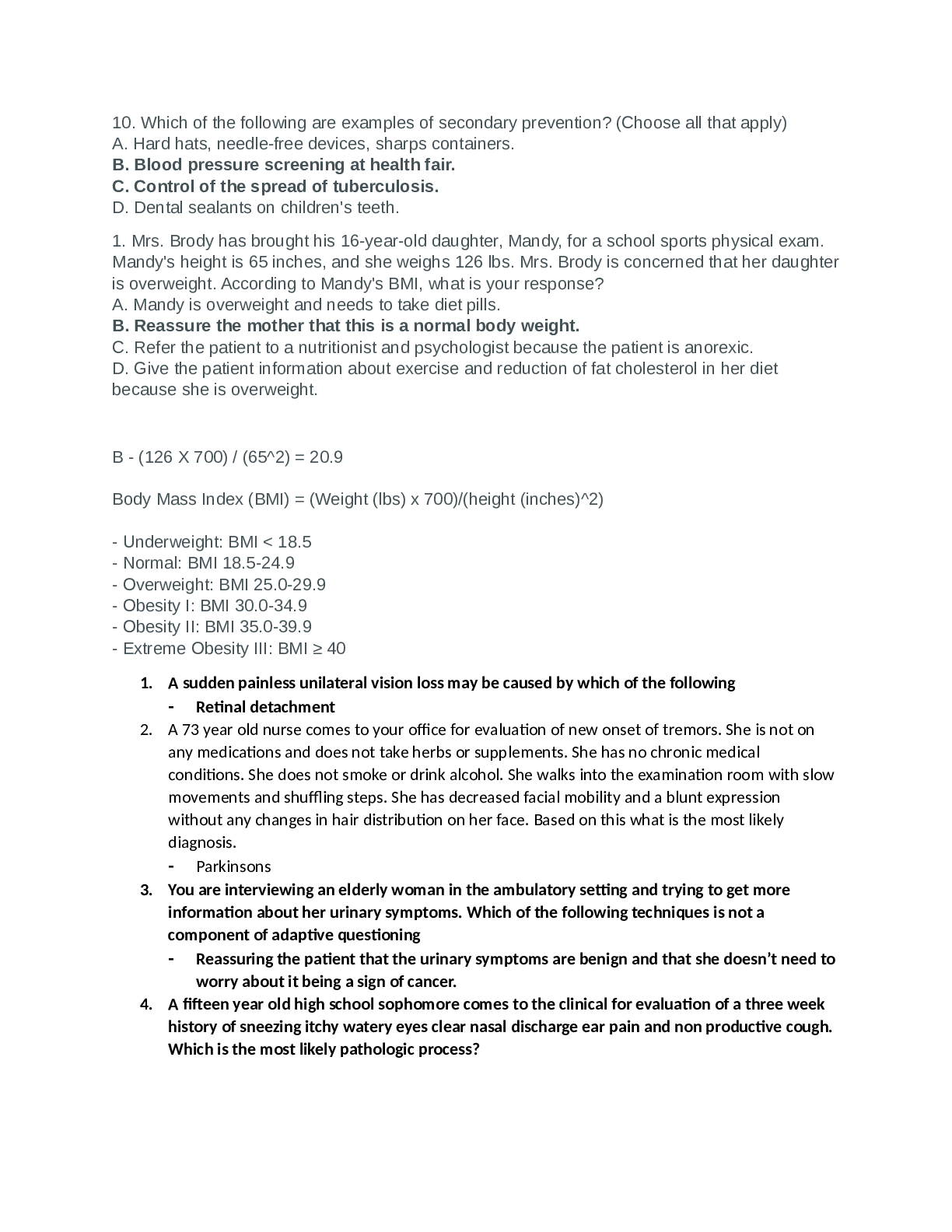
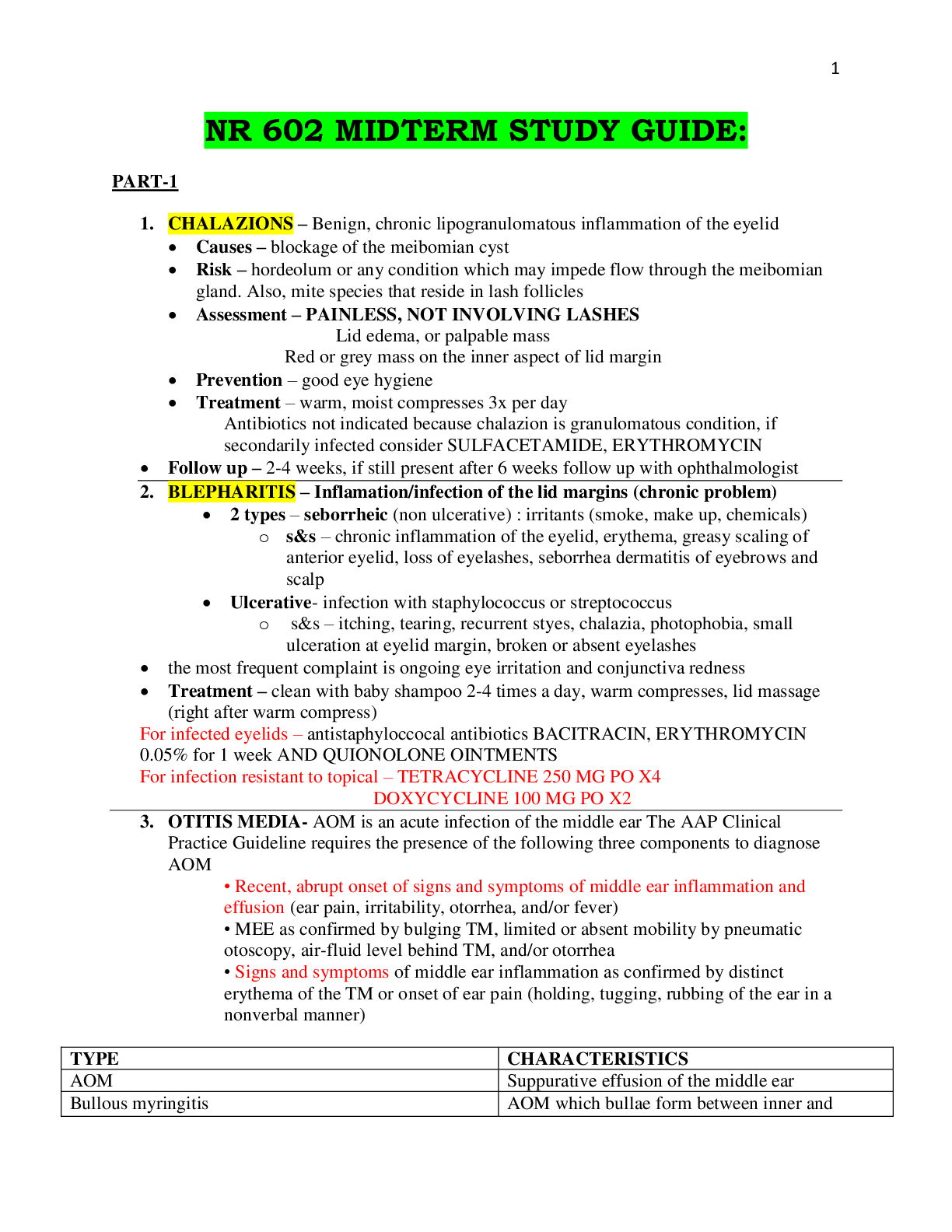
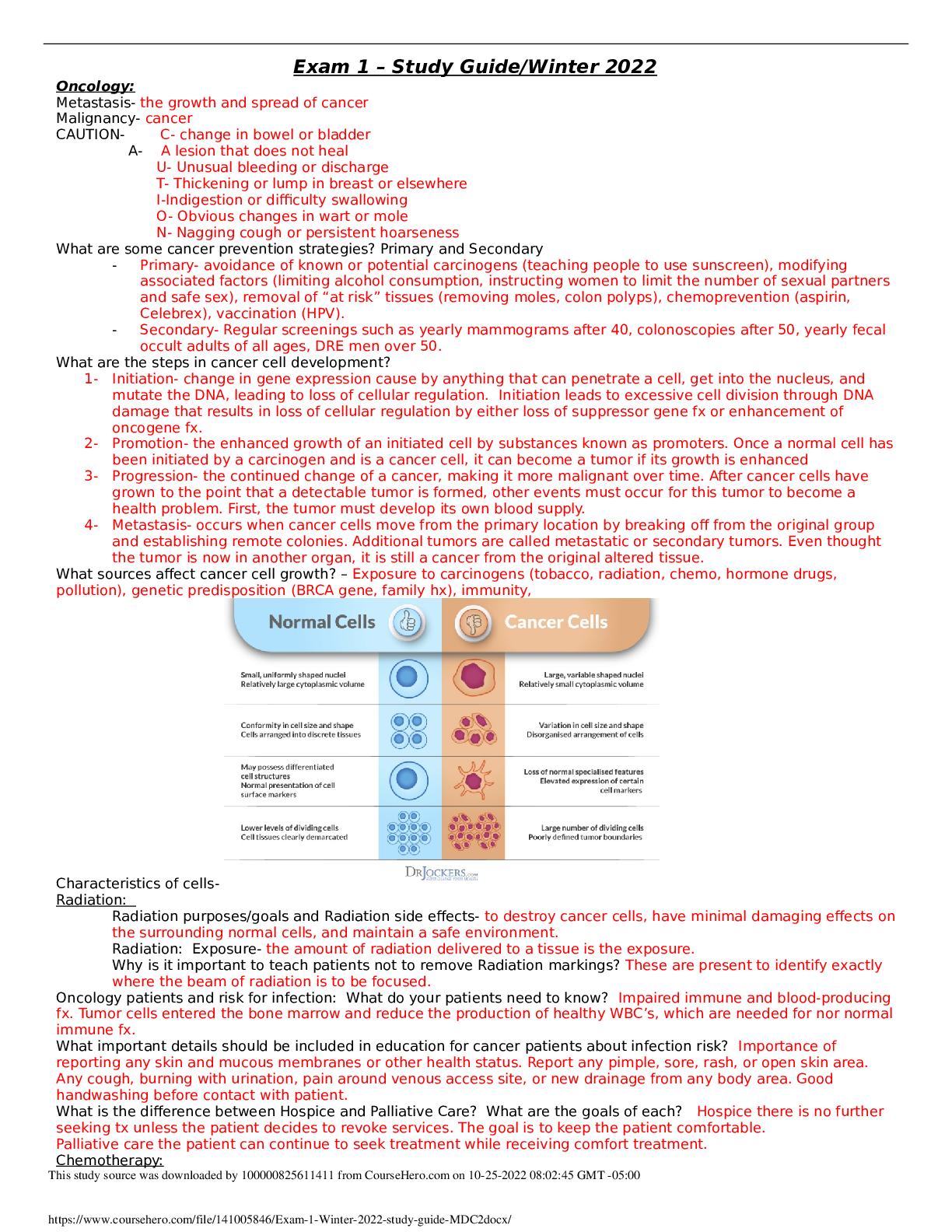
NR507 PATH FINAL EXAM STUDY GUIDE REPRODUCTIVE Endometrial cycle and occurrence of ovulation Manifestation of female reproductive functioning is menstrual bleeding, which starts with menarche (1st per... iod) and ends with menopause (cessation of menstrual flow for 1 year). Average age of menarche is 12 with a range of 9-17. Appears to be r/t body weight, especially body fat ratio. At first cycles are anovulatory and vary from 10-60 days or >. Then in adulthood range form 25-35 days. Length varies considerably. Cycle and regular ovulation are dependent on • The activity of gonadostat • Initial pituitary secretion of gonadotropin FSH • Estrogen positive feedback for the preovulatory FSH and LH surge, oocyte maturation, and corpus luteum formation and production of progesterone. The average menstrual cycle lasts 27 to 30 days and consists of three phases, which are named for ovarian and endometrial changes: the follicular/proliferative phase, the luteal/secretory phase, and the ischemic/menstrual phase. Phase 1-is the follicular phase in which begins on day one of one’s menstrual cycle. It lasts until about day 14. -In phase 1 the endometrium grows to form a lush lining inside of the uterus. Phase 2: Luteal phase-this is where the body secretes the hormones estrogen and progesterone. -These hormones work together to prepare the lining of the uterus for implantation. -This last for 12 days. Phase 3: Menstrual phase-The estrogen and progesterone start to decline and the endometrial lining begins to shed. This lasts for 3-5 days and the process restarts. Ovulation -Release of ovum -Present at the beginning of the luteal/secretory phase. -The ovarian follicle begins to transform into the corpus luteum. -Pulsatile secretion of the LH from the anterior pituitary stimulates the corpus luteum to secrete progesterone. -This will initiate the secretory phase of endometrial development. -Glands and blood vessels in the endometrium branch and curl through a functional layer, and the glands begin to secrete a thin glycogen-containing fluid= the secretory phase. *If conception occurs the nutrient-laden endometrium is ready for implantation. *The HCG hormone is secreted 3 days after fertilization by blastocytes and maintains the corpus luteum once implantation occurs at day 6 or 7. *HCG can be detected in maternal blood or urine about 8-10 days after ovulation. *Production of estrogen and progesterone continue until placenta can adequately maintain hormonal production. *Ovulatory cycles have a length of 24-26.5 days. *The primary ovarian follicle requires 10-12.5 days to develop. *The luteal phase appears at 14 days. Ovarian events of the menstrual cycle are controlled by gonadotropins. High FSH levels stimulate follicle and ovum maturation (follicular phase), then a surge of LH causes ovulation, which is followed by development of the corpus luteum (luteal phase). Ovarian hormones control the uterine (endometrial) events of the menstrual cycle. During the follicular/proliferative phase of the ovarian cycle, estrogen produced by the follicle causes the endometrium to proliferate (proliferative phase) and induces the LH surge and progesterone production in the granulosa layer. During the luteal/secretory phase, estrogen maintains the thickened endometrium, and progesterone causes it to develop blood vessels and secretory glands (secretory phase). As the corpus luteum degenerates, production of both hormones drops sharply, and the “starved” endometrium degenerates and sloughs off, causing menstruation, the ischemic/menstrual phase. Cyclic changes in hormone levels also cause thinning and thickening of the vaginal epithelium, thinning and thickening of cervical secretions, and changes in basal body temperature. Uterine Prolapse descent of cervix or entire uterus into vaginal canal. In severe cases the uterus falls completely through the vagina and protrudes from the introitus. Symptoms of other pelvic floor disorders may also be present. Tx depends on severity of symptoms and physical condition of woman. First line treatment is often a pessary- removable mechanical device that holds uterus in position. The pelvic fascia may be strengthened through kegels or by estrogen therapy in menopausal women. Healthy BMI, preventing constipation, and treating chronic cough may also help. Surgical repair with or without hysterectomy is the last resort. Page-771 fig 25.11 -Dropping of the cervix or the entire uterus into the vaginal canal. -In severe cases the uterus completely through the vagina and protrudes from the introitus. -Symptoms of other pelvic floor disorders may also be present. Symptoms: urinary-sensation of incomplete emptying of bladder, incontinence,frequency,bladder splinting to accomplish voiding. Bowel-constipation or feeling of rectal fullness, difficult defecation, stool or flatus incontinence. *Pain or bulging includes pelvic pressure, low back pain, and vagina, bladder or rectum bulging. *Sexual-decreased sensation, lubrication or arousal. -Dyspareunia Treatment: -Depends on age and severity. -Isometric exercise-strengthen the pubococcygeal muscle. KEGELS* -Estrogen-to improve tone and vascularity of fascial support POSTMENOPAUSAL* -Pessary—a removable device to hold pelvic organs in place. -Weight loss -Stool softeners to avoid constipation -tx of lung and cough conditions PCOS Polycystic ovary syndrome (PCOS) is a difficult syndrome to diagnose because several factors are involved. It is a syndrome in which at least two of the following are present: oligo-ovulation or anovulation, elevated levels of androgens, or clinical signs of hyperandrogenism and polycystic ovaries. Prolonged anovulation leads to infertility, menstrual bleeding disorders, hirsutism, acne, endometrial hyperplasia, cardiovascular disease, and diabetes mellitus in women with hyperinsulinemia. Presenting s/s: obesity, menstrual disturbance, oligomenorrhea, amenorrhea, regular menstruation, hyperandrogenism, infertility or they could be asymptomatic. Diagnosis of PCOS is based on evidence of androgen excess, chronic anovulation, and inappropriate gonadotropin secretion. Tests for impaired glucose tolerance are recommended. As stated, polycystic ovaries do noT have to be present and, conversely, their presence alone does not establish the diagnosis. Goals of treatment include reversing signs and symptoms of androgen excess, instituting cyclic menstruation, restoring fertility, and ameliorating any associated metabolic or endocrine, or both, disturbances. *Most common cause of anovulation and ovulatory dysfunction in women. *Leading cause of infertility and most common endocrine disturbance. *Mostly common in younger women *Usually has two/three of the following: irregular ovulation, elevated levels of androgens (testosterone), and the appearance of polycystic ovaries on ultrasound. *Polycystic ovaries do not need to be present to dx POS. *Thyroid dysfunction, hyperprolactinemia, and congenital adrenal hyperplasia must be ruled out first. *Associated with metabolic dysfunction, dyslipidemia, insulin resistance, and obesity. *Strong genetic component and possibly differentially inherited. *Difficult to diagnose as symptoms may change over time. *80% of women have one or more of the symptoms with normal ovaries. *More prominent sx as we age. *May be associated with Cushing’s syndrome, acromegaly, premature ovarian failure, obesity, congenital adrenal hyperplasia, thyroid disease and androgen producing adrenal tumors. Pathophysiology: *Underlying cause is unknown *Genetic involvement suggested because of steroid and androgen biosynthesis. *No single factor accounts for abnormalities of pcos. ***A HYPERANDROGENIC STATE IS A CARDINAL GEATURE IN THE PATHOGENSIS OF PCOS*** -3 X LIKELY TO HAVE INSULIN RESISTENCE. *Insulin stimulates androgen secretion by the ovarian stroma and reduces the serum sex hormone-binding globulin. * Free testosterone levels increase *Excessive androgens affect follicular growth and insulin affects follicular decline by suppressing apoptosis Decreased intraovarian receptors for estrogen receptor -a- or insulin like growth factor 1, increased leptin levels, or direct infrared redaction select ovarian cells. *Intrauterine and early child enviroment contribute to childhood development. *Weight gain aggravates symptoms and women will have an increased leptin level. *Leptin levels are increased in thin women as well *Leptin influences the hypothalamic pulsatility of GNRH and interaction with HPO. *Dysfunction in ovarian follicle development results from inappropriate gondatropin secretes and triggers the beginning of anovulation. *FSH is low and LH are high. *Persistent LH elevation causes an increase in androgens *DHEA (in adrenal glands and testosterone). And Androstenedione and dhea in the ovary. *Characterized by excessive levels of androgen and estrogen. -increased androgen contributes to a premature follicular failure (anovulation). -Persistent anovulation causes the pearly white smooth capsules (polycystic ovaries). -Thickening of the tunica, increased cortical stromal thickening, and hyperplasia. -**Women with PCOS 3 x greater of developing uterine cancer. Clinical Manifestations: *Appear within 2 years of puberty. *May not present until normal menstrual function or pregnancy. *Obese *Anovulation, hyperandrogenism, insulin resistance *infertility, hirsutism, acne, dysfunctional bleeding. *More likely to experience sleep apnea. Evaluation and Treatment: *dx is made based on androgen excess, chronic anovulation, and sonographic evidence of polycystic ovaries. *Must have 2 -3 of these. *Impaired glucose tolerance test is recommended *Goals are to suppress androgen, instituting menstruation, restore fertility, and reduce endocrine disturbance. **FIRST LINE TREATMENT= COMBINED ORAL CONTRACEPTIVES** -This helps to initiate regular menses. -Lifestyle modifications= exercise and weight loss. --Insulin resistance= metformin -If pregnancy is not desired- progesterone therapy is important to oppose estrogen effects on the endometrium to help monthly bleeding. **FOR OBESE WOMEN LIFESTYLE MODIFICATIONS ARE FIRST LINE** -CLOMIPHENE CITRATE CAN BE USED TO FACILITATE OVULATION* Testicular cancer & Risk factors Highly treatable, usually curable cancer most often develops in young and middle aged men. Rare, but most common form of cancer between young men 15-35. More common on R side than left. Germ cell tumors arising from male gametes: seminomans and nonseminomas. Seminomas are most common, least aggressive. Nonseminomas include embryonal carcinomas, teratomas, and choriocarcinomas, most aggressive but rare. Neoplasm cause is unknown. Genetic predisposition is suggested d/t incidence in brothers, identical twins and close male relatives. Risk factors: cryptochordism- neoplasms develop more commonly in contralateral testis. Abnormal testicular development, HIV and AIDS, Klinefelter syndrome, and hx of testicular cancer. Symptoms that require evaluation for Breast Cancer Clinical manifestation Pathophysiology Chest pain Metastasis to lung Dilated blood vessels Obstruction of venous return by fast growing tumor Dimpling of skin Can occur with invasion of dermal lymphatics because of retraction of cooper ligament Edeme of arm Local inflammation of lymphatic obstruction Hemorrhage Erosion of blood vessels Local pain Local obstruction by tumor Nipple/areolar eczema Paget disease Nipple discharge in a nonlactating woman Spontaneous and intermittent d/c caused by tumor obstruction Nipple retraction Shortening of mammary ducts Pitting of the skin Obstruction of subq lymphatics, resulting in fluid accumulation Reddened skin, local tenderness, warmth Inflammation Skin retraction Involvement of suspensory ligaments Ulceration Tumor necrosis Signs of premenstrual dysphoric disorder (PMDD) • The cyclic recurrence (in the luteal phase of the menstrual cycle) of distressing physical, physical, psychologic, or behavioral changes that impair interpersonal relationships or interfere with usual activities. • Neurotransmitters, GABA, and noradrenaline may have mediating or moderating roles on symptom manifestation. These neurotransmitters have demonstrated interactions with estrogen and progesterone and all of these are neuroactive with known mood and behavior effects, including negative mood, irritability, aggression, and impulse control. • Symptoms usually appear a week before menstruation and end a few days after your period starts. When this happens, some women have trouble functioning at home, at work and in relationships during this time. • Women show symptoms of irritability, nervousness, anger, insomnia, anxiety, paranoia, trouble sleeping, N&V, headaches, fainting. Dysfunctional uterine bleeding • DUB is heavy or irregular bleeding in the absence of organic disease, such as submucous fibroids, endometrial polyps, blood dyscrasias, pregnancy, infection, or systemic disease. • This accounts for 70% of all hysterectomies and almost all endometrial ablation procedures. • Caused by the lack of ovulation. Normal periods result in the complex interplay of the hypothalamus, the pituitary, the ovary, and the uterine endometrium. Disruptions in this system can affect the amount and structure of the uterine endometrium causing it to shed irregularly or heavily. • Occurs more in women ages 40-50 because they are at the end of their reproductive years and are more likely to ovulate irregularly. • PCOS can lead to irregular heavy uterine bleeding • The formation of the follicle and its rupture release an ovum which is a very important part of the menstrual cycle. As the follicles forms it produces estrogen. Following ovulations, the remain portions of the follicle, known as the corpus luteum, releases progesterone. Progesterone acts on the endometrium to limit growth and causes, which helps limit bleeding during endometrial shedding. • If a follicle forms but never releases in the ovum, the follicle may continue to produce estrogen which causes thickening of the endometrium. This causes the endometrium to be able to shed in a predictable fashion. Pathophysiology of prostate cancer • More than 95% of prostatic neoplasms are adenocarcinomas and most occur in the periphery of the prostate. Prostatic adenocarcinoma is a heterogenous group of tumors. • Estrogen receptor -a has shown evidence to participate in the pathogenesis of prostate cancer. • This ER-a receptor leads to inflammation, proliferation and development of premalignant lesions. ER-B leads to antiproliferative, anti-inflammatory, and potentially anticarcinogenic effect that tries to balance ER-a and the androgens involved. • Increased expression of ER-a has been shown to increase prostate cancer progression, metastasis. • The prostate glands require male hormones, known as androgens, to work properly. Androgens include testosterone, which is made in the testes, dehydroepiandrosterone, made in the adrenal glands; and dihydrotestosterone, which is converted from testosterone within the prostate itself. Androgens are also responsible for secondary sex characteristics such as facial hair and increased muscle mass. Prostate cancer is classified as an adenocarcinoma, or glandular cancer, that begins when normal semen- screening prostate gland cells mutate into cancer cells. The region of prostate gland where the adenocarcinoma is most common is the peripheral zone. Initially, small clumps of cancer cells remain confined to otherwise normal prostate glands, a condition known as carcinoma in situ or prostate intraepithelial neoplasia (PIN). Although there is no proof that PIN is a precursor, it is closely associated with cancer. Overtime, these cancer cells begin to multiply and spread to the surrounding prostate tissue (the stroma) forming a tumor. Eventually, the tumor may grow large enough to invade nearby organs such as the seminal vesicles, or the rectum, or the tumor cells may develop the ability to travel in the blood stream and lymphatic system HPV and development of cervical cancer • Cervical cancer is almost exclusively caused by cervical human papillomavirus (HPV) infection. • Infection with “high-risk” (oncogenic) types of HPV (predominately 16 and 18) is necessary precursor to development of precancerous cell changes, known as dysplasia of the cervix that leads to invasive cancer. • With these cell changes, they can be detected noninvasively through examination of the cervical cells. The cells can be destroyed to prevent cancer development if dysplasia can be detected early. • The line where two cell types meet, known as the transformation zone, is very vulnerable to oncogenic effects of HPV. In girls and young woman, a large portion of the cervix is covered with columnar epithelium, a condition called squamous metaplasia. As women age the transformation zone moves as the squamous epithelium covers the surface of the cervix. The younger the woman is when she contracts HPV, the more sensitive cervical cells are exposed. • Vaccinating against HPV early before the initiate of sexual activity is important • Normally, women can clear most HPV infections by the immune system. But some cannot which contributes to the develop of cervical cancer. ENDOCRINE NEURO Dermatomes genetic disorder in which fat and fibrous tissue infiltrate and weaken muscle tissues such as in the legs and pelvis, lungs, and heart; usually results in death before adulthood. - X-linked recessive disorder - 1 in 3500 males - Progressive muscle degeneration; affected individuals are unable to walk by the age 10 to 12 - Disease affects the heart and respiratory muscles, and death caused by respiratory or cardiac failure usually occurs before the age of 20 - Dystrophin: muscle protein o Dystrophin plays an important role in maintaining the structural integrity of muscle cells: one end of the protein binds to actin filaments in the cytoplasm of the cell, and other end binds to a group of membrane-spanning proteins known as dystrophin-associated glycoproteins o When Dystrophin is absent, as in individuals with DMD, the muscle cell cannot survive, and muscle deterioration ensues - Most cases of DMD is caused by deletions of portions of the DMD genes Neurofibromatosis Neurofibromatosis (NF) is an inherited autosomal dominant disorder accounting for 5% of all neuromas and is divided into two types: NF1 and NF2, which are clinically and genetically distinct disorders. The gene products are neurofibromin and merlin (schwannomin), both of which are thought to be tumor suppressors - Inherited autosomal dominant disorder accounting for 5% of all neuromas and is divided into two types: NF1 and NF2 - NF1 is associated with cutaneous manifestations, iris hamartomas, and tumors primarily involving the peripheral nervous systems and occasionally the CNS - NF2 is associated with cataracts, hearing loss, and tumors primarily in the CNS; most commonly vestibular schwannoma and meningioma - The tumors most commonly affect people older than 50, women more than men - The tumor originates most commonly just distal to the junction between the nerve roots and the brainstem o As the tumor grows, it extends into he posterior fossa to occupy the cerebropontine angle and compress adjacent nerves o Eventually, the brainstem is displaced, and the CSF flow is obstructed - Clinical manifestations: headache, tinnitus, hearing loss, impaired balance, unsteady gait, facial pain, and loss of facial sensations o Later, vertigo with nausea, vomiting, a sense of pressure in the ear, and moderate to severe unsteadiness with rapid position changes may appear - CT or MRI help diagnose o Posterior fossa dye studies maybe required - Treatment o Surgical excision o Radiotherapy of the neuroma nce of calcium, both of these proteins are attracted to calcium ions, leaving actin free to bind with myosin. Contraction begins as the calcium ions combine with troponin, a reaction that overcomes the inhibitory function of the troponin-tropomyosin system (troponin is attached to the protein tropomyosin and lies within the groove between actin filaments in muscle tissue. In a relaxed muscle, tropomyosin blocks the attachment site for the myosin crossbridge, preventing contraction). The thin filament actin then slides toward the thick filament myosin. The two ends of the myofibril shorten after contraction when the myosin heads attach to the actin molecules, forming a cross-bridge that constitutes an actin-myosin complex. ATP, located on the actin-myosin complex, is released when the cross-bridges attach. *the useful distance of contraction of a skeletal muscle is approximately 25-35% of the muscles length. The last step, Relaxation, begins as the sarcoplasmic reticulum absorbs the calcium molecules, removing them from interaction with troponin. Calcium is pumped back into the sarcoplasmic reticulum by means of an active transport process. The cross-bridges detach, and the sarcomere lengthens. Growth of long bones in children: 1592 Long bones of the body include: clavicles, humeri, radii, ulnae, metacarpals, femurs, tibiae, fibulae, metatarsals, and phalanges. Endochondral formation of bone is the development of new bone from cartilage. First, mesenchymal tissue forms a cartilage anlage, **the ilium, ischium and pubis together form a deep socket called acetabulum which articulates with the head of the femur Lower Extremities – total of 60 bones Femur (2) – only long bone of the thigh, heaviest and strongest bone in the body. Proximal end has ball like head (greater trochanter) that fits into the acetabulum of the coxal (hip) bone. Patella (2) – (kneecap) small, freestanding bone that rests between the femur and tibia. Femur has a dedicated groove which the kneecap slides. Tibia (2) – (shinbone) is the larger, medial bone of lower leg. Anterior surface forms an anterior border that can be easily felt, distally there is a process called the medial malleolus that forms the inner bulge of the ankle. Fibula (2) – long, slender bone lateral to the tibia. Distal part forms the lateral malleolus (outer part of ankle) Tarsals (14) – 2 notable tarsal bones are the calcaneus (heel bone), and the talus which articulates with the tibia to form hinge-like ankle joint Metatarsals (10) - form the sole of the foot Phalanges (28) – similar to phalanges of hand, great toe, like thumb, has only two phalanges. IMMUNITY How vaccines are performed – A vaccine is a biological preparation that provides active acquired immunity to a particular disease. A vaccine typically contains an agent that resembles a disease-causing microorganism and is often made from weakened or killed forms of the microbe, its toxins, or one of its surface proteins. Vaccines are like a training course for the immune system. They prepare the body to fight disease without exposing it to disease symptoms. When foreign invaders such as bacteria or viruses enter the body, immune cells called lymphocytes respond by producing antibodies, which are protein molecules. Antigens are present in extremely small quantities to elicit an immune response through a vaccine. The most common routes of administration are intravenous, intraperitoneal, subcutaneous, intranasal, and oral. Each route stimulates a different reside). Desensitization therapy Also known as allergen Immunotherapy. This is where minute quantities of the allergen are injected in increasing doses over a prolonged period. The therapy may reduce the severity of the allergic reaction in the treated individual. This therapy is associated with a risk of systemic anaphylaxis, which can be life threatening. This approach works best for routine respiratory allergies and biting insect allergies (80-90% rate of desensitization over 5 years of treatment). The mechanisms by which desensitization occurs may be several, one of which is the production of large amounts os so called blocking antibodies, usually circulating IgG. A blocking antibody presumably competes in the tissues or in the circulation for binding with antigenic determinants on the allergen so the allergen is “neutralized” and is unable to bind with IgE on the mast cells. Desensitization injections may also stimulate the generation of clones of T- regulatory lymphocytes which inhibit hypersensitivity by suppressing the production of IgE and anti-inflammatory cytokines. Cells involved in the “left shift” in the WBC count differential -Neutrophil left shift and white blood cell (WBC) count are routine laboratory tests used to assess neutrophil state, which depends on supply from the bone marrow and consumption in the tissues Early in the response to infection or inflammation, immature forms of neutrophils will be seen. These are call Stab or Band cells. The presence of these immature cells is called a "shift to the left" and can be the earliest sign of a WBC response, even before the WBC becomes elevated. Forms of Immunity -Innate, native- natural immunity (non-specific)- First line - physical, mechanical and biochemical barriers. Epithelial barrier and inflammation confer innate resistance and protection. Skin, mucous membranes, stomach acid, oils on skin (Barriers). Second line - The inflammatory response (redness, swelling, heat and pain). Cells involved in the inflammatory response are Phagocytes (WBC- DERMATOLOGY Process by which a deep pressure ulcer heals: Most significant cause is constant pressure that interrupts arterial and venous blood flow to and from the skin or deeper tissue. Healing requires continued relief of pressure, debridement of dead tissue, wound care products (dressings…), and repair with skin flaps for large/deep ulcers. Antibiotic treatment for infection. Stage I & II pressure ulcers and partial thickness wounds heal by tissue regeneration. Stage III & IV pressure ulcers and full thickness wounds heal by scar formation and contraction Phases of wound healing: Inflammatory-Proliferation-Maturation Inflammatory phase: 0 – 3 days • Hemostasis (bleeding stops) • Inflammation (redness, swelling, warmth and pain maybe present) • Phagocytosis (WBC’s engulf bacteria and foreign debris) • Growth factor stimulation stimulation Proliferation Phase: 3 – 21 days • Angiogenesis (new blood vessels develop) • Collagen synthesis (protein fibers) • Granulation formation • Epithelialization • Contraction Maturation Phase: 21 days – 2 years • Reorganization of collagen • Tensile strength improves (up to 80% of original) Complications of the development of contractures during wound healing: Contractures can form during wound healing due to an exaggeration of normal wound edge contraction forming deformities (more CARDIOVASCULAR Most common cardiac valve disease in women Defects in normal secretion of natriuretic hormones & impact on renal system; pg 1134 • Natriuretic hormones modulate renal sodium (Na ) excretion and require adequate potassium, calcium, and magnesium to function properly. • Natriuretic hormones include atrial natriuretic peptide (ANP), brain natriuretic peptide (BNP), C- type natriuretic peptide (CNP), and urodilatin. • These hormones induce diuresis; enhancement of renal blood flow and glomerular filtration rate, systemic vasodilation, and suppression of aldosterone, and inhibition of SNS. • Dysfunction of these hormones, along with alterations in the RAA system and the SNS cause an increase in vascular tone and a shift in the pressure natriuresis relationship. • When there is inadequate natriuretic function, serum levels of natriuretic peptides are increased. In hypertension, increased ANP and BNP levels are linked to an increased risk for ventricular hypertrophy, atherosclerosis, and heart failure. Salt retention leads to water retention and increased blood volume which leads to increased BP. Effects of increased sympathetic nervous system activity due to primary HTN; pg 1133 • The SNS contributes to the pathogenesis of hypertension in many people. • In a healthy individual, the SNS contributes to the maintenance of adequate blood pressure and tissue prefusion by promoting cardiac contractility and heart rate (maintenance of adequate cardiac output) and by inducing arteriolar vasoconstriction (maintenance of adequate peripheral resistance) • in patients with hypertension, overactivity of SNS can result from increased production of catecholamines (epi and norepi) or from increased receptor reactivity involving these neurotransmitters. • Increased SNS activity cause increased HR and systemic vasoconstriction thus raising BP. Complications of unstable plaque in the coronary arteries: CAD (buildup of plaque), leads to stable angina (on exertion and then resolves on rest) angina pectoris (strangling/tightening of heart muscle when there’s a lack of o2), acute coronary syndrome (unstable angina and MI). Unstable angina causes chest pain at rest. MI is the death of a part of the heart muscle. An MI or unstable angina are caused by rupture or erosion of a plaque with subsequent thrombus formation and occlusion of the artery. The most common cause of obstruction is atherosclerosis (ACS) Forms of dyslipidemia associated with the development of the fatty streak in atherosclerosis: High systemic vascular pressure LV contraction force ( afterload) LV unable to eject normal amount of blood LV preload (amount of blood remaining) LA unable to eject normal amount of blood LA preload (amount of blood remaining in LA) blood volume pressure in pulmonary veins fluid forced out into pulmonary tissues pulmonary edema dyspnea Rt HF= biventricular HF Right HF (Cor Pulmonale) o Inability of RV to provide enough adequate blood flow into pulmonary circulation o Cause: Pulmonary disease, Pulmonary HTN (most common), RV MI, RV hypertrophy, Pulmonary SLV or tricuspid valve damage, 2ndary to Lt HF RV MI- results in weakening of muscle RV hypertrophy- 2ndary to cardiac damage Pulmonary SLV or tricuspid valve damage- causing backflow of blood into RA or RV after ejection 2ndary to Lt HF- from buildup of pressure in damaged left ventricle o Disease Process High Pulmonary vascular resistance RV contraction force ( afterload) RV unable to empty completely PERIPHERAL VASCULAR DISEASE Peripheral vascular disease: Narrowing, blockage or spasming of veins and arteries. It can be difficult to differentiate PVD from Peripheral Arterial Disease (PAD). Consider what symptoms and problems are experienced as a result of an arterial occlusion as opposed to a venous occlusion. It is helpful to consider the five P’s when assessing these types of disorders: 1) Pallor (pale skin) 2) pain 3) pulselessness 4) paresthesia’s (pins and needles) 5) paralysis Types of PVD: Thromboangiitis obliterans (Buerger disease) is an inflammatory disease of the peripheral arteries. Raynaud phenomenon and Raynaud disease are characterized by attacks of vasospasm in the small arteries and arterioles of the fingers and, less commonly, the toes. Atherosclerosis is a form of arteriosclerosis in which thickening and hardening of the vessel are caused by the accumulation of lipid-laden macrophages within the arterial wall, which leads to the formation of a lesion called a plaque. Deep Vein Thrombosis pathophysiology DVTs are formed when platelets, fibrin mesh and RBCs clump together in the veins (most often near a valve) via the coagulation cascade to form a thrombus. Inflammation around the thrombus promotes further platelet aggregation and the thrombus propagates or grows proximally. Blood clot or thrombus in a deep vein, usually of the leg. Accumulation of clotting factors and platelets leads to thrombus formation in the vein, often near a venous valve. Inflammation around the thrombus promotes further platelet aggregation and the thrombus propagates or grows proximally. This inflammation may cause local symptoms, but because the vein is deep in the leg it is usually not accompanied by clinical symptoms or signs. If the thrombus creates significant obstruction to venous blood flow, increased pressure in the vein behind the clot may lead to edema of the extremity. Vichow’s traid: The etiology of a blood clot (venous thrombus) Hypoxemia, reduced oxygen levels in the blood, further contributes to cardiovascular dysfunction by causing dilations of arterioles, capillaries, and venules, thus leading to decreased vascular resistance and increased flow. Increased peripheral blood flow and venous return further contribute to an increase in heart rate and stroke volume in a continuing effort to meet normal oxygen demand and prevent cardiopulmonary congestion. These compensatory mechanisms may lead to heart failure. Populations at highest risk for developing folate deficiency anemia Humans are totally dependent on dietary intake meet the daily requirement of 50-200mcg/day. Increased amounts are required for pregnancy and lactating females. Folate deficiency is more common than B12 deficiency, particularly in alcoholics and individuals with chronic malnourishment. Alcohol interferes with folate metabolism in the liver, causing a profound depletion of folate stores. Fad diets and diets low in vegetables also may cause folate deficiency because of the absence of plant sources of folate. Cause of Iron Deficiency Anemia Iron deficiency Anemia can arise from one of two different etiologies or a combination of both- inadequate dietary intake or excessive blood loss. In both instances there is no intrinsic dysfunction in iron metabolism; however, both deplete iron stores and reduce hemoglobin synthesis. A second category is a metabolic or functional iron deficiency in which various metabolic disorders lead to either insufficient iron delivery to bone marrow or impaired iron use within the marrow. Paradoxically, iron stores may be sufficiency but delivery is inadequate to maintain heme synthesis, thus producing a functional or relative iron deficiency. The most common cause of IDA in developed countries is pregnancy and chronic blood loss. Blood loss of 2-4 ml/day (1-2 mg of iron) is sufficient to cause iron deficiency and may results in erosive esophagitis, gastric and duodenal ulcers, colon adenomas, or cancers. H. pylori infections also have been found to cause IDA of unknown origin, although H. pylori impairs iron uptake. In females, menorrhagia is a common cause of primary IDA. Other causes of IDA for both genders are 1. Use of medication that cause GI bleeding such as aspirin or NSAIDS 2. Surgical procedures that decrease stomach acidity, intestinal transit time, and absorptions such as with gastric bypass 3. Insufficient dietary intake of iron 4. Eating disorders, such as pica, which is the craving and eating of non-nutritional substances, such as dirt, chalk, and paper. Expected lab test results found in long standing Iron Deficiency Anemia Symptoms of IDA begin gradually, and individuals usually do not seek medical attention until hemoglobin level have decrease to 7-8 g/dl. Other lab values include: Hemoglobin – low, Hematocrit – low, Reticulocyte – Normal or slightly high or low, Mean corpuscular volume – low, Plasma iron – low, Total iron-binding capacity – high, Ferritin – low, Serum B12 – Normal, Folate – Normal, Bilirubin – Normal, Free erythrocyte protoporphyrin – High, Transferrin - Low Sickle Cell Anemia -Sickle cell anemia is an inherited (autosomal recessive) disorder of erythrocytes -300 million people are affected by a hemoglobinopathies (sickle cell or Thalassemia) -genes involved: Alpha=chromosome 16 Beta= chromosome 11 - -oxidative stress (hypoxia)--------------------- * All of these factors further decrease o2 -anxiety---------------------------------------------- from binding to hemoglobin and -fever----------------------------------------------- increases sickling tendencies of -Temp-cold--------------------------------------- hemoglobin. -dehydration--------------------------------------- Aplastic Anemia -Aplastic= without plasia/cell growth -Impaired RBC production -Considered a Normocytic-Normochromic Anemia Normocytic=normal cell size, Normochromic=Normal color (hgb) -Since the size and color (hgb) are normal in aplastic anemia, the problem is the decrease in the number of cells. Causes: cells -Considered a Normocytic-Normochromic Anemia Normocytic=normal cell size, Normochromic=normal color (hgb) Causes -infection *E.coli -transfusion reaction -hemolytic disease of newborn *RH compatibility -autoimmune reaction *congenital, idiopathic -drug induced *drugs auto oxidize (self-destruct) Pathophysiology Premature destruction of RBC’s due to enzymes/toxins produced by infectious agents, mediated by own immune system or the effects of certain chemicals/drugs. *Circulating blood has vit.C and RBC’s that contains glutathione=natural antioxidant to help protect cells. c renal failure FLUIDS & ELECTROLYTES Conditions that result in pure water deficit (hypertonic volume depleted) Hypertonic With fluid loss there is a blood volume and blood pressure decrease. Baroreceptors (volume/pressure sensitive receptors) located in the R/L atria, large veins, aorta, pulmonary arteries and carotid sinus also stimulate the release of ADH. When the arterial and atrial pressure drops baroreceptors signal the hypothalamus to release ADH. ADH also stimulates arterial vasoconstriction. Causes of hypernatremia Hypernatremia (sodium levels >147 mEq/L) may be caused by an acute increase in sodium level or a loss of water (most common cause). Some specific causes of hypernatremia from water loss include fever, respiratory tract infections (that increase respiratory rate and enhance water loss from the lungs), diabetes insipidus (deficiency of ADH), polyuria, profuse sweating, diarrhea. Insufficient water intake causes include individuals who are comatose or receiving gastric feedings and infants who can’t communicate thirst. Other causes of increased sodium retention are inappropriate administration of hypertonic saline solution, over secretion of aldosterone (hyperaldosteronism) and Cushing syndrome (excess secretion of adrenocorticotropic hormone (ACTH) which increases secretion of aldosterone). High amounts of dietary sodium rarely cause hypernatremia because healthy kidneys will eliminate excess sodium. Hypernatremia can cause thirst, dry mucous membranes, hypotension or hypertension (depending on cause of hypernatremia), tachycardia, pulmonary edema, confusion and convulsions. Treatment of hypernatremia is with an isotonic salt-free fluid (5% dextrose in water) and must be given slowly to prevent cerebral edema. -Isotonic conditions occur when the osmolality in the ICF and ECF are equal. -Normal fluid movement favors isotonic conditions. -Examples of isotonic solutions: 5% dextrose in water and normal (0.9%) saline solution Principle of capillary oncotic pressure -Capillary (plasma) oncotic pressure osmotically attracts water from the interstitial space back into the capillary. -Oncotic (colloid) pressure (OCP) - chemical force exerted by large molecules (e.g. – proteins/albumin) to pull fluid in = reabsorption -The movement of fluid back and forth across the capillary wall is called net filtration and is best described by the Starling hypothesis: -Net filtration= (Forces favoring filtration)- (Forces opposing filtration) -Forces favoring filtration= Capillary hydrostatic pressure and interstitial oncotic pressure -Forces opposing filtration= Capillary oncotic pressure and interstitial hydrostatic pressure Types of fluid compartments in • EDISPOSING FACTORS: Increased risk for thrombosis associated with hemodynamic stasis, hypercoagulability, and endothelial injury is known as Virchow’s triad Risk Factors include: • Venous Stasis: immobilization, heart failure • Hypercoagulability: inherited coagulation disorders, malignancy, hormone replacement, oral contraceptives, pregnancy • Endothelial injury: trauma, caustic intravenous infusion Prevention measures: • Venous stasis in hospitalized individuals is minimized by bed exercises, frequent position changes, early ambulation, and pneumatic calf compression. • prophylactic anticoagulation with unfractionated heparin, low-molecular-weight heparin, warfarin, or fondaparinux. • In individuals who have contraindications to anticoagulation, the placement of a filter in the inferior vena cava can prevent emboli from reaching the lungs. Risk factor recognition and elimination of predisposing factors. Most at-risk individuals also will receive prophylactic anticoagulation with unfractionated heparin, low-molecular-weight heparin, warfarin, or fondaparinux. In individuals who have contraindications to anticoagulation, the placement of a filter in the inferior vena cava can prevent emboli from reaching the lungs. Increased risk for thrombosis associated with hemodynamic stasis, hypercoagulability, and endothelial injury is known as Virchow’s triad144 (see Chapter 32). The ideal treatment of PE is prevention through risk factor recognition and elimination of predisposing factors. Venous stasis in hospitalized individuals is minimized by bed exercises, frequent position changes, early ambulation, and pneumatic calf compression.155 Most at-risk individuals also will receive prophylactic anticoagulation with unfractionated heparin, low-molecular-weight heparin, warfarin, or fondaparinux.156 In individuals who have contraindications to anticoagulation, the placement of a filter in the inferior vena cava can prevent emboli from reaching the lungs.157 when the practitioner will note tactile fremitus * increased with pneumonia because of the density o Tactile Fremitus: Normal lung transmits a palpable vibratory sensation to the chest wall = fremitus Detected by placing the ulnar aspects of both hangs firmly against either side of the chest while the patient says “Ninety-Nine” Repeated o e caused by a rupture in the visceral pleura or the parietal pleura and chest wall o Diagnosed with chest radiographs, ultrasound, and CT. o Types Primary (Spontaneous) Pneumothorax • Often caused by spontaneous rupture of blebs Secondary (Traumatic) Pneumothorax • Caused by chest trauma (rib fracture, stab, bullet) Iatrogenic Pneumothorax • Commonly caused by transthoracic needle aspiration o Spontaneous or Traumatic and present as open or tension Open Pneumothorax (Communicating pneumothorax) • Air pressure in the pleural space equals barometric pressure because air that is drawn into the pleural space during inspiration is forced back out during expiration Tension Pneumothorax • Site of pleural rupture acts as a one-way valve, permitting air to enter on inspiration, but prevents air escape by closing during expiration Pneumothorax is the presence of air or gas in the pleural space caused by a rupture in the visceral pleura (which surrounds the lungs) or the parietal pleura and chest wall. As air separates the visceral and parietal pleurae, it destroys the negative pressure of the pleural space. This disrupts the state of equilibrium that normally exists between elastic recoil forces of the lung and chest wall. No longer held in check by the recoil forces of the chest wall, the lung fulfills its tendency to recoil by collapsing toward the hilum. lung, and hypotension (low blood pressure) Results of the loss of alph-1- antitrypsin in emphysema Primary emphysema, which accounts for 1% to 3% of all cases of emphysema, is commonly linked to an inherited deficiency of the enzyme α1-antitrypsin.94 Normally α1-antitrypsin inhibits the action of many proteolytic enzymes (enzymes that break down proteins). Individuals who have α1-antitrypsin deficiency (an autosomal recessive trait) have an increased likelihood of developing emphysema, because proteolysis in lung tissues is not inhibited. Homozygous individuals have a 70% to 80% likelihood of developing lung disease. (Mechanisms of genetic inheritance are described in Chapter 4.) Persons with α1-antitrypsin deficiency who smoke are even more susceptible to emphysema than those with the deficiency alone. α1-Antitrypsin deficiency is suggested in nonsmokers and individuals who develop emphysema before age 40 years (or in their early forties). of surfactant, which is necessary to reduce surface tension in the alveoli and thus prevent lung collapse during expiration. Surfactant impairment can occur because of premature birth, acute respiratory distress syndrome, anesthesia, or mechanical ventilation. As the alveoli increase in size, the surfactant becomes more spread out over the surface of the liquid. This increases surface tension effectively slowing the rate of expansion of the alveoli. Surfactant reduces surface tension more readily when the alveoli are smaller because the surfactant is more concentrated. When there is not enough surfactant the tiny alveoli collapse with each breath, and as they collapse damaged cells collect in the airway causing further affect in breathing. Characteristics of Cheyne-Stokes respirations Alternating periods of deep and shallow breathing. Apnea lasting 15 to 60 seconds is followed by ventilations that increase in volume until a peak is reached, after which ventilation (tidal volume) decreases again to apnea. Cheyne-Stokes respirations result from any condition that slows the blood flow to the brainstem, which in turn slows impulses sending information to the respiratory centers of the brainstem. Neurologic impairment above the brainstem is also a contributing factor. Usually seen in comatose individuals having disease nervous centers respirations. SHOCK Causes of hypovolemic shock (7th Edition, pg. 1672-3) Hypovolemic shock is caused by NR 507 Week Five Quiz Study Guide 1. What controls the direct stimulation of the insulin-secreting cells? Neural; Direct stimulation of 2. Types of protein hormones 3. Assessing patients for elevated thyroxine production 4. Direct effect of insulin binding to receptors 5. Lipid-soluble hormone receptors crossing plasma membrane 6. Effects of the removal of the posterior pituitary 7. Insulin regulation 8. Hormone-secreting tumor of the pancreas—what would increase? 9. The effect of insulin on electrolytes 10. Hormonal regulation involved in child birth and stopping uterine bleeding? Types of immunity-e.g. innate, active, etc . I.e. maternal, immunotherapy. Temporary! Alveolar ventilation/perfusion- Dermatologic conditions e.g. pityriasis rosea Folliculitis Initial lesions: firm, red spots that enlarge/coalesce into clearly circumscribed, advancing edge, bright red, hot lesion with raised border. Vesicles may appear over lesion and at the border, producing a bullous form of the disease. Itching, burning and tenderness. Tx: Cold compresses, systemic antibiotics Croup Croup illnesses can be divided into 2 categories: all characterized by infection and upper airway obstruction: 1) acute laryngotracheobronchitis 2) spasmodic Laryngotracheobronchitis: Most common in children 6month-3years (peak 2 years) 85% cases caused by virus: parainfluenza most common, but also influenza A, RSV, rhinovirus, adenovirus and rubella (measles) as well as atypical bacterium (Mycoplasma pneumonia). Spasmodic croup: characterized by hoarseness, barking cough/stridor with sudden onset @ night Etiology unknown but often associated w/ viruses, allergies, asthma, GERD Patho: subglottic edema from the infection. The subglottic mucous membranes are looser than those of the larynx, which allows for mucosal and submucosal edema between the membranes and underlying cartilage. OF NOTE: the cricoid cartilage is the narrowest point of the airway so swelling in this area is critical. Increased airflow resistance leads to increased work of breathing, which generates more nebulized racemic epinephrine, which stimulates the alpha and beta-adrenergic receptors, which decreases airway secretions and mucosal edema. This is a temporary fix until steroids kick in. Heliox (helium-oxygen mixture of 80:20 or 70:30) may be used for severe cases but evidence remains lacking. Types of anemia Commonly result from: 1) Impaired erythrocyte production 2) Blood loss (acute or chronic) 3) Increased erythrocyte destruction 4) Combination of the above 3 Macrocytic-normochromic anemias: Large, abnormally shaped erythrocytes BUT normal hemoglobin concentrations Pernicious Anemia: Lack of B12 for erythropoiesis, abnormal DNA/RNA synthesis in erythroblast = premature cell death. Cause: congenital or acquired deficiency of intrinsic factor (IF), genetic disorder of DNA synthesis) S/Sx: early symptoms often vague (infection, mood swings, GI/cardiac/kidney ailments), later symptoms: nerve damage, confusion, dementia, memory loss, depression, nausea, heartburn, weight loss, smooth beefy tongue. Folate Deficiency Anemia: lack of folate for erythropoiesis premature cell death. Cause: dietary folate deficiency. S/SX: irritability, diarrhea and smooth tongue Microcytic-hypochromic anemias: Causes: Small, abnormally shaped erythrocytes AND reduced hemoglobin concentrations Iron Deficiency Anemia: lack of iron for hemoglobin production. Cause: chronic blood loss, dietary iron deficiency, disruption of iron metabolism or iron cycle. S/Sx: unusual cravings (ice, dirt), brittle nails, swollen/sore tongue, tiny cracks on side of mouth, frequent infections Sideroblastic Anemia: dysfunctional iron uptake by erythroblasts and defective porphyrin and heme synthesis. Cause: congenital dysfunction of iron metabolism in erythroblasts, acquired dysfunction of iron metabolism 2/2 drugs/toxins Thalassemia: impaired synthesis of (alpha/beta) chain of hemoglobin A, phagocytosis of abnormal erythroblasts in the marrow. Cause: congenital defect of globin synthesis Normocytic-normochromic Anemias: Normal size and normal hemoglobin concentrations Aplastic anemia: insufficient erythropoiesis. Cause: depressed stem cell proliferation resulting in bone marrow aplasia. S/SX: nausea and skin rashes Posthemorrhagic anemia: blood loss. Cause: acute/chronic hemorrhage that stimulates increased erythropoiesis, which depletes body iron. Hemolytic anemia: premature lysis of mature erythrocytes in circulation. Cause: increased fragility of erythrocytes. S/Sx: jaundice, leg ulcers and abdominal pain Anemia of chronic disease: abnormal increase in demand for new erythrocytes. Cause: chronic infection/inflammation or malignancy. Sickle cell anemia: abnormal hemoglobin synthesis, abnormal cell shape with susceptibility to damage, lysis and phagocytosis. Cause: congenital dysfunction of hemoglobin synthesis. S/Sx: Edema in hands/feet, damage to spleen Mnemonic for different types of anemia- Microcytic Anemia = TICS - Thalassemia, iron deficiency, chronic disease, sideroblastic anemia Normocytic Anemia = ABBRA - Anemia of chronic disease, bone marrow infiltration, bone marrow failure, renal failure, acute hemorrhage Macrocytic Anemia = BALD HAIR - B12/B9 deficiency, alcohol, liver disease, drugs (eg. phenytoin), hypothyroidism, aplastic anemia & myelodysplasia, increased reticulocytes The inflammatory process upon injury Inflammation occurs in vascularized tissue and when activated results in: redness, heat, swelling and pain. The purpose of the inflammatory process is: 1) To wall off intruder / prevent further infection 2) Acts to destroy and remove intruder 3) Stimulates/enhances further immune response 4) Promotes healing/repair Influx of fluid to dilute toxins produced by bacteria and dying cells, influx/activation of plasma protein systems (i.e. complement system, clotting system) and influx of cells (i.e. neutrophils, macrophages) that destroy cellular debris/infectious agents. The byproducts of cellular debris/infectious agents are removed vie channels through the epithelium or drainage by lymphatic vessels. On injury, acute inflammation has 2 parts: 1) Vascular response 2) WBC response Immediately one of the PRR’s (pattern-recognition receptors) recognizes a PAMP or DAMP and release inflammatory mediators, which is what causes the classic signs of inflammation. Redness / Heat: vasodilation of local arterioles, etc. Edema: increased permeability of vessels that cause plasma proteins/fluids to leak into tissue Pain: some of the released mediators (i.e. bradykinin) increase sensitivity to pain How does all this happen? Injury/Infection triggers mast cells to degranulate and release histamine, which causes immediate vascular response. Large vessels constrict which increases flow to capillaries Small vessels dilate and epithelial cells retract which increases permeability. Mast cells release other chemotactic factors that act as signals to recruit other types of WBCs to area to amplify inflammatory response. Mast cells have enzymes that allow them to synthesize other mediators, such as leukotrienes and prostaglandins GI symptoms resulting in heart burn Pulmonary terminology such as dyspnea, orthopnea, etc Dyspnea = difficult or labored breathing. AKA breathless, air hunger, SOB, increased work of breathing, chest tightness. Orthopnea = discomfort in breathing when lying down flat. Basically dyspnea that occurs when patient lies flat. Common in heart failure, lung disease, pulmonary edema, sleep apnea, COPD and valvular disease. Complications of gastric resection surgery Caused by changes in motor and control functions of the stomach and upper small intestine after gastric resection. Malabsorption Syndromes Interfere w/ nutrient absorption Classified as: maldigestion – failure of the chemical process of digestion to take place in the intestinal lumen or at the brush border of the intestinal mucosa of the small intestine. Usually caused by deficiencies of enzymes such as pancreatic lipase or intestinal lactase. Also, inadequate secretion of bile salts and inadequate reabsorption of bile in ileum. Malabsorption – failure of the mucosa to absorb (transport) the digested nutrients. As a result of mucosal disruption caused by gastric/intestinal resection, vascular disorders or intestinal disease. Dumping Syndrome The rapid emptying of hypertonic chyme into small intestine 10-20 minutes after eating. Factors that influence: loss of gastric capacity, loss of emptying control when pylorus removed and loss of feedback control by duodenum when removed. The rapid gastric emptying and creation of a nonphysiologic, high osmotic gradient within small intestines = sudden shift of fluid from vascular compartment to intestinal lumen. Plasma volume decreases = vasomotor response like tachycardia, hypotension, weakness, pallor, sweating and dizziness. Rapid intestinal distention = epigastric fullness, cramping, N/V. Diarrhea can either be frequent and persistent or intermittent, precipitous and unpredictable. Late dumping syndrome = 1-3 hours after meal. High carb meal causes hypoglycemia 2/2 increase in insulin secretion stimulated by hyperglycemia that follows large meal. Frequent, small meals that are high protein and low carb. Drink fluid between meals instead of with meals. Recline on left side after eating. Dermatology terminology-macules, nevi, etc Lesions: Primary Macule = (freckles, flat moles, petechiae, measles) flat, circumscribed area that is a change in color of skin. Papule = (wart, lichen planus, fibroma, insect bite) elevated, firm circumscribed area Patch = (vitiligo, port-wine stain, mongolion spot)- flat, non-palpable, irregular Plaque = (psoriasis, seborrheic/actinic keratosis)- elevated, firm, rough, flat top surface Wheal = (uritcaria, allergic reaction)- elevated, irregular shaped area of cutaneous edema, solid, transient Nodule = (erythema nodosum, lipomas)- elevated, firm circumscribed deeper lesion. Tumor = (neoplasms, lipoma, neurofibroma, hemangioma)- elevated, solid lesion, may be clearly demarcated, deeper. Vesicle = (chickenpox, shingles, herpes simplex)- elevated, circumscribed, superficial and does not extend into dermis Bulla = (blister, pemphigus vulgaris) Pustule = (impetigo, acne) Cyst = (sebaceous cyst, cystic acne) Telangiectasia = 2/2 capillary dilation (acne rosacea, venous HTN, systemic sclerosis or birthmarks) Nevi- mole are benign, pigmented lesions that form melanocytes beginning at age three. Secondary Scale = seborrheic dermatitis post-scarlet fever or drug reaction, dry skin Lichenification = chronic dermatitis Keloid Scar Excoriation = abrasion/scratch, scabies- loss of epidermis, linear, hollowed out, crusted area. Fissure = athlete’s foot, cracks @ corner of mouth, anal fissure, dermatitis- linear crack or break from epidermis to dermis-may be moist or dry Erosion = chemical injury- partial loss of epidermis; depressed, moist, flistening, follows rupure of a vesicle or bulla or chemical injury Ulcer = pressure ulcer, stasis ulcer- concave loss of epidermis and dermis Atrophy = ages skin, striae- Thinning of skin surface. Cutaneous Vasculitis Inflammation of blood vessels of the skin. Immune complexes, which initiate an uncontrolled inflammatory response, are often the cause of damage and the lesions are often polymorphic. Develops from the deposit of immune complexes in small vessels as a toxic response to drugs or allergens, as a response to strep/viral infections or as a component of systemic vasculitic syndromes Urticaria Hives! Most commonly associated w/ type-1 hypersensitivity reactions to drugs, foods, systemic diseases, physical agents or complement mediated reactions. Scleroderma Sclerosis of the skin. The skin is hard, hypopigmented, taut, shiny and tightly attached to the underlying tissue. Seborrheic Keratosis Benign proliferation of cutaneous basal cells. Tan to waxy yellow, flesh colored or dark brown/black lesions. Looks greasy hyperkeratotic stuck-on scaly. Keratoacanthoma Benign self-limiting tumor of squamous cell differentiation arising from hair follicles. Look like squamous cell carcinoma. Actinic Keratosis Premalignant, composed of aberrant proliferations of epidermal keratinocytes 2/2 prolonged UV radiation exposure. Lesions are rough, scaly and poorly defined pink to reddish or reddish brown papules that are felt more than seen. Considered an early in situ squamous cell carcinoma. Nevi Moles! Benign. Pigmented or non-pigmented. Form from melanocytes. May undergo transition to malignant melanomas. Junctional nevus = rarely develop into melanoma Compound nevus = rarely develop into melanoma Intradermal nevus = slight likelihood of developing into melanoma Chicken pox T-cell immune response Highly contagious and spread by contact and airborne droplets. Incubation 10-27 days (average 14). Children are contagious at least 1 day before rash and transmission can occur until 5-6 days after 1st lesion appears. In immunocompromised children must be considered contagious for 7-10 days. Uncommon but ulcerative lesions can pop up in mouth, conjunctiva and pharynx. Fever for 2-3 days between 101.3-104. Complications more common in adults. Transient hematuria, epistaxis, laryngeal edema, varicella PNA. 1 case of pox provides almost all needed immunity. If acquired during 1st trimester may cause fetal malformation (congenital varicella syndrome). If mom gets pox at any point during pregnancy, baby has higher risk of developing herpes zoster during first few years of life. Maternal varicella-zoster immunoglobulin before rash development (with or without antiviral medication can modify disease progression). Tx: symptom management. Baths/wet dressings/antihistamines. If secondary bacterial infection (from ruptured vesicles) then oral antistaphylococcal drugs. Zoster immune globulin for immunodeficient pts but must be given within 72 hours after exposure. Oral antivirals may relieve symptoms. Vaccine will prevent!! Maternal immune system At about 32 weeks gestation the placenta transports maternal Ab into fetal blood that protects child during it’s first few months of life. The maternal immune system changes during pregnancy in order to tolerate the semiallogenic fetus, but most pregnant women experience healthy pregnancies, which suggests that the immunological changes do not dramatically affect the integrity of the mother. IgG major class of Ab found in blood of fetus/newborn! Hemolytic Disease of the Newborn (this is r/t to immunity b/c it’s a alloimmune condition! This happens if antigens on fetal erythrocytes differ from antigens on maternal erythrocytes. Maternal-fetal incompatibility exists if mother and fetus differ in ABO blood type or if the fetus is Rh-positive and the mother is Rh-negative. Usually erythrocytes from 1st incompatible baby (offers no reaction) cause the mother’s immune system to produce Ab’s that affect the fetuses of subsequent incompatible pregnancies. Most cases of HDN are caused by ABO incompatibility than Rh reaction though. Candidiasis exacerbation Yeastlike fungus Candida albicans is normal on mucosa, skin, GI tract and vagina but can change to a pathogen in critically ill or immunosuppressed. Predisposition: moist, warm, macerated or occluded area systemic antibiotics pregnancy DM Cushing’s Debilitated states < 6 months old 2/2 decreased immune reactivity immunosuppression neoplastic disease of blood and monocyte-macrophage system Carbuncles Collection of infected hair follicles. Most often on back of neck, upper back and lateral thighs. Lesion begins in SQ tissue and lower dermis as a firm mass that evolves into an erythematous, painful, swollen mass that drains through many openings. Abscesses may develop. Chills, fever and malaise are systemic symptoms that can occur. Furuncles and carbuncles are treated with warm compresses. Abscess requires I&D. Recurrent infections, extensive lesions or those associated with cellulitis or systemic symptoms are treated with systemic Abx. Terms such as hypochromic, macrocytic, microcytic, etc Anisocytosis = assuming various sizes Poikilocytosis = assuming various shapes Eryptosis = premature death of damaged erythrocytes Macrocytic-normochromic anemias: Large, abnormally shaped erythrocytes BUT normal hemoglobin concentrations Microcytic-hypochromic anemias: Causes: Small, abnormally shaped erythrocytes AND reduced hemoglobin concentrations Microcytic Macrocytic Hypochromic Normochromic Antibodies, IgG, IgA, etc An antibody (or immunoglobulin) is a serum glycoprotein produced by plasma cells in response to challenge by an immunogen. The term immunoglobulin is used to denote all molecules that are known to have specificity for antigen. The term antibody is used to denote one particular set of immunoglobulins with specificity against a known antigen. There are 5 molecular classes of immunoglobulins: IgG – most abundant = 80-85% Account for most of the protective activity against infections. Placental transfer = so it’s the major class of Ab found in fetal/newborn blood Produced by plasma B cells Has 4 subclasses. Monomer structure / circulates 30-45 days IgA – secretory – has 2 subclasses! Plays crucial role in the immune function of mucous membranes. Found in high concentrations in mucosa (especially GI and respiratory), saliva, tears, and breast milk/colostrum. Dimer structure / circulates 12 days IgM – largest. Synthesized early in neonatal life and is the 1st Ab produced during initial response to antigen. Pentameter structure – it’s the first to respond but the large structure is unstable so it only circulates for 2 days IgE – the lease concentrated of all classes. It appears to have very specialized function as a mediator of many common allergic responses and in the defense against parasitic infections. Circulates 4 days IgD – information/role is limited and found in very low quantities in blood. They are primarily located on surface of developing B-lymphocytes and function as 1 type of B-cell antigen receptor. Circulates 6 days. Skin cancer Skin Cancer Basal cell carcinoma and squamous cell carcinoma most prevalent Malignant melanoma most deadly Chronic UV exposure causes most skin cancers. Less common in darker skinned people b/c the basal cells contain the pigment melanin, which is a protective factor against sun exposure. Basal Cell Carcinoma Most common in whites. Surface epithelial tumor from undifferentiated basal or germinative cells. They grow upward and laterally or downward to dermal-epidermal junction. Usually depressed center with rolled borders. As lesion grows, it ulcerates and develops crusting and becomes firm to the touch. If not treated they invade surrounding tissue and can destroy a nose, eyelid or ear. Metastatic spread is rare b/c they don’t invade vessels or lymph. From UV exposure, arsenic from groundwater wells and autosomal dominant nevoid basal cell carcinoma [Show More]
Last updated: 1 year ago
Preview 1 out of 99 pages
Instant download
Instant download
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Feb 11, 2021
Number of pages
99
Written in
Additional information
This document has been written for:
Uploaded
Feb 11, 2021
Downloads
0
Views
55



_2nd_E_Completed.png)