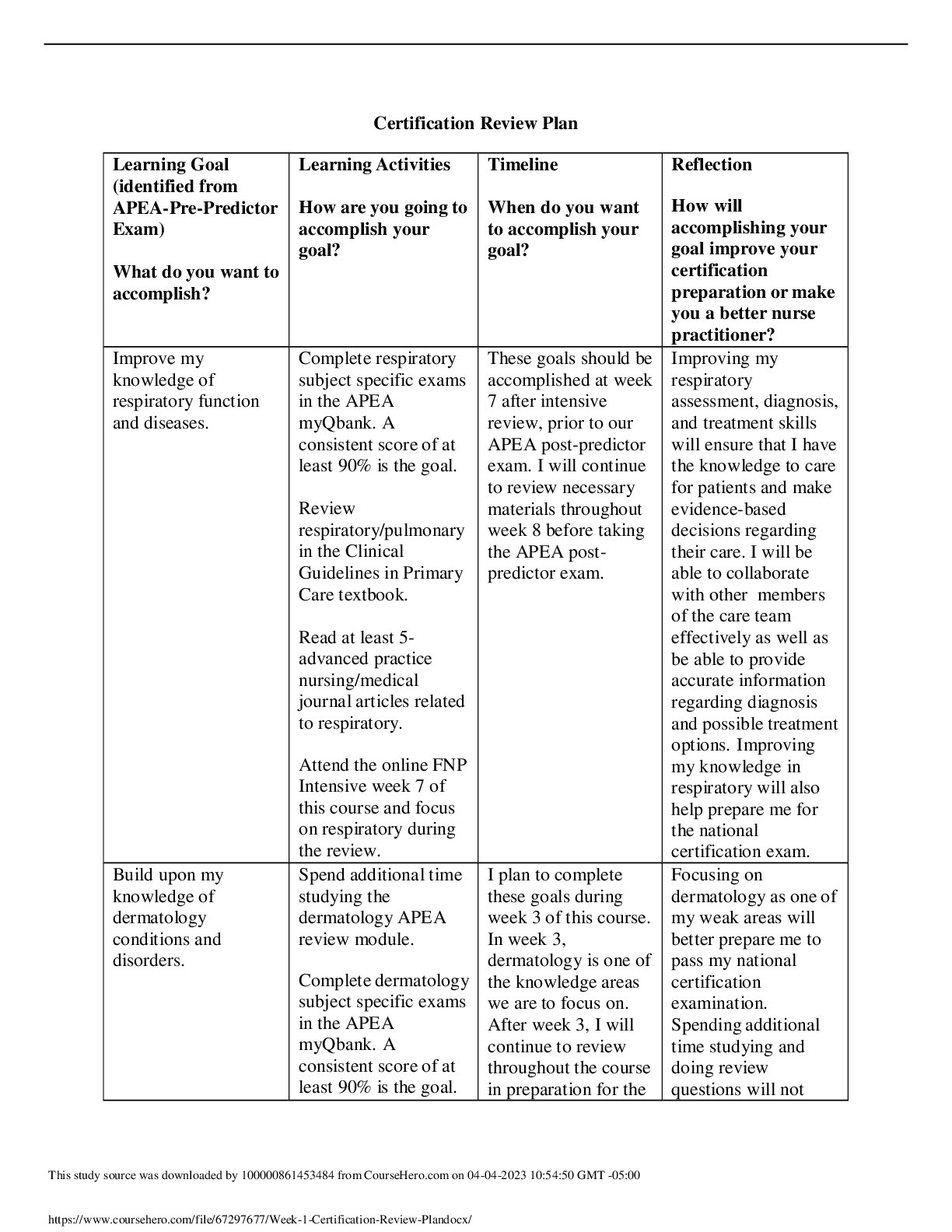
*NURSING > STUDY GUIDE > NR 509 Midterm Study Guide - Download To Score An A+ (All)
NR 509 Midterm Study Guide - Download To Score An A+
Document Content and Description Below
NR 509 Midterm Study Guide Basic and Advanced Interviewing Techniques Basic maximize patient's comfort, avoid unnecessary changes in position, enhance clinical efficiency, move head to toe, exa... mine the patient from their right side Active listening, empathic responses, guided questioning, nonverbal communication, validation, reassurance, partnering, summarization, transitions, empowering the patient Active Listening- closely attending to what the patient is communicating, connecting to the patient’s emotional state and using verbal and nonverbal skills to encourage the patient to expand on his or her feelings and concerns. Empathic Responses-the capacity to identify with the patient and feel the patient’s pain as your own, then respond in a supportive manner. Guided Questioning- show your sustained interest in the patient’s feelings and deepest disclosures and allows the interviewer to facilitate full communication, in the patient’s own words, without interruption. Non-verbal- includes eye contact, facial expression, posture, head position and movement such as shaking or nodding, interpersonal distance, and placement of the arms or legs-crossed, neutral, or open. Validation- helps to affirm the legitimacy of the patient’s emotional experience. Reassurance- an appropriate way to help the patient feel that problems have been fully understood and are being addressed. Partnering- building rapport with patients, express your commitment to an ongoing relationship. Summarization- giving a capsule summary of the patient’s story during the course of the interview to communicate that you have been listening carefully. Transitions- inform your patient when you are changing directions during the interview. Empowering the Patient- empower the patient to ask questions, express their concerns, and probe your recommendations in order to encourage them to adopt your advice, make lifestyle changes, or take medications as prescribed. Advanced: Determine scope of assessment: Focused vs. Comprehensive: pg5 Comprehensive: Used for patients you are seeing for the first time in the office or hospital. Includes all the elements of the health history and complete physical examination. A source fundamental and personalized knowledge about the patient, strengthens the clinician-patient relationship. ● Is appropriate for new patients in the office or hospital ● Provides fundamental and personalized knowledge about the patient ● Strengthens the clinician–patient relationship ● Helps identify or rule out physical causes related to patient concerns ● Provides a baseline for future assessments ● Creates a platform for health promotion through education and counseling ● Develops proficiency in the essential skills of physical examination Flexible Focused or problem-oriented assessment: For patients you know well returning for routine care, or those with specific “urgent care” concerns like sore throat or knee pain. You will adjust the scope of your history and physical examination to the situation at hand, keeping several factors in mind: the magnitude and severity of the patient’s problems; the need for thoroughness; the clinical setting—inpatient or outpatient, primary or subspecialty care; and the time available. ● Is appropriate for established patients, especially during routine or urgent care visits ● Addresses focused concerns or symptoms ● Assesses symptoms restricted to a specific body system ● Applies examination methods relevant to assessing the concern or problem as thoroughly and carefully as possible Tangential lighting: JVD, thyroid gland, and apical impulse of heart. Components of the Health History Jenna/Ashley Initial information Identifying data and source of the history; reliability Identifying data- age, gender, occupation, marital status Source of history- usually patient. Can be: a family member or friend, letter of referral, or clinical record. Reliability- Varies according to the patient’s memory, trust, and mood. Chief Complaint Chief Complaint- Make every attempt to quote the patient’s own words. Present Illness Complete, clear and chronological description of the problem prompting the patient visit Onset, setting in which it occurred, manifestations and any treatments Should include 7 attributes of a symptom: ● Location ● Quality ● Quantity or severity ● Timing, onset, duration, frequency ● Setting in which it occurs ● Aggravating or relieving factors ● Associated manifestations -Differential diagnosis is derived from the “pertinent positives” and “pertinent negatives” when doing Review of Systems that are relevant to the chief complaint. A list of potential causes for the patients problems. -Present illness should reveal patient’s responses to his or her symptoms and what effect this has on their life. -Each symptom needs its own paragraph and a full description. -Medication should be documented, name, dose, route, and frequency. Home remedies, non- prescriptions drugs, vitamins, minerals or herbal supplements, oral contraceptives, or borrowed medications. -Allergies-foods, insects, or environmental, including specific reaction Tobacco use, including the type. If someone has quit, note for how long -Alcohol and drug use should always be investigated and is often pertinent to the Presenting Illness. Past history -Childhood Illness: measles, rubella, mumps, whooping cough, chickenpox, rheumatic fever, scarlet fever, and polio. Also include any chronic childhood illness -Adult illnesses: Provide information in each of the 4 areas: ● Medical: diabetes, hypertension, hepatitis, asthma and HIV; hospitalizations; number and gender of sexual partners; and risk taking sexual practices. ● Surgical: dates, indications, and types of operations ● Obstetric/gynecologic: Obstetric history, menstrual history, methods of contraception, and sexual function. ● Psychiatric: Illness and time frame, diagnoses, hospitalizations, and treatments. -Health Maintenance: Find out if they are up to date on immunizations and screening tests. Review Tb tests, pap smears, mammograms, stool tests for occult blood, colonoscopy, cholesterol levels etc.. Family history Outlines or diagrams age and health, or age and cause of death, of siblings, parents, and grandparents Documents presence or absence of specific illnesses in family, such as hypertension, coronary artery disease, elevated cholesterol levels, stroke, diabetes, thyroid or renal disease, arthritis, tuberculosis, asthma or lung disease, headache, seizure disorder, mental illness, suicide, substance abuse, and allergies, and symptoms reported by patient. Ask about history of breast, ovarian, colon, or prostate cancer Ask about Genetically transmitted diseases Personal or social history Describes educational level, occupation, family of origin, current household, personal interests, and lifestyle Capture the patients personality and interests, sources of support, coping style, strengths, and concerns Includes lifestyle habits that promote health or create risk, such as exercise and diet, safety measures, sexual practices, and use of alcohol, drugs, and tobacco Expanded personal and social history personalizes your relationship with the patient and builds a rapport Review of systems pg 11-13 Documents presence or absence of common symptoms related to each of the major body systems Understanding and using Review of Systems questions may seem challenging at first. These “yes-no” questions should come at the end of the inter- view. Think about asking a series of questions going from “head to toe.” It is helpful to prepare the patient by saying, “The next part of the history may feel like a hundred questions, but it is important to make sure we have not missed anything.” Most Review of Systems questions pertain to symptoms, but on occasion, some clinicians include diseases like pneumonia or tuberculosis. Note that as you elicit the Present Illness, you may also draw on Review of Systems questions related to system(s) relevant to the Chief Complaint to establish “pertinent positives and negatives” that help clarify the diagnosis. For example, after a full description of chest pain, you may ask, “Do you have any history of high blood pressure . . . palpitations . . . shortness of breath . . . swelling in your ankles or feet?” or even move to questions from the Respiratory or Gastrointestinal Review of Systems The Review of Systems questions may uncover problems that the patient has overlooked, particularly in areas unrelated to the Present Illness. Significant health events, such as past surgery, hospitalization for a major prior illness, or a parent’s death, require full exploration. Keep your technique flexible. Remember that major health events discovered during the Review of Systems should be moved to the Present Illness Past History in your write-up. Some experienced clinicians do the Review of Systems during the physical examination, asking about the ears, for example, as they examine them. If the patient has only a few symptoms, this combination can be efficient. If there are multiple symptoms, however, this can disrupt the flow of both the history and examination, and necessary note taking becomes awkward The Review of Systems: Pg. 12-13 ROS Chart Copied from online book General: Usual weight, recent weight change, clothing that fits more tightly or loosely than before; weakness, fatigue, or fever. Skin: Rashes, lumps, sores, itching, dryness, changes in color; changes in hair or nails; changes in size or color of moles. Head, Eyes, Ears, Nose, Throat (HEENT): Head: Headache, head injury, dizziness, lightheadedness. Eyes: Vision, glasses or contact lenses, last examination, pain, redness, excessive tearing, double or blurred vision, spots, specks, flashing lights, glaucoma, cataracts. Ears: Hearing, tinnitus, vertigo, earaches, infection, discharge. If hearing is decreased, use or nonuse of hearing aids. Nose and sinuses: Frequent colds, nasal stuffiness, discharge, or itching, hay fever, nosebleeds, sinus trouble. Throat (or mouth and pharynx): Condition of teeth and gums, bleeding gums, dentures, if any, and how they fit, last dental examination, sore tongue, dry mouth, frequent sore throats, hoarseness. Neck: “Swollen glands,” goiter, lumps, pain, or stiffness in the neck. Breasts: Lumps, pain, or discomfort, nipple discharge, self-examination practices. Respiratory: Cough, sputum (color, quantity; presence of blood or hemoptysis), shortness of breath (dyspnea), wheezing, pain with a deep breath (pleuritic pain), last chest x-ray. You may wish to include asthma, bronchitis, emphysema, pneumonia, and tuberculosis. Cardiovascular: “Heart Trouble”; high blood pressure; rheumatic fever; heart murmurs; chest pain or discomfort; palpitations; shortness of breath; need to use pillows at night to ease breathing (orthopnea breathing (paroxysmal nocturnal dyspnea); swelling in the hands, ankles, or feet (edema); results of past electrocardiograms or other cardiovascular tests. Gastrointestinal: Trouble swallowing, heartburn, appetite, nausea. Bowel move-ments, stool color and size, change in bowel habits, pain with defecation, rectal bleeding or black or tarry stools, hemorrhoids, constipation, diarrhea. Abdominal pain, food intolerance, excessive belching or passing of gas. Jaundice, liver, or gallbladder trouble; hepatitis. Peripheral vascular: Intermittent leg pain with exertion (claudication); leg cramps; varicose veins; past clots in the veins; swelling in calves, legs, or feet; color change in fingertips or toes during cold weather; swelling with redness or tenderness. Urinary: Frequency of urination, polyuria, nocturia, urgency, burning or pain during urination, blood in the urine (hematuria), urinary infections, kidney or flank pain, kidney stones, ureteral colic, suprapubic pain, incontinence; in males, reduced caliber or force of the urinary stream, hesitancy, dribbling. Genital Male: Hernias, discharge from or sores on the penis, testicular pain or masses, scrotal pain or swelling, history of sexually transmitted infections and their treatments. Sexual habits, interest, function, satisfaction, birth control methods, condom use, and problems. Concerns about HIV infection. Female: Age at menarche, regularity, frequency, and duration of periods, amount of bleeding; bleeding between periods or after intercourse, last menstrual period, dysmenorrhea, premenstrual tension. Age at menopause, menopausal symptoms, postmenopausal bleeding. If the patient was born before 1971, exposure to diethylstilbestrol (DES) from maternal use during pregnancy (linked to cervical carcinoma). Vaginal discharge, itching, sores, lumps, sexually transmitted infections and treatments. Number of pregnancies, number and type of deliveries, number of abortions (spontaneous and induced), complications of pregnancy, birth-control methods. Sexual preference, interest, function, satisfaction, any problems, including dyspareunia. Concerns about HIV infection. Musculoskeletal: Muscle or joint pain, stiffness, arthritis, gout, backache. If present, describe the location of affected joints or muscles, any swelling, redness, pain, tenderness, stiffness, weakness, or limitation of motion or activity; include timing of symptoms (e.g., morning or evening), duration, and any history of trauma. Neck or low back pain. Joint pain with systemic symptoms such as fever, chills, rash, anorexia, weight loss, or weakness. Psychiatric: Nervousness, tension, mood, including depression, memory change, suicidal ideation, suicide plans or attempts. Past counseling, psycho-therapy, or psychiatric admissions. Neurologic: Changes in mood, attention, or speech; changes in orientation, memory, insight, or judgment; headache, dizziness, vertigo, fainting, black-outs; weakness, paralysis, numbness or loss of sensation, tingling or “pins and needles”. Subjective vs Objective Data Subjective- symptoms or what the patient tells you. Apparent only to the person affected; includes client’s perceptions, feelings, thoughts, and expectations. Cannot be directly observed and can be discovered only asking questions. Examples: low back pain, fatigue, immunizations, weight gain, stomach cramps. Objective- signs or what you observe. Detectable by an observer or can be tested against acceptable standard; tangible; observable facts; includes observation of client behavior, medical records, lab and diagnostic tests, data collected by physical exam. Examples: blood pressure, heart rate, wound appearance, lung sounds, ambulation description. Subjective Data (symptoms) Objective Data (signs) What the patient tells you What is observed during physical examination Patients history, from Chief Complaint through Review of Systems Laboratory information, test data Documentation- Documentation needs to be CLEAR, CONCISE, COMPREHENSIVE. -think order and readability, amount of detail. - Record: history, PE, and lab findings - describe what's observed not what was done -SOAP (subjective, objective, assessment, & plan) note is used for providers of various backgrounds/specialties to communicate with each other Chapter 2 Clinical Decision Making ashley Clinical decision making should be evidence based. The FNP should draw on a full range of knowledge and experience, and read widely. Clinical decision making is when the reading about diseases and abnormalities is most useful. By consulting the clinical literature, you are embarking on evidence-based decision making and clinical practice. There are five steps to generating a clinical hypotheses 1. Select the most specific and critical findings to support your hypothesis 2. Match findings against all the conditions that can produce them. 3. Eliminate the diagnostic possibilities that fail to explain findings. 4. Weigh the competing possibilities and select the most likely diagnosis 5. Give special attention to potentially life-threatening conditions Once the hypothesis is made it should be tested, this may include further history taking, testing or physical examination. The next step is to establish a working diagnosis such as “bacterial meningitis, pneumococcal”. The final step is developing a plan. The plan should make reference to diagnosis, treatment and patient education. It is important to discuss your assessment with the patient prior to finalizing the plan to ensure the patient is onboard. Critical Thinking and Reasoning Critical thinking- the mental process of actively and skillfully perception, analysis, synthesis and evaluation of collected information through observation, experience and communication that leads to a decision for action. The main critical thinking skills in which nursing students should be exercised during their studies are critical analysis, introductory and concluding justification, valid conclusion, distinguish between facts and opinions, evaluation the credibility of information sources, clarification of concepts and recognition of conditions. Critical thinking is an essential process for the safe, efficient and skillful nursing practice. The nursing education programs should adopt attitudes that promote critical thinking and mobilize the skills of critical reasoning. Critical thinking is the disciplined, intellectual process of applying skillful reasoning as a guide to belief or action. In nursing, critical thinking for clinical decision-making is the ability to think in a systematic and logical manner with openness to question and reflect on the reasoning process used to ensure safe nursing practice and quality care. Critical thinking when developed in the practitioner includes adherence to intellectual standards, proficiency in using reasoning, a commitment to develop and maintain intellectual traits of the mind and habits of thought and the competent use of thinking skills and abilities for sound clinical judgments and safe decision- making. Differential Diagnoses (obtained from book and week 1 review) - A list with potential causes of patient specific problem/CC -A chief complaint must be identified first. -Includes all medical diseases that may possibly explain problem/ CC. -The differential diagnosis list should begin with the most likely explanation or etiology for the problem/CC. EX: C/O vomiting blood: 1. Peptic ulcer 2.Cirrhosis with bleeding esophageal varices 3. Acute hemorrhagic gastritis -Differential diagnostic procedures are used by clinicians to diagnose the specific disease in a patient, or, at least, to eliminate any imminently life-threatening conditions. The differential diagnosis list is similar to, but different from, the problem list. -The differential diagnosis includes all of the medical diseases that may possibly explain the patient’s chief complaint or principal problem -A differential diagnosis list is focused on providing an explanation for a specific complaint. -In order to develop a differential list versus a problem list, you must first identify the chief complaint. Each differential diagnosis should offer an explanation or etiology for the same chief complaint. Pathological and Physiological Processes Pathologic Process- patient complaints often stem from a pathologic process involving diseases of a body system or structure. Common Classified: congenital, inflammatory or infectious, immunologic, neoplastic, metabolic, nutritional, degenerative, vascular, traumatic, and toxic. Example: Possible pathological causes of a headache include- sinus infection, concussion from trauma, subarachnoid hemorrhage, or brain tumor. Problem List -After you complete the clinical record, it is good clinical practice to generate a problem list that summarizes the patient’s problems that can be placed in the front of the office or hospital chart. -List the most active and serious problems first and record their date of onset. - Helps to individualize the patient’s care. On follow-up visits, provides a quick summary of the patient’s clinical history and a reminder to review the status of problems the patient may not mention. -An accurate Problem List allows better population management of patients, by using EHRs to track patients with specific problems, recall patients who are behind on appointments, and follow up on specific issues. -Allows other members of the health care team to learn about the patient’s health status at a glance. For example, in a patient who is vomiting blood and is known to have migraines and to be diabetic, the problem list might read: 1. Hematemesis 2. Diabetes Mellitus 3. Migraine 4. Recent divorce 5. Poverty Prioritization Generate problem list with all problems noted, differential diagnoses should cover all possible causes of chief complaint. Prioritize which complaints/problems are highest priority (urgent) for this visit. (i.e., Tina has diabetes, htn, and a slew of other issues, but utmost importance is her foot wound and ankle pain) Chapter 3 **Interpretation and Analysis (Area is lacking information) Heather and Stacy The clinician must focus on the patient to elicit the full story of the patient's symptoms, but the clinician must also interpret key information to reach an assessment and plan. Patient-centered interviews recognize the importance of patients' expressions of personal concerns, feelings, and emotions and evoke the personal context of the patient's symptoms and disease Sensitivity- true positive. The probability that a person with disease as a + test. Specificity- True negative. SnNOUT- a sensitive test with a negative result rule OUT disease SpPIN- a specific test with a positive result rules IN disease Bayes Theorem- one way to use likelihood ratios to revise probabilities for disease Natural frequencies- represents the joint frequency of two events, such as the number of patients with disease and the number who have a positive test result. Kappa score- reproductivity. Measures the amount of agreement that occurs beyond chance. Precision-reproductivity. Being able to apply the same test to the same unchanged person and obtain the same results. Logical Sequence pg 73 In general, an interview moves through several stages. Throughout this sequence, as the clinician you must remain attuned to the patient’s feelings, help the patient express them, respond to their content, and validate their significance. As a student, you will concentrate primarily on eliciting the patient’s story and creating a shared understanding of the patient’s concerns. Later on, as a practicing clinician, reaching an agreement on a plan for further evaluation and treatment becomes more important. Whether the interview is comprehensive or focused, pay close attention to the patient’s feelings and affect, always working on strengthening the relationship as you move through the typical sequence that follows. Including the patient’s feelings, ideas, and expectations leads to therapeutic interventions best suited to the patient’s needs, coping skills, and life circumstances. 1. Greeting the patient and establishing rapport. The initial moments of your encounter lay the foundation for your ongoing relationship. If this is the first contact, explain your role, your status as a student, and how you will be involved In the patient’s care. Use a formal title to address the patient. Avoid first names until you have permission, except with children and adolescents. Don’t be afraid to clarify how to pronounce a patient’s name. Acknowledge any visitors in the room and inquire about their names and relationship to the patient. Whenever visitors are present, YOU ARE OBLIGATED TO MAINTAIN THE PATIENT'S CONFIDENTIALITY. Let the patient decide if the visitors can stay in the room. ALWAYS BE ATTUNED TO THE PATIENT'S COMFORT. Consider the best way to arrange the room and how close you should be to the patient. Give the patient your undivided attention. 2. Taking Note As a novice, you may need to write down much of what you learn during the interview. Experienced clinicians usually recall much of the interview without any notes. Jot down short phrases, specific dates, or words, but do not let note taking or the laptop screen distract you from the patient. Maintain good eye contact. If the patient is talking about disturbing material, put your pen down and look away from the computer. Face the patient directly as you elicit the patient’s story, observing non-verbal behaviors. Look up from the computer as often as possible, readjusting your position as needed. 3. Establishing the Agenda=chief complaint Once you have established rapport, you are ready to pursue the patient’s reason for seeking care, traditionally called the chief complaint. In the ambulatory setting, where there are often three or four reasons for the visit, the phrase presenting problem(s) may be preferable. One benefit to this phrase is that it does not characterize the patient as a complainer. Begin with open-ended questions that allow full freedom of response: “What are your special concerns today?”, “How can I help you?”, or “Are there specific concerns that prompted your appointment today?” These questions encourage the patient to talk about any kinds of concerns, not just clinical ones. Note that the first problem the patient mentions may not be the one that is most important. Often, patients give one reason for the visit to the nurse and another to you. For some visits, patients do not have a specific concern and only “want a check-up”. Identifying all concerns allows you and the patient to decide which ones are most pressing and which can be postponed to another visit. Using questions such as, “Is there anything else?”, “Have we got everything?”, or “Is there anything we missed?”, can help to uncover the patient’s full agenda and “the real reason” for the visit. Identifying the full agenda protects time for the most important issues. Even negotiating the agenda at the outset doesn’t avert “oh by the way” concerns that suddenly emerge at the end of the visit. 4. Inviting the Patient’s story Once you have prioritized the agenda, invite the patient’s story by asking about the foremost concern, “Tell me more about...” Encourage patients to tell their stories in their own words, using an open-ended approach. Avoid biasing the patient’s story—do not inject new information or interrupt. Instead, use active listening skills: lean forward as you listen; add continuers such as nodding your head and phrases like “uh huh,” “go on,” or “I see.” Train yourself to follow the patient’s leads. If you ask specific questions prematurely, you risk suppressing details in the patient’s own words. Studies show that clinicians wait only 18 seconds before they interrupt.28 Once interrupted, patients usually do not resume their stories. After the patient’s initial description, explore the patient’s story in more depth. Ask, “How would you describe the pain?”, “What happened next?”, or “What else did you notice?” so that the patient enriches important details. 5. Exploring the Patient’s perspective The disease/illness distinction model helps elucidate the different yet complementary perspectives of the clinician and the patient. Disease is the explanation that the clinician uses to organize the symptoms that leads to a clinical diagnosis. Illness is a construct that explains how the patient experiences the disease, including its effects on relationships , function , and sense of well-being. FIFE The Patient’s Feelings, including fears or concerns, about the problem The patients Ideas about the nature and cause of the problem The effect of the problem on the patients’ life and Function The patient’s Expectations of the disease, of the clinician, or of health care, often based on prior personal or family experiences. 6. Identifying and Responding to the Patient’s emotional Cues. Illness is often accompanied by emotional distress; 30% to 40% of patients have anxiety and depression in primary care practices. Visits tend to be longer when clinicians miss emotional clues. Clues to the patients’ perspective on illness Direct statement by the patient of explanations, emotions, expectations, and effects of the illness Expression of feelings about the illness without naming the illness Attempts to explain or understand symptoms Speech clues (e.g., repetition, prolonged reflective pauses) Sharing a personal story Behavioral clues indicative of unidentified concerns, dissatisfaction, or unmet needs such as reluctance to accept recommendations, seeking a second opinion, or early return appointment Learn to respond attentively to emotional cues using techniques like reflection, feedback, and “continuers” that convey support. A mnemonic for responding to emotional cues is NURSE: Name- “that sounds like a scary experience for you”; Understand or legitimize- “It’s understandable that you feel that way”; Respect- “you’ve done better than most people would with this”; Support- “I will continue to work with you on this”; and Explore- “How else were you feeling about it”. 7. Generating and Testing Diagnostic Hypotheses As you gain experience listening to patient concerns, you will deepen your skills of clinical reasoning. You will generate and test diagnostic hypotheses about which disease process might be present. Identifying all the features of each symptom is fundamental to recognizing patterns of disease and to generate the differential diagnosis. It is important to fully flesh out the patient’s story. This avoids the common trap of premature closure, or shutting down the patient’s story too quickly, which can lead to errors in diagnosis. It is helpful to visualize the process of evoking a full description of each symptom as “the cone” First, open-ended questions to hear “the story of the symptom” in the patient’s own words Then more specific questions to elicit “the seven features of every symptom” Finally, the yes-no questions or “pertinent positives and negatives” from the relevant section of the review of systems Each symptom has its own “cone,” which becomes a paragraph in the History of Present Illness in the written record. Questions about clusters of symptoms in common clinical entities are also found in “The Health History” section of each of the regional physical examination chapters. The interview is your primary source of evidence for and against various diagnostic possibilities. The challenge is to avoid a clinician- centered agenda, letting focused questions take over that obscure the patient’s perspective and limit your opportunity to create an empathic therapeutic connection. 9. Sharing the treatment plan Learning about the disease and conceptualizing the illness allow you and the patient to create a shared picture of the patient’s problems. This multifaceted picture then forms the basis for planning further evaluation (e.g., physical examination, laboratory tests, consultations) and negotiating a treatment plan. Shared decision-making has been called the pinnacle of patient-centered care.36 Experts recommend a three-step process: introducing choices and describing options using patient decision support tools when available; exploring patient preferences; and moving to a decision, checking that the patient is ready to make a decision and offering more time, if needed. 10. Behavior change and Motivational Interviewing. Many of your patient visits will close with a discussion of behavior changes needed to optimize health or treat illness. These could include a change in diet, exercise habits, cessation of smoking or drinking, adherence to medication regimens, or self-management strategies, among others.38 Advanced techniques such as motivational interviewing and the therapeutic use of the clinician–patient relationship are beyond the scope of this book. Nonetheless, it is worthwhile to introduce the principles of motivational interviewing, a set of well-documented techniques that improve health outcomes, especially for patients with substance abuse.39 Motivational interviewing helps patients “to say why and how they might change, and is based on the use of a guiding style” of inter- viewing, rather than direct advice. It engages patients to express the pros and cons of a given behavior.40 Motivational interviewing makes the assumption that many patients already know what is best for them and helps them con- front their ambivalence to change.41 Using three core skills empowers the patient to provide ideas, solutions, and a timetable for change. The Guide Style of Motivational Interviewing: 1. “Ask” open-ended questions—invite the patient to consider how and why they might change. 2. “Listen” to understand your patient’s experience—“capture” their account with brief summaries or reflective listening statements such as “quitting smoking feels beyond you at the moment”; these express empathy, encourage the patient to elaborate, and are often the best way to respond to resistance. 3. “Inform”—by asking permission to provide information, and then asking what the implications might be for the patient. 11. Closing the Interview and the Visit. You may find that ending the health history interview, and later concluding the visit, are difficult. Patients often have many questions, and if you have done your job well, they feel engaged and affirmed as they talk with you. Let the patient know that the end of the interview or the visit is approaching to allow time for any final questions. Make sure the patient understands the mutual plans you have developed. For example, before gathering your papers or standing to leave the room, you can say, “We need to stop now. Do you have any questions about what we’ve covered?” As you close, summarizing plans for future evaluation, treatments, and follow-up is helpful. A useful technique to assess the patient’s understanding is to “teach back,” whereby you invite the patient to tell you, in his or her own words, the plan of care. An example would be: “Could you please tell me what you understand is our plan of care?” The patient should have a chance to ask any final questions, but the last few minutes are not a good time to bring up new topics. If this happens and the concern is not life threatening, simply assure the patient of your interest and make plans to address the problem at a future time. “That knee pain sounds concerning. Why don’t you make an appointment for next week so we can dis- cuss it?” Reaffirming your ongoing commitment to the patient’s health shows your involvement and esteem. 12. Taking Time for Self-Reflection The role of self-reflection, or mindfulness, in developing clinical empathy cannot be overemphasized. Mindfulness refers to the state of being “purposefully and nonjudgmentally attentive to [one’s] own experience, thoughts, and feelings.”44 As you encounter people of diverse ages, gender identities, social class, race, and ethnicity, being consistently respectful and open to individual differences is an ongoing challenge of clinical care. Because we bring our own values, assumptions, and biases to every encounter, we must look inward to see how our own expectations and reactions affect what we hear and how we behave. Self-reflection is a continual part of professional development in clinical work. It brings a deepening personal awareness to our work with patients. This personal awareness is one of the most rewarding aspects of patient care. Associated Symptoms OLD CARTS Seven Attributes of a Symptom 1.Location 2.Quality 3.Quantity or severity 4.Timing, including onset, duration, and frequency 5.The setting in which it occurs 6.Factors that have aggravated or relieved the symptoms 7. Associated manifestations Adaptive Questioning Guided Questioning: 1.Moving from open-ended to focused questions 2.Using questioning that elicits a graded response 3.Asking a series of questions, one at a time 4. Offering multiple choices for answers 5. Clarifying what the patient means 6.Encouraging with continuers 7.Using echoing Challenging Patients -Silent -Blind -Confusing -With impaired capacity -Talkative -Angry or disruptive -With a language barrier -With low literacy or low health literacy -With hearing impairment -With limited intelligence -Seeking personal advice -Seductive Chapter 4 General Approach to the Physical Examination Use open-ended questions-helps to encourage the patient to describe what they are experiencing Listen and ask common-sense questions Follow a thorough and systematic sequence to history taking and physical examination Keep an open mind toward both the patient and the clinical data Always include "the worst-case scenario" in your list of possible explanations of the patient's problem, and make sure it can be safely eliminated Analyze any mistakes in data collection or interpretation Confer with colleagues and review the pertinent clinical literature to clarify uncertainties Apply the principles of evaluating clinical evidence to patient information and testing As you talk with and examine the patient, heighten your focus on the patient’s mood, build, and behavior ○ 1. Reflect on your approach to the patient: When greeting the patient identify yourself as a student, beginners spend more time in certain areas and that is ok but just warn the patient that you may want to listen to their heart a little longer but that does not mean anything is wrong ■ Avoid interpreting your findings, you are not the patients primary care provider ■ Avoid negative reactions or showing distaste when finding abnormalities ○ 2. Adjust the lighting and the environment: set the stage so that both you and the patient are comfortable; good lighting and a quiet environment enhance what you see and hear however may be hard to arrange ○ 3. Check your equipment: The following equipment is needed: ■ An ophthalmoscope and an otoscope. If you are examining children, the otoscope could allow pneumatic otoscopy. ■ ●A flashlight or penlight ■ ● Tongue depressors ■ A ruler and a flexible tape measure, preferably marked in centimeters ■ ●Often a thermometer ■ ●A watch with a second hand ■ ●A sphygmomanometer ■ ●A stethoscope with the following characteristics: ■ ●Ear tips that fit snugly and painlessly. To get this fit, choose ear tips of the proper size, align the ear pieces with the angle of your ear canals, and adjust the spring of the connecting metal band to a comfortable tightness. ■ ●Thick-walled tubing as short as feasible to maximize the transmission of sound: ∼30 cm (12 inches), if possible, and no longer than 38 cm (15 inches) ■ ●A bell and a diaphragm with a good changeover mechanism ■ ●A visual acuity card ■ ●A reflex hammer ■ ●Tuning forks, both 128 Hz and 51 ■ Cotton swabs, safety pins, or other disposable objects for testing sensation and two-point discrimination ■ ●Cotton for testing the sense of light touch ■ ●Two test tubes (optional) for testing temperature sensation ■ ●Gloves and lubricant for oral, vaginal, and rectal examinations ■ ● Vaginal specula and equipment for cytologic and bacteriologic studies ■ ●Paper and pen or pencil, or desktop or laptop computer ○ 4. Make the patient comfortable. Show sensitivity to privacy and patient modesty; this conveys respect for the patients vulnerability ○ 5. Observe standard and universal precautions. ○ 6. Choose the sequence, scope, and positioning of examination **Interview Facilitation Vital Signs pg. 123: Blood pressure, heart rate, RR, and temperature Begin by measuring the blood pressure and heart rate. Count the heart rate for one minute by palpating the radial pulse with your fingers, or by listening for the apical pulse with stethoscope at the cardiac apex. Count respirations at this time to avoid the patient becoming alerted=change in pattern. Blood Pressure pg 124 Ambulatory and Home blood pressure monitoring are more predictive of cardiovascular disease and end organ damage than manual and automated measurements in the office Reference standard for confirming elevated office blood pressures- Measure blood pressure at preset intervals over 24 to 48 hours, usually every 15-20 minutes during the day and 30 to 60 minutes during the night. Gold Standard: Ambulatory blood pressure monitoring: automated. Provides 24 hour average blood pressures. Shows nocturnal blood pressure “dips” (normal) or stays elevated (Cardiovascular disease risk factor). Expensive and may not be covered by insurance. Types of hypertension: 1. White coat hypertension (isolated clinic hypertension) > 140/90 in medical settings and mean awake ambulatory readings <135/85 2. Masked hypertension office blood pressure <140/90, but elevated daytime blood pressure >135/85. 3.Nocturnal hypertension- “dipping occurs” in most patients at night as they shift from wakefulness to sleep. Selecting the Correct Size Cuff: Cuff too small= readings HIGH. Cuff too large= readings LOW Brachial Artery: brachial artery below heart= BP readings HIGHER. Brachial artery above heart level= BP readings LOW. Definitions of Hypertension ● Make sure patients understand all the steps needed to ensure accurate readings at home, as detailed in this section. Office manual or automated blood pressure based on the average of two readings on two separate occasions: ≥140/90 Classification of Hypertension Normal <120 systolic <80 diastolic Prehypertension 120-139 systolic 80-89 diastolic Stage 1 ages 18-60; diabetes or renal disease 140-159 systolic 90-99 diastolic Ages > 60 years 150-159 systolic >100 Stage 2 >160 systolic >100 diastolic Steps to Ensure Accurate Blood Pressure Measurement 1. The patient should avoid smoking, caffeine, or exercise for 30 minutes prior to measurement. 2. The examining room should be quiet and comfortably warm. 3. The patient should sit quietly for 5 minutes in a chair with feet on the floor, rather than on the examining table. 4. The arm selected should be free of clothing, fistulas for dialysis, scars from brachial artery cutdowns, or lymphedema from axillary node dissection or radiation therapy. 5. Palpate the brachial artery to confirm a viable pulse and position the arm so that the brachial artery, at the antecubital crease, is at heart level—roughly level with the fourth interspace at its junction with the sternum. 6. If the patient is seated, rest the arm on a table a little above the patient’s waist; if standing, try to support the patient’s arm at the mid-chest level Estimate the Systolic Pressure and Add 30 mm Hg : To decide how high to raise the cuff pressure, first estimate the systolic pressure by palpation. As you palpate the radial artery with the fingers of one hand, rapidly inflate the cuff until the radial pulse disappears. Read this pressure on the manometer and add 30 mm Hg. Using this sum for subsequent inflations prevents discomfort from unnecessarily high cuff pressures. It also avoids the occasional error caused by an auscultatory gap—a silent interval that may be present between the systolic and diastolic pressures (Fig. 4-5). Deflate the cuff promptly and completely and wait for 15 to 30 second Identify the Systolic Blood Pressure Inflate the cuff again rapidly to the target level, and then deflate the cuff slowly at a rate of about 2 to 3 mm Hg per second. Note the level when you hear the sounds of at least two consecutive beats. Identify the Diastolic Blood Pressure Continue to deflate the cuff slowly until the sounds become muffled and disappear. To confirm the disappearance point, listen as the pressure falls another 10 to 20 mm Hg. Then deflate the cuff rapidly to zero. The disappearance point, which is usually only a few mm Hg below the muffling point, provides the best estimate of diastolic pressure Average Two or More Readings Read both the systolic and diastolic levels to the nearest 2 mm Hg. Wait 2 or more minutes and repeat. Average your readings. If the first two readings differ by more than 5 mm Hg, take additional readings. When using an aneroid instrument, hold the dial so that it faces you directly. Avoid slow or repetitive inflations of the cuff because the resulting venous congestion can cause false readings Measure Blood Pressure in Both Arms At Least Once. Normally, there may be a difference in pressure of 5 mm Hg and sometimes up to 10 mm Hg. Subsequent readings should be made on the arm with the higher pressure. **A pressure difference of more than 10 to 15 mm Hg occurs in subclavian steal syndrome, supravalvular aortic stenosis, and aortic dissection, and should be investigated. Orthostatic Hypotension If indicated, assess orthostatic hypotension, common in older adults. Measure blood pressure and heart rate in two positions—supine after the patient is resting from 3 to 10 minutes, then within 3 minutes once the patient stands up. Normally, as the patient rises from the horizontal to the standing position, systolic pressure drops slightly or remains unchanged, whereas diastolic pressure rises slightly. Orthostatic hypotension is a drop in systolic blood pressure of at least 20 mm Hg or drop in diastolic blood pressure of at least 10 mm Hg within 3 minutes of standing. Causes of orthostatic hypotension include drugs, moderate or severe blood loss, prolonged bed rest, and diseases of the autonomic nervous system. The Hypertensive Patient with Systolic Blood Pressure Higher in the Arms than in the Legs Compare blood pressure in the arms and the legs and assess “femoral delay” at least once in every hypertensive patient. Coarctation of the aorta arises from narrowing of the thoracic aorta, classically presents with systolic hypertension greater in the arms than the legs. In normal patients, the systolic blood pressure should be 5 to 10 mm Hg higher in the lower extremities than in the arms. To determine blood pressure in the leg, use a wide, long thigh cuff that has a bladder size of 18 × 42 cm, and apply it to the midthigh. Center the bladder over the posterior surface, wrap it securely, and listen over the popliteal artery. If possible, the patient should be . Alternatively, ask the supine patient to flex one leg slightly, with the heel resting on the bed. Palpate the radial or brachial and femoral pulses at the same time, and compare their volume and timing. Normally, volume is equal and the pulses occur simultaneously. Temperature The core body temperature, measured internally, is approximately 37°C (98.6°F) and fluctuates approximately 1°C over the course of the day. It is lowest in the early morning and highest in the afternoon and evening. Women have a wider range of normal temperature than men. Although the research gold standard for core body temperature is the blood temperature in the pulmonary artery, clinical practice relies on noninvasive oral, rectal, axillary, tympanic membrane, and temporal artery measurements. -Feeling cold, goose bumps, and shivering = rising temperature -Feeling hot and sweating= falling temperature -Night sweats= tuberculosis and malignancy -mask fever= aspirin, acetaminophen, corticosteroids, nonsteroidal anti-inflammatory drugs-- Weight loss with high food intake= DM, hyperthyroidism, and malabsorption -Reducing weight by 5 to 10 %= improvement in blood pressure, lipids, and glucose tolerance, and reduce the risk for diabetes or hypertension -Oral and rectal temperature measurements remain common. Oral temperatures are generally lower than the core body temperature. They are also lower than rectal temperatures by an average of 0.4 to 0.5°C (0.7 to 0.9°F), and higher than axillary temperatures by approximately 1°. Axillary temperatures take 5 to 10 minutes to register and are considered less accurate than other measurements. -Tympanic membrane temperatures can be more variable than oral or rectal temperatures. Studies vary in methodology, but suggest that in adults, oral and temporal artery temperatures correlate more closely with the pulmonary artery temperature, but are about 0.5°C lower.54–56 Oral Temperatures. -For glass thermometers, shake the thermometer down to 35°C (96°F) or below, insert it under the tongue, instruct the patient to close both lips, and wait for 3 to 5 minutes. Then read the thermometer, reinsert it for a minute, and read it again. If the temperature is still rising, repeat this procedure until the reading remains stable. Note that hot or cold liquids, and even smoking, can alter the temperature reading. In these situations, delay taking the temperature for 10 to 15 minutes. -Rectal Temperatures. For a rectal temperature, ask the patient to lie on one side with the hip flexed. Select a rectal thermometer with a stubby tip, lubricate it, and insert it about 3 cm to 4 cm (1.5 inches) into the anal canal, in a direction pointing to the umbilicus. Remove it after 3 minutes, then read. Alternatively, use an electronic thermometer after lubricating the probe cover. Wait about 10 seconds for the digital temperature recording to appear -Tympanic Membrane Temperatures. The tympanic membrane shares the same blood supply as the hypothalamus, where temperature regulation occurs in the brain. Accurate temperature readings require access to the tympanic membrane. Make sure the external auditory canal is free of cerumen, which can lower temperature readings. Position the probe in the canal so that the infrared beam is aimed at the tympanic membrane, or otherwise the measurement will be invalid. Wait for 2 to 3 seconds until the digital temperature reading appears. This method takes advantage of the location of the temporal artery, which branches off the external carotid artery and lies within a millimeter of the skin surface of the forehead, cheek, and behind the ear lobes. Place the probe against the center of the forehead, depress the infrared scanning button, and brush the device across the forehead, down the cheek, and behind an earlobe. Read the display, which records the highest measure temperature. Industry information suggests that combined forehead and behind-the-ear contact is more accurate than scanning only the forehead is exposure to cold. Other causes include reduced movement as in paralysis, interference with vasoconstriction from sepsis or excess alcohol, starvation, hypothyroidism, and hypoglycemia. Older adults are especially susceptible to hypothermia and also less likely to develop fever. -Unable to Korotkoff sounds= use alternative methods using a doppler probe or direct arterial pressure tracings. Chapter 6 Integumentary Assessment and Modification for Age Dermoscopy- office practice for determining lesion benign vs malignant Normal VS. Abnormal Findings and Interpretation Melanoma pg 176 - Least common skin cancer but most lethal - Melanoma risk tool: 5 year risk of developing melanoma based on geographic location, gender, race, age, history of blistering sunburns, complexion, number of size of moles, freckling, and sun damage. - Risk factors: family history, > 50 common moles, Atypical/large moles, Red or light hair, Solar lentingines (acquired brown macules on sun-exposed areas), Freckles, UV radiation from heavy sun exposure, light eye or skin color, severe blistering sunburns in childhood, HIV or chemo, personal history of nonmelanoma skin cancer -Signs of sun damage: solar lentigines, solar elastosis, cutis rhomboidails, actinic purpa -Prevention: regular use of sunscreen at least SPF 30 -Full body examinations for patients over 50 -At least half of melanomas arise de novo form isolated melanocytes rather than pre- existing - use screening ABCE-EFG pg 178-179 -Asymmetry (one side of mole compared to other) -Border Irregularity (ragged, notched, or blurred) blue or black within a larger pigmented lesion is concerning for melanoma -Color Variations (more than two colors, especially blue-black, white, or red). -Diameter > 6mm (size of a pencil eraser) -Evolving (or changing rapidly in size, symptoms, or morphology) THE MOST SENSITIVE of CRITERIA -Elevated, Firm to palpation, Growing progressively over several weeks -HIGH RISK: a personal or family history of multiple or dysplastic nevi or pervious melanoma Primary and Secondary Skin Lesion Nomenclature Skin Lesions: flat, raised, vesicle, bulla, erosions, ulcers, nodules, ecchymoses, petechiae, palpable purpura. -Primary= flat, a macule or patch; raised, a papule or plaque ● Flat: You cannot palpate the lesion with your eyes closed. ● Macule: Lesion is flat and <1 cm. ● Patch: Lesion is flat and >1 cm. ● Raised: You can palpate the lesion with eyes closed. ● Papule: Lesion is raised, <1 cm, and not fluid filled. ● Plaque: Lesion is raised, >1 cm, but not fluid filled. Fluid ● Vesicle: Lesion is raised, <1 cm, and filled with fluid. ● Bulla: Lesion is raised, >1 cm, and fluid filled. Secondary Lesion=Acne with pitting and scars Number: Lesions can be solitary or multiple. If multiple, record how many. Consider estimating the total number of the type of lesion you are describing. Size: Measure with a ruler in millimeters or centimeters. For oval lesions, Measure in the long axis, then perpendicular to the axis. Shape: Some good words to learn are "circular," "oval," "annular" (ring-like, with central clearing), "nummular" (coin-like, no central clearing), and "Polygonal." Color: Use your imagination and be creative. Refer to a color wheel, if needed. There are many shades of tan and brown, but start with tan, light brown, and Dark brown if you are having trouble. Use "skin-colored" to describe a lesion that is the same shade as the patient’s skin. For red lesions or rashes, blanch the lesion by pressing it firmly with your finger or a glass slide to see if the redness temporarily lightens then refills. Texture: Palpate the lesion to see if it is smooth, fleshy, verrucous or warty, or scaly (fine, keratotic, or greasy scale). Location: Be as specific as possible. For single lesions, measure their distance from other landmarks (e.g., 1 cm lateral to left oral commissure). Configuration: Although not always necessary, describing patterns is often very helpful. Psoriasis pg 192 Table 6-1 If raised spot is small (<1 cm)= papule If raised spot is larger (>1 cm)=plaque -Guttate Psoriasis (papules raised, small)- scattered erythematous round drop-like, flat topped well circumscribed scaling papules and plaques on the trunk -Plaque psoriasis :Plaques (raised, large)- scattered erythematous to bright pink well- circumscribed flat-topped plaques on extensor knees and elbows, with overlying silvery scale -Tinea versicolor: multiple 2-5 mm hypopigmented, hyperpigmented, or tan round to oval macules on upper neck and back, upper chest, and arms with slight inducible scale on scraping -Tinea Cruris: bilateral erythematous, geographic patches with peripheral scaling, on the inner thighs bilaterally, sparing the scrotum “jock itch” Pityriasis Rosea pg 193 looks like ringworm Single, oval, flat topped superficial erythematous to skin-colored plaque on right abdomen= herald patch of pityriasis. Pityriasis Rosea=multiple round to oval scaling violaceous plaques on abdomen and back Chapter 7 Lymph Nodes The deep cervical chain is largely obscured by the overlying sternocleidomastoid muscle, but at its two extremes, the tonsillar node and supraclavicular nodes may be palpable. The submandibular nodes lie superficial to the submandibular gland, and should be differentiated. Nodes are normally round or ovoid, smooth, and smaller than the submandibular gland. The gland is larger and has a lobulated, slightly irregular surface (see p. 254). Note that the tonsillar, submandibular, and sub-mental nodes drain portions of the mouth and throat as well as the face. Lymphatic drainage patterns are helpful when assessing possible malignancy or infection: For suspected malignant or inflammatory lesions, look for enlargement of the neighboring regional lymph nodes; when a node is enlarged or tender, look for a source in its nearby drainage area. Assessing Lymph Nodes: 1. Inspect the neck, noting its symmetry and any masses or scars. Look for enlargement of the parotid or submandibular glands, and note any visible lymph nodes. 2. Palpate the lymph nodes. Using the pads of your index and middle fingers, press gently, moving the skin over the underlying tissues in each area. The patient should be relaxed, with the neck flexed slightly forward and, if needed, turned slightly toward the side being examined. You can usually examine both sides at once, noting both the presence of lymph nodes as well as asymmetry. For the submental node, however, it is helpful to feel with one hand while bracing the top of the head with the other. Feel in sequence for the following nodes 1. Preauricular—in front of the ear 2. Posterior auricular—superficial to the mastoid process 3.Occipital—at the base of the skull posteriorly 4.Tonsillar—at the angle of the mandible 5. Submandibular—midway between the angle and the tip of the mandible. These nodes are usually smaller and smoother than the lobulated submandibular gland against which they lie. 6. Submental—in the midline a few centimeters behind the tip of the mandible. 7.Superficial cervical—superficial to the sternocleidomastoid. 8. Posterior cervical—along the anterior edge of the trapezius. 9. Deep cervical chain—deep to the sternocleidomastoid and often inaccessible to examination. Hook your thumb and fingers around either side of the sternocleidomastoid muscle to find them. 10. Supraclavicular—deep in the angle formed by the clavicle and the sternocleidomastoid. Note lymph nodes size, shape, delimitation (discrete or matted together), mobility, consistency, and any tenderness. Small, mobile, discrete, nontender nodes, sometimes termed “shotty,” are frequently found in normal people. Describe enlarged nodes in two dimensions, maximal length and width, for example, 1 cm × 2 cm. Also note any overlying skin changes (erythema, induration, drain-age, or breakdown). Enlarged or tender nodes, if unexplained, call for (1) re-examination of the regions they drain and (2) careful assessment of lymph nodes in other regions to identify regional from generalized lymphadenopathy. For preauricular and cervical lymph nodes, adopt the techniques to follow. • Using the pads of the second and third fingers, palpate the preauricular nodes with a gentle rotary motion. Then examine the posterior auricular and occipital lymph nodes. • Palpate the anterior superficial and deep cervical chains, located anterior and superficial to the sternocleidomastoid. Then palpate the posterior cervical chain along the trapezius (anterior edge) and along the sternocleidomastoid (posterior edge). Flex the patient’s neck slightly forward toward the side being examined. Examine the supraclavicular nodes in the angle between the clavicle and the sternocleidomastoid). ***If you feel supraclavicular lymph nodes, a thorough work-up is warranted. Enlargement of supraclavicular lymph node – especially on the left suggests possible metastasis from a thoracic or abdominal malignancy.***Occasionally, you may mistake a band of muscle or an artery for a lymph node. Unlike a muscle or an artery, that **Tender nodes suggest inflammation. Hard or fixed nodules (fixed to underlying structures and not moveable on palpation) suggest malignancy. Cranial Nerves Cranial Nerves MNEUMONI C CRANIAL NERVE MOTOR/SENSOR Y MNEUMONIC On I Olfactory Sensory Some Old II Optic Sensory Say Olympus III Occularmotor Motor Marry Towering IV Trochlear Motor Money Tops V Trigeminal Both But A VI Abduscens Motor My Frenchman VII Facial Both Brother And VIII Acoustic Sensory Says German IX Glossopharyngeal Both Big Viewed X Vagus Both Brains Some XI Spinal Accessory Motor Matter Hops XII Hypoglossal Motor Most HEENT Assessment and Modification for Age/Normal vs Abnormal Findings and Interpretation HEENT Assessment and Modifications for Age. Normal and Abnormal Findings HEAD 1. Hair and scalp…Note its quantity, distribution, texture, and any pattern of loss. You may see loose flakes of dandruff. Part the hair in several places and look for scaliness, lumps, nevi, or other lesions. Fine hair is seen in hyperthyroidism, coarse hair in hypothyroidism. Tiny white ovoid granules that adhere to hairs may be nits (lice eggs). Look for redness and scaling that may indicate seborrheic dermatitis or psoriasis; soft lumps that may be pilar cysts (wens); and pigmented nevi that raise concern of melanoma. 2. Skull…. Observe the general size and contour of the skull. Note any deformities, depressions, lumps, or tenderness. Learn to recognize the irregularities in a normal skull, such as those near the suture lines between the parietal and occipital bones. a. An enlarged skull may signify hydrocephalus or Paget disease of bone. Palpable tenderness or bony step-offs may be present after head trauma 3. Face….Note the patient’s facial expression and contours. Observe for asymmetry, involuntary movements, edema, and masses 4. Skin… Observe the skin on the face and head, noting its color, pigmentation, texture, thickness, hair distribution, and any lesions a. Acne is common in adolescents. Hirsutism (excessive facial hair) may appear in some women with polycystic ovary syndrome EYES… Techniques of Examination Important Areas of Examination ● Visual acuity ● Visual fields ● Conjunctiva and sclera ● Cornea, lens, and pupils ● Extraocular movements= H test CN 3,4,6 ● Fundi, including: Optic disc and cup, retina, and retinal vessels -A light beam shining onto one retina causes pupillary constriction in both that eye, termed the direct reaction to light, and in the contra-lateral eye, the consensual reaction to light. -In the near reaction, when a person shifts gaze from a far object to a near object, the pupils constrict. Extraocular movement…. The coordinated action of six muscles, the four rectus and two oblique, control the eye. You can test the function of each muscle and its CN innervation by asking the patient to move the eye in the direction controlled by that muscle. Visual acuity To test the acuity of central vision, use a well-lit Snellen eye chart, if possible. Position the patient 20 feet from the chart. Patients who wear glasses other than for reading should put them on. Ask the patient to cover one eye with a card (to prevent looking through the fingers) and to read the smallest line of print possible. A patient who cannot read the largest letter should be positioned closer to the chart; note the intervening distance. Identify the smallest line of print where the patient can identify more than half the letters. Record the visual acuity designated at the side of this line, along with use of glasses, if any. Testing near vision with a hand-held card can help identify the need for reading glasses or bifocals in patients older than 45 years. If patients cannot read even the largest letters, test their ability to count your upraised fingers and distinguish light (such as your flashlight) from dark. a. Myopia (nearsightedness) causes focusing problems for distance vision. b. Presbyopia(farsighted) causes focusing problems for near vision, found in middle-aged and older adults. A presbyopic person often sees better when the card is farther away. c. legally blind when vision in the better eye, corrected by glasses, is 20/200 or less. Legal blindness also results from a constricted field of vision: 20° or less in the better eye. d. Vision of 20/200 means that at 20 feet the patient can read print that a person with normal vision could read at 200 feet. The larger the second number, the worse the vision. “20/40 corrected” means the patient could read the 20/40 line with glasses (a correction). Visual fields Recent studies recommend combining two tests to achieve the best results: the static finger wiggle test and the kinetic red target test. Static finger wiggle test: Position yourself about an arm’s length away from the patient. Close one eye and have the patient cover the opposite eye while staring at your open eye. So, for example, when the patient covers the left eye, to test the visual field of the patient’s right eye you should cover your right eye to mimic the patent’s field of view. Place your hands about 2 feet apart out of the patient’s view, roughly lateral to the patient’s ears. While in this position, wiggle your fingers and slowly bring your moving fingers forward into the patient’s center of view. Ask the patient to tell you as soon as he or she sees your finger movement. Test each clock hour, or at least each quadrant. Test each eye individually and record the extent of visits in each area. Note any abnormal “field cuts” Kinetic Red Target Test. Facing the patient, move a 5-mm red-topped pin inward from beyond the boundary of each quadrant along a line bisecting the horizontal and vertical meridians. Ask the patient when the pin first appears to be red. -An enlarged blind spot occurs in conditions affecting the optic nerve such as glaucoma, optic neuritis, and papilledema. -Graves disease or ocular tumors: Abnormalities include esotropia (inward deviation) or exotropia (out-ward deviation) of the eyes and also abnormal protrusion -Seborrheic dermatitis scaliness, lateral sparseness in hypothyroidism. -Down Syndrome Upslanting palpebral fissures. - Blepharitis- Red inflamed lid margins, often with crusting. Position and Alignment of the Eyes. Stand in front of the patient and survey the eyes for position and alignment. If one or both eyes seem to protrude, assess them from above (see p. 264). Eyebrows. Inspect the eyebrows, noting their fullness, hair distribution, and any scaliness of the underlying skin. Eyelids. Note the position of the lids in relation to the eyeballs. Inspect for the following: ■ Width of the palpebral fissures ■ Edema of the lids ■ Color of the lids ■ Lesions ■ Condition and direction of the eyelashes Adequacy of eyelid closure. Look for this especially when the eyes are unusually prominent, when there is facial paralysis, or when the patient is unconscious. Failure of the eyelids to close exposes the corneas to serious damage. Lacrimal Apparatus: Briefly inspect the regions of the lacrimal gland and lacrimal sac for swelling. -Excessive tearing->increased production -Conjunctival inflammation or corneal irritation -Impaired drainage, caused by ectropion and nasolacrimal duct obstruction. -Dryness from impaired secretion is seen in Sjogren syndrome. Conjunctiva and sclera. Ask the patient to look up as you depress both lower lids with your thumbs, exposing the sclera and conjunctiva. Inspect the sclera and palpebral conjunctiva for color. Note the vascular pattern against the white scleral background. If you need a fuller view of the eye, rest your thumb and finger on the bones of the cheek and brow, respectively, and spread the lids. Ask the patient to look to each side and down. This technique gives you a good view of the sclera and bulbar conjunctiva, but not of the palpebral conjunctiva of the upper lid. For this, you need to evert the lid. Cornea and Lens: With oblique lighting, inspect the cornea of each eye for opacities. Note any opacities in the lens that may be visible through the pupil. At the same time, inspect each iris. The markings should be clearly defined. With your light shining directly from the temporal side, look for a crescentic shadow on the medial side of the iris. Because the iris is normally fairly flat and forms a relatively open angle with the cornea, this lighting casts no shadow. a. Occasionally, the iris bows abnormally far forward, forming a very narrow angle with the cornea. The light then casts a crescentic shadow as shown here. This narrow angle increases the risk for acute narrow-angle glaucoma a sudden increase in IOP when drainage of the aqueous humor is blocked. In open-angle glaucoma, the common form of glaucoma, the normal spatial relation between iris and cornea is preserved and the iris is fully lit. b. Pupils. Light each eye from the side for inspection. In a dim light, inspect the size, shape, and symmetry of both pupils. Measure the pupils with a card showing black circles of varying sizes, and test the light reaction. Note if the pupils are large (>5 mm), small (<3 mm), or unequal. -Miosis refers to constriction of the pupils -Mydriasis to dilation. c. Pupillary sizes. Simple anisocoria, or a difference in pupillary diameter of 0.4 mm or greater without a known pathologic cause, is visible in approximately 35% of healthy people, and rarely exceeds 1 mm. -Simple anisocoria is considered benign if it is equal in dim and bright light, and there is brisk pupillary constriction to light (the light reaction). d. The Light Reaction. In dim light, test the pupillary reaction to light. Ask the patient to look into the distance, and shine a bright light obliquely into each pupil in turn. Both the distant gaze and the oblique lighting help to prevent a near reaction. Extraocular muscles The normal conjugate movements of the eyes in each direction. Note any deviation from normal, or dysconjugate gaze. ■ Nystagmus: a fine rhythmic oscillation of the eyes. A few beats of nystagmus on extreme lateral gaze are normal. If you see this, bring your finger in to within the field of binocular vision and look again. ■ Lid lag as the eyes move from up to down Test the Six EOMs (Extraocular Muscles): CN 3,4,6 Ask the patient to follow your finger or pencil as you sweep through the six cardinal directions of gaze. Making a wide H in the air, lead the patient’s gaze (Fig. 7-25): 1. to the patient’s extreme right, 2. to the right and upward, and 3. down on the right; then 4. without pausing in the middle, to the extreme left, 5. to the left and upward, and 6. down on the left. Pause during upward and lateral gaze to detect nystagmus. Move your finger or pencil at a comfortable distance from the patient. *Because middle-aged or older adults may have difficulty focusing on near objects, increase this distance. Some patients move their heads to follow your finger. If necessary, hold the head in the proper midline position. If you suspect lid lag or hyperthyroidism, ask the patient to follow your finger again as you move it slowly from up to down in the midline. The upper eyelid should overlap the iris slightly throughout this movement. The Optic Disk Inspect the optic disc. Note the following features: ● The sharpness or clarity of the disc outline. The nasal portion of the disc mar-gin may be somewhat blurred, a normal finding. ● The color of the disc, normally yellowish orange to creamy pink. White or pigmented crescents may ring the disc, a normal finding. ● The size of the central physiologic cup, if present. It is usually yellowish white. The horizontal diameter is usually less than half the horizontal diameter of the disc. ● The comparative symmetry of the eyes and findings in the fundi FINDINGS: In a refractive error, light rays from a distance do not focus on the retina -In myopia, they focus anterior to the retina -hyperopia, posterior to it -Retinal structures in a myopic eye look larger than normal -An enlarged cup suggests chronic open-angle glaucoma Detecting Papilledema Swelling of the optic disc and anterior bulging of the physiologic cup suggest papilledema= increased intracranial pressure. -This pressure is transmitted to the optic nerve, causing stasis of axoplasmic flow, intra- axonal edema, and swelling of the optic nerve head. Papilledema signals serious disorders of the brain, such as meningitis, subarachnoid hemorrhage, trauma, and mass lesions, so searching for this important disorder is a priority during all your funduscopic examinations . -Inspect the fundus for spontaneous venous pulsations (SVPs), rhythmic variations in the caliber of the retinal veins as they cross the fundus (narrower in systole; wider in diastole), present in 90% of normal patients. -The Retina—Arteries, Veins, Fovea, and Macula ● Inspect the retina, including arteries and veins as they extend. Arteries are light red, smaller, and bright. Veins are dark red, larger, and inconspicuous or absent. Lesions of the retina can be measured in terms of “disc diameters” from the optic disk. -Inspect the fovea and surrounding macula. Direct your light beam laterally or ask the patient to look directly into the light. In younger people, the tiny bright reflection at the center of the fovea helps to orient you; shimmering light reflections in the macular area are common. -Macula Light reflection/Macular degeneration is an important cause of poor central vision in older adults. Types include dry atrophic (more common but less severe) and wet exudative, or neovascular. Cellular debris, called drusen, may be hard and sharply defined or soft and confluent with altered pigmentation. Vitreous floaters are dark specks or strands seen between the fundus and the lens. Cataracts are densities in the lens EARS The Ear Anatomy and Physiology. The ear has three compartments: the external ear, the middle ear, and the inner ear. The External Ear 1. The external ear comprises the auricle and ear canal. The auricle consists chiefly of cartilage covered by skin and has a firm elastic consistency. Its prominent curved outer ridge is the helix. Parallel and anterior to the helix is another curved prominence, the antihelix. Inferiorly is the fleshy projection of the earlobe, or lobule. The ear canal opens behind the tragus, a nodular protrusion that points backward over the entrance to the canal. The ear canal curves inward and is approximately 24 mm long. Cartilage encases its outer two thirds. In this segment, the skin is hairy and contains glands that produce cerumen (wax). The inner third of the canal is surrounded by bone and lined by thin, hairless skin. Pressure on this latter area causes pain—a point to remember when you when you examine the ear. At the end of the ear canal lies the lateral tympanic membrane, or eardrum, marking the medial limit of the external ear. The external ear captures sound waves for transmission into the middle and inner ear. 2. The Middle Ear. In the air-filled middle ear, the ossicles—the malleus, the incus, and the stapes—transform sound vibrations into mechanical waves for the inner ear. The proximal end of the eustachian tube connects the middle ear to the nasopharynx. Two of the ossicles are visible through the tympanic membrane, and are angled obliquely and held inward at its center by the malleus (Fig. 7-36). Find the handle and the short process of the malleus, the two chief landmarks. From the umbo, where the eardrum meets the tip of the malleus, a light reflection called the cone of light fans down-ward and anteriorly. Above the short process lies a small portion of the eardrum called the pars flaccida. The remainder of the drum is the pars tensa. Anterior and posterior malleolar folds, which extend obliquely upward from the short process, separate the pars flaccida from the pars tensa, but are usually invisible unless the eardrum is retracted. A second ossicle, the incus, can sometimes be seen through the drum. 3. The Inner Ear. The inner ear includes the cochlea, the semicircular canals, and the distal end of the auditory nerve, also known as the vestibulocochlear nerve, or CN VIII. Movements of the stapes vibrate the perilymph in the labyrinth of the semicircular canals and the hair cells and endolymph in the ducts of the cochlea, producing electrical nerve impulses transmitted by the auditory nerve to the brain. Much of the middle ear and all of the inner ear are inaccessible to direct examination. Assess their condition by testing auditory function. a. Hearing disorders of the external and middle ear cause conductive hearing loss. External ear causes include cerumen impaction, infection (otitis externa), trauma, squamous cell carcinoma, and benign bony growths such as exostoses or osteomas. Middle ear disorders include otitis media, congenital conditions, cholesteatomas and otosclerosis, tumors, and perforation of the tympanic membrane. Bone conduction Disorders of the inner ear cause sensorineural hearing loss from congenital and hereditary conditions, presbycusis, viral infections such as rubella and cytomegalovirus, Ménière disease, noise exposure, ototoxic drug exposure, and acoustic neuroma. b. Air conduction (AC) describes the normal first phase in the hearing pathway. An alternative pathway, known as bone conduction (BC), bypasses the external and middle ear and is used for testing purposes. A vibrating tuning fork, placed on the head, sets the bone of the skull into vibration and stimulates the cochlea directly. In those with normal hearing, AC is more sensitive than BC (AC > BC). c. Equilibrium. The labyrinth of three semicircular canals in the inner ear senses the position and movements of the head and helps maintain balance. EAR ASSESSMENT 1. The Auricle. Inspect the auricle and surrounding tissue for deformities, lumps, or skin lesions. 2. Ear Canal and Drum. To see the ear canal and drum, use an otoscope with the largest ear speculum that inserts easily into the canal. Position the patient’s head so that you can see comfortably through the otoscope. To straighten the ear canal, grasp the auricle firmly but gently and pull it upward, backward, and slightly away from the head. Movement of the auricle and tragus (the “tug test”) is painful in acute otitis externa (inflammation of the ear canal), but not in otitis media (inflammation of the middle ear). Tenderness behind the ear occurs in otitis media. -Exostoses Nontender nodular swellings covered by normal skin deep in the ear canals suggest exostoses (nonmalignant overgrowths which may obscure the eardrums). Inspect the ear canal, noting any discharge, foreign bodies, redness of the skin, or swelling. -Cerumen which varies in color and consistency from yellow and flaky to brown and sticky or even to dark and hard, may wholly or partly obscure your view. Inspect the eardrum, noting its color and contour -The cone of light—usually easy to see—helps to orient you. -In chronic otitis externa, the skin of the canal is often thickened, red, and itchy. -Acute purulent otitis media- red bulging drum and amber drum of a serous effusion. Testing Auditory Acuity—Whispered Voice Test. To begin screening, ask the patient “Do you feel you have a hearing loss or difficulty hearing?” If the patient reports hearing loss, proceed to the whispered voice test. The whispered voice test is a reliable screening test for hearing loss if the examiner uses a standard method of testing and exhales before whispering. Whispered Voice Test for Auditory Acuity ● Stand 2 feet behind the seated patient so that the patient cannot read your lips. Occlude the non-test ear with a finger and gently rub the tragus in a circular motion to prevent transfer of sound to the non-test ear. ● Exhale a full breath before whispering to ensure a quiet voice. ● Whisper a combination of three numbers and letters, such as 3-U-1. Use a different number/letter combination for the other ear. ● Interpretation: -Normal: Patient repeats initial sequence correctly. Normal: Patient responds incorrectly, so test a second time with a different number/letter combination; patient repeats at least three out of the possible six numbers and letters correctly. -Abnormal: Four of the six possible numbers and letters are incorrect. Conduct further testing by audiometry Note that older adults with presbycusis have higher frequency hearing loss, making them more likely to miss consonants, which have higher frequency sounds than vowels Testing for Conductive Versus Neurosensory Hearing Loss: Tuning Fork Tests. For patients failing the whispered voice test, the Weber and Rinne fork tests may help determine if the hearing loss is conductive or sensorineural in origin. However, their precision, or test–retest reproducibility, and their accuracy compared to air–bone gap reference standards have been questioned. -To conduct these tests, make sure the room is quiet, and use a tuning fork of 512 Hz. These frequencies fall within the range of conversational speech, namely 500 to 3,000 Hz and between 45 and 60 decibels. Set the fork into light vibration by briskly stroking it between the thumb and index finger ( Note that older adults with presbycusis have higher frequency hearing loss, making them more likely to miss consonants, which have higher frequency sounds than vowels. ) or by tapping it on your forearm just in front of your elbow. -Test for lateralization (Weber test). Place the base of the lightly vibrating tuning fork firmly on top of the patient’s head or on the midforehead. -In unilateral conductive hearing loss, sound is heard in (lateralized to) the impaired ear. Explanations include otosclerosis, otitis media, perforation of the eardrum, and cerumen. Ask where the patient hears the sound: on one side or both sides? Normally, the vibration is heard in the midline or equally in both ears. If nothing is heard, try again, pressing the fork more firmly on the head. Restrict this test to patients with unilateral hearing loss since patients with normal hearing may lateralize, and patients with bilateral conductive or sensorineural deficits will not lateralize. ■ Compare AC and BC (Rinne test). Place the base of a lightly vibrating tuning fork on the mastoid bone, behind the ear and level with the canal. When the patient can no longer hear the sound, quickly place the fork close to the ear canal and ask if the patient hears a vibration. Here, the “U” of the fork should face forward, which maximizes sound transmission for the patient. Normally, the sound is heard longer through air than through bone (AC > BC) In unilateral sensorineural hearing loss= sound is heard in the good ear In conductive hearing loss= sound is heard through bone as long as or longer than it is through air (BC = AC or BC > AC). In sensorineural hearing loss=sound is heard longer through air (AC > BC). NOSE Techniques of Examination. Inspect the anterior and inferior surfaces of the nose. Gentle pressure on the tip of the nose with your thumb usually widens the nostrils. Use a penlight or otoscope light to obtain a partial view of each nasal vestibule. If the nasal tip is tender, be gentle and manipulate the nose as little as possible. Note any asymmetry or deformity of the nose. -Tenderness of the nasal tip or alae suggests local infection such as a furuncle, particularly if there is a small erythematous and swollen area. -Test for nasal obstruction, if indicated, by pressing on each alnasi in turn and asking the patient to breathe in. Inspect the inside of the nares with an otoscope and the largest available ear speculum.* Tilt the patient’s head back a bit and insert the speculum gently into the vestibule of each nostril, avoiding contact with the sensitive nasal septum. By directing the speculum posteriorly, then upward in small steps, try to see the inferior and middle turbinates, the nasal septum, and the narrow nasal passage between them. Some asymmetry of the two sides is normal. Inferior and middle turbinates. Inspect the nasal mucosa, the nasal septum, and any abnormalities. Inspect: ■ The nasal mucosa that covers the septum and turbinates. Note its color and any swelling, bleeding, or exudate. If exudate is present, note its character: clear, mucopurulent, or purulent. The nasal mucosa is normally somewhat redder than the oral mucosa. ■ The nasal septum. Note any deviation, inflammation, or perforation of the septum. The lower anterior portion of the septum (where the patient’s finger can reach) is a common source of epistaxis (nosebleed). -In viral rhinitis, the mucosa is reddened and swollen -allergic rhinitis, it may be pale, bluish, or red. Fresh blood or crusting may be seen. -Causes of septal perforation include trauma, surgery, and intranasal use of cocaine or amphetamines, which also cause septal ulceration. Palpate for sinus tenderness. Press up on the frontal sinuses from under the bony brows, avoiding pressure on the eyes. Then press up on the maxillary sinuses. -Local tenderness, together with symptoms such as facial pain, pressure or fullness, purulent nasal discharge, nasal obstructions, and smell disorder, especially when present for >7 days, suggest acute bacterial rhinosinusitis involving the frontal or maxillary sinuses. THROAT Techniques of Examination. If you detect any suspicious ulcers or nodules, put on a glove and palpate any lesions, noting any thickening or infiltration of the tissues that might suggest malignancy. Inspect the following: -The Lips. Observe their color and moisture, and note any lumps, ulcers, cracking, or scaliness. -The Oral Mucosa. Look into the patient’s mouth and, with a good light and the help of a tongue blade, inspect the oral mucosa for color, ulcers, white patches, and nodules. In this patient the wavy white line on the adjacent buccal mucosa developed where the upper and lower teeth meet, related to irritation from sucking or chewing. -The Gums and Teeth. Note the color of the gums, which are normally pink. Brown patches may be present, especially but not exclusively in dark-skinned individuals. Inspect the gum margins and the interdental papillae for swelling or ulceration. Inspect the teeth. Are any of them missing, discolored, misshapen, or abnormally positioned? To assess tooth, jaw, or facial pain, palpate the teeth for looseness and the gums with your gloved thumb and index finger. -The Roof of the Mouth. Inspect the color and architecture of the hard palate. A. Torus palatinus is a startling but benign midline lump B. Redness of the gingiva suggests gingivitis, a black line might indicate lead poisoning. The interdental papillae are swollen in gingivitis. C. Bright red edematous mucosa underneath a denture suggests denture stomatitis (denture sore mouth). There may be ulcers or papillary granulation tissue. Wearing gloves, palpate any lesions. Ask the patient to protrude the tongue. With your right hand, grasp the tip of the tongue with a square of gauze and gently pull it to the patient’s left. Inspect the side of the tongue, and then palpate it with your gloved left hand, feeling for any induration. Men aged >50 years, smokers, and heavy users of chewing tobacco and alcohol are at highest risk for cancers of the tongue and oral cavity, usually squamous cell carcinomas on the side or base of the tongue. Any persistent nodule or ulcer, red or white, is suspect, especially if indurated. These discolored lesions represent erythroplakia and leukoplakia and should be biopsied. Inspection and palpation remain the standard for detection of oral cancers. Pharynx With the patient’s mouth open but the tongue not protruded, ask the patient to say “ah” or yawn. This action helps you see the posterior pharynx well. You can also ask the patient to “open the back of your throat” since many adults have learned to inspect their own posterior pharynx while looking into a mirror. Alternatively, you can press a tongue blade firmly down on the midpoint of the arched tongue—back far enough to visualize the pharynx but not so far that you cause gagging. Simultaneously, ask for an “ah” or a yawn. Note the rise of the soft palate—a test of CN X (the vagal nerve). In CN X paralysis, the soft palate fails to rise and the uvula deviates to the opposite side (points “away from the lesion”). Inspect the soft palate, anterior and posterior pillars, uvula, tonsils, and pharynx. -Note their color and symmetry and look for exudate, swelling, ulceration, or tonsillar enlargement. If possible, palpate any suspicious area for induration or tenderness. Tonsils have crypts, or deep infoldings of squamous epithelium, where whitish spots of normal exfoliating epithelium may sometimes be seen. Discard your tongue blade after use. Neck ■ Observe the patient swallowing. Ask the patient to sip some water and to extend the neck again and swallow. Watch for upward movement of the thyroid gland, noting its contour and symmetry. The thyroid cartilage, the cricoid cartilage, and the thyroid gland all rise with swallowing and then fall to their resting positions -Auscultate breath sounds over the trachea. This allows subtle counting of the respiratory rate and establishes a point of reference when assessing upper versus lower airway causes of shortness of breath. When assessing shortness of breath, always remember to listen over the trachea for stridor for upper airway etiologies in addition to examining the lungs. Stridor is an ominous, high-pitched musical sound from severe subglottic or tracheal obstruction that signals a respiratory emergency. -Causes include epiglottitis, foreign body, goiter, and stenosis from placement of an artificial airway. -Inspect the neck for the thyroid gland. Tip the patient’s head slightly back. Using tangential lighting directed downward from the tip of the patient’s chin, inspect the region below the cricoid cartilage to identify the contours of the gland. Confirm your visual observations by palpating the gland outlines as you stand facing the patient. This helps prepare you for the more systematic palpation to follow. - Palpate the thyroid gland. Find your landmarks—the notched thyroid cartilage and the cricoid cartilage below it Locate the thyroid isthmus, usually overlying the second, third, and fourth tracheal rings. Palpate the thyroid gland. If the lower pole of the thyroid gland is not palpable, suspect a retrosternal location. If the thyroid gland is retrosternal, below the suprasternal notch, it is often not palpable. Steps for Palpating the Thyroid Gland (Posterior Approach) ● Ask the patient to flex the neck slightly forward to relax the sternocleidomastoid muscles. ● Place the fingers of both hands on the patient’s neck so that your index fingers are just below the cricoid cartilage. ● Ask the patient to sip and swallow water as before. Feel for the thyroid rising up under your finger pads. It is often, but not always, palpable. ● Displace the trachea to the right with the fingers of the left hand; with the right-hand fingers, palpate laterally for the right lobe of the thyroid in the space between the displaced trachea and the relaxed sternocleidomastoid. Find the lateral margin. In a similar fashion, examine the left lobe. The lobes are somewhat harder to feel than the isthmus, so practice is needed. The anterior surface of a lateral lobe is approximately the size of the distal phalanx of the thumb and feels somewhat rubbery. ● Note the size, shape, and consistency (soft, firm, or hard) of the gland and identify any nodules or tenderness. In general, benign (or colloid) nodules tend to be more uniform, ovoid structures and are not fixed to surrounding tissue. ● If the thyroid gland is enlarged, listen over the lateral lobes with a stethoscope to detect a bruit, a sound similar to a cardiac murmur but of not of cardiac origin. -When the thyroid gland is retrosternal, below the suprasternal notch, it is often not palpable. Retrosternal goiters can cause hoarseness, shortness of breath, stridor, or dysphagia from tracheal compression; neck hyperextension and arm elevation may cause flushing from compression of the thoracic inlet from the gland itself or from clavicular movement (Pemberton sign). -The thyroid is soft in Graves disease and may be nodular; it is firm in Hashi- moto thyroiditis (though not always uniformly) and malignancy. -The thyroid is tender in thyroiditis. -A localized systolic or continuous bruit may be heard in hyperthyroidism from Graves disease or toxic multinodular goiter. Visual Acuity=Snellen distance of patient from chart/distance a normal eye can read the line of letters - Visual decline normal with aging - assess any problems with face recognition, reading, performing tasks - Acuity tested by snellen eye chart: 20 feet from patient - Wear glasses , one eye at a time, read the smallest line of print possible - Visual acuity is expressed as two numbers (e.g., 20/30): the first indicates the distance of the patient from the chart, and the second, the distance at which a normal eye can read the line of letters. - Larger the number worse the vision Glaucoma=Optic disc Changes - Change in color and size of the optic disc - Leading cause of visual impairment and blindness (gradual loss of peripheral visual fields) IS TREATABLE - Loss of retinal ganglion cell axons: exam reveals pallor and increasing the size of the optic cup - Risk factors: African American, DM, Myopia, ocular hypertension Epistaxis - bleeding from nasal passage, paranasal sinuses or nasopharynx -Causes: trauma, inflammation, drying or crusting of nasal mucosa, tumors, foreign bodies, anticoagulants NSAIDS, vascular malformations, coagulopathies -Assess for hemoptysis and hematemesis Retinal Issues Cottonwood Patches & Drussen - Retina is found in the optic fundus - follow vessels peripherally in each direction (size and characteristics), ID any lesions: measured in terms of "disc diameters" - Fovea is the tiny bright reflection at the center: shimmering light reflections are common - look for opacities in the vitreous or lens (vitreous floaters are dark specs/strands send between fundus and lens) Cottonwood PATCHES: irregular patches= DM & HTN “Think of Tina” HARD DRUSSEN: Lipids and proteins/ older population, can lead to macular- degeneration. Citreous floaters are dark specs/strands between fundus and lens -A light beam shining onto one retina causes pupillary constriction in both that eye Chapter 8 - Lung/thorax assessment and modification for age Begin with inspection, then palpate, percuss, and auscultate o With patient sitting: examine posterior thorax and lungs. Arms should be folded across chest with hands resting on opposite shoulders if possible. This position increases access to lung fields. The ask pt to lie down. o With patient supine: Examine anterior thorax and lungs. This position allows breast to be gently displaced. It is acceptable to examine posterior and anterior chest with patient sitting. o EXAMINE POSTERIOR CHEST Inspection (shape of chest and how chest moves) • Assess for deformities or asymmetry of chest expansion o Asymmetric expansion occurs in large pleural effusions • Abnormal muscle retraction of the intercostal space during inspirations, most visible in the lower intercoastal spaces o Retraction occurs in severe asthma, COPD, or upper airway obstruction. • Impaired respiratory movement on one of both sides of a unilateral lag (or delay) in movement o Unilateral impairment or lagging suggests pleural disease from asbestosis or silicosis; it is also seen in phrenic nerve damage or trauma. Palpation (focus on areas of tenderness or bruising, respiratory expansion, and fremitus) • Intercostal tenderness can develop over inflamed pleurae, costal cartilage tenderness in costochondritis • Identify tender areas: palpate tender areas or where there is visible lesions or bruises. Nope any palpable crepitus (crackling sound over bones, joints, or skin with or without pain due to air in subq tissue. o Tenderness, bruising, and bony “step-offs” are common over a fractured rib. Crepitus may be palpable in overt fractures and arthritic joints; crepitus and chest wall edema are seen in mediastinitis. • Any skin abnormalities like masses or sinus tracts (blind, inflammatory, tube-like structures opening onto the skin) o Although rare, sinus tracts suggest infection of the underlying pleura and lung (as in tuberculosis or actino- mycosis). • Test Chest Expansion (or lung excursion): place thumbs at level of 10th ribs and hands lateral ribs loosely; tell patient to inhale deeply o Unilateral decrease or delay in chest expansion occurs in chronic fibrosis of the underlying lung or pleura, pleural effusion, lobar pneumonia, pleural pain with associated splinting, unilateral bronchial obstruction, and paralysis of the hemidiaphragm. • Palpate both lungs for symmetric tactile fremitus o Fremitus refers to the palpable vibrations that are transmitted through the bronchopulmonary tree to the chest wall as the patient is speaking and is normally symmetric. o Disappears below diaphragm. Easier to detect in the right lung than the left lung. o Imprecise assessment technique. o Ask patient to say “99” or “1-2-3” o Fremitus is decreased or absent when the voice is higher pitched or soft or when the transmission of vibrations from the larynx to the surface of the chest is impeded by a thick chest wall, an obstructed bronchus, COPD, or pleural effusion, fibrosis, air (pneumothorax), or an infiltrating tumor. o Asymmetric decreased fremitus raises the likelihood of unilateral pleural effusion, pneumothorax, or neoplasm, which decreases transmission of low-frequency sounds; Percussion: o Asymmetric increased fremitus occurs in unilateral pneumonia which increases transmission through consolidated tissue. • Percussion sets the chest wall and underlying tissues in motion, producing audible sound and palpable vibrations. Percussion helps you establish whether the underlying tissues are air-filled, fluid-filled, or consolidated. • Dullness replaces resonance when fluid or solid tissue replaces air-containing lung or occupies the pleural space beneath your percussing fingers. Examples include: lobar pneumonia, in which the alveoli are filled with fluid and blood cells; and pleural accumulations of serous fluid (pleural effusion), blood (hemothorax), pus (empyema), fibrous tissue, or tumor. Dullness makes pneumonic and pleural effusion three to four times more likely, respectively • Generalized hyperresonance is common over the hyperinflated lungs of COPD or asthma. Unilateral hyperresonance suggests a large pneumothorax or an air-filled bulla. Auscultation: • Before beginning auscultation, ask the patient to cough once or twice to clear mild atelectasis or airway mucus that can produce unimportant extra sounds. o Use ladder pattern to assess lungs. Hair can alter sounds; press harder or moisten hair on chest hair. o Air movement through a partially obstructed nose or nasopharynx can also introduce abnormal sounds. • Breath sounds usually louder at lower posterior lung fields. o Breath sounds may be decreased when air flow is decreased (as in obstructive lung disease or respiratory muscle weakness) or when the transmission of sound is poor (as in pleural effusion, pneumothorax, or COPD). o EXAMINE ANTERIOR CHEST: If performed with patient supine, arms should be slightly abducted. Raise HOB in those with difficulty breathing. Persons with severe COPD may prefer to sit leaning forward, with lips pursed during exhalation and arms supported on their knees or a table. Inspection • Observe shape, deformities, asymmetry of thorax • Check for abnormal retraction of the lower intercostal spaces during inspiration, or any supraclavicular retraction o Abnormal retraction occurs in severe asthma, COPD, or upper airway obstruction • Local lag or impairment of respiratory movement o Occurs in disease of lung or pleura Palpation • Identify tender area. o Tender pectoral muscles or costal cartilages suggest, but do not prove, that chest pain has a localized musculoskeletal origin. • Assess bruising, sinus tracts or skin changes. • Assess chest expansion. • Tactile fremitus Normally decreased or absent over precordium • The dullness of right middle lobe pneumonia typically occurs behind the right breast. Unless you displace the breast, you may miss the abnormal percussion note. - Normal VS abnormal findings and interpretation o Abnormalities in rate and rhythm of breathing (When observing respiratory patterns, note rate, depth, and regularity of patient’s breathing.) (p. 335) Normal: Adults – 14-20 per minute; infants – up to 44 per minute Slow breathing (bradypnea) - Slow breathing with or without an increase in tidal volume that maintains alveolar ventilation. Abnormal alveolar hypoventilation without increased tidal volume can arise from uremia, drug-induced respiratory depression, and increased intracranial pressure. Sighing Respiration- Breathing punctuated by frequent sighs suggests hyperventilation syndrome—a common cause of dyspnea and dizziness. Occasional sighs are normal. Rapid Shallow Breathing (Tachypnea)- Rapid shallow breathing has numerous causes, including salicylate intoxication, restrictive lung disease, pleuritic chest pain, and an elevated diaphragm Cheyne–Stokes Breathing - Periods of deep breathing alternate with periods of apnea (no breathing). This pattern is normal in children and older adults during sleep. Causes include heart failure, uremia, drug-induced respiratory depression, and brain injury (typically bihemispheric). Obstructive Breathing - In obstructive lung disease, expiration is prolonged due to narrowed airways increase the resistance to air flow. Causes include asthma, chronic bronchitis, and COPD. Rapid Deep Breathing (Hyperpnea, Hyperventilation) – • In hyperpnea, rapid deep breathing occurs in response to metabolic demand from causes such as exercise, high altitude, sepsis, and anemia. In hyperventilation, this pattern is independent of metabolic demand, except in respiratory acidosis. Light-headedness and tingling may arise from decreased CO2 concentration. In the comatose patient, consider hypoxia, or hypoglycemia affecting the midbrain or pons. Kussmaul breathing is compensatory over breathing due to systemic acidosis. The breathing rate may be fast, normal, or slow. Ataxic Breathing (Biot Breathing)- Breathing is irregular—periods of apnea alternate with regular deep breaths which stop suddenly for short intervals. Causes include meningitis, respiratory depression, and brain injury, typically at the medullary level. Tachypnea: >25 bpm • This increases the likelihood of pneumonia and cardiac disease o Assess for signs of respiratory distress: Assess for RR Inspect patient’s color for cyanosis or pallor. Check shape and color of fingernails. • Cyanosis in the lips, tongue, and oral mucosa signals hypoxia. • Pallor and sweating (diaphoresis) are common in heart failure. • Clubbing of the nails (see p. 211) occurs in bronchiectasis, congenital heart disease, pulmonary fibrosis, cystic fibrosis, lung abscess, and malignancy. Listen for audible sounds of breathing. Is there audible whistling during inspiration over neck or lungs? • Audible high-pitched inspiratory whistling, or stridor, is an ominous sign of upper airway obstruction in the larynx or trachea that requires urgent airway evaluation. • Wheezing is either expiratory or continuous. Inspect neck: During inspiration, is there contraction of the accessory muscles, namely the sternocleidomastoid muscle and scalene muscles, or supraclavicular retraction? During expiration, is there contraction of the intercostal or abdominal oblique muscles? Is the trachea midline? • Accessory muscle use signals difficulty breathing from COPD or respiratory muscle fatigue. Lateral displacement of the trachea occurs in pneumothorax, pleural effusion, and atelectasis. Barrel-chest appearance association with COPD. o Forced Expiratory Time: take a deep breath and breathe out. Quick and completely with mouth open; listen over trachea with diaphragm of stethoscope and count. Get 3 readings. Patients ≥age 60 years with a forced expiratory time of ≥9 seconds are four times more likely to have COPD. o Identify fracture rib: With one hand on sternum and one on thoracic spine, squeeze chest. Where is the pain? An increase in the local pain (distant from your hands) suggests rib fracture rather than just soft-tissue injury. - LUNG SOUNDS (breath sounds) o Adventitious (added) lung sounds: Causes and Qualities (p. 338) Crackles - Crackles are discontinuous nonmusical sounds that can be early inspiratory (as in COPD), late inspiratory (as in pulmonary fibrosis), or biphasic (as in pneumonia). When hearing crackles that do not clear with coughing, assess: loudness, pitch, and duration (fine or coarse), number, timing in resp cycle, location in chest wall, persistence of pattern from breath to breath, and any change after cough or position. • Fine crackles: softer, higher pitched, and more frequent per breath than coarse crackles. Heard from mid to late inspiration, especially in the dependent areas of the lung, and change according to body position. They have a shorter duration and higher frequency than coarse crackles. o Examples include pulmonary fibrosis (known for “Velcro rales”) and interstitial lung diseases such as interstitial fibrosis and interstitial pneumonitis. o Fine late inspiratory crackles that persist from breath to breath suggest abnormal lung tissue. • Coarse crackles; appear in early inspiration and last throughout expiration (biphasic), have a popping sound, are heard over any lung region, and do not vary with body position. They have a longer duration and lower frequency than fine crackles, change or disappear with coughing, and are transmitted to the mouth. Coarse crackles appear to result from “boluses of gas passing through airways as they open and close intermittently.” o Examples include COPD, asthma, bronchiectasis, pneumonia (crackles may become finer and change from mid to late inspiratory during recovery), and heart failure. o The crackles of heart failure are usually best heard in the posterior inferior lung fields. Wheezes and Rhonchi • Wheezes are continuous musical sounds that occur during rapid airflow when bronchial airways are narrowed almost to the point of closure. Wheezes can be inspiratory, expiratory, or biphasic. They may be localized, due to a foreign body, mucous plug, or tumor, or heard throughout the lung. o Although wheezes are typical of asthma, they can occur in a number of pulmonary diseases. • Rhonchi are considered by some to be a variant of wheezes, arising from the same mechanism, but lower in pitch. Unlike wheezes, rhonchi may disappear with coughing, so secretions may be involved. o Clearing of crackles, wheezes, or rhonchi after coughing or position change suggests inspissated secretions, seen in bronchitis or atelectasis. • Stridor is a continuous, high-frequency, high-pitched musical sound produced during airflow through a narrowing in the upper respiratory tract. Stridor is best heard over the neck during inspiration, but can be biphasic. Causes of the underlying airway obstruction include tracheal stenosis from intubation, airway edema after device removal, epiglottitis, foreign body, and anaphylaxis. Immediate intervention is warranted. Stridor and laryngeal sounds are loudest over the neck, whereas true wheezes and rhonchi are faint or absent over the neck. dysfunction can be transmitted to the chest and mistaken for wheezing, leading to inappropriate or delayed treatment inflammation and roughening of the visceral pleura as it slides against the parietal pleura. This nonmusical sound is biphasic, heard during inspiration and expiration, and often best heard in the axilla and base of the lungs. o Pleural rubs may be heard in pleurisy, pneumonia, and pulmonary embolism. Mediastinal Crunch (Hamman Sign) • A mediastinal crunch is a series of precordial crackles synchronous with the heartbeat, not with respiration. Best heard in the left lateral position, it arises from air entry into the mediastinum causing mediastinal emphysema (pneumomediastinum). It usually produces severe central chest pain and may be spontaneous. It has been reported in cases of tracheobronchial injury, blunt trauma, pulmonary disease, use of recreational drugs, childbirth, and rapid ascent from scuba diving. - Pneumonia o Pneumococcal Vaccination Streptococcal pneumonia causes pneumonia, bacteremia, and meningitis. Infants younger than age 2 years are vaccinated with the 13-valent pneumococcal conjugate vaccine (PCV13) Adults >65 are vaccinated with PVC13 and 23-valent inactivated pneumococcal polysaccharide vaccine (PPSV23). Adult who have not received the PPSV23 should 1st be given the PCV13 and then 6-12 months later, receive the PPSV23. Those who have previously been vaccinated with PPSV23 should receive a dose of PCV13 no earlier than 1 year following the recent PPSV23 vaccine. Use both vaccines for high-risk groups: • Adults >65 years • Children and adults from ages 2 to 64 years with chronic illnesses specifically associated with an increased risk of pneumococcal infection (sickle cell disease, cardiovascular and pulmonary disease, diabetes, alcoholism, cirrhosis, cochlear implants, and leaks of cerebrospinal fluid) • Any adult aged 19 to 64 years who is a smoker or has asthma • Adults and children older than age 2 years who are immunocompromised (including from HIV infection, AIDS, long-term steroids, Hodgkin disease, lymphoma or leukemia, kidney failure, multiple myeloma, nephrotic syndrome, organ transplant, damaged spleen or no spleen, radiation, or chemotherapy) • Residents of nursing homes or long-term care facilities o Lobar Pneumonia (consolidation): alveoli filled with fluid as in pneumonia. (p. 339) Percussion note: dull over airless area Trachea: midline Breath sounds: bronchial over the involved area Adventitious sounds: late inspiratory crackles over involved area Tactile fremitus and transmitted voice sounds: increased over the involved area, with egophony, bronchophony, and whispered pectoriloquy o Mycoplasma and viral pneumonias: cough and sputum include dry, hacking cough, may become productive and mucoid sputum. Associated with acute febrile illness, often with malaise, headache, and possibly dyspnea o Bacterial pneumonias: cough and sputum include sputum is mucoid or purulent; may be blood-streaked, diffusely pinkish, or rusty. Associated with acute illness with chills, often high fever, dyspnea, and chest pain. Commonly from streptococcus pneumonia, haemophilus influenza, Moraxella catarrhalis; klebsiella in alcoholism, especially in underlying smoking, chronic bronchitis and COPD, cardiovascular disease, diabetes. o Widespread, usually reversible, airflow obstruction with bronchial hyperresponsiveness and underlying inflammation. During attacks, as air flow decreases lungs hyperinflate. (p. 340) Percussion noted: Resonant to diffusely hyper-resonant Trachea: midline Breath sounds: often obscured by wheezes Adventitious sounds: wheezes, possible crackles Tactile fremitus and transmitted voice sounds: decreased Cough, at times with thick mucoid sputum, especially near end of an attack. Associated with episodic wheezing and dyspnea, but cough may occur alone. Often with a history of allergies. o In the advanced airway obstruction of severe asthma, wheezes and breath sounds may be absent due to low respiratory airflow (the “silent chest”), a clinical emergency. Chapter 16 Musculoskeletal Assessment and Modification for Age- -Osteoarthritis is more common in women. -The first goal of your evaluation of musculoskeletal disorders is to characterize the patient’s complaint in terms of four key features. Is the joint problem: ■ Articular or extra-articular ■ Acute (usually <6 weeks) or chronic (usually >12 weeks) ■ Inflammatory or noninflammatory ■ Localized (monoarticular) or diffuse (polyarticular) ● Articular structures include the joint capsule and articular cartilage, the synovium and synovial fluid, intra-articular ligaments, and juxta-articular bone. Articular disease typically involves swelling and tenderness of the entire joint, crepitus, instability, “locking,” or deformity, and limits both active and passive range of motion due to either stiffness or pain. ● Extra-articular structures include periarticular ligaments, tendons, bursae, muscle, fascia, bone, nerve, and overlying skin. Extra-articular disease typically involves “point or focal tenderness in regions adjacent to articular structures” and limits active range of motion. Extra-articular disease rarely causes swelling, instability, or joint deformity. -Age also provides clues to causes of joint pain: ■ If age <60 years, consider repetitive strain or overuse syndromes like tendinitis or bursitis, crystalline arthritis (gout; crystalline pyrophosphate deposition disease [CPPD]) (males), rheumatoid arthritis (RA), psoriatic arthritis and reactive (Reiter) arthritis (in inflammatory bowel disease [IBD]), and infectious arthritis from gonorrhea, Lyme disease, or viral or bacterial infections. TYPES OF JOINTS EXTENT OF MOVEMENT EXAMPLE Synovial Freely moveable Knee, shoulder Cartilagenous Slightly moveable Spine/vertebral column Fibrous Immoveable Bones of the skull Normal vs Abnormal Findings and Interpretation: Steps for Examining the Joints 1. Inspect for joint symmetry, alignment, bony deformities, and swelling 2. Inspect and palpate surrounding tissues for skin changes, nodules, muscle atrophy, tenderness. 3. Assess range of motion and maneuvers to test joint function and stability and the integrity of ligaments, tendons, bursae, especially if pain or trauma 4. Assess any areas of inflammation, especially tenderness, swelling, warmth, redness. Tips for Assessing Joint Pain--Acute joint pain typically lasts up to 6 weeks; chronic pain lasts >12 weeks. JOINT PAIN CONSIDERATIONS: -True pain from the hip joint is typically described in the groin. -Sacral/sacroiliac pain is often in the buttock. -Trochanteric pain from bursitis occurs on the lateral thigh. -Generalized “aches and pains” are called myalgias if in muscles, and arthralgias if there is pain but no evidence of arthritis. -Severe pain of rapid onset in a red swollen joint suggests acute septic arthritis or crystalline arthritis/gout in adults; or osteomyelitis in children. -Inflammation with fever and chills is seen in septic arthritis and gout. -Morning stiffness that gradually improves with activity is more common in inflammatory disorders like RA. -Intermittent stiffness and “gelling” (stiffness that occurs only after inactivity) are frequently seen in OA. -Monoarticular arthritis can be traumatic, crystalline, or septic. -Oligoarticular arthritis (2-4 joints) occurs in infection from gonorrhea or rheumatic fever, connective tissue disease, and OA. -Polyarthritis (4 or more joints) may be viral or inflammatory from RA, SLE, or psoriasis. Joint Pain and Associated Constitutional Symptoms and Systemic Manifestations from Other Organ Systems: Abnormal Findings -Some joint problems have associated constitutional symptoms such as fever, chills, rash, fatigue, anorexia, weight loss, and weakness. -In inflammatory conditions, order labs: Erythrocyte sedimentation rate (ESR), C- reactive protein (CRP), platelet count, and hematocrit. ● Notable skin conditions that may accompany joint pain: -Butterfly (malar) rash on the cheeks = Systemic lupus erythematosus -Scaly plaques, pitted nails = Psoriatic arthritis -Heliotrope rash on the upper eyelid = Dermatomyositis -Papules, pustules, or vesicles on distal extremities = Gonococcal arthritis -Expanding erythematous “bull’s eye” patch (early dz) = Lyme disease -Painful subcutaneous nodules (especially pretibial) = Sarcoidosis/Behçet dz -Palpable purpura = Vasculitis -Hives = Serum sickness/drug reaction -Erosions or scaling on the penis and crusted scaling papules on the soles and palms = Reactive (Reiter) arthritis (with urethritis, uveitis) -The maculopapular rash of rubella = arthritis of rubella -Nailfold capillary changes = Dermatomyositis, systemic sclerosis -Clubbing of the fingernails = Hypertrophic osteoarthropathy ● Red, burning, and itchy eyes (conjunctivitis), eye pain and blurred vision (uveitis) = Ankylosing spondylitis, Reactive (Reiter) arthritis, Behçet dz ● Preceding sore throat = Acute rheumatic fever or gonococcal arthritis Back Pain - pg 634one of the most common reasons for office visit -nonspecific > 90 % sprain or strain related to age related degenerative processes of the intervertebral discs and musculoligamentous injuries -nerve root entrapment with radiculopathy or spinal stenosis -5% -underlying disease 1-2 % -Midline back pain: musculoligamentous injury; disc herniation; vertebral collapse; spinal cord metastases; epidural abscess -Off the midline: muscle strain, sacroiliitis, trochanteric bursitis, sciatica, hip arthritis, renal conditions -Sciatica: radicular gluteal and posterior leg pain in the S1 that increases with cough or Valsalva. 85 % of cases are associated with a disc disorder, usually at L4-L5 or L5-S1 -Spinal stenosis- leg pain that resolves with rest and or lumbar forward flexion -Cauda Equina Syndrome- from an S2-S4 midline disc or tumor if bowel or bladder dysfunction especially if there is saddle anesthesia or perineal numbness. Purse immediate imaging and surgical intervention -Red Flags for low back pain from underlying systemic disease: age <20 or >50, Hx cancer, unexplained weight loss, fever, or decline in general health, pain lasting for more than 1 month or not responding to treatment, pain at night or present at rest, Hx of intravenous drug use, addiction, or immunosuppression, HIV, long-term steroid therapy, saddle anesthesia, bladder or bowel incontinence, Neurological symptoms or progressive neurological deficit Knee Pain -Partial or complete tear of the patellar tendon: tenderness over the tendon or inability to extend the knee -Pain and crepitus arise from the roughened undersurface of the patella as it articulates with the femur -Chondromalacia: pain with compression and patellar movement during quadricep contractions -Patellofemoral pain syndrome: 2 or 3= pain with quadriceps contraction, pain with squatting, and pain with palpation of the posterome-dial/ or lateral patellar border -Prepatellar bursitis: triggered by excessive kneeling -Anserine bursitis: triggered from excessive running - Effusion: fluid wave or bulge -Balloon sign: a positive palpable fluid wave into the suprapatellar pouch further confirms a major effusion, present in knee fractures. -Achilles tendon rupture: “like a gunshot”absent plantar flexion is a positive test, sudden severe pain, an ecchymosis from the calf into the heel, and a flat footed gait with absent “toe off” may also be present Elbow Pain : Olecranon Bursitis: Swelling and inflammation of the olecranon bursa may result from trauma, gout, or rheumatoid arthritis (RA). The swelling is superficial to the olecranon process and may reach 6 cm in diameter. Consider aspiration for both diagnosis and symptomatic relief. Rheumatoid Nodules: Subcutaneous nodules may develop at pressure points along the extensor surface of the ulna in patients with RA or acute rheumatic fever. They are firm and nontender. They are not attached to the overlying skin but may be attached to the underlying periosteum. They can develop in the area of the olecranon bursa, but often occur more distally. Arthritis of the Elbow: Synovial inflammation or fluid is felt best in the grooves between the olecranon process and the epicondyles on either side. Palpate for a boggy, soft, or fluctuant swelling and for tenderness. Causes include RA, gout and pseudogout, osteoarthritis, and trauma. Patients report pain, stiffness, and restricted motion. Epicondylitis: Lateral epicondylitis (tennis elbow) follows repetitive extension of the wrist or pronation–supination of the forearm. Pain and tenderness develop 1 cm distal to the lateral epicondyle and possibly in the extensor muscles close to it. When the patient tries to extend the wrist against resistance, pain increases. Medial epicondylitis (pitcher’s, golfer’s, or Little League elbow) follows repetitive wrist flexion such as throwing. Tenderness is maximal just lateral and distal to the medial epicondyle. Wrist flexion against resistance increases the pain. Rheumatoid Arthritis -Chronic inflammation of the synovial membranes with secondary erosion of adjacent cartilage and bone, and damage to ligaments and tendons. -Common Locations: hands (initially small joints), wrists, knees, elbows, and ankles -Symmetrically additive: progresses to other joints while persisting in initial joints -Usually insidious; human leukocyte antigen (HLA) and non-HLA genes account for >50 %of risk of disease, involves proinflammatory cytokines -Often chronic, with remissions and exacerbations -Frequent swelling of synovial tissue in joints or tendon sheaths; also subcutaneous nodules -Tender, often warm, but seldom red -Prominent stiffness, often in the mornings, and after inactivity -Joint contractures and subluxation, bursitis, and tendinopathy -Generalized symptoms: weakness, fatigue, weight loss, and low fever are common -Heberden nodes and Bouchard nodes Lyme Disease is a bacterial infection you get from the bite of an infected tick. The first symptom is usually a red rash, which may look like a bull's eye. But not all people with Lyme disease have a rash. As the infection spreads to other parts of the body, you may have a fever. Lyme disease is caused by the bacterium Borrelia burgdorferi and rarely, Borrelia mayonii. It is transmitted to humans through the bite of infected blacklegged ticks.Typical symptoms include fever, headache, fatigue, and a characteristic skin rash called erythema migrans. If left untreated, the infection can spread to joints, the heart, and the nervous system.Antibiotics commonly used for oral treatment include doxycycline, amoxicillin, or cefuroxime. People with certain neurological or cardiac forms of illness may require intravenous treatment with antibiotics such as ceftriaxone or penicillin Lyme Disease Systemic disorder characterized by expanding erythemous “bulls eye” rash in early illness which can result in neck stiffness, facial or other weakness and mental status change. Early Signs and Symptoms (3 to 30 Days After Tick Bite) "Classic" Erythema Migrans Rash • Fever, chills, headache, fatigue, muscle and joint aches, and swollen lymph nodes may occur in the absence of rash • Erythema migrans (EM) rash o Begins at the site of a tick bite after a delay of 3 to 30 days (average is about 7 days) o Expands gradually over several days reaching up to 12 inches or more (30 cm) across o May feel warm to the touch but is rarely itchy or painful o Sometimes clears as it enlarges, resulting in a target or “bull’s-eye” appearance o May appear on any area of the body Later Signs and Symptoms (days to months after tick bite) Swollen Knee Facial Palsy • Severe headaches and neck stiffness • Additional EM rashes on other areas of the body • Facial palsy (loss of muscle tone or droop on one or both sides of the face) • Arthritis with severe joint pain and swelling, particularly the knees and other large joints. • Intermittent pain in tendons, muscles, joints, and bones • Heart palpitations or an irregular heart beat (Lyme carditis) • Episodes of dizziness or shortness of breath • Inflammation of the brain and spinal cord • Nerve pain • Shooting pains, numbness, or tingling in the hands or feet Joint Pain: If age <60 years, consider repetitive strain or overuse syndromes like tendinitis or bursitis, crystalline arthritis (gout; crystalline pyrophosphate deposition disease [CPPD]) (males), rheumatoid arthritis (RA), psoriatic arthritis and reactive (Reiter) arthritis (in inflammatory bowel disease [IBD]), and infectious arthritis from gonorrhea, Lyme disease, or viral or bacterial infections. If age >60 years, look for OA, gout and pseudogout, polymyalgia rheumatica (PMR), osteoporotic fracture, and septic bacterial arthritis. Steps for Examining the Joints 1. Inspect for joint symmetry, alignment, bony deformities, and swelling 2. Inspect and palpate surrounding tissues for skin changes, nodules, muscle atrophy, tenderness 3. Assess range of motion and maneuvers to test joint function and stability and the integrity of ligaments, tendons, bursae, especially if pain or trauma 4. Assess any areas of inflammation, especially tenderness, swelling, warmth, redness Knee Pain • The knee joint: largest joint in the body o hinge joint involving three bones: the femur, the tibia, and the patella (or knee cap), o 3 articular surfaces, two between the femur and the tibia and one between the femur and the patella. o The two rounded condyles of the femur rest on the relatively flat tibial plateau. There is no inherent stability in the knee joint itself, making it dependent on four ligaments to hold its articulating femur and tibia in place. This feature, in addition to the lever action of the femur on the tibia and the lack of padding from overlying fat or muscle, makes the knee highly vulnerable to injury. Inspection: Inspect gait for a smooth rhythmic flow as the patient enters the room. The knee should be extended at heel strike and flexed at all other phases of swing and stance. Check the alignment and contours of the knees. Observe any atrophy of the quadriceps muscles. Inspect for any loss of the normal hollows around the patella, a sign of swelling in the knee joint and suprapatellar pouch; note any other swelling in or around the knee. > Stumbling or “giving way” of the knee during heel strike suggests quadriceps weakness or abnormal patellar tracking. Quadriceps atrophy signals hip girdle weakness in older adults. Swelling over the patella occurs in prepatellar bursitis (housemaid’s knee). Swelling over the tibial tubercle suggests infrapatellar or, if more medial, anserine bursitis Palpation: Ask the patient to sit on the edge of the examining table with the knees in flexion. In this position, bony landmarks are more visible, and the muscles, tendons, and ligaments are more relaxed, making them easier to palpate. Pay special attention to any areas of tenderness. Pain is a common complaint in knee problems, and localizing the structure causing pain is important for accurate evaluation. > Bony enlargement at the joint margins, genu varum deformity, and stiffness lasting ≤30 minutes are typical findings in OA A medial meniscus tear with joint line point tenderness is common after trauma and requires prompt further evaluation MCL tenderness after injury is suspicious for an MCL tear; LCL injuries are less frequent. Tenderness over the tendon or inability to extend the knee suggests a partial or complete tear of the patellar tendon. Pain and crepitus arise from the roughened undersurface of the patella as it articulates with the femur. Similar pain may occur when using the stairs or getting up from a chair. Pain with compression and patellar movement during quadriceps contraction occurs in chondromalacia. Findings most diagnostic of the patellofemoral pain syndrome: pain with quadriceps contraction; pain with squatting; and pain with palpation of the posteromedial or lateral patellar border. Swelling around the patella points to synovial thickening or effusion of the knee joint Thickening, bogginess, or warmth occurs with synovitis and nontender effusions from OA. Prepatellar bursitis is triggered by excessive kneeling anserine bursitis from running, valgus knee deformity, or OA popliteal or “Baker” cyst from distention of the gastrocnemius semimembranosus bursa from under-lying arthritis or trauma. Swollen or Tender Elbows: Inspection of the elbow: Support the patient’s forearm with your opposite hand so that the elbow is flexed to about 70°. Identify the medial and lateral epicondyles and the olecranon process of the ulna. Inspect the contours of the elbow, including the extensor surface of the ulna and the olecranon process. Note any nodules or swelling. Palpation. Palpate the olecranon process and press over the epicondyles for tenderness. Palpate the grooves between the epicondyles and the olecranon process, where the synovium is most easily examined. Normally the synovium and olecranon bursae are not palpable. The sensitive ulnar nerve can be palpated posteriorly between the olecranon process and the medial epicondyle. Palpate the epicondyles. Note any displacement of the olecranon process. Abnormal Findings: Elbow Range of Motion: Flexion: Biceps brachii, brachialis, brachioradialis. “Bend your elbow” Extension: Triceps brachii, anconeus. “Straighten your elbow”. Supination: Biceps brachii, supinator. “Turn your palms up, as if carrying a bowl” Pronation: Pronator teres, pronator quadratus. “Turn your palms down.” *After injury, preservation of active range of motion and full elbow extension makes fracture highly unlikely. Tenderness over the radial head, olecranon, or medial epicondyle and bruising, plus absent elbow extension, may improve these test characteristics. Full elbow extension also makes intra-articular effusion or hemarthrosis unlikely. Rheumatoid arthritis Joints affected polyarticular and symmetrical. Assess for subcutaneous nodules. Muscle atrophy and weakness present. Process: Chronic inflammation of synovial membranes with secondary erosion of adjacent cartilage and bone, and damage to ligaments and tendons Common Locations: Hands—initially small joints (PIP and MCP joints), feet (MTP joints), wrists, knees, elbows, ankle Pattern of Spread: Symmetrically additive: progresses to other joints while persisting in initial joints Onset: Usually insidious; human leukocyte antigen (HLA) and non-HLA genes account for >50% of risk of disease; involves proinflammatory cytokine Progression and Duration: Often chronic (in >50%), with remissions and exacerbations Acute RA: Tender, painful, stiff joints in RA, usually with symmetric involvement on both sides of the body. The distal interphalangeal (DIP), metacarpophalangeal (MCP), and wrist joints are the most frequently affected. Note the fusiform or spindle-shaped swelling of the PIP joints in acute disease. Chronic RA: In chronic disease, note the swelling and thickening of the MCP and PIP joints. Range of motion becomes limited, and fingers may deviate toward the ulnar side. The interosseous muscles atrophy. The fingers may show “swan neck” deformities (hyperextension of the PIP joints with fixed flexion of the distal interphalangeal [DIP] joints). Less common is a boutonnière deformity (persistent flexion of the PIP joint with hyperextension of the DIP joint). Rheumatoid nodules are seen in the acute or the chronic stage. Chapter 17 Neurological Assessment and Modification for Age Normal vs Abnormal Findings and Interpretation Subarachnoid hemorrhage- the worst headache of my life, with instantaneous onset Meningitis- stiff neck and severe headache Brain tumors or abscess- dull headache increased by coughing and sneezing, especially when reoccurring in the same location Migraine- an aura or prodrome. Five pound feature: pulsatile or throbbing, one day duration or at least 4 to 72 hours if untreated, Unilateral; Nausea or vomiting; Disabling or intensity causing interruption of daily activity. Guillain-Barre syndrome- progressive subacute onset of lower extremity weakness. Delirium- a multifactorial syndrome, an acute confusion state marked by sudden onset, fluctuating course, inattention, and at tome changing levels of consciousness. Dementia- declines in memory and cognitive ability that interfere with activities of daily living. Most common Alzheimer (>65 years old). CN 1- olfactory: sense of smell by presenting the patient with familiar non-irrigating odors. Loss of smell occurs=head trauma, smoking, aging, use of cocaine, and Parkinson disease CN 2- optic: test visual activity. Inspect optic fundi, paying close attention to the optic disc. Inspect each disc carefully for bulging and blurred margins (papilledema), pallor (optic atrophy), and cup enlargement (glaucoma). - Test visual fields by confrontation: test each eye separately and then together CN II and III- Inspect size and shape of the pupils, and compare one side with the other. Anisocoria= a difference of >0.4 mm in the diameter of one pupil compared to the other. - Intracranial aneurysm: large pupil reacts poorly to light or aniscoria worsens in light, the large pupil has abnormal pupillary constriction, and ptosis and ophthalmoplegia are also present and if the patient is awake. - Horner syndrome=if both pupils react to light and anisocoria worsens in darkness, the small pupil has abnormal pupillary dilation. CN III, IV, VI- Oculomotor, Trochlear, and Abducens: test the extraocular movements in the six cardinal directions of gaze and look for loss of conjugate movements in the aby the six directions, which causes diplopia CN V- trigeminal- palpate the temporal muscles and masseter muscles and check sensory CN VII- Facial, inspect the face both at rest and during conversation with the patient for symmetry. Ask the patient: raise eyebrows, frown, smile, close both eyes, show both upper and lower teeth, smile, puff out both cheeks. CN VII- Acoustic and Vestibula. Whisper test, Weber, and Rinne. -Vertigo and hearing loss= Meniere disease CN XI- Spinal accessory= stand behind the patient, look for atrophy or fasciculations in the trapezius muscles, and compare one side with the other. Ask patient to shrug both shoulders upward against hands. -Fasciculations= fine flickering irregular movements in small groups of muscle fibers. -Peripheral nerve disorder= trapezius weakness with atrophy and fasciculations points, the shoulder droops, and the scapular is displaced downward and laterally. CNXII- Listen to the articulation of the patient’s words, inspect the tongue as it lies on the floor of the mouth. Look for any atrophy or fasciculations. Some coarser restless movements are normal. Then with the patient’s tongue protruded, look for asymmetry, atrophy, or deviation from the midline. As the patient to move the tongue from side to side, and note symmetry of the movement. Romberg Test- test for position sense. The patient stand fairly well with eyes open but loses balance when they are closed= positive test (Ataxia) Babinski Reponses (Abnormal)- Dorsiflexion of the big toe. Arising from a CNS lesion affecting the corticospinal tract, can be positive in unconscious states from drug or alcohol. Occasionally accompanied by reflex flexion at hip and knee. Unconscious states from alcohol and drugs or seizures. Brudzinski Sign- Flexion of both the hip and knees is positive sign. As you flex the neck, watch the hips and knees in reaction to maneuver. Normally they should remain relaxed and motionless. Kernig sign- pain and increased resistance to knee extension are positive. Flex the patients leg at both the hip and the knee, and the slowly extend the leg and straighten the knee, discomfort behind the knee during full extension is normal but should not produce pain. Lumbosacral radiculopathy- pain radiating into the ipsilateral leg is positive straight leg test. Asterixis- metabolic encephalopathy in patients whose mental functions are impaired. Caused by abnormal function of the diencephalic motor centers that regulate agonist and antagonist muscle tone and maintain posture. Test by asking patient to “stop traffic”, observe for 1 to 2 minutes. Intention tremors- cerebellar disorders Oral-facial dyskinesias- bizarre movements of face= late complications of psychotropic drugs, psychoses, elderly, and edentulous Tics- brief and repetitive= Tourette syndrome and phenothiazines Athetosis- slower and twisting, writhing than choreifrom movements, larger amplitude= cerebral palsy Dystonia- similar to ahetoid movements, often involve large parts of the body. Grotesque, twisted postures. Caused by phenothiazines, torsion dystonia, and spasmodic torticollis. Chorea- brief, rapid, jerky, irregular movements, and unpredictable. Causes= sydenham chorea (with rheumatic fever) and Huntington disease. Aphonia- loss of voice that accompanies disease affecting the larynx or its never supply Dysarthria- defect in muscular control of the speech apparatus. Words may be nasal, slurred, or indistinct Aphasia- disorder in producing or understanding language -Wernicke a fluent receptive aphasia. Sentences lack meaning and words are malformed or invented. Speech may be totally incomprehensible. -Broca Aphasia non-fluent or expressive aphasia. Slow with words and laborious effort. Inflection and articulation are impaired but words are meaningful, with nouns, transitive verbs, and important adjectives. Small grammatical words are dropped. Seizure Disorder pg 724, 780, 781Jessica – patient reports “spells” or fainting - A sudden excessive electrical discharge from cortical neurons. - Symptomatic with an identifiable cause or idiopathic - Epilepsy: two or more seizures that are not provoked by other illnesses or circumstances. Does not always involve loss of consciousness, depends on type. Usually classified as generalized or partial, based on location in the cortex of the initial seizure focus. More common in infants and older adults, the baseline neurological exam is frequently normal. - Generalized epilepsy syndromes- usually begin in childhood or adolescence. - Tonic-clonic motor activity, bladder or bowel incontinence, and postictal state. Tongue biting or bruising of limbs may occur. Loses consciousness, and the body stiffness into tonic extensor rigidity. Breathing stops and patient becomes cyanotic. A clonic phase of rhythmic muscular contraction follows. Breathing resumes and is often noisy, with excessive salvation. - Partial- usually adult-onset seizures - Myclonic (drop attack) - sudden loss of consciousness with falling but no movements. - Absence- a sudden brief lapse of consciousness, with momentary blinking, starting, or movements of the lips and hands but no falling. Typical <10 sec. Atypical > 10 sec. Syncope pg 724 Jessica -Determine if consciousness was lost, external noise or voices throughout the episode, felt light-headed, or weak -Syncope= sudden but temporary loss of consciousness and postural tone from transient global hypoperfusion of the brain - Causes= seizures, vasovagal syncope, postural tachycardia syndrome, carotid sinus syncope, orthostatic hypotension, cardiac disease causes arrythmias. Stroke and subarachnoid hemorrhage are unlikely unless both hemispheres are affected. -Vasovagal Syncope- Most common cause: prodrome nausea, diaphoresis, and pallor triggered by a fearful or unpleasant event, then vagally mediated hypotension, often with slow onset and offset. -Syncope from arrythmias- onset and offset are sudden, reflecting loss and recovery of cerebral perfusion -Micturition syncope: vasovagal response, sudden hypotension. Precipitating= emptying the bladder after getting out of bed. Intracranial Pressure - The normal ICP is 5 - 15 mmHg. Cranial Nerves [Show More]
Last updated: 4 months ago
Preview 1 out of 69 pages
Instant download
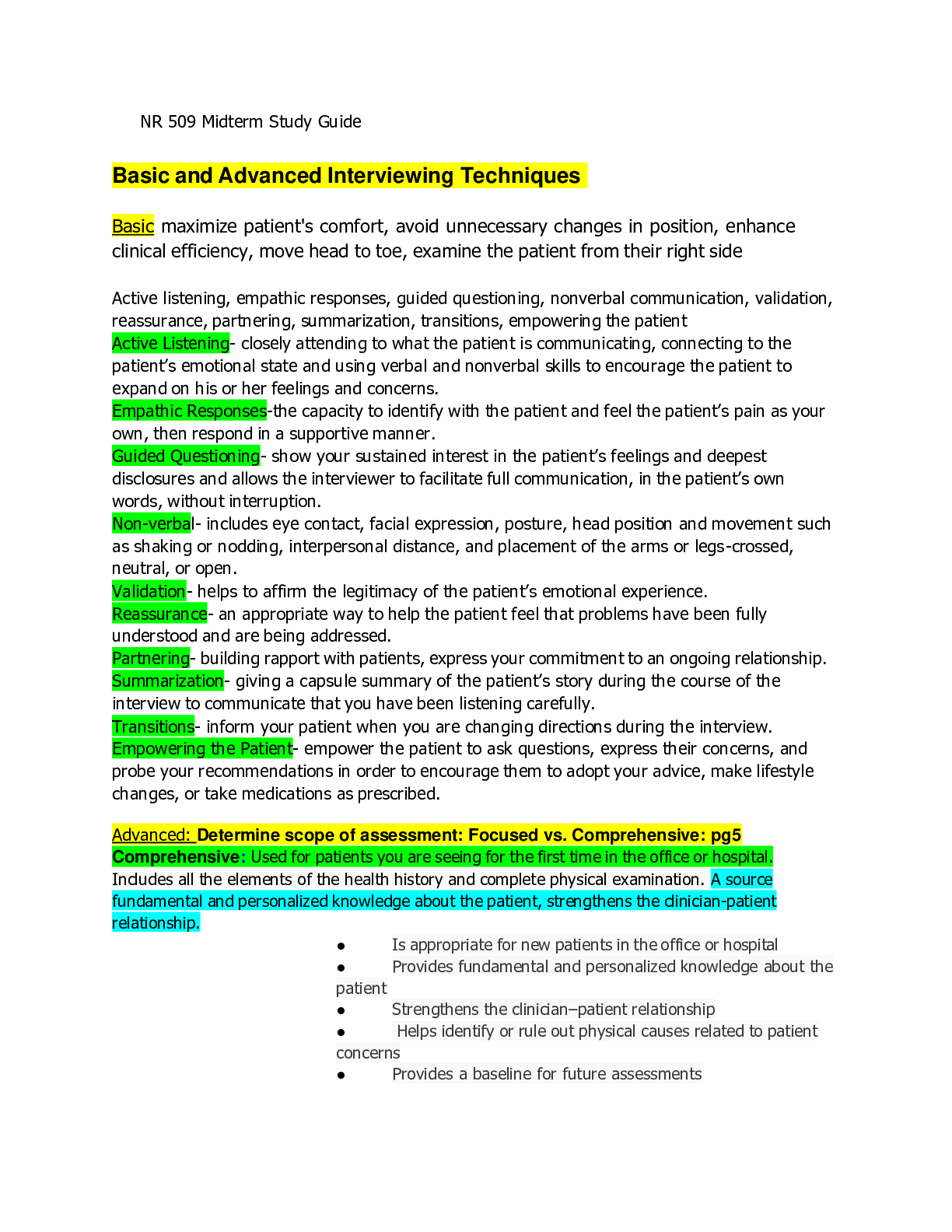
Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Feb 01, 2024
Number of pages
69
Written in
Additional information
This document has been written for:
Uploaded
Feb 01, 2024
Downloads
0
Views
16