*NURSING > EXAM REVIEW > NCSBN Online Review. Contains 171 pages_ Questions_Answers and Explantions. (All)
NCSBN Online Review. Contains 171 pages_ Questions_Answers and Explantions.
Document Content and Description Below
NCSBN ON-LINE REVIEW 1.A client has been hospitalized after an automobile accident. A full leg cast was applied in the emergency room. The most important reason for the nurse to elevate the casted l... eg is to A) Promote the client's comfort B) Reduce the drying time C) Decrease irritation to the skin D) Improve venous return D: Improve venous return. Elevating the leg both improves venous return and reduces swelling. Client comfort will be improved as well. 2. The nurse is reviewing with a client how to collect a clean catch urine specimen. What is the appropriate sequence to teach the client? A) Clean the meatus, begin voiding, then catch urine stream B) Void a little, clean the meatus, then collect specimen C) Clean the meatus, then urinate into container D) Void continuously and catch some of the urine A: Clean the meatus, begin voiding, then catch urine stream. A clean catch urine is difficult to obtain and requires clear directions. Instructing the client to carefully clean the meatus, then void naturally with a steady stream prevents surface bacteria from contaminating the urine specimen. As starting and stopping flow can be difficult, once the client begins voiding it’s best to just slip the container into the stream. Other responses do not reflect correct technique 3. Following change-of-shift report on an orthopedic unit, which client should the nurse see first? A) 16 year-old who had an open reduction of a fractured wrist 10 hours ago B) 20 year-old in skeletal traction for 2 weeks since a motor cycle accident C) 72 year-old recovering from surgery after a hip replacement 2 hours ago D) 75 year-old who is in skin traction prior to planned hip pinning surgery. C: Look for the client who has the most imminent risks and acute vulnerability. The client who returned from surgery 2 hours ago is at risk for life threatening hemorrhage and should be seen first. The 16 year-old should be seen next because it is still the first post-op day. The 75 year-old is potentially vulnerable to age-related physical and cognitive consequences in skin traction should be seen next. The client who can safely be seen last is the 20 year-old who is 2 weeks post-injury. 4. A client with Guillain Barre is in a nonresponsive state, yet vital signs are stable and breathing is independent. What should the nurse document to most accurately describe the client's condition? A) Comatose, breathing unlabored B) Glascow Coma Scale 8, respirations regular C) Appears to be sleeping, vital signs stable D) Glascow Coma Scale 13, no ventilator required B: Glascow Coma Scale 8, respirations regular. The Glascow Coma Scale provides a standard reference for assessing or monitoring level of consciousness. Any score less than 13 indicates a neurological impairment. Using the term comatose provides too much room for interpretation and is not very precise. 5. When caring for a client receiving warfarin sodium (Coumadin), which lab test would the nurse monitor to determine therapeutic response to the drug? A) Bleeding time B) Coagulation time C) Prothrombin time D) Partial thromboplastin time C: Prothrombin time. Coumadin is ordered daily, based on the client''s prothrombin time (PT). This test evaluates the adequacy of the extrinsic system and common pathway in the clotting cascade; Coumadin affects the Vitamin K dependent clotting factors. 6.A client with moderate persistent asthma is admitted for a minor surgical procedure. On admission the peak flow meter is measured at 480 liters/minute. Post-operatively the client is complaining of chest tightness. The peak flow has dropped to 200 liters/minute. What should the nurse do first? A) Notify both the surgeon and provider B) Administer the prn dose of albuterol C) Apply oxygen at 2 liters per nasal cannula D) Repeat the peak flow reading in 30 minutes B: Administer the prn dose of albuterol. Peak flow monitoring during exacerbations of asthma is recommended for clients with moderate-to-severe persistent asthma to determine the severity of the exacerbation and to guide the treatment. A peak flow reading of less than 50% of the client''s baseline reading is a medical alert condition and a short-acting beta-agonist must be taken immediately. 7.A client had 20 mg of Lasix (furosemide) PO at 10 AM. Which would be essential for the nurse to include at the change of shift report? A) The client lost 2 pounds in 24 hours 1B) The client’s potassium level is 4 mEq/liter. C) The client’s urine output was 1500 cc in 5 hours D) The client is to receive another dose of Lasix at 10 PM C: The client’s urine output was 1500 cc in 5 hours. Although all of these may be correct information to include in report, the essential piece would be the urine output. 8.A client has been tentatively diagnosed with Graves' disease (hyperthyroidism). Which of these findings noted on the initial nursing assessment requires quick intervention by the nurse? A) a report of 10 pounds weight loss in the last month B) a comment by the client "I just can't sit still." C) the appearance of eyeballs that appear to "pop" out of the client's eye sockets D) a report of the sudden onset of irritability in the past 2 weeks C: the appearance of eyeballs that appear to "pop" out of the client''s eye sockets. Exophthalmos or protruding eyeballs is a distinctive characteristic of Graves'' Disease. It can result in corneal abrasions with severe eye pain or damage when the eyelid is unable to blink down over the protruding eyeball. Eye drops or ointment may be needed. 9. The nurse has performed the initial assessments of 4 clients admitted with an acute episode of asthma. Which assessment finding would cause the nurse to call the provider immediately? A) prolonged inspiration with each breath B) expiratory wheezes that are suddenly absent in 1 lobe C) expectoration of large amounts of purulent mucous D) appearance of the use of abdominal muscles for breathing B: expiratory wheezes that are suddenly absent in 1 lobe. Acute asthma is characterized by expiratory wheezes caused by obstruction of the airways. Wheezes are a high pitched musical sounds produced by air moving through narrowed airways. Clients often associate wheezes with the feeling of tightness in the chest. However, sudden cessation of wheezing is an ominous or bad sign that indicates an emergency -- the small airways are now collapsed. 10.During the initial home visit, a nurse is discussing the care of a client newly diagnosed with Alzheimer's disease with family members. Which of these interventions would be most helpful at this time? A) leave a book about relaxation techniques B) write out a daily exercise routine for them to assist the client to do C) list actions to improve the client's daily nutritional intake D) suggest communication strategies D: suggest communication strategies. Alzheimer''s disease, a progressive chronic illness, greatly challenges caregivers. The nurse can be of greatest assistance in helping the family to use communication strategies to enhance their ability to relate to the client. By use of select verbal and nonverbal communication strategies the family can best support the client’s strengths and cope with any aberrant behavior. 11.An 80 year-old client admitted with a diagnosis of possible cerebral vascular accident has had a blood pressure from 160/100 to 180/110 over the past 2 hours. The nurse has also noted increased lethargy. Which assessment finding should the nurse report immediately to the provider? A) Slurred speech B) Incontinence C) Muscle weakness D) Rapid pulse A: Slurred speech. Changes in speech patterns and level of conscious can be indicators of continued intracranial bleeding or extension of the stroke. Further diagnostic testing may be indicated. 12. A school-aged child has had a long leg (hip to ankle) synthetic cast applied 4 hours ago. Which statement from the parent indicates that teaching has been inadequate? A) "I will keep the cast uncovered for the next day to prevent burning of the skin." B) "I can apply an ice pack over the area to relieve itching inside the cast." C) "The cast should be propped on at least 2 pillows when my child is lying down." D) "I think I remember that my child should not stand until after 72 hours." D: "I think I remember that my child should not stand until after 72 hours.". Synthetic casts will typically set up in 30 minutes and dry in a few hours. Thus, the client may stand within the initial 24 hours. With plaster casts, the set up and drying time, especially in a long leg cast which is thicker than an arm cast, can take up to 72 hours. Both types of casts give off a lot of heat when drying and it is preferable to keep the cast uncovered for the first 24 hours. Clients may complain of a chill from the wet cast and therefore can simply be covered lightly with a sheet or blanket. Applying ice is a safe method of relieving the itching. 13. Which blood serum finding in a client with diabetic ketoacidosis alerts the nurse that immediate action is required? A) pH below 7.3 B) Potassium of 5.0 C) HCT of 60 D) Pa O2 of 79% 2C: HCT of 60. This high hematocrit is indicative of severe dehydration which requires priority attention in diabetic ketoacidosis. Without sufficient hydration, all systems of the body are at risk for hypoxia from a lack of or sluggish circulation. In the absence of insulin, which facilitates the transport of glucose into the cell, the body breaks down fats and proteins to supply energy ketones, a by-product of fat metabolism. These accumulate causing metabolic acidosis (pH < 7.3), which would be the second concern for this client. The potassium and PaO2 levels are near normal. 14. The nurse is preparing a client with a deep vein thrombosis (DVT) for a Venous Doppler evaluation. Which of the following would be necessary for preparing the client for this test? A) Client should be NPO after midnight B) Client should receive a sedative medication prior to the test C) Discontinue anti-coagulant therapy prior to the test D) No special preparation is necessary D: No special preparation is necessary. This is a non-invasive procedure and does not require preparation other than client education. 15. A client is admitted with infective endocarditis (IE). Which finding would alert the nurse to a complication of this condition? A) dyspnea B) heart murmur C) macular rash D) Hemorrhage B: heart murmur. Large, soft, rapidly developing vegetations attach to the heart valves. They have a tendency to break off, causing emboli and leaving ulcerations on the valve leaflets. These emboli produce findings of cardiac murmur, fever, anorexia, malaise and neurologic sequelae of emboli. Furthermore, the vegetations may travel to various organs such as spleen, kidney, coronary artery, brain and lungs, and obstruct blood flow. 16. The nurse explains an autograft to a client scheduled for excision of a skin tumor. The nurse knows the client understands the procedure when the client says, "I will receive tissue from A) a tissue bank." B) a pig." C) my thigh." D) synthetic skin." C: my thigh.". Autografts are done with tissue transplanted from the client''s own skin. 17.A client is admitted to the emergency room following an acute asthma attack. Which of the following assessments would be expected by the nurse? A) Diffuse expiratory wheezing B) Loose, productive cough C) No relief from inhalant D) Fever and chills A: Diffuse expiratory wheezing. In asthma, the airways are narrowed, creating difficulty getting air in. A wheezing sound results. 18. A client has been admitted with a fractured femur and has been placed in skeletal traction. Which of the following nursing interventions should receive priority? A) Maintaining proper body alignment B) Frequent neurovascular assessments of the affected leg C) Inspection of pin sites for evidence of drainage or inflammation D) Applying an over-bed trapeze to assist the client with movement in bed B: Frequent neurovascular assessments of the affected leg. The most important activity for the nurse is to assess neurovascular status. Compartment syndrome is a serious complication of fractures. Prompt recognition of this neurovascular problem and early intervention may prevent permanent limb damage. 19. The nurse is assigned to care for a client who had a myocardial infarction (MI) 2 days ago. The client has many questions about this condition. What area is a priority for the nurse to discuss at this time? A) Daily needs and concerns B) The overview cardiac rehabilitation C) Medication and diet guideline D) Activity and rest guidelines A: Daily needs and concerns. At 2 days post-MI, the client’s education should be focused on the immediate needs and concerns for the day. 20. A 3 year-old child is brought to the clinic by his grandmother to be seen for "scratching his bottom and wetting the bed at night." Based on these complaints, the nurse would initially assess for which problem? A) allergies B) scabies C) regression D) pinworms 3D: pinworms. Signs of pinworm infection include intense perianal itching, poor sleep patterns, general irritability, restlessness, bed-wetting, distractibility and short attention span. Scabies is an itchy skin condition caused by a tiny, eight-legged burrowing mite called Sarcoptes scabiei . The presence of the mite leads to intense itching in the area of its burrows. 21. The nurse is caring for a newborn with tracheoesophageal fistula. Which nursing diagnosis is a priority? A) Risk for dehydration B) Ineffective airway clearance C) Altered nutrition D) Risk for injury B: Ineffective airway clearance. The most common form of TEF is one in which the proximal esophageal segment terminates in a blind pouch and the distal segment is connected to the trachea or primary bronchus by a short fistula at or near the bifurcation. Thus, a priority is maintaining an open airway, preventing aspiration. Other nursing diagnoses are then addressed. 22. The nurse is developing a meal plan that would provide the maximum possible amount of iron for a child with anemia. Which dinner menu would be best? A) Fish sticks, french fries, banana, cookies, milk B) Ground beef patty, lima beans, wheat roll, raisins, milk C) Chicken nuggets, macaroni, peas, cantaloupe, milk D) Peanut butter and jelly sandwich, apple slices, milk B: Ground beef patty, lima beans, wheat roll, raisins, milk. Iron rich foods include red meat, fish, egg yolks, green leafy vegetables, legumes, whole grains, and dried fruits such as raisins. This dinner is the best choice: It is high in iron and is appropriate for a toddler. 23. The nurse admitting a 5 month-old who vomited 9 times in the past 6 hours should observe for signs of which overall imbalance? A) Metabolic acidosis B) Metabolic alkalosis C) Some increase in the serum hemoglobin D) A little decrease in the serum potassium B: Metabolic alkalosis. Vomiting causes loss of acid from the stomach. Prolonged vomiting can result in excess loss of acid and lead to metabolic alkalosis. Findings include irritability, increased activity, hyperactive reflexes, muscle twitching and elevated pulse. Options C and D are correct answers but not the best answers since they are too general. 24. A two year-old child is brought to the provider's office with a chief complaint of mild diarrhea for two days. Nutritional counseling by the nurse should include which statement? A) Place the child on clear liquids and gelatin for 24 hours B) Continue with the regular diet and include oral rehydration fluids C) Give bananas, apples, rice and toast as tolerated D) Place NPO for 24 hours, then rehydrate with milk and water B: Continue with the regular diet and include oral rehydration fluids. Current recommendations for mild to moderate diarrhea are to maintain a normal diet with fluids to rehydrate. 25. The nurse is teaching parents about the appropriate diet for a 4 month-old infant with gastroenteritis and mild dehydration. In addition to oral rehydration fluids, the diet should include A) formula or breast milk B) broth and tea C) rice cereal and apple juice D) gelatin and ginger ale A: formula or breast milk. The usual diet for a young infant should be followed. 26. A child is injured on the school playground and appears to have a fractured leg. The first action the school nurse should take is A) call for emergency transport to the hospital B) immobilize the limb and joints above and below the injury C) assess the child and the extent of the injury D) apply cold compresses to the injured area C: assess the child and the extent of the injury. When applying the nursing process, assessment is the first step in providing care. The "5 Ps" of vascular impairment can be used as a guide (pain, pulse, pallor, paresthesia, paralysis). 27. The mother of a 3 month-old infant tells the nurse that she wants to change from formula to whole milk and add cereal and meats to the diet. What should be emphasized as the nurse teaches about infant nutrition? A) Solid foods should be introduced at 3-4 months B) Whole milk is difficult for a young infant to digest C) Fluoridated tap water should be used to dilute milk D) Supplemental apple juice can be used between feedings B: Whole milk is difficult for a young infant to digest. Cow''s milk is not given to infants younger than 1 year because the tough, hard curd is difficult to digest. In addition, it contains little iron and creates a high renal solute load. 428. The nurse is preparing a handout on infant feeding to be distributed to families visiting the clinic. Which notation should be included in the teaching materials? A) Solid foods are introduced one at a time beginning with cereal B) Finely ground meat should be started early to provide iron C) Egg white is added early to increase protein intake D) Solid foods should be mixed with formula in a bottle A: Solid foods are introduced one at a time beginning with cereal. Solid foods should be added one at a time between 4-6 months. If the infant is able to tolerate the food, another may be added in a week. Iron fortified cereal is the recommended first food. 29. The nurse planning care for a 12 year-old child with sickle cell disease in a vaso-occlusive crisis of the elbow should include which one of the following as a priority? A) Limit fluids B) Client controlled analgesia C) Cold compresses to elbow D) Passive range of motion exercise B: Client controlled analgesia. Management of a sickle cell crisis is directed towards supportive and symptomatic treatment. The priority of care is pain relief. In a 12 year-old child, client controlled analgesia promotes maximum comfort. 30. The nurse is performing a physical assessment on a toddler. Which of the following actions should be the first? A) Perform traumatic procedures B) Use minimal physical contact C) Proceed from head to toe D) Explain the exam in detail B: Use minimal physical contact. The nurse should approach the toddler slowly and use minimal physical contact initially so as to gain the toddler''s cooperation. Be flexible in the sequence of the exam, and give only brief simple explanations just prior to the action. 31. What finding signifies that children have attained the stage of concrete operations (Piaget)? A) Explores the environment with the use of sight and movement B) Thinks in mental images or word pictures C) Makes the moral judgment that "stealing is wrong" D) Reasons that homework is time-consuming yet necessary C: Makes the moral judgment that "stealing is wrong". The stage of concrete operations is depicted by logical thinking and moral judgments. 32. The mother of a child with a neural tube defect asks the nurse what she can do to decrease the chances of having another baby with a neural tube defect. What is the best response by the nurse? A) "Folic acid should be taken before and after conception." B) "Multivitamin supplements are recommended during pregnancy." C) "A well balanced diet promotes normal fetal development." D) "Increased dietary iron improves the health of mother and fetus." A: "Folic acid should be taken before and after conception.". The American Academy of Pediatrics recommends that all childbearing women increase folic acid from dietary sources and/or supplements. There is evidence that increased amounts of folic acid prevents neural tube defects. 33. The provider orders Lanoxin (digoxin) 0.125 mg PO and furosemide 40 mg every day. Which of these foods would the nurse reinforce for the client to eat at least daily? A) Spaghetti B) Watermelon C) Chicken D) Tomatoes B: Watermelon. Watermelon is high in potassium and will replace potassium lost by the diuretic. The other foods are not high in potassium. 34. While teaching the family of a child who will take phenytoin (Dilantin) regularly for seizure control, it is most important for the nurse to teach them about which of the following actions? A) Maintain good oral hygiene and dental care B) Omit medication if the child is seizure free C) Administer acetaminophen to promote sleep D) Serve a diet that is high in iron A: Maintain good oral hygiene and dental care. Swollen and tender gums occur often with use of phenytoin. Good oral hygiene and regular visits to the dentist should be emphasized. 35. The nurse is offering safety instructions to a parent with a four month-old infant and a four year-old child. Which statement by the parent indicates understanding of appropriate precautions to take with the children? 5A) "I strap the infant car seat on the front seat to face backwards." B) "I place my infant in the middle of the living room floor on a blanket to play with my four year-old while I make supper in the kitchen." C) "My sleeping baby lies so cute in the crib with the little buttocks stuck up in the air while the four year-old naps on the sofa." D) "I have the four year-old hold and help feed the four month-old a bottle in the kitchen while I make supper." D: The infant seat is to be placed on the rear seat. Small children and infants are not to be left unsupervised. 36. The nurse admits a 7 year-old to the emergency room after a leg injury. The x-rays show a femur fracture near the epiphysis. The parents ask what will be the outcome of this injury. The appropriate response by the nurse should be which of these statements? A) "The injury is expected to heal quickly because of thin periosteum." B) "In some instances the result is a retarded bone growth." C) "Bone growth is stimulated in the affected leg." D) "This type of injury shows more rapid union than that of younger children." B: "In some instances the result is a retarded bone growth.". An epiphyseal (growth) plate fracture in a 7 year-old often results in retarded bone growth. The leg often will be different in length than the uninjured leg. 37. The parents of a 4 year-old hospitalized child tell the nurse, “We are leaving now and will be back at 6 PM.” A few hours later the child asks the nurse when the parents will come again. What is the best response by the nurse? A) "They will be back right after supper." B) "In about 2 hours, you will see them." C) "After you play awhile, they will be here." D) "When the clock hands are on 6 and 12." A: "They will be back right after supper." Time is not completely understood by a 4 year-old. Preschoolers interpret time with their own frame of reference. Thus, it is best to explain time in relationship to a known, common event. 38. The nurse is giving instructions to the parents of a child with cystic fibrosis. The nurse would emphasize that pancreatic enzymes should be taken A) once each day B) 3 times daily after meals C) with each meal or snack D) each time carbohydrates are eaten C: Pancreatic enzymes should be taken with each meal and every snack to allow for digestion of all foods that are eaten. 39. A nurse is providing a parenting class to individuals living in a community of older homes. In discussing formula preparation, which of the following is most important to prevent lead poisoning? A) Use ready-to-feed commercial infant formula B) Boil the tap water for 10 minutes prior to preparing the formula C) Let tap water run for 2 minutes before adding to concentrate D) Buy bottled water labeled "lead free" to mix the formula C: Let tap water run for 2 minutes before adding to concentrate. Use of lead-contaminated water to prepare formula is a major source of poisoning in infants. Drinking water may be contaminated by lead from old lead pipes or lead solder used in sealing water pipes. Letting tap water run for several minutes will diminish the lead contamination. 40. Which of the following manifestations observed by the school nurse confirms the presence of pediculosis capitis in students? A) Scratching the head more than usual B) Flakes evident on a student's shoulders C) Oval pattern occipital hair loss D) Whitish oval specks sticking to the hair D: Whitish oval specks sticking to the hair. Diagnosis of pediculosis capitis is made by observation of the white eggs (nits) firmly attached to the hair shafts. Treatment can include application of a medicated shampoo with lindane for children over 2 years of age, and meticulous combing and removal of all nits. 41. When interviewing the parents of a child with asthma, it is most important to assess the child's environment for what factor? A) Household pets B) New furniture C) Lead based paint D) Plants such as cactus A: Household pets. Animal dander is a very common allergen affecting persons with asthma. Other triggers may include pollens, carpeting and household dust. 42. The mother of a 2 month-old baby calls the nurse 2 days after the first DTaP, IPV, Hepatitis B and HIB immunizations. She reports that the baby feels very warm, cries inconsolably for as long as 3 hours, and has had several shaking spells. In addition to referring her to the emergency room, the nurse should document the reaction on the baby's record and expect which immunization to be most associated with the findings the infant is displaying? 6A) DTaP B) Hepatitis B C) Polio D) H. Influenza A: DTaP. The majority of reactions occur with the administration of the DTaP vaccination. Contradictions to giving repeat DTaP immunizations include the occurrence of severe side effects after a previous dose as well as signs of encephalopathy within 7 days of the immunization. 43.The mother of a 2 year-old hospitalized child asks the nurse's advice about the child's screaming every time the mother gets ready to leave the hospital room. What is the best response by the nurse? A) "I think you or your partner needs to stay with the child while in the hospital." B) "Oh, that behavior will stop in a few days." C) "Keep in mind that for the age this is a normal response to being in the hospital." D) "You might want to "sneak out" of the room once the child falls asleep." C: The protest phase of separation anxiety is a normal response for a child this age. In toddlers, ages 1 to 3, separation anxiety is at its peak 44. A couple experienced the loss of a 7 month-old fetus. In planning for discharge, what should the nurse emphasize? A) To discuss feelings with each other and use support persons B) To focus on the other healthy children and move through the loss C) To seek causes for the fetal death and come to some safe conclusion D) To plan for another pregnancy within 2 years and maintain physical health A: To discuss feelings with each other and use support persons. To communicate in a therapeutic manner, the nurse''s goal is to help the couple begin the grief process by suggesting they talk to each other, seek family, friends and support groups to listen to their feelings. 45. The nurse is performing a pre-kindergarten physical on a 5 year-old. The last series of vaccines will be administered. What is the preferred site for injection by the nurse? A) vastus intermedius B) gluteus maximus C) vastus lateralis D) dorsogluteaI C: vastus lateralis. Vastus lateralis, a large and well developed muscle, is the preferred site, since it is removed from major nerves and blood vessels. 46. A 7 month pregnant woman is admitted with complaints of painless vaginal bleeding over several hours. The nurse should prepare the client for an immediate A) Non stress test B) Abdominal ultrasound C) Pelvic exam D) X-ray of abdomen B: Abdominal ultrasound. The standard for diagnosis of placenta previa, which is suggested in the client''s history of painless bleeding, is abdominal ultrasound. 47. A nurse entering the room of a postpartum mother observes the baby lying at the edge of the bed while the woman sits in a chair. The mother states "This is not my baby, and I do not want it." After repositioning the child safely, the nurse's best response is A) "This is a common occurrence after birth, but you will come to accept the baby." B) "Many women have postpartum blues and need some time to love the baby." C) "What a beautiful baby! Her eyes are just like yours." D) "You seem upset; tell me what the pregnancy and birth were like for you." D: "You seem upset; tell me what the pregnancy and birth were like for you." A non-judgmental, open ended response facilitates dialogue between the client and nurse. 48. The nurse notes that a 2 year-old child recovering from a tonsillectomy has an temperature of 98.2 degrees Fahrenheit at 8:00 AM. At 10:00 AM the child's parent reports that the child "feels very warm" to touch. The first action by the nurse should be to A) reassure the parent that this is normal B) offer the child cold oral fluids C) reassess the child's temperature D) administer the prescribed acetaminophen C: reassess the child''s temperature. A child''s temperature may have rapid fluctuations. The nurse should listen to and show respect for what parents say. Parental caretakers are often quite sensitive to variations in their children''s condition that may not be immediately evident to others. 749. The nurse is caring for a client who was successfully resuscitated from a pulseless dysrhythmia. Which of the following assessments is critical for the nurse to include in the plan of care? A) hourly urine output B) white blood count C) blood glucose every 4 hours D) temperature every 2 hours A: hourly urine output. Clients who have had an episode of decreased glomerular perfusion are at risk for pre-renal failure. This is caused by any abnormal decline in kidney perfusion that reduces glomerular perfusion. Pre-renal failure occurs when the effective arterial blood volume falls. Examples of this phenomena include a drop in circulating blood volume as in a cardiac arrest state or in low cardiac perfusion states such as congestive heart failure associated with a cardiomyopathy. Close observation of hourly urinary output is necessary for early detection of this condition. 50. A client is admitted to the rehabilitation unit following a cerebral vascular accident (CVA) and mild dysphagia. The most appropriate intervention for this client is to A) position client in upright position while eating B) place client on a clear liquid diet C) tilt head back to facilitate swallowing reflex D) offer finger foods such as crackers or pretzels A: position client in upright position while eating. An upright position facilitates proper chewing and swallowing. 51. A 72 year-old client with osteomyelitis requires a 6 week course of intravenous antibiotics. In planning for home care, what is the most important action by the nurse? A) Investigating the client's insurance coverage for home IV antibiotic therapy B) Determining if there are adequate hand washing facilities in the home C) Assessing the client's ability to participate in self care and/or the reliability of a caregiver D) Selecting the appropriate venous access device C: Assessing the client''s ability to participate in self care and/or the reliability of a caregiver. The cognitive ability of the client as well as the availability and reliability of a caregiver must be assessed to determine if home care is a feasible option. 52. A nurse administers the influenza vaccine to a client in a clinic. Within 15 minutes after the immunization was given, the client complains of itchy and watery eyes, increased anxiety, and difficulty breathing. The nurse expects that the first action in the sequence of care for this client will be to A) Maintain the airway B) Administer epinephrine 1:1000 as ordered C) Monitor for hypotension with shock D) Administer diphenhydramine as ordered B: Administer epinephrine 1:1000 as ordered. All the answers are correct given the circumstances, but the priority is to administer the epinephrine, then maintain the airway. In the early stages of anaphylaxis, when the patient has not lost consciousness and is normotensive, administering the epinephrine is first, and applying the oxygen, and watching for hypotension and shock, are later responses. The prevention of a severe crisis is maintained by using diphenhydramine. 53. The nurse instructs the client taking dexamethasone (Decadron) to take it with food or milk. The physiological basis for this instruction is that the medication A) retards pepsin production B) stimulates hydrochloric acid production C) slows stomach emptying time D) decreases production of hydrochloric acid B: stimulates hydrochloric acid production. Decadron increases the production of hydrochloric acid, which may cause gastrointestinal ulcers. 54. A client receiving chlorpromazine HCL (Thorazine) is in psychiatric home care. During a home visit the nurse observes the client smacking her lips alternately with grinding her teeth. The nurse recognizes this assessment finding as what? A) Dystonia B) Akathisia C) Brady dyskinesia D) Tardive dyskinesia D: Tardive dyskinesia. Signs of tardive dyskinesia include smacking lips, grinding of teeth and "fly catching" tongue movements. These findings are often described as Parkinsonian. 55. Which of the following findings contraindicate the use of haloperidol (Haldol) and warrant withholding the dose? A) Drowsiness, lethargy, and inactivity B) Dry mouth, nasal congestion, and blurred vision C) Rash, blood dyscrasias, severe depression D) Hyperglycemia, weight gain, and edema 8C: Rash, blood dyscrasias, severe depression. Rash and blood dyscrasias are side effects of anti-psychotic drugs. A history of severe depression is a contraindication to the use of neuroleptics. 56. The nurse is reinforcing teaching to a 24 year-old woman receiving acyclovir (Zovirax) for a Herpes Simplex Virus type 2 infection. Which of these instructions should the nurse give the client? A) Complete the entire course of the medication for an effective cure B) Begin treatment with acyclovir at the onset of symptoms of recurrence C) Stop treatment if she thinks she may be pregnant to prevent birth defects D) Continue to take prophylactic doses for at least 5 years after the diagnosis B: Begin treatment with acyclovir at the onset of symptoms of recurrence. When the client is aware of early symptoms, such as pain, itching or tingling, treatment is very effective. Medications for herpes simplex do not cure the disease; they simply decrease the level of symptoms. 57. A 14 month-old child ingested half a bottle of aspirin tablets. Which of the following would the nurse expect to see in the child? A) Hypothermia B) Edema C) Dyspnea D) Epistaxis D: Epistaxis. A large dose of aspirin inhibits prothrombin formation and lowers platelet levels. With an overdose, clotting time is prolonged. 58. An 80 year-old client on digitalis (Lanoxin) reports nausea, vomiting, abdominal cramps and halo vision. Which of the following laboratory results should the nurse analyze first? A) Potassium levels B) Blood pH C) Magnesium levels D) Blood urea nitrogen A: Potassium levels. The most common cause of digitalis toxicity is a low potassium level. Clients must be taught that it is important to have adequate potassium intake especially if taking diuretics that enhance the loss of potassium while they are taking digitalis. 59. A 42 year-old male client refuses to take propranolol hydrochloride (Inderal) as prescribed. Which client statement from the assessment data is likely to explain his noncompliance? A) "I have problems with diarrhea." B) "I have difficulty falling asleep." C) "I have diminished sexual function." D) "I often feel jittery." C: "I have diminished sexual function." Inderal, a beta-blocking agent used in hypertension, prohibits the release of epinephrine into the cells; this may result in hypotension which results in decreased libido and impotence. 60. The nurse caring for a 9 year-old child with a fractured femur is told that a medication error occurred. The child received twice the ordered dose of morphine an hour ago. Which nursing diagnosis is a priority at this time? A) Risk for fluid volume deficit related to morphine overdose B) Decreased gastrointestinal mobility related to mucosal irritation C) Ineffective breathing patterns related to central nervous system depression D) Altered nutrition related to inability to control nausea and vomiting C: Ineffective breathing patterns related to central nervous system depression. Respiratory depression is a life-threatening risk in this overdose. 61. Lactulose (Chronulac) has been prescribed for a client with advanced liver disease. Which of the following assessments would the nurse use to evaluate the effectiveness of this treatment? A) An increase in appetite B) A decrease in fluid retention C) A decrease in lethargy D) A reduction in jaundice C: A decrease in lethargy. Lactulose produces an acid environment in the bowel and traps ammonia in the gut; the laxative effect then aids in removing the ammonia from the body. This decreases the effects of hepatic encephalopathy, including lethargy and confusion. 62. The nurse is teaching a class on HIV prevention. Which of the following should be emphasized as increasing risk? A) Donating blood B) Using public bathrooms C) Unprotected sex D) Touching a person with AIDS C: Unprotected sex. Because HIV is spread through exposure to bodily fluids, unprotected intercourse and shared drug paraphernalia remain the highest risks for infection. 963. While interviewing a new admission, the nurse notices that the client is shifting positions, wringing her hands, and avoiding eye contact. It is important for the nurse to A) ask the client what she is feeling B) assess the client for auditory hallucination C) recognize the behavior as a side effect of medication D) re-focus the discussion on a less anxiety provoking topic A: ask the client what she is feeling. The initial step in anxiety intervention is observing, identifying, and assessing anxiety. The nurse should seek client validation of the accuracy of nursing assessments and avoid drawing conclusions based on limited data. In the situation above, the client may simply need to use the restroom but be reluctant to communicate her need! 64. A young adult seeks treatment in an outpatient mental health center. The client tells the nurse he is a government official being followed by spies. On further questioning, he reveals that his warnings must be heeded to prevent nuclear war. What is the most therapeutic approach by the nurse? A) Listen quietly without comment B) Ask for further information on the spies C) Confront the client’s delusion D) Contact the government agency A: Listen quietly without comment. The client''s comments demonstrate grandiose ideas. The most therapeutic response is to listen but avoid being incorporated into the client’s delusional system. 65. The nurse is assessing a 17 year-old female client with bulimia. Which of the following laboratory reports would the nurse anticipate? A) Increased serum glucose B) Decreased albumin C) Decreased potassium D) Increased sodium retention C: Decreased potassium. In bulimia, loss of electrolytes can occur in addition to other findings of starvation and dehydration. 66. A client, recovering from alcoholism, asks the nurse, "What can I do when I start recognizing relapse triggers within myself?" How might the nurse best respond? A) "When you have the impulse to stop in a bar, contact a sober friend and talk with him." B) "Go to an AA meeting when you feel the urge to drink." C) "It is important to exercise daily and get involved in activities that will cause you not to think about drug use." D) "Let’s talk about possible options you have when you recognize relapse triggers in yourself." D: This option encourages the process of self evaluation and problem solving, while avoiding telling the client what to do. Encouraging the client to brainstorm about response options validates the nurse’s belief in the client’s personal competency and reinforces a coping strategy that will be needed when the nurse may not be available to offer solutions. 67. Therapeutic nurse-client interaction occurs when the nurse A) assists the client to clarify the meaning of what the client has said B) interprets the client’s covert communication C) praises the client for appropriate feelings and behavior D) advises the client on ways to resolve problems A: assists the client to clarify the meaning of what the client has said. Clarification is a facilitating/therapeutic communication strategy. Interpretation, changing the focus/subject, giving approval, and advising are non-therapeutic/barriers to communication. 68. Which nursing intervention will be most effective in helping a withdrawn client to develop relationship skills? A) Offer the client frequent opportunities to interact with 1 person B) Provide the client with frequent opportunities to interact with other clients C) Assist the client to analyze the meaning of the withdrawn behavior D) Discuss with the client the focus that other clients have similar problems A: Offer the client frequent opportunities to interact with 1 person. The withdrawn client is uncomfortable in social interaction. The nurse-client relationship is a corrective relationship in which the client learns both tolerance and skills for relationships. 69. An important goal in the development of a therapeutic inpatient milieu is to A) provide a businesslike atmosphere where clients can work on individual goals B) provide a group forum in which clients decide on unit rules, regulations, and policies C) provide a testing ground for new patterns of behavior while the client takes responsibility for his or her own actions D) discourage expressions of anger because they can be disruptive to other clients C: provide a testing ground for new patterns of behavior while the client takes responsibility for his or her own actions. A therapeutic milieu is purposeful and planned to provide safety and a testing ground for new patterns of behavior. 1070. A client with paranoid delusions stares at the nurse over a period of several days. The client suddenly walks up to the nurse and shouts "You think you’re so perfect and pure and good." An appropriate response for the nurse is A) "Is that why you’ve been staring at me?" B) "You seem to be in a really bad mood." C) "Perfect? I don’t quite understand." D) "You seem angry right now." D: "You seem angry right now.". The nurse recognizes the underlying emotion with a matter of fact attitude, but avoids telling the clients how they feel. 71. A client who is a former actress enters the day room wearing a sheer nightgown, high heels, numerous bracelets, bright red lipstick and heavily rouged cheeks. Which nursing action is the best in response to the client’s attire? A) Gently remind her that she is no longer on stage B) Directly assist client to her room for appropriate apparel C) Quietly point out to her the dress of other clients on the unit D) Tactfully explain appropriate clothing for the hospital B: Directly assist client to her room for appropriate apparel. It assists the client to maintain self-esteem while modifying behavior. 72. When teaching suicide prevention to the parents of a 15 year-old who recently attempted suicide, the nurse describes the following behavioral cue as indicating a need for intervention. A) Angry outbursts at significant others B) Fear of being left alone C) Giving away valued personal items D) Experiencing the loss of a boyfriend C: Giving away valued personal items. Eighty percent of all potential suicide victims give some type of indication that selfdestructiveness should be addressed. These clues might lead one to suspect that a client is having suicidal thoughts or is developing a plan. 73. Which statement made by a client indicates to the nurse that the client may have a thought disorder? A) "I’m so angry about this. Wait until my partner hears about this." B) "I’m a little confused. What time is it?" C) "I can't find my 'mesmer' shoes. Have you seen them?" D) "I’m fine. It's my daughter who has the problem." C: "I can''t find my ''mesmer'' shoes. Have you seen them?". A neologism is a new word self invented by a person and not readily understood by another. Using neologisms is often associated with a thought disorder. 74. In a psychiatric setting, the nurse limits touch or contact used with clients to handshaking because A) some clients misconstrue hugs as an invitation to sexual advances B) handshaking keeps the gesture on a professional level C) refusal to touch a client denotes lack of concern D) inappropriate touch often results in charges of assault and battery A: some clients misconstrue hugs as an invitation to sexual advances. Touch denotes positive feelings for another person. The client may interpret hugging and holding hands as sexual advances. 75. A client with anorexia is hospitalized on a medical unit due to electrolyte imbalance and cardiac dysrhythmias. Additional assessment findings that the nurse would expect to observe are A) brittle hair, lanugo, amenorrhea B) diarrhea, nausea, vomiting, dental erosion C) hyperthermia, tachycardia, increased metabolic rate D) excessive anxiety about symptoms A: brittle hair, lanugo, amenorrhea. Physical findings associated with anorexia also include reduced metabolic rate and lower vital signs. 76. Which intervention best demonstrates the nurse's sensitivity to a 16 year-old’s appropriate need for autonomy? A) Alertness for feelings regarding body image B) Allows young siblings to visit C) Provides opportunity to discuss concerns without presence of parents D) Explores his feelings of resentment to identify causes C: Provides opportunity to discuss concerns without presence of parents. This intervention provides the teen with the opportunity to have control and encourages decision making. 77. The nurse's primary intervention for a client who is experiencing a panic attack is to A) develop a trusting relationship B) assist the client to describe his experience in detail 11C) maintain safety for the client D) teach the client to control his or her own behavior C: maintain safety for the client. Clients who display signs of severe anxiety need to be supervised closely until the anxiety is decreased because they may harm themselves or others. 78. A client was admitted to the eating disorder unit with bulimia nervosa. The nurse assessing for a history of complications of this disorder expects A) Respiratory distress, dyspnea B) Bacterial gastrointestinal infections, overhydration C) Metabolic acidosis, constricted colon D) Dental erosion, parotid gland enlargement D: Dental erosion, parotid gland enlargement. Dental erosion and parotid gland enlargement due to purging are common complications of binge eating followed by self-induced vomiting. 79. Which of the following times is a depressed client at highest risk for attempting suicide? A) Immediately after admission, during one-to-one observation B) 7 to 14 days after initiation of antidepressant medication and psychotherapy C) Following an angry outburst with family D) When the client is removed from the security room B: 7 to 14 days after initiation of antidepressant medication and psychotherapy. As the depression lessens, the depressed client acquires energy to follow the plan. 80. A client is admitted to a psychiatric unit with delusions. What findings could the nurse observe that would be consistent with delusional thought patterns? A) Flight of ideas and hyperactivity B) Suspiciousness and resistance to therapy C) Anorexia and hopelessness D) Panic and multiple physical complaints B: Suspiciousness and resistance to therapy. Clinical features of paranoid delusional disorder include extreme suspiciousness, jealousy, distrust, and a belief that others intend to invoke harm. 81. As the nurse takes a history of a 3 year-old with neuroblastoma, what comments by the parents require follow-up and are consistent with the diagnosis? A) "The child has been listless and has lost weight." B) "The urine is dark yellow and small in amounts." C) "Clothes are becoming tighter across her abdomen." D) "We notice muscle weakness and some unsteadiness." C: "Clothes are becoming tighter across her abdomen.". One of the most common signs of neuroblastoma is increased abdominal girth. The parents'' report that clothing is tight is significant, and should be responded to with additional assessments. 82. Parents call the emergency room to report that a toddler has swallowed drain cleaner. The triage nurse instructs them to call for emergency transport to the hospital. The nurse would also suggest that the parents give the toddler sips of _______ while waiting for an ambulance. A) Tea B) Water C) Milk D) Soda B: Water. Small amounts of water will dilute the corrosive substance prior to gastric lavage. 83. A 16 year-old enters the emergency department. The triage nurse identifies that this teenager is legally married and signs the consent form for treatment. What would be the appropriate action by the nurse? A) Ask the teenager to wait until a parent or legal guardian can be contacted B) Withhold treatment until telephone consent can be obtained from the partner C) Refer the teenager to a community pediatric hospital emergency department D) Proceed with the triage process in the same manner as any adult client D: Proceed with the triage process in the same manner as any adult client. Minors may become known as an "emancipated minor" through marriage, pregnancy, high school graduation, independent living or service in the military. Therefore, this married client has the legal capacity of an adult. 84. The pediatric clinic nurse examines a toddler with a tentative diagnosis of neuroblastoma. Findings observed by the nurse that is associated with this problem include which of these? A) Lymphedema and nerve palsy B) Hearing loss and ataxia C) Headaches and vomiting D) Abdominal mass and weakness 12D: Abdominal mass and weakness. Clinical manifestations of neuroblastoma include an irregular abdominal mass that crosses the midline, weakness, pallor, anorexia, weight loss and irritability. 85. The nurse is preparing the teaching plan for a group of parents about risks to toddlers and is including the proper communication in the event of accidental poisoning. The nurse should tell the parents to first state what substance was ingested and then what information should be the priority for the parents to communicate? A) The parents' name and telephone number B) The currency of the immunization and allergy history of the child C) The estimated time of the accidental poisoning and a confirmation that the parents will bring the containers of the ingested substance D) The affected child's age and weight D: The affected child''s age and weight. All of the above information is important. However, after the substance is identified the age and weight are the priorities. This gives the appropriate health care providers an opportunity to calculate the needed dosage for an antidote while the child is being transported to the emergency department. After this information, the time of the 86. The nurse has admitted a 4 year-old with the diagnosis of possible rheumatic fever. Which statement by the parent would the nurse suspect is relevant to this disease? A) Our child had chickenpox 6 months ago. B) Strep throat went through all the children at the day care last month. C) Both ears were infected at 3 months of age. D) Last week both feet had a fungal skin infection. B: Strep throat went through all the children at the day care last month.. Evidence supports a strong relationship between infection with Group A streptococci and subsequent rheumatic fever (usually within 2 to 6 weeks). Therefore, the history of playmates recovering from strep throat would indicate that the child most likely also had strep throat. Sometimes such an infection has no clinical symptoms. 87. The nurse provides discharge teaching to the parents of a 15 month-old child with Kawasaki disease. The child has received immunoglobulin therapy. Which instruction would be appropriate? A) High doses of aspirin will be continued for some time B) Complete recovery is expected within several days C) Active range of motion exercises should be done frequently D) The measles, mumps and rubella vaccine should be delayed D: The measles, mumps and rubella vaccine should be delayed. Discharge instructions for a child with Kawasaki disease should include the information that immunoglobulin therapy may interfere with the body''s ability to form appropriate amounts of antibodies. Therefore, live immunizations should be delayed. 88. A 10 year-old client is recovering from a splenectomy following a traumatic injury. The clients laboratory results show a hemoglobin of 9 g/dL and a hematocrit of 28 percent. The best approach for the nurse to use is to A) limit milk and milk products B) encourage bed activities and games C) plan nursing care around lengthy rest periods D) promote a diet rich in iron C: plan nursing care around lengthy rest periods. The initial priority for this client is rest due to the inability of red blood cells to carry oxygen. 89. The nurse is planning care for a 14 year-old client returning from scoliosis corrective surgery. Which of the following actions should receive priority in the plan? A) Antibiotic therapy for 10 days B) Teach client isometric exercises for legs C) Assess movement and sensation of extremities D) Assist to stand up at bedside within the first 24 hours C: Assess movement and sensation of extremities. Following corrective surgery for scoliosis, neurological status requires special attention and assessment, especially that of the extremities. 90. The nurse is teaching parents about accidental poisoning in children. Which point should be emphasized? A) Call the Poison Control Center once the situation is identified B) Empty the child's mouth in any case of possible poisoning C) Keep the child as quiet as possible if a toxic substance was inhaled D) Do not induce vomiting if the poison is a hydrocarbon B: Empty the child''s mouth in any case of possible poisoning. Emptying the mouth of poison prevents further ingestion and should be done first to limit damage from the substance. Note that all of the actions are correct, but option B is the priority. 91. The nurse is assessing an 8 month-old infant with a malfunctioning ventriculoperitoneal shunt. Which one of the following manifestations would the infant be most likely to exhibit? A) Lethargy 13B) Irritability C) Negative Moro D) Depressed fontanel B: Irritability. Signs of increased intracranial pressure (IICP) in infants include bulging fontanel, instability, high-pitched cry, and cries when held. Vital sign changes include pulse that is variable, e.g., rapid, slow and bounding, or feeble. Respirations are more often slow, deep, and irregular. 92. The nurse is caring for a 4 year-old two hours after tonsillectomy and adenoidectomy. Which of the following assessments must be reported immediately? A) Vomiting of dark emesis B) Complaints of throat pain C) Apical heart rate of 110 D) Increased restlessness D: Increased restlessness. Restlessness and increased respiratory and heart rates are often early signs of hemorrhage. 93. The nurse is caring for a client with sickle cell disease who is scheduled to receive a unit of packed red blood cells. Which of the following is an appropriate action for the nurse when administering the infusion? A) Storing the packed red cells in the medicine refrigerator while starting IV B) Slow the rate of infusion if the client develops fever or chills C) Limit the infusion time of each of the unit to a maximum of 4 hours D) Assess vital signs every 15 minutes throughout the entire infusion C: Limit the infusion time of each of the unit to a maximum of 4 hours. Infuse the specified amount of blood within 4 hours. If the infusion will exceed this time, the blood should be divided into appropriately sized quantities. 94. The nurse is caring for a 17 month-old with acetaminophen poisoning. Which of the following lab reports should the nurse review first? A) Prothrombin Time (PT) and partial thromboplastin time (PTT) B) Red blood cell and white blood cell counts C) Blood urea nitrogen and creatinine clearance D) Liver enzymes (AST and ALT) D: Liver enzymes (AST and ALT). Because acetaminophen is toxic to the liver and causes hepatic cellular necrosis, liver enzymes are released into the blood stream and serum levels of those enzymes rise. Other lab values are reviewed as well. 95. A nurse admits a premature infant who has respiratory distress syndrome (RDS). In planning care, nursing actions are based on the fact that the most likely cause of this problem stems from the infant's inability to A) stabilize thermoregulation B) maintain alveolar surface tension C) begin normal pulmonary blood flow D) regulate intracardiac pressure B: maintain alveolar surface tension. RDS is primarily a disease related to a developmental delay in lung maturation. Although many factors may lead to the development of the problem, the central factor is the lack of a normally functioning surfactant system in the alveolar sac from immaturity in lung development since the infant is premature. 96. The nurse is planning care for a 3 month-old infant immediately postoperative following placement of a ventriculoperitoneal shunt for hydrocephalus. The nurse needs to A) assess for abdominal distention B) maintain infant in an upright position C) begin formula feedings when infant is alert D) pump the shunt to assess for proper function A: assess for abdominal distention. The child is observed for abdominal distention because cerebrospinal fluid may cause peritonitis or a postoperative ileus as a complication of distal catheter placement. 97. A 6 year-old child is seen for the first time in the clinic. Upon assessment, the nurse finds that the child has deformities of the joints, limbs, and fingers, thinned upper lip, and small teeth with faulty enamel. The mother states: ”My child seems to have problems in learning to count and recognizing basic colors.” Based on this data, the nurse suspects that the child is most likely showing the effects of which problem? A) congenital abnormalities B) chronic toxoplasmosis C) fetal alcohol syndrome (FAS) D) lead poisoning C: fetal alcohol syndrome (FAS). Major features of FAS consist of facial and associated physical features, such as small head circumference and brain size (microcephaly), small eyelid openings, a sunken nasal bridge, an exceptionally thin upper lip, a short, upturned nose and a smooth skin surface between the nose and upper lip. Vision difficulties include nearsightedness (myopia). Other findings are mental retardation, delayed development, abnormal behavior such as short attention span, hyperactivity, poor impulse control, extreme nervousness and anxiety. Many behavioral problems, cognitive impairment and psychosocial deficits are also associated with this syndrome. 1498. A 15 year-old client has been placed in a Milwaukee brace. Which statement from the adolescent indicates the need for additional teaching? A) "I will only have to wear this for 6 months." B) "I should inspect my skin daily." C) "The brace will be worn day and night." D) "I can take it off when I shower." A: "I will only have to wear this for 6 months.". The brace must be worn long-term, during periods of growth, usually for 1 to 2 years. It is used to correct curvature of the spine. 99. The nurse is caring for a 4 year-old admitted after receiving burns to more than 50% of his body. Which laboratory data should be reviewed by the nurse as a priority in the first 24 hours? A) Blood urea nitrogen B) Hematocrit C) Blood glucose D) White blood count A: Blood urea nitrogen. Glomerular filtration is decreased in the initial response to severe burns, with fluid shift occurring. Kidney function must be monitored closely, or renal failure may follow in a few days. 100. The nurse is caring for a client with a colostomy pouch. During a teaching session, the nurse appropriately recommends that the pouch be emptied A) when it is 1/3 to 1/2 full B) prior to meals C) after each fecal elimination D) at the same time each day A: when it is 1/3 to 1/2 full. If the pouch becomes more than half full it may separate from the flange. 101. An 18 year-old client is admitted to intensive care from the emergency room following a diving accident. The injury is suspected to be at the level of the 2nd cervical vertebrae. The nurse's priority assessment should be the client’s A) response to stimuli B) bladder control C) respiratory function D) muscle weakness C: respiratory function. Spinal injury at the C-2 level results in quadriplegia. While the client will experience all of the problems identified, respiratory assessment is a priority. 102. A client has been admitted to the coronary care unit with a myocardial infarction. Which nursing diagnosis should have priority? A) pain related to ischemia B) risk for altered elimination: constipation C) risk for complication: dysrhythmias D) anxiety related to pain A: pain related to ischemia. Pain is related to ischemia of the heart muscle, and relief of pain will decrease myocardial oxygen demands, reduce blood pressure and heart rate and relieve anxiety. Pain also stimulates the sympathetic nervous system and increased preload, further increasing myocardial demands. 103.The nurse is caring for a client with a distal tibia fracture. The client has had a closed reduction and application of a toe to groin cast. 36 hours after surgery, the client suddenly becomes confused, short of breath and spikes a temperature of 103 degrees Fahrenheit. The first assessment the nurse should perform is A) orientation to time, place and person B) pulse oximetry C) circulation to casted extremity D) blood pressure B: pulse oximetry. Restlessness, confusion, irritability and disorientation may be the first signs of fat embolism syndrome followed by a very high temperature. The nurse needs to confirm hypoxia first. 104.The nurse is assessing a client with a Stage 2 skin ulcer. Which of the following treatments is most effective to promote healing? A) Covering the wound with a dry dressing B) Using hydrogen peroxide soak C) Leaving the area open to dry D) Applying a hydrocolloid or foam dressing D: Applying a hydrocolloid or foam dressing. While the previously accepted treatment was a transparent cover, evidence now indicates that the foam (DuoDerm) dressings work best. 15105.A client is recovering from a thyroidectomy. While monitoring the client's initial post-operative condition, which of the following should the nurse report immediately? A) Tetany and paresthesia B) Mild stridor and hoarseness C) Irritability and insomnia D) Headache and nausea A: Tetany and paresthesia. Because the parathyroid gland may be damaged in this surgery, secondary hypocalcemia may occur. Findings of hypoparathyroidism include tetany, paresthesia, muscle cramps and seizures. 106. A client is scheduled for an intravenous pyelogram (IVP). Which of the following data from the client’s history indicate a potential hazard for this test? A) Reflex incontinence B) Allergy to shellfish C) Claustrophobia D) Hypertension B: Allergy to shellfish. It is important to know if the client has an allergy to iodine or shellfish. If the client does, they may have an allergic reaction to the IVP contrast dye injected during the procedure. 107. A client enters the emergency department unconscious via ambulance. What document should be given priority to guide the direction of care for this client? A) The statement of client rights and the client self determination act B) Orders written by the provider C) A notarized original of advance directives brought in by the partner D) The clinical pathway protocol of the agency and the emergency department C: A notarized original of advance directives brought in by the partner. This document specifies the client''s wishes. 108. A client diagnosed with hepatitis C discusses his health history with the admitting nurse. The nurse should recognize which statement by the client as the most important? A) I got back from Central America a few weeks ago. B) I had the best raw oysters last week. C) I have many different sex partners. D) I had a blood transfusion 15 years ago. D: I had a blood transfusion 15 years ago.. The client who was transfused prior to blood screening for hepatitis C may show findings many years later. Options B and C are associated with risk of hepatitis B. 109. Which of these children at the site of a disaster at a child day care center would the triage nurse put in the "treat last" category? A) An infant with intermittent bulging anterior fontanel between crying episodes B) A toddler with severe deep abrasions over 98% of the body C) A preschooler with a lower leg fracture on one side and an upper leg fracture on the other D) A school-age child with singed eyebrows and hair on the arms B: A toddler with severe deep abrasions over 98% of the body. This child has the least chance of survival. Severe deep abrasions should be thought of as second and third degree burns. The child has great risk of both shock and infection combined. 110. A client has returned to the unit following a renal biopsy. Which of the following nursing interventions is appropriate? A) Ambulate the client 4 hours after procedure B) Maintain client on NPO status for 24 hours C) Monitor vital signs D) Change dressing every 8 hours C: Monitor vital signs. The potential complication of this procedure is internal hemorrhage. Monitoring vital signs is critical to detect early indications of bleeding. 111. The nurse is providing instructions for a client with asthma. Which of the following should the client monitor on a daily basis? A) Respiratory rate B) Peak air flow volumes C) Pulse oximetry D) Skin color B: Peak air flow volumes. The peak airflow volume decreases about 24 hours before clinical manifestations of exacerbation of asthma. 112.A client with a documented pulmonary embolism has the following arterial blood gases: PO2 - 70 mm hg, PCO2 - 32 mm hg, pH - 7.45, SaO2 - 87%, HCO3 - 22. Based on these data, what is the first nursing action? 16A) Review other lab data B) Notify the health care provider C) Administer oxygen D) Calm the client C: Administer oxygen. The client has a low PCO2 due to increased respiratory rate from the hypoxemia and signs of respiratory alkalosis. Immediate intervention is indicated. 113. The nurse is teaching a newly diagnosed asthma client on how to use a peak flow meter. The nurse explains that this should be used to A) determine oxygen saturation B) measure forced expiratory volume C) monitor atmosphere for presence of allergens D) provide metered doses for inhaled bronchodilator B: measure forced expiratory volume. The peak flow meter is used to measure peak expiratory flow volume. It provides useful information about the presence and/or severity of airway obstruction. 114. The nurse is assessing a 55 year-old female client who is scheduled for abdominal surgery. Which of the following information would indicate that the client is at risk for thrombus formation in the post-operative period? A) Estrogen replacement therapy B) 10% less than ideal body weight C) Hypersensitivity to heparin D) History of hepatitis A: Estrogen replacement therapy. Estrogen increases the hypercoagulability of the blood and increased the risk for development of thrombophlebitis. 115. During the check up of a 2 month-old infant at a well baby clinic, the mother expresses concern to the nurse because a flat pink birthmark on the baby's forehead and eyelid has not gone away. What is an appropriate response by the nurse? A) "Mongolian spots are a normal finding in dark-skinned children." B) "Port wine stains are often associated with other malformations." C) "Telangiectatic nevi are normal and will disappear as the baby grows." D) "The child is too young for consideration of surgical removal of these at this time." C: Telangiectatic nevi, salmon patch or stork bite birthmarks, are a normal variation and the facial nevi will generally disappear by ages 1 to 2 years. 116. A 3 year-old child diagnosed as having celiac disease attends a day care center. Which of the following would be an appropriate snack? A) Cheese crackers B) Peanut butter sandwich C) Potato chips D) Vanilla cookies C: Children with celiac disease should eat a gluten free diet. Gluten is found mainly in grains of wheat and rye and in smaller quantities in barley and oats. Corn, rice, soybeans and potatoes are digestible by persons with celiac disease.: F.A. Davis Company. 117. A nurse assigned to a manipulative client for 5 days becomes aware of feelings of reluctance to interact with the client. The next action by the nurse should be to A) Discuss the feeling of reluctance with an objective peer or supervisor B) Limit contacts with the client to avoid reinforcement of the manipulative behavior C) Confront the client about the negative effects of behaviors on other clients and staff D) Develop a behavior modification plan that will promote more functional behavior A: Discuss the feeling of reluctance with an objective peer or supervisor. The nurse who experiences stress in the therapeutic relationship can gain objectivity through supervision. The nurse must attempt to discover attitudes and feelings in the self that influence the nurse-client relationship. 118. A client is being treated for paranoid schizophrenia. When the client became loud and boisterous, the nurse immediately placed him in seclusion as a precautionary measure. The client willingly complied. The nurse’s action A) may result in charges of unlawful seclusion and restraint B) leaves the nurse vulnerable for charges of assault and battery C) was appropriate in view of a client history of violence D) was necessary to maintain the therapeutic milieu of the unit A: may result in charges of unlawful seclusion and restraint. Seclusion should only be used when there is an immediate threat of violence or threatening behavior toward the staff, the other clients, or the client himself. 119. The provisions of the law for the Americans with Disabilities Act require nurse managers to A) Maintain an environment free from associated hazards B) Provide reasonable accommodations for disabled individuals 17C) Make all necessary accommodations for disabled individuals D) Consider both mental and physical disabilities B: Provide reasonable accommodations for disabled individuals. The law is designed to permit persons with disabilities access to job opportunities. Employers must evaluate an applicant’s ability to perform the job and not discriminate on the basis of a disability. Employers also must make "reasonable accommodations." 120. Upon completing the admission documents, the nurse learns that the 87 year-old client does not have an advance directive. What action should the nurse take? A) Record the information on the chart B) Give information about advance directives C) Assume that this client wishes a full code D) Refer this issue to the unit secretary B: Give information about advance directives. For each admission, nurses should request a copy of the current advance directive. If there is none, the nurse must offer information about what an advance directive implies. It is then the client’s choice to sign it. In option 1 just recording the information is not sufficient. In option 3 the nurse should not assume that the client has been informed of choices for emergency care. In option 4 this represents an inappropriate delegation approach. 121.A client with a diagnosis of Methicillin resistant Staphylococcus aureus (MRSA) has died. Which type of precautions is appropriate to use when performing postmortem care? A) Airborne precautions B) Droplet precautions C) Contact precautions D) Compromised host precautions C: Contact precautions. The resistant bacteria remain alive for up to 3 days after the client dies. Therefore, contact precautions must still be implemented. The body should also be labeled as MRSA-contaminated so that the funeral home staff can protect themselves as well. Gown and gloves are required. 122. An 8 year-old client is admitted to the hospital for surgery. The child’s parent reports the allergies listed below. Which of these allergies should all health care personnel be aware of? A) Shellfish B) Molds C) Balloons D) Perfumed soap C: Balloons. Allergy to balloons indicates a latex allergy. All personnel in contact with the child will need to be aware of this condition and use non-latex gloves. 123.A nurse is stuck in the hand by an exposed used hypodermic needle. What immediate action should the nurse take? A) Look up the policy on needle sticks B) Contact employee health services C) Immediately wash the hands with vigor D) Notify the supervisor and risk management C: Immediately wash the hands with vigor. The immediate action of vigorously washing will help remove possible contamination. Then the sequence would be options D, A, B. 124. The nurse is having difficulty reading the health care provider's written order that was left just before the shift change. What action should be taken? A) Leave the order for the oncoming staff to follow-up on B) Contact the charge nurse for an interpretation C) Ask the pharmacy for assistance in the interpretation D) Call the provider for clarification D: Call the provider for clarification. Relying on anyone else''s interpretation is very risky. When in doubt, check it out with the person who wrote the difficult-to-read order. Order entry systems help to minimize this problem. 125. When admitting a client to an acute care facility, an identification bracelet is sent up with the admission form. In the event these do not match, the nurse’s best action is to A) change whichever item is incorrect to the correct information B) use the bracelet and admission form until a replacement is supplied C) notify the admissions office and wait to apply the bracelet D) make a corrected identification bracelet for the client C: notify the admissions office and wait to apply the bracelet. The Admissions Office has the responsibility to verify the client’s identity and keep all the records in the system consistent. Making the changes puts the client at risk for misidentification. Using an incorrect identification bracelet is unsafe. 18126.The nurse is planning discharge for a 90 year-old client with musculo-skeletal weakness. Which intervention should be included in the plan that would be most effective for the prevention of falls? A) Place nightlights in the bedroom B) Wear eyeglasses at all times C) Install grab bars in the bathroom D) Teach muscle strengthening exercises A: Place nightlights in the bedroom. Because more falls occur in the bedroom than any other location, begin there. However, work in partnership with the client and family so they are willing to move furniture, lamp cords, and storage areas, add lighting, remove throw rugs, and eliminate other environmental hazards. 127.An 8 year-old child is hospitalized during the edema phase of minimal change nephrotic syndrome. The nurse is assisting in choosing the lunch menu. Which menu is the best choice? A) Bologna sandwich, pudding, milk B) Frankfurter, baked potato, milk C) Chicken strips, corn on the cob, milk D) Grilled cheese sandwich, apple, milk C: Chicken strips, corn on the cob, milk. This menu is lowest in sodium. Ideally, low fat milk would be available. 128. The nurse is teaching a client with non-insulin dependent diabetes mellitus about the prescribed diet. The nurse should teach the client to A) maintain previous calorie intake B) keep a candy bar available at all times C) reduce carbohydrates intake to 25% of total calories D) keep a regular schedule of meals and snacks D: keep a regular schedule of meals and snacks. Currently, calorie-controlled diets with strict meal plans are rarely suggested for clients who have diabetes. Try to incorporate schedule or food changes into clients'' existing dietary patterns. Help clients learn to read labels and identify specific canned foods, frozen entrees, or other foods which are acceptable and those which should be avoided. 129. A depressed client in an assisted living facility tells the nurse that "life isn't worth living anymore." What is the best response to this statement? A) "Come on, it is not that bad." B) "Have you thought about hurting yourself?" C) "Did you tell that to your family?" D) "Think of the many positive things in life." B: "Have you thought about hurting yourself?". It is appropriate and necessary to determine if someone who has voiced thoughts about death is considering a suicidal act. This response is most therapeutic in the circumstances. Options A and D deny the validity of the client’s statement, and the purpose of option C is unclear and it lacks client focus. 130. The nurse is observing a client with an obsessive-compulsive disorder in an inpatient setting. Which behavior is consistent with this diagnosis? A) Repeatedly checking that the door is locked B) Verbalized suspicions about thefts C) Preference for consistent caregivers D) Repetitive, involuntary movements A: Repeatedly checking that the door is locked. Behaviors that are repeated are symptomatic of obsessive-compulsive disorders. These behaviors, performed to reduced feelings of anxiety, often interfere with normal function and employment. 131.A female client is admitted for a breast biopsy. She says, tearfully to the nurse, "If this turns out to be cancer and I have to have my breast removed, my partner will never come near me." The nurse's best response would be which of these statements? A) "I hear you saying that you have a fear for the loss of love." B) "You sound concerned that your partner will reject you." C) "Are you wondering about the effects on your sexuality?" D) "Are you worried that the surgery will lead to changes?" D: "Are you worried that the surgery will lead to changes?". This is a general lead in type of response that encourages further discussion without focusing on an area that the nurse, but possibly not the client, feels is a problem. 132. A client is admitted for treatment of a right upper lobe infiltrate and to rule out tuberculosis. Which of these would be the most appropriate self-protective action by the nurse ? A) Provide negative room ventilation B) Wear a face mask with shield C) Wear a particulate respirator mask D) Institute airborne precautions 19C: Wear a particulate respirator mask. Tight fitting, high-efficiency masks are required when caring for clients who have a suspected communicable disease of the airborne variety. 133. The charge nurse has a health care team that consists of 1 practical nurse (PN), 1 unlicensed assistive personnel (UAP) and 1 PN nursing student. Which assignment should be questioned by the nurse manager? A) An admission at the change of shifts with atrial fibrillation and heart failure - PN B) Client who had a major stroke 6 days ago - PN nursing student C) A child with burns who has packed cells and albumin IV running - charge nurse D) An elderly client who had a myocardial infarction a week ago – UAP A: An admission at the change of shifts with atrial fibrillation and heart failure - PN. The care for a new admissions should be performed by an RN. Since the client was admitted at the change of shifts, the stability of the client would not have been established. The charge nurse should take this client. The PN could monitor the IV fluids in option C. Tasks that do not require independent judgment should be delegated. The nurse may delegate the care for a stable client to a UAP. 134. The nurse is teaching an elderly client how to use MDI's (multi-dose inhalers). The nurse is concerned that the client is unable to coordinate the release of the medication with the inhalation phase. What is the nurse's best recommendation to improve delivery of the medication? A) Nebulized treatments for home care B) Adding a spacer device to the MDI canister C) Asking a family member to assist the client with the MDI D) Request a visiting nurse to follow the client at home B: Adding a spacer device to the MDI canister. If the client is not using the MDI properly, the medication can get trapped in the upper airway, resulting in dry mouth and throat irritation. Using a spacer will allow more drug to be deposited in the lungs and less in the mouth. It is especially useful in the elderly because it allows more time to inhale and requires less eye-hand coordination. 135.The nurse is teaching a client newly diagnosed with asthma how to use the metered-dose inhaler (MDI). The client asks when they will know the canister is empty. The best response is A) Drop the canister in water to observe floating B) Estimate how many doses are usually in the canister C) Count the number of doses as the inhaler is used D) Shake the canister to detect any fluid movement A: Drop the canister in water to observe floating. Dropping the canister into a bowl of water assesses the amount of medications remaining in a metered-dose inhaler. The client should obtain a refill when the inhaler rises to the surface and begins to tip over. Some of the newer canisters have counters. 136.A client has an order for 1000 ml of D5W over an 8 hour period. The nurse discovers that 800 ml has been infused after 4 hours. What is the priority nursing action? A) Ask the client if there are any breathing problems B) Have the client void as much as possible C) Check the vital signs D) Auscultate the lungs D: Auscultate the lungs. All of the options would be part of the evaluation for the effects of the large amount of fluid in a short period of time. However the worst result is heart failure with lung congestion so the auscultation of the lungs is the priority action. The sequence of actions would be D, A, C, B. 137. A nurse observes a family member administer a rectal suppository by having the client lie on the left side for the administration. The family member pushed the suppository until the finger went up to the second knuckle. After 10 minutes the client was told by the family member to turn to the right side and the client did this. What is the appropriate comment for the nurse to make? A) Why don’t we now have the client turn back to the left side. B) That was done correctly. Did you have any problems with the insertion? C) Let’s check to see if the suppository is in far enough. D) Did you feel any stool in the intestinal tract? B: That was done correctly. Did you have any problems with the insertion?. Left side-lying position is the optimal position for the client receiving rectal medications. Due to the position of the descending colon, left side-lying allows the medication to be inserted and move along the natural curve of the intestine and facilitates retention of the medication. After a short time it will not hurt the client to turn in any manner. The suppository should be somewhat melted after 10 to 15 minutes. The other responses are incorrect since no data are in the stem to support such comments. 138. As the nurse observes the student nurse during the administration of a narcotic analgesic IM injection, the nurse notes that the student begins to give the medication without first aspirating. What should the nurse do? A) Ask the student: "What did you forget to do?” B) Stop. Tell me why aspiration is needed. C) Loudly state: “You forgot to aspirate.” 20D) Walk up and whisper in the student’s ear “Stop. Aspirate. Then inject.” D: Walk up and whisper in the student’s ear “Stop. Aspirate. Then inject.”. This action is a direct threat to the client if the medication enters into the blood stream instead of the muscle. The purpose of aspiration with IM injections is to prevent the injection of the drug directly into the blood stream. Option 4 protects the client and is the most professional. 139. An adult client is found to be unresponsive on morning rounds. After checking for responsiveness and calling for help, the next action that should be taken by the nurse is to: A) check the carotid pulse B) deliver 5 abdominal thrusts C) give 2 rescue breaths D) ensure an open airway D: ensure an open airway. According to the ABCs of CPR the first step in rescuing an unresponsive victim after checking responsiveness and calling for help is to open the victims airway. The airway must be opened appropriately before the need for rescue breaths can be determined. The pulse is assessed, after breathing is evaluated. The need for abdominal thrusts is determined by inability to achieve chest rise when ventilation is attempted. 140. A practical nurse (PN) is assigned to care for a newborn with a neural tube defect. Which dressing, if applied by the PN, would need no further intervention by the charge nurse? A) Telfa dressing with antibiotic ointment B) Moist sterile nonadherent dressing C) Dry sterile dressing that is occlusive D) Sterile occlusive pressure dressing B: Moist sterile nonadherent dressing. Before surgical closure, the sac is prevented from drying by the application of a sterile, moist, nonadherent dressing over the defect. Dressings are changed frequently to keep them moist. 141. A parent brings her 3 month-old into the clinic, reporting that the child seems to be spitting up all the time and has a lot of gas. The nurse expects to find which of the following on the initial history and physical assessment? A) increased temperature and lethargy B) restlessness and increased mucus production C) increased sleeping and listlessness D) diarrhea and poor skin turgor B: restlessness and increased mucus production. This infant could be experiencing gastroesophageal reflux, or could be allergic to the formula. Restlessness, irritability and increased mucus production can develop if an allergy is present. Soy based formula is often recommended. 142.The nurse manager hears a provider loudly criticize one of the staff nurses within the hearing range of others. The nurse manager's next action should be to A) Walk up to the provider and quietly state: "Stop this unacceptable behavior." B) Allow the staff nurse to handle this situation without interference C) Notify the of the other administrative persons of a breech of professional conduct D) Request an immediate private meeting with the provider and staff nurse D: Request an immediate private meeting with the provider and staff nurse. Assertive communication respects the needs of all parties to express themselves, but not at the expense of others. The nurse manager needs first to protect clients and other staff from this display and come to the assistance of the nurse employee. 143. The charge nurse is planning assignments on a medical unit. The client with _______should be assigned to the unlicensed assistive personnel (UAP). A) d ifficulty swallowing after a mild stroke B) an order of enemas until clear prior to colonoscopy C) an order for a post-op abdominal dressing change D) transfer orders to a long term facility B: an order of enemas until clear prior to colonoscopy. The UAP can be assigned routine tasks which have predictable outcomes. 144. The nurse manager has been using a block scheduling plan to staff the nursing unit. However, staff have asked for many changes and exceptions to the schedule over the past few months. The manager considers self-scheduling knowing that this method will A) Improve the quality of care B) Decrease staff turnover C) Minimize the amount of overtime payouts D) Improve team morale D: Improve team morale. Nurses are more satisfied when opportunities exist for autonomy and control. The nurse manager becomes the facilitator of scheduling rather than the decision-maker of the schedule when self-scheduling exists. 145. A client is admitted to a voluntary hospital mental health unit due to suicidal ideation. The client has been on the unit for 2 days and now states “I demand to be released now!” The appropriate from the nurse is 21A) You cannot be released because you are still suicidal. B) You can be released only if you sign a no suicide contract. C) Let’s discuss your decision to leave and then we can prepare you for discharge. D) You have a right to sign out as soon as we get the provider's discharge order. C: Let’s discuss your decision to leave and then we can prepare you for discharge.. Clients voluntarily admitted to the hospital have a right to demand and obtain release. Discussing the decision initially allows an opportunity for other interventions. 146.The nurse is caring for a client who is post-op following a thoracotomy. The client has 2 chest tubes in place, connected to 1 chest drain. The nursing assessment reveals bubbling in the water seal chamber when the client coughs. What is the most appropriate nursing action? A) Clamp the chest tube B) Call the surgeon immediately C) Continue to monitor the client to see if the bubbling increases D) Instruct the client to try to avoid coughing C: Continue to monitor the client to see if the bubbling increases. Bubbling associated with coughing after lung surgery is to be expected as small amounts of air escape the pleural space when pressures inside the chest increase with coughing. Monitoring is the only nursing action required at this time. 147. A newly admitted elderly client is severely dehydrated. When planning care for this client, which task is appropriate to assign to an unlicensed assistive personnel (UAP)? A) Converse with the client to determine if the mucous membranes are impaired B) Report hourly outputs of less than 30 ml/hr C) Monitor client's ability for movement in the bed D) Check skin turgor every 4 hours B: Report hourly outputs of less than 30 ml/hr. When directing a UAP, the nurse must communicate clearly about each delegated task with specific instructions on what must be reported. Because the RN is responsible for all care-related decisions, only implementation tasks should be assigned because they do not require independent judgment. 148. Which statement best describes time management strategies applied to the role of a nurse manager? A) Schedule staff efficiently to cover the anticipated needs on the managed unit B) Assume a fair share of direct client care as a role model C) Set daily goals with a prioritization of the work D) Delegate tasks to reduce work load associated with direct care and meetings C: Set daily goals with a prioritization of the work. Time management strategies include setting goals and prioritization . This is similar to time management of direct care for clients 149. The charge nurse on the night shift at an urgent care center has to deal with admitting clients of a higher acuity than usual because of a large fire in the area. Which style of leadership and decision-making would be best in this circumstance? A) Assume a decision-making role B) Seek input from staff C) Use a non-directive approach D) Shared decision-making with others A: Assume a decision-making role. Authoritarian leadership assumes that decision-making is the role of the leader with little input by subordinates. This style is best used in emergency situations or as a triage nurse. 150. Which activity can the RN ask an unlicensed assistive personnel (UAP) to perform? A) Take a history on a newly admitted client B) Adjust the rate of a gastric tube feeding C) Check the blood pressure of a 2 hours post operative client D) Check on a client receiving chemotherapy C: Check the blood pressure of a 2 hours post operative client. UAPs must be assigned tasks that require no nursing judgment or decision making situations. Vital signs on stable clients are commonly assigned to unlicensed staff. 22Management of Care 1. The nurse receives a report on an older adult client with middle stage dementia. What information suggests the nurse should do immediate follow up rather than delegate care to the nursing assistant? The client A) has had a change in respiratory rate by an increase of 2 breaths B) has had a change in heart rate by an increase of 10 beats C) was minimally responsive to voice and touch D) has had a blood pressure change by a drop in 8 mmHg systolic C: was minimally responsive to voice and touch. A change in level of consciousness indicates delirium related to acute illness. This would require the assessment of a nurse. The other changes could occur within the range of normal fluctuations. 2. A client tells the nurse, "I have something very important to tell you if you promise not to tell." The best response by the nurse is A) "I must document and report any information." B) "I can’t make such a promise." C) "That depends on what you tell me." D) "I must report everything to the treatment team." B: "I can’t make such a promise." Secrets are inappropriate in therapeutic relationships and are counter productive to the therapeutic efforts of the interdisciplinary team. Secrets may be related to risk for harm to self or others. The nurse honors and helps clients to understand rights, limitations, and boundaries regarding confidentiality. 3. The nurse is caring for a 69 year-old client with a diagnosis of hyperglycemia. Which tasks could the nurse delegate to the unlicensed assistive personnel (UAP)? A) Test blood sugar every 2 hours by Accu-Check B) Review with family and client signs of hyperglycemia C) Monitor for mental status changes D) Check skin condition of lower extremities A: Test blood sugar every 2 hours by Accu-Check. The UAP can do standard, unchanging procedures. 4. A nurse from the maternity unit is floated to the critical care unit because of staff shortage on the evening shift. Which client would be appropriate to assign to this nurse? A client with A) a Dopamine drip IV with vital signs monitored every 5 minutes B) a myocardial infarction that is free from pain and dysrhythmias C) a tracheotomy of 24 hours in some respiratory distress D) a pacemaker inserted this morning with intermittent capture B: A myocardial infarction that is free from pain and dysrhythmias. This client is the most stable with minimal risk of complications or instability. The nurse can utilize basic nursing skills to care for this client. 5. Which task could be safely delegated by the nurse to an unlicensed assistive personnel (UAP)? A) Be with a client who self-administers insulin B) Cleanse and dress a small decubitus ulcer C) Monitor a client's response to passive range of motion exercises D) Apply and care for a client's rectal pouch D: Apply and care for a client''s rectal pouch. The RN may delegate the application and care of rectal pouches to a UAP. This is an uncomplicated, routine task. 6. The unlicensed assistive personnel (UAP) reports a sudden increase in temperature to 101 degrees Fahrenheit for a post surgical client. The nurse checks on the client’s condition and observes a cup of steaming coffee at the bedside. What instructions are appropriate to give to the UAP? 23A) Encourage oral fluids to prevent dehydration B) Recheck temperature 15 minutes after removing hot liquids from the bedside C) Ask the client to drink only cold water and juices D) Chart this temperature elevation on the flow sheet B: Recheck temperature 15 minutes after removing hot liquids from the bedside. Recheck temperature to eliminate possible artificial elevation of temperature. Hot liquids, smoking, eating, chewing gum, and talking can all elevate temperature. Waiting to take the temperature for 15 minutes will help the temperature return to its normal, in order to get an accurate reading. Avoid premature assumptions about explanations for findings. The other options are incorrect. 7. A client has a nasogastric tube after colon surgery. Which one of these tasks can be safely delegated to an unlicensed assistive personnel (UAP)? A) To observe the type and amount of nasogastric tube drainage B) Monitor the client for nausea or other complications C) Irrigate the nasogastric tube with the ordered irrigant D) Perform nostril and mouth care D: Perform nostril and mouth care. Skin care around a nasogastric tube is a routine task that is appropriate for UAPs. The other tasks would be appropriate for a PN or RN to do since they are advanced skills or require evaluation. 8. A client asks the nurse to call the police and states: “I need to report that I am being abused by a nurse.” The nurse should first A) focus on reality orientation to place and person B) assist with the report of the client’s complaint to the police C) obtain more details of the client’s claim of abuse D) document the statement on the client’s chart with a report to the manager C: Obtain more details of the client’s claim of abuse. The advocacy role of the professional nurse as well as the legal duty of the reasonable prudent nurse requires the investigation of claims of abuse or violation of rights. The nurse is legally accountable for actions delegated to others. The application of the nursing process requires that the nurse gather more information, further assessment, before documentation or the reporting of the complaint. 9. When assessing a client, it is important for the nurse to be informed about cultural issues related to the client's background because A) normal patterns of behavior may be labeled as deviant, immoral, or insane B) the meaning of the client's behavior can be derived from conventional wisdom C) personal values will guide the interaction between persons from 2 cultures D) the nurse should rely on her knowledge of different developmental mental stages A: Normal patterns of behavior may be labeled as deviant, immoral, or insane. Culture is an important variable in the assessment of individuals. To work effectively with clients, the nurse must be aware of a cultural distinctive qualities. 10. The nursing student is discussing with a preceptor the delegation of tasks to an unlicensed assistive personnel (UAP). Assigning which of these tasks to a UAP indicates the student needs further teaching about the delegation process? A) Assist a client post cerebral vascular accident to ambulate B) Feed a 2 year-old in balanced skeletal traction C) Care for a client with discharge orders D) Collect a sputum specimen for acid fast bacillus C: Care for a client with discharge orders. A registered nurse (RN) is the best person to do teaching or evaluation that is needed at time of discharge. 11. The nurse is responsible for several elderly clients, including a client on bed rest with a skin tear and hematoma from a fall 2 days ago. What is the best care assignment for this client? A) Assign an RN to provide total care of the client B) Assign a nursing assistant to help the client with self-care activities C) Delegate complete care to an unlicensed assistive personnel D) Supervise a nursing assistant for skin care D: Supervise a nursing assistant for skin care. The nursing assistant can inspect the skin while giving hygiene care, but the nurse should supervise skin care since assessment and analysis are needed. 12. A client continuously calls out to the nursing staff when anyone passes the client’s door and asks them to do something in the room. The best response by the charge nurse would be to A) keep the client’s room door cracked to minimize the distractions B) assign 1 of the nursing staff to visit the client regularly C) reassure the client that 1 staff person will check frequently if the client needs anything D) arrange for each staff member to go into the client’s room to check on needs every hour on the hour B: Assign 1 of the nursing staff to visit the client regularly. Regular, frequent, planned contact by 1 staff member provides continuity of care and communicates to the client that care will be available when needed. 2413. A client is admitted with a diagnosis of schizophrenia. The client refuses to take medication and states “I don’t think I need those medications. They make me too sleepy and drowsy. I insist that you explain their use and side effects.” The nurse should understand that A) a referral is needed to the psychiatrist who is to provide the client with answers B) the client has a right to know about the prescribed medications C) such education is an independent decision of the individual nurse whether or not to teach clients about their medications D) clients with schizophrenia are at a higher risk of psychosocial complications when they know about their medication side effects B: The client has a right to know about the prescribed medications. Clients have a right to informed consent which includes information about medications, treatments, and diagnostic studies. 14. The charge nurse is planning assignments on a medical unit. Which client should be assigned to the practical nurse (PN)? A) Test a stool specimen for occult blood B) Assist with the ambulation of a client with a chest tube system C) Irrigate and redress a leg wound D) Admit a client from the emergency room C: Irrigate and redress a leg wound. The PN is a licensed provider and can perform this complex task. Options A and B could be delegated to an unlicensed assistive personnel (UAP), and option D requires an RN. 15. An unlicensed assistive personnel (UAP), who usually works on a surgical unit is assigned to float to a pediatric unit. Which question by the charge nurse would be most appropriate when making delegation decisions? A) "How long have you been a UAP and what units you have worked on?" B) "What type of care do you give on the surgical unit and what ages of clients?" C) "What is your comfort level in caring for children and at what ages?" D) "Have you reviewed the list of expected skills you might need on this unit?" D: "Have you reviewed the list of expected skills you might need on this unit?". The UAP must be competent to accept the delegated task. Review of skills needed versus level of performance is the most efficient and effective way to determine this. 16. A client with a diagnosis of bipolar disorder has been referred to a local boarding home for consideration for placement. The social worker telephoned the hospital unit for information about the client’s mental status and adjustment. The appropriate response of the nurse should be which of these statements? A) "I am sorry. Referral information can only be provided by the client’s providers" B) "I can never give any information out by telephone. How do I know who you are?" C) "Since this is a referral, I can give you this information" D) "I need to get the client’s written consent before I release any information to you" D: In order to release information about a client there must be a signed consent form with designation of to whom information can be given, and what information can be shared. 17. A client frequently admitted to the locked psychiatric unit repeatedly compliments and invites one of the nurses to go out on a date. The nurse’s response should be to A) ask to not be assigned to this client or to work on another unit B) tell the client that such behavior is inappropriate C) inform the client that hospital policy prohibits staff to date clients D) discuss the boundaries of the therapeutic relationship with the client D: Discuss the boundaries of the therapeutic relationship with the client. The nurse-client relationship is one with professional not social boundaries. Consistent adherence to the limits of the professional relationship builds trust. 18. Which statement by the nurse is appropriate when directing an unlicensed assistive personnel (UAP) to assist a 69 year-old surgical client to ambulate for the first time? A) "Have the client sit on the side of the bed for at least 2 minutes before helping him stand." B) "If the client is dizzy on standing, ask him to take some deep breaths." C) "Assist the client to the bathroom at least twice on this shift." D) "After you assist him to the chair, let me know how he feels." A: Give clear information to the UAP about what is expected for client safety. 19. After working with a client, an unlicensed assistive personnel (UAP) tells the nurse, "I have had it with that demanding client. I just can’t do anything that pleases him. I’m not going in there again." The nurse should respond by saying A) "He has a lot of problems. You need to have patience with him." B) "I will talk with him and try to figure out what to do." C) "He may be scared and taking it out on you. Let's talk to figure out what to do." D) "Ignore him and get the rest of your work done. Someone else can take care of him for the rest of the day." C: "He may be scared and taking it out on you. Let''s talk to figure out what to do." This response explains the client''s behavior without belittling the UAP’s feelings. The UAP is encouraged to contribute to the plan of care to help solve the problem. 20. A nurse is working with one licensed practical nurse (PN), a student nurse and an unlicensed assistive personnel (UAP). Which newly admitted clients would be most appropriate to assign to the UAP? 25A) A 76-year-old client with severe depression B) A middle-aged client with an obsessive compulsive disorder C) An adolescent with dehydration and anorexia D) A young adult who is a heroin addict in withdrawal with hallucinations B: A middle-aged client with an obsessive compulsive disorder. The UAP can be assigned to care for a client with a chronic condition after an initial assessment by the nurse. This client has minimal risk of instability of condition. Delegation 1. Which statement by the nurse is appropriate when giving an assignment to an unlicensed assistive personnel (UAP) to help a client ambulate for the first time after a colon resection? A) "Have the client sit on the side of the bed before helping the client to walk." B) "If the client is dizzy ask the client to take some slow, deep breaths." C) "Help the client to walk in the room as often as the client wishes." D) "When you help the client to walk, ask if any pain occurs." A: This statement gives clear directions to the UAP about the task and is most closely associated with the information provided in the stem that this is the client''s first time out of bed after surgery. 2. The home care nurse has been managing a client for 6 weeks. What is the best method to determine the quality of care provided by a home health care aide assigned to assist with the care of this client? A) Ask the client and family if they are satisfied with the care given B) Determine if the home health aide's care is consistent with the plan of care C) Investigate if the home health aide is prompt and stays an appropriate length of time for care D) Check the documentation of the aide for appropriateness and comprehensiveness B: Although the nurse must complete all of the above responsibilities, evaluation of an adherence to the plan of care is the first priority. The plan of care is based on the reason for referral, provider''s orders, the initial nursing assessment, the client’s responses to the planned interventions, and the client''s and family''s feedback or inquires. The other possible answers represent aspects of accomplishing “B”. 3. Which task for a client with anemia and confusion could the nurse delegate to the unlicensed assistive personnel (UAP)? A) Assess and document skin turgor and color changes B) Test stool for occult blood and urine for glucose and report results C) Suggest foods high in iron and those easily consumed D) Report mental status changes and the degree of mental clarity B: Test stool for occult blood and urine for glucose and report results. The UAP can do standard, unchanging procedures that require no decision making. 4. The care of which of the following clients can the nurse safely delegate to an unlicensed assistive personnel (UAP)? A) A client with peripheral vascular disease and an ulceration of the lower leg. B) A pre-operative client awaiting adrenalectomy with a history of asthma C) An elderly client with hypertension and self-reported non-compliance D) A new admission with a history of transient ischemic attacks and dizziness A: A client with peripheral vascular disease and an ulceration of the lower leg. This client is stable with no risk of instability as compared to the other clients. And this client has a chronic condition, needs supportive care. 5. A practical nurse (PN) from the pediatric unit is assigned to work in a critical care unit. Which client assignment would be appropriate? A) A client admitted with multiple trauma with a history of a newly implanted pacemaker B) A new admission with left-sided weakness from a stroke and mild confusion C) A 53 year-old client diagnosed with cardiac arrest from a suspected myocardial infarction D) A 35 year-old client in balanced traction admitted 6 days ago after a motor vehicle accident 26D: A 35 year-old client in balanced traction admitted 6 days ago after a motor vehicle accident. This client is the most stable with a predictable outcome. 6. The RN delegates the task of taking vital signs of all the clients on the medical-surgical unit to an unlicensed assistive personnel (UAP). Specific written and verbal instructions are given to not take a post-mastectomy client’s blood pressure on the left arm. Later as the RN is making rounds, the nurse finds the blood pressure cuff on that client’s left arm. Which of these statements is most immediately accurate? A) The RN has no accountability for this situation B) The RN did not delegate appropriately C) The UAP is covered by the RN’s license D) The UAP is responsible for following instructions D: The UAP is responsible for carrying out the activity correctly once directions have been clearly communicated especially if given verbally and in writing. 7. As the RN responsible for a client in isolation, which can be delegated to the practical nurse (PN)? A) Reinforcement of isolation precautions B) Assessment of the client's attitude about infection control C) Evaluation of staffs' compliance with control measures D) Observation of the client's total environment for risks A: PNs and UAPs can reinforce information that was originally given by the RN. 8. A 25 year-old client, unresponsive after a motor vehicle accident, is being transferred from the hospital to a long term care facility. To which staff member should the charge nurse assign the client? A) Unlicensed assistive personnel (UAP) B) Senior nursing student C) PN D) RN D: RN. The RN is responsible for teaching and assessment associated with discharge and these activities cannot be delegated to the others listed. 9. The charge nurse on a cardiac step-down unit makes assignments for the team consisting of a registered nurse (RN), a practical nurse (PN), and an unlicensed assistive personnel (UAP). Which client should be assigned to the PN? A) A 49 year-old with new onset atrial fibrillation with a rapid ventricular response B) A 58 year-old hypertensive with possible angina C) A 35 year-old scheduled for cardiac catheterization D) A 65 year-old for discharge after angioplasty and stent placement B: A 58 year-old hypertensive with possible angina. This is the most stable client. The clients in options C and D require initial teaching. The client in option A is considered unstable since the dysrhythmia is a new onset. 10. The measurement and documentation of vital signs is expected for clients in a long term facility. Which staff type would it be a priority to delegate these tasks to? A) Practical nurse (PN) B) Registered Nurse (RN) C) Unlicensed assistive personnel (UAP) D) Volunteer C: Unlicensed assistive personnel (UAP). The measurement and recording of vital signs may be delegated to UAP. This falls under the umbrella of routine task with stable clients. Other considerations for delegation of care to UAP would be: Who is capable and is the least expensive worker to do each task? 11. Which of these clients would be appropriate to assign to a practical nurse (PN)? A) A trauma victim with multiple lacerations and requires complex dressings B) An elderly client with cystitis and an indwelling urethral catheter C) A confused client whose family complains about the nursing care 2 days after surgery D) A client admitted for possible transient ischemic attack with unstable neurological signs B: This is a stable client, with predictable outcome and care and minimal risk for complications. 12. Two people call in sick on the medical-surgical unit and no additional help is available. The team consists of an RN, an LPN and an unlicensed assistive personnel (UAP). Which of these activities should the nurse assign to the UAP? A) Assist with plans for any clients discharged B) Provide basic hygiene care to all clients on the unit C) Assess a client after an acute myocardial infarction D) Gather the vital signs of all clients on the unit B: Basic client care, which is routine, should be delegated to a UAP since the unit is short on help. The vital signs can be done by the RN and PN as they make rounds since this data is more critical to making decisions about the care of the clients. 13. A staff nurse complains to the nurse manager that an unlicensed assistive personnel (UAP) consistently leaves the work area untidy and does not restock supplies. The best initial response by the nurse manager is which of these statements? 27A) "I will arrange for a conference with you and the UAP within the next week" B) "I can assure you that I will look into the matter" C) "I would like for you to approach the UAP about the problem the next time it occurs" D) I will add this concern to the agenda for the next unit meeting C: Helping staff manage conflict is part of the manager''s role. It is appropriate to urge the nurse to confront the other staff member to work out problems without a manager''s intervention when possible. 14. A client has had a tracheostomy for 2 weeks after a motor vehicle accident. Which task could the RN safely delegate to unlicensed assistive personnel (UAP)? A) Teach the client how to cough up secretions B) Changes the tracheostomy trach ties C) Monitor if client has shortness of breath D) Perform routine tracheostomy dressing care D: Unlicensed assistive personnel should be able to perform routine tracheostomy care. 15. An RN from the women’s health clinic is temporarily reassigned to a medical-surgical unit. Which of these client assignments would be most appropriate for this nurse? A) A newly diagnosed client with type 2 diabetes mellitus who is learning foot care B) A client from a motor vehicle accident with an external fixation device on the leg C) A client admitted for a barium swallow after a transient ischemic attack D) A newly admitted client with a diagnosis of pancreatic cancer B: This client is the most stable, requires basic safety measures and has a predictable outcome. 16. The nurse in a same-day surgery unit assigns the unlicensed assistive personnel (UAP) to provide a hernia patient with a lunch tray. Which statement by the nurse is most appropriate? A) "Tell the family they can bring in a pizza if the patient would prefer that." B) "Make sure the patient gets at least 2 cartons of milk." C) "Stop the IV if the patient is able to eat solid food." D) "Encourage the patient to eat slowly to prevent gas." D: The professional nurse can delegate tasks with an expected outcome. The UAP is given adequate information about the task and how to promote the best outcome. 17. Which one of these tasks can be safely delegated to a practical nurse (PN)? A) Assess the function of a newly created ileostomy B) Care for a client with a recent complicated double barrel colostomy C) Provide stoma care for a client with a well functioning ostomy D) Teach ostomy care to a client and their family members C: Provide stoma care for a client with a well functioning ostomy. The care of a mature stoma and the application of an ostomy appliance may be delegated to a PN. This client has minimal risk of instability of the situation. 18. An unlicensed assistive personnel (UAP), who usually works in pediatrics is assigned to work on a medical-surgical unit. Which one of the questions by the charge nurse would be most appropriate prior to making delegation decisions? A) "How long have you been a UAP?” B) "What type of care did you give in pediatrics?” C) "Do you have your competency checklist that we can review?” D) "How comfortable are you to care for adult clients?” C: "Do you have your competency checklist that we can review?”. The UAP must be competent to accept the delegated task. Further assessment of the qualifications of the UAP is important in order to assign the right task. 19. During the interview of a prospective employee who just completed the agency orientation, which approach would be the best for the nurse manager to use to assess competence? A) "What degree of supervision for basic care do you think you need?" B) "Let’s review your skills check-list for type and level of skill" C) "Are you comfortable working independently?" D) "What client care tasks or assignments do you prefer?" B: The nurse needs to know that the employee has competence in certain tasks. One way to do this is to do mutual review of documented skills. 20. A charge nurse working in a long term care facility is making out assignments. Which assignment made by a registered nurse to an unlicensed assistive personnel (UAP) requires intervention by the supervisor? A) Provide decubitus ulcer care and apply a dry dressing B) Bathe and feed a client on bed rest C) Oral suctioning of an unresponsive elderly client D) Teaching a family intermittent (bolus) feedings via G-tube before discharge 28D: Teaching a family intermittent (bolus) feedings via G-tube before discharge. Initial teaching can not be delegated to a UAP or a PN and must be done by RNs. 21. Which of these clients would be most appropriate to assign to a practical nurse (PN)? A) A trauma victim with quadriplegia and a client 1 day post-op radical neck dissection B) A client with newly diagnosed type 2 diabetes mellitus and a client with a history of AIDS admitted for pneumonia C) A client with hemiplegia is fed by a nasogastric tube and client with a left leg amputation in rehabilitation D) A client with a history of schizophrenia in alcohol withdrawal and a client with chronic renal failure C: A client with hemiplegia is fed by a nasogastric tube and client with a left leg amputation in rehabilitation This client requires supportive care and interventions within the scope of practice of a PN. This client is stable with little risk of complications or instability. 22. The nurse assigns an unlicensed assistive personnel (UAP) to care for a client with a musculoskeletal disorder. The client ambulates with a leg splint. Which task requires supervision of the UAP? A) Report signs of redness overlying a joint B) Monitor the client's response to ambulatory activity C) Encouragement for the independence in self-care D) Assist the client to transfer from a bed to a chair B: Monitor the client''s response to ambulatory activity. Monitoring the client’s response to interventions requires assessment, a task to be performed by an RN. 23. When walking past a client’s room, the nurse hears 1 unlicensed assistive personnel (UAP) talking to another UAP. Which statement requires follow-up intervention? A) "If we work together we can get all of the client care completed." B) "Since I am late for lunch, would you do this one client's glucose test?" C) "This client seems confused, we need to watch monitor closely." D) "I’ll come back and make the bed after I go to the lab." B: Only the RN and PN can delegate to UAPs. One UAP can not delegate a task to another UAP. The RN or PN is legally accountable for the nursing care. 24. A client is receiving an intravenous (IV) infusion for pain control. When caring for this client, which one of these actions can the RN safely assign to an unlicensed assistive personnel (UAP)? A) Ask the client the degree of relief and document the client’s response B) Decrease the set rate on the pump by 2 ml/minute C) Check the IV site for drainage and loose tape D) Assist the client with ambulation and a gown change with supervision D: When directing the UAP, communicate clearly and specifically what the task is and what should be reported to the nurse. Implementation of routine tasks should be delegated since they do not require independent judgment. 25. Which client data should the nurse act upon when a home health aide calls the nurse from the client's home to report these items? A) "The client has complaints of not sleeping well for the past week" B) "The family wants to discontinue the home meal service, meals on wheels" C) "The urine in the urinary catheter bag is of a deeper amber, almost brown color" D) "The partner says the client has slower days every other day" C: Home health aides need to report diverse information to nurses through phone calls and documentation. The nurse who develops the plan of care for a specific client, and supervises the aide, must identify potential danger signs which require immediate action and follow-up. The color of the urine requires follow-up evaluation. 29Priority 1. The nurse must know that the most accurate oxygen delivery system available is A) the Venturi mask B) nasal cannula C) partial non-rebreather mask D) simple face mask A: the Venturi mask. The most accurate way to deliver oxygen to the client is through a Venturi system such as the Venti Mask. The Venti Mask is a high flow device that entrains room air into a reservoir device on the mask and mixes the room air with 100% oxygen. The size of the opening to the reservoir determines the concentration of oxygen. The client’s respiratory rate and respiratory pattern do not affect the concentration of oxygen delivered. The maximum amount of oxygen that can be delivered by this system is 55%. 2. A client arrives in the emergency department after a radiologic accident at a local factory. The first action of the nurse would be to A) begin decontamination procedures for the client B) ensure physiologic stability of the client C) wrap the client in blankets to minimize staff contamination D) double bag the client’s contaminated clothing B: ensure physiologic stability of the client. The nurse must initially assist in stabilizing the patient prior to performing the other tasks related to radiologic contamination. 3. The nurse is caring for a client on complete bed rest. Which action by the nurse is most important in preventing the formation of deep vein thrombosis? A) Elevate the foot of the bed B) Apply knee high support stockings C) Encourage passive exercises D) Prevent pressure at back of knees D: Prevent pressure at back of knees. Preventing popliteal pressure will prevent venous stasis and possibly deep vein thrombosis. 4. If a very active two year-old client pulls his tunneled central venous catheter out, what initial nursing action is appropriate? A) Obtain emergency equipment B) Assess heart rate, rhythm and all pulses C) Apply pressure to the vessel insertion site D) Use cold packs at the exit incision site C: If a central venous catheter is accidentally removed, pressure should be applied to the vein entry site. 5. The nurse assesses several post partum women in the clinic. Which of the following women is at highest risk for puerperal infection? A) 12 hours post partum, temperature of 100.4 degrees Fahrenheit since delivery B) 2 days post partum, temperature of 101.2 degrees Fahrenheit this morning C) 3 days post partum, temperature of 100.8 degrees Fahrenheit the past 2 days D) 4 days post partum, temperature of 100 degrees Fahrenheit since delivery 30C: A temperature of 100.4 degrees Fahrenheit or higher on 2 successive days, not counting the first 24 hours after birth, indicates a post partum infection. 6. The nurse is caring for a client with a chest tube. On the second postoperative day, the chest tube accidentally disconnects from the drainage tube. The first action the nurse should take is A) reconnect the tube B) raise the collection chamber above the client's chest C) call the health care provider D) clamp the chest tube D: clamp the chest tube. Immediate steps should be taken to prevent air from entering the chest cavity. Lung collapse may occur if air enters the chest cavity. Clamping the tube close to the client’s chest is the first action to take, followed by health care provider notification. 7. A client is placed on sulfamethoxazole-trimethoprim (Bactrim) for a recurrent urinary tract infection. Which of the following is appropriate reinforcement of information by the nurse? A) "Drink at least 8 glasses of water a day." B) "Be sure to take the medication with food." C) "It is safe to take with oral contraceptives." D) "Stop the medication after 5 days." A: "Drink at least 8 glasses of water a day." Bactrim is a highly insoluble drug and requires a large volume of fluid intake. It is not necessary to take it with food. Options C and D are incorrect instructions for those taking Bactrim. 8. A client calls the evening health clinic to state “I know I have a severely low sugar since the Lantus insulin was given 3 hours ago and it peaks in 2 hours.” What should be the nurse’s initial response to the client? A) What else do you know about this type of insulin? B) What are you feeling at this moment? C) Have you eaten anything today? D) Are you taking any other insulin or medication? B: What are you feeling at this moment? When a client has changed from stable to unstable, the nurse’s initial response should be to do further assessment of the client. 9. The nurse is caring for a client who is receiving total parenteral nutrition (TPN) (hyperalimentation and lipids). What is the priority nursing action on every 8 hour shift? A) Monitor blood pressure, temperature and weight B) Change the tubing under sterile conditions C) Check urine glucose, acetone and specific gravity D) Adjust the infusion rate to provide for total volume C: Check urine glucose, acetone and specific gravity. Because of the high dextrose and protein content in parenteral nutrition, the nurse should assess the urine at least every 8 hours. 10. The nurse reviews an order to administer Rh (D) immune globulin to an Rh negative woman following the birth of an Rh positive baby. Which assessment is a priority before the nurse gives the injection? A) Newborn's blood type B) Coombs' test results C) Previous RhoGAM history D) Gravida and parity B: Coombs'' test results. Rh (D) immune globulin (RhoGAM) is given only if antibody formation has not occurred. A negative Coombs'' test confirms this. 11. A client has been on antibiotics for 72 hours for cystitis. Which report from the client requires priority attention by the nurse? A) foul smelling urine B) burning on urination C) elevated temperature D) nausea and anorexia C: elevated temperature. Elevated temperature after 72 hours on an antibiotic indicates the antibiotic has not been effective in eradicating the offending organism. The provider should be informed immediately so that an appropriate medication can be prescribed, and complications such as pyelonephritis are prevented. Options A and B are expected with cystitis. Option D may be related to the antibiotics as a side effect and should also be reported to the provider. 12. The nurse is caring for a school-aged child with a diagnosis of secondary hyperparathyroidism following treatment for chronic renal disease. Which of the following lab data should receive priority attention? A) Calcium and phosphorus levels B) Blood sugar C) Urine specific gravity 31D) Blood urea nitrogen A: Calcium and phosphorus levels. Calcium and phosphorous levels will be elevated until the client is stabilized. 13. When caring for a client with urinary incontinence, which content should be reinforced by the nurse? A) hold the urine to increase bladder capacity B) avoid eating foods high in sodium C) restrict fluid to prevent elimination accidents D) avoid taking antihistamines D: avoid taking antihistamines. Antihistamines can aggravate urinary incontinence and should be avoided by these clients. Holding the urine, avoiding sodium, and restricting fluids have not been shown to reduce urinary incontinence. 14. A client returns from the operating room after a right orchiectomy. For the immediate post-operative period the nursing priority would be to A) maintain fluid and electrolyte balance B) manage post-operative pain C) ambulate the client within 1 hour of surgery D) control bladder spasms B: manage post-operative pain. Due to the location of the incision, pain management is the priority. Bladder spasms are more related to prostate surgery. 15. A client with a fracture of the radius had a plaster cast applied 2 days ago. The client complains of constant pain and swelling of the fingers. The first action of the nurse should be A) elevate the arm no higher than heart level B) remove the cast C) assess capillary refill of the exposed hand and fingers D) apply a warm soak to the hand C: assess capillary refill of the exposed hand and fingers. A deterioration in neurovascular status indicates the development of compartment syndrome (elevated tissue pressure within a confined area) which requires immediate pressure-reducing interventions. 16. A client is 2 days post operative. The vital signs are: BP - 120/70, HR -- 110 BPM, RR - 26, and Temperature - 100.4 degrees Fahrenheit (38 degrees Celsius). The client suddenly becomes profoundly short of breath, skin color is gray. Which assessment would have alerted the nurse first to the client's change in condition? A) Heart rate B) Respiratory rate C) Blood pressure D) Temperature B: Respiratory rate. Tachypnea is one of the first clues that the client is not oxygenating appropriately. The compensatory mechanism for decreased oxygenation is increased respiratory rate. 17. A client is waiting to have an intravenous pyelogram (IVP). The most important information to be obtained by the nurse prior to the procedure is A) time of the client's last meal B) client's allergy history C) assessment of the peripheral pulses D) results of the blood coagulation studies B: client''s allergy history. Intravenous Pyelogram is a dye study that uses an iodine-based contract. Therefore, the study is contraindicated in clients with allergy to iodine. 18. What must the nurse emphasize when teaching a client with depression about a new prescription for nortriptyline (Pamelor)? A) Symptom relief occurs in a few days B) Alcohol use is to be avoided C) Medication must be stored in the refrigerator D) Episodes of diarrhea can be expected B: Alcohol use is to be avoided. Alcohol potentiates the action of tricyclic antidepressants. 19. Before administering a feeding through a gastrostomy tube, what is the priority nursing assessment? A) Measure the vital signs B) Palpate the abdomen C) Assess for breath sounds D) Verify tube patency 32D: Verify tube patency. Tube patency should be checked prior to all feedings. The feeding should not be attempted if the tube is not patent. 20. The nurse is caring for a client with a vascular access for hemodialysis. Which of these findings necessitates immediate action by the nurse? A) pruritic rash B) dry, hacking cough C) chronic fatigue D) elevated temperature D: elevated temperature. It is a priority to report this finding since clients on hemodialysis are prone to infection, and the first sign is an elevated temperature. The other findings should be reported to the provider as well. 21. The nurse is caring for a client several days following a cerebral vascular accident. Coumadin (warfarin) has been prescribed. Today's prothrombin level is 40 seconds (normal range 10-14 seconds). Which of the following findings requires priority follow-up? A) Gum bleeding B) Lung sounds C) Homan's sign D) Generalized weakness A: Gum bleeding. The prothrombin time is elevated, indicating a high risk for bleeding. Neurological assessments remain important for post-CVA clients. 22. The registered nurse (RN) is making decisions regarding client room assignments on a pediatric unit. Which possible roommate would be most appropriate for a 3 year-old child with minimal change nephrotic syndrome? A) 2 year-old with respiratory infection B) 3 year-old fracture whose sibling has chickenpox C) 4 year-old with bilateral inguinal hernia repair D) 6 year-old with a sickle cell anemia crisis C: 4 year-old with bilateral inguinal hernia repair. The nurse must know that children with nephrotic syndrome are at high risk for development of infections as a result of the standard use of immunosuppressant therapy, as well as from the accumulation of fluid (edema). Therefore, these children must be protected from sources of possible infection. D is incorrect because the sickle cell crisis is potentially due to an infectious process. 23. The nurse is caring for a pregnant woman with pregnancy induced hypertension (PIH) receiving magnesium sulfate intravenously. In assessing the client, it is noted that respirations are 12, pulse and blood pressure have dropped significantly, and 8 hour output is 200 ml. What should the nurse do first? A) Administer calcium gluconate B) Call the provider immediately C) Discontinue the magnesium sulfate D) Perform additional assessments C: Discontinue the magnesium sulfate. The assessments strongly suggest magnesium sulfate toxicity. The nurse must discontinue the IV immediately and take measures to ensure the safety of the client. 24. A client has a serum glucose of 385 mg/dl. Which of these orders would the nurse question first? A) Repeat glycohemoglobin in 24 hours B) Document Accu-checks, intake and output every 4 hours C) Humulin N 20 units IV push D) IV fluids of 0.9% normal saline at 125 ml per hour C: Humulin N 20 units IV push. Regular insulin is the only insulin that can be given by the intravenous route. This is the initial order to question. Option A should also be questioned, although it is not a priority since the client would not be harmed by this action. This lab test gives the average glucose on the hemoglobin molecule for the past 2 to 3 months. There would be no need to repeat it at this time. A fasting glucose in the morning would be a more appropriate assessment. The other orders are within expected actions in this situation. 25. The nurse performs an assessment during a fluid exchange for the client who is 48 hours post-insertion of an abdominal Tenckhoff catheter for peritoneal dialysis. The nurse knows that the appearance of which of the following needs to be reported to the provider immediately? A) slight pink-tinged drainage B) abdominal discomfort C) muscle weakness D) cloudy drainage D: cloudy drainage. Cloudy drainage is a sign of infection that can lead to peritonitis (inflammation of the peritoneum). The other options are expected side effects of peritoneal dialysis. 33Safety and Infection Control 1. After an explosion at a factory one of the employees approaches the nurse and says “I am an unlicensed assistive personnel (UAP) at the local hospital.” Which of these tasks should the nurse assign first to this worker who wants to help care for the wounded workers? A) Get temperatures B) Take blood pressure C) Palpate pulses D) Check alertness C: Palpate pulses. The heart rates would indicate if the client is in shock or has potential for shock. If the pulses could not be palpated, those clients would need to be seen first. 2. A client is diagnosed with methicillin resistant staphylococcus aureus pneumonia (MRSA). What type of isolation is most appropriate for this client? A) Reverse B) Airborne C) Standard precautions D) Contact D: Contact. Contact precautions or Body Substance Isolation (BSI) involves the use of barrier protection (e.g. gloves, mask, gown, or protective eyewear as appropriate) whenever direct contact with any body fluid is expected. When determining the type of isolation to use, one must consider the mode of transmission. The hands of personnel continue to be the principal mode of transmission for methicillin resistant staphylococcus aureus (MRSA). Because the organism is limited to the sputum in this example, precautions are taken if contact with the patient''s sputum is expected. A private room and contact precautions , along with good hand washing techniques, are the best defenses against the spread of MRSA pneumonia. 3. A newly admitted adult client has a diagnosis of hepatitis A. The charge nurse should reinforce to the staff members that the most significant routine infection control strategy, in addition to handwashing, is which of these? A) Place appropriate signs outside and inside the room B) Use a mask with a shield if there is a risk of fluid splash C) Wear a gown to change soiled linens from incontinence D) Have gloves on while handling bedpans with feces D: Have gloves on while handling bedpans with feces. The specific measure to prevent the spread of hepatitis A is careful handling and protection while working with fecal material. All of the other actions are correct but not the most significant specific approach used with hepatitis A. 4. The nurse is assigned to a client newly diagnosed with active tuberculosis. Which of these interventions would be a priority for the nurse to implement? A) Have the client cough into a tissue and dispose in a separate bag B) Instruct the client to cover the mouth with a tissue when coughing C) Reinforce that everyone should wash their hands before and after entering the room D) Place client in a negative pressure private room and have all who enter the room use masks with shields 34D: Place client in a negative pressure private room and have all who enter the room use masks with shields. A client with active tuberculosis should be hospitalized in a negative pressure room to prevent respiratory droplets from leaving the room when the door is opened. Tuberculosis (TB) is caused by spore-forming mycobacteria, more often Mycobacterium tuberculosis. In developed countries the infection is airborne and is spread by inhalation of infected droplets. In underdeveloped countries, transmission also occurs by ingestion or by skin invasion, particularly when bovine TB is poorly controlled. 5. A nurse who is assigned to the emergency department needs to understand that gastric lavage is a priority in which situation? A) An infant who has been identified as suffering from botulism B) A toddler who has eaten a number of ibuprofen tablets C) A preschooler who has swallowed powdered plant food D) A school aged child who has taken a handful of vitamins A: An infant who has been identified as suffering from botulism C. botulinum forms a toxin in improperly processed foods in anaerobic conditions. It is a neurotoxin that impairs autonomic and voluntary neurotransmission and causes muscular paralysis. Findings appear within 36 hours of ingestion. The nurse should be aware that all of these clients may be candidates for gastric lavage or for activated charcoal administration. 6. The parents of a toddler who is being treated for pesticide poisoning ask: “Why is activated charcoal used? What does it do?” What is the nurse's best response? A) "Activated charcoal decreases the body’s absorption of the poison from the stomach." B) "The charcoal absorbs the poison and forms a compound that doesn't hurt your child." C) "This substance helps to get the poison out of the body through the gastrointestinal system." D) "The action may bind or inactivate the toxins or irritants that are ingested by children and adults." B: "The charcoal absorbs the poison and forms a compound that doesn''t hurt your child." All of the options are correct responses. However, option B is most accurate information to answer the parents’ questions about the use and action of activated charcoal. The language is appropriate for a parent''s understanding. 7. Which of these nursing diagnoses, appropriate for elderly clients, would indicate the client is at greatest risk for falls? A) Sensory perceptual alterations related to decreased vision B) Alteration in mobility related to fatigue C) Impaired gas exchange related to retained secretions D) Altered patterns of urinary elimination related to nocturia D: Altered patterns of urinary elimination related to nocturia. Nocturia is especially problematic because many elders fall when they rush to reach the bathroom at night. They may be confused or not fully alert. Inadequate lighting can increase their chances of stumbling, and then they may fall over furniture or carpets. 8. A child is admitted to the pediatric unit with a diagnosis of suspected meningococcal meningitis. Which admission orders should the nurse implement first? A) Institute seizure precautions B) Monitor neurologic status every hour C) Place in respiratory/secretion precautions D) Cefotaxime IV 50 mg/kg/day divided q6h C: Place in respiratory/secretion precautions Meningococcal meningitis is a bacterial infection that can be communicated to others. The initial therapeutic management of acute bacterial meningitis includes respiratory/secretions precautions, initiation of antimicrobial therapy, monitoring neurological status along with vital signs, instituting seizure precautions and lastly maintaining optimum hydration. The first action for nurses to take is initiate any necessary precautions to protect themselves and others from possible infection. Viral meningitis usually does not require protective measures of isolation. 9. Several clients are admitted to an adult medical unit. For which client condition(s) would the nurse institute airborne precautions? A) Autoimmune deficiency syndrome (AIDS) with cytomegalovirus (CMV) B) A positive purified protein derivative (PPD) test with an abnormal chest x-ray C) A tentative diagnosis of viral pneumonia with productive brown sputum D) Advanced carcinoma of the lung with hemoptysis B: A positive purified protein derivative (PPD) test with an abnormal chest x-ray. The client who must be placed in airborne precautions is the client with these findings that suggest a suspicious tuberculin lesion. A sputum smear for acid fast bacillus would be done next. CMV usually causes no signs or symptoms in children and adults with healthy immune systems. Good handwashing is recommended for CMV. When signs and symptoms do occur, they are often similar to those of mononucleosis, including sore throat, fever, muscle aches and fatigue. 10. A client is scheduled to receive an oral solution of radioactive iodine (131I). In order to reduce hazards, the priority information for the nurse to include in client teaching is which of these statements? A) "In the initial 48 hours, avoid contact with children and pregnant women, and flush the commode twice after urination or defecation." B) "Use disposable utensils for 2 days and if vomiting occurs within 10 hours of the dose, do so in the toilet and flush it twice." C) "Your family can use the same bathroom that you use without any special precautions." 35D) "Drink plenty of water and empty your bladder often during the initial 3 days of therapy." A: "In the initial 48 hours, avoid contact with children and pregnant women, and flush the commode twice after urination or defecation." The client's urine and saliva are radioactive for 24 hours after ingestion, and vomitus is radioactive for 6 to 8 hours. The client should drink 3 to 4 liters of fluid a day for the initial 48 hours to help remove the ( 131I) from the body. Staff should limit contact with hospitalized clients to 30 minutes per day per person. 11. The nurse is to administer a new medication to a client. Which of these actions best demonstrate awareness of safe, proficient nursing practice? A) Verify the order for the medication. Prior to giving the medication the nurse should say, "Please state your name." B) Upon entering the room the nurse should ask: "What is your name? What allergies do you have?" and then check the client's name band and allergy band. C) As the room is entered say "What is your name?" then check the client's name band. D) Verify the client's allergies on the admission sheet and order. Verify the client's name on the nameplate outside the room then as the nurse enters the room ask the client "What is your first, middle and last name?" B: Upon entering the room the nurse should ask: "What is your name? What allergies do you have?" and then check the client''s name band and allergy band. A dual check is always done for a client''s name. This would involve verbal and visual checks. Since this is a new medication an allergy check is appropriate. 12. The school nurse is teaching the faculty the most effective methods to prevent the spread of lice (Pediculus Humanus Capitis) in the school. The information that would be most important to include is reflected in which of these statements? A) "The treatment medication requires reapplication in 8 to 10 days." B) "Bedding and clothing can be boiled or steamed to kill lice." C) "Children should not share hats, scarves and combs." D) "Nit combs are necessary to comb lice eggs (nits) out of children's hair." C: "Children should not share hats, scarves and combs." Head lice live only on human beings and can be spread easily by sharing hats, combs, scarves, coats and other items of clothing that touch the hair. All of the options are correct statements, however they do not best answer the question of how to prevent the spread of lice in a school setting. 13. Which approach is the best way to prevent infections when providing care to clients in the home setting? A) Handwashing before and after examination of clients B) Wearing nonpowdered latex-free gloves to examine the client C) Using a barrier between the client's furniture and the nurse's bag D) Wearing a mask with a shield during any eye/mouth/nose examination A: Handwashing before and after examination of clients. Handwashing remains the most effective way to avoid spreading infection. However, too often nurses do not practice good handwashing techniques and do not teach families to do so. Nurses need to wash their hands before and after touching the client and before entering the nursing bag. All of the options are correct, and the sequence of priorities would be options A, C, B, and D. 14. A nurse is reinforcing teaching with a client about compromised host precautions. The client is receiving filgrastim (Neupogen) for neutropenia. Which lunch selection suggests the client has learned about necessary dietary changes? A) grilled chicken sandwich and skim milk B) roast beef, mashed potatoes, and green beans C) peanut butter sandwich, banana, and iced tea D) barbeque beef, baked beans, and cole slaw B: roast beef, mashed potatoes, and green beans. The client has correctly selected an appropriate lunch and appears to know the dietary restrictions. Low granulocyte counts and susceptibility to infection are expected. Compromised host precautions require that foods are either cooked or canned. Options A, C and D do not demonstrate learning, as raw fruits, vegetables, and milk are to be avoided. 15. A school nurse has a 10 year-old child with a history of epilepsy with tonic-clonic seizures attending classes regularly. The school nurse should inform the teacher that if the child experiences a seizure in the classroom, the most important action to take during the seizure would be to A) move any chairs or desks at least 3 feet away from the child B) note the sequence of movements with the time lapse of the event C) provide privacy as much as possible to minimize frightening the other children D) place the hands or a folded blanket under the head of the child D: place the hands or a folded blanket under the head of the child. The priority during seizure activity is to protect the person from physical injury. Place a pillow, folded blanket or your hands under the child''s head to prevent concussion or other head trauma. The other body parts are at less risk for injury, consequently the prioritized sequence of the actions above would be options D, A, B, and C. 16. A parent calls the hospital hot line and is connected to the triage nurse. The caller proclaims: “I found my child with odd stuff coming from the mouth and an unmarked bottle nearby.” Which of these comments would be the best tool for the nurse to determine if the child has swallowed a corrosive substance? A) "Ask the child if the mouth is burning or throat pain is present." B) "Take the child’s pulse at the wrist and see if the child is has trouble breathing lying flat." C) "What color is the child’s lips and nails and has the child voided today?" 36D) "Has the child had vomiting, diarrhea or stomach cramps?" A: "Ask the child if the mouth is burning or throat pain is present." Local irritation of tissues indicates a corrosive poisoning. The other comments may be helpful in determining the child’s overall condition, however the question concerns evaluation for ingesting a caustic substance. 17. Which of these clients would the nurse recommend keeping in the hospital during an internal disaster at that facility? A) An adolescent diagnosed with sepsis 7 days ago and whose vital signs are maintained within low normal limits. B) A middle-aged woman known to have had an uncomplicated myocardial infarction 4 days ago C) An elderly man admitted 2 days ago with an acute exacerbation of ulcerative colitis D) A young adult in the second day of treatment for an overdose of acetometaphen D: A young adult in the second day of treatment for an overdose of acetometaphen. An overdose of Tylenol requires close observation for 3 to 4 days as well as Mucomyst PO during that time . A strong risk of liver failure exists immediately following Tylenol overdose. 18. When an infant car seat is properly installed, the infant should face A) forward, so child may look out window B) backward, so child faces the seat C) the side window, to increase sensory stimulation D) upward, as child lies on back with seat installed sideways B: backward, so child faces the seat. Nurses are now responsible for promoting the continued safety of infants and children outside of the hospital. Emergency Department and Women’s Services staff are trained in child seat placement. Growth and development data indicate that infants still require support of the head. Therefore, they should be positioned reclining and facing the rear until their leg muscles are strong enough to kick away from the backseat (about 10-12 months-old) for the greatest protection. 19. Which of these clients is the priority for the nurse to report to the public health department within the next 24 hours? A) An infant with a positive culture of stool for Shigella B) An elderly factory worker with a lab report that is positive for acid-fast bacillus smear C) A young adult commercial pilot with a positive histopathological examination from an induced sputum for Pneumocystis carinii D) A middle-aged nurse with a history of varicella zoster virus and with crops of vesicles on an erythematous base that appear on the skin B: An elderly factory worker with a lab report that is positive for acid-fast bacillus smear. Tuberculosis is a reportable disease because persons who had contact with the client must be traced and often must be treated with chemoprophylaxis for a designated time. Options A and D may need contact isolation precautions. Option C -- findings may indicate the initial stage of autoimmune deficiency syndrome (AIDS). 20. Which of these actions is the primary nursing intervention designed to limit transmission of a client’s Salmonella infection? A) Wash hands thoroughly before and after client contact B) Wear gloves when in contact with body secretions C) Double glove when in contact with feces or vomitus D) Wear gloves when disposing of contaminated linens A: Wash hands thoroughly before and after client contact. Gram-negative bacilli cause Salmonella infection, and lack of sanitation is the primary means of contamination. Two million new cases appear each year. Thorough handwashing can prevent the spread of salmonella. Note that all of the options are appropriate activities, but handwashing is primary. 37Health Promotion and Maintenance 1. The nurse has been teaching adult clients about cardiac risks when they visit the hypertension clinic. Which evaluation data would best measure learning? A) Performance on written tests B) Responses to verbal questions C) Completion of a mailed survey D) Reported behavioral changes D: Reported behavioral changes. If the client alters behaviors such as smoking, drinking alcohol, and stress management, these suggest that learning has occurred. Additionally, physical assessments and lab data may confirm risk reduction. 2. The nurse is assessing a client who states her last menstrual period was March 16, and she has missed one period. She reports episodes of nausea and vomiting. Pregnancy is confirmed by a urine test. What will the nurse calculate as the estimated date of delivery (EDD)? A) April 8 B) January 15 C) February 11 D) December 23 D: December 23. Naegele''s rule states: Add 7 days and subtract 3 months from the first day of the last regular menstrual period to calculate the estimated date of delivery. 3. The parents of a child who has suddenly been hospitalized for an acute illness state that they should have taken the child to the pediatrician earlier. Which approach by the nurse is best when dealing with the parents' comments? A) Focus on the child's needs and recovery B) Explain the cause of the child's illness C) Acknowledge that early care would have been better D) Accept their feelings without judgment D: Accept their feelings without judgment. Parents often blame themselves for their child''s illness. Feeling helpless and angry is normal and these feelings must be accepted. 4. When observing 4 year-old children playing in the hospital playroom, what activity would the nurse expect to see the children participating in? A) Competitive board games with older children B) Playing with their own toys along side with other children C) Playing alone with hand held computer games D) Playing cooperatively with other preschoolers D: Playing cooperatively with other preschoolers. Cooperative play is typical of the late preschool period. 385. A 64 year-old client scheduled for surgery with a general anesthetic refuses to remove a set of dentures prior to leaving the unit for the operating room. What would be the most appropriate intervention by the nurse? A) Explain to the client that the dentures must come out as they may get lost or broken in operating room B) Ask the client if there are second thoughts about having the procedure C) Notify the anesthesia department and the surgeon of the client's refusal D) Ask the client if the preference would be to remove the dentures in the operating room receiving area D: Ask the client if the preference would be to remove the dentures in the operating room receiving area Clients anticipating surgery may experience a variety of fears. This choice allows the client control over the situation and fosters the client''s sense of self-esteem and self-concept. 6. When teaching a 10 year-old child about their impending heart surgery, which form of explanation meets the developmental needs of this age child? A) Provide a verbal explanation just prior to the surgery B) Provide the child with a booklet to read about the surgery C) Introduce the child to another child who had heart surgery 3 days ago D) Explain the surgery using a model of the heart D: Explain the surgery using a model of the heart. According to Piaget, the school age child is in the concrete operations stage of cognitive development. Using something concrete, like a model will help the child understand the explanation of the heart surgery. 7. When screening children for scoliosis, at what time of development would the nurse expect early signs to appear? A) Prenatally on ultrasound B) In early infancy C) When the child begins to bear weight D) During the preadolescent growth spurt D: During the preadolescent growth spurt. Idiopathic scoliosis is seldom apparent before 10 years of age and is most noticeable at the beginning of the preadolescent growth spurt. It is more common in females than in males. 8. A client is admitted to the hospital with a history of confusion. The client has difficulty remembering recent events and becomes disoriented when away from home. Which statement would provide the best reality orientation for this client? A) "Good morning. Do you remember where you are?" B) "Hello. My name is Elaine Jones and I am your nurse for today." C) "How are you today? Remember, you're in the hospital." D) "Good morning. You’re in the hospital. I am your nurse Elaine Jones." D: "Good morning. You’re in the hospital. I am your nurse Elaine Jones." As cognitive ability declines, the nurse provides a calm, predictable environment for the client. This response establishes time, location and the caregiver’s name. 9. The nurse is assessing a 4 month-old infant. Which motor skill would the nurse anticipate finding? A) Hold a rattle B) Bang two blocks C) Drink from a cup D) Wave "bye-bye" A: Hold a rattle. The age at which a baby will develop the skill of grasping a toy with help is 4 to 6 months. 10. An appropriate treatment goal for a client with anxiety would be to A) ventilate anxious feelings to the nurse B) establish contact with reality C) learn self-help techniques D) become desensitized to past trauma C: learn self-help techniques. Exploring alternative coping mechanisms will decrease present anxiety to a manageable level. Assisting the client to learn self-help techniques will assist in learning to cope with anxiety. 11. The family of a 6 year-old with a fractured femur asks the nurse if the child's height will be affected by the injury. Which statement is true concerning long bone fractures in children? A) Growth problems will occur if the fracture involves the periosteum B) Epiphyseal fractures often interrupt a child's normal growth pattern C) Children usually heal very quickly, so growth problems are rare D) Adequate blood supply to the bone prevents growth delay after fractures B: Epiphyseal fractures often interrupt a child''s normal growth pattern. The epiphyseal plate in children is where active bone growth occurs. Damage to this area may cause growth arrest in either longitudinal growth of the limb or in progressive deformity if the plate is involved. An epiphyseal fracture is serious because it can interrupt and alter growth. 12. While caring for a client, the nurse notes a pulsating mass in the client's periumbilical area. Which of the following assessments is appropriate for the nurse to perform? A) Measure the length of the mass 39B) Auscultate the mass C) Percuss the mass D) Palpate the mass B: Auscultate the mass. Auscultation of the abdomen and finding a bruit will confirm the presence of an abdominal aneurysm and will form the basis of information given to the provider. The mass should not be palpated because of the risk of rupture. 13. While the nurse is administering medications to a client, the client states "I do not want to take that medicine today." Which of the following responses by the nurse would be best? A) "That's OK, its all right to skip your medication now and then." B) "I will have to call your doctor and report this." C) "Is there a reason why you don't want to take your medicine?" D) "Do you understand the consequences of refusing your prescribed treatment?" C: When a new problem is identified, it is important for the nurse to collect accurate assessment data. This is crucial to ensure that client needs are adequately identified in order to select the best nursing care approaches. The nurse should try to discover the reason for the refusal which may be that the client has developed untoward side effects. 14. The nurse is teaching the parents of a 3 month-old infant about nutrition. What is the main source of fluids for an infant until about 12 months of age? A) Formula or breast milk B) Dilute nonfat dry milk C) Warmed fruit juice D) Fluoridated tap water A: Formula or breast milk. Formula or breast milk are the perfect food and source of nutrients and liquids up to 1 year of age. 15. A client states, "People think I’m no good, you know what I mean?" Which of these responses would be most therapeutic? A) "Well people often take their own feelings of inadequacy out on others." B) "I think you’re good. So you see, there’s one person who likes you." C) "I’m not sure what you mean. Tell me a bit more about that." D) "Let's discuss this to see the reasons you create this impression on people." C: "I’m not sure what you mean. Tell me a bit more about that." This therapeutic communication technique elicits more information, especially when delivered in an open, non-judgmental fashion. 16. When teaching effective stress management techniques to a client 1 hour before surgery, which of the following should the nurse recommend? A) Biofeedback B) Deep breathing C) Distraction D) Imagery B: Deep breathing. Deep breathing is a reliable and valid method for reducing stress, and can be taught and reinforced in a short period pre-operatively. 17. The nurse is planning care for an 18 month-old child. Which action should be included in the child's care? A) Hold and cuddle the child frequently B) Encourage the child to feed himself finger food C) Allow the child to walk independently on the nursing unit D) Engage the child in games with other children B: Encourage the child to feed himself finger food. According to Erikson, the toddler is in the stage of autonomy versus shame and doubt. The nurse should encourage increasingly independent activities of daily living that allow the toddler to assert his budding sense of control. 18. A client being treated for hypertension returns to the community clinic for follow up. The client says, "I know these pills are important, but I just can't take these water pills anymore. I drive a truck for a living, and I can't be stopping every 20 minutes to go to the bathroom." Which of these is the best nursing diagnosis? A) Noncompliance related to medication side effects B) Knowledge deficit related to misunderstanding of disease state C) Defensive coping related to chronic illness D) Altered health maintenance related to occupation A: Noncompliance related to medication side effects. The client kept his appointment, and stated he knew the pills were important. He is unable to comply with the regimen due to side effects, not because of a lack of knowledge about the disease process. 19. A client with congestive heart failure is newly admitted to home health care. The nurse discovers that the client has not been following the prescribed diet. What would be the most appropriate nursing action? A) Discharge the client from home health care because of noncompliance B) Notify the provider of the client's failure to follow prescribed diet 40C) Discuss diet with the client to learn the reasons for not following the diet D) Make a referral to Meals-on-Wheels C: Discuss diet with the client to learn the reasons for not following the diet. When new problems are identified, it is important for the nurse to collect accurate assessment data. Before reporting findings to the provider, it is best to have a complete understanding of the client''s behavior and feelings as a basis for future teaching and intervention. 20. A partner is concerned because the client frequently daydreams about moving to Arizona to get away from the pollution and crowding in southern California. The nurse explains that A) such fantasies can gratify unconscious wishes or prepare for anticipated future events B) detaching or dissociating in this way postpones painful feelings C) converting or transferring a mental conflict to a physical symptom can lead to conflict within the partnership D) isolating the feelings in this way reduces conflict within the client and with others A: such fantasies can gratify unconscious wishes or prepare for anticipated future events. Fantasy is imagined events (daydreaming) to express unconscious conflicts or gratify unconscious wishes. Basic Care and Comfort 1. The nurse is planning care for a client with a cerebral vascular accident (CVA). Which of the following measures planned by the nurse would be most effective in preventing skin breakdown? A) Place client in the wheelchair for four hours each day B) Pad the bony prominence C) Reposition every two hours D) Massage reddened bony prominence C: Reposition every two hours. Clients who are at risk for skin breakdown develop fewer pressure ulcers when turned every two hours. By relieving the pressure over bony prominences at frequent scheduled intervals, blood flow to areas of potential injury is maintained. 2. After a client has an enteral feeding tube inserted, the most accurate method for verification of placement is A) abdominal x-ray B) auscultation C) flushing tube with saline D) aspiration for gastric contents A: abdominal x-ray. Placement should be verified by radiograph to determine that the tube is in the stomach or intestine rather than in the airways. 3. The nurse has been teaching a client with congestive heart failure about proper nutrition. Which of these lunch selections indicates the client has learned about sodium restriction? A) Cheese sandwich with a glass of 2% milk B) Sliced turkey sandwich and canned pineapple C) Cheeseburger and baked potato D) Mushroom pizza and ice cream B: Sliced turkey sandwich and canned pineapple. Sliced turkey sandwich is appropriate since it is not a highly processed food and canned fruits are low in sodium. All of the other choices contain one or more high-sodium foods. 4. The nurse is caring for a 7 year-old with acute glomerulonephritis (AGN). Findings include moderate edema and oliguria. Serum blood urea nitrogen and creatinine are elevated. What dietary modifications are most appropriate? A) Decreased carbohydrates and fat B) Decreased sodium and potassium C) Increased potassium and protein D) Increased sodium and fluids B: Decreased sodium and potassium. Children with AGN who have edema, hypertension oliguria, and azotemia have dietary restrictions limiting sodium, potassium, fluids, and protein. 415. After a myocardial infarction, a client is placed on a sodium restricted diet. When the nurse is teaching the client about the diet, which meal plan would be the most appropriate to suggest? A) 3 oz. broiled fish, 1 baked potato, ½ cup canned beets, 1 orange, and milk B) 3 oz. canned salmon, fresh broccoli, 1 biscuit, tea, and 1 apple C) A bologna sandwich, fresh eggplant, 2 oz fresh fruit, tea, and apple juice D) 3 oz. turkey, 1 fresh sweet potato, 1/2 cup fresh green beans, milk, and 1 orange D: 3 oz. turkey, 1 fresh sweet potato, 1/2 cup fresh green beans, milk, and 1 orange. Canned fish and vegetables and cured meats are high in sodium. This meal does not contain any canned fish and/or vegetables or cured meats. 6. What finding of the nursing assessment of a paralyzed client would indicate the probable presence of a fecal impaction? A) Presence of blood in stools B) Oozing liquid stool C) Continuous rumbling flatulence D) Absence of bowel movements B: Oozing liquid stool. When the bowel is impacted with hardened feces, there is often a seepage of liquid feces around the obstruction. This is often mistaken for uncontrolled diarrhea. 7. The nurse is teaching the client to select foods rich in potassium to help prevent digitalis toxicity. Which choice indicates the client understands dietary needs? A) three apricots B) medium banana C) naval orange D) baked potato D: baked potato. A baked potato contains 610 milligrams of potassium. 8. When administering enteral feeding to a client via a jejunostomy tube, the nurse should administer the formula A) every four to six hours B) continuously C) in a bolus D) every hour B: continuously. Usually gastrostomy and jejunostomy feedings are given continuously to ensure proper absorption. However, initial feedings may be given by bolus to assess the client''s tolerance to formula. 9. An 86 year-old nursing home resident who has impaired mental status is hospitalized with pneumonic infiltrates in the right lower lobe. When the nurse assists the client with a clear liquid diet, the client begins to cough. What should the nurse do next? A) Add a thickening agent to the fluids B) Check the client’s gag reflex C) Feed the client only solid foods D) Increase the rate of intravenous fluids B: Check the client’s gag reflex. When a new problem emerges, the nurse should perform appropriate assessment so that suitable nursing interventions can be planned. Aspiration pneumonia follows aspiration of material from the mouth into the trachea and finally the lung. A loss or an impairment of the protective cough reflex can result in aspiration. 10. An 85 year-old client complains of generalized muscle aches and pains. The first action by the nurse should be A) assess the severity and location of the pain B) obtain an order for an analgesic C) reassure him that this is not unusual for his age D) encourage him to increase his activity A: assess the severity and location of the pain. Most older adults have 1 or more chronic painful illnesses, and in fact, they often must be asked about discomfort (rather than "pain") to reveal the presence of pain. There is no evidence that pain of older adults is less intense than younger adults. It is important for the nurse to assess the pain thoroughly before implementing pain relief measures. 11. A client was just taken off the ventilator after surgery and has a nasogastric tube draining bile-colored liquids. Which nursing measure will provide the most comfort to the client? A) Allow the client to melt ice chips in the mouth B) Provide mints to freshen the breath C) Perform frequent oral care with a tooth sponge D) Swab the mouth with glycerin swabs C: Perform frequent oral care with a tooth sponge. Frequent cleansing and stimulation of the mucous membrane is important for a client with a nasogastric tube to prevent development of lesions and to promote comfort. Ice chips or mints could be contraindicated, and do not stimulate the tissue. Glycerin swabs do not cleanse since they only moisturize. 4212. The nurse is instructing a 65 year-old female client diagnosed with osteoporosis. The most important instruction regarding exercise would be to A) exercise doing weight bearing activities B) exercise to reduce weight C) avoid exercise activities that increase the risk of fracture D) exercise to strengthen muscles and thereby protect bones A: exercise doing weight bearing activities. Weight bearing exercises are beneficial in the treatment of osteoporosis. Although loss of bone cannot be substantially reversed, further loss can be greatly reduced if the client includes weight bearing exercises along with estrogen replacement and calcium supplements in their treatment protocol. 13. A nurse is assessing several clients in a long term health care facility. Which client is at highest risk for development of decubitus ulcers? A) A 79 year-old malnourished client on bed rest B) An obese client who uses a wheelchair C) An incontinent client who has had 3 diarrhea stools D) An 80 year-old ambulatory diabetic client A: A 79 year-old malnourished client on bed rest. Weighing significantly less than ideal body weight increases the number and surface area of bony prominences which are susceptible to pressure ulcers. Thus, malnutrition is a major risk factor for decubiti, due in part to poor hydration and inadequate protein intake. 14. Constipation is one of the most frequent complaints of elders. When assessing this problem, which action should be the nurse's priority? A) obtain a complete blood count B) obtain a health and dietary history C) refer to a provider for a physical examination D) measure height and weight B: obtain a health and dietary history. Initially, the nurse should obtain information about the chronicity of and details about constipation, recent changes in bowel habits, physical and emotional health, medications, activity pattern, and food and fluid history. This information may suggest causes as well as an appropriate, safe treatment plan. 15. A nurse is working with a client in an extended care facility. Which bed position is preferred for a client, who is at risk for falls, as part of a prevention protocol? A) All 4 side rails up, wheels locked, bed closest to door B) Lower side rails up, bed facing doorway C) Knees bent, head slightly elevated, bed in lowest position D) Bed in lowest position, wheels locked, place bed against wall D: It is no longer advisable to use only the lower side rails. Using all 4 side rails (upper and lower siderails at the top and bottom of the bed) is an inappropriate use of restraint without an order. If all 4 are pulled up, an order for protective restraints is needed that usually has to be renewed in 48 to 72 hours along with more frequent documentation. Having all 4 side rails raised limits the client’s autonomy and freedom of movement. Using 3 of the 4 side rails pulled up is acceptable, because clients can safely exit the bed on their own initiative. Placing the bed against the wall permits getting out of bed on only 1 side. Locking the wheels keeps the bed from sliding. Keeping the bed in the lowest position (without bending limbs to restrict movement) provides a shorter distance to the ground if the client chooses to get out of bed. 16. The nurse is teaching an 87 year-old client methods for maintaining regular bowel movements. The nurse would caution the client to avoid A) glycerine suppositories B) fiber supplements C) laxatives D) stool softeners C: laxatives. Some elders are constipated because they have used over-the-counter laxatives for a long time. In addition, many people do not eat enough fiber, drink enough water, or exercise adequately. Certain medications, including opioid analgesics, are constipating. Elders are rarely constipated because of organic or pathological reasons. 17. Which statement best describes the effects of immobility in children? A) Immobility prevents the progression of language and fine motor development B) Immobility in children has similar physical effects to those found in adults C) Children are more susceptible to the effects of immobility than are adults D) Children are likely to have prolonged immobility with subsequent complications B: Immobility in children has similar physical effects to those found in adults Care of the immobile child includes efforts to prevent complications of muscle atrophy, contractures, skin breakdown, decreased metabolism and bone demineralization. Secondary alterations also occur in the cardiovascular, respiratory and renal systems. Similar effects and alterations occur in adults. 18. A client with diarrhea should avoid which of the following? 43A) orange juice B) tuna C) eggs D) macaroni A: Orange juice is contraindicated for a client with diarrhea because it increases the motility of the gastrointestinal tract. 19. A client is being maintained on heparin therapy for deep vein thrombosis (DVT). The nurse must closely monitor which of the following laboratory values? A) bleeding time B) platelet count C) activated PTT D) clotting time C: activated PTT. Heparin is used to prevent further clots from being formed and to prevent the present clot from enlarging. The Activated Prothromboplastin Time (APTT) test is a highly sensitive test to monitor the client on heparin. 20. A client in a long term care facility complains of pain. The nurse collects data about the client’s pain. The first step in pain assessment is for the nurse to A) have the client identify coping methods B) get the description of the location and intensity of the pain C) accept the client’s report of pain D) determine the client’s status of pain C: accept the client’s report of pain. Although all of the options above are correct, the first and most important piece of information in this client’s pain assessment is what the client is telling you about the pain --“the client’s report.” Pharmacological and Parenteral Therapies 1. A client is receiving intravenous heparin therapy. What medication should the nurse have available in the event of an overdose of heparin? A) Protamine B) Amicar C) Imferon D) Diltiazem A: Protamine. Protamine binds heparin, making it ineffective. 2. Although nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen (Motrin) are beneficial in managing arthritis pain, the nurse should caution clients about which of the following common side effects? A) Urinary incontinence B) Constipation C) Nystagmus D) Occult bleeding D: Occult bleeding. Nonsteroidal anti-inflammatory drugs (NSAIDs) taken for long periods of time may cause serious side effects, including bleeding in the gastrointestinal track. 3. A client is being discharged with a prescription for chlorpromazine (Thorazine). Before leaving for home, which of these findings should the nurse teach the client to report? A) Change in libido, breast enlargement B) Sore throat, fever C) Abdominal pain, nausea, diarrhea D) Dyspnea, nasal congestion B: A sore throat and fever may be findings of agranulocytosis, a serious side effect of chlorpromazine (Thorazine). 4. The nurse receives an order to give a client iron by deep injection. The nurse know that the reason for this route is to A) enhance absorption of the medication B) ensure that the entire dose of medication is given C) provide more even distribution of the drug D) prevent the drug from causing tissue irritation D: prevent the drug from causing tissue irritation. Deep injection or Z-track is a special method of giving medications via the intramuscular route. Use of this technique prevents irritating or staining medications from being tracked through tissue. Use of Ztrack does not affect dose, absorption, or distribution of the drug. 445. A client diagnosed with cirrhosis of the liver and ascites is receiving spironolactone (Aldactone). The nurse understands that this medication spares elimination of which element? A) Sodium B) Potassium C) Phosphate D) Albumin B: Potassium. If ascites is present in the client with cirrhosis of the liver, potassium-sparing diuretics such as Aldactone should be administered because it inhibits the action of aldosterone on the kidneys. 6. Discharge instructions for a client taking alprazolam (Xanax) should include which of the following? A) Sedative hypnotics are effective analgesics B) Sudden cessation of alprazolam (Xanax) can cause rebound insomnia and nightmares C) Caffeine beverages can increase the effect of sedative hypnotics D) Avoidance of excessive exercise and high temperature is recommended B: Sudden cessation of any medication, unless medically necessary, is ill-advised. 7. A client has received 2 units of whole blood today following an episode of GI bleeding. Which of the following laboratory reports would the nurse monitor most closely? A) Bleeding time B) Hemoglobin and hematocrit C) White blood cells D) Platelets B: Hemoglobin and hematocrit. The post-transfusion hematocrit provides immediate information about red cell replacement and about continued blood loss. 8. The nurse is caring for a client receiving a blood transfusion who develops urticaria one-half hour after the transfusion has begun. What is the first action the nurse should take? A) Stop the infusion B) Slow the rate of infusion C) Take vital signs and observe for further deterioration D) Administer Benadryl and continue the infusion A: Stop the infusion. This is an indication of an allergy to the plasma protein. The priority action of the nurse is to stop the transfusion. 9. A nurse is providing care to a 63 year-old client with pneumonia. Which intervention promotes the client’s comfort? A) Increase oral fluid intake B) Encourage visits from family and friends C) Keep conversations short D) Monitor vital signs frequently C: Keep conversations short. Keeping conversations short will promote the client’s comfort by decreasing demands on the client’s breathing and energy. Increased intake is not related to comfort. While the presence of family is supportive, demands on the client to interact with the visitors may interfere with the client’s rest. Monitoring vital signs is an important assessment but not related to promoting the client’s comfort. 10. An antibiotic IM injection for a 2 year-old child is ordered. The total volume of the injection equals 2.0 ml. The correct action is to A) administer the medication in 2 separate injections B) give the medication in the dorsal gluteal site C) call to get a smaller volume ordered D) check with pharmacy for a liquid form of the medication A: administer the medication in 2 separate injections. Intramuscular injections should not exceed a volume of 1 ml for small children. Medication doses exceeding this volume should be split into 2 separate injections of 1.0 ml each. In adults the maximum intramuscular injection volume is 5 ml per site 11. A client is recovering from a hip replacement and is taking Tylenol #3 every 3 hours for pain. In checking the client, which finding suggests a side effect of the analgesic? A) Bruising at the operative site B) Elevated heart rate C) Decreased platelet count D) No bowel movement for 3 days D: No bowel movement for 3 days. With opioid analgesics, observe for respiratory depression, sedation, and constipation. Bruising is not related to the analgesic, but could be the result of corticosteroids or previously used anticoagulants. Elevated heart rate could be the result of bronchodilators. Some antibiotics can lower platelet count. 12. Why is it important for the nurse to monitor blood pressure in clients receiving antipsychotic drugs? 45A) Orthostatic hypotension is a common side effect B) Most antipsychotic drugs cause elevated blood pressure C) This provides information on the amount of sodium allowed in the diet D) It will indicate the need to institute antiparkinsonian drugs A: Orthostatic hypotension is a common side effect. Clients should be made aware of the possibility of dizziness and syncope from postural hypotension for about an hour after receiving medication. They should be advised to get up slowly, especially from a supine position. 13. A parent asks the school nurse how to eliminate lice from their child. What is the most appropriate response by the nurse? A) Cut the child's hair short to remove the nits B) Apply warm soaks to the head twice daily C) Wash the child's linen and clothing in a bleach solution D) Application of pediculicides D: Application of pediculicides. Treatment of head lice consists of application of pediculicides. Pediculicides vary, and the directions must be followed carefully. 14. The nurse has given discharge instructions to parents of a child on phenytoin (Dilantin). Which of the following statements suggests that the teaching was effective? A) "We will call the health care provider if the child develops acne." B) "Our child should brush and floss carefully after every meal." C) "We will skip the next dose if vomiting or fever occur." D) "When our child is seizure-free for 6 months, we can stop the medication." B: "Our child should brush and floss carefully after every meal." Phenytoin causes lymphoid hyperplasia that is most noticeable in the gums. Frequent gum massage and careful attention to good oral hygiene may reduce the gingival hyperplasia. 15. A client with heart failure has Lanoxin (digoxin) ordered. What would the nurse expect to find when evaluating for the therapeutic effectiveness of this drug? A) Diaphoresis with decreased urinary output B) Increased heart rate with increased respirations C) Improved respiratory status and increased urinary output D) Decreased chest pain and decreased blood pressure C: Improved respiratory status and increased urinary output. Digoxin, a cardiac glycoside, is used in clients with heart failure to slow and strengthen the heartbeat. As cardiac output is improved, renal perfusion is improved and urinary output increases. Clients can become toxic on this drug, indicated by findings of bradycardia, dysrhythmia, and visual and GI disturbances. Clients being treated with digoxin should have their apical pulse evaluated for 1 full minute prior to the administration of the drug. 16. The nurse is teaching a client about precautions with Coumadin therapy. The client should be instructed to avoid which over-the-counter medication? A) Non-steroidal anti-inflammatory drugs (NSAIDs) B) Cough medicines with guaifenesin C) Histamine blockers D) Laxatives containing magnesium salts A: Non-steroidal anti-inflammatory drugs (NSAIDs). Medications with NSAIDs may increase the response to Coumadin (warfarin) and increase the risk of bleeding. 17. The nurse is caring for a client with clinical depression who is receiving a monoamine oxidase inhibitor (MAOI). When providing instructions about precautions with this medication, which action should the nurse stress to the client as important? A) Avoid chocolate and cheese B) Take frequent naps C) Take the medication with milk D) Avoid walking without assistance A: Avoid chocolate and cheese. Foods high in tryptophan, tyramine and caffeine, such as chocolate, wine and cheese may precipitate hypertensive crisis. 18. The nurse has been teaching a client with Insulin Dependent Diabetes Mellitus. Which statement by the client indicates a need for further teaching? A) "I use a sliding scale to adjust regular insulin to my sugar level." B) "Since my eyesight is so bad, I ask the nurse to fill several syringes." C) "I keep my regular insulin bottle in the refrigerator." D) "I always make sure to shake the NPH bottle hard to mix it well." D: "I always make sure to shake the NPH bottle hard to mix it well." The bottle should by rolled gently, not shaken. 19. A client with amyotrophic lateral sclerosis has a percutaneous endoscopic gastrostomy (PEG) tube for the administration of feedings and medications. Which nursing action is appropriate? 46A) Pulverize all medications to a powdery condition B) Squeeze the tube before using it to break up stagnant liquids C) Cleanse the skin around the tube daily with hydrogen peroxide D) Flush adequately with water before and after using the tube D: Flush adequately with water before and after using the tube. Flushing the tube before and after use not only provides for good flow and keeps the tube patent, it also provides water to maintain hydration. While medications should be crushed to pass through the tube, it is flushing that moves them through. Not all medications should be crushed, for example sustained release preparations should not be cut or pulverized. Stagnant liquids are reduced by flushing after tube use. Cleansing is important, but soap and water are sufficient without the added irritation of hydrogen peroxide 20. While providing home care to a client with congestive heart failure, the nurse is asked how long diuretics must be taken. What is the nurse’s best response? A) "As you urinate more, you will need less medication to control fluid." B) "You will have to take this medication for about a year." C) "The medication must be continued so the fluid problem is controlled." D) "Please talk to your health care provider about medications and treatments." C: "The medication must be continued so the fluid problem is controlled." This is the most therapeutic response and gives the client accurate information. Q&A Pharmacology 1. A post-operative client has a prescription for acetaminophen with codeine. What should the nurse recognizes as a primary effect of this combination? A) Enhanced pain relief B) Minimized side effects C) Prevention of drug tolerance D) Increased onset of action A: Enhanced pain relief. Combination of analgesics with different mechanisms of action can afford greater pain relief. 2. A nurse is caring for a client who is receiving methyldopa hydrochloride (Aldomet) intravenously. Which of the following assessment findings would indicate to the nurse that the client may be having an adverse reaction to the medication? A) Headache B) Mood changes C) Hyperkalemia D) Palpitations B: Mood changes. The nurse should assess the client for alterations in mental status such as mood changes. These symptoms should be reported promptly. 3. When providing discharge teaching to a client with asthma, the nurse will warn against the use of which of the following over-the-counter medications? A) Cortisone ointments for skin rashes B) Aspirin products for pain relief C) Cough medications containing guaifenesin D) Histamine blockers for gastric distress B: Aspirin products for pain relief. Aspirin is known to induce asthma attacks. Aspirin can also cause nasal polyps and rhinitis. Warn individuals with asthma about signs and symptoms resulting from complications due to aspirin ingestion. 4. The nurse practicing in a long term care facility recognizes that elderly clients are at greater risk for drug toxicity than younger adults because of which of the following physiological changes of advancing age? A) Drugs are absorbed more readily from the GI tract B) Elders have less body water and more fat C) The elderly have more rapid hepatic metabolism D) Older people are often malnourished and anemic B: Elders have less body water and more fat. Because elderly persons have decreased lean body tissue/water in which to distribute medications, more drug remains in the circulatory system with potential for drug toxicity. Increased body fat results in greater amounts of fat-soluble drugs being absorbed, leaving less in circulation, thus increasing the duration of action of the drug. 5. In providing care for a client with pain from a sickle cell crisis, which one of the following medication orders for pain control should be questioned by the nurse? A) Demerol B) Morphine C) Methadone D) Codeine 47A: Demerol. Meperidine is not recommended in clients with sickle cell disease. Normeperidine, a metabolite of meperidine, is a central nervous system stimulant that produces anxiety, tremors, myoclonus, and generalized seizures when it accumulates with repetitive dosing. Clients with sickle cell disease are particularly at risk for normeperidine-induced seizures. 6. The nurse is administering diltiazem (Cardizem) to a client. Prior to administration, it is important for the nurse to assess which parameter? A) Temperature B) Blood pressure C) Vision D) Bowel sounds B: Blood pressure. Diltiazem (Cardizem) is a calcium channel blocker that causes systemic vasodilation resulting in decreased blood pressure. 7. A client with an aplastic sickle cell crisis is receiving a blood transfusion and begins to complain of "feeling hot." Almost immediately, the client begins to wheeze. What is the nurse's first action? A) Stop the blood infusion B) Notify the health care provider C) Take/record vital signs D) Send blood samples to lab A: Stop the blood infusion. If a reaction of any type is suspected during administration of blood products, stop the infusion immediately, keep the line open with saline, notify the health care provider, monitor vital signs and other changes, and then send a blood sample to the lab. 8. A client with atrial fibrillation is receiving digoxin (Lanoxin). Which of these assessments is most important for the nurse to perform? A) Monitor blood pressure every 4 hours B) Measure apical pulse prior to administration C) Maintain accurate intake and output records D) Record an EKG strip after administration B: Measure apical pulse prior to administration. Digitoxin decreases conduction velocity through the AV node and prolongs the refractory period. If the apical heart rate is less than 60 beats/minute, withhold the drug. The apical pulse should be taken with a stethoscope so that there will be no mistake about what the heart rate actually is. 9. The nurse is caring for a 10 year-old client who will be placed on heparin therapy. Which assessment is critical for the nurse to make before initiating therapy A) Vital signs B) Weight C) Lung sounds D) Skin turgor B: Weight. Check the client''s weight because dosage is calculated on the basis of weight. 10. The use of atropine for treatment of symptomatic bradycardia is contraindicated for a client with which of the following conditions? A) Urinary incontinence B) Glaucoma C) Increased intracranial pressure D) Right sided heart failure B: Glaucoma. Atropine is contraindicated in clients with angle-closure glaucoma because it can cause pupillary dilation with an increase in aqueous humor, leading to a resultant increase in optic pressure. 11. The health care provider orders an IV aminophylline infusion at 30 mg/hr. The pharmacy sends a 1,000 ml bag of D5W containing 500 mg of aminophylline. In order to administer 30 mg per hour, the RN will set the infusion rate at: A) 20 ml per hour B) 30 ml per hour C) 50 ml per hour D) 60 ml per hour D: 60 ml per hour. Using the ratio method to calculate infusion rate: mg to be given (30) : ml to be infused (X) :: mg available (500) : ml of solution (1,000). Solve for X by cross-multiplying: 30 x 1,000 = 500 x X (or cancel), 30,000 = 500 X, X = 30,000/500, X = 60 ml per hour. 12. The nurse is applying silver sulfadiazine (Silvadene) to a child with severe burns to arms and legs. Which side effect should the nurse be monitoring for? A) Skin discoloration B) Hardened eschar C) Increased neutrophils D) Urine sulfa crystals 48D: Urine sulfa crystals. Silver sulfadiazine is a broad spectrum anti-microbial, especially effective against pseudomonas. When applied to extensive areas, however, it may cause a transient neutropenia, as well as renal function changes with sulfa crystals production and kernicterus. 13. The nurse is caring for a client who is receiving procainamide (Pronestyl) intravenously. It is important for the nurse to monitor which of the following parameters? A) Hourly urinary output B) Serum potassium levels C) Continuous EKG readings D) Neurological signs C: Continuous EKG readings. Procainamide (Pronestyl) is used to suppress cardiac arrhythmias. When administered intravenously, it must be accompanied by continuous cardiac monitoring by ECG. 14. The nurse is teaching a parent how to administer oral iron supplements to a 2 year-old child. Which of the following interventions should be included in the teaching? A) Stop the medication if the stools become tarry green B) Give the medicine with orange juice and through a straw C) Add the medicine to a bottle of formula D) Administer the iron with your child's meals B: Give the medicine with orange juice and through a straw. Absorption of iron is facilitated in an environment rich in Vitamin C. Since liquid iron preparation will stain teeth, a straw is preferred. 15. A client with bi-polar disorder is taking lithium (Lithane). What should the nurse emphasize when teaching about this medication? A) Take the medication before meals B) Maintain adequate daily salt intake C) Reduce fluid intake to minimize diuresis D) Use antacids to prevent heartburn B: Maintain adequate daily salt intake. Salt intake affects fluid volume, which can affect lithium (Lithane) levels; therefore, maintaining adequate salt intake is advised. 16. The nurse is assessing a 7 year-old after several days of treatment for a documented strep throat. Which of the following statements suggests that further teaching is needed? A) "Sometimes I take my medicine with fruit juice." B) "My mother makes me take my medicine right after school." C) "Sometimes I take the pills in the morning and other times at night." D) "I am feeling much better than I did last week." C: "Sometimes I take the pills in the morning and other times at night." Inconsistency in taking the prescribed medication indicates more teaching is needed. 17. An elderly client is on an anticholinergic metered dose inhaler (MDI) for chronic obstructive pulmonary disease. The nurse would suggest a spacer to A) enhance the administration of the medication B) increase client compliance C) improve aerosol delivery in clients who are not able to coordinate the MDI D) prevent exacerbation of COPD C: Spacers improve the medication delivery in clients who are unable to coordinate the movements of administering a dose with an MDI. 18. The nurse is providing education for a client with newly diagnosed tuberculosis. Which statement should be included in the information that is given to the client? A) "Isolate yourself from others until you are finished taking your medication." B) "Follow up with your primary care provider in 3 months." C) "Continue to take your medications even when you are feeling fine." D) "Continue to get yearly tuberculin skin tests." C: The most important piece of information the tuberculosis client needs is to understand the importance of medication compliance, even if no longer experiencing symptoms. Clients are most infectious early in the course of therapy. The numbers of acid-fast bacilli are greatly reduced as early as 2 weeks after therapy begins. 19. The nurse is administering an intravenous vesicant chemotherapeutic agent to a client. Which assessment would require the nurse's immediate action? A) Stomatitis lesion in the mouth B) Severe nausea and vomiting C) Complaints of pain at site of infusion D) A rash on the client's extremities 49C: Complaints of pain at site of infusion. A vesicant is a chemotherapeutic agent capable of causing blistering of tissues and possible tissue necrosis if there is extravasation. These agents are irritants which cause pain along the vein wall, with or without inflammation. 20. The nurse is instructing a client with moderate persistent asthma on the proper method for using MDIs (multi-dose inhalers). Which medication should be administered first? A) Steroid B) Anticholinergic C) Mast cell stabilizer D) Beta agonist D: Beta agonist. The beta-agonist drugs help to relieve bronchospasm by relaxing the smooth muscle of the airway. These drugs should be taken first so that other medications can reach the lungs. 21. The nurse is teaching a group of women in a community clinic about prevention of osteoporosis. Which of the following over-the-counter medications should the nurse recognize as having the most elemental calcium per tablet? A) Calcium chloride B) Calcium citrate C) Calcium gluconate D) Calcium carbonate D: Calcium carbonate. Calcium carbonate contains 400mg of elemental calcium in 1 gram of calcium carbonate. 22. The provider has ordered daily high doses of aspirin for a client with rheumatoid arthritis. The nurse instructs the client to discontinue the medication and contact the provider if which of the following symptoms occur? A) Infection of the gums B) Diarrhea for more than one day C) Numbness in the lower extremities D) Ringing in the ears D: Ringing in the ears. Aspirin stimulates the central nervous system which may result in ringing in the ears. 23. A 5 year-old has been rushed to the emergency room several hours after acetaminophen poisoning. Which laboratory result should receive attention by the nurse? A) Sedimentation rate B) Profile 2 C) Bilirubin D) Neutrophils C: Bilirubin. Bilirubin, along with liver enzymes ALT and AST, may rise in the second stage (1-3 days) after a significant overdose, indicating cellular necrosis and liver dysfunction. 24. The nurse is caring for a client with schizophrenia who has been treated with quetiapine (Seroquel) for 1 month. Today the client is increasingly agitated and complains of muscle stiffness. Which of these findings should be reported to the health care provider? A) Elevated temperature and sweating. B) Decreased pulse and blood pressure. C) Mental confusion and general weakness. D) Muscle spasms and seizures. A: Elevated temperature and sweating. Neuroleptic malignant syndrome (NMS) is a rare disorder that can occur as a side effect of antipsychotic medications. It is characterized by muscular rigidity, tachycardia, hyperthermia, sweating, altered consciousness, autonomic dysfunction, and increase in CPK. This is a life-threatening complication. 25. A client is receiving dexamethasone (Decadron) therapy. What should the nurse plan to monitor in this client? A) Urine output every 4 hours B) Blood glucose levels every 12 hours C) Neurological signs every 2 hours D) Oxygen saturation every 8 hours B: The drug Decadron increases glycogenesis. This may lead to hyperglycemia. Therefore the blood sugar level and acetone production must be monitored. 26. The nurse is teaching a child and the family about the medication phenytoin (Dilantin) prescribed for seizure control. Which of the following side effects is most likely to occur? A) Vertigo B) Drowsiness C) Gingival hyperplasia D) Vomiting 50C: Swollen and tender gums occur often with use of phenytoin. Good oral hygiene and regular visits to the dentist should be emphasized. 27. A newly admitted client has a diagnosis of depression. She complains of “twitching muscles” and a “racing heart”, and states she stopped taking Zoloft a few days ago because it was not helping her depression. Instead, she began to take her partner's Parnate. The nurse should immediately assess for which of these adverse reactions? A) Pulmonary edema B) Atrial fibrillation C) Mental status changes D) Muscle weakness C: Mental status changes. Use of serotonergic agents may result in Serotonin Syndrome with confusion, nausea, palpitations, increased muscle tone with twitching muscles, and agitation. Serotonin syndrome is most often reported in patients taking 2 or more medications that increase CNS serotonin levels by different mechanisms. The most common drug combinations associated with serotonin syndrome involve the MAOIs, SSRIs, and the tricyclic antidepressants.). Philadelphia: Saunders. 28. A client has been receiving dexamethasone (Decadron) for control of cerebral edema. Which of the following assessments would indicate that the treatment is effective? A) A positive Babinski's reflex B) Increased response to motor stimuli C) A widening pulse pressure D) Temperature of 37 degrees Celsius B: Decadron is a corticosteroid that acts on the cell membrane to decrease inflammatory responses as well as stabilize the bloodbrain barrier. Once Decadron reaches a therapeutic level, there should be a decrease in symptomology with improvement in motor skills. 29. The nurse is assessing a client who is on long term glucocorticoid therapy. Which of the following findings would the nurse expect? A) Buffalo hump B) Increased muscle mass C) Peripheral edema D) Jaundice A: Buffalo hump. With high doses of glucocorticoid, iatrogenic Cushing''s syndrome develops. The exaggerated physiological action causes abnormal fat distribution which results in a moon-shaped face, a intrascapular pad on the neck (buffalo hump) and truncal obesity with slender limbs. 30. A client is ordered atropine to be administered preoperatively. Which physiological effect should the nurse monitor for? A) Elevate blood pressure B) Drying up of secretions C) Reduce heart rate D) Enhance sedation B: Drying up of secretions. Atropine dries secretions which may get in the way during the operative procedure. 31. A client confides in the RN that a friend has told her the medication she takes for depression, Wellbutrin, was taken off the market because it caused seizures. What is an appropriate response by the nurse? A) "Ask your friend about the source of this information." B) "Omit the next doses until you talk with the doctor." C) "There were problems, but the recommended dose is changed." D) "Your health care provider knows the best drug for your condition." C: Wellbutrin was introduced in the U.S. in 1985 and then withdrawn because of the occurrence of seizures in some patients taking the drug. The drug was reintroduced in 1989 with specific recommendations regarding dose ranges to limit the occurrence of seizures. The risk of seizure appears to be strongly associated with dose. 32. A child presents to the Emergency Department with documented acetaminophen poisoning. In order to provide counseling and education for the parents, which principle must the nurse understand? A) The problem occurs in stages with recovery within 12-24 hours B) Hepatic problems may occur and may be life-threatening C) Full and rapid recovery can be expected in most children D) This poisoning is usually fatal, as no antidote is available B: Hepatic problems may occur and may be life-threatening. Clinical manifestations associated with acetaminophen poisoning occurs in 4 stages. The third stage is hepatic involvement which may last up to 7 days and be permanent. Clients who do not die in the hepatic stage gradually recover. 33. A client is receiving digitalis. The nurse should instruct the client to report which of the following side effects? A) Nausea, vomiting, fatigue B) Rash, dyspnea, edema C) Polyuria, thirst, dry skin 51D) Hunger, dizziness, diaphoresis A: Nausea, vomiting, fatigue. Side effects of digitalis toxicity include fatigue, nausea, vomiting, anorexia, and bradycardia. Digitalis inhibits the sodium potassium ATPase, which makes more calcium available for contractile proteins, resulting in increased cardiac output. 34. The provider has ordered transdermal nitroglycerin patches for a client. Which of these instructions should be included when teaching a client about how to use the patches? A) Remove the patch when swimming or bathing B) Apply the patch to any non-hairy area of the body C) Apply a second patch with chest pain D) Remove the patch if ankle edema occurs B: Apply the patch to any non-hairy area of the body. The patch application sites should be rotated. 35. A pregnant woman is hospitalized for treatment of pregnancy induced hypertension (PIH) in the third trimester. She is receiving magnesium sulfate intravenously. The nurse understands that this medication is used mainly for what purpose? A) Maintain normal blood pressure B) Prevent convulsive seizures C) Decrease the respiratory rate D) Increase uterine blood flow B: Prevent convulsive seizures. Magnesium sulfate is a central nervous system depressant. While it has many systemic effects, it is used in the client with pregnancy induced hypertension (PIH) to prevent seizures. 36. A client with anemia has a new prescription for ferrous sulfate. In teaching the client about diet and iron supplements, the nurse should emphasize that absorption of iron is enhanced if taken with which substance? A) Acetaminophen B) Orange juice C) Low fat milk D) An antacid B: Orange juice. Ascorbic acid enhances the absorption of iron. 37. The health care provider has written "Morphine sulfate 2 mgs IV every 3-4 hours prn for pain" on the chart of a child weighing 22 lb. (10 kg). What is the nurse's initial action? A) Check with the pharmacist B) Hold the medication and contact the provider C) Administer the prescribed dose as ordered D) Give the dose every 6-8 hours B: Hold the medication and contact the provider. The usual pediatric dose of morphine is 0.1 mg/kg every 3 to 4 hours. At 10 kg, this child typically should receive 1.0 mg every 3 to 4 hours. 38. The nurse is monitoring a client receiving a thrombolytic agent, alteplase (Activase tissue plasminogen activator), for treatment of a myocardial infarction. What outcome indicates the client is receiving adequate therapy within the first hours of treatment? A) Absence of a dysrhythmia (or arrhythmia) B) Blood pressure reduction C) Cardiac enzymes are within normal limits D) Return of ST segment to baseline on ECG D: Return of ST segment to baseline on ECG. Improved perfusion should result from this medication, along with the reduction of ST segment elevation. 39. A nurse is assigned to perform well-child assessments at a day care center. A staff member interrupts the examinations to ask for assistance. They find a crying 3 year-old child on the floor with mouth wide open and gums bleeding. Two unlabeled open bottles lie nearby. The nurse's first action should be A) call the poison control center, then 911 B) administer syrup of Ipecac to induce vomiting C) give the child milk to coat her stomach D) ask the staff about the contents of the bottles D: ask the staff about the contents of the bottles. The nurse needs to assess what the child ingested before determining the next action. Once the substance is identified, the poison control center and emergency response team should be called. 40. A client is receiving erythromycin 500mg IV every 6 hours to treat a pneumonia. Which of the following is the most common side effect of the medication? A) Blurred vision B) Nausea and vomiting C) Severe headache 52D) Insomnia B: Nausea and vomiting. Nausea is a common side-effect of erythromycin in both oral and intravenous forms. 41. A 4 year-old child is admitted with burns on his legs and lower abdomen. When assessing the child’s hydration status, which of the following indicates a less than adequate fluid replacement? A) Decreasing hematocrit and increasing urine volume B) Rising hematocrit and decreasing urine volume C) Falling hematocrit and decreasing urine volume D) Stable hematocrit and increasing urine volume B: Rising hematocrit and decreasing urine volume. A rising hematocrit indicates a decreased total blood volume, a finding consistent with dehydration. 42. Prior to administering Alteplase (TPA) to a client admitted for a cerebral vascular accident (CVA), it is critical that the nurse assess: A) Neuro signs B) Mental status C) Blood pressure D) PT/PTT D: PT/PTT. TPA is a potent thrombolytic enzyme. Because bleeding is the most common side effect, it is most essential to evaluate clotting studies including PT, PTT, APTT, platelets, and hematocrit before beginning therapy. 43. A nurse who has been named in a lawsuit can use which of these factors for the best protection in a court of law? A) Clinical specialty certification in the associated area of practice B) Documentation on the specific client record with a focus on the nursing process C) Yearly evaluations and proficiency reports prepared by nurse’s manager D) Verification of provider's orders for the plan of care with identification of outcomes B: Documentation is the key to protect nurses when a lawsuit is filed. The thorough documentation should include all steps of the nursing process – assessment, analysis, plan, intervention, evaluation. In addition, it should include pertinent data such as times, dosages and sites of actions, assessment data, the nurse’s response to a change in the client’s condition, specific actions taken, if and when the notification occurred to the provider or other health care team members, and what was prescribed along with the client’s outcomes. 44. The nurse is caring for clients over the age of 70. The nurse knows that due to age-related changes, the elderly clients tolerate diets that are A) high protein B) high carbohydrates C) low fat D) high calories C: low fat. Due to age related changes, the diet of the elderly should include a lower quantity and higher quality of food. Fewer carbohydrates and fats are required in their diets. 45. A client is to receive 3 doses of potassium chloride 10 mEq in 100cc normal saline to infuse over 30 minutes each. Which of the following is a priority assessment to perform before giving this medication? A) Oral fluid intake B) Bowel sounds C) Grip strength D) Urine output D: Urine output. Potassium chloride should only be administered after adequate urine output (>20cc/hour for 2 consecutive hours) has been established. Impaired ability to excrete potassium via the kidneys can result in hyperkalemia. 46. A hypertensive client is started on atenolol (Tenormin). The nurse instructs the client to immediately report which of these findings? A) Rapid breathing B) Slow, bounding pulse C) Jaundiced sclera D) Weight gain B: Slow, bounding pulse. Atenolol (Tenormin) is a beta-blocker that can cause side effects including bradycardia and hypotension. 47. During nursing rounds which of these assessments would require immediate corrective action and further instruction to the practical nurse (PN) about proper care? A) The weights of the skin traction of a client are hanging about 2 inches from the floor B) A client with a hip prosthesis 1 day post operatively is lying in bed with internal rotation and adduction of the affected leg C) The nurse observes that the PN moves the extremity of a client with an external fixation device by picking up the frame 53D) A client with skeletal traction states "The other nurse said that the clear, yellow and crusty drainage around the pin site is a good sign" B: A client with a hip prosthesis 1 day post operatively is lying in bed with internal rotation and adduction of the affected leg. This position should be prevented in order to prevent dislodgment of the hip prosthesis, especially in the first 48 to 72 hours postop. The other assessments are not of concern. 48. A client is scheduled for an intravenous pyelogram (IVP). After the contrast material is injected, which of the following client reactions should be reported immediately? A) Feeling warm B) Face flushing C) Salty taste D) Hives D: Hives. This is a sign of anaphylaxis and should be reported immediately. The other reactions are considered normal and the client should be informed that they may occur. 49. You are caring for a hypertensive client with a new order for captopril (Capoten). Which information should the nurse include in client teaching? A) Avoid green leafy vegetables B) Restrict fluids to 1000cc/day C) Avoid the use of salt substitutes D) Take the medication with meals C: Avoid the use of salt substitutes. Captopril can cause an accumulation of potassium or hyperkalemia. Clients should avoid the use of salt substitutes, which are generally potassium-based. 50. A client has bilateral knee pain from osteoarthritis. In addition to taking the prescribed non-steroidal anti-inflammatory drug (NSAID), the nurse should instruct the client to A) start a regular exercise program B) rest the knees as much as possible to decrease inflammation C) avoid foods high in citric acid D) keep the legs elevated when sitting A: start a regular exercise program. A regular exercise program is beneficial in treating osteoarthritis. It can restore self-esteem and improve physical functioning. 51. A client in respiratory distress is admitted with arterial blood gas results of: PH 7.30; PO2 58, PCO2 34; and HCO3 19. The nurse determines that the client is in A) metabolic acidosis B) metabolic alkalosis C) respiratory acidosis D) respiratory alkalosis A: metabolic acidosis. These lab values indicate metabolic acidosis: the PH is low, PCO2 is normal, and bicarbonate level is low. 52. A woman with a 28 week pregnancy is on the way to the emergency department by ambulance with a tentative diagnosis of abruptio placenta. Which should the nurse do first when the woman arrives? A) administer oxygen by mask at 100% B) start a second IV with an 18 gauge cannula C) check fetal heart rate every 15 minutes D) insert urethral catheter with hourly urine outputs A: administer oxygen by mask at 100%. Administering oxygen in this situation would increase the circulating oxygen in the mother’s circulation to the fetus’s circulation. This action will minimize complications. 53. You are caring for a client with deep vein thrombosis who is on Heparin IV. The latest APTT is 50 seconds. If the laboratory normal range is 16-24 seconds, you would anticipate A) maintaining the current heparin dose B) increasing the heparin as it does not appear therapeutic. C) giving protamine sulfate as an antidote. D) repeating the blood test 1 hour after giving heparin. A: maintaining the current heparin dose. The range for a therapeutic APTT is 1.5-2 times the control. Therefore the client is receiving a therapeutic dose of Heparin. 54. A client newly diagnosed with Type I Diabetes Mellitus asks the purpose of the test measuring glycosylated hemoglobin. The nurse should explain that the purpose of this test is to determine: A) The presence of anemia often associated with Diabetes B) The oxygen carrying capacity of the client's red cells C) The average blood glucose for the past 2-3 months D) The client's risk for cardiac complications 54C: The average blood glucose for the past 2-3 months. By testing the portion of the hemoglobin that absorbs glucose, it is possible to determine the average blood glucose over the life span of the red cell, 120 days. 55. An 80 year-old client is admitted with a diagnosis of malnutrition. In addition to physical assessments, which of the following lab tests should be closely monitored? A) Urine protein B) Urine creatinine C) Serum calcium D) Serum albumin D: Serum albumin. Serum albumin is a valuable indicator of protein deficiency and, later, nutritional status in adults. A normal reading for an elder’s serum albumin is between 3.0-5.0 g/dl. 56. A 66 year-old client is admitted for mitral valve replacement surgery. The client has a history of mitral valve regurgitation and mitral stenosis since her teenage years. During the admission assessment, the nurse should ask the client if as a child she had A) measles B) rheumatic fever C) hay fever D) encephalitis B: rheumatic fever. Clients that present with mitral stenosis often have a history of rheumatic fever or bacterial endocarditis. 57. Which of these clients should the charge nurse assign to the registered nurse (RN)? A) A 56 year-old with atrial fibrillation receiving digoxin B) A 60 year-old client with COPD on oxygen at 2 L/min C) A 24 year-old post-op client with type 1 diabetes in the process of discharge D) An 80 year-old client recovering 24 hours post right hip replacement C: Discharge teaching must be done by an RN. Practical nurses (PNs) or unlicensed assistive personnel (UAPs) can reinforce education after the RN does the initial teaching. 58. The nurse discusses nutrition with a pregnant woman who is iron deficient and follows a vegetarian diet. The selection of which foods indicates the woman has learned sources of iron? A) Cereal and dried fruits B) Whole grains and yellow vegetables C) Leafy green vegetables and oranges D) Fish and dairy products A: Cereal and dried fruits. Both of these foods would be a good source of iron. 59. A client diagnosed with gouty arthritis is admitted with severe pain and edema in the right foot. When the nurse develops a plan of care, which intervention should be included? A) high protein diet B) salicylates C) hot compresses to affected joints D) intake of at least 3000cc/day D: intake of at least 3000cc/day. Fluid intake should be increased to prevent precipitation of urate in the kidneys. 60. One hour before the first treatment is scheduled, the client becomes anxious and states he does not wish to go through with electroconvulsive therapy. Which response by the nurse is most appropriate? A) "I’ll go with you and will be there with you during the treatment." B) "You’ll be asleep and won’t remember anything." C) "You have the right to change your mind. You seem anxious. Can we talk about it?" D) "I’ll call the health care provider to notify them of your decision." C: This response indicates acknowledgment of the client’s rights and the opportunity for the client to clarify and ventilate concerns. After this, if the client continues to refuse, the provider should be notified. 61. A male client is admitted with a spinal cord injury at level C4. The client asks the nurse how the injury is going to affect his sexual function. The nurse would respond A) "Normal sexual function is not possible." B) "Sexual functioning will not be impaired at all." C) "Erections will be possible." D) "Ejaculation will be normal." C: "Erections will be possible." Because they are a reflex reaction, erections can be stimulated by stroking the genitalia. 62. An 82 year-old client complains of chronic constipation. To improve bowel function, the nurse should first suggest A) Increasing fiber intake to 20-30 grams daily B) Daily use of laxatives 55C) Avoidance of binding foods such as cheese and chocolate D) Monitoring a balance between activity and rest A: The incorporation of high fiber into the diet is an effective way to promote bowel elimination in the elderly. 63. The unlicensed assistive personnel (UAP) reports to the nurse that a client with cirrhosis who had a paracentesis yesterday has become more lethargic and has musty smelling breath. A critical assessment for increasing encephalopathy is A) monitor the client's clotting status B) assess upper abdomen for bruits C) assess for flap-like tremors of the hands D) measure abdominal girth changes C: assess for flap-like tremors of the hands. A client with cirrhosis of the liver who develops subtle changes in mental status and has a musty odor to the breath is at risk for developing more advanced signs of encephalopathy. 64. A client is admitted with a diagnosis of nodal bigeminy. The nurse knows that the atrioventricular (AV) node has an intrinsic rate of A) 60-100 beats/minute B) 10-30 beats/minute C) 40-70 beats/minute D) 20-50 beats/minute C: 40-70 beats/minute. The intrinsic rate of the AV node is within the range of 40-70 beats per minute. 65. A client is admitted for a possible pacemaker insertion. What is the intrinsic rate of the heart's own pacemaker? A) 30-50 beats/minute B) 60-100 beats/minute C) 20-60 beats/minute D) 90-100 beats/minute B: 60-100 beats/minute. This is the intrinsic rate of the SA node. 66. A client is diagnosed with gastroesophageal reflux disease (GERD). The nurse's instruction to the client regarding diet should be to A) avoid all raw fruits and vegetables B) increase intake of milk products C) decrease intake of fatty foods D) focus on 3 average size meals a day C: GERD may be aggravated by a fatty diet. A diet low in fat would decrease the symptoms of GERD. Other agents which should also be decreased or avoided are: cigarette smoking, caffeine, alcohol, chocolate, and meperidine (Demerol). 67. The nurse is teaching a client with chronic renal failure (CRF) about medications. The client questions the purpose of aluminum hydroxide (Amphojel) in her medication regimen. What is the best explanation for the nurse to give the client about the therapeutic effects of this medication? A) It decreases serum phosphate B) It will reduce serum calcium C) Amphojel increases urine output D) The drug is taken to control gastric acid secretion A: It decreases serum phosphate. Aluminum binds phosphates that tend to accumulate in the patient with chronic renal failure due to decreased filtration capacity of the kidney. Antacids such as Amphojel are commonly used to accomplish this. 68. The client with goiter is treated with potassium iodide preoperatively. What should the nurse recognize as the purpose of this medication? A) Reduce vascularity of the thyroid B) Correct chronic hyperthyroidism C) Destroy the thyroid gland function D) Balance enzymes and electrolytes A: Potassium iodide solution, or Lugol''s solution may be used preoperatively to reduce the size and vascularity of the thyroid gland. 69. A client with testicular cancer has had an orchiectomy. Prior to discharge the client expresses his fears related to his prognosis. Which principle should the nurse base the response on? A) Testicular cancer has a cure rate of 90% with early diagnosis B) Testicular cancer has a cure rate of 50% with early diagnosis C) Intensive chemotherapy is the treatment of choice D) Testicular cancer is usually fatal A: With aggressive treatment and early detection/diagnosis the cure rate is 90%. 70. The nurse is caring for clients over the age of 70. The nurse is aware that when giving medications to older clients, it is best to 56A) start low, go slow B) avoid stopping a medication entirely C) avoid drugs with side effects that impact cognition D) review the drug regimen yearly A: Due to physiological changes in the elderly, as well as conditions such as dehydration, hyperthermia, immobility and liver disease, the effective metabolism of drugs may decrease. As a result, drugs can accumulate to toxic levels and cause serious adverse reactions. 71. The nurse enters the room of a client diagnosed with COPD. The client’s skin is pink, and respirations are 8 per minute. The client’s oxygen is running at 6 liters per minute. What should be the nurse’s first action? A) Call the health care provider B) Put the client in Fowler’s position C) Lower the oxygen rate D) Take the vital signs C: In client’s diagnosed with COPD, the drive to breathe is hypoxia. If oxygen is delivered at too high of a concentration, this drive will be eliminated and the client’s depth and rate of respirations will decrease. Therefore the first action should be to lower the oxygen rate. 72. A client has an order for antibiotic therapy after hospital treatment of a staph infection. Which of the following should the nurse emphasize? A) Scheduling follow-up blood cultures B) Completing the full course of medications C) Visiting the provider in a few weeks D) Monitoring for signs of recurrent infection B: In order for antibiotic therapy to be effective in eradicating an infection, the client must compete the entire course of prescribed therapy. When findings subside, stopping the medication early may lead to recurrence or subsequent drug resistance. 73. A 55 year-old woman is taking Prednisone and aspirin (ASA) as part of her treatment for rheumatoid arthritis. Which of the following would be an appropriate intervention for the nurse? A) Assess the pulse rate q 4 hours B) Monitor her level of consciousness q shift C) Test her stools for occult blood D) Discuss fiber in the diet to prevent constipation C: Both Prednisone and ASA can lead to GI bleeding, therefore monitoring for occult blood would be appropriate. 74. A client is prescribed an inhaler. How should the nurse instruct the client to breathe in the medication? A) As quickly as possible B) As slowly as possible C) Deeply for 3-4 seconds D) Until hearing whistling by the spacer C: The client should be instructed to breath in the medication for 3-4 seconds in order to receive the correct dosage of medication. 75. After surgery, a client with a nasogastric tube complains of nausea. What action would the nurse take? A) Call the health care provider B) Administer an antiemetic C) Put the bed in Fowler’s position D) Check the patency of the tube D: Check the patency of the tube. An indication that the nasogastric tube is obstructed is a client’s complaint of nausea. Nasogastric tubes may become obstructed with mucus or sediment. 76. A 72 year-old client is admitted for possible dehydration. The nurse knows that older adults are particularly at risk for dehydration because they have A) an increased need for extravascular fluid B) a decreased sensation of thirst C) an increase in diaphoresis D) higher metabolic demands B: a decreased sensation of thirst. The elderly have a reduction in thirst sensation causing them to consume less fluid. Other risk factors may include fear of incontinence, inability to drink fluids independently and lack of motivation. 77. Upon admission to an intensive care unit, a client diagnosed with an acute myocardial infarction is ordered oxygen. The nurse knows that the major reason that oxygen is administered in this situation is to A) saturate the red blood cells B) relieve dyspnea 57C) decrease cyanosis D) increase oxygen level in the myocardium D: Anoxia of the myocardium occurs in myocardial infarction. Oxygen administration will help relieve dyspnea and cyanosis associated with the condition but the major purpose is to increase the oxygen concentration in the damaged myocardial tissue. 78. An arterial blood gases test (ABG) is ordered for a confused client. The respiratory therapist draws the blood and then asks the nurse to apply pressure to the area so the therapist can take the specimen to the lab. How long should the nurse apply pressure to the area? A) 3 minutes B) 5 minutes C) 8 minutes D) 10 minutes B: 5 minutes. It is necessary to apply pressure to the area for 5 minutes to prevent bleeding and the formation of hematomas. 79. A client receiving chemotherapy has developed sores in his mouth. He asks the nurse why this happened. What is the nurse’s best response? A) "It is a sign that the medication is working." B) "You need to have better oral hygiene." C) "The cells in the mouth are sensitive to the chemotherapy." D) "This always happens with chemotherapy." C: The epithelial cells in the mouth are very sensitive to chemotherapy due to their high rate of cell turnover. 80. A client with testicular cancer is scheduled for a right orchiectomy. The nurse knows that an orchiectomy is the A) surgical removal of the entire scrotum B) surgical removal of a testicle C) dissection of related lymph nodes D) partial surgical removal of the penis B: surgical removal of a testicle. The affected testicle is surgically removed along with its tunica and spermatic cord. Reduction of Risk Potential 1. The nurse is caring for a child immediately after surgical correction of a ventricular septal defect. Which of the following nursing assessments should be a priority? A) Blanch nail beds for color and refill B) Assess for post-operative arrhythmias C) Auscultate for pulmonary congestion D) Monitor equality of peripheral pulses B: Assess for post-operative arrhythmias. The atrioventricular bundle (bundle of His), a part of the electrical conduction system of the heart, extends from the atrioventricular node along each side of the interventricular septum and then divides into right and left bundle branches. Surgical repair of a ventricular septal defect consists of a purse-string approach or a patch sewn over the opening. 2. A client is receiving external beam radiation to the mediastinum for treatment of bronchial cancer. Addressing which of the following should take priority in planning care? A) Esophagitis B) Leukopenia C) Fatigue D) Skin irritation B: Leukopenia. Clients develop leukopenia due to the depressant effect of radiation therapy on bone marrow function. Infection is the most frequent cause of morbidity and death in clients with cancer. 3. A nurse is to collect a sputum specimen for acid-fast bacillus (AFB) from a client. Which action should the nurse take first? A) Ask client to cough sputum into container B) Have the client take several deep breaths C) Provide a appropriate specimen container D) Assist with oral hygiene D: Assist with oral hygiene. Obtain a specimen early in the morning after mouth care. The other responses follow this first action: the client should take several deep breaths then cough into the appropriate sterile container to obtain the AFB specimen of the sputum. 584. A client has a history of chronic obstructive pulmonary disease (COPD). As the nurse enters the client's room, his oxygen is running at 6 liters per minute, his color is flushed and his respirations are 8 per minute. What should the nurse do first? A) Obtain a 12-lead EKG B) Place client in high Fowler's position C) Lower the oxygen rate D) Take baseline vital signs C: Lower the oxygen rate. A low oxygen level acts as a stimulus for respiration. A high concentration of supplemental oxygen removes the hypoxic drive to breathe, leading to increased hypoventilation, respiratory decompensation, and the development of or worsening of respiratory acidosis. Unless corrected, it can lead to the client''s death. 5. A 4 year-old has been hospitalized for 24 hours with skeletal traction for treatment of a fracture of the right femur. The nurse finds that the child is now crying and the right foot is pale with the absence of a pulse. What should the nurse do first? A) Notify the health care provider B) Readjust the traction C) Administer the ordered prn medication D) Reassess the foot in fifteen minutes A: Notify the health care provider. The findings are indicative of circulatory impairment. The health care provider (or practitioner) must be notified immediately. 6. A nurse checks a client who is on a volume-cycled ventilator. Which finding indicates that the client may need suctioning? A) Drowsiness B) Complaint of nausea C) Pulse rate of 82 D) Restlessness D: Restlessness. Restlessness, increased heart and respiratory rates, and noisy expiration suggest hypoxia and are indications for suctioning. 7. A client has returned from a cardiac catheterization. Which one of the following findings would indicate the client is experiencing a complication from the procedure? A) Increased blood pressure B) Increased heart rate C) Loss of pulse in the extremity D) Decreased urine output C: Loss of pulse in the extremity. Loss of the pulse in the extremity would indicate impaired circulation. 8. The nurse is assessing a client 2 hours postoperatively after a femoral popliteal bypass. The upper leg dressing becomes saturated with blood. The nurse's first action should be to A) wrap the leg with elastic bandages B) apply pressure at the bleeding site C) reinforce the dressing and elevate the leg D) remove the dressings and re-dress the incision C: The interventions that must be taken are: reinforce the dressing, elevate the extremity to decrease blood flow into the extremity and thus decrease bleeding, and call the provider immediately. This is an emergency post surgical situation. 9. The most effective nursing intervention to prevent atelectasis from developing in a post-operative client is to A) maintain adequate hydration B) assist client to turn, deep breathe, and cough C) ambulate client within 12 hours D) splint incision B: assist client to turn, deep breathe, and cough. Deep air excursion by turning, deep breathing, and coughing will expand the lungs and stimulate surfactant production. The nurse should instruct the client on how to splint the chest when coughing. Humidification, hydration and nutrition all play a part in preventing atelectasis following surgery. 10. The nurse is reviewing laboratory results on a client with acute renal failure. Which one of the following should be reported immediately? A) Blood urea nitrogen 50 mg/dl B) Hemoglobin of 10.3 mg/dl C) Venous blood pH 7.30 D) Serum potassium 6 mEq/L D: Serum potassium 6 mEq/L. Although all of these findings are abnormal, the elevated potassium level is a life threatening finding and must be reported immediately. 5911. The nurse is caring for a client undergoing the placement of a central venous catheter line. Which of the following would require the nurse’s immediate attention? A) Pallor B) Increased temperature C) Dyspnea D) Involuntary muscle spasms C: Dyspnea. Client’s having the insertion of a central venous catheter are at risk for tension pneumothorax. Dyspnea, shortness of breath and chest pain are indications of this complication. 12. The nurse is caring for a client who requires a mechanical ventilator for breathing. The high pressure alarm goes off on the ventilator. What is the first action the nurse should perform? A) Disconnect the client from the ventilator and use a manual resuscitation bag B) Perform a quick assessment of the client's condition C) Call the respiratory therapist for help D) Press the alarm re-set button on the ventilator B: A number of situations can cause the high pressure alarm to sound. It can be as simple as the client coughing. A quick assessment of the client will alert the nurse to whether it is a more serious or complex situation that might then require using a manual resuscitation bag and calling the respiratory therapist. 13. A 60 year-old male client had a hernia repair in an outpatient surgery clinic. He is awake and alert, but has not been able to void since he returned from surgery 6 hours ago. He received 1000 mL of IV fluid. Which action would be most likely to help him void? A) Have him drink several glasses of water B) Perform Credé's method on the bladder from the bottom to the top C) Assist him to stand by the side of the bed to void D) Wait 2 hours and have him try to void again C: When a male is not able to use a urinal unassisted, the client should stand by the side of the bed to void. This is the most desirable position for normal voiding for male clients. Also, given his age, he most likely has some degree of prostate enlargement which may interfere with voiding. 14. The provider order reads "Aspirate nasogastric (NG) feeding tube every 4 hours and check pH of aspirate." The pH of the aspirate is 10. Which action should the nurse take? A) Hold the tube feeding and notify the provider B) Administer the tube feeding as scheduled C) Irrigate the tube with diet cola soda D) Apply intermittent suction to the feeding tube A: Hold the tube feeding and notify the provider. A pH of less than 4 indicates that the tube is appropriately placed in the stomach, a highly acidic environment. A pH higher than 4 (alkaline pH) indicates intestinal placement. 15. When caring for a client with a post-right thoracotomy who has undergone an upper lobectomy, the nurse focuses on pain management to promote A) relaxation and sleep B) deep breathing and coughing C) incisional healing D) range of motion exercises B: The priority is preventing postoperative respiratory complications. This client will quickly develop profound atelectasis and eventually pneumonia without adequate gas exchange. Client compliance with recommended deep breathing and coughing exercises will only be achieved with the appropriate pain management. 16. A client is diagnosed with a spontaneous pneumothorax necessitating the insertion of a chest tube. What is the best explanation for the nurse to provide this client? A) "The tube will drain fluid from your chest." B) "The tube will remove excess air from your chest." C) "The tube controls the amount of air that enters your chest." D) "The tube will seal the hole in your lung." B: The purpose of the chest tube is to create negative pressure and remove the air that has accumulated in the pleural space. 17. To prevent unnecessary hypoxia during suctioning of a tracheostomy, the nurse must A) apply suction for no more than 10 seconds B) maintain sterile technique C) lubricate 3 to 4 inches of the catheter tip D) withdraw catheter in a circular motion A: Applying suction for more than 10 seconds may result in hypoxia. Although options B, C, and D are important in during suctioning a tracheostomy, hypoxia results from actions that decrease the oxygen supply. 6018. A client has a chest tube inserted following a left lower lobectomy required by a stab wound to the chest. While repositioning the client, the nurse notices 200 cc of dark, red fluid flows into the collection chamber of the chest drain. What is the most appropriate nursing action? A) Clamp the chest tube B) Call the surgeon immediately C) Prepare for blood transfusion D) Continue to monitor the rate of drainage D: It is not unusual for blood to collect in the chest and be released into the chest drain when the client changes position. The dark color of the blood indicates it is not fresh bleeding inside the chest. 19. The nurse is preparing a client who will undergo a myelogram. Which of the following statements by the client indicates a contraindication for this test? A) "I can't lie in one position for more than thirty minutes." B) "I am allergic to shrimp." C) "I suffer from claustrophobia." D) "I developed a severe headache after a spinal tap." B: "I am allergic to shrimp." A client undergoing myelography should be questioned carefully about allergies to iodine and iodine-containing substances such as seafood. An allergy to iodine or seafood may indicate sensitivity to the radiopaque contrast agent used in the test. An allergic reaction could even include seizures. 20. The nurse is performing a physical assessment on a client who just had an endotracheal tube (ET) inserted. Which finding would call for immediate action by the nurse? A) Breath sounds can be heard bilaterally B) Mist is visible in the T-Piece C) Pulse oximetry of 88 BPM D) Client is unable to speak C: Pulse oximetry of 88 BPM. Pulse oximetry should not be lower than 90. Placement of the ET will need to be checked, along with the ventilator settings. Physiological Adaptation 1. A man diagnosed with epididymitis 2 days ago calls the nurse at a health clinic to discuss the problem. What information is most important for the nurse to ask about at this time? A) "What are you taking for pain and does it provide total relief?" B) "Did your provider recommend that you be tested for Chlamydia?" C) "Do you have any questions about your care?" D) "Did you know a consequence of epididymitis is infertility?" B: "Did your provider recommend that you be tested for Chlamydia?" Epididymitis can result from Chlamydia infection, in which case the client’s sexual partners should be tested as well. All of the questions should be asked, however, determining the reason for the client’s referral is the most important to start with. 2. A client with heart failure has a prescription for Digoxin. The nurse is aware that sufficient potassium should be included in the diet because hypokalemia in combination with this medication A) can predispose to dysrhythmias B) may lead to oliguria C) may cause irritability and anxiety D) sometimes alters consciousness A: can predispose to dysrhythmias. The nurse should be aware of a decrease in the client’s potassium levels because low potassium can enhance the effects of digoxin and predispose the client to dysrhythmias. The other options are seen in hyperkalemia. Muscle weakness occurs in both hyperkalemia and hypokalemia. 3. A client has altered renal function and is being treated at home. The nurse recognizes that the most accurate indicator of fluid balance during the weekly visits is A) difference in the intake and output B) changes in the mucous membranes 61C) skin turgor D) weekly weight D: weekly weight. The most accurate indicator of fluid balance in an acutely ill individual is the daily weight. A one-kilogram or 2.2 pounds of weight gain is equal to approximately 1,000 ml of retained fluid. Other options are considered as part of data collection, but they are not the most accurate indicators of fluid balance. 4. A nurse is performing CPR on an adult who went into cardiopulmonary arrest. Another nurse enters the room in response to the call. After checking the client’s pulse and respirations, what should be the function of the second nurse? A) Relieve the nurse performing CPR B) Go get the code cart C) Participate with the compressions or breathing D) Validate the client's advanced directive C: Participate with the compressions or breathing. Once CPR is started, it is to be continued using the approved technique until such time as a provider pronounces the client dead or the client becomes stable. American Heart Association studies have shown that the 2 person technique is most effective in sustaining the client. It is not appropriate to relieve the first nurse to leave the room for equipment. The client’s advanced directives should have been filed on admission and his choices known prior to the initiation of CPR. 5. Which these findings would the nurse more closely associate with anemia in a 10 month-old infant? A) hemoglobin level of 12 g/dL B) pale mucosa of the eyelids and lips C) hypoactivity D) a heart rate between 80 and 130 B: pale mucosa of the eyelids and lips. In iron-deficiency anemia, the physical exam reveals a pale, tired-appearing infant with mild to severe tachycardia. 6. An elderly client admitted after a fall begins to seize and loses consciousness. What action by the nurse is appropriate to do next? A) Stay with client and observe for airway obstruction B) Collect pillows and pad the side rails of the bed C) Place an oral airway in the mouth and suction D) Announce a cardiac arrest, and assist with intubation A: Stay with client and observe for airway obstruction. For the client’s safety, remain at the bedside and observe respirations and level of consciousness. Prepare to clear the airway if obstructed. Do not place anything in the client’s mouth. For safety, do not leave the client unattended. A cardiac arrest should only be announced if pulse or respirations are absent after the seizure 7. Which of these statements from clients who call the community health clinic would suggest the need for a same-day appointment to be seen by the health care provider? A) "I started my period and now my urine has turned bright red" B) "I am an diabetic and today I have been going to the bathroom every hour" C) "I was started on medicine yesterday for a urine infection. Now my lower belly hurts when I go to the bathroom" D) "I went to the bathroom and my urine looked very red and it didn’t hurt when I went" D: With this description of symptoms this client needs to be seen that day since painless gross hematuria is closely associated with bladder cancer. The other complaints can be handled over the phone. 8. A 14 year-old with a history of sickle cell disease is admitted to the hospital with a diagnosis of vaso-occlusive crisis. Which statements by the client would be most indicative of the etiology of this crisis? A) "I knew this would happen. I've been eating too much red meat lately." B) "I really enjoyed my fishing trip yesterday. I caught two fish." C) "I have really been working hard practicing with the debate team at school." D) "I went to get a cold checked out last week, and I have gotten worse." D: "I went to get a cold checked out last week, and I have gotten worse." Any condition that increases the body''s need for oxygen or alters the transport of oxygen, such as infection, trauma or dehydration may result in a sickle cell crisis. 9. The nurse assesses a 72 year-old client who was admitted for right-sided congestive heart failure. Which of the following would the nurse anticipate finding? A) Decreased urinary output B) Jugular vein distention C) Pleural effusion D) Bibasilar crackles B: Signs of right-sided heart failure include jugular vein distention, ascites, nausea, and vomiting. 10. The nurse is caring for a client in atrial fibrillation. The atrial heart rate is 250 and the ventricular rate is controlled at 75. Which of the following findings is cause for the most concern? A) Diminished bowel sounds 62B) Loss of appetite C) A cold, pale lower leg D) Tachypnea C: A cold, pale lower leg. This assessment suggests the presence of an embolus probably from the atrial fibrillation. Peripheral pulses should be checked immediately. 11. A client is admitted with a tentative diagnosis of congestive heart failure. Which of the following assessments would the nurse expect to be consistent with this problem? A) Chest pain B) Pallor C) Inspiratory crackles D) Heart murmur C: Inspiratory crackles. In congestive heart failure, fluid backs up into the lungs (creating crackles) as a result of inefficient cardiac pumping. 12. A client is admitted for first and second degree burns on the face, neck, anterior chest and hands. The nurse's priority should be to A) cover the areas with dry sterile dressings B) assess for dyspnea or stridor C) initiate intravenous therapy D) administer pain medication B: assess for dyspnea or stridor. Due to the location of the burns, the client is at risk for developing upper airway edema and subsequent respiratory distress. 13. A client with pneumococcal pneumonia was started on antibiotics 16 hours ago. During the nurse’s initial evening rounds the nurse notices a foul smell in the room. The client makes all of these statements during their conversation. Which one would alert the nurse to a complication? A) "I have a sharp pain in my chest when I take a breath." B) "I have been coughing up foul-tasting, brown, thick sputum." C) "I have been sweating all day." D) "I feel hot off and on." B:Foul smelling and tasting sputum signals a risk of a lung abscess. This puts the client is grave danger since abscesses are often caused by anaerobic organisms. This client most likely would need a change of antibiotics. Sharp chest pain on inspiration called pleuritic pain is an expected finding with this type of pneumonia. The other options are expected in the initial 24 to 48 hours of therapy for infections. 14. Which information is a priority for the nurse to reinforce to an older client after intravenous pyelography? A) Eat a light diet for the rest of the day B) Rest for the next 24 hours since the preparation and the test is tiring C) During waking hours drink at least 1 8-ounce glass of fluid every hour for the next 2 days D) Measure the urine output for the next day and immediately notify the health care provider if it should decrease D: This information would alert to the complication of acute renal failure which may occur as a complication from the dye and the procedure. Renal failure occurs most often in elderly patients who are chronically dehydrated before the dye injection. 15. A nurse is providing care to a 17 year-old client in the post-operative care unit (PACU) after an emergency appendectomy. Which finding is an early indication that the client is experiencing poor oxygenation? A) Abnormal breath sounds B) Cyanosis of the lips C) Increasing pulse rate D) Pulse oximeter reading of 92% C: The earliest sign of poor oxygenation is an increasing pulse rate as a part of the body’s compensatory mechanism. Abnormal breath sounds and cyanosis are late signs of poor oxygenation. A pulse oximetry reading of 92% is normal. 16. A nurse is observing a client during an excretory urogram. Which of these observations indicate a complication is occurring? A) "The client complains of a salty taste in the mouth when the dye is injected." B) "The client’s entire body turns a bright red color. C) "The client states “I have a feeling of getting warm.” D) "The client gags and complains “I am getting sick.” B: "The client’s entire body turns a bright red color. This observation suggest anaphylaxis which results in massive vasodilation. Other findings would be immediate wheezing and/or respiratory arrest. 17. The nurse is assessing an 8 month-old child with atonic cerebral palsy. Which statement from the parent supports the presence of this problem? 63A) "When I put my finger in the left hand the baby doesn’t respond with a grasp." B) "My baby doesn’t seem to follow when I shake toys in front of its face." C) "When it thundered loudly last night the baby didn’t even jump." D) "When I put the baby in a back lying position that’s how I find it hours later." D: "When I put the baby in a back lying position that’s how I find it hours later." Cerebral palsy is known as a condition whereby motor dysfunction occurs secondary to damage in the motor centers of the brain. Inability to roll over by 8 months of age would illustrate one delay in the infant''s attainment of developmental milestones. 18. A client who is to have antineoplastic chemotherapy tells the nurses of a fear of being sick all the time and indicates a wish to try acupuncture. Which of these beliefs stated by the client would be incorrect about acupuncture? A) "Some needles go as deep as 3 inches, depending on where they're placed in the body and what the treatment is for. The needles usually are left in for 15 to 30 minutes." B) "In traditional Chinese medicine, imbalances in the basic energetic flow of life — known as qi or chi — are thought to cause illness." C) "The flow of life is believed to flow through major pathways called nerve clusters in your body." D) "By inserting extremely fine needles into some of the over 400 acupuncture points in various combinations it is believed that energy flow will rebalance to allow the body's natural healing mechanisms to take over." C: The major pathways are called meridians, not nerve clusters. 19. A primigravida in the third trimester is hospitalized for preeclampsia. The nurse determines that the client’s blood pressure is increasing. Which action should the nurse take first? A) Check the protein level in urine B) Have the client turn to the left side C) Take the temperature D) Monitor the urine output B: A priority action is to turn the client to the left side to decrease pressure on the vena cava and promote adequate circulation to the placenta and kidneys. Urine protein level and output should be checked with each voiding. Temperature should be monitored every 4 hours or more often if indicated, but no data in the stem supports a check of temperature. 20. A client has viral pneumonia affecting 2/3 of the right lung. What would be the best position to teach the client to lie in every other hour during first 12 hours after admission? A) Side-lying on the left with the head elevated 10 degrees B) Side-lying on the left with the head elevated 35 degrees C) Side-lying on the right with the head elevated 10 degrees D) Side-lying on the right with the head elevated 35 degrees A: Side-lying on the left with the head elevated 10 degrees. Gravity will draw the most blood flow to the dependent portion of the lung. For unilateral chest disease, it is best to place the healthiest part of the lung in the dependent position to enhance blood flow to the area where gas exchange will be best. Ventilation would be minimally affected in the right dependent lung. This position also enhances the drainage of the infected part of the lung. A head elevation of 35 degrees is counterproductive to therapeutic blood flow and the drainage of secretions. 21. The nurse is caring for a client in hypertensive crisis in an intensive care unit. The priority assessment in the first hour of care is A) heart rate B) pedal pulses C) lung sounds D) pupil responses D: pupil responses. The organ most susceptible to damage in hypertensive crisis is the brain due to rupture of the cerebral blood vessels. Neurologic status must be closely monitored. 22. The nurse is performing an assessment on a client in congestive heart failure. Auscultation of the heart is most likely to reveal A) S3 ventricular gallop B) apical click C) systolic murmur D) split S2 A: S3 ventricular gallop. An S3 ventricular gallop is caused by blood flowing rapidly into a distended non-compliant ventricle. This is most common with congestive heart failure. 23. A 2 year-old child is brought to the emergency department at 2:00 in the afternoon. The mother states: “My child has not had a wet diaper all day.” The nurse finds the child is pale with a heart rate of 132. What assessment data should the nurse obtain next? A) Status of the eyes and the tongue B) Description of play activity C) History of fluid intake 64D) Dietary patterns A: Status of the eyes and the tongue. Clinical findings of dehydration include sunken eyes, dry tongue, lethargy, irritability, dry skin, decreased play activity, and increased pulse. The normal pulse rate in this age child is 70-110. 24. Which of these clients who are all in the terminal stage of cancer is least appropriate to suggest the use of patient controlled analgesia (PCA) with a pump? A) A young adult with a history of Down syndrome B) A teenager who reads at a 4th grade level C) An elderly client with numerous arthritic nodules on the hands D) A preschooler with intermittent episodes of alertness D: A preschooler with intermittent episodes of alertness. A preschooler is most likely of these clients to have difficulty with the use or understanding of a PCA pump. This very young child lacking a normal level of consciousness would not benefit from the use of a PCA pump. 25. The client with infective endocarditis must be assessed frequently by the home health nurse. Which finding suggests that antibiotic therapy is not effective, and must be reported by the nurse immediately to the provider? A) nausea and vomiting B) fever of 103 degrees Fahrenheit (39.5 degrees Celsius) C) diffuse macular rash D) muscle tenderness B: fever of 103 degrees Fahrenheit (39.5 degrees Celsius). Persistent, prolonged fever may be an indication that the antibiotics are not effective and may need to be changed. 26. The nurse is caring for a client with uncontrolled hypertension. Which findings require immediate nursing action? A) lower extremity pitting edema B) rales C) jugular vein distension D) weakness in left arm D: weakness in left arm. In a client with hypertension, weakness in the extremities is a sign of cerebral involvement with the potential for cerebral infarction or stroke. Cerebral infarctions account for about 80% of the strokes in clients with hypertension. The remaining 3 choices indicate mild fluid overload and are not medical emergencies. 27. A client has had heart failure. Which intervention is most important for the nurse to implement prior to the initial administration of digoxin to this client? A) Assess the apical pulse, counting for a full 60 seconds B) Take a radial pulse, counting for a full 60 seconds C) Use the pulse reading from the electronic blood pressure device D) Check for a pulse deficit A: Assess the apical pulse, counting for a full 60 seconds. It is the nurse’s responsibility to take the client’s pulse before administering digoxin. The correct technique for taking an apical pulse is to use the stethoscope and listen for a full 60 seconds. Digoxin is held for a pulse below 60 beats per minute. A radial pulse, potentially less accurate, or blood pressure are not part of the initial assessment before administering an initial dose of digoxin. 28. A client has been diagnosed with Zollinger-Ellison syndrome. Which information is most important for the nurse to reinforce? A) It is a condition in which one or more tumors called gastrinomas form in the pancreas or in the upper part of the small intestine (duodenum) B) It is critical to report promptly to your health care provider any findings of peptic ulcers C) Treatment consists of medications to reduce acid and heal any peptic ulcers and, if possible, surgery to remove any tumors D) With the average age at diagnosis at 50 years the peptic ulcers may occur at unusual areas of the stomach or intestine B: It is critical to report promptly to your health care provider any findings of peptic ulcers. Such findings include night-time awakening with burning, cramp-like abdominal pain, vomiting and even hematemesis, and change in appetite. Abdominal pain, rigidity and tenderness can signal perforation of the ulcer and should be reported to the provider immediately. Zollinger-Ellison syndrome can occur in both children and adults. 29. As the nurse is speaking with a group of teens, which of these side effects of chemotherapy for cancer would the nurse expect this group to be more interested in during the discussion? A) Mouth sores B) Fatigue C) Diarrhea D) Hair loss D: Hair loss. The major concern for adolescence is body image, so hair loss would be the most disturbing. 30. The nurse is discussing Kawasaki disease with a group of students. What statement made by a student about Kawasaki disease is incorrect? 65A) "It also called mucocutaneous lymph node syndrome because it affects the mucous membranes (inside the mouth, throat and nose), skin and lymph nodes." B) "In the second phase of the disease, findings include peeling of the skin on the hands and feet with joint and abdominal pain." C) "Kawasaki disease occurs most often in boys, children younger than age 5 and children of Hispanic descent." D) "Initially findings are a sudden high fever, usually above 104 degrees Fahrenheit, which lasts 1 to 2 weeks." C: Kawasaki disease occurs most often in boys, children younger than age 5 and children of Asian descent, particularly Japanese. Other findings in the initial phase are extremely red eyes (conjunctivitis), a rash on the main part of the body (trunk) and in the genital area, red, dry, cracked lips; a red, swollen tongue resembling a strawberry; swollen, red skin on the palms of the hands and the soles of the feet; swollen lymph nodes in the neck. Fever reduction signals the second phase, when the findings slowly go away. In the third phase findings, except for abnormal lab values, are gone unless complications associated with the heart develop. The disease lasts from 2 to 12 weeks without treatment. With treatment, the child usually improves within 24 hours. The cause of Kawasaki disease is not known. 31. The nurse is about to assess a 6 month-old child with non-organic failure-to-thrive (NOFTT). Upon entering the room, the nurse would expect the baby to be A) irritable and "colicky," making no attempts to pull to standing B) alert, laughing, playing with a rattle, and sitting with support C) dusky in color with poor skin turgor over abdomen D) pale, have thin arms and legs, and uninterested in surroundings D: pale, have thin arms and legs, and uninterested in surroundings. Diagnosis of NOFTT is made on anthropomorphic findings documenting growth retardation which would lead the nurse to expect muscle-wasting and paleness. In cases of NOFTT, the cause may be a variety of psychosocial factors and these children may be below normal in intellectual development, language and social interactions. 32. A client who was medicated with meperidine hydrochloride (Demerol) 100 mg and hydroxyzine hydrochloride (Vistaril Intramuscular) 50 mg IM for pain related to a fractured lower right leg 1 hour ago reports that the pain is getting worse. The nurse should recognize that the client may be developing which complication? A) acute compartment syndrome B) thromboembolitic complications C) fatty embolism D) osteomyelitis A: acute compartment syndrome. Increasing pain that is not relieved by narcotic analgesics is an indication of compartment syndrome after a bone fracture and requires immediate action by the nurse. Thromboembolic complications include deep vein thrombosis and pulmonary embolism which are not characterized by increasing pain at the site of injury. Both pulmonary embolism and fat embolism present with respiratory findings. Osteomyelitis is a bone infection which could occur some time after the initial injury, usually at least 48 to 72 hours. 33. Which statements by the client would indicate to the nurse an understanding of the issues with end stage renal disease? A) "I have to go at intervals for epoetin (Procrit) injections at the health department." B) "I know I have a high risk of clot formation since my blood is thick from too many red cells." C) "I expect to have periods of little water with voiding and then sometimes to have a lot of water." D) "My bones will be stronger with this disease since I will have higher calcium than normal." A: Anemia caused by reduced endogenous erythropoietin production, primarily end-stage renal disease is treated with subcutaneous injections of Procrit or Epogen to stimulate the bone marrow to produce red blood cells. 34. While caring for a client who was admitted with myocardial infarction (MI) 2 days ago, the nurse notes today's temperature is 101.1 degrees Fahrenheit (38.5 degrees Celsius). The appropriate nursing intervention is to A) call the health care provider immediately B) administer acetaminophen as ordered as this is normal at this time C) send blood, urine and sputum for culture D) increase the client's fluid intake B: Leukocytosis and fever are common starting on day 2 because of the inflammatory process associated with an acute MI. Nursing interventions should focus on promoting comfort. 35. A nurse is providing care to a primigravida whose membranes spontaneously ruptured (ROM) 4 hours ago. Labor is to be induced. At the time of the ROM, the vital signs were T-99.8 degrees Fahrenheit, P-84, R-20, BP-130/78, and fetal heart tones (FHT) 148 beats/min. Which assessment findings may be an early indication that the client is developing a complication of labor? A) FHT 168 beats/min B) Temperature 100 degrees Fahrenheit C) Cervical dilation of 4 cm D) BP 138/88 A: An increase in FHT may indicate maternal infection. The other assessment findings are normal. 36. A client who had a vasectomy is in the post recovery unit at an outpatient clinic. Which of these points is most important to be reinforced by the nurse? 66A) "Until the health care provider has determined that your ejaculate doesn't contain sperm, continue to use another form of contraception." B) "This procedure doesn't impede the production of male hormones or the production of sperm in the testicles. The sperm can no longer enter your semen and no sperm are in your ejaculate." C) "After your vasectomy, strenuous activity needs to be avoided for at least 48 hours. If your work doesn't involve hard physical labor, you can return to your job as soon as you feel to it. The stitches generally dissolve in 7-10 days." D) "The health care provider at this clinic recommends rest, ice, an athletic supporter or over-the-counter pain medication to relieve any discomfort." A: All of these options are correct information. The most important point to reinforce is the continuing need to take additional action for birth control. 37. A female client talks to the nurse in the provider’s office about uterine fibroids, also called leiomyomas or myomas. What statement by the woman indicates more education is needed? A) "I am the one out of every 4 women that get fibroids, and of women my age – between the 30s or 40s, fibroids occur more frequently." B) "My fibroids are noncancerous tumors that grow slowly." C) "My associated problems I have had are pelvic pressure and pain, urinary incontinence,and constipation." D) "Fibroids that cause no problems still need to be taken out." D: Fibroids that cause no findings may require only "watchful waiting" with no treatment. Only when the client’s findings become disturbing to them would surgical interventions be considered. 38. A client has an indwelling catheter with continuous bladder irrigation after undergoing a transurethral resection of the prostate (TURP) 12 hours ago. Which finding at this time should be reported to the health care provider? A) light, pink urine B) occasional suprapubic cramping C) minimal drainage into the urinary collection bag D) reports of the feeling of pulling on the urinary catheter C: Options A, B, and D are expected complaints after this procedure. Option C needs to be reported immediately since minimal urinary drainage puts the client at risk for bladder rupture. The flow rate of the continuous irrigation would need to be slowed until the provider is notified. If an order to irrigate the system is written, sterile technique would be used. 39. Which order can be associated with the prevention of atelectasis and pneumonia in a client with amyotrophic lateral sclerosis (ALS)? A) Active and passive range of motion exercises twice a day B) Use incentive spirometer every 4 hours C) Chest physiotherapy twice a day D) Repositioning every 2 hours around the clock C: Chest physiotherapy twice a day. These clients have potential inability to have voluntary and involuntary muscle movement or activity. Thus, options A and B may not be feasible for the immobilized client. Option D is not specific for prevention of complications associated with the lung. 40. A nurse assesses a young adult in the emergency room following a motor vehicle accident. Which of the following neurological signs is of most concern? A) Flaccid paralysis B) Pupils fixed and dilated C) Diminished spinal reflexes D) Reduced sensory responses B: Pupils fixed and dilated. Pupils that are fixed and dilated indicate overwhelming injury and intrinsic damage to the upper brain stem. It is a poor prognostic sign. 67Q&A Random Selection #1 1. An older adult client is to receive and antibiotic, gentamicin. What diagnostic finding indicates the client may have difficult excreting the medication? A) High gastric pH B) High serum creatinine C) Low serum albumin D) Low serum blood urea nitrogen B: High serum creatinine. An elevated serum creatinine indicates reduced renal function. Reduced renal function will delay the excretion of many medications. 2. A client is admitted to the hospital with findings of liver failure with ascites. The health care provider orders spironolactone (Aldactone). What is the pharmacological effect of this medication? A) Promotes sodium and chloride excretion B) Increases aldosterone levels C) Depletes potassium reserves D) Combines safely with antihypertensives A: Promotes sodium and chloride excretion. Spironolactone promotes sodium and chloride excretion while sparing potassium and decreasing aldosterone levels. It had no effect on ammonia levels. 3. A client with tuberculosis is started on Rifampin. Which one of the following statements by the nurse would be appropriate to include in teaching? "You may notice: A) an orange-red color to your urine." 68B) your appetite may increase for the first week.” C) it is common to experience occasional sleep disturbances." D) if you take the medication with food, you may have nausea." A: an orange-red color to your urine." Discoloration of the urine and other body fluids may occur. It is a harmless response to the drug, but the patient needs to be aware it may happen. 4. The nurse has just received report on a group of clients and plans to delegate care of several of the clients to a practical nurse (PN). The first thing the RN should do before the delegation of care is A) Provide a time-frame for the completion of the client care B) Assure the PN that the RN will be available for assistance C) Ask about prior experience with similar clients D) Review the specific procedures unique to the assignment C: Ask about prior experience with similar clients. The first step in delegation is to determine the qualifications of the person to whom one is delegating. By asking about the PN''s prior experience with similar clients/tasks, the RN can determine whether the PN has the requisite experience to care for the assigned clients. 5. Which of the following assessments by the nurse would indicate that the client is having a possible adverse response to the isoniazid (INH)? A) Severe headache B) Appearance of jaundice C) Tachycardia D) Decreased hearing B: Appearance of jaundice. Clients receiving INH therapy are at risk for developing drug induced hepatitis. The appearance of jaundice may indicate that the client has liver damage. 6. The nurse is caring for a client who is 4 days post-op for a transverse colostomy. The client is ready for discharge and asks the nurse to empty his colostomy pouch. What is the best response by the nurse? A) "You should be emptying the pouch yourself." B) "Let me demonstrate to you how to empty the pouch." C) "What have you learned about emptying your pouch?" D) "Show me what you have learned about emptying your pouch." D: Most adult learners obtain skills by participating in the activities. Anxiety about discharge can be causing the client to forget that they have mastered the skill of emptying the pouch. The client should show the nurse how the pouch is emptied. 7. A post-operative client is admitted to the post-anesthesia recovery room (PACU). The anesthetist reports that malignant hyperthermia occurred during surgery. The nurse recognizes that this complication is related to what factor? A) Allergy to general anesthesia B) Pre-existing bacterial infection C) A genetic predisposition D) Selected surgical procedures C: A genetic predisposition. Malignant hyperthermia is a rare, potentially fatal adverse reaction to inhaled anesthetics. There is a genetic predisposition to this disorder. 8. Which of the following laboratory results would suggest to the emergency room nurse that a client admitted after a severe motor vehicle crash is in acidosis? A) Hemoglobin 15 gm/dl B) Chloride 100 mEq/L C) Sodium 130 mEq/L D) Carbon dioxide 20 mEq/L D: Carbon dioxide 20 mEq/L. Serum carbon dioxide is an indicator of acid-base status. This finding would indicate acidosis. 9. The nurse is teaching a school-aged child and family about the use of inhalers prescribed for asthma. What is the best way to evaluate effectiveness of the treatments? A) Rely on child's self-report B) Use a peak-flow meter C) Note skin color changes D) Monitor pulse rate B: Use a peak-flow meter. The peak flowmeter, if used correctly, shows effectiveness of inhalants. 10. The nurse is providing care to a newly a hospitalized adolescent. What is the major threat experienced by the hospitalized adolescent? A) Pain management B) Restricted physical activity C) Altered body image D) Separation from family 69C: Altered body image. The hospitalized adolescent may see each of these as a threat, but the major threat that they feel when hospitalized is the fear of altered body image, because of the emphasis on physical appearance during this developmental stage. 11. A client on telemetry begins having premature ventricular beats (PVBs) at 12 per minute. In reviewing the most recent laboratory results, which would require immediate action by the nurse? A) Calcium 9 mg/dl B) Magnesium 2.5 mg/dl C) Potassium 2.5 mEq/L D) PTT 70 seconds C: Potassium 2.5 mEq/L. The patient is at risk for ventricular dysrhythmias when the potassium level is low. 12. A client has just been diagnosed with breast cancer. The nurse enters the room and the client tells the nurse that she is stupid. What is the most therapeutic response by the nurse? A) Explore what is going on with the client B) Accept the client’s statement without comment C) Tell the client that the comment is inappropriate D) Leave the client's room A: Explore what is going on with the client. Exploring feelings with the verbally aggressive client helps to put angry feelings into words and then to engage in problem solving. 13. A 12 year-old child is admitted with a broken arm and is told surgery is required. The nurse finds him crying and unwilling to talk. What is the most appropriate response by the nurse? A) Give him privacy B) Tell him he will get through the surgery with no problem C) Try to distract him D) Make arrangements for his friends to visit A: Give him privacy. A 12 year-old child needs the opportunity to express his emotions privately. 14. A nurse is assigned to care for a comatose diabetic on IV insulin therapy. Which task would be most appropriate to delegate to an unlicensed assistive personnel (UAP)? A) Check the client's level of consciousness B) Obtain the regular blood glucose readings C) Determine if special skin care is needed D) Answer questions from the client's spouse about the plan of care B: Obtain the regular blood glucose readings. The UAP can safely obtain blood glucose readings, which are routine tasks. 15. The clinic nurse is discussing health promotion with a group of parents. A mother is concerned about Reye's Syndrome, and asks about prevention. Which of these demonstrates appropriate teaching? A) "Immunize your child against this disease." B) "Seek medical attention for serious injuries." C) "Report exposure to this illness." D) "Avoid use of aspirin for viral infections." D: "Avoid use of aspirin for viral infections." The link between aspirin use and Reye''s Syndrome has not been confirmed, but evidence suggests that the risk is sufficiently grave to include the warning on aspirin products. 16. The nurse is caring for a client with a new order for bupropion (Wellbutrin) for treatment of depression. The order reads “Wellbutrin 175 mg. BID x 4 days.” What is the appropriate action? A) Give the medication as ordered B) Question this medication dose C) Observe the client for mood swings D) Monitor neuro signs frequently B: Question this medication dose. Bupropion (Wellbutrin) should be started at 100mg BID for three days then increased to 150mg BID. When used for depression, it may take up to four weeks for results. Common side effects are dry mouth, headache, and agitation. Doses should be administered in equally spaced time increments throughout the day to minimize the risk of seizures. 17. A 3 year-old child has tympanostomy tubes in place. The child's parent asks the nurse if he can swim in the family pool. The best response from the nurse is A) "Your child should not swim at all while the tubes are in place." B) "Your child may swim in your own pool but not in a lake or ocean." C) "Your child may swim if he wears ear plugs." D) "Your child may swim anywhere." C: "Your child may swim if he wears ear plugs." Water should not enter the ears. Children should use ear plugs when bathing or swimming and should not put their heads under the water. 7018. A nurse has administered several blood transfusions over 3 days to a 12 year-old client with Thalassemia. What lab value should the nurse monitor closely during this therapy? A) Hemoglobin B) Red Blood Cell Indices C) Platelet count D) Neutrophil percent A: Hemoglobin should be in a therapeutic range of approximately 10 g/dl (100gL). "This level is low enough to foster the patient''s own erythropoiesis without enlarging the spleen." (Lewis, p. 744) 19. The nurse is explaining the effects of cocaine abuse to a pregnant client. Which of the following must the nurse understand as a basis for teaching? A) Cocaine use can cause fetal growth retardation B) The drug has been linked to neural tube defects C) Newborn withdrawal generally occurs immediately after birth D) Breast feeding promotes positive parenting behaviors A: Cocaine use can cause fetal growth retardation. Cocaine is vasoconstrictive, and this effect in the placental vessels causes fetal hypoxia and diminished growth. Other risks of continued cocaine use during pregnancy include preterm labor, congenital abnormalities, altered brain development and subsequent behavioral problems in the infant. 20. The feeling of trust can best be established by the nurse during the process of the development of a nurse-client relationship by which of these characteristics? A) Reliability and kindness B) Demeanor and sincerity C) Honesty and consistency D) Sympathy and appreciativeness C: Honesty and consistency. Characteristics of a trusting relationship include respect, honesty, consistency, faith and caring. 21. A client is receiving and IV antibiotic infusion and is scheduled to have blood drawn at 1:00 pm for a "peak" antibiotic level measurement. The nurse notes that the IV infusion is running behind schedule and will not be competed by 1:00. The nurse should: A) Notify the client's health care provider B) Stop the infusion at 1:00 pm C) Reschedule the laboratory test D) Increase the infusion rate C: Reschedule the laboratory test. If the antibiotic infusion will not be completed at the time the peak blood level is due to be drawn, the nurse should ask that the blood sampling time be adjusted 22. A 52 year-old post menopausal woman asks the nurse how frequently she should have a mammogram. What is the nurse's best response? A) "Your doctor will advise you about your risks." B) "Unless you had previous problems, every 2 years is best." C) "Once a woman reaches 50, she should have a mammogram yearly." D) "Yearly mammograms are advised for all women over 35." C: "Once a woman reaches 50, she should have a mammogram yearly." The American Cancer Society recommends a screening mammogram by age 40, every 1 - 2 years for women 40-49, and every year from age 50. If there are family or personal health risks, other assessments may be recommended. 23. In discharge teaching, the nurse should emphasize that which of these is a common side effect of clozapine (Clozaril) therapy? A) Dry mouth B) Rhinitis C) Dry skin D) Extreme salivation D: Extreme salivation. A significant number of clients receiving Clozapine (Clozaril) therapy experience extreme salivation. 24. A client was admitted to the psychiatric unit for severe depression. After several days, the client continues to withdraw from the other clients. Which of these statements by the nurse would be the most appropriate to promote interaction with other clients? A) "Your team here thinks it's good for you to spend time with others. B) "It is important for you to participate in group activities." C) "Come with me so you can paint a picture to help you feel better." D) "Come play Chinese Checkers with Gloria and me." D: This gradually engages the client in interactions with others in small groups rather than large groups. In addition, focusing on an activity is less anxiety-provoking than unstructured discussion. The statement is an example of a positive behavioral expectation. 7125. The mother of a 4 month-old infant asks the nurse about the dangers of sunburn while they are on vacation at the beach. Which of the following is the best advice about sun protection for this child? A) "Use a sunscreen with a minimum sun protective factor of 15." B) "Applications of sunscreen should be repeated every few hours." C) "An infant should be protected by the maximum strength sunscreen." D) "Sunscreens are not recommended in children younger than 6 months." D: Infants under 6 months of age should be kept out of the sun or shielded from it. Even on a cloudy day, the infant can be sunburned while near water. A hat and light protective clothing should be worn. 26. A client has had a positive reaction to purified protein derivative (PPD). The client asks the nurse what this means. The nurse should indicate that the client has A) active tuberculosis B) been exposed to mycobacterium tuberculosis C) never had tuberculosis D) never been infected with mycobacterium tuberculosis B: been exposed to mycobacterium tuberculosis. The PPD skin test is used to determine the presence of tuberculosis antibodies and a positive result indicates that the person has been exposed to mycobacterium tuberculosis. Additional tests are needed to determine if active tuberculosis is present. 27. The nurse administers cimetidine (Tagamet) to a 79 year-old male with a gastric ulcer. Which parameter may be affected by this drug, and should be closely monitored by the nurse? A) Blood pressure B) Liver function C) Mental status D) Hemoglobin C: Mental status. The elderly are at risk for developing confusion when taking cimetidine, a drug that interacts with many other medications. 28. A 9 year-old is taken to the emergency room with right lower quadrant pain and vomiting. When preparing the child for an emergency appendectomy, what must the nurse expect to be the child's greatest fear? A) Change in body image B) An unfamiliar environment C) Perceived loss of control D) Guilt over being hospitalized C: Perceived loss of control. For school age children, major fears are loss of control and separation from friends/peers. 29. The nurse is planning care for a client who is taking cyclosporin (Neoral). What would be an appropriate nursing diagnosis for this client? A) Alteration in body image B) High risk for infection C) Altered growth and development D) Impaired physical mobility B: Cyclosporin (Neoral) inhibits normal immune responses. Clients receiving cyclosporin are at risk for infection. 30. A client with paranoid thoughts refuses to eat because of the belief that the food is poisoned. The appropriate statement at this time for the nurse to say is A) "Here, I will pour a little of the juice in a medicine cup to drink it to show you that it is OK." B) "The food has been prepared in our kitchen and is not poisoned." C) "Let's see if your partner could bring food from home." D) "If you don't eat, I will have to suggest for you to be tube fed." C: Reassurance is ineffective when a client is actively delusional. This option avoids both arguing with the client and agreeing with the delusional premise. Option D offers a logical response to a primarily affective concern. When the client’s condition has improved, gentle negation of the delusional premise can be employed. 31. A client has many delusions. As the nurse helps the client prepare for breakfast the client comments "Don’t waste good food on me. I’m dying from this disease I have." The appropriate response would be A) "You need some nutritious food to help you regain your weight." B) "None of the laboratory reports show that you have any physical disease." C) "Try to eat a little bit, breakfast is the most important meal of the day." D) "I know you believe that you have an incurable disease." D: This response does not challenge the client’s delusional system and thus forms an alliance by providing reassurance of desire to help the client. 32. A client tells the RN she has decided to stop taking sertraline (Zoloft) because she doesn’t like the nightmares, sex dreams, and obsessions she’s experiencing since starting on the medication. What is an appropriate response by the nurse? 72A) "It is unsafe to abruptly stop taking any prescribed medication." B) "Side effects and benefits should be discussed with your health care provider." C) "This medication should be continued despite unpleasant symptoms." D) "Many medications have potential side effects." A: Abrupt withdrawal may occasionally cause serotonin syndrome, consisting of lethargy, nausea, headache, fever, sweating and chills. A slow withdrawal may be prescribed with sertraline to avoid dizziness, nausea, vomiting, and diarrhea. 33. The nurse is beginning nutritional counseling/teaching with a pregnant woman. What is the initial step in this interaction? ********************************** CONTINUED IN THE ATTACHMENT *********************************** [Show More]
Last updated: 1 year ago
Preview 1 out of 171 pages
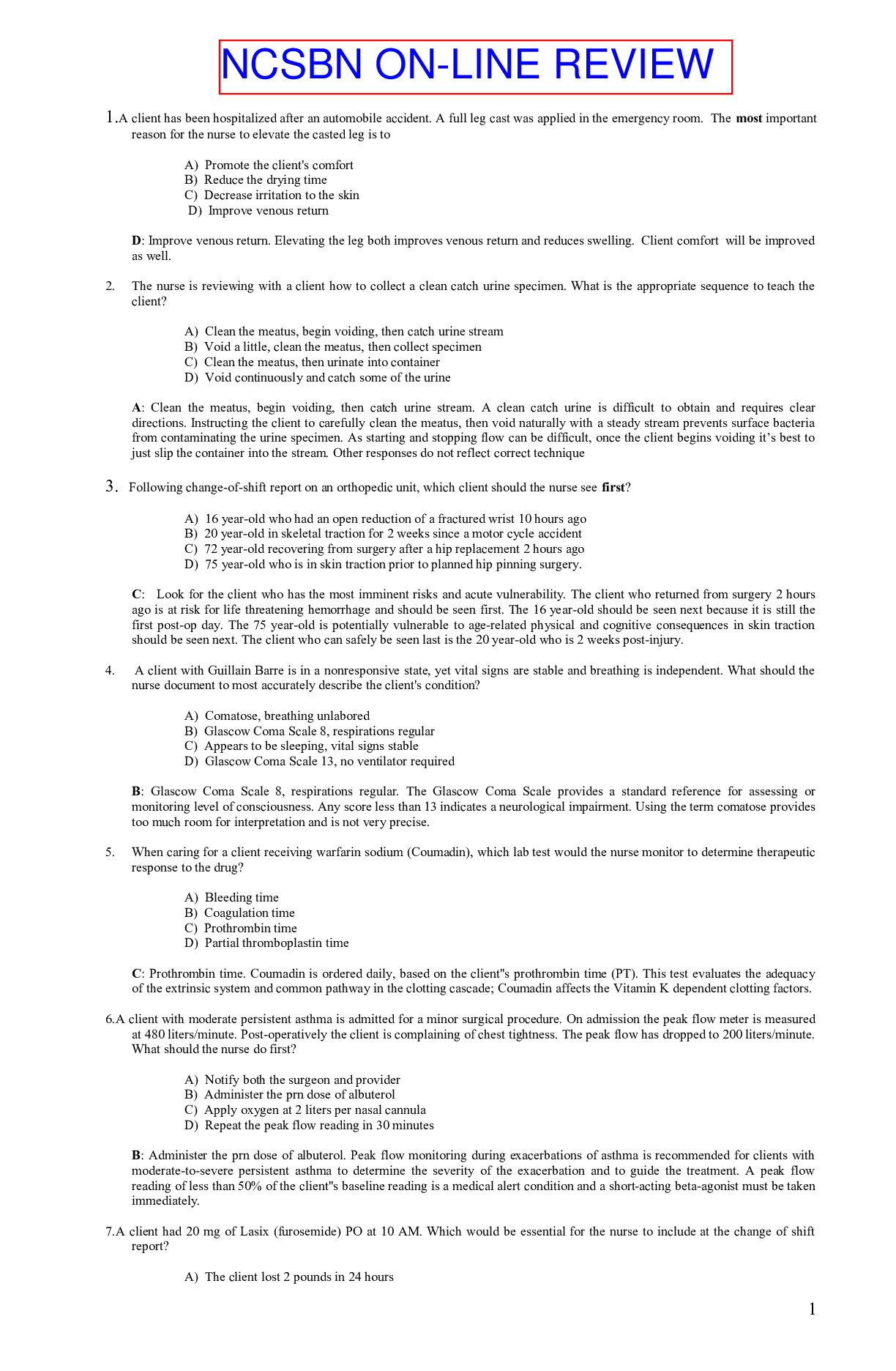
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Mar 26, 2021
Number of pages
171
Written in
Additional information
This document has been written for:
Uploaded
Mar 26, 2021
Downloads
0
Views
51

.png)